User login
Aggressive Glycemic Control Not Beneficial in Diabetic CABG Patients
Aggressive glycemic control in diabetic patients undergoing coronary artery bypass graft surgery resulted in a sharp upswing in hypoglycemic events while providing no advantage in clinical cardiovascular outcomes, compared with moderate control, according to a randomized, controlled trial.
The impetus for this trial was the fact that the optimal blood glucose level in diabetic patients undergoing CABG surgery isn’t known, according to Dr. Harold L. Lazar. The Society of Thoracic Surgeons recommends that blood glucose be kept below 180 mg/dL during cardiac surgery and afterwards in the ICU (Ann. Thorac. Surg. 2009;87:663-9).
This recommendation is based on solid evidence of benefit; for example, a previous study by Dr. Lazar and his coworkers showed that maintaining blood glucose in the 120-180 mg/dL range in diabetic CABG patients resulted in less atrial fibrillation, fewer sternal wound infections, shorter hospital stays, better left ventricular function, and increased 5-year survival, compared with diabetic patients whose blood glucose was greater than 180 mg/dL (Circulation 2004;109:1497-502).
However, there have subsequently been conflicting reports as to whether maintaining blood glucose levels even lower (below 120 mg/dL) provides added benefit or might actually be harmful.
In the current study, 82 CABG patients with diabetes were randomized to moderate glycemic control if they had a blood glucose level of 120-180 mg/dL, or aggressive control if they had a blood glucose of 90-120 mg/dL. Levels were maintained using continuous intravenous insulin solutions, starting at the induction of anesthesia and continuing for 18 hours after surgery. All patients were on standard cardioprotective medications, including a beta-blocker, statin, and aspirin.
The moderate-control group achieved a mean blood glucose of 135 mg/dL, compared with 103 mg/dL in the tight-control group, Dr. Lazar said at the annual meeting of the American Surgical Association, where he presented the study results.
The primary end point was the 30-day rate of major adverse events, a composite that included death, MI, cerebrovascular accidents, atrial fibrillation, and deep sternal infections. The rate was 40% in the moderate-control group and 35% with aggressive glycemic control, a nonsignificant difference. Rates of each of the individual components of the composite end point were similar in the two groups as well. Nor did the two study arms differ significantly in secondary end points, including time on the ventilator, weight gain, need for inotropic support, or length of hospital or ICU stay, said Dr. Lazar of Boston Medical Center.
One or more hypoglycemic events were experienced by 10% of the moderate-control group vs. 75% of the aggressively managed group, although none of these episodes resulted in a neurologic event.
There was a trend for serum free fatty acid levels (a surrogate marker for a systemic inflammatory response) to be lower in the aggressive-control group than in the moderate-control group when they were measured 18 hours postoperatively.
Audience members questioned whether the 82-patient trial was powered sufficiently to draw firm conclusions regarding major adverse cardiovascular event rates. Dr. Lazar agreed that this is a legitimate concern. He said long-term follow-up of the study participants is planned to determine whether the lower free fatty acid levels in the aggressive glycemic control group will eventually be reflected in better graft patency and fewer ischemic events.
Dr. Lazar declared having no financial conflicts.
Aggressive glycemic control in diabetic patients undergoing coronary artery bypass graft surgery resulted in a sharp upswing in hypoglycemic events while providing no advantage in clinical cardiovascular outcomes, compared with moderate control, according to a randomized, controlled trial.
The impetus for this trial was the fact that the optimal blood glucose level in diabetic patients undergoing CABG surgery isn’t known, according to Dr. Harold L. Lazar. The Society of Thoracic Surgeons recommends that blood glucose be kept below 180 mg/dL during cardiac surgery and afterwards in the ICU (Ann. Thorac. Surg. 2009;87:663-9).
This recommendation is based on solid evidence of benefit; for example, a previous study by Dr. Lazar and his coworkers showed that maintaining blood glucose in the 120-180 mg/dL range in diabetic CABG patients resulted in less atrial fibrillation, fewer sternal wound infections, shorter hospital stays, better left ventricular function, and increased 5-year survival, compared with diabetic patients whose blood glucose was greater than 180 mg/dL (Circulation 2004;109:1497-502).
However, there have subsequently been conflicting reports as to whether maintaining blood glucose levels even lower (below 120 mg/dL) provides added benefit or might actually be harmful.
In the current study, 82 CABG patients with diabetes were randomized to moderate glycemic control if they had a blood glucose level of 120-180 mg/dL, or aggressive control if they had a blood glucose of 90-120 mg/dL. Levels were maintained using continuous intravenous insulin solutions, starting at the induction of anesthesia and continuing for 18 hours after surgery. All patients were on standard cardioprotective medications, including a beta-blocker, statin, and aspirin.
The moderate-control group achieved a mean blood glucose of 135 mg/dL, compared with 103 mg/dL in the tight-control group, Dr. Lazar said at the annual meeting of the American Surgical Association, where he presented the study results.
The primary end point was the 30-day rate of major adverse events, a composite that included death, MI, cerebrovascular accidents, atrial fibrillation, and deep sternal infections. The rate was 40% in the moderate-control group and 35% with aggressive glycemic control, a nonsignificant difference. Rates of each of the individual components of the composite end point were similar in the two groups as well. Nor did the two study arms differ significantly in secondary end points, including time on the ventilator, weight gain, need for inotropic support, or length of hospital or ICU stay, said Dr. Lazar of Boston Medical Center.
One or more hypoglycemic events were experienced by 10% of the moderate-control group vs. 75% of the aggressively managed group, although none of these episodes resulted in a neurologic event.
There was a trend for serum free fatty acid levels (a surrogate marker for a systemic inflammatory response) to be lower in the aggressive-control group than in the moderate-control group when they were measured 18 hours postoperatively.
Audience members questioned whether the 82-patient trial was powered sufficiently to draw firm conclusions regarding major adverse cardiovascular event rates. Dr. Lazar agreed that this is a legitimate concern. He said long-term follow-up of the study participants is planned to determine whether the lower free fatty acid levels in the aggressive glycemic control group will eventually be reflected in better graft patency and fewer ischemic events.
Dr. Lazar declared having no financial conflicts.
Aggressive glycemic control in diabetic patients undergoing coronary artery bypass graft surgery resulted in a sharp upswing in hypoglycemic events while providing no advantage in clinical cardiovascular outcomes, compared with moderate control, according to a randomized, controlled trial.
The impetus for this trial was the fact that the optimal blood glucose level in diabetic patients undergoing CABG surgery isn’t known, according to Dr. Harold L. Lazar. The Society of Thoracic Surgeons recommends that blood glucose be kept below 180 mg/dL during cardiac surgery and afterwards in the ICU (Ann. Thorac. Surg. 2009;87:663-9).
This recommendation is based on solid evidence of benefit; for example, a previous study by Dr. Lazar and his coworkers showed that maintaining blood glucose in the 120-180 mg/dL range in diabetic CABG patients resulted in less atrial fibrillation, fewer sternal wound infections, shorter hospital stays, better left ventricular function, and increased 5-year survival, compared with diabetic patients whose blood glucose was greater than 180 mg/dL (Circulation 2004;109:1497-502).
However, there have subsequently been conflicting reports as to whether maintaining blood glucose levels even lower (below 120 mg/dL) provides added benefit or might actually be harmful.
In the current study, 82 CABG patients with diabetes were randomized to moderate glycemic control if they had a blood glucose level of 120-180 mg/dL, or aggressive control if they had a blood glucose of 90-120 mg/dL. Levels were maintained using continuous intravenous insulin solutions, starting at the induction of anesthesia and continuing for 18 hours after surgery. All patients were on standard cardioprotective medications, including a beta-blocker, statin, and aspirin.
The moderate-control group achieved a mean blood glucose of 135 mg/dL, compared with 103 mg/dL in the tight-control group, Dr. Lazar said at the annual meeting of the American Surgical Association, where he presented the study results.
The primary end point was the 30-day rate of major adverse events, a composite that included death, MI, cerebrovascular accidents, atrial fibrillation, and deep sternal infections. The rate was 40% in the moderate-control group and 35% with aggressive glycemic control, a nonsignificant difference. Rates of each of the individual components of the composite end point were similar in the two groups as well. Nor did the two study arms differ significantly in secondary end points, including time on the ventilator, weight gain, need for inotropic support, or length of hospital or ICU stay, said Dr. Lazar of Boston Medical Center.
One or more hypoglycemic events were experienced by 10% of the moderate-control group vs. 75% of the aggressively managed group, although none of these episodes resulted in a neurologic event.
There was a trend for serum free fatty acid levels (a surrogate marker for a systemic inflammatory response) to be lower in the aggressive-control group than in the moderate-control group when they were measured 18 hours postoperatively.
Audience members questioned whether the 82-patient trial was powered sufficiently to draw firm conclusions regarding major adverse cardiovascular event rates. Dr. Lazar agreed that this is a legitimate concern. He said long-term follow-up of the study participants is planned to determine whether the lower free fatty acid levels in the aggressive glycemic control group will eventually be reflected in better graft patency and fewer ischemic events.
Dr. Lazar declared having no financial conflicts.
Major Finding: Diabetic patients whose blood glucose level was maintained at 90-120 mg/dL during CABG and for 18 hours afterwards had more hypoglycemic events but no significant reduction in major adverse cardiovascular events, compared with those randomized to a level of 120-180 mg/dL.
Data Source: A randomized, controlled trial of 82 patients.
Disclosures: Dr. Lazar declared having no financial conflicts.
Trauma Capillary Leak Syndrome Carries High Mortality
Traumatic-induced capillary leak syndrome is the name being given to a newly described, highly lethal disease process in critically injured trauma patients. As yet, there is no effective treatment, but some studies have been conducted to better understand its characteristics, with an eye toward ultimately finding a way to prevent it.
Traumatic-induced capillary leak syndrome (TICS) is characterized by acute hypotension, hemoconcentration, and shock, but its chief hallmark is hypoalbuminemia within 2 hours of the injury. The lower the serum albumin at that time, the worse the patient’s prognosis – independent of all the standard predictors. The prognosis is somewhat modified, however, if the serum albumin rises during the next 3 days, said Dr. Grant Bochicchio of the University of Maryland, Baltimore.
In a study of more than 1,000 critically injured trauma patients, Dr. Bochicchio reported that a serum albumin level below 2.6 mg/dL was associated with increased morbidity and mortality (Am. Surg. 2004;70:1099-102). His new prospective study, which he presented at the annual meeting of the American Surgical Association, included a different cohort of 2,348 trauma patients admitted to the ICU, all with a serum albumin measurement obtained within 2 hours post-injury and monitored over the next 7 days.
In all, 79% of the patients had blunt trauma injuries. Their mean age was 43 years, with an ISS (Injury Severity Score) of 27 and an APACHE (Acute Physiology and Chronic Health Evaluation) II score of 13. The mean initial serum albumin level was 2.9 mg/dL. TICS was graded on a 1-5 scale, with grade 1 being an initial serum albumin below 1.0 mg/dL, and grade 5 being a normal serum albumin of 3.5 mg/dL or more.
There were 84 patients with grade 1 TICS. They had an overall 70% mortality. Moreover, patients with grade 1 TICS had a 91% mortality rate if their serum albumin failed to improve by more than 50% over the next 72 hours, reported Dr. Bochicchio.
Patients with TICS grade 1 were significantly older and had higher ISS and APACHE II scores than did those with a normal albumin level. This was true as well for the 409 patients with TICS grade 2 (that is, an initial serum albumin of 1.0-1.99 mg/dL).
In a multivariate logistic regression analysis adjusted for age, APACHE II score, ISS, and sex, patients who were TICS grade 1 or 2 spent an average of 9 more days on a ventilator, 11 more days in the ICU, and 12 more days in the hospital, and they had a 10-fold greater risk of mortality than did the 732 grade 5 patients.
The majority of deaths in TICS grade 1 or 2 patients resulted from multisystem organ failure.
In all, 777 infections were diagnosed in the study population during the first week. The infection rate was 62% in patients with grade 1 TICS, 50% with grade 2, and 12% with grade 3 (that is, an initial serum albumin of 2.0-2.6 mg/dL), compared with just 5% in grade 5 patients.
Dr. Bochicchio said that his research focus is shifting to TICS prevention. Toward this end, he’ll be taking a close look at inflammatory markers and seeking a means to reduce the amount of fluid that TICS patients typically require. He hopes that prevention will prove to be more fruitful than the various attempts at treatment to date.
"Every study I’ve seen shows that administering exogenous albumin actually increases mortality," he noted.
Several discussants questioned whether the association Dr. Bochicchio has documented between low serum albumin and increased morbidity and mortality in critically injured trauma patients is actually causal.
"If you’re injured and older, you tend to present with a lower albumin. You’re calling it the traumatic-induced capillary leak syndrome, but my hypothesis would be that those patients are actually getting more fluid and bleeding more: You bleed more, you get more fluid, and you end up with a lower albumin. What this study may really be showing us is [that] aggressive resuscitation may be killing people; it may have nothing to do with the capillary leak syndrome," contended Dr. Martin A. Schreiber, professor of surgery at Oregon Health and Science University, Portland.
Dr. Bochicchio replied that patients with severe TICS didn’t get more fluid before arriving at the hospital than did other trauma patients, although after reaching the hospital, they did.
Dr. Bochicchio declared having no financial conflicts of interest.
Traumatic-induced capillary leak syndrome is the name being given to a newly described, highly lethal disease process in critically injured trauma patients. As yet, there is no effective treatment, but some studies have been conducted to better understand its characteristics, with an eye toward ultimately finding a way to prevent it.
Traumatic-induced capillary leak syndrome (TICS) is characterized by acute hypotension, hemoconcentration, and shock, but its chief hallmark is hypoalbuminemia within 2 hours of the injury. The lower the serum albumin at that time, the worse the patient’s prognosis – independent of all the standard predictors. The prognosis is somewhat modified, however, if the serum albumin rises during the next 3 days, said Dr. Grant Bochicchio of the University of Maryland, Baltimore.
In a study of more than 1,000 critically injured trauma patients, Dr. Bochicchio reported that a serum albumin level below 2.6 mg/dL was associated with increased morbidity and mortality (Am. Surg. 2004;70:1099-102). His new prospective study, which he presented at the annual meeting of the American Surgical Association, included a different cohort of 2,348 trauma patients admitted to the ICU, all with a serum albumin measurement obtained within 2 hours post-injury and monitored over the next 7 days.
In all, 79% of the patients had blunt trauma injuries. Their mean age was 43 years, with an ISS (Injury Severity Score) of 27 and an APACHE (Acute Physiology and Chronic Health Evaluation) II score of 13. The mean initial serum albumin level was 2.9 mg/dL. TICS was graded on a 1-5 scale, with grade 1 being an initial serum albumin below 1.0 mg/dL, and grade 5 being a normal serum albumin of 3.5 mg/dL or more.
There were 84 patients with grade 1 TICS. They had an overall 70% mortality. Moreover, patients with grade 1 TICS had a 91% mortality rate if their serum albumin failed to improve by more than 50% over the next 72 hours, reported Dr. Bochicchio.
Patients with TICS grade 1 were significantly older and had higher ISS and APACHE II scores than did those with a normal albumin level. This was true as well for the 409 patients with TICS grade 2 (that is, an initial serum albumin of 1.0-1.99 mg/dL).
In a multivariate logistic regression analysis adjusted for age, APACHE II score, ISS, and sex, patients who were TICS grade 1 or 2 spent an average of 9 more days on a ventilator, 11 more days in the ICU, and 12 more days in the hospital, and they had a 10-fold greater risk of mortality than did the 732 grade 5 patients.
The majority of deaths in TICS grade 1 or 2 patients resulted from multisystem organ failure.
In all, 777 infections were diagnosed in the study population during the first week. The infection rate was 62% in patients with grade 1 TICS, 50% with grade 2, and 12% with grade 3 (that is, an initial serum albumin of 2.0-2.6 mg/dL), compared with just 5% in grade 5 patients.
Dr. Bochicchio said that his research focus is shifting to TICS prevention. Toward this end, he’ll be taking a close look at inflammatory markers and seeking a means to reduce the amount of fluid that TICS patients typically require. He hopes that prevention will prove to be more fruitful than the various attempts at treatment to date.
"Every study I’ve seen shows that administering exogenous albumin actually increases mortality," he noted.
Several discussants questioned whether the association Dr. Bochicchio has documented between low serum albumin and increased morbidity and mortality in critically injured trauma patients is actually causal.
"If you’re injured and older, you tend to present with a lower albumin. You’re calling it the traumatic-induced capillary leak syndrome, but my hypothesis would be that those patients are actually getting more fluid and bleeding more: You bleed more, you get more fluid, and you end up with a lower albumin. What this study may really be showing us is [that] aggressive resuscitation may be killing people; it may have nothing to do with the capillary leak syndrome," contended Dr. Martin A. Schreiber, professor of surgery at Oregon Health and Science University, Portland.
Dr. Bochicchio replied that patients with severe TICS didn’t get more fluid before arriving at the hospital than did other trauma patients, although after reaching the hospital, they did.
Dr. Bochicchio declared having no financial conflicts of interest.
Traumatic-induced capillary leak syndrome is the name being given to a newly described, highly lethal disease process in critically injured trauma patients. As yet, there is no effective treatment, but some studies have been conducted to better understand its characteristics, with an eye toward ultimately finding a way to prevent it.
Traumatic-induced capillary leak syndrome (TICS) is characterized by acute hypotension, hemoconcentration, and shock, but its chief hallmark is hypoalbuminemia within 2 hours of the injury. The lower the serum albumin at that time, the worse the patient’s prognosis – independent of all the standard predictors. The prognosis is somewhat modified, however, if the serum albumin rises during the next 3 days, said Dr. Grant Bochicchio of the University of Maryland, Baltimore.
In a study of more than 1,000 critically injured trauma patients, Dr. Bochicchio reported that a serum albumin level below 2.6 mg/dL was associated with increased morbidity and mortality (Am. Surg. 2004;70:1099-102). His new prospective study, which he presented at the annual meeting of the American Surgical Association, included a different cohort of 2,348 trauma patients admitted to the ICU, all with a serum albumin measurement obtained within 2 hours post-injury and monitored over the next 7 days.
In all, 79% of the patients had blunt trauma injuries. Their mean age was 43 years, with an ISS (Injury Severity Score) of 27 and an APACHE (Acute Physiology and Chronic Health Evaluation) II score of 13. The mean initial serum albumin level was 2.9 mg/dL. TICS was graded on a 1-5 scale, with grade 1 being an initial serum albumin below 1.0 mg/dL, and grade 5 being a normal serum albumin of 3.5 mg/dL or more.
There were 84 patients with grade 1 TICS. They had an overall 70% mortality. Moreover, patients with grade 1 TICS had a 91% mortality rate if their serum albumin failed to improve by more than 50% over the next 72 hours, reported Dr. Bochicchio.
Patients with TICS grade 1 were significantly older and had higher ISS and APACHE II scores than did those with a normal albumin level. This was true as well for the 409 patients with TICS grade 2 (that is, an initial serum albumin of 1.0-1.99 mg/dL).
In a multivariate logistic regression analysis adjusted for age, APACHE II score, ISS, and sex, patients who were TICS grade 1 or 2 spent an average of 9 more days on a ventilator, 11 more days in the ICU, and 12 more days in the hospital, and they had a 10-fold greater risk of mortality than did the 732 grade 5 patients.
The majority of deaths in TICS grade 1 or 2 patients resulted from multisystem organ failure.
In all, 777 infections were diagnosed in the study population during the first week. The infection rate was 62% in patients with grade 1 TICS, 50% with grade 2, and 12% with grade 3 (that is, an initial serum albumin of 2.0-2.6 mg/dL), compared with just 5% in grade 5 patients.
Dr. Bochicchio said that his research focus is shifting to TICS prevention. Toward this end, he’ll be taking a close look at inflammatory markers and seeking a means to reduce the amount of fluid that TICS patients typically require. He hopes that prevention will prove to be more fruitful than the various attempts at treatment to date.
"Every study I’ve seen shows that administering exogenous albumin actually increases mortality," he noted.
Several discussants questioned whether the association Dr. Bochicchio has documented between low serum albumin and increased morbidity and mortality in critically injured trauma patients is actually causal.
"If you’re injured and older, you tend to present with a lower albumin. You’re calling it the traumatic-induced capillary leak syndrome, but my hypothesis would be that those patients are actually getting more fluid and bleeding more: You bleed more, you get more fluid, and you end up with a lower albumin. What this study may really be showing us is [that] aggressive resuscitation may be killing people; it may have nothing to do with the capillary leak syndrome," contended Dr. Martin A. Schreiber, professor of surgery at Oregon Health and Science University, Portland.
Dr. Bochicchio replied that patients with severe TICS didn’t get more fluid before arriving at the hospital than did other trauma patients, although after reaching the hospital, they did.
Dr. Bochicchio declared having no financial conflicts of interest.
Laparoscopic Sleeve Gastrectomy Appears Safe in Major Observational Study
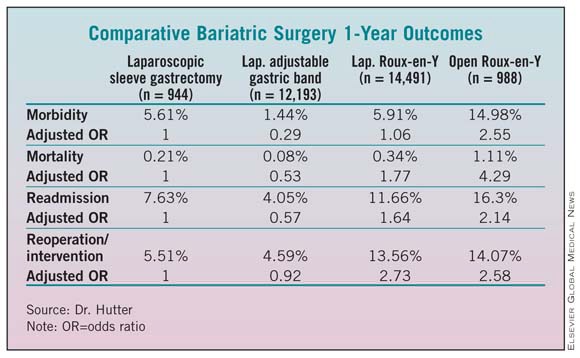
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Laparoscopic Sleeve Gastrectomy Appears Safe in Major Observational Study
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Data Source: An analysis of 1-year outcomes for 944 laparoscopic sleeve gastrectomy patients, 12,193 laparoscopic adjustable gastric band patients, 14,491 laparoscopic Roux-en-Y gastric bypass patients, and 988 open Roux-en-Y gastric bypass patients.
Disclosures: Dr. Hutter reported having no relevant financial conflicts.
Laparoscopic Sleeve Gastrectomy Appears Safe in Major Observational Study
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.
|
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Data Source: An analysis of 1-year outcomes for 944 laparoscopic sleeve gastrectomy patients, 12,193 laparoscopic adjustable gastric band patients, 14,491 laparoscopic Roux-en-Y gastric bypass patients, and 988 open Roux-en-Y gastric bypass patients.
Disclosures: Dr. Hutter reported having no relevant financial conflicts.
Risk Scores Define Likely Liver Retransplant Failure
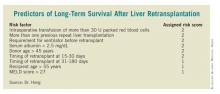
BOCA RATON, FLA. — A new risk-stratification formula provides a practical means of predicting long-term survival likelihood after liver retransplantation for a failing allograft.
For the 22% of liver transplant recipients who develop graft failure, retransplantation offers the only salvage therapy. This new risk-scoring system can help to optimize utilization of a scarce resource by identifying a substantial patient subgroup for whom liver retransplantation is likely to be futile, Dr. Johnny C. Hong said at the annual meeting of the American Surgical Association.
Liver transplantation has become increasingly challenging in the last decade. Not only has the gap between donor organ supply and demand grown larger, but lately the donor organs are more often compromised in quality. Donors have become older and more obese, and often they have died of cardiac disease – all of which makes for a suboptimal liver for purposes of transplantation, noted Dr. Hong of the University of California, Los Angeles.
He presented a predictive index derived by analysis of the 466 liver retransplantations performed in 426 adult recipients at UCLA over the past 26 years. The recipients had a mean age of 49 years. In all, 90% of them had one prior liver transplant. The median interval between the previous transplant and retransplantation was 20 days. One-third of the patients required urgent retransplantation, and 56% were on mechanical ventilation prior to repeat transplantation. The median MELD (Model for End-Stage Liver Disease) score was 30, reflecting the high degree of acuity of their illness.
Multivariate analysis of more than 20 recipient, donor, and operative variables identified 8 independent predictors of retransplant graft failure. Each of these eight predictors was associated with a 20%-90% increased risk. Dr. Hong and his coworkers assigned each predictor a risk score of 1 or 2 based on its predictive strength. (See box.)
The 101 liver retransplants in the high-risk category (based on a total predictive score of 5-12 points) had a 5-year graft failure–free survival rate of only 20%. In contrast, this rate was 47% among the 335 intermediate-risk patients having a score of 1-4, and 65% in the 30 low-risk patients who had a score of 0.
The 5-year overall survival followed the same pattern (22% in the high-risk group, 53% in those at intermediate risk, and 79% in the small low-risk group).
Sepsis was the No. 1 cause of graft failure after repeat liver transplantation, accounting for 46% of the 272 cases, followed by recurrent disease (14%). Of note, despite the technical complexity of repeat transplantation surgery, vascular and biliary complications accounted for only 7% and 5% of graft failures, respectively.
Some 40% of repeat liver transplant recipients had recurrent hepatitis C. A notable finding was that their survival rate was no different from that of recipients without hepatitis C infection, Dr. Hong observed.
Discussant Dr. John Fung, chairman of the Digestive Disease Institute at the Cleveland Clinic Foundation, congratulated Dr. Hong on presenting the largest-ever, single-center patient series on repeat liver transplantation. He wondered whether the predictive model might be enhanced by the elimination of intraoperative transfusion information and donor age from the equation, instead focusing entirely on the recipient factors. The reason for this proposal is that intraoperative blood loss can’t really be predicted at the time the transplant team is deciding whether to go ahead with retransplantation, and the donor age may not be known, either.
Dr. Hong replied that the formula would still work. For example, a patient with a history of more than one prior liver retransplant who requires mechanical ventilation, who has a MELD score greater than 27 and a serum albumin below 2.5 mg/dL, and who needs another liver 15-180 days after the prior transplant would have a risk score of 8, squarely within the high-risk category.
Dr. Hong declared having no financial conflicts.
BOCA RATON, FLA. — A new risk-stratification formula provides a practical means of predicting long-term survival likelihood after liver retransplantation for a failing allograft.
For the 22% of liver transplant recipients who develop graft failure, retransplantation offers the only salvage therapy. This new risk-scoring system can help to optimize utilization of a scarce resource by identifying a substantial patient subgroup for whom liver retransplantation is likely to be futile, Dr. Johnny C. Hong said at the annual meeting of the American Surgical Association.
Liver transplantation has become increasingly challenging in the last decade. Not only has the gap between donor organ supply and demand grown larger, but lately the donor organs are more often compromised in quality. Donors have become older and more obese, and often they have died of cardiac disease – all of which makes for a suboptimal liver for purposes of transplantation, noted Dr. Hong of the University of California, Los Angeles.
He presented a predictive index derived by analysis of the 466 liver retransplantations performed in 426 adult recipients at UCLA over the past 26 years. The recipients had a mean age of 49 years. In all, 90% of them had one prior liver transplant. The median interval between the previous transplant and retransplantation was 20 days. One-third of the patients required urgent retransplantation, and 56% were on mechanical ventilation prior to repeat transplantation. The median MELD (Model for End-Stage Liver Disease) score was 30, reflecting the high degree of acuity of their illness.
Multivariate analysis of more than 20 recipient, donor, and operative variables identified 8 independent predictors of retransplant graft failure. Each of these eight predictors was associated with a 20%-90% increased risk. Dr. Hong and his coworkers assigned each predictor a risk score of 1 or 2 based on its predictive strength. (See box.)
The 101 liver retransplants in the high-risk category (based on a total predictive score of 5-12 points) had a 5-year graft failure–free survival rate of only 20%. In contrast, this rate was 47% among the 335 intermediate-risk patients having a score of 1-4, and 65% in the 30 low-risk patients who had a score of 0.
The 5-year overall survival followed the same pattern (22% in the high-risk group, 53% in those at intermediate risk, and 79% in the small low-risk group).
Sepsis was the No. 1 cause of graft failure after repeat liver transplantation, accounting for 46% of the 272 cases, followed by recurrent disease (14%). Of note, despite the technical complexity of repeat transplantation surgery, vascular and biliary complications accounted for only 7% and 5% of graft failures, respectively.
Some 40% of repeat liver transplant recipients had recurrent hepatitis C. A notable finding was that their survival rate was no different from that of recipients without hepatitis C infection, Dr. Hong observed.
Discussant Dr. John Fung, chairman of the Digestive Disease Institute at the Cleveland Clinic Foundation, congratulated Dr. Hong on presenting the largest-ever, single-center patient series on repeat liver transplantation. He wondered whether the predictive model might be enhanced by the elimination of intraoperative transfusion information and donor age from the equation, instead focusing entirely on the recipient factors. The reason for this proposal is that intraoperative blood loss can’t really be predicted at the time the transplant team is deciding whether to go ahead with retransplantation, and the donor age may not be known, either.
Dr. Hong replied that the formula would still work. For example, a patient with a history of more than one prior liver retransplant who requires mechanical ventilation, who has a MELD score greater than 27 and a serum albumin below 2.5 mg/dL, and who needs another liver 15-180 days after the prior transplant would have a risk score of 8, squarely within the high-risk category.
Dr. Hong declared having no financial conflicts.
BOCA RATON, FLA. — A new risk-stratification formula provides a practical means of predicting long-term survival likelihood after liver retransplantation for a failing allograft.
For the 22% of liver transplant recipients who develop graft failure, retransplantation offers the only salvage therapy. This new risk-scoring system can help to optimize utilization of a scarce resource by identifying a substantial patient subgroup for whom liver retransplantation is likely to be futile, Dr. Johnny C. Hong said at the annual meeting of the American Surgical Association.
Liver transplantation has become increasingly challenging in the last decade. Not only has the gap between donor organ supply and demand grown larger, but lately the donor organs are more often compromised in quality. Donors have become older and more obese, and often they have died of cardiac disease – all of which makes for a suboptimal liver for purposes of transplantation, noted Dr. Hong of the University of California, Los Angeles.
He presented a predictive index derived by analysis of the 466 liver retransplantations performed in 426 adult recipients at UCLA over the past 26 years. The recipients had a mean age of 49 years. In all, 90% of them had one prior liver transplant. The median interval between the previous transplant and retransplantation was 20 days. One-third of the patients required urgent retransplantation, and 56% were on mechanical ventilation prior to repeat transplantation. The median MELD (Model for End-Stage Liver Disease) score was 30, reflecting the high degree of acuity of their illness.
Multivariate analysis of more than 20 recipient, donor, and operative variables identified 8 independent predictors of retransplant graft failure. Each of these eight predictors was associated with a 20%-90% increased risk. Dr. Hong and his coworkers assigned each predictor a risk score of 1 or 2 based on its predictive strength. (See box.)
The 101 liver retransplants in the high-risk category (based on a total predictive score of 5-12 points) had a 5-year graft failure–free survival rate of only 20%. In contrast, this rate was 47% among the 335 intermediate-risk patients having a score of 1-4, and 65% in the 30 low-risk patients who had a score of 0.
The 5-year overall survival followed the same pattern (22% in the high-risk group, 53% in those at intermediate risk, and 79% in the small low-risk group).
Sepsis was the No. 1 cause of graft failure after repeat liver transplantation, accounting for 46% of the 272 cases, followed by recurrent disease (14%). Of note, despite the technical complexity of repeat transplantation surgery, vascular and biliary complications accounted for only 7% and 5% of graft failures, respectively.
Some 40% of repeat liver transplant recipients had recurrent hepatitis C. A notable finding was that their survival rate was no different from that of recipients without hepatitis C infection, Dr. Hong observed.
Discussant Dr. John Fung, chairman of the Digestive Disease Institute at the Cleveland Clinic Foundation, congratulated Dr. Hong on presenting the largest-ever, single-center patient series on repeat liver transplantation. He wondered whether the predictive model might be enhanced by the elimination of intraoperative transfusion information and donor age from the equation, instead focusing entirely on the recipient factors. The reason for this proposal is that intraoperative blood loss can’t really be predicted at the time the transplant team is deciding whether to go ahead with retransplantation, and the donor age may not be known, either.
Dr. Hong replied that the formula would still work. For example, a patient with a history of more than one prior liver retransplant who requires mechanical ventilation, who has a MELD score greater than 27 and a serum albumin below 2.5 mg/dL, and who needs another liver 15-180 days after the prior transplant would have a risk score of 8, squarely within the high-risk category.
Dr. Hong declared having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: Eight independent predictors of liver retransplant graft failure were identified based on recipient, donor, and operative variables, and each was associated with a 20%-90% increased risk.
Data Source: Analysis of the 466 liver retransplantations performed in 426 adult recipients at UCLA over the past 26 years.
Disclosures: Dr. Hong declared having no financial conflicts.
Data Analysis Favors Laparoscopic Abdominal Wall Hernia Repair
BOCA RATON, FLA. – Laparoscopic repair of anterior abdominal wall hernia was associated with significantly less morbidity, a shorter hospitalization stay, and lower mortality than was open repair in a study of more than 71,000 patients in the American College of Surgeons’ National Surgical Quality Improvement Program database.
"Laparoscopic repair is underutilized," Dr. Rodney J. Mason said, noting that only 17% of the repairs in the study were performed laparoscopically.
The laparoscopic and open-repair patients were quite different in terms of baseline characteristics, so he and his coinvestigators performed two separate analyses of the NSQIP data. The first incorporated the full 71,026 patients; a second matched-pair analysis involved a subgroup comprising 7,060 open-repair patients and 7,069 similar patients with laparoscopic repair, Dr. Mason explained at the annual meeting of the American Surgical Association.
He and his colleagues turned to the NSQIP database because adverse-event rates associated with anterior abdominal wall hernia repair are so low that a definitive, randomized, controlled trial would require more than 100,000 patients in each study arm, according to Dr. Mason of the University of Southern California in Los Angeles.
In the matched-pair analysis, the 30-day overall morbidity rate was significantly lower in the laparoscopic repair group (2.83%) than in the patients undergoing open repair (5.14%). The serious complication rate was also significantly less (0.99% vs. 1.71% with open repair). Pulmonary embolism, sepsis, wound infection, and urinary tract infection were among the serious complications that were significantly less frequent with laparoscopic repair. In contrast, 30-day mortality rates weren’t significantly different (0.08% with laparoscopic and 0.06% with open repair).
However, in the full analysis of 71,026 patients, mortality was significantly lower in the laparoscopic repair group at 0.18%, which was roughly half the 0.33% rate with open repair. Similarly, the laparoscopic repair group’s 1.57% serious complication rate was significantly better than the 2.54% rate with open repair. Overall complication rates were 3.8% for laparoscopic repair vs. 6.02% for open repair.
Overall and serious morbidity rates were significantly lower with laparoscopic repair of nearly all types of abdominal wall hernias, including umbilical, incisional, ventral, incarcerated, strangulated, recurrent, and reducible hernias. In fact, the only setting in which there was no significant difference in complications between the two surgical approaches was in repair of initial primary hernias.
The average length of hospital stay was 2.71 days with laparoscopic repair in the matched-pair comparison – significantly shorter than the 3.36 days with open repair. The margin of difference was larger in the full analysis (3.25 days with laparoscopic vs. 4.43 days for open repair).
The new analysis of NSQIP data is particularly timely in light of a recent Cochrane review that concluded that laparoscopic repair hasn’t been shown to be superior to open repair in terms of complications, Dr. Mason observed (Cochrane Database Syst. Rev. 2011 [doi:10.1002/14651858.CD007781.pub2]).
Discussant Dr. Hobart W. Harris commented that with more than 400,000 incisional and ventral hernia repairs being performed annually, the incidence of this problem rivals that of acute appendicitis. Yet to date, no standardized hernia classification systems or evidence-based treatment guidelines exist.
"This is a common yet inadequately studied condition that adds several billion dollars to our annual health care expenditures," said Dr. Harris, professor of surgery and chief of the division of general surgery at the University of California, San Francisco.
He offered some tough love for Dr. Mason and his coinvestigators: "Enthusiasm must not overshadow the evidence or lack thereof. Due to the limitations of the ACS NSQIP data, my respected colleagues are unable to comment on postoperative pain or recovery time, let alone operating room time or costs, or – perhaps most importantly – the recurrence rates for the two techniques," Dr. Harris pointed out.
Although the NSQIP analysis demonstrated statistically significant differences favoring laparoscopic repair, these differences are arguably too small to be clinically meaningful, in his view.
"In the absence of equivalent or superior long-term recurrence rate data, I fear that the jury is still out. And I am not alone in that view, given that only one in five of these hernias were repaired using laparoscopic techniques," Dr. Harris said.
Dr. John M. Kellum Jr. cautioned Dr. Mason against making sweeping declarations regarding the superiority of laparoscopic repair.
"I have a concern that the message from your study will be that if you don’t do a laparoscopic incisional hernia repair, you’re lacking in testosterone," said Dr. Kellum, professor of surgery at Virginia Commonwealth University, Richmond.
Dr. Kellum said that he likes doing laparoscopic hernia repairs, but if the CT scan of a large hernia shows significant adhesions of intestine to the abdominal wall, an open repair is probably the best way to go.
Dr. Mason declared having no financial conflicts.
BOCA RATON, FLA. – Laparoscopic repair of anterior abdominal wall hernia was associated with significantly less morbidity, a shorter hospitalization stay, and lower mortality than was open repair in a study of more than 71,000 patients in the American College of Surgeons’ National Surgical Quality Improvement Program database.
"Laparoscopic repair is underutilized," Dr. Rodney J. Mason said, noting that only 17% of the repairs in the study were performed laparoscopically.
The laparoscopic and open-repair patients were quite different in terms of baseline characteristics, so he and his coinvestigators performed two separate analyses of the NSQIP data. The first incorporated the full 71,026 patients; a second matched-pair analysis involved a subgroup comprising 7,060 open-repair patients and 7,069 similar patients with laparoscopic repair, Dr. Mason explained at the annual meeting of the American Surgical Association.
He and his colleagues turned to the NSQIP database because adverse-event rates associated with anterior abdominal wall hernia repair are so low that a definitive, randomized, controlled trial would require more than 100,000 patients in each study arm, according to Dr. Mason of the University of Southern California in Los Angeles.
In the matched-pair analysis, the 30-day overall morbidity rate was significantly lower in the laparoscopic repair group (2.83%) than in the patients undergoing open repair (5.14%). The serious complication rate was also significantly less (0.99% vs. 1.71% with open repair). Pulmonary embolism, sepsis, wound infection, and urinary tract infection were among the serious complications that were significantly less frequent with laparoscopic repair. In contrast, 30-day mortality rates weren’t significantly different (0.08% with laparoscopic and 0.06% with open repair).
However, in the full analysis of 71,026 patients, mortality was significantly lower in the laparoscopic repair group at 0.18%, which was roughly half the 0.33% rate with open repair. Similarly, the laparoscopic repair group’s 1.57% serious complication rate was significantly better than the 2.54% rate with open repair. Overall complication rates were 3.8% for laparoscopic repair vs. 6.02% for open repair.
Overall and serious morbidity rates were significantly lower with laparoscopic repair of nearly all types of abdominal wall hernias, including umbilical, incisional, ventral, incarcerated, strangulated, recurrent, and reducible hernias. In fact, the only setting in which there was no significant difference in complications between the two surgical approaches was in repair of initial primary hernias.
The average length of hospital stay was 2.71 days with laparoscopic repair in the matched-pair comparison – significantly shorter than the 3.36 days with open repair. The margin of difference was larger in the full analysis (3.25 days with laparoscopic vs. 4.43 days for open repair).
The new analysis of NSQIP data is particularly timely in light of a recent Cochrane review that concluded that laparoscopic repair hasn’t been shown to be superior to open repair in terms of complications, Dr. Mason observed (Cochrane Database Syst. Rev. 2011 [doi:10.1002/14651858.CD007781.pub2]).
Discussant Dr. Hobart W. Harris commented that with more than 400,000 incisional and ventral hernia repairs being performed annually, the incidence of this problem rivals that of acute appendicitis. Yet to date, no standardized hernia classification systems or evidence-based treatment guidelines exist.
"This is a common yet inadequately studied condition that adds several billion dollars to our annual health care expenditures," said Dr. Harris, professor of surgery and chief of the division of general surgery at the University of California, San Francisco.
He offered some tough love for Dr. Mason and his coinvestigators: "Enthusiasm must not overshadow the evidence or lack thereof. Due to the limitations of the ACS NSQIP data, my respected colleagues are unable to comment on postoperative pain or recovery time, let alone operating room time or costs, or – perhaps most importantly – the recurrence rates for the two techniques," Dr. Harris pointed out.
Although the NSQIP analysis demonstrated statistically significant differences favoring laparoscopic repair, these differences are arguably too small to be clinically meaningful, in his view.
"In the absence of equivalent or superior long-term recurrence rate data, I fear that the jury is still out. And I am not alone in that view, given that only one in five of these hernias were repaired using laparoscopic techniques," Dr. Harris said.
Dr. John M. Kellum Jr. cautioned Dr. Mason against making sweeping declarations regarding the superiority of laparoscopic repair.
"I have a concern that the message from your study will be that if you don’t do a laparoscopic incisional hernia repair, you’re lacking in testosterone," said Dr. Kellum, professor of surgery at Virginia Commonwealth University, Richmond.
Dr. Kellum said that he likes doing laparoscopic hernia repairs, but if the CT scan of a large hernia shows significant adhesions of intestine to the abdominal wall, an open repair is probably the best way to go.
Dr. Mason declared having no financial conflicts.
BOCA RATON, FLA. – Laparoscopic repair of anterior abdominal wall hernia was associated with significantly less morbidity, a shorter hospitalization stay, and lower mortality than was open repair in a study of more than 71,000 patients in the American College of Surgeons’ National Surgical Quality Improvement Program database.
"Laparoscopic repair is underutilized," Dr. Rodney J. Mason said, noting that only 17% of the repairs in the study were performed laparoscopically.
The laparoscopic and open-repair patients were quite different in terms of baseline characteristics, so he and his coinvestigators performed two separate analyses of the NSQIP data. The first incorporated the full 71,026 patients; a second matched-pair analysis involved a subgroup comprising 7,060 open-repair patients and 7,069 similar patients with laparoscopic repair, Dr. Mason explained at the annual meeting of the American Surgical Association.
He and his colleagues turned to the NSQIP database because adverse-event rates associated with anterior abdominal wall hernia repair are so low that a definitive, randomized, controlled trial would require more than 100,000 patients in each study arm, according to Dr. Mason of the University of Southern California in Los Angeles.
In the matched-pair analysis, the 30-day overall morbidity rate was significantly lower in the laparoscopic repair group (2.83%) than in the patients undergoing open repair (5.14%). The serious complication rate was also significantly less (0.99% vs. 1.71% with open repair). Pulmonary embolism, sepsis, wound infection, and urinary tract infection were among the serious complications that were significantly less frequent with laparoscopic repair. In contrast, 30-day mortality rates weren’t significantly different (0.08% with laparoscopic and 0.06% with open repair).
However, in the full analysis of 71,026 patients, mortality was significantly lower in the laparoscopic repair group at 0.18%, which was roughly half the 0.33% rate with open repair. Similarly, the laparoscopic repair group’s 1.57% serious complication rate was significantly better than the 2.54% rate with open repair. Overall complication rates were 3.8% for laparoscopic repair vs. 6.02% for open repair.
Overall and serious morbidity rates were significantly lower with laparoscopic repair of nearly all types of abdominal wall hernias, including umbilical, incisional, ventral, incarcerated, strangulated, recurrent, and reducible hernias. In fact, the only setting in which there was no significant difference in complications between the two surgical approaches was in repair of initial primary hernias.
The average length of hospital stay was 2.71 days with laparoscopic repair in the matched-pair comparison – significantly shorter than the 3.36 days with open repair. The margin of difference was larger in the full analysis (3.25 days with laparoscopic vs. 4.43 days for open repair).
The new analysis of NSQIP data is particularly timely in light of a recent Cochrane review that concluded that laparoscopic repair hasn’t been shown to be superior to open repair in terms of complications, Dr. Mason observed (Cochrane Database Syst. Rev. 2011 [doi:10.1002/14651858.CD007781.pub2]).
Discussant Dr. Hobart W. Harris commented that with more than 400,000 incisional and ventral hernia repairs being performed annually, the incidence of this problem rivals that of acute appendicitis. Yet to date, no standardized hernia classification systems or evidence-based treatment guidelines exist.
"This is a common yet inadequately studied condition that adds several billion dollars to our annual health care expenditures," said Dr. Harris, professor of surgery and chief of the division of general surgery at the University of California, San Francisco.
He offered some tough love for Dr. Mason and his coinvestigators: "Enthusiasm must not overshadow the evidence or lack thereof. Due to the limitations of the ACS NSQIP data, my respected colleagues are unable to comment on postoperative pain or recovery time, let alone operating room time or costs, or – perhaps most importantly – the recurrence rates for the two techniques," Dr. Harris pointed out.
Although the NSQIP analysis demonstrated statistically significant differences favoring laparoscopic repair, these differences are arguably too small to be clinically meaningful, in his view.
"In the absence of equivalent or superior long-term recurrence rate data, I fear that the jury is still out. And I am not alone in that view, given that only one in five of these hernias were repaired using laparoscopic techniques," Dr. Harris said.
Dr. John M. Kellum Jr. cautioned Dr. Mason against making sweeping declarations regarding the superiority of laparoscopic repair.
"I have a concern that the message from your study will be that if you don’t do a laparoscopic incisional hernia repair, you’re lacking in testosterone," said Dr. Kellum, professor of surgery at Virginia Commonwealth University, Richmond.
Dr. Kellum said that he likes doing laparoscopic hernia repairs, but if the CT scan of a large hernia shows significant adhesions of intestine to the abdominal wall, an open repair is probably the best way to go.
Dr. Mason declared having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: The 0.18% mortality rate in the group having laparoscopic abdominal wall hernia repair was roughly half the 0.33% mortality rate in patients undergoing open repair. Complication and morbidity rates were also lower in the laparoscopic group.
Data Source: Database analysis of 71,026 patients.
Disclosures: Dr. Mason declared having no financial conflicts.
Aortic Dissection Repair: Tight BP Control Avoids Late Reoperation
BOCA RATON, FLA. – Beta-blocker therapy and strict, lifelong control of hypertension are key to avoiding late reoperation after repair of acute type A aortic dissection, according to a large, 25-year, single-center follow-up study.
Operative mortality was 16% among 252 patients who underwent repair of acute type A aortic dissection at the hands of 26 surgeons at Barnes-Jewish Hospital in St. Louis during 1984-2009. Of 28 variables that were scrutinized in a multivariate analysis, only one proved to be an independent risk factor for operative mortality: branch vessel malperfusion at presentation, with an associated 2.5-fold increased risk, Dr. Spencer J. Melby reported at the annual meeting of the American Surgical Association.
Some 27 of 211 operative survivors required 30 late reoperations. Four variables were independently predictive of late reoperation: male sex, Marfan syndrome, not being on a beta-blocker at last follow-up, and systolic blood pressure (SBP) greater than 120 mm Hg, according to Dr. Melby of Washington University in St. Louis.
The rates of freedom from reoperation among patients on beta-blocker therapy at 10 and 15 years were 86% and 83%, respectively, compared with 57% and 37% in patients who were not on the medication.
Patients who maintained their SBP below 120 mm Hg had 10- and 15-year rates of freedom from reoperation of 92%. Among those whose SBP was 120-140 mm Hg, the rates were 74% and 66%. In patients who maintained SBP in excess of 140 mm Hg, the 10- and 15-year rates of freedom from reoperation was 49% and 30%.
In terms of perfusion techniques that were utilized in the initial repair, 35% of patients were placed on an aortic cross-clamp only, 30% had hypothermic cardiac arrest with retrograde cerebral perfusion, and 35% got hypothermic cardiac arrest without retrograde cerebral perfusion.
Importantly, long-term survival was not related to operative approach. Late survival was decreased, however, in patients with previous stroke or chronic renal insufficiency.
Discussant Dr. Thoralf M. Sundt III noted that although acute aortic dissection is an uncommon condition, it is nonetheless the most common fatal catastrophe of the aorta. Multiple studies over the years indicate that not much progress has been made in improving the high perioperative and long-term morbidity and mortality.
"We don’t seem to be learning very much over time. It’s not getting better. So a study such as this one that can impact the long-term results in these patients is important," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital, Boston.
He particularly welcomed Dr. Melby’s emphasis on lifelong beta-blocker therapy.
"It may seem a bit odd for surgeons to be focusing on pharmacologic treatment, but in fact aortic disease is really a disease that’s most often treated by surgeons. There are few medical vascular specialists, and so it really is important for us to follow these patients. This is a chronic condition, and we ought to adopt a posture towards that condition where we are responsible for caring for these patients over time," according to the surgeon.
Dr. Sundt noted that many surgeons have adopted as dogma that these repairs should be done under hypothermic circulatory arrest rather than cross-clamp. "Your group is bucking the trend," he commented.
Dr. Melby agreed that hypothermic cardiac arrest is "trendy." Some surgeons at Barnes-Jewish use it routinely. But in the study, the risk of reoperation for bleeding was 17% in patients who were managed via hypothermic cardiac arrest, compared with 7% with cross-clamp. Cardiopulmonary bypass time was about 30 minutes shorter with the cross-clamp.
"One of the conclusions of our paper is that because we found [that] long-term outcomes were independent of the technique, it’s safe to say that surgeons should treat this problem in the way they’re most comfortable," he added.
Dr. Melby said that he has no relevant financial interests.
BOCA RATON, FLA. – Beta-blocker therapy and strict, lifelong control of hypertension are key to avoiding late reoperation after repair of acute type A aortic dissection, according to a large, 25-year, single-center follow-up study.
Operative mortality was 16% among 252 patients who underwent repair of acute type A aortic dissection at the hands of 26 surgeons at Barnes-Jewish Hospital in St. Louis during 1984-2009. Of 28 variables that were scrutinized in a multivariate analysis, only one proved to be an independent risk factor for operative mortality: branch vessel malperfusion at presentation, with an associated 2.5-fold increased risk, Dr. Spencer J. Melby reported at the annual meeting of the American Surgical Association.
Some 27 of 211 operative survivors required 30 late reoperations. Four variables were independently predictive of late reoperation: male sex, Marfan syndrome, not being on a beta-blocker at last follow-up, and systolic blood pressure (SBP) greater than 120 mm Hg, according to Dr. Melby of Washington University in St. Louis.
The rates of freedom from reoperation among patients on beta-blocker therapy at 10 and 15 years were 86% and 83%, respectively, compared with 57% and 37% in patients who were not on the medication.
Patients who maintained their SBP below 120 mm Hg had 10- and 15-year rates of freedom from reoperation of 92%. Among those whose SBP was 120-140 mm Hg, the rates were 74% and 66%. In patients who maintained SBP in excess of 140 mm Hg, the 10- and 15-year rates of freedom from reoperation was 49% and 30%.
In terms of perfusion techniques that were utilized in the initial repair, 35% of patients were placed on an aortic cross-clamp only, 30% had hypothermic cardiac arrest with retrograde cerebral perfusion, and 35% got hypothermic cardiac arrest without retrograde cerebral perfusion.
Importantly, long-term survival was not related to operative approach. Late survival was decreased, however, in patients with previous stroke or chronic renal insufficiency.
Discussant Dr. Thoralf M. Sundt III noted that although acute aortic dissection is an uncommon condition, it is nonetheless the most common fatal catastrophe of the aorta. Multiple studies over the years indicate that not much progress has been made in improving the high perioperative and long-term morbidity and mortality.
"We don’t seem to be learning very much over time. It’s not getting better. So a study such as this one that can impact the long-term results in these patients is important," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital, Boston.
He particularly welcomed Dr. Melby’s emphasis on lifelong beta-blocker therapy.
"It may seem a bit odd for surgeons to be focusing on pharmacologic treatment, but in fact aortic disease is really a disease that’s most often treated by surgeons. There are few medical vascular specialists, and so it really is important for us to follow these patients. This is a chronic condition, and we ought to adopt a posture towards that condition where we are responsible for caring for these patients over time," according to the surgeon.
Dr. Sundt noted that many surgeons have adopted as dogma that these repairs should be done under hypothermic circulatory arrest rather than cross-clamp. "Your group is bucking the trend," he commented.
Dr. Melby agreed that hypothermic cardiac arrest is "trendy." Some surgeons at Barnes-Jewish use it routinely. But in the study, the risk of reoperation for bleeding was 17% in patients who were managed via hypothermic cardiac arrest, compared with 7% with cross-clamp. Cardiopulmonary bypass time was about 30 minutes shorter with the cross-clamp.
"One of the conclusions of our paper is that because we found [that] long-term outcomes were independent of the technique, it’s safe to say that surgeons should treat this problem in the way they’re most comfortable," he added.
Dr. Melby said that he has no relevant financial interests.
BOCA RATON, FLA. – Beta-blocker therapy and strict, lifelong control of hypertension are key to avoiding late reoperation after repair of acute type A aortic dissection, according to a large, 25-year, single-center follow-up study.
Operative mortality was 16% among 252 patients who underwent repair of acute type A aortic dissection at the hands of 26 surgeons at Barnes-Jewish Hospital in St. Louis during 1984-2009. Of 28 variables that were scrutinized in a multivariate analysis, only one proved to be an independent risk factor for operative mortality: branch vessel malperfusion at presentation, with an associated 2.5-fold increased risk, Dr. Spencer J. Melby reported at the annual meeting of the American Surgical Association.
Some 27 of 211 operative survivors required 30 late reoperations. Four variables were independently predictive of late reoperation: male sex, Marfan syndrome, not being on a beta-blocker at last follow-up, and systolic blood pressure (SBP) greater than 120 mm Hg, according to Dr. Melby of Washington University in St. Louis.
The rates of freedom from reoperation among patients on beta-blocker therapy at 10 and 15 years were 86% and 83%, respectively, compared with 57% and 37% in patients who were not on the medication.
Patients who maintained their SBP below 120 mm Hg had 10- and 15-year rates of freedom from reoperation of 92%. Among those whose SBP was 120-140 mm Hg, the rates were 74% and 66%. In patients who maintained SBP in excess of 140 mm Hg, the 10- and 15-year rates of freedom from reoperation was 49% and 30%.
In terms of perfusion techniques that were utilized in the initial repair, 35% of patients were placed on an aortic cross-clamp only, 30% had hypothermic cardiac arrest with retrograde cerebral perfusion, and 35% got hypothermic cardiac arrest without retrograde cerebral perfusion.
Importantly, long-term survival was not related to operative approach. Late survival was decreased, however, in patients with previous stroke or chronic renal insufficiency.
Discussant Dr. Thoralf M. Sundt III noted that although acute aortic dissection is an uncommon condition, it is nonetheless the most common fatal catastrophe of the aorta. Multiple studies over the years indicate that not much progress has been made in improving the high perioperative and long-term morbidity and mortality.
"We don’t seem to be learning very much over time. It’s not getting better. So a study such as this one that can impact the long-term results in these patients is important," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital, Boston.
He particularly welcomed Dr. Melby’s emphasis on lifelong beta-blocker therapy.
"It may seem a bit odd for surgeons to be focusing on pharmacologic treatment, but in fact aortic disease is really a disease that’s most often treated by surgeons. There are few medical vascular specialists, and so it really is important for us to follow these patients. This is a chronic condition, and we ought to adopt a posture towards that condition where we are responsible for caring for these patients over time," according to the surgeon.
Dr. Sundt noted that many surgeons have adopted as dogma that these repairs should be done under hypothermic circulatory arrest rather than cross-clamp. "Your group is bucking the trend," he commented.
Dr. Melby agreed that hypothermic cardiac arrest is "trendy." Some surgeons at Barnes-Jewish use it routinely. But in the study, the risk of reoperation for bleeding was 17% in patients who were managed via hypothermic cardiac arrest, compared with 7% with cross-clamp. Cardiopulmonary bypass time was about 30 minutes shorter with the cross-clamp.
"One of the conclusions of our paper is that because we found [that] long-term outcomes were independent of the technique, it’s safe to say that surgeons should treat this problem in the way they’re most comfortable," he added.
Dr. Melby said that he has no relevant financial interests.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: The rates of freedom from reoperation after aortic dissection repair among patients on beta-blocker therapy at 10 and 15 years were 86% and 83%, respectively, compared with 57% and 37% in patients not on the medication.
Data Source: A follow-up study of 252 patients who underwent repair of acute type A aortic dissection a single center during 1984-2009.
Disclosures: Dr. Melby said that he has no relevant financial interests.
Aortic Dissection Repair: Tight BP Control Avoids Late Reoperation
BOCA RATON, FLA. – Beta-blocker therapy and strict, lifelong control of hypertension are key to avoiding late reoperation after repair of acute type A aortic dissection, according to a large, 25-year, single-center follow-up study.
Operative mortality was 16% among 252 patients who underwent repair of acute type A aortic dissection at the hands of 26 surgeons at Barnes-Jewish Hospital in St. Louis during 1984-2009. Of 28 variables that were scrutinized in a multivariate analysis, only one proved to be an independent risk factor for operative mortality: branch vessel malperfusion at presentation, with an associated 2.5-fold increased risk, Dr. Spencer J. Melby reported at the annual meeting of the American Surgical Association.
Some 27 of 211 operative survivors required 30 late reoperations. Four variables were independently predictive of late reoperation: male sex, Marfan syndrome, not being on a beta-blocker at last follow-up, and systolic blood pressure (SBP) greater than 120 mm Hg, according to Dr. Melby of Washington University in St. Louis.
The rates of freedom from reoperation among patients on beta-blocker therapy at 10 and 15 years were 86% and 83%, respectively, compared with 57% and 37% in patients who were not on the medication.
Patients who maintained their SBP below 120 mm Hg had 10- and 15-year rates of freedom from reoperation of 92%. Among those whose SBP was 120-140 mm Hg, the rates were 74% and 66%. In patients who maintained SBP in excess of 140 mm Hg, the 10- and 15-year rates of freedom from reoperation was 49% and 30%.
In terms of perfusion techniques that were utilized in the initial repair, 35% of patients were placed on an aortic cross-clamp only, 30% had hypothermic cardiac arrest with retrograde cerebral perfusion, and 35% got hypothermic cardiac arrest without retrograde cerebral perfusion.
Importantly, long-term survival was not related to operative approach. Late survival was decreased, however, in patients with previous stroke or chronic renal insufficiency.
Discussant Dr. Thoralf M. Sundt III noted that although acute aortic dissection is an uncommon condition, it is nonetheless the most common fatal catastrophe of the aorta. Multiple studies over the years indicate that not much progress has been made in improving the high perioperative and long-term morbidity and mortality.
"We don’t seem to be learning very much over time. It’s not getting better. So a study such as this one that can impact the long-term results in these patients is important," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital, Boston.
He particularly welcomed Dr. Melby’s emphasis on lifelong beta-blocker therapy.
"It may seem a bit odd for surgeons to be focusing on pharmacologic treatment, but in fact aortic disease is really a disease that’s most often treated by surgeons. There are few medical vascular specialists, and so it really is important for us to follow these patients. This is a chronic condition, and we ought to adopt a posture towards that condition where we are responsible for caring for these patients over time," according to the surgeon.
Dr. Sundt noted that many surgeons have adopted as dogma that these repairs should be done under hypothermic circulatory arrest rather than cross-clamp. "Your group is bucking the trend," he commented.
Dr. Melby agreed that hypothermic cardiac arrest is "trendy." Some surgeons at Barnes-Jewish use it routinely. But in the study, the risk of reoperation for bleeding was 17% in patients who were managed via hypothermic cardiac arrest, compared with 7% with cross-clamp. Cardiopulmonary bypass time was about 30 minutes shorter with the cross-clamp.
"One of the conclusions of our paper is that because we found [that] long-term outcomes were independent of the technique, it’s safe to say that surgeons should treat this problem in the way they’re most comfortable," he added.
Dr. Melby said that he has no relevant financial interests.
Spencer J. Melby
Body text goes here
Doctor’s Bio
Body text goes here
Doctor’s Bio
Body text goes here
Doctor’s Bio
BOCA RATON, FLA. – Beta-blocker therapy and strict, lifelong control of hypertension are key to avoiding late reoperation after repair of acute type A aortic dissection, according to a large, 25-year, single-center follow-up study.
Operative mortality was 16% among 252 patients who underwent repair of acute type A aortic dissection at the hands of 26 surgeons at Barnes-Jewish Hospital in St. Louis during 1984-2009. Of 28 variables that were scrutinized in a multivariate analysis, only one proved to be an independent risk factor for operative mortality: branch vessel malperfusion at presentation, with an associated 2.5-fold increased risk, Dr. Spencer J. Melby reported at the annual meeting of the American Surgical Association.
Some 27 of 211 operative survivors required 30 late reoperations. Four variables were independently predictive of late reoperation: male sex, Marfan syndrome, not being on a beta-blocker at last follow-up, and systolic blood pressure (SBP) greater than 120 mm Hg, according to Dr. Melby of Washington University in St. Louis.
The rates of freedom from reoperation among patients on beta-blocker therapy at 10 and 15 years were 86% and 83%, respectively, compared with 57% and 37% in patients who were not on the medication.
Patients who maintained their SBP below 120 mm Hg had 10- and 15-year rates of freedom from reoperation of 92%. Among those whose SBP was 120-140 mm Hg, the rates were 74% and 66%. In patients who maintained SBP in excess of 140 mm Hg, the 10- and 15-year rates of freedom from reoperation was 49% and 30%.
In terms of perfusion techniques that were utilized in the initial repair, 35% of patients were placed on an aortic cross-clamp only, 30% had hypothermic cardiac arrest with retrograde cerebral perfusion, and 35% got hypothermic cardiac arrest without retrograde cerebral perfusion.
Importantly, long-term survival was not related to operative approach. Late survival was decreased, however, in patients with previous stroke or chronic renal insufficiency.
Discussant Dr. Thoralf M. Sundt III noted that although acute aortic dissection is an uncommon condition, it is nonetheless the most common fatal catastrophe of the aorta. Multiple studies over the years indicate that not much progress has been made in improving the high perioperative and long-term morbidity and mortality.
"We don’t seem to be learning very much over time. It’s not getting better. So a study such as this one that can impact the long-term results in these patients is important," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital, Boston.
He particularly welcomed Dr. Melby’s emphasis on lifelong beta-blocker therapy.
"It may seem a bit odd for surgeons to be focusing on pharmacologic treatment, but in fact aortic disease is really a disease that’s most often treated by surgeons. There are few medical vascular specialists, and so it really is important for us to follow these patients. This is a chronic condition, and we ought to adopt a posture towards that condition where we are responsible for caring for these patients over time," according to the surgeon.
Dr. Sundt noted that many surgeons have adopted as dogma that these repairs should be done under hypothermic circulatory arrest rather than cross-clamp. "Your group is bucking the trend," he commented.
Dr. Melby agreed that hypothermic cardiac arrest is "trendy." Some surgeons at Barnes-Jewish use it routinely. But in the study, the risk of reoperation for bleeding was 17% in patients who were managed via hypothermic cardiac arrest, compared with 7% with cross-clamp. Cardiopulmonary bypass time was about 30 minutes shorter with the cross-clamp.
"One of the conclusions of our paper is that because we found [that] long-term outcomes were independent of the technique, it’s safe to say that surgeons should treat this problem in the way they’re most comfortable," he added.
Dr. Melby said that he has no relevant financial interests.
Spencer J. Melby
BOCA RATON, FLA. – Beta-blocker therapy and strict, lifelong control of hypertension are key to avoiding late reoperation after repair of acute type A aortic dissection, according to a large, 25-year, single-center follow-up study.
Operative mortality was 16% among 252 patients who underwent repair of acute type A aortic dissection at the hands of 26 surgeons at Barnes-Jewish Hospital in St. Louis during 1984-2009. Of 28 variables that were scrutinized in a multivariate analysis, only one proved to be an independent risk factor for operative mortality: branch vessel malperfusion at presentation, with an associated 2.5-fold increased risk, Dr. Spencer J. Melby reported at the annual meeting of the American Surgical Association.
Some 27 of 211 operative survivors required 30 late reoperations. Four variables were independently predictive of late reoperation: male sex, Marfan syndrome, not being on a beta-blocker at last follow-up, and systolic blood pressure (SBP) greater than 120 mm Hg, according to Dr. Melby of Washington University in St. Louis.
The rates of freedom from reoperation among patients on beta-blocker therapy at 10 and 15 years were 86% and 83%, respectively, compared with 57% and 37% in patients who were not on the medication.
Patients who maintained their SBP below 120 mm Hg had 10- and 15-year rates of freedom from reoperation of 92%. Among those whose SBP was 120-140 mm Hg, the rates were 74% and 66%. In patients who maintained SBP in excess of 140 mm Hg, the 10- and 15-year rates of freedom from reoperation was 49% and 30%.
In terms of perfusion techniques that were utilized in the initial repair, 35% of patients were placed on an aortic cross-clamp only, 30% had hypothermic cardiac arrest with retrograde cerebral perfusion, and 35% got hypothermic cardiac arrest without retrograde cerebral perfusion.
Importantly, long-term survival was not related to operative approach. Late survival was decreased, however, in patients with previous stroke or chronic renal insufficiency.
Discussant Dr. Thoralf M. Sundt III noted that although acute aortic dissection is an uncommon condition, it is nonetheless the most common fatal catastrophe of the aorta. Multiple studies over the years indicate that not much progress has been made in improving the high perioperative and long-term morbidity and mortality.
"We don’t seem to be learning very much over time. It’s not getting better. So a study such as this one that can impact the long-term results in these patients is important," said Dr. Sundt, chief of cardiac surgery at Massachusetts General Hospital, Boston.
He particularly welcomed Dr. Melby’s emphasis on lifelong beta-blocker therapy.
"It may seem a bit odd for surgeons to be focusing on pharmacologic treatment, but in fact aortic disease is really a disease that’s most often treated by surgeons. There are few medical vascular specialists, and so it really is important for us to follow these patients. This is a chronic condition, and we ought to adopt a posture towards that condition where we are responsible for caring for these patients over time," according to the surgeon.
Dr. Sundt noted that many surgeons have adopted as dogma that these repairs should be done under hypothermic circulatory arrest rather than cross-clamp. "Your group is bucking the trend," he commented.
Dr. Melby agreed that hypothermic cardiac arrest is "trendy." Some surgeons at Barnes-Jewish use it routinely. But in the study, the risk of reoperation for bleeding was 17% in patients who were managed via hypothermic cardiac arrest, compared with 7% with cross-clamp. Cardiopulmonary bypass time was about 30 minutes shorter with the cross-clamp.
"One of the conclusions of our paper is that because we found [that] long-term outcomes were independent of the technique, it’s safe to say that surgeons should treat this problem in the way they’re most comfortable," he added.
Dr. Melby said that he has no relevant financial interests.
Spencer J. Melby
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: The rates of freedom from reoperation after aortic dissection repair among patients on beta-blocker therapy at 10 and 15 years were 86% and 83%, respectively, compared with 57% and 37% in patients not on the medication.
Data Source: A follow-up study of 252 patients who underwent repair of acute type A aortic dissection a single center during 1984-2009.
Disclosures: Dr. Melby said that he has no relevant financial interests.
Bariatric Surgery Risk Scoring Tool May Predict Serious Complications
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION