User login
Allo-HSCT leads to long-term survival in MF
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
HERCULES: Caplacizumab improved platelet response in aTTP
ATLANTA – Adding caplacizumab to standard therapy for acquired thrombotic thrombocytopenic purpura (aTTP) significantly improved platelet response and prevented recurrent episodes in an international, randomized, double-blind, phase 3 placebo-controlled trial.
“Patients were 55% more likely to achieve normalization of platelet count in the caplacizumab group, and this was highly significant,” Marie Scully, MD, said during a late-breaking presentation at the annual meeting of the American Society of Hematology.
“So far, phase 2 and phase 3 studies confirm no deaths in patients treated with caplacizumab,” said Dr. Scully of University College London Hospitals NHS Trust.
Acquired TTP is an acute, life-threatening thrombotic microangiopathy that occurs when inhibitory autoantibodies cause a deficiency of ADAMTS13, an enzyme that cleaves von Willebrand factor (vWF). Inadequate levels of ADAMTS13 activity lead to the formation of ultra-large vWF multimers, platelet strings, and microthrombi. Caplacizumab is a humanized immunoglobulin that helps stop this process by binding the A1 domain of vWF.
“Caplacizumab addresses the pathophysiological platelet aggregation that leads to the formation of microthrombi,” Dr. Scully said.
In this phase 3 trial (HERCULES), 145 patients who had received plasma exchange (PE) at least once for an acute episode of aTTP were randomly assigned to receive caplacizumab or placebo injections plus daily PE and corticosteroids. Caplacizumab (10-mg) therapy consisted of one IV bolus followed by subcutaneous treatment for 30 days. Patients whose ADAMTS13 activity remained below 10% were able to continue treatment for another 28 days, after which all patients were followed for another 28 days without treatment.
At any given time, platelet normalization was 55% more likely with caplacizumab (10 mg) than placebo (platelet normalization rate ratio, 1.55; 95% confidence interval, 1.10-2.20; P less than .01).
Rates of a key combined secondary endpoint – aTTP-related death/recurrence/major thrombotic events – were 12.7% with caplacizumab and 49.3% with placebo (P less than .0001).
Rates of major thrombotic events were 8% in each arm, and deaths were rare overall, meaning that the difference in rates of recurrence drove most of the effect on the combined secondary endpoint. However, patients who received caplacizumab also received 41% less plasma and had 38% fewer days of PE, 65% fewer days in the intensive care unit, and 31% fewer days in the hospital than patients in the placebo arm.
Refractory aTTP affected 4.2% of placebo patients and no caplacizumab patients, which trended toward statistical significance (P = .057). Caplacizumab therapy also led to a faster normalization of several markers of organ damage, including lactate dehydrogenase, cardiac troponin 1, and serum creatinine.
Safety findings reflected earlier-phase studies and caplacizumab’s mechanism of action, Dr. Scully said. Nearly all trial participants experienced at least one treatment-emergent adverse event. Such events led 7% of patients to stop caplacizumab and 12% to stop placebo. Caplacizumab was associated with a range of bleeding-related events, most commonly epistaxis (23.9 vs. 1.4% with placebo), gingival bleeding (11.3% vs. 0%), bruising (7.0% vs. 4.1%), and hematuria (5.6% vs. 1.4%).
Patients in both arms tended to be in their 40s and two-thirds were female. At baseline, about 85% had less than 10% ADAMTS13 activity, and about 40% had severe aTTP (French severity scores of at least 3 or severe neurologic or cardiac involvement).
“Most [66%] patients in the caplacizumab group presented with de novo aTTP, and this is relevant because patients who are in their first episode are much harder to treat,” Dr. Scully said. About half of placebo patients had de novo disease.
In July 2017, caplacizumab received a fast-track designation from the Food and Drug Administration for aTTP after a phase 2 trial showed that platelet counts normalized 39% faster with caplacizumab versus placebo plus standard of care (P = .005). Of eight patients in that study who relapsed within a month of stopping caplacizumab, seven still had less than 10% ADAMTS13 activity, “suggesting unresolved autoimmune activity,” the investigators wrote at the time in the New England Journal of Medicine (2016;374:511-22).
Dr. Scully reported similar findings in the phase 3 HERCULES trial, noting that all patients had ADAMTS13 levels less than 5% on stopping caplacizumab.
Ablynx provided funding for the study. Dr. Scully reported financial relationships with Ablynx, Shire, Novartis, and Alexion.
SOURCE: Scully M et al., ASH 2017 Abstract LBA-1.
ATLANTA – Adding caplacizumab to standard therapy for acquired thrombotic thrombocytopenic purpura (aTTP) significantly improved platelet response and prevented recurrent episodes in an international, randomized, double-blind, phase 3 placebo-controlled trial.
“Patients were 55% more likely to achieve normalization of platelet count in the caplacizumab group, and this was highly significant,” Marie Scully, MD, said during a late-breaking presentation at the annual meeting of the American Society of Hematology.
“So far, phase 2 and phase 3 studies confirm no deaths in patients treated with caplacizumab,” said Dr. Scully of University College London Hospitals NHS Trust.
Acquired TTP is an acute, life-threatening thrombotic microangiopathy that occurs when inhibitory autoantibodies cause a deficiency of ADAMTS13, an enzyme that cleaves von Willebrand factor (vWF). Inadequate levels of ADAMTS13 activity lead to the formation of ultra-large vWF multimers, platelet strings, and microthrombi. Caplacizumab is a humanized immunoglobulin that helps stop this process by binding the A1 domain of vWF.
“Caplacizumab addresses the pathophysiological platelet aggregation that leads to the formation of microthrombi,” Dr. Scully said.
In this phase 3 trial (HERCULES), 145 patients who had received plasma exchange (PE) at least once for an acute episode of aTTP were randomly assigned to receive caplacizumab or placebo injections plus daily PE and corticosteroids. Caplacizumab (10-mg) therapy consisted of one IV bolus followed by subcutaneous treatment for 30 days. Patients whose ADAMTS13 activity remained below 10% were able to continue treatment for another 28 days, after which all patients were followed for another 28 days without treatment.
At any given time, platelet normalization was 55% more likely with caplacizumab (10 mg) than placebo (platelet normalization rate ratio, 1.55; 95% confidence interval, 1.10-2.20; P less than .01).
Rates of a key combined secondary endpoint – aTTP-related death/recurrence/major thrombotic events – were 12.7% with caplacizumab and 49.3% with placebo (P less than .0001).
Rates of major thrombotic events were 8% in each arm, and deaths were rare overall, meaning that the difference in rates of recurrence drove most of the effect on the combined secondary endpoint. However, patients who received caplacizumab also received 41% less plasma and had 38% fewer days of PE, 65% fewer days in the intensive care unit, and 31% fewer days in the hospital than patients in the placebo arm.
Refractory aTTP affected 4.2% of placebo patients and no caplacizumab patients, which trended toward statistical significance (P = .057). Caplacizumab therapy also led to a faster normalization of several markers of organ damage, including lactate dehydrogenase, cardiac troponin 1, and serum creatinine.
Safety findings reflected earlier-phase studies and caplacizumab’s mechanism of action, Dr. Scully said. Nearly all trial participants experienced at least one treatment-emergent adverse event. Such events led 7% of patients to stop caplacizumab and 12% to stop placebo. Caplacizumab was associated with a range of bleeding-related events, most commonly epistaxis (23.9 vs. 1.4% with placebo), gingival bleeding (11.3% vs. 0%), bruising (7.0% vs. 4.1%), and hematuria (5.6% vs. 1.4%).
Patients in both arms tended to be in their 40s and two-thirds were female. At baseline, about 85% had less than 10% ADAMTS13 activity, and about 40% had severe aTTP (French severity scores of at least 3 or severe neurologic or cardiac involvement).
“Most [66%] patients in the caplacizumab group presented with de novo aTTP, and this is relevant because patients who are in their first episode are much harder to treat,” Dr. Scully said. About half of placebo patients had de novo disease.
In July 2017, caplacizumab received a fast-track designation from the Food and Drug Administration for aTTP after a phase 2 trial showed that platelet counts normalized 39% faster with caplacizumab versus placebo plus standard of care (P = .005). Of eight patients in that study who relapsed within a month of stopping caplacizumab, seven still had less than 10% ADAMTS13 activity, “suggesting unresolved autoimmune activity,” the investigators wrote at the time in the New England Journal of Medicine (2016;374:511-22).
Dr. Scully reported similar findings in the phase 3 HERCULES trial, noting that all patients had ADAMTS13 levels less than 5% on stopping caplacizumab.
Ablynx provided funding for the study. Dr. Scully reported financial relationships with Ablynx, Shire, Novartis, and Alexion.
SOURCE: Scully M et al., ASH 2017 Abstract LBA-1.
ATLANTA – Adding caplacizumab to standard therapy for acquired thrombotic thrombocytopenic purpura (aTTP) significantly improved platelet response and prevented recurrent episodes in an international, randomized, double-blind, phase 3 placebo-controlled trial.
“Patients were 55% more likely to achieve normalization of platelet count in the caplacizumab group, and this was highly significant,” Marie Scully, MD, said during a late-breaking presentation at the annual meeting of the American Society of Hematology.
“So far, phase 2 and phase 3 studies confirm no deaths in patients treated with caplacizumab,” said Dr. Scully of University College London Hospitals NHS Trust.
Acquired TTP is an acute, life-threatening thrombotic microangiopathy that occurs when inhibitory autoantibodies cause a deficiency of ADAMTS13, an enzyme that cleaves von Willebrand factor (vWF). Inadequate levels of ADAMTS13 activity lead to the formation of ultra-large vWF multimers, platelet strings, and microthrombi. Caplacizumab is a humanized immunoglobulin that helps stop this process by binding the A1 domain of vWF.
“Caplacizumab addresses the pathophysiological platelet aggregation that leads to the formation of microthrombi,” Dr. Scully said.
In this phase 3 trial (HERCULES), 145 patients who had received plasma exchange (PE) at least once for an acute episode of aTTP were randomly assigned to receive caplacizumab or placebo injections plus daily PE and corticosteroids. Caplacizumab (10-mg) therapy consisted of one IV bolus followed by subcutaneous treatment for 30 days. Patients whose ADAMTS13 activity remained below 10% were able to continue treatment for another 28 days, after which all patients were followed for another 28 days without treatment.
At any given time, platelet normalization was 55% more likely with caplacizumab (10 mg) than placebo (platelet normalization rate ratio, 1.55; 95% confidence interval, 1.10-2.20; P less than .01).
Rates of a key combined secondary endpoint – aTTP-related death/recurrence/major thrombotic events – were 12.7% with caplacizumab and 49.3% with placebo (P less than .0001).
Rates of major thrombotic events were 8% in each arm, and deaths were rare overall, meaning that the difference in rates of recurrence drove most of the effect on the combined secondary endpoint. However, patients who received caplacizumab also received 41% less plasma and had 38% fewer days of PE, 65% fewer days in the intensive care unit, and 31% fewer days in the hospital than patients in the placebo arm.
Refractory aTTP affected 4.2% of placebo patients and no caplacizumab patients, which trended toward statistical significance (P = .057). Caplacizumab therapy also led to a faster normalization of several markers of organ damage, including lactate dehydrogenase, cardiac troponin 1, and serum creatinine.
Safety findings reflected earlier-phase studies and caplacizumab’s mechanism of action, Dr. Scully said. Nearly all trial participants experienced at least one treatment-emergent adverse event. Such events led 7% of patients to stop caplacizumab and 12% to stop placebo. Caplacizumab was associated with a range of bleeding-related events, most commonly epistaxis (23.9 vs. 1.4% with placebo), gingival bleeding (11.3% vs. 0%), bruising (7.0% vs. 4.1%), and hematuria (5.6% vs. 1.4%).
Patients in both arms tended to be in their 40s and two-thirds were female. At baseline, about 85% had less than 10% ADAMTS13 activity, and about 40% had severe aTTP (French severity scores of at least 3 or severe neurologic or cardiac involvement).
“Most [66%] patients in the caplacizumab group presented with de novo aTTP, and this is relevant because patients who are in their first episode are much harder to treat,” Dr. Scully said. About half of placebo patients had de novo disease.
In July 2017, caplacizumab received a fast-track designation from the Food and Drug Administration for aTTP after a phase 2 trial showed that platelet counts normalized 39% faster with caplacizumab versus placebo plus standard of care (P = .005). Of eight patients in that study who relapsed within a month of stopping caplacizumab, seven still had less than 10% ADAMTS13 activity, “suggesting unresolved autoimmune activity,” the investigators wrote at the time in the New England Journal of Medicine (2016;374:511-22).
Dr. Scully reported similar findings in the phase 3 HERCULES trial, noting that all patients had ADAMTS13 levels less than 5% on stopping caplacizumab.
Ablynx provided funding for the study. Dr. Scully reported financial relationships with Ablynx, Shire, Novartis, and Alexion.
SOURCE: Scully M et al., ASH 2017 Abstract LBA-1.
REPORTING FROM ASH 2017
Key clinical point:
Major finding: The rate of platelet normalization was 55% faster for caplacizumab vs. placebo plus standard of care (platelet normalization rate ratio, 1.55; P less than .01).
Study details: A randomized double-blind phase 3 trial of 145 patients.
Disclosures: Ablynx provided funding for the study. Dr. Scully reported financial relationships with Ablynx, Shire, Novartis, and Alexion.
Source: Scully M et al. ASH 2017 Abstract LBA-1.
Edoxaban noninferior to dalteparin for VTE in cancer
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
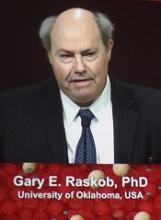
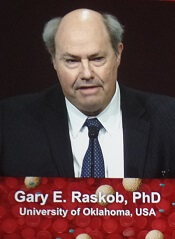
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
ATLANTA—Edoxaban is noninferior to dalteparin for the treatment of cancer-associated venous thromboembolism (VTE), a phase 3 study suggests.
In the Hokusai-VTE CANCER study, patients who received edoxaban had a lower rate of VTE recurrence but a higher rate of major bleeding than patients who received dalteparin.
Rates of VTE recurrence and major bleeding combined were similar between the treatment groups, as were rates of survival free from VTE or major bleeding.
Gary E. Raskob, PhD, of the University of Oklahoma Health Sciences Center in Oklahoma City, presented these results at the 2017 ASH Annual Meeting (LBA-6).
Results were simultaneously published in NEJM. The study was funded by Daiichi Sankyo.
Patients and treatment
Hokusai-VTE CANCER enrolled 1050 adult cancer patients with acute VTE confirmed by imaging. Patients had either active cancer or had been diagnosed with cancer within 2 years from study enrollment. Patients with basal-cell or squamous-cell skin cancer were excluded.
Patients were randomized to receive edoxaban or dalteparin for at least 6 months and up to 12 months.
Edoxaban was given at 60 mg once daily (reduced to 30 mg for patients with creatinine clearance 30-50 mL/min, body weight ≤ 60 kg, or concomitant use of P-glycoprotein inhibitors), following treatment with low-molecular-weight heparin for at least 5 days.
Dalteparin was given at 200 IU/kg once daily for 30 days, then at 150 IU/kg once daily for the remainder of the study.
The median treatment duration was 211 days (interquartile range, 76 to 357) in the edoxaban arm and 184 days (interquartile range, 85 to 341) in the dalteparin arm.
Baseline characteristics were similar between the treatment arms. The median age was 64 in both arms, and about half of patients in each arm were male.
Roughly 98% of patients in each arm had active cancer, 53% had metastatic disease, 29% (dalteparin) and 31% (edoxaban) had recurrent cancer, and 72% (edoxaban) and 73% (dalteparin) had received cancer treatment in the previous 4 weeks.
About 63% of patients in each arm had pulmonary embolism (PE) with or without deep-vein thrombosis (DVT), and 37% had DVT only.
About 18% of patients had 0 risk factors for bleeding, 28% (edoxaban) and 29% (dalteparin) had 1 risk factor, 30% (dalteparin) and 33% (edoxaban) had 2 risk factors, and 21% (edoxaban) and 23% (dalteparin) had 3 or more risk factors for bleeding.
Results
The study’s primary outcome was a composite of first recurrent VTE and major bleeding event during the 12 months after randomization, regardless of treatment duration.
This outcome occurred in 12.8% (67/522) of patients in the edoxaban arm and 13.5% (71/524) of patients in the dalteparin arm. The hazard ratio (HR) with edoxaban was 0.97 (P=0.006 for non-inferiority, P=0.87 for superiority).
“Oral edoxaban is noninferior to subcutaneous dalteparin for the primary outcome of recurrent VTE or major bleeding,” Dr Raskob noted. “The lower rate of recurrent VTE observed with edoxaban was offset by a similar increase in the risk of major bleeding.”
The rate of recurrent VTE during the 12-month study period was 7.9% (n=41) in the edoxaban arm and 11.3% (n=59) in the dalteparin arm (HR=0.71, P=0.09). The rates of recurrent DVT were 3.6% and 6.7%, respectively (HR=0.56), and the rates of recurrent PE were 5.2% and 5.3%, respectively (HR=1.00).
The rate of major bleeding during the 12-month period was 6.9% (n=36) in the edoxaban arm and 4.0% (n=21) in the dalteparin arm (HR=1.77, P=0.04). The rates of clinically relevant nonmajor bleeding were 14.6% and 11.1%, respectively (HR=1.38), and the rates of major or clinically relevant nonmajor bleeding were 18.6% and 13.9%, respectively (HR=1.40).
“There was more upper GI [gastrointestinal] bleeding with edoxaban,” Dr Raskob noted. “It occurred predominantly in patients with GI cancer at the time of entry in the study.”
Death from any cause occurred in 39.5% of patients in the edoxaban arm and 36.6% of patients in the dalteparin arm (HR=1.12).
The rate of event-free survival (absence of recurrent VTE, major bleeding, and death) was 55.0% in the edoxaban arm and 56.5% in the dalteparin arm (HR=0.93).
“The bottom line for patients and oncologists is, ‘Does the patient survive free of these complications?’” Dr Raskob said. “Survival free of recurrent VTE or major bleeding was similar with these regimens.” ![]()
Ruxolitinib improves survival for MF patients in CP-e
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures. ![]()
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures. ![]()
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures. ![]()
CRB-410 update: Multiple myeloma response rates remain high with bb2121 CAR T-cell therapy
ATLANTA – A novel chimeric antigen receptor (CAR) T-cell therapy that targets B-cell maturation antigen showed promising efficacy with a manageable adverse event profile in heavily pretreated patients with relapsed/refractory multiple myeloma in the CRB-410 multicenter phase 1 dose escalation trial.
The product, known as bb2121, received breakthrough therapy designation from the Food and Drug Administration in November 2017 based on preliminary data from the ongoing trial. Those data showed that as of May 2017, the overall response rate at 1 month in 18 evaluable patients was 89%, whereas the response in those who received active dosing (150 x 106 CAR+ T cells or higher) was 100%.
Multiple myeloma currently is “essentially incurable,” and new treatments are desperately needed; B-cell maturation antigen (BCMA) – which is a member of the tumor necrosis factor superfamily that is expressed primarily by malignant myeloma cells, plasma cells, and some mature B cells – is a promising target, said Dr. Kochenderfer of the National Cancer Institute, Bethesda, Md.
The bb2121 product is a second-generation CAR construct targeting BCMA to redirect T cells to multiple myeloma cells. It was tested at doses of 50, 150, 450, and 800 x 106 CAR+ T cells in patients who first underwent chemotherapy as a conditioning regimen to enhance the activity of the CAR T cells.
A total of 24 patients were enrolled, but three had clinical deterioration and were not dosed. The remaining 21 patients had a median age of 58 years, performance scores of 0 or 1, and a median of 5 years since multiple myeloma diagnosis. A high percentage (43%) had high-risk cytogenetics. The median number of prior lines of therapy was seven, and all patients had undergone prior autologous stem cell transplant.
“Generally, this was a very well tolerated CAR T-cell product, especially in comparison to other protocols that I’ve participated in,” he said, noting that the incidence of adverse events, including dose-limiting toxicities, was the primary outcome measure of this phase of the study.
Cytokine release syndrome occurred in 71% of the 21 patients evaluable for response with a median follow-up of 35 weeks at the Oct. 2, 2017, data cutoff, but was grade 3 or greater in just 10% of those patients. Neurological toxicity occurred in 24% of patients, as well, but no cases were grade 3 or above, he said.
“The neurotoxicity was generally much milder and less prevalent than what I’ve seen in previous anti-CD19 CAR studies,” he said.
Neutropenia, thrombocytopenia, and anemia also occurred, but there were no dose-limiting toxicities observed during dose escalation.
Five deaths occurred. Three were due to disease progression and occurred in patients on the lowest dose (50 x 106 CAR+ T cells), which was deemed inactive. The other deaths occurred in patients receiving higher (active) doses; one was a result of myelodysplastic syndrome, and one from cardiac arrest, he said.
One or more serious adverse events occurred in 14 patients, and in some cases were characterized as such due to strict study protocols, Dr. Kochenderfer said.
Of note, one patient out of 12 in an ongoing dose expansion phase of the study, for which data have not yet been fully reported, experienced a delayed onset reversible grade 4 neurological toxicity associated with tumor lysis syndrome and cytokine release syndrome. The patient, who had the highest disease burden in the trial, completely recovered and has obtained a very good partial response despite low BCMA expression on the myeloma cells, Dr. Kochenderfer said.
In terms of response rates, 17 of 18 patients who received doses above 50 x 106 CAR+ T cells had overall responses, and 10 of the 18 achieved complete remission.
The median time to first response was 1 month, and the times to best response and complete response were 3.74 and 3.84 months, respectively. The rates of progression-free survival were 81% at 6 months, and 71% at 9 months, and responses deepened over time: as of May, the complete response rate was 27%, and as of October, it was 56%.
“Five of these patients so far have met the 1-year progression-free survival standard,” Dr. Kochenderfer said, adding that responses have endured for more than a year in several patients. The longest was 68 weeks at the time of the data presentation, and responses continued to improve as late as 15 months, with very good partial remission to complete remission transitions.
The median progression-free survival had not been reached in the active dose cohorts.
“So, in general, very impressive responses compared to my previous experience treating multiple myeloma,” he said.
The findings support the potential of CAR T therapy with bb2121 as a new treatment paradigm in relapsed/refractory multiple myeloma, he concluded, noting that a global pivotal trial of bb2121 (the phase 2 KarMMa trial) is now enrolling and will dose patients at between 150 and 350 x 106 CAR+ T cells. Under the breakthrough therapy designation granted for bb2121, the product will receive expedited review by the FDA.The CRB-410 trial is sponsored by bluebird bio and Celgene. Dr. Kochenderfer reported receiving research funding from bluebird bio and Kite Pharma, and having multiple patents in the CAR field.
ATLANTA – A novel chimeric antigen receptor (CAR) T-cell therapy that targets B-cell maturation antigen showed promising efficacy with a manageable adverse event profile in heavily pretreated patients with relapsed/refractory multiple myeloma in the CRB-410 multicenter phase 1 dose escalation trial.
The product, known as bb2121, received breakthrough therapy designation from the Food and Drug Administration in November 2017 based on preliminary data from the ongoing trial. Those data showed that as of May 2017, the overall response rate at 1 month in 18 evaluable patients was 89%, whereas the response in those who received active dosing (150 x 106 CAR+ T cells or higher) was 100%.
Multiple myeloma currently is “essentially incurable,” and new treatments are desperately needed; B-cell maturation antigen (BCMA) – which is a member of the tumor necrosis factor superfamily that is expressed primarily by malignant myeloma cells, plasma cells, and some mature B cells – is a promising target, said Dr. Kochenderfer of the National Cancer Institute, Bethesda, Md.
The bb2121 product is a second-generation CAR construct targeting BCMA to redirect T cells to multiple myeloma cells. It was tested at doses of 50, 150, 450, and 800 x 106 CAR+ T cells in patients who first underwent chemotherapy as a conditioning regimen to enhance the activity of the CAR T cells.
A total of 24 patients were enrolled, but three had clinical deterioration and were not dosed. The remaining 21 patients had a median age of 58 years, performance scores of 0 or 1, and a median of 5 years since multiple myeloma diagnosis. A high percentage (43%) had high-risk cytogenetics. The median number of prior lines of therapy was seven, and all patients had undergone prior autologous stem cell transplant.
“Generally, this was a very well tolerated CAR T-cell product, especially in comparison to other protocols that I’ve participated in,” he said, noting that the incidence of adverse events, including dose-limiting toxicities, was the primary outcome measure of this phase of the study.
Cytokine release syndrome occurred in 71% of the 21 patients evaluable for response with a median follow-up of 35 weeks at the Oct. 2, 2017, data cutoff, but was grade 3 or greater in just 10% of those patients. Neurological toxicity occurred in 24% of patients, as well, but no cases were grade 3 or above, he said.
“The neurotoxicity was generally much milder and less prevalent than what I’ve seen in previous anti-CD19 CAR studies,” he said.
Neutropenia, thrombocytopenia, and anemia also occurred, but there were no dose-limiting toxicities observed during dose escalation.
Five deaths occurred. Three were due to disease progression and occurred in patients on the lowest dose (50 x 106 CAR+ T cells), which was deemed inactive. The other deaths occurred in patients receiving higher (active) doses; one was a result of myelodysplastic syndrome, and one from cardiac arrest, he said.
One or more serious adverse events occurred in 14 patients, and in some cases were characterized as such due to strict study protocols, Dr. Kochenderfer said.
Of note, one patient out of 12 in an ongoing dose expansion phase of the study, for which data have not yet been fully reported, experienced a delayed onset reversible grade 4 neurological toxicity associated with tumor lysis syndrome and cytokine release syndrome. The patient, who had the highest disease burden in the trial, completely recovered and has obtained a very good partial response despite low BCMA expression on the myeloma cells, Dr. Kochenderfer said.
In terms of response rates, 17 of 18 patients who received doses above 50 x 106 CAR+ T cells had overall responses, and 10 of the 18 achieved complete remission.
The median time to first response was 1 month, and the times to best response and complete response were 3.74 and 3.84 months, respectively. The rates of progression-free survival were 81% at 6 months, and 71% at 9 months, and responses deepened over time: as of May, the complete response rate was 27%, and as of October, it was 56%.
“Five of these patients so far have met the 1-year progression-free survival standard,” Dr. Kochenderfer said, adding that responses have endured for more than a year in several patients. The longest was 68 weeks at the time of the data presentation, and responses continued to improve as late as 15 months, with very good partial remission to complete remission transitions.
The median progression-free survival had not been reached in the active dose cohorts.
“So, in general, very impressive responses compared to my previous experience treating multiple myeloma,” he said.
The findings support the potential of CAR T therapy with bb2121 as a new treatment paradigm in relapsed/refractory multiple myeloma, he concluded, noting that a global pivotal trial of bb2121 (the phase 2 KarMMa trial) is now enrolling and will dose patients at between 150 and 350 x 106 CAR+ T cells. Under the breakthrough therapy designation granted for bb2121, the product will receive expedited review by the FDA.The CRB-410 trial is sponsored by bluebird bio and Celgene. Dr. Kochenderfer reported receiving research funding from bluebird bio and Kite Pharma, and having multiple patents in the CAR field.
ATLANTA – A novel chimeric antigen receptor (CAR) T-cell therapy that targets B-cell maturation antigen showed promising efficacy with a manageable adverse event profile in heavily pretreated patients with relapsed/refractory multiple myeloma in the CRB-410 multicenter phase 1 dose escalation trial.
The product, known as bb2121, received breakthrough therapy designation from the Food and Drug Administration in November 2017 based on preliminary data from the ongoing trial. Those data showed that as of May 2017, the overall response rate at 1 month in 18 evaluable patients was 89%, whereas the response in those who received active dosing (150 x 106 CAR+ T cells or higher) was 100%.
Multiple myeloma currently is “essentially incurable,” and new treatments are desperately needed; B-cell maturation antigen (BCMA) – which is a member of the tumor necrosis factor superfamily that is expressed primarily by malignant myeloma cells, plasma cells, and some mature B cells – is a promising target, said Dr. Kochenderfer of the National Cancer Institute, Bethesda, Md.
The bb2121 product is a second-generation CAR construct targeting BCMA to redirect T cells to multiple myeloma cells. It was tested at doses of 50, 150, 450, and 800 x 106 CAR+ T cells in patients who first underwent chemotherapy as a conditioning regimen to enhance the activity of the CAR T cells.
A total of 24 patients were enrolled, but three had clinical deterioration and were not dosed. The remaining 21 patients had a median age of 58 years, performance scores of 0 or 1, and a median of 5 years since multiple myeloma diagnosis. A high percentage (43%) had high-risk cytogenetics. The median number of prior lines of therapy was seven, and all patients had undergone prior autologous stem cell transplant.
“Generally, this was a very well tolerated CAR T-cell product, especially in comparison to other protocols that I’ve participated in,” he said, noting that the incidence of adverse events, including dose-limiting toxicities, was the primary outcome measure of this phase of the study.
Cytokine release syndrome occurred in 71% of the 21 patients evaluable for response with a median follow-up of 35 weeks at the Oct. 2, 2017, data cutoff, but was grade 3 or greater in just 10% of those patients. Neurological toxicity occurred in 24% of patients, as well, but no cases were grade 3 or above, he said.
“The neurotoxicity was generally much milder and less prevalent than what I’ve seen in previous anti-CD19 CAR studies,” he said.
Neutropenia, thrombocytopenia, and anemia also occurred, but there were no dose-limiting toxicities observed during dose escalation.
Five deaths occurred. Three were due to disease progression and occurred in patients on the lowest dose (50 x 106 CAR+ T cells), which was deemed inactive. The other deaths occurred in patients receiving higher (active) doses; one was a result of myelodysplastic syndrome, and one from cardiac arrest, he said.
One or more serious adverse events occurred in 14 patients, and in some cases were characterized as such due to strict study protocols, Dr. Kochenderfer said.
Of note, one patient out of 12 in an ongoing dose expansion phase of the study, for which data have not yet been fully reported, experienced a delayed onset reversible grade 4 neurological toxicity associated with tumor lysis syndrome and cytokine release syndrome. The patient, who had the highest disease burden in the trial, completely recovered and has obtained a very good partial response despite low BCMA expression on the myeloma cells, Dr. Kochenderfer said.
In terms of response rates, 17 of 18 patients who received doses above 50 x 106 CAR+ T cells had overall responses, and 10 of the 18 achieved complete remission.
The median time to first response was 1 month, and the times to best response and complete response were 3.74 and 3.84 months, respectively. The rates of progression-free survival were 81% at 6 months, and 71% at 9 months, and responses deepened over time: as of May, the complete response rate was 27%, and as of October, it was 56%.
“Five of these patients so far have met the 1-year progression-free survival standard,” Dr. Kochenderfer said, adding that responses have endured for more than a year in several patients. The longest was 68 weeks at the time of the data presentation, and responses continued to improve as late as 15 months, with very good partial remission to complete remission transitions.
The median progression-free survival had not been reached in the active dose cohorts.
“So, in general, very impressive responses compared to my previous experience treating multiple myeloma,” he said.
The findings support the potential of CAR T therapy with bb2121 as a new treatment paradigm in relapsed/refractory multiple myeloma, he concluded, noting that a global pivotal trial of bb2121 (the phase 2 KarMMa trial) is now enrolling and will dose patients at between 150 and 350 x 106 CAR+ T cells. Under the breakthrough therapy designation granted for bb2121, the product will receive expedited review by the FDA.The CRB-410 trial is sponsored by bluebird bio and Celgene. Dr. Kochenderfer reported receiving research funding from bluebird bio and Kite Pharma, and having multiple patents in the CAR field.
REPORTING FROM ASH 2017
Key clinical point:
Major finding: The overall response rate was 94%.
Study details: An update from the phase 1 CRB-410 dose trial of 21 patients.
Disclosures: The CRB-410 trial is sponsored by bluebird bio and Celgene. Dr. Kochenderfer reported receiving research funding from bluebird bio and Kite Pharma, and having multiple patents in the CAR field.
Source: Berdeja J et al. ASH 2017 Abstract 740.
Primary analysis confirms interim findings of CTL019 in DLBCL
ATLANTA—The first chimeric antigen receptor (CAR) T-cell therapy approved in the US to treat children and young adults with leukemia is also producing high response rates in lymphoma, according to investigators of the JULIET trial.
They reported that tisagenlecleucel (formerly CTL019) produced an overall response rate (ORR) of 53% and a complete response (CR) rate of 40% in patients with diffuse large B-cell lymphoma (DLBCL).
Additionally, researchers say the stability in the response rate at 3 and 6 months—38% and 37%, respectively—indicates the durability of the therapy.
At 3 months, 32% of patients who achieved CR remained in CR. At 6 months, 30% remained in CR.
Researchers believe these results confirm the durable clinical benefit reported previously.
Stephen J. Schuster, MD, of the University of Pennsylvania in Philadelphia, presented the JULIET data at the 2017 ASH Annual Meeting (abstract 577).
“Only about half of relapsed diffuse large B-cell lymphoma patients are eligible for transplant,” Dr Schuster said. “[O]f those patients, only about a half respond to salvage chemotherapy, and a significant number of patients relapse post-transplant. So there is really a large unmet need for these patients, and CAR T-cell therapy is a potential agent [for them].”
The JULIET trial was a global, single-arm, phase 2 trial evaluating tisagenlecleucel in DLBCL patients. Tisagenlecleucel (Kymriah™) consists of CAR T cells with a CD19 antigen-binding domain, a 4-1BB costimulatory domain, and a CD3-zeta signaling domain.
The trial was conducted at 27 sites in 10 countries across North America, Europe, Australia, and Asia. There were 2 centralized manufacturing sites, one in Europe and one in the US.
Patients had to be 18 years or older, have had 2 or more prior lines of therapy for DLBCL, and have progressive disease or be ineligible for autologous stem cell transplant (auto-SCT). They could not have had any prior anti-CD19 therapy, and they could not have any central nervous system involvement.
The primary endpoint was best ORR using Lugano criteria with assessment by an independent review committee. Secondary endpoints included duration of response, overall survival (OS), and safety.
Study design and enrollment
Patients were screened and underwent apheresis with cryopreservation of their leukapheresis products during screening, which “allowed for enrollment of all eligible patients,” Dr Schuster said.
Patients could receive bridging chemotherapy while they awaited the manufacture of the CAR T cells.
“What’s important to note is that, early on in the trial, there was a shortage of manufacturing capacity, and this led to a longer-than-anticipated interval between enrollment and treatment,” Dr Schuster said. “This interval decreased as manufacturing capacity improved throughout the trial.”
When their CAR T cells were ready, patients were restaged, lymphodepleted, and received the tisagenlecleucel infusion. The dose ranged from 0.6 x 108 to 6.0 x 108 CAR-positive T cells.
The infusion could be conducted on an inpatient or outpatient basis at the investigator’s discretion, Dr Schuster said.
As of the data cutoff in March 2017, investigators enrolled 147 patients and infused 99 with tisagenlecleucel.
Forty-three patients discontinued before infusion, 9 because of an inability to manufacture the T-cell product and 34 due to death (n=16), physician decision (n=12), patient decision (n=3), adverse event (n=2), and protocol deviation (n=1). Five patients were pending infusion.
There were 81 patients with at least 3 months of follow-up or earlier disease progression evaluable for response.
Patient characteristics
Patients were a median age of 56 (range, 22–76), and 23% were 65 or older. All had an ECOG performance status of 0 or 1, 80% had DLBCL, and 19% had transformed follicular lymphoma.
Fifteen percent had double or triple hits in CMYC, BCL2, and BCL6 genes, and 52% had germinal center B-cell type disease.
Forty-four percent had 2 prior lines of therapy, 31% had 3 prior lines of therapy, and 19% had 4 to 6 prior lines of therapy. All were either refractory to or relapsed from their last therapy.
Forty-seven percent had undergone prior auto-SCT.
Eighty-nine of the 99 patients infused with tisagenlecleucel received bridging therapy, and 92 received lymphodepleting therapy.
Twenty-six patients were infused as outpatients, and 20 remained as outpatients for 3 or more days after the infusion.
Efficacy
The trial met its primary endpoint with an ORR of 53% tested against the null hypothesis of 20% or less. Forty percent of patients achieved a CR, and 14% had a partial response.
The ORR was consistent across all subgroups, including age, sex, lines of prior antineoplastic therapy, cell of origin, and rearranged MYC/BCL2/BCL6.
“The durability of response, however, which is really the message, is shown by the stability between 3- and 6-month response rates, 38% and 37%, respectively,” Dr Schuster said. “The response rate at 3 months is really indicative of the long-term benefit of this treatment approach.”
The investigators observed no apparent relationship between tumor response at month 3 and dose. And they observed responses at all dose levels.
The very early response may be due, to a certain extent, to the chemotherapy, according to Dr Schuster.
“The effect of the T cells becomes evident as you follow these patients over time,” he said.
The median duration of response and overall response have not been reached. And 74% of patients were relapse-free at 6 months.
“Importantly, almost all the complete responders at month 3 remained in complete response,” Dr Schuster said.
Safety
Adverse events of special interest that occurred within 8 weeks of the infusion included:
- Cytokine release syndrome (CRS)—58% all grades, 15% grade 3, 8% grade 4
- Neurologic events—21% all grades, 8% grade 3, 4% grade 4
- Prolonged cytopenia—36% all grades, 15% grade 3, 12% grade 4
- Infections—34% all grades, 18% grade 3, 2% grade 4
- Febrile neutropenia—13% all grades, 11% grade 3, 2% grade 4
No deaths occurred due to tisagenlecleucel, CRS, or cerebral edema.
Fifty-seven patients developed CRS. The median time to onset of CRS was 3 days (range, 1–9), and the median duration of CRS was 7 days (range, 2–30).
Twenty-eight percent of patients developed hypotension that required intervention, 6% requiring high-dose vasopressors. Eight percent were intubated, and 16% received anticytokine therapy—15% with tocilizumab and 11% with corticosteroids.
Investigators did not observe a relationship between dose and neurological events. However, they did detect a higher probability of CRS with the higher doses of tisagenlecleucel.
They also noted that dose and exposure were independent.
Dr Schuster indicated that these data are the basis for global regulatory submissions.
Manufacture of tisagenlecleucel was centralized, and investigators believe the trial shows the feasibility of global distribution of CAR T-cell therapy using cryopreserved apheresis and centralized manufacturing.
Novartis Pharmaceuticals, the sponsor of the trial, is now able to commercially manufacture the CAR T cells in 22 days.
Dr Schuster disclosed research funding and consulting fees from Novartis and Celgene. ![]()
ATLANTA—The first chimeric antigen receptor (CAR) T-cell therapy approved in the US to treat children and young adults with leukemia is also producing high response rates in lymphoma, according to investigators of the JULIET trial.
They reported that tisagenlecleucel (formerly CTL019) produced an overall response rate (ORR) of 53% and a complete response (CR) rate of 40% in patients with diffuse large B-cell lymphoma (DLBCL).
Additionally, researchers say the stability in the response rate at 3 and 6 months—38% and 37%, respectively—indicates the durability of the therapy.
At 3 months, 32% of patients who achieved CR remained in CR. At 6 months, 30% remained in CR.
Researchers believe these results confirm the durable clinical benefit reported previously.
Stephen J. Schuster, MD, of the University of Pennsylvania in Philadelphia, presented the JULIET data at the 2017 ASH Annual Meeting (abstract 577).
“Only about half of relapsed diffuse large B-cell lymphoma patients are eligible for transplant,” Dr Schuster said. “[O]f those patients, only about a half respond to salvage chemotherapy, and a significant number of patients relapse post-transplant. So there is really a large unmet need for these patients, and CAR T-cell therapy is a potential agent [for them].”
The JULIET trial was a global, single-arm, phase 2 trial evaluating tisagenlecleucel in DLBCL patients. Tisagenlecleucel (Kymriah™) consists of CAR T cells with a CD19 antigen-binding domain, a 4-1BB costimulatory domain, and a CD3-zeta signaling domain.
The trial was conducted at 27 sites in 10 countries across North America, Europe, Australia, and Asia. There were 2 centralized manufacturing sites, one in Europe and one in the US.
Patients had to be 18 years or older, have had 2 or more prior lines of therapy for DLBCL, and have progressive disease or be ineligible for autologous stem cell transplant (auto-SCT). They could not have had any prior anti-CD19 therapy, and they could not have any central nervous system involvement.
The primary endpoint was best ORR using Lugano criteria with assessment by an independent review committee. Secondary endpoints included duration of response, overall survival (OS), and safety.
Study design and enrollment
Patients were screened and underwent apheresis with cryopreservation of their leukapheresis products during screening, which “allowed for enrollment of all eligible patients,” Dr Schuster said.
Patients could receive bridging chemotherapy while they awaited the manufacture of the CAR T cells.
“What’s important to note is that, early on in the trial, there was a shortage of manufacturing capacity, and this led to a longer-than-anticipated interval between enrollment and treatment,” Dr Schuster said. “This interval decreased as manufacturing capacity improved throughout the trial.”
When their CAR T cells were ready, patients were restaged, lymphodepleted, and received the tisagenlecleucel infusion. The dose ranged from 0.6 x 108 to 6.0 x 108 CAR-positive T cells.
The infusion could be conducted on an inpatient or outpatient basis at the investigator’s discretion, Dr Schuster said.
As of the data cutoff in March 2017, investigators enrolled 147 patients and infused 99 with tisagenlecleucel.
Forty-three patients discontinued before infusion, 9 because of an inability to manufacture the T-cell product and 34 due to death (n=16), physician decision (n=12), patient decision (n=3), adverse event (n=2), and protocol deviation (n=1). Five patients were pending infusion.
There were 81 patients with at least 3 months of follow-up or earlier disease progression evaluable for response.
Patient characteristics
Patients were a median age of 56 (range, 22–76), and 23% were 65 or older. All had an ECOG performance status of 0 or 1, 80% had DLBCL, and 19% had transformed follicular lymphoma.
Fifteen percent had double or triple hits in CMYC, BCL2, and BCL6 genes, and 52% had germinal center B-cell type disease.
Forty-four percent had 2 prior lines of therapy, 31% had 3 prior lines of therapy, and 19% had 4 to 6 prior lines of therapy. All were either refractory to or relapsed from their last therapy.
Forty-seven percent had undergone prior auto-SCT.
Eighty-nine of the 99 patients infused with tisagenlecleucel received bridging therapy, and 92 received lymphodepleting therapy.
Twenty-six patients were infused as outpatients, and 20 remained as outpatients for 3 or more days after the infusion.
Efficacy
The trial met its primary endpoint with an ORR of 53% tested against the null hypothesis of 20% or less. Forty percent of patients achieved a CR, and 14% had a partial response.
The ORR was consistent across all subgroups, including age, sex, lines of prior antineoplastic therapy, cell of origin, and rearranged MYC/BCL2/BCL6.
“The durability of response, however, which is really the message, is shown by the stability between 3- and 6-month response rates, 38% and 37%, respectively,” Dr Schuster said. “The response rate at 3 months is really indicative of the long-term benefit of this treatment approach.”
The investigators observed no apparent relationship between tumor response at month 3 and dose. And they observed responses at all dose levels.
The very early response may be due, to a certain extent, to the chemotherapy, according to Dr Schuster.
“The effect of the T cells becomes evident as you follow these patients over time,” he said.
The median duration of response and overall response have not been reached. And 74% of patients were relapse-free at 6 months.
“Importantly, almost all the complete responders at month 3 remained in complete response,” Dr Schuster said.
Safety
Adverse events of special interest that occurred within 8 weeks of the infusion included:
- Cytokine release syndrome (CRS)—58% all grades, 15% grade 3, 8% grade 4
- Neurologic events—21% all grades, 8% grade 3, 4% grade 4
- Prolonged cytopenia—36% all grades, 15% grade 3, 12% grade 4
- Infections—34% all grades, 18% grade 3, 2% grade 4
- Febrile neutropenia—13% all grades, 11% grade 3, 2% grade 4
No deaths occurred due to tisagenlecleucel, CRS, or cerebral edema.
Fifty-seven patients developed CRS. The median time to onset of CRS was 3 days (range, 1–9), and the median duration of CRS was 7 days (range, 2–30).
Twenty-eight percent of patients developed hypotension that required intervention, 6% requiring high-dose vasopressors. Eight percent were intubated, and 16% received anticytokine therapy—15% with tocilizumab and 11% with corticosteroids.
Investigators did not observe a relationship between dose and neurological events. However, they did detect a higher probability of CRS with the higher doses of tisagenlecleucel.
They also noted that dose and exposure were independent.
Dr Schuster indicated that these data are the basis for global regulatory submissions.
Manufacture of tisagenlecleucel was centralized, and investigators believe the trial shows the feasibility of global distribution of CAR T-cell therapy using cryopreserved apheresis and centralized manufacturing.
Novartis Pharmaceuticals, the sponsor of the trial, is now able to commercially manufacture the CAR T cells in 22 days.
Dr Schuster disclosed research funding and consulting fees from Novartis and Celgene. ![]()
ATLANTA—The first chimeric antigen receptor (CAR) T-cell therapy approved in the US to treat children and young adults with leukemia is also producing high response rates in lymphoma, according to investigators of the JULIET trial.
They reported that tisagenlecleucel (formerly CTL019) produced an overall response rate (ORR) of 53% and a complete response (CR) rate of 40% in patients with diffuse large B-cell lymphoma (DLBCL).
Additionally, researchers say the stability in the response rate at 3 and 6 months—38% and 37%, respectively—indicates the durability of the therapy.
At 3 months, 32% of patients who achieved CR remained in CR. At 6 months, 30% remained in CR.
Researchers believe these results confirm the durable clinical benefit reported previously.
Stephen J. Schuster, MD, of the University of Pennsylvania in Philadelphia, presented the JULIET data at the 2017 ASH Annual Meeting (abstract 577).
“Only about half of relapsed diffuse large B-cell lymphoma patients are eligible for transplant,” Dr Schuster said. “[O]f those patients, only about a half respond to salvage chemotherapy, and a significant number of patients relapse post-transplant. So there is really a large unmet need for these patients, and CAR T-cell therapy is a potential agent [for them].”
The JULIET trial was a global, single-arm, phase 2 trial evaluating tisagenlecleucel in DLBCL patients. Tisagenlecleucel (Kymriah™) consists of CAR T cells with a CD19 antigen-binding domain, a 4-1BB costimulatory domain, and a CD3-zeta signaling domain.
The trial was conducted at 27 sites in 10 countries across North America, Europe, Australia, and Asia. There were 2 centralized manufacturing sites, one in Europe and one in the US.
Patients had to be 18 years or older, have had 2 or more prior lines of therapy for DLBCL, and have progressive disease or be ineligible for autologous stem cell transplant (auto-SCT). They could not have had any prior anti-CD19 therapy, and they could not have any central nervous system involvement.
The primary endpoint was best ORR using Lugano criteria with assessment by an independent review committee. Secondary endpoints included duration of response, overall survival (OS), and safety.
Study design and enrollment
Patients were screened and underwent apheresis with cryopreservation of their leukapheresis products during screening, which “allowed for enrollment of all eligible patients,” Dr Schuster said.
Patients could receive bridging chemotherapy while they awaited the manufacture of the CAR T cells.
“What’s important to note is that, early on in the trial, there was a shortage of manufacturing capacity, and this led to a longer-than-anticipated interval between enrollment and treatment,” Dr Schuster said. “This interval decreased as manufacturing capacity improved throughout the trial.”
When their CAR T cells were ready, patients were restaged, lymphodepleted, and received the tisagenlecleucel infusion. The dose ranged from 0.6 x 108 to 6.0 x 108 CAR-positive T cells.
The infusion could be conducted on an inpatient or outpatient basis at the investigator’s discretion, Dr Schuster said.
As of the data cutoff in March 2017, investigators enrolled 147 patients and infused 99 with tisagenlecleucel.
Forty-three patients discontinued before infusion, 9 because of an inability to manufacture the T-cell product and 34 due to death (n=16), physician decision (n=12), patient decision (n=3), adverse event (n=2), and protocol deviation (n=1). Five patients were pending infusion.
There were 81 patients with at least 3 months of follow-up or earlier disease progression evaluable for response.
Patient characteristics
Patients were a median age of 56 (range, 22–76), and 23% were 65 or older. All had an ECOG performance status of 0 or 1, 80% had DLBCL, and 19% had transformed follicular lymphoma.
Fifteen percent had double or triple hits in CMYC, BCL2, and BCL6 genes, and 52% had germinal center B-cell type disease.
Forty-four percent had 2 prior lines of therapy, 31% had 3 prior lines of therapy, and 19% had 4 to 6 prior lines of therapy. All were either refractory to or relapsed from their last therapy.
Forty-seven percent had undergone prior auto-SCT.
Eighty-nine of the 99 patients infused with tisagenlecleucel received bridging therapy, and 92 received lymphodepleting therapy.
Twenty-six patients were infused as outpatients, and 20 remained as outpatients for 3 or more days after the infusion.
Efficacy
The trial met its primary endpoint with an ORR of 53% tested against the null hypothesis of 20% or less. Forty percent of patients achieved a CR, and 14% had a partial response.
The ORR was consistent across all subgroups, including age, sex, lines of prior antineoplastic therapy, cell of origin, and rearranged MYC/BCL2/BCL6.
“The durability of response, however, which is really the message, is shown by the stability between 3- and 6-month response rates, 38% and 37%, respectively,” Dr Schuster said. “The response rate at 3 months is really indicative of the long-term benefit of this treatment approach.”
The investigators observed no apparent relationship between tumor response at month 3 and dose. And they observed responses at all dose levels.
The very early response may be due, to a certain extent, to the chemotherapy, according to Dr Schuster.
“The effect of the T cells becomes evident as you follow these patients over time,” he said.
The median duration of response and overall response have not been reached. And 74% of patients were relapse-free at 6 months.
“Importantly, almost all the complete responders at month 3 remained in complete response,” Dr Schuster said.
Safety
Adverse events of special interest that occurred within 8 weeks of the infusion included:
- Cytokine release syndrome (CRS)—58% all grades, 15% grade 3, 8% grade 4
- Neurologic events—21% all grades, 8% grade 3, 4% grade 4
- Prolonged cytopenia—36% all grades, 15% grade 3, 12% grade 4
- Infections—34% all grades, 18% grade 3, 2% grade 4
- Febrile neutropenia—13% all grades, 11% grade 3, 2% grade 4
No deaths occurred due to tisagenlecleucel, CRS, or cerebral edema.
Fifty-seven patients developed CRS. The median time to onset of CRS was 3 days (range, 1–9), and the median duration of CRS was 7 days (range, 2–30).
Twenty-eight percent of patients developed hypotension that required intervention, 6% requiring high-dose vasopressors. Eight percent were intubated, and 16% received anticytokine therapy—15% with tocilizumab and 11% with corticosteroids.
Investigators did not observe a relationship between dose and neurological events. However, they did detect a higher probability of CRS with the higher doses of tisagenlecleucel.
They also noted that dose and exposure were independent.
Dr Schuster indicated that these data are the basis for global regulatory submissions.
Manufacture of tisagenlecleucel was centralized, and investigators believe the trial shows the feasibility of global distribution of CAR T-cell therapy using cryopreserved apheresis and centralized manufacturing.
Novartis Pharmaceuticals, the sponsor of the trial, is now able to commercially manufacture the CAR T cells in 22 days.
Dr Schuster disclosed research funding and consulting fees from Novartis and Celgene. ![]()
VIDEO - New lymphoma drug approvals: Clinical use, future directions
ATLANTA – 2017 was a banner year for the approval of new drugs to treat hematologic disorders.
At a special interest session at the annual meeting of American Society of Hematology, representatives from the Food and Drug Administration joined forces with clinicians to discuss the use of the newly approved treatments in the real-world setting.
In this video interview,
“This is extremely exciting,” she said regarding the pace of new approvals for hematologic malignancies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Axicabtagene ciloleucel, a CAR T-cell product approved in October for the treatment of relapsed/refractory large B-cell lymphoma in adults, is particularly interesting, she said.
“The data shows that if you look at a population of diffuse large B-cell lymphoma patients, that historically have a very poor outcome, there is definitely an impressive response rate and improved survival, compared to the natural history cohort,” said Dr. Heslop of Baylor College of Medicine, Houston.
However, while the findings are encouraging, only 30%-40% are having a durable response, she added.
“So I think there’ll be lots of efforts to try and improve the response rate by combination with other agents such as checkpoint inhibitors or other immunomodulators,” she said.
With respect to the second-generation Bruton’s tyrosine kinase inhibitor acalabrutinib, which was approved in October for adults with mantle cell lymphoma who have been treated with at least one prior therapy, she discussed the potential for improved outcomes and the importance of looking further into its use in patients who have failed ibrutinib therapy, as well as its use in combination with other agents, such as bendamustine and rituximab early in the course of disease.
Copanlisib, a PI3 kinase inhibitor approved in September, is an addition to the armamentarium for adult patients with relapsed follicular lymphoma after two lines of previous therapy.
“It still does have some side effects, as do other drugs in this class, so I think it’s place will still need to be defined,” Dr. Heslop said.
She reported having no relevant financial disclosures.
ATLANTA – 2017 was a banner year for the approval of new drugs to treat hematologic disorders.
At a special interest session at the annual meeting of American Society of Hematology, representatives from the Food and Drug Administration joined forces with clinicians to discuss the use of the newly approved treatments in the real-world setting.
In this video interview,
“This is extremely exciting,” she said regarding the pace of new approvals for hematologic malignancies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Axicabtagene ciloleucel, a CAR T-cell product approved in October for the treatment of relapsed/refractory large B-cell lymphoma in adults, is particularly interesting, she said.
“The data shows that if you look at a population of diffuse large B-cell lymphoma patients, that historically have a very poor outcome, there is definitely an impressive response rate and improved survival, compared to the natural history cohort,” said Dr. Heslop of Baylor College of Medicine, Houston.
However, while the findings are encouraging, only 30%-40% are having a durable response, she added.
“So I think there’ll be lots of efforts to try and improve the response rate by combination with other agents such as checkpoint inhibitors or other immunomodulators,” she said.
With respect to the second-generation Bruton’s tyrosine kinase inhibitor acalabrutinib, which was approved in October for adults with mantle cell lymphoma who have been treated with at least one prior therapy, she discussed the potential for improved outcomes and the importance of looking further into its use in patients who have failed ibrutinib therapy, as well as its use in combination with other agents, such as bendamustine and rituximab early in the course of disease.
Copanlisib, a PI3 kinase inhibitor approved in September, is an addition to the armamentarium for adult patients with relapsed follicular lymphoma after two lines of previous therapy.
“It still does have some side effects, as do other drugs in this class, so I think it’s place will still need to be defined,” Dr. Heslop said.
She reported having no relevant financial disclosures.
ATLANTA – 2017 was a banner year for the approval of new drugs to treat hematologic disorders.
At a special interest session at the annual meeting of American Society of Hematology, representatives from the Food and Drug Administration joined forces with clinicians to discuss the use of the newly approved treatments in the real-world setting.
In this video interview,
“This is extremely exciting,” she said regarding the pace of new approvals for hematologic malignancies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Axicabtagene ciloleucel, a CAR T-cell product approved in October for the treatment of relapsed/refractory large B-cell lymphoma in adults, is particularly interesting, she said.
“The data shows that if you look at a population of diffuse large B-cell lymphoma patients, that historically have a very poor outcome, there is definitely an impressive response rate and improved survival, compared to the natural history cohort,” said Dr. Heslop of Baylor College of Medicine, Houston.
However, while the findings are encouraging, only 30%-40% are having a durable response, she added.
“So I think there’ll be lots of efforts to try and improve the response rate by combination with other agents such as checkpoint inhibitors or other immunomodulators,” she said.
With respect to the second-generation Bruton’s tyrosine kinase inhibitor acalabrutinib, which was approved in October for adults with mantle cell lymphoma who have been treated with at least one prior therapy, she discussed the potential for improved outcomes and the importance of looking further into its use in patients who have failed ibrutinib therapy, as well as its use in combination with other agents, such as bendamustine and rituximab early in the course of disease.
Copanlisib, a PI3 kinase inhibitor approved in September, is an addition to the armamentarium for adult patients with relapsed follicular lymphoma after two lines of previous therapy.
“It still does have some side effects, as do other drugs in this class, so I think it’s place will still need to be defined,” Dr. Heslop said.
She reported having no relevant financial disclosures.
REPORTING FROM ASH 2017
VIDEO: Joint FDA-ASH session highlights new AML drugs
ATLANTA – The past year brought a flurry of new drug approvals for the treatment of acute myeloid leukemia (AML), including CPX-351, midostaurin, gemtuzumab ozogamicin, and enasidenib.
During a special interest session at the annual meeting of the American Society of Hematology, Food and Drug Administration representatives discussed the available data and approval process for these drugs, and clinicians discussed their use in the real-world setting.
In this video interview, – a liposome-encapsulated combination of daunorubicin and cytarabine approved in August for patients with newly diagnosed therapy-related AML or AML with myelodysplasia-related changes, and midostaurin (Rydapt), which was approved in April for the treatment of newly diagnosed AML patients who are FLT3 mutation-positive. She also discussed future directions for these agents.
“So what clinicians are faced with is, all of a sudden, a number of new agents, and no particularly vetted or data-based algorithm by which to assign patients from one to the other,” said Dr. Michaelis, of the Medical College of Wisconsin, Milwaukee, adding that none of the drugs have been compared against one another.
In her own practice, when it comes to CPX-351, she said she first discusses the pros and cons with patients.
“This drug is used for older individuals ... with very adverse risk disease, and so the first question is do you fit the trial entry criteria, do you want to go through induction, do you understand what that’s going to mean, and am I going to take you to transplant after we go through this.”
As for midostaurin, she said she tries to use it on anyone who fits the trial criteria and is FLT-3 positive.
“The trick with that is that we don’t know the FLT-3 status at the time we have to start induction, so it’s hard to determine the exact right doses of your induction regimen knowing that you’re not going to get the test back until day 6, 7, 8, and you’re supposed to start delivering the drug on day 8, so we still have a ways as a care community to catch up with being able to give these drugs in a manner that was the same as what was delivered in the trials that led to approval.”
She also discussed the potential for combining treatments.
“I think there’s really room for studies on combinations of inhibitors plus the CPX, the safety of using a variety of induction regimens alongside midostaurin, and safety of combining things, like with midostaurin for example, with some of our antifungals ... and to make sure that that’s safe. So yeah, we’ve got a lot more to do,” she said.
Dr. Michaelis serves on an advisory board for Novartis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – The past year brought a flurry of new drug approvals for the treatment of acute myeloid leukemia (AML), including CPX-351, midostaurin, gemtuzumab ozogamicin, and enasidenib.
During a special interest session at the annual meeting of the American Society of Hematology, Food and Drug Administration representatives discussed the available data and approval process for these drugs, and clinicians discussed their use in the real-world setting.
In this video interview, – a liposome-encapsulated combination of daunorubicin and cytarabine approved in August for patients with newly diagnosed therapy-related AML or AML with myelodysplasia-related changes, and midostaurin (Rydapt), which was approved in April for the treatment of newly diagnosed AML patients who are FLT3 mutation-positive. She also discussed future directions for these agents.
“So what clinicians are faced with is, all of a sudden, a number of new agents, and no particularly vetted or data-based algorithm by which to assign patients from one to the other,” said Dr. Michaelis, of the Medical College of Wisconsin, Milwaukee, adding that none of the drugs have been compared against one another.
In her own practice, when it comes to CPX-351, she said she first discusses the pros and cons with patients.
“This drug is used for older individuals ... with very adverse risk disease, and so the first question is do you fit the trial entry criteria, do you want to go through induction, do you understand what that’s going to mean, and am I going to take you to transplant after we go through this.”
As for midostaurin, she said she tries to use it on anyone who fits the trial criteria and is FLT-3 positive.
“The trick with that is that we don’t know the FLT-3 status at the time we have to start induction, so it’s hard to determine the exact right doses of your induction regimen knowing that you’re not going to get the test back until day 6, 7, 8, and you’re supposed to start delivering the drug on day 8, so we still have a ways as a care community to catch up with being able to give these drugs in a manner that was the same as what was delivered in the trials that led to approval.”
She also discussed the potential for combining treatments.
“I think there’s really room for studies on combinations of inhibitors plus the CPX, the safety of using a variety of induction regimens alongside midostaurin, and safety of combining things, like with midostaurin for example, with some of our antifungals ... and to make sure that that’s safe. So yeah, we’ve got a lot more to do,” she said.
Dr. Michaelis serves on an advisory board for Novartis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – The past year brought a flurry of new drug approvals for the treatment of acute myeloid leukemia (AML), including CPX-351, midostaurin, gemtuzumab ozogamicin, and enasidenib.
During a special interest session at the annual meeting of the American Society of Hematology, Food and Drug Administration representatives discussed the available data and approval process for these drugs, and clinicians discussed their use in the real-world setting.
In this video interview, – a liposome-encapsulated combination of daunorubicin and cytarabine approved in August for patients with newly diagnosed therapy-related AML or AML with myelodysplasia-related changes, and midostaurin (Rydapt), which was approved in April for the treatment of newly diagnosed AML patients who are FLT3 mutation-positive. She also discussed future directions for these agents.
“So what clinicians are faced with is, all of a sudden, a number of new agents, and no particularly vetted or data-based algorithm by which to assign patients from one to the other,” said Dr. Michaelis, of the Medical College of Wisconsin, Milwaukee, adding that none of the drugs have been compared against one another.
In her own practice, when it comes to CPX-351, she said she first discusses the pros and cons with patients.
“This drug is used for older individuals ... with very adverse risk disease, and so the first question is do you fit the trial entry criteria, do you want to go through induction, do you understand what that’s going to mean, and am I going to take you to transplant after we go through this.”
As for midostaurin, she said she tries to use it on anyone who fits the trial criteria and is FLT-3 positive.
“The trick with that is that we don’t know the FLT-3 status at the time we have to start induction, so it’s hard to determine the exact right doses of your induction regimen knowing that you’re not going to get the test back until day 6, 7, 8, and you’re supposed to start delivering the drug on day 8, so we still have a ways as a care community to catch up with being able to give these drugs in a manner that was the same as what was delivered in the trials that led to approval.”
She also discussed the potential for combining treatments.
“I think there’s really room for studies on combinations of inhibitors plus the CPX, the safety of using a variety of induction regimens alongside midostaurin, and safety of combining things, like with midostaurin for example, with some of our antifungals ... and to make sure that that’s safe. So yeah, we’ve got a lot more to do,” she said.
Dr. Michaelis serves on an advisory board for Novartis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM ASH 2017
A+AVD improves modified PFS in advanced HL
ATLANTA—Phase 3 trial results suggest one 4-drug combination may be more effective than another as frontline treatment for advanced Hodgkin lymphoma (HL).
In the ECHELON-1 trial, treatment with brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) staved off progression, death, and the need for subsequent therapy more effectively than treatment with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
However, there was no significant difference between the treatment arms when it came to response rates or overall survival.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
These data were presented at the 2017 ASH Annual Meeting (abstract 6) and simultaneously published in The New England Journal of Medicine. The trial was funded by Millennium Pharmaceuticals and Seattle Genetics, Inc.
“The standard of care in the treatment of Hodgkin lymphoma has not changed over the last several decades, and there remains an unmet need for additional regimens in frontline treatment,” said Joseph M. Connors, MD, of BC Cancer in Vancouver, British Columbia, Canada.
With this in mind, he and his colleagues conducted ECHELON-1. The study enrolled 1334 patients who had stage III or IV HL and had not previously received systemic chemotherapy or radiotherapy.
Fifty-eight percent of patients were male, and the median age was 36 (range, 18-83). Sixty-four percent of patients had stage IV disease, 62% had extranodal involvement at diagnosis, and 58% had B symptoms.
The patients were randomized to receive A+AVD (n=664) or ABVD (n=670) on days 1 and 15 of each 28-day cycle for up to 6 cycles. Baseline characteristics were well-balanced between the treatment arms.
The median follow-up was 24.9 months (range, 0-49.3).
Primary endpoint
The study’s primary endpoint is modified progression-free survival (PFS), which is defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
“Reducing the risk of relapse is an important concern for patients and their physicians,” Dr Connors noted. “In the trial, 33% fewer patients [in the A+AVD arm] required subsequent salvage chemotherapy or high-dose chemotherapy and transplant compared to the patients treated with ABVD.”
According to the independent review facility, the 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
Certain pre-specified subgroups of patients appeared to benefit more with A+AVD than with ABVD, including:
- Males
- Patients treated in North America
- Patients with involvement of more than 1 extranodal site
- Patients with International Prognostic Scores of 4 to 7
- Patients with stage IV disease
- Patients younger than 60.
Secondary endpoints
Secondary endpoints trended in favor of the A+AVD arm, although there were no significant differences between the treatment arms.
The objective response rate at the end of the randomized regimen was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The proportion of patients with a Deauville score ≤2 after the completion of frontline therapy was 85% in the A+AVD arm and 80% in the ABVD arm (P=0.03).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
Safety
“[T]he safety profile [of A+AVD] was generally consistent with that known for the single-agent components of the regimen,” Dr Connors said.
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Common AEs (in the A+AVD and ABVD arms, respectively) included neutropenia (58% and 45%), constipation (42% and 37%), vomiting (33% and 28%), fatigue (both 32%), diarrhea (27% and 18%), pyrexia (27% and 22%), abdominal pain (21% and 10%), and stomatitis (21% and 16%).
Peripheral neuropathy events were observed in 67% of patients in the A+AVD arm and 43% in the ABVD arm. Grade 3 or higher peripheral neuropathy was reported in 11% and 2%, respectively.
Febrile neutropenia occurred in 19% of patients in the A+AVD arm and 8% of those in the ABVD arm. However, prophylaxis with granulocyte colony-stimulating factor (G-CSF) was able to reduce the incidence of febrile neutropenia. In the A+AVD arm, the rate of febrile neutropenia was 11% among patients who received G-CSF and 21% among patients who did not.
Pulmonary toxicity occurred in 2% of patients in the A+AVD arm and 7% of those in the ABVD arm. Grade 3 or higher pulmonary toxicity was reported in 0.76% and 3%, respectively.
There were 9 deaths during treatment in the A+AVD arm. Seven were due to neutropenia or associated complications, and 2 were due to myocardial infarction. One of the patients who died of neutropenia had the condition prior to trial enrollment. The remaining 6 patients did not receive G-CSF prophylaxis.
In the ABVD arm, there were 13 deaths during treatment. Eleven were due to or associated with pulmonary-related toxicity, 1 was due to cardiopulmonary failure, and 1 death had an unknown cause. ![]()
ATLANTA—Phase 3 trial results suggest one 4-drug combination may be more effective than another as frontline treatment for advanced Hodgkin lymphoma (HL).
In the ECHELON-1 trial, treatment with brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) staved off progression, death, and the need for subsequent therapy more effectively than treatment with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
However, there was no significant difference between the treatment arms when it came to response rates or overall survival.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
These data were presented at the 2017 ASH Annual Meeting (abstract 6) and simultaneously published in The New England Journal of Medicine. The trial was funded by Millennium Pharmaceuticals and Seattle Genetics, Inc.
“The standard of care in the treatment of Hodgkin lymphoma has not changed over the last several decades, and there remains an unmet need for additional regimens in frontline treatment,” said Joseph M. Connors, MD, of BC Cancer in Vancouver, British Columbia, Canada.
With this in mind, he and his colleagues conducted ECHELON-1. The study enrolled 1334 patients who had stage III or IV HL and had not previously received systemic chemotherapy or radiotherapy.
Fifty-eight percent of patients were male, and the median age was 36 (range, 18-83). Sixty-four percent of patients had stage IV disease, 62% had extranodal involvement at diagnosis, and 58% had B symptoms.
The patients were randomized to receive A+AVD (n=664) or ABVD (n=670) on days 1 and 15 of each 28-day cycle for up to 6 cycles. Baseline characteristics were well-balanced between the treatment arms.
The median follow-up was 24.9 months (range, 0-49.3).
Primary endpoint
The study’s primary endpoint is modified progression-free survival (PFS), which is defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
“Reducing the risk of relapse is an important concern for patients and their physicians,” Dr Connors noted. “In the trial, 33% fewer patients [in the A+AVD arm] required subsequent salvage chemotherapy or high-dose chemotherapy and transplant compared to the patients treated with ABVD.”
According to the independent review facility, the 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
Certain pre-specified subgroups of patients appeared to benefit more with A+AVD than with ABVD, including:
- Males
- Patients treated in North America
- Patients with involvement of more than 1 extranodal site
- Patients with International Prognostic Scores of 4 to 7
- Patients with stage IV disease
- Patients younger than 60.
Secondary endpoints
Secondary endpoints trended in favor of the A+AVD arm, although there were no significant differences between the treatment arms.
The objective response rate at the end of the randomized regimen was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The proportion of patients with a Deauville score ≤2 after the completion of frontline therapy was 85% in the A+AVD arm and 80% in the ABVD arm (P=0.03).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
Safety
“[T]he safety profile [of A+AVD] was generally consistent with that known for the single-agent components of the regimen,” Dr Connors said.
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Common AEs (in the A+AVD and ABVD arms, respectively) included neutropenia (58% and 45%), constipation (42% and 37%), vomiting (33% and 28%), fatigue (both 32%), diarrhea (27% and 18%), pyrexia (27% and 22%), abdominal pain (21% and 10%), and stomatitis (21% and 16%).
Peripheral neuropathy events were observed in 67% of patients in the A+AVD arm and 43% in the ABVD arm. Grade 3 or higher peripheral neuropathy was reported in 11% and 2%, respectively.
Febrile neutropenia occurred in 19% of patients in the A+AVD arm and 8% of those in the ABVD arm. However, prophylaxis with granulocyte colony-stimulating factor (G-CSF) was able to reduce the incidence of febrile neutropenia. In the A+AVD arm, the rate of febrile neutropenia was 11% among patients who received G-CSF and 21% among patients who did not.
Pulmonary toxicity occurred in 2% of patients in the A+AVD arm and 7% of those in the ABVD arm. Grade 3 or higher pulmonary toxicity was reported in 0.76% and 3%, respectively.
There were 9 deaths during treatment in the A+AVD arm. Seven were due to neutropenia or associated complications, and 2 were due to myocardial infarction. One of the patients who died of neutropenia had the condition prior to trial enrollment. The remaining 6 patients did not receive G-CSF prophylaxis.
In the ABVD arm, there were 13 deaths during treatment. Eleven were due to or associated with pulmonary-related toxicity, 1 was due to cardiopulmonary failure, and 1 death had an unknown cause. ![]()
ATLANTA—Phase 3 trial results suggest one 4-drug combination may be more effective than another as frontline treatment for advanced Hodgkin lymphoma (HL).
In the ECHELON-1 trial, treatment with brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) staved off progression, death, and the need for subsequent therapy more effectively than treatment with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
However, there was no significant difference between the treatment arms when it came to response rates or overall survival.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
These data were presented at the 2017 ASH Annual Meeting (abstract 6) and simultaneously published in The New England Journal of Medicine. The trial was funded by Millennium Pharmaceuticals and Seattle Genetics, Inc.
“The standard of care in the treatment of Hodgkin lymphoma has not changed over the last several decades, and there remains an unmet need for additional regimens in frontline treatment,” said Joseph M. Connors, MD, of BC Cancer in Vancouver, British Columbia, Canada.
With this in mind, he and his colleagues conducted ECHELON-1. The study enrolled 1334 patients who had stage III or IV HL and had not previously received systemic chemotherapy or radiotherapy.
Fifty-eight percent of patients were male, and the median age was 36 (range, 18-83). Sixty-four percent of patients had stage IV disease, 62% had extranodal involvement at diagnosis, and 58% had B symptoms.
The patients were randomized to receive A+AVD (n=664) or ABVD (n=670) on days 1 and 15 of each 28-day cycle for up to 6 cycles. Baseline characteristics were well-balanced between the treatment arms.
The median follow-up was 24.9 months (range, 0-49.3).
Primary endpoint
The study’s primary endpoint is modified progression-free survival (PFS), which is defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
“Reducing the risk of relapse is an important concern for patients and their physicians,” Dr Connors noted. “In the trial, 33% fewer patients [in the A+AVD arm] required subsequent salvage chemotherapy or high-dose chemotherapy and transplant compared to the patients treated with ABVD.”
According to the independent review facility, the 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
Certain pre-specified subgroups of patients appeared to benefit more with A+AVD than with ABVD, including:
- Males
- Patients treated in North America
- Patients with involvement of more than 1 extranodal site
- Patients with International Prognostic Scores of 4 to 7
- Patients with stage IV disease
- Patients younger than 60.
Secondary endpoints
Secondary endpoints trended in favor of the A+AVD arm, although there were no significant differences between the treatment arms.
The objective response rate at the end of the randomized regimen was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The proportion of patients with a Deauville score ≤2 after the completion of frontline therapy was 85% in the A+AVD arm and 80% in the ABVD arm (P=0.03).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
Safety
“[T]he safety profile [of A+AVD] was generally consistent with that known for the single-agent components of the regimen,” Dr Connors said.
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Common AEs (in the A+AVD and ABVD arms, respectively) included neutropenia (58% and 45%), constipation (42% and 37%), vomiting (33% and 28%), fatigue (both 32%), diarrhea (27% and 18%), pyrexia (27% and 22%), abdominal pain (21% and 10%), and stomatitis (21% and 16%).
Peripheral neuropathy events were observed in 67% of patients in the A+AVD arm and 43% in the ABVD arm. Grade 3 or higher peripheral neuropathy was reported in 11% and 2%, respectively.
Febrile neutropenia occurred in 19% of patients in the A+AVD arm and 8% of those in the ABVD arm. However, prophylaxis with granulocyte colony-stimulating factor (G-CSF) was able to reduce the incidence of febrile neutropenia. In the A+AVD arm, the rate of febrile neutropenia was 11% among patients who received G-CSF and 21% among patients who did not.
Pulmonary toxicity occurred in 2% of patients in the A+AVD arm and 7% of those in the ABVD arm. Grade 3 or higher pulmonary toxicity was reported in 0.76% and 3%, respectively.
There were 9 deaths during treatment in the A+AVD arm. Seven were due to neutropenia or associated complications, and 2 were due to myocardial infarction. One of the patients who died of neutropenia had the condition prior to trial enrollment. The remaining 6 patients did not receive G-CSF prophylaxis.
In the ABVD arm, there were 13 deaths during treatment. Eleven were due to or associated with pulmonary-related toxicity, 1 was due to cardiopulmonary failure, and 1 death had an unknown cause. ![]()
VIDEO: Ibrutinib PFS is nearly 3 years in MCL patients who had one prior therapy
ATLANTA – Ibrutinib yielded a median progression-free survival (PFS) of nearly 3 years for patients with relapsed or refractory mantle cell lymphoma (MCL) treated with the agent after just one prior line of therapy, according to pooled long-term follow-up data presented at the annual meeting of the American Society of Hematology.
With a 3.5-year median follow-up, a median PFS of 33.6 months was reported for MCL patients with one prior line of therapy, compared to 8.4 months for patients who had two or more prior lines of therapy, reported lead study author Simon Rule, MD, of Plymouth (England) University Medical School.
“I think the take-home message from the ibrutinib data is the earlier you use the drug in the relapse setting, the better the outcomes you’re going to get,” Dr. Rule said in an interview. “It is quite dramatic, the difference between one prior line of therapy and subsequent lines of therapy.”
Response rates were also higher in MCL patients who had only one prior line of therapy, Dr. Rule said.
The overall and complete response rates for that group were 77.8% and 36.4%, respectively, according to data Dr. Rule presented in an oral presentation. For patients receiving more than one line of therapy prior to ibrutinib, overall and complete response rates were 66.8% and 22.9%.
The pooled analysis presented by Dr. Rule included 370 patients enrolled in ibrutinib trials between 2011 and 2013. Patients in those trials received oral ibrutinib 560 mg daily until progressive disease or unacceptable toxicity.
Patients achieving a CR had an “extraordinary” PFS of nearly 4 years and a median duration of response of 55 months, Dr. Rule said.
Atrial fibrillation (AF) rates were reported to be 5.7% (21/370 patients). A total of 53 patients in the analysis had ongoing controlled AF/arrhythmia or had a history of it. Over the course of follow-up, 70% of them (37 patients) had no recurrences, according to Dr. Rule and his colleagues.
No patients discontinued ibrutinib because of grade 3-4 AF, they reported. Moreover, less than 2% of the 370 patients discontinued or reduced dose of ibrutinib because of grade 3-4 bleeding or AF.
New onset grade 3-4 adverse events were more common in the first year of treatment and generally were less frequent over time, Dr. Rule said.
Patients with only one prior line of therapy were less likely to have grade 3-4 adverse events, suggesting again that “the earlier you use [ibrutinib], the fewer side effects you get, particularly with hematologic toxicity,” Dr. Rule said.
Sponsorship for the research came from Janssen, and funding for writing assistance came from Janssen Global Services. Dr. Rule reported financial relationships with Janssen and several other companies.
SOURCE: Rule S et al. ASH 2017 Abstract 151.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – Ibrutinib yielded a median progression-free survival (PFS) of nearly 3 years for patients with relapsed or refractory mantle cell lymphoma (MCL) treated with the agent after just one prior line of therapy, according to pooled long-term follow-up data presented at the annual meeting of the American Society of Hematology.
With a 3.5-year median follow-up, a median PFS of 33.6 months was reported for MCL patients with one prior line of therapy, compared to 8.4 months for patients who had two or more prior lines of therapy, reported lead study author Simon Rule, MD, of Plymouth (England) University Medical School.
“I think the take-home message from the ibrutinib data is the earlier you use the drug in the relapse setting, the better the outcomes you’re going to get,” Dr. Rule said in an interview. “It is quite dramatic, the difference between one prior line of therapy and subsequent lines of therapy.”
Response rates were also higher in MCL patients who had only one prior line of therapy, Dr. Rule said.
The overall and complete response rates for that group were 77.8% and 36.4%, respectively, according to data Dr. Rule presented in an oral presentation. For patients receiving more than one line of therapy prior to ibrutinib, overall and complete response rates were 66.8% and 22.9%.
The pooled analysis presented by Dr. Rule included 370 patients enrolled in ibrutinib trials between 2011 and 2013. Patients in those trials received oral ibrutinib 560 mg daily until progressive disease or unacceptable toxicity.
Patients achieving a CR had an “extraordinary” PFS of nearly 4 years and a median duration of response of 55 months, Dr. Rule said.
Atrial fibrillation (AF) rates were reported to be 5.7% (21/370 patients). A total of 53 patients in the analysis had ongoing controlled AF/arrhythmia or had a history of it. Over the course of follow-up, 70% of them (37 patients) had no recurrences, according to Dr. Rule and his colleagues.
No patients discontinued ibrutinib because of grade 3-4 AF, they reported. Moreover, less than 2% of the 370 patients discontinued or reduced dose of ibrutinib because of grade 3-4 bleeding or AF.
New onset grade 3-4 adverse events were more common in the first year of treatment and generally were less frequent over time, Dr. Rule said.
Patients with only one prior line of therapy were less likely to have grade 3-4 adverse events, suggesting again that “the earlier you use [ibrutinib], the fewer side effects you get, particularly with hematologic toxicity,” Dr. Rule said.
Sponsorship for the research came from Janssen, and funding for writing assistance came from Janssen Global Services. Dr. Rule reported financial relationships with Janssen and several other companies.
SOURCE: Rule S et al. ASH 2017 Abstract 151.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – Ibrutinib yielded a median progression-free survival (PFS) of nearly 3 years for patients with relapsed or refractory mantle cell lymphoma (MCL) treated with the agent after just one prior line of therapy, according to pooled long-term follow-up data presented at the annual meeting of the American Society of Hematology.
With a 3.5-year median follow-up, a median PFS of 33.6 months was reported for MCL patients with one prior line of therapy, compared to 8.4 months for patients who had two or more prior lines of therapy, reported lead study author Simon Rule, MD, of Plymouth (England) University Medical School.
“I think the take-home message from the ibrutinib data is the earlier you use the drug in the relapse setting, the better the outcomes you’re going to get,” Dr. Rule said in an interview. “It is quite dramatic, the difference between one prior line of therapy and subsequent lines of therapy.”
Response rates were also higher in MCL patients who had only one prior line of therapy, Dr. Rule said.
The overall and complete response rates for that group were 77.8% and 36.4%, respectively, according to data Dr. Rule presented in an oral presentation. For patients receiving more than one line of therapy prior to ibrutinib, overall and complete response rates were 66.8% and 22.9%.
The pooled analysis presented by Dr. Rule included 370 patients enrolled in ibrutinib trials between 2011 and 2013. Patients in those trials received oral ibrutinib 560 mg daily until progressive disease or unacceptable toxicity.
Patients achieving a CR had an “extraordinary” PFS of nearly 4 years and a median duration of response of 55 months, Dr. Rule said.
Atrial fibrillation (AF) rates were reported to be 5.7% (21/370 patients). A total of 53 patients in the analysis had ongoing controlled AF/arrhythmia or had a history of it. Over the course of follow-up, 70% of them (37 patients) had no recurrences, according to Dr. Rule and his colleagues.
No patients discontinued ibrutinib because of grade 3-4 AF, they reported. Moreover, less than 2% of the 370 patients discontinued or reduced dose of ibrutinib because of grade 3-4 bleeding or AF.
New onset grade 3-4 adverse events were more common in the first year of treatment and generally were less frequent over time, Dr. Rule said.
Patients with only one prior line of therapy were less likely to have grade 3-4 adverse events, suggesting again that “the earlier you use [ibrutinib], the fewer side effects you get, particularly with hematologic toxicity,” Dr. Rule said.
Sponsorship for the research came from Janssen, and funding for writing assistance came from Janssen Global Services. Dr. Rule reported financial relationships with Janssen and several other companies.
SOURCE: Rule S et al. ASH 2017 Abstract 151.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM ASH 2017
Key clinical point:
Major finding: Median PFS was 33.6 months for MCL patients with one prior line of therapy, versus 8.4 months for patients who had two or more prior lines of therapy.
Study details: A pooled analysis of 370 patients enrolled in ibrutinib clinical trials with a median 3.5-year follow-up.
Disclosures: Janssen sponsored the research and Janssen Global Services funded writing assistance. Lead author Simon Rule, MD, reported financial relationships with Janssen and several other companies.
Source: Rule S et al. ASH 2017 Abstract 151.