User login
Society of Critical Care Medicine (SCCM): Critical Care Congress
Palliative care shortens ICU, hospital stays, review shows
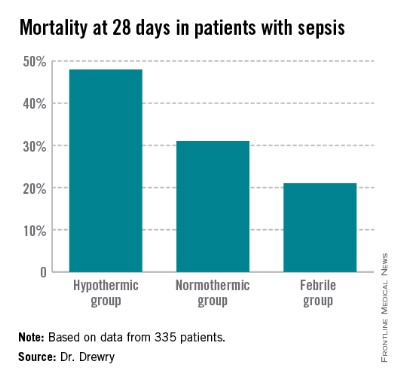
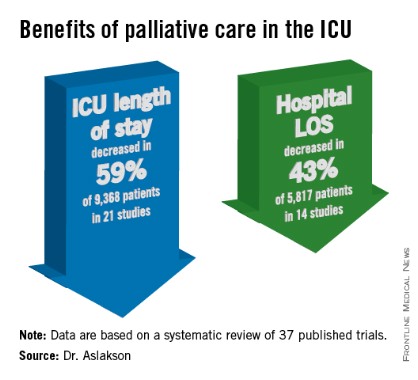
SAN FRANCISCO – Palliative care in the intensive care unit reduces the length of stay in the ICU and the hospital without changing mortality rates or family satisfaction, according to a review of the literature.
Although measurements of family satisfaction overall didn’t change much from palliative care of a loved one in the ICU, some measures of components of satisfaction increased with palliative care, such as improved communication with the physician, better consensus around the goals of care, and decreased anxiety and depression in family members, reported Dr. Rebecca A. Aslakson of Johns Hopkins University, Baltimore, and her colleagues.
Dr. Aslakson presented the findings at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.

Dr. Aslakson and her associates were unable to perform a formal meta-analysis of the 37 published trials of palliative care in the ICU because of the heterogeneity of the studies, which looked at more than 40 different outcomes.
Instead, their systematic review grouped results under four outcomes that commonly were measured, and assessed those either by the number of studies or by the number of patients studied.
ICU length of stay decreased with palliative care in 13 of 21 studies (62%) that used this outcome and in 59% of 9,368 patients in those studies.
Hospital length of stay decreased with palliative care in 8 of 14 studies (57%) and in 43% of 5,817 patients. Family satisfaction did not decrease in any studies or families and increased in only 1 of 14 studies (7%) and in 2% of families of 4,927 patients, Dr. Aslakson and her colleagues reported (J. Palliat. Med. 2014;17:219-35).
Mortality rates did not change with palliative care in 14 of 16 studies (88%) that assessed mortality and in 57% of 5,969 patients in those studies. Mortality increased in one small study (6%) and decreased in one larger study (6%).
"Talking about big-picture issues and goals of care doesn’t lead to people dying," Dr. Aslakson said.
"No harm came in any of these studies." Some separate studies of palliative care outside of ICUs reported that this increases hope, "because people feel that they have more control over their choices and what’s happening to their loved ones," she added.
Integrative vs. consultative model
Dr. Aslakson and her associates also reviewed studies based on whether the interventions used integrative or consultative models of palliative care.
Generally, consultative models bring outsiders into the ICU to help provide palliative care, and integrative models train the ICU team to be the palliative care providers. In reality, the two models may overlap. For this review, the investigators applied mutually exclusive definitions to 36 of the studies.
In 18 studies of integrative interventions, members of the ICU team were the only caregivers in face-to-face interactions with the patient and families. In 18 studies of consultative interventions, palliative care providers included others besides the ICU team.
In the studies of integrative palliative care, ICU length of stay decreased with palliative care in four of nine studies (44%) that measured this outcome and in 52% of 6,963 patients in those studies, she reported. Hospital length of stay decreased in two of five studies (40%) and in 24% of 3,812 patients. Family satisfaction changed in none of 15 studies, and mortality decreased in 1 of 5 studies (20%) and in 34% of 3,807 patients.
In the studies of consultative care, ICU length of stay decreased with palliative care in 9 of 12 studies (75%) that measured this outcome and in 79% of 2,405 patients in those studies. Hospital length of stay decreased in six of nine studies (67%) and in 79% of 2,005 patients. Family satisfaction increased in one of four studies (25%) and in 21% of 429 patients. Mortality increased in 1 of 11 studies (9%) and in 5% of 2,162 patients.
One model isn’t necessarily better than the other, Dr. Aslakson said. Integrative palliative care may work best in a closed ICU with perhaps four or five intensivists in a relatively small unit. An integrative approach can be much more difficult in open or semiopen ICUs that have "40 different doctors floating around," she said. "We tried that in my unit, and it didn’t work that well."
Different ICUs need palliative care models that fit them. "Look at your unit, the way it works, and who the providers are, then look at the literature and see what matches that and what might work for your unit," she said.
Outcomes of better communication
A previous, separate review of the medical literature identified 21 controlled trials of 16 interventions to improve communication in ICUs between families and care providers. Overall, the interventions improved emotional outcomes for families and reduced ICU length of stay and treatment intensity (Chest 2011;139:543-54), she noted.
Yet another prior review of the literature reported that interventions to promote family meetings, use empathetic communication skills, and employ palliative care consultations improved family satisfaction and reduced ICU length of stay and the adverse effects of family bereavement (Curr. Opin. Crit. Care 2009;15:569-77).
Dr. Aslakson reported having no financial disclosures.
Dr. Jennifer Cox, FCCP, comments: Dr. Aslakson and colleagues’ systematic review adds to the body of literature that demonstrates no mortality increase when palliative care measures are initiated in the ICU. Shorter lengths of stay both in the ICU and hospital were other positive outcomes noted without a significant change in patient or family satisfaction.
These findings were independent of whether an integrative or consultative approach to palliative care was undertaken. This should encourage physicians to examine their practice setting and determine which approach meets the needs of their ICU and begin to utilize palliative care earlier and more aggressively without fear of increasing mortality.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – Palliative care in the intensive care unit reduces the length of stay in the ICU and the hospital without changing mortality rates or family satisfaction, according to a review of the literature.
Although measurements of family satisfaction overall didn’t change much from palliative care of a loved one in the ICU, some measures of components of satisfaction increased with palliative care, such as improved communication with the physician, better consensus around the goals of care, and decreased anxiety and depression in family members, reported Dr. Rebecca A. Aslakson of Johns Hopkins University, Baltimore, and her colleagues.
Dr. Aslakson presented the findings at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.

Dr. Aslakson and her associates were unable to perform a formal meta-analysis of the 37 published trials of palliative care in the ICU because of the heterogeneity of the studies, which looked at more than 40 different outcomes.
Instead, their systematic review grouped results under four outcomes that commonly were measured, and assessed those either by the number of studies or by the number of patients studied.
ICU length of stay decreased with palliative care in 13 of 21 studies (62%) that used this outcome and in 59% of 9,368 patients in those studies.
Hospital length of stay decreased with palliative care in 8 of 14 studies (57%) and in 43% of 5,817 patients. Family satisfaction did not decrease in any studies or families and increased in only 1 of 14 studies (7%) and in 2% of families of 4,927 patients, Dr. Aslakson and her colleagues reported (J. Palliat. Med. 2014;17:219-35).
Mortality rates did not change with palliative care in 14 of 16 studies (88%) that assessed mortality and in 57% of 5,969 patients in those studies. Mortality increased in one small study (6%) and decreased in one larger study (6%).
"Talking about big-picture issues and goals of care doesn’t lead to people dying," Dr. Aslakson said.
"No harm came in any of these studies." Some separate studies of palliative care outside of ICUs reported that this increases hope, "because people feel that they have more control over their choices and what’s happening to their loved ones," she added.
Integrative vs. consultative model
Dr. Aslakson and her associates also reviewed studies based on whether the interventions used integrative or consultative models of palliative care.
Generally, consultative models bring outsiders into the ICU to help provide palliative care, and integrative models train the ICU team to be the palliative care providers. In reality, the two models may overlap. For this review, the investigators applied mutually exclusive definitions to 36 of the studies.
In 18 studies of integrative interventions, members of the ICU team were the only caregivers in face-to-face interactions with the patient and families. In 18 studies of consultative interventions, palliative care providers included others besides the ICU team.
In the studies of integrative palliative care, ICU length of stay decreased with palliative care in four of nine studies (44%) that measured this outcome and in 52% of 6,963 patients in those studies, she reported. Hospital length of stay decreased in two of five studies (40%) and in 24% of 3,812 patients. Family satisfaction changed in none of 15 studies, and mortality decreased in 1 of 5 studies (20%) and in 34% of 3,807 patients.
In the studies of consultative care, ICU length of stay decreased with palliative care in 9 of 12 studies (75%) that measured this outcome and in 79% of 2,405 patients in those studies. Hospital length of stay decreased in six of nine studies (67%) and in 79% of 2,005 patients. Family satisfaction increased in one of four studies (25%) and in 21% of 429 patients. Mortality increased in 1 of 11 studies (9%) and in 5% of 2,162 patients.
One model isn’t necessarily better than the other, Dr. Aslakson said. Integrative palliative care may work best in a closed ICU with perhaps four or five intensivists in a relatively small unit. An integrative approach can be much more difficult in open or semiopen ICUs that have "40 different doctors floating around," she said. "We tried that in my unit, and it didn’t work that well."
Different ICUs need palliative care models that fit them. "Look at your unit, the way it works, and who the providers are, then look at the literature and see what matches that and what might work for your unit," she said.
Outcomes of better communication
A previous, separate review of the medical literature identified 21 controlled trials of 16 interventions to improve communication in ICUs between families and care providers. Overall, the interventions improved emotional outcomes for families and reduced ICU length of stay and treatment intensity (Chest 2011;139:543-54), she noted.
Yet another prior review of the literature reported that interventions to promote family meetings, use empathetic communication skills, and employ palliative care consultations improved family satisfaction and reduced ICU length of stay and the adverse effects of family bereavement (Curr. Opin. Crit. Care 2009;15:569-77).
Dr. Aslakson reported having no financial disclosures.
Dr. Jennifer Cox, FCCP, comments: Dr. Aslakson and colleagues’ systematic review adds to the body of literature that demonstrates no mortality increase when palliative care measures are initiated in the ICU. Shorter lengths of stay both in the ICU and hospital were other positive outcomes noted without a significant change in patient or family satisfaction.
These findings were independent of whether an integrative or consultative approach to palliative care was undertaken. This should encourage physicians to examine their practice setting and determine which approach meets the needs of their ICU and begin to utilize palliative care earlier and more aggressively without fear of increasing mortality.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – Palliative care in the intensive care unit reduces the length of stay in the ICU and the hospital without changing mortality rates or family satisfaction, according to a review of the literature.
Although measurements of family satisfaction overall didn’t change much from palliative care of a loved one in the ICU, some measures of components of satisfaction increased with palliative care, such as improved communication with the physician, better consensus around the goals of care, and decreased anxiety and depression in family members, reported Dr. Rebecca A. Aslakson of Johns Hopkins University, Baltimore, and her colleagues.
Dr. Aslakson presented the findings at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.

Dr. Aslakson and her associates were unable to perform a formal meta-analysis of the 37 published trials of palliative care in the ICU because of the heterogeneity of the studies, which looked at more than 40 different outcomes.
Instead, their systematic review grouped results under four outcomes that commonly were measured, and assessed those either by the number of studies or by the number of patients studied.
ICU length of stay decreased with palliative care in 13 of 21 studies (62%) that used this outcome and in 59% of 9,368 patients in those studies.
Hospital length of stay decreased with palliative care in 8 of 14 studies (57%) and in 43% of 5,817 patients. Family satisfaction did not decrease in any studies or families and increased in only 1 of 14 studies (7%) and in 2% of families of 4,927 patients, Dr. Aslakson and her colleagues reported (J. Palliat. Med. 2014;17:219-35).
Mortality rates did not change with palliative care in 14 of 16 studies (88%) that assessed mortality and in 57% of 5,969 patients in those studies. Mortality increased in one small study (6%) and decreased in one larger study (6%).
"Talking about big-picture issues and goals of care doesn’t lead to people dying," Dr. Aslakson said.
"No harm came in any of these studies." Some separate studies of palliative care outside of ICUs reported that this increases hope, "because people feel that they have more control over their choices and what’s happening to their loved ones," she added.
Integrative vs. consultative model
Dr. Aslakson and her associates also reviewed studies based on whether the interventions used integrative or consultative models of palliative care.
Generally, consultative models bring outsiders into the ICU to help provide palliative care, and integrative models train the ICU team to be the palliative care providers. In reality, the two models may overlap. For this review, the investigators applied mutually exclusive definitions to 36 of the studies.
In 18 studies of integrative interventions, members of the ICU team were the only caregivers in face-to-face interactions with the patient and families. In 18 studies of consultative interventions, palliative care providers included others besides the ICU team.
In the studies of integrative palliative care, ICU length of stay decreased with palliative care in four of nine studies (44%) that measured this outcome and in 52% of 6,963 patients in those studies, she reported. Hospital length of stay decreased in two of five studies (40%) and in 24% of 3,812 patients. Family satisfaction changed in none of 15 studies, and mortality decreased in 1 of 5 studies (20%) and in 34% of 3,807 patients.
In the studies of consultative care, ICU length of stay decreased with palliative care in 9 of 12 studies (75%) that measured this outcome and in 79% of 2,405 patients in those studies. Hospital length of stay decreased in six of nine studies (67%) and in 79% of 2,005 patients. Family satisfaction increased in one of four studies (25%) and in 21% of 429 patients. Mortality increased in 1 of 11 studies (9%) and in 5% of 2,162 patients.
One model isn’t necessarily better than the other, Dr. Aslakson said. Integrative palliative care may work best in a closed ICU with perhaps four or five intensivists in a relatively small unit. An integrative approach can be much more difficult in open or semiopen ICUs that have "40 different doctors floating around," she said. "We tried that in my unit, and it didn’t work that well."
Different ICUs need palliative care models that fit them. "Look at your unit, the way it works, and who the providers are, then look at the literature and see what matches that and what might work for your unit," she said.
Outcomes of better communication
A previous, separate review of the medical literature identified 21 controlled trials of 16 interventions to improve communication in ICUs between families and care providers. Overall, the interventions improved emotional outcomes for families and reduced ICU length of stay and treatment intensity (Chest 2011;139:543-54), she noted.
Yet another prior review of the literature reported that interventions to promote family meetings, use empathetic communication skills, and employ palliative care consultations improved family satisfaction and reduced ICU length of stay and the adverse effects of family bereavement (Curr. Opin. Crit. Care 2009;15:569-77).
Dr. Aslakson reported having no financial disclosures.
Dr. Jennifer Cox, FCCP, comments: Dr. Aslakson and colleagues’ systematic review adds to the body of literature that demonstrates no mortality increase when palliative care measures are initiated in the ICU. Shorter lengths of stay both in the ICU and hospital were other positive outcomes noted without a significant change in patient or family satisfaction.
These findings were independent of whether an integrative or consultative approach to palliative care was undertaken. This should encourage physicians to examine their practice setting and determine which approach meets the needs of their ICU and begin to utilize palliative care earlier and more aggressively without fear of increasing mortality.
[email protected]
On Twitter @sherryboschert
Relatively few in ICUs get end-of-life dialogue training
SAN FRANCISCO – Despite training recommendations, half of physicians and less than a third of nurses surveyed in adult intensive care units at 56 California hospitals reported receiving formal training in talking with patients and families about the end of life.
A 2008 consensus statement by the American College of Critical Care Medicine included a recommendation for end-of-life communication skills training for clinicians to improve the care of patients dying in ICUs ((Crit. Care Med. 2008;36:953-63).
Dr. Matthew H.R. Anstey and his associates approached 149 California hospitals to gauge the extent of implementation of this recommendation. At 56 hospitals, doctors and nurses who work in adult ICUs voluntarily completed an anonymous web-based survey. Eighty-four percent of the 1,363 respondents were nurses, he reported in a poster presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Overall, 32% of the respondents said they had received formal training in communication skills. A significantly higher percentage of doctors had undergone training (50%) compared with nurses (29%), said Dr. Anstey, who is currently a lecturer in anesthesia at Harvard Medical School, Boston.
Sixty-six percent of all respondents agreed that "nurses are present during the communication of end-of-life information to the family" at their institution. Nurses were significantly more likely to agree with this statement (69%) than were doctors (52%).
Both doctors and nurses were very supportive of the idea of formal communication training for ICU providers. When asked about possible strategies to reduce inappropriate care for ICU patients, 91% of respondents said communication training would have a positive effect, Dr. Anstey reported.
This could be accomplished by requiring ICU physicians to complete a communication training module for ongoing credentialing, he said in an e-mail interview. Either individual hospitals could require this as part of credentialing for privileges to work in the ICU, or state medical boards could require it, similar to the California Medical Board’s requirement that physicians obtain some continuing medical education in pain management, he suggested.
The characteristics of participating hospitals were similar to those of nonparticipating hospitals in the sizes of the hospitals and ICUs, their regional location in California, and the proportions of hospitals that are teaching facilities.
The 93 nonparticipating hospitals were significantly more likely to be for-profit hospitals (59%) compared with participating hospitals (7%), and significantly less likely to be part of a hospital system containing more than three hospitals (54%) compared with participating hospitals (75%).
Dr. Anstey reported having no financial disclosures. His research was in conjunction with a Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice for which he was placed at Kaiser Permanente in California.
Dr. Paul A. Selecky, FCCP, comments: Physicians are notorious about not doing a good job of communicating with patients in general, and when you focus on a vital subject as end-of-life care, it is of even greater importance. The findings in this study are not surprising. The unanswered question is how to fix it.
On Twitter @sherryboschert
SAN FRANCISCO – Despite training recommendations, half of physicians and less than a third of nurses surveyed in adult intensive care units at 56 California hospitals reported receiving formal training in talking with patients and families about the end of life.
A 2008 consensus statement by the American College of Critical Care Medicine included a recommendation for end-of-life communication skills training for clinicians to improve the care of patients dying in ICUs ((Crit. Care Med. 2008;36:953-63).
Dr. Matthew H.R. Anstey and his associates approached 149 California hospitals to gauge the extent of implementation of this recommendation. At 56 hospitals, doctors and nurses who work in adult ICUs voluntarily completed an anonymous web-based survey. Eighty-four percent of the 1,363 respondents were nurses, he reported in a poster presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Overall, 32% of the respondents said they had received formal training in communication skills. A significantly higher percentage of doctors had undergone training (50%) compared with nurses (29%), said Dr. Anstey, who is currently a lecturer in anesthesia at Harvard Medical School, Boston.
Sixty-six percent of all respondents agreed that "nurses are present during the communication of end-of-life information to the family" at their institution. Nurses were significantly more likely to agree with this statement (69%) than were doctors (52%).
Both doctors and nurses were very supportive of the idea of formal communication training for ICU providers. When asked about possible strategies to reduce inappropriate care for ICU patients, 91% of respondents said communication training would have a positive effect, Dr. Anstey reported.
This could be accomplished by requiring ICU physicians to complete a communication training module for ongoing credentialing, he said in an e-mail interview. Either individual hospitals could require this as part of credentialing for privileges to work in the ICU, or state medical boards could require it, similar to the California Medical Board’s requirement that physicians obtain some continuing medical education in pain management, he suggested.
The characteristics of participating hospitals were similar to those of nonparticipating hospitals in the sizes of the hospitals and ICUs, their regional location in California, and the proportions of hospitals that are teaching facilities.
The 93 nonparticipating hospitals were significantly more likely to be for-profit hospitals (59%) compared with participating hospitals (7%), and significantly less likely to be part of a hospital system containing more than three hospitals (54%) compared with participating hospitals (75%).
Dr. Anstey reported having no financial disclosures. His research was in conjunction with a Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice for which he was placed at Kaiser Permanente in California.
Dr. Paul A. Selecky, FCCP, comments: Physicians are notorious about not doing a good job of communicating with patients in general, and when you focus on a vital subject as end-of-life care, it is of even greater importance. The findings in this study are not surprising. The unanswered question is how to fix it.
On Twitter @sherryboschert
SAN FRANCISCO – Despite training recommendations, half of physicians and less than a third of nurses surveyed in adult intensive care units at 56 California hospitals reported receiving formal training in talking with patients and families about the end of life.
A 2008 consensus statement by the American College of Critical Care Medicine included a recommendation for end-of-life communication skills training for clinicians to improve the care of patients dying in ICUs ((Crit. Care Med. 2008;36:953-63).
Dr. Matthew H.R. Anstey and his associates approached 149 California hospitals to gauge the extent of implementation of this recommendation. At 56 hospitals, doctors and nurses who work in adult ICUs voluntarily completed an anonymous web-based survey. Eighty-four percent of the 1,363 respondents were nurses, he reported in a poster presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Overall, 32% of the respondents said they had received formal training in communication skills. A significantly higher percentage of doctors had undergone training (50%) compared with nurses (29%), said Dr. Anstey, who is currently a lecturer in anesthesia at Harvard Medical School, Boston.
Sixty-six percent of all respondents agreed that "nurses are present during the communication of end-of-life information to the family" at their institution. Nurses were significantly more likely to agree with this statement (69%) than were doctors (52%).
Both doctors and nurses were very supportive of the idea of formal communication training for ICU providers. When asked about possible strategies to reduce inappropriate care for ICU patients, 91% of respondents said communication training would have a positive effect, Dr. Anstey reported.
This could be accomplished by requiring ICU physicians to complete a communication training module for ongoing credentialing, he said in an e-mail interview. Either individual hospitals could require this as part of credentialing for privileges to work in the ICU, or state medical boards could require it, similar to the California Medical Board’s requirement that physicians obtain some continuing medical education in pain management, he suggested.
The characteristics of participating hospitals were similar to those of nonparticipating hospitals in the sizes of the hospitals and ICUs, their regional location in California, and the proportions of hospitals that are teaching facilities.
The 93 nonparticipating hospitals were significantly more likely to be for-profit hospitals (59%) compared with participating hospitals (7%), and significantly less likely to be part of a hospital system containing more than three hospitals (54%) compared with participating hospitals (75%).
Dr. Anstey reported having no financial disclosures. His research was in conjunction with a Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice for which he was placed at Kaiser Permanente in California.
Dr. Paul A. Selecky, FCCP, comments: Physicians are notorious about not doing a good job of communicating with patients in general, and when you focus on a vital subject as end-of-life care, it is of even greater importance. The findings in this study are not surprising. The unanswered question is how to fix it.
On Twitter @sherryboschert
Major finding: Half of doctors and 29% of nurses in ICUs said they had received formal training in end-of-life communications.
Data source: A voluntary web-based survey of 1,363 doctors and nurses working in adult ICUs in 56 California hospitals.
Disclosures: Dr. Anstey reported having no financial disclosures. His research was in conjunction with a Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice, for which he was placed at Kaiser Permanente in California.
Palliative care is not just for the dying
SAN FRANCISCO – Palliative care is not just for the dying.
Understanding that premise is the first step to integrating palliative care into intensive care units, Dr. Zara Cooper said. Palliative care treats patient illness and can be delivered concurrently in the ICU with curative care that treats disease.
As options for curative treatment decrease, the role of palliative care may increase and does not stop at the patient’s death. "It’s important that we provide ongoing bereavement support not only to family members and survivors but also to caregivers and members of our medical team," added Dr. Cooper, an assistant professor of surgery at Harvard Medical School and a surgical intensivist at Brigham and Women’s Hospital, Boston.
Getting intensive care colleagues to agree on a definition of palliative care is the first barrier to integrating palliative care into an ICU, Dr. Cooper said. She paraphrased the World Health Organization’s definition by saying, "Palliative care makes patients feel better." It is specialized medical care that focuses on preventing and relieving symptoms, pain, and stress associated with life-threatening illness – whatever the diagnosis – and is appropriate at any stage in a serious illness.
Typically provided by a team, palliative care may involve physicians, nurses, social workers, pharmacists, chaplains, pain experts, ethicists, rehabilitation therapists, psychiatry consultants, and bereavement counselors. The team can take a load off busy intensivists by handling the often lengthy conversations with patients and families facing life-threatening illness, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Palliative care providers can be embedded in ICUs or in a team that’s available as consultants. "I think we have to do both" models, depending on the needs of individual institutions, said Dr. Cooper.
Once a definition is agreed upon, the next steps to convincing colleagues and administrators to make better use of palliative care are to make it relevant for them and to normalize its presence in the ICU, she said. "Palliative care is just as essential as med management, antibiotics, pharmacology – it’s part of what we do well."
Predicting which patients will die, and when, is difficult. Patient preferences for care or end-of-life treatment often are unclear. The goals of treatment depend on the patient’s condition and must be dynamic. "Is it end-of-life care if we don’t know the patient is dying?" she asked.
One way to consider which ICU patients might benefit from palliative care is to ask, "Would I be surprised if this patient died within a year?" even if discharged from the ICU or the hospital, she suggested.
Four studies in the medical literature separately reported that 20% of Americans die in the hospital after an ICU admission, 80% of deaths in ICUs occur after life support is withdrawn or withheld, nearly half of dying patients receive unwanted therapy, and a majority of dying patients experience pain and suffering, Dr. Cooper said. Five other studies reported high mortality rates in patients with sepsis, acute respiratory distress syndrome, ICU stays longer than 14 days, admission to long-term acute care, or initiation of dialysis in the elderly.
A recent study of 25,558 elderly patients undergoing emergency surgery reported 30-day mortality rates of 37% in those with preexisting do-not-resuscitate (DNR) orders and 22% in those without DNR orders. Major complications occurred in more than 40% in each group (Ann. Surg. 2012;256:453-61). Risk factors increase the likelihood of death, but "all of these patients are experiencing serious illness" and would benefit from palliative care, Dr. Cooper said.
One recent study of 518 patients in three ICUs found good adherence to only two of nine palliative care processes – pain assessment and management. Interdisciplinary family meetings had been held by day 5 in the ICU for less than 20% of patients, and adherence to six other palliative care practices ranged from 8% to 43% (Crit. Care Med. 2012;40:1105-12).
Normalizing palliative care in the ICU means adopting the attitude that "it’s just part of what we do, the same way that we manage our vents, etc." Dr. Cooper said.
Adopting proactive screening criteria (patient factors) that trigger palliative care consultations would reduce utilization of ICUs without increasing mortality, and would increase the availability of palliative care for patients and families, according to a recent report from the Improving Palliative Care in the ICU Project’s advisory board (Crit. Care Med. 2013;41:2318-27).
The triggers should be specific to each ICU and patient population and developed through a process with stakeholders, with outcomes evaluated. "This is not a one-size-fits-all strategy," Dr. Cooper said. "The triggers in the MICU [medical ICU] and the SICU [surgical ICU] cannot be the same. It won’t work. I’ve actually seen that in my own institution," Dr. Cooper said.
The triggers also shouldn’t focus only on the patients most obviously likely to die or they will perpetuate the misconception that palliative care is only for the dying, she added.
To integrate palliative care into an ICU, "just do it," she said. "Commit yourself" to intensive symptom management and multidisciplinary family meetings within 72 hours of ICU admission. Institute an intensive communication plan to provide emotional, educational, and decision support for patients and families. Offer pastoral and psychosocial support. Start end-of-life-care discussions sooner, and provide bereavement services when patients die.
Lastly, don’t hesitate to bill insurers for these services, Dr. Cooper said. In-person or phone meetings about treatment options when the patient lacks the capacity to decide can be billed as critical care, as can discussions about DNR codes. Also bill for treating acute pain, agitation, delirium, and other life-threatening symptoms as critical care.
Dr. Cooper reported having no financial disclosures.
On Twitter @sherryboschert
|
| Dr. Geoffrey P. Dunn |
This is an excellent perspective on the ongoing assimilation of palliative care principles and practices into the venue where it is most needed. Dr. Cooper, who is board certified in hospice and palliative medicine in addition to her surgical certification, is eminently qualified to speak to this topic. She represents a new generation of surgeons who see the potential for palliative care principles and practices for all seriously ill surgical patients.
She is right in suggesting we understand palliative care as a way of caring, not a prognostic indicator. As far back as 1999, intensivist and pulmonologist Judith Nelson argued in a memorable editorial in Annals of Internal Medicine that we should not try to pick and choose who needs palliative care in the ICU setting because prognosis is so hard to determine, but rather meet the comfort and quality of life needs of all ICU patients and their families.
Geoffrey P. Dunn, M.D., an ACS Fellow based in Erie, Pa., is chair of the ACS Surgical Palliative Care Task Force.
|
| Dr. Geoffrey P. Dunn |
This is an excellent perspective on the ongoing assimilation of palliative care principles and practices into the venue where it is most needed. Dr. Cooper, who is board certified in hospice and palliative medicine in addition to her surgical certification, is eminently qualified to speak to this topic. She represents a new generation of surgeons who see the potential for palliative care principles and practices for all seriously ill surgical patients.
She is right in suggesting we understand palliative care as a way of caring, not a prognostic indicator. As far back as 1999, intensivist and pulmonologist Judith Nelson argued in a memorable editorial in Annals of Internal Medicine that we should not try to pick and choose who needs palliative care in the ICU setting because prognosis is so hard to determine, but rather meet the comfort and quality of life needs of all ICU patients and their families.
Geoffrey P. Dunn, M.D., an ACS Fellow based in Erie, Pa., is chair of the ACS Surgical Palliative Care Task Force.
|
| Dr. Geoffrey P. Dunn |
This is an excellent perspective on the ongoing assimilation of palliative care principles and practices into the venue where it is most needed. Dr. Cooper, who is board certified in hospice and palliative medicine in addition to her surgical certification, is eminently qualified to speak to this topic. She represents a new generation of surgeons who see the potential for palliative care principles and practices for all seriously ill surgical patients.
She is right in suggesting we understand palliative care as a way of caring, not a prognostic indicator. As far back as 1999, intensivist and pulmonologist Judith Nelson argued in a memorable editorial in Annals of Internal Medicine that we should not try to pick and choose who needs palliative care in the ICU setting because prognosis is so hard to determine, but rather meet the comfort and quality of life needs of all ICU patients and their families.
Geoffrey P. Dunn, M.D., an ACS Fellow based in Erie, Pa., is chair of the ACS Surgical Palliative Care Task Force.
SAN FRANCISCO – Palliative care is not just for the dying.
Understanding that premise is the first step to integrating palliative care into intensive care units, Dr. Zara Cooper said. Palliative care treats patient illness and can be delivered concurrently in the ICU with curative care that treats disease.
As options for curative treatment decrease, the role of palliative care may increase and does not stop at the patient’s death. "It’s important that we provide ongoing bereavement support not only to family members and survivors but also to caregivers and members of our medical team," added Dr. Cooper, an assistant professor of surgery at Harvard Medical School and a surgical intensivist at Brigham and Women’s Hospital, Boston.
Getting intensive care colleagues to agree on a definition of palliative care is the first barrier to integrating palliative care into an ICU, Dr. Cooper said. She paraphrased the World Health Organization’s definition by saying, "Palliative care makes patients feel better." It is specialized medical care that focuses on preventing and relieving symptoms, pain, and stress associated with life-threatening illness – whatever the diagnosis – and is appropriate at any stage in a serious illness.
Typically provided by a team, palliative care may involve physicians, nurses, social workers, pharmacists, chaplains, pain experts, ethicists, rehabilitation therapists, psychiatry consultants, and bereavement counselors. The team can take a load off busy intensivists by handling the often lengthy conversations with patients and families facing life-threatening illness, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Palliative care providers can be embedded in ICUs or in a team that’s available as consultants. "I think we have to do both" models, depending on the needs of individual institutions, said Dr. Cooper.
Once a definition is agreed upon, the next steps to convincing colleagues and administrators to make better use of palliative care are to make it relevant for them and to normalize its presence in the ICU, she said. "Palliative care is just as essential as med management, antibiotics, pharmacology – it’s part of what we do well."
Predicting which patients will die, and when, is difficult. Patient preferences for care or end-of-life treatment often are unclear. The goals of treatment depend on the patient’s condition and must be dynamic. "Is it end-of-life care if we don’t know the patient is dying?" she asked.
One way to consider which ICU patients might benefit from palliative care is to ask, "Would I be surprised if this patient died within a year?" even if discharged from the ICU or the hospital, she suggested.
Four studies in the medical literature separately reported that 20% of Americans die in the hospital after an ICU admission, 80% of deaths in ICUs occur after life support is withdrawn or withheld, nearly half of dying patients receive unwanted therapy, and a majority of dying patients experience pain and suffering, Dr. Cooper said. Five other studies reported high mortality rates in patients with sepsis, acute respiratory distress syndrome, ICU stays longer than 14 days, admission to long-term acute care, or initiation of dialysis in the elderly.
A recent study of 25,558 elderly patients undergoing emergency surgery reported 30-day mortality rates of 37% in those with preexisting do-not-resuscitate (DNR) orders and 22% in those without DNR orders. Major complications occurred in more than 40% in each group (Ann. Surg. 2012;256:453-61). Risk factors increase the likelihood of death, but "all of these patients are experiencing serious illness" and would benefit from palliative care, Dr. Cooper said.
One recent study of 518 patients in three ICUs found good adherence to only two of nine palliative care processes – pain assessment and management. Interdisciplinary family meetings had been held by day 5 in the ICU for less than 20% of patients, and adherence to six other palliative care practices ranged from 8% to 43% (Crit. Care Med. 2012;40:1105-12).
Normalizing palliative care in the ICU means adopting the attitude that "it’s just part of what we do, the same way that we manage our vents, etc." Dr. Cooper said.
Adopting proactive screening criteria (patient factors) that trigger palliative care consultations would reduce utilization of ICUs without increasing mortality, and would increase the availability of palliative care for patients and families, according to a recent report from the Improving Palliative Care in the ICU Project’s advisory board (Crit. Care Med. 2013;41:2318-27).
The triggers should be specific to each ICU and patient population and developed through a process with stakeholders, with outcomes evaluated. "This is not a one-size-fits-all strategy," Dr. Cooper said. "The triggers in the MICU [medical ICU] and the SICU [surgical ICU] cannot be the same. It won’t work. I’ve actually seen that in my own institution," Dr. Cooper said.
The triggers also shouldn’t focus only on the patients most obviously likely to die or they will perpetuate the misconception that palliative care is only for the dying, she added.
To integrate palliative care into an ICU, "just do it," she said. "Commit yourself" to intensive symptom management and multidisciplinary family meetings within 72 hours of ICU admission. Institute an intensive communication plan to provide emotional, educational, and decision support for patients and families. Offer pastoral and psychosocial support. Start end-of-life-care discussions sooner, and provide bereavement services when patients die.
Lastly, don’t hesitate to bill insurers for these services, Dr. Cooper said. In-person or phone meetings about treatment options when the patient lacks the capacity to decide can be billed as critical care, as can discussions about DNR codes. Also bill for treating acute pain, agitation, delirium, and other life-threatening symptoms as critical care.
Dr. Cooper reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Palliative care is not just for the dying.
Understanding that premise is the first step to integrating palliative care into intensive care units, Dr. Zara Cooper said. Palliative care treats patient illness and can be delivered concurrently in the ICU with curative care that treats disease.
As options for curative treatment decrease, the role of palliative care may increase and does not stop at the patient’s death. "It’s important that we provide ongoing bereavement support not only to family members and survivors but also to caregivers and members of our medical team," added Dr. Cooper, an assistant professor of surgery at Harvard Medical School and a surgical intensivist at Brigham and Women’s Hospital, Boston.
Getting intensive care colleagues to agree on a definition of palliative care is the first barrier to integrating palliative care into an ICU, Dr. Cooper said. She paraphrased the World Health Organization’s definition by saying, "Palliative care makes patients feel better." It is specialized medical care that focuses on preventing and relieving symptoms, pain, and stress associated with life-threatening illness – whatever the diagnosis – and is appropriate at any stage in a serious illness.
Typically provided by a team, palliative care may involve physicians, nurses, social workers, pharmacists, chaplains, pain experts, ethicists, rehabilitation therapists, psychiatry consultants, and bereavement counselors. The team can take a load off busy intensivists by handling the often lengthy conversations with patients and families facing life-threatening illness, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Palliative care providers can be embedded in ICUs or in a team that’s available as consultants. "I think we have to do both" models, depending on the needs of individual institutions, said Dr. Cooper.
Once a definition is agreed upon, the next steps to convincing colleagues and administrators to make better use of palliative care are to make it relevant for them and to normalize its presence in the ICU, she said. "Palliative care is just as essential as med management, antibiotics, pharmacology – it’s part of what we do well."
Predicting which patients will die, and when, is difficult. Patient preferences for care or end-of-life treatment often are unclear. The goals of treatment depend on the patient’s condition and must be dynamic. "Is it end-of-life care if we don’t know the patient is dying?" she asked.
One way to consider which ICU patients might benefit from palliative care is to ask, "Would I be surprised if this patient died within a year?" even if discharged from the ICU or the hospital, she suggested.
Four studies in the medical literature separately reported that 20% of Americans die in the hospital after an ICU admission, 80% of deaths in ICUs occur after life support is withdrawn or withheld, nearly half of dying patients receive unwanted therapy, and a majority of dying patients experience pain and suffering, Dr. Cooper said. Five other studies reported high mortality rates in patients with sepsis, acute respiratory distress syndrome, ICU stays longer than 14 days, admission to long-term acute care, or initiation of dialysis in the elderly.
A recent study of 25,558 elderly patients undergoing emergency surgery reported 30-day mortality rates of 37% in those with preexisting do-not-resuscitate (DNR) orders and 22% in those without DNR orders. Major complications occurred in more than 40% in each group (Ann. Surg. 2012;256:453-61). Risk factors increase the likelihood of death, but "all of these patients are experiencing serious illness" and would benefit from palliative care, Dr. Cooper said.
One recent study of 518 patients in three ICUs found good adherence to only two of nine palliative care processes – pain assessment and management. Interdisciplinary family meetings had been held by day 5 in the ICU for less than 20% of patients, and adherence to six other palliative care practices ranged from 8% to 43% (Crit. Care Med. 2012;40:1105-12).
Normalizing palliative care in the ICU means adopting the attitude that "it’s just part of what we do, the same way that we manage our vents, etc." Dr. Cooper said.
Adopting proactive screening criteria (patient factors) that trigger palliative care consultations would reduce utilization of ICUs without increasing mortality, and would increase the availability of palliative care for patients and families, according to a recent report from the Improving Palliative Care in the ICU Project’s advisory board (Crit. Care Med. 2013;41:2318-27).
The triggers should be specific to each ICU and patient population and developed through a process with stakeholders, with outcomes evaluated. "This is not a one-size-fits-all strategy," Dr. Cooper said. "The triggers in the MICU [medical ICU] and the SICU [surgical ICU] cannot be the same. It won’t work. I’ve actually seen that in my own institution," Dr. Cooper said.
The triggers also shouldn’t focus only on the patients most obviously likely to die or they will perpetuate the misconception that palliative care is only for the dying, she added.
To integrate palliative care into an ICU, "just do it," she said. "Commit yourself" to intensive symptom management and multidisciplinary family meetings within 72 hours of ICU admission. Institute an intensive communication plan to provide emotional, educational, and decision support for patients and families. Offer pastoral and psychosocial support. Start end-of-life-care discussions sooner, and provide bereavement services when patients die.
Lastly, don’t hesitate to bill insurers for these services, Dr. Cooper said. In-person or phone meetings about treatment options when the patient lacks the capacity to decide can be billed as critical care, as can discussions about DNR codes. Also bill for treating acute pain, agitation, delirium, and other life-threatening symptoms as critical care.
Dr. Cooper reported having no financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM THE CRITICAL CARE CONGRESS
Palliative care is not just for the dying
SAN FRANCISCO – Palliative care is not just for the dying.
Understanding that premise is the first step to integrating palliative care into intensive care units, Dr. Zara Cooper said. Palliative care treats patient illness and can be delivered concurrently in the ICU with curative care that treats disease.
As options for curative treatment decrease, the role of palliative care may increase and does not stop at the patient’s death. "It’s important that we provide ongoing bereavement support not only to family members and survivors but also to caregivers and members of our medical team," added Dr. Cooper, an assistant professor of surgery at Harvard Medical School and a surgical intensivist at Brigham and Women’s Hospital, Boston.
Getting intensive care colleagues to agree on a definition of palliative care is the first barrier to integrating palliative care into an ICU, Dr. Cooper said. She paraphrased the World Health Organization’s definition by saying, "Palliative care makes patients feel better." It is specialized medical care that focuses on preventing and relieving symptoms, pain, and stress associated with life-threatening illness – whatever the diagnosis – and is appropriate at any stage in a serious illness.
Typically provided by a team, palliative care may involve physicians, nurses, social workers, pharmacists, chaplains, pain experts, ethicists, rehabilitation therapists, psychiatry consultants, and bereavement counselors. The team can take a load off busy intensivists by handling the often lengthy conversations with patients and families facing life-threatening illness, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Palliative care providers can be embedded in ICUs or in a team that’s available as consultants. "I think we have to do both" models, depending on the needs of individual institutions, said Dr. Cooper.
Once a definition is agreed upon, the next steps to convincing colleagues and administrators to make better use of palliative care are to make it relevant for them and to normalize its presence in the ICU, she said. "Palliative care is just as essential as med management, antibiotics, pharmacology – it’s part of what we do well."
Predicting which patients will die, and when, is difficult. Patient preferences for care or end-of-life treatment often are unclear. The goals of treatment depend on the patient’s condition and must be dynamic. "Is it end-of-life care if we don’t know the patient is dying?" she asked.
One way to consider which ICU patients might benefit from palliative care is to ask, "Would I be surprised if this patient died within a year?" even if discharged from the ICU or the hospital, she suggested.
Four studies in the medical literature separately reported that 20% of Americans die in the hospital after an ICU admission, 80% of deaths in ICUs occur after life support is withdrawn or withheld, nearly half of dying patients receive unwanted therapy, and a majority of dying patients experience pain and suffering, Dr. Cooper said. Five other studies reported high mortality rates in patients with sepsis, acute respiratory distress syndrome, ICU stays longer than 14 days, admission to long-term acute care, or initiation of dialysis in the elderly.
A recent study of 25,558 elderly patients undergoing emergency surgery reported 30-day mortality rates of 37% in those with preexisting do-not-resuscitate (DNR) orders and 22% in those without DNR orders. Major complications occurred in more than 40% in each group (Ann. Surg. 2012;256:453-61). Risk factors increase the likelihood of death, but "all of these patients are experiencing serious illness" and would benefit from palliative care, Dr. Cooper said.
One recent study of 518 patients in three ICUs found good adherence to only two of nine palliative care processes – pain assessment and management. Interdisciplinary family meetings had been held by day 5 in the ICU for less than 20% of patients, and adherence to six other palliative care practices ranged from 8% to 43% (Crit. Care Med. 2012;40:1105-12).
Normalizing palliative care in the ICU means adopting the attitude that "it’s just part of what we do, the same way that we manage our vents, etc." Dr. Cooper said.
Adopting proactive screening criteria (patient factors) that trigger palliative care consultations would reduce utilization of ICUs without increasing mortality, and would increase the availability of palliative care for patients and families, according to a recent report from the Improving Palliative Care in the ICU Project’s advisory board (Crit. Care Med. 2013;41:2318-27).
The triggers should be specific to each ICU and patient population and developed through a process with stakeholders, with outcomes evaluated. "This is not a one-size-fits-all strategy," Dr. Cooper said. "The triggers in the MICU [medical ICU] and the SICU [surgical ICU] cannot be the same. It won’t work. I’ve actually seen that in my own institution," Dr. Cooper said.
The triggers also shouldn’t focus only on the patients most obviously likely to die or they will perpetuate the misconception that palliative care is only for the dying, she added.
To integrate palliative care into an ICU, "just do it," she said. "Commit yourself" to intensive symptom management and multidisciplinary family meetings within 72 hours of ICU admission. Institute an intensive communication plan to provide emotional, educational, and decision support for patients and families. Offer pastoral and psychosocial support. Start end-of-life-care discussions sooner, and provide bereavement services when patients die.
Lastly, don’t hesitate to bill insurers for these services, Dr. Cooper said. In-person or phone meetings about treatment options when the patient lacks the capacity to decide can be billed as critical care, as can discussions about DNR codes. Also bill for treating acute pain, agitation, delirium, and other life-threatening symptoms as critical care.
Dr. Cooper reported having no financial disclosures.
If you’re interested in more about these topics, you can join a discussion on this topic within the Critical Care e-Community. Simply log in to ecommunity.chestnet.org and find the Critical Care group. If you’re not part of the Critical Care NetWork, log in to chestnet.org and add the Critical Care NetWork to your profile.
Questions? Contact [email protected].
On Twitter @sherryboschert
|
| Dr. Geoffrey P. Dunn |
This is an excellent perspective on the ongoing assimilation of palliative care principles and practices into the venue where it is most needed. Dr. Cooper, who is board certified in hospice and palliative medicine in addition to her surgical certification, is eminently qualified to speak to this topic. She represents a new generation of surgeons who see the potential for palliative care principles and practices for all seriously ill surgical patients.
She is right in suggesting we understand palliative care as a way of caring, not a prognostic indicator. As far back as 1999, intensivist and pulmonologist Judith Nelson argued in a memorable editorial in Annals of Internal Medicine that we should not try to pick and choose who needs palliative care in the ICU setting because prognosis is so hard to determine, but rather meet the comfort and quality of life needs of all ICU patients and their families.
Geoffrey P. Dunn, M.D., an ACS Fellow based in Erie, Pa., is chair of the ACS Surgical Palliative Care Task Force.
|
| Dr. Geoffrey P. Dunn |
This is an excellent perspective on the ongoing assimilation of palliative care principles and practices into the venue where it is most needed. Dr. Cooper, who is board certified in hospice and palliative medicine in addition to her surgical certification, is eminently qualified to speak to this topic. She represents a new generation of surgeons who see the potential for palliative care principles and practices for all seriously ill surgical patients.
She is right in suggesting we understand palliative care as a way of caring, not a prognostic indicator. As far back as 1999, intensivist and pulmonologist Judith Nelson argued in a memorable editorial in Annals of Internal Medicine that we should not try to pick and choose who needs palliative care in the ICU setting because prognosis is so hard to determine, but rather meet the comfort and quality of life needs of all ICU patients and their families.
Geoffrey P. Dunn, M.D., an ACS Fellow based in Erie, Pa., is chair of the ACS Surgical Palliative Care Task Force.
|
| Dr. Geoffrey P. Dunn |
This is an excellent perspective on the ongoing assimilation of palliative care principles and practices into the venue where it is most needed. Dr. Cooper, who is board certified in hospice and palliative medicine in addition to her surgical certification, is eminently qualified to speak to this topic. She represents a new generation of surgeons who see the potential for palliative care principles and practices for all seriously ill surgical patients.
She is right in suggesting we understand palliative care as a way of caring, not a prognostic indicator. As far back as 1999, intensivist and pulmonologist Judith Nelson argued in a memorable editorial in Annals of Internal Medicine that we should not try to pick and choose who needs palliative care in the ICU setting because prognosis is so hard to determine, but rather meet the comfort and quality of life needs of all ICU patients and their families.
Geoffrey P. Dunn, M.D., an ACS Fellow based in Erie, Pa., is chair of the ACS Surgical Palliative Care Task Force.
SAN FRANCISCO – Palliative care is not just for the dying.
Understanding that premise is the first step to integrating palliative care into intensive care units, Dr. Zara Cooper said. Palliative care treats patient illness and can be delivered concurrently in the ICU with curative care that treats disease.
As options for curative treatment decrease, the role of palliative care may increase and does not stop at the patient’s death. "It’s important that we provide ongoing bereavement support not only to family members and survivors but also to caregivers and members of our medical team," added Dr. Cooper, an assistant professor of surgery at Harvard Medical School and a surgical intensivist at Brigham and Women’s Hospital, Boston.
Getting intensive care colleagues to agree on a definition of palliative care is the first barrier to integrating palliative care into an ICU, Dr. Cooper said. She paraphrased the World Health Organization’s definition by saying, "Palliative care makes patients feel better." It is specialized medical care that focuses on preventing and relieving symptoms, pain, and stress associated with life-threatening illness – whatever the diagnosis – and is appropriate at any stage in a serious illness.
Typically provided by a team, palliative care may involve physicians, nurses, social workers, pharmacists, chaplains, pain experts, ethicists, rehabilitation therapists, psychiatry consultants, and bereavement counselors. The team can take a load off busy intensivists by handling the often lengthy conversations with patients and families facing life-threatening illness, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Palliative care providers can be embedded in ICUs or in a team that’s available as consultants. "I think we have to do both" models, depending on the needs of individual institutions, said Dr. Cooper.
Once a definition is agreed upon, the next steps to convincing colleagues and administrators to make better use of palliative care are to make it relevant for them and to normalize its presence in the ICU, she said. "Palliative care is just as essential as med management, antibiotics, pharmacology – it’s part of what we do well."
Predicting which patients will die, and when, is difficult. Patient preferences for care or end-of-life treatment often are unclear. The goals of treatment depend on the patient’s condition and must be dynamic. "Is it end-of-life care if we don’t know the patient is dying?" she asked.
One way to consider which ICU patients might benefit from palliative care is to ask, "Would I be surprised if this patient died within a year?" even if discharged from the ICU or the hospital, she suggested.
Four studies in the medical literature separately reported that 20% of Americans die in the hospital after an ICU admission, 80% of deaths in ICUs occur after life support is withdrawn or withheld, nearly half of dying patients receive unwanted therapy, and a majority of dying patients experience pain and suffering, Dr. Cooper said. Five other studies reported high mortality rates in patients with sepsis, acute respiratory distress syndrome, ICU stays longer than 14 days, admission to long-term acute care, or initiation of dialysis in the elderly.
A recent study of 25,558 elderly patients undergoing emergency surgery reported 30-day mortality rates of 37% in those with preexisting do-not-resuscitate (DNR) orders and 22% in those without DNR orders. Major complications occurred in more than 40% in each group (Ann. Surg. 2012;256:453-61). Risk factors increase the likelihood of death, but "all of these patients are experiencing serious illness" and would benefit from palliative care, Dr. Cooper said.
One recent study of 518 patients in three ICUs found good adherence to only two of nine palliative care processes – pain assessment and management. Interdisciplinary family meetings had been held by day 5 in the ICU for less than 20% of patients, and adherence to six other palliative care practices ranged from 8% to 43% (Crit. Care Med. 2012;40:1105-12).
Normalizing palliative care in the ICU means adopting the attitude that "it’s just part of what we do, the same way that we manage our vents, etc." Dr. Cooper said.
Adopting proactive screening criteria (patient factors) that trigger palliative care consultations would reduce utilization of ICUs without increasing mortality, and would increase the availability of palliative care for patients and families, according to a recent report from the Improving Palliative Care in the ICU Project’s advisory board (Crit. Care Med. 2013;41:2318-27).
The triggers should be specific to each ICU and patient population and developed through a process with stakeholders, with outcomes evaluated. "This is not a one-size-fits-all strategy," Dr. Cooper said. "The triggers in the MICU [medical ICU] and the SICU [surgical ICU] cannot be the same. It won’t work. I’ve actually seen that in my own institution," Dr. Cooper said.
The triggers also shouldn’t focus only on the patients most obviously likely to die or they will perpetuate the misconception that palliative care is only for the dying, she added.
To integrate palliative care into an ICU, "just do it," she said. "Commit yourself" to intensive symptom management and multidisciplinary family meetings within 72 hours of ICU admission. Institute an intensive communication plan to provide emotional, educational, and decision support for patients and families. Offer pastoral and psychosocial support. Start end-of-life-care discussions sooner, and provide bereavement services when patients die.
Lastly, don’t hesitate to bill insurers for these services, Dr. Cooper said. In-person or phone meetings about treatment options when the patient lacks the capacity to decide can be billed as critical care, as can discussions about DNR codes. Also bill for treating acute pain, agitation, delirium, and other life-threatening symptoms as critical care.
Dr. Cooper reported having no financial disclosures.
If you’re interested in more about these topics, you can join a discussion on this topic within the Critical Care e-Community. Simply log in to ecommunity.chestnet.org and find the Critical Care group. If you’re not part of the Critical Care NetWork, log in to chestnet.org and add the Critical Care NetWork to your profile.
Questions? Contact [email protected].
On Twitter @sherryboschert
SAN FRANCISCO – Palliative care is not just for the dying.
Understanding that premise is the first step to integrating palliative care into intensive care units, Dr. Zara Cooper said. Palliative care treats patient illness and can be delivered concurrently in the ICU with curative care that treats disease.
As options for curative treatment decrease, the role of palliative care may increase and does not stop at the patient’s death. "It’s important that we provide ongoing bereavement support not only to family members and survivors but also to caregivers and members of our medical team," added Dr. Cooper, an assistant professor of surgery at Harvard Medical School and a surgical intensivist at Brigham and Women’s Hospital, Boston.
Getting intensive care colleagues to agree on a definition of palliative care is the first barrier to integrating palliative care into an ICU, Dr. Cooper said. She paraphrased the World Health Organization’s definition by saying, "Palliative care makes patients feel better." It is specialized medical care that focuses on preventing and relieving symptoms, pain, and stress associated with life-threatening illness – whatever the diagnosis – and is appropriate at any stage in a serious illness.
Typically provided by a team, palliative care may involve physicians, nurses, social workers, pharmacists, chaplains, pain experts, ethicists, rehabilitation therapists, psychiatry consultants, and bereavement counselors. The team can take a load off busy intensivists by handling the often lengthy conversations with patients and families facing life-threatening illness, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Palliative care providers can be embedded in ICUs or in a team that’s available as consultants. "I think we have to do both" models, depending on the needs of individual institutions, said Dr. Cooper.
Once a definition is agreed upon, the next steps to convincing colleagues and administrators to make better use of palliative care are to make it relevant for them and to normalize its presence in the ICU, she said. "Palliative care is just as essential as med management, antibiotics, pharmacology – it’s part of what we do well."
Predicting which patients will die, and when, is difficult. Patient preferences for care or end-of-life treatment often are unclear. The goals of treatment depend on the patient’s condition and must be dynamic. "Is it end-of-life care if we don’t know the patient is dying?" she asked.
One way to consider which ICU patients might benefit from palliative care is to ask, "Would I be surprised if this patient died within a year?" even if discharged from the ICU or the hospital, she suggested.
Four studies in the medical literature separately reported that 20% of Americans die in the hospital after an ICU admission, 80% of deaths in ICUs occur after life support is withdrawn or withheld, nearly half of dying patients receive unwanted therapy, and a majority of dying patients experience pain and suffering, Dr. Cooper said. Five other studies reported high mortality rates in patients with sepsis, acute respiratory distress syndrome, ICU stays longer than 14 days, admission to long-term acute care, or initiation of dialysis in the elderly.
A recent study of 25,558 elderly patients undergoing emergency surgery reported 30-day mortality rates of 37% in those with preexisting do-not-resuscitate (DNR) orders and 22% in those without DNR orders. Major complications occurred in more than 40% in each group (Ann. Surg. 2012;256:453-61). Risk factors increase the likelihood of death, but "all of these patients are experiencing serious illness" and would benefit from palliative care, Dr. Cooper said.
One recent study of 518 patients in three ICUs found good adherence to only two of nine palliative care processes – pain assessment and management. Interdisciplinary family meetings had been held by day 5 in the ICU for less than 20% of patients, and adherence to six other palliative care practices ranged from 8% to 43% (Crit. Care Med. 2012;40:1105-12).
Normalizing palliative care in the ICU means adopting the attitude that "it’s just part of what we do, the same way that we manage our vents, etc." Dr. Cooper said.
Adopting proactive screening criteria (patient factors) that trigger palliative care consultations would reduce utilization of ICUs without increasing mortality, and would increase the availability of palliative care for patients and families, according to a recent report from the Improving Palliative Care in the ICU Project’s advisory board (Crit. Care Med. 2013;41:2318-27).
The triggers should be specific to each ICU and patient population and developed through a process with stakeholders, with outcomes evaluated. "This is not a one-size-fits-all strategy," Dr. Cooper said. "The triggers in the MICU [medical ICU] and the SICU [surgical ICU] cannot be the same. It won’t work. I’ve actually seen that in my own institution," Dr. Cooper said.
The triggers also shouldn’t focus only on the patients most obviously likely to die or they will perpetuate the misconception that palliative care is only for the dying, she added.
To integrate palliative care into an ICU, "just do it," she said. "Commit yourself" to intensive symptom management and multidisciplinary family meetings within 72 hours of ICU admission. Institute an intensive communication plan to provide emotional, educational, and decision support for patients and families. Offer pastoral and psychosocial support. Start end-of-life-care discussions sooner, and provide bereavement services when patients die.
Lastly, don’t hesitate to bill insurers for these services, Dr. Cooper said. In-person or phone meetings about treatment options when the patient lacks the capacity to decide can be billed as critical care, as can discussions about DNR codes. Also bill for treating acute pain, agitation, delirium, and other life-threatening symptoms as critical care.
Dr. Cooper reported having no financial disclosures.
If you’re interested in more about these topics, you can join a discussion on this topic within the Critical Care e-Community. Simply log in to ecommunity.chestnet.org and find the Critical Care group. If you’re not part of the Critical Care NetWork, log in to chestnet.org and add the Critical Care NetWork to your profile.
Questions? Contact [email protected].
On Twitter @sherryboschert
EXPERT ANALYSIS FROM THE CRITICAL CARE CONGRESS
Hypothermia associated with persistent lymphopenia in sepsis
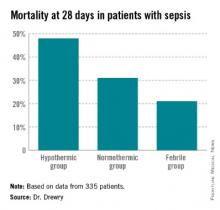
SAN FRANCISCO – Patients with sepsis had significantly higher rates of persistent lymphopenia, 28-day mortality, and 1-year mortality if they were hypothermic, compared with normothermic patients in a small retrospective study.
In the study, 32 of 58 septic patients who were hypothermic within 24 hours of their blood cultures developed persistent lymphopenia (55%), compared with 43% of 183 normothermic patients and 48% of 204 febrile patients.
Dr. Anne Drewry reported that hypothermia was associated with a nearly tripled risk for persistent lymphopenia (odds ratio, 2.7) compared with normothermic patients in a multivariate logistic regression analysis to account for confounding variables. The likelihood of persistent lymphopenia in febrile patients was not significantly different from that of normothermic patients.
The significantly higher risk of persistent lymphopenia in patients with hypothermia compared with normothermia was accompanied by significantly higher risk for some secondary adverse outcomes in the observational cohort study, she reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Thirty-nine hypothermic patients developed septic shock (67%), compared with 55% of normothermic patients and 47% of febrile patients.
Mortality rates at 28 days were 48% in the hypothermic group (28 patients), 31% in the normothermic group, and 21% in the febrile group (which was significantly lower compared with the normothermic patients). At 1 year, 35 hypothermic patients had died (60%) compared with 45% of normothermic patients and 39% of febrile patients, she said.
"Hypothermic patients may be candidates for early treatment with agents that reverse sepsis-induced lymphopenia in future clinical trials," said Dr. Drewry of Washington University, St. Louis.
She and her associates studied data on 455 patients hospitalized between January 2010 and July 2012 and diagnosed with sepsis, and whose blood cultures were positive for bacterial or fungal organisms within 5 days of admission. They considered patients to be hypothermic if their most extreme temperature values within the first 24 hours of blood cultures were less than 36° C and to be febrile if the temperature values were 38.3° C or higher.
Data on 335 patients were analyzed for the primary outcome of persistent lymphopenia, not counting 110 patients who died or were discharged prior to day 4 after sepsis diagnosis or who had no blood counts drawn on day 4.
Mean APACHE II (Acute Physiology and Chronic Health Evaluation II) scores at baseline were 22 in the hypothermic group, significantly higher than the mean score of 16 in normothermic patients and 17 in febrile patients. Higher APACHE II scores were the only variable besides hypothermia to be significantly associated with increased risk of persistent lymphopenia; higher scores conferred a 7% increase in risk.
Hypothermic patients were significantly more likely to be infected with gram-negative organisms (50%) than were normothermic patients (36%) or febrile patients (34%).
The three groups did not differ significantly in rates of acute kidney injury, secondary infection, or need for mechanical ventilation, among secondary outcomes in a univariate analysis. Factors that were not significantly associated with persistent lymphopenia risk in the multivariable analysis included the presence of comorbidity and the type of organism (gram-positive, gram-negative, fungal, or polymicrobial).
Hypothermia occurs in 10%-25% of critically ill patients with sepsis, Dr. Drewry said. A prior study by other investigators suggested that severely septic patients with hypothermia are older, have more severe disease, and are at higher risk of death than normothermic or febrile patients (Crit. Care 2013;17:R271).
"Previous data from our group suggests that persistent lymphopenia predicts mortality and secondary infection in septic patients and may be a marker for sepsis-induced immunosuppression" even after accounting for possible confounders, Dr. Drewry said.
It’s unclear why some patients don’t mount a fever in response to infection and why these patients have worse outcomes, she added. "Our overarching hypothesis is that hypothermia in response to infection is a sign of an underlying predisposition to sepsis-induced immunosuppression."
The study excluded patients diagnosed with hematological or immunological disease and patients treated with chemotherapy or corticosteroids while hospitalized or within 6 months before admission.
Dr. Drewry reported having no financial disclosures.
[email protected] On Twitter @sherryboschert
SAN FRANCISCO – Patients with sepsis had significantly higher rates of persistent lymphopenia, 28-day mortality, and 1-year mortality if they were hypothermic, compared with normothermic patients in a small retrospective study.
In the study, 32 of 58 septic patients who were hypothermic within 24 hours of their blood cultures developed persistent lymphopenia (55%), compared with 43% of 183 normothermic patients and 48% of 204 febrile patients.
Dr. Anne Drewry reported that hypothermia was associated with a nearly tripled risk for persistent lymphopenia (odds ratio, 2.7) compared with normothermic patients in a multivariate logistic regression analysis to account for confounding variables. The likelihood of persistent lymphopenia in febrile patients was not significantly different from that of normothermic patients.
The significantly higher risk of persistent lymphopenia in patients with hypothermia compared with normothermia was accompanied by significantly higher risk for some secondary adverse outcomes in the observational cohort study, she reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Thirty-nine hypothermic patients developed septic shock (67%), compared with 55% of normothermic patients and 47% of febrile patients.
Mortality rates at 28 days were 48% in the hypothermic group (28 patients), 31% in the normothermic group, and 21% in the febrile group (which was significantly lower compared with the normothermic patients). At 1 year, 35 hypothermic patients had died (60%) compared with 45% of normothermic patients and 39% of febrile patients, she said.
"Hypothermic patients may be candidates for early treatment with agents that reverse sepsis-induced lymphopenia in future clinical trials," said Dr. Drewry of Washington University, St. Louis.
She and her associates studied data on 455 patients hospitalized between January 2010 and July 2012 and diagnosed with sepsis, and whose blood cultures were positive for bacterial or fungal organisms within 5 days of admission. They considered patients to be hypothermic if their most extreme temperature values within the first 24 hours of blood cultures were less than 36° C and to be febrile if the temperature values were 38.3° C or higher.
Data on 335 patients were analyzed for the primary outcome of persistent lymphopenia, not counting 110 patients who died or were discharged prior to day 4 after sepsis diagnosis or who had no blood counts drawn on day 4.
Mean APACHE II (Acute Physiology and Chronic Health Evaluation II) scores at baseline were 22 in the hypothermic group, significantly higher than the mean score of 16 in normothermic patients and 17 in febrile patients. Higher APACHE II scores were the only variable besides hypothermia to be significantly associated with increased risk of persistent lymphopenia; higher scores conferred a 7% increase in risk.
Hypothermic patients were significantly more likely to be infected with gram-negative organisms (50%) than were normothermic patients (36%) or febrile patients (34%).
The three groups did not differ significantly in rates of acute kidney injury, secondary infection, or need for mechanical ventilation, among secondary outcomes in a univariate analysis. Factors that were not significantly associated with persistent lymphopenia risk in the multivariable analysis included the presence of comorbidity and the type of organism (gram-positive, gram-negative, fungal, or polymicrobial).
Hypothermia occurs in 10%-25% of critically ill patients with sepsis, Dr. Drewry said. A prior study by other investigators suggested that severely septic patients with hypothermia are older, have more severe disease, and are at higher risk of death than normothermic or febrile patients (Crit. Care 2013;17:R271).
"Previous data from our group suggests that persistent lymphopenia predicts mortality and secondary infection in septic patients and may be a marker for sepsis-induced immunosuppression" even after accounting for possible confounders, Dr. Drewry said.
It’s unclear why some patients don’t mount a fever in response to infection and why these patients have worse outcomes, she added. "Our overarching hypothesis is that hypothermia in response to infection is a sign of an underlying predisposition to sepsis-induced immunosuppression."
The study excluded patients diagnosed with hematological or immunological disease and patients treated with chemotherapy or corticosteroids while hospitalized or within 6 months before admission.
Dr. Drewry reported having no financial disclosures.
[email protected] On Twitter @sherryboschert
SAN FRANCISCO – Patients with sepsis had significantly higher rates of persistent lymphopenia, 28-day mortality, and 1-year mortality if they were hypothermic, compared with normothermic patients in a small retrospective study.
In the study, 32 of 58 septic patients who were hypothermic within 24 hours of their blood cultures developed persistent lymphopenia (55%), compared with 43% of 183 normothermic patients and 48% of 204 febrile patients.
Dr. Anne Drewry reported that hypothermia was associated with a nearly tripled risk for persistent lymphopenia (odds ratio, 2.7) compared with normothermic patients in a multivariate logistic regression analysis to account for confounding variables. The likelihood of persistent lymphopenia in febrile patients was not significantly different from that of normothermic patients.
The significantly higher risk of persistent lymphopenia in patients with hypothermia compared with normothermia was accompanied by significantly higher risk for some secondary adverse outcomes in the observational cohort study, she reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Thirty-nine hypothermic patients developed septic shock (67%), compared with 55% of normothermic patients and 47% of febrile patients.
Mortality rates at 28 days were 48% in the hypothermic group (28 patients), 31% in the normothermic group, and 21% in the febrile group (which was significantly lower compared with the normothermic patients). At 1 year, 35 hypothermic patients had died (60%) compared with 45% of normothermic patients and 39% of febrile patients, she said.
"Hypothermic patients may be candidates for early treatment with agents that reverse sepsis-induced lymphopenia in future clinical trials," said Dr. Drewry of Washington University, St. Louis.
She and her associates studied data on 455 patients hospitalized between January 2010 and July 2012 and diagnosed with sepsis, and whose blood cultures were positive for bacterial or fungal organisms within 5 days of admission. They considered patients to be hypothermic if their most extreme temperature values within the first 24 hours of blood cultures were less than 36° C and to be febrile if the temperature values were 38.3° C or higher.
Data on 335 patients were analyzed for the primary outcome of persistent lymphopenia, not counting 110 patients who died or were discharged prior to day 4 after sepsis diagnosis or who had no blood counts drawn on day 4.
Mean APACHE II (Acute Physiology and Chronic Health Evaluation II) scores at baseline were 22 in the hypothermic group, significantly higher than the mean score of 16 in normothermic patients and 17 in febrile patients. Higher APACHE II scores were the only variable besides hypothermia to be significantly associated with increased risk of persistent lymphopenia; higher scores conferred a 7% increase in risk.
Hypothermic patients were significantly more likely to be infected with gram-negative organisms (50%) than were normothermic patients (36%) or febrile patients (34%).
The three groups did not differ significantly in rates of acute kidney injury, secondary infection, or need for mechanical ventilation, among secondary outcomes in a univariate analysis. Factors that were not significantly associated with persistent lymphopenia risk in the multivariable analysis included the presence of comorbidity and the type of organism (gram-positive, gram-negative, fungal, or polymicrobial).
Hypothermia occurs in 10%-25% of critically ill patients with sepsis, Dr. Drewry said. A prior study by other investigators suggested that severely septic patients with hypothermia are older, have more severe disease, and are at higher risk of death than normothermic or febrile patients (Crit. Care 2013;17:R271).
"Previous data from our group suggests that persistent lymphopenia predicts mortality and secondary infection in septic patients and may be a marker for sepsis-induced immunosuppression" even after accounting for possible confounders, Dr. Drewry said.
It’s unclear why some patients don’t mount a fever in response to infection and why these patients have worse outcomes, she added. "Our overarching hypothesis is that hypothermia in response to infection is a sign of an underlying predisposition to sepsis-induced immunosuppression."
The study excluded patients diagnosed with hematological or immunological disease and patients treated with chemotherapy or corticosteroids while hospitalized or within 6 months before admission.
Dr. Drewry reported having no financial disclosures.
[email protected] On Twitter @sherryboschert
AT THE CRITICAL CARE CONGRESS
Major finding: Persistent lymphopenia occurred in 55% of hypothermic patients, 43% of normothermic, and 48% of febrile patients with sepsis.
Data source: A retrospective, observational cohort study of 455 hospitalized patients diagnosed with sepsis.
Disclosures: Dr. Drewry reported having no financial disclosures.
Sepsis resuscitation reduces mortality, even after 6 hours
SAN FRANCISCO – Meeting the goals of the Surviving Sepsis Campaign’s resuscitation care bundle significantly decreased the risk for in-hospital mortality, even when the goals were met beyond the recommended 6-hour window after diagnosis of severe sepsis, a study of 395 patients found.
In-hospital mortality rates were 88% lower in the 85 patients who met the resuscitation bundle goals 6-18 hours after diagnosis and 55% lower in the 95 patients who met the goals within the desired 6 hours after diagnosis compared with 216 patients who did not reach the goals within 18 hours of diagnosis, Dr. Zerihun A. Bunaye reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
For resuscitation care in severe sepsis, it’s better late than never, he said. "Definitely this is showing that there’s a benefit if we continue to aggressively resuscitate the patients beyond 6 hours and try to achieve the goals," said Dr. Bunaye of Mercy Hospital, St. Louis. The lead investigator in the study was Dr. Farid Sadaka, also of the hospital.
Better survival in the group that complied with resuscitation bundle goals in 6-18 hours compared with the 6-hour compliance group surprised the investigators and may be due to several confounding factors that were not analyzed in the study, he said.
The Surviving Sepsis Campaign recommends two sets of "bundles" of care (sets of elements of care selected from evidence-based practice guidelines that have an effect on outcomes when implemented as a group that’s beyond the effect of individual implementation), some to be completed within 3 hours and other goals to be met within 6 hours.
The resuscitation bundle of care aims to prescribe appropriate antibiotics within 3 hours and within 6 hours to get the patient’s mean arterial pressure above 65 mm Hg, get central venous pressure above 8 mm Hg, achieve central venous oxygen saturation greater than 70%, and measure lactic acid, Dr. Bunaye said.
The investigators prospectively collected data as part of a performance improvement project with feedback mechanisms for alerting physicians when bundle goals were not being met so they could continue efforts to meet the goals beyond the recommended deadlines.
The study included patients with septic shock treated between July 2011 and January 2013 in a 54-bed ICU at the large university-affiliated hospital. It compared compliance with the resuscitation bundles within 18 hours of diagnosis and survival rates during approximately 31 days in the hospital.
Compared with the 54% of cases that did not comply with the resuscitation bundles within 18 hours, the hazard ratio for mortality was 0.45 in the 24% of cases that complied within 6 hours and 0.12 in the 22% that complied within 18 hours, Dr. Bunaye reported. Patients in the three groups did not differ significantly at baseline by age, weight, or Sequential Organ Failure Assessment score.
Previous studies have suggested that only 30%-40% of hospitals adhere to the Surviving Sepsis Campaign guidelines. The current study suggests that continuing efforts to meet the goals beyond 6 hours are beneficial, he said.
The findings are limited by the small sample size and the focus on a single institution. The study also did not account for potential confounding variables.
Severe sepsis in the United States is more common than AIDS, colon cancer, and breast cancer combined and is the leading cause of death in noncoronary ICUs, the literature suggests. The United States sees more than 500,000 cases of severe sepsis and septic shock each year, leading to death in 20% of patients with severe sepsis and 45% of those with septic shock, Dr. Bunaye said.
The investigators reported that they have no relevant financial disclosures.
Data suggest better late than never
Dr. Steven Q. Simpson, FCCP, comments: It is very encouraging to see that benefit accrues to patients who meet SSC (and National Quality Forum) bundle goals for physiological parameters, even if they are not met until later in the course of severe sepsis treatment. It seems a bit paradoxical that those who meet physiological goals between 6 and 16 hours after presentation have a higher mortality reduction than those who meet goals within 6 hours. Unfortunately, the study was not set up to determine how or why that may have happened, and whether the phenomenon is real.
The key point, though, is that these are valid goals to work toward in patients with severe sepsis and septic shock, and that we should follow through even when we miss the 6-hour time frame.
On Twitter @sherryboschert
SAN FRANCISCO – Meeting the goals of the Surviving Sepsis Campaign’s resuscitation care bundle significantly decreased the risk for in-hospital mortality, even when the goals were met beyond the recommended 6-hour window after diagnosis of severe sepsis, a study of 395 patients found.
In-hospital mortality rates were 88% lower in the 85 patients who met the resuscitation bundle goals 6-18 hours after diagnosis and 55% lower in the 95 patients who met the goals within the desired 6 hours after diagnosis compared with 216 patients who did not reach the goals within 18 hours of diagnosis, Dr. Zerihun A. Bunaye reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
For resuscitation care in severe sepsis, it’s better late than never, he said. "Definitely this is showing that there’s a benefit if we continue to aggressively resuscitate the patients beyond 6 hours and try to achieve the goals," said Dr. Bunaye of Mercy Hospital, St. Louis. The lead investigator in the study was Dr. Farid Sadaka, also of the hospital.
Better survival in the group that complied with resuscitation bundle goals in 6-18 hours compared with the 6-hour compliance group surprised the investigators and may be due to several confounding factors that were not analyzed in the study, he said.
The Surviving Sepsis Campaign recommends two sets of "bundles" of care (sets of elements of care selected from evidence-based practice guidelines that have an effect on outcomes when implemented as a group that’s beyond the effect of individual implementation), some to be completed within 3 hours and other goals to be met within 6 hours.
The resuscitation bundle of care aims to prescribe appropriate antibiotics within 3 hours and within 6 hours to get the patient’s mean arterial pressure above 65 mm Hg, get central venous pressure above 8 mm Hg, achieve central venous oxygen saturation greater than 70%, and measure lactic acid, Dr. Bunaye said.
The investigators prospectively collected data as part of a performance improvement project with feedback mechanisms for alerting physicians when bundle goals were not being met so they could continue efforts to meet the goals beyond the recommended deadlines.
The study included patients with septic shock treated between July 2011 and January 2013 in a 54-bed ICU at the large university-affiliated hospital. It compared compliance with the resuscitation bundles within 18 hours of diagnosis and survival rates during approximately 31 days in the hospital.
Compared with the 54% of cases that did not comply with the resuscitation bundles within 18 hours, the hazard ratio for mortality was 0.45 in the 24% of cases that complied within 6 hours and 0.12 in the 22% that complied within 18 hours, Dr. Bunaye reported. Patients in the three groups did not differ significantly at baseline by age, weight, or Sequential Organ Failure Assessment score.
Previous studies have suggested that only 30%-40% of hospitals adhere to the Surviving Sepsis Campaign guidelines. The current study suggests that continuing efforts to meet the goals beyond 6 hours are beneficial, he said.
The findings are limited by the small sample size and the focus on a single institution. The study also did not account for potential confounding variables.
Severe sepsis in the United States is more common than AIDS, colon cancer, and breast cancer combined and is the leading cause of death in noncoronary ICUs, the literature suggests. The United States sees more than 500,000 cases of severe sepsis and septic shock each year, leading to death in 20% of patients with severe sepsis and 45% of those with septic shock, Dr. Bunaye said.
The investigators reported that they have no relevant financial disclosures.
Data suggest better late than never
Dr. Steven Q. Simpson, FCCP, comments: It is very encouraging to see that benefit accrues to patients who meet SSC (and National Quality Forum) bundle goals for physiological parameters, even if they are not met until later in the course of severe sepsis treatment. It seems a bit paradoxical that those who meet physiological goals between 6 and 16 hours after presentation have a higher mortality reduction than those who meet goals within 6 hours. Unfortunately, the study was not set up to determine how or why that may have happened, and whether the phenomenon is real.
The key point, though, is that these are valid goals to work toward in patients with severe sepsis and septic shock, and that we should follow through even when we miss the 6-hour time frame.
On Twitter @sherryboschert
SAN FRANCISCO – Meeting the goals of the Surviving Sepsis Campaign’s resuscitation care bundle significantly decreased the risk for in-hospital mortality, even when the goals were met beyond the recommended 6-hour window after diagnosis of severe sepsis, a study of 395 patients found.
In-hospital mortality rates were 88% lower in the 85 patients who met the resuscitation bundle goals 6-18 hours after diagnosis and 55% lower in the 95 patients who met the goals within the desired 6 hours after diagnosis compared with 216 patients who did not reach the goals within 18 hours of diagnosis, Dr. Zerihun A. Bunaye reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
For resuscitation care in severe sepsis, it’s better late than never, he said. "Definitely this is showing that there’s a benefit if we continue to aggressively resuscitate the patients beyond 6 hours and try to achieve the goals," said Dr. Bunaye of Mercy Hospital, St. Louis. The lead investigator in the study was Dr. Farid Sadaka, also of the hospital.
Better survival in the group that complied with resuscitation bundle goals in 6-18 hours compared with the 6-hour compliance group surprised the investigators and may be due to several confounding factors that were not analyzed in the study, he said.
The Surviving Sepsis Campaign recommends two sets of "bundles" of care (sets of elements of care selected from evidence-based practice guidelines that have an effect on outcomes when implemented as a group that’s beyond the effect of individual implementation), some to be completed within 3 hours and other goals to be met within 6 hours.
The resuscitation bundle of care aims to prescribe appropriate antibiotics within 3 hours and within 6 hours to get the patient’s mean arterial pressure above 65 mm Hg, get central venous pressure above 8 mm Hg, achieve central venous oxygen saturation greater than 70%, and measure lactic acid, Dr. Bunaye said.
The investigators prospectively collected data as part of a performance improvement project with feedback mechanisms for alerting physicians when bundle goals were not being met so they could continue efforts to meet the goals beyond the recommended deadlines.
The study included patients with septic shock treated between July 2011 and January 2013 in a 54-bed ICU at the large university-affiliated hospital. It compared compliance with the resuscitation bundles within 18 hours of diagnosis and survival rates during approximately 31 days in the hospital.
Compared with the 54% of cases that did not comply with the resuscitation bundles within 18 hours, the hazard ratio for mortality was 0.45 in the 24% of cases that complied within 6 hours and 0.12 in the 22% that complied within 18 hours, Dr. Bunaye reported. Patients in the three groups did not differ significantly at baseline by age, weight, or Sequential Organ Failure Assessment score.
Previous studies have suggested that only 30%-40% of hospitals adhere to the Surviving Sepsis Campaign guidelines. The current study suggests that continuing efforts to meet the goals beyond 6 hours are beneficial, he said.
The findings are limited by the small sample size and the focus on a single institution. The study also did not account for potential confounding variables.
Severe sepsis in the United States is more common than AIDS, colon cancer, and breast cancer combined and is the leading cause of death in noncoronary ICUs, the literature suggests. The United States sees more than 500,000 cases of severe sepsis and septic shock each year, leading to death in 20% of patients with severe sepsis and 45% of those with septic shock, Dr. Bunaye said.
The investigators reported that they have no relevant financial disclosures.
Data suggest better late than never
Dr. Steven Q. Simpson, FCCP, comments: It is very encouraging to see that benefit accrues to patients who meet SSC (and National Quality Forum) bundle goals for physiological parameters, even if they are not met until later in the course of severe sepsis treatment. It seems a bit paradoxical that those who meet physiological goals between 6 and 16 hours after presentation have a higher mortality reduction than those who meet goals within 6 hours. Unfortunately, the study was not set up to determine how or why that may have happened, and whether the phenomenon is real.
The key point, though, is that these are valid goals to work toward in patients with severe sepsis and septic shock, and that we should follow through even when we miss the 6-hour time frame.
On Twitter @sherryboschert
Major finding: The risk for death during hospitalization was 55% lower in patients who met resuscitation bundle goals within 6 hours and 88% lower in patients who met the goals in 6-18 hours compared with those who did not reach the goals within 18 hours.
Data source: An observational study of 395 patients with severe sepsis at a single institution.
Disclosures: Financial disclosures for the investigators were not available at press time.
Sepsis less common, less deadly in pregnancy
SAN FRANCISCO – The incidence of severe sepsis was nearly five times lower and the risk of death from severe sepsis was 43% lower during pregnancy, compared with nonpregnant women, in a large retrospective study of data on more than 47 million pregnancy-related discharges.
The decreased mortality rate in pregnancy remained after investigators controlled for the effects of age, comorbidities, and severity of illness, Dr. Gagan Kumar reported.
The incidence of sepsis in pregnancy increased fourfold from 2000 to 2009 – from 0.01% to 0.04% – and tripled in nonpregnant women – from 0.06% to 0.18% – while the U.S. pregnancy rate and the rate of hospitalizations during pregnancy remained relatively stable during that period, he said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
In-hospital mortality from severe sepsis decreased gradually for nonpregnant patients from about 30% in 2000 to approximately 18% in 2009, but remained relatively stable in pregnant patients, increasing from approximately 3% in 2000 to 10% in 2009, he said.
The investigators studied claims data from 2000 to 2009 from the Nationwide Inpatient Sample for 47,027,806 pregnancy-related discharges of women aged 15-44 years. Of these, 0.03% had a diagnosis of severe sepsis. Among all cases of severe sepsis in the cohort, 2.4% were during pregnancy (643,417 cases).
Eight percent of pregnant women with severe sepsis died, compared with 22% of nonpregnant women with severe sepsis, a significant difference. The median time to death was significantly longer in pregnancy (10 days) than without pregnancy (8.5 days). The median length of stay was significantly shorter in pregnant women who survived severe sepsis (8 days), compared with nonpregnant survivors (11 days). Pregnant survivors were more likely to be discharged home and less likely to go to a skilled nursing facility or have home care compared with nonpregnant survivors, reported Dr. Kumar of the Medical College of Wisconsin, Milwaukee.
Compared with nonpregnant women, pregnant women were significantly less likely to have three or more organs fail (16% vs. 22%) or to have cardiac, renal, hepatic, hematologic, metabolic, or neurologic failure. Pregnant women were significantly more likely to have respiratory failure than were nonpregnant women.
The likelihood of dying of severe sepsis was 62% lower in pregnant women, compared with nonpregnant women, in an unadjusted analysis and 41%-43% lower than in nonpregnant women under three separate analyses that adjusted for various risk factors or incorporated matched data, Dr. Kumar said.
Although the rate of in-hospital mortality decreased in nonpregnant women from approximately 30% in 2000 to approximately 18% in 2009, the rate increased in pregnant women from approximately 4% in 2000 to 10% in 2009.
Published data are limited and suggested that sepsis in pregnancy is rare, affecting approximately 0.1% of pregnancies, with septic shock in approximately 0.01%-0.001%. These studies relied predominantly on single centers, and used varying definitions of severe sepsis; most were conducted before the year 2000. Since then, the average age of mothers in pregnancy has risen, invasive tests are more common, the rate of cesarean deliveries increased by 7% per year between 1996 and 2011, and the rates of comorbidities such as obesity and diabetes during pregnancy have increased, he said.
Pregnant patients with severe sepsis were 7 years younger on average (27 years of age), compared with nonpregnant women with severe sepsis (age 34 years). Severe sepsis in pregnancy was significantly more common in Hispanics (17%) and Asians (4%), compared with nonpregnant patients (9% and 2%, respectively). Pregnant patients with severe sepsis also had less comorbidity, obesity, and atrial fibrillation, compared with nonpregnant patients with severe sepsis.
Previously Dr. Kumar and his associates reported that the rate of hospitalizations for severe sepsis increased from 143/100,000 persons in 2000 to 343/100,000 in 2007, while mortality rates from severe sepsis decreased from 39% to 27% (Chest 2011;40:1223-31).
The findings of the current study raise questions worth pursuing in future studies, he said, such as the reasons for rising rates of severe sepsis in pregnancy despite no increase in pregnancies or hospitalizations during pregnancy. Pregnancy is considered an immunocompromised state, so why are incidence and mortality rates for severe sepsis lower in pregnancy? he asked. And why has mortality from severe sepsis in pregnancy not improved over the past 10 years?
Dr. Kumar reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – The incidence of severe sepsis was nearly five times lower and the risk of death from severe sepsis was 43% lower during pregnancy, compared with nonpregnant women, in a large retrospective study of data on more than 47 million pregnancy-related discharges.
The decreased mortality rate in pregnancy remained after investigators controlled for the effects of age, comorbidities, and severity of illness, Dr. Gagan Kumar reported.
The incidence of sepsis in pregnancy increased fourfold from 2000 to 2009 – from 0.01% to 0.04% – and tripled in nonpregnant women – from 0.06% to 0.18% – while the U.S. pregnancy rate and the rate of hospitalizations during pregnancy remained relatively stable during that period, he said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
In-hospital mortality from severe sepsis decreased gradually for nonpregnant patients from about 30% in 2000 to approximately 18% in 2009, but remained relatively stable in pregnant patients, increasing from approximately 3% in 2000 to 10% in 2009, he said.
The investigators studied claims data from 2000 to 2009 from the Nationwide Inpatient Sample for 47,027,806 pregnancy-related discharges of women aged 15-44 years. Of these, 0.03% had a diagnosis of severe sepsis. Among all cases of severe sepsis in the cohort, 2.4% were during pregnancy (643,417 cases).
Eight percent of pregnant women with severe sepsis died, compared with 22% of nonpregnant women with severe sepsis, a significant difference. The median time to death was significantly longer in pregnancy (10 days) than without pregnancy (8.5 days). The median length of stay was significantly shorter in pregnant women who survived severe sepsis (8 days), compared with nonpregnant survivors (11 days). Pregnant survivors were more likely to be discharged home and less likely to go to a skilled nursing facility or have home care compared with nonpregnant survivors, reported Dr. Kumar of the Medical College of Wisconsin, Milwaukee.
Compared with nonpregnant women, pregnant women were significantly less likely to have three or more organs fail (16% vs. 22%) or to have cardiac, renal, hepatic, hematologic, metabolic, or neurologic failure. Pregnant women were significantly more likely to have respiratory failure than were nonpregnant women.
The likelihood of dying of severe sepsis was 62% lower in pregnant women, compared with nonpregnant women, in an unadjusted analysis and 41%-43% lower than in nonpregnant women under three separate analyses that adjusted for various risk factors or incorporated matched data, Dr. Kumar said.
Although the rate of in-hospital mortality decreased in nonpregnant women from approximately 30% in 2000 to approximately 18% in 2009, the rate increased in pregnant women from approximately 4% in 2000 to 10% in 2009.
Published data are limited and suggested that sepsis in pregnancy is rare, affecting approximately 0.1% of pregnancies, with septic shock in approximately 0.01%-0.001%. These studies relied predominantly on single centers, and used varying definitions of severe sepsis; most were conducted before the year 2000. Since then, the average age of mothers in pregnancy has risen, invasive tests are more common, the rate of cesarean deliveries increased by 7% per year between 1996 and 2011, and the rates of comorbidities such as obesity and diabetes during pregnancy have increased, he said.
Pregnant patients with severe sepsis were 7 years younger on average (27 years of age), compared with nonpregnant women with severe sepsis (age 34 years). Severe sepsis in pregnancy was significantly more common in Hispanics (17%) and Asians (4%), compared with nonpregnant patients (9% and 2%, respectively). Pregnant patients with severe sepsis also had less comorbidity, obesity, and atrial fibrillation, compared with nonpregnant patients with severe sepsis.
Previously Dr. Kumar and his associates reported that the rate of hospitalizations for severe sepsis increased from 143/100,000 persons in 2000 to 343/100,000 in 2007, while mortality rates from severe sepsis decreased from 39% to 27% (Chest 2011;40:1223-31).
The findings of the current study raise questions worth pursuing in future studies, he said, such as the reasons for rising rates of severe sepsis in pregnancy despite no increase in pregnancies or hospitalizations during pregnancy. Pregnancy is considered an immunocompromised state, so why are incidence and mortality rates for severe sepsis lower in pregnancy? he asked. And why has mortality from severe sepsis in pregnancy not improved over the past 10 years?
Dr. Kumar reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – The incidence of severe sepsis was nearly five times lower and the risk of death from severe sepsis was 43% lower during pregnancy, compared with nonpregnant women, in a large retrospective study of data on more than 47 million pregnancy-related discharges.
The decreased mortality rate in pregnancy remained after investigators controlled for the effects of age, comorbidities, and severity of illness, Dr. Gagan Kumar reported.
The incidence of sepsis in pregnancy increased fourfold from 2000 to 2009 – from 0.01% to 0.04% – and tripled in nonpregnant women – from 0.06% to 0.18% – while the U.S. pregnancy rate and the rate of hospitalizations during pregnancy remained relatively stable during that period, he said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
In-hospital mortality from severe sepsis decreased gradually for nonpregnant patients from about 30% in 2000 to approximately 18% in 2009, but remained relatively stable in pregnant patients, increasing from approximately 3% in 2000 to 10% in 2009, he said.
The investigators studied claims data from 2000 to 2009 from the Nationwide Inpatient Sample for 47,027,806 pregnancy-related discharges of women aged 15-44 years. Of these, 0.03% had a diagnosis of severe sepsis. Among all cases of severe sepsis in the cohort, 2.4% were during pregnancy (643,417 cases).
Eight percent of pregnant women with severe sepsis died, compared with 22% of nonpregnant women with severe sepsis, a significant difference. The median time to death was significantly longer in pregnancy (10 days) than without pregnancy (8.5 days). The median length of stay was significantly shorter in pregnant women who survived severe sepsis (8 days), compared with nonpregnant survivors (11 days). Pregnant survivors were more likely to be discharged home and less likely to go to a skilled nursing facility or have home care compared with nonpregnant survivors, reported Dr. Kumar of the Medical College of Wisconsin, Milwaukee.
Compared with nonpregnant women, pregnant women were significantly less likely to have three or more organs fail (16% vs. 22%) or to have cardiac, renal, hepatic, hematologic, metabolic, or neurologic failure. Pregnant women were significantly more likely to have respiratory failure than were nonpregnant women.
The likelihood of dying of severe sepsis was 62% lower in pregnant women, compared with nonpregnant women, in an unadjusted analysis and 41%-43% lower than in nonpregnant women under three separate analyses that adjusted for various risk factors or incorporated matched data, Dr. Kumar said.
Although the rate of in-hospital mortality decreased in nonpregnant women from approximately 30% in 2000 to approximately 18% in 2009, the rate increased in pregnant women from approximately 4% in 2000 to 10% in 2009.
Published data are limited and suggested that sepsis in pregnancy is rare, affecting approximately 0.1% of pregnancies, with septic shock in approximately 0.01%-0.001%. These studies relied predominantly on single centers, and used varying definitions of severe sepsis; most were conducted before the year 2000. Since then, the average age of mothers in pregnancy has risen, invasive tests are more common, the rate of cesarean deliveries increased by 7% per year between 1996 and 2011, and the rates of comorbidities such as obesity and diabetes during pregnancy have increased, he said.
Pregnant patients with severe sepsis were 7 years younger on average (27 years of age), compared with nonpregnant women with severe sepsis (age 34 years). Severe sepsis in pregnancy was significantly more common in Hispanics (17%) and Asians (4%), compared with nonpregnant patients (9% and 2%, respectively). Pregnant patients with severe sepsis also had less comorbidity, obesity, and atrial fibrillation, compared with nonpregnant patients with severe sepsis.
Previously Dr. Kumar and his associates reported that the rate of hospitalizations for severe sepsis increased from 143/100,000 persons in 2000 to 343/100,000 in 2007, while mortality rates from severe sepsis decreased from 39% to 27% (Chest 2011;40:1223-31).
The findings of the current study raise questions worth pursuing in future studies, he said, such as the reasons for rising rates of severe sepsis in pregnancy despite no increase in pregnancies or hospitalizations during pregnancy. Pregnancy is considered an immunocompromised state, so why are incidence and mortality rates for severe sepsis lower in pregnancy? he asked. And why has mortality from severe sepsis in pregnancy not improved over the past 10 years?
Dr. Kumar reported having no financial disclosures.
On Twitter @sherryboschert
AT THE CRITICAL CARE CONGRESS
Major finding: The odds of death in women with severe sepsis were 43% lower during pregnancy, compared with nonpregnant women.
Data source: A retrospective analysis of nationwide data on more than 47 million pregnancy-related discharges.
Disclosures: Dr. Kumar reported having no financial disclosures.
Relatively few in ICUs get end-of-life communication training
SAN FRANCISCO – Despite training recommendations, half of physicians and less than a third of nurses surveyed in adult intensive care units at 56 California hospitals reported receiving formal training in talking with patients and families about end-of-life.
A 2008 consensus statement by the American College of Critical Care Medicine included a recommendation for end-of-life communication skills training for clinicians to improve the care of patients dying in ICUs (Crit. Care Med. 2008;36:953-63).
Dr. Matthew H.R. Anstey and his associates approached 149 California hospitals to gauge the extent of implementation of this recommendation. At 56 hospitals, doctors and nurses who work in adult ICUs voluntarily completed an anonymous web-based survey. Eighty-four percent of the 1,363 respondents were nurses, he reported in a poster presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Overall, 32% of the respondents said they had received formal training in communication skills. A significantly higher percentage of doctors had undergone training (50%) compared with nurses (29%), said Dr. Anstey, who is currently a lecturer in anesthesia at Harvard Medical School, Boston.
Sixty-six percent of all respondents agreed that "nurses are present during the communication of end-of-life information to the family" at their institution. Nurses were significantly more likely to agree with this statement (69%) than were doctors (52%).
Both doctors and nurses were very supportive of the idea of formal communication training for ICU providers. When asked about possible strategies to reduce inappropriate care for ICU patients, 91% of respondents said communication training would have a positive effect, Dr. Anstey reported.
This could be accomplished by requiring ICU physicians to complete a communication training module for ongoing credentialing, he said in an interview. Either individual hospitals could require this as part of credentialing for privileges to work in the ICU, or state medical boards could require it, similar to the California Medical Board’s requirement that physicians obtain some continuing medical education in pain management, he suggested.
The characteristics of participating hospitals were similar to those of nonparticipating hospitals in the sizes of the hospitals and ICUs, their regional location in California, and the proportions of hospitals that are teaching facilities. The 93 nonparticipating hospitals were significantly more likely to be for-profit hospitals (59%) compared with participating hospitals (7%), and significantly less likely to be part of a hospital system containing more than three hospitals (54%) compared with participating hospitals (75%).
Dr. Anstey reported having no financial disclosures. His research was in conjunction with a Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice for which he was placed at Kaiser Permanente in California.
On Twitter @sherryboschert
I am not at all surprised, nor am I disappointed by these findings. As a nation we are headed in the right direction with improving communication around end-of-life (EOL) issues.

|
|
One of the recommendations coming from 2008 guidelines by the American College of Physicians has to do with communicating advance directives and addressing the EOL topic with our patients. I am thrilled that we are beginning to have guidelines and recommendations like these to use as stimulation and leverage, improving the patient experience. If we reflect on some relatively depressing data from the last few years looking at internal medicine physicians at the University of California, San Francisco, admitting acutely ill patients and having advance directive discussions with them (J. Gen. Intern. Med. 2011;26:359-66), then I am encouraged by the findings in this ICU study. While the patient population (medical floor vs. ICU) is somewhat different, both populations benefit from advance care planning.
Barriers to end-of-life communications in ICUs include deficits in communication skills and a lack of time. The average amount of time, conservatively, is 45 minutes for these discussions. Care providers may avoid these discussions because of difficulty with their own emotions, perceiving the family as "difficult," a lack of understanding between the health care provider and the patient or family, and poor compliance. There’s little – if any – reimbursement, space is an issue as there are very few family conference rooms in hospitals, and there is mixed messaging by the numerous teams or specialties involved. The list goes on!
The Gundersen Health System in La Crosse, Wisc., is a good example of how to create a successful system of advance care planning. No one does it better. Also, the "premier programs" listed on the website of the Improving Palliative Care in the ICU (IPAL-ICU) Project are examples of leaders in the field.
Training in advance care planning is part of the education of students and residents at our institution. The University of Texas and Seton Healthcare jointly are creating a medical school in Austin. We plan to have all medical students spend time with our palliative care team and learn these communication skills. We began work on the IPAL-ICU program at two of our large hospitals. We also have put in a proposal to teach these skills to our providers and other providers within our community.
Finally, our program is collaborating with elderly advocacy groups in town to train their nurses and social workers in having upstream discussions with the population they serve so that decisions are addressed before hospitalization.
Dr. Stephen J. Bekanich, codirector of the palliative care program at Seton Healthcare, Austin, Tex., coauthors the Palliatively Speaking blog for Hospitalist News. He reported having no financial disclosures.
I am not at all surprised, nor am I disappointed by these findings. As a nation we are headed in the right direction with improving communication around end-of-life (EOL) issues.

|
|
One of the recommendations coming from 2008 guidelines by the American College of Physicians has to do with communicating advance directives and addressing the EOL topic with our patients. I am thrilled that we are beginning to have guidelines and recommendations like these to use as stimulation and leverage, improving the patient experience. If we reflect on some relatively depressing data from the last few years looking at internal medicine physicians at the University of California, San Francisco, admitting acutely ill patients and having advance directive discussions with them (J. Gen. Intern. Med. 2011;26:359-66), then I am encouraged by the findings in this ICU study. While the patient population (medical floor vs. ICU) is somewhat different, both populations benefit from advance care planning.
Barriers to end-of-life communications in ICUs include deficits in communication skills and a lack of time. The average amount of time, conservatively, is 45 minutes for these discussions. Care providers may avoid these discussions because of difficulty with their own emotions, perceiving the family as "difficult," a lack of understanding between the health care provider and the patient or family, and poor compliance. There’s little – if any – reimbursement, space is an issue as there are very few family conference rooms in hospitals, and there is mixed messaging by the numerous teams or specialties involved. The list goes on!
The Gundersen Health System in La Crosse, Wisc., is a good example of how to create a successful system of advance care planning. No one does it better. Also, the "premier programs" listed on the website of the Improving Palliative Care in the ICU (IPAL-ICU) Project are examples of leaders in the field.
Training in advance care planning is part of the education of students and residents at our institution. The University of Texas and Seton Healthcare jointly are creating a medical school in Austin. We plan to have all medical students spend time with our palliative care team and learn these communication skills. We began work on the IPAL-ICU program at two of our large hospitals. We also have put in a proposal to teach these skills to our providers and other providers within our community.
Finally, our program is collaborating with elderly advocacy groups in town to train their nurses and social workers in having upstream discussions with the population they serve so that decisions are addressed before hospitalization.
Dr. Stephen J. Bekanich, codirector of the palliative care program at Seton Healthcare, Austin, Tex., coauthors the Palliatively Speaking blog for Hospitalist News. He reported having no financial disclosures.
I am not at all surprised, nor am I disappointed by these findings. As a nation we are headed in the right direction with improving communication around end-of-life (EOL) issues.

|
|
One of the recommendations coming from 2008 guidelines by the American College of Physicians has to do with communicating advance directives and addressing the EOL topic with our patients. I am thrilled that we are beginning to have guidelines and recommendations like these to use as stimulation and leverage, improving the patient experience. If we reflect on some relatively depressing data from the last few years looking at internal medicine physicians at the University of California, San Francisco, admitting acutely ill patients and having advance directive discussions with them (J. Gen. Intern. Med. 2011;26:359-66), then I am encouraged by the findings in this ICU study. While the patient population (medical floor vs. ICU) is somewhat different, both populations benefit from advance care planning.
Barriers to end-of-life communications in ICUs include deficits in communication skills and a lack of time. The average amount of time, conservatively, is 45 minutes for these discussions. Care providers may avoid these discussions because of difficulty with their own emotions, perceiving the family as "difficult," a lack of understanding between the health care provider and the patient or family, and poor compliance. There’s little – if any – reimbursement, space is an issue as there are very few family conference rooms in hospitals, and there is mixed messaging by the numerous teams or specialties involved. The list goes on!
The Gundersen Health System in La Crosse, Wisc., is a good example of how to create a successful system of advance care planning. No one does it better. Also, the "premier programs" listed on the website of the Improving Palliative Care in the ICU (IPAL-ICU) Project are examples of leaders in the field.
Training in advance care planning is part of the education of students and residents at our institution. The University of Texas and Seton Healthcare jointly are creating a medical school in Austin. We plan to have all medical students spend time with our palliative care team and learn these communication skills. We began work on the IPAL-ICU program at two of our large hospitals. We also have put in a proposal to teach these skills to our providers and other providers within our community.
Finally, our program is collaborating with elderly advocacy groups in town to train their nurses and social workers in having upstream discussions with the population they serve so that decisions are addressed before hospitalization.
Dr. Stephen J. Bekanich, codirector of the palliative care program at Seton Healthcare, Austin, Tex., coauthors the Palliatively Speaking blog for Hospitalist News. He reported having no financial disclosures.
SAN FRANCISCO – Despite training recommendations, half of physicians and less than a third of nurses surveyed in adult intensive care units at 56 California hospitals reported receiving formal training in talking with patients and families about end-of-life.
A 2008 consensus statement by the American College of Critical Care Medicine included a recommendation for end-of-life communication skills training for clinicians to improve the care of patients dying in ICUs (Crit. Care Med. 2008;36:953-63).
Dr. Matthew H.R. Anstey and his associates approached 149 California hospitals to gauge the extent of implementation of this recommendation. At 56 hospitals, doctors and nurses who work in adult ICUs voluntarily completed an anonymous web-based survey. Eighty-four percent of the 1,363 respondents were nurses, he reported in a poster presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Overall, 32% of the respondents said they had received formal training in communication skills. A significantly higher percentage of doctors had undergone training (50%) compared with nurses (29%), said Dr. Anstey, who is currently a lecturer in anesthesia at Harvard Medical School, Boston.
Sixty-six percent of all respondents agreed that "nurses are present during the communication of end-of-life information to the family" at their institution. Nurses were significantly more likely to agree with this statement (69%) than were doctors (52%).
Both doctors and nurses were very supportive of the idea of formal communication training for ICU providers. When asked about possible strategies to reduce inappropriate care for ICU patients, 91% of respondents said communication training would have a positive effect, Dr. Anstey reported.
This could be accomplished by requiring ICU physicians to complete a communication training module for ongoing credentialing, he said in an interview. Either individual hospitals could require this as part of credentialing for privileges to work in the ICU, or state medical boards could require it, similar to the California Medical Board’s requirement that physicians obtain some continuing medical education in pain management, he suggested.
The characteristics of participating hospitals were similar to those of nonparticipating hospitals in the sizes of the hospitals and ICUs, their regional location in California, and the proportions of hospitals that are teaching facilities. The 93 nonparticipating hospitals were significantly more likely to be for-profit hospitals (59%) compared with participating hospitals (7%), and significantly less likely to be part of a hospital system containing more than three hospitals (54%) compared with participating hospitals (75%).
Dr. Anstey reported having no financial disclosures. His research was in conjunction with a Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice for which he was placed at Kaiser Permanente in California.
On Twitter @sherryboschert
SAN FRANCISCO – Despite training recommendations, half of physicians and less than a third of nurses surveyed in adult intensive care units at 56 California hospitals reported receiving formal training in talking with patients and families about end-of-life.
A 2008 consensus statement by the American College of Critical Care Medicine included a recommendation for end-of-life communication skills training for clinicians to improve the care of patients dying in ICUs (Crit. Care Med. 2008;36:953-63).
Dr. Matthew H.R. Anstey and his associates approached 149 California hospitals to gauge the extent of implementation of this recommendation. At 56 hospitals, doctors and nurses who work in adult ICUs voluntarily completed an anonymous web-based survey. Eighty-four percent of the 1,363 respondents were nurses, he reported in a poster presentation at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Overall, 32% of the respondents said they had received formal training in communication skills. A significantly higher percentage of doctors had undergone training (50%) compared with nurses (29%), said Dr. Anstey, who is currently a lecturer in anesthesia at Harvard Medical School, Boston.
Sixty-six percent of all respondents agreed that "nurses are present during the communication of end-of-life information to the family" at their institution. Nurses were significantly more likely to agree with this statement (69%) than were doctors (52%).
Both doctors and nurses were very supportive of the idea of formal communication training for ICU providers. When asked about possible strategies to reduce inappropriate care for ICU patients, 91% of respondents said communication training would have a positive effect, Dr. Anstey reported.
This could be accomplished by requiring ICU physicians to complete a communication training module for ongoing credentialing, he said in an interview. Either individual hospitals could require this as part of credentialing for privileges to work in the ICU, or state medical boards could require it, similar to the California Medical Board’s requirement that physicians obtain some continuing medical education in pain management, he suggested.
The characteristics of participating hospitals were similar to those of nonparticipating hospitals in the sizes of the hospitals and ICUs, their regional location in California, and the proportions of hospitals that are teaching facilities. The 93 nonparticipating hospitals were significantly more likely to be for-profit hospitals (59%) compared with participating hospitals (7%), and significantly less likely to be part of a hospital system containing more than three hospitals (54%) compared with participating hospitals (75%).
Dr. Anstey reported having no financial disclosures. His research was in conjunction with a Commonwealth Fund Harkness Fellowship in Health Care Policy and Practice for which he was placed at Kaiser Permanente in California.
On Twitter @sherryboschert
AT THE CRITICAL CARE CONGRESS
Palliative care shortens ICU, hospital stays, review data show
SAN FRANCISCO – Palliative care in the intensive care unit reduces the length of stay in the ICU and the hospital without changing mortality rates or family satisfaction, according to a review of the literature.
Although measurements of family satisfaction overall didn’t change much from palliative care of a loved one in the ICU, some measures of components of satisfaction increased with palliative care, such as improved communication with the physician, better consensus around the goals of care, and decreased anxiety and depression in family members, reported Dr. Rebecca A. Aslakson of Johns Hopkins University, Baltimore.

The findings have been submitted for publication, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Dr. Aslakson and her associates were unable to perform a formal meta-analysis of the 37 published trials of palliative care in the ICU because of the heterogeneity of the studies, which looked at more than 40 different outcomes. Instead, their systematic review grouped results under four outcomes that commonly were measured, and assessed those either by the number of studies or by the number of patients studied.
ICU length of stay decreased with palliative care in 13 of 21 studies (62%) that used this outcome and in 59% of 9,368 patients in those studies. Hospital length of stay decreased with palliative care in 8 of 14 studies (57%) and in 43% of 5,817 patients. Family satisfaction did not decrease in any studies or families and increased in only 1 of 14 studies (7%) and in 2% of families of 4,927 patients, Dr. Aslakson reported.
Mortality rates did not change with palliative care in 14 of 16 studies (88%) that assessed mortality and in 57% of 5,969 patients in those studies. Mortality increased in one small study (6%) and decreased in one larger study (6%).
"Talking about big-picture issues and goals of care doesn’t lead to people dying," Dr. Aslakson said. "No harm came in any of these studies." Some separate studies of palliative care outside of ICUs reported that this increases hope, "because people feel that they have more control over their choices and what’s happening to their loved ones," she added.
Integrative vs. consultative model
Dr. Aslakson and her associates also reviewed studies based on whether the interventions used integrative or consultative models of palliative care.
Generally, consultative models bring outsiders into the ICU to help provide palliative care, and integrative models train the ICU team to be the palliative care providers. In reality, the two models may overlap. For this review, the investigators applied mutually exclusive definitions to 36 of the studies. In 18 studies of integrative interventions, members of the ICU team were the only caregivers in face-to-face interactions with the patient and families. In 18 studies of consultative interventions, palliative care providers included others besides the ICU team.
In the studies of integrative palliative care, ICU length of stay decreased with palliative care in four of nine studies (44%) that measured this outcome and in 52% of 6,963 patients in those studies, she reported. Hospital length of stay decreased in two of five studies (40%) and in 24% of 3,812 patients. Family satisfaction changed in none of 15 studies, and mortality decreased in 1 of 5 studies (20%) and in 34% of 3,807 patients.
In the studies of consultative care, ICU length of stay decreased with palliative care in 9 of 12 studies (75%) that measured this outcome and in 79% of 2,405 patients in those studies. Hospital length of stay decreased in six of nine studies (67%) and in 79% of 2,005 patients. Family satisfaction increased in one of four studies (25%) and in 21% of 429 patients. Mortality increased in 1 of 11 studies (9%) and in 5% of 2,162 patients.
One model isn’t necessarily better than the other, Dr. Aslakson said. Integrative palliative care may work best in a closed ICU with perhaps four or five intensivists in a relatively small unit. An integrative approach can be much more difficult in open or semiopen ICUs that have "40 different doctors floating around," she said. "We tried that in my unit, and it didn’t work that well."
Different ICUs need palliative care models that fit them. "Look at your unit, the way it works, and who the providers are, then look at the literature and see what matches that and what might work for your unit," she said.
Outcomes of improved communication
A previous, separate review of the medical literature identified 21 controlled trials of 16 interventions to improve communication in ICUs between families and care providers. Overall, the interventions improved emotional outcomes for families and reduced ICU length of stay and treatment intensity (Chest 2011;139:543-54), she noted.
Yet another prior review of the literature reported that interventions to promote family meetings, use empathetic communication skills, and employ palliative care consultations improved family satisfaction and reduced ICU length of stay and the adverse effects of family bereavement (Curr. Opin. Crit. Care 2009;15:569-77).
Dr. Aslakson reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – Palliative care in the intensive care unit reduces the length of stay in the ICU and the hospital without changing mortality rates or family satisfaction, according to a review of the literature.
Although measurements of family satisfaction overall didn’t change much from palliative care of a loved one in the ICU, some measures of components of satisfaction increased with palliative care, such as improved communication with the physician, better consensus around the goals of care, and decreased anxiety and depression in family members, reported Dr. Rebecca A. Aslakson of Johns Hopkins University, Baltimore.

The findings have been submitted for publication, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Dr. Aslakson and her associates were unable to perform a formal meta-analysis of the 37 published trials of palliative care in the ICU because of the heterogeneity of the studies, which looked at more than 40 different outcomes. Instead, their systematic review grouped results under four outcomes that commonly were measured, and assessed those either by the number of studies or by the number of patients studied.
ICU length of stay decreased with palliative care in 13 of 21 studies (62%) that used this outcome and in 59% of 9,368 patients in those studies. Hospital length of stay decreased with palliative care in 8 of 14 studies (57%) and in 43% of 5,817 patients. Family satisfaction did not decrease in any studies or families and increased in only 1 of 14 studies (7%) and in 2% of families of 4,927 patients, Dr. Aslakson reported.
Mortality rates did not change with palliative care in 14 of 16 studies (88%) that assessed mortality and in 57% of 5,969 patients in those studies. Mortality increased in one small study (6%) and decreased in one larger study (6%).
"Talking about big-picture issues and goals of care doesn’t lead to people dying," Dr. Aslakson said. "No harm came in any of these studies." Some separate studies of palliative care outside of ICUs reported that this increases hope, "because people feel that they have more control over their choices and what’s happening to their loved ones," she added.
Integrative vs. consultative model
Dr. Aslakson and her associates also reviewed studies based on whether the interventions used integrative or consultative models of palliative care.
Generally, consultative models bring outsiders into the ICU to help provide palliative care, and integrative models train the ICU team to be the palliative care providers. In reality, the two models may overlap. For this review, the investigators applied mutually exclusive definitions to 36 of the studies. In 18 studies of integrative interventions, members of the ICU team were the only caregivers in face-to-face interactions with the patient and families. In 18 studies of consultative interventions, palliative care providers included others besides the ICU team.
In the studies of integrative palliative care, ICU length of stay decreased with palliative care in four of nine studies (44%) that measured this outcome and in 52% of 6,963 patients in those studies, she reported. Hospital length of stay decreased in two of five studies (40%) and in 24% of 3,812 patients. Family satisfaction changed in none of 15 studies, and mortality decreased in 1 of 5 studies (20%) and in 34% of 3,807 patients.
In the studies of consultative care, ICU length of stay decreased with palliative care in 9 of 12 studies (75%) that measured this outcome and in 79% of 2,405 patients in those studies. Hospital length of stay decreased in six of nine studies (67%) and in 79% of 2,005 patients. Family satisfaction increased in one of four studies (25%) and in 21% of 429 patients. Mortality increased in 1 of 11 studies (9%) and in 5% of 2,162 patients.
One model isn’t necessarily better than the other, Dr. Aslakson said. Integrative palliative care may work best in a closed ICU with perhaps four or five intensivists in a relatively small unit. An integrative approach can be much more difficult in open or semiopen ICUs that have "40 different doctors floating around," she said. "We tried that in my unit, and it didn’t work that well."
Different ICUs need palliative care models that fit them. "Look at your unit, the way it works, and who the providers are, then look at the literature and see what matches that and what might work for your unit," she said.
Outcomes of improved communication
A previous, separate review of the medical literature identified 21 controlled trials of 16 interventions to improve communication in ICUs between families and care providers. Overall, the interventions improved emotional outcomes for families and reduced ICU length of stay and treatment intensity (Chest 2011;139:543-54), she noted.
Yet another prior review of the literature reported that interventions to promote family meetings, use empathetic communication skills, and employ palliative care consultations improved family satisfaction and reduced ICU length of stay and the adverse effects of family bereavement (Curr. Opin. Crit. Care 2009;15:569-77).
Dr. Aslakson reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – Palliative care in the intensive care unit reduces the length of stay in the ICU and the hospital without changing mortality rates or family satisfaction, according to a review of the literature.
Although measurements of family satisfaction overall didn’t change much from palliative care of a loved one in the ICU, some measures of components of satisfaction increased with palliative care, such as improved communication with the physician, better consensus around the goals of care, and decreased anxiety and depression in family members, reported Dr. Rebecca A. Aslakson of Johns Hopkins University, Baltimore.

The findings have been submitted for publication, she said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Dr. Aslakson and her associates were unable to perform a formal meta-analysis of the 37 published trials of palliative care in the ICU because of the heterogeneity of the studies, which looked at more than 40 different outcomes. Instead, their systematic review grouped results under four outcomes that commonly were measured, and assessed those either by the number of studies or by the number of patients studied.
ICU length of stay decreased with palliative care in 13 of 21 studies (62%) that used this outcome and in 59% of 9,368 patients in those studies. Hospital length of stay decreased with palliative care in 8 of 14 studies (57%) and in 43% of 5,817 patients. Family satisfaction did not decrease in any studies or families and increased in only 1 of 14 studies (7%) and in 2% of families of 4,927 patients, Dr. Aslakson reported.
Mortality rates did not change with palliative care in 14 of 16 studies (88%) that assessed mortality and in 57% of 5,969 patients in those studies. Mortality increased in one small study (6%) and decreased in one larger study (6%).
"Talking about big-picture issues and goals of care doesn’t lead to people dying," Dr. Aslakson said. "No harm came in any of these studies." Some separate studies of palliative care outside of ICUs reported that this increases hope, "because people feel that they have more control over their choices and what’s happening to their loved ones," she added.
Integrative vs. consultative model
Dr. Aslakson and her associates also reviewed studies based on whether the interventions used integrative or consultative models of palliative care.
Generally, consultative models bring outsiders into the ICU to help provide palliative care, and integrative models train the ICU team to be the palliative care providers. In reality, the two models may overlap. For this review, the investigators applied mutually exclusive definitions to 36 of the studies. In 18 studies of integrative interventions, members of the ICU team were the only caregivers in face-to-face interactions with the patient and families. In 18 studies of consultative interventions, palliative care providers included others besides the ICU team.
In the studies of integrative palliative care, ICU length of stay decreased with palliative care in four of nine studies (44%) that measured this outcome and in 52% of 6,963 patients in those studies, she reported. Hospital length of stay decreased in two of five studies (40%) and in 24% of 3,812 patients. Family satisfaction changed in none of 15 studies, and mortality decreased in 1 of 5 studies (20%) and in 34% of 3,807 patients.
In the studies of consultative care, ICU length of stay decreased with palliative care in 9 of 12 studies (75%) that measured this outcome and in 79% of 2,405 patients in those studies. Hospital length of stay decreased in six of nine studies (67%) and in 79% of 2,005 patients. Family satisfaction increased in one of four studies (25%) and in 21% of 429 patients. Mortality increased in 1 of 11 studies (9%) and in 5% of 2,162 patients.
One model isn’t necessarily better than the other, Dr. Aslakson said. Integrative palliative care may work best in a closed ICU with perhaps four or five intensivists in a relatively small unit. An integrative approach can be much more difficult in open or semiopen ICUs that have "40 different doctors floating around," she said. "We tried that in my unit, and it didn’t work that well."
Different ICUs need palliative care models that fit them. "Look at your unit, the way it works, and who the providers are, then look at the literature and see what matches that and what might work for your unit," she said.
Outcomes of improved communication
A previous, separate review of the medical literature identified 21 controlled trials of 16 interventions to improve communication in ICUs between families and care providers. Overall, the interventions improved emotional outcomes for families and reduced ICU length of stay and treatment intensity (Chest 2011;139:543-54), she noted.
Yet another prior review of the literature reported that interventions to promote family meetings, use empathetic communication skills, and employ palliative care consultations improved family satisfaction and reduced ICU length of stay and the adverse effects of family bereavement (Curr. Opin. Crit. Care 2009;15:569-77).
Dr. Aslakson reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
AT THE CRITICAL CARE CONGRESS
Which specialty can fill the intensivist shortage?
SAN FRANCISCO – Hospitalists are the most logical source of physicians to fill a shortage of intensive care providers. Or, maybe it’s emergency physicians. But it could be internists, depending on which of three speakers at the Critical Care Congress you find most persuasive.
Whether it’s any of those specialties or all three, there are barriers to be overcome with each strategy, the speakers said in a session on critical care practitioners.
Hospitalists already are doing critical care, Dr. Andrew D. Auerbach said. "Even if not hired primarily for that, they’re doing it anyway," said Dr. Auerbach, a hospitalist and researcher at the University of California, San Francisco. A 2010 study found that 34 of 72 open intensive care units in Michigan had hospitalists as ICU attending physicians (J. Hosp. Med. 2010;5:4-9). These included smaller hospitals outside major population centers, not just small community hospitals, he said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Hospitalists in those settings become "the first-line providers in critical care" when, for example, a patient with respiratory failure and sepsis needs to go to the ICU at 2 a.m. "The pulmonologist is trying to do their best, but is at home. The emergency physician is in the emergency department trying to take care of broken legs and car crashes. The anesthesiologist is doing airways and epidurals up on the obstetrics floor."
These hospitalists need to be supported in their intensivist roles by "giving them the training – whether it be for an added certification or board certification, I don’t care," Dr. Auerbach said. Intensivists also could benefit by forging clinical partnerships with hospitalists to tap hospitalists’ expertise in sepsis care, patient monitoring, antimicrobial stewardship, comanaging surgical patients, and transitioning patient care, he suggested.
"Hospitalists want to go into critical care medicine but have been at times in limbo because there is no pathway for them except to do the 2 years of fellowship training," Dr. Stephen M. Pastores agreed in a separate presentation. "We need to help our hospitalists get to the promised land of the ICU," either by creating a shortened training pathway or by offering new incentives.
Community hospitals that want more intensivists could pay for hospitalists to pursue fellowship training and guarantee them an intensivist job when training is finished, said Dr. Pastores, director of the critical care fellowship program at Memorial Sloan-Kettering Cancer Center, New York, and a board-certified internist, pulmonologist, and intensivist there.
Hospitals that are determined to have intensivists run the ICU might consider that approach, which could offset the hassle of leaving one’s job and taking a temporary pay cut in order to pursue a critical care fellowship, Dr. Franklin A. Michota agreed in a phone interview. Or, they simply could offer higher salaries to recruit intensivists. "It’s a supply-and-demand phenomenon," said Dr. Michota, director of academic affairs in the department of hospitalist medicine at the Cleveland Clinic.
On the other hand, intensive care is within the scope and training of hospitalists, and any hospitalists working in ICUs should be pursuing critical care CME already, he added. Doing a 2-year critical care fellowship "on top of that won’t change the skill set" but will increase the salary that a physician can command, he said.
Besides hospitalists, Dr. Pastores sees greater possibilities from expanding the pipeline of internists into critical care.
"I’d argue that the internal medicine–based trained intensivists really have no competing responsibilities" compared with pulmonologists, surgeons, or other specialists and thus are more likely to work full-time in an ICU, he said. "From that perspective, why are there only 34 stand-alone programs in internal medicine critical care compared to 134 programs in pulmonary critical care? Maybe that could be addressed in a more efficient way."
Pulmonary critical care medicine programs also could be doing more. Although it’s not well known, the Accreditation Council for Graduate Medical Education (ACGME) allows pulmonary critical care programs every other year to train a fellow who does not want to be certified in pulmonary medicine but only wants to do critical care medicine, Dr. Pastores said. If the programs took advantage of that, the number of full-time critical care providers would increase.
A paper to be published by Dr. Pastores and his colleagues this spring in the journal Critical Care Medicine will propose that the ACGME relax some "very restrictive mandates" on internal medicine–based critical care medicine training programs.
One hurdle requires the critical care medicine program’s primary site to offer at least three out of five key fellowship programs. "That can be very difficult for many of the smaller programs that are not major academic centers, where they may not have things like fellowships in infectious diseases, nephrology, pulmonary, et cetera," he said.
Another barrier excludes physicians who are not certified in internal medicine from being counted as key faculty in internal medicine–based critical care training programs. "In my program, we have anesthesiologists and surgeons who are teaching our fellows, and there’s no good reason they shouldn’t be counted as key faculty," he said.
He and Dr. Brian Wessman, who also spoke at the meeting, cited another ACGME barrier, this one blocking the pipeline of emergency medicine physicians. Internal medicine–based critical care medicine training programs must limit the proportion of emergency medicine trainees to 25% of their programs.
Emergency medicine physicians are the ideal candidates for critical care medicine because their training already includes exposure to undifferentiated critical care patients and development of a "robust procedural acumen applicable to critical care," said Dr. Wessman, an emergency medicine physician and codirector of the critical care fellowship program at Washington University, St. Louis.
There now are three paths to obtaining certification in emergency medicine/critical care medicine, he said. Medicine-based critical care programs limit trainees from emergency medicine to 25% of slots. As of July 2013, emergency medicine physicians could enter surgical critical care fellowships at three institutions. And beginning in the 2014 academic year, 10 anesthesiology critical care medicine fellowship programs will offer an emergency medicine/critical care medicine training tract.
"If you haven’t run across an emergency medicine intensivist yet, you will," Dr. Wessman said. "I think you will see our numbers grow exponentially now that there are ways for us to go forward, if we can remove some of the barriers."
None of the speakers had financial disclosures relevant to this topic. Dr. Pastores reported receiving research grants from Spectral Diagnostics and Bayer Healthcare. Dr. Michota reported financial associations with Boehringer Ingelheim, Daiichi-Sankyo, and other companies. Dr. Wessman and Dr. Auerbach reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Hospitalists are the most logical source of physicians to fill a shortage of intensive care providers. Or, maybe it’s emergency physicians. But it could be internists, depending on which of three speakers at the Critical Care Congress you find most persuasive.
Whether it’s any of those specialties or all three, there are barriers to be overcome with each strategy, the speakers said in a session on critical care practitioners.
Hospitalists already are doing critical care, Dr. Andrew D. Auerbach said. "Even if not hired primarily for that, they’re doing it anyway," said Dr. Auerbach, a hospitalist and researcher at the University of California, San Francisco. A 2010 study found that 34 of 72 open intensive care units in Michigan had hospitalists as ICU attending physicians (J. Hosp. Med. 2010;5:4-9). These included smaller hospitals outside major population centers, not just small community hospitals, he said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Hospitalists in those settings become "the first-line providers in critical care" when, for example, a patient with respiratory failure and sepsis needs to go to the ICU at 2 a.m. "The pulmonologist is trying to do their best, but is at home. The emergency physician is in the emergency department trying to take care of broken legs and car crashes. The anesthesiologist is doing airways and epidurals up on the obstetrics floor."
These hospitalists need to be supported in their intensivist roles by "giving them the training – whether it be for an added certification or board certification, I don’t care," Dr. Auerbach said. Intensivists also could benefit by forging clinical partnerships with hospitalists to tap hospitalists’ expertise in sepsis care, patient monitoring, antimicrobial stewardship, comanaging surgical patients, and transitioning patient care, he suggested.
"Hospitalists want to go into critical care medicine but have been at times in limbo because there is no pathway for them except to do the 2 years of fellowship training," Dr. Stephen M. Pastores agreed in a separate presentation. "We need to help our hospitalists get to the promised land of the ICU," either by creating a shortened training pathway or by offering new incentives.
Community hospitals that want more intensivists could pay for hospitalists to pursue fellowship training and guarantee them an intensivist job when training is finished, said Dr. Pastores, director of the critical care fellowship program at Memorial Sloan-Kettering Cancer Center, New York, and a board-certified internist, pulmonologist, and intensivist there.
Hospitals that are determined to have intensivists run the ICU might consider that approach, which could offset the hassle of leaving one’s job and taking a temporary pay cut in order to pursue a critical care fellowship, Dr. Franklin A. Michota agreed in a phone interview. Or, they simply could offer higher salaries to recruit intensivists. "It’s a supply-and-demand phenomenon," said Dr. Michota, director of academic affairs in the department of hospitalist medicine at the Cleveland Clinic.
On the other hand, intensive care is within the scope and training of hospitalists, and any hospitalists working in ICUs should be pursuing critical care CME already, he added. Doing a 2-year critical care fellowship "on top of that won’t change the skill set" but will increase the salary that a physician can command, he said.
Besides hospitalists, Dr. Pastores sees greater possibilities from expanding the pipeline of internists into critical care.
"I’d argue that the internal medicine–based trained intensivists really have no competing responsibilities" compared with pulmonologists, surgeons, or other specialists and thus are more likely to work full-time in an ICU, he said. "From that perspective, why are there only 34 stand-alone programs in internal medicine critical care compared to 134 programs in pulmonary critical care? Maybe that could be addressed in a more efficient way."
Pulmonary critical care medicine programs also could be doing more. Although it’s not well known, the Accreditation Council for Graduate Medical Education (ACGME) allows pulmonary critical care programs every other year to train a fellow who does not want to be certified in pulmonary medicine but only wants to do critical care medicine, Dr. Pastores said. If the programs took advantage of that, the number of full-time critical care providers would increase.
A paper to be published by Dr. Pastores and his colleagues this spring in the journal Critical Care Medicine will propose that the ACGME relax some "very restrictive mandates" on internal medicine–based critical care medicine training programs.
One hurdle requires the critical care medicine program’s primary site to offer at least three out of five key fellowship programs. "That can be very difficult for many of the smaller programs that are not major academic centers, where they may not have things like fellowships in infectious diseases, nephrology, pulmonary, et cetera," he said.
Another barrier excludes physicians who are not certified in internal medicine from being counted as key faculty in internal medicine–based critical care training programs. "In my program, we have anesthesiologists and surgeons who are teaching our fellows, and there’s no good reason they shouldn’t be counted as key faculty," he said.
He and Dr. Brian Wessman, who also spoke at the meeting, cited another ACGME barrier, this one blocking the pipeline of emergency medicine physicians. Internal medicine–based critical care medicine training programs must limit the proportion of emergency medicine trainees to 25% of their programs.
Emergency medicine physicians are the ideal candidates for critical care medicine because their training already includes exposure to undifferentiated critical care patients and development of a "robust procedural acumen applicable to critical care," said Dr. Wessman, an emergency medicine physician and codirector of the critical care fellowship program at Washington University, St. Louis.
There now are three paths to obtaining certification in emergency medicine/critical care medicine, he said. Medicine-based critical care programs limit trainees from emergency medicine to 25% of slots. As of July 2013, emergency medicine physicians could enter surgical critical care fellowships at three institutions. And beginning in the 2014 academic year, 10 anesthesiology critical care medicine fellowship programs will offer an emergency medicine/critical care medicine training tract.
"If you haven’t run across an emergency medicine intensivist yet, you will," Dr. Wessman said. "I think you will see our numbers grow exponentially now that there are ways for us to go forward, if we can remove some of the barriers."
None of the speakers had financial disclosures relevant to this topic. Dr. Pastores reported receiving research grants from Spectral Diagnostics and Bayer Healthcare. Dr. Michota reported financial associations with Boehringer Ingelheim, Daiichi-Sankyo, and other companies. Dr. Wessman and Dr. Auerbach reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Hospitalists are the most logical source of physicians to fill a shortage of intensive care providers. Or, maybe it’s emergency physicians. But it could be internists, depending on which of three speakers at the Critical Care Congress you find most persuasive.
Whether it’s any of those specialties or all three, there are barriers to be overcome with each strategy, the speakers said in a session on critical care practitioners.
Hospitalists already are doing critical care, Dr. Andrew D. Auerbach said. "Even if not hired primarily for that, they’re doing it anyway," said Dr. Auerbach, a hospitalist and researcher at the University of California, San Francisco. A 2010 study found that 34 of 72 open intensive care units in Michigan had hospitalists as ICU attending physicians (J. Hosp. Med. 2010;5:4-9). These included smaller hospitals outside major population centers, not just small community hospitals, he said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Hospitalists in those settings become "the first-line providers in critical care" when, for example, a patient with respiratory failure and sepsis needs to go to the ICU at 2 a.m. "The pulmonologist is trying to do their best, but is at home. The emergency physician is in the emergency department trying to take care of broken legs and car crashes. The anesthesiologist is doing airways and epidurals up on the obstetrics floor."
These hospitalists need to be supported in their intensivist roles by "giving them the training – whether it be for an added certification or board certification, I don’t care," Dr. Auerbach said. Intensivists also could benefit by forging clinical partnerships with hospitalists to tap hospitalists’ expertise in sepsis care, patient monitoring, antimicrobial stewardship, comanaging surgical patients, and transitioning patient care, he suggested.
"Hospitalists want to go into critical care medicine but have been at times in limbo because there is no pathway for them except to do the 2 years of fellowship training," Dr. Stephen M. Pastores agreed in a separate presentation. "We need to help our hospitalists get to the promised land of the ICU," either by creating a shortened training pathway or by offering new incentives.
Community hospitals that want more intensivists could pay for hospitalists to pursue fellowship training and guarantee them an intensivist job when training is finished, said Dr. Pastores, director of the critical care fellowship program at Memorial Sloan-Kettering Cancer Center, New York, and a board-certified internist, pulmonologist, and intensivist there.
Hospitals that are determined to have intensivists run the ICU might consider that approach, which could offset the hassle of leaving one’s job and taking a temporary pay cut in order to pursue a critical care fellowship, Dr. Franklin A. Michota agreed in a phone interview. Or, they simply could offer higher salaries to recruit intensivists. "It’s a supply-and-demand phenomenon," said Dr. Michota, director of academic affairs in the department of hospitalist medicine at the Cleveland Clinic.
On the other hand, intensive care is within the scope and training of hospitalists, and any hospitalists working in ICUs should be pursuing critical care CME already, he added. Doing a 2-year critical care fellowship "on top of that won’t change the skill set" but will increase the salary that a physician can command, he said.
Besides hospitalists, Dr. Pastores sees greater possibilities from expanding the pipeline of internists into critical care.
"I’d argue that the internal medicine–based trained intensivists really have no competing responsibilities" compared with pulmonologists, surgeons, or other specialists and thus are more likely to work full-time in an ICU, he said. "From that perspective, why are there only 34 stand-alone programs in internal medicine critical care compared to 134 programs in pulmonary critical care? Maybe that could be addressed in a more efficient way."
Pulmonary critical care medicine programs also could be doing more. Although it’s not well known, the Accreditation Council for Graduate Medical Education (ACGME) allows pulmonary critical care programs every other year to train a fellow who does not want to be certified in pulmonary medicine but only wants to do critical care medicine, Dr. Pastores said. If the programs took advantage of that, the number of full-time critical care providers would increase.
A paper to be published by Dr. Pastores and his colleagues this spring in the journal Critical Care Medicine will propose that the ACGME relax some "very restrictive mandates" on internal medicine–based critical care medicine training programs.
One hurdle requires the critical care medicine program’s primary site to offer at least three out of five key fellowship programs. "That can be very difficult for many of the smaller programs that are not major academic centers, where they may not have things like fellowships in infectious diseases, nephrology, pulmonary, et cetera," he said.
Another barrier excludes physicians who are not certified in internal medicine from being counted as key faculty in internal medicine–based critical care training programs. "In my program, we have anesthesiologists and surgeons who are teaching our fellows, and there’s no good reason they shouldn’t be counted as key faculty," he said.
He and Dr. Brian Wessman, who also spoke at the meeting, cited another ACGME barrier, this one blocking the pipeline of emergency medicine physicians. Internal medicine–based critical care medicine training programs must limit the proportion of emergency medicine trainees to 25% of their programs.
Emergency medicine physicians are the ideal candidates for critical care medicine because their training already includes exposure to undifferentiated critical care patients and development of a "robust procedural acumen applicable to critical care," said Dr. Wessman, an emergency medicine physician and codirector of the critical care fellowship program at Washington University, St. Louis.
There now are three paths to obtaining certification in emergency medicine/critical care medicine, he said. Medicine-based critical care programs limit trainees from emergency medicine to 25% of slots. As of July 2013, emergency medicine physicians could enter surgical critical care fellowships at three institutions. And beginning in the 2014 academic year, 10 anesthesiology critical care medicine fellowship programs will offer an emergency medicine/critical care medicine training tract.
"If you haven’t run across an emergency medicine intensivist yet, you will," Dr. Wessman said. "I think you will see our numbers grow exponentially now that there are ways for us to go forward, if we can remove some of the barriers."
None of the speakers had financial disclosures relevant to this topic. Dr. Pastores reported receiving research grants from Spectral Diagnostics and Bayer Healthcare. Dr. Michota reported financial associations with Boehringer Ingelheim, Daiichi-Sankyo, and other companies. Dr. Wessman and Dr. Auerbach reported having no financial disclosures.
On Twitter @sherryboschert
AT THE CRITICAL CARE CONGRESS