User login
Preparing for pancreatic cancer ‘tsunami’ ahead
ORLANDO – Overall cancer death rates are dropping dramatically, but pancreatic cancer mortality remains high.
“By 2020 we expect [pancreatic cancer] to be the second most common cause of cancer-related death, exceeded only by lung cancer, and if lung cancer deaths continue to fall – which we expect that they will – it will be the most common cause of cancer-related death,” Margaret A. Tempero, MD, said at the annual conference of the National Comprehensive Cancer Network.
Further, as the population ages there will be an increasing number of patients presenting with pancreatic cancer, said Dr. Tempero of the University of California, San Francisco.
Currently, 80% of pancreatic cancer patients are diagnosed with disease that is not amenable to resection, and 80% of those who have resection and adjuvant therapy experience relapse. The overall survival rate is only about 9%.
“This is really, really an aggressive malignancy,” Dr. Tempero said, noting that the survival among those with metastases who do not receive treatment is only about 3 months.
There are no early symptoms that direct attention to the pancreas. Additionally, some patients experience very early invasion and metastases; in fact, up to two-thirds of patients with lesions only 1 cm in size will already have lymph node metastasis, she said.
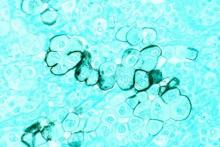
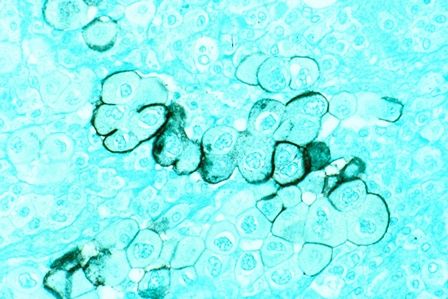
The disease tends to be chemoresistant, although this may be changing with treatment advances, but it is characterized by “a lot of desmoplastic stroma, so there’s a lot of microenvironment that’s perturbed around the malignancy,” making it difficult for drugs to permeate the stroma.
“That’s something we’re actively working on – ways that we can actually change the stroma so that we can get more drug into the cancer,” she said.
Another challenge is the disease’s “habit of elaborating a lot of cytokines that disable the person with the disease,” which can lead to frailty that makes it difficult to deliver potentially effective therapies that are well tolerated in patients with other types of cancer, she noted.
An important question is whether pancreatic cancer is diagnosed too late or metastasizes too early, and there is evidence to support both possibilities.
“Either way ... we need to work on better treatment,” she said.
Resectable/borderline resectable disease
One noteworthy recent advance for patients with resectable/borderline resectable disease is the addition of capecitabine to gemcitabine for adjuvant therapy. In the ESPAC 4 study published in March in the Lancet, the combination of gemcitabine and capecitabine showed a clear benefit over gemcitabine alone.
“So that has now entered [the NCCN] guidelines as an important option for adjuvant therapy,” said Dr. Tempero, chair of the NCCN pancreatic cancer guidelines panel.
Ongoing trials are also looking at the FOLFIRINOX (irinotecan plus 5-fluorouracil plus leucovorin plus oxaliplatin) and gemcitabine/nanoparticle albumin-bound paclitaxel (nab-P) regimens in the adjuvant setting. These have previously shown some efficacy in the metastatic setting.
“So we really wanted to get these therapies into the adjuvant setting as soon as we could,” she said.
In the ACCORD trial, FOLFIRINOX is being compared with gemcitabine in the postoperative adjuvant setting, and the APACT trial comparing gemcitabine/nab-P to gemcitabine monotherapy completed accrual last year.
“I’m pretty sure that we’ll have enough events on the APACT study by the end of this year, and hopefully we can present that data in the spring. I’m hoping it will be a positive trial for us,” she said.
Neoadjuvant therapy – a successful strategy used in many other malignancies – is also being looked at for pancreatic cancer.
A pilot study (A021101) completed last year suggested that chemotherapy (FOLFIRINOX for 2 months) and chemoradiation (capecitabine and radiation at 50.4 Gy) followed by surgical resection and adjuvant chemotherapy (gemcitabine for 2 months) provided some benefit in patients with borderline resectable pancreatic cancer. This trial led to another ongoing study (S1505) in which patients with borderline resectable disease will be treated with 4 months of FOLFIRINOX prior to resection, followed by chemoradiation and surgery or FOLFIRINOX and surgery, and patients with resectable disease will undergo resection followed by FOLFIRINOX and surgery or gemcitabine/nab-P and surgery.
“The goal is not to compare the two regimens; the goal is to identify the benchmarks that we get with these regimens. In other words, if you’re going to give FOLFIRINOX, what pathologic complete response rate can you expect? What will your R1 resection rate be? With gemcitabine and nab-paclitaxel, the same thing, because if you want to continue to build on these regimens in the neoadjuvant setting you need to know what you’re likely to get so you can make clinical trial assumptions when you add new drugs.
“Once we have these benchmarking data we can really sail in the neoadjuvant setting. It’s a great window-of-opportunity setting for new drugs, because you’re getting serial tissue,” Dr. Tempero said, explaining that in addition to resection of tissue, there is opportunity to get biopsies ahead of time and look at the effects of the drug.
Locally advanced disease
For locally advanced disease, studies have failed to show a benefit of adding radiation after chemotherapy, but radiation oncologists who argue that, “when your therapy gets better, my therapy gets better,” have a valid point, Dr. Tempero said.
For that reason, the Radiation Therapy Oncology group launched a trial to look at gemcitabine/nab-P with and without radiation, but had difficulty with enrollment due to resistance among some physicians who are opposed to radiation in this setting .
“So I don’t know that we will ever answer this question in locally advanced disease. What I can say ... is, in my mind, in locally advanced disease, the most important component is the chemotherapy,” she said.
Metastatic disease
When it comes to trials involving pancreatic cancer patients with metastatic disease, it is important to understand – and to convey to policymakers – that the goal is not only to provide better care in these patients who are at the end of their life, but also to identify strategies that can be used in the adjuvant and neoadjuvant settings, as this is part of the “overall mission of helping patients to feel better and live longer and be cured,” Dr. Tempero said.
One regimen currently used in the metastatic setting is FOLFIRINOX, which was shown in the Prodige 4-ACCORD 11 trial to be superior to gemcitabine monotherapy for survival (hazard ratio, 0.57).
“This is the first time we ever saw a hazard ratio below 0.6 in this disease,” she said, adding that for some patients this means “they can get tremendous benefit, they can come off chemotherapy and have a chemotherapy holiday,” she said.
That said, it’s a tough regimen, she added, explaining that it has dominating toxicities of myelosuppression, diarrhea, and neuropathy that can be irreversible.
Frail patients may not be able to tolerate the regimen, but modifications to the regimen may help. For example, the 5-fluorourasil bolus is often omitted, and doses are sometimes reduced. Chemotherapy holidays can also be of benefit.
Another regimen for the metastatic setting involves the use of nab-P plus gemcitabine, which was shown in a phase III trial to improve survival (HR for death, 0.72).
The results aren’t quite as dramatic as those seen with FOLFIRINOX, but the regimen is slightly easier to manage, Dr. Tempero said, adding: “It’s still not a walk in the park.”
Myelosuppression, arthralgias, and neuropathy still occur, she explained.
Gemcitabine/capecitabine, which has been shown to improve progression-free survival, can also be used, and may be preferable in elderly patients who aren’t fit enough for the other regimens, she said.
“When I select treatment, I really sit down with the patient, and I look at their comorbidities and let them review the toxicities. They decide,” she said, explaining that she provides recommendations based on their concerns and input. “We do have a conversation and we talk about the goals of treatment, we talk about the toxicities.”
Future efforts for metastatic disease should build upon both FOLFIRINOX and gemcitabine/nab-P, she said.
However, because of the difficulty with administering FOLFIRINOX, only two of the 54 open phase I-III trials ongoing in the United States for metastatic disease incorporate the regimen.
Other treatment options include gemcitabine/cisplatin, GTX (gemcitabine/docetaxel/capecitabine), and gemcitabine/erlotinib. The former remains in the NCCN guidelines, primarily for those with hereditary forms of pancreatic cancer, and in particular for those in the DNA repair pathway (BRCA patients, for example).
“We actually have trials now focusing on just BRCA-related pancreatic cancer,” she said, noting that these patients are “exquisitely sensitive to cisplatin and don’t need a harsh regimen like FOLFIRINOX to get the same benefit.
GTX is a very active regimen, although it has never been compared with gemcitabine monotherapy in a randomized trial. However, because of its clear activity it remains in the NCCN guidelines as an option.
Gemcitabine/erlotinib also remains in the guidelines because of a tiny trial that showed a small benefit, but it is not a preferred combination, she said.
Future therapies
Efforts going forward are focusing on finding drugs that inactivate activated RAS, which is “a really big driver” in many cancers, as well as on addressing the microenvironment (such as the desmoplastic stroma that may help encourage invasion of metastases and/or impede drug delivery to the cancer), Dr. Tempero said.
“So there is a lot of interest right now in various forms of immunotherapy or in stromal remodeling so we can see what impact that has on the progression of this disease,” she said, noting that new agents in registration trials include ibrutinib, laparib, PEGPH20, and insulinlike growth factor 1 (IGF-1) inhibitors, and those in planning stages include chemokine (C-C motif) receptor 2 (CCR2) inhibitors and palbociclib.
“And I think we have opportunities in the maintenance setting and in the neoadjuvant setting to do window-of-opportunity trials where we can test new concepts, where we can get pharmacodynamic and biologic data to understand what these new agents are doing,” she said.
Collaborative effort to identify patients at risk
Population-level screening strategies for pancreatic cancer aren’t feasible because of the relatively low incidence of the disease, but efforts are underway to identify and screen high-risk groups.
“We actually have some tests that you could screen with, but they’re not perfect, and with a disease that occurs at the rate that [pancreatic cancer] does, you can’t screen the whole population, because you will find false positives, and you will cause unnecessary procedures more than you’ll find the cancer, Dr. Tempero said during a meeting with press at the NCCN annual conference.
Instead, it is important to identify and screen only those at high risk, she added.
Such a group might include patients with new-onset diabetes who experience weight loss.
New-onset diabetes can be caused by pancreatic cancer, and weight loss with diabetes is unexpected and should raise a red flag, Dr. Temepero explained, adding that an education gap among community physicians means these patients are sometimes cheered for the weight loss instead – and then they end up in the pancreatic disease clinic with metastatic disease 2 years later.
In an effort to better define and characterize this and other high-risk groups, the National Institute for Diabetes and Digestive and Kidney Diseases and the National Cancer Institute are working together to fund a network of institutions that will develop high-risk cohorts and begin deploying screening strategies. The effort is partly in response to the Recalcitrant Cancer Act passed in 2012 to “force more attention on funding pancreatic cancer research through the branches of the NIH,” she explained.
In this particular high-risk group, the institutions will look at the character of diabetes and the clinical correlates with pancreatic cancer.
“Once we hone in on these, we can use those – what we hope are – early-detection biomarkers, and if those are positive, then we would ask the patient to have a CT scan to look for pancreatic cancer,” she said.
Dr. Tempero reported serving as a scientific advisor and/or receiving grant/research support, consulting fees, and/or honoraria from Celgene Corporation, Champion Oncology, Cornerstone Pharmaceuticals, Eli Lilly, EMD Serono, Gilead Sciences, Halozyme Therapeutics, MCS Biotech Resources, NeoHealth, Novocure, Opsona Therapeutics, Pfizer, Portola Pharmaceuticals, and Threshold Pharmaceuticals.
ORLANDO – Overall cancer death rates are dropping dramatically, but pancreatic cancer mortality remains high.
“By 2020 we expect [pancreatic cancer] to be the second most common cause of cancer-related death, exceeded only by lung cancer, and if lung cancer deaths continue to fall – which we expect that they will – it will be the most common cause of cancer-related death,” Margaret A. Tempero, MD, said at the annual conference of the National Comprehensive Cancer Network.
Further, as the population ages there will be an increasing number of patients presenting with pancreatic cancer, said Dr. Tempero of the University of California, San Francisco.
Currently, 80% of pancreatic cancer patients are diagnosed with disease that is not amenable to resection, and 80% of those who have resection and adjuvant therapy experience relapse. The overall survival rate is only about 9%.
“This is really, really an aggressive malignancy,” Dr. Tempero said, noting that the survival among those with metastases who do not receive treatment is only about 3 months.
There are no early symptoms that direct attention to the pancreas. Additionally, some patients experience very early invasion and metastases; in fact, up to two-thirds of patients with lesions only 1 cm in size will already have lymph node metastasis, she said.
The disease tends to be chemoresistant, although this may be changing with treatment advances, but it is characterized by “a lot of desmoplastic stroma, so there’s a lot of microenvironment that’s perturbed around the malignancy,” making it difficult for drugs to permeate the stroma.
“That’s something we’re actively working on – ways that we can actually change the stroma so that we can get more drug into the cancer,” she said.
Another challenge is the disease’s “habit of elaborating a lot of cytokines that disable the person with the disease,” which can lead to frailty that makes it difficult to deliver potentially effective therapies that are well tolerated in patients with other types of cancer, she noted.
An important question is whether pancreatic cancer is diagnosed too late or metastasizes too early, and there is evidence to support both possibilities.
“Either way ... we need to work on better treatment,” she said.
Resectable/borderline resectable disease
One noteworthy recent advance for patients with resectable/borderline resectable disease is the addition of capecitabine to gemcitabine for adjuvant therapy. In the ESPAC 4 study published in March in the Lancet, the combination of gemcitabine and capecitabine showed a clear benefit over gemcitabine alone.
“So that has now entered [the NCCN] guidelines as an important option for adjuvant therapy,” said Dr. Tempero, chair of the NCCN pancreatic cancer guidelines panel.
Ongoing trials are also looking at the FOLFIRINOX (irinotecan plus 5-fluorouracil plus leucovorin plus oxaliplatin) and gemcitabine/nanoparticle albumin-bound paclitaxel (nab-P) regimens in the adjuvant setting. These have previously shown some efficacy in the metastatic setting.
“So we really wanted to get these therapies into the adjuvant setting as soon as we could,” she said.
In the ACCORD trial, FOLFIRINOX is being compared with gemcitabine in the postoperative adjuvant setting, and the APACT trial comparing gemcitabine/nab-P to gemcitabine monotherapy completed accrual last year.
“I’m pretty sure that we’ll have enough events on the APACT study by the end of this year, and hopefully we can present that data in the spring. I’m hoping it will be a positive trial for us,” she said.
Neoadjuvant therapy – a successful strategy used in many other malignancies – is also being looked at for pancreatic cancer.
A pilot study (A021101) completed last year suggested that chemotherapy (FOLFIRINOX for 2 months) and chemoradiation (capecitabine and radiation at 50.4 Gy) followed by surgical resection and adjuvant chemotherapy (gemcitabine for 2 months) provided some benefit in patients with borderline resectable pancreatic cancer. This trial led to another ongoing study (S1505) in which patients with borderline resectable disease will be treated with 4 months of FOLFIRINOX prior to resection, followed by chemoradiation and surgery or FOLFIRINOX and surgery, and patients with resectable disease will undergo resection followed by FOLFIRINOX and surgery or gemcitabine/nab-P and surgery.
“The goal is not to compare the two regimens; the goal is to identify the benchmarks that we get with these regimens. In other words, if you’re going to give FOLFIRINOX, what pathologic complete response rate can you expect? What will your R1 resection rate be? With gemcitabine and nab-paclitaxel, the same thing, because if you want to continue to build on these regimens in the neoadjuvant setting you need to know what you’re likely to get so you can make clinical trial assumptions when you add new drugs.
“Once we have these benchmarking data we can really sail in the neoadjuvant setting. It’s a great window-of-opportunity setting for new drugs, because you’re getting serial tissue,” Dr. Tempero said, explaining that in addition to resection of tissue, there is opportunity to get biopsies ahead of time and look at the effects of the drug.
Locally advanced disease
For locally advanced disease, studies have failed to show a benefit of adding radiation after chemotherapy, but radiation oncologists who argue that, “when your therapy gets better, my therapy gets better,” have a valid point, Dr. Tempero said.
For that reason, the Radiation Therapy Oncology group launched a trial to look at gemcitabine/nab-P with and without radiation, but had difficulty with enrollment due to resistance among some physicians who are opposed to radiation in this setting .
“So I don’t know that we will ever answer this question in locally advanced disease. What I can say ... is, in my mind, in locally advanced disease, the most important component is the chemotherapy,” she said.
Metastatic disease
When it comes to trials involving pancreatic cancer patients with metastatic disease, it is important to understand – and to convey to policymakers – that the goal is not only to provide better care in these patients who are at the end of their life, but also to identify strategies that can be used in the adjuvant and neoadjuvant settings, as this is part of the “overall mission of helping patients to feel better and live longer and be cured,” Dr. Tempero said.
One regimen currently used in the metastatic setting is FOLFIRINOX, which was shown in the Prodige 4-ACCORD 11 trial to be superior to gemcitabine monotherapy for survival (hazard ratio, 0.57).
“This is the first time we ever saw a hazard ratio below 0.6 in this disease,” she said, adding that for some patients this means “they can get tremendous benefit, they can come off chemotherapy and have a chemotherapy holiday,” she said.
That said, it’s a tough regimen, she added, explaining that it has dominating toxicities of myelosuppression, diarrhea, and neuropathy that can be irreversible.
Frail patients may not be able to tolerate the regimen, but modifications to the regimen may help. For example, the 5-fluorourasil bolus is often omitted, and doses are sometimes reduced. Chemotherapy holidays can also be of benefit.
Another regimen for the metastatic setting involves the use of nab-P plus gemcitabine, which was shown in a phase III trial to improve survival (HR for death, 0.72).
The results aren’t quite as dramatic as those seen with FOLFIRINOX, but the regimen is slightly easier to manage, Dr. Tempero said, adding: “It’s still not a walk in the park.”
Myelosuppression, arthralgias, and neuropathy still occur, she explained.
Gemcitabine/capecitabine, which has been shown to improve progression-free survival, can also be used, and may be preferable in elderly patients who aren’t fit enough for the other regimens, she said.
“When I select treatment, I really sit down with the patient, and I look at their comorbidities and let them review the toxicities. They decide,” she said, explaining that she provides recommendations based on their concerns and input. “We do have a conversation and we talk about the goals of treatment, we talk about the toxicities.”
Future efforts for metastatic disease should build upon both FOLFIRINOX and gemcitabine/nab-P, she said.
However, because of the difficulty with administering FOLFIRINOX, only two of the 54 open phase I-III trials ongoing in the United States for metastatic disease incorporate the regimen.
Other treatment options include gemcitabine/cisplatin, GTX (gemcitabine/docetaxel/capecitabine), and gemcitabine/erlotinib. The former remains in the NCCN guidelines, primarily for those with hereditary forms of pancreatic cancer, and in particular for those in the DNA repair pathway (BRCA patients, for example).
“We actually have trials now focusing on just BRCA-related pancreatic cancer,” she said, noting that these patients are “exquisitely sensitive to cisplatin and don’t need a harsh regimen like FOLFIRINOX to get the same benefit.
GTX is a very active regimen, although it has never been compared with gemcitabine monotherapy in a randomized trial. However, because of its clear activity it remains in the NCCN guidelines as an option.
Gemcitabine/erlotinib also remains in the guidelines because of a tiny trial that showed a small benefit, but it is not a preferred combination, she said.
Future therapies
Efforts going forward are focusing on finding drugs that inactivate activated RAS, which is “a really big driver” in many cancers, as well as on addressing the microenvironment (such as the desmoplastic stroma that may help encourage invasion of metastases and/or impede drug delivery to the cancer), Dr. Tempero said.
“So there is a lot of interest right now in various forms of immunotherapy or in stromal remodeling so we can see what impact that has on the progression of this disease,” she said, noting that new agents in registration trials include ibrutinib, laparib, PEGPH20, and insulinlike growth factor 1 (IGF-1) inhibitors, and those in planning stages include chemokine (C-C motif) receptor 2 (CCR2) inhibitors and palbociclib.
“And I think we have opportunities in the maintenance setting and in the neoadjuvant setting to do window-of-opportunity trials where we can test new concepts, where we can get pharmacodynamic and biologic data to understand what these new agents are doing,” she said.
Collaborative effort to identify patients at risk
Population-level screening strategies for pancreatic cancer aren’t feasible because of the relatively low incidence of the disease, but efforts are underway to identify and screen high-risk groups.
“We actually have some tests that you could screen with, but they’re not perfect, and with a disease that occurs at the rate that [pancreatic cancer] does, you can’t screen the whole population, because you will find false positives, and you will cause unnecessary procedures more than you’ll find the cancer, Dr. Tempero said during a meeting with press at the NCCN annual conference.
Instead, it is important to identify and screen only those at high risk, she added.
Such a group might include patients with new-onset diabetes who experience weight loss.
New-onset diabetes can be caused by pancreatic cancer, and weight loss with diabetes is unexpected and should raise a red flag, Dr. Temepero explained, adding that an education gap among community physicians means these patients are sometimes cheered for the weight loss instead – and then they end up in the pancreatic disease clinic with metastatic disease 2 years later.
In an effort to better define and characterize this and other high-risk groups, the National Institute for Diabetes and Digestive and Kidney Diseases and the National Cancer Institute are working together to fund a network of institutions that will develop high-risk cohorts and begin deploying screening strategies. The effort is partly in response to the Recalcitrant Cancer Act passed in 2012 to “force more attention on funding pancreatic cancer research through the branches of the NIH,” she explained.
In this particular high-risk group, the institutions will look at the character of diabetes and the clinical correlates with pancreatic cancer.
“Once we hone in on these, we can use those – what we hope are – early-detection biomarkers, and if those are positive, then we would ask the patient to have a CT scan to look for pancreatic cancer,” she said.
Dr. Tempero reported serving as a scientific advisor and/or receiving grant/research support, consulting fees, and/or honoraria from Celgene Corporation, Champion Oncology, Cornerstone Pharmaceuticals, Eli Lilly, EMD Serono, Gilead Sciences, Halozyme Therapeutics, MCS Biotech Resources, NeoHealth, Novocure, Opsona Therapeutics, Pfizer, Portola Pharmaceuticals, and Threshold Pharmaceuticals.
ORLANDO – Overall cancer death rates are dropping dramatically, but pancreatic cancer mortality remains high.
“By 2020 we expect [pancreatic cancer] to be the second most common cause of cancer-related death, exceeded only by lung cancer, and if lung cancer deaths continue to fall – which we expect that they will – it will be the most common cause of cancer-related death,” Margaret A. Tempero, MD, said at the annual conference of the National Comprehensive Cancer Network.
Further, as the population ages there will be an increasing number of patients presenting with pancreatic cancer, said Dr. Tempero of the University of California, San Francisco.
Currently, 80% of pancreatic cancer patients are diagnosed with disease that is not amenable to resection, and 80% of those who have resection and adjuvant therapy experience relapse. The overall survival rate is only about 9%.
“This is really, really an aggressive malignancy,” Dr. Tempero said, noting that the survival among those with metastases who do not receive treatment is only about 3 months.
There are no early symptoms that direct attention to the pancreas. Additionally, some patients experience very early invasion and metastases; in fact, up to two-thirds of patients with lesions only 1 cm in size will already have lymph node metastasis, she said.
The disease tends to be chemoresistant, although this may be changing with treatment advances, but it is characterized by “a lot of desmoplastic stroma, so there’s a lot of microenvironment that’s perturbed around the malignancy,” making it difficult for drugs to permeate the stroma.
“That’s something we’re actively working on – ways that we can actually change the stroma so that we can get more drug into the cancer,” she said.
Another challenge is the disease’s “habit of elaborating a lot of cytokines that disable the person with the disease,” which can lead to frailty that makes it difficult to deliver potentially effective therapies that are well tolerated in patients with other types of cancer, she noted.
An important question is whether pancreatic cancer is diagnosed too late or metastasizes too early, and there is evidence to support both possibilities.
“Either way ... we need to work on better treatment,” she said.
Resectable/borderline resectable disease
One noteworthy recent advance for patients with resectable/borderline resectable disease is the addition of capecitabine to gemcitabine for adjuvant therapy. In the ESPAC 4 study published in March in the Lancet, the combination of gemcitabine and capecitabine showed a clear benefit over gemcitabine alone.
“So that has now entered [the NCCN] guidelines as an important option for adjuvant therapy,” said Dr. Tempero, chair of the NCCN pancreatic cancer guidelines panel.
Ongoing trials are also looking at the FOLFIRINOX (irinotecan plus 5-fluorouracil plus leucovorin plus oxaliplatin) and gemcitabine/nanoparticle albumin-bound paclitaxel (nab-P) regimens in the adjuvant setting. These have previously shown some efficacy in the metastatic setting.
“So we really wanted to get these therapies into the adjuvant setting as soon as we could,” she said.
In the ACCORD trial, FOLFIRINOX is being compared with gemcitabine in the postoperative adjuvant setting, and the APACT trial comparing gemcitabine/nab-P to gemcitabine monotherapy completed accrual last year.
“I’m pretty sure that we’ll have enough events on the APACT study by the end of this year, and hopefully we can present that data in the spring. I’m hoping it will be a positive trial for us,” she said.
Neoadjuvant therapy – a successful strategy used in many other malignancies – is also being looked at for pancreatic cancer.
A pilot study (A021101) completed last year suggested that chemotherapy (FOLFIRINOX for 2 months) and chemoradiation (capecitabine and radiation at 50.4 Gy) followed by surgical resection and adjuvant chemotherapy (gemcitabine for 2 months) provided some benefit in patients with borderline resectable pancreatic cancer. This trial led to another ongoing study (S1505) in which patients with borderline resectable disease will be treated with 4 months of FOLFIRINOX prior to resection, followed by chemoradiation and surgery or FOLFIRINOX and surgery, and patients with resectable disease will undergo resection followed by FOLFIRINOX and surgery or gemcitabine/nab-P and surgery.
“The goal is not to compare the two regimens; the goal is to identify the benchmarks that we get with these regimens. In other words, if you’re going to give FOLFIRINOX, what pathologic complete response rate can you expect? What will your R1 resection rate be? With gemcitabine and nab-paclitaxel, the same thing, because if you want to continue to build on these regimens in the neoadjuvant setting you need to know what you’re likely to get so you can make clinical trial assumptions when you add new drugs.
“Once we have these benchmarking data we can really sail in the neoadjuvant setting. It’s a great window-of-opportunity setting for new drugs, because you’re getting serial tissue,” Dr. Tempero said, explaining that in addition to resection of tissue, there is opportunity to get biopsies ahead of time and look at the effects of the drug.
Locally advanced disease
For locally advanced disease, studies have failed to show a benefit of adding radiation after chemotherapy, but radiation oncologists who argue that, “when your therapy gets better, my therapy gets better,” have a valid point, Dr. Tempero said.
For that reason, the Radiation Therapy Oncology group launched a trial to look at gemcitabine/nab-P with and without radiation, but had difficulty with enrollment due to resistance among some physicians who are opposed to radiation in this setting .
“So I don’t know that we will ever answer this question in locally advanced disease. What I can say ... is, in my mind, in locally advanced disease, the most important component is the chemotherapy,” she said.
Metastatic disease
When it comes to trials involving pancreatic cancer patients with metastatic disease, it is important to understand – and to convey to policymakers – that the goal is not only to provide better care in these patients who are at the end of their life, but also to identify strategies that can be used in the adjuvant and neoadjuvant settings, as this is part of the “overall mission of helping patients to feel better and live longer and be cured,” Dr. Tempero said.
One regimen currently used in the metastatic setting is FOLFIRINOX, which was shown in the Prodige 4-ACCORD 11 trial to be superior to gemcitabine monotherapy for survival (hazard ratio, 0.57).
“This is the first time we ever saw a hazard ratio below 0.6 in this disease,” she said, adding that for some patients this means “they can get tremendous benefit, they can come off chemotherapy and have a chemotherapy holiday,” she said.
That said, it’s a tough regimen, she added, explaining that it has dominating toxicities of myelosuppression, diarrhea, and neuropathy that can be irreversible.
Frail patients may not be able to tolerate the regimen, but modifications to the regimen may help. For example, the 5-fluorourasil bolus is often omitted, and doses are sometimes reduced. Chemotherapy holidays can also be of benefit.
Another regimen for the metastatic setting involves the use of nab-P plus gemcitabine, which was shown in a phase III trial to improve survival (HR for death, 0.72).
The results aren’t quite as dramatic as those seen with FOLFIRINOX, but the regimen is slightly easier to manage, Dr. Tempero said, adding: “It’s still not a walk in the park.”
Myelosuppression, arthralgias, and neuropathy still occur, she explained.
Gemcitabine/capecitabine, which has been shown to improve progression-free survival, can also be used, and may be preferable in elderly patients who aren’t fit enough for the other regimens, she said.
“When I select treatment, I really sit down with the patient, and I look at their comorbidities and let them review the toxicities. They decide,” she said, explaining that she provides recommendations based on their concerns and input. “We do have a conversation and we talk about the goals of treatment, we talk about the toxicities.”
Future efforts for metastatic disease should build upon both FOLFIRINOX and gemcitabine/nab-P, she said.
However, because of the difficulty with administering FOLFIRINOX, only two of the 54 open phase I-III trials ongoing in the United States for metastatic disease incorporate the regimen.
Other treatment options include gemcitabine/cisplatin, GTX (gemcitabine/docetaxel/capecitabine), and gemcitabine/erlotinib. The former remains in the NCCN guidelines, primarily for those with hereditary forms of pancreatic cancer, and in particular for those in the DNA repair pathway (BRCA patients, for example).
“We actually have trials now focusing on just BRCA-related pancreatic cancer,” she said, noting that these patients are “exquisitely sensitive to cisplatin and don’t need a harsh regimen like FOLFIRINOX to get the same benefit.
GTX is a very active regimen, although it has never been compared with gemcitabine monotherapy in a randomized trial. However, because of its clear activity it remains in the NCCN guidelines as an option.
Gemcitabine/erlotinib also remains in the guidelines because of a tiny trial that showed a small benefit, but it is not a preferred combination, she said.
Future therapies
Efforts going forward are focusing on finding drugs that inactivate activated RAS, which is “a really big driver” in many cancers, as well as on addressing the microenvironment (such as the desmoplastic stroma that may help encourage invasion of metastases and/or impede drug delivery to the cancer), Dr. Tempero said.
“So there is a lot of interest right now in various forms of immunotherapy or in stromal remodeling so we can see what impact that has on the progression of this disease,” she said, noting that new agents in registration trials include ibrutinib, laparib, PEGPH20, and insulinlike growth factor 1 (IGF-1) inhibitors, and those in planning stages include chemokine (C-C motif) receptor 2 (CCR2) inhibitors and palbociclib.
“And I think we have opportunities in the maintenance setting and in the neoadjuvant setting to do window-of-opportunity trials where we can test new concepts, where we can get pharmacodynamic and biologic data to understand what these new agents are doing,” she said.
Collaborative effort to identify patients at risk
Population-level screening strategies for pancreatic cancer aren’t feasible because of the relatively low incidence of the disease, but efforts are underway to identify and screen high-risk groups.
“We actually have some tests that you could screen with, but they’re not perfect, and with a disease that occurs at the rate that [pancreatic cancer] does, you can’t screen the whole population, because you will find false positives, and you will cause unnecessary procedures more than you’ll find the cancer, Dr. Tempero said during a meeting with press at the NCCN annual conference.
Instead, it is important to identify and screen only those at high risk, she added.
Such a group might include patients with new-onset diabetes who experience weight loss.
New-onset diabetes can be caused by pancreatic cancer, and weight loss with diabetes is unexpected and should raise a red flag, Dr. Temepero explained, adding that an education gap among community physicians means these patients are sometimes cheered for the weight loss instead – and then they end up in the pancreatic disease clinic with metastatic disease 2 years later.
In an effort to better define and characterize this and other high-risk groups, the National Institute for Diabetes and Digestive and Kidney Diseases and the National Cancer Institute are working together to fund a network of institutions that will develop high-risk cohorts and begin deploying screening strategies. The effort is partly in response to the Recalcitrant Cancer Act passed in 2012 to “force more attention on funding pancreatic cancer research through the branches of the NIH,” she explained.
In this particular high-risk group, the institutions will look at the character of diabetes and the clinical correlates with pancreatic cancer.
“Once we hone in on these, we can use those – what we hope are – early-detection biomarkers, and if those are positive, then we would ask the patient to have a CT scan to look for pancreatic cancer,” she said.
Dr. Tempero reported serving as a scientific advisor and/or receiving grant/research support, consulting fees, and/or honoraria from Celgene Corporation, Champion Oncology, Cornerstone Pharmaceuticals, Eli Lilly, EMD Serono, Gilead Sciences, Halozyme Therapeutics, MCS Biotech Resources, NeoHealth, Novocure, Opsona Therapeutics, Pfizer, Portola Pharmaceuticals, and Threshold Pharmaceuticals.
AT THE NCCN ANNUAL CONFERENCE
Key clinical point:
Disclosures: Dr. Tempero reported serving as a scientific advisor and/or receiving grant/research support, consulting fees, and/or honoraria from Celgene Corporation, Champion Oncology, Cornerstone Pharmaceuticals, Eli Lilly, EMD Serono, Gilead Sciences, Halozyme Therapeutics, MCS Biotech Resources, NeoHealth, Novocure, Opsona Therapeutics, Pfizer, Portola Pharmaceuticals, and Threshold Pharmaceuticals.
Myelofibrosis therapies moving beyond ruxolitinib
ORLANDO – Ruxolitinib is currently the only drug approved for the treatment of myelofibrosis, but a number of other therapies are in clinical trials and showing promise, according to Ruben A. Mesa, MD.
“Our field ... is rapidly in evolution,” he said at the annual conference of the National Comprehensive Cancer Network, adding that efforts are underway to determine where these drugs might fit in.
Among those being considered specifically for myelofibrosis are pacritinib, momelotinib, PRM-151, and imetelstat, he said.
Pacritinib
This JAK2/FT3 inhibitor reduces splenomegaly and its related symptoms, but may also help patients who have low platelet counts and a worse prognosis. Pacritinib has demonstrated safety in that population, said Dr. Mesa of Mayo Clinic Cancer Center, Phoenix, Ariz.
Concerns about increased mortality related to risk of intracranial hemorrhage and cardiovascular events led the Food and Drug Administration to place a full clinical hold on pacritinib in February 2016. That hold was lifted in January 2017 when data from the randomized, controlled, phase III PERSIST-2 study, as presented at the American Society of Hematology annual meeting in December 2016, showed the risks did not hold up among study patients.
PERSIST-2 compared pacritinib doses of 400 mg once daily and 200 mg twice daily with best alternative therapy, which was ruxolitinib in most patients, Dr. Mesa said. He noted that the study included patients who had marked thrombocytopenia and were allowed prior JAK2 inhibitor exposure.
The 200-mg twice-daily dosing was superior in achieving spleen volume reductions greater than 35%: 22% of patients in the 200-mg dosing group vs. 15% in the 400-mg once-daily dosing group, compared with 3% of those receiving best available therapy. The twice-daily dosing group also experienced greater symptom improvement: Thirty-two percent in the 200-mg twice-daily group vs. 17% in the 400-mg once-daily group achieved at least a 50% reduction in total symptom scale scores, compared with 14% of those receiving best available therapy.
Additional studies of pacritinib will begin enrolling soon, Dr. Mesa said, noting that these studies will look at lower doses in an effort to identify the minimally effective dose with the optimal balance of safety and efficacy.
Momelotinib
Momelotinib, a JAK1/JAK2 inhibitor, was evaluated in two large recently concluded phase III trials (SIMPLIFY-1 and SIMPLIFY-2). SIMPIFY-1 compared momelotinib to ruxolitinib in the front-line setting, and showed momelotinib to be noninferior for reducing splenomegaly.
“However, it was inferior for improvement in the symptom burden,” Dr. Mesa said, noting that while there seemed to be a favorable difference in terms of anemia, the study was structured in such a way that the agent needed to be noninferior for both spleen and symptoms for the anemia response to be evaluable.
SIMPLIFY-2 evaluated momelotinib in patients who had not responded to ruxolitinib. In this second-line setting, momelotinib was not superior to the best alternative therapy, but since the vast majority of the ruxolitinib failure patients remained on ruxolitinib, it is “a bit of a confounded study to assess,” he said.
The top-line data from these studies were issued in a press release from the manufacturer (Gilead) in November 2016, and the complete results are expected to be made public in the near future, at which time more will be known about the next steps for momelotinib, he said.
If approved, pacritinib and momelotinib could ultimately be positioned as a front-line and/or second-line treatment for myelofibrosis, Dr. Mesa predicted.
There has been a goal, in terms of trial design, to see if there is a niche for these drugs in the front-line setting based on blood counts.
“Those recommendations would clearly be very much dependent on the risk, the safety, and the efficacy,” he said.
PRM-151
This antifibrosing agent was shown to be active in early-phase trials – including in stage 1 of an adaptive phase II trial. PRM-151 is currently being evaluated in the fully-accrued ongoing phase II PROMOTE study to determine whether it improves splenomegaly, symptoms, and cytopenia. The primary endpoint of the study is the bone marrow response rate. Study subjects are patients with primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocythemia myelofibrosis, and grade 2-3 fibrosis, said Dr. Mesa, who is the principal investigator for the study.
Imetelstat
This telomerase inhibitor is being evaluated in the randomized, multicenter, phase II IMbark study, designed to assess spleen volume and total symptom score as primary end points. Earlier studies have shown deep responses in patients with myelofibrosis who were treated with imetelstat, Dr. Mesa said.
The IMbark study (NCT02426086) was originally designed to evaluate two dosing regimens administered as a single agent to participants with intermediate-2 or high-risk myelofibrosis who were refractory to or relapsed after JAK inhibitor treatment. Participants received either 9.4 mg/kg or 4.7 mg/kg intravenously every 3 weeks until disease progression, unacceptable toxicity, or study end.
According to information from Geron, which is developing the agent, enrollment of new participants is currently suspended following a planned internal data review, but enrollment “may be resumed after a second internal data review that is planned by the end of the second quarter of 2017.” If resumed, enrollment would be only to the higher-dose treatment arm; patients initially randomized to that arm may continue treatment, and those randomized to the lower-dose arm may see their dose increased at the investigator’s discretion.
If approved, PRM-151 and imetelstat would likely be positioned as second-line treatments for myelofibrosis, Dr. Mesa said, noting that determining which patients would be most likely to benefit from treatment with these agents would require a close look at the evidence from second-line studies.
Combination therapies
In addition to these investigational treatments, nearly 20 different combination treatments involving ruxolitinib plus another agent have been looked at to try to further improve activity. Some improvements in splenomegaly have been seen with combinations including ruxolitinib and either panobinostat (a histone deacytelase inhibitor), LDE225 (a hedgehog signaling pathway inhibitor), and BKM120 (a PI3-kinase inhibitor), he noted.
“For the area of greatest interest – which was to see incremental improvements in thrombocytopenia, anemia, or fibrosis – there have been favorable data, but they have been modest. It’s not quite clear that there is a combination that is ready for prime time, nor is there yet a combination that we have recommended through the treatment guidelines to be utilized for these patients,” he said.
Dr. Mesa has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals; Celgene Corporation, CTI BioPharma, the maker of pacritinib; Galena Biopharma; Gilead, the maker of momelotinib; Incyte, the maker of ruxolitinib; Novartis, the maker of panobinostat and BKM120; and Promedior, the maker of PRM-151.
ORLANDO – Ruxolitinib is currently the only drug approved for the treatment of myelofibrosis, but a number of other therapies are in clinical trials and showing promise, according to Ruben A. Mesa, MD.
“Our field ... is rapidly in evolution,” he said at the annual conference of the National Comprehensive Cancer Network, adding that efforts are underway to determine where these drugs might fit in.
Among those being considered specifically for myelofibrosis are pacritinib, momelotinib, PRM-151, and imetelstat, he said.
Pacritinib
This JAK2/FT3 inhibitor reduces splenomegaly and its related symptoms, but may also help patients who have low platelet counts and a worse prognosis. Pacritinib has demonstrated safety in that population, said Dr. Mesa of Mayo Clinic Cancer Center, Phoenix, Ariz.
Concerns about increased mortality related to risk of intracranial hemorrhage and cardiovascular events led the Food and Drug Administration to place a full clinical hold on pacritinib in February 2016. That hold was lifted in January 2017 when data from the randomized, controlled, phase III PERSIST-2 study, as presented at the American Society of Hematology annual meeting in December 2016, showed the risks did not hold up among study patients.
PERSIST-2 compared pacritinib doses of 400 mg once daily and 200 mg twice daily with best alternative therapy, which was ruxolitinib in most patients, Dr. Mesa said. He noted that the study included patients who had marked thrombocytopenia and were allowed prior JAK2 inhibitor exposure.
The 200-mg twice-daily dosing was superior in achieving spleen volume reductions greater than 35%: 22% of patients in the 200-mg dosing group vs. 15% in the 400-mg once-daily dosing group, compared with 3% of those receiving best available therapy. The twice-daily dosing group also experienced greater symptom improvement: Thirty-two percent in the 200-mg twice-daily group vs. 17% in the 400-mg once-daily group achieved at least a 50% reduction in total symptom scale scores, compared with 14% of those receiving best available therapy.
Additional studies of pacritinib will begin enrolling soon, Dr. Mesa said, noting that these studies will look at lower doses in an effort to identify the minimally effective dose with the optimal balance of safety and efficacy.
Momelotinib
Momelotinib, a JAK1/JAK2 inhibitor, was evaluated in two large recently concluded phase III trials (SIMPLIFY-1 and SIMPLIFY-2). SIMPIFY-1 compared momelotinib to ruxolitinib in the front-line setting, and showed momelotinib to be noninferior for reducing splenomegaly.
“However, it was inferior for improvement in the symptom burden,” Dr. Mesa said, noting that while there seemed to be a favorable difference in terms of anemia, the study was structured in such a way that the agent needed to be noninferior for both spleen and symptoms for the anemia response to be evaluable.
SIMPLIFY-2 evaluated momelotinib in patients who had not responded to ruxolitinib. In this second-line setting, momelotinib was not superior to the best alternative therapy, but since the vast majority of the ruxolitinib failure patients remained on ruxolitinib, it is “a bit of a confounded study to assess,” he said.
The top-line data from these studies were issued in a press release from the manufacturer (Gilead) in November 2016, and the complete results are expected to be made public in the near future, at which time more will be known about the next steps for momelotinib, he said.
If approved, pacritinib and momelotinib could ultimately be positioned as a front-line and/or second-line treatment for myelofibrosis, Dr. Mesa predicted.
There has been a goal, in terms of trial design, to see if there is a niche for these drugs in the front-line setting based on blood counts.
“Those recommendations would clearly be very much dependent on the risk, the safety, and the efficacy,” he said.
PRM-151
This antifibrosing agent was shown to be active in early-phase trials – including in stage 1 of an adaptive phase II trial. PRM-151 is currently being evaluated in the fully-accrued ongoing phase II PROMOTE study to determine whether it improves splenomegaly, symptoms, and cytopenia. The primary endpoint of the study is the bone marrow response rate. Study subjects are patients with primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocythemia myelofibrosis, and grade 2-3 fibrosis, said Dr. Mesa, who is the principal investigator for the study.
Imetelstat
This telomerase inhibitor is being evaluated in the randomized, multicenter, phase II IMbark study, designed to assess spleen volume and total symptom score as primary end points. Earlier studies have shown deep responses in patients with myelofibrosis who were treated with imetelstat, Dr. Mesa said.
The IMbark study (NCT02426086) was originally designed to evaluate two dosing regimens administered as a single agent to participants with intermediate-2 or high-risk myelofibrosis who were refractory to or relapsed after JAK inhibitor treatment. Participants received either 9.4 mg/kg or 4.7 mg/kg intravenously every 3 weeks until disease progression, unacceptable toxicity, or study end.
According to information from Geron, which is developing the agent, enrollment of new participants is currently suspended following a planned internal data review, but enrollment “may be resumed after a second internal data review that is planned by the end of the second quarter of 2017.” If resumed, enrollment would be only to the higher-dose treatment arm; patients initially randomized to that arm may continue treatment, and those randomized to the lower-dose arm may see their dose increased at the investigator’s discretion.
If approved, PRM-151 and imetelstat would likely be positioned as second-line treatments for myelofibrosis, Dr. Mesa said, noting that determining which patients would be most likely to benefit from treatment with these agents would require a close look at the evidence from second-line studies.
Combination therapies
In addition to these investigational treatments, nearly 20 different combination treatments involving ruxolitinib plus another agent have been looked at to try to further improve activity. Some improvements in splenomegaly have been seen with combinations including ruxolitinib and either panobinostat (a histone deacytelase inhibitor), LDE225 (a hedgehog signaling pathway inhibitor), and BKM120 (a PI3-kinase inhibitor), he noted.
“For the area of greatest interest – which was to see incremental improvements in thrombocytopenia, anemia, or fibrosis – there have been favorable data, but they have been modest. It’s not quite clear that there is a combination that is ready for prime time, nor is there yet a combination that we have recommended through the treatment guidelines to be utilized for these patients,” he said.
Dr. Mesa has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals; Celgene Corporation, CTI BioPharma, the maker of pacritinib; Galena Biopharma; Gilead, the maker of momelotinib; Incyte, the maker of ruxolitinib; Novartis, the maker of panobinostat and BKM120; and Promedior, the maker of PRM-151.
ORLANDO – Ruxolitinib is currently the only drug approved for the treatment of myelofibrosis, but a number of other therapies are in clinical trials and showing promise, according to Ruben A. Mesa, MD.
“Our field ... is rapidly in evolution,” he said at the annual conference of the National Comprehensive Cancer Network, adding that efforts are underway to determine where these drugs might fit in.
Among those being considered specifically for myelofibrosis are pacritinib, momelotinib, PRM-151, and imetelstat, he said.
Pacritinib
This JAK2/FT3 inhibitor reduces splenomegaly and its related symptoms, but may also help patients who have low platelet counts and a worse prognosis. Pacritinib has demonstrated safety in that population, said Dr. Mesa of Mayo Clinic Cancer Center, Phoenix, Ariz.
Concerns about increased mortality related to risk of intracranial hemorrhage and cardiovascular events led the Food and Drug Administration to place a full clinical hold on pacritinib in February 2016. That hold was lifted in January 2017 when data from the randomized, controlled, phase III PERSIST-2 study, as presented at the American Society of Hematology annual meeting in December 2016, showed the risks did not hold up among study patients.
PERSIST-2 compared pacritinib doses of 400 mg once daily and 200 mg twice daily with best alternative therapy, which was ruxolitinib in most patients, Dr. Mesa said. He noted that the study included patients who had marked thrombocytopenia and were allowed prior JAK2 inhibitor exposure.
The 200-mg twice-daily dosing was superior in achieving spleen volume reductions greater than 35%: 22% of patients in the 200-mg dosing group vs. 15% in the 400-mg once-daily dosing group, compared with 3% of those receiving best available therapy. The twice-daily dosing group also experienced greater symptom improvement: Thirty-two percent in the 200-mg twice-daily group vs. 17% in the 400-mg once-daily group achieved at least a 50% reduction in total symptom scale scores, compared with 14% of those receiving best available therapy.
Additional studies of pacritinib will begin enrolling soon, Dr. Mesa said, noting that these studies will look at lower doses in an effort to identify the minimally effective dose with the optimal balance of safety and efficacy.
Momelotinib
Momelotinib, a JAK1/JAK2 inhibitor, was evaluated in two large recently concluded phase III trials (SIMPLIFY-1 and SIMPLIFY-2). SIMPIFY-1 compared momelotinib to ruxolitinib in the front-line setting, and showed momelotinib to be noninferior for reducing splenomegaly.
“However, it was inferior for improvement in the symptom burden,” Dr. Mesa said, noting that while there seemed to be a favorable difference in terms of anemia, the study was structured in such a way that the agent needed to be noninferior for both spleen and symptoms for the anemia response to be evaluable.
SIMPLIFY-2 evaluated momelotinib in patients who had not responded to ruxolitinib. In this second-line setting, momelotinib was not superior to the best alternative therapy, but since the vast majority of the ruxolitinib failure patients remained on ruxolitinib, it is “a bit of a confounded study to assess,” he said.
The top-line data from these studies were issued in a press release from the manufacturer (Gilead) in November 2016, and the complete results are expected to be made public in the near future, at which time more will be known about the next steps for momelotinib, he said.
If approved, pacritinib and momelotinib could ultimately be positioned as a front-line and/or second-line treatment for myelofibrosis, Dr. Mesa predicted.
There has been a goal, in terms of trial design, to see if there is a niche for these drugs in the front-line setting based on blood counts.
“Those recommendations would clearly be very much dependent on the risk, the safety, and the efficacy,” he said.
PRM-151
This antifibrosing agent was shown to be active in early-phase trials – including in stage 1 of an adaptive phase II trial. PRM-151 is currently being evaluated in the fully-accrued ongoing phase II PROMOTE study to determine whether it improves splenomegaly, symptoms, and cytopenia. The primary endpoint of the study is the bone marrow response rate. Study subjects are patients with primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocythemia myelofibrosis, and grade 2-3 fibrosis, said Dr. Mesa, who is the principal investigator for the study.
Imetelstat
This telomerase inhibitor is being evaluated in the randomized, multicenter, phase II IMbark study, designed to assess spleen volume and total symptom score as primary end points. Earlier studies have shown deep responses in patients with myelofibrosis who were treated with imetelstat, Dr. Mesa said.
The IMbark study (NCT02426086) was originally designed to evaluate two dosing regimens administered as a single agent to participants with intermediate-2 or high-risk myelofibrosis who were refractory to or relapsed after JAK inhibitor treatment. Participants received either 9.4 mg/kg or 4.7 mg/kg intravenously every 3 weeks until disease progression, unacceptable toxicity, or study end.
According to information from Geron, which is developing the agent, enrollment of new participants is currently suspended following a planned internal data review, but enrollment “may be resumed after a second internal data review that is planned by the end of the second quarter of 2017.” If resumed, enrollment would be only to the higher-dose treatment arm; patients initially randomized to that arm may continue treatment, and those randomized to the lower-dose arm may see their dose increased at the investigator’s discretion.
If approved, PRM-151 and imetelstat would likely be positioned as second-line treatments for myelofibrosis, Dr. Mesa said, noting that determining which patients would be most likely to benefit from treatment with these agents would require a close look at the evidence from second-line studies.
Combination therapies
In addition to these investigational treatments, nearly 20 different combination treatments involving ruxolitinib plus another agent have been looked at to try to further improve activity. Some improvements in splenomegaly have been seen with combinations including ruxolitinib and either panobinostat (a histone deacytelase inhibitor), LDE225 (a hedgehog signaling pathway inhibitor), and BKM120 (a PI3-kinase inhibitor), he noted.
“For the area of greatest interest – which was to see incremental improvements in thrombocytopenia, anemia, or fibrosis – there have been favorable data, but they have been modest. It’s not quite clear that there is a combination that is ready for prime time, nor is there yet a combination that we have recommended through the treatment guidelines to be utilized for these patients,” he said.
Dr. Mesa has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals; Celgene Corporation, CTI BioPharma, the maker of pacritinib; Galena Biopharma; Gilead, the maker of momelotinib; Incyte, the maker of ruxolitinib; Novartis, the maker of panobinostat and BKM120; and Promedior, the maker of PRM-151.
EXPERT ANALYSIS AT THE NCCN ANNUAL CONFERENCE
NCCN myelofibrosis guideline: Patient voice is key
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
EXPERT ANALYSIS AT THE NCCN ANNUAL CONFERENCE
Venetoclax produces durable effects in relapsed/refractory CLL
ORLANDO – In patients with relapsed or refractory chronic lymphocytic leukemia (CLL), the results with venetoclax continue to be encouraging, and recent findings from a multicenter phase Ib study hint that venetoclax may also provide durable responses – even with treatment discontinuation.
Venetoclax is an orally bioavailable selective BCL2 inhibitor that is typically given in an open-ended fashion. Toxicity – including tumor lysis syndrome – is always a concern, however, and the issue of whether open-ended administration is necessary is an important question, Andrew D. Zelenetz, MD, PhD, said at the annual conference of the National Comprehensive Cancer Network.
In one phase II multicenter study of venetoclax monotherapy in 107 patients with relapsed/refractory CLL with del(17p) at 31 centers in the United States, Canada, and Europe, the overall response rate was 79.4% based on an independent review committee assessment, (Lancet Oncol. 2016[17]:768-78).
Treatment included once-daily venetoclax beginning with a dose of 20 mg that was ramped up to 50, 100, 200, and 400 mg over 4-5 weeks, followed by daily 400 mg continuous dosing until disease progression or discontinuation for another reason.
Notably, 18 of 85 patients from the study who achieved an objective response were minimal residual disease (MRD)–negative in peripheral blood samples – an outcome that has not been seen with tyrosine kinase inhibitors, noted Dr. Zelenetz of Memorial Sloan Kettering Cancer Center, New York.
The durability of venetoclax’s activity in the study was 84.7% at 12 months in all responders; 100% in those who achieved complete response, complete response with incomplete recovery of blood counts, or nodular partial remission; and 94.4% in the MRD-negative patients.
The authors concluded that venetoclax monotherapy is active and well tolerated in patients with relapsed or refractory del(17p) chronic lymphocytic leukemia, and that given the distinct mechanism of action of this new therapeutic option for these very poor-prognosis patients, it deserves further investigation as part of a combination or as part of sequential treatment with other novel targeted agents.
The finding that patients on venetoclax can achieve MRD negativity also raised the question of whether treatment can be stopped, Dr. Zelenetz said.
“Because who wants to be on a drug forever? Nobody,” he added.
This question was explored in a study published in February by Seymour et al., which provided early evidence that stopping treatment may indeed be feasible in some patients (Lancet Oncol. 2017;18[2]:230-40).
Venetoclax in this study was given in a dose-escalating fashion to target doses of 200-600 mg daily, in 49 patients with relapsed or refractory “moderately heavily pretreated” CLL. Rituximab was added at a dose of 375 mg/m2 in month 1 and 500 mg/m2 in months 2-6.
Patients had the option of stopping treatment if they achieved a complete response.
The overall response rate was 86%, including a complete response in 51% of patients. Two-year estimates for progression-free survival and ongoing response were 82% and 89% respectively.
MRD negativity was attained in 80% of complete responders and 57% of patients overall. Thirteen responders discontinued all treatment, and at the time of publication, 11 MRD-negative responders who discontinued therapy remained progression free off therapy. Two MRD-positive patients who achieved complete response and discontinued therapy progressed after 2 years, but were able to recapture response once they restarted the drug.
“So it’s really quite interesting. We might have durable responses after discontinuation of this drug in an MRD-negative state,” Dr. Zelenetz said.
Of note, the latest update to the NCCN guidelines for the treatment of CLL/SLL (small lymphocytic lymphoma) included the addition of “+/– rituximab” as part of the “suggested treatment regimen” of venetoclax in the relapsed/refractory disease setting. This recommendation is category 2A, meaning it is based on lower level evidence with uniform NCCN consensus that the intervention is appropriate.
Venetoclax: adverse events of special interest
In these studies, venetoclax was considered well tolerated, but attention to adverse events and their prevention and management – particularly with respect to tumor lysis syndrome – is essential, Dr. Zelenetz said.
In the phase II study by Stilgenbauer et al., adverse events of special interest included grade 3/4 neutropenia, which occurred in 40% of patients. This was manageable with dose interruptions (five patients) or reductions (four patients), or with granulocyte–colony stimulating factor and antibiotics (six patients, including one who received only antibiotics). None of the patients permanently discontinued treatment.
Infections occurred in 72% of patients, and grade 3 or greater infections occurred in 20% of patients. The most common overall were upper respiratory infections (15%), nasopharyngitis (14%), and urinary tract infections (9%).
Serious infections occurring in two or more patients were pneumonia, lower respiratory tract infection, and upper respiratory tract infection. One patient died from septic shock, 10 had infections leading to venetoclax interruption, and 2 had infections leading to dose reduction.
No mandated infection prophylaxis was used in this study.
Serious adverse events occurred in 59 patients (55%). The most common, occurring in at least 5% of patients, were pyrexia, autoimmune hemolytic anemia, pneumonia, and febrile neutropenia. Thirteen had adverse events leading to dose reductions, most commonly due to neutropenia, thrombocytopenia, and febrile neutropenia.
Laboratory-confirmed tumor lysis syndrome was reported in five patients during the ramp-up period, including four who developed the syndrome within the first 2 days of treatment. All cases resolved without clinical sequelae. Treatment was continued without interruption in three patients with tumor lysis syndrome, who received only electrolyte management, and two patients had a 1-day treatment interruption. Both resumed dosing the next day.
In the phase Ib study by Seymour et al., common grade 1-2 toxicities included upper respiratory tract infections, diarrhea, and nausea occurring in 57%, 55%, and 53% of patients, respectively. Grade 3-4 adverse events occurred in 76% of 49 patients, and most often included neutropenia (12% of patients), thrombocytopenia (16%), anemia (14%), febrile neutropenia (12%), and leukopenia (12%). The most common serious adverse events were pyrexia (12%), febrile neutropenia (10%), lower respiratory tract infection (6%), and pneumonia (6%). Clinical tumor lysis syndrome occurred in two patients who initiated venetoclax at 50 mg, one of whom died as a result.
After enhancement of tumor lysis syndrome prophylaxis measures and reduction of the starting dose of venetoclax to 20 mg, no additional cases occurred, the authors reported.
Mitigating tumor lysis syndrome risk
General measures for mitigating the risk of tumor lysis syndrome include identification of patients at increased risk, initiation of prophylaxis with hydration and a uric acid reducing agent, and initiation of venetoclax at a 20 mg dose for 1 week, with gradual step-wise ramp-up over 5 weeks to the target dose, Dr. Zelenetz noted.
As reported by Stilgenbauer, et al., patients with a nodal mass less than 5 cm and absolute lymphocyte count (ALC) of 25,000 or less are considered at low risk for tumor lysis syndrome, those with a nodal mass of 5 cm to less than 10 cm or ALC greater than 25,000 are at medium risk, and those with a nodal mass of 10 cm or greater or nodal mass of 5 cm or greater and ALC of greater than 25,000 are considered to be at high risk.
High-risk patients in the study received inpatient venetoclax dosing and monitoring at 4, 8, 12, and 24 hours with 20 mg and 50 mg dosing, as well as outpatient intravenous hydration at 100 mg if there was no indication to hospitalize, and post-dose 8-24 hour laboratory monitoring at 100 mg and above.
Medium-risk patients received IV hydration at 20 and 50 mg dosing, inpatient care if creatinine clearance was less than 80 mL/min or if there was a high tumor burden, and postdose 8- and 24-hour laboratory monitoring after the initial dose and at dose escalations. Low-risk patients received outpatient dosing at all dose levels in the absence of an indication to hospitalize, and postdose 8- and 24-hour laboratory monitoring after the initial dose and at dose increases.
“Unfortunately, the dose-limiting toxicity of venetoclax is fatal tumor lysis,” Dr. Zelenetz said, adding that by increasing the dose slowly over time according to current treatment recommendations – from 20 mg, to 50, 100, 200, and 400 mg at weekly intervals, this complication can be avoided.
Dr. Zelenetz reported receiving consulting fees, honoraria, and/or grant/research support from Genentech, the maker of venetoclax (Venclexta), and a wide variety of other drug companies.
ORLANDO – In patients with relapsed or refractory chronic lymphocytic leukemia (CLL), the results with venetoclax continue to be encouraging, and recent findings from a multicenter phase Ib study hint that venetoclax may also provide durable responses – even with treatment discontinuation.
Venetoclax is an orally bioavailable selective BCL2 inhibitor that is typically given in an open-ended fashion. Toxicity – including tumor lysis syndrome – is always a concern, however, and the issue of whether open-ended administration is necessary is an important question, Andrew D. Zelenetz, MD, PhD, said at the annual conference of the National Comprehensive Cancer Network.
In one phase II multicenter study of venetoclax monotherapy in 107 patients with relapsed/refractory CLL with del(17p) at 31 centers in the United States, Canada, and Europe, the overall response rate was 79.4% based on an independent review committee assessment, (Lancet Oncol. 2016[17]:768-78).
Treatment included once-daily venetoclax beginning with a dose of 20 mg that was ramped up to 50, 100, 200, and 400 mg over 4-5 weeks, followed by daily 400 mg continuous dosing until disease progression or discontinuation for another reason.
Notably, 18 of 85 patients from the study who achieved an objective response were minimal residual disease (MRD)–negative in peripheral blood samples – an outcome that has not been seen with tyrosine kinase inhibitors, noted Dr. Zelenetz of Memorial Sloan Kettering Cancer Center, New York.
The durability of venetoclax’s activity in the study was 84.7% at 12 months in all responders; 100% in those who achieved complete response, complete response with incomplete recovery of blood counts, or nodular partial remission; and 94.4% in the MRD-negative patients.
The authors concluded that venetoclax monotherapy is active and well tolerated in patients with relapsed or refractory del(17p) chronic lymphocytic leukemia, and that given the distinct mechanism of action of this new therapeutic option for these very poor-prognosis patients, it deserves further investigation as part of a combination or as part of sequential treatment with other novel targeted agents.
The finding that patients on venetoclax can achieve MRD negativity also raised the question of whether treatment can be stopped, Dr. Zelenetz said.
“Because who wants to be on a drug forever? Nobody,” he added.
This question was explored in a study published in February by Seymour et al., which provided early evidence that stopping treatment may indeed be feasible in some patients (Lancet Oncol. 2017;18[2]:230-40).
Venetoclax in this study was given in a dose-escalating fashion to target doses of 200-600 mg daily, in 49 patients with relapsed or refractory “moderately heavily pretreated” CLL. Rituximab was added at a dose of 375 mg/m2 in month 1 and 500 mg/m2 in months 2-6.
Patients had the option of stopping treatment if they achieved a complete response.
The overall response rate was 86%, including a complete response in 51% of patients. Two-year estimates for progression-free survival and ongoing response were 82% and 89% respectively.
MRD negativity was attained in 80% of complete responders and 57% of patients overall. Thirteen responders discontinued all treatment, and at the time of publication, 11 MRD-negative responders who discontinued therapy remained progression free off therapy. Two MRD-positive patients who achieved complete response and discontinued therapy progressed after 2 years, but were able to recapture response once they restarted the drug.
“So it’s really quite interesting. We might have durable responses after discontinuation of this drug in an MRD-negative state,” Dr. Zelenetz said.
Of note, the latest update to the NCCN guidelines for the treatment of CLL/SLL (small lymphocytic lymphoma) included the addition of “+/– rituximab” as part of the “suggested treatment regimen” of venetoclax in the relapsed/refractory disease setting. This recommendation is category 2A, meaning it is based on lower level evidence with uniform NCCN consensus that the intervention is appropriate.
Venetoclax: adverse events of special interest
In these studies, venetoclax was considered well tolerated, but attention to adverse events and their prevention and management – particularly with respect to tumor lysis syndrome – is essential, Dr. Zelenetz said.
In the phase II study by Stilgenbauer et al., adverse events of special interest included grade 3/4 neutropenia, which occurred in 40% of patients. This was manageable with dose interruptions (five patients) or reductions (four patients), or with granulocyte–colony stimulating factor and antibiotics (six patients, including one who received only antibiotics). None of the patients permanently discontinued treatment.
Infections occurred in 72% of patients, and grade 3 or greater infections occurred in 20% of patients. The most common overall were upper respiratory infections (15%), nasopharyngitis (14%), and urinary tract infections (9%).
Serious infections occurring in two or more patients were pneumonia, lower respiratory tract infection, and upper respiratory tract infection. One patient died from septic shock, 10 had infections leading to venetoclax interruption, and 2 had infections leading to dose reduction.
No mandated infection prophylaxis was used in this study.
Serious adverse events occurred in 59 patients (55%). The most common, occurring in at least 5% of patients, were pyrexia, autoimmune hemolytic anemia, pneumonia, and febrile neutropenia. Thirteen had adverse events leading to dose reductions, most commonly due to neutropenia, thrombocytopenia, and febrile neutropenia.
Laboratory-confirmed tumor lysis syndrome was reported in five patients during the ramp-up period, including four who developed the syndrome within the first 2 days of treatment. All cases resolved without clinical sequelae. Treatment was continued without interruption in three patients with tumor lysis syndrome, who received only electrolyte management, and two patients had a 1-day treatment interruption. Both resumed dosing the next day.
In the phase Ib study by Seymour et al., common grade 1-2 toxicities included upper respiratory tract infections, diarrhea, and nausea occurring in 57%, 55%, and 53% of patients, respectively. Grade 3-4 adverse events occurred in 76% of 49 patients, and most often included neutropenia (12% of patients), thrombocytopenia (16%), anemia (14%), febrile neutropenia (12%), and leukopenia (12%). The most common serious adverse events were pyrexia (12%), febrile neutropenia (10%), lower respiratory tract infection (6%), and pneumonia (6%). Clinical tumor lysis syndrome occurred in two patients who initiated venetoclax at 50 mg, one of whom died as a result.
After enhancement of tumor lysis syndrome prophylaxis measures and reduction of the starting dose of venetoclax to 20 mg, no additional cases occurred, the authors reported.
Mitigating tumor lysis syndrome risk
General measures for mitigating the risk of tumor lysis syndrome include identification of patients at increased risk, initiation of prophylaxis with hydration and a uric acid reducing agent, and initiation of venetoclax at a 20 mg dose for 1 week, with gradual step-wise ramp-up over 5 weeks to the target dose, Dr. Zelenetz noted.
As reported by Stilgenbauer, et al., patients with a nodal mass less than 5 cm and absolute lymphocyte count (ALC) of 25,000 or less are considered at low risk for tumor lysis syndrome, those with a nodal mass of 5 cm to less than 10 cm or ALC greater than 25,000 are at medium risk, and those with a nodal mass of 10 cm or greater or nodal mass of 5 cm or greater and ALC of greater than 25,000 are considered to be at high risk.
High-risk patients in the study received inpatient venetoclax dosing and monitoring at 4, 8, 12, and 24 hours with 20 mg and 50 mg dosing, as well as outpatient intravenous hydration at 100 mg if there was no indication to hospitalize, and post-dose 8-24 hour laboratory monitoring at 100 mg and above.
Medium-risk patients received IV hydration at 20 and 50 mg dosing, inpatient care if creatinine clearance was less than 80 mL/min or if there was a high tumor burden, and postdose 8- and 24-hour laboratory monitoring after the initial dose and at dose escalations. Low-risk patients received outpatient dosing at all dose levels in the absence of an indication to hospitalize, and postdose 8- and 24-hour laboratory monitoring after the initial dose and at dose increases.
“Unfortunately, the dose-limiting toxicity of venetoclax is fatal tumor lysis,” Dr. Zelenetz said, adding that by increasing the dose slowly over time according to current treatment recommendations – from 20 mg, to 50, 100, 200, and 400 mg at weekly intervals, this complication can be avoided.
Dr. Zelenetz reported receiving consulting fees, honoraria, and/or grant/research support from Genentech, the maker of venetoclax (Venclexta), and a wide variety of other drug companies.
ORLANDO – In patients with relapsed or refractory chronic lymphocytic leukemia (CLL), the results with venetoclax continue to be encouraging, and recent findings from a multicenter phase Ib study hint that venetoclax may also provide durable responses – even with treatment discontinuation.
Venetoclax is an orally bioavailable selective BCL2 inhibitor that is typically given in an open-ended fashion. Toxicity – including tumor lysis syndrome – is always a concern, however, and the issue of whether open-ended administration is necessary is an important question, Andrew D. Zelenetz, MD, PhD, said at the annual conference of the National Comprehensive Cancer Network.
In one phase II multicenter study of venetoclax monotherapy in 107 patients with relapsed/refractory CLL with del(17p) at 31 centers in the United States, Canada, and Europe, the overall response rate was 79.4% based on an independent review committee assessment, (Lancet Oncol. 2016[17]:768-78).
Treatment included once-daily venetoclax beginning with a dose of 20 mg that was ramped up to 50, 100, 200, and 400 mg over 4-5 weeks, followed by daily 400 mg continuous dosing until disease progression or discontinuation for another reason.
Notably, 18 of 85 patients from the study who achieved an objective response were minimal residual disease (MRD)–negative in peripheral blood samples – an outcome that has not been seen with tyrosine kinase inhibitors, noted Dr. Zelenetz of Memorial Sloan Kettering Cancer Center, New York.
The durability of venetoclax’s activity in the study was 84.7% at 12 months in all responders; 100% in those who achieved complete response, complete response with incomplete recovery of blood counts, or nodular partial remission; and 94.4% in the MRD-negative patients.
The authors concluded that venetoclax monotherapy is active and well tolerated in patients with relapsed or refractory del(17p) chronic lymphocytic leukemia, and that given the distinct mechanism of action of this new therapeutic option for these very poor-prognosis patients, it deserves further investigation as part of a combination or as part of sequential treatment with other novel targeted agents.
The finding that patients on venetoclax can achieve MRD negativity also raised the question of whether treatment can be stopped, Dr. Zelenetz said.
“Because who wants to be on a drug forever? Nobody,” he added.
This question was explored in a study published in February by Seymour et al., which provided early evidence that stopping treatment may indeed be feasible in some patients (Lancet Oncol. 2017;18[2]:230-40).
Venetoclax in this study was given in a dose-escalating fashion to target doses of 200-600 mg daily, in 49 patients with relapsed or refractory “moderately heavily pretreated” CLL. Rituximab was added at a dose of 375 mg/m2 in month 1 and 500 mg/m2 in months 2-6.
Patients had the option of stopping treatment if they achieved a complete response.
The overall response rate was 86%, including a complete response in 51% of patients. Two-year estimates for progression-free survival and ongoing response were 82% and 89% respectively.
MRD negativity was attained in 80% of complete responders and 57% of patients overall. Thirteen responders discontinued all treatment, and at the time of publication, 11 MRD-negative responders who discontinued therapy remained progression free off therapy. Two MRD-positive patients who achieved complete response and discontinued therapy progressed after 2 years, but were able to recapture response once they restarted the drug.
“So it’s really quite interesting. We might have durable responses after discontinuation of this drug in an MRD-negative state,” Dr. Zelenetz said.
Of note, the latest update to the NCCN guidelines for the treatment of CLL/SLL (small lymphocytic lymphoma) included the addition of “+/– rituximab” as part of the “suggested treatment regimen” of venetoclax in the relapsed/refractory disease setting. This recommendation is category 2A, meaning it is based on lower level evidence with uniform NCCN consensus that the intervention is appropriate.
Venetoclax: adverse events of special interest
In these studies, venetoclax was considered well tolerated, but attention to adverse events and their prevention and management – particularly with respect to tumor lysis syndrome – is essential, Dr. Zelenetz said.
In the phase II study by Stilgenbauer et al., adverse events of special interest included grade 3/4 neutropenia, which occurred in 40% of patients. This was manageable with dose interruptions (five patients) or reductions (four patients), or with granulocyte–colony stimulating factor and antibiotics (six patients, including one who received only antibiotics). None of the patients permanently discontinued treatment.
Infections occurred in 72% of patients, and grade 3 or greater infections occurred in 20% of patients. The most common overall were upper respiratory infections (15%), nasopharyngitis (14%), and urinary tract infections (9%).
Serious infections occurring in two or more patients were pneumonia, lower respiratory tract infection, and upper respiratory tract infection. One patient died from septic shock, 10 had infections leading to venetoclax interruption, and 2 had infections leading to dose reduction.
No mandated infection prophylaxis was used in this study.
Serious adverse events occurred in 59 patients (55%). The most common, occurring in at least 5% of patients, were pyrexia, autoimmune hemolytic anemia, pneumonia, and febrile neutropenia. Thirteen had adverse events leading to dose reductions, most commonly due to neutropenia, thrombocytopenia, and febrile neutropenia.
Laboratory-confirmed tumor lysis syndrome was reported in five patients during the ramp-up period, including four who developed the syndrome within the first 2 days of treatment. All cases resolved without clinical sequelae. Treatment was continued without interruption in three patients with tumor lysis syndrome, who received only electrolyte management, and two patients had a 1-day treatment interruption. Both resumed dosing the next day.
In the phase Ib study by Seymour et al., common grade 1-2 toxicities included upper respiratory tract infections, diarrhea, and nausea occurring in 57%, 55%, and 53% of patients, respectively. Grade 3-4 adverse events occurred in 76% of 49 patients, and most often included neutropenia (12% of patients), thrombocytopenia (16%), anemia (14%), febrile neutropenia (12%), and leukopenia (12%). The most common serious adverse events were pyrexia (12%), febrile neutropenia (10%), lower respiratory tract infection (6%), and pneumonia (6%). Clinical tumor lysis syndrome occurred in two patients who initiated venetoclax at 50 mg, one of whom died as a result.
After enhancement of tumor lysis syndrome prophylaxis measures and reduction of the starting dose of venetoclax to 20 mg, no additional cases occurred, the authors reported.
Mitigating tumor lysis syndrome risk
General measures for mitigating the risk of tumor lysis syndrome include identification of patients at increased risk, initiation of prophylaxis with hydration and a uric acid reducing agent, and initiation of venetoclax at a 20 mg dose for 1 week, with gradual step-wise ramp-up over 5 weeks to the target dose, Dr. Zelenetz noted.
As reported by Stilgenbauer, et al., patients with a nodal mass less than 5 cm and absolute lymphocyte count (ALC) of 25,000 or less are considered at low risk for tumor lysis syndrome, those with a nodal mass of 5 cm to less than 10 cm or ALC greater than 25,000 are at medium risk, and those with a nodal mass of 10 cm or greater or nodal mass of 5 cm or greater and ALC of greater than 25,000 are considered to be at high risk.
High-risk patients in the study received inpatient venetoclax dosing and monitoring at 4, 8, 12, and 24 hours with 20 mg and 50 mg dosing, as well as outpatient intravenous hydration at 100 mg if there was no indication to hospitalize, and post-dose 8-24 hour laboratory monitoring at 100 mg and above.
Medium-risk patients received IV hydration at 20 and 50 mg dosing, inpatient care if creatinine clearance was less than 80 mL/min or if there was a high tumor burden, and postdose 8- and 24-hour laboratory monitoring after the initial dose and at dose escalations. Low-risk patients received outpatient dosing at all dose levels in the absence of an indication to hospitalize, and postdose 8- and 24-hour laboratory monitoring after the initial dose and at dose increases.
“Unfortunately, the dose-limiting toxicity of venetoclax is fatal tumor lysis,” Dr. Zelenetz said, adding that by increasing the dose slowly over time according to current treatment recommendations – from 20 mg, to 50, 100, 200, and 400 mg at weekly intervals, this complication can be avoided.
Dr. Zelenetz reported receiving consulting fees, honoraria, and/or grant/research support from Genentech, the maker of venetoclax (Venclexta), and a wide variety of other drug companies.
EXPERT ANALYSIS AT THE NCCN ANNUAL CONFERENCE
Advanced CLL treatment approach depends on comorbidity burden
ORLANDO – The choice of first-line therapy in symptomatic chronic lymphocytic leukemia patients depends largely on comorbidity burden, Andrew D. Zelenetz, MD, PhD, said at the annual conference of the National Comprehensive Cancer Network.
“This is a disease of elderly patients. Frequently they have comorbidities,” he said. Categorizing these patients as having a low or high comorbidity burden can be done with the Cumulative Index Rating Scale score, which involves scoring of all organ systems on a 0-5 scale representing “not affected” to “extremely disabled.”
“We use this to determine first-line therapy,” said Dr. Zelenetz of Memorial Sloan Kettering Cancer Center, New York. Dr. Zelenetz is chair of the NCCN Non-Hodgkin Lymphoma Guidelines panel.
Patients with a score of greater than 12 on the 0- to 56-point scale, are “no-go” patients with respect to therapy, and are typically treated only with palliative approaches. Those with a score of 7-12 (“slow-go” patients) have a significant comorbidity burden, but can undergo treatment, thought typically to be at reduced intensity. Those with a score of 0-6 are “go-go” patients with respect to treatment, as they are physically fit, have excellent renal function, and have no significant comorbidities, he said.
Treatment options for ‘go-go’ CLL patients
Among the treatment options for the latter is FCR–the combination of fludarabine, cyclophosphamide, and rituximab, which was shown in the phase III CLL10 trial of patients with advanced CLL to be associated with improved complete response rates compared with the popular regimen of bendamustine and rituximab (BR), both overall and in patients under age 65. In older patients, the advantage disappeared, Dr. Zelenetz said.
FCR was also associated with improved outcomes vs. BR in patients with del(11q).
The primary endpoint of the study was progression-free survival, which favored FCR (median of 55.2 vs. 41.7 months; hazard ratio, 1.643), he said, noting that no difference was seen between the two regimens in terms of overall survival.
In a recent publication, MD Anderson Cancer Center reported its experience with its first 300 CLL patients treated with FCR. With long-term follow-up of at least 9-10 years (median of 12.8 years), patients in this trial have done extremely well.
“But interestingly, when you stratify these patients by whether they have IGHV [immunoglobulin heavy chain variable] mutated or unmutated [disease], the IGHV mutated patients have something that looks a whole lot like a survival plateau, and that survival plateau is not trivial – it’s about 60%,” he said. “So there is a group of patients with CLL who are, in fact, curable with conventional chemoimmunotherapy.
“This is an appropriate treatment for a young, fit, ‘go-go’ patient, and it has a big implication,” he said. That is, patients who are young and fit require IGHV mutation testing, as “you will absolutely choose FCR chemotherapy for the fit, young patients who has IGHV mutated disease.
“In that setting IGHV testing is now mandatory,” he stressed, noting that the benefits in this population extend to overall survival as well as progression-free survival.
Dr. Zelenetz also emphasized the need for increasing the single dose of rituximab from 375 mg/m2 during cycle 1 to 500 mg/m2 during cycles 2-6 in those receiving FCR, as this is often forgotten.
The data demonstrating the efficacy of FCR were based on this approach, he said.
Fludarabine is to be given at a dose of 25 mg/m2, and cyclophosphamide at a dose of 250 mg/m2 – both for 2-4 days during cycle 1 and for 1-3 days during cycles 2-6.
Treatment options for ‘slow-go’ CLL patients
In “slow-go” patients, an interesting approach is to use new anti-CD20 antibodies such as ofatumumab and obinutuzumab, which have features that are distinct from rituximab.
Both have been studied in CLL. The CLL11 trial compared chlorambucil, rituximab+chlorambucil, and obinutuzumab+chlorambucil, and the latest analysis showed substantial improvement in progression-free survival with obinutuzumab+chlorambucil vs. the other two regimens (26.7 months vs. 11.1 and 16.3 months, respectively), Dr. Zelenetz said, noting that rituximab+chlorambucil was also superior to chlorambucil alone, but that only the obinutuzumab regimen had an overall survival advantage vs. chlorambucil alone.
An updated analysis to be reported soon will show emerging evidence of a survival advantage of obinutuzumab+chlorambucil vs. rituximab+chlorambucil, he said.
“This suggests that obinutuzumab is a far better antibody,” he added, noting that the reasons for that are under debate, “but the way it’s given, it works better in CLL, and that, I think is unequivocal.”
A similar study looking at chlorambucil with and without ofatumumab in “slow-go” patients also demonstrated an improvement in PFS with ofatumumab, but showed “no difference whatsoever in overall survival.”
“This is actually very similar to the rituximab result, and I actually call this the ‘death of ofatumumab’ study, because clearly obinutuzumab in CLL is, I think, a superior anti-CD20 antibody,” Dr. Zelenetz said.
Studies in which obinutuzumab is substituted for rituximab in the FCR combination are currently underway as are a number of other studies of obinutuzumab, he noted.
Another treatment option in the up-front setting is ibrutinib, which was shown to be effective in the RESONATE 2 trial .
“But notice, a very, very small [complete response rate]. CRs are very difficult to achieve with ibrutinib alone, so this drug is given continuously, lifelong,” Dr. Zelenetz said, noting that it was, however, associated with an overall survival advantage vs. chlorambucil.
“Should this be the standard of care? I think it is in patients who have del(17p) or mutation of TP53. Outside of that setting, I’m still concerned about the cost of long-term tolerability of the agent,” he said.
Future of first-line CLL treatment
Avoidance of long-term therapy and conventional chemotherapy in patients with CLL is a goal, he added, noting that new understanding from studies in patients in the relapsed/refractory CLL setting – such as recent findings from a phase Ib study of venetoclax plus rituximab, which demonstrated potentially durable responses after treatment discontinuation in minimal residual disease (MRD)–negative patients – are providing insights into achieving MRD negativity that could be applied in the front line treatment setting.
“We’re still trying to figure out how to best use this. We want to try to use some of this knowledge about achievement of MRD negativity in the up-front setting so we don’t have to give patients long-term therapy, and we would like to avoid conventional chemotherapy,” he said. “So I’m hoping we’re going to be able to replace chronic long-term therapy of CLL with a defined course of treatment with high levels of MRD negativity.”
Dr. Zelenetz reported receiving consulting fees, honoraria, and/or grant/research support from Acerta Pharma, Amgen Inc., BeiGene, Bristol-Myers Squibb, Celgene Corporation, Genentech, Gilead Sciences, Janssen Pharmaceutica Products, MEI Pharma, NanoString Technologies, Pharmacyclics, Portola Pharmaceuticals, Roche Laboratories, and Takeda Pharmaceuticals North America.
ORLANDO – The choice of first-line therapy in symptomatic chronic lymphocytic leukemia patients depends largely on comorbidity burden, Andrew D. Zelenetz, MD, PhD, said at the annual conference of the National Comprehensive Cancer Network.
“This is a disease of elderly patients. Frequently they have comorbidities,” he said. Categorizing these patients as having a low or high comorbidity burden can be done with the Cumulative Index Rating Scale score, which involves scoring of all organ systems on a 0-5 scale representing “not affected” to “extremely disabled.”
“We use this to determine first-line therapy,” said Dr. Zelenetz of Memorial Sloan Kettering Cancer Center, New York. Dr. Zelenetz is chair of the NCCN Non-Hodgkin Lymphoma Guidelines panel.
Patients with a score of greater than 12 on the 0- to 56-point scale, are “no-go” patients with respect to therapy, and are typically treated only with palliative approaches. Those with a score of 7-12 (“slow-go” patients) have a significant comorbidity burden, but can undergo treatment, thought typically to be at reduced intensity. Those with a score of 0-6 are “go-go” patients with respect to treatment, as they are physically fit, have excellent renal function, and have no significant comorbidities, he said.
Treatment options for ‘go-go’ CLL patients
Among the treatment options for the latter is FCR–the combination of fludarabine, cyclophosphamide, and rituximab, which was shown in the phase III CLL10 trial of patients with advanced CLL to be associated with improved complete response rates compared with the popular regimen of bendamustine and rituximab (BR), both overall and in patients under age 65. In older patients, the advantage disappeared, Dr. Zelenetz said.
FCR was also associated with improved outcomes vs. BR in patients with del(11q).
The primary endpoint of the study was progression-free survival, which favored FCR (median of 55.2 vs. 41.7 months; hazard ratio, 1.643), he said, noting that no difference was seen between the two regimens in terms of overall survival.
In a recent publication, MD Anderson Cancer Center reported its experience with its first 300 CLL patients treated with FCR. With long-term follow-up of at least 9-10 years (median of 12.8 years), patients in this trial have done extremely well.
“But interestingly, when you stratify these patients by whether they have IGHV [immunoglobulin heavy chain variable] mutated or unmutated [disease], the IGHV mutated patients have something that looks a whole lot like a survival plateau, and that survival plateau is not trivial – it’s about 60%,” he said. “So there is a group of patients with CLL who are, in fact, curable with conventional chemoimmunotherapy.
“This is an appropriate treatment for a young, fit, ‘go-go’ patient, and it has a big implication,” he said. That is, patients who are young and fit require IGHV mutation testing, as “you will absolutely choose FCR chemotherapy for the fit, young patients who has IGHV mutated disease.
“In that setting IGHV testing is now mandatory,” he stressed, noting that the benefits in this population extend to overall survival as well as progression-free survival.
Dr. Zelenetz also emphasized the need for increasing the single dose of rituximab from 375 mg/m2 during cycle 1 to 500 mg/m2 during cycles 2-6 in those receiving FCR, as this is often forgotten.
The data demonstrating the efficacy of FCR were based on this approach, he said.
Fludarabine is to be given at a dose of 25 mg/m2, and cyclophosphamide at a dose of 250 mg/m2 – both for 2-4 days during cycle 1 and for 1-3 days during cycles 2-6.
Treatment options for ‘slow-go’ CLL patients
In “slow-go” patients, an interesting approach is to use new anti-CD20 antibodies such as ofatumumab and obinutuzumab, which have features that are distinct from rituximab.
Both have been studied in CLL. The CLL11 trial compared chlorambucil, rituximab+chlorambucil, and obinutuzumab+chlorambucil, and the latest analysis showed substantial improvement in progression-free survival with obinutuzumab+chlorambucil vs. the other two regimens (26.7 months vs. 11.1 and 16.3 months, respectively), Dr. Zelenetz said, noting that rituximab+chlorambucil was also superior to chlorambucil alone, but that only the obinutuzumab regimen had an overall survival advantage vs. chlorambucil alone.
An updated analysis to be reported soon will show emerging evidence of a survival advantage of obinutuzumab+chlorambucil vs. rituximab+chlorambucil, he said.
“This suggests that obinutuzumab is a far better antibody,” he added, noting that the reasons for that are under debate, “but the way it’s given, it works better in CLL, and that, I think is unequivocal.”
A similar study looking at chlorambucil with and without ofatumumab in “slow-go” patients also demonstrated an improvement in PFS with ofatumumab, but showed “no difference whatsoever in overall survival.”
“This is actually very similar to the rituximab result, and I actually call this the ‘death of ofatumumab’ study, because clearly obinutuzumab in CLL is, I think, a superior anti-CD20 antibody,” Dr. Zelenetz said.
Studies in which obinutuzumab is substituted for rituximab in the FCR combination are currently underway as are a number of other studies of obinutuzumab, he noted.
Another treatment option in the up-front setting is ibrutinib, which was shown to be effective in the RESONATE 2 trial .
“But notice, a very, very small [complete response rate]. CRs are very difficult to achieve with ibrutinib alone, so this drug is given continuously, lifelong,” Dr. Zelenetz said, noting that it was, however, associated with an overall survival advantage vs. chlorambucil.
“Should this be the standard of care? I think it is in patients who have del(17p) or mutation of TP53. Outside of that setting, I’m still concerned about the cost of long-term tolerability of the agent,” he said.
Future of first-line CLL treatment
Avoidance of long-term therapy and conventional chemotherapy in patients with CLL is a goal, he added, noting that new understanding from studies in patients in the relapsed/refractory CLL setting – such as recent findings from a phase Ib study of venetoclax plus rituximab, which demonstrated potentially durable responses after treatment discontinuation in minimal residual disease (MRD)–negative patients – are providing insights into achieving MRD negativity that could be applied in the front line treatment setting.
“We’re still trying to figure out how to best use this. We want to try to use some of this knowledge about achievement of MRD negativity in the up-front setting so we don’t have to give patients long-term therapy, and we would like to avoid conventional chemotherapy,” he said. “So I’m hoping we’re going to be able to replace chronic long-term therapy of CLL with a defined course of treatment with high levels of MRD negativity.”
Dr. Zelenetz reported receiving consulting fees, honoraria, and/or grant/research support from Acerta Pharma, Amgen Inc., BeiGene, Bristol-Myers Squibb, Celgene Corporation, Genentech, Gilead Sciences, Janssen Pharmaceutica Products, MEI Pharma, NanoString Technologies, Pharmacyclics, Portola Pharmaceuticals, Roche Laboratories, and Takeda Pharmaceuticals North America.
ORLANDO – The choice of first-line therapy in symptomatic chronic lymphocytic leukemia patients depends largely on comorbidity burden, Andrew D. Zelenetz, MD, PhD, said at the annual conference of the National Comprehensive Cancer Network.
“This is a disease of elderly patients. Frequently they have comorbidities,” he said. Categorizing these patients as having a low or high comorbidity burden can be done with the Cumulative Index Rating Scale score, which involves scoring of all organ systems on a 0-5 scale representing “not affected” to “extremely disabled.”
“We use this to determine first-line therapy,” said Dr. Zelenetz of Memorial Sloan Kettering Cancer Center, New York. Dr. Zelenetz is chair of the NCCN Non-Hodgkin Lymphoma Guidelines panel.
Patients with a score of greater than 12 on the 0- to 56-point scale, are “no-go” patients with respect to therapy, and are typically treated only with palliative approaches. Those with a score of 7-12 (“slow-go” patients) have a significant comorbidity burden, but can undergo treatment, thought typically to be at reduced intensity. Those with a score of 0-6 are “go-go” patients with respect to treatment, as they are physically fit, have excellent renal function, and have no significant comorbidities, he said.
Treatment options for ‘go-go’ CLL patients
Among the treatment options for the latter is FCR–the combination of fludarabine, cyclophosphamide, and rituximab, which was shown in the phase III CLL10 trial of patients with advanced CLL to be associated with improved complete response rates compared with the popular regimen of bendamustine and rituximab (BR), both overall and in patients under age 65. In older patients, the advantage disappeared, Dr. Zelenetz said.
FCR was also associated with improved outcomes vs. BR in patients with del(11q).
The primary endpoint of the study was progression-free survival, which favored FCR (median of 55.2 vs. 41.7 months; hazard ratio, 1.643), he said, noting that no difference was seen between the two regimens in terms of overall survival.
In a recent publication, MD Anderson Cancer Center reported its experience with its first 300 CLL patients treated with FCR. With long-term follow-up of at least 9-10 years (median of 12.8 years), patients in this trial have done extremely well.
“But interestingly, when you stratify these patients by whether they have IGHV [immunoglobulin heavy chain variable] mutated or unmutated [disease], the IGHV mutated patients have something that looks a whole lot like a survival plateau, and that survival plateau is not trivial – it’s about 60%,” he said. “So there is a group of patients with CLL who are, in fact, curable with conventional chemoimmunotherapy.
“This is an appropriate treatment for a young, fit, ‘go-go’ patient, and it has a big implication,” he said. That is, patients who are young and fit require IGHV mutation testing, as “you will absolutely choose FCR chemotherapy for the fit, young patients who has IGHV mutated disease.
“In that setting IGHV testing is now mandatory,” he stressed, noting that the benefits in this population extend to overall survival as well as progression-free survival.
Dr. Zelenetz also emphasized the need for increasing the single dose of rituximab from 375 mg/m2 during cycle 1 to 500 mg/m2 during cycles 2-6 in those receiving FCR, as this is often forgotten.
The data demonstrating the efficacy of FCR were based on this approach, he said.
Fludarabine is to be given at a dose of 25 mg/m2, and cyclophosphamide at a dose of 250 mg/m2 – both for 2-4 days during cycle 1 and for 1-3 days during cycles 2-6.
Treatment options for ‘slow-go’ CLL patients
In “slow-go” patients, an interesting approach is to use new anti-CD20 antibodies such as ofatumumab and obinutuzumab, which have features that are distinct from rituximab.
Both have been studied in CLL. The CLL11 trial compared chlorambucil, rituximab+chlorambucil, and obinutuzumab+chlorambucil, and the latest analysis showed substantial improvement in progression-free survival with obinutuzumab+chlorambucil vs. the other two regimens (26.7 months vs. 11.1 and 16.3 months, respectively), Dr. Zelenetz said, noting that rituximab+chlorambucil was also superior to chlorambucil alone, but that only the obinutuzumab regimen had an overall survival advantage vs. chlorambucil alone.
An updated analysis to be reported soon will show emerging evidence of a survival advantage of obinutuzumab+chlorambucil vs. rituximab+chlorambucil, he said.
“This suggests that obinutuzumab is a far better antibody,” he added, noting that the reasons for that are under debate, “but the way it’s given, it works better in CLL, and that, I think is unequivocal.”
A similar study looking at chlorambucil with and without ofatumumab in “slow-go” patients also demonstrated an improvement in PFS with ofatumumab, but showed “no difference whatsoever in overall survival.”
“This is actually very similar to the rituximab result, and I actually call this the ‘death of ofatumumab’ study, because clearly obinutuzumab in CLL is, I think, a superior anti-CD20 antibody,” Dr. Zelenetz said.
Studies in which obinutuzumab is substituted for rituximab in the FCR combination are currently underway as are a number of other studies of obinutuzumab, he noted.
Another treatment option in the up-front setting is ibrutinib, which was shown to be effective in the RESONATE 2 trial .
“But notice, a very, very small [complete response rate]. CRs are very difficult to achieve with ibrutinib alone, so this drug is given continuously, lifelong,” Dr. Zelenetz said, noting that it was, however, associated with an overall survival advantage vs. chlorambucil.
“Should this be the standard of care? I think it is in patients who have del(17p) or mutation of TP53. Outside of that setting, I’m still concerned about the cost of long-term tolerability of the agent,” he said.
Future of first-line CLL treatment
Avoidance of long-term therapy and conventional chemotherapy in patients with CLL is a goal, he added, noting that new understanding from studies in patients in the relapsed/refractory CLL setting – such as recent findings from a phase Ib study of venetoclax plus rituximab, which demonstrated potentially durable responses after treatment discontinuation in minimal residual disease (MRD)–negative patients – are providing insights into achieving MRD negativity that could be applied in the front line treatment setting.
“We’re still trying to figure out how to best use this. We want to try to use some of this knowledge about achievement of MRD negativity in the up-front setting so we don’t have to give patients long-term therapy, and we would like to avoid conventional chemotherapy,” he said. “So I’m hoping we’re going to be able to replace chronic long-term therapy of CLL with a defined course of treatment with high levels of MRD negativity.”
Dr. Zelenetz reported receiving consulting fees, honoraria, and/or grant/research support from Acerta Pharma, Amgen Inc., BeiGene, Bristol-Myers Squibb, Celgene Corporation, Genentech, Gilead Sciences, Janssen Pharmaceutica Products, MEI Pharma, NanoString Technologies, Pharmacyclics, Portola Pharmaceuticals, Roche Laboratories, and Takeda Pharmaceuticals North America.
EXPERT ANALYSIS FROM THE NCCN ANNUAL CONFERENCE
NCCN: Myelofibrosis guideline is first in series on MPNs
ORLANDO – A guideline published late last year for the diagnostic work-up of myeloproliferative neoplasms and for the management of myelofibrosis in particular is just the first in a series of National Comprehensive Cancer Network guidelines on this “family of myeloid neoplasms,” according to the guideline panel chair, Ruben A. Mesa, MD.
The myeloproliferative neoplasm (MPN) guideline panel first worked to develop a framework based on existing understanding of the MPNs. Members consulted with two other panels working in the area of chronic myeloid diseases, including chronic myeloid leukemia and myelodysplastic syndrome.
“We were in agreement that these are different entities, and our treatments are different, our guidelines are different,” Dr. Mesa of the Mayo Clinic Cancer Center, Phoenix, said at the annual conference of the National Comprehensive Cancer Network.
That said, there are also some shared circumstances. For example, all three sets of diseases can progress to acute myeloid leukemia.
“Indeed, I view this very much as pieces in a jigsaw puzzle. … It is important that we recognize their interdependencies as well as those aspects that are disease specific,” he said.
In essence, however, the MPN guideline development is a from-scratch effort, as these are the first guidelines for these disorders, he noted.
The effort is timely, as the diagnosis and management of patients with MPNs have rapidly evolved since the identification of mutations that activate the JAK pathway, including JAK2, CALR, and MPL mutations. Further, the development of targeted therapies – such as the JAK1 and JAK2 inhibitor ruxolitinib, which was the first drug approved for the treatment of myelofibrosis – has resulted in significant improvements in disease-related symptoms and quality of life.
The panel is focusing first on the “core classic” Philadelphia chromosome–negative MPNs: myelofibrosis, polycythemia vera, and essential thrombocythemia. The first piece to be placed in the MPN puzzle was the guideline for the diagnostic work-up of these entities and for risk stratification, treatment, and supportive care strategies for the management of myelofibrosis, which the panel considered “the greatest unmet need and the most urgent in terms of guidance,” Dr. Mesa said.
This initial MPN guideline was published in December (J Natl Compr Canc Netw. 2016;14:1572-611) and, because of the evolving understanding of MPNs, updates are already under consideration as additional MPN guidelines are being developed.
“We have been actively working … to develop the next set of treatment guidelines, which are the treatment guidelines for polycythemia vera and essential thrombocythemia. Finally, we will work to include the atypical MPNs,” he said, noting that the latter include hypereosinophilic disease, systemic mast cell disease, and other atypical illnesses.
These represent a small number of patients, but “their management is key, it’s distinct from the others, and there is no good guidance,” Dr. Mesa said.
“Once this is fleshed out, we will then have a fully developed set of guidelines that then will be maintained along the traditional process that NCCN follows, which is first an annual review, but second, a monitoring in real time of key developments that could impact the guidelines during the off-cycle,” he said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
ORLANDO – A guideline published late last year for the diagnostic work-up of myeloproliferative neoplasms and for the management of myelofibrosis in particular is just the first in a series of National Comprehensive Cancer Network guidelines on this “family of myeloid neoplasms,” according to the guideline panel chair, Ruben A. Mesa, MD.
The myeloproliferative neoplasm (MPN) guideline panel first worked to develop a framework based on existing understanding of the MPNs. Members consulted with two other panels working in the area of chronic myeloid diseases, including chronic myeloid leukemia and myelodysplastic syndrome.
“We were in agreement that these are different entities, and our treatments are different, our guidelines are different,” Dr. Mesa of the Mayo Clinic Cancer Center, Phoenix, said at the annual conference of the National Comprehensive Cancer Network.
That said, there are also some shared circumstances. For example, all three sets of diseases can progress to acute myeloid leukemia.
“Indeed, I view this very much as pieces in a jigsaw puzzle. … It is important that we recognize their interdependencies as well as those aspects that are disease specific,” he said.
In essence, however, the MPN guideline development is a from-scratch effort, as these are the first guidelines for these disorders, he noted.
The effort is timely, as the diagnosis and management of patients with MPNs have rapidly evolved since the identification of mutations that activate the JAK pathway, including JAK2, CALR, and MPL mutations. Further, the development of targeted therapies – such as the JAK1 and JAK2 inhibitor ruxolitinib, which was the first drug approved for the treatment of myelofibrosis – has resulted in significant improvements in disease-related symptoms and quality of life.
The panel is focusing first on the “core classic” Philadelphia chromosome–negative MPNs: myelofibrosis, polycythemia vera, and essential thrombocythemia. The first piece to be placed in the MPN puzzle was the guideline for the diagnostic work-up of these entities and for risk stratification, treatment, and supportive care strategies for the management of myelofibrosis, which the panel considered “the greatest unmet need and the most urgent in terms of guidance,” Dr. Mesa said.
This initial MPN guideline was published in December (J Natl Compr Canc Netw. 2016;14:1572-611) and, because of the evolving understanding of MPNs, updates are already under consideration as additional MPN guidelines are being developed.
“We have been actively working … to develop the next set of treatment guidelines, which are the treatment guidelines for polycythemia vera and essential thrombocythemia. Finally, we will work to include the atypical MPNs,” he said, noting that the latter include hypereosinophilic disease, systemic mast cell disease, and other atypical illnesses.
These represent a small number of patients, but “their management is key, it’s distinct from the others, and there is no good guidance,” Dr. Mesa said.
“Once this is fleshed out, we will then have a fully developed set of guidelines that then will be maintained along the traditional process that NCCN follows, which is first an annual review, but second, a monitoring in real time of key developments that could impact the guidelines during the off-cycle,” he said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
ORLANDO – A guideline published late last year for the diagnostic work-up of myeloproliferative neoplasms and for the management of myelofibrosis in particular is just the first in a series of National Comprehensive Cancer Network guidelines on this “family of myeloid neoplasms,” according to the guideline panel chair, Ruben A. Mesa, MD.
The myeloproliferative neoplasm (MPN) guideline panel first worked to develop a framework based on existing understanding of the MPNs. Members consulted with two other panels working in the area of chronic myeloid diseases, including chronic myeloid leukemia and myelodysplastic syndrome.
“We were in agreement that these are different entities, and our treatments are different, our guidelines are different,” Dr. Mesa of the Mayo Clinic Cancer Center, Phoenix, said at the annual conference of the National Comprehensive Cancer Network.
That said, there are also some shared circumstances. For example, all three sets of diseases can progress to acute myeloid leukemia.
“Indeed, I view this very much as pieces in a jigsaw puzzle. … It is important that we recognize their interdependencies as well as those aspects that are disease specific,” he said.
In essence, however, the MPN guideline development is a from-scratch effort, as these are the first guidelines for these disorders, he noted.
The effort is timely, as the diagnosis and management of patients with MPNs have rapidly evolved since the identification of mutations that activate the JAK pathway, including JAK2, CALR, and MPL mutations. Further, the development of targeted therapies – such as the JAK1 and JAK2 inhibitor ruxolitinib, which was the first drug approved for the treatment of myelofibrosis – has resulted in significant improvements in disease-related symptoms and quality of life.
The panel is focusing first on the “core classic” Philadelphia chromosome–negative MPNs: myelofibrosis, polycythemia vera, and essential thrombocythemia. The first piece to be placed in the MPN puzzle was the guideline for the diagnostic work-up of these entities and for risk stratification, treatment, and supportive care strategies for the management of myelofibrosis, which the panel considered “the greatest unmet need and the most urgent in terms of guidance,” Dr. Mesa said.
This initial MPN guideline was published in December (J Natl Compr Canc Netw. 2016;14:1572-611) and, because of the evolving understanding of MPNs, updates are already under consideration as additional MPN guidelines are being developed.
“We have been actively working … to develop the next set of treatment guidelines, which are the treatment guidelines for polycythemia vera and essential thrombocythemia. Finally, we will work to include the atypical MPNs,” he said, noting that the latter include hypereosinophilic disease, systemic mast cell disease, and other atypical illnesses.
These represent a small number of patients, but “their management is key, it’s distinct from the others, and there is no good guidance,” Dr. Mesa said.
“Once this is fleshed out, we will then have a fully developed set of guidelines that then will be maintained along the traditional process that NCCN follows, which is first an annual review, but second, a monitoring in real time of key developments that could impact the guidelines during the off-cycle,” he said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
AT THE NCCN ANNUAL CONFERENCE