User login
‘Achilles heels’ open doors to myeloma advances
NEW YORK – Three “Achilles heels” of multiple myeloma offer exciting promise for additional advances that will begin to see therapeutic payoffs within the next year, according to Kenneth C. Anderson, MD.
The three targets – excess protein production, immune suppression, and genomic abnormalities – can be addressed by focusing on protein degradation, restoring anti–multiple myeloma immunity, and targeting and overcoming genomic abnormalities, respectively, Dr. Anderson of Dana-Farber Cancer Institute in Boston said at Imedex: Lymphoma & Myeloma, an international congress on hematologic malignancies.
“So if you block those so-called DUBs, you block this same pathway upstream of the proteasome,” he said.
One DUB inhibitor (P5091) was shown in a preclinical trial to overcome bortezomib resistance in multiple myeloma, as was another novel, more user-friendly agent (b-AP15) that blocks USP14/UCHL5 and can be active with immunomodulatory drugs. A clinical trial of b-AP15 is ongoing, Dr. Anderson said.
In contrast to the conventional approach of inhibiting proteins and signaling pathways needed for the survival of the cancer cells, a new technology called “degronimids” turns on the cereblon gene and delivers protein-degrading machinery to targeted proteins. Cereblon, a protein-degrading enzyme that forms part of the ubiquitin E3 ligase complex, tags proteins in the cell for destruction, he noted.
As for immune suppression, he said, the selective plasma cell antigen BCMA (B-cell maturation antigen) is “probably a better target than either CD38 or SLAMF7,” and has already been targeted with an auristatin immunotoxin that induced strong anti–multiple myeloma effects.
“Excitingly, there is this concept of BCMA-BiTEs (B-cell maturation antigen–bispecific T-cell engagers) where we have one linkage of BCMA to the myeloma cell and CD3 attracting a local immune response,” he said.
Other promising new approaches with respect to immune suppression involve checkpoint inhibitors, histone deacetylase (HDAC) inhibitors, and chimeric antigen receptor (CAR) T-cells, he added.
Genomic abnormalities represent another potential vulnerability, and venetoclax (Venclexta) could prove to be the first precision medicine for multiple myeloma, he suggested.
In myeloma, “we are trying to treat the abnormality, but what about treating the genetic consequences of this abnormality,” he said, adding that clinical trials that target the consequences of genomic heterogeneity or instability are on the horizon.
Dr. Anderson reported serving as a consultant for, or receiving other financial support from Acetylon, Bristol-Myers Squibb, C4 Therapeutics, Celgene, Gilead, Millennium, and OncoPep.
NEW YORK – Three “Achilles heels” of multiple myeloma offer exciting promise for additional advances that will begin to see therapeutic payoffs within the next year, according to Kenneth C. Anderson, MD.
The three targets – excess protein production, immune suppression, and genomic abnormalities – can be addressed by focusing on protein degradation, restoring anti–multiple myeloma immunity, and targeting and overcoming genomic abnormalities, respectively, Dr. Anderson of Dana-Farber Cancer Institute in Boston said at Imedex: Lymphoma & Myeloma, an international congress on hematologic malignancies.
“So if you block those so-called DUBs, you block this same pathway upstream of the proteasome,” he said.
One DUB inhibitor (P5091) was shown in a preclinical trial to overcome bortezomib resistance in multiple myeloma, as was another novel, more user-friendly agent (b-AP15) that blocks USP14/UCHL5 and can be active with immunomodulatory drugs. A clinical trial of b-AP15 is ongoing, Dr. Anderson said.
In contrast to the conventional approach of inhibiting proteins and signaling pathways needed for the survival of the cancer cells, a new technology called “degronimids” turns on the cereblon gene and delivers protein-degrading machinery to targeted proteins. Cereblon, a protein-degrading enzyme that forms part of the ubiquitin E3 ligase complex, tags proteins in the cell for destruction, he noted.
As for immune suppression, he said, the selective plasma cell antigen BCMA (B-cell maturation antigen) is “probably a better target than either CD38 or SLAMF7,” and has already been targeted with an auristatin immunotoxin that induced strong anti–multiple myeloma effects.
“Excitingly, there is this concept of BCMA-BiTEs (B-cell maturation antigen–bispecific T-cell engagers) where we have one linkage of BCMA to the myeloma cell and CD3 attracting a local immune response,” he said.
Other promising new approaches with respect to immune suppression involve checkpoint inhibitors, histone deacetylase (HDAC) inhibitors, and chimeric antigen receptor (CAR) T-cells, he added.
Genomic abnormalities represent another potential vulnerability, and venetoclax (Venclexta) could prove to be the first precision medicine for multiple myeloma, he suggested.
In myeloma, “we are trying to treat the abnormality, but what about treating the genetic consequences of this abnormality,” he said, adding that clinical trials that target the consequences of genomic heterogeneity or instability are on the horizon.
Dr. Anderson reported serving as a consultant for, or receiving other financial support from Acetylon, Bristol-Myers Squibb, C4 Therapeutics, Celgene, Gilead, Millennium, and OncoPep.
NEW YORK – Three “Achilles heels” of multiple myeloma offer exciting promise for additional advances that will begin to see therapeutic payoffs within the next year, according to Kenneth C. Anderson, MD.
The three targets – excess protein production, immune suppression, and genomic abnormalities – can be addressed by focusing on protein degradation, restoring anti–multiple myeloma immunity, and targeting and overcoming genomic abnormalities, respectively, Dr. Anderson of Dana-Farber Cancer Institute in Boston said at Imedex: Lymphoma & Myeloma, an international congress on hematologic malignancies.
“So if you block those so-called DUBs, you block this same pathway upstream of the proteasome,” he said.
One DUB inhibitor (P5091) was shown in a preclinical trial to overcome bortezomib resistance in multiple myeloma, as was another novel, more user-friendly agent (b-AP15) that blocks USP14/UCHL5 and can be active with immunomodulatory drugs. A clinical trial of b-AP15 is ongoing, Dr. Anderson said.
In contrast to the conventional approach of inhibiting proteins and signaling pathways needed for the survival of the cancer cells, a new technology called “degronimids” turns on the cereblon gene and delivers protein-degrading machinery to targeted proteins. Cereblon, a protein-degrading enzyme that forms part of the ubiquitin E3 ligase complex, tags proteins in the cell for destruction, he noted.
As for immune suppression, he said, the selective plasma cell antigen BCMA (B-cell maturation antigen) is “probably a better target than either CD38 or SLAMF7,” and has already been targeted with an auristatin immunotoxin that induced strong anti–multiple myeloma effects.
“Excitingly, there is this concept of BCMA-BiTEs (B-cell maturation antigen–bispecific T-cell engagers) where we have one linkage of BCMA to the myeloma cell and CD3 attracting a local immune response,” he said.
Other promising new approaches with respect to immune suppression involve checkpoint inhibitors, histone deacetylase (HDAC) inhibitors, and chimeric antigen receptor (CAR) T-cells, he added.
Genomic abnormalities represent another potential vulnerability, and venetoclax (Venclexta) could prove to be the first precision medicine for multiple myeloma, he suggested.
In myeloma, “we are trying to treat the abnormality, but what about treating the genetic consequences of this abnormality,” he said, adding that clinical trials that target the consequences of genomic heterogeneity or instability are on the horizon.
Dr. Anderson reported serving as a consultant for, or receiving other financial support from Acetylon, Bristol-Myers Squibb, C4 Therapeutics, Celgene, Gilead, Millennium, and OncoPep.
EXPERT ANALYSIS FROM IMEDEX: LYMPHOMA & MYELOMA
Doc provides perspective on CAR T-cell therapy in CLL

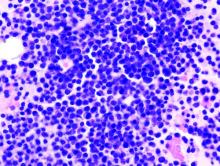
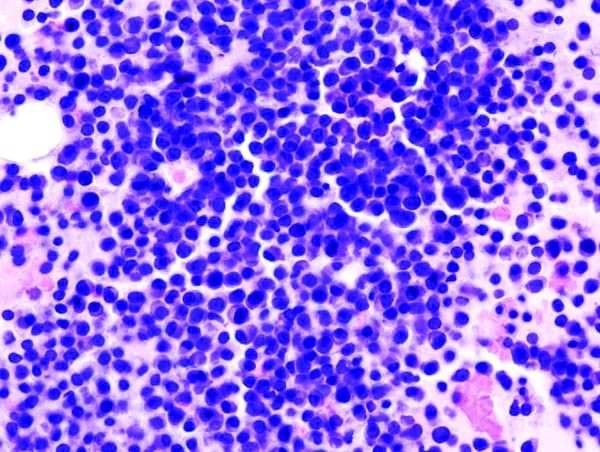
Photo from Penn Medicine
NEW YORK—Trial data on the use of chimeric antigen receptor (CAR) T cells in chronic lymphocytic leukemia (CLL) are maturing, and a speaker at Lymphoma & Myeloma 2016 provided some perspective on the therapy as it now stands.
Stephen J. Schuster, MD, of the University of Pennsylvania in Philadelphia, noted that some CLL patients treated with CAR T cells remain in complete remission (CR) for more than 5 years.
Therefore, CAR T cells may be a consideration for patients who are resistant to chemotherapy.
“[I]mportantly, this immunologic approach, like other immunologic approaches . . ., tends to be non-cross-resistant to chemotherapy,” Dr Schuster said.
He made these and other observations while discussing trials of CAR T-cell therapy (particularly CTL019) in CLL.
Pilot study of CTL019 in CLL
CTL019, which is the CAR T-cell therapy used by investigators at the University of Pennsylvania, is licensed to Novartis.
The pilot study of CTL019, begun in 2009, enrolled 14 patients who had failed at least 2 prior therapies and progressed within 2 years of their last treatment.
Four patients (29%) achieved a CR, and 4 (29%) achieved a partial response (PR), for an overall response rate of 57%. Detailed results from this trial were reported earlier in HematologyTimes.
Two patients in this trial are still in CR beyond 5 years.
When investigators analyzed the different variables that might affect response—including age, number of prior therapies, p53 status, CAR T-cell dose, and the presence of cytokine release syndrome (CRS)—2 things became apparent.
First, patients who responded tended to have greater in vivo expansion of the CAR T cells than non-responders. And second, the responders had a greater incidence of CRS than non-responders.
Additionally, complete responders were negative for minimal residual disease (MRD) and had durable responses.
“This actually is different from the data you see in lymphoma with CAR cells,” Dr Schuster said. “[However,] it’s what we see in ALL [acute lymphoblastic leukemia] as well.”
Investigators also discovered that persistence of CAR T cells correlates with B-cell aplasia. In this trial, persistence of CAR T cells and B-cell aplasia were apparent at 12 and 18 months, and, in some cases, even longer.
“This is in distinction to what we are observing in trials with the lymphomas,” Dr Schuster said. “So what’s going to emerge is that the different diseases will have different response rates, different degrees of persistence of CAR cells and different toxicities.”
“When we compare B-cell ALL, B-cell non-Hodgkin lymphomas, you’ll get different responses across the subtypes of lymphomas, some unique toxicities, and differences in CLL. So these are all different diseases.”
Dose-finding trial of CTL019 in CLL
The second trial of CTL019 in relapsed/refractory CLL patients was a dose-finding study. Updated results from this study were presented at ASCO 2016.
The high-dose arm (5x108 CTL019) had a 10 times higher dose of CAR T cells than the low-dose arm (5x107 CTL019).
Investigators treated 12 patients in each arm in the first phase of the study, and then expanded the trial to include another 8 patients at the recommended dose. The phase 2 trial was powered for response rates but not duration of response.
Twenty-eight patients were enrolled, with 24 evaluable, 11 in the high-dose arm and 13 in the low-dose arm.
Their median age was 62 (range, 51-75), the median number of prior therapies was 4 (range, 2–7), 38% had p53 deletion, and 12% had received prior ibrutinib therapy.
With the 2 arms pooled together, 25% of patients achieved a CR, and 17% achieved a PR, for an overall response rate of 42%.
“Toxicities were identical in each group,” Dr Schuster said.
He noted that the CRS rate was “fairly high.” The incidence was 55% in the high-dose arm and 54% in the low-dose arm.
There was a tendency, although not statistically significant, for the higher-dose patients to have a greater response rate than the lower-dose group—54% and 31%, respectively.
So the investigators decided the expansion cohort should be conducted with the higher dose, “even though we weren’t sure there really was a difference,” Dr Schuster said.
Seventeen evaluable patients received the higher dose in the expansion cohort. Six (35%) achieved a CR, and 3 (18%) achieved a PR, for an overall response rate of 53%.
“Most [adverse] events happen in the first 3 months,” after infusion, Dr Schuster said. “And then nothing much happens. That’s because the patients that are responsive to this therapy have durable responses.”
Of all the patients who achieved a CR, only 2 have relapsed, he said, “and now many of these patients have passed the 5-year mark for complete remissions.”
Toxicity of CTL019 in CLL
“When you give the cells, there’s not much toxicity,” Dr Schuster said. “These are the patients’ own cells; they’re not reacting adversely to that. It’s what happens afterwards that you have to be on the lookout for as the cells begin to expand in vivo.”
Patients experience some reversible renal toxicity, mostly hypertension-related, and some tumor lysis syndrome (TLS). No deaths occurred from TLS in CLL.
B-cell aplasia and hypogammaglobulinema occur in responding patients. They receive gamma globulin replacement as supportive therapy and generally experience no excessive or unusual infections.
“Cytokine release syndrome is the real thing to look at,” Dr Schuster said, “and that’s where early recognition and management will be life-saving.”
In both CLL and ALL, almost all responding patients develop CRS, which can be rapidly reversed with tocilizumab, the IL-6 receptor blocker.
Other CAR T-cell trials in CLL
Institutions other than the University of Pennsylvania have conducted trials of CAR T-cell therapies other than CTL019, and response rates in CLL patients have ranged from 25% (MSKCC) to 46% (Seattle), as reported at ASCO this year.
“But what’s really important to keep in mind is almost all patients who achieve complete response to date have stayed in complete response,” Dr Schuster said.
Combination trials with ibrutinib
Dr Schuster noted that patients in CAR T-cell trials who had been on ibrutinib for more than 5 months “had really robust T-cell expansion.”
So investigators believe treatment with ibrutinib may be a way of enhancing T-cell function.
A combination trial of ibrutinib and CTL019 is underway (NCT02640209). Six patients have been treated thus far, and although the follow-up is short, all 6 achieved CR at the 3-month assessment.
“So the hope is that this is going to be a partner [therapy],” Dr Schuster said. “And maybe these complete responses will be very durable, like the responses in earlier trials of CAR therapy in patients with CLL.” ![]()

Photo from Penn Medicine
NEW YORK—Trial data on the use of chimeric antigen receptor (CAR) T cells in chronic lymphocytic leukemia (CLL) are maturing, and a speaker at Lymphoma & Myeloma 2016 provided some perspective on the therapy as it now stands.
Stephen J. Schuster, MD, of the University of Pennsylvania in Philadelphia, noted that some CLL patients treated with CAR T cells remain in complete remission (CR) for more than 5 years.
Therefore, CAR T cells may be a consideration for patients who are resistant to chemotherapy.
“[I]mportantly, this immunologic approach, like other immunologic approaches . . ., tends to be non-cross-resistant to chemotherapy,” Dr Schuster said.
He made these and other observations while discussing trials of CAR T-cell therapy (particularly CTL019) in CLL.
Pilot study of CTL019 in CLL
CTL019, which is the CAR T-cell therapy used by investigators at the University of Pennsylvania, is licensed to Novartis.
The pilot study of CTL019, begun in 2009, enrolled 14 patients who had failed at least 2 prior therapies and progressed within 2 years of their last treatment.
Four patients (29%) achieved a CR, and 4 (29%) achieved a partial response (PR), for an overall response rate of 57%. Detailed results from this trial were reported earlier in HematologyTimes.
Two patients in this trial are still in CR beyond 5 years.
When investigators analyzed the different variables that might affect response—including age, number of prior therapies, p53 status, CAR T-cell dose, and the presence of cytokine release syndrome (CRS)—2 things became apparent.
First, patients who responded tended to have greater in vivo expansion of the CAR T cells than non-responders. And second, the responders had a greater incidence of CRS than non-responders.
Additionally, complete responders were negative for minimal residual disease (MRD) and had durable responses.
“This actually is different from the data you see in lymphoma with CAR cells,” Dr Schuster said. “[However,] it’s what we see in ALL [acute lymphoblastic leukemia] as well.”
Investigators also discovered that persistence of CAR T cells correlates with B-cell aplasia. In this trial, persistence of CAR T cells and B-cell aplasia were apparent at 12 and 18 months, and, in some cases, even longer.
“This is in distinction to what we are observing in trials with the lymphomas,” Dr Schuster said. “So what’s going to emerge is that the different diseases will have different response rates, different degrees of persistence of CAR cells and different toxicities.”
“When we compare B-cell ALL, B-cell non-Hodgkin lymphomas, you’ll get different responses across the subtypes of lymphomas, some unique toxicities, and differences in CLL. So these are all different diseases.”
Dose-finding trial of CTL019 in CLL
The second trial of CTL019 in relapsed/refractory CLL patients was a dose-finding study. Updated results from this study were presented at ASCO 2016.
The high-dose arm (5x108 CTL019) had a 10 times higher dose of CAR T cells than the low-dose arm (5x107 CTL019).
Investigators treated 12 patients in each arm in the first phase of the study, and then expanded the trial to include another 8 patients at the recommended dose. The phase 2 trial was powered for response rates but not duration of response.
Twenty-eight patients were enrolled, with 24 evaluable, 11 in the high-dose arm and 13 in the low-dose arm.
Their median age was 62 (range, 51-75), the median number of prior therapies was 4 (range, 2–7), 38% had p53 deletion, and 12% had received prior ibrutinib therapy.
With the 2 arms pooled together, 25% of patients achieved a CR, and 17% achieved a PR, for an overall response rate of 42%.
“Toxicities were identical in each group,” Dr Schuster said.
He noted that the CRS rate was “fairly high.” The incidence was 55% in the high-dose arm and 54% in the low-dose arm.
There was a tendency, although not statistically significant, for the higher-dose patients to have a greater response rate than the lower-dose group—54% and 31%, respectively.
So the investigators decided the expansion cohort should be conducted with the higher dose, “even though we weren’t sure there really was a difference,” Dr Schuster said.
Seventeen evaluable patients received the higher dose in the expansion cohort. Six (35%) achieved a CR, and 3 (18%) achieved a PR, for an overall response rate of 53%.
“Most [adverse] events happen in the first 3 months,” after infusion, Dr Schuster said. “And then nothing much happens. That’s because the patients that are responsive to this therapy have durable responses.”
Of all the patients who achieved a CR, only 2 have relapsed, he said, “and now many of these patients have passed the 5-year mark for complete remissions.”
Toxicity of CTL019 in CLL
“When you give the cells, there’s not much toxicity,” Dr Schuster said. “These are the patients’ own cells; they’re not reacting adversely to that. It’s what happens afterwards that you have to be on the lookout for as the cells begin to expand in vivo.”
Patients experience some reversible renal toxicity, mostly hypertension-related, and some tumor lysis syndrome (TLS). No deaths occurred from TLS in CLL.
B-cell aplasia and hypogammaglobulinema occur in responding patients. They receive gamma globulin replacement as supportive therapy and generally experience no excessive or unusual infections.
“Cytokine release syndrome is the real thing to look at,” Dr Schuster said, “and that’s where early recognition and management will be life-saving.”
In both CLL and ALL, almost all responding patients develop CRS, which can be rapidly reversed with tocilizumab, the IL-6 receptor blocker.
Other CAR T-cell trials in CLL
Institutions other than the University of Pennsylvania have conducted trials of CAR T-cell therapies other than CTL019, and response rates in CLL patients have ranged from 25% (MSKCC) to 46% (Seattle), as reported at ASCO this year.
“But what’s really important to keep in mind is almost all patients who achieve complete response to date have stayed in complete response,” Dr Schuster said.
Combination trials with ibrutinib
Dr Schuster noted that patients in CAR T-cell trials who had been on ibrutinib for more than 5 months “had really robust T-cell expansion.”
So investigators believe treatment with ibrutinib may be a way of enhancing T-cell function.
A combination trial of ibrutinib and CTL019 is underway (NCT02640209). Six patients have been treated thus far, and although the follow-up is short, all 6 achieved CR at the 3-month assessment.
“So the hope is that this is going to be a partner [therapy],” Dr Schuster said. “And maybe these complete responses will be very durable, like the responses in earlier trials of CAR therapy in patients with CLL.” ![]()

Photo from Penn Medicine
NEW YORK—Trial data on the use of chimeric antigen receptor (CAR) T cells in chronic lymphocytic leukemia (CLL) are maturing, and a speaker at Lymphoma & Myeloma 2016 provided some perspective on the therapy as it now stands.
Stephen J. Schuster, MD, of the University of Pennsylvania in Philadelphia, noted that some CLL patients treated with CAR T cells remain in complete remission (CR) for more than 5 years.
Therefore, CAR T cells may be a consideration for patients who are resistant to chemotherapy.
“[I]mportantly, this immunologic approach, like other immunologic approaches . . ., tends to be non-cross-resistant to chemotherapy,” Dr Schuster said.
He made these and other observations while discussing trials of CAR T-cell therapy (particularly CTL019) in CLL.
Pilot study of CTL019 in CLL
CTL019, which is the CAR T-cell therapy used by investigators at the University of Pennsylvania, is licensed to Novartis.
The pilot study of CTL019, begun in 2009, enrolled 14 patients who had failed at least 2 prior therapies and progressed within 2 years of their last treatment.
Four patients (29%) achieved a CR, and 4 (29%) achieved a partial response (PR), for an overall response rate of 57%. Detailed results from this trial were reported earlier in HematologyTimes.
Two patients in this trial are still in CR beyond 5 years.
When investigators analyzed the different variables that might affect response—including age, number of prior therapies, p53 status, CAR T-cell dose, and the presence of cytokine release syndrome (CRS)—2 things became apparent.
First, patients who responded tended to have greater in vivo expansion of the CAR T cells than non-responders. And second, the responders had a greater incidence of CRS than non-responders.
Additionally, complete responders were negative for minimal residual disease (MRD) and had durable responses.
“This actually is different from the data you see in lymphoma with CAR cells,” Dr Schuster said. “[However,] it’s what we see in ALL [acute lymphoblastic leukemia] as well.”
Investigators also discovered that persistence of CAR T cells correlates with B-cell aplasia. In this trial, persistence of CAR T cells and B-cell aplasia were apparent at 12 and 18 months, and, in some cases, even longer.
“This is in distinction to what we are observing in trials with the lymphomas,” Dr Schuster said. “So what’s going to emerge is that the different diseases will have different response rates, different degrees of persistence of CAR cells and different toxicities.”
“When we compare B-cell ALL, B-cell non-Hodgkin lymphomas, you’ll get different responses across the subtypes of lymphomas, some unique toxicities, and differences in CLL. So these are all different diseases.”
Dose-finding trial of CTL019 in CLL
The second trial of CTL019 in relapsed/refractory CLL patients was a dose-finding study. Updated results from this study were presented at ASCO 2016.
The high-dose arm (5x108 CTL019) had a 10 times higher dose of CAR T cells than the low-dose arm (5x107 CTL019).
Investigators treated 12 patients in each arm in the first phase of the study, and then expanded the trial to include another 8 patients at the recommended dose. The phase 2 trial was powered for response rates but not duration of response.
Twenty-eight patients were enrolled, with 24 evaluable, 11 in the high-dose arm and 13 in the low-dose arm.
Their median age was 62 (range, 51-75), the median number of prior therapies was 4 (range, 2–7), 38% had p53 deletion, and 12% had received prior ibrutinib therapy.
With the 2 arms pooled together, 25% of patients achieved a CR, and 17% achieved a PR, for an overall response rate of 42%.
“Toxicities were identical in each group,” Dr Schuster said.
He noted that the CRS rate was “fairly high.” The incidence was 55% in the high-dose arm and 54% in the low-dose arm.
There was a tendency, although not statistically significant, for the higher-dose patients to have a greater response rate than the lower-dose group—54% and 31%, respectively.
So the investigators decided the expansion cohort should be conducted with the higher dose, “even though we weren’t sure there really was a difference,” Dr Schuster said.
Seventeen evaluable patients received the higher dose in the expansion cohort. Six (35%) achieved a CR, and 3 (18%) achieved a PR, for an overall response rate of 53%.
“Most [adverse] events happen in the first 3 months,” after infusion, Dr Schuster said. “And then nothing much happens. That’s because the patients that are responsive to this therapy have durable responses.”
Of all the patients who achieved a CR, only 2 have relapsed, he said, “and now many of these patients have passed the 5-year mark for complete remissions.”
Toxicity of CTL019 in CLL
“When you give the cells, there’s not much toxicity,” Dr Schuster said. “These are the patients’ own cells; they’re not reacting adversely to that. It’s what happens afterwards that you have to be on the lookout for as the cells begin to expand in vivo.”
Patients experience some reversible renal toxicity, mostly hypertension-related, and some tumor lysis syndrome (TLS). No deaths occurred from TLS in CLL.
B-cell aplasia and hypogammaglobulinema occur in responding patients. They receive gamma globulin replacement as supportive therapy and generally experience no excessive or unusual infections.
“Cytokine release syndrome is the real thing to look at,” Dr Schuster said, “and that’s where early recognition and management will be life-saving.”
In both CLL and ALL, almost all responding patients develop CRS, which can be rapidly reversed with tocilizumab, the IL-6 receptor blocker.
Other CAR T-cell trials in CLL
Institutions other than the University of Pennsylvania have conducted trials of CAR T-cell therapies other than CTL019, and response rates in CLL patients have ranged from 25% (MSKCC) to 46% (Seattle), as reported at ASCO this year.
“But what’s really important to keep in mind is almost all patients who achieve complete response to date have stayed in complete response,” Dr Schuster said.
Combination trials with ibrutinib
Dr Schuster noted that patients in CAR T-cell trials who had been on ibrutinib for more than 5 months “had really robust T-cell expansion.”
So investigators believe treatment with ibrutinib may be a way of enhancing T-cell function.
A combination trial of ibrutinib and CTL019 is underway (NCT02640209). Six patients have been treated thus far, and although the follow-up is short, all 6 achieved CR at the 3-month assessment.
“So the hope is that this is going to be a partner [therapy],” Dr Schuster said. “And maybe these complete responses will be very durable, like the responses in earlier trials of CAR therapy in patients with CLL.” ![]()