User login
Simplified HCT-CI better predicts outcomes in young patients
NEWPORT BEACH, CALIF. – A revised hematopoietic stem cell transplantation comorbidity index developed for adolescents and young adults is useful for predicting nonrelapse mortality in this specific population, according to Brian Friend, MD.
In a retrospective study of 241 patients aged 15-39 years who underwent a first allogeneic hematopoietic stem cell transplant (HCT) between 2005 and 2015 at the University of California, Los Angeles, nonrelapse mortality incidence was particularly high, with rates of 26%, 28%, and 30% at 1, 2, and 3 years, respectively, Dr. Friend, a clinical research fellow at the David Geffen School of Medicine, Los Angeles, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Rather, a history of pulmonary disease – found in 44% of the patients – was the most common comorbidity, and although this was based on pulmonary function tests alone and not necessarily on patient symptoms, it was a surprising finding, he said. It was associated with lower overall survival and with nonrelapse mortality, he added.
A psychosocial component, which took into account factors such as stressors, social support, financial issues, and substance abuse, was also fairly frequent in the patients, but was not necessarily associated with worse outcomes, he noted.
“In multivariable analysis, only a history of prior malignancy (hazard ratio, 2.04) and moderate and severe pulmonary disease (hazard ratios, 1.39 and 1.84, respectively) were associated with a higher incidence of nonrelapse mortality,” he reported.
The existing HCT-CI was developed in adults to help risk-stratify patients undergoing transplant, but adolescents and young adults undergoing HCT tend to have fewer comorbidities compared with older adults, though they still having a significant nonrelapse mortality rate, Dr. Friend said.
“We sought to develop a modified HCT-CI that would be more practical and efficient in predicting outcomes of adolescent and young adult patients,” he wrote.
Data were collected on 15 comorbidities included in the original HCT-CI study, as well as the psychosocial risk factors. The relationship between multiple variables and the incidence of nonrelapse mortality was investigated via the Fine and Gray competing risk model with adjustments for patient- and transplant-specific factors.
A few things were “looked at differently,” he said, explaining, for example, that multiple cardiovascular risk factors were combined into one since they are rare in younger patients.
The study demonstrated that an index including only a few comorbidities important in adolescents and young adults is more predictive in these younger patients vs. adults, suggesting that a simpler model is more practical and useful, Dr. Friend said.
A larger study is planned in conjunction with the Center for International Blood and Marrow Transplant Research (CIBMTR). The researchers for that study will take an in-depth look at this younger population in an effort to develop a novel risk score for them. Other future efforts will focus on developing interventions to target high risk patients – and in particular, modifiable risk factors – with a focus on preventive measures, he said.
Dr. Friend reported having no financial disclosures.
NEWPORT BEACH, CALIF. – A revised hematopoietic stem cell transplantation comorbidity index developed for adolescents and young adults is useful for predicting nonrelapse mortality in this specific population, according to Brian Friend, MD.
In a retrospective study of 241 patients aged 15-39 years who underwent a first allogeneic hematopoietic stem cell transplant (HCT) between 2005 and 2015 at the University of California, Los Angeles, nonrelapse mortality incidence was particularly high, with rates of 26%, 28%, and 30% at 1, 2, and 3 years, respectively, Dr. Friend, a clinical research fellow at the David Geffen School of Medicine, Los Angeles, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Rather, a history of pulmonary disease – found in 44% of the patients – was the most common comorbidity, and although this was based on pulmonary function tests alone and not necessarily on patient symptoms, it was a surprising finding, he said. It was associated with lower overall survival and with nonrelapse mortality, he added.
A psychosocial component, which took into account factors such as stressors, social support, financial issues, and substance abuse, was also fairly frequent in the patients, but was not necessarily associated with worse outcomes, he noted.
“In multivariable analysis, only a history of prior malignancy (hazard ratio, 2.04) and moderate and severe pulmonary disease (hazard ratios, 1.39 and 1.84, respectively) were associated with a higher incidence of nonrelapse mortality,” he reported.
The existing HCT-CI was developed in adults to help risk-stratify patients undergoing transplant, but adolescents and young adults undergoing HCT tend to have fewer comorbidities compared with older adults, though they still having a significant nonrelapse mortality rate, Dr. Friend said.
“We sought to develop a modified HCT-CI that would be more practical and efficient in predicting outcomes of adolescent and young adult patients,” he wrote.
Data were collected on 15 comorbidities included in the original HCT-CI study, as well as the psychosocial risk factors. The relationship between multiple variables and the incidence of nonrelapse mortality was investigated via the Fine and Gray competing risk model with adjustments for patient- and transplant-specific factors.
A few things were “looked at differently,” he said, explaining, for example, that multiple cardiovascular risk factors were combined into one since they are rare in younger patients.
The study demonstrated that an index including only a few comorbidities important in adolescents and young adults is more predictive in these younger patients vs. adults, suggesting that a simpler model is more practical and useful, Dr. Friend said.
A larger study is planned in conjunction with the Center for International Blood and Marrow Transplant Research (CIBMTR). The researchers for that study will take an in-depth look at this younger population in an effort to develop a novel risk score for them. Other future efforts will focus on developing interventions to target high risk patients – and in particular, modifiable risk factors – with a focus on preventive measures, he said.
Dr. Friend reported having no financial disclosures.
NEWPORT BEACH, CALIF. – A revised hematopoietic stem cell transplantation comorbidity index developed for adolescents and young adults is useful for predicting nonrelapse mortality in this specific population, according to Brian Friend, MD.
In a retrospective study of 241 patients aged 15-39 years who underwent a first allogeneic hematopoietic stem cell transplant (HCT) between 2005 and 2015 at the University of California, Los Angeles, nonrelapse mortality incidence was particularly high, with rates of 26%, 28%, and 30% at 1, 2, and 3 years, respectively, Dr. Friend, a clinical research fellow at the David Geffen School of Medicine, Los Angeles, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Rather, a history of pulmonary disease – found in 44% of the patients – was the most common comorbidity, and although this was based on pulmonary function tests alone and not necessarily on patient symptoms, it was a surprising finding, he said. It was associated with lower overall survival and with nonrelapse mortality, he added.
A psychosocial component, which took into account factors such as stressors, social support, financial issues, and substance abuse, was also fairly frequent in the patients, but was not necessarily associated with worse outcomes, he noted.
“In multivariable analysis, only a history of prior malignancy (hazard ratio, 2.04) and moderate and severe pulmonary disease (hazard ratios, 1.39 and 1.84, respectively) were associated with a higher incidence of nonrelapse mortality,” he reported.
The existing HCT-CI was developed in adults to help risk-stratify patients undergoing transplant, but adolescents and young adults undergoing HCT tend to have fewer comorbidities compared with older adults, though they still having a significant nonrelapse mortality rate, Dr. Friend said.
“We sought to develop a modified HCT-CI that would be more practical and efficient in predicting outcomes of adolescent and young adult patients,” he wrote.
Data were collected on 15 comorbidities included in the original HCT-CI study, as well as the psychosocial risk factors. The relationship between multiple variables and the incidence of nonrelapse mortality was investigated via the Fine and Gray competing risk model with adjustments for patient- and transplant-specific factors.
A few things were “looked at differently,” he said, explaining, for example, that multiple cardiovascular risk factors were combined into one since they are rare in younger patients.
The study demonstrated that an index including only a few comorbidities important in adolescents and young adults is more predictive in these younger patients vs. adults, suggesting that a simpler model is more practical and useful, Dr. Friend said.
A larger study is planned in conjunction with the Center for International Blood and Marrow Transplant Research (CIBMTR). The researchers for that study will take an in-depth look at this younger population in an effort to develop a novel risk score for them. Other future efforts will focus on developing interventions to target high risk patients – and in particular, modifiable risk factors – with a focus on preventive measures, he said.
Dr. Friend reported having no financial disclosures.
REPORTING FROM ALF 2018
Key clinical point:
Major finding: As many as 60% of the comorbidities included in the HCT-CI had no significant prevalence in young patients.
Study details: A retrospective study of 241 adolescents and young adults.
Disclosures: Dr. Friend reported having no financial disclosures.
Source: Friend B et al. ALF 2018, Poster Session.
Checkpoint inhibition after HiDAC shows promise in AML
NEWPORT BEACH, CALIF. – Adding pembrolizumab after high-dose cytarabine in patients with relapsed or refractory acute myeloid leukemia (AML) appears safe and feasible and shows promising efficacy, according to early results from a multicenter phase 2 study.
The overall response rate to this novel treatment approach in 19 evaluable patients (of 20 enrolled to date) was 42%, with 7 patients (37%) achieving a complete response or complete response with incomplete blood count recovery, and 1 (5%) achieving a partial response, reported Joshua Zeidner, MD, in a poster at the Acute Leukemia Forum of Hemedicus.
Those who went on to allogeneic stem cell transplant included three patients in complete response and one of the five who received pembrolizumab maintenance. That patient on pembrolizumab maintenance went to transplant after two cycles, three others on it relapsed after a median duration of 2.8 months in complete response, and one initially achieved a partial response and had stable disease for a “pretty remarkable” 12 cycles before progressing, he said.
Preliminary analyses in the first six patients, including three with complete response and three nonresponders, showed increased posttreatment diversity of the T-cell receptor repertoire versus baseline in peripheral blood CD8+ T cells in the complete response patients, compared with nonresponders. This suggests that T-cell diversity at baseline is a promising biomarker for programmed death-1 (PD-1) blockade response, Dr. Zeidner noted.
PD-1 suppresses immune activation, and the PD-1 pathway is exploited by AML cells to evade immune surveillance, Dr. Zeidner explained. PD-1 blockade has been shown to have antileukemic effects in vivo, there is expression of multiple coinhibitory receptors in AML patients at the time of diagnosis (that persists in refractory AML), and the ligand for PD-1 is up-regulated on AML blasts, particularly in relapsed/refractory disease, he added.
He and his colleagues hypothesized that targeting PD-1 with pembrolizumab after high-dose cytarabine (HiDAC) salvage chemotherapy would stimulate a T cell–mediated antileukemic immune response and lead to improved efficacy in patients with relapsed or refractory AML.
The ongoing study, with planned enrollment of 37 patients, includes patients aged 18-70 years with relapsed/refractory AML (median age of first 20 enrolled is 54 years). Those under age 60 years receive 2 g/m2 of intravenous HiDAC every 12 hours on days 1-5, and those over age 60 years receive 1.5 g/m2 every 12 hours on days 1-5. In both age groups, this is followed by intravenous pembrolizumab given at 200 mg on day 14.
Overall responders receive maintenance phase intravenous pembrolizumab at 200 mg every 3 weeks for up to 2 years until relapse or progression. Patients are allowed to proceed to stem cell transplant before or after the maintenance phase.
A number of correlative studies, including serial peripheral blood and bone marrow flow cytometry and T-cell receptor clonality studies, also are being conducted to look for predictive biomarkers of response, Dr. Zeidner said.
The study population to date is a relatively young, very-high-risk subgroup of AML patients; European LeukemiaNet-2017 genetic risk status was favorable in only 3 of the first 20 patients (15%), intermediate in 7 (35%), and adverse in 10 (50%). Treatment has been well tolerated; toxicities have been rare and manageable. “Overall, there have been no unexpected toxicities,” he said.
The most common overall toxicities included febrile neutropenia in 70% of patients; transaminitis (including one grade 3 case) in 50%, hyperbilirubinemia in 35%, and fatigue, increased alkaline phosphatase, and rash in 25% each.
Novel therapies for relapsed/refractory AML are urgently needed, and these early results demonstrated the safety and feasibility of adding pembrolizumab after HiDAC chemotherapy in relapsed/refractory AML patients. The preliminary finding that broadening of the immune repertoire, which may occur via increasing T-cell responses beyond endogenous viral responses, was associated with complete response was particularly encouraging, Dr. Zeidner said. The investigators hope to determine predictors of response to immune checkpoint blockade in AML through a comprehensive immune biomarker discovery approach, he added.
This study was funded by Merck. Dr. Zeidner reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Zeidner J et al. ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Adding pembrolizumab after high-dose cytarabine in patients with relapsed or refractory acute myeloid leukemia (AML) appears safe and feasible and shows promising efficacy, according to early results from a multicenter phase 2 study.
The overall response rate to this novel treatment approach in 19 evaluable patients (of 20 enrolled to date) was 42%, with 7 patients (37%) achieving a complete response or complete response with incomplete blood count recovery, and 1 (5%) achieving a partial response, reported Joshua Zeidner, MD, in a poster at the Acute Leukemia Forum of Hemedicus.
Those who went on to allogeneic stem cell transplant included three patients in complete response and one of the five who received pembrolizumab maintenance. That patient on pembrolizumab maintenance went to transplant after two cycles, three others on it relapsed after a median duration of 2.8 months in complete response, and one initially achieved a partial response and had stable disease for a “pretty remarkable” 12 cycles before progressing, he said.
Preliminary analyses in the first six patients, including three with complete response and three nonresponders, showed increased posttreatment diversity of the T-cell receptor repertoire versus baseline in peripheral blood CD8+ T cells in the complete response patients, compared with nonresponders. This suggests that T-cell diversity at baseline is a promising biomarker for programmed death-1 (PD-1) blockade response, Dr. Zeidner noted.
PD-1 suppresses immune activation, and the PD-1 pathway is exploited by AML cells to evade immune surveillance, Dr. Zeidner explained. PD-1 blockade has been shown to have antileukemic effects in vivo, there is expression of multiple coinhibitory receptors in AML patients at the time of diagnosis (that persists in refractory AML), and the ligand for PD-1 is up-regulated on AML blasts, particularly in relapsed/refractory disease, he added.
He and his colleagues hypothesized that targeting PD-1 with pembrolizumab after high-dose cytarabine (HiDAC) salvage chemotherapy would stimulate a T cell–mediated antileukemic immune response and lead to improved efficacy in patients with relapsed or refractory AML.
The ongoing study, with planned enrollment of 37 patients, includes patients aged 18-70 years with relapsed/refractory AML (median age of first 20 enrolled is 54 years). Those under age 60 years receive 2 g/m2 of intravenous HiDAC every 12 hours on days 1-5, and those over age 60 years receive 1.5 g/m2 every 12 hours on days 1-5. In both age groups, this is followed by intravenous pembrolizumab given at 200 mg on day 14.
Overall responders receive maintenance phase intravenous pembrolizumab at 200 mg every 3 weeks for up to 2 years until relapse or progression. Patients are allowed to proceed to stem cell transplant before or after the maintenance phase.
A number of correlative studies, including serial peripheral blood and bone marrow flow cytometry and T-cell receptor clonality studies, also are being conducted to look for predictive biomarkers of response, Dr. Zeidner said.
The study population to date is a relatively young, very-high-risk subgroup of AML patients; European LeukemiaNet-2017 genetic risk status was favorable in only 3 of the first 20 patients (15%), intermediate in 7 (35%), and adverse in 10 (50%). Treatment has been well tolerated; toxicities have been rare and manageable. “Overall, there have been no unexpected toxicities,” he said.
The most common overall toxicities included febrile neutropenia in 70% of patients; transaminitis (including one grade 3 case) in 50%, hyperbilirubinemia in 35%, and fatigue, increased alkaline phosphatase, and rash in 25% each.
Novel therapies for relapsed/refractory AML are urgently needed, and these early results demonstrated the safety and feasibility of adding pembrolizumab after HiDAC chemotherapy in relapsed/refractory AML patients. The preliminary finding that broadening of the immune repertoire, which may occur via increasing T-cell responses beyond endogenous viral responses, was associated with complete response was particularly encouraging, Dr. Zeidner said. The investigators hope to determine predictors of response to immune checkpoint blockade in AML through a comprehensive immune biomarker discovery approach, he added.
This study was funded by Merck. Dr. Zeidner reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Zeidner J et al. ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Adding pembrolizumab after high-dose cytarabine in patients with relapsed or refractory acute myeloid leukemia (AML) appears safe and feasible and shows promising efficacy, according to early results from a multicenter phase 2 study.
The overall response rate to this novel treatment approach in 19 evaluable patients (of 20 enrolled to date) was 42%, with 7 patients (37%) achieving a complete response or complete response with incomplete blood count recovery, and 1 (5%) achieving a partial response, reported Joshua Zeidner, MD, in a poster at the Acute Leukemia Forum of Hemedicus.
Those who went on to allogeneic stem cell transplant included three patients in complete response and one of the five who received pembrolizumab maintenance. That patient on pembrolizumab maintenance went to transplant after two cycles, three others on it relapsed after a median duration of 2.8 months in complete response, and one initially achieved a partial response and had stable disease for a “pretty remarkable” 12 cycles before progressing, he said.
Preliminary analyses in the first six patients, including three with complete response and three nonresponders, showed increased posttreatment diversity of the T-cell receptor repertoire versus baseline in peripheral blood CD8+ T cells in the complete response patients, compared with nonresponders. This suggests that T-cell diversity at baseline is a promising biomarker for programmed death-1 (PD-1) blockade response, Dr. Zeidner noted.
PD-1 suppresses immune activation, and the PD-1 pathway is exploited by AML cells to evade immune surveillance, Dr. Zeidner explained. PD-1 blockade has been shown to have antileukemic effects in vivo, there is expression of multiple coinhibitory receptors in AML patients at the time of diagnosis (that persists in refractory AML), and the ligand for PD-1 is up-regulated on AML blasts, particularly in relapsed/refractory disease, he added.
He and his colleagues hypothesized that targeting PD-1 with pembrolizumab after high-dose cytarabine (HiDAC) salvage chemotherapy would stimulate a T cell–mediated antileukemic immune response and lead to improved efficacy in patients with relapsed or refractory AML.
The ongoing study, with planned enrollment of 37 patients, includes patients aged 18-70 years with relapsed/refractory AML (median age of first 20 enrolled is 54 years). Those under age 60 years receive 2 g/m2 of intravenous HiDAC every 12 hours on days 1-5, and those over age 60 years receive 1.5 g/m2 every 12 hours on days 1-5. In both age groups, this is followed by intravenous pembrolizumab given at 200 mg on day 14.
Overall responders receive maintenance phase intravenous pembrolizumab at 200 mg every 3 weeks for up to 2 years until relapse or progression. Patients are allowed to proceed to stem cell transplant before or after the maintenance phase.
A number of correlative studies, including serial peripheral blood and bone marrow flow cytometry and T-cell receptor clonality studies, also are being conducted to look for predictive biomarkers of response, Dr. Zeidner said.
The study population to date is a relatively young, very-high-risk subgroup of AML patients; European LeukemiaNet-2017 genetic risk status was favorable in only 3 of the first 20 patients (15%), intermediate in 7 (35%), and adverse in 10 (50%). Treatment has been well tolerated; toxicities have been rare and manageable. “Overall, there have been no unexpected toxicities,” he said.
The most common overall toxicities included febrile neutropenia in 70% of patients; transaminitis (including one grade 3 case) in 50%, hyperbilirubinemia in 35%, and fatigue, increased alkaline phosphatase, and rash in 25% each.
Novel therapies for relapsed/refractory AML are urgently needed, and these early results demonstrated the safety and feasibility of adding pembrolizumab after HiDAC chemotherapy in relapsed/refractory AML patients. The preliminary finding that broadening of the immune repertoire, which may occur via increasing T-cell responses beyond endogenous viral responses, was associated with complete response was particularly encouraging, Dr. Zeidner said. The investigators hope to determine predictors of response to immune checkpoint blockade in AML through a comprehensive immune biomarker discovery approach, he added.
This study was funded by Merck. Dr. Zeidner reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Zeidner J et al. ALF 2018, Poster Session.
REPORTING FROM ALF 2018
Key clinical point:
Major finding: The overall response rate was 42%; 37% of patients achieved complete response or CR with incomplete blood count recovery, and 5% achieved partial response.
Study details: A multicenter, phase 2 study with early results from the first 20 patients enrolled.
Disclosures: This study was funded by Merck. Dr. Zeidner reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
Source: Zeidner J et al. ALF 2018, Poster Session.
5- and 10-day decitabine go head-to-head in poor-risk AML
NEWPORT BEACH, CALIF. – Response and survival rates are similar with 5- and 10-day dosing of decitabine in poor-risk older adults with previously untreated acute myeloid leukemia, according to findings from a randomized phase 2 trial.
The overall response rates in 25 patients randomized to receive 5 days of decitabine and 40 patients randomized to receive 10 days of decitabine were 44% and 38%, respectively. Complete response rates were 28% and 30%, respectively, and the median number of cycles to best response was two in both arms, Nicholas J. Short, MD, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Patients were followed for a median of 38 months. Median remission duration was 9.4 months in 11 responders who received 5 days of decitabine, and 6.4 months in 15 responders in the 10-day treatment arm. The 1-year continued remission rates were 25% and 30%, respectively (P = .85). Median overall survival was 4.9 and 7.1 months, respectively, and 1-year overall survival rates were 27% and 25%, respectively, he said, adding that none of the differences in the groups were statistically significant.
Further, no differences in survival were seen when patients in the two treatment arms were stratified by cytogenetics, de novo versus secondary or treatment-related disease, or TP53 mutations; however, these subgroups were small, he noted.
Study subjects were adults aged 60 years or older (median, 77 and 78 years) with newly diagnosed and untreated acute myeloid leukemia (AML), and adults under age 60 years who were not suitable candidates for intensive chemotherapy. They were enrolled between February 2013 and July 2017. About 30% of patients had performance status scores of 2-3, and 45% of patients had secondary AML.
“About 40% of patients in the 5-day arm had poor-risk cytogenetics, and about half in the 10-day arm had poor-risk cytogenetics,” Dr. Short said in an interview, adding that 6 of 21 tested patients in the 5-day arm and 16 of 38 tested patients in the 10-day arm had a TP53 mutation.
Patients received intravenous decitabine at a dose of 20 mg/m2 for the assigned duration of either 5 or 10 consecutive days for the first three cycles of induction, and those who responded to treatment received additional consolidation cycles every 4-8 weeks for up to 24 total cycles. Patients in the 10-day arm were switched to 5-day dosing after achieving complete response or complete response with incomplete blood count recovery.
The groups were well balanced with respect to baseline characteristics and the imbalance in patient numbers in the arms was mainly because of adaptive randomization; the 10-day patients had better responses during the early part of the study, Dr. Short explained.
None of the patients underwent allogeneic stem cell transplantation, he added.
Older patients with acute AML often have poor tolerance for intensive chemotherapy, but decitabine has been shown to improve survival when compared with supportive care or low-dose cytarabine in these patients. However, while some single-arm studies have suggested that 5- and 10-day dosing may result in similar outcomes, and another suggested that 10-day dosing may be superior in TP53-mutated AML, no studies have directly compared 5- and 10-day dosing, he said.
“In this relatively poor-risk cohort of older adults with newly diagnosed AML, decitabine for 5 and 10 days resulted in similar response rates, survival, and early mortality,” he concluded.
This study was funded by a University of Texas MD Anderson Cancer Center support grant. Dr. Short reported having no financial disclosures.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Short NJ et al. ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Response and survival rates are similar with 5- and 10-day dosing of decitabine in poor-risk older adults with previously untreated acute myeloid leukemia, according to findings from a randomized phase 2 trial.
The overall response rates in 25 patients randomized to receive 5 days of decitabine and 40 patients randomized to receive 10 days of decitabine were 44% and 38%, respectively. Complete response rates were 28% and 30%, respectively, and the median number of cycles to best response was two in both arms, Nicholas J. Short, MD, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Patients were followed for a median of 38 months. Median remission duration was 9.4 months in 11 responders who received 5 days of decitabine, and 6.4 months in 15 responders in the 10-day treatment arm. The 1-year continued remission rates were 25% and 30%, respectively (P = .85). Median overall survival was 4.9 and 7.1 months, respectively, and 1-year overall survival rates were 27% and 25%, respectively, he said, adding that none of the differences in the groups were statistically significant.
Further, no differences in survival were seen when patients in the two treatment arms were stratified by cytogenetics, de novo versus secondary or treatment-related disease, or TP53 mutations; however, these subgroups were small, he noted.
Study subjects were adults aged 60 years or older (median, 77 and 78 years) with newly diagnosed and untreated acute myeloid leukemia (AML), and adults under age 60 years who were not suitable candidates for intensive chemotherapy. They were enrolled between February 2013 and July 2017. About 30% of patients had performance status scores of 2-3, and 45% of patients had secondary AML.
“About 40% of patients in the 5-day arm had poor-risk cytogenetics, and about half in the 10-day arm had poor-risk cytogenetics,” Dr. Short said in an interview, adding that 6 of 21 tested patients in the 5-day arm and 16 of 38 tested patients in the 10-day arm had a TP53 mutation.
Patients received intravenous decitabine at a dose of 20 mg/m2 for the assigned duration of either 5 or 10 consecutive days for the first three cycles of induction, and those who responded to treatment received additional consolidation cycles every 4-8 weeks for up to 24 total cycles. Patients in the 10-day arm were switched to 5-day dosing after achieving complete response or complete response with incomplete blood count recovery.
The groups were well balanced with respect to baseline characteristics and the imbalance in patient numbers in the arms was mainly because of adaptive randomization; the 10-day patients had better responses during the early part of the study, Dr. Short explained.
None of the patients underwent allogeneic stem cell transplantation, he added.
Older patients with acute AML often have poor tolerance for intensive chemotherapy, but decitabine has been shown to improve survival when compared with supportive care or low-dose cytarabine in these patients. However, while some single-arm studies have suggested that 5- and 10-day dosing may result in similar outcomes, and another suggested that 10-day dosing may be superior in TP53-mutated AML, no studies have directly compared 5- and 10-day dosing, he said.
“In this relatively poor-risk cohort of older adults with newly diagnosed AML, decitabine for 5 and 10 days resulted in similar response rates, survival, and early mortality,” he concluded.
This study was funded by a University of Texas MD Anderson Cancer Center support grant. Dr. Short reported having no financial disclosures.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Short NJ et al. ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Response and survival rates are similar with 5- and 10-day dosing of decitabine in poor-risk older adults with previously untreated acute myeloid leukemia, according to findings from a randomized phase 2 trial.
The overall response rates in 25 patients randomized to receive 5 days of decitabine and 40 patients randomized to receive 10 days of decitabine were 44% and 38%, respectively. Complete response rates were 28% and 30%, respectively, and the median number of cycles to best response was two in both arms, Nicholas J. Short, MD, reported in a poster at the Acute Leukemia Forum of Hemedicus.
Patients were followed for a median of 38 months. Median remission duration was 9.4 months in 11 responders who received 5 days of decitabine, and 6.4 months in 15 responders in the 10-day treatment arm. The 1-year continued remission rates were 25% and 30%, respectively (P = .85). Median overall survival was 4.9 and 7.1 months, respectively, and 1-year overall survival rates were 27% and 25%, respectively, he said, adding that none of the differences in the groups were statistically significant.
Further, no differences in survival were seen when patients in the two treatment arms were stratified by cytogenetics, de novo versus secondary or treatment-related disease, or TP53 mutations; however, these subgroups were small, he noted.
Study subjects were adults aged 60 years or older (median, 77 and 78 years) with newly diagnosed and untreated acute myeloid leukemia (AML), and adults under age 60 years who were not suitable candidates for intensive chemotherapy. They were enrolled between February 2013 and July 2017. About 30% of patients had performance status scores of 2-3, and 45% of patients had secondary AML.
“About 40% of patients in the 5-day arm had poor-risk cytogenetics, and about half in the 10-day arm had poor-risk cytogenetics,” Dr. Short said in an interview, adding that 6 of 21 tested patients in the 5-day arm and 16 of 38 tested patients in the 10-day arm had a TP53 mutation.
Patients received intravenous decitabine at a dose of 20 mg/m2 for the assigned duration of either 5 or 10 consecutive days for the first three cycles of induction, and those who responded to treatment received additional consolidation cycles every 4-8 weeks for up to 24 total cycles. Patients in the 10-day arm were switched to 5-day dosing after achieving complete response or complete response with incomplete blood count recovery.
The groups were well balanced with respect to baseline characteristics and the imbalance in patient numbers in the arms was mainly because of adaptive randomization; the 10-day patients had better responses during the early part of the study, Dr. Short explained.
None of the patients underwent allogeneic stem cell transplantation, he added.
Older patients with acute AML often have poor tolerance for intensive chemotherapy, but decitabine has been shown to improve survival when compared with supportive care or low-dose cytarabine in these patients. However, while some single-arm studies have suggested that 5- and 10-day dosing may result in similar outcomes, and another suggested that 10-day dosing may be superior in TP53-mutated AML, no studies have directly compared 5- and 10-day dosing, he said.
“In this relatively poor-risk cohort of older adults with newly diagnosed AML, decitabine for 5 and 10 days resulted in similar response rates, survival, and early mortality,” he concluded.
This study was funded by a University of Texas MD Anderson Cancer Center support grant. Dr. Short reported having no financial disclosures.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Short NJ et al. ALF 2018, Poster Session.
REPORTING FROM ALF 2018
Key clinical point:
Major finding: Overall response rates were 44% with 5-day dosing and 38% with 10-day dosing.
Study details: A randomized phase 2 study of 65 patients.
Disclosures: This study was funded by an University of Texas MD Anderson Cancer Center support grant. Dr. Short reported having no financial disclosures.
Source: Short NJ et al. ALF 2018, Poster Session.
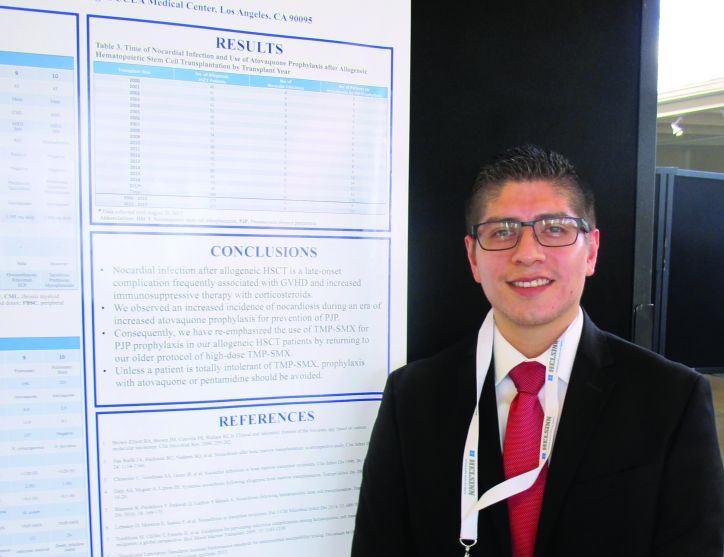
Study: Stick with TMP-SMX for posttransplant PJP prophylaxis
NEWPORT BEACH, CALIF. – Use of atovaquone or pentamidine for Pneumocystis jiroveci pneumonia (PJP) prophylaxis was associated with an increased incidence of nocardiosis in allogeneic hematopoietic stem call transplant (HSCT) recipients at the University of California, Los Angeles, according to a review of patient records.
Of 10 cases of late-onset nocardiosis identified among patients who received HSCT between Jan. 1, 2000, and Aug. 30, 2017, 9 cases occurred in 411 patients (2.2%) treated between 2012 and 2017 – a period of increased use of atovaquone prophylaxis, compared with only 1 in 575 patients (0.17%) treated in the prior 12 years when trimethoprim-sulfamethoxazole (TMP-SMX) was used for prophylaxis, Alfonso Molina reported in a poster at the Acute Leukemia Forum of Hemedicus.
None of the 575 patients treated between 2000 and 2012, versus 119 of the 411 treated after 2012, received atovaquone, he reported.
To assess the potential relationship between the use of atovaquone and the increased incidence of nocardiosis, he and his colleagues reviewed patient medical records and UCLA Clinical Microbiology Laboratory culture results.
Nocardiosis occurred mainly in patients on high doses of corticosteroids for graft-versus-host disease, and 8 of the 10 affected patients were not receiving TMP-SMX for PJP prophylaxis; 7 were on atovaquone, and 1 was on intravenous pentamidine, Mr. Molina said.
The findings suggest that TMP-SMX should remain the agent of choice for PJP prophylaxis in HSCT recipients and have prompted a return to the older protocol of high-dose TMP-SMX for this purpose at UCLA, he said.
“Unless a patient is totally intolerant of TMP-SMX, prophylaxis with atovaquone or pentamidine should be avoided,” he concluded.
Mr. Molina reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Molina A et al., ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Use of atovaquone or pentamidine for Pneumocystis jiroveci pneumonia (PJP) prophylaxis was associated with an increased incidence of nocardiosis in allogeneic hematopoietic stem call transplant (HSCT) recipients at the University of California, Los Angeles, according to a review of patient records.
Of 10 cases of late-onset nocardiosis identified among patients who received HSCT between Jan. 1, 2000, and Aug. 30, 2017, 9 cases occurred in 411 patients (2.2%) treated between 2012 and 2017 – a period of increased use of atovaquone prophylaxis, compared with only 1 in 575 patients (0.17%) treated in the prior 12 years when trimethoprim-sulfamethoxazole (TMP-SMX) was used for prophylaxis, Alfonso Molina reported in a poster at the Acute Leukemia Forum of Hemedicus.
None of the 575 patients treated between 2000 and 2012, versus 119 of the 411 treated after 2012, received atovaquone, he reported.
To assess the potential relationship between the use of atovaquone and the increased incidence of nocardiosis, he and his colleagues reviewed patient medical records and UCLA Clinical Microbiology Laboratory culture results.
Nocardiosis occurred mainly in patients on high doses of corticosteroids for graft-versus-host disease, and 8 of the 10 affected patients were not receiving TMP-SMX for PJP prophylaxis; 7 were on atovaquone, and 1 was on intravenous pentamidine, Mr. Molina said.
The findings suggest that TMP-SMX should remain the agent of choice for PJP prophylaxis in HSCT recipients and have prompted a return to the older protocol of high-dose TMP-SMX for this purpose at UCLA, he said.
“Unless a patient is totally intolerant of TMP-SMX, prophylaxis with atovaquone or pentamidine should be avoided,” he concluded.
Mr. Molina reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Molina A et al., ALF 2018, Poster Session.
NEWPORT BEACH, CALIF. – Use of atovaquone or pentamidine for Pneumocystis jiroveci pneumonia (PJP) prophylaxis was associated with an increased incidence of nocardiosis in allogeneic hematopoietic stem call transplant (HSCT) recipients at the University of California, Los Angeles, according to a review of patient records.
Of 10 cases of late-onset nocardiosis identified among patients who received HSCT between Jan. 1, 2000, and Aug. 30, 2017, 9 cases occurred in 411 patients (2.2%) treated between 2012 and 2017 – a period of increased use of atovaquone prophylaxis, compared with only 1 in 575 patients (0.17%) treated in the prior 12 years when trimethoprim-sulfamethoxazole (TMP-SMX) was used for prophylaxis, Alfonso Molina reported in a poster at the Acute Leukemia Forum of Hemedicus.
None of the 575 patients treated between 2000 and 2012, versus 119 of the 411 treated after 2012, received atovaquone, he reported.
To assess the potential relationship between the use of atovaquone and the increased incidence of nocardiosis, he and his colleagues reviewed patient medical records and UCLA Clinical Microbiology Laboratory culture results.
Nocardiosis occurred mainly in patients on high doses of corticosteroids for graft-versus-host disease, and 8 of the 10 affected patients were not receiving TMP-SMX for PJP prophylaxis; 7 were on atovaquone, and 1 was on intravenous pentamidine, Mr. Molina said.
The findings suggest that TMP-SMX should remain the agent of choice for PJP prophylaxis in HSCT recipients and have prompted a return to the older protocol of high-dose TMP-SMX for this purpose at UCLA, he said.
“Unless a patient is totally intolerant of TMP-SMX, prophylaxis with atovaquone or pentamidine should be avoided,” he concluded.
Mr. Molina reported having no financial disclosures. The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
SOURCE: Molina A et al., ALF 2018, Poster Session.
REPORTING FROM ALF 2018
Key clinical point:
Major finding: The incidence of nocardiosis was 2.2% during atovaquone use versus 0.17% prior to its use.
Study details: A retrospective review of records for 986 patients.
Disclosures: Mr. Molina reported having no financial disclosures.
Source: Molina A et al. ALF 2018, Poster Session.