User login
Severe ipsilateral headache
On the basis of the patient's presentation, family history, and personal history of headache, she seems to be presenting with hemiplegic migraine, an uncommon migraine subtype characterized by recurrent headaches associated with temporary unilateral hemiparesis or hemiplegia. The hemiparesis may resolve before the headache, as seen in the present case, or it may persist for days to weeks. These episodes are sometimes accompanied by ipsilateral numbness, tingling, or paresthesia, with or without a speech disturbance. Visual defects (ie, scintillating scotoma and hemianopia) and aphasia may occur.
Hemiplegic migraine can be sporadic or familial. Familial hemiplegic migraine is the only migraine subtype for which an autosomal dominant mode of inheritance has been identified. The onset is generally in adolescence between 12 and 17 years of age, with an estimated prevalence of 0.01%. Female patients are more likely to have these types of migraines.
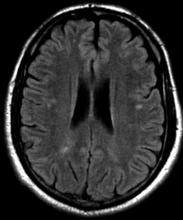
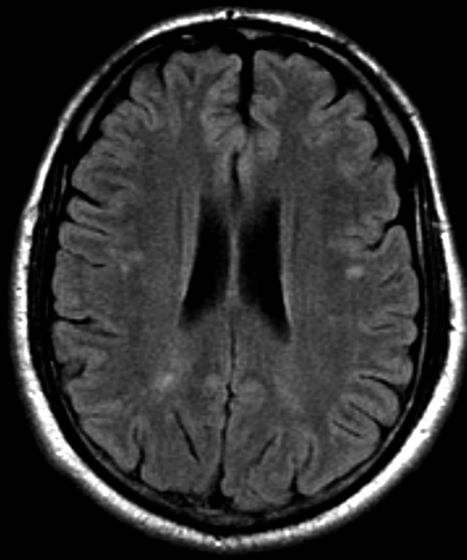
Diagnosis of hemiplegic migraine is centered on exclusion of other possible causes of headache with motor weakness. When a patient presents with motor deficit, these symptoms can also be the result of a secondary headache rather than a primary headache disorder. Because of this neurologic aspect of presentation, the differential diagnosis is broad and should span other migraine subtypes, inflammatory or metabolic disorders, and mitochondrial diseases, as well as any condition that shows neurologic deficits without radiologic alterations. Pediatric patients with hemiplegic migraine are often misdiagnosed with epilepsy. Compared with hemiplegic migraine, seizures are much more brief, and any associated hemiparesis is usually characterized by limb jerking, head turning, and loss of consciousness. Of note, up to 7% of patients with familial hemiplegic migraine do eventually develop epilepsy. Although there are no telltale pathognomonic clinical, laboratory, or radiologic findings of hemiplegic migraine, electroencephalography may show asymmetric slow-wave activity contralateral to the hemiparesis.
In hemiplegic migraine, acute treatment options include antiemetics, NSAIDs, and nonnarcotic pain relievers; triptans and ergotamine preparations are contraindicated in this setting because of their potential vasoconstrictive effects. Even if episode frequency is low, the American Headache Society advises that prophylactic treatment should also be considered in the management of uncommon migraine subtypes such as this one.
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
On the basis of the patient's presentation, family history, and personal history of headache, she seems to be presenting with hemiplegic migraine, an uncommon migraine subtype characterized by recurrent headaches associated with temporary unilateral hemiparesis or hemiplegia. The hemiparesis may resolve before the headache, as seen in the present case, or it may persist for days to weeks. These episodes are sometimes accompanied by ipsilateral numbness, tingling, or paresthesia, with or without a speech disturbance. Visual defects (ie, scintillating scotoma and hemianopia) and aphasia may occur.
Hemiplegic migraine can be sporadic or familial. Familial hemiplegic migraine is the only migraine subtype for which an autosomal dominant mode of inheritance has been identified. The onset is generally in adolescence between 12 and 17 years of age, with an estimated prevalence of 0.01%. Female patients are more likely to have these types of migraines.
Diagnosis of hemiplegic migraine is centered on exclusion of other possible causes of headache with motor weakness. When a patient presents with motor deficit, these symptoms can also be the result of a secondary headache rather than a primary headache disorder. Because of this neurologic aspect of presentation, the differential diagnosis is broad and should span other migraine subtypes, inflammatory or metabolic disorders, and mitochondrial diseases, as well as any condition that shows neurologic deficits without radiologic alterations. Pediatric patients with hemiplegic migraine are often misdiagnosed with epilepsy. Compared with hemiplegic migraine, seizures are much more brief, and any associated hemiparesis is usually characterized by limb jerking, head turning, and loss of consciousness. Of note, up to 7% of patients with familial hemiplegic migraine do eventually develop epilepsy. Although there are no telltale pathognomonic clinical, laboratory, or radiologic findings of hemiplegic migraine, electroencephalography may show asymmetric slow-wave activity contralateral to the hemiparesis.
In hemiplegic migraine, acute treatment options include antiemetics, NSAIDs, and nonnarcotic pain relievers; triptans and ergotamine preparations are contraindicated in this setting because of their potential vasoconstrictive effects. Even if episode frequency is low, the American Headache Society advises that prophylactic treatment should also be considered in the management of uncommon migraine subtypes such as this one.
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
On the basis of the patient's presentation, family history, and personal history of headache, she seems to be presenting with hemiplegic migraine, an uncommon migraine subtype characterized by recurrent headaches associated with temporary unilateral hemiparesis or hemiplegia. The hemiparesis may resolve before the headache, as seen in the present case, or it may persist for days to weeks. These episodes are sometimes accompanied by ipsilateral numbness, tingling, or paresthesia, with or without a speech disturbance. Visual defects (ie, scintillating scotoma and hemianopia) and aphasia may occur.
Hemiplegic migraine can be sporadic or familial. Familial hemiplegic migraine is the only migraine subtype for which an autosomal dominant mode of inheritance has been identified. The onset is generally in adolescence between 12 and 17 years of age, with an estimated prevalence of 0.01%. Female patients are more likely to have these types of migraines.
Diagnosis of hemiplegic migraine is centered on exclusion of other possible causes of headache with motor weakness. When a patient presents with motor deficit, these symptoms can also be the result of a secondary headache rather than a primary headache disorder. Because of this neurologic aspect of presentation, the differential diagnosis is broad and should span other migraine subtypes, inflammatory or metabolic disorders, and mitochondrial diseases, as well as any condition that shows neurologic deficits without radiologic alterations. Pediatric patients with hemiplegic migraine are often misdiagnosed with epilepsy. Compared with hemiplegic migraine, seizures are much more brief, and any associated hemiparesis is usually characterized by limb jerking, head turning, and loss of consciousness. Of note, up to 7% of patients with familial hemiplegic migraine do eventually develop epilepsy. Although there are no telltale pathognomonic clinical, laboratory, or radiologic findings of hemiplegic migraine, electroencephalography may show asymmetric slow-wave activity contralateral to the hemiparesis.
In hemiplegic migraine, acute treatment options include antiemetics, NSAIDs, and nonnarcotic pain relievers; triptans and ergotamine preparations are contraindicated in this setting because of their potential vasoconstrictive effects. Even if episode frequency is low, the American Headache Society advises that prophylactic treatment should also be considered in the management of uncommon migraine subtypes such as this one.
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 16-year-old female patient presents with a severe ipsilateral headache. She describes that before the onset of head pain, she felt like she could not control her facial muscles on one side, and she was unable to speak in full sentences. She reports that these symptoms probably lasted an hour or so, and she was worried that she was experiencing an allergic reaction, though she reports no known allergies. In terms of family history, the patient explains that she does not have a close relationship with her father, but she recalls that he experienced similar episodes. She notes a history of frequent and recurrent headaches, varying in severity, for which she usually takes a high dose of nonsteroidal anti-inflammatory drugs (NSAIDs).
Migraine: Treatment Basics
Retro-orbital headache and nausea
On the basis of his presentation, this patient is probably experiencing migraine with visual aura. Migraine is a condition in children and adolescents whose prevalence increases with age: 1%-3% between age 3 and 7 years, 4%-11% between age 7 and 11 years, and 8%-23% by age 15 years. Although migraine without aura is relatively uncommon in the pediatric population, visual aura is a hallmark sign of migraine headache and excludes the other headache types in the differential diagnosis. Basilar migraine is unlikely because the patient has not experienced symptoms that suggest occipital or brainstem area dysfunction post-aura.
The diagnosis of migraine is largely clinical, but the American Academy of Neurology (AAN) guidelines for the acute treatment of pediatric migraine recommend that when assessing children and adolescents with headache, clinicians should diagnose a specific headache type: primary, secondary, or other headache syndrome. Migraine in pediatric patients is often related to triggering factors such as infection, physical or psychological stress, or dietary choices, but on the basis of the patient's history, this headache appears to be primary in nature.
Most pediatric patients can achieve control of their migraines with acute treatments and benefit from nonprescription oral analgesics, including acetaminophen, ibuprofen, and naproxen. Clinicians should prescribe ibuprofen orally (10 mg/kg) as an initial treatment for children and adolescents with migraine. The US Food and Drug Administration has only approved certain triptans for pediatric patients: almotriptan, sumatriptan-naproxen, and zolmitriptan nasal spray for patients aged 12 years or older and rizatriptan for patients aged 6-17 years.
The AAN guidelines for the pharmacologic treatment of pediatric migraine prevention report that for those who experience migraine with aura, taking a triptan during the aura is safe, though it may be more effective when taken at the onset of head pain, as is the case with other acute treatments.
In pediatric patients, avoidance of known headache triggers is generally sufficient for migraine prevention. This includes managing anxiety, depression, attention-deficit/hyperactivity disorder, and other psychiatric comorbidities that can exacerbate headache. Lifestyle management also includes ensuring adequate sleep, exercise, hydration, and stress management.
The guidelines conclude that although the majority of randomized controlled trials exploring the efficacy of preventive medications in the pediatric population fail to demonstrate superiority to placebo, migraine prophylaxis should be considered when headaches occur with high frequency and severity and cause migraine-related disability based on the Pediatric Migraine Disability Assessment (PedMIDAS).
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships
On the basis of his presentation, this patient is probably experiencing migraine with visual aura. Migraine is a condition in children and adolescents whose prevalence increases with age: 1%-3% between age 3 and 7 years, 4%-11% between age 7 and 11 years, and 8%-23% by age 15 years. Although migraine without aura is relatively uncommon in the pediatric population, visual aura is a hallmark sign of migraine headache and excludes the other headache types in the differential diagnosis. Basilar migraine is unlikely because the patient has not experienced symptoms that suggest occipital or brainstem area dysfunction post-aura.
The diagnosis of migraine is largely clinical, but the American Academy of Neurology (AAN) guidelines for the acute treatment of pediatric migraine recommend that when assessing children and adolescents with headache, clinicians should diagnose a specific headache type: primary, secondary, or other headache syndrome. Migraine in pediatric patients is often related to triggering factors such as infection, physical or psychological stress, or dietary choices, but on the basis of the patient's history, this headache appears to be primary in nature.
Most pediatric patients can achieve control of their migraines with acute treatments and benefit from nonprescription oral analgesics, including acetaminophen, ibuprofen, and naproxen. Clinicians should prescribe ibuprofen orally (10 mg/kg) as an initial treatment for children and adolescents with migraine. The US Food and Drug Administration has only approved certain triptans for pediatric patients: almotriptan, sumatriptan-naproxen, and zolmitriptan nasal spray for patients aged 12 years or older and rizatriptan for patients aged 6-17 years.
The AAN guidelines for the pharmacologic treatment of pediatric migraine prevention report that for those who experience migraine with aura, taking a triptan during the aura is safe, though it may be more effective when taken at the onset of head pain, as is the case with other acute treatments.
In pediatric patients, avoidance of known headache triggers is generally sufficient for migraine prevention. This includes managing anxiety, depression, attention-deficit/hyperactivity disorder, and other psychiatric comorbidities that can exacerbate headache. Lifestyle management also includes ensuring adequate sleep, exercise, hydration, and stress management.
The guidelines conclude that although the majority of randomized controlled trials exploring the efficacy of preventive medications in the pediatric population fail to demonstrate superiority to placebo, migraine prophylaxis should be considered when headaches occur with high frequency and severity and cause migraine-related disability based on the Pediatric Migraine Disability Assessment (PedMIDAS).
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships
On the basis of his presentation, this patient is probably experiencing migraine with visual aura. Migraine is a condition in children and adolescents whose prevalence increases with age: 1%-3% between age 3 and 7 years, 4%-11% between age 7 and 11 years, and 8%-23% by age 15 years. Although migraine without aura is relatively uncommon in the pediatric population, visual aura is a hallmark sign of migraine headache and excludes the other headache types in the differential diagnosis. Basilar migraine is unlikely because the patient has not experienced symptoms that suggest occipital or brainstem area dysfunction post-aura.
The diagnosis of migraine is largely clinical, but the American Academy of Neurology (AAN) guidelines for the acute treatment of pediatric migraine recommend that when assessing children and adolescents with headache, clinicians should diagnose a specific headache type: primary, secondary, or other headache syndrome. Migraine in pediatric patients is often related to triggering factors such as infection, physical or psychological stress, or dietary choices, but on the basis of the patient's history, this headache appears to be primary in nature.
Most pediatric patients can achieve control of their migraines with acute treatments and benefit from nonprescription oral analgesics, including acetaminophen, ibuprofen, and naproxen. Clinicians should prescribe ibuprofen orally (10 mg/kg) as an initial treatment for children and adolescents with migraine. The US Food and Drug Administration has only approved certain triptans for pediatric patients: almotriptan, sumatriptan-naproxen, and zolmitriptan nasal spray for patients aged 12 years or older and rizatriptan for patients aged 6-17 years.
The AAN guidelines for the pharmacologic treatment of pediatric migraine prevention report that for those who experience migraine with aura, taking a triptan during the aura is safe, though it may be more effective when taken at the onset of head pain, as is the case with other acute treatments.
In pediatric patients, avoidance of known headache triggers is generally sufficient for migraine prevention. This includes managing anxiety, depression, attention-deficit/hyperactivity disorder, and other psychiatric comorbidities that can exacerbate headache. Lifestyle management also includes ensuring adequate sleep, exercise, hydration, and stress management.
The guidelines conclude that although the majority of randomized controlled trials exploring the efficacy of preventive medications in the pediatric population fail to demonstrate superiority to placebo, migraine prophylaxis should be considered when headaches occur with high frequency and severity and cause migraine-related disability based on the Pediatric Migraine Disability Assessment (PedMIDAS).
Jasmin Harpe, MD, MPH, Headache Fellow, Department of Neurology, Harvard University, John R. Graham Headache Center, Mass General Brigham, Boston, MA
Jasmin Harpe, MD, MPH, has disclosed no relevant financial relationships
A 7-year-old boy presents with a retro-orbital headache, nausea, and photophobia. Height is 4 ft 2 in and weight is 70 lb (BMI 19.7). The patient's mother reports that he described seeing "rainbow shapes" in his line of vision about 20 minutes before the onset of head pain and notes that she herself has a history of headache. The patient is nonfebrile but sweating and drowsy. Physical examination is unrevealing. The patient has no known allergies and is not currently on medication.
Psychiatric comorbidities highly prevalent in children hospitalized with migraine
Key clinical point: Children hospitalized with migraine showed a high prevalence of psychiatric comorbidities, the presence of which was associated with increased medication use, a longer length of stay (LOS), and increased readmission.
Major finding: Psychiatric comorbidities were prevalent in 32% of children hospitalized for migraine headaches, with the prevalence of anxiety (11.2%), depression (6.7%), and attention-deficit/hyperactivity disorder (6.5%) being the highest. Children with vs. without psychiatric comorbidity were significantly more likely to receive dihydroergotamine, topiramate, and valproate, and had a longer mean LOS and higher 30-day readmission (all P < .001).
Study details: This multicenter, retrospective, cohort study included 21,436 children aged 6-18 years who were hospitalized for migraine headache.
Disclosures: No funding was received for this study. The authors declared no conflict of interests.
Source: Kafle M et al. Association of psychiatric comorbidities with treatment and outcomes in pediatric migraines. Hosp Pediatr. 2022;12(3):e101-e105 (Feb 14). Doi: 10.1542/hpeds.2021-006085
Key clinical point: Children hospitalized with migraine showed a high prevalence of psychiatric comorbidities, the presence of which was associated with increased medication use, a longer length of stay (LOS), and increased readmission.
Major finding: Psychiatric comorbidities were prevalent in 32% of children hospitalized for migraine headaches, with the prevalence of anxiety (11.2%), depression (6.7%), and attention-deficit/hyperactivity disorder (6.5%) being the highest. Children with vs. without psychiatric comorbidity were significantly more likely to receive dihydroergotamine, topiramate, and valproate, and had a longer mean LOS and higher 30-day readmission (all P < .001).
Study details: This multicenter, retrospective, cohort study included 21,436 children aged 6-18 years who were hospitalized for migraine headache.
Disclosures: No funding was received for this study. The authors declared no conflict of interests.
Source: Kafle M et al. Association of psychiatric comorbidities with treatment and outcomes in pediatric migraines. Hosp Pediatr. 2022;12(3):e101-e105 (Feb 14). Doi: 10.1542/hpeds.2021-006085
Key clinical point: Children hospitalized with migraine showed a high prevalence of psychiatric comorbidities, the presence of which was associated with increased medication use, a longer length of stay (LOS), and increased readmission.
Major finding: Psychiatric comorbidities were prevalent in 32% of children hospitalized for migraine headaches, with the prevalence of anxiety (11.2%), depression (6.7%), and attention-deficit/hyperactivity disorder (6.5%) being the highest. Children with vs. without psychiatric comorbidity were significantly more likely to receive dihydroergotamine, topiramate, and valproate, and had a longer mean LOS and higher 30-day readmission (all P < .001).
Study details: This multicenter, retrospective, cohort study included 21,436 children aged 6-18 years who were hospitalized for migraine headache.
Disclosures: No funding was received for this study. The authors declared no conflict of interests.
Source: Kafle M et al. Association of psychiatric comorbidities with treatment and outcomes in pediatric migraines. Hosp Pediatr. 2022;12(3):e101-e105 (Feb 14). Doi: 10.1542/hpeds.2021-006085
Neck pain highly prevalent in migraine
Key clinical point: Neck pain is frequent in migraine, with the likelihood of neck pain being 12 times higher in patients with migraine than in nonheadache control individuals.
Major finding: Patients with migraine (77.0%; 95% CI 69.0%-86.4%) displayed a higher relative frequency of neck pain vs. nonheadache control individuals (23.2%; 95% CI 18.6%-28.5%) and a 12 times higher likelihood of experiencing neck pain (odds ratio 11.5; 95% CI 5.8-22.4).
Study details: Findings are from a meta-analysis of 24 clinic-based studies including 4,352 patients with migraine.
Disclosures: No funding was received for this study. Some of the authors declared receiving speaking fees, honoraria, consultant fees, personal fees, or research grants from or serving as a principal investigator of clinical trials for various organizations.
Source: Al-Khazali HM et al. Prevalence of neck pain in migraine: A systematic review and meta-analysis. Cephalalgia. 2022 (Feb 15). Doi: 10.1177/03331024211068073
Key clinical point: Neck pain is frequent in migraine, with the likelihood of neck pain being 12 times higher in patients with migraine than in nonheadache control individuals.
Major finding: Patients with migraine (77.0%; 95% CI 69.0%-86.4%) displayed a higher relative frequency of neck pain vs. nonheadache control individuals (23.2%; 95% CI 18.6%-28.5%) and a 12 times higher likelihood of experiencing neck pain (odds ratio 11.5; 95% CI 5.8-22.4).
Study details: Findings are from a meta-analysis of 24 clinic-based studies including 4,352 patients with migraine.
Disclosures: No funding was received for this study. Some of the authors declared receiving speaking fees, honoraria, consultant fees, personal fees, or research grants from or serving as a principal investigator of clinical trials for various organizations.
Source: Al-Khazali HM et al. Prevalence of neck pain in migraine: A systematic review and meta-analysis. Cephalalgia. 2022 (Feb 15). Doi: 10.1177/03331024211068073
Key clinical point: Neck pain is frequent in migraine, with the likelihood of neck pain being 12 times higher in patients with migraine than in nonheadache control individuals.
Major finding: Patients with migraine (77.0%; 95% CI 69.0%-86.4%) displayed a higher relative frequency of neck pain vs. nonheadache control individuals (23.2%; 95% CI 18.6%-28.5%) and a 12 times higher likelihood of experiencing neck pain (odds ratio 11.5; 95% CI 5.8-22.4).
Study details: Findings are from a meta-analysis of 24 clinic-based studies including 4,352 patients with migraine.
Disclosures: No funding was received for this study. Some of the authors declared receiving speaking fees, honoraria, consultant fees, personal fees, or research grants from or serving as a principal investigator of clinical trials for various organizations.
Source: Al-Khazali HM et al. Prevalence of neck pain in migraine: A systematic review and meta-analysis. Cephalalgia. 2022 (Feb 15). Doi: 10.1177/03331024211068073
Meta-analysis strengthens evidence of increased inflammation in migraine
Key clinical point: Patients with migraine had significantly higher serum levels of interleukin (IL)-6, IL-1β, C-reactive protein (CRP), and tumor necrosis factor alpha (TNF-α) than healthy controls, with no significant difference being observed in the serum levels of IL-2 or IL-10.
Major finding: Patients with migraine vs. healthy controls had significantly higher serum levels of CRP (standardized mean difference [SMD] 1.48; P < .001), IL-1β (SMD 0.75; P < .001), IL-6 (SMD 1.18; P < .001), and TNF-α (SMD 0.69; P = .003); however, no significant difference was noted in serum IL-2 (P = .25) or IL-10 (P = .88) levels.
Study details: The data come from a meta-analysis of 10 studies that compared the peripheral cytokine levels between patients with migraine and healthy controls.
Disclosures: This study was supported by the Key Project of Henan Provincial Science and Technology Department. The authors declared no conflict of interests.
Source: Geng C et al. Aberrations in peripheral inflammatory cytokine levels in migraine: A systematic review and meta-analysis. J Clin Neurosci. 2022;98:213-218 (Feb 21). Doi: 10.1016/j.jocn.2022.02.026
Key clinical point: Patients with migraine had significantly higher serum levels of interleukin (IL)-6, IL-1β, C-reactive protein (CRP), and tumor necrosis factor alpha (TNF-α) than healthy controls, with no significant difference being observed in the serum levels of IL-2 or IL-10.
Major finding: Patients with migraine vs. healthy controls had significantly higher serum levels of CRP (standardized mean difference [SMD] 1.48; P < .001), IL-1β (SMD 0.75; P < .001), IL-6 (SMD 1.18; P < .001), and TNF-α (SMD 0.69; P = .003); however, no significant difference was noted in serum IL-2 (P = .25) or IL-10 (P = .88) levels.
Study details: The data come from a meta-analysis of 10 studies that compared the peripheral cytokine levels between patients with migraine and healthy controls.
Disclosures: This study was supported by the Key Project of Henan Provincial Science and Technology Department. The authors declared no conflict of interests.
Source: Geng C et al. Aberrations in peripheral inflammatory cytokine levels in migraine: A systematic review and meta-analysis. J Clin Neurosci. 2022;98:213-218 (Feb 21). Doi: 10.1016/j.jocn.2022.02.026
Key clinical point: Patients with migraine had significantly higher serum levels of interleukin (IL)-6, IL-1β, C-reactive protein (CRP), and tumor necrosis factor alpha (TNF-α) than healthy controls, with no significant difference being observed in the serum levels of IL-2 or IL-10.
Major finding: Patients with migraine vs. healthy controls had significantly higher serum levels of CRP (standardized mean difference [SMD] 1.48; P < .001), IL-1β (SMD 0.75; P < .001), IL-6 (SMD 1.18; P < .001), and TNF-α (SMD 0.69; P = .003); however, no significant difference was noted in serum IL-2 (P = .25) or IL-10 (P = .88) levels.
Study details: The data come from a meta-analysis of 10 studies that compared the peripheral cytokine levels between patients with migraine and healthy controls.
Disclosures: This study was supported by the Key Project of Henan Provincial Science and Technology Department. The authors declared no conflict of interests.
Source: Geng C et al. Aberrations in peripheral inflammatory cytokine levels in migraine: A systematic review and meta-analysis. J Clin Neurosci. 2022;98:213-218 (Feb 21). Doi: 10.1016/j.jocn.2022.02.026
Inflammatory potential of diets alters the frequency and severity of migraine attacks
Key clinical point: Diets with higher proinflammatory effects as indicated by higher Dietary Inflammatory Index (DII) values are significantly associated with an increased frequency and severity of migraine headaches.
Major finding: After adjusting for potential confounders, an increase in the DII score from −4.04 to −1.83 increased the headache frequency by 3.48 (β 3.48; P = .001) and was associated with a higher risk for severe headaches (odds ratio 2.25; P = .015).
Study details: Findings are from a population-based cross-sectional study including 262 patients with migraine having a body mass index of 18.5-30.0 kg/m2 and daily energy consumption of 800-4,200 kcal/day.
Disclosures: The study was funded by Isfahan University of Medical Sciences, Iran. The authors declared no conflict of interests.
Source: Ghoreishy SM et al. Associations between potential inflammatory properties of the diet and frequency, duration, and severity of migraine headaches: a cross-sectional study. Sci Rep. 2022;12:2878 (Feb 21). Doi: 10.1038/s41598-022-06819-y
Key clinical point: Diets with higher proinflammatory effects as indicated by higher Dietary Inflammatory Index (DII) values are significantly associated with an increased frequency and severity of migraine headaches.
Major finding: After adjusting for potential confounders, an increase in the DII score from −4.04 to −1.83 increased the headache frequency by 3.48 (β 3.48; P = .001) and was associated with a higher risk for severe headaches (odds ratio 2.25; P = .015).
Study details: Findings are from a population-based cross-sectional study including 262 patients with migraine having a body mass index of 18.5-30.0 kg/m2 and daily energy consumption of 800-4,200 kcal/day.
Disclosures: The study was funded by Isfahan University of Medical Sciences, Iran. The authors declared no conflict of interests.
Source: Ghoreishy SM et al. Associations between potential inflammatory properties of the diet and frequency, duration, and severity of migraine headaches: a cross-sectional study. Sci Rep. 2022;12:2878 (Feb 21). Doi: 10.1038/s41598-022-06819-y
Key clinical point: Diets with higher proinflammatory effects as indicated by higher Dietary Inflammatory Index (DII) values are significantly associated with an increased frequency and severity of migraine headaches.
Major finding: After adjusting for potential confounders, an increase in the DII score from −4.04 to −1.83 increased the headache frequency by 3.48 (β 3.48; P = .001) and was associated with a higher risk for severe headaches (odds ratio 2.25; P = .015).
Study details: Findings are from a population-based cross-sectional study including 262 patients with migraine having a body mass index of 18.5-30.0 kg/m2 and daily energy consumption of 800-4,200 kcal/day.
Disclosures: The study was funded by Isfahan University of Medical Sciences, Iran. The authors declared no conflict of interests.
Source: Ghoreishy SM et al. Associations between potential inflammatory properties of the diet and frequency, duration, and severity of migraine headaches: a cross-sectional study. Sci Rep. 2022;12:2878 (Feb 21). Doi: 10.1038/s41598-022-06819-y
Chronic migraine with medication overuse: Optimizing consumption of the overused medication
Key clinical point: Moderate-to-severe headache days in chronic migraine with medication overuse (CMMO) could be lowered with preventive medication irrespective of whether the overused symptomatic medication is continued or switched to a limited-use alternative.
Major finding: The number of monthly moderate-to-severe headache days achieved with the no switching strategy was not significantly different from that with the switching strategy both during weeks 1-2 (6.4 vs. 6.6 days; P = .57) and 9-12 (9.1 vs. 9.3 days; P = .75) after randomization.
Study details: The data come from MOTS trial including 720 patients aged ≥21 years with CMMO who were randomly assigned to receive migraine prophylactic medication and concurrently either switch from the overused medication to an alternative (≤2 days/week) or continue the overused medication with no maximum limit.
Disclosures: The study was sponsored by a Patient-Centered Outcomes Research Institute Award. Some authors reported receiving personal compensation, research grants, stock options, or royalties from various pharmaceutical companies.
Source: Schwedt T et al. Patient-centered treatment of chronic migraine with medication overuse: A prospective, randomized, pragmatic clinical trial. Neurology. 2022 (Feb 15). Doi: 10.1212/WNL.0000000000200117
Key clinical point: Moderate-to-severe headache days in chronic migraine with medication overuse (CMMO) could be lowered with preventive medication irrespective of whether the overused symptomatic medication is continued or switched to a limited-use alternative.
Major finding: The number of monthly moderate-to-severe headache days achieved with the no switching strategy was not significantly different from that with the switching strategy both during weeks 1-2 (6.4 vs. 6.6 days; P = .57) and 9-12 (9.1 vs. 9.3 days; P = .75) after randomization.
Study details: The data come from MOTS trial including 720 patients aged ≥21 years with CMMO who were randomly assigned to receive migraine prophylactic medication and concurrently either switch from the overused medication to an alternative (≤2 days/week) or continue the overused medication with no maximum limit.
Disclosures: The study was sponsored by a Patient-Centered Outcomes Research Institute Award. Some authors reported receiving personal compensation, research grants, stock options, or royalties from various pharmaceutical companies.
Source: Schwedt T et al. Patient-centered treatment of chronic migraine with medication overuse: A prospective, randomized, pragmatic clinical trial. Neurology. 2022 (Feb 15). Doi: 10.1212/WNL.0000000000200117
Key clinical point: Moderate-to-severe headache days in chronic migraine with medication overuse (CMMO) could be lowered with preventive medication irrespective of whether the overused symptomatic medication is continued or switched to a limited-use alternative.
Major finding: The number of monthly moderate-to-severe headache days achieved with the no switching strategy was not significantly different from that with the switching strategy both during weeks 1-2 (6.4 vs. 6.6 days; P = .57) and 9-12 (9.1 vs. 9.3 days; P = .75) after randomization.
Study details: The data come from MOTS trial including 720 patients aged ≥21 years with CMMO who were randomly assigned to receive migraine prophylactic medication and concurrently either switch from the overused medication to an alternative (≤2 days/week) or continue the overused medication with no maximum limit.
Disclosures: The study was sponsored by a Patient-Centered Outcomes Research Institute Award. Some authors reported receiving personal compensation, research grants, stock options, or royalties from various pharmaceutical companies.
Source: Schwedt T et al. Patient-centered treatment of chronic migraine with medication overuse: A prospective, randomized, pragmatic clinical trial. Neurology. 2022 (Feb 15). Doi: 10.1212/WNL.0000000000200117