User login
Ablative fractional lasers treat scars like ‘a magic wand’
SAN DIEGO – .
“I tell patients it’s like boiling water in a tea kettle and watching the vapor form,” Dr. Waibel, a dermatologist with the Miami Dermatology and Laser Institute, said at the annual Masters of Aesthetics Symposium. “You literally ‘steam off’ their bad scar and the human body will heal that wound to almost normal skin. It’s the closest thing we have to a magic wand.”
In the not-too-distant past, dermatologists “were treating scars just to make them look better,” she said. However, thanks to groundbreaking work by clinicians at Naval Medical Center San Diego, the use of ablative fractional lasers to treat scars was found to improve range of motion in patients, as well as their pain and pruritus. “It represents a major innovation that heals in ways not previously possible,” said Dr. Waibel, who is also chief of dermatology at Baptist Hospital in Miami. “We’re not just healing the scar; we’re healing the skin back to its physiological normal place. A lot of these patients suffer quite a bit.”
Dr. Waibel likened her scar treatment approach to a three-course meal. Lesion color drives her choice of what device to use as an “appetizer” treatment. Most scars are either red (erythematous), brown (hyperpigmented), or white (hypopigmented). Though every scar is unique and individually evaluated for treatment, typically she uses pulsed dye laser, intense pulsed light, or broadband light therapy to treat erythematous/early scars; nonablative fractional lasers to treat atrophic scars, and the thulium or 1,470-nm laser to treat hyperpigmented scars. The “main course” device in her practice is an ablative fractional erbium or CO2 laser.
“Once I treat the scar three to five times, I might switch to a nonablative laser, but I’m really an ablative fractional user,” Dr. Waibel said. “Dessert” can be whatever adjunctive therapies you need, she continued. This may include triamcinolone acetonide, 5-fluorouracil, poly-l-lactic acid, hyaluronidase, Z-plasty, punch biopsies, shave biopsies, compression, chemical reconstruction of skin scars (CROSS), and subcision.
For erythematous surgical and trauma scars, she uses a combination of pulsed dye laser and ablative fractional laser. “Same day, same treatment; one after each other,” she said. She favors using intense pulsed light for donor sites because it has filters that address both melanin and hemosiderin, superiority for scar erythema, and deeper penetration with greater speed to treat large surface areas.
One recent advance in the vascular arena is the new 595-nm pulsed dye laser by Candela, known as the VBeam Prima. It features increased energy, a 15-nm spot size, a zoom hand piece, once-a-day calibration, and contact cooling, which may be better for pigmented and possibly microvascular structures. The device is cleared for treating conditions like rosacea, acne, spider veins, port-wine stains, wrinkles, warts and stretch marks, as well as photoaging and benign pigmented lesions.
Dr. Waibel’s go-to device for treating a hypertrophic, hyperpigmented surgical scar is a 1927-nm or 1470-nm nonablative fractional laser, followed by a fractional ablative laser and injection of 1-2 ccs of 5-fluorouracil only to elevated areas. Hypopigmented scars are “by far the toughest to treat,” she said. However, she has a formula for these, too, and recently conducted a trial comparing the efficacy of nonablative fractional laser, ablative fractional laser, and ablative fractional laser followed by laser-assisted delivery of bimatoprost (Latisse) to treat hypopigmentation.
Surgical scars get better on their own in many cases, but sometimes early intervention is warranted. “Most surgeons will tell patients, ‘Wait a year. What you have [in terms of scar formation] is what you have,’” Dr. Waibel said. “If a surgical scar becomes hypertrophic, it does so within a month of surgery. I don’t prophylactically treat surgical scars unless the patient has had multiple surgeries in the same location with trouble healing. But if it’s been 6 months to a year, or if the patient is developing hypertrophic scars, then I will treat.”
Acne scars are challenging, because patients want to look good right away. “With deep scars, it takes several treatments to see good improvements,” she said. “I tell all my acne scar patients it takes a year [to get good results].”
Most burn patients require three to six treatment sessions, “but sometimes you get remarkable improvement sooner,” she said. “That’s due to the patient’s healing.” She and her associates recently completed an unpublished study that examined early intervention of fractional ablative laser versus control in 20 subjects with acute burn injuries who ranged in age from 18 to 80 years. The subjects underwent treatment with an ablative fractional CO2 laser within 3 months of sustaining the burn injury, leaving an untreated control area for comparison. According to Dr. Waibel, 100% of the blinded physician evaluators graded the laser-treated area correctly, compared with the control area. In addition, a significant improvement in all points of the Manchester Scar Scale was observed in the laser-treated area. “The earlier you treat burn and trauma patients, the easier it is to get them back to normal,” she said.
Dr. Waibel disclosed that she has conducted clinical research for Aquavit, Cytrellis, Lumenis, Lutronic, Michelson Diagnostics, RegenX, Sciton, Sebacia, and Syneron/Candela. She is also a consultant for RegenX, Strata, and Syneron/Candela and is a member of the advisory board for Dominion Technologies, Sciton, and Sebacia.
SAN DIEGO – .
“I tell patients it’s like boiling water in a tea kettle and watching the vapor form,” Dr. Waibel, a dermatologist with the Miami Dermatology and Laser Institute, said at the annual Masters of Aesthetics Symposium. “You literally ‘steam off’ their bad scar and the human body will heal that wound to almost normal skin. It’s the closest thing we have to a magic wand.”
In the not-too-distant past, dermatologists “were treating scars just to make them look better,” she said. However, thanks to groundbreaking work by clinicians at Naval Medical Center San Diego, the use of ablative fractional lasers to treat scars was found to improve range of motion in patients, as well as their pain and pruritus. “It represents a major innovation that heals in ways not previously possible,” said Dr. Waibel, who is also chief of dermatology at Baptist Hospital in Miami. “We’re not just healing the scar; we’re healing the skin back to its physiological normal place. A lot of these patients suffer quite a bit.”
Dr. Waibel likened her scar treatment approach to a three-course meal. Lesion color drives her choice of what device to use as an “appetizer” treatment. Most scars are either red (erythematous), brown (hyperpigmented), or white (hypopigmented). Though every scar is unique and individually evaluated for treatment, typically she uses pulsed dye laser, intense pulsed light, or broadband light therapy to treat erythematous/early scars; nonablative fractional lasers to treat atrophic scars, and the thulium or 1,470-nm laser to treat hyperpigmented scars. The “main course” device in her practice is an ablative fractional erbium or CO2 laser.
“Once I treat the scar three to five times, I might switch to a nonablative laser, but I’m really an ablative fractional user,” Dr. Waibel said. “Dessert” can be whatever adjunctive therapies you need, she continued. This may include triamcinolone acetonide, 5-fluorouracil, poly-l-lactic acid, hyaluronidase, Z-plasty, punch biopsies, shave biopsies, compression, chemical reconstruction of skin scars (CROSS), and subcision.
For erythematous surgical and trauma scars, she uses a combination of pulsed dye laser and ablative fractional laser. “Same day, same treatment; one after each other,” she said. She favors using intense pulsed light for donor sites because it has filters that address both melanin and hemosiderin, superiority for scar erythema, and deeper penetration with greater speed to treat large surface areas.
One recent advance in the vascular arena is the new 595-nm pulsed dye laser by Candela, known as the VBeam Prima. It features increased energy, a 15-nm spot size, a zoom hand piece, once-a-day calibration, and contact cooling, which may be better for pigmented and possibly microvascular structures. The device is cleared for treating conditions like rosacea, acne, spider veins, port-wine stains, wrinkles, warts and stretch marks, as well as photoaging and benign pigmented lesions.
Dr. Waibel’s go-to device for treating a hypertrophic, hyperpigmented surgical scar is a 1927-nm or 1470-nm nonablative fractional laser, followed by a fractional ablative laser and injection of 1-2 ccs of 5-fluorouracil only to elevated areas. Hypopigmented scars are “by far the toughest to treat,” she said. However, she has a formula for these, too, and recently conducted a trial comparing the efficacy of nonablative fractional laser, ablative fractional laser, and ablative fractional laser followed by laser-assisted delivery of bimatoprost (Latisse) to treat hypopigmentation.
Surgical scars get better on their own in many cases, but sometimes early intervention is warranted. “Most surgeons will tell patients, ‘Wait a year. What you have [in terms of scar formation] is what you have,’” Dr. Waibel said. “If a surgical scar becomes hypertrophic, it does so within a month of surgery. I don’t prophylactically treat surgical scars unless the patient has had multiple surgeries in the same location with trouble healing. But if it’s been 6 months to a year, or if the patient is developing hypertrophic scars, then I will treat.”
Acne scars are challenging, because patients want to look good right away. “With deep scars, it takes several treatments to see good improvements,” she said. “I tell all my acne scar patients it takes a year [to get good results].”
Most burn patients require three to six treatment sessions, “but sometimes you get remarkable improvement sooner,” she said. “That’s due to the patient’s healing.” She and her associates recently completed an unpublished study that examined early intervention of fractional ablative laser versus control in 20 subjects with acute burn injuries who ranged in age from 18 to 80 years. The subjects underwent treatment with an ablative fractional CO2 laser within 3 months of sustaining the burn injury, leaving an untreated control area for comparison. According to Dr. Waibel, 100% of the blinded physician evaluators graded the laser-treated area correctly, compared with the control area. In addition, a significant improvement in all points of the Manchester Scar Scale was observed in the laser-treated area. “The earlier you treat burn and trauma patients, the easier it is to get them back to normal,” she said.
Dr. Waibel disclosed that she has conducted clinical research for Aquavit, Cytrellis, Lumenis, Lutronic, Michelson Diagnostics, RegenX, Sciton, Sebacia, and Syneron/Candela. She is also a consultant for RegenX, Strata, and Syneron/Candela and is a member of the advisory board for Dominion Technologies, Sciton, and Sebacia.
SAN DIEGO – .
“I tell patients it’s like boiling water in a tea kettle and watching the vapor form,” Dr. Waibel, a dermatologist with the Miami Dermatology and Laser Institute, said at the annual Masters of Aesthetics Symposium. “You literally ‘steam off’ their bad scar and the human body will heal that wound to almost normal skin. It’s the closest thing we have to a magic wand.”
In the not-too-distant past, dermatologists “were treating scars just to make them look better,” she said. However, thanks to groundbreaking work by clinicians at Naval Medical Center San Diego, the use of ablative fractional lasers to treat scars was found to improve range of motion in patients, as well as their pain and pruritus. “It represents a major innovation that heals in ways not previously possible,” said Dr. Waibel, who is also chief of dermatology at Baptist Hospital in Miami. “We’re not just healing the scar; we’re healing the skin back to its physiological normal place. A lot of these patients suffer quite a bit.”
Dr. Waibel likened her scar treatment approach to a three-course meal. Lesion color drives her choice of what device to use as an “appetizer” treatment. Most scars are either red (erythematous), brown (hyperpigmented), or white (hypopigmented). Though every scar is unique and individually evaluated for treatment, typically she uses pulsed dye laser, intense pulsed light, or broadband light therapy to treat erythematous/early scars; nonablative fractional lasers to treat atrophic scars, and the thulium or 1,470-nm laser to treat hyperpigmented scars. The “main course” device in her practice is an ablative fractional erbium or CO2 laser.
“Once I treat the scar three to five times, I might switch to a nonablative laser, but I’m really an ablative fractional user,” Dr. Waibel said. “Dessert” can be whatever adjunctive therapies you need, she continued. This may include triamcinolone acetonide, 5-fluorouracil, poly-l-lactic acid, hyaluronidase, Z-plasty, punch biopsies, shave biopsies, compression, chemical reconstruction of skin scars (CROSS), and subcision.
For erythematous surgical and trauma scars, she uses a combination of pulsed dye laser and ablative fractional laser. “Same day, same treatment; one after each other,” she said. She favors using intense pulsed light for donor sites because it has filters that address both melanin and hemosiderin, superiority for scar erythema, and deeper penetration with greater speed to treat large surface areas.
One recent advance in the vascular arena is the new 595-nm pulsed dye laser by Candela, known as the VBeam Prima. It features increased energy, a 15-nm spot size, a zoom hand piece, once-a-day calibration, and contact cooling, which may be better for pigmented and possibly microvascular structures. The device is cleared for treating conditions like rosacea, acne, spider veins, port-wine stains, wrinkles, warts and stretch marks, as well as photoaging and benign pigmented lesions.
Dr. Waibel’s go-to device for treating a hypertrophic, hyperpigmented surgical scar is a 1927-nm or 1470-nm nonablative fractional laser, followed by a fractional ablative laser and injection of 1-2 ccs of 5-fluorouracil only to elevated areas. Hypopigmented scars are “by far the toughest to treat,” she said. However, she has a formula for these, too, and recently conducted a trial comparing the efficacy of nonablative fractional laser, ablative fractional laser, and ablative fractional laser followed by laser-assisted delivery of bimatoprost (Latisse) to treat hypopigmentation.
Surgical scars get better on their own in many cases, but sometimes early intervention is warranted. “Most surgeons will tell patients, ‘Wait a year. What you have [in terms of scar formation] is what you have,’” Dr. Waibel said. “If a surgical scar becomes hypertrophic, it does so within a month of surgery. I don’t prophylactically treat surgical scars unless the patient has had multiple surgeries in the same location with trouble healing. But if it’s been 6 months to a year, or if the patient is developing hypertrophic scars, then I will treat.”
Acne scars are challenging, because patients want to look good right away. “With deep scars, it takes several treatments to see good improvements,” she said. “I tell all my acne scar patients it takes a year [to get good results].”
Most burn patients require three to six treatment sessions, “but sometimes you get remarkable improvement sooner,” she said. “That’s due to the patient’s healing.” She and her associates recently completed an unpublished study that examined early intervention of fractional ablative laser versus control in 20 subjects with acute burn injuries who ranged in age from 18 to 80 years. The subjects underwent treatment with an ablative fractional CO2 laser within 3 months of sustaining the burn injury, leaving an untreated control area for comparison. According to Dr. Waibel, 100% of the blinded physician evaluators graded the laser-treated area correctly, compared with the control area. In addition, a significant improvement in all points of the Manchester Scar Scale was observed in the laser-treated area. “The earlier you treat burn and trauma patients, the easier it is to get them back to normal,” she said.
Dr. Waibel disclosed that she has conducted clinical research for Aquavit, Cytrellis, Lumenis, Lutronic, Michelson Diagnostics, RegenX, Sciton, Sebacia, and Syneron/Candela. She is also a consultant for RegenX, Strata, and Syneron/Candela and is a member of the advisory board for Dominion Technologies, Sciton, and Sebacia.
REPORTING FROM MOAS 2018
Laser treatment tips for pigmented lesions
SAN DIEGO –
Victor Ross, MD, turns to the Q-switched alexandrite laser as his device of choice for most pigmented lesions. “I also use the Q-switched 1,064 nm Nd:YAG and sometimes use the Q-switched 532 nm Nd:YAG, particularly for lighter-skinned patients with lighter lesions,” he said at the annual Masters of Aesthetics Symposium.
Compared with long-pulsed devices, the Q-switched 532 nm neodymium:YAG laser is better for one-time pigment reduction and better for treating lighter pigmented spots, yet it’s associated with a higher risk of postinflammatory hyperpigmentation and short-term crusting. “The Q-switched 532 nm Nd:YAG laser will even treat very tight lentigines, but vascular effects tend to cause an immediate bright red color and more postinflammatory hyperpigmentation,” said Dr. Ross, director of laser and cosmetic dermatology at the Scripps Clinic in San Diego. He cautioned that the Q-switched 532 nm Nd:YAG laser may cause prolonged redness on the legs and arms of some patients. “This laser is best reserved for lighter skinned patients with very light lentigines – the brisk purpura can prove distasteful short term for cosmetic patients,” he said. “For darker lentigines, I prefer the IPL [intense pulse light], KTP [potassium titanyl phosphate] laser, or Q-switched alexandrite lasers.”
Meanwhile, treating pigmented lesions treated with long-pulse IPL, KTP, and pulsed dye lasers show less risk of postinflammatory hyperpigmentation and better coverage rates. However, they are sensitive to background color and are less likely to achieve complete one-time removal. The first treatment works the best because the “low hanging fruit” (darker lesions) will do well, he said.
For clinicians looking to improve their skills in treating pigmented lesions with lasers, Dr. Ross recommended using a skin meter such as Cynosure’s Skintel Melanin Reader, which measures the real-time pigment of skin. “You measure the pigment, and it gives you a reading,” he said. “It gives you a recommended setting based on the hand piece and the pulse duration.”
Melasma remains a difficult condition to treat with laser and light. In fact, Dr. Ross joked that he wouldn’t mind if the words “He cured melasma” graced his tombstone one day. “I have been treating melasma patients for 29 years now, and I’m not closer to a cure than when I started out,” he said. “I’ve tried lots of things. In my defense, I’ve made more people better than worse.”
His approach to treating melasma is to begin with a KTP laser or a gentle IPL if discrete lesions or telangiectasia are present. Next, he applies hydroquinone followed by a series of treatment sessions with the Q-switched Nd:YAG laser or a conservative fractional laser. “This tends to induce remission, but is associated with a high rate of relapse,” he said.
Dr. Ross disclosed having research and financial ties to numerous pharmaceutical and device companies.
SAN DIEGO –
Victor Ross, MD, turns to the Q-switched alexandrite laser as his device of choice for most pigmented lesions. “I also use the Q-switched 1,064 nm Nd:YAG and sometimes use the Q-switched 532 nm Nd:YAG, particularly for lighter-skinned patients with lighter lesions,” he said at the annual Masters of Aesthetics Symposium.
Compared with long-pulsed devices, the Q-switched 532 nm neodymium:YAG laser is better for one-time pigment reduction and better for treating lighter pigmented spots, yet it’s associated with a higher risk of postinflammatory hyperpigmentation and short-term crusting. “The Q-switched 532 nm Nd:YAG laser will even treat very tight lentigines, but vascular effects tend to cause an immediate bright red color and more postinflammatory hyperpigmentation,” said Dr. Ross, director of laser and cosmetic dermatology at the Scripps Clinic in San Diego. He cautioned that the Q-switched 532 nm Nd:YAG laser may cause prolonged redness on the legs and arms of some patients. “This laser is best reserved for lighter skinned patients with very light lentigines – the brisk purpura can prove distasteful short term for cosmetic patients,” he said. “For darker lentigines, I prefer the IPL [intense pulse light], KTP [potassium titanyl phosphate] laser, or Q-switched alexandrite lasers.”
Meanwhile, treating pigmented lesions treated with long-pulse IPL, KTP, and pulsed dye lasers show less risk of postinflammatory hyperpigmentation and better coverage rates. However, they are sensitive to background color and are less likely to achieve complete one-time removal. The first treatment works the best because the “low hanging fruit” (darker lesions) will do well, he said.
For clinicians looking to improve their skills in treating pigmented lesions with lasers, Dr. Ross recommended using a skin meter such as Cynosure’s Skintel Melanin Reader, which measures the real-time pigment of skin. “You measure the pigment, and it gives you a reading,” he said. “It gives you a recommended setting based on the hand piece and the pulse duration.”
Melasma remains a difficult condition to treat with laser and light. In fact, Dr. Ross joked that he wouldn’t mind if the words “He cured melasma” graced his tombstone one day. “I have been treating melasma patients for 29 years now, and I’m not closer to a cure than when I started out,” he said. “I’ve tried lots of things. In my defense, I’ve made more people better than worse.”
His approach to treating melasma is to begin with a KTP laser or a gentle IPL if discrete lesions or telangiectasia are present. Next, he applies hydroquinone followed by a series of treatment sessions with the Q-switched Nd:YAG laser or a conservative fractional laser. “This tends to induce remission, but is associated with a high rate of relapse,” he said.
Dr. Ross disclosed having research and financial ties to numerous pharmaceutical and device companies.
SAN DIEGO –
Victor Ross, MD, turns to the Q-switched alexandrite laser as his device of choice for most pigmented lesions. “I also use the Q-switched 1,064 nm Nd:YAG and sometimes use the Q-switched 532 nm Nd:YAG, particularly for lighter-skinned patients with lighter lesions,” he said at the annual Masters of Aesthetics Symposium.
Compared with long-pulsed devices, the Q-switched 532 nm neodymium:YAG laser is better for one-time pigment reduction and better for treating lighter pigmented spots, yet it’s associated with a higher risk of postinflammatory hyperpigmentation and short-term crusting. “The Q-switched 532 nm Nd:YAG laser will even treat very tight lentigines, but vascular effects tend to cause an immediate bright red color and more postinflammatory hyperpigmentation,” said Dr. Ross, director of laser and cosmetic dermatology at the Scripps Clinic in San Diego. He cautioned that the Q-switched 532 nm Nd:YAG laser may cause prolonged redness on the legs and arms of some patients. “This laser is best reserved for lighter skinned patients with very light lentigines – the brisk purpura can prove distasteful short term for cosmetic patients,” he said. “For darker lentigines, I prefer the IPL [intense pulse light], KTP [potassium titanyl phosphate] laser, or Q-switched alexandrite lasers.”
Meanwhile, treating pigmented lesions treated with long-pulse IPL, KTP, and pulsed dye lasers show less risk of postinflammatory hyperpigmentation and better coverage rates. However, they are sensitive to background color and are less likely to achieve complete one-time removal. The first treatment works the best because the “low hanging fruit” (darker lesions) will do well, he said.
For clinicians looking to improve their skills in treating pigmented lesions with lasers, Dr. Ross recommended using a skin meter such as Cynosure’s Skintel Melanin Reader, which measures the real-time pigment of skin. “You measure the pigment, and it gives you a reading,” he said. “It gives you a recommended setting based on the hand piece and the pulse duration.”
Melasma remains a difficult condition to treat with laser and light. In fact, Dr. Ross joked that he wouldn’t mind if the words “He cured melasma” graced his tombstone one day. “I have been treating melasma patients for 29 years now, and I’m not closer to a cure than when I started out,” he said. “I’ve tried lots of things. In my defense, I’ve made more people better than worse.”
His approach to treating melasma is to begin with a KTP laser or a gentle IPL if discrete lesions or telangiectasia are present. Next, he applies hydroquinone followed by a series of treatment sessions with the Q-switched Nd:YAG laser or a conservative fractional laser. “This tends to induce remission, but is associated with a high rate of relapse,” he said.
Dr. Ross disclosed having research and financial ties to numerous pharmaceutical and device companies.
EXPERT ANALYSIS FROM MOAS 2018
When treating the lower face and neck, ‘don’t forget the platysma muscle’
SAN DIEGO – Of all the data points featured in a 2017 survey on cosmetic dermatologic procedures, one stands out to Jean Carruthers, MD: Among the 7,322 consumers surveyed, about 70% cited the lower face and submental contour as a significant cosmetic and social concern.
“That is quite a key statistic,” she said at the annual Masters of Aesthetics Symposium. The Consumer Survey on Cosmetic Dermatologic Procedures was conducted by the American Society for Dermatologic Surgery.
Dr. Carruthers, who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox), said that the world’s great sculptors “think that there is a difference between the classical faces of males and females, and we all know instinctually what those changes are, with a square face and larger jawline in males and a smooth oval, heart-shaped face in women,” she said.
“But what about the neck?” She cited an article by Greg J. Goodman, MD, and colleagues, which defined an ideal neck as the distinct inferior mandibular border from mentum to angle with no jowl overhang (Dermatol Surg 2016;42:S260-2). It includes subhyoid depression, which visually enhances the impression that the neck is thin and long; visible thyroid cartilage bulge; a visible anterior border of the sternocleidomastoid muscle, distinct in its entire course from the mastoid to the sternum; and a cervicomental angle between 105 and 120 degrees. An angle greater than 120 degrees appears as a double chin or heavy neck, according to the authors.
In the past, clinicians used to think of the lower face and neck as two separate cosmetic units, but now they are considered one cosmetic unit, said Dr. Carruthers, of the University of British Columbia, Vancouver. “Don’t forget the platysma muscle,” she added. “The platysma is a lower facial muscle of expression and it affects all the other muscles. It interdigitates with the depressor anguli oris, with orbicularis oris, and depressor labii inferioris muscles, and it goes backwards into the masseter muscle.”
She and two Brazilian investigators published a retrospective analysis of 161 patients treated by a Botox injection pattern encompassing the facial platysma components, aiming to block the lower face as a whole complex (Dermatol Surg. 2017;43[8]:1042-9). According to the article, results included “frontal and lateral enhancement of lower facial contour, relaxation of high horizontal lines located just below the lateral mandibular border, and lower deep vertical smile lines present lateral to the oral commissures and melomental folds.”
Fillers and tightening the face and neck envelope without surgery takes maintenance, Dr. Carruthers said. She also noted that deoxycholic acid works on jowls as well as submental fat. Noninvasive combinations for lower face and neck include neuromodulators and deep and superficial fillers, cryolipolysis and deoxycholic acid, energy-based devices, and microneedling. “I think that these are fantastic combinations, and they don’t have to all be done at the same time on the same day,” Dr. Carruthers said. “I’m very impressed with cryolipolysis as the unheralded skin tightener. I looked at our first 464 patients and saw tremendous skin tightening.”
Of all the injectable products on the market, she said that neuromodulators “have set a new gold standard for all aesthetic treatments. It’s the most powerful primary aesthetic modulator and enhances the result of everything else that you do.”
Dr. Carruthers disclosed that she is a consultant to and has received research support from Allergan, Alphaeon, Bonti, Merz, Revance, and Zeltiq.
SAN DIEGO – Of all the data points featured in a 2017 survey on cosmetic dermatologic procedures, one stands out to Jean Carruthers, MD: Among the 7,322 consumers surveyed, about 70% cited the lower face and submental contour as a significant cosmetic and social concern.
“That is quite a key statistic,” she said at the annual Masters of Aesthetics Symposium. The Consumer Survey on Cosmetic Dermatologic Procedures was conducted by the American Society for Dermatologic Surgery.
Dr. Carruthers, who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox), said that the world’s great sculptors “think that there is a difference between the classical faces of males and females, and we all know instinctually what those changes are, with a square face and larger jawline in males and a smooth oval, heart-shaped face in women,” she said.
“But what about the neck?” She cited an article by Greg J. Goodman, MD, and colleagues, which defined an ideal neck as the distinct inferior mandibular border from mentum to angle with no jowl overhang (Dermatol Surg 2016;42:S260-2). It includes subhyoid depression, which visually enhances the impression that the neck is thin and long; visible thyroid cartilage bulge; a visible anterior border of the sternocleidomastoid muscle, distinct in its entire course from the mastoid to the sternum; and a cervicomental angle between 105 and 120 degrees. An angle greater than 120 degrees appears as a double chin or heavy neck, according to the authors.
In the past, clinicians used to think of the lower face and neck as two separate cosmetic units, but now they are considered one cosmetic unit, said Dr. Carruthers, of the University of British Columbia, Vancouver. “Don’t forget the platysma muscle,” she added. “The platysma is a lower facial muscle of expression and it affects all the other muscles. It interdigitates with the depressor anguli oris, with orbicularis oris, and depressor labii inferioris muscles, and it goes backwards into the masseter muscle.”
She and two Brazilian investigators published a retrospective analysis of 161 patients treated by a Botox injection pattern encompassing the facial platysma components, aiming to block the lower face as a whole complex (Dermatol Surg. 2017;43[8]:1042-9). According to the article, results included “frontal and lateral enhancement of lower facial contour, relaxation of high horizontal lines located just below the lateral mandibular border, and lower deep vertical smile lines present lateral to the oral commissures and melomental folds.”
Fillers and tightening the face and neck envelope without surgery takes maintenance, Dr. Carruthers said. She also noted that deoxycholic acid works on jowls as well as submental fat. Noninvasive combinations for lower face and neck include neuromodulators and deep and superficial fillers, cryolipolysis and deoxycholic acid, energy-based devices, and microneedling. “I think that these are fantastic combinations, and they don’t have to all be done at the same time on the same day,” Dr. Carruthers said. “I’m very impressed with cryolipolysis as the unheralded skin tightener. I looked at our first 464 patients and saw tremendous skin tightening.”
Of all the injectable products on the market, she said that neuromodulators “have set a new gold standard for all aesthetic treatments. It’s the most powerful primary aesthetic modulator and enhances the result of everything else that you do.”
Dr. Carruthers disclosed that she is a consultant to and has received research support from Allergan, Alphaeon, Bonti, Merz, Revance, and Zeltiq.
SAN DIEGO – Of all the data points featured in a 2017 survey on cosmetic dermatologic procedures, one stands out to Jean Carruthers, MD: Among the 7,322 consumers surveyed, about 70% cited the lower face and submental contour as a significant cosmetic and social concern.
“That is quite a key statistic,” she said at the annual Masters of Aesthetics Symposium. The Consumer Survey on Cosmetic Dermatologic Procedures was conducted by the American Society for Dermatologic Surgery.
Dr. Carruthers, who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox), said that the world’s great sculptors “think that there is a difference between the classical faces of males and females, and we all know instinctually what those changes are, with a square face and larger jawline in males and a smooth oval, heart-shaped face in women,” she said.
“But what about the neck?” She cited an article by Greg J. Goodman, MD, and colleagues, which defined an ideal neck as the distinct inferior mandibular border from mentum to angle with no jowl overhang (Dermatol Surg 2016;42:S260-2). It includes subhyoid depression, which visually enhances the impression that the neck is thin and long; visible thyroid cartilage bulge; a visible anterior border of the sternocleidomastoid muscle, distinct in its entire course from the mastoid to the sternum; and a cervicomental angle between 105 and 120 degrees. An angle greater than 120 degrees appears as a double chin or heavy neck, according to the authors.
In the past, clinicians used to think of the lower face and neck as two separate cosmetic units, but now they are considered one cosmetic unit, said Dr. Carruthers, of the University of British Columbia, Vancouver. “Don’t forget the platysma muscle,” she added. “The platysma is a lower facial muscle of expression and it affects all the other muscles. It interdigitates with the depressor anguli oris, with orbicularis oris, and depressor labii inferioris muscles, and it goes backwards into the masseter muscle.”
She and two Brazilian investigators published a retrospective analysis of 161 patients treated by a Botox injection pattern encompassing the facial platysma components, aiming to block the lower face as a whole complex (Dermatol Surg. 2017;43[8]:1042-9). According to the article, results included “frontal and lateral enhancement of lower facial contour, relaxation of high horizontal lines located just below the lateral mandibular border, and lower deep vertical smile lines present lateral to the oral commissures and melomental folds.”
Fillers and tightening the face and neck envelope without surgery takes maintenance, Dr. Carruthers said. She also noted that deoxycholic acid works on jowls as well as submental fat. Noninvasive combinations for lower face and neck include neuromodulators and deep and superficial fillers, cryolipolysis and deoxycholic acid, energy-based devices, and microneedling. “I think that these are fantastic combinations, and they don’t have to all be done at the same time on the same day,” Dr. Carruthers said. “I’m very impressed with cryolipolysis as the unheralded skin tightener. I looked at our first 464 patients and saw tremendous skin tightening.”
Of all the injectable products on the market, she said that neuromodulators “have set a new gold standard for all aesthetic treatments. It’s the most powerful primary aesthetic modulator and enhances the result of everything else that you do.”
Dr. Carruthers disclosed that she is a consultant to and has received research support from Allergan, Alphaeon, Bonti, Merz, Revance, and Zeltiq.
AT MOAS 2018
Tribulus terrestris
A member of the Zygophyllaceae family, Tribulus terrestris, also known as Gokshura, Gokharu, or puncture vine, is an annual herb; its aerial parts, roots, and fruits have been used in traditional medicine for anti-inflammatory, diuretic, tonic, antimicrobial, and aphrodisiac purposes for thousands of years in China, India, Pakistan, and Sudan.1-3 In modern times, the health benefits of T. terrestris have been attributed to the constituent saponins, flavonoids, alkaloids, lignins, amides, and glycosides that have been isolated and found as bioactive compounds in the plant.2-4
In an ethnobotanical survey of medicinal plants used in Nepal that was conducted in 2010 and 2011, Singh et al. found that T. terrestris was one of the 66 plant species important in the region. They also reported that it is one of the threatened species requiring conservation efforts.5 Although T. terrestris has long had a reputation for aphrodisiac qualities, critical reviews of the literature have undermined this historical reputation.1,6 Nevertheless, the botanical agent is used most often to treat infertility and loss of libido.4 More germane to the dermatologic realm, T. terrestris is thought to exhibit antioxidant, anticarcinogenic, and immunomodulatory potential, among other health benefits.4
Skin lightening activity
In a study published in 2002, Deng et al. evaluated the effects of a decoction of T. terrestris on tyrosinase activity and melanogenesis on cultured human melanocytes. They found that the amount of melanin increased when the decoction was administered in higher concentrations (optimally 1.5 mg/mL) but the effects were reversed at lower concentrations (0.5 mg/mL). Similarly, tyrosinase activity was facilitated by high concentrations of the decoction (optimally 100 mg/mL) and hindered at low concentrations (10 mg/mL). The investigators concluded that T. terrestris showed intriguing potential for use as a skin lightening agent that warranted further study.7
A mouse study performed by Yang et al. in 2006 revealed that T. terrestris extract administered orally to C57BL/6J mice resulted in a significantly higher expression of melanocyte-stimulating hormone in the hair follicles of treated mice (75%), compared with that in the control group (18.75%). The researchers concluded that T. terrestris galvanizes tyrosinase activity and fosters melanocyte increase, melanin production, and the epidermal movement of dormant melanocytes.8
Anticancer activity
Kumar et al. showed in 2006 that the aqueous extracts of T. terrestris roots and fruits displayed chemopreventive activity in male Swiss albino mice. Specifically, oral administration of T. terrestris before, during, and after papillomagenesis induced by 7, 12-Dimethylbenz(a)anthracene (DMBA) resulted in significant decreases in tumor incidence, tumor burden, and cumulative number of papillomas, as well as a significant increase in average latent period as compared with the control group treated with DMBA and croton oil.9
The next year, Neychev et al. published a study on the effects of T. terrestris–derived saponins on normal human skin fibroblasts with a focus on anticancer activities. The researchers noted that the botanical engendered a dose-dependent reduction in [3H]-thymidine incorporation into the DNA of treated fibroblasts, which was not the case for untreated controls. This and several other metrics suggested that T. terrestris poses much less toxicity to normal human skin fibroblasts than multiple previously explored cancer lines by virtue of the up-regulation and down-regulation of polyamine homeostasis, hampering proliferation, and apoptosis induction.10
In 2012, Sisto et al. investigated the effects of T. terrestris–derived saponins on apoptosis in normal human keratinocytes exposed to UVB, as well as their antitumoral activity. They found that the saponins blunted UVB-induced apoptosis in normal human keratinocytes and did not render malignant keratinocytes more resistant to UVB in squamous cell carcinomas. The investigators concluded that their findings suggest a preventive capacity of T. terrestris against UVB-induced damage and carcinogenesis.11
Conclusion
As is the case with numerous botanical agents used for health purposes, where there’s smoke, there’s fire. That is, T. terrestris has warranted investigation for its applicability in the modern health armamentarium. I hope that conservation efforts for this plant will prevail, as much more research is necessary to determine whether it can become useful in the dermatologic realm.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), as well as a New York Times Best Sellers book for consumers,“The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems.
References
1. Qureshi A et al. J Diet Suppl. 2014 Mar;11(1):64-79.
2. Zhu W et al. Chem Cent J. 2017 Jul 11;11(1):60.
3. Chhatre S et al. Pharmacogn Rev. 2014 Jan;8(15):45-51
4. Shahid M et al. J Biol Regul Homeost Agents. 2016 Jul-Sep;30(3):785-8.
5. Singh AG et al. J Ethnobiol Ethnomed. 2012 May 16;8:19.
6. Neychev V et al. J Ethnopharmacol. 2016 Feb 17;179:345-55.
7. Deng Y et al. Di Yi Jun Yi Da Xue Xue Bao. 2002 Nov;22(11):1017-9.
8. Yang L et al. Nan Fang Yi Ke Da Xue Xue Bao. 2006 Dec;26(12):1777-9.
9. Kumar M et al. Asian Pac J Cancer Prev. 2006 Apr-Jun;7(2):289-94.
10. Neychev VK et al. Exp Biol Med (Maywood). 2007 Jan;232(1):126-33.
11. Sisto M et al. J Photochem Photobiol B. 2012 Dec 5;117:193-201.
A member of the Zygophyllaceae family, Tribulus terrestris, also known as Gokshura, Gokharu, or puncture vine, is an annual herb; its aerial parts, roots, and fruits have been used in traditional medicine for anti-inflammatory, diuretic, tonic, antimicrobial, and aphrodisiac purposes for thousands of years in China, India, Pakistan, and Sudan.1-3 In modern times, the health benefits of T. terrestris have been attributed to the constituent saponins, flavonoids, alkaloids, lignins, amides, and glycosides that have been isolated and found as bioactive compounds in the plant.2-4
In an ethnobotanical survey of medicinal plants used in Nepal that was conducted in 2010 and 2011, Singh et al. found that T. terrestris was one of the 66 plant species important in the region. They also reported that it is one of the threatened species requiring conservation efforts.5 Although T. terrestris has long had a reputation for aphrodisiac qualities, critical reviews of the literature have undermined this historical reputation.1,6 Nevertheless, the botanical agent is used most often to treat infertility and loss of libido.4 More germane to the dermatologic realm, T. terrestris is thought to exhibit antioxidant, anticarcinogenic, and immunomodulatory potential, among other health benefits.4
Skin lightening activity
In a study published in 2002, Deng et al. evaluated the effects of a decoction of T. terrestris on tyrosinase activity and melanogenesis on cultured human melanocytes. They found that the amount of melanin increased when the decoction was administered in higher concentrations (optimally 1.5 mg/mL) but the effects were reversed at lower concentrations (0.5 mg/mL). Similarly, tyrosinase activity was facilitated by high concentrations of the decoction (optimally 100 mg/mL) and hindered at low concentrations (10 mg/mL). The investigators concluded that T. terrestris showed intriguing potential for use as a skin lightening agent that warranted further study.7
A mouse study performed by Yang et al. in 2006 revealed that T. terrestris extract administered orally to C57BL/6J mice resulted in a significantly higher expression of melanocyte-stimulating hormone in the hair follicles of treated mice (75%), compared with that in the control group (18.75%). The researchers concluded that T. terrestris galvanizes tyrosinase activity and fosters melanocyte increase, melanin production, and the epidermal movement of dormant melanocytes.8
Anticancer activity
Kumar et al. showed in 2006 that the aqueous extracts of T. terrestris roots and fruits displayed chemopreventive activity in male Swiss albino mice. Specifically, oral administration of T. terrestris before, during, and after papillomagenesis induced by 7, 12-Dimethylbenz(a)anthracene (DMBA) resulted in significant decreases in tumor incidence, tumor burden, and cumulative number of papillomas, as well as a significant increase in average latent period as compared with the control group treated with DMBA and croton oil.9
The next year, Neychev et al. published a study on the effects of T. terrestris–derived saponins on normal human skin fibroblasts with a focus on anticancer activities. The researchers noted that the botanical engendered a dose-dependent reduction in [3H]-thymidine incorporation into the DNA of treated fibroblasts, which was not the case for untreated controls. This and several other metrics suggested that T. terrestris poses much less toxicity to normal human skin fibroblasts than multiple previously explored cancer lines by virtue of the up-regulation and down-regulation of polyamine homeostasis, hampering proliferation, and apoptosis induction.10
In 2012, Sisto et al. investigated the effects of T. terrestris–derived saponins on apoptosis in normal human keratinocytes exposed to UVB, as well as their antitumoral activity. They found that the saponins blunted UVB-induced apoptosis in normal human keratinocytes and did not render malignant keratinocytes more resistant to UVB in squamous cell carcinomas. The investigators concluded that their findings suggest a preventive capacity of T. terrestris against UVB-induced damage and carcinogenesis.11
Conclusion
As is the case with numerous botanical agents used for health purposes, where there’s smoke, there’s fire. That is, T. terrestris has warranted investigation for its applicability in the modern health armamentarium. I hope that conservation efforts for this plant will prevail, as much more research is necessary to determine whether it can become useful in the dermatologic realm.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), as well as a New York Times Best Sellers book for consumers,“The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems.
References
1. Qureshi A et al. J Diet Suppl. 2014 Mar;11(1):64-79.
2. Zhu W et al. Chem Cent J. 2017 Jul 11;11(1):60.
3. Chhatre S et al. Pharmacogn Rev. 2014 Jan;8(15):45-51
4. Shahid M et al. J Biol Regul Homeost Agents. 2016 Jul-Sep;30(3):785-8.
5. Singh AG et al. J Ethnobiol Ethnomed. 2012 May 16;8:19.
6. Neychev V et al. J Ethnopharmacol. 2016 Feb 17;179:345-55.
7. Deng Y et al. Di Yi Jun Yi Da Xue Xue Bao. 2002 Nov;22(11):1017-9.
8. Yang L et al. Nan Fang Yi Ke Da Xue Xue Bao. 2006 Dec;26(12):1777-9.
9. Kumar M et al. Asian Pac J Cancer Prev. 2006 Apr-Jun;7(2):289-94.
10. Neychev VK et al. Exp Biol Med (Maywood). 2007 Jan;232(1):126-33.
11. Sisto M et al. J Photochem Photobiol B. 2012 Dec 5;117:193-201.
A member of the Zygophyllaceae family, Tribulus terrestris, also known as Gokshura, Gokharu, or puncture vine, is an annual herb; its aerial parts, roots, and fruits have been used in traditional medicine for anti-inflammatory, diuretic, tonic, antimicrobial, and aphrodisiac purposes for thousands of years in China, India, Pakistan, and Sudan.1-3 In modern times, the health benefits of T. terrestris have been attributed to the constituent saponins, flavonoids, alkaloids, lignins, amides, and glycosides that have been isolated and found as bioactive compounds in the plant.2-4
In an ethnobotanical survey of medicinal plants used in Nepal that was conducted in 2010 and 2011, Singh et al. found that T. terrestris was one of the 66 plant species important in the region. They also reported that it is one of the threatened species requiring conservation efforts.5 Although T. terrestris has long had a reputation for aphrodisiac qualities, critical reviews of the literature have undermined this historical reputation.1,6 Nevertheless, the botanical agent is used most often to treat infertility and loss of libido.4 More germane to the dermatologic realm, T. terrestris is thought to exhibit antioxidant, anticarcinogenic, and immunomodulatory potential, among other health benefits.4
Skin lightening activity
In a study published in 2002, Deng et al. evaluated the effects of a decoction of T. terrestris on tyrosinase activity and melanogenesis on cultured human melanocytes. They found that the amount of melanin increased when the decoction was administered in higher concentrations (optimally 1.5 mg/mL) but the effects were reversed at lower concentrations (0.5 mg/mL). Similarly, tyrosinase activity was facilitated by high concentrations of the decoction (optimally 100 mg/mL) and hindered at low concentrations (10 mg/mL). The investigators concluded that T. terrestris showed intriguing potential for use as a skin lightening agent that warranted further study.7
A mouse study performed by Yang et al. in 2006 revealed that T. terrestris extract administered orally to C57BL/6J mice resulted in a significantly higher expression of melanocyte-stimulating hormone in the hair follicles of treated mice (75%), compared with that in the control group (18.75%). The researchers concluded that T. terrestris galvanizes tyrosinase activity and fosters melanocyte increase, melanin production, and the epidermal movement of dormant melanocytes.8
Anticancer activity
Kumar et al. showed in 2006 that the aqueous extracts of T. terrestris roots and fruits displayed chemopreventive activity in male Swiss albino mice. Specifically, oral administration of T. terrestris before, during, and after papillomagenesis induced by 7, 12-Dimethylbenz(a)anthracene (DMBA) resulted in significant decreases in tumor incidence, tumor burden, and cumulative number of papillomas, as well as a significant increase in average latent period as compared with the control group treated with DMBA and croton oil.9
The next year, Neychev et al. published a study on the effects of T. terrestris–derived saponins on normal human skin fibroblasts with a focus on anticancer activities. The researchers noted that the botanical engendered a dose-dependent reduction in [3H]-thymidine incorporation into the DNA of treated fibroblasts, which was not the case for untreated controls. This and several other metrics suggested that T. terrestris poses much less toxicity to normal human skin fibroblasts than multiple previously explored cancer lines by virtue of the up-regulation and down-regulation of polyamine homeostasis, hampering proliferation, and apoptosis induction.10
In 2012, Sisto et al. investigated the effects of T. terrestris–derived saponins on apoptosis in normal human keratinocytes exposed to UVB, as well as their antitumoral activity. They found that the saponins blunted UVB-induced apoptosis in normal human keratinocytes and did not render malignant keratinocytes more resistant to UVB in squamous cell carcinomas. The investigators concluded that their findings suggest a preventive capacity of T. terrestris against UVB-induced damage and carcinogenesis.11
Conclusion
As is the case with numerous botanical agents used for health purposes, where there’s smoke, there’s fire. That is, T. terrestris has warranted investigation for its applicability in the modern health armamentarium. I hope that conservation efforts for this plant will prevail, as much more research is necessary to determine whether it can become useful in the dermatologic realm.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), as well as a New York Times Best Sellers book for consumers,“The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems.
References
1. Qureshi A et al. J Diet Suppl. 2014 Mar;11(1):64-79.
2. Zhu W et al. Chem Cent J. 2017 Jul 11;11(1):60.
3. Chhatre S et al. Pharmacogn Rev. 2014 Jan;8(15):45-51
4. Shahid M et al. J Biol Regul Homeost Agents. 2016 Jul-Sep;30(3):785-8.
5. Singh AG et al. J Ethnobiol Ethnomed. 2012 May 16;8:19.
6. Neychev V et al. J Ethnopharmacol. 2016 Feb 17;179:345-55.
7. Deng Y et al. Di Yi Jun Yi Da Xue Xue Bao. 2002 Nov;22(11):1017-9.
8. Yang L et al. Nan Fang Yi Ke Da Xue Xue Bao. 2006 Dec;26(12):1777-9.
9. Kumar M et al. Asian Pac J Cancer Prev. 2006 Apr-Jun;7(2):289-94.
10. Neychev VK et al. Exp Biol Med (Maywood). 2007 Jan;232(1):126-33.
11. Sisto M et al. J Photochem Photobiol B. 2012 Dec 5;117:193-201.
Five common pitfalls of retailing skin care
Others believe that providing patients with the correct skin care product recommendations for their skin’s needs is a crucial step to improving outcomes and educating patients.
There is a wide range of challenges related to skin care retail that many physicians face. I will be running a course on Skin Care Retail at the American Society for Dermatologic Surgery meeting in October in Scottsdale, Ariz., if you want to learn more or share your opinions. I have surveyed plastic surgeons and dermatologists via LinkedIn about what they believe are some of the biggest pitfalls to retailing skin care. Here, I will share some of their insights and suggestions for overcoming these obstacles.
1. Patients are more knowledgeable about skin care than ever before
Facing an increasing number of over-the-counter skin care products available, as well as buzzwords like “organic ingredients” and “vegan,” patients are now bombarded with information from a variety of different sources. Because of this, patients come to the doctor with preconceived ideas that can affect compliance if their specific needs and beliefs are not properly addressed.
For New York plastic surgeon Sonita M. Sadio, MD, this is one of the reasons why she chooses not to sell skin care in her office.
“My practice is highly consultative, and ongoing skin care recommendations are a significant part of what I do to optimize patient outcomes,” Dr. Sadio said. “Patients are well-educated about skin care today. They know their ingredients and insist on clean formulations, free of certain ingredients, such as ‘cruelty-free’ and ‘vegan.’ Others feel deprived if they are not using an expensive product in elegant packaging. Still, others insist on drugstore favorites or ‘eco’ offerings and have their own sense of what that means. My job is to optimize the clinical outcome while also meeting these patients needs to ensure compliance.”
Not all doctors have the time, knowledge or desire to personally design each patient’s skin care regimen. Many delegate this to the staff. However, it is impossible to ensure that your staff matches patients to the proper products unless they have had extensive training on both skin care products and how to match them to the patient’s skin issues.
2. Patients are wary when the doctors sells only one product brand
Many studies have shown that, although consumers desire a choice when making purchases, they get overwhelmed if they are presented with too many options. One study showed that it is optimal to carry at least 3 brands of products. For this reason, limiting the skin care you sell to one brand or doing your own private label is not optimal.
New York dermatologist Rebecca Tamez, MD, pointed out the same problem when selling practice-specific skin care. “At my previous job, we sold skin care products directly to patients. I had no issues selling products that were readily available in drugstores or online (such as Vanicream and EltaMD). We usually sold these around the same cost as the drugstore or Amazon. However, it was harder to sell the practice-specific skin care line. I feel patients were more wary of these products.”
3. Doctors do not want to feel like salespeople
If you have read my Dermatology News columns in the past, you may know that I think it is unethical for dermatologists to not offer specific skin care advice to their patients. If patients do not get ethical and scientific recommendations from us, they will follow the advice of a friend or salesperson or purchase based on often inflated marketing claims.
Dermatologists often tell me: “I am not a cosmetic dermatologist so I do not sell skin care.” I feel strongly that general dermatologists should be giving specific written skin care recommendations for their patients too. Acne, rosacea, melasma, eczema, psoriasis, keratosis pilaris, and many other conditions will improve faster with an efficacious skin care regimen, assuming the patient is compliant with the instructions. Retailing skin care improves compliance by eliminating a few barriers to beginning the skin care regimen. I believe that the mindset of dermatologists needs to change: It is not about selling products to patients, it is about educating them on what to use and offering the products out of convenience and the desire to improve compliance.
Meadowbrook, Pa., dermatologist Michael A. Tomeo, MD, explained an obstacle faced by many dermatologists:
“I suspect, like many of my colleagues,” said Dr. Tomeo, “that I am held back in terms of salesmanship, having been trained in the traditional way. Physicians of my generation were taught to be ethical and professional and to focus on academic and clinical excellence, and salesmanship and advertising one’s services were frowned upon. It takes time to reset one’s former proclivities. Cosmeceuticals and nutraceuticals are revolutionizing the skin care world, and as experts in all things skin, we need to be well informed and offer our patients safe, effective, and cutting-edge treatments.”
4. Providers are concerned about product costs and time constraints
Providing excellent patient care and improving outcomes is at the forefront of our business, but financial concerns and time constraints prevent some doctors from offering skin care to their patients.
Rochester Hills, Mich., plastic surgeon Richard Hainer, MD, has found that “skin care is often too complex with too many products and is not very profitable.” For those reasons, Dr. Hainer has chosen not to retail skin care in his practice.
Nampa, Idaho, dermatologist Ryan S. Owsley, MD, explained that “the required minimum purchases by some of the product lines can leave the practice with expired product if it is not selling a particular line well. Cost can also be an issue for some patients in the area we are located.”
As a burn survivor and burn surgeon, Mark McDonough, MD, from Orlando “has a long history with skin care and rejuvenation. I did have a private label skin care line, including a moisturizer, a hydroquinone product, a retinol cream, and a sunscreen,” Dr. McDonough said. “However, and regrettably, I have not kept up with marketing and promotion, with most of my energy invested in trauma and disease survivors through a book, a blog, and my platform through my website.”
Doing your own product line is costly and spending the time and resources to promote it is not always possible. Buying the minimum order of products is often expensive, and you will not be able to sell them without a proven methodology in place. New products enter the market frequently, and it is expensive to always carry the latest technologies because new minimum orders must be met with each new brand that you add.
5. Selling skin care requires ongoing education
Properly recommending and retailing skin care involves physician, staff, and patient education. Unfortunately, most practices rely on training from the cosmeceutical sales reps who obviously have a brand bias. There is minimal unbiased “brand agnostic” skin care training for dermatologists and their staff. In fact, the AAD meeting has only a few skin care lectures in the program. Plastic surgeon Gaurav Bharti, MD, of Charlotte, N.C., explained that “motivating staff to help with retail skin care can be challenging. The first step is to get the staff familiar with the products with open discussions with the representatives. The next step has been to have the staff actually use the products and believe in them. Once they believe in the product, we have used an incentivization model that’s simple, transparent, and predictable.”
We are all too busy to spend adequate time with our patients, so it is critical that our staff be able to properly recommended skin care for us. We have to ensure that our staff is taking an ethical and scientific approach to skin care retail rather than a financial one. Rigorous staff training on how to match skin care products to skin type is the key to improving outcomes with skin care recommendations.
In a similar sense, Cincinnati plastic surgeon Richard Williams, MD, commented that “aestheticians often succumb to the desires of our patients to carry too many products in inventory, for which they do not have enough knowledge of the product’s benefits. This can be a very frustrating challenge.”
Conclusion
Although there are many obstacles to retailing skin care in your medical practice, the benefits that it provides to both your patients (improved outcomes) and your practice (increased profitability) far outweigh the challenges. I solved these pitfalls in my own practice by developing a standardized staff training program and skin care diagnostic software that is now used by over 100 medical practices. If you want to start retaining skin care, my advice is develop a training plan and a methodology for the recommendation and patient education process before you spend a lot of money on the required minimum product order. Feel free to contact me for advice. Alternatively, if you already do a great job of retailing skin care and want to provide tips to include in my American Society for Dermatologic Surgery course, contact me on LinkedIn or [email protected]. You can also find blogs I have written on skin care retail advice at STSFranchise.com.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also wrote a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems.
Others believe that providing patients with the correct skin care product recommendations for their skin’s needs is a crucial step to improving outcomes and educating patients.
There is a wide range of challenges related to skin care retail that many physicians face. I will be running a course on Skin Care Retail at the American Society for Dermatologic Surgery meeting in October in Scottsdale, Ariz., if you want to learn more or share your opinions. I have surveyed plastic surgeons and dermatologists via LinkedIn about what they believe are some of the biggest pitfalls to retailing skin care. Here, I will share some of their insights and suggestions for overcoming these obstacles.
1. Patients are more knowledgeable about skin care than ever before
Facing an increasing number of over-the-counter skin care products available, as well as buzzwords like “organic ingredients” and “vegan,” patients are now bombarded with information from a variety of different sources. Because of this, patients come to the doctor with preconceived ideas that can affect compliance if their specific needs and beliefs are not properly addressed.
For New York plastic surgeon Sonita M. Sadio, MD, this is one of the reasons why she chooses not to sell skin care in her office.
“My practice is highly consultative, and ongoing skin care recommendations are a significant part of what I do to optimize patient outcomes,” Dr. Sadio said. “Patients are well-educated about skin care today. They know their ingredients and insist on clean formulations, free of certain ingredients, such as ‘cruelty-free’ and ‘vegan.’ Others feel deprived if they are not using an expensive product in elegant packaging. Still, others insist on drugstore favorites or ‘eco’ offerings and have their own sense of what that means. My job is to optimize the clinical outcome while also meeting these patients needs to ensure compliance.”
Not all doctors have the time, knowledge or desire to personally design each patient’s skin care regimen. Many delegate this to the staff. However, it is impossible to ensure that your staff matches patients to the proper products unless they have had extensive training on both skin care products and how to match them to the patient’s skin issues.
2. Patients are wary when the doctors sells only one product brand
Many studies have shown that, although consumers desire a choice when making purchases, they get overwhelmed if they are presented with too many options. One study showed that it is optimal to carry at least 3 brands of products. For this reason, limiting the skin care you sell to one brand or doing your own private label is not optimal.
New York dermatologist Rebecca Tamez, MD, pointed out the same problem when selling practice-specific skin care. “At my previous job, we sold skin care products directly to patients. I had no issues selling products that were readily available in drugstores or online (such as Vanicream and EltaMD). We usually sold these around the same cost as the drugstore or Amazon. However, it was harder to sell the practice-specific skin care line. I feel patients were more wary of these products.”
3. Doctors do not want to feel like salespeople
If you have read my Dermatology News columns in the past, you may know that I think it is unethical for dermatologists to not offer specific skin care advice to their patients. If patients do not get ethical and scientific recommendations from us, they will follow the advice of a friend or salesperson or purchase based on often inflated marketing claims.
Dermatologists often tell me: “I am not a cosmetic dermatologist so I do not sell skin care.” I feel strongly that general dermatologists should be giving specific written skin care recommendations for their patients too. Acne, rosacea, melasma, eczema, psoriasis, keratosis pilaris, and many other conditions will improve faster with an efficacious skin care regimen, assuming the patient is compliant with the instructions. Retailing skin care improves compliance by eliminating a few barriers to beginning the skin care regimen. I believe that the mindset of dermatologists needs to change: It is not about selling products to patients, it is about educating them on what to use and offering the products out of convenience and the desire to improve compliance.
Meadowbrook, Pa., dermatologist Michael A. Tomeo, MD, explained an obstacle faced by many dermatologists:
“I suspect, like many of my colleagues,” said Dr. Tomeo, “that I am held back in terms of salesmanship, having been trained in the traditional way. Physicians of my generation were taught to be ethical and professional and to focus on academic and clinical excellence, and salesmanship and advertising one’s services were frowned upon. It takes time to reset one’s former proclivities. Cosmeceuticals and nutraceuticals are revolutionizing the skin care world, and as experts in all things skin, we need to be well informed and offer our patients safe, effective, and cutting-edge treatments.”
4. Providers are concerned about product costs and time constraints
Providing excellent patient care and improving outcomes is at the forefront of our business, but financial concerns and time constraints prevent some doctors from offering skin care to their patients.
Rochester Hills, Mich., plastic surgeon Richard Hainer, MD, has found that “skin care is often too complex with too many products and is not very profitable.” For those reasons, Dr. Hainer has chosen not to retail skin care in his practice.
Nampa, Idaho, dermatologist Ryan S. Owsley, MD, explained that “the required minimum purchases by some of the product lines can leave the practice with expired product if it is not selling a particular line well. Cost can also be an issue for some patients in the area we are located.”
As a burn survivor and burn surgeon, Mark McDonough, MD, from Orlando “has a long history with skin care and rejuvenation. I did have a private label skin care line, including a moisturizer, a hydroquinone product, a retinol cream, and a sunscreen,” Dr. McDonough said. “However, and regrettably, I have not kept up with marketing and promotion, with most of my energy invested in trauma and disease survivors through a book, a blog, and my platform through my website.”
Doing your own product line is costly and spending the time and resources to promote it is not always possible. Buying the minimum order of products is often expensive, and you will not be able to sell them without a proven methodology in place. New products enter the market frequently, and it is expensive to always carry the latest technologies because new minimum orders must be met with each new brand that you add.
5. Selling skin care requires ongoing education
Properly recommending and retailing skin care involves physician, staff, and patient education. Unfortunately, most practices rely on training from the cosmeceutical sales reps who obviously have a brand bias. There is minimal unbiased “brand agnostic” skin care training for dermatologists and their staff. In fact, the AAD meeting has only a few skin care lectures in the program. Plastic surgeon Gaurav Bharti, MD, of Charlotte, N.C., explained that “motivating staff to help with retail skin care can be challenging. The first step is to get the staff familiar with the products with open discussions with the representatives. The next step has been to have the staff actually use the products and believe in them. Once they believe in the product, we have used an incentivization model that’s simple, transparent, and predictable.”
We are all too busy to spend adequate time with our patients, so it is critical that our staff be able to properly recommended skin care for us. We have to ensure that our staff is taking an ethical and scientific approach to skin care retail rather than a financial one. Rigorous staff training on how to match skin care products to skin type is the key to improving outcomes with skin care recommendations.
In a similar sense, Cincinnati plastic surgeon Richard Williams, MD, commented that “aestheticians often succumb to the desires of our patients to carry too many products in inventory, for which they do not have enough knowledge of the product’s benefits. This can be a very frustrating challenge.”
Conclusion
Although there are many obstacles to retailing skin care in your medical practice, the benefits that it provides to both your patients (improved outcomes) and your practice (increased profitability) far outweigh the challenges. I solved these pitfalls in my own practice by developing a standardized staff training program and skin care diagnostic software that is now used by over 100 medical practices. If you want to start retaining skin care, my advice is develop a training plan and a methodology for the recommendation and patient education process before you spend a lot of money on the required minimum product order. Feel free to contact me for advice. Alternatively, if you already do a great job of retailing skin care and want to provide tips to include in my American Society for Dermatologic Surgery course, contact me on LinkedIn or [email protected]. You can also find blogs I have written on skin care retail advice at STSFranchise.com.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also wrote a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems.
Others believe that providing patients with the correct skin care product recommendations for their skin’s needs is a crucial step to improving outcomes and educating patients.
There is a wide range of challenges related to skin care retail that many physicians face. I will be running a course on Skin Care Retail at the American Society for Dermatologic Surgery meeting in October in Scottsdale, Ariz., if you want to learn more or share your opinions. I have surveyed plastic surgeons and dermatologists via LinkedIn about what they believe are some of the biggest pitfalls to retailing skin care. Here, I will share some of their insights and suggestions for overcoming these obstacles.
1. Patients are more knowledgeable about skin care than ever before
Facing an increasing number of over-the-counter skin care products available, as well as buzzwords like “organic ingredients” and “vegan,” patients are now bombarded with information from a variety of different sources. Because of this, patients come to the doctor with preconceived ideas that can affect compliance if their specific needs and beliefs are not properly addressed.
For New York plastic surgeon Sonita M. Sadio, MD, this is one of the reasons why she chooses not to sell skin care in her office.
“My practice is highly consultative, and ongoing skin care recommendations are a significant part of what I do to optimize patient outcomes,” Dr. Sadio said. “Patients are well-educated about skin care today. They know their ingredients and insist on clean formulations, free of certain ingredients, such as ‘cruelty-free’ and ‘vegan.’ Others feel deprived if they are not using an expensive product in elegant packaging. Still, others insist on drugstore favorites or ‘eco’ offerings and have their own sense of what that means. My job is to optimize the clinical outcome while also meeting these patients needs to ensure compliance.”
Not all doctors have the time, knowledge or desire to personally design each patient’s skin care regimen. Many delegate this to the staff. However, it is impossible to ensure that your staff matches patients to the proper products unless they have had extensive training on both skin care products and how to match them to the patient’s skin issues.
2. Patients are wary when the doctors sells only one product brand
Many studies have shown that, although consumers desire a choice when making purchases, they get overwhelmed if they are presented with too many options. One study showed that it is optimal to carry at least 3 brands of products. For this reason, limiting the skin care you sell to one brand or doing your own private label is not optimal.
New York dermatologist Rebecca Tamez, MD, pointed out the same problem when selling practice-specific skin care. “At my previous job, we sold skin care products directly to patients. I had no issues selling products that were readily available in drugstores or online (such as Vanicream and EltaMD). We usually sold these around the same cost as the drugstore or Amazon. However, it was harder to sell the practice-specific skin care line. I feel patients were more wary of these products.”
3. Doctors do not want to feel like salespeople
If you have read my Dermatology News columns in the past, you may know that I think it is unethical for dermatologists to not offer specific skin care advice to their patients. If patients do not get ethical and scientific recommendations from us, they will follow the advice of a friend or salesperson or purchase based on often inflated marketing claims.
Dermatologists often tell me: “I am not a cosmetic dermatologist so I do not sell skin care.” I feel strongly that general dermatologists should be giving specific written skin care recommendations for their patients too. Acne, rosacea, melasma, eczema, psoriasis, keratosis pilaris, and many other conditions will improve faster with an efficacious skin care regimen, assuming the patient is compliant with the instructions. Retailing skin care improves compliance by eliminating a few barriers to beginning the skin care regimen. I believe that the mindset of dermatologists needs to change: It is not about selling products to patients, it is about educating them on what to use and offering the products out of convenience and the desire to improve compliance.
Meadowbrook, Pa., dermatologist Michael A. Tomeo, MD, explained an obstacle faced by many dermatologists:
“I suspect, like many of my colleagues,” said Dr. Tomeo, “that I am held back in terms of salesmanship, having been trained in the traditional way. Physicians of my generation were taught to be ethical and professional and to focus on academic and clinical excellence, and salesmanship and advertising one’s services were frowned upon. It takes time to reset one’s former proclivities. Cosmeceuticals and nutraceuticals are revolutionizing the skin care world, and as experts in all things skin, we need to be well informed and offer our patients safe, effective, and cutting-edge treatments.”
4. Providers are concerned about product costs and time constraints
Providing excellent patient care and improving outcomes is at the forefront of our business, but financial concerns and time constraints prevent some doctors from offering skin care to their patients.
Rochester Hills, Mich., plastic surgeon Richard Hainer, MD, has found that “skin care is often too complex with too many products and is not very profitable.” For those reasons, Dr. Hainer has chosen not to retail skin care in his practice.
Nampa, Idaho, dermatologist Ryan S. Owsley, MD, explained that “the required minimum purchases by some of the product lines can leave the practice with expired product if it is not selling a particular line well. Cost can also be an issue for some patients in the area we are located.”
As a burn survivor and burn surgeon, Mark McDonough, MD, from Orlando “has a long history with skin care and rejuvenation. I did have a private label skin care line, including a moisturizer, a hydroquinone product, a retinol cream, and a sunscreen,” Dr. McDonough said. “However, and regrettably, I have not kept up with marketing and promotion, with most of my energy invested in trauma and disease survivors through a book, a blog, and my platform through my website.”
Doing your own product line is costly and spending the time and resources to promote it is not always possible. Buying the minimum order of products is often expensive, and you will not be able to sell them without a proven methodology in place. New products enter the market frequently, and it is expensive to always carry the latest technologies because new minimum orders must be met with each new brand that you add.
5. Selling skin care requires ongoing education
Properly recommending and retailing skin care involves physician, staff, and patient education. Unfortunately, most practices rely on training from the cosmeceutical sales reps who obviously have a brand bias. There is minimal unbiased “brand agnostic” skin care training for dermatologists and their staff. In fact, the AAD meeting has only a few skin care lectures in the program. Plastic surgeon Gaurav Bharti, MD, of Charlotte, N.C., explained that “motivating staff to help with retail skin care can be challenging. The first step is to get the staff familiar with the products with open discussions with the representatives. The next step has been to have the staff actually use the products and believe in them. Once they believe in the product, we have used an incentivization model that’s simple, transparent, and predictable.”
We are all too busy to spend adequate time with our patients, so it is critical that our staff be able to properly recommended skin care for us. We have to ensure that our staff is taking an ethical and scientific approach to skin care retail rather than a financial one. Rigorous staff training on how to match skin care products to skin type is the key to improving outcomes with skin care recommendations.
In a similar sense, Cincinnati plastic surgeon Richard Williams, MD, commented that “aestheticians often succumb to the desires of our patients to carry too many products in inventory, for which they do not have enough knowledge of the product’s benefits. This can be a very frustrating challenge.”
Conclusion
Although there are many obstacles to retailing skin care in your medical practice, the benefits that it provides to both your patients (improved outcomes) and your practice (increased profitability) far outweigh the challenges. I solved these pitfalls in my own practice by developing a standardized staff training program and skin care diagnostic software that is now used by over 100 medical practices. If you want to start retaining skin care, my advice is develop a training plan and a methodology for the recommendation and patient education process before you spend a lot of money on the required minimum product order. Feel free to contact me for advice. Alternatively, if you already do a great job of retailing skin care and want to provide tips to include in my American Society for Dermatologic Surgery course, contact me on LinkedIn or [email protected]. You can also find blogs I have written on skin care retail advice at STSFranchise.com.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also wrote a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems.
Low hyaluronidase doses may be adequate for addressing filler asymmetry
, and in some cases, slightly larger doses may move things along more rapidly, according to the authors of a small split-arm clinical trial.
“These findings offer clinicians a means to modify and fine-tune filler-associated skin contour without resorting to high-dose injections that completely remove all filler from the treatment site,” wrote the authors, led by Murad Alam, MD, professor of dermatology and chief of cutaneous and aesthetic surgery in the department of dermatology, Northwestern University, Chicago. The study was published online in JAMA Dermatology.
The study, conducted during 2013-2014, analyzed the impact of various small doses of hyaluronidase on two types of fillers that had been administered into the upper inner arms of nine women (seven white, two black; mean age, 46 years). Another participant withdrew because of a fear of needles.
In one arm in each woman, researchers injected four aliquots of Juvéderm Ultra XC (0.4 mL each). Then, at 1, 2, and 3 weeks, they administered 1.5 U, 3.0 U, or 9.0 U hyaluronidase per 0.1 mL or saline control (at a constant volume of 0.1 mL) into each site. In the other arms, researchers performed the same protocol, but with Restylane-L. A 5-point scale was used to rate detectability of each site ranging from 0 (undetectable) and 1 (faintly perceptible) to 4 (“very” perceptible).
A blinded physician visually rated the effects of saline versus hyaluronidase at 4 weeks and found a significant difference between assessments of the hyaluronidase-treated sites and saline control sites at 4 weeks, favoring the hyaluronidase sites for visual detection (mean difference, 1.15; P less than .001) and palpability (mean difference, 1.22; P less than .001). Participant self-assessments at 4 weeks produced similar results for visual detection (mean difference, 0.87; P = .006) and palpability (mean difference, 1.59; P less than .001).
Similar differences favoring hyaluronidase persisted at 4 months.
The researchers also found that 9.0-U treatments of hyaluronidase led to significantly less palpability than 1.5-U treatments at 4 weeks and 4 months. The researchers noticed a larger dose-related difference for hyaluronidase for Restylane-L sites, and they noted that all the filler nodules diminished over time regardless of the study treatment.
“The clinical relevance of these findings is clear,” they concluded. “Minor filler-associated asymmetries, nodules, and textural abnormalities may be corrected safely and effectively with low-volume, low-dose hyaluronidase. Rather than dissolving all the offending filler, waiting, and then reinjecting fresh filler weeks or months later, dermatologists may precisely sculpt already injected excess filler by titration with low-volume, low-dose hyaluronidase to the desired skin contour.”
Other types of hyaluronidase may work in different ways, the study authors noted, and larger doses may be needed to treat longer-lasting types of fillers.
In an accompanying commentary, Derek H. Jones, MD, of Skin Care and Laser Physicians of Beverly Hills, Calif., praised the study, which he wrote, “proves that smaller, less-concentrated doses of hyaluronidase are capable of removing small amounts of HA [hyaluronic acid] without removing the entire implant.”
Dr. Jones added that he uses 10 U of Vitrase (hyaluronidase) for each 0.1 cc of Juvéderm that he estimates should be removed. He also uses 5 U of Vitrase for each 0.1 cc of Restylane, and 30 U for each 0.1 cc of Juvéderm Voluma.
“When attempting to remove smaller or partial amounts of HA implant,” he added, “I often dilute Vitrase with normal saline to go from 20 U/0.1 cc to 10 U/0.1 cc or less.”
Northwestern University funded the study. Dr. Alam, the lead author, reported various disclosures, and the university disclosed that its clinical trials branch receives various government and corporate grants. The other authors reported no disclosures. Dr. Jones disclosed serving as an investigator, consultant, and/or speaker for Allergan, Merz, and Galderma.
SOURCE: Alam M et al. JAMA Dermatol. 2018 Apr 25. doi: 10.1001/jamadermatol.2018.0515.
, and in some cases, slightly larger doses may move things along more rapidly, according to the authors of a small split-arm clinical trial.
“These findings offer clinicians a means to modify and fine-tune filler-associated skin contour without resorting to high-dose injections that completely remove all filler from the treatment site,” wrote the authors, led by Murad Alam, MD, professor of dermatology and chief of cutaneous and aesthetic surgery in the department of dermatology, Northwestern University, Chicago. The study was published online in JAMA Dermatology.
The study, conducted during 2013-2014, analyzed the impact of various small doses of hyaluronidase on two types of fillers that had been administered into the upper inner arms of nine women (seven white, two black; mean age, 46 years). Another participant withdrew because of a fear of needles.
In one arm in each woman, researchers injected four aliquots of Juvéderm Ultra XC (0.4 mL each). Then, at 1, 2, and 3 weeks, they administered 1.5 U, 3.0 U, or 9.0 U hyaluronidase per 0.1 mL or saline control (at a constant volume of 0.1 mL) into each site. In the other arms, researchers performed the same protocol, but with Restylane-L. A 5-point scale was used to rate detectability of each site ranging from 0 (undetectable) and 1 (faintly perceptible) to 4 (“very” perceptible).
A blinded physician visually rated the effects of saline versus hyaluronidase at 4 weeks and found a significant difference between assessments of the hyaluronidase-treated sites and saline control sites at 4 weeks, favoring the hyaluronidase sites for visual detection (mean difference, 1.15; P less than .001) and palpability (mean difference, 1.22; P less than .001). Participant self-assessments at 4 weeks produced similar results for visual detection (mean difference, 0.87; P = .006) and palpability (mean difference, 1.59; P less than .001).
Similar differences favoring hyaluronidase persisted at 4 months.
The researchers also found that 9.0-U treatments of hyaluronidase led to significantly less palpability than 1.5-U treatments at 4 weeks and 4 months. The researchers noticed a larger dose-related difference for hyaluronidase for Restylane-L sites, and they noted that all the filler nodules diminished over time regardless of the study treatment.
“The clinical relevance of these findings is clear,” they concluded. “Minor filler-associated asymmetries, nodules, and textural abnormalities may be corrected safely and effectively with low-volume, low-dose hyaluronidase. Rather than dissolving all the offending filler, waiting, and then reinjecting fresh filler weeks or months later, dermatologists may precisely sculpt already injected excess filler by titration with low-volume, low-dose hyaluronidase to the desired skin contour.”
Other types of hyaluronidase may work in different ways, the study authors noted, and larger doses may be needed to treat longer-lasting types of fillers.
In an accompanying commentary, Derek H. Jones, MD, of Skin Care and Laser Physicians of Beverly Hills, Calif., praised the study, which he wrote, “proves that smaller, less-concentrated doses of hyaluronidase are capable of removing small amounts of HA [hyaluronic acid] without removing the entire implant.”
Dr. Jones added that he uses 10 U of Vitrase (hyaluronidase) for each 0.1 cc of Juvéderm that he estimates should be removed. He also uses 5 U of Vitrase for each 0.1 cc of Restylane, and 30 U for each 0.1 cc of Juvéderm Voluma.
“When attempting to remove smaller or partial amounts of HA implant,” he added, “I often dilute Vitrase with normal saline to go from 20 U/0.1 cc to 10 U/0.1 cc or less.”
Northwestern University funded the study. Dr. Alam, the lead author, reported various disclosures, and the university disclosed that its clinical trials branch receives various government and corporate grants. The other authors reported no disclosures. Dr. Jones disclosed serving as an investigator, consultant, and/or speaker for Allergan, Merz, and Galderma.
SOURCE: Alam M et al. JAMA Dermatol. 2018 Apr 25. doi: 10.1001/jamadermatol.2018.0515.
, and in some cases, slightly larger doses may move things along more rapidly, according to the authors of a small split-arm clinical trial.
“These findings offer clinicians a means to modify and fine-tune filler-associated skin contour without resorting to high-dose injections that completely remove all filler from the treatment site,” wrote the authors, led by Murad Alam, MD, professor of dermatology and chief of cutaneous and aesthetic surgery in the department of dermatology, Northwestern University, Chicago. The study was published online in JAMA Dermatology.
The study, conducted during 2013-2014, analyzed the impact of various small doses of hyaluronidase on two types of fillers that had been administered into the upper inner arms of nine women (seven white, two black; mean age, 46 years). Another participant withdrew because of a fear of needles.
In one arm in each woman, researchers injected four aliquots of Juvéderm Ultra XC (0.4 mL each). Then, at 1, 2, and 3 weeks, they administered 1.5 U, 3.0 U, or 9.0 U hyaluronidase per 0.1 mL or saline control (at a constant volume of 0.1 mL) into each site. In the other arms, researchers performed the same protocol, but with Restylane-L. A 5-point scale was used to rate detectability of each site ranging from 0 (undetectable) and 1 (faintly perceptible) to 4 (“very” perceptible).
A blinded physician visually rated the effects of saline versus hyaluronidase at 4 weeks and found a significant difference between assessments of the hyaluronidase-treated sites and saline control sites at 4 weeks, favoring the hyaluronidase sites for visual detection (mean difference, 1.15; P less than .001) and palpability (mean difference, 1.22; P less than .001). Participant self-assessments at 4 weeks produced similar results for visual detection (mean difference, 0.87; P = .006) and palpability (mean difference, 1.59; P less than .001).
Similar differences favoring hyaluronidase persisted at 4 months.
The researchers also found that 9.0-U treatments of hyaluronidase led to significantly less palpability than 1.5-U treatments at 4 weeks and 4 months. The researchers noticed a larger dose-related difference for hyaluronidase for Restylane-L sites, and they noted that all the filler nodules diminished over time regardless of the study treatment.
“The clinical relevance of these findings is clear,” they concluded. “Minor filler-associated asymmetries, nodules, and textural abnormalities may be corrected safely and effectively with low-volume, low-dose hyaluronidase. Rather than dissolving all the offending filler, waiting, and then reinjecting fresh filler weeks or months later, dermatologists may precisely sculpt already injected excess filler by titration with low-volume, low-dose hyaluronidase to the desired skin contour.”
Other types of hyaluronidase may work in different ways, the study authors noted, and larger doses may be needed to treat longer-lasting types of fillers.
In an accompanying commentary, Derek H. Jones, MD, of Skin Care and Laser Physicians of Beverly Hills, Calif., praised the study, which he wrote, “proves that smaller, less-concentrated doses of hyaluronidase are capable of removing small amounts of HA [hyaluronic acid] without removing the entire implant.”
Dr. Jones added that he uses 10 U of Vitrase (hyaluronidase) for each 0.1 cc of Juvéderm that he estimates should be removed. He also uses 5 U of Vitrase for each 0.1 cc of Restylane, and 30 U for each 0.1 cc of Juvéderm Voluma.
“When attempting to remove smaller or partial amounts of HA implant,” he added, “I often dilute Vitrase with normal saline to go from 20 U/0.1 cc to 10 U/0.1 cc or less.”
Northwestern University funded the study. Dr. Alam, the lead author, reported various disclosures, and the university disclosed that its clinical trials branch receives various government and corporate grants. The other authors reported no disclosures. Dr. Jones disclosed serving as an investigator, consultant, and/or speaker for Allergan, Merz, and Galderma.
SOURCE: Alam M et al. JAMA Dermatol. 2018 Apr 25. doi: 10.1001/jamadermatol.2018.0515.
FROM JAMA DERMATOLOGY
Key clinical point: Low doses of hyaluronidase can effectively remove unwanted hyaluronic acid filler.
Major finding: At 4 weeks, palpability favored hyaluronidase vs. saline (mean difference, 1.22; P less than .001).
Study details: A split-arm, parallel-group randomized clinical trial of nine women. Arms were given one of two types of filler injections and saline or various doses of hyaluronidase.
Disclosures: Northwestern University funded the study. One author reported various financial disclosures.
Source: Alam M et al. JAMA Dermatol. 2018 Apr 25. doi: 10.1001/jamadermatol.2018.0515.
Cryolipolysis leads surge in body sculpting
during 2012-2017, according to a survey from the American Society for Dermatologic Surgery.
A total of 434,000 body sculpting procedures were performed by ASDS members in 2017, compared with 146,000 in 2012, the ASDS reported based on data from 667 survey respondents, which were generalized to the society’s membership of over 6,400 physicians.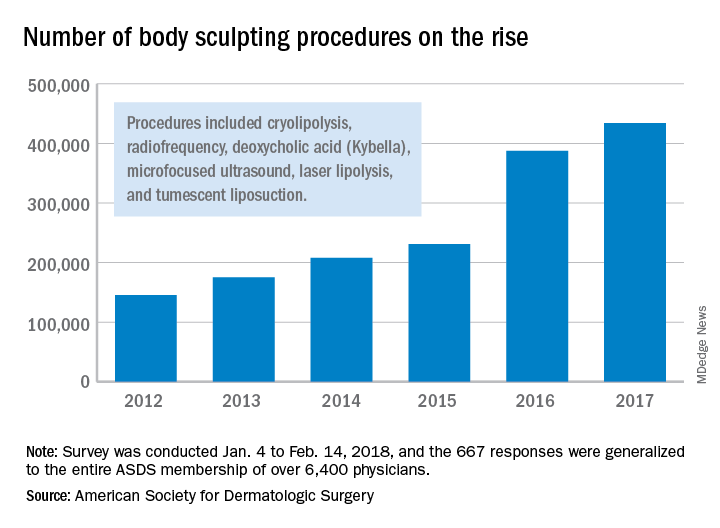
“An increase in media coverage and in celebrities acknowledging their procedures are growing awareness among the general public and improving the comfort level of diverse audiences to explore treatments,” ASDS president Lisa Donofrio, MD, said in a written statement. The survey was conducted from Jan. 4 to Feb. 14, 2018.
during 2012-2017, according to a survey from the American Society for Dermatologic Surgery.
A total of 434,000 body sculpting procedures were performed by ASDS members in 2017, compared with 146,000 in 2012, the ASDS reported based on data from 667 survey respondents, which were generalized to the society’s membership of over 6,400 physicians.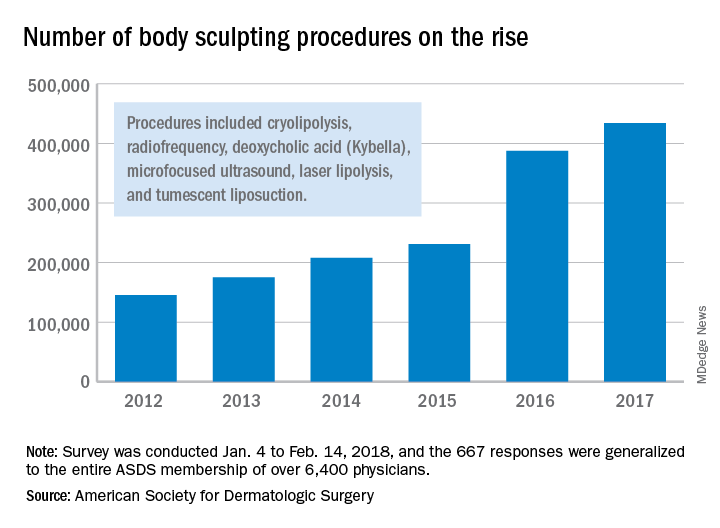
“An increase in media coverage and in celebrities acknowledging their procedures are growing awareness among the general public and improving the comfort level of diverse audiences to explore treatments,” ASDS president Lisa Donofrio, MD, said in a written statement. The survey was conducted from Jan. 4 to Feb. 14, 2018.
during 2012-2017, according to a survey from the American Society for Dermatologic Surgery.
A total of 434,000 body sculpting procedures were performed by ASDS members in 2017, compared with 146,000 in 2012, the ASDS reported based on data from 667 survey respondents, which were generalized to the society’s membership of over 6,400 physicians.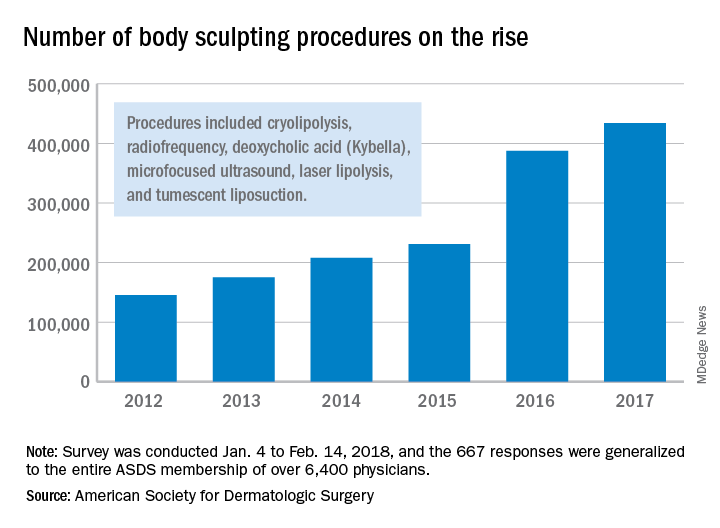
“An increase in media coverage and in celebrities acknowledging their procedures are growing awareness among the general public and improving the comfort level of diverse audiences to explore treatments,” ASDS president Lisa Donofrio, MD, said in a written statement. The survey was conducted from Jan. 4 to Feb. 14, 2018.
Sesamol
The protective effects of the antioxidative compound sesamol against radiation were reported as early as 1991.1 The water-soluble lignan sesamol, a natural phenolic compound derived from Sesamum indicum (sesame) seed oil, has since become known as a potent antioxidant with significant anticancer potential.2,3 As a constituent found in food oils such as sesame and sunflower oil, sesamol has been studied for the dietary benefits that it has been said to impart. Sesame oil, in particular, has been used in Ayurveda, traditional Chinese medicine, as well as in folk medicine in Nigeria and other African countries.Data on its antioxidant and chemopreventive properties also have prompted investigations into its potential in the dermatologic realm because sesamol has demonstrated an increasingly wide array of cutaneous applications.
Antibacterial effects
In 2007, Bankole et al. ascertained the synergistic antimicrobial properties of the essential oils and lignans found in the leaf extracts of S. radiatum and S. indicum. Phytochemical screening of methanolic extracts revealed the presence of phenolic compounds such as the potent antioxidants sesamol, sesamolin, and sesamin, as well as carboxylic acids. Methanolic and ethanolic extracts were shown to exhibit broad-spectrum antimicrobial effects against all of the pathogens tested except Streptococcus pneumoniae (methanolic extracts) and Staphylococcus aureus (ethanolic extracts). The investigators concluded that their results buttressed long-held traditional claims in multiple regions in Nigeria where consumption of sesame leaf extracts has been known to confer antibacterial effects with effectiveness reported for common skin infections.4
Anticancer activity
Kapadia et al. studied the dietary components resveratrol, sesamol, sesame oil, and sunflower oil in various protocols, including a murine two-stage skin cancer model, for their potential as cancer chemopreventive agents. In this 2002 study, the mouse skin tumor model, sesamol was found to provide a 50% reduction in skin papillomas at 20 weeks after promotion with 12-O-tetradecanoylphorbol 13-acetate. The researchers concluded that all of the dietary constituents appeared to provide chemopreventive effects.5
In 2010, Ramachandran et al. observed that pretreating human skin dermal fibroblast adult cells with sesamol before irradiation with UVB yielded significant reductions in cytotoxicity, intracellular reactive oxygen species levels, lipid peroxidation, and apoptosis. In noting increases in enzymatic and nonenzymatic antioxidant activity in sesamol-pretreated UVB-exposed fibroblasts, the investigators ascribed the apparent protective effects of sesamol to its antioxidant scavenging of reactive oxygen species.6
Seven years later, Bhardwaj et al. evaluated the chemopreventive efficacy of free and encapsulated sesamol in a 7,12-dimethylbenz[a]-anthracene–induced skin cancer animal model. The investigators found that in both forms sesamol significantly reduced tumor burden and lipid peroxidation while raising antioxidant levels. This resulted in the inhibition of skin tumor development and promotion. Apoptosis in tumor cells also was found to result from the down-regulation of Bcl-2 and stimulation of Bcl-2–associated X protein expression from administration of both free and encapsulated sesamol. Furthermore, the irritant qualities of sesamol were mitigated by encapsulation, which also aided in direct targeting of the skin.2
Potential cosmeceutical applications: Anti-aging and skin-whitening activity
In 2006, Sharma and Kaur demonstrated in mouse skin, through biochemical and histopathologic evaluations, that a topical sesamol formulation was effective in preventing photodamage (such as alterations in skin integrity, lesions, ulcers) from chronic UV exposure. They suggested the merits of further testing and consideration of sesamol as an antiaging agent.7
Almost a decade later, Srisayam et al. conducted a systematic study of the antimelanogenic and skin protective activities of sesamol. They found that sesamol exhibited significant scavenging activity of the 2,2-Diphenyl-1-picrylhydrazyl hydrate radical with an IC50 value less than 14.48 mcm. The antioxidant also suppressed lipid peroxidation (IC50 value of 6.15 mcm), and displayed a whitening effect via mushroom tyrosinase inhibition as well as inhibition of cellular tyrosinase. In noting the potent antioxidant and antityrosinase activity in comparison to the positive control – kojic acid and beta-arbutin – the researchers highlighted the potential cosmeceutical applications of sesamol.8
Baek and Lee showed in 2015 that sesamol potently suppressed melanin biosynthesis by down-regulating tyrosinase activity and regulating gene expression of melanogenesis-related proteins via microphthalmia-associated transcription factor (MITF) activity modulation. They concluded that sesamol warrants attention in the cosmetic realm as a new skin-whitening agent.9
Formulation issues
Earlier that year, Geetha et al. confirmed the apoptotic characteristics of sesamol in in vitro antiproliferative and DNA-fragmentation studies in HL60 cell lines. Because of its small size, low molecular weight, and easy permeability, its viability in topical applications is considered minimal. The investigators addressed this issue by preparing sesamol-loaded solid-lipid nanoparticles, which, when applied in a cream base in mice, revealed significant retention in the skin. Its use in in vivo anticancer studies performed on tumor production induced by 12-O-tetradecanoylphorbol 13-acetate and initiated by benzo(a)pyrene in mouse epidermis resulted in the normalization of skin cancers.10
More recently, Puglia et al. set out to improve the delivery of the benefits of sesamol to the skin by developing a nanostructured lipid carrier for topical administration. They synthesized two different carrier systems and performed an in vitro percutaneous absorption study in excised human skin to determine antioxidant activity. The carrier systems differed by oil phase: One contained Miglyol 812 (nanostructured lipid carrier–M) and the other contained sesame oil (nanostructured lipid carrier–PLUS). Greater encapsulation efficiency was reported when sesame oil was employed as the oil phase, but both products displayed the capacity in vitro to control the rate of sesamol diffusion through the skin, compared with reference preparations. Both formulations also showed the extended antioxidant activity of sesamol, particularly the nanostructured lipid carrier–PLUS.3
Conclusion
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014). She also wrote a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Sato Y et al. Yakugaku Zasshi. 1991 Jan;111(1):51-8.
2. Bhardwaj R et al. Anticancer Agents Med Chem. 2017;17(5):726-33.
3. Puglia C et al. Planta Med. 2017 Mar;83(5):398-404.
4. Bankole MA et al. Afr J Tradit Complement Altern Med. 2007; 4(4): 427-33.
5. Kapadia GJ et al. Pharmacol Res. 2002 Jun;45(6):499-505.
6. Ramachandran S et al. Arch Dermatol Res. 2010 Dec;302(10):733-44.
7. Sharma S and Kaur IP. Int J Dermatol. 2006 Mar;45(3):200-8.
8. Srisayam M et al. J Cosmet Sci. 2014 Mar-Apr;65(2):69-79.
9. Baek SH and Lee SH. Exp Dermatol. 2015 Oct;24(10):761-6.
10. Geetha T et al. J Drug Target. 2015 Feb;23(2):159-69.
The protective effects of the antioxidative compound sesamol against radiation were reported as early as 1991.1 The water-soluble lignan sesamol, a natural phenolic compound derived from Sesamum indicum (sesame) seed oil, has since become known as a potent antioxidant with significant anticancer potential.2,3 As a constituent found in food oils such as sesame and sunflower oil, sesamol has been studied for the dietary benefits that it has been said to impart. Sesame oil, in particular, has been used in Ayurveda, traditional Chinese medicine, as well as in folk medicine in Nigeria and other African countries.Data on its antioxidant and chemopreventive properties also have prompted investigations into its potential in the dermatologic realm because sesamol has demonstrated an increasingly wide array of cutaneous applications.
Antibacterial effects
In 2007, Bankole et al. ascertained the synergistic antimicrobial properties of the essential oils and lignans found in the leaf extracts of S. radiatum and S. indicum. Phytochemical screening of methanolic extracts revealed the presence of phenolic compounds such as the potent antioxidants sesamol, sesamolin, and sesamin, as well as carboxylic acids. Methanolic and ethanolic extracts were shown to exhibit broad-spectrum antimicrobial effects against all of the pathogens tested except Streptococcus pneumoniae (methanolic extracts) and Staphylococcus aureus (ethanolic extracts). The investigators concluded that their results buttressed long-held traditional claims in multiple regions in Nigeria where consumption of sesame leaf extracts has been known to confer antibacterial effects with effectiveness reported for common skin infections.4
Anticancer activity
Kapadia et al. studied the dietary components resveratrol, sesamol, sesame oil, and sunflower oil in various protocols, including a murine two-stage skin cancer model, for their potential as cancer chemopreventive agents. In this 2002 study, the mouse skin tumor model, sesamol was found to provide a 50% reduction in skin papillomas at 20 weeks after promotion with 12-O-tetradecanoylphorbol 13-acetate. The researchers concluded that all of the dietary constituents appeared to provide chemopreventive effects.5
In 2010, Ramachandran et al. observed that pretreating human skin dermal fibroblast adult cells with sesamol before irradiation with UVB yielded significant reductions in cytotoxicity, intracellular reactive oxygen species levels, lipid peroxidation, and apoptosis. In noting increases in enzymatic and nonenzymatic antioxidant activity in sesamol-pretreated UVB-exposed fibroblasts, the investigators ascribed the apparent protective effects of sesamol to its antioxidant scavenging of reactive oxygen species.6
Seven years later, Bhardwaj et al. evaluated the chemopreventive efficacy of free and encapsulated sesamol in a 7,12-dimethylbenz[a]-anthracene–induced skin cancer animal model. The investigators found that in both forms sesamol significantly reduced tumor burden and lipid peroxidation while raising antioxidant levels. This resulted in the inhibition of skin tumor development and promotion. Apoptosis in tumor cells also was found to result from the down-regulation of Bcl-2 and stimulation of Bcl-2–associated X protein expression from administration of both free and encapsulated sesamol. Furthermore, the irritant qualities of sesamol were mitigated by encapsulation, which also aided in direct targeting of the skin.2
Potential cosmeceutical applications: Anti-aging and skin-whitening activity
In 2006, Sharma and Kaur demonstrated in mouse skin, through biochemical and histopathologic evaluations, that a topical sesamol formulation was effective in preventing photodamage (such as alterations in skin integrity, lesions, ulcers) from chronic UV exposure. They suggested the merits of further testing and consideration of sesamol as an antiaging agent.7
Almost a decade later, Srisayam et al. conducted a systematic study of the antimelanogenic and skin protective activities of sesamol. They found that sesamol exhibited significant scavenging activity of the 2,2-Diphenyl-1-picrylhydrazyl hydrate radical with an IC50 value less than 14.48 mcm. The antioxidant also suppressed lipid peroxidation (IC50 value of 6.15 mcm), and displayed a whitening effect via mushroom tyrosinase inhibition as well as inhibition of cellular tyrosinase. In noting the potent antioxidant and antityrosinase activity in comparison to the positive control – kojic acid and beta-arbutin – the researchers highlighted the potential cosmeceutical applications of sesamol.8
Baek and Lee showed in 2015 that sesamol potently suppressed melanin biosynthesis by down-regulating tyrosinase activity and regulating gene expression of melanogenesis-related proteins via microphthalmia-associated transcription factor (MITF) activity modulation. They concluded that sesamol warrants attention in the cosmetic realm as a new skin-whitening agent.9
Formulation issues
Earlier that year, Geetha et al. confirmed the apoptotic characteristics of sesamol in in vitro antiproliferative and DNA-fragmentation studies in HL60 cell lines. Because of its small size, low molecular weight, and easy permeability, its viability in topical applications is considered minimal. The investigators addressed this issue by preparing sesamol-loaded solid-lipid nanoparticles, which, when applied in a cream base in mice, revealed significant retention in the skin. Its use in in vivo anticancer studies performed on tumor production induced by 12-O-tetradecanoylphorbol 13-acetate and initiated by benzo(a)pyrene in mouse epidermis resulted in the normalization of skin cancers.10
More recently, Puglia et al. set out to improve the delivery of the benefits of sesamol to the skin by developing a nanostructured lipid carrier for topical administration. They synthesized two different carrier systems and performed an in vitro percutaneous absorption study in excised human skin to determine antioxidant activity. The carrier systems differed by oil phase: One contained Miglyol 812 (nanostructured lipid carrier–M) and the other contained sesame oil (nanostructured lipid carrier–PLUS). Greater encapsulation efficiency was reported when sesame oil was employed as the oil phase, but both products displayed the capacity in vitro to control the rate of sesamol diffusion through the skin, compared with reference preparations. Both formulations also showed the extended antioxidant activity of sesamol, particularly the nanostructured lipid carrier–PLUS.3
Conclusion
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014). She also wrote a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Sato Y et al. Yakugaku Zasshi. 1991 Jan;111(1):51-8.
2. Bhardwaj R et al. Anticancer Agents Med Chem. 2017;17(5):726-33.
3. Puglia C et al. Planta Med. 2017 Mar;83(5):398-404.
4. Bankole MA et al. Afr J Tradit Complement Altern Med. 2007; 4(4): 427-33.
5. Kapadia GJ et al. Pharmacol Res. 2002 Jun;45(6):499-505.
6. Ramachandran S et al. Arch Dermatol Res. 2010 Dec;302(10):733-44.
7. Sharma S and Kaur IP. Int J Dermatol. 2006 Mar;45(3):200-8.
8. Srisayam M et al. J Cosmet Sci. 2014 Mar-Apr;65(2):69-79.
9. Baek SH and Lee SH. Exp Dermatol. 2015 Oct;24(10):761-6.
10. Geetha T et al. J Drug Target. 2015 Feb;23(2):159-69.
The protective effects of the antioxidative compound sesamol against radiation were reported as early as 1991.1 The water-soluble lignan sesamol, a natural phenolic compound derived from Sesamum indicum (sesame) seed oil, has since become known as a potent antioxidant with significant anticancer potential.2,3 As a constituent found in food oils such as sesame and sunflower oil, sesamol has been studied for the dietary benefits that it has been said to impart. Sesame oil, in particular, has been used in Ayurveda, traditional Chinese medicine, as well as in folk medicine in Nigeria and other African countries.Data on its antioxidant and chemopreventive properties also have prompted investigations into its potential in the dermatologic realm because sesamol has demonstrated an increasingly wide array of cutaneous applications.
Antibacterial effects
In 2007, Bankole et al. ascertained the synergistic antimicrobial properties of the essential oils and lignans found in the leaf extracts of S. radiatum and S. indicum. Phytochemical screening of methanolic extracts revealed the presence of phenolic compounds such as the potent antioxidants sesamol, sesamolin, and sesamin, as well as carboxylic acids. Methanolic and ethanolic extracts were shown to exhibit broad-spectrum antimicrobial effects against all of the pathogens tested except Streptococcus pneumoniae (methanolic extracts) and Staphylococcus aureus (ethanolic extracts). The investigators concluded that their results buttressed long-held traditional claims in multiple regions in Nigeria where consumption of sesame leaf extracts has been known to confer antibacterial effects with effectiveness reported for common skin infections.4
Anticancer activity
Kapadia et al. studied the dietary components resveratrol, sesamol, sesame oil, and sunflower oil in various protocols, including a murine two-stage skin cancer model, for their potential as cancer chemopreventive agents. In this 2002 study, the mouse skin tumor model, sesamol was found to provide a 50% reduction in skin papillomas at 20 weeks after promotion with 12-O-tetradecanoylphorbol 13-acetate. The researchers concluded that all of the dietary constituents appeared to provide chemopreventive effects.5
In 2010, Ramachandran et al. observed that pretreating human skin dermal fibroblast adult cells with sesamol before irradiation with UVB yielded significant reductions in cytotoxicity, intracellular reactive oxygen species levels, lipid peroxidation, and apoptosis. In noting increases in enzymatic and nonenzymatic antioxidant activity in sesamol-pretreated UVB-exposed fibroblasts, the investigators ascribed the apparent protective effects of sesamol to its antioxidant scavenging of reactive oxygen species.6
Seven years later, Bhardwaj et al. evaluated the chemopreventive efficacy of free and encapsulated sesamol in a 7,12-dimethylbenz[a]-anthracene–induced skin cancer animal model. The investigators found that in both forms sesamol significantly reduced tumor burden and lipid peroxidation while raising antioxidant levels. This resulted in the inhibition of skin tumor development and promotion. Apoptosis in tumor cells also was found to result from the down-regulation of Bcl-2 and stimulation of Bcl-2–associated X protein expression from administration of both free and encapsulated sesamol. Furthermore, the irritant qualities of sesamol were mitigated by encapsulation, which also aided in direct targeting of the skin.2
Potential cosmeceutical applications: Anti-aging and skin-whitening activity
In 2006, Sharma and Kaur demonstrated in mouse skin, through biochemical and histopathologic evaluations, that a topical sesamol formulation was effective in preventing photodamage (such as alterations in skin integrity, lesions, ulcers) from chronic UV exposure. They suggested the merits of further testing and consideration of sesamol as an antiaging agent.7
Almost a decade later, Srisayam et al. conducted a systematic study of the antimelanogenic and skin protective activities of sesamol. They found that sesamol exhibited significant scavenging activity of the 2,2-Diphenyl-1-picrylhydrazyl hydrate radical with an IC50 value less than 14.48 mcm. The antioxidant also suppressed lipid peroxidation (IC50 value of 6.15 mcm), and displayed a whitening effect via mushroom tyrosinase inhibition as well as inhibition of cellular tyrosinase. In noting the potent antioxidant and antityrosinase activity in comparison to the positive control – kojic acid and beta-arbutin – the researchers highlighted the potential cosmeceutical applications of sesamol.8
Baek and Lee showed in 2015 that sesamol potently suppressed melanin biosynthesis by down-regulating tyrosinase activity and regulating gene expression of melanogenesis-related proteins via microphthalmia-associated transcription factor (MITF) activity modulation. They concluded that sesamol warrants attention in the cosmetic realm as a new skin-whitening agent.9
Formulation issues
Earlier that year, Geetha et al. confirmed the apoptotic characteristics of sesamol in in vitro antiproliferative and DNA-fragmentation studies in HL60 cell lines. Because of its small size, low molecular weight, and easy permeability, its viability in topical applications is considered minimal. The investigators addressed this issue by preparing sesamol-loaded solid-lipid nanoparticles, which, when applied in a cream base in mice, revealed significant retention in the skin. Its use in in vivo anticancer studies performed on tumor production induced by 12-O-tetradecanoylphorbol 13-acetate and initiated by benzo(a)pyrene in mouse epidermis resulted in the normalization of skin cancers.10
More recently, Puglia et al. set out to improve the delivery of the benefits of sesamol to the skin by developing a nanostructured lipid carrier for topical administration. They synthesized two different carrier systems and performed an in vitro percutaneous absorption study in excised human skin to determine antioxidant activity. The carrier systems differed by oil phase: One contained Miglyol 812 (nanostructured lipid carrier–M) and the other contained sesame oil (nanostructured lipid carrier–PLUS). Greater encapsulation efficiency was reported when sesame oil was employed as the oil phase, but both products displayed the capacity in vitro to control the rate of sesamol diffusion through the skin, compared with reference preparations. Both formulations also showed the extended antioxidant activity of sesamol, particularly the nanostructured lipid carrier–PLUS.3
Conclusion
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014). She also wrote a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Sato Y et al. Yakugaku Zasshi. 1991 Jan;111(1):51-8.
2. Bhardwaj R et al. Anticancer Agents Med Chem. 2017;17(5):726-33.
3. Puglia C et al. Planta Med. 2017 Mar;83(5):398-404.
4. Bankole MA et al. Afr J Tradit Complement Altern Med. 2007; 4(4): 427-33.
5. Kapadia GJ et al. Pharmacol Res. 2002 Jun;45(6):499-505.
6. Ramachandran S et al. Arch Dermatol Res. 2010 Dec;302(10):733-44.
7. Sharma S and Kaur IP. Int J Dermatol. 2006 Mar;45(3):200-8.
8. Srisayam M et al. J Cosmet Sci. 2014 Mar-Apr;65(2):69-79.
9. Baek SH and Lee SH. Exp Dermatol. 2015 Oct;24(10):761-6.
10. Geetha T et al. J Drug Target. 2015 Feb;23(2):159-69.
Study pits cryolipolysis versus HIFU for fat reduction in the flank region
DALLAS – While cryolipolysis and high-intensity focused ultrasound are both effective at reducing subcutaneous fat in the flank region, cryolipolysis appeared to be less painful and more effective in a small, randomized trial.
Noninvasive subcutaneous fat reduction is becoming increasingly popular, study author Farhaad R. Riyaz, MD, observed at the annual conference of the American Society for Laser Medicine and Surgery. “High-intensity focused ultrasound seems to be less popular than cryolipolysis. It uses sound waves to create heat and is similar in technology to light traveling through a magnifying glass to create heat at a focal point. But the two technologies really haven’t been rigorously compared in the literature,” he added.
Dr. Riyaz and his associates in the division of cutaneous and aesthetic surgery at Northwestern University, Chicago, enrolled 12 healthy female participants with a body mass index between 18 and 30 kg/m2 and moderate fat in the abdomen flanks. In the split-body, parallel-group trial, the subjects were randomized to cryolipolysis on one flank and to high-intensity focused ultrasound (HIFU) on the contralateral side. Study participants were asked to maintain their weight throughout the 12-week study. Treatments were performed at baseline, week 4, and week 8, with a follow-up visit at week 12. The primary outcome was thickness of subcutaneous fat as measured by ultrasound; secondary outcomes included pain, patient-reported improvement, and total circumference of the abdomen and flanks.
The mean age of the 12 participants was 39 years, 8 were white, and most had Fitzpatrick skin types II and IV (33% and 42%, respectively). Dr. Riyaz reported that (P = .0007 and P = .0341, respectively), as measured by diagnostic ultrasound. The researchers noted significantly less fat in the flanks on the sides treated with cryolipolysis, compared with the sides treated with HIFU (P = .007). Study participants reported significantly more pain with HIFU compared with cryolipolysis (P = .0002).
“Although participant-reported improvement in the appearance of their flanks was significant for both treatments [P less than .0001], patients couldn’t appreciate a difference between the side that was treated with HIFU and the side that was treated with cryolipolysis,” Dr. Riyaz said. “In addition, the total abdominal circumference did not change throughout the study for either group.”
He reported having no financial disclosures.
DALLAS – While cryolipolysis and high-intensity focused ultrasound are both effective at reducing subcutaneous fat in the flank region, cryolipolysis appeared to be less painful and more effective in a small, randomized trial.
Noninvasive subcutaneous fat reduction is becoming increasingly popular, study author Farhaad R. Riyaz, MD, observed at the annual conference of the American Society for Laser Medicine and Surgery. “High-intensity focused ultrasound seems to be less popular than cryolipolysis. It uses sound waves to create heat and is similar in technology to light traveling through a magnifying glass to create heat at a focal point. But the two technologies really haven’t been rigorously compared in the literature,” he added.
Dr. Riyaz and his associates in the division of cutaneous and aesthetic surgery at Northwestern University, Chicago, enrolled 12 healthy female participants with a body mass index between 18 and 30 kg/m2 and moderate fat in the abdomen flanks. In the split-body, parallel-group trial, the subjects were randomized to cryolipolysis on one flank and to high-intensity focused ultrasound (HIFU) on the contralateral side. Study participants were asked to maintain their weight throughout the 12-week study. Treatments were performed at baseline, week 4, and week 8, with a follow-up visit at week 12. The primary outcome was thickness of subcutaneous fat as measured by ultrasound; secondary outcomes included pain, patient-reported improvement, and total circumference of the abdomen and flanks.
The mean age of the 12 participants was 39 years, 8 were white, and most had Fitzpatrick skin types II and IV (33% and 42%, respectively). Dr. Riyaz reported that (P = .0007 and P = .0341, respectively), as measured by diagnostic ultrasound. The researchers noted significantly less fat in the flanks on the sides treated with cryolipolysis, compared with the sides treated with HIFU (P = .007). Study participants reported significantly more pain with HIFU compared with cryolipolysis (P = .0002).
“Although participant-reported improvement in the appearance of their flanks was significant for both treatments [P less than .0001], patients couldn’t appreciate a difference between the side that was treated with HIFU and the side that was treated with cryolipolysis,” Dr. Riyaz said. “In addition, the total abdominal circumference did not change throughout the study for either group.”
He reported having no financial disclosures.
DALLAS – While cryolipolysis and high-intensity focused ultrasound are both effective at reducing subcutaneous fat in the flank region, cryolipolysis appeared to be less painful and more effective in a small, randomized trial.
Noninvasive subcutaneous fat reduction is becoming increasingly popular, study author Farhaad R. Riyaz, MD, observed at the annual conference of the American Society for Laser Medicine and Surgery. “High-intensity focused ultrasound seems to be less popular than cryolipolysis. It uses sound waves to create heat and is similar in technology to light traveling through a magnifying glass to create heat at a focal point. But the two technologies really haven’t been rigorously compared in the literature,” he added.
Dr. Riyaz and his associates in the division of cutaneous and aesthetic surgery at Northwestern University, Chicago, enrolled 12 healthy female participants with a body mass index between 18 and 30 kg/m2 and moderate fat in the abdomen flanks. In the split-body, parallel-group trial, the subjects were randomized to cryolipolysis on one flank and to high-intensity focused ultrasound (HIFU) on the contralateral side. Study participants were asked to maintain their weight throughout the 12-week study. Treatments were performed at baseline, week 4, and week 8, with a follow-up visit at week 12. The primary outcome was thickness of subcutaneous fat as measured by ultrasound; secondary outcomes included pain, patient-reported improvement, and total circumference of the abdomen and flanks.
The mean age of the 12 participants was 39 years, 8 were white, and most had Fitzpatrick skin types II and IV (33% and 42%, respectively). Dr. Riyaz reported that (P = .0007 and P = .0341, respectively), as measured by diagnostic ultrasound. The researchers noted significantly less fat in the flanks on the sides treated with cryolipolysis, compared with the sides treated with HIFU (P = .007). Study participants reported significantly more pain with HIFU compared with cryolipolysis (P = .0002).
“Although participant-reported improvement in the appearance of their flanks was significant for both treatments [P less than .0001], patients couldn’t appreciate a difference between the side that was treated with HIFU and the side that was treated with cryolipolysis,” Dr. Riyaz said. “In addition, the total abdominal circumference did not change throughout the study for either group.”
He reported having no financial disclosures.
Key clinical point: Both cryolipolysis and high-intensity focused ultrasound (HIFU) are effective at reducing subcutaneous fat in the flank region.
Major finding: At week 12 follow-up, both cryolipolysis and HIFU significantly reduced fat in the flanks, compared with baseline (P = .0007 and P = .0341, respectively), as measured by diagnostic ultrasound.
Study details: A split-body, parallel-group trial in which 12 women were randomized to cryolipolysis on one flank and to HIFU on the contralateral side.
Disclosures: Dr. Riyaz reported having no financial disclosures.
Survey sheds light on consumer preferences regarding cosmetic procedures
DALLAS – The most important referral sources for cosmetic procedures are physicians and family members and friends, but there appears to be a knowledge gap as to which cosmetic providers are actually medical doctors, results from an online survey found.
“There are approximately 16 million cosmetic procedures performed in the U.S., and that number is growing rapidly,” study author Adam J. Wulkan, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “They’re performed by dermatologists, plastic surgeons, facial plastic surgeons, nurses, aestheticians, dentists, and more. Yet little is known regarding how consumers choose cosmetic procedures and providers.”
In an effort to elucidate how consumers research, self-educate, and choose cosmetic surgery procedures and providers, Dr. Wulkan and his associates used Survey Monkey to send a 20-item survey to 931 individuals in the United States. Respondents qualified for participation if they acknowledged having obtained or considered obtaining a cosmetic procedure. Of the 931 individuals polled, 323 (35%) met inclusion criteria; 84 (9%) had received a cosmetic procedure, and 239 (26%) had considered one. Nearly three-quarters of respondents (73%) were female; 22% of respondents were aged 18-29 years, 25% were aged 30-44 years, 29% were aged 45-59 years, and 24% were aged 60 years and older.
The top three sources for referral to cosmetic procedures/providers were physicians (67%), family or friends (57%), and Google searches (51%). However, fewer than half of respondents (42.5%) had a procedure performed after having a consultation. Reasons for this could be related to several factors, Dr. Wulkan said, including the cost of the procedure, fear of adverse events, or not being an appropriate candidate for treatment at the time of consultation.
The most popular cosmetic procedures were laser hair removal (28%), laser/light therapy (25%), abdominoplasty (25%), injectables (24%), and noninvasive fat reduction (24%). The survey also asked whether certain providers were medical doctors or not, and 89% of respondents thought plastic surgeons were medical doctors, and 82% thought that dermatologists were medical doctors; the respondents also thought dentists (52%), aestheticians (20%), and nurses (11%) were medical doctors. “There’s an education gap regarding which providers are medical doctors,” said Dr. Wulkan, who is a cosmetic laser and dermatology fellow at Massachusetts General Hospital, Boston. “With the growing number of nonphysician aesthetic providers, consumer education might be a valuable tool.”
Most respondents (82%) checked physician credentials prior to treatment. In addition, they were most likely to have their cosmetic procedures performed by either a plastic surgeon or by a dermatologist.
Dr. Wulkan acknowledged certain limitations of the study, including the sample size and reliability of the answers. He reported having no financial disclosures. One study coauthor had various ties to industry companies, including Allergan, Revance Therapeutics, and Cytrellis Biosystems.
DALLAS – The most important referral sources for cosmetic procedures are physicians and family members and friends, but there appears to be a knowledge gap as to which cosmetic providers are actually medical doctors, results from an online survey found.
“There are approximately 16 million cosmetic procedures performed in the U.S., and that number is growing rapidly,” study author Adam J. Wulkan, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “They’re performed by dermatologists, plastic surgeons, facial plastic surgeons, nurses, aestheticians, dentists, and more. Yet little is known regarding how consumers choose cosmetic procedures and providers.”
In an effort to elucidate how consumers research, self-educate, and choose cosmetic surgery procedures and providers, Dr. Wulkan and his associates used Survey Monkey to send a 20-item survey to 931 individuals in the United States. Respondents qualified for participation if they acknowledged having obtained or considered obtaining a cosmetic procedure. Of the 931 individuals polled, 323 (35%) met inclusion criteria; 84 (9%) had received a cosmetic procedure, and 239 (26%) had considered one. Nearly three-quarters of respondents (73%) were female; 22% of respondents were aged 18-29 years, 25% were aged 30-44 years, 29% were aged 45-59 years, and 24% were aged 60 years and older.
The top three sources for referral to cosmetic procedures/providers were physicians (67%), family or friends (57%), and Google searches (51%). However, fewer than half of respondents (42.5%) had a procedure performed after having a consultation. Reasons for this could be related to several factors, Dr. Wulkan said, including the cost of the procedure, fear of adverse events, or not being an appropriate candidate for treatment at the time of consultation.
The most popular cosmetic procedures were laser hair removal (28%), laser/light therapy (25%), abdominoplasty (25%), injectables (24%), and noninvasive fat reduction (24%). The survey also asked whether certain providers were medical doctors or not, and 89% of respondents thought plastic surgeons were medical doctors, and 82% thought that dermatologists were medical doctors; the respondents also thought dentists (52%), aestheticians (20%), and nurses (11%) were medical doctors. “There’s an education gap regarding which providers are medical doctors,” said Dr. Wulkan, who is a cosmetic laser and dermatology fellow at Massachusetts General Hospital, Boston. “With the growing number of nonphysician aesthetic providers, consumer education might be a valuable tool.”
Most respondents (82%) checked physician credentials prior to treatment. In addition, they were most likely to have their cosmetic procedures performed by either a plastic surgeon or by a dermatologist.
Dr. Wulkan acknowledged certain limitations of the study, including the sample size and reliability of the answers. He reported having no financial disclosures. One study coauthor had various ties to industry companies, including Allergan, Revance Therapeutics, and Cytrellis Biosystems.
DALLAS – The most important referral sources for cosmetic procedures are physicians and family members and friends, but there appears to be a knowledge gap as to which cosmetic providers are actually medical doctors, results from an online survey found.
“There are approximately 16 million cosmetic procedures performed in the U.S., and that number is growing rapidly,” study author Adam J. Wulkan, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “They’re performed by dermatologists, plastic surgeons, facial plastic surgeons, nurses, aestheticians, dentists, and more. Yet little is known regarding how consumers choose cosmetic procedures and providers.”
In an effort to elucidate how consumers research, self-educate, and choose cosmetic surgery procedures and providers, Dr. Wulkan and his associates used Survey Monkey to send a 20-item survey to 931 individuals in the United States. Respondents qualified for participation if they acknowledged having obtained or considered obtaining a cosmetic procedure. Of the 931 individuals polled, 323 (35%) met inclusion criteria; 84 (9%) had received a cosmetic procedure, and 239 (26%) had considered one. Nearly three-quarters of respondents (73%) were female; 22% of respondents were aged 18-29 years, 25% were aged 30-44 years, 29% were aged 45-59 years, and 24% were aged 60 years and older.
The top three sources for referral to cosmetic procedures/providers were physicians (67%), family or friends (57%), and Google searches (51%). However, fewer than half of respondents (42.5%) had a procedure performed after having a consultation. Reasons for this could be related to several factors, Dr. Wulkan said, including the cost of the procedure, fear of adverse events, or not being an appropriate candidate for treatment at the time of consultation.
The most popular cosmetic procedures were laser hair removal (28%), laser/light therapy (25%), abdominoplasty (25%), injectables (24%), and noninvasive fat reduction (24%). The survey also asked whether certain providers were medical doctors or not, and 89% of respondents thought plastic surgeons were medical doctors, and 82% thought that dermatologists were medical doctors; the respondents also thought dentists (52%), aestheticians (20%), and nurses (11%) were medical doctors. “There’s an education gap regarding which providers are medical doctors,” said Dr. Wulkan, who is a cosmetic laser and dermatology fellow at Massachusetts General Hospital, Boston. “With the growing number of nonphysician aesthetic providers, consumer education might be a valuable tool.”
Most respondents (82%) checked physician credentials prior to treatment. In addition, they were most likely to have their cosmetic procedures performed by either a plastic surgeon or by a dermatologist.
Dr. Wulkan acknowledged certain limitations of the study, including the sample size and reliability of the answers. He reported having no financial disclosures. One study coauthor had various ties to industry companies, including Allergan, Revance Therapeutics, and Cytrellis Biosystems.
REPORTING FROM ASLMS 2018
Key clinical point: An education gap exists regarding which cosmetic surgery providers are medical doctors.
Major finding: Physicians were the top source of referral to cosmetic procedures/providers, yet only 82% of consumers believe that dermatologists are medical doctors.
Study details: Responses from 323 consumers who completed a 20-item online survey about cosmetic surgery procedures and providers.
Disclosures: Dr. Wulkan reported having no financial disclosures. One study coauthor had various ties to industry companies, including Allergan, Revance, and Cytrellis.












