User login
Hospitalist Bob Wachter Tops Modern Healthcare’s Physician Leadership List
For the first time, a hospitalist tops Modern Healthcare’s 50 Most Influential Physician Executives and Leaders list.
The who’s who of standout physicians starts with HM pioneer Robert Wachter, MD, MHM, chief of the division of hospital medicine at the University of California San Francisco Medical Center, who's recognized for nearly two decades spent tackling topics that "challenge the status quo," writes Modern Healthcare.
The list features three hospitalists in total, including:
- Patrick Conway, MD, MSc, MHM, pediatric hospitalist, CMO for the Centers for Medicare & Medicaid Services (CMS), and CMS' acting deputy principal administrator for innovation and quality, ranked 11; and
- Vivek Murthy, MD, MBA, newly appointed U.S. Surgeon General and practicing hospitalist at Brigham and Women’s Hospital in Boston, ranked 16.
"Having three people on that list speaks volumes to our ability to identify those things that are issues in our healthcare system and impact them," says SHM President Robert Harrington Jr., MD, SFHM, chief medical officer at Reliant Post-Acute Care Solutions in Atlanta.
Dr. Harrington says that placing three hospitalists in the top 16 of a list like this one shows that while HM is a young specialty, it is at the nexus of dynamic change in care delivery.
"We've placed our bets in the right places when it comes to healthcare," he says. "[It] really is all about our patients, patient safety, quality, value."
Although Dr. Harrington likes the adulation the list can bring the specialty, he says if people move on and off of it, that's fine, too.
"As long as we continue to get a seat at the table in terms of healthcare policy formation and quality improvement organizations and patient safety organizations, and we continue to be respected in those arenas, for me, that’s what it’s about," he adds. "The list is nice, but the results are more important to us."
Visit our website for more information on hospitalist leadership.
For the first time, a hospitalist tops Modern Healthcare’s 50 Most Influential Physician Executives and Leaders list.
The who’s who of standout physicians starts with HM pioneer Robert Wachter, MD, MHM, chief of the division of hospital medicine at the University of California San Francisco Medical Center, who's recognized for nearly two decades spent tackling topics that "challenge the status quo," writes Modern Healthcare.
The list features three hospitalists in total, including:
- Patrick Conway, MD, MSc, MHM, pediatric hospitalist, CMO for the Centers for Medicare & Medicaid Services (CMS), and CMS' acting deputy principal administrator for innovation and quality, ranked 11; and
- Vivek Murthy, MD, MBA, newly appointed U.S. Surgeon General and practicing hospitalist at Brigham and Women’s Hospital in Boston, ranked 16.
"Having three people on that list speaks volumes to our ability to identify those things that are issues in our healthcare system and impact them," says SHM President Robert Harrington Jr., MD, SFHM, chief medical officer at Reliant Post-Acute Care Solutions in Atlanta.
Dr. Harrington says that placing three hospitalists in the top 16 of a list like this one shows that while HM is a young specialty, it is at the nexus of dynamic change in care delivery.
"We've placed our bets in the right places when it comes to healthcare," he says. "[It] really is all about our patients, patient safety, quality, value."
Although Dr. Harrington likes the adulation the list can bring the specialty, he says if people move on and off of it, that's fine, too.
"As long as we continue to get a seat at the table in terms of healthcare policy formation and quality improvement organizations and patient safety organizations, and we continue to be respected in those arenas, for me, that’s what it’s about," he adds. "The list is nice, but the results are more important to us."
Visit our website for more information on hospitalist leadership.
For the first time, a hospitalist tops Modern Healthcare’s 50 Most Influential Physician Executives and Leaders list.
The who’s who of standout physicians starts with HM pioneer Robert Wachter, MD, MHM, chief of the division of hospital medicine at the University of California San Francisco Medical Center, who's recognized for nearly two decades spent tackling topics that "challenge the status quo," writes Modern Healthcare.
The list features three hospitalists in total, including:
- Patrick Conway, MD, MSc, MHM, pediatric hospitalist, CMO for the Centers for Medicare & Medicaid Services (CMS), and CMS' acting deputy principal administrator for innovation and quality, ranked 11; and
- Vivek Murthy, MD, MBA, newly appointed U.S. Surgeon General and practicing hospitalist at Brigham and Women’s Hospital in Boston, ranked 16.
"Having three people on that list speaks volumes to our ability to identify those things that are issues in our healthcare system and impact them," says SHM President Robert Harrington Jr., MD, SFHM, chief medical officer at Reliant Post-Acute Care Solutions in Atlanta.
Dr. Harrington says that placing three hospitalists in the top 16 of a list like this one shows that while HM is a young specialty, it is at the nexus of dynamic change in care delivery.
"We've placed our bets in the right places when it comes to healthcare," he says. "[It] really is all about our patients, patient safety, quality, value."
Although Dr. Harrington likes the adulation the list can bring the specialty, he says if people move on and off of it, that's fine, too.
"As long as we continue to get a seat at the table in terms of healthcare policy formation and quality improvement organizations and patient safety organizations, and we continue to be respected in those arenas, for me, that’s what it’s about," he adds. "The list is nice, but the results are more important to us."
Visit our website for more information on hospitalist leadership.
Hospice, Palliative Care Groups Release Quality Care Measures
The American Academy of Hospice and Palliative Medicine (AAHPM) and the Hospice & Palliative Nurses Association (HPNA) recently published a list of performance measures to assess the quality of palliative and hospice patient care.
Refined over two years, the groups' Measuring What Matters recommendations [PDF] outline 10 clinically relevant measures to drive quality care. The list includes:
- Documenting patients’ preferences for life-sustaining treatments and their surrogate decision makers’ names;
- Screening patients for physical symptoms;
- Treating pain;
- Screening and managing dyspnea; and,
- Discussing patients' emotional and psychological needs.
"I'd say these things are relevant for hospitalists' patients, and for all seriously ill patients, whether or not a palliative care need has been identified," says Joe Rotella, MD, MBA, AAHPM's CMO and co-chair of the Measuring What Matters clinical user panel. The measures should make it possible to raise awareness about what constitutes quality of care for seriously ill patients and to compare quality between settings and between patients who receive palliative care and equally ill patients who do not, he notes.
The quality indicators, which have been reviewed by the National Quality Forum, focus on processes of providing palliative and hospice care and seek to achieve consistency in care quality among providers. For instance, do patients who screen positive for at least moderate pain receive treatments within 24 hours? Likewise, patients receiving hospice care should have a documented discussion of their spiritual concerns or of their preference not to have such a discussion, the recommendations state.
"It's worth looking at what really matters to these patients and maybe adapting a few measures for your hospital's quality improvement program," Dr. Rotella says.
Listen to our recent podcast on hospitalists and palliative care.
The American Academy of Hospice and Palliative Medicine (AAHPM) and the Hospice & Palliative Nurses Association (HPNA) recently published a list of performance measures to assess the quality of palliative and hospice patient care.
Refined over two years, the groups' Measuring What Matters recommendations [PDF] outline 10 clinically relevant measures to drive quality care. The list includes:
- Documenting patients’ preferences for life-sustaining treatments and their surrogate decision makers’ names;
- Screening patients for physical symptoms;
- Treating pain;
- Screening and managing dyspnea; and,
- Discussing patients' emotional and psychological needs.
"I'd say these things are relevant for hospitalists' patients, and for all seriously ill patients, whether or not a palliative care need has been identified," says Joe Rotella, MD, MBA, AAHPM's CMO and co-chair of the Measuring What Matters clinical user panel. The measures should make it possible to raise awareness about what constitutes quality of care for seriously ill patients and to compare quality between settings and between patients who receive palliative care and equally ill patients who do not, he notes.
The quality indicators, which have been reviewed by the National Quality Forum, focus on processes of providing palliative and hospice care and seek to achieve consistency in care quality among providers. For instance, do patients who screen positive for at least moderate pain receive treatments within 24 hours? Likewise, patients receiving hospice care should have a documented discussion of their spiritual concerns or of their preference not to have such a discussion, the recommendations state.
"It's worth looking at what really matters to these patients and maybe adapting a few measures for your hospital's quality improvement program," Dr. Rotella says.
Listen to our recent podcast on hospitalists and palliative care.
The American Academy of Hospice and Palliative Medicine (AAHPM) and the Hospice & Palliative Nurses Association (HPNA) recently published a list of performance measures to assess the quality of palliative and hospice patient care.
Refined over two years, the groups' Measuring What Matters recommendations [PDF] outline 10 clinically relevant measures to drive quality care. The list includes:
- Documenting patients’ preferences for life-sustaining treatments and their surrogate decision makers’ names;
- Screening patients for physical symptoms;
- Treating pain;
- Screening and managing dyspnea; and,
- Discussing patients' emotional and psychological needs.
"I'd say these things are relevant for hospitalists' patients, and for all seriously ill patients, whether or not a palliative care need has been identified," says Joe Rotella, MD, MBA, AAHPM's CMO and co-chair of the Measuring What Matters clinical user panel. The measures should make it possible to raise awareness about what constitutes quality of care for seriously ill patients and to compare quality between settings and between patients who receive palliative care and equally ill patients who do not, he notes.
The quality indicators, which have been reviewed by the National Quality Forum, focus on processes of providing palliative and hospice care and seek to achieve consistency in care quality among providers. For instance, do patients who screen positive for at least moderate pain receive treatments within 24 hours? Likewise, patients receiving hospice care should have a documented discussion of their spiritual concerns or of their preference not to have such a discussion, the recommendations state.
"It's worth looking at what really matters to these patients and maybe adapting a few measures for your hospital's quality improvement program," Dr. Rotella says.
Listen to our recent podcast on hospitalists and palliative care.
Hospital Medicine 2015 Photo Gallery - Day Three
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9476,9477,9479,9480,9481,9482,9483,9484,9485,9486,9487,9488,9489,9490,9491,9492,9493,9494,9495,9496,9497,9498,9499,9500,9501,9502,9503,9504,9505,9506,9507,9508,9509,9510,9511,9512,9516,9518,9519,9520,9521,9522,9523,9524,9525,9526,9528,9529,9530,9531,9532,9533,9534,9535,9536,9538,9540,9541,9542,9543,9545,9546,9548,9549,9551"]
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9476,9477,9479,9480,9481,9482,9483,9484,9485,9486,9487,9488,9489,9490,9491,9492,9493,9494,9495,9496,9497,9498,9499,9500,9501,9502,9503,9504,9505,9506,9507,9508,9509,9510,9511,9512,9516,9518,9519,9520,9521,9522,9523,9524,9525,9526,9528,9529,9530,9531,9532,9533,9534,9535,9536,9538,9540,9541,9542,9543,9545,9546,9548,9549,9551"]
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9476,9477,9479,9480,9481,9482,9483,9484,9485,9486,9487,9488,9489,9490,9491,9492,9493,9494,9495,9496,9497,9498,9499,9500,9501,9502,9503,9504,9505,9506,9507,9508,9509,9510,9511,9512,9516,9518,9519,9520,9521,9522,9523,9524,9525,9526,9528,9529,9530,9531,9532,9533,9534,9535,9536,9538,9540,9541,9542,9543,9545,9546,9548,9549,9551"]
Hospital Medicine 2015 Photo Gallery - Day Two
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9426,9427,9428,9429,9430,9431,9432,9433,9434,9435,9436,9437,9439,9440,9441,9442,9444,9445,9447,9449,9450,9451,9452,9453,9454,9455,9457,9458,9459,9460,9461,9462,9463,9464,9465,9467,9468,9469,9471,9472,9474"]
tk
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9426,9427,9428,9429,9430,9431,9432,9433,9434,9435,9436,9437,9439,9440,9441,9442,9444,9445,9447,9449,9450,9451,9452,9453,9454,9455,9457,9458,9459,9460,9461,9462,9463,9464,9465,9467,9468,9469,9471,9472,9474"]
tk
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9426,9427,9428,9429,9430,9431,9432,9433,9434,9435,9436,9437,9439,9440,9441,9442,9444,9445,9447,9449,9450,9451,9452,9453,9454,9455,9457,9458,9459,9460,9461,9462,9463,9464,9465,9467,9468,9469,9471,9472,9474"]
tk
Restrictive Transfusion Strategy No Benefit for Cardiac Surgery Patients
Clinical question: Does a restrictive transfusion strategy improve outcomes following nonemergent cardiac surgery?
Bottom line: For patients undergoing cardiac surgery, using a restrictive transfusion strategy with a hemoglobin threshold of 7.5 g/dL does not decrease serious infections or ischemic events and may lead to increased all-cause mortality at 90 days. (LOE = 1b)
Study design: Randomized controlled trial (single-blinded)
Funding source: Government
Allocation: Concealed
Setting: Inpatient (any location)
Synopsis
This is yet another study that compares restrictive and liberal transfusion strategies, this time in a cardiac surgery population. These investigators enrolled patients undergoing nonemergency cardiac surgery (mostly coronary artery bypass grafts or valvular procedures) who had a drop of hemoglobin level to below 9 g/dL following surgery.
Patients were randomized, using concealed allocation, to the restrictive transfusion threshold group (threshold hemoglobin 7.5 g/dL) or liberal transfusion threshold group (threshold hemoglobin 9 g/dL). Patients were masked but physicians and nurses were aware of the group assignments.
In the liberal group, patients received one unit of red cell transfusion immediately after randomization followed by an additional unit if the hemoglobin level remained below or dropped below 9 g/dL again during the hospitalization. In the restrictive group, patients received one unit of red cells only if the hemoglobin level dropped below 7.5 g/dL. An additional unit was then given if hemoglobin remained below or dropped below 7.5 g/dL again during the hospitalization. The 2 groups were similar at baseline and analysis was by intention to treat. Not surprisingly, more patients in the liberal strategy group received transfusions than did those in the restrictive strategy group (95% vs 64%).
For the primary outcome—a composite of sepsis, wound infection, stroke, myocardial infarction, gut infarction, or acute kidney injury within 3 months of randomization—there was no significant difference detected between the 2 groups. However, the restrictive group had a higher mortality rate than the liberal group (4.2% vs 2.6%; P = .045). Although this was a secondary outcome, it is possible that a restrictive strategy may be harmful in this cohort, given that they may have less cardiovascular reserve than the general patient population.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question: Does a restrictive transfusion strategy improve outcomes following nonemergent cardiac surgery?
Bottom line: For patients undergoing cardiac surgery, using a restrictive transfusion strategy with a hemoglobin threshold of 7.5 g/dL does not decrease serious infections or ischemic events and may lead to increased all-cause mortality at 90 days. (LOE = 1b)
Study design: Randomized controlled trial (single-blinded)
Funding source: Government
Allocation: Concealed
Setting: Inpatient (any location)
Synopsis
This is yet another study that compares restrictive and liberal transfusion strategies, this time in a cardiac surgery population. These investigators enrolled patients undergoing nonemergency cardiac surgery (mostly coronary artery bypass grafts or valvular procedures) who had a drop of hemoglobin level to below 9 g/dL following surgery.
Patients were randomized, using concealed allocation, to the restrictive transfusion threshold group (threshold hemoglobin 7.5 g/dL) or liberal transfusion threshold group (threshold hemoglobin 9 g/dL). Patients were masked but physicians and nurses were aware of the group assignments.
In the liberal group, patients received one unit of red cell transfusion immediately after randomization followed by an additional unit if the hemoglobin level remained below or dropped below 9 g/dL again during the hospitalization. In the restrictive group, patients received one unit of red cells only if the hemoglobin level dropped below 7.5 g/dL. An additional unit was then given if hemoglobin remained below or dropped below 7.5 g/dL again during the hospitalization. The 2 groups were similar at baseline and analysis was by intention to treat. Not surprisingly, more patients in the liberal strategy group received transfusions than did those in the restrictive strategy group (95% vs 64%).
For the primary outcome—a composite of sepsis, wound infection, stroke, myocardial infarction, gut infarction, or acute kidney injury within 3 months of randomization—there was no significant difference detected between the 2 groups. However, the restrictive group had a higher mortality rate than the liberal group (4.2% vs 2.6%; P = .045). Although this was a secondary outcome, it is possible that a restrictive strategy may be harmful in this cohort, given that they may have less cardiovascular reserve than the general patient population.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question: Does a restrictive transfusion strategy improve outcomes following nonemergent cardiac surgery?
Bottom line: For patients undergoing cardiac surgery, using a restrictive transfusion strategy with a hemoglobin threshold of 7.5 g/dL does not decrease serious infections or ischemic events and may lead to increased all-cause mortality at 90 days. (LOE = 1b)
Study design: Randomized controlled trial (single-blinded)
Funding source: Government
Allocation: Concealed
Setting: Inpatient (any location)
Synopsis
This is yet another study that compares restrictive and liberal transfusion strategies, this time in a cardiac surgery population. These investigators enrolled patients undergoing nonemergency cardiac surgery (mostly coronary artery bypass grafts or valvular procedures) who had a drop of hemoglobin level to below 9 g/dL following surgery.
Patients were randomized, using concealed allocation, to the restrictive transfusion threshold group (threshold hemoglobin 7.5 g/dL) or liberal transfusion threshold group (threshold hemoglobin 9 g/dL). Patients were masked but physicians and nurses were aware of the group assignments.
In the liberal group, patients received one unit of red cell transfusion immediately after randomization followed by an additional unit if the hemoglobin level remained below or dropped below 9 g/dL again during the hospitalization. In the restrictive group, patients received one unit of red cells only if the hemoglobin level dropped below 7.5 g/dL. An additional unit was then given if hemoglobin remained below or dropped below 7.5 g/dL again during the hospitalization. The 2 groups were similar at baseline and analysis was by intention to treat. Not surprisingly, more patients in the liberal strategy group received transfusions than did those in the restrictive strategy group (95% vs 64%).
For the primary outcome—a composite of sepsis, wound infection, stroke, myocardial infarction, gut infarction, or acute kidney injury within 3 months of randomization—there was no significant difference detected between the 2 groups. However, the restrictive group had a higher mortality rate than the liberal group (4.2% vs 2.6%; P = .045). Although this was a secondary outcome, it is possible that a restrictive strategy may be harmful in this cohort, given that they may have less cardiovascular reserve than the general patient population.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Endovascular Treatment for Acute Ischemic Stroke Decreases Mortality
Clinical question: Does endovascular treatment improve outcomes for patients with acute ischemic stroke?
Bottom line: For patients with acute ischemic stroke and imaging that suggests a proximal artery occlusion with evidence of good collateral circulation, the use of rapid endovascular treatment improves functional outcomes and reduces mortality. (LOE = 1b)
Study design: Randomized controlled trial (nonblinded)
Funding source: Industry
Allocation: Concealed
Setting: Inpatient (any location) with outpatient follow-up
Synopsis
The recent MR CLEAN study showed improved functional outcomes with the use of endovascular therapy for the treatment of acute ischemic stroke (N Engl J Med 2015;372:11-20).
In this study, investigators enrolled patients with acute disabling ischemic strokes and computed tomographic evidence of a small infarct core, an occluded proximal artery in the anterior circulation, and moderate-to-good collateral circulation. Patients were randomized, using concealed allocation, to receive either usual care or usual care plus rapid endovascular treatment with the use of mechanical thrombectomy and retrievable stents.
The 2 groups had similar baseline characteristics with a mean age of 70 years and a median National Institutes of Health Stroke Scale score of 16 to 17. The median time from stroke onset to reperfusion was 4 hours in the intervention group. The trial was stopped early because of the efficacy of the endovascular therapy. The primary outcome was a common odds ratio, indicating the odds of improvement by 1 point on the modified Rankin scale of 0 to 6 (0 = no symptoms, 1–2 = slight disability, 6 = death). This ratio favored the intervention (common odds ratio 2.6, 95% CI 1.7-3.8; P < .001).
Overall, at 90-day follow-up, the intervention group had a greater proportion of patients with a modified Rankin score of 0–2 (53% vs. 29%; P < .001), as well as decreased mortality (10% vs 19% in control group, P = .04). There was no difference between the 2 groups in the rate of symptomatic intracerebral bleeds.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question: Does endovascular treatment improve outcomes for patients with acute ischemic stroke?
Bottom line: For patients with acute ischemic stroke and imaging that suggests a proximal artery occlusion with evidence of good collateral circulation, the use of rapid endovascular treatment improves functional outcomes and reduces mortality. (LOE = 1b)
Study design: Randomized controlled trial (nonblinded)
Funding source: Industry
Allocation: Concealed
Setting: Inpatient (any location) with outpatient follow-up
Synopsis
The recent MR CLEAN study showed improved functional outcomes with the use of endovascular therapy for the treatment of acute ischemic stroke (N Engl J Med 2015;372:11-20).
In this study, investigators enrolled patients with acute disabling ischemic strokes and computed tomographic evidence of a small infarct core, an occluded proximal artery in the anterior circulation, and moderate-to-good collateral circulation. Patients were randomized, using concealed allocation, to receive either usual care or usual care plus rapid endovascular treatment with the use of mechanical thrombectomy and retrievable stents.
The 2 groups had similar baseline characteristics with a mean age of 70 years and a median National Institutes of Health Stroke Scale score of 16 to 17. The median time from stroke onset to reperfusion was 4 hours in the intervention group. The trial was stopped early because of the efficacy of the endovascular therapy. The primary outcome was a common odds ratio, indicating the odds of improvement by 1 point on the modified Rankin scale of 0 to 6 (0 = no symptoms, 1–2 = slight disability, 6 = death). This ratio favored the intervention (common odds ratio 2.6, 95% CI 1.7-3.8; P < .001).
Overall, at 90-day follow-up, the intervention group had a greater proportion of patients with a modified Rankin score of 0–2 (53% vs. 29%; P < .001), as well as decreased mortality (10% vs 19% in control group, P = .04). There was no difference between the 2 groups in the rate of symptomatic intracerebral bleeds.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question: Does endovascular treatment improve outcomes for patients with acute ischemic stroke?
Bottom line: For patients with acute ischemic stroke and imaging that suggests a proximal artery occlusion with evidence of good collateral circulation, the use of rapid endovascular treatment improves functional outcomes and reduces mortality. (LOE = 1b)
Study design: Randomized controlled trial (nonblinded)
Funding source: Industry
Allocation: Concealed
Setting: Inpatient (any location) with outpatient follow-up
Synopsis
The recent MR CLEAN study showed improved functional outcomes with the use of endovascular therapy for the treatment of acute ischemic stroke (N Engl J Med 2015;372:11-20).
In this study, investigators enrolled patients with acute disabling ischemic strokes and computed tomographic evidence of a small infarct core, an occluded proximal artery in the anterior circulation, and moderate-to-good collateral circulation. Patients were randomized, using concealed allocation, to receive either usual care or usual care plus rapid endovascular treatment with the use of mechanical thrombectomy and retrievable stents.
The 2 groups had similar baseline characteristics with a mean age of 70 years and a median National Institutes of Health Stroke Scale score of 16 to 17. The median time from stroke onset to reperfusion was 4 hours in the intervention group. The trial was stopped early because of the efficacy of the endovascular therapy. The primary outcome was a common odds ratio, indicating the odds of improvement by 1 point on the modified Rankin scale of 0 to 6 (0 = no symptoms, 1–2 = slight disability, 6 = death). This ratio favored the intervention (common odds ratio 2.6, 95% CI 1.7-3.8; P < .001).
Overall, at 90-day follow-up, the intervention group had a greater proportion of patients with a modified Rankin score of 0–2 (53% vs. 29%; P < .001), as well as decreased mortality (10% vs 19% in control group, P = .04). There was no difference between the 2 groups in the rate of symptomatic intracerebral bleeds.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Hospital Medicine 2015 Photo Gallery - Day One
Photographs from the first day of Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9553,9555,9556,9557,9558,9559,9560,9561,9562,9563,9564,9565,9566,9567,9568,9569,9570,9571,9572,9573,9574,9575,9576,9577,9578,9579,9580,9581,9582,9583,9584"]
Photographs from the first day of Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9553,9555,9556,9557,9558,9559,9560,9561,9562,9563,9564,9565,9566,9567,9568,9569,9570,9571,9572,9573,9574,9575,9576,9577,9578,9579,9580,9581,9582,9583,9584"]
Photographs from the first day of Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9553,9555,9556,9557,9558,9559,9560,9561,9562,9563,9564,9565,9566,9567,9568,9569,9570,9571,9572,9573,9574,9575,9576,9577,9578,9579,9580,9581,9582,9583,9584"]
Society of Hospital Medicine’s RIV Poster Contest Draws Best, Brightest
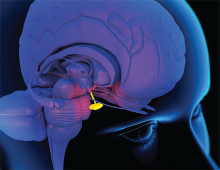
When Should Hypopituitarism Be Suspected?
Case
A 53-year-old woman with a history of a suprasellar meningioma resected nine years ago with recurrence of a 4.5x2 cm mass one year ago and recent ventriculoperitoneal (VP) shunt placement for hydrocephalus presented with altered mental status (AMS) and hallucinations. She was admitted for radiation therapy to the mass. The patient had little improvement in her mental status four weeks into a six-week, 4860 cGy course of photon therapy.
The internal medicine service was consulted for new onset tachycardia (103), hypotension (83/55), and fever (38.6 C). Laboratory data revealed a white blood cell count 4.8 x 109 cells/L, sodium 137 mmol/L, potassium 4.1 mmol/L, chloride 110 mmol/L, bicarbonate 28 mmol/L, blood urea nitrogen 3 mg/dl, creatinine 0.6 mg/dl, and glucose 91 mg/dl. Thyroid-stimulating hormone (TSH) was low at 0.38 mIU/mL. Urine specific gravity was 1.006. Workups for infectious and thromboembolic diseases were unremarkable.
Discussion
Hypopituitarism is a disorder of impaired hormone production from the anterior and, less commonly, posterior pituitary gland. The condition can originate from several broad categories of diseases affecting the hypothalamus, pituitary stalk, or pituitary gland. In adults, the etiology is often from the mass effect of tumors or from treatment with surgery or radiotherapy. Other causes include vascular, infectious, infiltrative, inflammatory, and idiopathic. Well-substantiated data on the incidence and prevalence of hypopituitarism is sparse. It has an estimated prevalence of 45.5 cases per 100,000 and incidence of 4.2 cases per 100,000 per year.1
Clinical manifestations of hypopituitarism depend on the type and severity of hormone deficiency. The consequences of adrenal insufficiency (AI) range from smoldering and nonspecific findings (e.g. fatigue, lethargy, indistinct gastrointestinal symptoms, eosinophilia, fever) to full-fledged crisis (e.g. AMS, severe electrolyte abnormalities, hemodynamic compromise, shock). The presentation of central AI (i.e., arising from hypothalamic or pituitary pathology) is often more subtle than primary AI. In central AI, only glucocorticoid (GC) function is disrupted, leaving the renin-angiotensin-aldosterone system and mineralocorticoid (MC) function intact. This is in stark contrast to primary AI resulting from direct adrenal gland injury, which nearly always disrupts both GC and MC function, leading to more profound circulatory collapse and electrolyte disturbance.2
Aside from orthostatic blood pressure or possible low-grade fever, few physical exam features are associated with central AI. Hyperpigmentation is not seen due to the lack of anterior pituitary-derived melanocortins that stimulate melanocytes and induce pigmentation. As for laboratory findings, hyperkalemia is a feature of primary AI (due to hypoaldosteronism) but is not seen in central AI. Hyponatremia occurs in both types of AI and is vasopressin-mediated. Hyponatremia is more common in primary AI, resulting from appropriate vasopressin release that occurs due to hypotension. Hyponatremia also occurs in secondary AI because of increased vasopressin secretion mediated directly by hypocortisolemia.3,4
In summary, hyperpigmentation and the electrolyte pattern of hyponatremia and hyperkalemia are distinguishing clinical characteristics of primary AI, occurring in up to 90% of cases, but these features would not be expected with central AI.5
In the hospitalized patient with multiple active acute illnesses and infectious risk factors, it can be difficult to recognize the diagnosis of AI or hypopituitarism. Not only do signs and symptoms frequently overlap, but concomitant acute illness is usually a triggering event. Crisis should be suspected in the setting of unexplained fever, dehydration, or shock out of proportion to severity of current illness.5
Not surprisingly, high rates of partial or complete hypopituitarism are seen in patients following surgical removal of pituitary tumors or nearby neoplasms (e.g. craniopharyngiomas). Both surgery and radiotherapy for non-pituitary brain tumors are also major risk factors for development of hypopituitarism, occurring in up to 38% and 41% of patients, respectively.6 The strongest predictors of hormone failure are higher radiation doses, proximity to the pituitary-hypothalamus, and longer time interval after completion of radiotherapy. Within 10 years after a median dose of 5000 rad (50Gy) directed at the skull base, nasopharynx, or cranium, up to three-fourths of patients will develop some degree of pituitary insufficiency. Later onset of hormone failure usually reflects hypothalamic injury, whereas higher irradiation doses can lead to earlier onset pituitary damage.5
Not all hormone-secreting cells of the hypothalamus or pituitary are equally susceptible to injury; there is a characteristic sequence of hormonal failure. The typical order of hormone deficiency from pituitary compression or destruction is as follows: growth hormone (GH) > follicle-stimulating hormone (FSH) > luteinizing hormone (LH) > TSH > adrenocorticotropic hormone (ACTH) > vasopressin. A similar pattern is seen following brain irradiation: GH > FSH and LH > ACTH > TSH. A recent systematic review of 18 studies with 813 patients receiving cranial radiotherapy for non-pituitary tumors found pituitary dysfunction was 45% for GH deficiency, compared to 22% for ACTH deficiency.7
Biochemical diagnosis of hypopituitarism consists of measuring the various pituitary and target hormone levels as well as provocation testing. When interpreting these tests, whether to identify excess or deficient states, it is important to remember the individual values are part of the broader hypothalamic-pituitary axis feedback loops. Thus, it can be more useful designating if a high or low test value is appropriately or inappropriately high or low. In the presented case, low TSH level could be misinterpreted as excess thyroid hormone supplementation. An appropriately elevated free T4 level would confirm this, but an inappropriately low free T4 would raise suspicion of central hypothalamic-pituitary dysfunction.
With high enough clinical suspicion of hypopituitarism, empiric treatment with thyroid supplementation and corticosteroids should be started before confirmation of the diagnosis, to prevent secondary organ dysfunction and improve morbidity and mortality.2 Rapid administration with intravenous levothyroxine can be given in severe hypothyroidism or myxedema.
“Stress-dose” steroids are generally recommended for patients who are also administered levothyroxine, as the desired increased in metabolic rate can deplete existing pituitary-adrenocortical hormone reserves, precipitating adrenal crisis.5 Stress-dose corticosteroids also ensure recruitment of a mineralocorticoid response. Cortisol has both GC and MC stimulating effects but is rapidly metabolized to cortisone, which lacks MC stimulating effects. Thus, high doses overwhelm this conversion step and allow remaining cortisol to stimulate MC receptors.2 These high doses may not be necessary in secondary AI (i.e., preserved MC function) but would be reasonable in an unstable patient or until confirmation is made with an inappropriately low ACTH.
Back to the Case
Morning cortisol returned undetectable, and ACTH was 14 pg/mL (6-58). Past records revealed a down-trending TSH from 1.12 to 0.38 mIU/mL, which had inappropriately prompted a levothyroxine dose reduction from 50 mcg to 25 mcg. A free thyroxine (T4) was low at 0.67 ng/dL (0.89-1.76). Estradiol, FSH, and LH were undetectable. Prolactin was 23 ng/mL (3-27). She was started on prednisone, 5 mg daily, and her levothyroxine was adjusted to a weight-based dose. Her fever resolved with the initiation of prednisone, and all cultures remained negative. Over two weeks, she improved back to her baseline, was discharged to a rehabilitation center, and eventually returned home.
Dr. Inman is a hospitalist at St. Mary’s Hospital and Regional Medical Center in Grand Junction, Colo. Dr. Bridenstine is an endocrinologist at the University of Colorado Denver. Dr. Cumbler is a hospitalist at the University of Colorado Denver.
References
- Regal M, Pàramo C, Sierra SM, Garcia-Mayor RV. Prevalence and incidence of hypopituitarism in an adult Caucasian population in northwestern Spain. Clin Endocrinol. 2001;55(6):735-740.
- Bouillon R. Acute adrenal insufficiency. Endocrinol Metab Clin North Am. 2006;35(4):767-75, ix.
- Raff H. Glucocorticoid inhibition of neurohypophysial vasopressin secretion. Am J Physiol. 1987;252(4 Pt 2):R635-644.
- Erkut ZA, Pool C, Swaab DF. Glucocorticoids suppress corticotropin-releasing hormone and vasopressin expression in human hypothalamic neurons. J Clin Endocrinol Metab. 1998;83(6):2066-2073.
- Melmed S, Polonski KS, Reed Larsen P, Kronenberg HM. Williams Textbook of Endocrinology. 12th ed. Philadelphia, Pa.: Saunders/Elsevier; 2012.
- Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E. Hypopituitarism. Lancet. 2007;369(9571):1461-1470.
- Appelman-Dijkstra NM, Kokshoorn NE, Dekkers OM, et al. Pituitary dysfunction in adult patients after cranial radiotherapy: systematic review and meta-analysis. J Clin Endocrinol Metabol. 2011;96(8):2330-2340.
Case
A 53-year-old woman with a history of a suprasellar meningioma resected nine years ago with recurrence of a 4.5x2 cm mass one year ago and recent ventriculoperitoneal (VP) shunt placement for hydrocephalus presented with altered mental status (AMS) and hallucinations. She was admitted for radiation therapy to the mass. The patient had little improvement in her mental status four weeks into a six-week, 4860 cGy course of photon therapy.
The internal medicine service was consulted for new onset tachycardia (103), hypotension (83/55), and fever (38.6 C). Laboratory data revealed a white blood cell count 4.8 x 109 cells/L, sodium 137 mmol/L, potassium 4.1 mmol/L, chloride 110 mmol/L, bicarbonate 28 mmol/L, blood urea nitrogen 3 mg/dl, creatinine 0.6 mg/dl, and glucose 91 mg/dl. Thyroid-stimulating hormone (TSH) was low at 0.38 mIU/mL. Urine specific gravity was 1.006. Workups for infectious and thromboembolic diseases were unremarkable.
Discussion
Hypopituitarism is a disorder of impaired hormone production from the anterior and, less commonly, posterior pituitary gland. The condition can originate from several broad categories of diseases affecting the hypothalamus, pituitary stalk, or pituitary gland. In adults, the etiology is often from the mass effect of tumors or from treatment with surgery or radiotherapy. Other causes include vascular, infectious, infiltrative, inflammatory, and idiopathic. Well-substantiated data on the incidence and prevalence of hypopituitarism is sparse. It has an estimated prevalence of 45.5 cases per 100,000 and incidence of 4.2 cases per 100,000 per year.1
Clinical manifestations of hypopituitarism depend on the type and severity of hormone deficiency. The consequences of adrenal insufficiency (AI) range from smoldering and nonspecific findings (e.g. fatigue, lethargy, indistinct gastrointestinal symptoms, eosinophilia, fever) to full-fledged crisis (e.g. AMS, severe electrolyte abnormalities, hemodynamic compromise, shock). The presentation of central AI (i.e., arising from hypothalamic or pituitary pathology) is often more subtle than primary AI. In central AI, only glucocorticoid (GC) function is disrupted, leaving the renin-angiotensin-aldosterone system and mineralocorticoid (MC) function intact. This is in stark contrast to primary AI resulting from direct adrenal gland injury, which nearly always disrupts both GC and MC function, leading to more profound circulatory collapse and electrolyte disturbance.2
Aside from orthostatic blood pressure or possible low-grade fever, few physical exam features are associated with central AI. Hyperpigmentation is not seen due to the lack of anterior pituitary-derived melanocortins that stimulate melanocytes and induce pigmentation. As for laboratory findings, hyperkalemia is a feature of primary AI (due to hypoaldosteronism) but is not seen in central AI. Hyponatremia occurs in both types of AI and is vasopressin-mediated. Hyponatremia is more common in primary AI, resulting from appropriate vasopressin release that occurs due to hypotension. Hyponatremia also occurs in secondary AI because of increased vasopressin secretion mediated directly by hypocortisolemia.3,4
In summary, hyperpigmentation and the electrolyte pattern of hyponatremia and hyperkalemia are distinguishing clinical characteristics of primary AI, occurring in up to 90% of cases, but these features would not be expected with central AI.5
In the hospitalized patient with multiple active acute illnesses and infectious risk factors, it can be difficult to recognize the diagnosis of AI or hypopituitarism. Not only do signs and symptoms frequently overlap, but concomitant acute illness is usually a triggering event. Crisis should be suspected in the setting of unexplained fever, dehydration, or shock out of proportion to severity of current illness.5
Not surprisingly, high rates of partial or complete hypopituitarism are seen in patients following surgical removal of pituitary tumors or nearby neoplasms (e.g. craniopharyngiomas). Both surgery and radiotherapy for non-pituitary brain tumors are also major risk factors for development of hypopituitarism, occurring in up to 38% and 41% of patients, respectively.6 The strongest predictors of hormone failure are higher radiation doses, proximity to the pituitary-hypothalamus, and longer time interval after completion of radiotherapy. Within 10 years after a median dose of 5000 rad (50Gy) directed at the skull base, nasopharynx, or cranium, up to three-fourths of patients will develop some degree of pituitary insufficiency. Later onset of hormone failure usually reflects hypothalamic injury, whereas higher irradiation doses can lead to earlier onset pituitary damage.5
Not all hormone-secreting cells of the hypothalamus or pituitary are equally susceptible to injury; there is a characteristic sequence of hormonal failure. The typical order of hormone deficiency from pituitary compression or destruction is as follows: growth hormone (GH) > follicle-stimulating hormone (FSH) > luteinizing hormone (LH) > TSH > adrenocorticotropic hormone (ACTH) > vasopressin. A similar pattern is seen following brain irradiation: GH > FSH and LH > ACTH > TSH. A recent systematic review of 18 studies with 813 patients receiving cranial radiotherapy for non-pituitary tumors found pituitary dysfunction was 45% for GH deficiency, compared to 22% for ACTH deficiency.7
Biochemical diagnosis of hypopituitarism consists of measuring the various pituitary and target hormone levels as well as provocation testing. When interpreting these tests, whether to identify excess or deficient states, it is important to remember the individual values are part of the broader hypothalamic-pituitary axis feedback loops. Thus, it can be more useful designating if a high or low test value is appropriately or inappropriately high or low. In the presented case, low TSH level could be misinterpreted as excess thyroid hormone supplementation. An appropriately elevated free T4 level would confirm this, but an inappropriately low free T4 would raise suspicion of central hypothalamic-pituitary dysfunction.
With high enough clinical suspicion of hypopituitarism, empiric treatment with thyroid supplementation and corticosteroids should be started before confirmation of the diagnosis, to prevent secondary organ dysfunction and improve morbidity and mortality.2 Rapid administration with intravenous levothyroxine can be given in severe hypothyroidism or myxedema.
“Stress-dose” steroids are generally recommended for patients who are also administered levothyroxine, as the desired increased in metabolic rate can deplete existing pituitary-adrenocortical hormone reserves, precipitating adrenal crisis.5 Stress-dose corticosteroids also ensure recruitment of a mineralocorticoid response. Cortisol has both GC and MC stimulating effects but is rapidly metabolized to cortisone, which lacks MC stimulating effects. Thus, high doses overwhelm this conversion step and allow remaining cortisol to stimulate MC receptors.2 These high doses may not be necessary in secondary AI (i.e., preserved MC function) but would be reasonable in an unstable patient or until confirmation is made with an inappropriately low ACTH.
Back to the Case
Morning cortisol returned undetectable, and ACTH was 14 pg/mL (6-58). Past records revealed a down-trending TSH from 1.12 to 0.38 mIU/mL, which had inappropriately prompted a levothyroxine dose reduction from 50 mcg to 25 mcg. A free thyroxine (T4) was low at 0.67 ng/dL (0.89-1.76). Estradiol, FSH, and LH were undetectable. Prolactin was 23 ng/mL (3-27). She was started on prednisone, 5 mg daily, and her levothyroxine was adjusted to a weight-based dose. Her fever resolved with the initiation of prednisone, and all cultures remained negative. Over two weeks, she improved back to her baseline, was discharged to a rehabilitation center, and eventually returned home.
Dr. Inman is a hospitalist at St. Mary’s Hospital and Regional Medical Center in Grand Junction, Colo. Dr. Bridenstine is an endocrinologist at the University of Colorado Denver. Dr. Cumbler is a hospitalist at the University of Colorado Denver.
References
- Regal M, Pàramo C, Sierra SM, Garcia-Mayor RV. Prevalence and incidence of hypopituitarism in an adult Caucasian population in northwestern Spain. Clin Endocrinol. 2001;55(6):735-740.
- Bouillon R. Acute adrenal insufficiency. Endocrinol Metab Clin North Am. 2006;35(4):767-75, ix.
- Raff H. Glucocorticoid inhibition of neurohypophysial vasopressin secretion. Am J Physiol. 1987;252(4 Pt 2):R635-644.
- Erkut ZA, Pool C, Swaab DF. Glucocorticoids suppress corticotropin-releasing hormone and vasopressin expression in human hypothalamic neurons. J Clin Endocrinol Metab. 1998;83(6):2066-2073.
- Melmed S, Polonski KS, Reed Larsen P, Kronenberg HM. Williams Textbook of Endocrinology. 12th ed. Philadelphia, Pa.: Saunders/Elsevier; 2012.
- Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E. Hypopituitarism. Lancet. 2007;369(9571):1461-1470.
- Appelman-Dijkstra NM, Kokshoorn NE, Dekkers OM, et al. Pituitary dysfunction in adult patients after cranial radiotherapy: systematic review and meta-analysis. J Clin Endocrinol Metabol. 2011;96(8):2330-2340.
Case
A 53-year-old woman with a history of a suprasellar meningioma resected nine years ago with recurrence of a 4.5x2 cm mass one year ago and recent ventriculoperitoneal (VP) shunt placement for hydrocephalus presented with altered mental status (AMS) and hallucinations. She was admitted for radiation therapy to the mass. The patient had little improvement in her mental status four weeks into a six-week, 4860 cGy course of photon therapy.
The internal medicine service was consulted for new onset tachycardia (103), hypotension (83/55), and fever (38.6 C). Laboratory data revealed a white blood cell count 4.8 x 109 cells/L, sodium 137 mmol/L, potassium 4.1 mmol/L, chloride 110 mmol/L, bicarbonate 28 mmol/L, blood urea nitrogen 3 mg/dl, creatinine 0.6 mg/dl, and glucose 91 mg/dl. Thyroid-stimulating hormone (TSH) was low at 0.38 mIU/mL. Urine specific gravity was 1.006. Workups for infectious and thromboembolic diseases were unremarkable.
Discussion
Hypopituitarism is a disorder of impaired hormone production from the anterior and, less commonly, posterior pituitary gland. The condition can originate from several broad categories of diseases affecting the hypothalamus, pituitary stalk, or pituitary gland. In adults, the etiology is often from the mass effect of tumors or from treatment with surgery or radiotherapy. Other causes include vascular, infectious, infiltrative, inflammatory, and idiopathic. Well-substantiated data on the incidence and prevalence of hypopituitarism is sparse. It has an estimated prevalence of 45.5 cases per 100,000 and incidence of 4.2 cases per 100,000 per year.1
Clinical manifestations of hypopituitarism depend on the type and severity of hormone deficiency. The consequences of adrenal insufficiency (AI) range from smoldering and nonspecific findings (e.g. fatigue, lethargy, indistinct gastrointestinal symptoms, eosinophilia, fever) to full-fledged crisis (e.g. AMS, severe electrolyte abnormalities, hemodynamic compromise, shock). The presentation of central AI (i.e., arising from hypothalamic or pituitary pathology) is often more subtle than primary AI. In central AI, only glucocorticoid (GC) function is disrupted, leaving the renin-angiotensin-aldosterone system and mineralocorticoid (MC) function intact. This is in stark contrast to primary AI resulting from direct adrenal gland injury, which nearly always disrupts both GC and MC function, leading to more profound circulatory collapse and electrolyte disturbance.2
Aside from orthostatic blood pressure or possible low-grade fever, few physical exam features are associated with central AI. Hyperpigmentation is not seen due to the lack of anterior pituitary-derived melanocortins that stimulate melanocytes and induce pigmentation. As for laboratory findings, hyperkalemia is a feature of primary AI (due to hypoaldosteronism) but is not seen in central AI. Hyponatremia occurs in both types of AI and is vasopressin-mediated. Hyponatremia is more common in primary AI, resulting from appropriate vasopressin release that occurs due to hypotension. Hyponatremia also occurs in secondary AI because of increased vasopressin secretion mediated directly by hypocortisolemia.3,4
In summary, hyperpigmentation and the electrolyte pattern of hyponatremia and hyperkalemia are distinguishing clinical characteristics of primary AI, occurring in up to 90% of cases, but these features would not be expected with central AI.5
In the hospitalized patient with multiple active acute illnesses and infectious risk factors, it can be difficult to recognize the diagnosis of AI or hypopituitarism. Not only do signs and symptoms frequently overlap, but concomitant acute illness is usually a triggering event. Crisis should be suspected in the setting of unexplained fever, dehydration, or shock out of proportion to severity of current illness.5
Not surprisingly, high rates of partial or complete hypopituitarism are seen in patients following surgical removal of pituitary tumors or nearby neoplasms (e.g. craniopharyngiomas). Both surgery and radiotherapy for non-pituitary brain tumors are also major risk factors for development of hypopituitarism, occurring in up to 38% and 41% of patients, respectively.6 The strongest predictors of hormone failure are higher radiation doses, proximity to the pituitary-hypothalamus, and longer time interval after completion of radiotherapy. Within 10 years after a median dose of 5000 rad (50Gy) directed at the skull base, nasopharynx, or cranium, up to three-fourths of patients will develop some degree of pituitary insufficiency. Later onset of hormone failure usually reflects hypothalamic injury, whereas higher irradiation doses can lead to earlier onset pituitary damage.5
Not all hormone-secreting cells of the hypothalamus or pituitary are equally susceptible to injury; there is a characteristic sequence of hormonal failure. The typical order of hormone deficiency from pituitary compression or destruction is as follows: growth hormone (GH) > follicle-stimulating hormone (FSH) > luteinizing hormone (LH) > TSH > adrenocorticotropic hormone (ACTH) > vasopressin. A similar pattern is seen following brain irradiation: GH > FSH and LH > ACTH > TSH. A recent systematic review of 18 studies with 813 patients receiving cranial radiotherapy for non-pituitary tumors found pituitary dysfunction was 45% for GH deficiency, compared to 22% for ACTH deficiency.7
Biochemical diagnosis of hypopituitarism consists of measuring the various pituitary and target hormone levels as well as provocation testing. When interpreting these tests, whether to identify excess or deficient states, it is important to remember the individual values are part of the broader hypothalamic-pituitary axis feedback loops. Thus, it can be more useful designating if a high or low test value is appropriately or inappropriately high or low. In the presented case, low TSH level could be misinterpreted as excess thyroid hormone supplementation. An appropriately elevated free T4 level would confirm this, but an inappropriately low free T4 would raise suspicion of central hypothalamic-pituitary dysfunction.
With high enough clinical suspicion of hypopituitarism, empiric treatment with thyroid supplementation and corticosteroids should be started before confirmation of the diagnosis, to prevent secondary organ dysfunction and improve morbidity and mortality.2 Rapid administration with intravenous levothyroxine can be given in severe hypothyroidism or myxedema.
“Stress-dose” steroids are generally recommended for patients who are also administered levothyroxine, as the desired increased in metabolic rate can deplete existing pituitary-adrenocortical hormone reserves, precipitating adrenal crisis.5 Stress-dose corticosteroids also ensure recruitment of a mineralocorticoid response. Cortisol has both GC and MC stimulating effects but is rapidly metabolized to cortisone, which lacks MC stimulating effects. Thus, high doses overwhelm this conversion step and allow remaining cortisol to stimulate MC receptors.2 These high doses may not be necessary in secondary AI (i.e., preserved MC function) but would be reasonable in an unstable patient or until confirmation is made with an inappropriately low ACTH.
Back to the Case
Morning cortisol returned undetectable, and ACTH was 14 pg/mL (6-58). Past records revealed a down-trending TSH from 1.12 to 0.38 mIU/mL, which had inappropriately prompted a levothyroxine dose reduction from 50 mcg to 25 mcg. A free thyroxine (T4) was low at 0.67 ng/dL (0.89-1.76). Estradiol, FSH, and LH were undetectable. Prolactin was 23 ng/mL (3-27). She was started on prednisone, 5 mg daily, and her levothyroxine was adjusted to a weight-based dose. Her fever resolved with the initiation of prednisone, and all cultures remained negative. Over two weeks, she improved back to her baseline, was discharged to a rehabilitation center, and eventually returned home.
Dr. Inman is a hospitalist at St. Mary’s Hospital and Regional Medical Center in Grand Junction, Colo. Dr. Bridenstine is an endocrinologist at the University of Colorado Denver. Dr. Cumbler is a hospitalist at the University of Colorado Denver.
References
- Regal M, Pàramo C, Sierra SM, Garcia-Mayor RV. Prevalence and incidence of hypopituitarism in an adult Caucasian population in northwestern Spain. Clin Endocrinol. 2001;55(6):735-740.
- Bouillon R. Acute adrenal insufficiency. Endocrinol Metab Clin North Am. 2006;35(4):767-75, ix.
- Raff H. Glucocorticoid inhibition of neurohypophysial vasopressin secretion. Am J Physiol. 1987;252(4 Pt 2):R635-644.
- Erkut ZA, Pool C, Swaab DF. Glucocorticoids suppress corticotropin-releasing hormone and vasopressin expression in human hypothalamic neurons. J Clin Endocrinol Metab. 1998;83(6):2066-2073.
- Melmed S, Polonski KS, Reed Larsen P, Kronenberg HM. Williams Textbook of Endocrinology. 12th ed. Philadelphia, Pa.: Saunders/Elsevier; 2012.
- Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E. Hypopituitarism. Lancet. 2007;369(9571):1461-1470.
- Appelman-Dijkstra NM, Kokshoorn NE, Dekkers OM, et al. Pituitary dysfunction in adult patients after cranial radiotherapy: systematic review and meta-analysis. J Clin Endocrinol Metabol. 2011;96(8):2330-2340.
Hospital Medicine 2015 Photo Gallery - Day Four
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9197,9196,9195,9194,9193,9192,9191,9190,9189,9188,9187,9186,9185,9184,9183,9182,9181,9180,9179,9178,9177,9176,9175,9171"]
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9197,9196,9195,9194,9193,9192,9191,9190,9189,9188,9187,9186,9185,9184,9183,9182,9181,9180,9179,9178,9177,9176,9175,9171"]
Photographs from Hospital Medicine 2015, which took place March 29-April 1 at the Gaylord National Hotel and Conference Center in National Harbor, Md.
Photos by Manuel Noguera
[gallery ids="9197,9196,9195,9194,9193,9192,9191,9190,9189,9188,9187,9186,9185,9184,9183,9182,9181,9180,9179,9178,9177,9176,9175,9171"]