User login
Hospitalists’ Skill Sets, Work Experience Perfect for Hospitals' C-Suite Positions
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
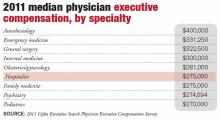
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
New SHM President Outlines “Next Evolution” of Hospitalist Practice
LAS VEGAS—Newly minted SHM President Burke Kealey, MD, SFHM, wants hospitalists to change how they look at health-care affordability, patient health, and the patient experience: He wants you to view them as one thing, not three.
“We put the energy and the effort of the moment behind the squeaky wheel,” Dr. Kealey said in his inaugural address Wednesday at the Mandalay Bay Resort and Casino. “What I would like us to do is all start thinking about all three at the same time, and with equal weight at all times. To me, this is the next evolution of the hospitalist.”
Dr. Kealey, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., borrowed the approach from the Institute of Healthcare Improvement, whose “Triple Aim” initiative has the same goals. In his address, he told HM14 attendees that to focus on any of the three areas while giving short shrift to the others misses the point of bettering the overall health-care system.
“To improve health, but then people can’t afford that health care, is a nonstarter,” he said. “To make things finally affordable, but then people stay away because it’s a bad experience, makes no sense, either. We must do it all together.”
Dr. Kealey, who replaces Eric Howell, MD, SFHM, as president for the next year, says that as value-based purchasing further connects cost of care to the quality of delivery, hospitalists who link health, experience, and affordability will have success.
“This movement goes beyond just improving scores,” he says. “It improves the health of our patients.”
LAS VEGAS—Newly minted SHM President Burke Kealey, MD, SFHM, wants hospitalists to change how they look at health-care affordability, patient health, and the patient experience: He wants you to view them as one thing, not three.
“We put the energy and the effort of the moment behind the squeaky wheel,” Dr. Kealey said in his inaugural address Wednesday at the Mandalay Bay Resort and Casino. “What I would like us to do is all start thinking about all three at the same time, and with equal weight at all times. To me, this is the next evolution of the hospitalist.”
Dr. Kealey, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., borrowed the approach from the Institute of Healthcare Improvement, whose “Triple Aim” initiative has the same goals. In his address, he told HM14 attendees that to focus on any of the three areas while giving short shrift to the others misses the point of bettering the overall health-care system.
“To improve health, but then people can’t afford that health care, is a nonstarter,” he said. “To make things finally affordable, but then people stay away because it’s a bad experience, makes no sense, either. We must do it all together.”
Dr. Kealey, who replaces Eric Howell, MD, SFHM, as president for the next year, says that as value-based purchasing further connects cost of care to the quality of delivery, hospitalists who link health, experience, and affordability will have success.
“This movement goes beyond just improving scores,” he says. “It improves the health of our patients.”
LAS VEGAS—Newly minted SHM President Burke Kealey, MD, SFHM, wants hospitalists to change how they look at health-care affordability, patient health, and the patient experience: He wants you to view them as one thing, not three.
“We put the energy and the effort of the moment behind the squeaky wheel,” Dr. Kealey said in his inaugural address Wednesday at the Mandalay Bay Resort and Casino. “What I would like us to do is all start thinking about all three at the same time, and with equal weight at all times. To me, this is the next evolution of the hospitalist.”
Dr. Kealey, medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn., borrowed the approach from the Institute of Healthcare Improvement, whose “Triple Aim” initiative has the same goals. In his address, he told HM14 attendees that to focus on any of the three areas while giving short shrift to the others misses the point of bettering the overall health-care system.
“To improve health, but then people can’t afford that health care, is a nonstarter,” he said. “To make things finally affordable, but then people stay away because it’s a bad experience, makes no sense, either. We must do it all together.”
Dr. Kealey, who replaces Eric Howell, MD, SFHM, as president for the next year, says that as value-based purchasing further connects cost of care to the quality of delivery, hospitalists who link health, experience, and affordability will have success.
“This movement goes beyond just improving scores,” he says. “It improves the health of our patients.”
Grassroots Hospitalists Anxious for Bob Wachter’s Keynote
LAS VEGAS—Hospitalist Jennifer Johnson, MD, knows exactly where she’ll be at noon today: sitting in a banquet chair listening to “the father of hospital medicine,” Bob Wachter, MD, MHM, give his annual meeting address.
When you work in technology, “you don’t get to listen to Bill Gates talk,” says Dr. Johnson, who practices at Aurora Medical Center in Grafton, Wis. “It’s one of the few times you get to be in the same room with and hear how the real people at the forefront are thinking. I think that’s very helpful.”
Dr. Johnson, who last heard Dr. Wachter speak at HM12 in San Diego, says she relishes his vision, which goes beyond what most hospitalists’ day-to-day duties encompass.
“No matter what your vocation is, it’s always good to be reminded what more you could do,” she says. “How better you could improve yourself. Instead of stagnating…there’s always a next level, a next step. He’s the guy who thinks that way.”
She’s not alone in that view. Dr. Wachter’s presentation has become a rite of SHM’s annual meeting and an unofficial wrap-up of the four-day convention. This year’s edition is titled “Ten Years of Wachter Keynote: And Now For Something Completely Different.”
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., spoke with Dr. Wachter earlier this week, as he wasn’t sure he could stay long enough for the formal address. But whether it’s Dr. Wachter or any of the keynote speakers, Dr. Kartham enjoys hearing HM’s leaders give advice.
“When you’re individual physicians,” he says, “you don’t know what to expect in the future. When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
For his part, Dr. Wachter has been priming the crowd for his talk. Earlier this week, he tweeted about his talk: “last 6 min wil b highlight (or lowlite) of conf, posibly of my life.”
LAS VEGAS—Hospitalist Jennifer Johnson, MD, knows exactly where she’ll be at noon today: sitting in a banquet chair listening to “the father of hospital medicine,” Bob Wachter, MD, MHM, give his annual meeting address.
When you work in technology, “you don’t get to listen to Bill Gates talk,” says Dr. Johnson, who practices at Aurora Medical Center in Grafton, Wis. “It’s one of the few times you get to be in the same room with and hear how the real people at the forefront are thinking. I think that’s very helpful.”
Dr. Johnson, who last heard Dr. Wachter speak at HM12 in San Diego, says she relishes his vision, which goes beyond what most hospitalists’ day-to-day duties encompass.
“No matter what your vocation is, it’s always good to be reminded what more you could do,” she says. “How better you could improve yourself. Instead of stagnating…there’s always a next level, a next step. He’s the guy who thinks that way.”
She’s not alone in that view. Dr. Wachter’s presentation has become a rite of SHM’s annual meeting and an unofficial wrap-up of the four-day convention. This year’s edition is titled “Ten Years of Wachter Keynote: And Now For Something Completely Different.”
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., spoke with Dr. Wachter earlier this week, as he wasn’t sure he could stay long enough for the formal address. But whether it’s Dr. Wachter or any of the keynote speakers, Dr. Kartham enjoys hearing HM’s leaders give advice.
“When you’re individual physicians,” he says, “you don’t know what to expect in the future. When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
For his part, Dr. Wachter has been priming the crowd for his talk. Earlier this week, he tweeted about his talk: “last 6 min wil b highlight (or lowlite) of conf, posibly of my life.”
LAS VEGAS—Hospitalist Jennifer Johnson, MD, knows exactly where she’ll be at noon today: sitting in a banquet chair listening to “the father of hospital medicine,” Bob Wachter, MD, MHM, give his annual meeting address.
When you work in technology, “you don’t get to listen to Bill Gates talk,” says Dr. Johnson, who practices at Aurora Medical Center in Grafton, Wis. “It’s one of the few times you get to be in the same room with and hear how the real people at the forefront are thinking. I think that’s very helpful.”
Dr. Johnson, who last heard Dr. Wachter speak at HM12 in San Diego, says she relishes his vision, which goes beyond what most hospitalists’ day-to-day duties encompass.
“No matter what your vocation is, it’s always good to be reminded what more you could do,” she says. “How better you could improve yourself. Instead of stagnating…there’s always a next level, a next step. He’s the guy who thinks that way.”
She’s not alone in that view. Dr. Wachter’s presentation has become a rite of SHM’s annual meeting and an unofficial wrap-up of the four-day convention. This year’s edition is titled “Ten Years of Wachter Keynote: And Now For Something Completely Different.”
Sunil Kartham, MD, a hospitalist at Altru Health System in Grand Forks, N.D., spoke with Dr. Wachter earlier this week, as he wasn’t sure he could stay long enough for the formal address. But whether it’s Dr. Wachter or any of the keynote speakers, Dr. Kartham enjoys hearing HM’s leaders give advice.
“When you’re individual physicians,” he says, “you don’t know what to expect in the future. When the leaders come and speak, they lay out a map for you…so you can prepare yourself.”
For his part, Dr. Wachter has been priming the crowd for his talk. Earlier this week, he tweeted about his talk: “last 6 min wil b highlight (or lowlite) of conf, posibly of my life.”
Three Join Ranks of Masters in Hospital Medicine
LAS VEGAS—For three hospitalists at SHM's annual meeting at the Mandalay Bay Resort and Casino, today will be a masterful day. Patrick Conway, MD, MSc, FAAP, MHM, Steven Pantilat, MD, MHM, and Jack Percelay, MD, MPH, MHM, will be designated Masters in Hospital Medicine (MHM), the growing cadre of hospitalists who have attained SHM’s highest rank. Sixteen hospitalists have attained the MHM designation. The 2014 designees will be honored on stage today during ceremonies that include the announcement of all of SHM’s new fellows and SHM’s Annual Awards of Excellence.
Dr. Pantilat, who was also a member of the inaugural class of Senior Fellows in Hospital Medicine (SFHM), is a professor of medicine in the department of medicine at the University of California at San Francisco (UCSF). He’s the founding director of the UCSF Palliative Care Program and serves as director of its Leadership Center, which trains hospitalists nationwide about how to establish palliative-care services. He is also a former SHM board member and the first recipient of the SHM Excellence in Teaching Award.
"I've never been a master of anything and despite my increasing age, somehow still feel too young to be a master," Dr. Pantilat adds. "Being bestowed with this highest honor in hospital medicine definitely ranks at the top."
Dr. Conway is used to being honored, but he says he still is humbled by the designation. As a former chairman of SHM's Public Policy Committee and the current chief medical officer for the Centers for Medicare & Medicaid Services (CMS) and its deputy administrator for innovation and quality, Dr. Conway is well known—and lauded—for giving HM a voice in Washington, D.C. He views his MHM as the latest sign that his specialty continues to grow and spur positive change in health-care delivery.
"I think the designation demonstrates that hospital medicine is a maturing specialty with strong leaders," he wrote in an email. "In addition, when you look at the current and former masters…it is a stellar group of leaders who are not only advancing hospital medicine, but also changing the face of health care across our nation and improving our health system."
Dr. Percelay is so humbled that he brought his wife, daughter, and mother with him to celebrate the moment. He’s also particularly honored that he and Dr. Conway represent the field of pediatric HM, which he believes has grown tremendously in reputation over the course of his career.
"We've been able to build upon the successes of adult hospital medicine and nurture the inherent 'playing nice in the sandbox' attitude of pediatrics to grow the discipline and work force to the point it's at now where pediatric hospitalists are seen as the experts and innovators for high value pediatric inpatient care," he wrote in an email.
Dr. Percelay is a hospitalist in the pediatric ICU at Saint Barnabas Medical Center in Livingston, N.J., and teaches in the department of physician studies at Pace University of College of Health Professions in New York. He was the founding chairman for the American Academy of Pediatrics Section on Hospital Medicine, an SHM board member from 2005 to 2012, and an associate editor of the Journal of Hospital Medicine. He says attaining the rank of master ranks just behind “being my daughter's father" on his list of personal accomplishments.
"I've received scholarships in high school, college, and medical school, but those acknowledged at most four years of work," he writes. "This award recognizes 20-plus years of work practicing as a pediatric hospitalist in community settings, caring for children and their families, and contributing to the field as a whole."
LAS VEGAS—For three hospitalists at SHM's annual meeting at the Mandalay Bay Resort and Casino, today will be a masterful day. Patrick Conway, MD, MSc, FAAP, MHM, Steven Pantilat, MD, MHM, and Jack Percelay, MD, MPH, MHM, will be designated Masters in Hospital Medicine (MHM), the growing cadre of hospitalists who have attained SHM’s highest rank. Sixteen hospitalists have attained the MHM designation. The 2014 designees will be honored on stage today during ceremonies that include the announcement of all of SHM’s new fellows and SHM’s Annual Awards of Excellence.
Dr. Pantilat, who was also a member of the inaugural class of Senior Fellows in Hospital Medicine (SFHM), is a professor of medicine in the department of medicine at the University of California at San Francisco (UCSF). He’s the founding director of the UCSF Palliative Care Program and serves as director of its Leadership Center, which trains hospitalists nationwide about how to establish palliative-care services. He is also a former SHM board member and the first recipient of the SHM Excellence in Teaching Award.
"I've never been a master of anything and despite my increasing age, somehow still feel too young to be a master," Dr. Pantilat adds. "Being bestowed with this highest honor in hospital medicine definitely ranks at the top."
Dr. Conway is used to being honored, but he says he still is humbled by the designation. As a former chairman of SHM's Public Policy Committee and the current chief medical officer for the Centers for Medicare & Medicaid Services (CMS) and its deputy administrator for innovation and quality, Dr. Conway is well known—and lauded—for giving HM a voice in Washington, D.C. He views his MHM as the latest sign that his specialty continues to grow and spur positive change in health-care delivery.
"I think the designation demonstrates that hospital medicine is a maturing specialty with strong leaders," he wrote in an email. "In addition, when you look at the current and former masters…it is a stellar group of leaders who are not only advancing hospital medicine, but also changing the face of health care across our nation and improving our health system."
Dr. Percelay is so humbled that he brought his wife, daughter, and mother with him to celebrate the moment. He’s also particularly honored that he and Dr. Conway represent the field of pediatric HM, which he believes has grown tremendously in reputation over the course of his career.
"We've been able to build upon the successes of adult hospital medicine and nurture the inherent 'playing nice in the sandbox' attitude of pediatrics to grow the discipline and work force to the point it's at now where pediatric hospitalists are seen as the experts and innovators for high value pediatric inpatient care," he wrote in an email.
Dr. Percelay is a hospitalist in the pediatric ICU at Saint Barnabas Medical Center in Livingston, N.J., and teaches in the department of physician studies at Pace University of College of Health Professions in New York. He was the founding chairman for the American Academy of Pediatrics Section on Hospital Medicine, an SHM board member from 2005 to 2012, and an associate editor of the Journal of Hospital Medicine. He says attaining the rank of master ranks just behind “being my daughter's father" on his list of personal accomplishments.
"I've received scholarships in high school, college, and medical school, but those acknowledged at most four years of work," he writes. "This award recognizes 20-plus years of work practicing as a pediatric hospitalist in community settings, caring for children and their families, and contributing to the field as a whole."
LAS VEGAS—For three hospitalists at SHM's annual meeting at the Mandalay Bay Resort and Casino, today will be a masterful day. Patrick Conway, MD, MSc, FAAP, MHM, Steven Pantilat, MD, MHM, and Jack Percelay, MD, MPH, MHM, will be designated Masters in Hospital Medicine (MHM), the growing cadre of hospitalists who have attained SHM’s highest rank. Sixteen hospitalists have attained the MHM designation. The 2014 designees will be honored on stage today during ceremonies that include the announcement of all of SHM’s new fellows and SHM’s Annual Awards of Excellence.
Dr. Pantilat, who was also a member of the inaugural class of Senior Fellows in Hospital Medicine (SFHM), is a professor of medicine in the department of medicine at the University of California at San Francisco (UCSF). He’s the founding director of the UCSF Palliative Care Program and serves as director of its Leadership Center, which trains hospitalists nationwide about how to establish palliative-care services. He is also a former SHM board member and the first recipient of the SHM Excellence in Teaching Award.
"I've never been a master of anything and despite my increasing age, somehow still feel too young to be a master," Dr. Pantilat adds. "Being bestowed with this highest honor in hospital medicine definitely ranks at the top."
Dr. Conway is used to being honored, but he says he still is humbled by the designation. As a former chairman of SHM's Public Policy Committee and the current chief medical officer for the Centers for Medicare & Medicaid Services (CMS) and its deputy administrator for innovation and quality, Dr. Conway is well known—and lauded—for giving HM a voice in Washington, D.C. He views his MHM as the latest sign that his specialty continues to grow and spur positive change in health-care delivery.
"I think the designation demonstrates that hospital medicine is a maturing specialty with strong leaders," he wrote in an email. "In addition, when you look at the current and former masters…it is a stellar group of leaders who are not only advancing hospital medicine, but also changing the face of health care across our nation and improving our health system."
Dr. Percelay is so humbled that he brought his wife, daughter, and mother with him to celebrate the moment. He’s also particularly honored that he and Dr. Conway represent the field of pediatric HM, which he believes has grown tremendously in reputation over the course of his career.
"We've been able to build upon the successes of adult hospital medicine and nurture the inherent 'playing nice in the sandbox' attitude of pediatrics to grow the discipline and work force to the point it's at now where pediatric hospitalists are seen as the experts and innovators for high value pediatric inpatient care," he wrote in an email.
Dr. Percelay is a hospitalist in the pediatric ICU at Saint Barnabas Medical Center in Livingston, N.J., and teaches in the department of physician studies at Pace University of College of Health Professions in New York. He was the founding chairman for the American Academy of Pediatrics Section on Hospital Medicine, an SHM board member from 2005 to 2012, and an associate editor of the Journal of Hospital Medicine. He says attaining the rank of master ranks just behind “being my daughter's father" on his list of personal accomplishments.
"I've received scholarships in high school, college, and medical school, but those acknowledged at most four years of work," he writes. "This award recognizes 20-plus years of work practicing as a pediatric hospitalist in community settings, caring for children and their families, and contributing to the field as a whole."
Hospitalists Central To U.S. Health System Transformation
LAS VEGAS—Hospitalists are poised to be industry leaders and change agents as the rigmarole of healthcare reform shakes out over the next few years, a keynote speaker told a standing-room-only crowd Tuesday at HM14.
Ian Morrison, PhD, a founding partner of Strategic Health Perspectives, a forecasting service for the health-care industry that includes joint-venture partners Harris Interactive and the Harvard School of Public Health’s department of health policy and management, says that while the Affordable Care Act struggled with the rollout of its health exchanges, the broader movement from fee-for-service payment structures to population-based has "turned the corner…and we ain’t going back."
"You, as a society, you, as a group, need to take the long view," Dr. Morrison told 3,500 hospitalists at the Mandalay Bay Resort and Casino. "You are going to be central to this transformation."
Morrison, a native of Scotland whose delivery is half stand-up comic, half policy wonk, says hospitalists will be on the front lines as health care shifts from local health systems to just 100 to 200 regional or super-regional systems.
And while politicians and pundits dicker over how a generational shift in policies will be implemented, hospitalists will be the ones balancing that change with patients' needs.
"This is the work of the future," Morrison says. "And it is not policy wonk work; it is clinical work. It is about the transformation of the delivery system. That is the central challenge of the future. We've got to integrate across the continuum of care, using all the innovation that both public and private sectors can deliver.
"This is not going to be determined by CMS, in my view, but by the kind of innovation that America is always good at."
LAS VEGAS—Hospitalists are poised to be industry leaders and change agents as the rigmarole of healthcare reform shakes out over the next few years, a keynote speaker told a standing-room-only crowd Tuesday at HM14.
Ian Morrison, PhD, a founding partner of Strategic Health Perspectives, a forecasting service for the health-care industry that includes joint-venture partners Harris Interactive and the Harvard School of Public Health’s department of health policy and management, says that while the Affordable Care Act struggled with the rollout of its health exchanges, the broader movement from fee-for-service payment structures to population-based has "turned the corner…and we ain’t going back."
"You, as a society, you, as a group, need to take the long view," Dr. Morrison told 3,500 hospitalists at the Mandalay Bay Resort and Casino. "You are going to be central to this transformation."
Morrison, a native of Scotland whose delivery is half stand-up comic, half policy wonk, says hospitalists will be on the front lines as health care shifts from local health systems to just 100 to 200 regional or super-regional systems.
And while politicians and pundits dicker over how a generational shift in policies will be implemented, hospitalists will be the ones balancing that change with patients' needs.
"This is the work of the future," Morrison says. "And it is not policy wonk work; it is clinical work. It is about the transformation of the delivery system. That is the central challenge of the future. We've got to integrate across the continuum of care, using all the innovation that both public and private sectors can deliver.
"This is not going to be determined by CMS, in my view, but by the kind of innovation that America is always good at."
LAS VEGAS—Hospitalists are poised to be industry leaders and change agents as the rigmarole of healthcare reform shakes out over the next few years, a keynote speaker told a standing-room-only crowd Tuesday at HM14.
Ian Morrison, PhD, a founding partner of Strategic Health Perspectives, a forecasting service for the health-care industry that includes joint-venture partners Harris Interactive and the Harvard School of Public Health’s department of health policy and management, says that while the Affordable Care Act struggled with the rollout of its health exchanges, the broader movement from fee-for-service payment structures to population-based has "turned the corner…and we ain’t going back."
"You, as a society, you, as a group, need to take the long view," Dr. Morrison told 3,500 hospitalists at the Mandalay Bay Resort and Casino. "You are going to be central to this transformation."
Morrison, a native of Scotland whose delivery is half stand-up comic, half policy wonk, says hospitalists will be on the front lines as health care shifts from local health systems to just 100 to 200 regional or super-regional systems.
And while politicians and pundits dicker over how a generational shift in policies will be implemented, hospitalists will be the ones balancing that change with patients' needs.
"This is the work of the future," Morrison says. "And it is not policy wonk work; it is clinical work. It is about the transformation of the delivery system. That is the central challenge of the future. We've got to integrate across the continuum of care, using all the innovation that both public and private sectors can deliver.
"This is not going to be determined by CMS, in my view, but by the kind of innovation that America is always good at."
Hospitalists Focus on Matters of the Heart
LAS VEGAS—Hospitalist Michael Hoftiezer, MD, has been to pre-courses at annual meetings before HM14, but yesterday’s lineup offered a new option: “Cardiology: What Hospitalists Need to Know as Front-Line Providers.”
The eight-hour seminar was one of three new pre-courses at SHM’s annual meeting, along with “Efficient High-Value Evidence-Based Medicine for the Practicing Hospitalist” and “NP/PA Playbook for Hospital Medicine.” The offerings drew hundreds of hospitalists to the unofficial first day of HM14 at Mandalay Bay Resort and Casino.
“It’s nice to have an extra day of learning,” says Dr. Hoftiezer, who practices at Holy Family Memorial Medical Center in Manitowoc, Wis. And “it’s concentrated on one subject. It’s a good overview of a single subject, rather than bouncing around different things.” Course director Matthews Chacko, MD, of Johns Hopkins Hospital in Baltimore, says the time is right for hospitalists to devote a full-day pre-course focused on cardiology. “Cardiovascular disease is the most common reason we die,” he says.
“It’s something hospital-based practitioners see often. Providing a comprehensive but yet simplified overview of the way to manage some of these diseases with talks given by some of the leading experts in the field seemed very appropriate for this meeting.”
The course covered such topics as arrhythmia, heart failure, peripheral artery disease, and unstable myocardial infarction. Dr. Hoftiezer says he gleaned tips he can take back to his hospital—including the mechanisms of atrial fibrillation and when to measure rhythm versus rate—and that’s what made the pre-course valuable.
“The more relevant, the better,” he adds. “My favorite lectures are the ones that change something I do.”
LAS VEGAS—Hospitalist Michael Hoftiezer, MD, has been to pre-courses at annual meetings before HM14, but yesterday’s lineup offered a new option: “Cardiology: What Hospitalists Need to Know as Front-Line Providers.”
The eight-hour seminar was one of three new pre-courses at SHM’s annual meeting, along with “Efficient High-Value Evidence-Based Medicine for the Practicing Hospitalist” and “NP/PA Playbook for Hospital Medicine.” The offerings drew hundreds of hospitalists to the unofficial first day of HM14 at Mandalay Bay Resort and Casino.
“It’s nice to have an extra day of learning,” says Dr. Hoftiezer, who practices at Holy Family Memorial Medical Center in Manitowoc, Wis. And “it’s concentrated on one subject. It’s a good overview of a single subject, rather than bouncing around different things.” Course director Matthews Chacko, MD, of Johns Hopkins Hospital in Baltimore, says the time is right for hospitalists to devote a full-day pre-course focused on cardiology. “Cardiovascular disease is the most common reason we die,” he says.
“It’s something hospital-based practitioners see often. Providing a comprehensive but yet simplified overview of the way to manage some of these diseases with talks given by some of the leading experts in the field seemed very appropriate for this meeting.”
The course covered such topics as arrhythmia, heart failure, peripheral artery disease, and unstable myocardial infarction. Dr. Hoftiezer says he gleaned tips he can take back to his hospital—including the mechanisms of atrial fibrillation and when to measure rhythm versus rate—and that’s what made the pre-course valuable.
“The more relevant, the better,” he adds. “My favorite lectures are the ones that change something I do.”
LAS VEGAS—Hospitalist Michael Hoftiezer, MD, has been to pre-courses at annual meetings before HM14, but yesterday’s lineup offered a new option: “Cardiology: What Hospitalists Need to Know as Front-Line Providers.”
The eight-hour seminar was one of three new pre-courses at SHM’s annual meeting, along with “Efficient High-Value Evidence-Based Medicine for the Practicing Hospitalist” and “NP/PA Playbook for Hospital Medicine.” The offerings drew hundreds of hospitalists to the unofficial first day of HM14 at Mandalay Bay Resort and Casino.
“It’s nice to have an extra day of learning,” says Dr. Hoftiezer, who practices at Holy Family Memorial Medical Center in Manitowoc, Wis. And “it’s concentrated on one subject. It’s a good overview of a single subject, rather than bouncing around different things.” Course director Matthews Chacko, MD, of Johns Hopkins Hospital in Baltimore, says the time is right for hospitalists to devote a full-day pre-course focused on cardiology. “Cardiovascular disease is the most common reason we die,” he says.
“It’s something hospital-based practitioners see often. Providing a comprehensive but yet simplified overview of the way to manage some of these diseases with talks given by some of the leading experts in the field seemed very appropriate for this meeting.”
The course covered such topics as arrhythmia, heart failure, peripheral artery disease, and unstable myocardial infarction. Dr. Hoftiezer says he gleaned tips he can take back to his hospital—including the mechanisms of atrial fibrillation and when to measure rhythm versus rate—and that’s what made the pre-course valuable.
“The more relevant, the better,” he adds. “My favorite lectures are the ones that change something I do.”
Relevance Fuels HM14 Schedule Decisions
LAS VEGAS—For the next two and a half days at the Mandalay Bay Resort and Casino, some 3,000 hospitalists attending SHM’s annual meeting will have 10 learning tracks and 115 educational sessions to choose from. Which raises a good question: How does a hospitalist make the difficult choice between two sessions of interest that are scheduled at the same time?
“What’s guiding me is: What’s more relevant to what I’m doing?” says hospitalist and first-time attendee Uzoeshi Anukam, MD, of Methodist Mansfield Medical Center in Texas. “What’s more relevant to my patient care? I see a lot of chest pain, so I’m going to jump on chest pain [sessions]. It’s relevant for me.”
The smorgasbord of educational tracks, rapid-fire sessions, and small-group workshops is a recipe for conflict, though. Multiple sessions could offer similar relevance.
“It’s pick your poison, sort of,” says Curt Lawrence, MD, a hospitalist who does locums tenens work in Miami. “To me, most of the topics are pretty interesting and informative. It’s a good problem to have, wanting to go to multiple things.”
Dr. Lawrence says SHM’s online repository of presentations, podcasts, and on-demand videos helps to fill the gaps when he misses a session. And Dr. Anukam says the HM14 At Hand application for smartphones and tablets assists in winnowing down choices and setting goals for which sessions to attend.
“Objectives put things in perspective and guide what things to go to,” Dr. Lawrence says. “My goal is to get as much as information as you can. As a hospitalist, it’s go-go-go-go. I want to spend this time to just stop and get information.”
LAS VEGAS—For the next two and a half days at the Mandalay Bay Resort and Casino, some 3,000 hospitalists attending SHM’s annual meeting will have 10 learning tracks and 115 educational sessions to choose from. Which raises a good question: How does a hospitalist make the difficult choice between two sessions of interest that are scheduled at the same time?
“What’s guiding me is: What’s more relevant to what I’m doing?” says hospitalist and first-time attendee Uzoeshi Anukam, MD, of Methodist Mansfield Medical Center in Texas. “What’s more relevant to my patient care? I see a lot of chest pain, so I’m going to jump on chest pain [sessions]. It’s relevant for me.”
The smorgasbord of educational tracks, rapid-fire sessions, and small-group workshops is a recipe for conflict, though. Multiple sessions could offer similar relevance.
“It’s pick your poison, sort of,” says Curt Lawrence, MD, a hospitalist who does locums tenens work in Miami. “To me, most of the topics are pretty interesting and informative. It’s a good problem to have, wanting to go to multiple things.”
Dr. Lawrence says SHM’s online repository of presentations, podcasts, and on-demand videos helps to fill the gaps when he misses a session. And Dr. Anukam says the HM14 At Hand application for smartphones and tablets assists in winnowing down choices and setting goals for which sessions to attend.
“Objectives put things in perspective and guide what things to go to,” Dr. Lawrence says. “My goal is to get as much as information as you can. As a hospitalist, it’s go-go-go-go. I want to spend this time to just stop and get information.”
LAS VEGAS—For the next two and a half days at the Mandalay Bay Resort and Casino, some 3,000 hospitalists attending SHM’s annual meeting will have 10 learning tracks and 115 educational sessions to choose from. Which raises a good question: How does a hospitalist make the difficult choice between two sessions of interest that are scheduled at the same time?
“What’s guiding me is: What’s more relevant to what I’m doing?” says hospitalist and first-time attendee Uzoeshi Anukam, MD, of Methodist Mansfield Medical Center in Texas. “What’s more relevant to my patient care? I see a lot of chest pain, so I’m going to jump on chest pain [sessions]. It’s relevant for me.”
The smorgasbord of educational tracks, rapid-fire sessions, and small-group workshops is a recipe for conflict, though. Multiple sessions could offer similar relevance.
“It’s pick your poison, sort of,” says Curt Lawrence, MD, a hospitalist who does locums tenens work in Miami. “To me, most of the topics are pretty interesting and informative. It’s a good problem to have, wanting to go to multiple things.”
Dr. Lawrence says SHM’s online repository of presentations, podcasts, and on-demand videos helps to fill the gaps when he misses a session. And Dr. Anukam says the HM14 At Hand application for smartphones and tablets assists in winnowing down choices and setting goals for which sessions to attend.
“Objectives put things in perspective and guide what things to go to,” Dr. Lawrence says. “My goal is to get as much as information as you can. As a hospitalist, it’s go-go-go-go. I want to spend this time to just stop and get information.”
HM14 Lineup Packed with Learning, Networking Opportunities
LAS VEGAS—Welcome to HM14! Now, let's get to work.
While most visitors that arrive at Mandalay Bay Resort and Casino are up for fun and frolicking, the nearly 3,000 hospitalists expected to attend this year’s HM confab are here for education and inspiration. And the meeting's slate of sessions, speakers, and mental stimulation is expected to provide both.
"What you're getting are those thought leaders, as well as the academics, as well as real-life business education, all in one area," says Darren Swenson MD, a regional medical advisor for IPC The Hospitalist Co. in Las Vegas and founder of the city's SHM chapter. "And when you're able to choose your tracks to identify those programs that are of interest to you at that point in your career, it makes it very attractive."
Here are five tips to get the most out of your meeting:
- Think ahead and design a daily itinerary to take advantage of courses applicable back home, but don't be a slave to a schedule. Be open to changing course when opportunities for a meeting or event arise.
- Don't skip the keynotes. Whether it's a new panel discussion on Obamacare, an address by health strategist Ian Morrison, PhD, or the annual crowd pleaser from hospital medicine dean and blogger Bob Wachter, MD, MHM, the plenary sessions feature industry leaders’ views on important and compelling topics.
- Step outside your comfort zone. Reinforcing knowledge is certainly important, but course directors always encourage attendees to seize the opportunity to learn new skills.
- Network, network, network. There is no larger gathering of your colleagues than the annual meeting, so take advantage.
- Don't forget the Town Hall. For those planning to attend the meeting’s final session, the Town Hall is a chance to talk directly to SHM’s top staff and its board of directors.
Visit our website for more on making the most of HM14.
LAS VEGAS—Welcome to HM14! Now, let's get to work.
While most visitors that arrive at Mandalay Bay Resort and Casino are up for fun and frolicking, the nearly 3,000 hospitalists expected to attend this year’s HM confab are here for education and inspiration. And the meeting's slate of sessions, speakers, and mental stimulation is expected to provide both.
"What you're getting are those thought leaders, as well as the academics, as well as real-life business education, all in one area," says Darren Swenson MD, a regional medical advisor for IPC The Hospitalist Co. in Las Vegas and founder of the city's SHM chapter. "And when you're able to choose your tracks to identify those programs that are of interest to you at that point in your career, it makes it very attractive."
Here are five tips to get the most out of your meeting:
- Think ahead and design a daily itinerary to take advantage of courses applicable back home, but don't be a slave to a schedule. Be open to changing course when opportunities for a meeting or event arise.
- Don't skip the keynotes. Whether it's a new panel discussion on Obamacare, an address by health strategist Ian Morrison, PhD, or the annual crowd pleaser from hospital medicine dean and blogger Bob Wachter, MD, MHM, the plenary sessions feature industry leaders’ views on important and compelling topics.
- Step outside your comfort zone. Reinforcing knowledge is certainly important, but course directors always encourage attendees to seize the opportunity to learn new skills.
- Network, network, network. There is no larger gathering of your colleagues than the annual meeting, so take advantage.
- Don't forget the Town Hall. For those planning to attend the meeting’s final session, the Town Hall is a chance to talk directly to SHM’s top staff and its board of directors.
Visit our website for more on making the most of HM14.
LAS VEGAS—Welcome to HM14! Now, let's get to work.
While most visitors that arrive at Mandalay Bay Resort and Casino are up for fun and frolicking, the nearly 3,000 hospitalists expected to attend this year’s HM confab are here for education and inspiration. And the meeting's slate of sessions, speakers, and mental stimulation is expected to provide both.
"What you're getting are those thought leaders, as well as the academics, as well as real-life business education, all in one area," says Darren Swenson MD, a regional medical advisor for IPC The Hospitalist Co. in Las Vegas and founder of the city's SHM chapter. "And when you're able to choose your tracks to identify those programs that are of interest to you at that point in your career, it makes it very attractive."
Here are five tips to get the most out of your meeting:
- Think ahead and design a daily itinerary to take advantage of courses applicable back home, but don't be a slave to a schedule. Be open to changing course when opportunities for a meeting or event arise.
- Don't skip the keynotes. Whether it's a new panel discussion on Obamacare, an address by health strategist Ian Morrison, PhD, or the annual crowd pleaser from hospital medicine dean and blogger Bob Wachter, MD, MHM, the plenary sessions feature industry leaders’ views on important and compelling topics.
- Step outside your comfort zone. Reinforcing knowledge is certainly important, but course directors always encourage attendees to seize the opportunity to learn new skills.
- Network, network, network. There is no larger gathering of your colleagues than the annual meeting, so take advantage.
- Don't forget the Town Hall. For those planning to attend the meeting’s final session, the Town Hall is a chance to talk directly to SHM’s top staff and its board of directors.
Visit our website for more on making the most of HM14.
Bright Lights, Big City: Las Vegas Is More Than the Strip
LAS VEGAS – Now that you're here, focus on the valuable opportunities that HM14 offers. Well, until dusk. Then get out of the hotel and focus on the opportunities that are Las Vegas.
The fun isn't just the famed Strip, says Zubin Damania, MD, founder of Turntable Health in Las Vegas, who might be better known for his comedic alter ego, ZDoggMD. It's the lesser-known side of Las Vegas, known locally as "downtown."
"When I have friends in town, I tell them not to go to the Strip and to come hang out with me downtown or in the suburbs of Vegas—where the real fun is to be had," says Dr. Damania, even though he realizes he can't tell that to 3,000 "rabid hospitalists looking to relive 'The Hangover 3.'"
His recommendations include:
- Chinatown. The district is along Spring Mountain Road, about four miles north of Mandalay Bay, and includes several enclosed shopping malls. Restaurants to try include Raku, which specializes in Japanese food, and Kabuto, which has "the best sushi" ZDoggMD's ever had.
- Red Rock Canyon National Conservation Area. Breathtaking views and hiking opportunities abound in natural Nevada.
- The Zappos factory. A tour of the firm’s downtown headquarters showcases the mindset of the millennial generation and potential lessons on workplace attitude that can be applied to HM.
- Turntable Health. Dr. Damania’s clinic is open to any hospitalists curious to visit. If you want to set up a tour, or want more personalized advice on what to do while in town, e-mail him at [email protected].
Visit our website for more of ZDoggMD's recommendations.
LAS VEGAS – Now that you're here, focus on the valuable opportunities that HM14 offers. Well, until dusk. Then get out of the hotel and focus on the opportunities that are Las Vegas.
The fun isn't just the famed Strip, says Zubin Damania, MD, founder of Turntable Health in Las Vegas, who might be better known for his comedic alter ego, ZDoggMD. It's the lesser-known side of Las Vegas, known locally as "downtown."
"When I have friends in town, I tell them not to go to the Strip and to come hang out with me downtown or in the suburbs of Vegas—where the real fun is to be had," says Dr. Damania, even though he realizes he can't tell that to 3,000 "rabid hospitalists looking to relive 'The Hangover 3.'"
His recommendations include:
- Chinatown. The district is along Spring Mountain Road, about four miles north of Mandalay Bay, and includes several enclosed shopping malls. Restaurants to try include Raku, which specializes in Japanese food, and Kabuto, which has "the best sushi" ZDoggMD's ever had.
- Red Rock Canyon National Conservation Area. Breathtaking views and hiking opportunities abound in natural Nevada.
- The Zappos factory. A tour of the firm’s downtown headquarters showcases the mindset of the millennial generation and potential lessons on workplace attitude that can be applied to HM.
- Turntable Health. Dr. Damania’s clinic is open to any hospitalists curious to visit. If you want to set up a tour, or want more personalized advice on what to do while in town, e-mail him at [email protected].
Visit our website for more of ZDoggMD's recommendations.
LAS VEGAS – Now that you're here, focus on the valuable opportunities that HM14 offers. Well, until dusk. Then get out of the hotel and focus on the opportunities that are Las Vegas.
The fun isn't just the famed Strip, says Zubin Damania, MD, founder of Turntable Health in Las Vegas, who might be better known for his comedic alter ego, ZDoggMD. It's the lesser-known side of Las Vegas, known locally as "downtown."
"When I have friends in town, I tell them not to go to the Strip and to come hang out with me downtown or in the suburbs of Vegas—where the real fun is to be had," says Dr. Damania, even though he realizes he can't tell that to 3,000 "rabid hospitalists looking to relive 'The Hangover 3.'"
His recommendations include:
- Chinatown. The district is along Spring Mountain Road, about four miles north of Mandalay Bay, and includes several enclosed shopping malls. Restaurants to try include Raku, which specializes in Japanese food, and Kabuto, which has "the best sushi" ZDoggMD's ever had.
- Red Rock Canyon National Conservation Area. Breathtaking views and hiking opportunities abound in natural Nevada.
- The Zappos factory. A tour of the firm’s downtown headquarters showcases the mindset of the millennial generation and potential lessons on workplace attitude that can be applied to HM.
- Turntable Health. Dr. Damania’s clinic is open to any hospitalists curious to visit. If you want to set up a tour, or want more personalized advice on what to do while in town, e-mail him at [email protected].
Visit our website for more of ZDoggMD's recommendations.
CDC Report Calls for Hospitalists to Focus on Antibiotic Stewardship
A Centers for Disease Control and Prevention (CDC) report this month on antibiotic stewardship highlights the need for continued attention and improvement around the topic, says a hospitalist who has studied the issue.
The CDC announcement, "Antibiotic Rx in Hospitals: Proceed with Caution," circulated in its monthly report, CDC Vital Signs, urged hospital leaders to adopt at least a basic stewardship program and "work with other healthcare facilities to prevent infections, transmission, and resistance."
David Rosenberg, MD, MPH, FACP, SFHM, chief of the division of hospital medicine at North Shore University Hospital's department of medicine in Manhasset, N.Y., says the alert can serve as a spotlight.
"While we all agree that this is an important topic, there's a certain amount of inertia around it," Dr. Rosenberg says. "When the CDC comes out with statements like this, it really helps drive this forward. It really should be viewed as a call to action."
The CDC alert highlights the variability of antibiotic use. It notes that doctors in some hospitals prescribed three times as many antibiotics as doctors at others. The disparity in treatment standards makes stewardship a broad issue to tackle, Dr. Rosenberg says.
"It's not a simple fix," he adds. "You have to do it one piece at a time. How are you going to manage urinary-tract infections? How are you going to manage pneumonias? How are you going to manage bloodstream infections? We want ultimately to integrate the approach into the day-to-day practice of hospitalists, but there's a lot of data you need in a very organized format to inform those decisions. Stewardship programs organize the information in a way that can influence and change practice."
Visit our website for more information on antibiotic stewardship.
A Centers for Disease Control and Prevention (CDC) report this month on antibiotic stewardship highlights the need for continued attention and improvement around the topic, says a hospitalist who has studied the issue.
The CDC announcement, "Antibiotic Rx in Hospitals: Proceed with Caution," circulated in its monthly report, CDC Vital Signs, urged hospital leaders to adopt at least a basic stewardship program and "work with other healthcare facilities to prevent infections, transmission, and resistance."
David Rosenberg, MD, MPH, FACP, SFHM, chief of the division of hospital medicine at North Shore University Hospital's department of medicine in Manhasset, N.Y., says the alert can serve as a spotlight.
"While we all agree that this is an important topic, there's a certain amount of inertia around it," Dr. Rosenberg says. "When the CDC comes out with statements like this, it really helps drive this forward. It really should be viewed as a call to action."
The CDC alert highlights the variability of antibiotic use. It notes that doctors in some hospitals prescribed three times as many antibiotics as doctors at others. The disparity in treatment standards makes stewardship a broad issue to tackle, Dr. Rosenberg says.
"It's not a simple fix," he adds. "You have to do it one piece at a time. How are you going to manage urinary-tract infections? How are you going to manage pneumonias? How are you going to manage bloodstream infections? We want ultimately to integrate the approach into the day-to-day practice of hospitalists, but there's a lot of data you need in a very organized format to inform those decisions. Stewardship programs organize the information in a way that can influence and change practice."
Visit our website for more information on antibiotic stewardship.
A Centers for Disease Control and Prevention (CDC) report this month on antibiotic stewardship highlights the need for continued attention and improvement around the topic, says a hospitalist who has studied the issue.
The CDC announcement, "Antibiotic Rx in Hospitals: Proceed with Caution," circulated in its monthly report, CDC Vital Signs, urged hospital leaders to adopt at least a basic stewardship program and "work with other healthcare facilities to prevent infections, transmission, and resistance."
David Rosenberg, MD, MPH, FACP, SFHM, chief of the division of hospital medicine at North Shore University Hospital's department of medicine in Manhasset, N.Y., says the alert can serve as a spotlight.
"While we all agree that this is an important topic, there's a certain amount of inertia around it," Dr. Rosenberg says. "When the CDC comes out with statements like this, it really helps drive this forward. It really should be viewed as a call to action."
The CDC alert highlights the variability of antibiotic use. It notes that doctors in some hospitals prescribed three times as many antibiotics as doctors at others. The disparity in treatment standards makes stewardship a broad issue to tackle, Dr. Rosenberg says.
"It's not a simple fix," he adds. "You have to do it one piece at a time. How are you going to manage urinary-tract infections? How are you going to manage pneumonias? How are you going to manage bloodstream infections? We want ultimately to integrate the approach into the day-to-day practice of hospitalists, but there's a lot of data you need in a very organized format to inform those decisions. Stewardship programs organize the information in a way that can influence and change practice."
Visit our website for more information on antibiotic stewardship.