User login
Resident Handoff Program Reduces Medical Errors at Pediatric Hospital
A standardized handoff program can reduce medical errors and can be replicated at hospitals across the country, says the lead researcher of a new study published in JAMA.
Researchers reviewed the medical literature for successful handoff-intervention programs that they could teach to residents and senior interns working within two units at Boston Children’s Hospital. They ultimately settled on a bundle that included standardized communication and handoff training, a verbal mnemonic to help staff members remember what information to pass off to the next team, and a handoff structure that involved junior and senior physicians meeting in a quiet room to discuss the handoff. In addition, on one unit, residents used a computerized tool linked to the electronic medical record that made it easier for them to pass along important information about the patient.
The analysis included 642 handoffs that occurred before the intervention and 613 that happened afterwards. Researchers found that medical errors decreased from 33.8 per 100 admissions (95% CI, 27.3–40.3) prior to the intervention to 18.3 per 100 admissions (95% CI, 14.7–21.9; P?P=0.04).
Amy Starmer, MD, MPH, associate scientific researcher at Boston Children’s Hospital and lecturer in pediatrics at Harvard Medical School in Boston, says that when implementing an intervention program, it’s important to involve staff from all levels of the hospital.
“We thought carefully about who should be able to make transformational change happen,” says Dr. Starmer. “That included resident program directors, educators, attending physicians who help observe the residents, and senior administrative people in the hospital who knew this was going on and were supportive. Even the technology team was able to devote programming support and resources to allow the development of a computerized tool.”
Visit our website for more information on hospital handoff programs.
A standardized handoff program can reduce medical errors and can be replicated at hospitals across the country, says the lead researcher of a new study published in JAMA.
Researchers reviewed the medical literature for successful handoff-intervention programs that they could teach to residents and senior interns working within two units at Boston Children’s Hospital. They ultimately settled on a bundle that included standardized communication and handoff training, a verbal mnemonic to help staff members remember what information to pass off to the next team, and a handoff structure that involved junior and senior physicians meeting in a quiet room to discuss the handoff. In addition, on one unit, residents used a computerized tool linked to the electronic medical record that made it easier for them to pass along important information about the patient.
The analysis included 642 handoffs that occurred before the intervention and 613 that happened afterwards. Researchers found that medical errors decreased from 33.8 per 100 admissions (95% CI, 27.3–40.3) prior to the intervention to 18.3 per 100 admissions (95% CI, 14.7–21.9; P?P=0.04).
Amy Starmer, MD, MPH, associate scientific researcher at Boston Children’s Hospital and lecturer in pediatrics at Harvard Medical School in Boston, says that when implementing an intervention program, it’s important to involve staff from all levels of the hospital.
“We thought carefully about who should be able to make transformational change happen,” says Dr. Starmer. “That included resident program directors, educators, attending physicians who help observe the residents, and senior administrative people in the hospital who knew this was going on and were supportive. Even the technology team was able to devote programming support and resources to allow the development of a computerized tool.”
Visit our website for more information on hospital handoff programs.
A standardized handoff program can reduce medical errors and can be replicated at hospitals across the country, says the lead researcher of a new study published in JAMA.
Researchers reviewed the medical literature for successful handoff-intervention programs that they could teach to residents and senior interns working within two units at Boston Children’s Hospital. They ultimately settled on a bundle that included standardized communication and handoff training, a verbal mnemonic to help staff members remember what information to pass off to the next team, and a handoff structure that involved junior and senior physicians meeting in a quiet room to discuss the handoff. In addition, on one unit, residents used a computerized tool linked to the electronic medical record that made it easier for them to pass along important information about the patient.
The analysis included 642 handoffs that occurred before the intervention and 613 that happened afterwards. Researchers found that medical errors decreased from 33.8 per 100 admissions (95% CI, 27.3–40.3) prior to the intervention to 18.3 per 100 admissions (95% CI, 14.7–21.9; P?P=0.04).
Amy Starmer, MD, MPH, associate scientific researcher at Boston Children’s Hospital and lecturer in pediatrics at Harvard Medical School in Boston, says that when implementing an intervention program, it’s important to involve staff from all levels of the hospital.
“We thought carefully about who should be able to make transformational change happen,” says Dr. Starmer. “That included resident program directors, educators, attending physicians who help observe the residents, and senior administrative people in the hospital who knew this was going on and were supportive. Even the technology team was able to devote programming support and resources to allow the development of a computerized tool.”
Visit our website for more information on hospital handoff programs.
Side Effects of Synthetic Marijuana Blamed for Thousands of ED Visits
A report outlining the alarming side effects of synthetic marijuana use in young adults acts as a call to attention for hospitalists, as thousands of patients per year are exposed to the chemicals found in the cannabinoid.
The report from the federal Substance Abuse and Mental Health Services Administration shows that synthetic marijuana was responsible for 11,400 ED visits in one year, with brain and kidney damage, hallucinations, and violent behavior among the severe reactions found in users.
Synthetic marijuana is herbs sprayed or soaked in chemicals, making it difficult for drug tests to detect and more dangerous to consume. Some of the chemicals are found in fertilizers, painkillers, and cancer treatments, creating an unsafe and potentially deadly concoction. It is inexpensive, available online or in convenience stores sold under such brand names as “potpourri,” “K2,” and “spice,” and labeled “not for human consumption.”
The multiple reasons why patients may be having psychoactive effects could be a daunting mystery to solve. However, two hospitalists provide insight on possible treatment options. Scott Carney, MD, FAAP, assistant professor and program director at University of South Carolina School of Medicine in Columbia, and Melissa Schafer, MD, assistant professor of pediatrics at SUNY Upstate Medical University in Syracuse, N.Y., advise hospitalists to treat these patients with IV fluids and close monitoring while they metabolize. A toxicology consultation and psychological evaluation should be ordered, and Dr. Schafer suggests poison control can “help with knowing what is on the streets in your area and what to expect.”
Visit our website for more information on treating symptoms of drug overdose.
A report outlining the alarming side effects of synthetic marijuana use in young adults acts as a call to attention for hospitalists, as thousands of patients per year are exposed to the chemicals found in the cannabinoid.
The report from the federal Substance Abuse and Mental Health Services Administration shows that synthetic marijuana was responsible for 11,400 ED visits in one year, with brain and kidney damage, hallucinations, and violent behavior among the severe reactions found in users.
Synthetic marijuana is herbs sprayed or soaked in chemicals, making it difficult for drug tests to detect and more dangerous to consume. Some of the chemicals are found in fertilizers, painkillers, and cancer treatments, creating an unsafe and potentially deadly concoction. It is inexpensive, available online or in convenience stores sold under such brand names as “potpourri,” “K2,” and “spice,” and labeled “not for human consumption.”
The multiple reasons why patients may be having psychoactive effects could be a daunting mystery to solve. However, two hospitalists provide insight on possible treatment options. Scott Carney, MD, FAAP, assistant professor and program director at University of South Carolina School of Medicine in Columbia, and Melissa Schafer, MD, assistant professor of pediatrics at SUNY Upstate Medical University in Syracuse, N.Y., advise hospitalists to treat these patients with IV fluids and close monitoring while they metabolize. A toxicology consultation and psychological evaluation should be ordered, and Dr. Schafer suggests poison control can “help with knowing what is on the streets in your area and what to expect.”
Visit our website for more information on treating symptoms of drug overdose.
A report outlining the alarming side effects of synthetic marijuana use in young adults acts as a call to attention for hospitalists, as thousands of patients per year are exposed to the chemicals found in the cannabinoid.
The report from the federal Substance Abuse and Mental Health Services Administration shows that synthetic marijuana was responsible for 11,400 ED visits in one year, with brain and kidney damage, hallucinations, and violent behavior among the severe reactions found in users.
Synthetic marijuana is herbs sprayed or soaked in chemicals, making it difficult for drug tests to detect and more dangerous to consume. Some of the chemicals are found in fertilizers, painkillers, and cancer treatments, creating an unsafe and potentially deadly concoction. It is inexpensive, available online or in convenience stores sold under such brand names as “potpourri,” “K2,” and “spice,” and labeled “not for human consumption.”
The multiple reasons why patients may be having psychoactive effects could be a daunting mystery to solve. However, two hospitalists provide insight on possible treatment options. Scott Carney, MD, FAAP, assistant professor and program director at University of South Carolina School of Medicine in Columbia, and Melissa Schafer, MD, assistant professor of pediatrics at SUNY Upstate Medical University in Syracuse, N.Y., advise hospitalists to treat these patients with IV fluids and close monitoring while they metabolize. A toxicology consultation and psychological evaluation should be ordered, and Dr. Schafer suggests poison control can “help with knowing what is on the streets in your area and what to expect.”
Visit our website for more information on treating symptoms of drug overdose.
Five Reasons To Pursue ABIM's Hospitalist-Focused MOC
By now, most hospitalists have at least heard about the Recognition in Focused Practice in Hospital Medicine (RFPHM), which is offered as a variation in certification for internal medicine- and family medicine-trained graduates who are pursuing Maintenance of Certification (MOC). Although the requirements are relatively straightforward, it may not be abundantly clear exactly why a hospitalist would pursue this pathway. As a recent “graduate” of the first cycle of the program, I can testify it is wholly worth the time and energy for the following reasons:
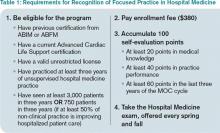
1. The requirements are relatively easy. Table 1 outlines the requirements for eligibility for enrolling in the program through the American Board of Internal Medicine (ABIM); enrollment through the American Board of Family Medicine (ABFM) also is available. These are basic requirements, and most practicing hospitalists will easily qualify simply by doing their daily jobs. Enrollment does require an administrative fee, but many HM programs can—and should—reimburse you for these fees, so be sure to ask if your program will cover the cost.
After enrolling and paying the fee, your next step is to accumulate points toward certification. Of note, the 100 points do not all have to be accumulated prior to sitting for the exam, but accumulating these points generally prepares you for the exam, so it is a good idea to complete this task before the exam, in most circumstances.
The medical knowledge modules can be completed through ABIM/ABFM, the Society of Hospital Medicine (SHM), or the New England Journal of Medicine.1 A repertoire of clinical and non-clinical modules are offered by ABIM, and there are two modules on quality-patient safety offered by SHM. You can attend a number of pre-courses offered at local-regional-national HM meetings; these modules can be completed individually or in a group setting. A list of available group learning sessions can be found at www.abim.org. You can earn CME credit for completing these modules. Not only are the medical knowledge modules readily available, but they are also well written, are easy to complete, and prepare you well for the exam.
The practice performance modules can be completed through ABIM/ABFM or through a number of medical centers that participate in the American Board of Medical Specialties “Portfolio Program.” For organizations that participate in the program, hospitalists within the organizational network who have completed a quality improvement project may qualify for module credit. A list of these sponsoring organizations can be found at http://mocportfolioprogram.org/approved-portfolio-sponsors.
Hospitalists can earn practice improvement module (PIM) credit for being involved in a number of large collaborative projects, including SHM’s mentored implementation programs (e.g. glycemic control, VTE, and Project BOOST).3
For those completing a PIM through the ABIM, the most straightforward are the self-directed PIM or the completed project PIM.2
2. The exam content is known. Table 2 lists the content categories of the secure exam, published by ABIM, with approximate percentages of the content within overall categories and subcategories. This information helps you focus your efforts in preparing for the exam and is aligned with what most hospitalists practice on a daily basis.
3. The exam preparation is easy. Not only is the content outlined in the blueprint in Table 2, but practice exams are available online from the ABIM and a tutorial can be found at www.abim.org/hospital-medicine-tutorial. This tutorial simulates the actual exam, to enhance preparation and reduce testing anxiety.
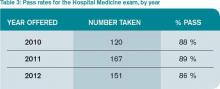
4. The exam pass rate is high. Table 3 lists pass rates from the 2010-2012 hospital medicine exam. These pass rates are equivalent to the general medicine exam, and they exceed some of the other specialty exam pass rates.
5. RFPHM is gaining more of the recognition it deserves. Given this growth in recognition, from employers, peers, patients, and maybe even payors, it would serve you well to start the process early, because it is highly likely to gain traction in the coming years.
Join Us
All told, RFPHM enrollment, preparation, and exam completion are straightforward, relatively easy, and worth the time and energy. I hope you join me and the 418 other hospitalists who have pursued this recognition. You will be glad you invested in your future.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- American Board of Internal Medicine. List of self-evaluation modules. Available at: http://www.abim.org/maintenance-of-certification/medical-knowledge/modules.aspx#hosp. Accessed November 27, 2013.
- American Board of Internal Medicine. List of PIMs from ABIM. Available at: http://www.abim.org/moc/earning-points.aspx. Accessed November 27, 2013.
- American Board of Internal Medicine. List of PIMs from sponsoring institutions. Available at: http://www.abim.org/moc/earning-points/productinfo-demo-ordering.aspx#aqi. Accessed November 27, 2013.
By now, most hospitalists have at least heard about the Recognition in Focused Practice in Hospital Medicine (RFPHM), which is offered as a variation in certification for internal medicine- and family medicine-trained graduates who are pursuing Maintenance of Certification (MOC). Although the requirements are relatively straightforward, it may not be abundantly clear exactly why a hospitalist would pursue this pathway. As a recent “graduate” of the first cycle of the program, I can testify it is wholly worth the time and energy for the following reasons:
1. The requirements are relatively easy. Table 1 outlines the requirements for eligibility for enrolling in the program through the American Board of Internal Medicine (ABIM); enrollment through the American Board of Family Medicine (ABFM) also is available. These are basic requirements, and most practicing hospitalists will easily qualify simply by doing their daily jobs. Enrollment does require an administrative fee, but many HM programs can—and should—reimburse you for these fees, so be sure to ask if your program will cover the cost.
After enrolling and paying the fee, your next step is to accumulate points toward certification. Of note, the 100 points do not all have to be accumulated prior to sitting for the exam, but accumulating these points generally prepares you for the exam, so it is a good idea to complete this task before the exam, in most circumstances.
The medical knowledge modules can be completed through ABIM/ABFM, the Society of Hospital Medicine (SHM), or the New England Journal of Medicine.1 A repertoire of clinical and non-clinical modules are offered by ABIM, and there are two modules on quality-patient safety offered by SHM. You can attend a number of pre-courses offered at local-regional-national HM meetings; these modules can be completed individually or in a group setting. A list of available group learning sessions can be found at www.abim.org. You can earn CME credit for completing these modules. Not only are the medical knowledge modules readily available, but they are also well written, are easy to complete, and prepare you well for the exam.
The practice performance modules can be completed through ABIM/ABFM or through a number of medical centers that participate in the American Board of Medical Specialties “Portfolio Program.” For organizations that participate in the program, hospitalists within the organizational network who have completed a quality improvement project may qualify for module credit. A list of these sponsoring organizations can be found at http://mocportfolioprogram.org/approved-portfolio-sponsors.
Hospitalists can earn practice improvement module (PIM) credit for being involved in a number of large collaborative projects, including SHM’s mentored implementation programs (e.g. glycemic control, VTE, and Project BOOST).3
For those completing a PIM through the ABIM, the most straightforward are the self-directed PIM or the completed project PIM.2
2. The exam content is known. Table 2 lists the content categories of the secure exam, published by ABIM, with approximate percentages of the content within overall categories and subcategories. This information helps you focus your efforts in preparing for the exam and is aligned with what most hospitalists practice on a daily basis.
3. The exam preparation is easy. Not only is the content outlined in the blueprint in Table 2, but practice exams are available online from the ABIM and a tutorial can be found at www.abim.org/hospital-medicine-tutorial. This tutorial simulates the actual exam, to enhance preparation and reduce testing anxiety.
4. The exam pass rate is high. Table 3 lists pass rates from the 2010-2012 hospital medicine exam. These pass rates are equivalent to the general medicine exam, and they exceed some of the other specialty exam pass rates.
5. RFPHM is gaining more of the recognition it deserves. Given this growth in recognition, from employers, peers, patients, and maybe even payors, it would serve you well to start the process early, because it is highly likely to gain traction in the coming years.
Join Us
All told, RFPHM enrollment, preparation, and exam completion are straightforward, relatively easy, and worth the time and energy. I hope you join me and the 418 other hospitalists who have pursued this recognition. You will be glad you invested in your future.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- American Board of Internal Medicine. List of self-evaluation modules. Available at: http://www.abim.org/maintenance-of-certification/medical-knowledge/modules.aspx#hosp. Accessed November 27, 2013.
- American Board of Internal Medicine. List of PIMs from ABIM. Available at: http://www.abim.org/moc/earning-points.aspx. Accessed November 27, 2013.
- American Board of Internal Medicine. List of PIMs from sponsoring institutions. Available at: http://www.abim.org/moc/earning-points/productinfo-demo-ordering.aspx#aqi. Accessed November 27, 2013.
By now, most hospitalists have at least heard about the Recognition in Focused Practice in Hospital Medicine (RFPHM), which is offered as a variation in certification for internal medicine- and family medicine-trained graduates who are pursuing Maintenance of Certification (MOC). Although the requirements are relatively straightforward, it may not be abundantly clear exactly why a hospitalist would pursue this pathway. As a recent “graduate” of the first cycle of the program, I can testify it is wholly worth the time and energy for the following reasons:
1. The requirements are relatively easy. Table 1 outlines the requirements for eligibility for enrolling in the program through the American Board of Internal Medicine (ABIM); enrollment through the American Board of Family Medicine (ABFM) also is available. These are basic requirements, and most practicing hospitalists will easily qualify simply by doing their daily jobs. Enrollment does require an administrative fee, but many HM programs can—and should—reimburse you for these fees, so be sure to ask if your program will cover the cost.
After enrolling and paying the fee, your next step is to accumulate points toward certification. Of note, the 100 points do not all have to be accumulated prior to sitting for the exam, but accumulating these points generally prepares you for the exam, so it is a good idea to complete this task before the exam, in most circumstances.
The medical knowledge modules can be completed through ABIM/ABFM, the Society of Hospital Medicine (SHM), or the New England Journal of Medicine.1 A repertoire of clinical and non-clinical modules are offered by ABIM, and there are two modules on quality-patient safety offered by SHM. You can attend a number of pre-courses offered at local-regional-national HM meetings; these modules can be completed individually or in a group setting. A list of available group learning sessions can be found at www.abim.org. You can earn CME credit for completing these modules. Not only are the medical knowledge modules readily available, but they are also well written, are easy to complete, and prepare you well for the exam.
The practice performance modules can be completed through ABIM/ABFM or through a number of medical centers that participate in the American Board of Medical Specialties “Portfolio Program.” For organizations that participate in the program, hospitalists within the organizational network who have completed a quality improvement project may qualify for module credit. A list of these sponsoring organizations can be found at http://mocportfolioprogram.org/approved-portfolio-sponsors.
Hospitalists can earn practice improvement module (PIM) credit for being involved in a number of large collaborative projects, including SHM’s mentored implementation programs (e.g. glycemic control, VTE, and Project BOOST).3
For those completing a PIM through the ABIM, the most straightforward are the self-directed PIM or the completed project PIM.2
2. The exam content is known. Table 2 lists the content categories of the secure exam, published by ABIM, with approximate percentages of the content within overall categories and subcategories. This information helps you focus your efforts in preparing for the exam and is aligned with what most hospitalists practice on a daily basis.
3. The exam preparation is easy. Not only is the content outlined in the blueprint in Table 2, but practice exams are available online from the ABIM and a tutorial can be found at www.abim.org/hospital-medicine-tutorial. This tutorial simulates the actual exam, to enhance preparation and reduce testing anxiety.
4. The exam pass rate is high. Table 3 lists pass rates from the 2010-2012 hospital medicine exam. These pass rates are equivalent to the general medicine exam, and they exceed some of the other specialty exam pass rates.
5. RFPHM is gaining more of the recognition it deserves. Given this growth in recognition, from employers, peers, patients, and maybe even payors, it would serve you well to start the process early, because it is highly likely to gain traction in the coming years.
Join Us
All told, RFPHM enrollment, preparation, and exam completion are straightforward, relatively easy, and worth the time and energy. I hope you join me and the 418 other hospitalists who have pursued this recognition. You will be glad you invested in your future.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
- American Board of Internal Medicine. List of self-evaluation modules. Available at: http://www.abim.org/maintenance-of-certification/medical-knowledge/modules.aspx#hosp. Accessed November 27, 2013.
- American Board of Internal Medicine. List of PIMs from ABIM. Available at: http://www.abim.org/moc/earning-points.aspx. Accessed November 27, 2013.
- American Board of Internal Medicine. List of PIMs from sponsoring institutions. Available at: http://www.abim.org/moc/earning-points/productinfo-demo-ordering.aspx#aqi. Accessed November 27, 2013.
Centers for Medicare & Medicaid Services (CMS) Allowing Specialty Society Registries To Submit Quality Data to PQRS
Hospitalists shouldn't get too excited over the recent decision by the Centers for Medicare & Medicaid Services (CMS) that allows specialty society-run clinical data registries to submit their own quality metrics under the Physician Quality Reporting System (PQRS).
CMS earlier this month agreed to let specialist medical societies draw up their own quality measures, but to qualify, societies must have a certified clinical data registry. SHM’s Public Policy Committee (PPC) and Performance Measurement and Reporting Committee (PMRC) consistently provide feedback to CMS on the current PQRS quality measures and is reviewing the potential value of a clinical data registry for SHM members in the future.
PPC and Team Hospitalist member Joshua Lenchus, DO, RPh, FACP, SFHM, says he and other hospitalist leaders will discuss CMS' decision, but he wonders whether the reporting system's average payment adjustment for foreseeable program years and hospitalist interest is high enough to make establishing a data registry worthwhile. “The question begs,” Dr. Lenchus says, “is the benefit worth the effort?”
The 2014 Medicare physician fee schedule [PDF] reported that 26,515 medical practices with 266,521 eligible professionals participated in PQRS in 2011—or about 27% of eligible providers. SHM has encouraged its members to participate since the system's inception in 2007 to both take advantage of incentive payments that were available and to prepare for upcoming penalties for failure to report. Starting in 2015 and based on 2013 performance, there will be a penalty for not reporting PQRS quality measures.
Dr. Lenchus says PPC members will continue to monitor and advocate for quality metrics that are more in line with daily hospitalist duties. Similarly, SHM's Performance Measurement and Reporting Committee (PMRC) has been working to identify and ensure measures applicable to HM are included in PQRS.
"The committee is deeply concerned about the limited number of PQRS measures broadly applicable to hospitalists, and we are working to change this disparity," wrote Greg Seymann, MD, SFHM, chief of the division of hospital medicine at the University of California at San Diego and chair of SHM’s PMRC, and Josh Boswell, SHM’s senior manager of government relations in The Hospitalist last month.
Dr. Lenchus adds that while SHM and other societies can weigh in on the measures, CMS remains the final arbiter.
"Groups will submit whatever metrics they would like to be assessed against and those metrics will not be taken carte blanche, but rather will require CMS approval," he says.
Visit our website for more information about PQRS.
Hospitalists shouldn't get too excited over the recent decision by the Centers for Medicare & Medicaid Services (CMS) that allows specialty society-run clinical data registries to submit their own quality metrics under the Physician Quality Reporting System (PQRS).
CMS earlier this month agreed to let specialist medical societies draw up their own quality measures, but to qualify, societies must have a certified clinical data registry. SHM’s Public Policy Committee (PPC) and Performance Measurement and Reporting Committee (PMRC) consistently provide feedback to CMS on the current PQRS quality measures and is reviewing the potential value of a clinical data registry for SHM members in the future.
PPC and Team Hospitalist member Joshua Lenchus, DO, RPh, FACP, SFHM, says he and other hospitalist leaders will discuss CMS' decision, but he wonders whether the reporting system's average payment adjustment for foreseeable program years and hospitalist interest is high enough to make establishing a data registry worthwhile. “The question begs,” Dr. Lenchus says, “is the benefit worth the effort?”
The 2014 Medicare physician fee schedule [PDF] reported that 26,515 medical practices with 266,521 eligible professionals participated in PQRS in 2011—or about 27% of eligible providers. SHM has encouraged its members to participate since the system's inception in 2007 to both take advantage of incentive payments that were available and to prepare for upcoming penalties for failure to report. Starting in 2015 and based on 2013 performance, there will be a penalty for not reporting PQRS quality measures.
Dr. Lenchus says PPC members will continue to monitor and advocate for quality metrics that are more in line with daily hospitalist duties. Similarly, SHM's Performance Measurement and Reporting Committee (PMRC) has been working to identify and ensure measures applicable to HM are included in PQRS.
"The committee is deeply concerned about the limited number of PQRS measures broadly applicable to hospitalists, and we are working to change this disparity," wrote Greg Seymann, MD, SFHM, chief of the division of hospital medicine at the University of California at San Diego and chair of SHM’s PMRC, and Josh Boswell, SHM’s senior manager of government relations in The Hospitalist last month.
Dr. Lenchus adds that while SHM and other societies can weigh in on the measures, CMS remains the final arbiter.
"Groups will submit whatever metrics they would like to be assessed against and those metrics will not be taken carte blanche, but rather will require CMS approval," he says.
Visit our website for more information about PQRS.
Hospitalists shouldn't get too excited over the recent decision by the Centers for Medicare & Medicaid Services (CMS) that allows specialty society-run clinical data registries to submit their own quality metrics under the Physician Quality Reporting System (PQRS).
CMS earlier this month agreed to let specialist medical societies draw up their own quality measures, but to qualify, societies must have a certified clinical data registry. SHM’s Public Policy Committee (PPC) and Performance Measurement and Reporting Committee (PMRC) consistently provide feedback to CMS on the current PQRS quality measures and is reviewing the potential value of a clinical data registry for SHM members in the future.
PPC and Team Hospitalist member Joshua Lenchus, DO, RPh, FACP, SFHM, says he and other hospitalist leaders will discuss CMS' decision, but he wonders whether the reporting system's average payment adjustment for foreseeable program years and hospitalist interest is high enough to make establishing a data registry worthwhile. “The question begs,” Dr. Lenchus says, “is the benefit worth the effort?”
The 2014 Medicare physician fee schedule [PDF] reported that 26,515 medical practices with 266,521 eligible professionals participated in PQRS in 2011—or about 27% of eligible providers. SHM has encouraged its members to participate since the system's inception in 2007 to both take advantage of incentive payments that were available and to prepare for upcoming penalties for failure to report. Starting in 2015 and based on 2013 performance, there will be a penalty for not reporting PQRS quality measures.
Dr. Lenchus says PPC members will continue to monitor and advocate for quality metrics that are more in line with daily hospitalist duties. Similarly, SHM's Performance Measurement and Reporting Committee (PMRC) has been working to identify and ensure measures applicable to HM are included in PQRS.
"The committee is deeply concerned about the limited number of PQRS measures broadly applicable to hospitalists, and we are working to change this disparity," wrote Greg Seymann, MD, SFHM, chief of the division of hospital medicine at the University of California at San Diego and chair of SHM’s PMRC, and Josh Boswell, SHM’s senior manager of government relations in The Hospitalist last month.
Dr. Lenchus adds that while SHM and other societies can weigh in on the measures, CMS remains the final arbiter.
"Groups will submit whatever metrics they would like to be assessed against and those metrics will not be taken carte blanche, but rather will require CMS approval," he says.
Visit our website for more information about PQRS.
Infection Prevention Campaign Solicits Patient Participation
How would hospitalists feel if patients or families asked them to wash their hands when they entered the hospital room? A new campaign called "Infection Prevention and You," engages patients to help hospitals overcome one of the most persistent barriers to preventing hospital-acquired infections (HAIs)—healthcare professionals failing to practice proper hand hygiene.
Launched by the Association for Professionals in Infection Control and Epidemiology (APIC), the organization"s executives contend that everyone plays a role in infection prevention.
"We know that washing hands is important, and so many things have been tried," says Carol McLay, DrPH, MPH, RN, CIC, infection prevention consultant and chair of APIC's Communications Committee. "Patient empowerment is one of the newer approaches. Studies have shown that patients really like the idea, but often are afraid to speak up."
Dr. McLay says hand-washing advocacy is one piece of a larger campaign for preventing HAIs across settings of care.
"I would hope that physicians, including hospitalists, would view it as an opportunity to do the right thing, to serve as effective role models, and to say to their patients, 'Your health is important to me,'" she says.
"The aspiration of having anyone and everyone speak up and ask providers to apply hand hygiene is laudable," says hospitalist Ethan Cumbler, MD, FACP, who has spearheaded a multidisciplinary hand hygiene initiative at University of Colorado Hospital in Aurora. But he says it is naive to expect all providers to respond positively to being corrected in this way. "At first, we may bristle at being challenged on hand hygiene, but when we consider what kind of physicians we want to be, and what kind of culture we want to work in, I believe it is a challenge we will come to appreciate," Dr. Cumbler says.
Visit our website for more information about hospitalists and infection prevention.
How would hospitalists feel if patients or families asked them to wash their hands when they entered the hospital room? A new campaign called "Infection Prevention and You," engages patients to help hospitals overcome one of the most persistent barriers to preventing hospital-acquired infections (HAIs)—healthcare professionals failing to practice proper hand hygiene.
Launched by the Association for Professionals in Infection Control and Epidemiology (APIC), the organization"s executives contend that everyone plays a role in infection prevention.
"We know that washing hands is important, and so many things have been tried," says Carol McLay, DrPH, MPH, RN, CIC, infection prevention consultant and chair of APIC's Communications Committee. "Patient empowerment is one of the newer approaches. Studies have shown that patients really like the idea, but often are afraid to speak up."
Dr. McLay says hand-washing advocacy is one piece of a larger campaign for preventing HAIs across settings of care.
"I would hope that physicians, including hospitalists, would view it as an opportunity to do the right thing, to serve as effective role models, and to say to their patients, 'Your health is important to me,'" she says.
"The aspiration of having anyone and everyone speak up and ask providers to apply hand hygiene is laudable," says hospitalist Ethan Cumbler, MD, FACP, who has spearheaded a multidisciplinary hand hygiene initiative at University of Colorado Hospital in Aurora. But he says it is naive to expect all providers to respond positively to being corrected in this way. "At first, we may bristle at being challenged on hand hygiene, but when we consider what kind of physicians we want to be, and what kind of culture we want to work in, I believe it is a challenge we will come to appreciate," Dr. Cumbler says.
Visit our website for more information about hospitalists and infection prevention.
How would hospitalists feel if patients or families asked them to wash their hands when they entered the hospital room? A new campaign called "Infection Prevention and You," engages patients to help hospitals overcome one of the most persistent barriers to preventing hospital-acquired infections (HAIs)—healthcare professionals failing to practice proper hand hygiene.
Launched by the Association for Professionals in Infection Control and Epidemiology (APIC), the organization"s executives contend that everyone plays a role in infection prevention.
"We know that washing hands is important, and so many things have been tried," says Carol McLay, DrPH, MPH, RN, CIC, infection prevention consultant and chair of APIC's Communications Committee. "Patient empowerment is one of the newer approaches. Studies have shown that patients really like the idea, but often are afraid to speak up."
Dr. McLay says hand-washing advocacy is one piece of a larger campaign for preventing HAIs across settings of care.
"I would hope that physicians, including hospitalists, would view it as an opportunity to do the right thing, to serve as effective role models, and to say to their patients, 'Your health is important to me,'" she says.
"The aspiration of having anyone and everyone speak up and ask providers to apply hand hygiene is laudable," says hospitalist Ethan Cumbler, MD, FACP, who has spearheaded a multidisciplinary hand hygiene initiative at University of Colorado Hospital in Aurora. But he says it is naive to expect all providers to respond positively to being corrected in this way. "At first, we may bristle at being challenged on hand hygiene, but when we consider what kind of physicians we want to be, and what kind of culture we want to work in, I believe it is a challenge we will come to appreciate," Dr. Cumbler says.
Visit our website for more information about hospitalists and infection prevention.
Simple Tool Improves Communication Between Patients, Hospitalists
Hospitalists at the University of Michigan Health System in Ann Arbor have developed a tool to help facilitate patient communication with physicians and to "actively participate in their treatments," says Aaron Farberg, MD. "Their treatment plans will, in turn, be more effective," Dr. Farberg adds.
Called Dear Doctor (DD) notes, the tool is a pre-formatted notepad placed on a bedside table for hospital patients to consult throughout their stay. Patients can write down questions under three suggested prompts: diagnosis and treatment, tests and procedures, and medications. Such a simple tool is "absent in the inpatient setting, and can have an impact on a patient’s perceived and actual medical care," Dr. Farberg says.
Family members of patients can also benefit from DD notes by voicing their questions or concerns to the physicians. “Often their active participation in the healthcare plan is an essential element in successful treatment,” Dr. Farberg says.
Surveyed patients experienced better communication with hospitalists and had an enhanced experience with their providers and hospital. Patients and their families were happy their questions were answered and not forgotten. They had a sense of control and accountability in their own care. The study urges hospitalists and care providers to be mindful of the patient’s entire experience throughout hospital stay. TH
Visit our website for more information on hospitalists and patient communication.
Hospitalists at the University of Michigan Health System in Ann Arbor have developed a tool to help facilitate patient communication with physicians and to "actively participate in their treatments," says Aaron Farberg, MD. "Their treatment plans will, in turn, be more effective," Dr. Farberg adds.
Called Dear Doctor (DD) notes, the tool is a pre-formatted notepad placed on a bedside table for hospital patients to consult throughout their stay. Patients can write down questions under three suggested prompts: diagnosis and treatment, tests and procedures, and medications. Such a simple tool is "absent in the inpatient setting, and can have an impact on a patient’s perceived and actual medical care," Dr. Farberg says.
Family members of patients can also benefit from DD notes by voicing their questions or concerns to the physicians. “Often their active participation in the healthcare plan is an essential element in successful treatment,” Dr. Farberg says.
Surveyed patients experienced better communication with hospitalists and had an enhanced experience with their providers and hospital. Patients and their families were happy their questions were answered and not forgotten. They had a sense of control and accountability in their own care. The study urges hospitalists and care providers to be mindful of the patient’s entire experience throughout hospital stay. TH
Visit our website for more information on hospitalists and patient communication.
Hospitalists at the University of Michigan Health System in Ann Arbor have developed a tool to help facilitate patient communication with physicians and to "actively participate in their treatments," says Aaron Farberg, MD. "Their treatment plans will, in turn, be more effective," Dr. Farberg adds.
Called Dear Doctor (DD) notes, the tool is a pre-formatted notepad placed on a bedside table for hospital patients to consult throughout their stay. Patients can write down questions under three suggested prompts: diagnosis and treatment, tests and procedures, and medications. Such a simple tool is "absent in the inpatient setting, and can have an impact on a patient’s perceived and actual medical care," Dr. Farberg says.
Family members of patients can also benefit from DD notes by voicing their questions or concerns to the physicians. “Often their active participation in the healthcare plan is an essential element in successful treatment,” Dr. Farberg says.
Surveyed patients experienced better communication with hospitalists and had an enhanced experience with their providers and hospital. Patients and their families were happy their questions were answered and not forgotten. They had a sense of control and accountability in their own care. The study urges hospitalists and care providers to be mindful of the patient’s entire experience throughout hospital stay. TH
Visit our website for more information on hospitalists and patient communication.
Intravenous Haloperidol Does Not Prevent ICU Delirium
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Visit our website for more information on treating delirium in hospitalized patients.
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Visit our website for more information on treating delirium in hospitalized patients.
Clinical question: Can haloperidol reduce delirium in critically ill patients if initiated early in ICU stay?
Background: Prior studies suggest antipsychotics reduce intensity and duration of delirium in hospitalized patients. Evidence is mixed for preventing delirium. A trial of risperidone demonstrated delirium rate reduction in coronary artery bypass grafting (CABG) patients, but another trial of haloperidol in hip surgery patients failed to prevent onset of delirium. There is little evidence on antipsychotics in ICU delirium.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single, adult ICU in England.
Synopsis: The study randomized 142 critically ill patients to receive 2.5 mg of intravenous haloperidol versus placebo every eight hours for up to 14 days. There was no significant difference between groups in the total time spent free of delirium or coma. Limitations include the use of open-label haloperidol in 21% of the placebo group patients. More sedation but less agitation was seen with the use of haloperidol, which also prolonged QTc. No severe adverse effects were observed.
This study supports the idea that scheduled antipsychotics should not be used to reduce ICU delirium. Addressing modifiable risk factors and using dexmedetomidine rather than lorazepam for sedation in the ICU continue to be first-line strategies to lower delirium rates.
Bottom line: Prophylactic haloperidol should not be used to prevent ICU delirium.
Citation: Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 2013;1(7):515-523.
Visit our website for more information on treating delirium in hospitalized patients.
Hospitalist Group Tackles Palliative Care; National Chain Explores Opportunities
At the Kaiser Permanente Medical Center in San Rafael, Calif., the 20 members of the hospitalist group were encouraged to study together in preparation for the October 2012 HPM boards. The group undertook weekly study sessions for the five months leading up to the exam. Sixteen hospitalists sat for the exam, along with oncologists, nephrologists, pulmonologists, and primary care physicians from the medical center.
All passed.
“For years, our hospitalist group has been doing actual rounding with the palliative care team on their own patients,” says Shideh Shadan, MD, the hospitalist group leader. “Everyone was on board with palliative care. It is now part of our daily care, and all we had to do was to sit down and study for the exam.”
Most of Kaiser’s HMO medical centers have designated interdisciplinary palliative care consultation teams. The one at San Rafael includes nurses, social workers, chaplains, and a part-time physician who is a hospitalist, Clay Angel, MD. Dr. Angel agrees that a cultural transformation has come about at Kaiser San Rafael through this collaboration. The two services are separate but closely connected.
“In hospital medicine, if you keep farming out what you do to specialists—if you’re not embracing palliative care as a hospitalist—you lose part of your practice,” he says.
Dr. Shadan says the study group “helped us to be more cohesive and more comfortable going to each other to ask for help. Palliative care is part of what we do—part of hospital medicine and of providing good care.”
Meanwhile, North Hollywood, Calif.-based IPC The Hospitalist Company, which is well-established in post-acute and long-term-care settings beyond the hospital walls, is now starting to explore palliative care approaches at the local level in a few of its 35 markets. Heather Zinzella-Cox, MD, who was part of a panel presentation on palliative care at HM13, is hospitalist practice group leader for IPC-Delaware. She also works part time as an associate medical director for a community hospice and helped to develop an inpatient palliative care team at a local community hospital.
“For me, as a post-acute hospitalist, every patient I see, I think about whether palliative care might benefit them,” says Dr. Zinzella-Cox, who is board certified in pain and in hospice and palliative medicine.
She says hospitalists need tools for identifying appropriate palliative care patients, along with training for how to communicate with them around goals of care, including simple language to help cue these conversations. She notes a “significant voltage drop” in information at the time of discharge, and the most careful discharge plans can fall apart in a hurry after the patient goes home.
IPC’s national practice group does not have a current policy or initiative for palliative care; however, there may be opportunities for further integrating palliative care with hospital medicine, says hospitalist Thomas Mathew, MD.
Larry Beresford is a freelance writer in San Francisco.
At the Kaiser Permanente Medical Center in San Rafael, Calif., the 20 members of the hospitalist group were encouraged to study together in preparation for the October 2012 HPM boards. The group undertook weekly study sessions for the five months leading up to the exam. Sixteen hospitalists sat for the exam, along with oncologists, nephrologists, pulmonologists, and primary care physicians from the medical center.
All passed.
“For years, our hospitalist group has been doing actual rounding with the palliative care team on their own patients,” says Shideh Shadan, MD, the hospitalist group leader. “Everyone was on board with palliative care. It is now part of our daily care, and all we had to do was to sit down and study for the exam.”
Most of Kaiser’s HMO medical centers have designated interdisciplinary palliative care consultation teams. The one at San Rafael includes nurses, social workers, chaplains, and a part-time physician who is a hospitalist, Clay Angel, MD. Dr. Angel agrees that a cultural transformation has come about at Kaiser San Rafael through this collaboration. The two services are separate but closely connected.
“In hospital medicine, if you keep farming out what you do to specialists—if you’re not embracing palliative care as a hospitalist—you lose part of your practice,” he says.
Dr. Shadan says the study group “helped us to be more cohesive and more comfortable going to each other to ask for help. Palliative care is part of what we do—part of hospital medicine and of providing good care.”
Meanwhile, North Hollywood, Calif.-based IPC The Hospitalist Company, which is well-established in post-acute and long-term-care settings beyond the hospital walls, is now starting to explore palliative care approaches at the local level in a few of its 35 markets. Heather Zinzella-Cox, MD, who was part of a panel presentation on palliative care at HM13, is hospitalist practice group leader for IPC-Delaware. She also works part time as an associate medical director for a community hospice and helped to develop an inpatient palliative care team at a local community hospital.
“For me, as a post-acute hospitalist, every patient I see, I think about whether palliative care might benefit them,” says Dr. Zinzella-Cox, who is board certified in pain and in hospice and palliative medicine.
She says hospitalists need tools for identifying appropriate palliative care patients, along with training for how to communicate with them around goals of care, including simple language to help cue these conversations. She notes a “significant voltage drop” in information at the time of discharge, and the most careful discharge plans can fall apart in a hurry after the patient goes home.
IPC’s national practice group does not have a current policy or initiative for palliative care; however, there may be opportunities for further integrating palliative care with hospital medicine, says hospitalist Thomas Mathew, MD.
Larry Beresford is a freelance writer in San Francisco.
At the Kaiser Permanente Medical Center in San Rafael, Calif., the 20 members of the hospitalist group were encouraged to study together in preparation for the October 2012 HPM boards. The group undertook weekly study sessions for the five months leading up to the exam. Sixteen hospitalists sat for the exam, along with oncologists, nephrologists, pulmonologists, and primary care physicians from the medical center.
All passed.
“For years, our hospitalist group has been doing actual rounding with the palliative care team on their own patients,” says Shideh Shadan, MD, the hospitalist group leader. “Everyone was on board with palliative care. It is now part of our daily care, and all we had to do was to sit down and study for the exam.”
Most of Kaiser’s HMO medical centers have designated interdisciplinary palliative care consultation teams. The one at San Rafael includes nurses, social workers, chaplains, and a part-time physician who is a hospitalist, Clay Angel, MD. Dr. Angel agrees that a cultural transformation has come about at Kaiser San Rafael through this collaboration. The two services are separate but closely connected.
“In hospital medicine, if you keep farming out what you do to specialists—if you’re not embracing palliative care as a hospitalist—you lose part of your practice,” he says.
Dr. Shadan says the study group “helped us to be more cohesive and more comfortable going to each other to ask for help. Palliative care is part of what we do—part of hospital medicine and of providing good care.”
Meanwhile, North Hollywood, Calif.-based IPC The Hospitalist Company, which is well-established in post-acute and long-term-care settings beyond the hospital walls, is now starting to explore palliative care approaches at the local level in a few of its 35 markets. Heather Zinzella-Cox, MD, who was part of a panel presentation on palliative care at HM13, is hospitalist practice group leader for IPC-Delaware. She also works part time as an associate medical director for a community hospice and helped to develop an inpatient palliative care team at a local community hospital.
“For me, as a post-acute hospitalist, every patient I see, I think about whether palliative care might benefit them,” says Dr. Zinzella-Cox, who is board certified in pain and in hospice and palliative medicine.
She says hospitalists need tools for identifying appropriate palliative care patients, along with training for how to communicate with them around goals of care, including simple language to help cue these conversations. She notes a “significant voltage drop” in information at the time of discharge, and the most careful discharge plans can fall apart in a hurry after the patient goes home.
IPC’s national practice group does not have a current policy or initiative for palliative care; however, there may be opportunities for further integrating palliative care with hospital medicine, says hospitalist Thomas Mathew, MD.
Larry Beresford is a freelance writer in San Francisco.
American Academy of Hospice and Palliative Medicine EVP Explains Hospitalists' Important Role in End-of-Life Planning
Click here for excerpts of our interview with Porter Storey, MD, executive vice president of the American Academy of Hospice and Palliative Medicine.
Click here for excerpts of our interview with Porter Storey, MD, executive vice president of the American Academy of Hospice and Palliative Medicine.
Click here for excerpts of our interview with Porter Storey, MD, executive vice president of the American Academy of Hospice and Palliative Medicine.
Society of Hospital Medicine (SHM) Epitomizes Professional Diversity
I just got back from a trip to SHM headquarters in Philadelphia, and all I can say is “wow.” I was visiting there for a meeting with the staff, many SHM members and committee leaders, and the SHM board of directors. The first day we all went into a big, modern, beautiful room at SHM headquarters—there must have been more than 100 people—and we went around the room and introduced ourselves. The diversity of the staff that support our society, and the diversity of the members there, was truly breathtaking. What I saw was a microcosm of our society and our specialty.
Looking around the room, it was easy to see some aspects of our diverse organization: both genders and a variety of ethnicities and age groups were well represented. These traditional measures of diversity are critical to a healthy environment, in my opinion, and the data bear out the idea that a diverse workforce can reduce turnover and be more creative and qualified.1,2 Our diversity is not an accident. It is part of a larger, deliberate strategy by SHM to be “the home” for healthcare professionals who provide hospital-based patient care. SHM embraces diversity, whether it’s skin deep or deeply cognitive.
Although we are continually working to enrich the traditional aspects of diversity, we are also very hard at work to make SHM a place of professional diversity.
Open and Inclusive
Over the past several years, SHM has worked hard to be openly inclusive. Many of the committees and sections within the society have been developed specifically to embrace important aspects of hospital medicine that have special or common interests, characteristics, or needs. Examples include the international section, med-peds section, administrators’ committee, and the nurse practitioner and physician assistant committee. These venues allow individuals under a Big Tent to find others with similar interests or training, so that they can address unique aspects of hospital medicine as it relates directly to them. SHM’s virtual world is following our committee and section structure, which has some of the most actively growing HMXchange communities coming from the “administrators” community and the “NP/PA” community.
SHM has put its money where its mouth is, dedicating significant resources for educational programs that will help benefit professionals with a variety of backgrounds. Some are focused on the special needs of our diverse physician population, including the Academic Hospitalist Academy, the Quality and Safety Educators Academy, and the Pediatric Hospital Medicine annual meeting (through a partnership with the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association). Other events are focused specifically on helping our non-physician colleagues, like the boot camp that is presented in collaboration with the American Academy of Physician Assistants and American Association of Nurse Practitioners. The SHM Leadership Academies attract a venerable alphabet soup of professional designations, including many MDs and DOs, of course, but also increasing numbers of PAs and NPs, a growing number of administrators, and now even a few ED and OB docs! Now that’s a Big Tent.
My understanding is that these events are always popular and often sold out.
Maybe the most powerful evidence that our Big Tent philosophy is working is found in the relationships SHM has forged with other hospital-based specialties, like obstetrics, neurology, and surgery. The president of the Society of OB/GYN Hospitalists (societyofobgynhospitalists.com) has attended the SHM annual meeting and at least one of the Leadership Academies. Although “traditional” hospitalists like me may not be able to help in the OR or birthing suite, we have a lot of experience in quality improvement, leadership, and, of course, addressing the needs of a new and growing professional segment. The emergence and growth of these “specialty hospitalists” offers a unique opportunity for traditional hospitalists to partner with our subspecialty colleagues in a new way, so that together we can continue to improve patient care within the hospital across multiple disciplines.
What’s Ahead?
Based on the data I recently saw while at SHM headquarters, the Big Tent philosophy is a measurable success. Membership for NPs, PAs, and administrators is growing, with nearly 200 new members in those categories combined. Incredibly, we have ED physicians joining our organization—albeit, at a number dwarfed by internists—and the relationships with the specialty hospitalists are moving forward in a meaningful way. Looking at committees and committee chairs, there is plenty of ethnic, professional, and gender diversity.
What does all of this focus outside of internal medicine and physician groups mean for us internists? Will we be left behind? Fret not. Physicians make up more than 85% of our 12,000-plus members, with internists outnumbering—by a huge number—all of the other segments of our society combined. There is no Big Tent so large that physicians, or even internists, will ever be in jeopardy. We occupy plenty of space under this Big Tent and still have lots of room to spare for our colleagues. In welcoming others, we all strengthen our own standing, by elevating the entire field.
As a terrific mentor once said, a rising tide floats all boats. And the way to raise the tide of hospital medicine can be through partnerships whose gravity is a strong pull on the hospital medicine tide, as the moon pulls the ocean’s tides.
One area in which our society plans to place more effort in expanding the Big Tent is with trainees. Students and housestaff are one of the smallest groups in our organization, with the smallest growth. Those statistics are cause for concern. The need for future hospitalist growth, both in numbers and skill set, makes attracting this segment of paramount importance, in my view.
Fortunately, SHM is developing a strategy to make our society a valuable home to trainees. I have touched on those strategies previously, including a Physicians in Training Committee, free membership for students, $100 memberships for housestaff, and our “1,000 Challenge” to recruit 1,000 students and housestaff in the coming months.
In Sum
I am a firm believer in professional and personal diversity. I am proud to work in a society that also embraces this philosophy, places real value on it, and works hard to be inclusive. So, the next time you meet an NP, PA, student, or even a hospital-based OB physician, bring them under the SHM Big Tent, and encourage them to join us in making the hospital world a better place. They, we, and our patients will be better off for it.
Dr. Howell is president of SHM, chief of the division of hospital medicine at Johns Hopkins Bayview in Baltimore, and spends a significant part of his time and research on hospital operations. Email questions or comments to [email protected].
References
- Egan ME. Global diversity and inclusion: Fostering innovation through a diverse workforce. Forbes Insights. Forbes website. Available at: http://images.forbes.com/forbesinsights/StudyPDFs/Innovation_Through_Diversity.pdf. Accessed October 23, 2013.
- Kerby S, Burns C. The top 10 economic facts of diversity in the workplace. Center for American Progress website. Available at: http://www.americanprogress.org/issues/labor/news/2012/07/12/11900/the-top-10-economic-facts-of-diversity-in-the-workplace. Accessed October 23, 2013.
I just got back from a trip to SHM headquarters in Philadelphia, and all I can say is “wow.” I was visiting there for a meeting with the staff, many SHM members and committee leaders, and the SHM board of directors. The first day we all went into a big, modern, beautiful room at SHM headquarters—there must have been more than 100 people—and we went around the room and introduced ourselves. The diversity of the staff that support our society, and the diversity of the members there, was truly breathtaking. What I saw was a microcosm of our society and our specialty.
Looking around the room, it was easy to see some aspects of our diverse organization: both genders and a variety of ethnicities and age groups were well represented. These traditional measures of diversity are critical to a healthy environment, in my opinion, and the data bear out the idea that a diverse workforce can reduce turnover and be more creative and qualified.1,2 Our diversity is not an accident. It is part of a larger, deliberate strategy by SHM to be “the home” for healthcare professionals who provide hospital-based patient care. SHM embraces diversity, whether it’s skin deep or deeply cognitive.
Although we are continually working to enrich the traditional aspects of diversity, we are also very hard at work to make SHM a place of professional diversity.
Open and Inclusive
Over the past several years, SHM has worked hard to be openly inclusive. Many of the committees and sections within the society have been developed specifically to embrace important aspects of hospital medicine that have special or common interests, characteristics, or needs. Examples include the international section, med-peds section, administrators’ committee, and the nurse practitioner and physician assistant committee. These venues allow individuals under a Big Tent to find others with similar interests or training, so that they can address unique aspects of hospital medicine as it relates directly to them. SHM’s virtual world is following our committee and section structure, which has some of the most actively growing HMXchange communities coming from the “administrators” community and the “NP/PA” community.
SHM has put its money where its mouth is, dedicating significant resources for educational programs that will help benefit professionals with a variety of backgrounds. Some are focused on the special needs of our diverse physician population, including the Academic Hospitalist Academy, the Quality and Safety Educators Academy, and the Pediatric Hospital Medicine annual meeting (through a partnership with the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association). Other events are focused specifically on helping our non-physician colleagues, like the boot camp that is presented in collaboration with the American Academy of Physician Assistants and American Association of Nurse Practitioners. The SHM Leadership Academies attract a venerable alphabet soup of professional designations, including many MDs and DOs, of course, but also increasing numbers of PAs and NPs, a growing number of administrators, and now even a few ED and OB docs! Now that’s a Big Tent.
My understanding is that these events are always popular and often sold out.
Maybe the most powerful evidence that our Big Tent philosophy is working is found in the relationships SHM has forged with other hospital-based specialties, like obstetrics, neurology, and surgery. The president of the Society of OB/GYN Hospitalists (societyofobgynhospitalists.com) has attended the SHM annual meeting and at least one of the Leadership Academies. Although “traditional” hospitalists like me may not be able to help in the OR or birthing suite, we have a lot of experience in quality improvement, leadership, and, of course, addressing the needs of a new and growing professional segment. The emergence and growth of these “specialty hospitalists” offers a unique opportunity for traditional hospitalists to partner with our subspecialty colleagues in a new way, so that together we can continue to improve patient care within the hospital across multiple disciplines.
What’s Ahead?
Based on the data I recently saw while at SHM headquarters, the Big Tent philosophy is a measurable success. Membership for NPs, PAs, and administrators is growing, with nearly 200 new members in those categories combined. Incredibly, we have ED physicians joining our organization—albeit, at a number dwarfed by internists—and the relationships with the specialty hospitalists are moving forward in a meaningful way. Looking at committees and committee chairs, there is plenty of ethnic, professional, and gender diversity.
What does all of this focus outside of internal medicine and physician groups mean for us internists? Will we be left behind? Fret not. Physicians make up more than 85% of our 12,000-plus members, with internists outnumbering—by a huge number—all of the other segments of our society combined. There is no Big Tent so large that physicians, or even internists, will ever be in jeopardy. We occupy plenty of space under this Big Tent and still have lots of room to spare for our colleagues. In welcoming others, we all strengthen our own standing, by elevating the entire field.
As a terrific mentor once said, a rising tide floats all boats. And the way to raise the tide of hospital medicine can be through partnerships whose gravity is a strong pull on the hospital medicine tide, as the moon pulls the ocean’s tides.
One area in which our society plans to place more effort in expanding the Big Tent is with trainees. Students and housestaff are one of the smallest groups in our organization, with the smallest growth. Those statistics are cause for concern. The need for future hospitalist growth, both in numbers and skill set, makes attracting this segment of paramount importance, in my view.
Fortunately, SHM is developing a strategy to make our society a valuable home to trainees. I have touched on those strategies previously, including a Physicians in Training Committee, free membership for students, $100 memberships for housestaff, and our “1,000 Challenge” to recruit 1,000 students and housestaff in the coming months.
In Sum
I am a firm believer in professional and personal diversity. I am proud to work in a society that also embraces this philosophy, places real value on it, and works hard to be inclusive. So, the next time you meet an NP, PA, student, or even a hospital-based OB physician, bring them under the SHM Big Tent, and encourage them to join us in making the hospital world a better place. They, we, and our patients will be better off for it.
Dr. Howell is president of SHM, chief of the division of hospital medicine at Johns Hopkins Bayview in Baltimore, and spends a significant part of his time and research on hospital operations. Email questions or comments to [email protected].
References
- Egan ME. Global diversity and inclusion: Fostering innovation through a diverse workforce. Forbes Insights. Forbes website. Available at: http://images.forbes.com/forbesinsights/StudyPDFs/Innovation_Through_Diversity.pdf. Accessed October 23, 2013.
- Kerby S, Burns C. The top 10 economic facts of diversity in the workplace. Center for American Progress website. Available at: http://www.americanprogress.org/issues/labor/news/2012/07/12/11900/the-top-10-economic-facts-of-diversity-in-the-workplace. Accessed October 23, 2013.
I just got back from a trip to SHM headquarters in Philadelphia, and all I can say is “wow.” I was visiting there for a meeting with the staff, many SHM members and committee leaders, and the SHM board of directors. The first day we all went into a big, modern, beautiful room at SHM headquarters—there must have been more than 100 people—and we went around the room and introduced ourselves. The diversity of the staff that support our society, and the diversity of the members there, was truly breathtaking. What I saw was a microcosm of our society and our specialty.
Looking around the room, it was easy to see some aspects of our diverse organization: both genders and a variety of ethnicities and age groups were well represented. These traditional measures of diversity are critical to a healthy environment, in my opinion, and the data bear out the idea that a diverse workforce can reduce turnover and be more creative and qualified.1,2 Our diversity is not an accident. It is part of a larger, deliberate strategy by SHM to be “the home” for healthcare professionals who provide hospital-based patient care. SHM embraces diversity, whether it’s skin deep or deeply cognitive.
Although we are continually working to enrich the traditional aspects of diversity, we are also very hard at work to make SHM a place of professional diversity.
Open and Inclusive
Over the past several years, SHM has worked hard to be openly inclusive. Many of the committees and sections within the society have been developed specifically to embrace important aspects of hospital medicine that have special or common interests, characteristics, or needs. Examples include the international section, med-peds section, administrators’ committee, and the nurse practitioner and physician assistant committee. These venues allow individuals under a Big Tent to find others with similar interests or training, so that they can address unique aspects of hospital medicine as it relates directly to them. SHM’s virtual world is following our committee and section structure, which has some of the most actively growing HMXchange communities coming from the “administrators” community and the “NP/PA” community.
SHM has put its money where its mouth is, dedicating significant resources for educational programs that will help benefit professionals with a variety of backgrounds. Some are focused on the special needs of our diverse physician population, including the Academic Hospitalist Academy, the Quality and Safety Educators Academy, and the Pediatric Hospital Medicine annual meeting (through a partnership with the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association). Other events are focused specifically on helping our non-physician colleagues, like the boot camp that is presented in collaboration with the American Academy of Physician Assistants and American Association of Nurse Practitioners. The SHM Leadership Academies attract a venerable alphabet soup of professional designations, including many MDs and DOs, of course, but also increasing numbers of PAs and NPs, a growing number of administrators, and now even a few ED and OB docs! Now that’s a Big Tent.
My understanding is that these events are always popular and often sold out.
Maybe the most powerful evidence that our Big Tent philosophy is working is found in the relationships SHM has forged with other hospital-based specialties, like obstetrics, neurology, and surgery. The president of the Society of OB/GYN Hospitalists (societyofobgynhospitalists.com) has attended the SHM annual meeting and at least one of the Leadership Academies. Although “traditional” hospitalists like me may not be able to help in the OR or birthing suite, we have a lot of experience in quality improvement, leadership, and, of course, addressing the needs of a new and growing professional segment. The emergence and growth of these “specialty hospitalists” offers a unique opportunity for traditional hospitalists to partner with our subspecialty colleagues in a new way, so that together we can continue to improve patient care within the hospital across multiple disciplines.
What’s Ahead?
Based on the data I recently saw while at SHM headquarters, the Big Tent philosophy is a measurable success. Membership for NPs, PAs, and administrators is growing, with nearly 200 new members in those categories combined. Incredibly, we have ED physicians joining our organization—albeit, at a number dwarfed by internists—and the relationships with the specialty hospitalists are moving forward in a meaningful way. Looking at committees and committee chairs, there is plenty of ethnic, professional, and gender diversity.
What does all of this focus outside of internal medicine and physician groups mean for us internists? Will we be left behind? Fret not. Physicians make up more than 85% of our 12,000-plus members, with internists outnumbering—by a huge number—all of the other segments of our society combined. There is no Big Tent so large that physicians, or even internists, will ever be in jeopardy. We occupy plenty of space under this Big Tent and still have lots of room to spare for our colleagues. In welcoming others, we all strengthen our own standing, by elevating the entire field.
As a terrific mentor once said, a rising tide floats all boats. And the way to raise the tide of hospital medicine can be through partnerships whose gravity is a strong pull on the hospital medicine tide, as the moon pulls the ocean’s tides.
One area in which our society plans to place more effort in expanding the Big Tent is with trainees. Students and housestaff are one of the smallest groups in our organization, with the smallest growth. Those statistics are cause for concern. The need for future hospitalist growth, both in numbers and skill set, makes attracting this segment of paramount importance, in my view.
Fortunately, SHM is developing a strategy to make our society a valuable home to trainees. I have touched on those strategies previously, including a Physicians in Training Committee, free membership for students, $100 memberships for housestaff, and our “1,000 Challenge” to recruit 1,000 students and housestaff in the coming months.
In Sum
I am a firm believer in professional and personal diversity. I am proud to work in a society that also embraces this philosophy, places real value on it, and works hard to be inclusive. So, the next time you meet an NP, PA, student, or even a hospital-based OB physician, bring them under the SHM Big Tent, and encourage them to join us in making the hospital world a better place. They, we, and our patients will be better off for it.
Dr. Howell is president of SHM, chief of the division of hospital medicine at Johns Hopkins Bayview in Baltimore, and spends a significant part of his time and research on hospital operations. Email questions or comments to [email protected].
References
- Egan ME. Global diversity and inclusion: Fostering innovation through a diverse workforce. Forbes Insights. Forbes website. Available at: http://images.forbes.com/forbesinsights/StudyPDFs/Innovation_Through_Diversity.pdf. Accessed October 23, 2013.
- Kerby S, Burns C. The top 10 economic facts of diversity in the workplace. Center for American Progress website. Available at: http://www.americanprogress.org/issues/labor/news/2012/07/12/11900/the-top-10-economic-facts-of-diversity-in-the-workplace. Accessed October 23, 2013.