User login
Acknowledgment
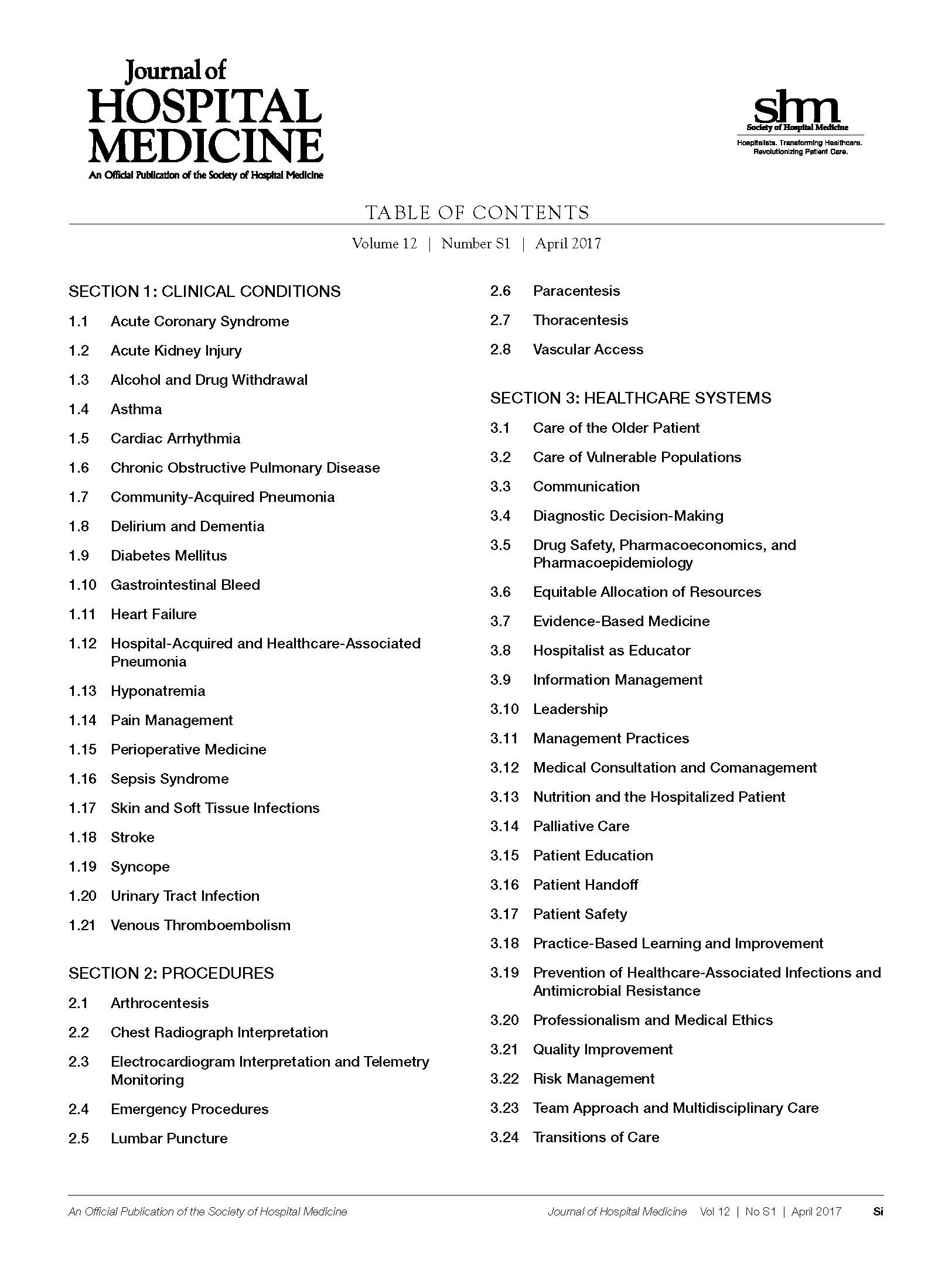
Core Competencies Table of Contents
The Revised Edition of The Core Competencies would not have been possible without the support and assistance of the Society of Hospital Medicine staff and countless practicing Hospitalists across the United States. The editors thank Nick Marzano for project coordination. Special thanks to Abbie Young for her thorough medical editing and updates to chapter introductions. The editors also thank their families for all their patience and support throughout the development process.
Society of Hospital Medicine leadership and subject matter experts who provided content, review and guidance include:
CHAPTER AUTHORS
Alberto Puig, MD, PhD, FACP, SFHM
Jeffrey Genato, MD, SFHM, UHM
Lorenzo Difrancesco, MD
Alpesh Amin, MD, MBA, MACP, SFHM
Nurcan Ilksoy, MD, FHM
John David Halporn, MD
Eugene Chu, MD, FHM
Brian Donovan, MD, SFHM
Alexander Carbo, MD, SFHM
Valeria Lang, MD, FHM
David Feinbloom, MD, SFHM
Richard Rohr, MD, SFHM
Lakshmi Halasyamani, MD, SFHM
Vijay Rajput, MBBS, FACP, SFHM
Tosha Wetterneck, MD, SFHM
Michael Ruhlen, MD, FAAP, FACHE, MHSc
Gregory Seymann, MD, SFHM
Jeffrey Barsuk, MD, SFHM
David J. Likosky, MD, FACP
Bindu Sangani, MD
Scott Flanders, MD, FACP, MHM
Chad Whelan, MD, FACP, FHM
Shaun Frost, MD, SFHM
Amir Jaffer, MD, MBA, SFHM
Michael Lukela, MD, SFHM, FACP, FAAP
Jonathan Crocker, MD, FHM
CORE COMPETENCIES TASK FORCE (2012-2016)
Satyen Nichani, MD, FHM (Chair)
Nick Fitterman, MD, SFHM, FACP
Michael Lukela, MD, SFHM, FACP, FAAP
Jonathan Crocker, MD, FHM
Tarun Ghosh, MD, FRCS, SFHM
Vikas Parekh, MD, FACP, SFHM
Nick Marzano, MEd
SHM EDUCATION COMMITTEE REVIEWERS
Jessie Kimbrough-Sugick, MD, MPH
Danielle Scheurer, MD, SFHM, MSCR
Amit Pahwa, MD
Anthony Breu, MD
Nathan Houchens, MD, FACP, FHM
Jeffrey Bates, MD, FACP, FHM
Ian Jenkins, MD, SFHM
Neel Shah, MB, BCh, SFHM
Elizabeth Cerceo, MD, FACP, FHM
Jeffrey Greenwald, MD, SFHM
Haruka Torok, MD, SFHM
Bartho Caponi, MD, FHM
Leonard Feldman, MD, FACP, FAAP, SFHM
Daniel Brotman, MD, SFHM
Alfred Burger, MD, SFHM
Jocelyn Carter, MD, MPH
Vinh-Tung Nguyen, MD
Kurt Pfeifer, MD, FACP, SFHM
Alberto Puig, MD, PhD, FACP, SFHM
Richard Vestal, MD
Judy Vu, MD, FAAP
CONTENT EXPERTS
Jason Persoff, MD, SFHM
Nilam Soni, MD, FHM
Lynnea Mills, MD
Wendy Anderson, MD, MS
Jeffrey Frank, MD, FACP, MBA
Howard Epstein, MD, SFHM, CHIE
Kendall Rogers, MD, SFHM
Prateek Gandiga, MD, FACP
Jeffrey Glasheen, MD, SFHM
Melissa Mattison, MD, SFHM
Vineet Arora, MD, MPP, MHM
Peter Lindenauer, MD, MSc, FACP, MHM
Tomas Villanueva, DO, MBA, SFHM
Ethan Cumbler, MD, FACP, FHM
Vineet Chopra, MD, MSc, FHM
Core Competencies Table of Contents
The Revised Edition of The Core Competencies would not have been possible without the support and assistance of the Society of Hospital Medicine staff and countless practicing Hospitalists across the United States. The editors thank Nick Marzano for project coordination. Special thanks to Abbie Young for her thorough medical editing and updates to chapter introductions. The editors also thank their families for all their patience and support throughout the development process.
Society of Hospital Medicine leadership and subject matter experts who provided content, review and guidance include:
CHAPTER AUTHORS
Alberto Puig, MD, PhD, FACP, SFHM
Jeffrey Genato, MD, SFHM, UHM
Lorenzo Difrancesco, MD
Alpesh Amin, MD, MBA, MACP, SFHM
Nurcan Ilksoy, MD, FHM
John David Halporn, MD
Eugene Chu, MD, FHM
Brian Donovan, MD, SFHM
Alexander Carbo, MD, SFHM
Valeria Lang, MD, FHM
David Feinbloom, MD, SFHM
Richard Rohr, MD, SFHM
Lakshmi Halasyamani, MD, SFHM
Vijay Rajput, MBBS, FACP, SFHM
Tosha Wetterneck, MD, SFHM
Michael Ruhlen, MD, FAAP, FACHE, MHSc
Gregory Seymann, MD, SFHM
Jeffrey Barsuk, MD, SFHM
David J. Likosky, MD, FACP
Bindu Sangani, MD
Scott Flanders, MD, FACP, MHM
Chad Whelan, MD, FACP, FHM
Shaun Frost, MD, SFHM
Amir Jaffer, MD, MBA, SFHM
Michael Lukela, MD, SFHM, FACP, FAAP
Jonathan Crocker, MD, FHM
CORE COMPETENCIES TASK FORCE (2012-2016)
Satyen Nichani, MD, FHM (Chair)
Nick Fitterman, MD, SFHM, FACP
Michael Lukela, MD, SFHM, FACP, FAAP
Jonathan Crocker, MD, FHM
Tarun Ghosh, MD, FRCS, SFHM
Vikas Parekh, MD, FACP, SFHM
Nick Marzano, MEd
SHM EDUCATION COMMITTEE REVIEWERS
Jessie Kimbrough-Sugick, MD, MPH
Danielle Scheurer, MD, SFHM, MSCR
Amit Pahwa, MD
Anthony Breu, MD
Nathan Houchens, MD, FACP, FHM
Jeffrey Bates, MD, FACP, FHM
Ian Jenkins, MD, SFHM
Neel Shah, MB, BCh, SFHM
Elizabeth Cerceo, MD, FACP, FHM
Jeffrey Greenwald, MD, SFHM
Haruka Torok, MD, SFHM
Bartho Caponi, MD, FHM
Leonard Feldman, MD, FACP, FAAP, SFHM
Daniel Brotman, MD, SFHM
Alfred Burger, MD, SFHM
Jocelyn Carter, MD, MPH
Vinh-Tung Nguyen, MD
Kurt Pfeifer, MD, FACP, SFHM
Alberto Puig, MD, PhD, FACP, SFHM
Richard Vestal, MD
Judy Vu, MD, FAAP
CONTENT EXPERTS
Jason Persoff, MD, SFHM
Nilam Soni, MD, FHM
Lynnea Mills, MD
Wendy Anderson, MD, MS
Jeffrey Frank, MD, FACP, MBA
Howard Epstein, MD, SFHM, CHIE
Kendall Rogers, MD, SFHM
Prateek Gandiga, MD, FACP
Jeffrey Glasheen, MD, SFHM
Melissa Mattison, MD, SFHM
Vineet Arora, MD, MPP, MHM
Peter Lindenauer, MD, MSc, FACP, MHM
Tomas Villanueva, DO, MBA, SFHM
Ethan Cumbler, MD, FACP, FHM
Vineet Chopra, MD, MSc, FHM
Core Competencies Table of Contents
The Revised Edition of The Core Competencies would not have been possible without the support and assistance of the Society of Hospital Medicine staff and countless practicing Hospitalists across the United States. The editors thank Nick Marzano for project coordination. Special thanks to Abbie Young for her thorough medical editing and updates to chapter introductions. The editors also thank their families for all their patience and support throughout the development process.
Society of Hospital Medicine leadership and subject matter experts who provided content, review and guidance include:
CHAPTER AUTHORS
Alberto Puig, MD, PhD, FACP, SFHM
Jeffrey Genato, MD, SFHM, UHM
Lorenzo Difrancesco, MD
Alpesh Amin, MD, MBA, MACP, SFHM
Nurcan Ilksoy, MD, FHM
John David Halporn, MD
Eugene Chu, MD, FHM
Brian Donovan, MD, SFHM
Alexander Carbo, MD, SFHM
Valeria Lang, MD, FHM
David Feinbloom, MD, SFHM
Richard Rohr, MD, SFHM
Lakshmi Halasyamani, MD, SFHM
Vijay Rajput, MBBS, FACP, SFHM
Tosha Wetterneck, MD, SFHM
Michael Ruhlen, MD, FAAP, FACHE, MHSc
Gregory Seymann, MD, SFHM
Jeffrey Barsuk, MD, SFHM
David J. Likosky, MD, FACP
Bindu Sangani, MD
Scott Flanders, MD, FACP, MHM
Chad Whelan, MD, FACP, FHM
Shaun Frost, MD, SFHM
Amir Jaffer, MD, MBA, SFHM
Michael Lukela, MD, SFHM, FACP, FAAP
Jonathan Crocker, MD, FHM
CORE COMPETENCIES TASK FORCE (2012-2016)
Satyen Nichani, MD, FHM (Chair)
Nick Fitterman, MD, SFHM, FACP
Michael Lukela, MD, SFHM, FACP, FAAP
Jonathan Crocker, MD, FHM
Tarun Ghosh, MD, FRCS, SFHM
Vikas Parekh, MD, FACP, SFHM
Nick Marzano, MEd
SHM EDUCATION COMMITTEE REVIEWERS
Jessie Kimbrough-Sugick, MD, MPH
Danielle Scheurer, MD, SFHM, MSCR
Amit Pahwa, MD
Anthony Breu, MD
Nathan Houchens, MD, FACP, FHM
Jeffrey Bates, MD, FACP, FHM
Ian Jenkins, MD, SFHM
Neel Shah, MB, BCh, SFHM
Elizabeth Cerceo, MD, FACP, FHM
Jeffrey Greenwald, MD, SFHM
Haruka Torok, MD, SFHM
Bartho Caponi, MD, FHM
Leonard Feldman, MD, FACP, FAAP, SFHM
Daniel Brotman, MD, SFHM
Alfred Burger, MD, SFHM
Jocelyn Carter, MD, MPH
Vinh-Tung Nguyen, MD
Kurt Pfeifer, MD, FACP, SFHM
Alberto Puig, MD, PhD, FACP, SFHM
Richard Vestal, MD
Judy Vu, MD, FAAP
CONTENT EXPERTS
Jason Persoff, MD, SFHM
Nilam Soni, MD, FHM
Lynnea Mills, MD
Wendy Anderson, MD, MS
Jeffrey Frank, MD, FACP, MBA
Howard Epstein, MD, SFHM, CHIE
Kendall Rogers, MD, SFHM
Prateek Gandiga, MD, FACP
Jeffrey Glasheen, MD, SFHM
Melissa Mattison, MD, SFHM
Vineet Arora, MD, MPP, MHM
Peter Lindenauer, MD, MSc, FACP, MHM
Tomas Villanueva, DO, MBA, SFHM
Ethan Cumbler, MD, FACP, FHM
Vineet Chopra, MD, MSc, FHM
© 2017 Society of Hospital Medicine
Updating the core competencies in hospital medicine—2017 revision: Introduction and methodology
In 2006, the Society of Hospital Medicine (SHM) first published The Core Competencies in Hospital Medicine: A Framework for Curricular Development (henceforth described as the Core Competencies) to help define the role and expectations of hospitalists.1,2 The Core Competencies provided a framework for evaluating clinical skills and professional expertise within a rapidly developing field and highlighted opportunities for growth. Since the initial development and publication of the Core Competencies, changes in the healthcare landscape and hospitalist practice environment have prompted this revision.
Over the past decade, the field of hospital medicine has experienced exponential growth. In 2005, just over 16,000 hospitalists were practicing in the United States. By 2015, that number had increased to an estimated 44,000 hospitalists, accounting for approximately 6% of the physician workforce.3 Hospitalists have expanded the scope of hospital medicine in many ways. In their roles, hospitalists lead and participate in hospital-based care models that emphasize interprofessional collaboration and a focus on the delivery of high-quality and cost-effective care across a variety of clinical domains (eg, the Choosing Wisely initiative).4 They are also engaged in patient safety and quality initiatives that are increasingly being used as benchmarks to rate hospitals and as factors for hospital payment (eg, Hospital Inpatient Value-Based Purchasing Program).5 In fact, the American Board of Internal Medicine (ABIM) created a Focused Practice in Hospital Medicine Maintenance of Certification program in response to the growing number of internists choosing to concentrate their practice in the hospital setting. This decision by the ABIM underscores the value that hospitalists bring to improving patient care in the hospital setting. The ABIM also recognizes the Core Competencies as a curricular framework for a focused practice in hospital medicine.6
Changes within the educational environment have demanded attentive and active participation by many hospitalists. For example, in 2012, the Accreditation Council for Graduate Medical Education (ACGME) introduced the Milestones Project, a new outcomes-based framework designed to more effectively assess learner performance across the 6 core competencies.7 These milestones assessments create intentional opportunities to guide the development of physicians during their training, including in the inpatient environments in which hospitalists practice. Where applicable, existing Core Competencies learning objectives were compared with external sources such as the individual ACGME performance milestones for this revision.
THE CORE COMPETENCIES
The Core Competencies focus on adult hospital medicine. The Pediatric Hospital Medicine Core Competencies are published separately.8 Importantly, the Core Competencies document is not intended to define an absolute set of clinical, procedural, or system-based topics described in textbooks or used by graduate medical education training programs. It does not define or limit the scope of the practice of hospital medicine. Rather, the Core Competencies serve as measurable learning objectives that encourage teaching faculty, practicing hospitalists, and administrators to develop individual skill sets and programs to improve patient care contextualized to the needs of an individual, care setting, or institution. To permit this flexibility, individual chapter-specific objectives are intentionally general in nature. Finally, the Core Competencies document is not a set of practice guidelines, nor does it offer any representation of a “standard of care.” Readers are encouraged to explore the article by McKean et al.9 to review examples of application of the Core Competencies and suggestions for curricular development.
The purpose of this article is to describe the criteria for inclusion of new chapters in the Core Competencies and the methodology of the review and revision process. It outlines the process of initial review and editing of the existing chapters; needs assessment for new topics; new chapter production; and the process of review and revision of individual chapters to create the complete document. The revised Core Competencies document is available online at http://www.journalofhospitalmedicine.com/jhospmed/issue/134981/journal-hospital-medicine-124-suppl-1.
REVIEW AND REVISION PROCESS
In 2012, the Society of Hospital Medicine (SHM) Education Committee created a Core Competencies Task Force (CCTF) in response to the SHM Board of Directors’ charge that it review and update the initial Core Competencies document. The CCTF comprised of 5 physician SHM Education Committee members and one SHM staff representative. CCTF membership included hospitalists with an interest and familiarity with the Core Competencies document. The SHM Education Committee nominated the CCTF chair, who determined the optimal size, qualifications, and composition of the task force with approval from the Committee. The CCTF communicated through frequent conference calls and via e-mail correspondence to conduct an initial review of the existing chapters and to perform a needs assessment for new topics.
Individual Chapter Review
The SHM Education Committee provided critical input and approved the chapter review process designed by the CCTF (Figure). The CCTF reviewed each chapter of the Core Competencies document to assess its continuing relevance to the field of hospital medicine with a standardized tool (Appendix 1). The process required that at least 2 CCTF members reviewed each chapter. Preliminary reviewers assessed the current relevance of each chapter, determined whether individual learning objectives required additional investigation or modification, and developed new learning objectives to fill any educational gaps. All CCTF members then discussed assimilated feedback from the initial CCTF review, using consensus decision making to determine chapter changes and modifications. The CCTF found each of the existing chapters to be relevant to the field and identified none for removal.
The CCTF rewrote all chapters. It then disseminated proposed chapter changes to a panel of diverse independent reviewers to solicit suggestions and comments to ensure a multidisciplinary and balanced review process. Independent reviewers included authors of the original Core Competencies chapters, invited content experts, and members of the SHM Education Committee. When appropriate, corresponding SHM Committees reviewed individual chapters for updates and revisions. For example, the SHM Hospital Quality and Patient Safety Committee reviewed the chapters on patient safety and quality improvement, and the SHM Practice Management Committee reviewed the chapter on management practices. Four CCTF section editors managed an independent portfolio of chapters. Each CCTF section editor assimilated the various draft versions, corresponded with individual reviewers when necessary, and compiled the changes into a subsequent draft. This process ensured that the final version of every chapter reflected the thoughtful input from all parties involved in the review. Throughout the process, the CCTF used consensus decision making to adjudicate chapter changes and modifications. The 2006 Core Competencies Editorial team also reviewed the revision and provided critical input. The SHM Education Committee and the SHM Board of Directors reviewed and approved the final version of the Core Competencies document.
Needs Assessment and Selection of New Core Competency Chapters
The CCTF issued a call for new topics to the members of the SHM Education Committee for inclusion in the Core Competencies. Topics were also identified from the following sources: the top 100 adult medical diagnoses at hospital discharge in the Healthcare Cost and Utilization Project database in 2010; topics in hospital medicine textbooks; curricula presented at the 3 most recent SHM annual meetings; and responses from SHM annual meeting surveys. Table 1 lists the topics considered for addition.
Members of the SHM Education Committee rated each of the potential topics considered for inclusion based on the following characteristics: relevance to the field of hospital medicine; intersection of the topic with medical subspecialties; and its appropriateness as a separate, stand-alone chapter. In addition, topics more frequently encountered by hospitalists, those deemed clinically important with a known risk of complications or management inconsistencies, and those with significant opportunities for quality improvement initiatives carried more weight. Syncope and hyponatremia were the only 2 clinical conditions identified that met all of the inclusion criteria. No additional topics met the criteria for new chapter development in the Procedures or Healthcare Systems sections. The SHM Education Committee identified the use of point-of-care ultrasonography as an important advancement in the field. Where appropriate, the individual procedure chapters now include a new competency-based objective highlighting its role. In addition, a separate SHM task force is working to develop a practice guideline for the use of point-of-care ultrasonography by hospitalists.
Contributors
The SHM Education Committee determined authorship for the new chapters (syncope and hyponatremia). It assigned 2 CCTF members with content expertise and familiarity with the Core Competencies to each author one chapter. Given the limited number of new chapters, it made a decision to develop the content internally rather than through an open-call for authorship nominations to practicing SHM members. The authors made an effort to maintain consistency with the educational theory used to develop the initial Core Competencies. Each of the new topics underwent rigorous review as previously described, including additional independent reviews by hospitalists with content expertise in these areas.
CHAPTER FORMAT AND CONTENT CHANGES
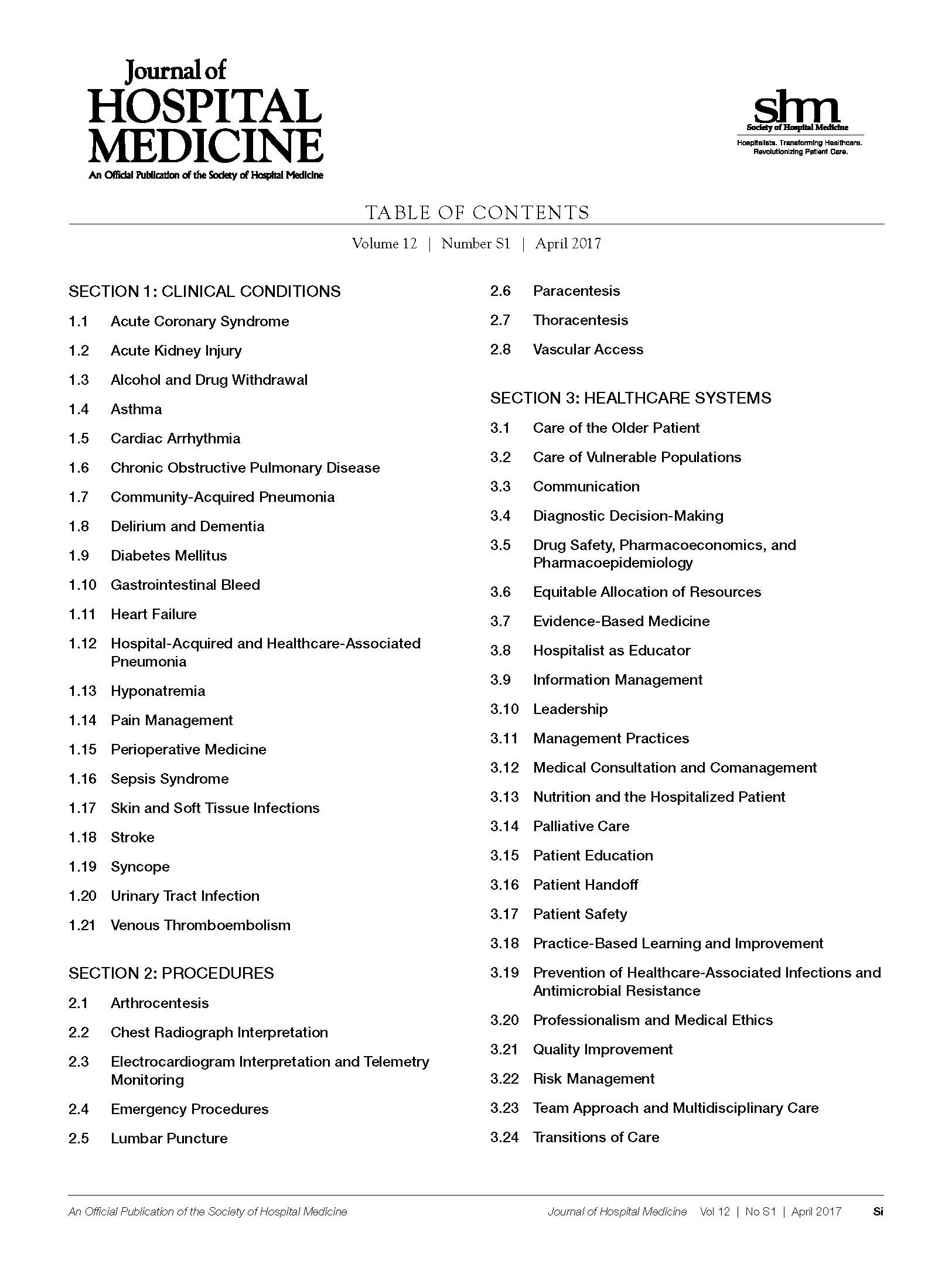
Following the same format as the earlier version, the 2017 Core Competencies revision contains 53 chapters, divided into 3 sections—Clinical Conditions, Procedures, and Healthcare Systems (Table 2) —all integral components of the practice of hospital medicine. The design allows individual chapters to stand alone. However, each chapter should be considered in the context of the entire document because a particular concept may be only briefly discussed in one chapter, but described in greater depth in another given the potential overlap across topics.
The chapters maintain the same content structure as the original version. Each chapter begins with an introductory paragraph followed by a list of competency-based objectives grouped in subsections according to the educational theory of learning domains: cognitive (knowledge), psychomotor (skills), and affective (attitudes).10 In addition, a subsection for System Organization and Improvement is included in the Clinical Conditions and Procedure chapters to emphasize the importance of interprofessional collaboration for optimal patient care. These subsections were not included in the Healthcare Systems chapters, as system organization and improvement is intrinsic to these subjects.
The introductory paragraph provides background information and describes how the chapter remains relevant to the current practice of hospital medicine. Individual competency-based objectives outline a relevant concept and expected level of proficiency as defined by Bloom’s taxonomy.10 New objectives reflect changes in the healthcare landscape over the past decade or further enhance each chapter’s concepts. Chapter authors made an effort to develop chapter and learning objective concepts that are consistent with external resources such as the ACGME Milestones Project and practice guideline objectives developed by a variety of professional organizations.
SUMMARY AND FUTURE DIRECTIONS
The Core Competencies document serves as a resource for hospitalists and hospital medicine programs to evaluate, develop, and improve individual and collective skills and the practice environment. The Core Competencies also provide a framework for medical school clerkship directors and residency and fellowship program directors, as well as course directors of Continuing Medical Education programs, to develop curricula to enhance educational experiences for trainees and hospital medicine providers. The updates in every chapter in this revision to the Core Competencies reflects the changes in the healthcare landscape and hospitalist practice environment over the past decade, and we encourage readers to revisit the entire compendium. Table 3 highlights some of the salient changes in this revision.
Hospital medicine continues to evolve as a specialty. The Core Competencies define hospitalists as agents of change and foster the development of a culture of safe and effective patient care within the hospital environment. Although the CCTF hopes that the Core Competencies will preserve their relevance over time, it recognizes the importance of their periodic reevaluation and adaptation. Additionally, SHM developed the Core Competencies primarily for physicians practicing as hospitalists. As the number of physician assistants and nurse practitioners engaged in the practice of hospital medicine increases, and hospital medicine expands into nontraditional specialties such as surgical comanagement, it may be necessary to consider the development of additional or separate Hospital Medicine Core Competencies tailored to the needs of these subsets of clinicians.
Acknowledgments
The authors and the CCTF are immensely grateful to Nick Marzano for project coordination and Abbie Young for her assistance with medical editing and chapter formatting. We extend our sincerest appreciation and gratitude to the index team of authors and editors whose efforts laid the foundation for this body of work. The initial development and this revision of the Core Competencies would not have been possible without the support and assistance of the SHM staff, the SHM Education Committee, and the scores of contributors and reviewers who participated in its creation (complete list of individuals is available in Appendix 2). We thank everyone for his or her invaluable input and effort.
Disclosures
The Society of Hospital Medicine (SHM) provided administrative support for project coordination. SHM, or any of its representatives, had no role in the development of topic areas, refinement, or vetting of the topic list. No member of the Core Competencies Task Force or the SHM Education Committee received compensation for their participation in revising the Core Competencies. The authors report no conflicts of inte
1. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1 Suppl 1:2-95.
2. Dressler DD, Pistoria MJ, Budnitz TL, McKean SCW, Amin AN. Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(1):48-56.
3. Hospital Medicine News, Society of Hospital Medicine. http://www.hospitalmedicine.org/press. Accessed June 16, 2016.
4. Bulger J, Nickel W, Messler J, et al. Choosing wisely in adult hospital medicine: five opportunities for improved healthcare value. J Hosp Med. 2013;8(9):486-492.
5. Conway PH. Value-driven health care: implications for hospitals and hospitalists. J Hosp Med. 2009;4(8):507-511.
6. American Board of Internal Medicine. Questions and Answers Regarding ABIM’s Maintenance of Certification in Internal Medicine with a Focused Practice in Hospital Medicine Program. 2009. http://www.abim.org/news/focused-practice-hospital-medicine-questions-answers.aspx. Accessed November 11, 2016.
7. The Internal Medicine Milestone Project. http://www.acgme.org/acgmeweb/portals/0/pdfs/milestones/internalmedicinemilestones.pdf. Accessed February 29, 2016.
8. Stucky ER, Ottolini MC, Maniscalco J. Pediatric hospital medicine core competencies: development and methodology. J Hosp Med. 2010;5(6):339-343.
9. McKean SC, Budnitz TL, Dressler DD, Amin AN, Pistoria MJ. How to use the core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1 Suppl 1:57-67.
10. Anderson LW, Krathwohl DR (eds). A Taxonomy for Learning, Teaching and Assessing: A Revision of Bloom’s Taxonomy of Educational Outcomes. Complete edition. New York, NY: Longman; 2001.
In 2006, the Society of Hospital Medicine (SHM) first published The Core Competencies in Hospital Medicine: A Framework for Curricular Development (henceforth described as the Core Competencies) to help define the role and expectations of hospitalists.1,2 The Core Competencies provided a framework for evaluating clinical skills and professional expertise within a rapidly developing field and highlighted opportunities for growth. Since the initial development and publication of the Core Competencies, changes in the healthcare landscape and hospitalist practice environment have prompted this revision.
Over the past decade, the field of hospital medicine has experienced exponential growth. In 2005, just over 16,000 hospitalists were practicing in the United States. By 2015, that number had increased to an estimated 44,000 hospitalists, accounting for approximately 6% of the physician workforce.3 Hospitalists have expanded the scope of hospital medicine in many ways. In their roles, hospitalists lead and participate in hospital-based care models that emphasize interprofessional collaboration and a focus on the delivery of high-quality and cost-effective care across a variety of clinical domains (eg, the Choosing Wisely initiative).4 They are also engaged in patient safety and quality initiatives that are increasingly being used as benchmarks to rate hospitals and as factors for hospital payment (eg, Hospital Inpatient Value-Based Purchasing Program).5 In fact, the American Board of Internal Medicine (ABIM) created a Focused Practice in Hospital Medicine Maintenance of Certification program in response to the growing number of internists choosing to concentrate their practice in the hospital setting. This decision by the ABIM underscores the value that hospitalists bring to improving patient care in the hospital setting. The ABIM also recognizes the Core Competencies as a curricular framework for a focused practice in hospital medicine.6
Changes within the educational environment have demanded attentive and active participation by many hospitalists. For example, in 2012, the Accreditation Council for Graduate Medical Education (ACGME) introduced the Milestones Project, a new outcomes-based framework designed to more effectively assess learner performance across the 6 core competencies.7 These milestones assessments create intentional opportunities to guide the development of physicians during their training, including in the inpatient environments in which hospitalists practice. Where applicable, existing Core Competencies learning objectives were compared with external sources such as the individual ACGME performance milestones for this revision.
THE CORE COMPETENCIES
The Core Competencies focus on adult hospital medicine. The Pediatric Hospital Medicine Core Competencies are published separately.8 Importantly, the Core Competencies document is not intended to define an absolute set of clinical, procedural, or system-based topics described in textbooks or used by graduate medical education training programs. It does not define or limit the scope of the practice of hospital medicine. Rather, the Core Competencies serve as measurable learning objectives that encourage teaching faculty, practicing hospitalists, and administrators to develop individual skill sets and programs to improve patient care contextualized to the needs of an individual, care setting, or institution. To permit this flexibility, individual chapter-specific objectives are intentionally general in nature. Finally, the Core Competencies document is not a set of practice guidelines, nor does it offer any representation of a “standard of care.” Readers are encouraged to explore the article by McKean et al.9 to review examples of application of the Core Competencies and suggestions for curricular development.
The purpose of this article is to describe the criteria for inclusion of new chapters in the Core Competencies and the methodology of the review and revision process. It outlines the process of initial review and editing of the existing chapters; needs assessment for new topics; new chapter production; and the process of review and revision of individual chapters to create the complete document. The revised Core Competencies document is available online at http://www.journalofhospitalmedicine.com/jhospmed/issue/134981/journal-hospital-medicine-124-suppl-1.
REVIEW AND REVISION PROCESS
In 2012, the Society of Hospital Medicine (SHM) Education Committee created a Core Competencies Task Force (CCTF) in response to the SHM Board of Directors’ charge that it review and update the initial Core Competencies document. The CCTF comprised of 5 physician SHM Education Committee members and one SHM staff representative. CCTF membership included hospitalists with an interest and familiarity with the Core Competencies document. The SHM Education Committee nominated the CCTF chair, who determined the optimal size, qualifications, and composition of the task force with approval from the Committee. The CCTF communicated through frequent conference calls and via e-mail correspondence to conduct an initial review of the existing chapters and to perform a needs assessment for new topics.
Individual Chapter Review
The SHM Education Committee provided critical input and approved the chapter review process designed by the CCTF (Figure). The CCTF reviewed each chapter of the Core Competencies document to assess its continuing relevance to the field of hospital medicine with a standardized tool (Appendix 1). The process required that at least 2 CCTF members reviewed each chapter. Preliminary reviewers assessed the current relevance of each chapter, determined whether individual learning objectives required additional investigation or modification, and developed new learning objectives to fill any educational gaps. All CCTF members then discussed assimilated feedback from the initial CCTF review, using consensus decision making to determine chapter changes and modifications. The CCTF found each of the existing chapters to be relevant to the field and identified none for removal.
The CCTF rewrote all chapters. It then disseminated proposed chapter changes to a panel of diverse independent reviewers to solicit suggestions and comments to ensure a multidisciplinary and balanced review process. Independent reviewers included authors of the original Core Competencies chapters, invited content experts, and members of the SHM Education Committee. When appropriate, corresponding SHM Committees reviewed individual chapters for updates and revisions. For example, the SHM Hospital Quality and Patient Safety Committee reviewed the chapters on patient safety and quality improvement, and the SHM Practice Management Committee reviewed the chapter on management practices. Four CCTF section editors managed an independent portfolio of chapters. Each CCTF section editor assimilated the various draft versions, corresponded with individual reviewers when necessary, and compiled the changes into a subsequent draft. This process ensured that the final version of every chapter reflected the thoughtful input from all parties involved in the review. Throughout the process, the CCTF used consensus decision making to adjudicate chapter changes and modifications. The 2006 Core Competencies Editorial team also reviewed the revision and provided critical input. The SHM Education Committee and the SHM Board of Directors reviewed and approved the final version of the Core Competencies document.
Needs Assessment and Selection of New Core Competency Chapters
The CCTF issued a call for new topics to the members of the SHM Education Committee for inclusion in the Core Competencies. Topics were also identified from the following sources: the top 100 adult medical diagnoses at hospital discharge in the Healthcare Cost and Utilization Project database in 2010; topics in hospital medicine textbooks; curricula presented at the 3 most recent SHM annual meetings; and responses from SHM annual meeting surveys. Table 1 lists the topics considered for addition.
Members of the SHM Education Committee rated each of the potential topics considered for inclusion based on the following characteristics: relevance to the field of hospital medicine; intersection of the topic with medical subspecialties; and its appropriateness as a separate, stand-alone chapter. In addition, topics more frequently encountered by hospitalists, those deemed clinically important with a known risk of complications or management inconsistencies, and those with significant opportunities for quality improvement initiatives carried more weight. Syncope and hyponatremia were the only 2 clinical conditions identified that met all of the inclusion criteria. No additional topics met the criteria for new chapter development in the Procedures or Healthcare Systems sections. The SHM Education Committee identified the use of point-of-care ultrasonography as an important advancement in the field. Where appropriate, the individual procedure chapters now include a new competency-based objective highlighting its role. In addition, a separate SHM task force is working to develop a practice guideline for the use of point-of-care ultrasonography by hospitalists.
Contributors
The SHM Education Committee determined authorship for the new chapters (syncope and hyponatremia). It assigned 2 CCTF members with content expertise and familiarity with the Core Competencies to each author one chapter. Given the limited number of new chapters, it made a decision to develop the content internally rather than through an open-call for authorship nominations to practicing SHM members. The authors made an effort to maintain consistency with the educational theory used to develop the initial Core Competencies. Each of the new topics underwent rigorous review as previously described, including additional independent reviews by hospitalists with content expertise in these areas.
CHAPTER FORMAT AND CONTENT CHANGES
Following the same format as the earlier version, the 2017 Core Competencies revision contains 53 chapters, divided into 3 sections—Clinical Conditions, Procedures, and Healthcare Systems (Table 2) —all integral components of the practice of hospital medicine. The design allows individual chapters to stand alone. However, each chapter should be considered in the context of the entire document because a particular concept may be only briefly discussed in one chapter, but described in greater depth in another given the potential overlap across topics.
The chapters maintain the same content structure as the original version. Each chapter begins with an introductory paragraph followed by a list of competency-based objectives grouped in subsections according to the educational theory of learning domains: cognitive (knowledge), psychomotor (skills), and affective (attitudes).10 In addition, a subsection for System Organization and Improvement is included in the Clinical Conditions and Procedure chapters to emphasize the importance of interprofessional collaboration for optimal patient care. These subsections were not included in the Healthcare Systems chapters, as system organization and improvement is intrinsic to these subjects.
The introductory paragraph provides background information and describes how the chapter remains relevant to the current practice of hospital medicine. Individual competency-based objectives outline a relevant concept and expected level of proficiency as defined by Bloom’s taxonomy.10 New objectives reflect changes in the healthcare landscape over the past decade or further enhance each chapter’s concepts. Chapter authors made an effort to develop chapter and learning objective concepts that are consistent with external resources such as the ACGME Milestones Project and practice guideline objectives developed by a variety of professional organizations.
SUMMARY AND FUTURE DIRECTIONS
The Core Competencies document serves as a resource for hospitalists and hospital medicine programs to evaluate, develop, and improve individual and collective skills and the practice environment. The Core Competencies also provide a framework for medical school clerkship directors and residency and fellowship program directors, as well as course directors of Continuing Medical Education programs, to develop curricula to enhance educational experiences for trainees and hospital medicine providers. The updates in every chapter in this revision to the Core Competencies reflects the changes in the healthcare landscape and hospitalist practice environment over the past decade, and we encourage readers to revisit the entire compendium. Table 3 highlights some of the salient changes in this revision.
Hospital medicine continues to evolve as a specialty. The Core Competencies define hospitalists as agents of change and foster the development of a culture of safe and effective patient care within the hospital environment. Although the CCTF hopes that the Core Competencies will preserve their relevance over time, it recognizes the importance of their periodic reevaluation and adaptation. Additionally, SHM developed the Core Competencies primarily for physicians practicing as hospitalists. As the number of physician assistants and nurse practitioners engaged in the practice of hospital medicine increases, and hospital medicine expands into nontraditional specialties such as surgical comanagement, it may be necessary to consider the development of additional or separate Hospital Medicine Core Competencies tailored to the needs of these subsets of clinicians.
Acknowledgments
The authors and the CCTF are immensely grateful to Nick Marzano for project coordination and Abbie Young for her assistance with medical editing and chapter formatting. We extend our sincerest appreciation and gratitude to the index team of authors and editors whose efforts laid the foundation for this body of work. The initial development and this revision of the Core Competencies would not have been possible without the support and assistance of the SHM staff, the SHM Education Committee, and the scores of contributors and reviewers who participated in its creation (complete list of individuals is available in Appendix 2). We thank everyone for his or her invaluable input and effort.
Disclosures
The Society of Hospital Medicine (SHM) provided administrative support for project coordination. SHM, or any of its representatives, had no role in the development of topic areas, refinement, or vetting of the topic list. No member of the Core Competencies Task Force or the SHM Education Committee received compensation for their participation in revising the Core Competencies. The authors report no conflicts of inte
In 2006, the Society of Hospital Medicine (SHM) first published The Core Competencies in Hospital Medicine: A Framework for Curricular Development (henceforth described as the Core Competencies) to help define the role and expectations of hospitalists.1,2 The Core Competencies provided a framework for evaluating clinical skills and professional expertise within a rapidly developing field and highlighted opportunities for growth. Since the initial development and publication of the Core Competencies, changes in the healthcare landscape and hospitalist practice environment have prompted this revision.
Over the past decade, the field of hospital medicine has experienced exponential growth. In 2005, just over 16,000 hospitalists were practicing in the United States. By 2015, that number had increased to an estimated 44,000 hospitalists, accounting for approximately 6% of the physician workforce.3 Hospitalists have expanded the scope of hospital medicine in many ways. In their roles, hospitalists lead and participate in hospital-based care models that emphasize interprofessional collaboration and a focus on the delivery of high-quality and cost-effective care across a variety of clinical domains (eg, the Choosing Wisely initiative).4 They are also engaged in patient safety and quality initiatives that are increasingly being used as benchmarks to rate hospitals and as factors for hospital payment (eg, Hospital Inpatient Value-Based Purchasing Program).5 In fact, the American Board of Internal Medicine (ABIM) created a Focused Practice in Hospital Medicine Maintenance of Certification program in response to the growing number of internists choosing to concentrate their practice in the hospital setting. This decision by the ABIM underscores the value that hospitalists bring to improving patient care in the hospital setting. The ABIM also recognizes the Core Competencies as a curricular framework for a focused practice in hospital medicine.6
Changes within the educational environment have demanded attentive and active participation by many hospitalists. For example, in 2012, the Accreditation Council for Graduate Medical Education (ACGME) introduced the Milestones Project, a new outcomes-based framework designed to more effectively assess learner performance across the 6 core competencies.7 These milestones assessments create intentional opportunities to guide the development of physicians during their training, including in the inpatient environments in which hospitalists practice. Where applicable, existing Core Competencies learning objectives were compared with external sources such as the individual ACGME performance milestones for this revision.
THE CORE COMPETENCIES
The Core Competencies focus on adult hospital medicine. The Pediatric Hospital Medicine Core Competencies are published separately.8 Importantly, the Core Competencies document is not intended to define an absolute set of clinical, procedural, or system-based topics described in textbooks or used by graduate medical education training programs. It does not define or limit the scope of the practice of hospital medicine. Rather, the Core Competencies serve as measurable learning objectives that encourage teaching faculty, practicing hospitalists, and administrators to develop individual skill sets and programs to improve patient care contextualized to the needs of an individual, care setting, or institution. To permit this flexibility, individual chapter-specific objectives are intentionally general in nature. Finally, the Core Competencies document is not a set of practice guidelines, nor does it offer any representation of a “standard of care.” Readers are encouraged to explore the article by McKean et al.9 to review examples of application of the Core Competencies and suggestions for curricular development.
The purpose of this article is to describe the criteria for inclusion of new chapters in the Core Competencies and the methodology of the review and revision process. It outlines the process of initial review and editing of the existing chapters; needs assessment for new topics; new chapter production; and the process of review and revision of individual chapters to create the complete document. The revised Core Competencies document is available online at http://www.journalofhospitalmedicine.com/jhospmed/issue/134981/journal-hospital-medicine-124-suppl-1.
REVIEW AND REVISION PROCESS
In 2012, the Society of Hospital Medicine (SHM) Education Committee created a Core Competencies Task Force (CCTF) in response to the SHM Board of Directors’ charge that it review and update the initial Core Competencies document. The CCTF comprised of 5 physician SHM Education Committee members and one SHM staff representative. CCTF membership included hospitalists with an interest and familiarity with the Core Competencies document. The SHM Education Committee nominated the CCTF chair, who determined the optimal size, qualifications, and composition of the task force with approval from the Committee. The CCTF communicated through frequent conference calls and via e-mail correspondence to conduct an initial review of the existing chapters and to perform a needs assessment for new topics.
Individual Chapter Review
The SHM Education Committee provided critical input and approved the chapter review process designed by the CCTF (Figure). The CCTF reviewed each chapter of the Core Competencies document to assess its continuing relevance to the field of hospital medicine with a standardized tool (Appendix 1). The process required that at least 2 CCTF members reviewed each chapter. Preliminary reviewers assessed the current relevance of each chapter, determined whether individual learning objectives required additional investigation or modification, and developed new learning objectives to fill any educational gaps. All CCTF members then discussed assimilated feedback from the initial CCTF review, using consensus decision making to determine chapter changes and modifications. The CCTF found each of the existing chapters to be relevant to the field and identified none for removal.
The CCTF rewrote all chapters. It then disseminated proposed chapter changes to a panel of diverse independent reviewers to solicit suggestions and comments to ensure a multidisciplinary and balanced review process. Independent reviewers included authors of the original Core Competencies chapters, invited content experts, and members of the SHM Education Committee. When appropriate, corresponding SHM Committees reviewed individual chapters for updates and revisions. For example, the SHM Hospital Quality and Patient Safety Committee reviewed the chapters on patient safety and quality improvement, and the SHM Practice Management Committee reviewed the chapter on management practices. Four CCTF section editors managed an independent portfolio of chapters. Each CCTF section editor assimilated the various draft versions, corresponded with individual reviewers when necessary, and compiled the changes into a subsequent draft. This process ensured that the final version of every chapter reflected the thoughtful input from all parties involved in the review. Throughout the process, the CCTF used consensus decision making to adjudicate chapter changes and modifications. The 2006 Core Competencies Editorial team also reviewed the revision and provided critical input. The SHM Education Committee and the SHM Board of Directors reviewed and approved the final version of the Core Competencies document.
Needs Assessment and Selection of New Core Competency Chapters
The CCTF issued a call for new topics to the members of the SHM Education Committee for inclusion in the Core Competencies. Topics were also identified from the following sources: the top 100 adult medical diagnoses at hospital discharge in the Healthcare Cost and Utilization Project database in 2010; topics in hospital medicine textbooks; curricula presented at the 3 most recent SHM annual meetings; and responses from SHM annual meeting surveys. Table 1 lists the topics considered for addition.
Members of the SHM Education Committee rated each of the potential topics considered for inclusion based on the following characteristics: relevance to the field of hospital medicine; intersection of the topic with medical subspecialties; and its appropriateness as a separate, stand-alone chapter. In addition, topics more frequently encountered by hospitalists, those deemed clinically important with a known risk of complications or management inconsistencies, and those with significant opportunities for quality improvement initiatives carried more weight. Syncope and hyponatremia were the only 2 clinical conditions identified that met all of the inclusion criteria. No additional topics met the criteria for new chapter development in the Procedures or Healthcare Systems sections. The SHM Education Committee identified the use of point-of-care ultrasonography as an important advancement in the field. Where appropriate, the individual procedure chapters now include a new competency-based objective highlighting its role. In addition, a separate SHM task force is working to develop a practice guideline for the use of point-of-care ultrasonography by hospitalists.
Contributors
The SHM Education Committee determined authorship for the new chapters (syncope and hyponatremia). It assigned 2 CCTF members with content expertise and familiarity with the Core Competencies to each author one chapter. Given the limited number of new chapters, it made a decision to develop the content internally rather than through an open-call for authorship nominations to practicing SHM members. The authors made an effort to maintain consistency with the educational theory used to develop the initial Core Competencies. Each of the new topics underwent rigorous review as previously described, including additional independent reviews by hospitalists with content expertise in these areas.
CHAPTER FORMAT AND CONTENT CHANGES
Following the same format as the earlier version, the 2017 Core Competencies revision contains 53 chapters, divided into 3 sections—Clinical Conditions, Procedures, and Healthcare Systems (Table 2) —all integral components of the practice of hospital medicine. The design allows individual chapters to stand alone. However, each chapter should be considered in the context of the entire document because a particular concept may be only briefly discussed in one chapter, but described in greater depth in another given the potential overlap across topics.
The chapters maintain the same content structure as the original version. Each chapter begins with an introductory paragraph followed by a list of competency-based objectives grouped in subsections according to the educational theory of learning domains: cognitive (knowledge), psychomotor (skills), and affective (attitudes).10 In addition, a subsection for System Organization and Improvement is included in the Clinical Conditions and Procedure chapters to emphasize the importance of interprofessional collaboration for optimal patient care. These subsections were not included in the Healthcare Systems chapters, as system organization and improvement is intrinsic to these subjects.
The introductory paragraph provides background information and describes how the chapter remains relevant to the current practice of hospital medicine. Individual competency-based objectives outline a relevant concept and expected level of proficiency as defined by Bloom’s taxonomy.10 New objectives reflect changes in the healthcare landscape over the past decade or further enhance each chapter’s concepts. Chapter authors made an effort to develop chapter and learning objective concepts that are consistent with external resources such as the ACGME Milestones Project and practice guideline objectives developed by a variety of professional organizations.
SUMMARY AND FUTURE DIRECTIONS
The Core Competencies document serves as a resource for hospitalists and hospital medicine programs to evaluate, develop, and improve individual and collective skills and the practice environment. The Core Competencies also provide a framework for medical school clerkship directors and residency and fellowship program directors, as well as course directors of Continuing Medical Education programs, to develop curricula to enhance educational experiences for trainees and hospital medicine providers. The updates in every chapter in this revision to the Core Competencies reflects the changes in the healthcare landscape and hospitalist practice environment over the past decade, and we encourage readers to revisit the entire compendium. Table 3 highlights some of the salient changes in this revision.
Hospital medicine continues to evolve as a specialty. The Core Competencies define hospitalists as agents of change and foster the development of a culture of safe and effective patient care within the hospital environment. Although the CCTF hopes that the Core Competencies will preserve their relevance over time, it recognizes the importance of their periodic reevaluation and adaptation. Additionally, SHM developed the Core Competencies primarily for physicians practicing as hospitalists. As the number of physician assistants and nurse practitioners engaged in the practice of hospital medicine increases, and hospital medicine expands into nontraditional specialties such as surgical comanagement, it may be necessary to consider the development of additional or separate Hospital Medicine Core Competencies tailored to the needs of these subsets of clinicians.
Acknowledgments
The authors and the CCTF are immensely grateful to Nick Marzano for project coordination and Abbie Young for her assistance with medical editing and chapter formatting. We extend our sincerest appreciation and gratitude to the index team of authors and editors whose efforts laid the foundation for this body of work. The initial development and this revision of the Core Competencies would not have been possible without the support and assistance of the SHM staff, the SHM Education Committee, and the scores of contributors and reviewers who participated in its creation (complete list of individuals is available in Appendix 2). We thank everyone for his or her invaluable input and effort.
Disclosures
The Society of Hospital Medicine (SHM) provided administrative support for project coordination. SHM, or any of its representatives, had no role in the development of topic areas, refinement, or vetting of the topic list. No member of the Core Competencies Task Force or the SHM Education Committee received compensation for their participation in revising the Core Competencies. The authors report no conflicts of inte
1. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1 Suppl 1:2-95.
2. Dressler DD, Pistoria MJ, Budnitz TL, McKean SCW, Amin AN. Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(1):48-56.
3. Hospital Medicine News, Society of Hospital Medicine. http://www.hospitalmedicine.org/press. Accessed June 16, 2016.
4. Bulger J, Nickel W, Messler J, et al. Choosing wisely in adult hospital medicine: five opportunities for improved healthcare value. J Hosp Med. 2013;8(9):486-492.
5. Conway PH. Value-driven health care: implications for hospitals and hospitalists. J Hosp Med. 2009;4(8):507-511.
6. American Board of Internal Medicine. Questions and Answers Regarding ABIM’s Maintenance of Certification in Internal Medicine with a Focused Practice in Hospital Medicine Program. 2009. http://www.abim.org/news/focused-practice-hospital-medicine-questions-answers.aspx. Accessed November 11, 2016.
7. The Internal Medicine Milestone Project. http://www.acgme.org/acgmeweb/portals/0/pdfs/milestones/internalmedicinemilestones.pdf. Accessed February 29, 2016.
8. Stucky ER, Ottolini MC, Maniscalco J. Pediatric hospital medicine core competencies: development and methodology. J Hosp Med. 2010;5(6):339-343.
9. McKean SC, Budnitz TL, Dressler DD, Amin AN, Pistoria MJ. How to use the core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1 Suppl 1:57-67.
10. Anderson LW, Krathwohl DR (eds). A Taxonomy for Learning, Teaching and Assessing: A Revision of Bloom’s Taxonomy of Educational Outcomes. Complete edition. New York, NY: Longman; 2001.
1. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1 Suppl 1:2-95.
2. Dressler DD, Pistoria MJ, Budnitz TL, McKean SCW, Amin AN. Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(1):48-56.
3. Hospital Medicine News, Society of Hospital Medicine. http://www.hospitalmedicine.org/press. Accessed June 16, 2016.
4. Bulger J, Nickel W, Messler J, et al. Choosing wisely in adult hospital medicine: five opportunities for improved healthcare value. J Hosp Med. 2013;8(9):486-492.
5. Conway PH. Value-driven health care: implications for hospitals and hospitalists. J Hosp Med. 2009;4(8):507-511.
6. American Board of Internal Medicine. Questions and Answers Regarding ABIM’s Maintenance of Certification in Internal Medicine with a Focused Practice in Hospital Medicine Program. 2009. http://www.abim.org/news/focused-practice-hospital-medicine-questions-answers.aspx. Accessed November 11, 2016.
7. The Internal Medicine Milestone Project. http://www.acgme.org/acgmeweb/portals/0/pdfs/milestones/internalmedicinemilestones.pdf. Accessed February 29, 2016.
8. Stucky ER, Ottolini MC, Maniscalco J. Pediatric hospital medicine core competencies: development and methodology. J Hosp Med. 2010;5(6):339-343.
9. McKean SC, Budnitz TL, Dressler DD, Amin AN, Pistoria MJ. How to use the core competencies in hospital medicine: a framework for curriculum development. J Hosp Med. 2006;1 Suppl 1:57-67.
10. Anderson LW, Krathwohl DR (eds). A Taxonomy for Learning, Teaching and Assessing: A Revision of Bloom’s Taxonomy of Educational Outcomes. Complete edition. New York, NY: Longman; 2001.
© 2017 Society of Hospital Medicine
The 2017 JHM Core Competencies Table of Contents.
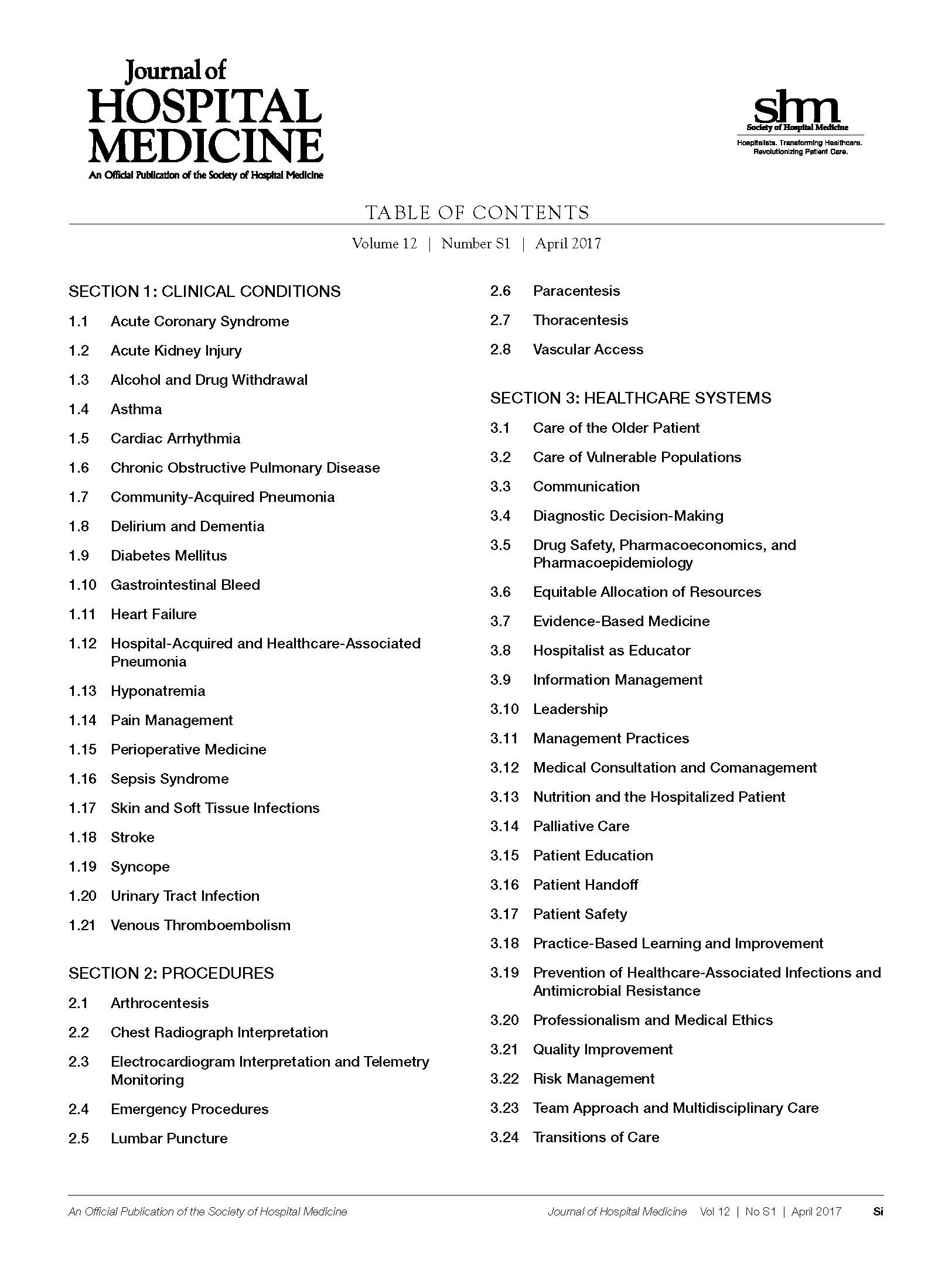
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
Acute Kidney Injury. 2017 Hospital Medicine Revised Core Competencies
Acute kidney injury (AKI), also known as acute renal failure (ARF), is a decline in renal function over a period of hours or days that results in the accumulation of nitrogenous waste products and an impaired ability to maintain fluid/electrolyte/acid-base homeostasis. Epidemiologic studies of AKI are confounded by inconsistent definitions and underreporting. The average incidence is estimated to be 23.8 cases per 1000 hospital discharges.1Approximately 5% to 20% of critically ill patients experience AKI during the course of their illness.2 AKI may present in isolation, develop as a complication of other comorbid illness, or result as a deleterious adverse effect of treatment or diagnostic interventions. Uncomplicated AKI is associated with a mortality rate of up to 10%.3-6 Patients with AKI and multiorgan failure have mortality rates higher than 50%.3-6 AKI is associated with an increased length of hospital stay; a rise in serum creatinine of 0.5 mg/dL or greater while hospitalized confers a 3.5-day increase in length of stay.7 Hospitalists facilitate the expeditious evaluation and management of AKI to improve patient outcomes, optimize resource use, and reduce length of stay. Hospitalists can also advocate and initiate preventive strategies to reduce the incidence of secondary AKI.
KNOWLEDGE
Hospitalists should be able to:
Describe the symptoms and signs of AKI.
Describe and differentiate pathophysiologic causes of AKI including prerenal, intrinsic renal, and postrenal processes.
Differentiate among the causes of prerenal, intrinsic renal, and postrenal types of AKI.
Describe a logical sequence of indicated tests required to evaluate etiologies of AKI based on classification of AKI type.
List common potentially nephrotoxic agents that can cause or worsen AKI.
Explain the indications, contraindications, and mechanisms of action of the interventions used to treat AKI.
Explain the indications, contraindications, benefits, and risks of acute hemodialysis.
Recognize indications for specialty consultation for AKI and the role of nephrology and/or urology specialists.
Describe criteria, including specific measures of clinical stability, that must be met before discharging patients with AKI.
Explain the specific goals that should be met to ensure safe transitions of care for patients with AKI.
SKILLS
Hospitalists should be able to:
Assess patients with suspected AKI in a timely manner and manage or comanage the patient with the primary requesting service.
Elicit a thorough and relevant medical history with emphasis on factors predisposing or contributing to the development of AKI.
Review all drug use including prescription and over-the-counter medications, herbal remedies, nutritional supplements, and illicit drugs to identify common potential nephrotoxins.
Perform a physical examination to assess volume status and to identify underlying comorbid states that may predispose to the development of AKI.
Order and interpret results of indicated diagnostic studies that may include urinalysis and microscopic sediment analysis, urinary diagnostic indices, urinary protein excretion, serologic evaluation, and renal imaging.
Interpret common clinical, laboratory, and imaging findings used to evaluate and follow the severity of AKI.
Diagnose common complications, such as electrolyte abnormalities, that occur with AKI and institute corrective measures.
Calculate estimated creatinine clearance for medication dosage adjustments when indicated.
Identify patients at risk for developing AKI and institute appropriate preventive measures including avoidance of unnecessary radiographic contrast exposure and adherence to evidence-based interventions to reduce the risk of contrast-induced nephropathy.
Coordinate appropriate nutritional and metabolic interventions.
Formulate an AKI treatment plan tailored to the individual patient, which may include fluid management, pharmacologic agents, nutritional recommendations, and patient education.
Identify and treat factors that may complicate the management of AKI, including extreme blood pressure, underlying infections, and the sequelae of electrolyte abnormalities.
Communicate with patients and families to explain the cause and prognosis of AKI.
Communicate with patients and families to explain the rationale for the use of radiographic tests and procedures and the benefit and potential adverse effects of radiographic contrast agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, and pharmacy services, in the care of patients with AKI that begins at admission and continues through all care transitions.
Follow evidence-based recommendations, protocols, and risk-stratification tools for the treatment of AKI.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Advocate for, establish, and support initiatives to reduce the incidence of iatrogenic AKI.
Lead, coordinate, and/or participate in multidisciplinary teams (including nephrology, nursing, pharmacy, and nutrition services) to improve processes that facilitate early identification of AKI and improved patient outcomes.
Lead, coordinate, and/or participate in multidisciplinary initiatives to promote patient safety and optimize management strategies for AKI.
1. Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992-2001. J Am Soc Nephrol. 2006;17(4):1135-1142.
2. Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30(9):2051-2058.
3. Cosentino F, Chaff C, Piedmonte M. Risk factors influencing survival in ICU acute renal failure. Nephrol Dial Transplant. 1994;9(Suppl 4):179-182.
4. Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital-acquired renal insufficiency: a prospective study. Am H Med. 1983;74(2):243-248.
5. Liano F, Junco E, Pascual J, Madero R, Verde E. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl. 1998;66:S16-S24.
6. Shusterman N, Strom BL, Murray TG, Morrison G, West SL, Maislin G. Risk factors and outcome of hospital-acquired acute renal failure. Clinical epidemiologic study. Am J Med. 1987;83(1):65-71.
7. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16(11):3365-3370.
Acute kidney injury (AKI), also known as acute renal failure (ARF), is a decline in renal function over a period of hours or days that results in the accumulation of nitrogenous waste products and an impaired ability to maintain fluid/electrolyte/acid-base homeostasis. Epidemiologic studies of AKI are confounded by inconsistent definitions and underreporting. The average incidence is estimated to be 23.8 cases per 1000 hospital discharges.1Approximately 5% to 20% of critically ill patients experience AKI during the course of their illness.2 AKI may present in isolation, develop as a complication of other comorbid illness, or result as a deleterious adverse effect of treatment or diagnostic interventions. Uncomplicated AKI is associated with a mortality rate of up to 10%.3-6 Patients with AKI and multiorgan failure have mortality rates higher than 50%.3-6 AKI is associated with an increased length of hospital stay; a rise in serum creatinine of 0.5 mg/dL or greater while hospitalized confers a 3.5-day increase in length of stay.7 Hospitalists facilitate the expeditious evaluation and management of AKI to improve patient outcomes, optimize resource use, and reduce length of stay. Hospitalists can also advocate and initiate preventive strategies to reduce the incidence of secondary AKI.
KNOWLEDGE
Hospitalists should be able to:
Describe the symptoms and signs of AKI.
Describe and differentiate pathophysiologic causes of AKI including prerenal, intrinsic renal, and postrenal processes.
Differentiate among the causes of prerenal, intrinsic renal, and postrenal types of AKI.
Describe a logical sequence of indicated tests required to evaluate etiologies of AKI based on classification of AKI type.
List common potentially nephrotoxic agents that can cause or worsen AKI.
Explain the indications, contraindications, and mechanisms of action of the interventions used to treat AKI.
Explain the indications, contraindications, benefits, and risks of acute hemodialysis.
Recognize indications for specialty consultation for AKI and the role of nephrology and/or urology specialists.
Describe criteria, including specific measures of clinical stability, that must be met before discharging patients with AKI.
Explain the specific goals that should be met to ensure safe transitions of care for patients with AKI.
SKILLS
Hospitalists should be able to:
Assess patients with suspected AKI in a timely manner and manage or comanage the patient with the primary requesting service.
Elicit a thorough and relevant medical history with emphasis on factors predisposing or contributing to the development of AKI.
Review all drug use including prescription and over-the-counter medications, herbal remedies, nutritional supplements, and illicit drugs to identify common potential nephrotoxins.
Perform a physical examination to assess volume status and to identify underlying comorbid states that may predispose to the development of AKI.
Order and interpret results of indicated diagnostic studies that may include urinalysis and microscopic sediment analysis, urinary diagnostic indices, urinary protein excretion, serologic evaluation, and renal imaging.
Interpret common clinical, laboratory, and imaging findings used to evaluate and follow the severity of AKI.
Diagnose common complications, such as electrolyte abnormalities, that occur with AKI and institute corrective measures.
Calculate estimated creatinine clearance for medication dosage adjustments when indicated.
Identify patients at risk for developing AKI and institute appropriate preventive measures including avoidance of unnecessary radiographic contrast exposure and adherence to evidence-based interventions to reduce the risk of contrast-induced nephropathy.
Coordinate appropriate nutritional and metabolic interventions.
Formulate an AKI treatment plan tailored to the individual patient, which may include fluid management, pharmacologic agents, nutritional recommendations, and patient education.
Identify and treat factors that may complicate the management of AKI, including extreme blood pressure, underlying infections, and the sequelae of electrolyte abnormalities.
Communicate with patients and families to explain the cause and prognosis of AKI.
Communicate with patients and families to explain the rationale for the use of radiographic tests and procedures and the benefit and potential adverse effects of radiographic contrast agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, and pharmacy services, in the care of patients with AKI that begins at admission and continues through all care transitions.
Follow evidence-based recommendations, protocols, and risk-stratification tools for the treatment of AKI.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Advocate for, establish, and support initiatives to reduce the incidence of iatrogenic AKI.
Lead, coordinate, and/or participate in multidisciplinary teams (including nephrology, nursing, pharmacy, and nutrition services) to improve processes that facilitate early identification of AKI and improved patient outcomes.
Lead, coordinate, and/or participate in multidisciplinary initiatives to promote patient safety and optimize management strategies for AKI.
Acute kidney injury (AKI), also known as acute renal failure (ARF), is a decline in renal function over a period of hours or days that results in the accumulation of nitrogenous waste products and an impaired ability to maintain fluid/electrolyte/acid-base homeostasis. Epidemiologic studies of AKI are confounded by inconsistent definitions and underreporting. The average incidence is estimated to be 23.8 cases per 1000 hospital discharges.1Approximately 5% to 20% of critically ill patients experience AKI during the course of their illness.2 AKI may present in isolation, develop as a complication of other comorbid illness, or result as a deleterious adverse effect of treatment or diagnostic interventions. Uncomplicated AKI is associated with a mortality rate of up to 10%.3-6 Patients with AKI and multiorgan failure have mortality rates higher than 50%.3-6 AKI is associated with an increased length of hospital stay; a rise in serum creatinine of 0.5 mg/dL or greater while hospitalized confers a 3.5-day increase in length of stay.7 Hospitalists facilitate the expeditious evaluation and management of AKI to improve patient outcomes, optimize resource use, and reduce length of stay. Hospitalists can also advocate and initiate preventive strategies to reduce the incidence of secondary AKI.
KNOWLEDGE
Hospitalists should be able to:
Describe the symptoms and signs of AKI.
Describe and differentiate pathophysiologic causes of AKI including prerenal, intrinsic renal, and postrenal processes.
Differentiate among the causes of prerenal, intrinsic renal, and postrenal types of AKI.
Describe a logical sequence of indicated tests required to evaluate etiologies of AKI based on classification of AKI type.
List common potentially nephrotoxic agents that can cause or worsen AKI.
Explain the indications, contraindications, and mechanisms of action of the interventions used to treat AKI.
Explain the indications, contraindications, benefits, and risks of acute hemodialysis.
Recognize indications for specialty consultation for AKI and the role of nephrology and/or urology specialists.
Describe criteria, including specific measures of clinical stability, that must be met before discharging patients with AKI.
Explain the specific goals that should be met to ensure safe transitions of care for patients with AKI.
SKILLS
Hospitalists should be able to:
Assess patients with suspected AKI in a timely manner and manage or comanage the patient with the primary requesting service.
Elicit a thorough and relevant medical history with emphasis on factors predisposing or contributing to the development of AKI.
Review all drug use including prescription and over-the-counter medications, herbal remedies, nutritional supplements, and illicit drugs to identify common potential nephrotoxins.
Perform a physical examination to assess volume status and to identify underlying comorbid states that may predispose to the development of AKI.
Order and interpret results of indicated diagnostic studies that may include urinalysis and microscopic sediment analysis, urinary diagnostic indices, urinary protein excretion, serologic evaluation, and renal imaging.
Interpret common clinical, laboratory, and imaging findings used to evaluate and follow the severity of AKI.
Diagnose common complications, such as electrolyte abnormalities, that occur with AKI and institute corrective measures.
Calculate estimated creatinine clearance for medication dosage adjustments when indicated.
Identify patients at risk for developing AKI and institute appropriate preventive measures including avoidance of unnecessary radiographic contrast exposure and adherence to evidence-based interventions to reduce the risk of contrast-induced nephropathy.
Coordinate appropriate nutritional and metabolic interventions.
Formulate an AKI treatment plan tailored to the individual patient, which may include fluid management, pharmacologic agents, nutritional recommendations, and patient education.
Identify and treat factors that may complicate the management of AKI, including extreme blood pressure, underlying infections, and the sequelae of electrolyte abnormalities.
Communicate with patients and families to explain the cause and prognosis of AKI.
Communicate with patients and families to explain the rationale for the use of radiographic tests and procedures and the benefit and potential adverse effects of radiographic contrast agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, and pharmacy services, in the care of patients with AKI that begins at admission and continues through all care transitions.
Follow evidence-based recommendations, protocols, and risk-stratification tools for the treatment of AKI.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Advocate for, establish, and support initiatives to reduce the incidence of iatrogenic AKI.
Lead, coordinate, and/or participate in multidisciplinary teams (including nephrology, nursing, pharmacy, and nutrition services) to improve processes that facilitate early identification of AKI and improved patient outcomes.
Lead, coordinate, and/or participate in multidisciplinary initiatives to promote patient safety and optimize management strategies for AKI.
1. Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992-2001. J Am Soc Nephrol. 2006;17(4):1135-1142.
2. Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30(9):2051-2058.
3. Cosentino F, Chaff C, Piedmonte M. Risk factors influencing survival in ICU acute renal failure. Nephrol Dial Transplant. 1994;9(Suppl 4):179-182.
4. Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital-acquired renal insufficiency: a prospective study. Am H Med. 1983;74(2):243-248.
5. Liano F, Junco E, Pascual J, Madero R, Verde E. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl. 1998;66:S16-S24.
6. Shusterman N, Strom BL, Murray TG, Morrison G, West SL, Maislin G. Risk factors and outcome of hospital-acquired acute renal failure. Clinical epidemiologic study. Am J Med. 1987;83(1):65-71.
7. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16(11):3365-3370.
1. Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992-2001. J Am Soc Nephrol. 2006;17(4):1135-1142.
2. Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30(9):2051-2058.
3. Cosentino F, Chaff C, Piedmonte M. Risk factors influencing survival in ICU acute renal failure. Nephrol Dial Transplant. 1994;9(Suppl 4):179-182.
4. Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital-acquired renal insufficiency: a prospective study. Am H Med. 1983;74(2):243-248.
5. Liano F, Junco E, Pascual J, Madero R, Verde E. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl. 1998;66:S16-S24.
6. Shusterman N, Strom BL, Murray TG, Morrison G, West SL, Maislin G. Risk factors and outcome of hospital-acquired acute renal failure. Clinical epidemiologic study. Am J Med. 1987;83(1):65-71.
7. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16(11):3365-3370.
© 2017 Society of Hospital Medicine
Alcohol and Drug Withdrawal. 2017 Hospital Medicine Revised Core Competencies
Alcohol and drug withdrawal is a set of signs and symptoms that develops in association with sudden cessation or reduction in the use of alcohol or a number of prescription (particularly opioids and benzodiazepines), over-the-counter (OTC), or illicit drugs. Withdrawal syndromes encompass a broad range of symptoms from mild anxiety and tremulousness to more serious manifestations such as delirium tremens, which occurs in up to 5% of alcohol-dependent persons who undergo withdrawal.1 Withdrawal may occur before hospitalization or during the course of hospitalization. Alcohol- and substance-related disorders account for more than 400,000 hospital discharges each year and are associated with a mean length of stay of approximately 4.6 days.2 Alcohol and drug dependence is often an end product of a combination of biopsychosocial influences, and in most cases, a multidisciplinary approach is necessary to successfully treat affected individuals. Hospitalists can lead their institutions in evidence-based treatment protocols that improve care, reduce costs and length of stay, and facilitate better overall outcomes in patients with substance-related withdrawal syndromes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Describe the effects of drug and alcohol withdrawal on medical illness and the effects of medical illness on substance withdrawal.
Recognize the symptoms and signs of alcohol and drug withdrawal, including withdrawal from prescription and OTC drugs.
Recognize the medical complications from substance use and dependence.
Determine when consultation with a medical toxicologist or expert is necessary.
Distinguish alcohol or drug withdrawal from other causes of delirium.
Differentiate delirium tremens from other alcohol withdrawal syndromes.
Differentiate the clinical manifestations of alcohol or drug intoxication from those of withdrawal.
Recognize different characteristic withdrawal syndromes, such as abstinence syndrome of opioid withdrawal and delirium tremens of alcohol withdrawal.
Describe the tests indicated to evaluate alcohol or drug withdrawal.
Identify patients at increased risk for drug and alcohol withdrawal according to current diagnostic criteria.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat acute alcohol and drug withdrawal.
Identify local trends in illicit drug use.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with drug or alcohol withdrawal.
Explain patient characteristics that portend a poor prognosis.
Explain patient characteristics that indicate a requirement for a higher level of care and/or monitoring.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, with emphasis on substance use.
Assess patients with suspected alcohol or drug withdrawal in a timely manner, identify the level of care required, and manage or comanage the patient with the primary requesting service.
Perform a rapid, efficient, and targeted physical examination to assess for alcohol or drug withdrawal and determine whether life-threatening comorbidities are present.
Assess for common comorbidities in patients with a history of alcohol and drug use.
Formulate a treatment plan tailored to the individual patient, which may include appropriate pharmacologic agents and dosing, route of administration, and nutritional supplementation.
Integrate existing literature and federal regulations into the management of patients with opioid withdrawal syndromes. For patients who are undergoing existing treatment for opioid dependency, communicate with outpatient treatment centers and integrate dosing regimens into care management.
Manage withdrawal syndromes in patients with concomitant medical or surgical issues.
Diagnose oversedation and other complications associated with withdrawal therapies.
Recommend the use of restraints and direct observation to ensure patient safety when appropriate.
Reassure, reorient, and frequently monitor patients in a calm environment.
Use the acute hospitalization as an opportunity to counsel patients about abstinence, recovery, and the medical risks of drug and alcohol use.
Initiate preventive measures before discharge, including alcohol and drug cessation measures.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transition of care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include psychiatry, pharmacy, nursing, and social services, in the treatment of patients with substance use or dependency.
Follow evidence-based national recommendations to guide diagnosis, monitoring, and treatment of withdrawal symptoms.
Act in a nonjudgmental manner when managing the hospitalized patient with substance use.
Establish and maintain an open dialogue with patients and families regarding care goals and limitations.
Appreciate and document the value of appropriate treatment in reducing mortality, duration of delirium, time required to control agitation, adequate control of delirium, treatment of complications, and cost.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include psychiatry and toxicology, to improve patient safety and management strategies for patients with substance abuse.
Lead, coordinate, and/or participate in the development and promotion of guidelines and/or pathways that facilitate efficient and timely evaluation and treatment of patients with alcohol and drug withdrawal.
Promote the development and use of evidence-based guidelines and protocols for the treatment of withdrawal syndromes.
Advocate for hospital resources to improve the care of patients with substance withdrawal and the environment in which the care is delivered.
Establish relationships with and develop knowledge of community-based organizations that provide support to patients with substance use disorders.
Promote awareness of substance use disorders and screening for them.
Coordinate initiatives to address the increased risk of readmissions associated with substance and polysubstance abuse.
1. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed May 2015.
Alcohol and drug withdrawal is a set of signs and symptoms that develops in association with sudden cessation or reduction in the use of alcohol or a number of prescription (particularly opioids and benzodiazepines), over-the-counter (OTC), or illicit drugs. Withdrawal syndromes encompass a broad range of symptoms from mild anxiety and tremulousness to more serious manifestations such as delirium tremens, which occurs in up to 5% of alcohol-dependent persons who undergo withdrawal.1 Withdrawal may occur before hospitalization or during the course of hospitalization. Alcohol- and substance-related disorders account for more than 400,000 hospital discharges each year and are associated with a mean length of stay of approximately 4.6 days.2 Alcohol and drug dependence is often an end product of a combination of biopsychosocial influences, and in most cases, a multidisciplinary approach is necessary to successfully treat affected individuals. Hospitalists can lead their institutions in evidence-based treatment protocols that improve care, reduce costs and length of stay, and facilitate better overall outcomes in patients with substance-related withdrawal syndromes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Describe the effects of drug and alcohol withdrawal on medical illness and the effects of medical illness on substance withdrawal.
Recognize the symptoms and signs of alcohol and drug withdrawal, including withdrawal from prescription and OTC drugs.
Recognize the medical complications from substance use and dependence.
Determine when consultation with a medical toxicologist or expert is necessary.
Distinguish alcohol or drug withdrawal from other causes of delirium.
Differentiate delirium tremens from other alcohol withdrawal syndromes.
Differentiate the clinical manifestations of alcohol or drug intoxication from those of withdrawal.
Recognize different characteristic withdrawal syndromes, such as abstinence syndrome of opioid withdrawal and delirium tremens of alcohol withdrawal.
Describe the tests indicated to evaluate alcohol or drug withdrawal.
Identify patients at increased risk for drug and alcohol withdrawal according to current diagnostic criteria.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat acute alcohol and drug withdrawal.
Identify local trends in illicit drug use.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with drug or alcohol withdrawal.
Explain patient characteristics that portend a poor prognosis.
Explain patient characteristics that indicate a requirement for a higher level of care and/or monitoring.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, with emphasis on substance use.
Assess patients with suspected alcohol or drug withdrawal in a timely manner, identify the level of care required, and manage or comanage the patient with the primary requesting service.
Perform a rapid, efficient, and targeted physical examination to assess for alcohol or drug withdrawal and determine whether life-threatening comorbidities are present.
Assess for common comorbidities in patients with a history of alcohol and drug use.
Formulate a treatment plan tailored to the individual patient, which may include appropriate pharmacologic agents and dosing, route of administration, and nutritional supplementation.
Integrate existing literature and federal regulations into the management of patients with opioid withdrawal syndromes. For patients who are undergoing existing treatment for opioid dependency, communicate with outpatient treatment centers and integrate dosing regimens into care management.
Manage withdrawal syndromes in patients with concomitant medical or surgical issues.
Diagnose oversedation and other complications associated with withdrawal therapies.
Recommend the use of restraints and direct observation to ensure patient safety when appropriate.
Reassure, reorient, and frequently monitor patients in a calm environment.
Use the acute hospitalization as an opportunity to counsel patients about abstinence, recovery, and the medical risks of drug and alcohol use.
Initiate preventive measures before discharge, including alcohol and drug cessation measures.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transition of care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include psychiatry, pharmacy, nursing, and social services, in the treatment of patients with substance use or dependency.
Follow evidence-based national recommendations to guide diagnosis, monitoring, and treatment of withdrawal symptoms.
Act in a nonjudgmental manner when managing the hospitalized patient with substance use.
Establish and maintain an open dialogue with patients and families regarding care goals and limitations.
Appreciate and document the value of appropriate treatment in reducing mortality, duration of delirium, time required to control agitation, adequate control of delirium, treatment of complications, and cost.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include psychiatry and toxicology, to improve patient safety and management strategies for patients with substance abuse.
Lead, coordinate, and/or participate in the development and promotion of guidelines and/or pathways that facilitate efficient and timely evaluation and treatment of patients with alcohol and drug withdrawal.
Promote the development and use of evidence-based guidelines and protocols for the treatment of withdrawal syndromes.
Advocate for hospital resources to improve the care of patients with substance withdrawal and the environment in which the care is delivered.
Establish relationships with and develop knowledge of community-based organizations that provide support to patients with substance use disorders.
Promote awareness of substance use disorders and screening for them.
Coordinate initiatives to address the increased risk of readmissions associated with substance and polysubstance abuse.
Alcohol and drug withdrawal is a set of signs and symptoms that develops in association with sudden cessation or reduction in the use of alcohol or a number of prescription (particularly opioids and benzodiazepines), over-the-counter (OTC), or illicit drugs. Withdrawal syndromes encompass a broad range of symptoms from mild anxiety and tremulousness to more serious manifestations such as delirium tremens, which occurs in up to 5% of alcohol-dependent persons who undergo withdrawal.1 Withdrawal may occur before hospitalization or during the course of hospitalization. Alcohol- and substance-related disorders account for more than 400,000 hospital discharges each year and are associated with a mean length of stay of approximately 4.6 days.2 Alcohol and drug dependence is often an end product of a combination of biopsychosocial influences, and in most cases, a multidisciplinary approach is necessary to successfully treat affected individuals. Hospitalists can lead their institutions in evidence-based treatment protocols that improve care, reduce costs and length of stay, and facilitate better overall outcomes in patients with substance-related withdrawal syndromes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Describe the effects of drug and alcohol withdrawal on medical illness and the effects of medical illness on substance withdrawal.
Recognize the symptoms and signs of alcohol and drug withdrawal, including withdrawal from prescription and OTC drugs.
Recognize the medical complications from substance use and dependence.
Determine when consultation with a medical toxicologist or expert is necessary.
Distinguish alcohol or drug withdrawal from other causes of delirium.
Differentiate delirium tremens from other alcohol withdrawal syndromes.
Differentiate the clinical manifestations of alcohol or drug intoxication from those of withdrawal.
Recognize different characteristic withdrawal syndromes, such as abstinence syndrome of opioid withdrawal and delirium tremens of alcohol withdrawal.
Describe the tests indicated to evaluate alcohol or drug withdrawal.
Identify patients at increased risk for drug and alcohol withdrawal according to current diagnostic criteria.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat acute alcohol and drug withdrawal.
Identify local trends in illicit drug use.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with drug or alcohol withdrawal.
Explain patient characteristics that portend a poor prognosis.
Explain patient characteristics that indicate a requirement for a higher level of care and/or monitoring.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, with emphasis on substance use.
Assess patients with suspected alcohol or drug withdrawal in a timely manner, identify the level of care required, and manage or comanage the patient with the primary requesting service.
Perform a rapid, efficient, and targeted physical examination to assess for alcohol or drug withdrawal and determine whether life-threatening comorbidities are present.
Assess for common comorbidities in patients with a history of alcohol and drug use.
Formulate a treatment plan tailored to the individual patient, which may include appropriate pharmacologic agents and dosing, route of administration, and nutritional supplementation.
Integrate existing literature and federal regulations into the management of patients with opioid withdrawal syndromes. For patients who are undergoing existing treatment for opioid dependency, communicate with outpatient treatment centers and integrate dosing regimens into care management.
Manage withdrawal syndromes in patients with concomitant medical or surgical issues.
Diagnose oversedation and other complications associated with withdrawal therapies.
Recommend the use of restraints and direct observation to ensure patient safety when appropriate.
Reassure, reorient, and frequently monitor patients in a calm environment.
Use the acute hospitalization as an opportunity to counsel patients about abstinence, recovery, and the medical risks of drug and alcohol use.
Initiate preventive measures before discharge, including alcohol and drug cessation measures.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transition of care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include psychiatry, pharmacy, nursing, and social services, in the treatment of patients with substance use or dependency.
Follow evidence-based national recommendations to guide diagnosis, monitoring, and treatment of withdrawal symptoms.
Act in a nonjudgmental manner when managing the hospitalized patient with substance use.
Establish and maintain an open dialogue with patients and families regarding care goals and limitations.
Appreciate and document the value of appropriate treatment in reducing mortality, duration of delirium, time required to control agitation, adequate control of delirium, treatment of complications, and cost.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include psychiatry and toxicology, to improve patient safety and management strategies for patients with substance abuse.
Lead, coordinate, and/or participate in the development and promotion of guidelines and/or pathways that facilitate efficient and timely evaluation and treatment of patients with alcohol and drug withdrawal.
Promote the development and use of evidence-based guidelines and protocols for the treatment of withdrawal syndromes.
Advocate for hospital resources to improve the care of patients with substance withdrawal and the environment in which the care is delivered.
Establish relationships with and develop knowledge of community-based organizations that provide support to patients with substance use disorders.
Promote awareness of substance use disorders and screening for them.
Coordinate initiatives to address the increased risk of readmissions associated with substance and polysubstance abuse.
1. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed May 2015.
1. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed May 2015.
© 2017 Society of Hospital Medicine
Asthma. 2017 Hospital Medicine Revised Core Competencies
Asthma is a chronic disease characterized by airway inflammation and reversible airflow limitation. It is one of the most common chronic conditions and it leads to marked morbidity and mortality in hospitalized patients. In the United States, 1 in 12 persons has asthma and nearly 50% of affected individuals experience an asthma exacerbation each year, accounting for 1.8 million emergency department visits.1,2 Annually, more than 400,000 hospital discharges occur with asthma as the primary diagnosis, with an average length of stay of 3.2 days.2Hospitalists are central to the provision of care for patients with asthma through the use of evidence-based approaches to manage acute exacerbations and to prevent their recurrence. Hospitalists should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to improve efficiency and quality of care and to reduce readmission rates and morbidity and mortality from asthma.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define asthma and describe the pathophysiologic processes that lead to reversible airway obstruction and inflammation.
Identify precipitants of asthma exacerbation, including environmental and occupational exposures.
Recognize the clinical presentation of asthma exacerbation and differentiate it from other acute respiratory and nonrespiratory syndromes.
Describe the role of diagnostic testing, including peak flow monitoring, used for evaluation of asthma exacerbation.
Recognize indications for specialty consultation, including pulmonary and allergy medicine.
Describe evidence-based therapies for the treatment of asthma exacerbations, which may include bronchodilators, systemic corticosteroids, and oxygen.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat asthma.
Recognize signs and symptoms of impending respiratory failure.
Explain the indications for invasive and noninvasive ventilatory support.
List the risk factors for disease severity and death from asthma.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify triggers of asthma and symptoms consistent with asthma exacerbation.
Perform a targeted physical examination to elicit signs consistent with asthma exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Select appropriate diagnostic studies to evaluate severity of asthma exacerbation and interpret the results.
Recognize indications for transfer to the intensive care unit, including impending respiratory failure, and coordinate intubation or noninvasive mechanical ventilation when indicated.
Prescribe appropriate evidence-based pharmacologic therapies during asthma exacerbation, recommending the most appropriate route, dose, frequency, and duration of treatment.
Communicate with patients and families to explain the natural history and prognosis of asthma.
Facilitate discharge planning early during hospitalization.
Develop an asthma action plan in preparation for discharge.
Educate patients and families regarding the indications and appropriate use of daily use inhalers and rescue inhalers for asthmatic control.
Ensure that patients receive training of proper inhaler and peak flow techniques before hospital discharge.
Communicate with patients and families to explain symptoms and signs that should prompt emergent medical attention.
Communicate with patients and families to explain the goals of care, including clinical stability criteria, the importance of preventive measures (such as smoking cessation, avoidance of second-hand smoke, appropriate vaccinations, and modification of environmental exposures), and required follow-up care.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with asthma exacerbation.
Follow evidence-based recommendations for the treatment of patients with asthma exacerbations.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Contribute to and/or develop educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for asthma exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead, coordinate, and/or participate in efforts to educate staff on the importance of smoking cessation counseling and other preventive measures.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists and respiratory therapists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with asthma.
1. Centers for Disease Control and Prevention. CDC Vital Signs: Asthma in the US. Available at: http://www.cdc.gov/vitalsigns/asthma/. Accessed June 2015.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
Asthma is a chronic disease characterized by airway inflammation and reversible airflow limitation. It is one of the most common chronic conditions and it leads to marked morbidity and mortality in hospitalized patients. In the United States, 1 in 12 persons has asthma and nearly 50% of affected individuals experience an asthma exacerbation each year, accounting for 1.8 million emergency department visits.1,2 Annually, more than 400,000 hospital discharges occur with asthma as the primary diagnosis, with an average length of stay of 3.2 days.2Hospitalists are central to the provision of care for patients with asthma through the use of evidence-based approaches to manage acute exacerbations and to prevent their recurrence. Hospitalists should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to improve efficiency and quality of care and to reduce readmission rates and morbidity and mortality from asthma.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define asthma and describe the pathophysiologic processes that lead to reversible airway obstruction and inflammation.
Identify precipitants of asthma exacerbation, including environmental and occupational exposures.
Recognize the clinical presentation of asthma exacerbation and differentiate it from other acute respiratory and nonrespiratory syndromes.
Describe the role of diagnostic testing, including peak flow monitoring, used for evaluation of asthma exacerbation.
Recognize indications for specialty consultation, including pulmonary and allergy medicine.
Describe evidence-based therapies for the treatment of asthma exacerbations, which may include bronchodilators, systemic corticosteroids, and oxygen.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat asthma.
Recognize signs and symptoms of impending respiratory failure.
Explain the indications for invasive and noninvasive ventilatory support.
List the risk factors for disease severity and death from asthma.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify triggers of asthma and symptoms consistent with asthma exacerbation.
Perform a targeted physical examination to elicit signs consistent with asthma exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Select appropriate diagnostic studies to evaluate severity of asthma exacerbation and interpret the results.
Recognize indications for transfer to the intensive care unit, including impending respiratory failure, and coordinate intubation or noninvasive mechanical ventilation when indicated.
Prescribe appropriate evidence-based pharmacologic therapies during asthma exacerbation, recommending the most appropriate route, dose, frequency, and duration of treatment.
Communicate with patients and families to explain the natural history and prognosis of asthma.
Facilitate discharge planning early during hospitalization.
Develop an asthma action plan in preparation for discharge.
Educate patients and families regarding the indications and appropriate use of daily use inhalers and rescue inhalers for asthmatic control.
Ensure that patients receive training of proper inhaler and peak flow techniques before hospital discharge.
Communicate with patients and families to explain symptoms and signs that should prompt emergent medical attention.
Communicate with patients and families to explain the goals of care, including clinical stability criteria, the importance of preventive measures (such as smoking cessation, avoidance of second-hand smoke, appropriate vaccinations, and modification of environmental exposures), and required follow-up care.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with asthma exacerbation.
Follow evidence-based recommendations for the treatment of patients with asthma exacerbations.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Contribute to and/or develop educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for asthma exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead, coordinate, and/or participate in efforts to educate staff on the importance of smoking cessation counseling and other preventive measures.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists and respiratory therapists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with asthma.
Asthma is a chronic disease characterized by airway inflammation and reversible airflow limitation. It is one of the most common chronic conditions and it leads to marked morbidity and mortality in hospitalized patients. In the United States, 1 in 12 persons has asthma and nearly 50% of affected individuals experience an asthma exacerbation each year, accounting for 1.8 million emergency department visits.1,2 Annually, more than 400,000 hospital discharges occur with asthma as the primary diagnosis, with an average length of stay of 3.2 days.2Hospitalists are central to the provision of care for patients with asthma through the use of evidence-based approaches to manage acute exacerbations and to prevent their recurrence. Hospitalists should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to improve efficiency and quality of care and to reduce readmission rates and morbidity and mortality from asthma.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define asthma and describe the pathophysiologic processes that lead to reversible airway obstruction and inflammation.
Identify precipitants of asthma exacerbation, including environmental and occupational exposures.
Recognize the clinical presentation of asthma exacerbation and differentiate it from other acute respiratory and nonrespiratory syndromes.
Describe the role of diagnostic testing, including peak flow monitoring, used for evaluation of asthma exacerbation.
Recognize indications for specialty consultation, including pulmonary and allergy medicine.
Describe evidence-based therapies for the treatment of asthma exacerbations, which may include bronchodilators, systemic corticosteroids, and oxygen.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat asthma.
Recognize signs and symptoms of impending respiratory failure.
Explain the indications for invasive and noninvasive ventilatory support.
List the risk factors for disease severity and death from asthma.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify triggers of asthma and symptoms consistent with asthma exacerbation.
Perform a targeted physical examination to elicit signs consistent with asthma exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Select appropriate diagnostic studies to evaluate severity of asthma exacerbation and interpret the results.
Recognize indications for transfer to the intensive care unit, including impending respiratory failure, and coordinate intubation or noninvasive mechanical ventilation when indicated.
Prescribe appropriate evidence-based pharmacologic therapies during asthma exacerbation, recommending the most appropriate route, dose, frequency, and duration of treatment.
Communicate with patients and families to explain the natural history and prognosis of asthma.
Facilitate discharge planning early during hospitalization.
Develop an asthma action plan in preparation for discharge.
Educate patients and families regarding the indications and appropriate use of daily use inhalers and rescue inhalers for asthmatic control.
Ensure that patients receive training of proper inhaler and peak flow techniques before hospital discharge.
Communicate with patients and families to explain symptoms and signs that should prompt emergent medical attention.
Communicate with patients and families to explain the goals of care, including clinical stability criteria, the importance of preventive measures (such as smoking cessation, avoidance of second-hand smoke, appropriate vaccinations, and modification of environmental exposures), and required follow-up care.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with asthma exacerbation.
Follow evidence-based recommendations for the treatment of patients with asthma exacerbations.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Contribute to and/or develop educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for asthma exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead, coordinate, and/or participate in efforts to educate staff on the importance of smoking cessation counseling and other preventive measures.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists and respiratory therapists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with asthma.
1. Centers for Disease Control and Prevention. CDC Vital Signs: Asthma in the US. Available at: http://www.cdc.gov/vitalsigns/asthma/. Accessed June 2015.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
1. Centers for Disease Control and Prevention. CDC Vital Signs: Asthma in the US. Available at: http://www.cdc.gov/vitalsigns/asthma/. Accessed June 2015.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
© 2017 Society of Hospital Medicine
Cardiac Arrhythmia. 2017 Hospital Medicine Revised Core Competencies
Cardiac arrhythmias are a group of conditions characterized by an abnormal heart rate or rhythm. These are common and affect approximately 5% of the population in the United States. More than 250,000 Americans die each year of sudden cardiac arrest, and most cases are thought to be due to ventricular fibrillation or ventricular tachycardia.1 Several cardiac arrhythmias can cause instability, prompting hospitalization, or they may result from complications during hospitalization. Annually, more than 740,000 hospital discharges are associated with a primary diagnosis of cardiac arrhythmia.2 Hospitalists identify and treat all types of arrhythmias, coordinate specialty and primary care resources, and transition patients safely and cost-effectively through the acute hospitalization and into the outpatient setting.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Identify and differentiate the common clinical presentations of both benign and pathologic arrhythmias.
Explain the causes of atrial and ventricular arrhythmias.
Describe the indicated tests required to evaluate arrhythmias.
Explain how medications, metabolic abnormalities, and medical comorbidities may precipitate various arrhythmias.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat cardiac arrhythmias. Discuss the management options and goals for patients hospitalized with arrhythmias.
Describe the patient characteristics and comorbid conditions that predict outcomes in patients with arrhythmias.
Recognize indications for specialty consultation, which may include cardiology and cardiac electrophysiology.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
Recall appropriate indications for both initiation and discontinuation of continuous telemetry monitoring in the hospitalized patient.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, including medications, family history, and social history.
Perform a targeted physical examination with emphasis on identifying signs associated with hemodynamic instability, tissue perfusion, and occult cardiac and vascular disease.
Identify common benign and pathologic arrhythmias on electrocardiography, rhythm strips, and continuous telemetry monitoring.
Determine the appropriate level of care required based on risk stratification of patients with cardiac arrhythmias.
Identify and prioritize high-risk arrhythmias that require urgent intervention and implement emergency protocols as indicated.
Formulate patient-specific and evidence-based care plans incorporating diagnostic findings, prognosis, and patient characteristics.
Develop patient-specific care plans that may include rate-controlling interventions, cardioversion, defibrillation, or implantable medical devices.
Communicate with patients and families to explain the natural history and prognosis of cardiac arrhythmias.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain drug interactions for antiarrhythmic drugs and the importance of strict adherence to medication regimens and laboratory monitoring.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include primary care, cardiology, nursing, and social services, in the care of patients with cardiac arrhythmias that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of cardiac arrhythmias.
Acknowledge and ameliorate patient discomfort from uncontrolled arrhythmias and electrical cardioversion therapies.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop patient care guidelines and/or pathways on the basis of peer-reviewed outcomes research, patient and physician satisfaction, and cost.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, The Joint Commission, American Heart Association, American College of Cardiology, Agency for Healthcare Research and Quality).
Lead, coordinate, and/or participate in quality improvement initiatives to promote early identification of arrhythmias, reduce preventable complications, and promote appropriate use of telemetry resources.
Cardiac arrhythmias are a group of conditions characterized by an abnormal heart rate or rhythm. These are common and affect approximately 5% of the population in the United States. More than 250,000 Americans die each year of sudden cardiac arrest, and most cases are thought to be due to ventricular fibrillation or ventricular tachycardia.1 Several cardiac arrhythmias can cause instability, prompting hospitalization, or they may result from complications during hospitalization. Annually, more than 740,000 hospital discharges are associated with a primary diagnosis of cardiac arrhythmia.2 Hospitalists identify and treat all types of arrhythmias, coordinate specialty and primary care resources, and transition patients safely and cost-effectively through the acute hospitalization and into the outpatient setting.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Identify and differentiate the common clinical presentations of both benign and pathologic arrhythmias.
Explain the causes of atrial and ventricular arrhythmias.
Describe the indicated tests required to evaluate arrhythmias.
Explain how medications, metabolic abnormalities, and medical comorbidities may precipitate various arrhythmias.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat cardiac arrhythmias. Discuss the management options and goals for patients hospitalized with arrhythmias.
Describe the patient characteristics and comorbid conditions that predict outcomes in patients with arrhythmias.
Recognize indications for specialty consultation, which may include cardiology and cardiac electrophysiology.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
Recall appropriate indications for both initiation and discontinuation of continuous telemetry monitoring in the hospitalized patient.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, including medications, family history, and social history.
Perform a targeted physical examination with emphasis on identifying signs associated with hemodynamic instability, tissue perfusion, and occult cardiac and vascular disease.
Identify common benign and pathologic arrhythmias on electrocardiography, rhythm strips, and continuous telemetry monitoring.
Determine the appropriate level of care required based on risk stratification of patients with cardiac arrhythmias.
Identify and prioritize high-risk arrhythmias that require urgent intervention and implement emergency protocols as indicated.
Formulate patient-specific and evidence-based care plans incorporating diagnostic findings, prognosis, and patient characteristics.
Develop patient-specific care plans that may include rate-controlling interventions, cardioversion, defibrillation, or implantable medical devices.
Communicate with patients and families to explain the natural history and prognosis of cardiac arrhythmias.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain drug interactions for antiarrhythmic drugs and the importance of strict adherence to medication regimens and laboratory monitoring.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include primary care, cardiology, nursing, and social services, in the care of patients with cardiac arrhythmias that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of cardiac arrhythmias.
Acknowledge and ameliorate patient discomfort from uncontrolled arrhythmias and electrical cardioversion therapies.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop patient care guidelines and/or pathways on the basis of peer-reviewed outcomes research, patient and physician satisfaction, and cost.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, The Joint Commission, American Heart Association, American College of Cardiology, Agency for Healthcare Research and Quality).
Lead, coordinate, and/or participate in quality improvement initiatives to promote early identification of arrhythmias, reduce preventable complications, and promote appropriate use of telemetry resources.
Cardiac arrhythmias are a group of conditions characterized by an abnormal heart rate or rhythm. These are common and affect approximately 5% of the population in the United States. More than 250,000 Americans die each year of sudden cardiac arrest, and most cases are thought to be due to ventricular fibrillation or ventricular tachycardia.1 Several cardiac arrhythmias can cause instability, prompting hospitalization, or they may result from complications during hospitalization. Annually, more than 740,000 hospital discharges are associated with a primary diagnosis of cardiac arrhythmia.2 Hospitalists identify and treat all types of arrhythmias, coordinate specialty and primary care resources, and transition patients safely and cost-effectively through the acute hospitalization and into the outpatient setting.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Identify and differentiate the common clinical presentations of both benign and pathologic arrhythmias.
Explain the causes of atrial and ventricular arrhythmias.
Describe the indicated tests required to evaluate arrhythmias.
Explain how medications, metabolic abnormalities, and medical comorbidities may precipitate various arrhythmias.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat cardiac arrhythmias. Discuss the management options and goals for patients hospitalized with arrhythmias.
Describe the patient characteristics and comorbid conditions that predict outcomes in patients with arrhythmias.
Recognize indications for specialty consultation, which may include cardiology and cardiac electrophysiology.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
Recall appropriate indications for both initiation and discontinuation of continuous telemetry monitoring in the hospitalized patient.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, including medications, family history, and social history.
Perform a targeted physical examination with emphasis on identifying signs associated with hemodynamic instability, tissue perfusion, and occult cardiac and vascular disease.
Identify common benign and pathologic arrhythmias on electrocardiography, rhythm strips, and continuous telemetry monitoring.
Determine the appropriate level of care required based on risk stratification of patients with cardiac arrhythmias.
Identify and prioritize high-risk arrhythmias that require urgent intervention and implement emergency protocols as indicated.
Formulate patient-specific and evidence-based care plans incorporating diagnostic findings, prognosis, and patient characteristics.
Develop patient-specific care plans that may include rate-controlling interventions, cardioversion, defibrillation, or implantable medical devices.
Communicate with patients and families to explain the natural history and prognosis of cardiac arrhythmias.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain drug interactions for antiarrhythmic drugs and the importance of strict adherence to medication regimens and laboratory monitoring.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include primary care, cardiology, nursing, and social services, in the care of patients with cardiac arrhythmias that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of cardiac arrhythmias.
Acknowledge and ameliorate patient discomfort from uncontrolled arrhythmias and electrical cardioversion therapies.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop patient care guidelines and/or pathways on the basis of peer-reviewed outcomes research, patient and physician satisfaction, and cost.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, The Joint Commission, American Heart Association, American College of Cardiology, Agency for Healthcare Research and Quality).
Lead, coordinate, and/or participate in quality improvement initiatives to promote early identification of arrhythmias, reduce preventable complications, and promote appropriate use of telemetry resources.
© 2017 Society of Hospital Medicine
Chronic Obstructive Pulmonary Disease. 2017 Hospital Medicine Revised Core Competencies
Chronic obstructive pulmonary disease (COPD) is a heterogeneous group of respiratory conditions, predominantly composed of chronic bronchitis and emphysema. COPD is defined by airflow limitation that is not completely reversible, and it is associated with an abnormal airway inflammatory response. Exposure to tobacco smoke is the main risk factor. COPD affects more than 12 million Americans and is the third leading cause of death in the United States. A COPD exacerbation is defined as an increase in the usual symptoms of COPD that is beyond day-to-day variations and leads to a change in medication and often results in hospitalization. Annually, more than 670,000 hospital discharges occur with COPD as the primary diagnosis, and nearly 1 of every 5 hospitalized patients 40 years or older has COPD.1,2The average length of stay is 4.3 days.1 COPD is a substantial cause of disability and carries a large economic burden, accounting for almost $17 billion of total hospital charges billed to Medicare each year.3 The early detection and prompt treatment of exacerbations are essential to ensure optimal outcomes and to reduce the burden of COPD. Hospitalists use evidence-based approaches to optimize care, and they should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to reduce readmission rates and mortality from COPD exacerbations.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define COPD and describe the pathophysiologic processes that lead to small airway obstruction and alveolar destruction.
Describe potential precipitants of exacerbation, including both infectious and noninfectious etiologies.
Differentiate the clinical presentation of a COPD exacerbation from asthma, heart failure, and other acute respiratory and nonrespiratory syndromes.
List the indicators of disease severity.
Describe the role of diagnostic testing used for the evaluation of COPD.
Describe the role of pulmonary function tests in the treatment of a COPD exacerbation.
Distinguish the medical management of patients with COPD exacerbations from that of patients with stable COPD.
Recognize indications for specialty consultation, which may include pulmonary medicine.
Describe the evidence-based therapies for treatment of COPD exacerbations, which may include bronchodilators, systemic corticosteroids, oxygen, and antibiotics.
Identify the potential risks of supplemental oxygen therapy, including development of hypercarbia in patients with chronic respiratory acidosis.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat COPD.
Describe and differentiate the means of ventilatory support, including the use of noninvasive positive pressure ventilation in COPD exacerbation.
Recognize anxiety and depression as important comorbid conditions that negatively affect outcomes.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with a COPD exacerbation and etiologic precipitants.
Perform a targeted physical examination to elicit signs consistent with a COPD exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Diagnose a COPD exacerbation on the basis of history, physical examination, and radiographic data.
Select and interpret appropriate diagnostic studies to evaluate the severity of a COPD exacerbation.
Recognize symptoms, signs, and severity of impending respiratory failure and select the indicated evidence-based ventilatory approach.
Select patients with COPD exacerbation who would benefit from use of positive pressure ventilation and identify those in whom this intervention is contraindicated.
Prescribe appropriate evidence-based pharmacologic therapies during COPD exacerbation, recommending the most appropriate drug route, dose, frequency, and duration of treatment.
Address treatment preferences, including advance directives early during hospital stay; implement end-of-life decisions by patients and/or families when indicated or desired.
Evaluate COPD in perioperative risk assessment, recommend measures to optimize perioperative management of COPD, and manage postoperative complications related to underlying COPD.
Identify patients with COPD who may benefit from pulmonary rehabilitation.
Communicate with patients and families to explain the natural history and prognosis of COPD.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Ensure that patients receive training on proper inhaler techniques and use before hospital discharge.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with a COPD exacerbation, beginning at admission and continuing through all care transitions.
Engage in a collaborative way with primary care physicians and emergency physicians in making admission decisions.
Promote and encourage preventive strategies, including smoking cessation, vaccinations, and venous thromboembolism prophylaxis.
Establish and maintain an open dialogue with patients and/or families regarding goals and limitations of care, including palliative care and end-of-life wishes.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with COPD.
Lead, coordinate, and/or participate in the development of educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for COPD exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead efforts to educate patients and staff on the importance of smoking cessation and other preventive measures.
1. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
2. Wier LM, Elizhauser A, Pfuntner A, Au DH. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Overview of Hospitalizations Among Patients With COPD, 2008. Statistical Brief #106. Rockville, MD; Agency for Health Care Policy and Research (US). 2011. Available at: http://www.ncbi.nlm.nih.gov/books/NBK53969/. Accessed June 2015.
3. Agency for Healthcare Research and Quality. Chronic obstructive pulmonary disease (COPD): hospital 30-day, all-cause, risk-standardized mortality rate following acute exacerbation of COPD. Available at http://www.qualitymeasures.ahrq.gov/content.aspx?id=48198. Accessed June 2015.
Chronic obstructive pulmonary disease (COPD) is a heterogeneous group of respiratory conditions, predominantly composed of chronic bronchitis and emphysema. COPD is defined by airflow limitation that is not completely reversible, and it is associated with an abnormal airway inflammatory response. Exposure to tobacco smoke is the main risk factor. COPD affects more than 12 million Americans and is the third leading cause of death in the United States. A COPD exacerbation is defined as an increase in the usual symptoms of COPD that is beyond day-to-day variations and leads to a change in medication and often results in hospitalization. Annually, more than 670,000 hospital discharges occur with COPD as the primary diagnosis, and nearly 1 of every 5 hospitalized patients 40 years or older has COPD.1,2The average length of stay is 4.3 days.1 COPD is a substantial cause of disability and carries a large economic burden, accounting for almost $17 billion of total hospital charges billed to Medicare each year.3 The early detection and prompt treatment of exacerbations are essential to ensure optimal outcomes and to reduce the burden of COPD. Hospitalists use evidence-based approaches to optimize care, and they should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to reduce readmission rates and mortality from COPD exacerbations.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define COPD and describe the pathophysiologic processes that lead to small airway obstruction and alveolar destruction.
Describe potential precipitants of exacerbation, including both infectious and noninfectious etiologies.
Differentiate the clinical presentation of a COPD exacerbation from asthma, heart failure, and other acute respiratory and nonrespiratory syndromes.
List the indicators of disease severity.
Describe the role of diagnostic testing used for the evaluation of COPD.
Describe the role of pulmonary function tests in the treatment of a COPD exacerbation.
Distinguish the medical management of patients with COPD exacerbations from that of patients with stable COPD.
Recognize indications for specialty consultation, which may include pulmonary medicine.
Describe the evidence-based therapies for treatment of COPD exacerbations, which may include bronchodilators, systemic corticosteroids, oxygen, and antibiotics.
Identify the potential risks of supplemental oxygen therapy, including development of hypercarbia in patients with chronic respiratory acidosis.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat COPD.
Describe and differentiate the means of ventilatory support, including the use of noninvasive positive pressure ventilation in COPD exacerbation.
Recognize anxiety and depression as important comorbid conditions that negatively affect outcomes.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with a COPD exacerbation and etiologic precipitants.
Perform a targeted physical examination to elicit signs consistent with a COPD exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Diagnose a COPD exacerbation on the basis of history, physical examination, and radiographic data.
Select and interpret appropriate diagnostic studies to evaluate the severity of a COPD exacerbation.
Recognize symptoms, signs, and severity of impending respiratory failure and select the indicated evidence-based ventilatory approach.
Select patients with COPD exacerbation who would benefit from use of positive pressure ventilation and identify those in whom this intervention is contraindicated.
Prescribe appropriate evidence-based pharmacologic therapies during COPD exacerbation, recommending the most appropriate drug route, dose, frequency, and duration of treatment.
Address treatment preferences, including advance directives early during hospital stay; implement end-of-life decisions by patients and/or families when indicated or desired.
Evaluate COPD in perioperative risk assessment, recommend measures to optimize perioperative management of COPD, and manage postoperative complications related to underlying COPD.
Identify patients with COPD who may benefit from pulmonary rehabilitation.
Communicate with patients and families to explain the natural history and prognosis of COPD.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Ensure that patients receive training on proper inhaler techniques and use before hospital discharge.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with a COPD exacerbation, beginning at admission and continuing through all care transitions.
Engage in a collaborative way with primary care physicians and emergency physicians in making admission decisions.
Promote and encourage preventive strategies, including smoking cessation, vaccinations, and venous thromboembolism prophylaxis.
Establish and maintain an open dialogue with patients and/or families regarding goals and limitations of care, including palliative care and end-of-life wishes.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with COPD.
Lead, coordinate, and/or participate in the development of educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for COPD exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead efforts to educate patients and staff on the importance of smoking cessation and other preventive measures.
Chronic obstructive pulmonary disease (COPD) is a heterogeneous group of respiratory conditions, predominantly composed of chronic bronchitis and emphysema. COPD is defined by airflow limitation that is not completely reversible, and it is associated with an abnormal airway inflammatory response. Exposure to tobacco smoke is the main risk factor. COPD affects more than 12 million Americans and is the third leading cause of death in the United States. A COPD exacerbation is defined as an increase in the usual symptoms of COPD that is beyond day-to-day variations and leads to a change in medication and often results in hospitalization. Annually, more than 670,000 hospital discharges occur with COPD as the primary diagnosis, and nearly 1 of every 5 hospitalized patients 40 years or older has COPD.1,2The average length of stay is 4.3 days.1 COPD is a substantial cause of disability and carries a large economic burden, accounting for almost $17 billion of total hospital charges billed to Medicare each year.3 The early detection and prompt treatment of exacerbations are essential to ensure optimal outcomes and to reduce the burden of COPD. Hospitalists use evidence-based approaches to optimize care, and they should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to reduce readmission rates and mortality from COPD exacerbations.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define COPD and describe the pathophysiologic processes that lead to small airway obstruction and alveolar destruction.
Describe potential precipitants of exacerbation, including both infectious and noninfectious etiologies.
Differentiate the clinical presentation of a COPD exacerbation from asthma, heart failure, and other acute respiratory and nonrespiratory syndromes.
List the indicators of disease severity.
Describe the role of diagnostic testing used for the evaluation of COPD.
Describe the role of pulmonary function tests in the treatment of a COPD exacerbation.
Distinguish the medical management of patients with COPD exacerbations from that of patients with stable COPD.
Recognize indications for specialty consultation, which may include pulmonary medicine.
Describe the evidence-based therapies for treatment of COPD exacerbations, which may include bronchodilators, systemic corticosteroids, oxygen, and antibiotics.
Identify the potential risks of supplemental oxygen therapy, including development of hypercarbia in patients with chronic respiratory acidosis.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat COPD.
Describe and differentiate the means of ventilatory support, including the use of noninvasive positive pressure ventilation in COPD exacerbation.
Recognize anxiety and depression as important comorbid conditions that negatively affect outcomes.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with a COPD exacerbation and etiologic precipitants.
Perform a targeted physical examination to elicit signs consistent with a COPD exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Diagnose a COPD exacerbation on the basis of history, physical examination, and radiographic data.
Select and interpret appropriate diagnostic studies to evaluate the severity of a COPD exacerbation.
Recognize symptoms, signs, and severity of impending respiratory failure and select the indicated evidence-based ventilatory approach.
Select patients with COPD exacerbation who would benefit from use of positive pressure ventilation and identify those in whom this intervention is contraindicated.
Prescribe appropriate evidence-based pharmacologic therapies during COPD exacerbation, recommending the most appropriate drug route, dose, frequency, and duration of treatment.
Address treatment preferences, including advance directives early during hospital stay; implement end-of-life decisions by patients and/or families when indicated or desired.
Evaluate COPD in perioperative risk assessment, recommend measures to optimize perioperative management of COPD, and manage postoperative complications related to underlying COPD.
Identify patients with COPD who may benefit from pulmonary rehabilitation.
Communicate with patients and families to explain the natural history and prognosis of COPD.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Ensure that patients receive training on proper inhaler techniques and use before hospital discharge.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with a COPD exacerbation, beginning at admission and continuing through all care transitions.
Engage in a collaborative way with primary care physicians and emergency physicians in making admission decisions.
Promote and encourage preventive strategies, including smoking cessation, vaccinations, and venous thromboembolism prophylaxis.
Establish and maintain an open dialogue with patients and/or families regarding goals and limitations of care, including palliative care and end-of-life wishes.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with COPD.
Lead, coordinate, and/or participate in the development of educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for COPD exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead efforts to educate patients and staff on the importance of smoking cessation and other preventive measures.
1. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
2. Wier LM, Elizhauser A, Pfuntner A, Au DH. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Overview of Hospitalizations Among Patients With COPD, 2008. Statistical Brief #106. Rockville, MD; Agency for Health Care Policy and Research (US). 2011. Available at: http://www.ncbi.nlm.nih.gov/books/NBK53969/. Accessed June 2015.
3. Agency for Healthcare Research and Quality. Chronic obstructive pulmonary disease (COPD): hospital 30-day, all-cause, risk-standardized mortality rate following acute exacerbation of COPD. Available at http://www.qualitymeasures.ahrq.gov/content.aspx?id=48198. Accessed June 2015.
1. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
2. Wier LM, Elizhauser A, Pfuntner A, Au DH. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Overview of Hospitalizations Among Patients With COPD, 2008. Statistical Brief #106. Rockville, MD; Agency for Health Care Policy and Research (US). 2011. Available at: http://www.ncbi.nlm.nih.gov/books/NBK53969/. Accessed June 2015.
3. Agency for Healthcare Research and Quality. Chronic obstructive pulmonary disease (COPD): hospital 30-day, all-cause, risk-standardized mortality rate following acute exacerbation of COPD. Available at http://www.qualitymeasures.ahrq.gov/content.aspx?id=48198. Accessed June 2015.
© 2017 Society of Hospital Medicine
Community-Acquired Pneumonia. 2017 Hospital Medicine Revised Core Competencies
Community-acquired pneumonia (CAP) is an infection of the lung parenchyma that occurs in the community or is diagnosed within 48 hours of hospital admission. CAP is a common and potentially life-threatening infection, and it is a leading cause of death from infectious diseases. Approximately 25% of persons with CAP require hospitalization, and 10% to 20% of these patients require admission to the intensive care unit.1-3 The mortality rate ranges from about 13% in hospitalized patients to 36% in patients admitted to the intensive care unit.1-3 CAP is a curable condition and an organized approach to management is likely to improve clinical results and reduce mortality. Pneumonia outcome measures are used to evaluate performance of healthcare providers and organizations. Hospitalists apply evidence-based guidelines to the management of patients hospitalized with pneumonia and lead initiatives to improve quality of care and reduce practice variability.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define CAP, list the likely etiologies and the signs and symptoms, and distinguish CAP from hospital-acquired pneumonia and healthcare-associated pneumonia.
Describe other causes of pulmonary infiltrates on radiographic studies.
Describe the tests indicated to evaluate and treat CAP.
Explain indications for respiratory isolation.
Identify patients with comorbidities (such as immunocompromise, diabetes mellitus, and extremes of age) who are at high risk of a complicated course.
Identify specific pathogens that predispose patients to a complicated course.
Recognize indications for specialty consultation.
Describe indicated therapeutic modalities for CAP, including oxygen therapy, respiratory care modalities, appropriate antimicrobial selection and duration, and other evidence-based treatments.
Predict patient risk for morbidity and mortality from CAP using a validated risk score.
Explain goals for hospital discharge, including evidence-based measures of clinical stability for safe care transition.
Describe factors associated with a nonresponding pneumonia.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with CAP and demographic factors that may predispose patients to CAP.
Perform a targeted physical examination to elicit signs consistent with CAP and differentiate it from other mimicking conditions.
Order and interpret laboratory, microbiologic, and radiologic studies to confirm the diagnosis of CAP and risk stratify patients.
Apply evidence-based tools (such as the Pneumonia Severity Index) to triage decisions and identify factors that support the need for intensive care unit admission.
Initiate empiric antimicrobials for CAP on the basis of illness severity and evidence-based national guidelines, incorporating local resistance patterns.
Formulate a subsequent treatment plan that includes narrowing antimicrobial therapies on the basis of available culture data and patient response to treatment.
Recognize the criteria for clinical stability, including the appropriate deescalation of treatment such as transitioning from parenteral to oral antimicrobials.
Recognize and address complications of CAP and/or inadequate response to therapy, including respiratory failure and parapneumonic effusions.
Communicate with patients and families to explain the pathophysiology and prognosis of CAP.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain the use and potential adverse effects of pharmacologic agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures such as smoking cessation), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Recognize and address barriers to follow-up care and anticipated postdischarge requirements.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, respiratory therapy, nutrition, and pharmacy services, to the care of patients with CAP through all care transitions.
Follow evidence-based recommendations for the treatment of patients with CAP.
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with infectious disease and pulmonary specialists, to promote patient safety and cost-effective diagnostic and management strategies for patients with CAP.
Lead, coordinate, and/or participate in efforts to identify, address, and monitor quality indicators for CAP.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, Centers for Medicare & Medicaid Services, Infectious Diseases Society of America, American Thoracic Society).
Integrate evidence-based clinical severity scores and clinical judgment into admission decisions.
Lead efforts to educate staff on the importance of smoking cessation counseling, vaccinations, and other preventive measures.
1. File TM Jr, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122(2):130-141.
2. Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134.
3. Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, et al; American Thoracic Society. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163(7):1730-1754.
Community-acquired pneumonia (CAP) is an infection of the lung parenchyma that occurs in the community or is diagnosed within 48 hours of hospital admission. CAP is a common and potentially life-threatening infection, and it is a leading cause of death from infectious diseases. Approximately 25% of persons with CAP require hospitalization, and 10% to 20% of these patients require admission to the intensive care unit.1-3 The mortality rate ranges from about 13% in hospitalized patients to 36% in patients admitted to the intensive care unit.1-3 CAP is a curable condition and an organized approach to management is likely to improve clinical results and reduce mortality. Pneumonia outcome measures are used to evaluate performance of healthcare providers and organizations. Hospitalists apply evidence-based guidelines to the management of patients hospitalized with pneumonia and lead initiatives to improve quality of care and reduce practice variability.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define CAP, list the likely etiologies and the signs and symptoms, and distinguish CAP from hospital-acquired pneumonia and healthcare-associated pneumonia.
Describe other causes of pulmonary infiltrates on radiographic studies.
Describe the tests indicated to evaluate and treat CAP.
Explain indications for respiratory isolation.
Identify patients with comorbidities (such as immunocompromise, diabetes mellitus, and extremes of age) who are at high risk of a complicated course.
Identify specific pathogens that predispose patients to a complicated course.
Recognize indications for specialty consultation.
Describe indicated therapeutic modalities for CAP, including oxygen therapy, respiratory care modalities, appropriate antimicrobial selection and duration, and other evidence-based treatments.
Predict patient risk for morbidity and mortality from CAP using a validated risk score.
Explain goals for hospital discharge, including evidence-based measures of clinical stability for safe care transition.
Describe factors associated with a nonresponding pneumonia.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with CAP and demographic factors that may predispose patients to CAP.
Perform a targeted physical examination to elicit signs consistent with CAP and differentiate it from other mimicking conditions.
Order and interpret laboratory, microbiologic, and radiologic studies to confirm the diagnosis of CAP and risk stratify patients.
Apply evidence-based tools (such as the Pneumonia Severity Index) to triage decisions and identify factors that support the need for intensive care unit admission.
Initiate empiric antimicrobials for CAP on the basis of illness severity and evidence-based national guidelines, incorporating local resistance patterns.
Formulate a subsequent treatment plan that includes narrowing antimicrobial therapies on the basis of available culture data and patient response to treatment.
Recognize the criteria for clinical stability, including the appropriate deescalation of treatment such as transitioning from parenteral to oral antimicrobials.
Recognize and address complications of CAP and/or inadequate response to therapy, including respiratory failure and parapneumonic effusions.
Communicate with patients and families to explain the pathophysiology and prognosis of CAP.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain the use and potential adverse effects of pharmacologic agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures such as smoking cessation), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Recognize and address barriers to follow-up care and anticipated postdischarge requirements.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, respiratory therapy, nutrition, and pharmacy services, to the care of patients with CAP through all care transitions.
Follow evidence-based recommendations for the treatment of patients with CAP.
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with infectious disease and pulmonary specialists, to promote patient safety and cost-effective diagnostic and management strategies for patients with CAP.
Lead, coordinate, and/or participate in efforts to identify, address, and monitor quality indicators for CAP.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, Centers for Medicare & Medicaid Services, Infectious Diseases Society of America, American Thoracic Society).
Integrate evidence-based clinical severity scores and clinical judgment into admission decisions.
Lead efforts to educate staff on the importance of smoking cessation counseling, vaccinations, and other preventive measures.
Community-acquired pneumonia (CAP) is an infection of the lung parenchyma that occurs in the community or is diagnosed within 48 hours of hospital admission. CAP is a common and potentially life-threatening infection, and it is a leading cause of death from infectious diseases. Approximately 25% of persons with CAP require hospitalization, and 10% to 20% of these patients require admission to the intensive care unit.1-3 The mortality rate ranges from about 13% in hospitalized patients to 36% in patients admitted to the intensive care unit.1-3 CAP is a curable condition and an organized approach to management is likely to improve clinical results and reduce mortality. Pneumonia outcome measures are used to evaluate performance of healthcare providers and organizations. Hospitalists apply evidence-based guidelines to the management of patients hospitalized with pneumonia and lead initiatives to improve quality of care and reduce practice variability.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define CAP, list the likely etiologies and the signs and symptoms, and distinguish CAP from hospital-acquired pneumonia and healthcare-associated pneumonia.
Describe other causes of pulmonary infiltrates on radiographic studies.
Describe the tests indicated to evaluate and treat CAP.
Explain indications for respiratory isolation.
Identify patients with comorbidities (such as immunocompromise, diabetes mellitus, and extremes of age) who are at high risk of a complicated course.
Identify specific pathogens that predispose patients to a complicated course.
Recognize indications for specialty consultation.
Describe indicated therapeutic modalities for CAP, including oxygen therapy, respiratory care modalities, appropriate antimicrobial selection and duration, and other evidence-based treatments.
Predict patient risk for morbidity and mortality from CAP using a validated risk score.
Explain goals for hospital discharge, including evidence-based measures of clinical stability for safe care transition.
Describe factors associated with a nonresponding pneumonia.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with CAP and demographic factors that may predispose patients to CAP.
Perform a targeted physical examination to elicit signs consistent with CAP and differentiate it from other mimicking conditions.
Order and interpret laboratory, microbiologic, and radiologic studies to confirm the diagnosis of CAP and risk stratify patients.
Apply evidence-based tools (such as the Pneumonia Severity Index) to triage decisions and identify factors that support the need for intensive care unit admission.
Initiate empiric antimicrobials for CAP on the basis of illness severity and evidence-based national guidelines, incorporating local resistance patterns.
Formulate a subsequent treatment plan that includes narrowing antimicrobial therapies on the basis of available culture data and patient response to treatment.
Recognize the criteria for clinical stability, including the appropriate deescalation of treatment such as transitioning from parenteral to oral antimicrobials.
Recognize and address complications of CAP and/or inadequate response to therapy, including respiratory failure and parapneumonic effusions.
Communicate with patients and families to explain the pathophysiology and prognosis of CAP.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain the use and potential adverse effects of pharmacologic agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures such as smoking cessation), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Recognize and address barriers to follow-up care and anticipated postdischarge requirements.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, respiratory therapy, nutrition, and pharmacy services, to the care of patients with CAP through all care transitions.
Follow evidence-based recommendations for the treatment of patients with CAP.
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with infectious disease and pulmonary specialists, to promote patient safety and cost-effective diagnostic and management strategies for patients with CAP.
Lead, coordinate, and/or participate in efforts to identify, address, and monitor quality indicators for CAP.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, Centers for Medicare & Medicaid Services, Infectious Diseases Society of America, American Thoracic Society).
Integrate evidence-based clinical severity scores and clinical judgment into admission decisions.
Lead efforts to educate staff on the importance of smoking cessation counseling, vaccinations, and other preventive measures.
1. File TM Jr, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122(2):130-141.
2. Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134.
3. Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, et al; American Thoracic Society. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163(7):1730-1754.
1. File TM Jr, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122(2):130-141.
2. Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134.
3. Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, et al; American Thoracic Society. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163(7):1730-1754.
© 2017 Society of Hospital Medicine
Delirium and Dementia. 2017 Hospital Medicine Revised Core Competencies
DELIRIUM
Delirium is defined as an acute, transient, global disorder of cognition. In two-thirds of cases, delirium occurs in patients with baseline vulnerability, including those with underlying dementia.1 Although up to 30% of older medical patients experience delirium during hospitalization, this condition is unrecognized in nearly two-thirds of cases.2-4 Patients with delirium experience an average increase in length of hospital stay of 8 days and mortality rates that are twice as high as those of patients without delirium.5,6 In addition, delirium is associated with high rates of functional and cognitive decline and skilled nursing facility placement after hospitalization. The cost of caring for patients with delirium has a marked impact on individual patients, families, and hospital systems. Hospitalists lead their institutions in the development of screening and prevention protocols for patients at risk for delirium, as well as in the promotion of safe treatment approaches. Hospitalists also develop strategies to operationalize cost-effective delirium prevention programs that improve outcomes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
DELIRIUM KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate delirium from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate delirium.
Describe the causes of delirium in the hospital setting including environmental and iatrogenic risk factors.
Identify medications known to precipitate delirium.
Recognize the indications for specialty consultations.
Describe methods for the prevention of delirium.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat delirium.
Describe nonpharmacologic therapies to manage delirium.
Describe the complications of delirium in the hospitalized patient.
Discuss the multifaceted impact that delirium has on patients and their families.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
DELIRIUM SKILLS
Hospitalists should be able to:
Predict a patient’s risk for the development of delirium on the basis of initial history and physical examination.
Perform appropriate screening for delirium.
Develop active strategies to reduce delirium in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected delirium in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Perform a focused evaluation for the underlying etiology of delirium and institute prompt treatment to lessen its severity.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with delirium.
Lead multidisciplinary teams to develop and implement care plans for patients with delirium.
Develop an appropriate pharmacologic plan to manage delirium.
Develop an appropriate nonpharmacologic plan to manage delirium.
Develop an appropriate management plan for patients with delirium in the postoperative setting.
Document an appropriate treatment plan to reduce mortality, limit the duration of delirium and the time required to control agitation, maintain adequate control of delirium, address complications, and manage cost of treatment.
Use a patient- and family-centered approach in the care of older inpatients.
Establish goals and boundaries of care with patients and their families.
Communicate with patients and families to explain the history and prognosis of delirium.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DELIRIUM ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with delirium that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of delirium and its causes.
Value a patient- and family-centered approach in the care of older inpatients.
DELIRIUM SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for delirium.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration with geriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with delirium.
DEMENTIA
Dementia is defined as a chronic, often progressive, decline in cognitive function, eventually limiting daily activities. Dementia is a common comorbidity in the hospitalized older patient. Alzheimer disease is the most prevalent form of dementia in older patients, and it accounts for up to 80% of cases.7,8 More than 5 million persons older than 65 years have Alzheimer disease in the United States.7,8 Patients with dementia are at increased risk for delirium, falls, and functional decline during hospitalization. Patients with baseline cognitive impairment have prolonged lengths of stay and complex needs after discharge. Agitation and behavioral symptoms of dementia can be exacerbated in the hospital setting and are often difficult to manage. Care of the patient with dementia requires that hospitalists engage in a multidisciplinary approach to inpatient and transitional care. Hospitalists may also become involved in hospital quality and safety initiatives that pertain to areas such as restraint use and fall prevention.
DEMENTIA KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate dementia from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate dementia.
Describe the causes of potentially reversible dementias or dementia-like conditions.
List indications, contraindications, and mechanisms of action of pharmacologic agents used to treat dementia.
Describe nonpharmacologic therapies to manage dementia symptoms.
Recognize the indications for specialty consultations.
Describe the complications of dementia in the hospitalized patient.
Discuss the multifaceted impact that dementia has on patients and their families.
Explain goals for hospital discharge including specific measures of clinical stability for safe care transition.
DEMENTIA SKILLS
Hospitalists should be able to:
Perform appropriate screening for dementia.
Develop active strategies to reduce development of delirium in patients with dementia in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected dementia in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Assess patients for potentially reversible causes of dementia or dementia-like conditions. Assess severity of cognitive impairment and perform a focused evaluation for the underlying etiology of dementia when appropriate.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with dementia.
Formulate and lead multidisciplinary teams to develop and implement care plans for patients with dementia.
Develop an appropriate pharmacologic plan to manage dementia.
Develop an appropriate nonpharmacologic plan to manage dementia.
Use a patient- and family-centered approach in the care of older inpatients.
Communicate with patients and families to explain the history and prognosis of dementia.
Use evidence-based methods and tools to assess patients’ medical decision-making capacity.
Defend patients’ right to autonomy when so qualified.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DEMENTIA ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with dementia that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of dementia and its causes.
Value a patient- and family-centered approach to educate and engage families and caregivers in the care of older inpatients.
Responsibly address and respect end-of-life care wishes for patients with advanced dementia.
DEMENTIA SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for poor outcomes related to dementia.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration withgeriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with dementia.
1. Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7-21.
2. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
3. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242.
4. Francis J. Delirium in older patients. J Am Geriatr Soc. 1992;40(8):829-838.
5. Cole MG, Primeau FJ. Prognosis of delirium in elderly hospital patients. CMAJ. 1993;149(1):41.
6. McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162(4):457-463.
7. Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. Available at: https://www.alz.org/downloads/Facts_Figures_2014.pdf. Accessed July 2015.
8. Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
DELIRIUM
Delirium is defined as an acute, transient, global disorder of cognition. In two-thirds of cases, delirium occurs in patients with baseline vulnerability, including those with underlying dementia.1 Although up to 30% of older medical patients experience delirium during hospitalization, this condition is unrecognized in nearly two-thirds of cases.2-4 Patients with delirium experience an average increase in length of hospital stay of 8 days and mortality rates that are twice as high as those of patients without delirium.5,6 In addition, delirium is associated with high rates of functional and cognitive decline and skilled nursing facility placement after hospitalization. The cost of caring for patients with delirium has a marked impact on individual patients, families, and hospital systems. Hospitalists lead their institutions in the development of screening and prevention protocols for patients at risk for delirium, as well as in the promotion of safe treatment approaches. Hospitalists also develop strategies to operationalize cost-effective delirium prevention programs that improve outcomes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
DELIRIUM KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate delirium from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate delirium.
Describe the causes of delirium in the hospital setting including environmental and iatrogenic risk factors.
Identify medications known to precipitate delirium.
Recognize the indications for specialty consultations.
Describe methods for the prevention of delirium.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat delirium.
Describe nonpharmacologic therapies to manage delirium.
Describe the complications of delirium in the hospitalized patient.
Discuss the multifaceted impact that delirium has on patients and their families.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
DELIRIUM SKILLS
Hospitalists should be able to:
Predict a patient’s risk for the development of delirium on the basis of initial history and physical examination.
Perform appropriate screening for delirium.
Develop active strategies to reduce delirium in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected delirium in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Perform a focused evaluation for the underlying etiology of delirium and institute prompt treatment to lessen its severity.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with delirium.
Lead multidisciplinary teams to develop and implement care plans for patients with delirium.
Develop an appropriate pharmacologic plan to manage delirium.
Develop an appropriate nonpharmacologic plan to manage delirium.
Develop an appropriate management plan for patients with delirium in the postoperative setting.
Document an appropriate treatment plan to reduce mortality, limit the duration of delirium and the time required to control agitation, maintain adequate control of delirium, address complications, and manage cost of treatment.
Use a patient- and family-centered approach in the care of older inpatients.
Establish goals and boundaries of care with patients and their families.
Communicate with patients and families to explain the history and prognosis of delirium.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DELIRIUM ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with delirium that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of delirium and its causes.
Value a patient- and family-centered approach in the care of older inpatients.
DELIRIUM SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for delirium.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration with geriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with delirium.
DEMENTIA
Dementia is defined as a chronic, often progressive, decline in cognitive function, eventually limiting daily activities. Dementia is a common comorbidity in the hospitalized older patient. Alzheimer disease is the most prevalent form of dementia in older patients, and it accounts for up to 80% of cases.7,8 More than 5 million persons older than 65 years have Alzheimer disease in the United States.7,8 Patients with dementia are at increased risk for delirium, falls, and functional decline during hospitalization. Patients with baseline cognitive impairment have prolonged lengths of stay and complex needs after discharge. Agitation and behavioral symptoms of dementia can be exacerbated in the hospital setting and are often difficult to manage. Care of the patient with dementia requires that hospitalists engage in a multidisciplinary approach to inpatient and transitional care. Hospitalists may also become involved in hospital quality and safety initiatives that pertain to areas such as restraint use and fall prevention.
DEMENTIA KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate dementia from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate dementia.
Describe the causes of potentially reversible dementias or dementia-like conditions.
List indications, contraindications, and mechanisms of action of pharmacologic agents used to treat dementia.
Describe nonpharmacologic therapies to manage dementia symptoms.
Recognize the indications for specialty consultations.
Describe the complications of dementia in the hospitalized patient.
Discuss the multifaceted impact that dementia has on patients and their families.
Explain goals for hospital discharge including specific measures of clinical stability for safe care transition.
DEMENTIA SKILLS
Hospitalists should be able to:
Perform appropriate screening for dementia.
Develop active strategies to reduce development of delirium in patients with dementia in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected dementia in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Assess patients for potentially reversible causes of dementia or dementia-like conditions. Assess severity of cognitive impairment and perform a focused evaluation for the underlying etiology of dementia when appropriate.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with dementia.
Formulate and lead multidisciplinary teams to develop and implement care plans for patients with dementia.
Develop an appropriate pharmacologic plan to manage dementia.
Develop an appropriate nonpharmacologic plan to manage dementia.
Use a patient- and family-centered approach in the care of older inpatients.
Communicate with patients and families to explain the history and prognosis of dementia.
Use evidence-based methods and tools to assess patients’ medical decision-making capacity.
Defend patients’ right to autonomy when so qualified.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DEMENTIA ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with dementia that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of dementia and its causes.
Value a patient- and family-centered approach to educate and engage families and caregivers in the care of older inpatients.
Responsibly address and respect end-of-life care wishes for patients with advanced dementia.
DEMENTIA SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for poor outcomes related to dementia.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration withgeriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with dementia.
DELIRIUM
Delirium is defined as an acute, transient, global disorder of cognition. In two-thirds of cases, delirium occurs in patients with baseline vulnerability, including those with underlying dementia.1 Although up to 30% of older medical patients experience delirium during hospitalization, this condition is unrecognized in nearly two-thirds of cases.2-4 Patients with delirium experience an average increase in length of hospital stay of 8 days and mortality rates that are twice as high as those of patients without delirium.5,6 In addition, delirium is associated with high rates of functional and cognitive decline and skilled nursing facility placement after hospitalization. The cost of caring for patients with delirium has a marked impact on individual patients, families, and hospital systems. Hospitalists lead their institutions in the development of screening and prevention protocols for patients at risk for delirium, as well as in the promotion of safe treatment approaches. Hospitalists also develop strategies to operationalize cost-effective delirium prevention programs that improve outcomes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
DELIRIUM KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate delirium from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate delirium.
Describe the causes of delirium in the hospital setting including environmental and iatrogenic risk factors.
Identify medications known to precipitate delirium.
Recognize the indications for specialty consultations.
Describe methods for the prevention of delirium.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat delirium.
Describe nonpharmacologic therapies to manage delirium.
Describe the complications of delirium in the hospitalized patient.
Discuss the multifaceted impact that delirium has on patients and their families.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
DELIRIUM SKILLS
Hospitalists should be able to:
Predict a patient’s risk for the development of delirium on the basis of initial history and physical examination.
Perform appropriate screening for delirium.
Develop active strategies to reduce delirium in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected delirium in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Perform a focused evaluation for the underlying etiology of delirium and institute prompt treatment to lessen its severity.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with delirium.
Lead multidisciplinary teams to develop and implement care plans for patients with delirium.
Develop an appropriate pharmacologic plan to manage delirium.
Develop an appropriate nonpharmacologic plan to manage delirium.
Develop an appropriate management plan for patients with delirium in the postoperative setting.
Document an appropriate treatment plan to reduce mortality, limit the duration of delirium and the time required to control agitation, maintain adequate control of delirium, address complications, and manage cost of treatment.
Use a patient- and family-centered approach in the care of older inpatients.
Establish goals and boundaries of care with patients and their families.
Communicate with patients and families to explain the history and prognosis of delirium.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DELIRIUM ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with delirium that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of delirium and its causes.
Value a patient- and family-centered approach in the care of older inpatients.
DELIRIUM SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for delirium.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration with geriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with delirium.
DEMENTIA
Dementia is defined as a chronic, often progressive, decline in cognitive function, eventually limiting daily activities. Dementia is a common comorbidity in the hospitalized older patient. Alzheimer disease is the most prevalent form of dementia in older patients, and it accounts for up to 80% of cases.7,8 More than 5 million persons older than 65 years have Alzheimer disease in the United States.7,8 Patients with dementia are at increased risk for delirium, falls, and functional decline during hospitalization. Patients with baseline cognitive impairment have prolonged lengths of stay and complex needs after discharge. Agitation and behavioral symptoms of dementia can be exacerbated in the hospital setting and are often difficult to manage. Care of the patient with dementia requires that hospitalists engage in a multidisciplinary approach to inpatient and transitional care. Hospitalists may also become involved in hospital quality and safety initiatives that pertain to areas such as restraint use and fall prevention.
DEMENTIA KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate dementia from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate dementia.
Describe the causes of potentially reversible dementias or dementia-like conditions.
List indications, contraindications, and mechanisms of action of pharmacologic agents used to treat dementia.
Describe nonpharmacologic therapies to manage dementia symptoms.
Recognize the indications for specialty consultations.
Describe the complications of dementia in the hospitalized patient.
Discuss the multifaceted impact that dementia has on patients and their families.
Explain goals for hospital discharge including specific measures of clinical stability for safe care transition.
DEMENTIA SKILLS
Hospitalists should be able to:
Perform appropriate screening for dementia.
Develop active strategies to reduce development of delirium in patients with dementia in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected dementia in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Assess patients for potentially reversible causes of dementia or dementia-like conditions. Assess severity of cognitive impairment and perform a focused evaluation for the underlying etiology of dementia when appropriate.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with dementia.
Formulate and lead multidisciplinary teams to develop and implement care plans for patients with dementia.
Develop an appropriate pharmacologic plan to manage dementia.
Develop an appropriate nonpharmacologic plan to manage dementia.
Use a patient- and family-centered approach in the care of older inpatients.
Communicate with patients and families to explain the history and prognosis of dementia.
Use evidence-based methods and tools to assess patients’ medical decision-making capacity.
Defend patients’ right to autonomy when so qualified.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DEMENTIA ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with dementia that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of dementia and its causes.
Value a patient- and family-centered approach to educate and engage families and caregivers in the care of older inpatients.
Responsibly address and respect end-of-life care wishes for patients with advanced dementia.
DEMENTIA SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for poor outcomes related to dementia.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration withgeriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with dementia.
1. Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7-21.
2. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
3. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242.
4. Francis J. Delirium in older patients. J Am Geriatr Soc. 1992;40(8):829-838.
5. Cole MG, Primeau FJ. Prognosis of delirium in elderly hospital patients. CMAJ. 1993;149(1):41.
6. McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162(4):457-463.
7. Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. Available at: https://www.alz.org/downloads/Facts_Figures_2014.pdf. Accessed July 2015.
8. Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
1. Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7-21.
2. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
3. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242.
4. Francis J. Delirium in older patients. J Am Geriatr Soc. 1992;40(8):829-838.
5. Cole MG, Primeau FJ. Prognosis of delirium in elderly hospital patients. CMAJ. 1993;149(1):41.
6. McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162(4):457-463.
7. Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. Available at: https://www.alz.org/downloads/Facts_Figures_2014.pdf. Accessed July 2015.
8. Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
© 2017 Society of Hospital Medicine