User login
How has hospital medicine changed since you started?

HM19 attendees relay their perspectives on how the practice of hospital medicine has evolved over the course of their careers.

HM19 attendees relay their perspectives on how the practice of hospital medicine has evolved over the course of their careers.

HM19 attendees relay their perspectives on how the practice of hospital medicine has evolved over the course of their careers.
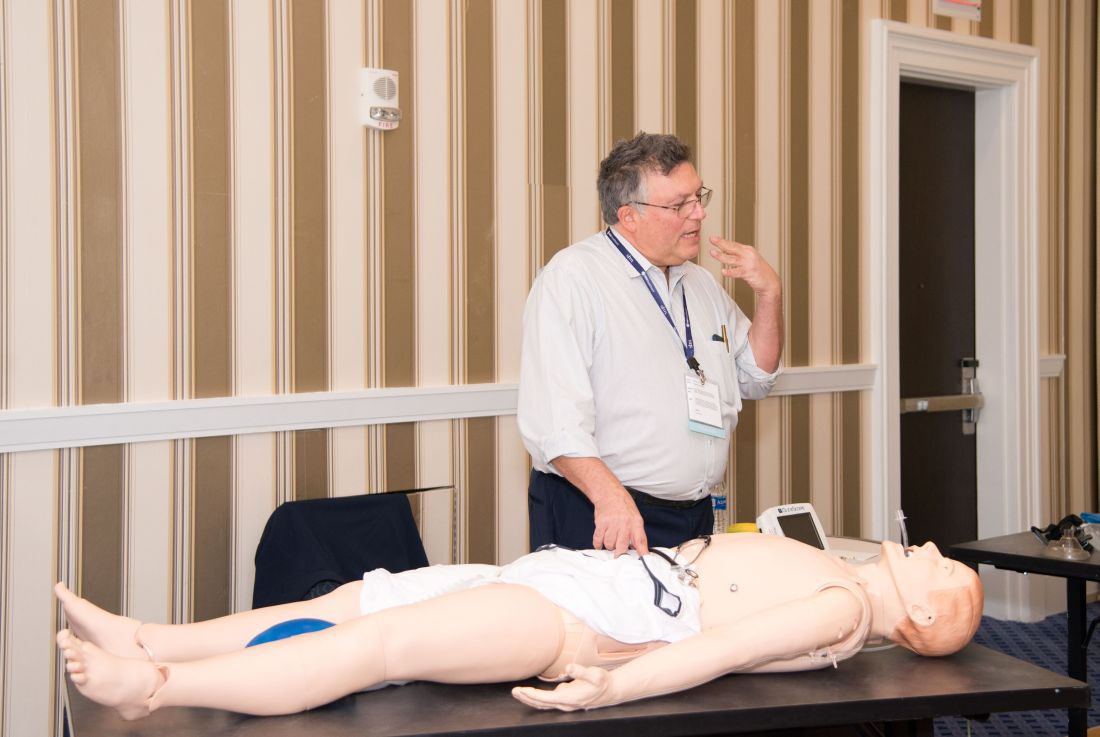
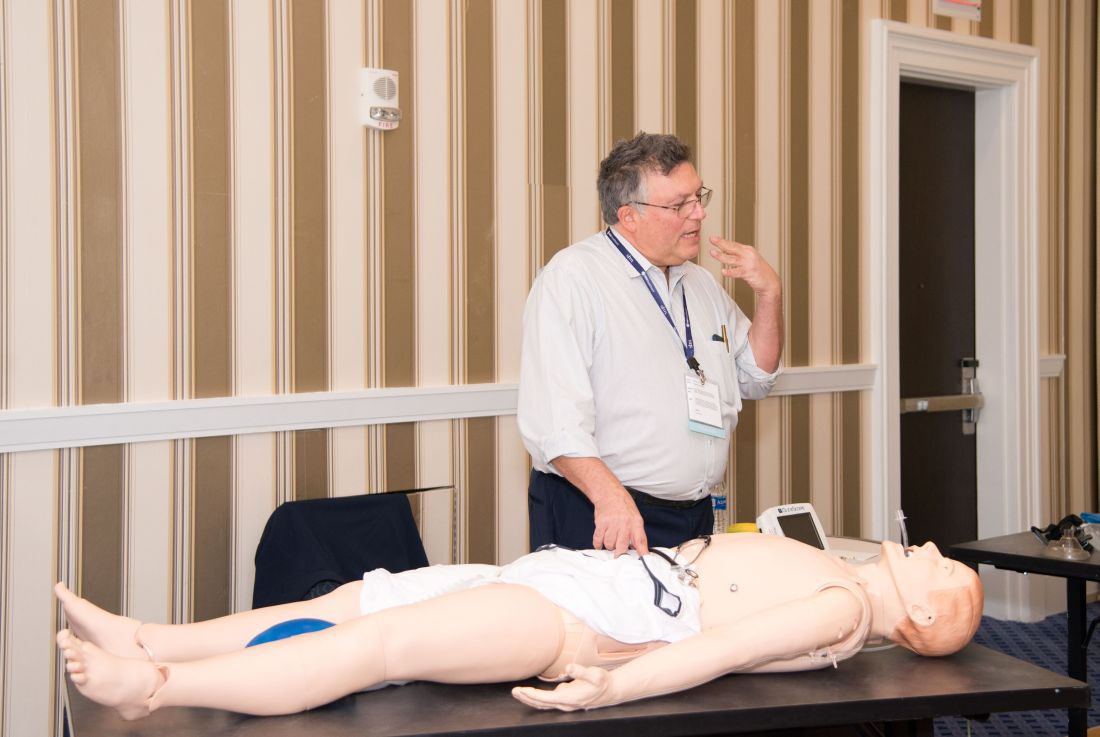
Hands-on critical care lessons provided at HM19
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
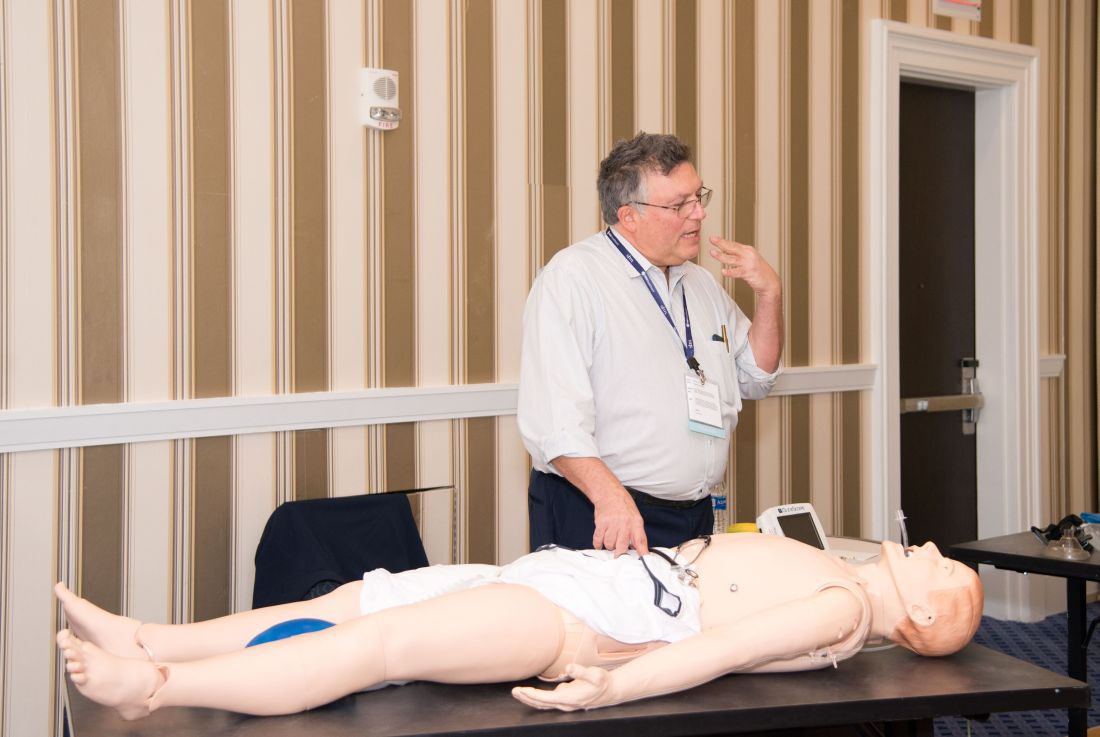
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
Planning for change in hospitalist practice management
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
Syncope session showcases latest research and guidance for practice
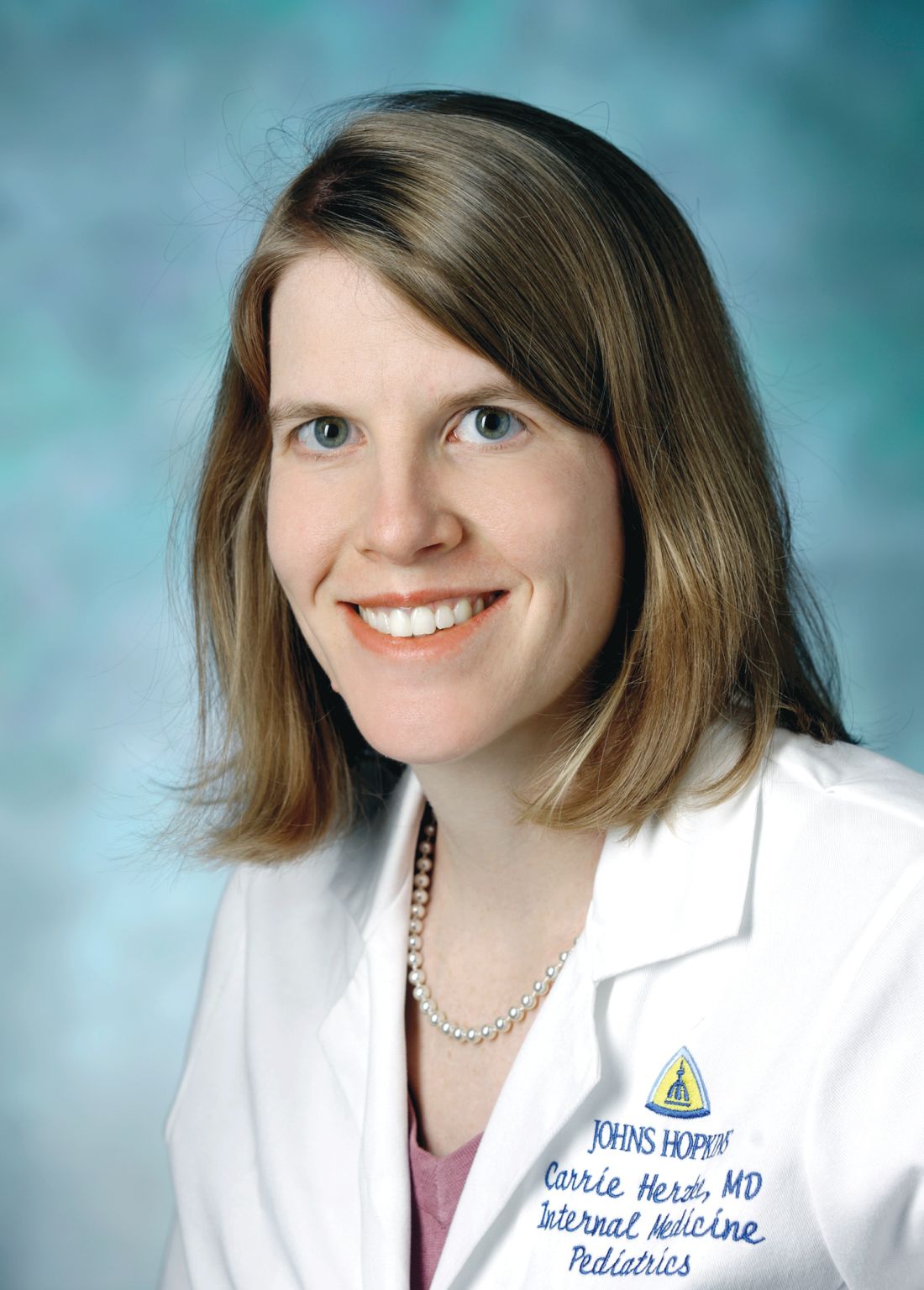
Syncope is a common problem, but an area in which practice likely varies by region and provider, according to Carrie Herzke, MD, SFHM, of Johns Hopkins University in Baltimore.
The variation in practice also suggests opportunities to safely cut costs, Dr. Herzke said in an interview.
Dr. Herzke will review the recent literature and summarize the current guidelines related to the treatment of syncope in her session, “SyncopE – Effective, Efficient and Economic Evaluations,” on Monday, March 25, at HM19.
“At the end of this session I am hopeful attendees will have a better understanding of the current guidelines, as well as which tests are most likely to be high value in the evaluation of syncope,” Dr. Herzke said. But before testing, clinicians should keep in mind that a history and physical examination are key components to evaluating syncope, she noted.
The European Society of Cardiology Guidelines for Syncope, published in 2018, feature several new concepts for evaluating and managing syncope in clinical settings and testing, including tilt testing, a greater role for prolonged ECG monitoring, use of video recording for suspected syncope, consideration of adenosine sensitive syncope, and consideration of neurological causes of syncope.
The ESC guidelines include using algorithms to determine the appropriate therapy for reflex syncope based on age, severity, and clinical forms. The guidelines also address diagnostic tests, monitoring in and out of the hospital, and treatment options including lifestyle changes and education as well as pharmacotherapy.
Dr. Herzke also will review the 2017 ACC/AHA/HRS Guideline for Patients With Syncope, published in 2017 in the journal Circulation. This guideline has an algorithm for initial evaluation of patients with syncope that includes a history, physical, and ECG. If the cause is known, patients should be assessed for risk and treated; syncope of unknown cause requires further evaluation, and the guideline presents recommendations for additional assessment through means including cardiac imaging, stress testing, blood testing, neurological testing, and tilt table testing.
“The selection of a given diagnostic test, after the initial history, physical examination, and baseline ECG, is a clinical decision based on the patient’s clinical presentation, risk stratification, and a clear understanding of diagnostic and prognostic value of any further testing,” according to the guideline authors.
The 2017 ACC/AHA/HRS Guideline for Patients With Syncope also provides recommendations for the management of cardiovascular conditions, including arrhythmic and structural conditions.
Dr. Herzke said she thinks that the topic of pulmonary embolism and syncope may prompt the liveliest discussion, and she will include several recent articles on this topic in her literature review.
“There has been some debate about how often PE is present in patients presenting after a syncopal episode,” she said. A recent study published in JAMA Internal Medicine found a prevalence of PE from 0.06% to 0.55% among all adults presenting to an ED with syncope and a prevalence of PE from 0.14% to 0.83%.
SyncopE – Effective, Efficient and Economic Evaluations
Monday 1:10 pm
Maryland BD/4-6
Syncope is a common problem, but an area in which practice likely varies by region and provider, according to Carrie Herzke, MD, SFHM, of Johns Hopkins University in Baltimore.
The variation in practice also suggests opportunities to safely cut costs, Dr. Herzke said in an interview.
Dr. Herzke will review the recent literature and summarize the current guidelines related to the treatment of syncope in her session, “SyncopE – Effective, Efficient and Economic Evaluations,” on Monday, March 25, at HM19.
“At the end of this session I am hopeful attendees will have a better understanding of the current guidelines, as well as which tests are most likely to be high value in the evaluation of syncope,” Dr. Herzke said. But before testing, clinicians should keep in mind that a history and physical examination are key components to evaluating syncope, she noted.
The European Society of Cardiology Guidelines for Syncope, published in 2018, feature several new concepts for evaluating and managing syncope in clinical settings and testing, including tilt testing, a greater role for prolonged ECG monitoring, use of video recording for suspected syncope, consideration of adenosine sensitive syncope, and consideration of neurological causes of syncope.
The ESC guidelines include using algorithms to determine the appropriate therapy for reflex syncope based on age, severity, and clinical forms. The guidelines also address diagnostic tests, monitoring in and out of the hospital, and treatment options including lifestyle changes and education as well as pharmacotherapy.
Dr. Herzke also will review the 2017 ACC/AHA/HRS Guideline for Patients With Syncope, published in 2017 in the journal Circulation. This guideline has an algorithm for initial evaluation of patients with syncope that includes a history, physical, and ECG. If the cause is known, patients should be assessed for risk and treated; syncope of unknown cause requires further evaluation, and the guideline presents recommendations for additional assessment through means including cardiac imaging, stress testing, blood testing, neurological testing, and tilt table testing.
“The selection of a given diagnostic test, after the initial history, physical examination, and baseline ECG, is a clinical decision based on the patient’s clinical presentation, risk stratification, and a clear understanding of diagnostic and prognostic value of any further testing,” according to the guideline authors.
The 2017 ACC/AHA/HRS Guideline for Patients With Syncope also provides recommendations for the management of cardiovascular conditions, including arrhythmic and structural conditions.
Dr. Herzke said she thinks that the topic of pulmonary embolism and syncope may prompt the liveliest discussion, and she will include several recent articles on this topic in her literature review.
“There has been some debate about how often PE is present in patients presenting after a syncopal episode,” she said. A recent study published in JAMA Internal Medicine found a prevalence of PE from 0.06% to 0.55% among all adults presenting to an ED with syncope and a prevalence of PE from 0.14% to 0.83%.
SyncopE – Effective, Efficient and Economic Evaluations
Monday 1:10 pm
Maryland BD/4-6
Syncope is a common problem, but an area in which practice likely varies by region and provider, according to Carrie Herzke, MD, SFHM, of Johns Hopkins University in Baltimore.
The variation in practice also suggests opportunities to safely cut costs, Dr. Herzke said in an interview.
Dr. Herzke will review the recent literature and summarize the current guidelines related to the treatment of syncope in her session, “SyncopE – Effective, Efficient and Economic Evaluations,” on Monday, March 25, at HM19.
“At the end of this session I am hopeful attendees will have a better understanding of the current guidelines, as well as which tests are most likely to be high value in the evaluation of syncope,” Dr. Herzke said. But before testing, clinicians should keep in mind that a history and physical examination are key components to evaluating syncope, she noted.
The European Society of Cardiology Guidelines for Syncope, published in 2018, feature several new concepts for evaluating and managing syncope in clinical settings and testing, including tilt testing, a greater role for prolonged ECG monitoring, use of video recording for suspected syncope, consideration of adenosine sensitive syncope, and consideration of neurological causes of syncope.
The ESC guidelines include using algorithms to determine the appropriate therapy for reflex syncope based on age, severity, and clinical forms. The guidelines also address diagnostic tests, monitoring in and out of the hospital, and treatment options including lifestyle changes and education as well as pharmacotherapy.
Dr. Herzke also will review the 2017 ACC/AHA/HRS Guideline for Patients With Syncope, published in 2017 in the journal Circulation. This guideline has an algorithm for initial evaluation of patients with syncope that includes a history, physical, and ECG. If the cause is known, patients should be assessed for risk and treated; syncope of unknown cause requires further evaluation, and the guideline presents recommendations for additional assessment through means including cardiac imaging, stress testing, blood testing, neurological testing, and tilt table testing.
“The selection of a given diagnostic test, after the initial history, physical examination, and baseline ECG, is a clinical decision based on the patient’s clinical presentation, risk stratification, and a clear understanding of diagnostic and prognostic value of any further testing,” according to the guideline authors.
The 2017 ACC/AHA/HRS Guideline for Patients With Syncope also provides recommendations for the management of cardiovascular conditions, including arrhythmic and structural conditions.
Dr. Herzke said she thinks that the topic of pulmonary embolism and syncope may prompt the liveliest discussion, and she will include several recent articles on this topic in her literature review.
“There has been some debate about how often PE is present in patients presenting after a syncopal episode,” she said. A recent study published in JAMA Internal Medicine found a prevalence of PE from 0.06% to 0.55% among all adults presenting to an ED with syncope and a prevalence of PE from 0.14% to 0.83%.
SyncopE – Effective, Efficient and Economic Evaluations
Monday 1:10 pm
Maryland BD/4-6
The power of policy at HM19
Mini-track features CMS insights
Due to the steadily growing interest of SHM members in health care policy and advocacy issues, the 2019 Annual Conference will include a mini-track dedicated to policy issues.
To be held on Monday, March 25th at HM19 in Orlando, the health care policy mini-track will update conference attendees on some of the Washington developments that affect hospitalists, said Josh Boswell, director of government relations at SHM.
“Many of the policy developments in D.C. are directly impacting our members’ practices,” he said. “A couple of years ago, it was decided to add a specific track at the annual conference to cover some of these policy issues, and we’ve generally had positive feedback on the sessions.”
This year, the mini-track will consist of two separate sessions, held back to back. “Both sessions are designed to give attendees an entrée into health policy and explain developments that are happening right now in Washington that impact their practice,” said Joshua Lapps, government relations manager at SHM.
The first session – “CMS Policy Update: An Overview of Meaningful Measures and the Quality Payment Program” – will take place from 2:00 to 3:30 p.m., and will feature Reena Duseja, MD, MS, the acting director for Quality Measurement and Value-Based Incentives Group in the Centers for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services. Dr. Duseja oversees the development of measures and analyses for a variety of CMS quality reporting and value-based purchasing programs. She is also an emergency medicine physician and was an associate professor at the University of California, San Francisco, in the department of emergency medicine, where she led quality improvement activities.
“The session with Dr. Duseja will be an inside look into the approach that CMS is taking for quality measurement and pay-for-performance programs, specifically looking at the quality payment program which came out of the Medicare Access and Chip Reauthorization Act,” Mr. Lapps said. “It will be a high-level discussion about how the programs affect hospitalists, and how hospitalists participate in the programs. It’s also a chance for attendees to hear some of the thinking inside CMS.”
Dr. Duseja is also hoping to get feedback from HM19 attendees. “She wants the session to be educational for our members, as well as an opportunity for her to learn from hospitalists,” Mr. Lapps said.
According to Dr. Duseja, her presentation will provide attendees with an overview of the Quality Payment Program under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), specifically highlighting policy changes from 2018 to 2019 to the Merit-based Incentive Payment System (MIPS) and Meaningful Measures Initiative. Attendees will learn more about CMS’s approach to quality and quality measurement, as well as the future of quality reporting programs.
Following Dr. Duseja’s presentation, the second mini-track session will take place from 3:40 to 4:25 p.m. It will focus more intently on the processes around health care policy making.
“We heard from our members who attended this mini-track at the past two annual conferences that they would like us to explain how policy making works: the play-by-play in D.C. on how we get to where we are,” Mr. Boswell said.
The second session will feature a presentation by Jennifer Bell, founding partner at Chamber Hill Strategies, who represents SHM in Washington. “Jennifer will be discussing how Washington works, the policy process and the pressure points at which SHM and its members can exert influence,” Mr. Lapps said.
Attendees can expect to learn a lot from either session, Mr. Lapps said. “Attendees will learn about the basic contours of the Quality Payment Program that Medicare oversees, and some of the specific new elements of that program this year that were designed with hospitalists in mind. For example, Dr. Duseja will be talking about a facility-based reporting option under the Merit-Based Incentive Payment System. I think our members should gain a concrete understanding of some of the new directions that CMS is heading this year. Overall, they’ll have a better sense of the vision behind quality measures and quality measurement. This is a really exciting opportunity to hear from someone who is both a clinician and works on policy at CMS.”
The policy mini-track offers hospitalists a chance to get a look “behind the curtain” at policy making from someone who is helping to write the rules.
“Attendees will gain insight on where they fit in these programs – and also have the opportunity to tell Dr. Duseja if they don’t feel these programs are a good fit for them,” Mr. Boswell said. “Oftentimes these programs are not structured ideally for hospitalists. So, hearing directly from hospitalists who are experiencing problems would be extraordinarily helpful to a CMS official. I think attendees should view the policy track not only as an opportunity to learn from CMS, but as an opportunity to educate CMS about our issues.”
Mini-track features CMS insights
Mini-track features CMS insights
Due to the steadily growing interest of SHM members in health care policy and advocacy issues, the 2019 Annual Conference will include a mini-track dedicated to policy issues.
To be held on Monday, March 25th at HM19 in Orlando, the health care policy mini-track will update conference attendees on some of the Washington developments that affect hospitalists, said Josh Boswell, director of government relations at SHM.
“Many of the policy developments in D.C. are directly impacting our members’ practices,” he said. “A couple of years ago, it was decided to add a specific track at the annual conference to cover some of these policy issues, and we’ve generally had positive feedback on the sessions.”
This year, the mini-track will consist of two separate sessions, held back to back. “Both sessions are designed to give attendees an entrée into health policy and explain developments that are happening right now in Washington that impact their practice,” said Joshua Lapps, government relations manager at SHM.
The first session – “CMS Policy Update: An Overview of Meaningful Measures and the Quality Payment Program” – will take place from 2:00 to 3:30 p.m., and will feature Reena Duseja, MD, MS, the acting director for Quality Measurement and Value-Based Incentives Group in the Centers for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services. Dr. Duseja oversees the development of measures and analyses for a variety of CMS quality reporting and value-based purchasing programs. She is also an emergency medicine physician and was an associate professor at the University of California, San Francisco, in the department of emergency medicine, where she led quality improvement activities.
“The session with Dr. Duseja will be an inside look into the approach that CMS is taking for quality measurement and pay-for-performance programs, specifically looking at the quality payment program which came out of the Medicare Access and Chip Reauthorization Act,” Mr. Lapps said. “It will be a high-level discussion about how the programs affect hospitalists, and how hospitalists participate in the programs. It’s also a chance for attendees to hear some of the thinking inside CMS.”
Dr. Duseja is also hoping to get feedback from HM19 attendees. “She wants the session to be educational for our members, as well as an opportunity for her to learn from hospitalists,” Mr. Lapps said.
According to Dr. Duseja, her presentation will provide attendees with an overview of the Quality Payment Program under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), specifically highlighting policy changes from 2018 to 2019 to the Merit-based Incentive Payment System (MIPS) and Meaningful Measures Initiative. Attendees will learn more about CMS’s approach to quality and quality measurement, as well as the future of quality reporting programs.
Following Dr. Duseja’s presentation, the second mini-track session will take place from 3:40 to 4:25 p.m. It will focus more intently on the processes around health care policy making.
“We heard from our members who attended this mini-track at the past two annual conferences that they would like us to explain how policy making works: the play-by-play in D.C. on how we get to where we are,” Mr. Boswell said.
The second session will feature a presentation by Jennifer Bell, founding partner at Chamber Hill Strategies, who represents SHM in Washington. “Jennifer will be discussing how Washington works, the policy process and the pressure points at which SHM and its members can exert influence,” Mr. Lapps said.
Attendees can expect to learn a lot from either session, Mr. Lapps said. “Attendees will learn about the basic contours of the Quality Payment Program that Medicare oversees, and some of the specific new elements of that program this year that were designed with hospitalists in mind. For example, Dr. Duseja will be talking about a facility-based reporting option under the Merit-Based Incentive Payment System. I think our members should gain a concrete understanding of some of the new directions that CMS is heading this year. Overall, they’ll have a better sense of the vision behind quality measures and quality measurement. This is a really exciting opportunity to hear from someone who is both a clinician and works on policy at CMS.”
The policy mini-track offers hospitalists a chance to get a look “behind the curtain” at policy making from someone who is helping to write the rules.
“Attendees will gain insight on where they fit in these programs – and also have the opportunity to tell Dr. Duseja if they don’t feel these programs are a good fit for them,” Mr. Boswell said. “Oftentimes these programs are not structured ideally for hospitalists. So, hearing directly from hospitalists who are experiencing problems would be extraordinarily helpful to a CMS official. I think attendees should view the policy track not only as an opportunity to learn from CMS, but as an opportunity to educate CMS about our issues.”
Due to the steadily growing interest of SHM members in health care policy and advocacy issues, the 2019 Annual Conference will include a mini-track dedicated to policy issues.
To be held on Monday, March 25th at HM19 in Orlando, the health care policy mini-track will update conference attendees on some of the Washington developments that affect hospitalists, said Josh Boswell, director of government relations at SHM.
“Many of the policy developments in D.C. are directly impacting our members’ practices,” he said. “A couple of years ago, it was decided to add a specific track at the annual conference to cover some of these policy issues, and we’ve generally had positive feedback on the sessions.”
This year, the mini-track will consist of two separate sessions, held back to back. “Both sessions are designed to give attendees an entrée into health policy and explain developments that are happening right now in Washington that impact their practice,” said Joshua Lapps, government relations manager at SHM.
The first session – “CMS Policy Update: An Overview of Meaningful Measures and the Quality Payment Program” – will take place from 2:00 to 3:30 p.m., and will feature Reena Duseja, MD, MS, the acting director for Quality Measurement and Value-Based Incentives Group in the Centers for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services. Dr. Duseja oversees the development of measures and analyses for a variety of CMS quality reporting and value-based purchasing programs. She is also an emergency medicine physician and was an associate professor at the University of California, San Francisco, in the department of emergency medicine, where she led quality improvement activities.
“The session with Dr. Duseja will be an inside look into the approach that CMS is taking for quality measurement and pay-for-performance programs, specifically looking at the quality payment program which came out of the Medicare Access and Chip Reauthorization Act,” Mr. Lapps said. “It will be a high-level discussion about how the programs affect hospitalists, and how hospitalists participate in the programs. It’s also a chance for attendees to hear some of the thinking inside CMS.”
Dr. Duseja is also hoping to get feedback from HM19 attendees. “She wants the session to be educational for our members, as well as an opportunity for her to learn from hospitalists,” Mr. Lapps said.
According to Dr. Duseja, her presentation will provide attendees with an overview of the Quality Payment Program under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), specifically highlighting policy changes from 2018 to 2019 to the Merit-based Incentive Payment System (MIPS) and Meaningful Measures Initiative. Attendees will learn more about CMS’s approach to quality and quality measurement, as well as the future of quality reporting programs.
Following Dr. Duseja’s presentation, the second mini-track session will take place from 3:40 to 4:25 p.m. It will focus more intently on the processes around health care policy making.
“We heard from our members who attended this mini-track at the past two annual conferences that they would like us to explain how policy making works: the play-by-play in D.C. on how we get to where we are,” Mr. Boswell said.
The second session will feature a presentation by Jennifer Bell, founding partner at Chamber Hill Strategies, who represents SHM in Washington. “Jennifer will be discussing how Washington works, the policy process and the pressure points at which SHM and its members can exert influence,” Mr. Lapps said.
Attendees can expect to learn a lot from either session, Mr. Lapps said. “Attendees will learn about the basic contours of the Quality Payment Program that Medicare oversees, and some of the specific new elements of that program this year that were designed with hospitalists in mind. For example, Dr. Duseja will be talking about a facility-based reporting option under the Merit-Based Incentive Payment System. I think our members should gain a concrete understanding of some of the new directions that CMS is heading this year. Overall, they’ll have a better sense of the vision behind quality measures and quality measurement. This is a really exciting opportunity to hear from someone who is both a clinician and works on policy at CMS.”
The policy mini-track offers hospitalists a chance to get a look “behind the curtain” at policy making from someone who is helping to write the rules.
“Attendees will gain insight on where they fit in these programs – and also have the opportunity to tell Dr. Duseja if they don’t feel these programs are a good fit for them,” Mr. Boswell said. “Oftentimes these programs are not structured ideally for hospitalists. So, hearing directly from hospitalists who are experiencing problems would be extraordinarily helpful to a CMS official. I think attendees should view the policy track not only as an opportunity to learn from CMS, but as an opportunity to educate CMS about our issues.”
Learning from the history of hospitals
Storytelling can inform medical practice
Every year the Society of Hospital Medicine’s Annual Conference Committee examines prior attendee surveys, reviews the content presented the preceding year, and asks itself what new areas of learning are needed by hospitalists, said Dustin Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University School of Medicine in Atlanta, and HM19 course director.
“The conference’s schedule-at-a-glance of content can be overwhelming, so we have tried to use distinct educational tracks to provide focus and clarity for conference attendees,” he said. “Every year there are a few areas where questions often come up about complex clinical situations where established medical guidelines aren’t much help.”
As a result, for HM19 an educational mini-track called “Between the Guidelines” was developed to gather up several of these areas of clinical complexity where what’s available in established clinical practice guidelines doesn’t offer clear answers, Dr. Smith said. These include controversies around antithrombotic therapy in patients with major bleeds, and a debate on controversial aspects of guidelines to direct inpatient care.
Another planned session, “The History of Hospitals via Arts and Stories,” fits nicely into this mini-track, Dr. Smith noted.
“It’s a history lesson you can’t glean from medical guidelines, which maybe points us toward what to incorporate and what not to repeat from across the history of hospitals,” he said. “That could help us better appreciate the work hospitalists are doing today and into the future.”
Jordan Messler, MD, a hospitalist with the Morton Plant Hospitalist group in Clearwater, Fla., will lead the session and thinks that modern physicians can learn a lot from both the history of medicine and the evolution of hospitals, starting with the ancient Greek physician, Galen (129-200 AD), who directed the celebrated Asclepeion or hospital in Pergamon (present-day Bergama, Turkey). Dr. Messler said this ancient hospital’s treatment of disease also addressed the senses, the emotions, and the spirit – an early prototype for whole-person care – with an emphasis on self-therapy through rest, relaxation, exercise, and the promotion of healthy lifestyles.1
A different perspective on hospitals
“People used to travel to Pergamon for healing at the Asclepeion, next to the amphitheater, where plays and music were presented, and to be outdoors in the natural elements. Now we’re seeing hospitals being built with healing gardens, and a new emphasis on how artwork and music and environmental design can assist in healing,” Dr. Messler said.
Dr. Messler explained that his “History of Hospitals” presentation will also survey the advent of more recent hospitals in France in the 18th century, pioneering work done at Johns Hopkins Hospital in Baltimore and Bellevue Hospital in New York, and the influence on the modern hospital of nursing pioneer Florence Nightingale (1820-1910). Dr. Messler said she helped improve hospitals in her day, which still influences their modern design, and fundamentally changed the role of nursing in hospitals, introducing professional training standards for nurses.
He also noted that the portico of the beautiful 15th century Hospital of the Innocents in Florence, Italy, the first organic creation of Filippo Brunelleschi (1377-1446), marks the birth of Renaissance architecture in Florence. The Hospital of Santa Maria Nuova, founded in 1288, is the oldest hospital still active in Florence.
Part of the goal for this new annual conference session is to take a break from more clinically focused presentations, and to think about the hospital from a different perspective, Dr. Messler said. His session will emphasize the power of stories and storytelling to inform and inspire medical practice.
“This is not something that can be applied clinically the next day, but lessons from the past can inform the design of hospitals and how we manage patients,” he said. “We need to ask ourselves, ‘How can we analyze hospital history to inform what we do today?’ ”
References
“Asclepeion.” Wikipedia. Accessed Jan. 28, 2019: https://en.wikipedia.org/wiki/Asclepeion.
Storytelling can inform medical practice
Storytelling can inform medical practice
Every year the Society of Hospital Medicine’s Annual Conference Committee examines prior attendee surveys, reviews the content presented the preceding year, and asks itself what new areas of learning are needed by hospitalists, said Dustin Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University School of Medicine in Atlanta, and HM19 course director.
“The conference’s schedule-at-a-glance of content can be overwhelming, so we have tried to use distinct educational tracks to provide focus and clarity for conference attendees,” he said. “Every year there are a few areas where questions often come up about complex clinical situations where established medical guidelines aren’t much help.”
As a result, for HM19 an educational mini-track called “Between the Guidelines” was developed to gather up several of these areas of clinical complexity where what’s available in established clinical practice guidelines doesn’t offer clear answers, Dr. Smith said. These include controversies around antithrombotic therapy in patients with major bleeds, and a debate on controversial aspects of guidelines to direct inpatient care.
Another planned session, “The History of Hospitals via Arts and Stories,” fits nicely into this mini-track, Dr. Smith noted.
“It’s a history lesson you can’t glean from medical guidelines, which maybe points us toward what to incorporate and what not to repeat from across the history of hospitals,” he said. “That could help us better appreciate the work hospitalists are doing today and into the future.”
Jordan Messler, MD, a hospitalist with the Morton Plant Hospitalist group in Clearwater, Fla., will lead the session and thinks that modern physicians can learn a lot from both the history of medicine and the evolution of hospitals, starting with the ancient Greek physician, Galen (129-200 AD), who directed the celebrated Asclepeion or hospital in Pergamon (present-day Bergama, Turkey). Dr. Messler said this ancient hospital’s treatment of disease also addressed the senses, the emotions, and the spirit – an early prototype for whole-person care – with an emphasis on self-therapy through rest, relaxation, exercise, and the promotion of healthy lifestyles.1
A different perspective on hospitals
“People used to travel to Pergamon for healing at the Asclepeion, next to the amphitheater, where plays and music were presented, and to be outdoors in the natural elements. Now we’re seeing hospitals being built with healing gardens, and a new emphasis on how artwork and music and environmental design can assist in healing,” Dr. Messler said.
Dr. Messler explained that his “History of Hospitals” presentation will also survey the advent of more recent hospitals in France in the 18th century, pioneering work done at Johns Hopkins Hospital in Baltimore and Bellevue Hospital in New York, and the influence on the modern hospital of nursing pioneer Florence Nightingale (1820-1910). Dr. Messler said she helped improve hospitals in her day, which still influences their modern design, and fundamentally changed the role of nursing in hospitals, introducing professional training standards for nurses.
He also noted that the portico of the beautiful 15th century Hospital of the Innocents in Florence, Italy, the first organic creation of Filippo Brunelleschi (1377-1446), marks the birth of Renaissance architecture in Florence. The Hospital of Santa Maria Nuova, founded in 1288, is the oldest hospital still active in Florence.
Part of the goal for this new annual conference session is to take a break from more clinically focused presentations, and to think about the hospital from a different perspective, Dr. Messler said. His session will emphasize the power of stories and storytelling to inform and inspire medical practice.
“This is not something that can be applied clinically the next day, but lessons from the past can inform the design of hospitals and how we manage patients,” he said. “We need to ask ourselves, ‘How can we analyze hospital history to inform what we do today?’ ”
References
“Asclepeion.” Wikipedia. Accessed Jan. 28, 2019: https://en.wikipedia.org/wiki/Asclepeion.
Every year the Society of Hospital Medicine’s Annual Conference Committee examines prior attendee surveys, reviews the content presented the preceding year, and asks itself what new areas of learning are needed by hospitalists, said Dustin Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University School of Medicine in Atlanta, and HM19 course director.
“The conference’s schedule-at-a-glance of content can be overwhelming, so we have tried to use distinct educational tracks to provide focus and clarity for conference attendees,” he said. “Every year there are a few areas where questions often come up about complex clinical situations where established medical guidelines aren’t much help.”
As a result, for HM19 an educational mini-track called “Between the Guidelines” was developed to gather up several of these areas of clinical complexity where what’s available in established clinical practice guidelines doesn’t offer clear answers, Dr. Smith said. These include controversies around antithrombotic therapy in patients with major bleeds, and a debate on controversial aspects of guidelines to direct inpatient care.
Another planned session, “The History of Hospitals via Arts and Stories,” fits nicely into this mini-track, Dr. Smith noted.
“It’s a history lesson you can’t glean from medical guidelines, which maybe points us toward what to incorporate and what not to repeat from across the history of hospitals,” he said. “That could help us better appreciate the work hospitalists are doing today and into the future.”
Jordan Messler, MD, a hospitalist with the Morton Plant Hospitalist group in Clearwater, Fla., will lead the session and thinks that modern physicians can learn a lot from both the history of medicine and the evolution of hospitals, starting with the ancient Greek physician, Galen (129-200 AD), who directed the celebrated Asclepeion or hospital in Pergamon (present-day Bergama, Turkey). Dr. Messler said this ancient hospital’s treatment of disease also addressed the senses, the emotions, and the spirit – an early prototype for whole-person care – with an emphasis on self-therapy through rest, relaxation, exercise, and the promotion of healthy lifestyles.1
A different perspective on hospitals
“People used to travel to Pergamon for healing at the Asclepeion, next to the amphitheater, where plays and music were presented, and to be outdoors in the natural elements. Now we’re seeing hospitals being built with healing gardens, and a new emphasis on how artwork and music and environmental design can assist in healing,” Dr. Messler said.
Dr. Messler explained that his “History of Hospitals” presentation will also survey the advent of more recent hospitals in France in the 18th century, pioneering work done at Johns Hopkins Hospital in Baltimore and Bellevue Hospital in New York, and the influence on the modern hospital of nursing pioneer Florence Nightingale (1820-1910). Dr. Messler said she helped improve hospitals in her day, which still influences their modern design, and fundamentally changed the role of nursing in hospitals, introducing professional training standards for nurses.
He also noted that the portico of the beautiful 15th century Hospital of the Innocents in Florence, Italy, the first organic creation of Filippo Brunelleschi (1377-1446), marks the birth of Renaissance architecture in Florence. The Hospital of Santa Maria Nuova, founded in 1288, is the oldest hospital still active in Florence.
Part of the goal for this new annual conference session is to take a break from more clinically focused presentations, and to think about the hospital from a different perspective, Dr. Messler said. His session will emphasize the power of stories and storytelling to inform and inspire medical practice.
“This is not something that can be applied clinically the next day, but lessons from the past can inform the design of hospitals and how we manage patients,” he said. “We need to ask ourselves, ‘How can we analyze hospital history to inform what we do today?’ ”
References
“Asclepeion.” Wikipedia. Accessed Jan. 28, 2019: https://en.wikipedia.org/wiki/Asclepeion.
Heart failure remains a common, costly concern
Heart failure remains one of the deadliest chronic medical conditions, with 5-year mortality rates approaching 50%, and is the most common diagnosis for adults aged 65 years and older who are admitted to the hospital, according to Albert J. Hicks III, MD.
Dr. Hicks, a cardiologist at Baylor Scott & White Health in Temple, Tex., will discuss the latest challenges and hottest topics surrounding heart failure in the “Updates in Heart Failure” session on Monday, at HM19.
The growth of an aging population in the United States further emphasizes the importance of heart failure as a topic of interest to clinicians, Dr. Hicks said in an interview. He noted that heart failure is the highest medical expenditure for Medicare, and estimates suggest the condition will cost the U.S. health care system $30 billion by the year 2030, he said. With these numbers in mind, the timing of referring patients to an advanced heart failure team is a key issue.
But the timing of referral for advanced care is just one of the hot topics on the agenda for the “Updates in Heart Failure” session, Dr. Hicks said. Other topics include heart failure epidemiology (incidence, prevalence, morbidity, mortality, and disparities); economics of heart failure (burden of care on the U.S. health care system); heart failure hospitalizations and readmissions (risk factors, comorbidities, patient compliance issues); pathophysiology (why heart failure is so deadly); signs and symptoms of heart failure (how to recognize them); treatment of stage C heart failure, with a review of old and new drugs and devices; and treatment of stage D heart failure, including palliative care, mechanical circulatory support, and heart transplantation.
Dr. Hicks’ primary goal for the session is to “increase awareness of the high mortality associated with a heart failure diagnosis,” he said. He also hopes to educate hospitalists about the latest medications, devices, and resources for heart failure patients and to give them the tools and knowledge to help reduce morbidity and mortality in their heart failure patients.
Session attendees also will benefit from Dr. Hicks’ practical advice on identifying warning signs that indicate a heart failure patient may need a medical assist device or a heart transplant and on encouraging early referral of heart failure patients to advanced heart failure specialists before irreversible end-organ damage occurs.
Dr. Hicks hypothesized that the high mortality associated with a heart failure diagnosis, hospital readmission, and late referral will generate the liveliest discussion because issues of costs and resources continue to evolve.
His take-home message: “Early recognition and referral of heart failure patients to a heart failure cardiologist can improve patient costs, morbidity, and survival.
Dr. Hicks had no relevant financial conflicts to disclose.
Updates in Heart Failure
Monday, 2:00-2:40 p.m.
Woodrow Wilson
Heart failure remains one of the deadliest chronic medical conditions, with 5-year mortality rates approaching 50%, and is the most common diagnosis for adults aged 65 years and older who are admitted to the hospital, according to Albert J. Hicks III, MD.
Dr. Hicks, a cardiologist at Baylor Scott & White Health in Temple, Tex., will discuss the latest challenges and hottest topics surrounding heart failure in the “Updates in Heart Failure” session on Monday, at HM19.
The growth of an aging population in the United States further emphasizes the importance of heart failure as a topic of interest to clinicians, Dr. Hicks said in an interview. He noted that heart failure is the highest medical expenditure for Medicare, and estimates suggest the condition will cost the U.S. health care system $30 billion by the year 2030, he said. With these numbers in mind, the timing of referring patients to an advanced heart failure team is a key issue.
But the timing of referral for advanced care is just one of the hot topics on the agenda for the “Updates in Heart Failure” session, Dr. Hicks said. Other topics include heart failure epidemiology (incidence, prevalence, morbidity, mortality, and disparities); economics of heart failure (burden of care on the U.S. health care system); heart failure hospitalizations and readmissions (risk factors, comorbidities, patient compliance issues); pathophysiology (why heart failure is so deadly); signs and symptoms of heart failure (how to recognize them); treatment of stage C heart failure, with a review of old and new drugs and devices; and treatment of stage D heart failure, including palliative care, mechanical circulatory support, and heart transplantation.
Dr. Hicks’ primary goal for the session is to “increase awareness of the high mortality associated with a heart failure diagnosis,” he said. He also hopes to educate hospitalists about the latest medications, devices, and resources for heart failure patients and to give them the tools and knowledge to help reduce morbidity and mortality in their heart failure patients.
Session attendees also will benefit from Dr. Hicks’ practical advice on identifying warning signs that indicate a heart failure patient may need a medical assist device or a heart transplant and on encouraging early referral of heart failure patients to advanced heart failure specialists before irreversible end-organ damage occurs.
Dr. Hicks hypothesized that the high mortality associated with a heart failure diagnosis, hospital readmission, and late referral will generate the liveliest discussion because issues of costs and resources continue to evolve.
His take-home message: “Early recognition and referral of heart failure patients to a heart failure cardiologist can improve patient costs, morbidity, and survival.
Dr. Hicks had no relevant financial conflicts to disclose.
Updates in Heart Failure
Monday, 2:00-2:40 p.m.
Woodrow Wilson
Heart failure remains one of the deadliest chronic medical conditions, with 5-year mortality rates approaching 50%, and is the most common diagnosis for adults aged 65 years and older who are admitted to the hospital, according to Albert J. Hicks III, MD.
Dr. Hicks, a cardiologist at Baylor Scott & White Health in Temple, Tex., will discuss the latest challenges and hottest topics surrounding heart failure in the “Updates in Heart Failure” session on Monday, at HM19.
The growth of an aging population in the United States further emphasizes the importance of heart failure as a topic of interest to clinicians, Dr. Hicks said in an interview. He noted that heart failure is the highest medical expenditure for Medicare, and estimates suggest the condition will cost the U.S. health care system $30 billion by the year 2030, he said. With these numbers in mind, the timing of referring patients to an advanced heart failure team is a key issue.
But the timing of referral for advanced care is just one of the hot topics on the agenda for the “Updates in Heart Failure” session, Dr. Hicks said. Other topics include heart failure epidemiology (incidence, prevalence, morbidity, mortality, and disparities); economics of heart failure (burden of care on the U.S. health care system); heart failure hospitalizations and readmissions (risk factors, comorbidities, patient compliance issues); pathophysiology (why heart failure is so deadly); signs and symptoms of heart failure (how to recognize them); treatment of stage C heart failure, with a review of old and new drugs and devices; and treatment of stage D heart failure, including palliative care, mechanical circulatory support, and heart transplantation.
Dr. Hicks’ primary goal for the session is to “increase awareness of the high mortality associated with a heart failure diagnosis,” he said. He also hopes to educate hospitalists about the latest medications, devices, and resources for heart failure patients and to give them the tools and knowledge to help reduce morbidity and mortality in their heart failure patients.
Session attendees also will benefit from Dr. Hicks’ practical advice on identifying warning signs that indicate a heart failure patient may need a medical assist device or a heart transplant and on encouraging early referral of heart failure patients to advanced heart failure specialists before irreversible end-organ damage occurs.
Dr. Hicks hypothesized that the high mortality associated with a heart failure diagnosis, hospital readmission, and late referral will generate the liveliest discussion because issues of costs and resources continue to evolve.
His take-home message: “Early recognition and referral of heart failure patients to a heart failure cardiologist can improve patient costs, morbidity, and survival.
Dr. Hicks had no relevant financial conflicts to disclose.
Updates in Heart Failure
Monday, 2:00-2:40 p.m.
Woodrow Wilson
Developing clinical mastery at HM19
Boosting your bedside diagnostic skills
A new three-session minitrack devoted to the clinical mastery of diagnostic and treatment skills at the hospitalized patient’s bedside should be a highlight of the Society of Hospital Medicine’s 2019 annual conference.
The “Clinical Mastery” track is designed to help hospitalists enhance their skills in making expert diagnoses at the bedside, said Dustin T. Smith, MD, SFHM, course director for HM19, and associate professor of medicine at Emory University, Atlanta. “We feel that all of the didactic sessions offered at HM19 are highly useful for hospitalists, but there is growing interest in having sessions devoted to learning clinical pearls that can aid in practicing medicine and acquiring the skill set of a master clinician.”
The three clinical mastery sessions at HM19 will address neurologic symptoms, ECG interpretation, and the role of point-of-care ultrasound (POCUS), currently a hot topic in hospital medicine. Recent advances in ultrasound technology have resulted in probes that can cost as little as $2,000, fit inside a lab coat pocket, and be read from a smartphone – making ultrasound far easier to bring to the bedside of hospitalized patients, said Ria Dancel, MD, FHM, associate professor of internal medicine and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Dancel will copresent the POCUS clinical mastery track at HM19. “Our focus will be on how POCUS and the physical exam relate to each other. These are not competing technologies but complementary, reflecting the evolution in bedside medicine. Because these new devices will soon be in the pockets of your colleagues, residents, physician assistants, and others, you should at least have the knowledge and vocabulary to communicate with them,” she said.
POCUS is a new technology that is not yet in wide use at the hospital bedside, but clearly a wave is building, said Dr. Dancel’s copresenter, Michael Janjigian, MD, associate professor in the department of medicine at NYU Langone Health in New York City.
“We’re at the inflection point where the cost of the machine and the availability of training means that hospitals need to decide if it’s time to embrace it,” he said. Hospitalists may also consider petitioning their hospital’s leadership to offer the machines and training.
“Hospitalists’ competencies and strengths lie primarily in making diagnoses,” Dr. Janjigian said. “We like to think of ourselves as master diagnosticians. Our session at HM19 will explore the strengths and weaknesses of both the physical exam and POCUS, presenting clinical scenarios common to hospital medicine. This course is designed for those who have never picked up an ultrasound probe and want to better understand why they should, and for those who want a better sense of how they might integrate it into their practice.”
While radiology and cardiology have been using ultrasound for decades, internists are finding uses at the bedside to speed diagnosis or focus their next diagnostic steps, Dr. Dancel noted. For certain diagnoses, the physical exam is still the tool of choice. But when looking for fluid around the heart or ascites buildup in the abdomen or when looking at the heart itself, she said, there is no better tool at the bedside than ultrasound.
In January 2019, the SHM issued a position statement on POCUS1, which is intended to inform hospitalists about the technology and its uses, encourage them to be more integrally involved in decision making processes surrounding POCUS program management for their hospitals, and promote development of standards for hospitalists in POCUS training and assessment. The SHM has also developed a pathway to teach the use of ultrasound, the Point-of-Care Ultrasound Certificate of Completion.
In order to qualify, clinicians complete online training modules, attend two live learning courses, compile a portfolio of ultrasound video clips on the job that are reviewed by a panel of experts, and then pass a final exam. The exam will be offered at HM19 for clinicians who have completed preliminary work for this new certificate – as well as precourses devoted to ultrasound and other procedures – and another workshop on POCUS.
Earning the POCUS certificate of completion requires a lot of effort, Dr. Dancel acknowledged. “It is a big commitment, and we don’t want hospitalists thinking that just because they have completed the certificate that they have fully mastered ultrasound. We encourage hospitalists to find a proctor in their own hospitals and to work with them to continue to refine their skills.”
Dr. Dancel and Dr. Janjigian reported no relevant disclosures.
References
1. Soni NJ et al. Point-of-care ultrasound for hospitalists: A position statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2. doi: 10.12788/jhm.3079.
Boosting your bedside diagnostic skills
Boosting your bedside diagnostic skills
A new three-session minitrack devoted to the clinical mastery of diagnostic and treatment skills at the hospitalized patient’s bedside should be a highlight of the Society of Hospital Medicine’s 2019 annual conference.
The “Clinical Mastery” track is designed to help hospitalists enhance their skills in making expert diagnoses at the bedside, said Dustin T. Smith, MD, SFHM, course director for HM19, and associate professor of medicine at Emory University, Atlanta. “We feel that all of the didactic sessions offered at HM19 are highly useful for hospitalists, but there is growing interest in having sessions devoted to learning clinical pearls that can aid in practicing medicine and acquiring the skill set of a master clinician.”
The three clinical mastery sessions at HM19 will address neurologic symptoms, ECG interpretation, and the role of point-of-care ultrasound (POCUS), currently a hot topic in hospital medicine. Recent advances in ultrasound technology have resulted in probes that can cost as little as $2,000, fit inside a lab coat pocket, and be read from a smartphone – making ultrasound far easier to bring to the bedside of hospitalized patients, said Ria Dancel, MD, FHM, associate professor of internal medicine and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Dancel will copresent the POCUS clinical mastery track at HM19. “Our focus will be on how POCUS and the physical exam relate to each other. These are not competing technologies but complementary, reflecting the evolution in bedside medicine. Because these new devices will soon be in the pockets of your colleagues, residents, physician assistants, and others, you should at least have the knowledge and vocabulary to communicate with them,” she said.
POCUS is a new technology that is not yet in wide use at the hospital bedside, but clearly a wave is building, said Dr. Dancel’s copresenter, Michael Janjigian, MD, associate professor in the department of medicine at NYU Langone Health in New York City.
“We’re at the inflection point where the cost of the machine and the availability of training means that hospitals need to decide if it’s time to embrace it,” he said. Hospitalists may also consider petitioning their hospital’s leadership to offer the machines and training.
“Hospitalists’ competencies and strengths lie primarily in making diagnoses,” Dr. Janjigian said. “We like to think of ourselves as master diagnosticians. Our session at HM19 will explore the strengths and weaknesses of both the physical exam and POCUS, presenting clinical scenarios common to hospital medicine. This course is designed for those who have never picked up an ultrasound probe and want to better understand why they should, and for those who want a better sense of how they might integrate it into their practice.”
While radiology and cardiology have been using ultrasound for decades, internists are finding uses at the bedside to speed diagnosis or focus their next diagnostic steps, Dr. Dancel noted. For certain diagnoses, the physical exam is still the tool of choice. But when looking for fluid around the heart or ascites buildup in the abdomen or when looking at the heart itself, she said, there is no better tool at the bedside than ultrasound.
In January 2019, the SHM issued a position statement on POCUS1, which is intended to inform hospitalists about the technology and its uses, encourage them to be more integrally involved in decision making processes surrounding POCUS program management for their hospitals, and promote development of standards for hospitalists in POCUS training and assessment. The SHM has also developed a pathway to teach the use of ultrasound, the Point-of-Care Ultrasound Certificate of Completion.
In order to qualify, clinicians complete online training modules, attend two live learning courses, compile a portfolio of ultrasound video clips on the job that are reviewed by a panel of experts, and then pass a final exam. The exam will be offered at HM19 for clinicians who have completed preliminary work for this new certificate – as well as precourses devoted to ultrasound and other procedures – and another workshop on POCUS.
Earning the POCUS certificate of completion requires a lot of effort, Dr. Dancel acknowledged. “It is a big commitment, and we don’t want hospitalists thinking that just because they have completed the certificate that they have fully mastered ultrasound. We encourage hospitalists to find a proctor in their own hospitals and to work with them to continue to refine their skills.”
Dr. Dancel and Dr. Janjigian reported no relevant disclosures.
References
1. Soni NJ et al. Point-of-care ultrasound for hospitalists: A position statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2. doi: 10.12788/jhm.3079.
A new three-session minitrack devoted to the clinical mastery of diagnostic and treatment skills at the hospitalized patient’s bedside should be a highlight of the Society of Hospital Medicine’s 2019 annual conference.
The “Clinical Mastery” track is designed to help hospitalists enhance their skills in making expert diagnoses at the bedside, said Dustin T. Smith, MD, SFHM, course director for HM19, and associate professor of medicine at Emory University, Atlanta. “We feel that all of the didactic sessions offered at HM19 are highly useful for hospitalists, but there is growing interest in having sessions devoted to learning clinical pearls that can aid in practicing medicine and acquiring the skill set of a master clinician.”
The three clinical mastery sessions at HM19 will address neurologic symptoms, ECG interpretation, and the role of point-of-care ultrasound (POCUS), currently a hot topic in hospital medicine. Recent advances in ultrasound technology have resulted in probes that can cost as little as $2,000, fit inside a lab coat pocket, and be read from a smartphone – making ultrasound far easier to bring to the bedside of hospitalized patients, said Ria Dancel, MD, FHM, associate professor of internal medicine and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Dancel will copresent the POCUS clinical mastery track at HM19. “Our focus will be on how POCUS and the physical exam relate to each other. These are not competing technologies but complementary, reflecting the evolution in bedside medicine. Because these new devices will soon be in the pockets of your colleagues, residents, physician assistants, and others, you should at least have the knowledge and vocabulary to communicate with them,” she said.
POCUS is a new technology that is not yet in wide use at the hospital bedside, but clearly a wave is building, said Dr. Dancel’s copresenter, Michael Janjigian, MD, associate professor in the department of medicine at NYU Langone Health in New York City.
“We’re at the inflection point where the cost of the machine and the availability of training means that hospitals need to decide if it’s time to embrace it,” he said. Hospitalists may also consider petitioning their hospital’s leadership to offer the machines and training.
“Hospitalists’ competencies and strengths lie primarily in making diagnoses,” Dr. Janjigian said. “We like to think of ourselves as master diagnosticians. Our session at HM19 will explore the strengths and weaknesses of both the physical exam and POCUS, presenting clinical scenarios common to hospital medicine. This course is designed for those who have never picked up an ultrasound probe and want to better understand why they should, and for those who want a better sense of how they might integrate it into their practice.”
While radiology and cardiology have been using ultrasound for decades, internists are finding uses at the bedside to speed diagnosis or focus their next diagnostic steps, Dr. Dancel noted. For certain diagnoses, the physical exam is still the tool of choice. But when looking for fluid around the heart or ascites buildup in the abdomen or when looking at the heart itself, she said, there is no better tool at the bedside than ultrasound.
In January 2019, the SHM issued a position statement on POCUS1, which is intended to inform hospitalists about the technology and its uses, encourage them to be more integrally involved in decision making processes surrounding POCUS program management for their hospitals, and promote development of standards for hospitalists in POCUS training and assessment. The SHM has also developed a pathway to teach the use of ultrasound, the Point-of-Care Ultrasound Certificate of Completion.
In order to qualify, clinicians complete online training modules, attend two live learning courses, compile a portfolio of ultrasound video clips on the job that are reviewed by a panel of experts, and then pass a final exam. The exam will be offered at HM19 for clinicians who have completed preliminary work for this new certificate – as well as precourses devoted to ultrasound and other procedures – and another workshop on POCUS.
Earning the POCUS certificate of completion requires a lot of effort, Dr. Dancel acknowledged. “It is a big commitment, and we don’t want hospitalists thinking that just because they have completed the certificate that they have fully mastered ultrasound. We encourage hospitalists to find a proctor in their own hospitals and to work with them to continue to refine their skills.”
Dr. Dancel and Dr. Janjigian reported no relevant disclosures.
References
1. Soni NJ et al. Point-of-care ultrasound for hospitalists: A position statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2. doi: 10.12788/jhm.3079.
Crafting a “well-rounded” program
New tracks, interactive programs highlight HM19
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”
New tracks, interactive programs highlight HM19
New tracks, interactive programs highlight HM19
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”