User login
This month in the journal CHEST®
Editor’s Picks
Editorials
Pulmonary Embolism Cardiac Arrest: Thrombolysis During Cardiopulmonary Resuscitation and Improved Survival. By Drs. B. W. Bottiger and W. A. Wetsch.
Interstitial Lung Abnormalities: A Word of Caution.
By Drs. V. Tzilas and D. Bouros.
Original Research
Thrombolysis During Resuscitation for Out-of-Hospital Cardiac Arrest Caused by Pulmonary Embolism Increases 30-Day Survival: Findings From the French National Cardiac Arrest Registry.
By Dr. F. Javaudin, et al.Interstitial Lung Abnormalities and Lung Cancer Risk in the National Lung Screening Trial. By Dr. S-A. Whittaker Brown, et al.
Commentary
Publishing a Clinical Research Manuscript: Guidance for Early-Career Researchers With a Focus on Pulmonary and Critical Care Medicine.
By Dr. E. M. Viglianti, et al.
Editor’s Picks
Editor’s Picks
Editorials
Pulmonary Embolism Cardiac Arrest: Thrombolysis During Cardiopulmonary Resuscitation and Improved Survival. By Drs. B. W. Bottiger and W. A. Wetsch.
Interstitial Lung Abnormalities: A Word of Caution.
By Drs. V. Tzilas and D. Bouros.
Original Research
Thrombolysis During Resuscitation for Out-of-Hospital Cardiac Arrest Caused by Pulmonary Embolism Increases 30-Day Survival: Findings From the French National Cardiac Arrest Registry.
By Dr. F. Javaudin, et al.Interstitial Lung Abnormalities and Lung Cancer Risk in the National Lung Screening Trial. By Dr. S-A. Whittaker Brown, et al.
Commentary
Publishing a Clinical Research Manuscript: Guidance for Early-Career Researchers With a Focus on Pulmonary and Critical Care Medicine.
By Dr. E. M. Viglianti, et al.
Editorials
Pulmonary Embolism Cardiac Arrest: Thrombolysis During Cardiopulmonary Resuscitation and Improved Survival. By Drs. B. W. Bottiger and W. A. Wetsch.
Interstitial Lung Abnormalities: A Word of Caution.
By Drs. V. Tzilas and D. Bouros.
Original Research
Thrombolysis During Resuscitation for Out-of-Hospital Cardiac Arrest Caused by Pulmonary Embolism Increases 30-Day Survival: Findings From the French National Cardiac Arrest Registry.
By Dr. F. Javaudin, et al.Interstitial Lung Abnormalities and Lung Cancer Risk in the National Lung Screening Trial. By Dr. S-A. Whittaker Brown, et al.
Commentary
Publishing a Clinical Research Manuscript: Guidance for Early-Career Researchers With a Focus on Pulmonary and Critical Care Medicine.
By Dr. E. M. Viglianti, et al.
Environmental Scan: Drivers of philanthropy
Philanthropy is a driving force supporting and promoting pioneering research and programs in many fields of medicine. Charitable giving, foundation support, and grants touch the lives of millions of patients and also have an impact across all fields of practice of medical practice. But philanthropy is being transformed by changing technology, interests of the giving public, and demands for accountability and transparency. Understanding where these trends are going will give physicians insights into what they can expect from philanthropy and what it might mean for their own institutions and interests.
In 2019, Charity Navigator reported total giving to charitable organizations was $427.1 billion, 0.7% measured in current dollars over the revised total of $424.74 billion contributed in 2017. Yet adjusted for inflation, overall giving declined 1.7%, primarily because individual giving declined. Foundation giving increased by an estimated 7.3% over 2017, to $75.86 billion in 2018 (an increase of 4.7%, adjusted for inflation). Giving by corporations is estimated to have increased by 5.4% in 2018, totaling $20.05 billion (an increase of 2.9%, adjusted for inflation).1
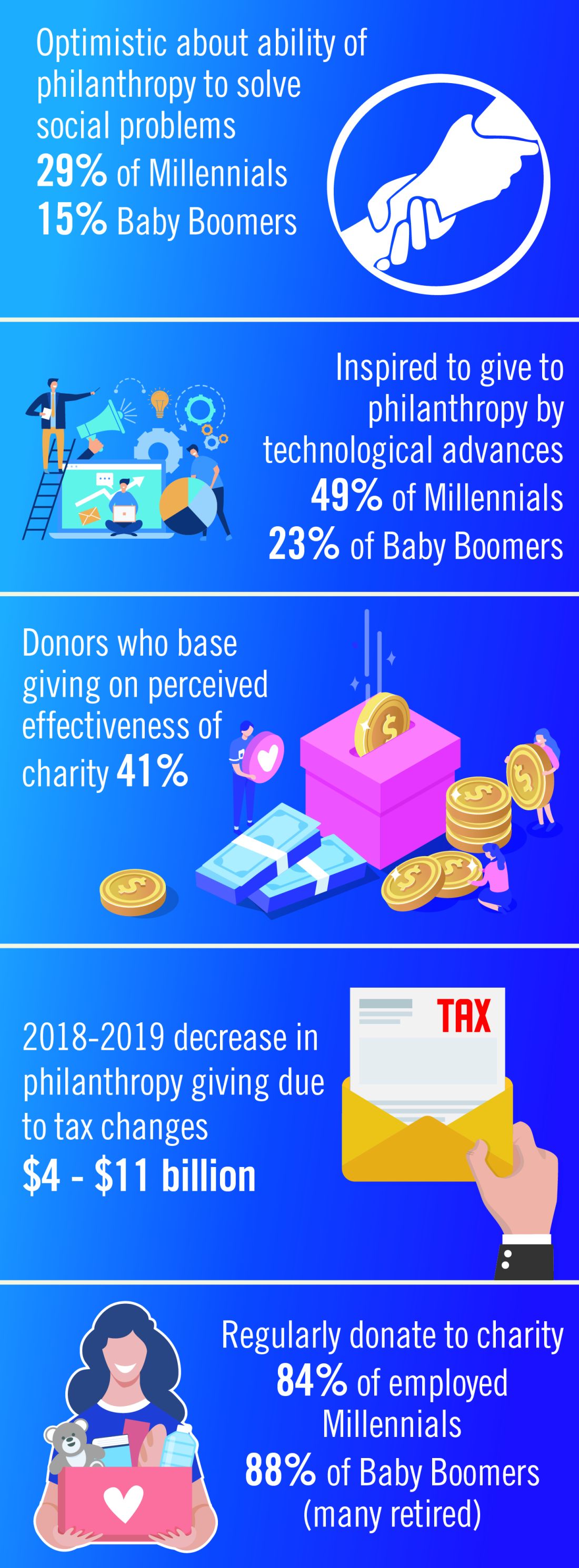
Impact investing, transparency, and trust
The demand for increased accountability in philanthropy is growing. Today’s donors want to know their contributions will have a real impact in causes they believe in. As donors become more focused on results, organizations will need to demonstrate their ability to achieve short-term goals that bring them closer to accomplishing their mission and vision. This sentiment may be strongest among Millennials. Nonprofit organizations should expect an increased level of due diligence and a higher level of personal involvement by donors. At least 41% of donors have changed their giving because of increased knowledge about nonprofit effectiveness. Foundations and corporations donate to medical centers and research institutions, but recipients are have an expectation of close involvement of donors, the need for detailed accounts of how funds are spent, and a responsibility to show progress or measurable outcomes.2
Health care–related issues
Two of the top three issues identified by donors as a challenge to be addressed are related to health care, according to Fidelity Charitable. Thirty-nine percent identified “developing treatment or cures for a disease” and 33% cited “access to basic health services” as priority issues. A study by Giving USA estimated that charitable giving to health care organizations rose a strong 7.3% (5.5% adjusted for inflation) in 2017, but giving that year was fueled by a booming stock market and a favorable tax environment. Charitable donations to hospitals tend to reflect the economic health of the community in which the institution is located. Donations to rural hospitals in depressed communities are likely to be far less than to urban institutions in economically strong areas.3
Tax reform
The Tax Cuts and Jobs Act of 2017 will likely affect donations to charitable organizations in 2019. Specifically, the 2017 Tax Act doubled the standard tax deduction, thereby reducing the number of households having to itemize their deductions and eliminating many tax benefits for charitable donations. Middle-class families are expected to opt for the standard deduction while wealthier taxpayers will likely continue itemizing their deductions. As a result, some predict that donors may switch from giving annually to giving every third year so they can itemize in their giving years to get the deduction. Estimates that charitable donations from individuals may decrease as much as $4 billion to $11 billion because of the increase in standard deductions and $0.9 billion to $2.1 billion because of the decrease in the marginal tax rate.4
Technology and peer-to-peer giving
Technological advances that make researching and giving easier and more convenient are likely to have a significant impact on many charitable organizations in 2019. Online donations are likely to increase as organizations make it simple to donate from mobile devices, social media platforms and their websites. Although charitable organizations will continue to directly ask individuals for a donation, many are expanding their efforts to include online social campaigns that leverage peer-to-peer giving. Other technological advancements likely to affect donations in the future include the ability for organizations to incorporate contactless payment programs and blockchain technology. Online giving grew by 12.1% over 2018-2019 with monthly automatic giving increasing by 40% over 2016 to 2017.5
Generational differences in giving
Although the trends identified above are likely to affect the decision to give in 2019, there are some meaningful differences in how different generations embrace these changes. Technological advances, the rise of alternative forms of giving, and increased opportunities to connect with peers about giving influence Millennials significantly more than Baby Boomers. Millennials are more likely to say that they give to make a meaningful difference while Boomers are likely to say that giving is part of their values. Millennials also are more likely to say their giving is more spontaneous while Boomers say their giving is more planned. As many as 49% of Millennials cite technological advances influencing their giving, compared with only 23% of Baby Boomers. This trend continues for the rise of alternative forms of giving (32% of Millennials, compared with 14% of Boomers) and increased opportunities to connect with peers about giving (30%, compared with 11%).
Twenty-nine percent of Millennials are very optimistic about philanthropy’s ability to solve the issues most important to them, compared with only 15% of Baby Boomers.2
One thing they have in common is their priorities. Both generations prioritize challenges related to health, hunger, and the environment.6
Today, foundations need to focus on impact, not just education programs or scholarships. New tech-driven trends in giving, such as the emergence of digital peer-to-peer giving and crowdfunding campaigns, make it possible to tap into high-volume, small-amount donations. To recruit new donors, organizations will need to target their messages based on the audience segment.
References:
1. Giving USA 2019: Annual report for philanthropy for 2018. Accessed Nov. 14, 2019.
2. Fidelity Charitable (2019) Future of philanthropy. Accessed Nov. 10, 2019.3. Betbeze, Philip (2018) Charitable giving to health giving to health organizations rose 7.3% last year. Health Leaders. July 11.
4. Martis & Landy/Indiana University Lilly Family School of Philanthropy (2018) The Philanthropy Outlook 2018 & 2019.
5. M&R Benchmarks 2019.
6. Nonprofit Source (2019) The ultimate list of charitable giving statistics for 2018. Accessed Nov. 10, 2019.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Philanthropy is a driving force supporting and promoting pioneering research and programs in many fields of medicine. Charitable giving, foundation support, and grants touch the lives of millions of patients and also have an impact across all fields of practice of medical practice. But philanthropy is being transformed by changing technology, interests of the giving public, and demands for accountability and transparency. Understanding where these trends are going will give physicians insights into what they can expect from philanthropy and what it might mean for their own institutions and interests.
In 2019, Charity Navigator reported total giving to charitable organizations was $427.1 billion, 0.7% measured in current dollars over the revised total of $424.74 billion contributed in 2017. Yet adjusted for inflation, overall giving declined 1.7%, primarily because individual giving declined. Foundation giving increased by an estimated 7.3% over 2017, to $75.86 billion in 2018 (an increase of 4.7%, adjusted for inflation). Giving by corporations is estimated to have increased by 5.4% in 2018, totaling $20.05 billion (an increase of 2.9%, adjusted for inflation).1
Impact investing, transparency, and trust
The demand for increased accountability in philanthropy is growing. Today’s donors want to know their contributions will have a real impact in causes they believe in. As donors become more focused on results, organizations will need to demonstrate their ability to achieve short-term goals that bring them closer to accomplishing their mission and vision. This sentiment may be strongest among Millennials. Nonprofit organizations should expect an increased level of due diligence and a higher level of personal involvement by donors. At least 41% of donors have changed their giving because of increased knowledge about nonprofit effectiveness. Foundations and corporations donate to medical centers and research institutions, but recipients are have an expectation of close involvement of donors, the need for detailed accounts of how funds are spent, and a responsibility to show progress or measurable outcomes.2
Health care–related issues
Two of the top three issues identified by donors as a challenge to be addressed are related to health care, according to Fidelity Charitable. Thirty-nine percent identified “developing treatment or cures for a disease” and 33% cited “access to basic health services” as priority issues. A study by Giving USA estimated that charitable giving to health care organizations rose a strong 7.3% (5.5% adjusted for inflation) in 2017, but giving that year was fueled by a booming stock market and a favorable tax environment. Charitable donations to hospitals tend to reflect the economic health of the community in which the institution is located. Donations to rural hospitals in depressed communities are likely to be far less than to urban institutions in economically strong areas.3
Tax reform
The Tax Cuts and Jobs Act of 2017 will likely affect donations to charitable organizations in 2019. Specifically, the 2017 Tax Act doubled the standard tax deduction, thereby reducing the number of households having to itemize their deductions and eliminating many tax benefits for charitable donations. Middle-class families are expected to opt for the standard deduction while wealthier taxpayers will likely continue itemizing their deductions. As a result, some predict that donors may switch from giving annually to giving every third year so they can itemize in their giving years to get the deduction. Estimates that charitable donations from individuals may decrease as much as $4 billion to $11 billion because of the increase in standard deductions and $0.9 billion to $2.1 billion because of the decrease in the marginal tax rate.4
Technology and peer-to-peer giving
Technological advances that make researching and giving easier and more convenient are likely to have a significant impact on many charitable organizations in 2019. Online donations are likely to increase as organizations make it simple to donate from mobile devices, social media platforms and their websites. Although charitable organizations will continue to directly ask individuals for a donation, many are expanding their efforts to include online social campaigns that leverage peer-to-peer giving. Other technological advancements likely to affect donations in the future include the ability for organizations to incorporate contactless payment programs and blockchain technology. Online giving grew by 12.1% over 2018-2019 with monthly automatic giving increasing by 40% over 2016 to 2017.5
Generational differences in giving
Although the trends identified above are likely to affect the decision to give in 2019, there are some meaningful differences in how different generations embrace these changes. Technological advances, the rise of alternative forms of giving, and increased opportunities to connect with peers about giving influence Millennials significantly more than Baby Boomers. Millennials are more likely to say that they give to make a meaningful difference while Boomers are likely to say that giving is part of their values. Millennials also are more likely to say their giving is more spontaneous while Boomers say their giving is more planned. As many as 49% of Millennials cite technological advances influencing their giving, compared with only 23% of Baby Boomers. This trend continues for the rise of alternative forms of giving (32% of Millennials, compared with 14% of Boomers) and increased opportunities to connect with peers about giving (30%, compared with 11%).
Twenty-nine percent of Millennials are very optimistic about philanthropy’s ability to solve the issues most important to them, compared with only 15% of Baby Boomers.2
One thing they have in common is their priorities. Both generations prioritize challenges related to health, hunger, and the environment.6
Today, foundations need to focus on impact, not just education programs or scholarships. New tech-driven trends in giving, such as the emergence of digital peer-to-peer giving and crowdfunding campaigns, make it possible to tap into high-volume, small-amount donations. To recruit new donors, organizations will need to target their messages based on the audience segment.
References:
1. Giving USA 2019: Annual report for philanthropy for 2018. Accessed Nov. 14, 2019.
2. Fidelity Charitable (2019) Future of philanthropy. Accessed Nov. 10, 2019.3. Betbeze, Philip (2018) Charitable giving to health giving to health organizations rose 7.3% last year. Health Leaders. July 11.
4. Martis & Landy/Indiana University Lilly Family School of Philanthropy (2018) The Philanthropy Outlook 2018 & 2019.
5. M&R Benchmarks 2019.
6. Nonprofit Source (2019) The ultimate list of charitable giving statistics for 2018. Accessed Nov. 10, 2019.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
Philanthropy is a driving force supporting and promoting pioneering research and programs in many fields of medicine. Charitable giving, foundation support, and grants touch the lives of millions of patients and also have an impact across all fields of practice of medical practice. But philanthropy is being transformed by changing technology, interests of the giving public, and demands for accountability and transparency. Understanding where these trends are going will give physicians insights into what they can expect from philanthropy and what it might mean for their own institutions and interests.
In 2019, Charity Navigator reported total giving to charitable organizations was $427.1 billion, 0.7% measured in current dollars over the revised total of $424.74 billion contributed in 2017. Yet adjusted for inflation, overall giving declined 1.7%, primarily because individual giving declined. Foundation giving increased by an estimated 7.3% over 2017, to $75.86 billion in 2018 (an increase of 4.7%, adjusted for inflation). Giving by corporations is estimated to have increased by 5.4% in 2018, totaling $20.05 billion (an increase of 2.9%, adjusted for inflation).1
Impact investing, transparency, and trust
The demand for increased accountability in philanthropy is growing. Today’s donors want to know their contributions will have a real impact in causes they believe in. As donors become more focused on results, organizations will need to demonstrate their ability to achieve short-term goals that bring them closer to accomplishing their mission and vision. This sentiment may be strongest among Millennials. Nonprofit organizations should expect an increased level of due diligence and a higher level of personal involvement by donors. At least 41% of donors have changed their giving because of increased knowledge about nonprofit effectiveness. Foundations and corporations donate to medical centers and research institutions, but recipients are have an expectation of close involvement of donors, the need for detailed accounts of how funds are spent, and a responsibility to show progress or measurable outcomes.2
Health care–related issues
Two of the top three issues identified by donors as a challenge to be addressed are related to health care, according to Fidelity Charitable. Thirty-nine percent identified “developing treatment or cures for a disease” and 33% cited “access to basic health services” as priority issues. A study by Giving USA estimated that charitable giving to health care organizations rose a strong 7.3% (5.5% adjusted for inflation) in 2017, but giving that year was fueled by a booming stock market and a favorable tax environment. Charitable donations to hospitals tend to reflect the economic health of the community in which the institution is located. Donations to rural hospitals in depressed communities are likely to be far less than to urban institutions in economically strong areas.3
Tax reform
The Tax Cuts and Jobs Act of 2017 will likely affect donations to charitable organizations in 2019. Specifically, the 2017 Tax Act doubled the standard tax deduction, thereby reducing the number of households having to itemize their deductions and eliminating many tax benefits for charitable donations. Middle-class families are expected to opt for the standard deduction while wealthier taxpayers will likely continue itemizing their deductions. As a result, some predict that donors may switch from giving annually to giving every third year so they can itemize in their giving years to get the deduction. Estimates that charitable donations from individuals may decrease as much as $4 billion to $11 billion because of the increase in standard deductions and $0.9 billion to $2.1 billion because of the decrease in the marginal tax rate.4
Technology and peer-to-peer giving
Technological advances that make researching and giving easier and more convenient are likely to have a significant impact on many charitable organizations in 2019. Online donations are likely to increase as organizations make it simple to donate from mobile devices, social media platforms and their websites. Although charitable organizations will continue to directly ask individuals for a donation, many are expanding their efforts to include online social campaigns that leverage peer-to-peer giving. Other technological advancements likely to affect donations in the future include the ability for organizations to incorporate contactless payment programs and blockchain technology. Online giving grew by 12.1% over 2018-2019 with monthly automatic giving increasing by 40% over 2016 to 2017.5
Generational differences in giving
Although the trends identified above are likely to affect the decision to give in 2019, there are some meaningful differences in how different generations embrace these changes. Technological advances, the rise of alternative forms of giving, and increased opportunities to connect with peers about giving influence Millennials significantly more than Baby Boomers. Millennials are more likely to say that they give to make a meaningful difference while Boomers are likely to say that giving is part of their values. Millennials also are more likely to say their giving is more spontaneous while Boomers say their giving is more planned. As many as 49% of Millennials cite technological advances influencing their giving, compared with only 23% of Baby Boomers. This trend continues for the rise of alternative forms of giving (32% of Millennials, compared with 14% of Boomers) and increased opportunities to connect with peers about giving (30%, compared with 11%).
Twenty-nine percent of Millennials are very optimistic about philanthropy’s ability to solve the issues most important to them, compared with only 15% of Baby Boomers.2
One thing they have in common is their priorities. Both generations prioritize challenges related to health, hunger, and the environment.6
Today, foundations need to focus on impact, not just education programs or scholarships. New tech-driven trends in giving, such as the emergence of digital peer-to-peer giving and crowdfunding campaigns, make it possible to tap into high-volume, small-amount donations. To recruit new donors, organizations will need to target their messages based on the audience segment.
References:
1. Giving USA 2019: Annual report for philanthropy for 2018. Accessed Nov. 14, 2019.
2. Fidelity Charitable (2019) Future of philanthropy. Accessed Nov. 10, 2019.3. Betbeze, Philip (2018) Charitable giving to health giving to health organizations rose 7.3% last year. Health Leaders. July 11.
4. Martis & Landy/Indiana University Lilly Family School of Philanthropy (2018) The Philanthropy Outlook 2018 & 2019.
5. M&R Benchmarks 2019.
6. Nonprofit Source (2019) The ultimate list of charitable giving statistics for 2018. Accessed Nov. 10, 2019.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
CHEST 2020 Honor Lectures and Award Nominations
Each year, CHEST honors physicians and others who are making significant or meritorious contributions to chest medicine. All honorees are recognized for advancing work in specific areas of chest medicine, mentorship, and training, furthering the work of CHEST, and more.
If you believe you have a colleague who should be recognized for their distinguished work, please submit a nomination. Those selected for an annual award and honor lecture will be featured at CHEST 2020 in Chicago.
Deadline: Monday, January 6, 2020
Questions? Please contact Emily Petraglia, Manager, Volunteer Engagement ([email protected]).
The following awards are now open for nominations:
Annual Awards
College Medalist Award
Distinguished Service AwardMaster FCCP
Honor and Memorial Lectures
Edward C. Rosenow III, MD, Master FCCP/Master Teacher Endowed Honor Lecture.
Roger C. Bone Memorial Lecture in Critical CareMurray Kornfeld Memorial Founders Award
Distinguished Scientist Honor Lecture in Cardiopulmonary PhysiologyPasquale Ciaglia Memorial Lecture in Interventional MedicineMargaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical VentilationThomas L. Petty, MD, Master FCCP Endowed Memorial Lecture
Educator Awards
Early Career Clinician Educator
Master Clinician Educator
Each year, CHEST honors physicians and others who are making significant or meritorious contributions to chest medicine. All honorees are recognized for advancing work in specific areas of chest medicine, mentorship, and training, furthering the work of CHEST, and more.
If you believe you have a colleague who should be recognized for their distinguished work, please submit a nomination. Those selected for an annual award and honor lecture will be featured at CHEST 2020 in Chicago.
Deadline: Monday, January 6, 2020
Questions? Please contact Emily Petraglia, Manager, Volunteer Engagement ([email protected]).
The following awards are now open for nominations:
Annual Awards
College Medalist Award
Distinguished Service AwardMaster FCCP
Honor and Memorial Lectures
Edward C. Rosenow III, MD, Master FCCP/Master Teacher Endowed Honor Lecture.
Roger C. Bone Memorial Lecture in Critical CareMurray Kornfeld Memorial Founders Award
Distinguished Scientist Honor Lecture in Cardiopulmonary PhysiologyPasquale Ciaglia Memorial Lecture in Interventional MedicineMargaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical VentilationThomas L. Petty, MD, Master FCCP Endowed Memorial Lecture
Educator Awards
Early Career Clinician Educator
Master Clinician Educator
Each year, CHEST honors physicians and others who are making significant or meritorious contributions to chest medicine. All honorees are recognized for advancing work in specific areas of chest medicine, mentorship, and training, furthering the work of CHEST, and more.
If you believe you have a colleague who should be recognized for their distinguished work, please submit a nomination. Those selected for an annual award and honor lecture will be featured at CHEST 2020 in Chicago.
Deadline: Monday, January 6, 2020
Questions? Please contact Emily Petraglia, Manager, Volunteer Engagement ([email protected]).
The following awards are now open for nominations:
Annual Awards
College Medalist Award
Distinguished Service AwardMaster FCCP
Honor and Memorial Lectures
Edward C. Rosenow III, MD, Master FCCP/Master Teacher Endowed Honor Lecture.
Roger C. Bone Memorial Lecture in Critical CareMurray Kornfeld Memorial Founders Award
Distinguished Scientist Honor Lecture in Cardiopulmonary PhysiologyPasquale Ciaglia Memorial Lecture in Interventional MedicineMargaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical VentilationThomas L. Petty, MD, Master FCCP Endowed Memorial Lecture
Educator Awards
Early Career Clinician Educator
Master Clinician Educator
Environmental Scan: Drivers of social, political and environmental change
We are living through an era of rapidly accelerated social, political, and environmental change. Spiraling costs of medical care, consumer activism around health care delivery, an aging population, and growing evidence of climate change are just some of the big currents of change. These trends are national and global in scope, and as such, far beyond any one profession or sector to shape or control. It remains for the medical profession to understand the currents of the time and adapt in order to thrive in the future.
Regulatory environment in flux
Hospitals and clinicians continue to struggle with a regulatory framework designed to improve higher quality of care yet may be creating additional barriers to access and efficiency. The passionate debate about health care costs and coverage is ongoing at the national level and appears to be a central issue on the minds of voters. Although the outcome of the debate cannot be foreseen, it will be left to the medical profession to maintain standards of care. Although the Affordable Care Act may not be repealed, the federal government’s role may diminish as policy is likely to be made by state politicians and bureaucrats.1 As a result, organizations operating in multiple states may find it difficult to develop organization-wide business strategies. And with the shift to value-based reimbursement and issues related to data breaches regarding private patient health care information, many health care professionals will need better support and documentation tools to remain compliant. This puts a large burden on medical organizations to invest even more in information technology, data management systems, and a wide range of training up and down the organizational chart. Keeping up with the needs of physicians for secure data management will be costly but critical.
Patients will feel climate change
Environmental factors affecting the air we breathe are of primary concern for patients with a broad range of cardiorespiratory conditions.2 Healthy but vulnerable infants, children, pregnant women, and the elderly may also feel the effects.3 Air pollution, increased levels of pollen and ground-level ozone, and wildfire smoke are all tied to climate change and all can have a direct impact on the patients seen by chest physicians.4 Individuals exposed to these environmental conditions may experience diminished lung function, resulting in increased hospital admissions.
Keeping up with the latest research on probable health impacts of these environmental trends will be on the agenda of most chest physicians.5 Professional societies will need to prepare to serve the educational needs of members in this regard. Continuing education content on these topics will be needed. The field will respond with new diagnostic tools and new treatments.6 Climate change may be a global-level phenomenon, but for many chest physicians, it means treating increasing numbers of patients affected by pulmonary disease.
Mind the generation gap
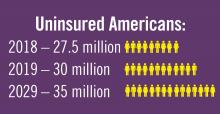
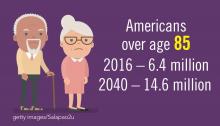
The population in the United States is primarily under the age of 65 years (84%), but the number of older citizens is on the rise. In 2016, there were 49.2 million people age 65 or older, and this number is projected to almost double to 98 million in 2060. The 85-and-over population is projected to more than double from 6.4 million in 2016 to 14.6 million in 2040 (a 129% increase).7
The medical needs of the aging population are already part of most medical institution’s planning but the current uncertainty in the health insurance market and the potential changes in Medicare coverage, not to mention the well-documented upcoming physician shortage, are complicating the planning process.8 Almost all acknowledge the “graying” of the population, but current approaches may not be sufficient given the projected the scale of the problems such as major increases in patients with chronic illnesses and the need for upscaling long-term geriatric care.
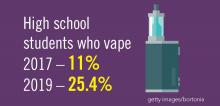
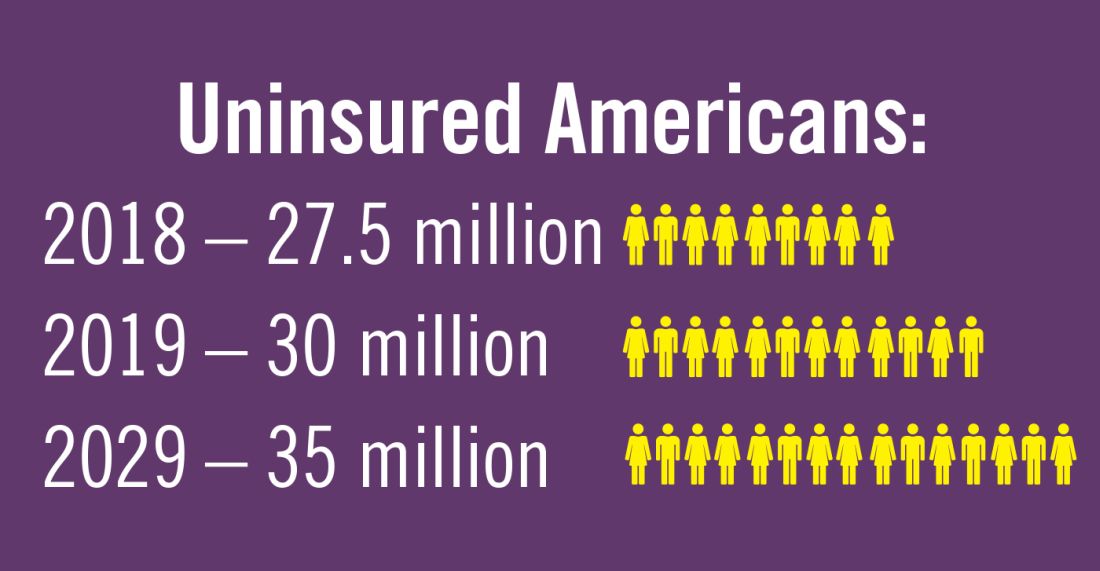
Planning for treating a growing elderly population shouldn’t mean ignoring some trends appearing among the younger population. E-cigarette use among middle- and high-school students may be creating millions of future patients with lung damage and nicotine addictions.9 Government intervention in this smoking epidemic is lagging behind the rapid spread of this unhealthy habit among young people.10 In 2019, health coverage of adults has begun to decline again after a decade of gains, and the possibility of this becoming a long-term trend has to be considered in planning for their treatment.11,12
References
1. Statistica. “Affordable Care Act - Statistics & Facts,” Matej Mikulic. 2019 Aug 14.
2. American Public Health Association and Centers for Disease Control and Prevention (2018). Climate Change Decreases the Quality of the Air We Breathe. Accessed 2019 Oct 7.
3. JAMA. 2019 Aug 13;322(6):546-56. doi: 10.1001/jama.2019.10255.
4. Lelieveld J et al. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J. 2019;40(20); 1590-6. doi: 10.1093/eurheartj/ehz135
5. European Respiratory Society. CME Online: Air pollution and respiratory health. 2018 Jun 21.
6. Environmental Protection Agency. “Particle Pollution and Your Patients’ Health,” Continuing Education for Particle Pollution Course. 2019 May 13.
7. U.S. Department of Health & Human Services. Administration on Aging. 2017 Profile of Older Americans. Accessed 2019 Oct 7.
8. Association of American Medical Colleges. Complexities of Physician Supply and Demand: Projection from 2017 to 2032. 2019 Apr.
9. Miech R et al. Trends in Adolescent Vaping, 2017-2019. N Eng J Med. 2019 Sep 18. doi: 10.1056/NEJMc1910739
10. Ned Sharpless, MD, Food and Drug Administration Acting Commissioner. “How the FDA is Regulating E-Cigarettes,” 2019 Sep 10.
11. Congressional Budget Office. Federal Subsidies for Health Insurance Coverage for People Under Age 65: 2019 to 2029. Washington D;C.: GPO, 2029
12. Galewitz P. “Breaking a 10-year streak, the number of uninsured Americans rises.” Internal Medicine News, 2019 Sep 11.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
We are living through an era of rapidly accelerated social, political, and environmental change. Spiraling costs of medical care, consumer activism around health care delivery, an aging population, and growing evidence of climate change are just some of the big currents of change. These trends are national and global in scope, and as such, far beyond any one profession or sector to shape or control. It remains for the medical profession to understand the currents of the time and adapt in order to thrive in the future.
Regulatory environment in flux
Hospitals and clinicians continue to struggle with a regulatory framework designed to improve higher quality of care yet may be creating additional barriers to access and efficiency. The passionate debate about health care costs and coverage is ongoing at the national level and appears to be a central issue on the minds of voters. Although the outcome of the debate cannot be foreseen, it will be left to the medical profession to maintain standards of care. Although the Affordable Care Act may not be repealed, the federal government’s role may diminish as policy is likely to be made by state politicians and bureaucrats.1 As a result, organizations operating in multiple states may find it difficult to develop organization-wide business strategies. And with the shift to value-based reimbursement and issues related to data breaches regarding private patient health care information, many health care professionals will need better support and documentation tools to remain compliant. This puts a large burden on medical organizations to invest even more in information technology, data management systems, and a wide range of training up and down the organizational chart. Keeping up with the needs of physicians for secure data management will be costly but critical.
Patients will feel climate change
Environmental factors affecting the air we breathe are of primary concern for patients with a broad range of cardiorespiratory conditions.2 Healthy but vulnerable infants, children, pregnant women, and the elderly may also feel the effects.3 Air pollution, increased levels of pollen and ground-level ozone, and wildfire smoke are all tied to climate change and all can have a direct impact on the patients seen by chest physicians.4 Individuals exposed to these environmental conditions may experience diminished lung function, resulting in increased hospital admissions.
Keeping up with the latest research on probable health impacts of these environmental trends will be on the agenda of most chest physicians.5 Professional societies will need to prepare to serve the educational needs of members in this regard. Continuing education content on these topics will be needed. The field will respond with new diagnostic tools and new treatments.6 Climate change may be a global-level phenomenon, but for many chest physicians, it means treating increasing numbers of patients affected by pulmonary disease.
Mind the generation gap
The population in the United States is primarily under the age of 65 years (84%), but the number of older citizens is on the rise. In 2016, there were 49.2 million people age 65 or older, and this number is projected to almost double to 98 million in 2060. The 85-and-over population is projected to more than double from 6.4 million in 2016 to 14.6 million in 2040 (a 129% increase).7
The medical needs of the aging population are already part of most medical institution’s planning but the current uncertainty in the health insurance market and the potential changes in Medicare coverage, not to mention the well-documented upcoming physician shortage, are complicating the planning process.8 Almost all acknowledge the “graying” of the population, but current approaches may not be sufficient given the projected the scale of the problems such as major increases in patients with chronic illnesses and the need for upscaling long-term geriatric care.
Planning for treating a growing elderly population shouldn’t mean ignoring some trends appearing among the younger population. E-cigarette use among middle- and high-school students may be creating millions of future patients with lung damage and nicotine addictions.9 Government intervention in this smoking epidemic is lagging behind the rapid spread of this unhealthy habit among young people.10 In 2019, health coverage of adults has begun to decline again after a decade of gains, and the possibility of this becoming a long-term trend has to be considered in planning for their treatment.11,12
References
1. Statistica. “Affordable Care Act - Statistics & Facts,” Matej Mikulic. 2019 Aug 14.
2. American Public Health Association and Centers for Disease Control and Prevention (2018). Climate Change Decreases the Quality of the Air We Breathe. Accessed 2019 Oct 7.
3. JAMA. 2019 Aug 13;322(6):546-56. doi: 10.1001/jama.2019.10255.
4. Lelieveld J et al. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J. 2019;40(20); 1590-6. doi: 10.1093/eurheartj/ehz135
5. European Respiratory Society. CME Online: Air pollution and respiratory health. 2018 Jun 21.
6. Environmental Protection Agency. “Particle Pollution and Your Patients’ Health,” Continuing Education for Particle Pollution Course. 2019 May 13.
7. U.S. Department of Health & Human Services. Administration on Aging. 2017 Profile of Older Americans. Accessed 2019 Oct 7.
8. Association of American Medical Colleges. Complexities of Physician Supply and Demand: Projection from 2017 to 2032. 2019 Apr.
9. Miech R et al. Trends in Adolescent Vaping, 2017-2019. N Eng J Med. 2019 Sep 18. doi: 10.1056/NEJMc1910739
10. Ned Sharpless, MD, Food and Drug Administration Acting Commissioner. “How the FDA is Regulating E-Cigarettes,” 2019 Sep 10.
11. Congressional Budget Office. Federal Subsidies for Health Insurance Coverage for People Under Age 65: 2019 to 2029. Washington D;C.: GPO, 2029
12. Galewitz P. “Breaking a 10-year streak, the number of uninsured Americans rises.” Internal Medicine News, 2019 Sep 11.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
We are living through an era of rapidly accelerated social, political, and environmental change. Spiraling costs of medical care, consumer activism around health care delivery, an aging population, and growing evidence of climate change are just some of the big currents of change. These trends are national and global in scope, and as such, far beyond any one profession or sector to shape or control. It remains for the medical profession to understand the currents of the time and adapt in order to thrive in the future.
Regulatory environment in flux
Hospitals and clinicians continue to struggle with a regulatory framework designed to improve higher quality of care yet may be creating additional barriers to access and efficiency. The passionate debate about health care costs and coverage is ongoing at the national level and appears to be a central issue on the minds of voters. Although the outcome of the debate cannot be foreseen, it will be left to the medical profession to maintain standards of care. Although the Affordable Care Act may not be repealed, the federal government’s role may diminish as policy is likely to be made by state politicians and bureaucrats.1 As a result, organizations operating in multiple states may find it difficult to develop organization-wide business strategies. And with the shift to value-based reimbursement and issues related to data breaches regarding private patient health care information, many health care professionals will need better support and documentation tools to remain compliant. This puts a large burden on medical organizations to invest even more in information technology, data management systems, and a wide range of training up and down the organizational chart. Keeping up with the needs of physicians for secure data management will be costly but critical.
Patients will feel climate change
Environmental factors affecting the air we breathe are of primary concern for patients with a broad range of cardiorespiratory conditions.2 Healthy but vulnerable infants, children, pregnant women, and the elderly may also feel the effects.3 Air pollution, increased levels of pollen and ground-level ozone, and wildfire smoke are all tied to climate change and all can have a direct impact on the patients seen by chest physicians.4 Individuals exposed to these environmental conditions may experience diminished lung function, resulting in increased hospital admissions.
Keeping up with the latest research on probable health impacts of these environmental trends will be on the agenda of most chest physicians.5 Professional societies will need to prepare to serve the educational needs of members in this regard. Continuing education content on these topics will be needed. The field will respond with new diagnostic tools and new treatments.6 Climate change may be a global-level phenomenon, but for many chest physicians, it means treating increasing numbers of patients affected by pulmonary disease.
Mind the generation gap
The population in the United States is primarily under the age of 65 years (84%), but the number of older citizens is on the rise. In 2016, there were 49.2 million people age 65 or older, and this number is projected to almost double to 98 million in 2060. The 85-and-over population is projected to more than double from 6.4 million in 2016 to 14.6 million in 2040 (a 129% increase).7
The medical needs of the aging population are already part of most medical institution’s planning but the current uncertainty in the health insurance market and the potential changes in Medicare coverage, not to mention the well-documented upcoming physician shortage, are complicating the planning process.8 Almost all acknowledge the “graying” of the population, but current approaches may not be sufficient given the projected the scale of the problems such as major increases in patients with chronic illnesses and the need for upscaling long-term geriatric care.
Planning for treating a growing elderly population shouldn’t mean ignoring some trends appearing among the younger population. E-cigarette use among middle- and high-school students may be creating millions of future patients with lung damage and nicotine addictions.9 Government intervention in this smoking epidemic is lagging behind the rapid spread of this unhealthy habit among young people.10 In 2019, health coverage of adults has begun to decline again after a decade of gains, and the possibility of this becoming a long-term trend has to be considered in planning for their treatment.11,12
References
1. Statistica. “Affordable Care Act - Statistics & Facts,” Matej Mikulic. 2019 Aug 14.
2. American Public Health Association and Centers for Disease Control and Prevention (2018). Climate Change Decreases the Quality of the Air We Breathe. Accessed 2019 Oct 7.
3. JAMA. 2019 Aug 13;322(6):546-56. doi: 10.1001/jama.2019.10255.
4. Lelieveld J et al. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J. 2019;40(20); 1590-6. doi: 10.1093/eurheartj/ehz135
5. European Respiratory Society. CME Online: Air pollution and respiratory health. 2018 Jun 21.
6. Environmental Protection Agency. “Particle Pollution and Your Patients’ Health,” Continuing Education for Particle Pollution Course. 2019 May 13.
7. U.S. Department of Health & Human Services. Administration on Aging. 2017 Profile of Older Americans. Accessed 2019 Oct 7.
8. Association of American Medical Colleges. Complexities of Physician Supply and Demand: Projection from 2017 to 2032. 2019 Apr.
9. Miech R et al. Trends in Adolescent Vaping, 2017-2019. N Eng J Med. 2019 Sep 18. doi: 10.1056/NEJMc1910739
10. Ned Sharpless, MD, Food and Drug Administration Acting Commissioner. “How the FDA is Regulating E-Cigarettes,” 2019 Sep 10.
11. Congressional Budget Office. Federal Subsidies for Health Insurance Coverage for People Under Age 65: 2019 to 2029. Washington D;C.: GPO, 2029
12. Galewitz P. “Breaking a 10-year streak, the number of uninsured Americans rises.” Internal Medicine News, 2019 Sep 11.
Note: Background research performed by Avenue M Group.
CHEST Inspiration is a collection of programmatic initiatives developed by the American College of Chest Physicians leadership and aimed at stimulating and encouraging innovation within the association. One of the components of CHEST Inspiration is the Environmental Scan, a series of articles focusing on the internal and external environmental factors that bear on success currently and in the future. See “Envisioning the Future: The CHEST Environmental Scan,” CHEST Physician, June 2019, p. 44, for an introduction to the series.
How to carve out a career as an educator during fellowship
Editor’s Note - As CHEST has just awarded the designation of Distinguished CHEST Educator (DCE) to 173 honorees at CHEST 2019 in New Orleans, this blog reminds fellows to start early to pursue a clinician educator role throughout their career.
While fellowship training is a time to continue building the foundation of expert clinical knowledge, it also offers an opportunity to start assembling a portfolio as a clinician educator. It takes time to compile educational scholarship and to establish a reputation within the communities of both teachers and learners, so it pays to get a head start. Moreover, it also takes time to master techniques for effective teaching to become that outstanding educator that you once looked up to as a medical student or resident. Below are some things that I found helpful in jump-starting that path during fellowship training.
Find a Capable Mentor
As with any sort of career planning, mentorship is key. Mentorship can open doors to expand your network and introduce opportunities for scholarship activities. Find a mentor who shares similar views and values with something that you feel passionate about. If you are planning on starting a scholarly project, make sure that your mentor has the background suited to help you maximize the experience and offer you the tools needed to achieve that end.
Determine What You Are Passionate About
Medical education is a vast field. Try to find something in medical education that is meaningful to you, whether it be in undergraduate medical education or graduate medical education or something else altogether. You want to be able to set yourself up for success, so the work has to be worthwhile.
Seek Out Opportunities to Teach
There are always opportunities to teach whether it entails precepting medical students on patient interviews or going over pulmonary/critical care topics at resident noon conferences. What I have found is that active participation in teaching opportunities tends to open a cascade of doors to more teaching opportunities.
Look for Opportunities to Be Involved in Educational Committees
Medical education, much like medicine, is a highly changing field. Leadership in medical education is always looking for resident/fellow representatives to bring new life and perspective to educational initiatives. Most of these opportunities do not require too much of a time commitment, and most committees often meet on a once-monthly basis. However, it connects you with faculty who are part of the leadership who can guide and help set you up for future success in medical education. During residency, I was able to take part in the intern curriculum committee to advise the direction of intern report. Now as a fellow, I’ve been able to meet many faculty and fellows with similar interests as mine in the CHEST Trainee Work Group.
Engage in Scholarly Activities
It is one thing to have a portfolio detailing teaching experiences, but it is another thing to have demonstrated published works in the space of medical education. It shows long-term promise as a clinician educator, and it shows leadership potential in advancing the field. It doesn’t take much to produce publications in medical education—there are always journals who look for trainees to contribute to the field whether it be an editorial or systematic review or innovative ideas.
About the Author
Justin K. Lui, MD, is a graduate of Boston University School of Medicine. He completed an internal medicine residency and chief residency at the University of Massachusetts Medical School. He is currently a second-year pulmonary and critical care medicine fellow at Boston University School of Medicine.
Reprinted from CHEST’s Thought Leader’s Blog, July 2019. This post is part of Our Life as a Fellow blog post series and includes “fellow life lessons” from current trainees in leadership with CHEST.
Editor’s Note - As CHEST has just awarded the designation of Distinguished CHEST Educator (DCE) to 173 honorees at CHEST 2019 in New Orleans, this blog reminds fellows to start early to pursue a clinician educator role throughout their career.
While fellowship training is a time to continue building the foundation of expert clinical knowledge, it also offers an opportunity to start assembling a portfolio as a clinician educator. It takes time to compile educational scholarship and to establish a reputation within the communities of both teachers and learners, so it pays to get a head start. Moreover, it also takes time to master techniques for effective teaching to become that outstanding educator that you once looked up to as a medical student or resident. Below are some things that I found helpful in jump-starting that path during fellowship training.
Find a Capable Mentor
As with any sort of career planning, mentorship is key. Mentorship can open doors to expand your network and introduce opportunities for scholarship activities. Find a mentor who shares similar views and values with something that you feel passionate about. If you are planning on starting a scholarly project, make sure that your mentor has the background suited to help you maximize the experience and offer you the tools needed to achieve that end.
Determine What You Are Passionate About
Medical education is a vast field. Try to find something in medical education that is meaningful to you, whether it be in undergraduate medical education or graduate medical education or something else altogether. You want to be able to set yourself up for success, so the work has to be worthwhile.
Seek Out Opportunities to Teach
There are always opportunities to teach whether it entails precepting medical students on patient interviews or going over pulmonary/critical care topics at resident noon conferences. What I have found is that active participation in teaching opportunities tends to open a cascade of doors to more teaching opportunities.
Look for Opportunities to Be Involved in Educational Committees
Medical education, much like medicine, is a highly changing field. Leadership in medical education is always looking for resident/fellow representatives to bring new life and perspective to educational initiatives. Most of these opportunities do not require too much of a time commitment, and most committees often meet on a once-monthly basis. However, it connects you with faculty who are part of the leadership who can guide and help set you up for future success in medical education. During residency, I was able to take part in the intern curriculum committee to advise the direction of intern report. Now as a fellow, I’ve been able to meet many faculty and fellows with similar interests as mine in the CHEST Trainee Work Group.
Engage in Scholarly Activities
It is one thing to have a portfolio detailing teaching experiences, but it is another thing to have demonstrated published works in the space of medical education. It shows long-term promise as a clinician educator, and it shows leadership potential in advancing the field. It doesn’t take much to produce publications in medical education—there are always journals who look for trainees to contribute to the field whether it be an editorial or systematic review or innovative ideas.
About the Author
Justin K. Lui, MD, is a graduate of Boston University School of Medicine. He completed an internal medicine residency and chief residency at the University of Massachusetts Medical School. He is currently a second-year pulmonary and critical care medicine fellow at Boston University School of Medicine.
Reprinted from CHEST’s Thought Leader’s Blog, July 2019. This post is part of Our Life as a Fellow blog post series and includes “fellow life lessons” from current trainees in leadership with CHEST.
Editor’s Note - As CHEST has just awarded the designation of Distinguished CHEST Educator (DCE) to 173 honorees at CHEST 2019 in New Orleans, this blog reminds fellows to start early to pursue a clinician educator role throughout their career.
While fellowship training is a time to continue building the foundation of expert clinical knowledge, it also offers an opportunity to start assembling a portfolio as a clinician educator. It takes time to compile educational scholarship and to establish a reputation within the communities of both teachers and learners, so it pays to get a head start. Moreover, it also takes time to master techniques for effective teaching to become that outstanding educator that you once looked up to as a medical student or resident. Below are some things that I found helpful in jump-starting that path during fellowship training.
Find a Capable Mentor
As with any sort of career planning, mentorship is key. Mentorship can open doors to expand your network and introduce opportunities for scholarship activities. Find a mentor who shares similar views and values with something that you feel passionate about. If you are planning on starting a scholarly project, make sure that your mentor has the background suited to help you maximize the experience and offer you the tools needed to achieve that end.
Determine What You Are Passionate About
Medical education is a vast field. Try to find something in medical education that is meaningful to you, whether it be in undergraduate medical education or graduate medical education or something else altogether. You want to be able to set yourself up for success, so the work has to be worthwhile.
Seek Out Opportunities to Teach
There are always opportunities to teach whether it entails precepting medical students on patient interviews or going over pulmonary/critical care topics at resident noon conferences. What I have found is that active participation in teaching opportunities tends to open a cascade of doors to more teaching opportunities.
Look for Opportunities to Be Involved in Educational Committees
Medical education, much like medicine, is a highly changing field. Leadership in medical education is always looking for resident/fellow representatives to bring new life and perspective to educational initiatives. Most of these opportunities do not require too much of a time commitment, and most committees often meet on a once-monthly basis. However, it connects you with faculty who are part of the leadership who can guide and help set you up for future success in medical education. During residency, I was able to take part in the intern curriculum committee to advise the direction of intern report. Now as a fellow, I’ve been able to meet many faculty and fellows with similar interests as mine in the CHEST Trainee Work Group.
Engage in Scholarly Activities
It is one thing to have a portfolio detailing teaching experiences, but it is another thing to have demonstrated published works in the space of medical education. It shows long-term promise as a clinician educator, and it shows leadership potential in advancing the field. It doesn’t take much to produce publications in medical education—there are always journals who look for trainees to contribute to the field whether it be an editorial or systematic review or innovative ideas.
About the Author
Justin K. Lui, MD, is a graduate of Boston University School of Medicine. He completed an internal medicine residency and chief residency at the University of Massachusetts Medical School. He is currently a second-year pulmonary and critical care medicine fellow at Boston University School of Medicine.
Reprinted from CHEST’s Thought Leader’s Blog, July 2019. This post is part of Our Life as a Fellow blog post series and includes “fellow life lessons” from current trainees in leadership with CHEST.
Meet the new CHEST® journal Deputy Editors
Christopher L. Carroll, MD, MS, FCCP
Dr. Carroll is a pediatric critical care physician at Connecticut Children’s Medical Center and a Professor of Pediatrics at the University of Connecticut. Dr. Carroll has a long-standing interest in social media and its use in academic medicine and medical education. He was an early adopter of social media in pulmonary and critical care medicine,and researches the use of social media in academic medicine. Dr. Carroll has served on numerous committees within CHEST, including most recently as Trustee of the CHEST Foundation and Chair of the Critical Care NetWork. Before being appointed Deputy Editor for Web and Multimedia for the journal CHEST, Dr. Carroll served as Social Media Section Editor from 2012-2018, and then Web and Multimedia Editor for the journal. He also co-chairs the Social Media Workgroup for CHEST. When not working or tweeting, Dr. Carroll can be found camping with his Boy Scout troop and parenting three amazingly nerdy and talented children who are fortunate to take after their grandparents.
Darcy D. Marciniuk, MD, FCCP
Dr. Marciniuk is a Professor of Respirology, Critical Care, and Sleep Medicine, and Associate Vice-President Research at the University of Saskatchewan, Saskatoon, SK, Canada. He is recognized internationally as an expert and leader in clinical exercise physiology, COPD, and pulmonary rehabilitation. Dr. Marciniuk is a Past President of CHEST and served as a founding Steering Committee member of Canada’s National Lung Health Framework, member and Chair of the Royal College of Physicians and Surgeons of Canada Respirology Examination Board, President of the Canadian Thoracic Society (CTS), and Co-Chair of the 2016 CHEST World Congress and 2005 CHEST Annual Meeting. He was the lead author of three COPD clinical practice guidelines, a panel member of international clinical practice guidelines in COPD, cardiopulmonary exercise testing, and pulmonary rehabilitation, and was a co-author of the published joint Canadian Thoracic Society/CHEST clinical practice guideline on preventing acute exacerbations of COPD.Susan Murin, MD, MSc, MBA, FCCP
Dr. Murin is currently serving as Vice-Dean for Clinical Affairs and Executive Director of the UC Davis Practice Management Group. She previously served as Program Director for the Pulmonary and Critical Care fellowship, Chief of the Division of Pulmonary, Critical Care and Sleep Medicine, and Vice-Chair for Clinical Affairs at UC Davis. Her past national service has included membership on the ACGME’s Internal Medicine RRC, Chair of the Pulmonary Medicine test-writing committee for the ABIM, and Chair of the Association of Pulmonary and Critical Care Medicine Program Directors. She has a long history of service to the college in a variety of roles and served as an Associate Editor of the CHEST journal or 14 years. Dr. Murin’s research has been focused in two areas: epidemiology of venous thromboembolism and the effects of smoking on the natural history of breast cancer. She remains active in clinical care and teaching at both UC Davis and the Northern California VA. When not working, she enjoys spending time with her three grown children, scuba diving, and tennis.
Christopher L. Carroll, MD, MS, FCCP
Dr. Carroll is a pediatric critical care physician at Connecticut Children’s Medical Center and a Professor of Pediatrics at the University of Connecticut. Dr. Carroll has a long-standing interest in social media and its use in academic medicine and medical education. He was an early adopter of social media in pulmonary and critical care medicine,and researches the use of social media in academic medicine. Dr. Carroll has served on numerous committees within CHEST, including most recently as Trustee of the CHEST Foundation and Chair of the Critical Care NetWork. Before being appointed Deputy Editor for Web and Multimedia for the journal CHEST, Dr. Carroll served as Social Media Section Editor from 2012-2018, and then Web and Multimedia Editor for the journal. He also co-chairs the Social Media Workgroup for CHEST. When not working or tweeting, Dr. Carroll can be found camping with his Boy Scout troop and parenting three amazingly nerdy and talented children who are fortunate to take after their grandparents.
Darcy D. Marciniuk, MD, FCCP
Dr. Marciniuk is a Professor of Respirology, Critical Care, and Sleep Medicine, and Associate Vice-President Research at the University of Saskatchewan, Saskatoon, SK, Canada. He is recognized internationally as an expert and leader in clinical exercise physiology, COPD, and pulmonary rehabilitation. Dr. Marciniuk is a Past President of CHEST and served as a founding Steering Committee member of Canada’s National Lung Health Framework, member and Chair of the Royal College of Physicians and Surgeons of Canada Respirology Examination Board, President of the Canadian Thoracic Society (CTS), and Co-Chair of the 2016 CHEST World Congress and 2005 CHEST Annual Meeting. He was the lead author of three COPD clinical practice guidelines, a panel member of international clinical practice guidelines in COPD, cardiopulmonary exercise testing, and pulmonary rehabilitation, and was a co-author of the published joint Canadian Thoracic Society/CHEST clinical practice guideline on preventing acute exacerbations of COPD.Susan Murin, MD, MSc, MBA, FCCP
Dr. Murin is currently serving as Vice-Dean for Clinical Affairs and Executive Director of the UC Davis Practice Management Group. She previously served as Program Director for the Pulmonary and Critical Care fellowship, Chief of the Division of Pulmonary, Critical Care and Sleep Medicine, and Vice-Chair for Clinical Affairs at UC Davis. Her past national service has included membership on the ACGME’s Internal Medicine RRC, Chair of the Pulmonary Medicine test-writing committee for the ABIM, and Chair of the Association of Pulmonary and Critical Care Medicine Program Directors. She has a long history of service to the college in a variety of roles and served as an Associate Editor of the CHEST journal or 14 years. Dr. Murin’s research has been focused in two areas: epidemiology of venous thromboembolism and the effects of smoking on the natural history of breast cancer. She remains active in clinical care and teaching at both UC Davis and the Northern California VA. When not working, she enjoys spending time with her three grown children, scuba diving, and tennis.
Christopher L. Carroll, MD, MS, FCCP
Dr. Carroll is a pediatric critical care physician at Connecticut Children’s Medical Center and a Professor of Pediatrics at the University of Connecticut. Dr. Carroll has a long-standing interest in social media and its use in academic medicine and medical education. He was an early adopter of social media in pulmonary and critical care medicine,and researches the use of social media in academic medicine. Dr. Carroll has served on numerous committees within CHEST, including most recently as Trustee of the CHEST Foundation and Chair of the Critical Care NetWork. Before being appointed Deputy Editor for Web and Multimedia for the journal CHEST, Dr. Carroll served as Social Media Section Editor from 2012-2018, and then Web and Multimedia Editor for the journal. He also co-chairs the Social Media Workgroup for CHEST. When not working or tweeting, Dr. Carroll can be found camping with his Boy Scout troop and parenting three amazingly nerdy and talented children who are fortunate to take after their grandparents.
Darcy D. Marciniuk, MD, FCCP
Dr. Marciniuk is a Professor of Respirology, Critical Care, and Sleep Medicine, and Associate Vice-President Research at the University of Saskatchewan, Saskatoon, SK, Canada. He is recognized internationally as an expert and leader in clinical exercise physiology, COPD, and pulmonary rehabilitation. Dr. Marciniuk is a Past President of CHEST and served as a founding Steering Committee member of Canada’s National Lung Health Framework, member and Chair of the Royal College of Physicians and Surgeons of Canada Respirology Examination Board, President of the Canadian Thoracic Society (CTS), and Co-Chair of the 2016 CHEST World Congress and 2005 CHEST Annual Meeting. He was the lead author of three COPD clinical practice guidelines, a panel member of international clinical practice guidelines in COPD, cardiopulmonary exercise testing, and pulmonary rehabilitation, and was a co-author of the published joint Canadian Thoracic Society/CHEST clinical practice guideline on preventing acute exacerbations of COPD.Susan Murin, MD, MSc, MBA, FCCP
Dr. Murin is currently serving as Vice-Dean for Clinical Affairs and Executive Director of the UC Davis Practice Management Group. She previously served as Program Director for the Pulmonary and Critical Care fellowship, Chief of the Division of Pulmonary, Critical Care and Sleep Medicine, and Vice-Chair for Clinical Affairs at UC Davis. Her past national service has included membership on the ACGME’s Internal Medicine RRC, Chair of the Pulmonary Medicine test-writing committee for the ABIM, and Chair of the Association of Pulmonary and Critical Care Medicine Program Directors. She has a long history of service to the college in a variety of roles and served as an Associate Editor of the CHEST journal or 14 years. Dr. Murin’s research has been focused in two areas: epidemiology of venous thromboembolism and the effects of smoking on the natural history of breast cancer. She remains active in clinical care and teaching at both UC Davis and the Northern California VA. When not working, she enjoys spending time with her three grown children, scuba diving, and tennis.
From the President: Wisdom of our crowd
About a year ago, I had the opportunity to don the honorary regalia of the American College of Chest Physicians as its 81st President. On that memorable day on the dais in San Antonio, I used the example of James Surowiecki’s book, “The Wisdom of Crowds: Why the Many Are Smarter than the Few and How Collective Wisdom Shapes Business, Economics, Societies, and Nations” to explain how we would use the collective wisdom of our members, our committee and NetWork members, and our talented association staff to build and shape CHEST over the coming year. For those of you not familiar with this concept, Surowiecki, a business columnist for New Yorker, outlines the concept that large groups of people are actually smarter than an elite few at solving the problems of an organization, fostering innovation, collectively coming to wise decisions, or even predicting the future. In channeling the lessons from the book, it has become obvious that listening to our members and partners, rather than trying to make all decisions from the top down, has been an effective method for coming to wise decisions about the strategy and operation of CHEST. Now that it’s already time to hand the responsibility of the organization as President over to my friend and colleague Dr. Stephanie Levine, I’ve reflected on actually how effectively we have listened and how smart the collective crowd has been in moving the success of CHEST forward.
We heard from members that it was difficult to know how to get involved and what happens at the highest leadership levels of the organization. This prompted the development of podcasts dubbed “The Inside Scoop,” recorded live approximately every 2 months and featured various leaders of the organization with an informal way for members to better understand how to become involved in CHEST activities and to feel the pulse of activity of the association between the time the annual meeting ends and the next one begins.
The crowd informed us that communication at the Board of Regents level could be better. To address this, regular communications were sent out to the Board of Regents to update them on activities and discussion of issues between scheduled board meetings, as well as providing board members the opportunity to have access to the minutes of phone calls of the “5Ps,” calls that included the Immediate Past, President-Elect, President-Designate, and current President of the association, as well as the CHEST Foundation President.
We were told by members through focus groups and surveys, then again told by experts we invited to the June board meetings from education, business, design, and venture capital sectors (and who were naïve to CHEST as an association) that we needed to double down on virtual educational offerings to learners across the health-care delivery team and to revamp its information technology infrastructure. To that end, a digital strategy work group was convened with expertise in information technology, social media, and marketing to inventory all digital assets of the College and make recommendations for not just improvement, but for a complete transformation of digital technology created and promulgated by CHEST. The board then approved a budget of nearly $1 million to upgrade and rebuild the user experience within CHEST’s digital environment, including its learning management system. We also opened a multimedia studio at CHEST headquarters, increased the numbers of serious educational gaming opportunities at the annual meeting, and are developing a line of serious game platforms that will allow for “edutainment” opportunities for our members and other learners around the world using various digital platforms.
Colleagues from around the world reminded us that 20% of CHEST membership was international and that our strategic plan included an international strategy. Thanks to the support of our colleagues around the world, we were able to enjoy a tremendously successful CHEST Congress in Bangkok, Thailand, in April, and a smaller regional meeting in June in Athens, Greece. Efforts of the Governance Committee have reshaped the structure of international representation, making it more relevant and allowing its members to have a stronger voice to the Board of Regents. Plans are underway for the next CHEST Congress in June 2020 in Bologna, Italy, to be held in collaboration with the Italian Chapter of CHEST in that country.
In an era when the majority of association annual meetings across multiple specialties are driving toward parity with similar looks, marketing, formats, and expectations, we listened to the needs and desires of attendees of last year’s meeting and have improved CHEST 2019 in New Orleans even more. With the most simulation courses ever delivered at an annual meeting, more serious game opportunities, CHEST Challenge finals, a new innovation competition called “FISH Bowl,” and even a medical escape room, CHEST volunteer leaders and organization staff have worked hard to provide a world class meeting that has a different look and feel from all the others. Plus, the crowd also told us that having CME and MOC credit available for the entire meeting was another variable that was desired, and has now been achieved.
The wisdom of the proverbial crowd of membership has spoken in terms of the need for philanthropic efforts in our specialty. The CHEST Foundation has responded by awarding tens of thousands of dollars to our members to recognize cutting-edge research, community service efforts, and, in addition, has allowed dozens of providers early on in training or in their career to attend the annual meeting with the help of travel grants.
CHEST guidelines continue to be updated and new ones created based on input from expert panel teams. The CHEST journal submission process, review turnaround times, and quality of manuscripts have improved each year thanks to useful feedback from authors and readers. Publications such as CHEST Physician are modified each year based upon feedback from our readers. Critiques from the board review courses have been the driving force keeping live learning formats and the electronic SEEK board preparation questions current and accurate when the science is constantly changing.
Truly, the collective wisdom of our members, talented clinicians and researchers, and colleagues in industry has provided incredibly valuable input to the CHEST leadership team. You have spoken, and we have been listening. Thanks to each of you who have reached out to me during this year as President. Traveling to four continents this past year to better understand the needs of members who are clinicians, educators, researchers, and caregivers positioned in each geographic region has been enlightening, educational, and transformative for me and my family. Your meaningful feedback, keen insights, and passion for outstanding patient care, impactful educational experiences, and life-changing research have helped push CHEST to a higher level of excellence and to offer unparalleled experiences for our members to ultimately provide the very best care to patients.
About a year ago, I had the opportunity to don the honorary regalia of the American College of Chest Physicians as its 81st President. On that memorable day on the dais in San Antonio, I used the example of James Surowiecki’s book, “The Wisdom of Crowds: Why the Many Are Smarter than the Few and How Collective Wisdom Shapes Business, Economics, Societies, and Nations” to explain how we would use the collective wisdom of our members, our committee and NetWork members, and our talented association staff to build and shape CHEST over the coming year. For those of you not familiar with this concept, Surowiecki, a business columnist for New Yorker, outlines the concept that large groups of people are actually smarter than an elite few at solving the problems of an organization, fostering innovation, collectively coming to wise decisions, or even predicting the future. In channeling the lessons from the book, it has become obvious that listening to our members and partners, rather than trying to make all decisions from the top down, has been an effective method for coming to wise decisions about the strategy and operation of CHEST. Now that it’s already time to hand the responsibility of the organization as President over to my friend and colleague Dr. Stephanie Levine, I’ve reflected on actually how effectively we have listened and how smart the collective crowd has been in moving the success of CHEST forward.
We heard from members that it was difficult to know how to get involved and what happens at the highest leadership levels of the organization. This prompted the development of podcasts dubbed “The Inside Scoop,” recorded live approximately every 2 months and featured various leaders of the organization with an informal way for members to better understand how to become involved in CHEST activities and to feel the pulse of activity of the association between the time the annual meeting ends and the next one begins.
The crowd informed us that communication at the Board of Regents level could be better. To address this, regular communications were sent out to the Board of Regents to update them on activities and discussion of issues between scheduled board meetings, as well as providing board members the opportunity to have access to the minutes of phone calls of the “5Ps,” calls that included the Immediate Past, President-Elect, President-Designate, and current President of the association, as well as the CHEST Foundation President.
We were told by members through focus groups and surveys, then again told by experts we invited to the June board meetings from education, business, design, and venture capital sectors (and who were naïve to CHEST as an association) that we needed to double down on virtual educational offerings to learners across the health-care delivery team and to revamp its information technology infrastructure. To that end, a digital strategy work group was convened with expertise in information technology, social media, and marketing to inventory all digital assets of the College and make recommendations for not just improvement, but for a complete transformation of digital technology created and promulgated by CHEST. The board then approved a budget of nearly $1 million to upgrade and rebuild the user experience within CHEST’s digital environment, including its learning management system. We also opened a multimedia studio at CHEST headquarters, increased the numbers of serious educational gaming opportunities at the annual meeting, and are developing a line of serious game platforms that will allow for “edutainment” opportunities for our members and other learners around the world using various digital platforms.
Colleagues from around the world reminded us that 20% of CHEST membership was international and that our strategic plan included an international strategy. Thanks to the support of our colleagues around the world, we were able to enjoy a tremendously successful CHEST Congress in Bangkok, Thailand, in April, and a smaller regional meeting in June in Athens, Greece. Efforts of the Governance Committee have reshaped the structure of international representation, making it more relevant and allowing its members to have a stronger voice to the Board of Regents. Plans are underway for the next CHEST Congress in June 2020 in Bologna, Italy, to be held in collaboration with the Italian Chapter of CHEST in that country.
In an era when the majority of association annual meetings across multiple specialties are driving toward parity with similar looks, marketing, formats, and expectations, we listened to the needs and desires of attendees of last year’s meeting and have improved CHEST 2019 in New Orleans even more. With the most simulation courses ever delivered at an annual meeting, more serious game opportunities, CHEST Challenge finals, a new innovation competition called “FISH Bowl,” and even a medical escape room, CHEST volunteer leaders and organization staff have worked hard to provide a world class meeting that has a different look and feel from all the others. Plus, the crowd also told us that having CME and MOC credit available for the entire meeting was another variable that was desired, and has now been achieved.
The wisdom of the proverbial crowd of membership has spoken in terms of the need for philanthropic efforts in our specialty. The CHEST Foundation has responded by awarding tens of thousands of dollars to our members to recognize cutting-edge research, community service efforts, and, in addition, has allowed dozens of providers early on in training or in their career to attend the annual meeting with the help of travel grants.
CHEST guidelines continue to be updated and new ones created based on input from expert panel teams. The CHEST journal submission process, review turnaround times, and quality of manuscripts have improved each year thanks to useful feedback from authors and readers. Publications such as CHEST Physician are modified each year based upon feedback from our readers. Critiques from the board review courses have been the driving force keeping live learning formats and the electronic SEEK board preparation questions current and accurate when the science is constantly changing.
Truly, the collective wisdom of our members, talented clinicians and researchers, and colleagues in industry has provided incredibly valuable input to the CHEST leadership team. You have spoken, and we have been listening. Thanks to each of you who have reached out to me during this year as President. Traveling to four continents this past year to better understand the needs of members who are clinicians, educators, researchers, and caregivers positioned in each geographic region has been enlightening, educational, and transformative for me and my family. Your meaningful feedback, keen insights, and passion for outstanding patient care, impactful educational experiences, and life-changing research have helped push CHEST to a higher level of excellence and to offer unparalleled experiences for our members to ultimately provide the very best care to patients.
About a year ago, I had the opportunity to don the honorary regalia of the American College of Chest Physicians as its 81st President. On that memorable day on the dais in San Antonio, I used the example of James Surowiecki’s book, “The Wisdom of Crowds: Why the Many Are Smarter than the Few and How Collective Wisdom Shapes Business, Economics, Societies, and Nations” to explain how we would use the collective wisdom of our members, our committee and NetWork members, and our talented association staff to build and shape CHEST over the coming year. For those of you not familiar with this concept, Surowiecki, a business columnist for New Yorker, outlines the concept that large groups of people are actually smarter than an elite few at solving the problems of an organization, fostering innovation, collectively coming to wise decisions, or even predicting the future. In channeling the lessons from the book, it has become obvious that listening to our members and partners, rather than trying to make all decisions from the top down, has been an effective method for coming to wise decisions about the strategy and operation of CHEST. Now that it’s already time to hand the responsibility of the organization as President over to my friend and colleague Dr. Stephanie Levine, I’ve reflected on actually how effectively we have listened and how smart the collective crowd has been in moving the success of CHEST forward.
We heard from members that it was difficult to know how to get involved and what happens at the highest leadership levels of the organization. This prompted the development of podcasts dubbed “The Inside Scoop,” recorded live approximately every 2 months and featured various leaders of the organization with an informal way for members to better understand how to become involved in CHEST activities and to feel the pulse of activity of the association between the time the annual meeting ends and the next one begins.
The crowd informed us that communication at the Board of Regents level could be better. To address this, regular communications were sent out to the Board of Regents to update them on activities and discussion of issues between scheduled board meetings, as well as providing board members the opportunity to have access to the minutes of phone calls of the “5Ps,” calls that included the Immediate Past, President-Elect, President-Designate, and current President of the association, as well as the CHEST Foundation President.
We were told by members through focus groups and surveys, then again told by experts we invited to the June board meetings from education, business, design, and venture capital sectors (and who were naïve to CHEST as an association) that we needed to double down on virtual educational offerings to learners across the health-care delivery team and to revamp its information technology infrastructure. To that end, a digital strategy work group was convened with expertise in information technology, social media, and marketing to inventory all digital assets of the College and make recommendations for not just improvement, but for a complete transformation of digital technology created and promulgated by CHEST. The board then approved a budget of nearly $1 million to upgrade and rebuild the user experience within CHEST’s digital environment, including its learning management system. We also opened a multimedia studio at CHEST headquarters, increased the numbers of serious educational gaming opportunities at the annual meeting, and are developing a line of serious game platforms that will allow for “edutainment” opportunities for our members and other learners around the world using various digital platforms.
Colleagues from around the world reminded us that 20% of CHEST membership was international and that our strategic plan included an international strategy. Thanks to the support of our colleagues around the world, we were able to enjoy a tremendously successful CHEST Congress in Bangkok, Thailand, in April, and a smaller regional meeting in June in Athens, Greece. Efforts of the Governance Committee have reshaped the structure of international representation, making it more relevant and allowing its members to have a stronger voice to the Board of Regents. Plans are underway for the next CHEST Congress in June 2020 in Bologna, Italy, to be held in collaboration with the Italian Chapter of CHEST in that country.
In an era when the majority of association annual meetings across multiple specialties are driving toward parity with similar looks, marketing, formats, and expectations, we listened to the needs and desires of attendees of last year’s meeting and have improved CHEST 2019 in New Orleans even more. With the most simulation courses ever delivered at an annual meeting, more serious game opportunities, CHEST Challenge finals, a new innovation competition called “FISH Bowl,” and even a medical escape room, CHEST volunteer leaders and organization staff have worked hard to provide a world class meeting that has a different look and feel from all the others. Plus, the crowd also told us that having CME and MOC credit available for the entire meeting was another variable that was desired, and has now been achieved.
The wisdom of the proverbial crowd of membership has spoken in terms of the need for philanthropic efforts in our specialty. The CHEST Foundation has responded by awarding tens of thousands of dollars to our members to recognize cutting-edge research, community service efforts, and, in addition, has allowed dozens of providers early on in training or in their career to attend the annual meeting with the help of travel grants.
CHEST guidelines continue to be updated and new ones created based on input from expert panel teams. The CHEST journal submission process, review turnaround times, and quality of manuscripts have improved each year thanks to useful feedback from authors and readers. Publications such as CHEST Physician are modified each year based upon feedback from our readers. Critiques from the board review courses have been the driving force keeping live learning formats and the electronic SEEK board preparation questions current and accurate when the science is constantly changing.
Truly, the collective wisdom of our members, talented clinicians and researchers, and colleagues in industry has provided incredibly valuable input to the CHEST leadership team. You have spoken, and we have been listening. Thanks to each of you who have reached out to me during this year as President. Traveling to four continents this past year to better understand the needs of members who are clinicians, educators, researchers, and caregivers positioned in each geographic region has been enlightening, educational, and transformative for me and my family. Your meaningful feedback, keen insights, and passion for outstanding patient care, impactful educational experiences, and life-changing research have helped push CHEST to a higher level of excellence and to offer unparalleled experiences for our members to ultimately provide the very best care to patients.
Robotic-assisted bronchoscopy. PARDS. Vaping alert. PR and COPD.
Interventional Chest/Diagnostic Procedures
Emergence of robotic-assisted bronchoscopy for the diagnosis of peripheral lung lesions
The diagnostic chest medicine community saw exciting advances in technology for diagnosis of peripheral lung lesions (PLL) with the recent FDA approval of two robotic-assisted bronchoscopy systems (RBS): the Monarch Platform from Auris Health (2018) and the Ion system from Intuitive Surgical (2019). Small pilot studies of 15 (Monarch) and 29 (Ion) subjects, respectively, demonstrated safety and feasibility of biopsy and diagnosis of PLL using RBS (Rojas-Solano, et al. J Bronchol Intervent Pulmonol. 2018;25:168; Fielding et al. Respiration. 2019;98[2]:142). While these studies were not powered to evaluate diagnostic yield, they suggested the potential for improved yields over current technologies.
Current bronchoscopic modalities for diagnosis of PLL include electromagnetic navigation bronchoscopy, radial endobronchial ultrasound, and fluoroscopic guidance, all of which have favorable safety profiles but have been plagued by a wide range in diagnostic yields (38% to 88%) (Eberhardt R, et al. Am J Respir Crit Med. 2007;176[1]:36; Ost DE, et al. Am J Respir Crit Care Med. 2016;193[1]:68). Despite the discordant history of efficacy of PLL sampling modalities, they have gained widespread adoption due to the increasing need to access the periphery. That said, many operators have been left wanting, making new technologies attractive options despite a lack of data. The emergence of RBS may present an opportunity to change the way we approach bronchoscopic procedures, making what was a manual procedure into one the is machine-assisted and, perhaps, improving our accuracy of repetition. The robotic age of lung medicine is an exciting proposition, however, it is paramount that we pursue a robust evidence-based strategy with multicentered clinical trials and move beyond the limitations of registry data in order to carefully embrace these new technologies.
Christina MacRosty, DO
Incoming Fellow-in-Training Member
Jason Akulian, MD, MPH, FCCP
Steering Committee Member
Pediatric Chest Medicine
PARDS: A new definition
Pediatric Acute Respiratory Distress Syndrome (PARDS) is a multifactorial clinical syndrome associated with high morbidity and mortality in children. It is caused by disruption of the alveolar epithelial–endothelial permeability barrier leading to accumulation of protein-rich fluid in the alveoli and surfactant degradation. These changes result in a restrictive lung disease characterized by hypoxemia, radiographic opacities, decreased FRC, and lung compliance and increased physiologic dead space. Resolution usually occurs after several weeks, with potential development of fibrosis. The most common cause of ARDS in children is viral respiratory infection, although associated with many underlying conditions, including pneumonia, sepsis, trauma, burns, pancreatitis, inhalation, transfusion, and cardiopulmonary bypass.
In 2015, an international panel of experts convened the Pediatric Acute Lung Injury Consensus Conference (PALICC) to establish new definitions and guidelines for PARDS. The 2015 PALICC definition broadens to include any new parenchymal infiltrate(s) and allows use of pulse oximetry to avoid underestimating ARDS prevalence in children. It also allows utilization of the oxygenation index (OI) and oxygenation saturation index (OSI) rather than the PaO2/Fio2 (P/F) ratio to assess hypoxemia (PARDS: consensus. Pediatr Crit Care Med. 2015;16[5]:428; Orloff et al. Pediatr Allergy Immunol Pulmonol. 2019;32[2]:35).
In a follow-up international, prospective, cross-sectional, observational study across 27 countries, the PALICC definition identified more children as having PARDS than the Berlin definition. The PALICC PARDS severity groupings improved mortality risk stratification. The PALICC PARDS framework appears to be a better tool for future epidemiologic and therapeutic research among children with PARDS (Khemani et al. Lancet Respir Med. 2019;7[2]:115).
Harish Rao, MD
Steering Committee Member
SEVEN people have died! Need action now
Pediatricians nationwide have raised the alarm as the numbers of middle- and high-school students who are vaping continues to skyrocket. The National Youth Tobacco survey (2018) showed a 78 % increase in e-cigarette use in high school students with a 48 % increase in middle school students between 2017-2018. Now considered a public health crisis with hundreds of cases of severe respiratory illnesses and seven deaths linked to vaping, physicians, legislators, educators, and respiratory health organizations are joining forces to curb its use in adolescents.
The American College of Chest Physicians has long supported regulation of e-cigarettes, joining the Forum of International Respiratory Societies in a position statement recommending bans on flavored e-cigarettes and the restricting use in areas where children are present.
The Administration announced this week its intention to “ clear the market “ of all flavored e-cigarettes. Sweet and fruit flavorings are known to entice adolescents to try e-cigarettes while the variety and ability to choose their own combinations of flavors continues to bring teens back again and again. We know that the brain continues to develop into our mid-twenties, causing teens to be more vulnerable to the addictive properties of nicotine.
Increasing numbers of exposures in adolescents and the severity of vaping-related illnesses have prompted states to take a proactive approach to keep e-cigarettes out of the hands of children. Michigan was the first state to ban the sale of flavored e-cigarettes online and in brick and mortar stores with compliance to take effect within the next 30 days. Other states are expected to follow suit.
Legislation is an important step in our efforts to curb vaping and protect our children.
Mary Cataletto MD, FAAP, FCCP
NetWork Chair
Pulmonary Physiology, Function and Rehabilitation
Pulmonary rehab and COPD
The introduction of pulmonary rehabilitation (PR) into the care of a patient with COPD can be a life-changing intervention. It has not only been shown to significantly improve symptoms, daily function, and quality of life – but also reduce the risk of acute exacerbation (Spruit et al. Am J Respir Crit Care Med. 2013;188[8]:e13). However, the referral rate for PR is extremely low, and many patients with COPD, despite having high symptom burdens, may be unaware of its existence. Unfortunately, this problem is worsened by PR program availability and proximity, with recent estimates suggesting that there are only 831 PR centers in the US for 24 million patients with COPD (Bhatt. Ann Am Thorac Soc. 2019;16[1]:55). As a result, there is an immediate need to explore alternative strategies that enable patients to realize the benefits of PR outside of a facility-based program (Rochester, et al. Am J Respir Crit Care Med. 2015;192[11]:1373).
Recently, there have been many proposals for adapting PR programs to accommodate the maximum number of participants; these have included home-, telehealth- or internet-based programs, and low-impact exercise (eg, yoga or tai-chi) regimens. While these interventions may benefit our patients with COPD, current data do not support that they are a replacement for or replicate the robust outcomes of a formal PR program. It is important that in the process of expanding the availability of “pulmonary rehab,” we do not dilute the process as to limit its returns. Significant attention is being paid to developing novel program designs that utilize technology and nonfacility-based programs – and in the end, there will be a balance struck between beneficial outcomes, program personalization, and proper patient selection for a given regimen.
Eric Gartman, MD, FCCP
Steering Committee Member
Thoracic Oncology
A new era in lung cancer diagnostics: Robotic-assisted bronchoscopy
Lung cancer screening leads to increased detection of early stage lung cancer (LC). The majority of nodules detected are peripherally located.
Image-guided bronchoscopic modalities, including radial probe endobronchial ultrasound (r-EBUS) and electromagnetic navigation bronchoscopy (ENB), allow diagnosis of peripheral nodules with a low rate of complications. Although a meta-analysis of image-guided bronchoscopic procedures reported a diagnostic yield of 70% (Wang Memoli JS, et al. Chest. 2012;142[2]:385), the diagnostic yield remains inferior to CT-guided biopsy. Robotic-assisted bronchoscopy (RAB) with four-way steering, 180 degrees of deflection in any direction and better access to peripheral airways may improve the diagnostic yield. Two FDA-approved platforms are commercially available. The Monarch System, (Auris Health) has a 3.2-mm outer diameter and a 1.2-mm working channel. Results from an ongoing prospective, multicenter study in 24 patients revealed successful localization of targeted lesion in 92%, with no significant adverse events (Chen, et al. Am J Respir Crit Care Med. 2019;199:A7304/NCT03727425; Clinical Trials. 2019. https://clinicaltrials.gov/ct2/show/NCT03727425).
The Ion Endoluminal System (Intuitive Surgical) has a 3.5-mm outer diameter and a 2.0-mm working channel. Preliminary data revealed 96.6% of target lesions were successfully reached, and no adverse events (Fielding et al. Chest. 2017;152[4]:A858). A prospective, multicenter randomized trial is currently ongoing (Clinical Trials. 2019. https://clinicaltrials.gov/ct2/show/NCT03893539).
The aim of bronchoscopic procedures is to safely and effectively diagnose early stage LC. RAB shows a great deal of potential in the future of LC diagnostics.
Priya Patel MD
Fellow-in-Training Member
Adnan Majid, MD
NetWork Member
Interventional Chest/Diagnostic Procedures
Emergence of robotic-assisted bronchoscopy for the diagnosis of peripheral lung lesions
The diagnostic chest medicine community saw exciting advances in technology for diagnosis of peripheral lung lesions (PLL) with the recent FDA approval of two robotic-assisted bronchoscopy systems (RBS): the Monarch Platform from Auris Health (2018) and the Ion system from Intuitive Surgical (2019). Small pilot studies of 15 (Monarch) and 29 (Ion) subjects, respectively, demonstrated safety and feasibility of biopsy and diagnosis of PLL using RBS (Rojas-Solano, et al. J Bronchol Intervent Pulmonol. 2018;25:168; Fielding et al. Respiration. 2019;98[2]:142). While these studies were not powered to evaluate diagnostic yield, they suggested the potential for improved yields over current technologies.
Current bronchoscopic modalities for diagnosis of PLL include electromagnetic navigation bronchoscopy, radial endobronchial ultrasound, and fluoroscopic guidance, all of which have favorable safety profiles but have been plagued by a wide range in diagnostic yields (38% to 88%) (Eberhardt R, et al. Am J Respir Crit Med. 2007;176[1]:36; Ost DE, et al. Am J Respir Crit Care Med. 2016;193[1]:68). Despite the discordant history of efficacy of PLL sampling modalities, they have gained widespread adoption due to the increasing need to access the periphery. That said, many operators have been left wanting, making new technologies attractive options despite a lack of data. The emergence of RBS may present an opportunity to change the way we approach bronchoscopic procedures, making what was a manual procedure into one the is machine-assisted and, perhaps, improving our accuracy of repetition. The robotic age of lung medicine is an exciting proposition, however, it is paramount that we pursue a robust evidence-based strategy with multicentered clinical trials and move beyond the limitations of registry data in order to carefully embrace these new technologies.
Christina MacRosty, DO
Incoming Fellow-in-Training Member
Jason Akulian, MD, MPH, FCCP
Steering Committee Member
Pediatric Chest Medicine
PARDS: A new definition
Pediatric Acute Respiratory Distress Syndrome (PARDS) is a multifactorial clinical syndrome associated with high morbidity and mortality in children. It is caused by disruption of the alveolar epithelial–endothelial permeability barrier leading to accumulation of protein-rich fluid in the alveoli and surfactant degradation. These changes result in a restrictive lung disease characterized by hypoxemia, radiographic opacities, decreased FRC, and lung compliance and increased physiologic dead space. Resolution usually occurs after several weeks, with potential development of fibrosis. The most common cause of ARDS in children is viral respiratory infection, although associated with many underlying conditions, including pneumonia, sepsis, trauma, burns, pancreatitis, inhalation, transfusion, and cardiopulmonary bypass.
In 2015, an international panel of experts convened the Pediatric Acute Lung Injury Consensus Conference (PALICC) to establish new definitions and guidelines for PARDS. The 2015 PALICC definition broadens to include any new parenchymal infiltrate(s) and allows use of pulse oximetry to avoid underestimating ARDS prevalence in children. It also allows utilization of the oxygenation index (OI) and oxygenation saturation index (OSI) rather than the PaO2/Fio2 (P/F) ratio to assess hypoxemia (PARDS: consensus. Pediatr Crit Care Med. 2015;16[5]:428; Orloff et al. Pediatr Allergy Immunol Pulmonol. 2019;32[2]:35).
In a follow-up international, prospective, cross-sectional, observational study across 27 countries, the PALICC definition identified more children as having PARDS than the Berlin definition. The PALICC PARDS severity groupings improved mortality risk stratification. The PALICC PARDS framework appears to be a better tool for future epidemiologic and therapeutic research among children with PARDS (Khemani et al. Lancet Respir Med. 2019;7[2]:115).
Harish Rao, MD
Steering Committee Member
SEVEN people have died! Need action now
Pediatricians nationwide have raised the alarm as the numbers of middle- and high-school students who are vaping continues to skyrocket. The National Youth Tobacco survey (2018) showed a 78 % increase in e-cigarette use in high school students with a 48 % increase in middle school students between 2017-2018. Now considered a public health crisis with hundreds of cases of severe respiratory illnesses and seven deaths linked to vaping, physicians, legislators, educators, and respiratory health organizations are joining forces to curb its use in adolescents.
The American College of Chest Physicians has long supported regulation of e-cigarettes, joining the Forum of International Respiratory Societies in a position statement recommending bans on flavored e-cigarettes and the restricting use in areas where children are present.
The Administration announced this week its intention to “ clear the market “ of all flavored e-cigarettes. Sweet and fruit flavorings are known to entice adolescents to try e-cigarettes while the variety and ability to choose their own combinations of flavors continues to bring teens back again and again. We know that the brain continues to develop into our mid-twenties, causing teens to be more vulnerable to the addictive properties of nicotine.
Increasing numbers of exposures in adolescents and the severity of vaping-related illnesses have prompted states to take a proactive approach to keep e-cigarettes out of the hands of children. Michigan was the first state to ban the sale of flavored e-cigarettes online and in brick and mortar stores with compliance to take effect within the next 30 days. Other states are expected to follow suit.
Legislation is an important step in our efforts to curb vaping and protect our children.
Mary Cataletto MD, FAAP, FCCP
NetWork Chair
Pulmonary Physiology, Function and Rehabilitation
Pulmonary rehab and COPD
The introduction of pulmonary rehabilitation (PR) into the care of a patient with COPD can be a life-changing intervention. It has not only been shown to significantly improve symptoms, daily function, and quality of life – but also reduce the risk of acute exacerbation (Spruit et al. Am J Respir Crit Care Med. 2013;188[8]:e13). However, the referral rate for PR is extremely low, and many patients with COPD, despite having high symptom burdens, may be unaware of its existence. Unfortunately, this problem is worsened by PR program availability and proximity, with recent estimates suggesting that there are only 831 PR centers in the US for 24 million patients with COPD (Bhatt. Ann Am Thorac Soc. 2019;16[1]:55). As a result, there is an immediate need to explore alternative strategies that enable patients to realize the benefits of PR outside of a facility-based program (Rochester, et al. Am J Respir Crit Care Med. 2015;192[11]:1373).
Recently, there have been many proposals for adapting PR programs to accommodate the maximum number of participants; these have included home-, telehealth- or internet-based programs, and low-impact exercise (eg, yoga or tai-chi) regimens. While these interventions may benefit our patients with COPD, current data do not support that they are a replacement for or replicate the robust outcomes of a formal PR program. It is important that in the process of expanding the availability of “pulmonary rehab,” we do not dilute the process as to limit its returns. Significant attention is being paid to developing novel program designs that utilize technology and nonfacility-based programs – and in the end, there will be a balance struck between beneficial outcomes, program personalization, and proper patient selection for a given regimen.
Eric Gartman, MD, FCCP
Steering Committee Member
Thoracic Oncology
A new era in lung cancer diagnostics: Robotic-assisted bronchoscopy
Lung cancer screening leads to increased detection of early stage lung cancer (LC). The majority of nodules detected are peripherally located.
Image-guided bronchoscopic modalities, including radial probe endobronchial ultrasound (r-EBUS) and electromagnetic navigation bronchoscopy (ENB), allow diagnosis of peripheral nodules with a low rate of complications. Although a meta-analysis of image-guided bronchoscopic procedures reported a diagnostic yield of 70% (Wang Memoli JS, et al. Chest. 2012;142[2]:385), the diagnostic yield remains inferior to CT-guided biopsy. Robotic-assisted bronchoscopy (RAB) with four-way steering, 180 degrees of deflection in any direction and better access to peripheral airways may improve the diagnostic yield. Two FDA-approved platforms are commercially available. The Monarch System, (Auris Health) has a 3.2-mm outer diameter and a 1.2-mm working channel. Results from an ongoing prospective, multicenter study in 24 patients revealed successful localization of targeted lesion in 92%, with no significant adverse events (Chen, et al. Am J Respir Crit Care Med. 2019;199:A7304/NCT03727425; Clinical Trials. 2019. https://clinicaltrials.gov/ct2/show/NCT03727425).
The Ion Endoluminal System (Intuitive Surgical) has a 3.5-mm outer diameter and a 2.0-mm working channel. Preliminary data revealed 96.6% of target lesions were successfully reached, and no adverse events (Fielding et al. Chest. 2017;152[4]:A858). A prospective, multicenter randomized trial is currently ongoing (Clinical Trials. 2019. https://clinicaltrials.gov/ct2/show/NCT03893539).
The aim of bronchoscopic procedures is to safely and effectively diagnose early stage LC. RAB shows a great deal of potential in the future of LC diagnostics.
Priya Patel MD
Fellow-in-Training Member
Adnan Majid, MD
NetWork Member
Interventional Chest/Diagnostic Procedures
Emergence of robotic-assisted bronchoscopy for the diagnosis of peripheral lung lesions
The diagnostic chest medicine community saw exciting advances in technology for diagnosis of peripheral lung lesions (PLL) with the recent FDA approval of two robotic-assisted bronchoscopy systems (RBS): the Monarch Platform from Auris Health (2018) and the Ion system from Intuitive Surgical (2019). Small pilot studies of 15 (Monarch) and 29 (Ion) subjects, respectively, demonstrated safety and feasibility of biopsy and diagnosis of PLL using RBS (Rojas-Solano, et al. J Bronchol Intervent Pulmonol. 2018;25:168; Fielding et al. Respiration. 2019;98[2]:142). While these studies were not powered to evaluate diagnostic yield, they suggested the potential for improved yields over current technologies.
Current bronchoscopic modalities for diagnosis of PLL include electromagnetic navigation bronchoscopy, radial endobronchial ultrasound, and fluoroscopic guidance, all of which have favorable safety profiles but have been plagued by a wide range in diagnostic yields (38% to 88%) (Eberhardt R, et al. Am J Respir Crit Med. 2007;176[1]:36; Ost DE, et al. Am J Respir Crit Care Med. 2016;193[1]:68). Despite the discordant history of efficacy of PLL sampling modalities, they have gained widespread adoption due to the increasing need to access the periphery. That said, many operators have been left wanting, making new technologies attractive options despite a lack of data. The emergence of RBS may present an opportunity to change the way we approach bronchoscopic procedures, making what was a manual procedure into one the is machine-assisted and, perhaps, improving our accuracy of repetition. The robotic age of lung medicine is an exciting proposition, however, it is paramount that we pursue a robust evidence-based strategy with multicentered clinical trials and move beyond the limitations of registry data in order to carefully embrace these new technologies.
Christina MacRosty, DO
Incoming Fellow-in-Training Member
Jason Akulian, MD, MPH, FCCP
Steering Committee Member
Pediatric Chest Medicine
PARDS: A new definition
Pediatric Acute Respiratory Distress Syndrome (PARDS) is a multifactorial clinical syndrome associated with high morbidity and mortality in children. It is caused by disruption of the alveolar epithelial–endothelial permeability barrier leading to accumulation of protein-rich fluid in the alveoli and surfactant degradation. These changes result in a restrictive lung disease characterized by hypoxemia, radiographic opacities, decreased FRC, and lung compliance and increased physiologic dead space. Resolution usually occurs after several weeks, with potential development of fibrosis. The most common cause of ARDS in children is viral respiratory infection, although associated with many underlying conditions, including pneumonia, sepsis, trauma, burns, pancreatitis, inhalation, transfusion, and cardiopulmonary bypass.
In 2015, an international panel of experts convened the Pediatric Acute Lung Injury Consensus Conference (PALICC) to establish new definitions and guidelines for PARDS. The 2015 PALICC definition broadens to include any new parenchymal infiltrate(s) and allows use of pulse oximetry to avoid underestimating ARDS prevalence in children. It also allows utilization of the oxygenation index (OI) and oxygenation saturation index (OSI) rather than the PaO2/Fio2 (P/F) ratio to assess hypoxemia (PARDS: consensus. Pediatr Crit Care Med. 2015;16[5]:428; Orloff et al. Pediatr Allergy Immunol Pulmonol. 2019;32[2]:35).
In a follow-up international, prospective, cross-sectional, observational study across 27 countries, the PALICC definition identified more children as having PARDS than the Berlin definition. The PALICC PARDS severity groupings improved mortality risk stratification. The PALICC PARDS framework appears to be a better tool for future epidemiologic and therapeutic research among children with PARDS (Khemani et al. Lancet Respir Med. 2019;7[2]:115).
Harish Rao, MD
Steering Committee Member
SEVEN people have died! Need action now
Pediatricians nationwide have raised the alarm as the numbers of middle- and high-school students who are vaping continues to skyrocket. The National Youth Tobacco survey (2018) showed a 78 % increase in e-cigarette use in high school students with a 48 % increase in middle school students between 2017-2018. Now considered a public health crisis with hundreds of cases of severe respiratory illnesses and seven deaths linked to vaping, physicians, legislators, educators, and respiratory health organizations are joining forces to curb its use in adolescents.
The American College of Chest Physicians has long supported regulation of e-cigarettes, joining the Forum of International Respiratory Societies in a position statement recommending bans on flavored e-cigarettes and the restricting use in areas where children are present.
The Administration announced this week its intention to “ clear the market “ of all flavored e-cigarettes. Sweet and fruit flavorings are known to entice adolescents to try e-cigarettes while the variety and ability to choose their own combinations of flavors continues to bring teens back again and again. We know that the brain continues to develop into our mid-twenties, causing teens to be more vulnerable to the addictive properties of nicotine.
Increasing numbers of exposures in adolescents and the severity of vaping-related illnesses have prompted states to take a proactive approach to keep e-cigarettes out of the hands of children. Michigan was the first state to ban the sale of flavored e-cigarettes online and in brick and mortar stores with compliance to take effect within the next 30 days. Other states are expected to follow suit.
Legislation is an important step in our efforts to curb vaping and protect our children.
Mary Cataletto MD, FAAP, FCCP
NetWork Chair
Pulmonary Physiology, Function and Rehabilitation
Pulmonary rehab and COPD
The introduction of pulmonary rehabilitation (PR) into the care of a patient with COPD can be a life-changing intervention. It has not only been shown to significantly improve symptoms, daily function, and quality of life – but also reduce the risk of acute exacerbation (Spruit et al. Am J Respir Crit Care Med. 2013;188[8]:e13). However, the referral rate for PR is extremely low, and many patients with COPD, despite having high symptom burdens, may be unaware of its existence. Unfortunately, this problem is worsened by PR program availability and proximity, with recent estimates suggesting that there are only 831 PR centers in the US for 24 million patients with COPD (Bhatt. Ann Am Thorac Soc. 2019;16[1]:55). As a result, there is an immediate need to explore alternative strategies that enable patients to realize the benefits of PR outside of a facility-based program (Rochester, et al. Am J Respir Crit Care Med. 2015;192[11]:1373).
Recently, there have been many proposals for adapting PR programs to accommodate the maximum number of participants; these have included home-, telehealth- or internet-based programs, and low-impact exercise (eg, yoga or tai-chi) regimens. While these interventions may benefit our patients with COPD, current data do not support that they are a replacement for or replicate the robust outcomes of a formal PR program. It is important that in the process of expanding the availability of “pulmonary rehab,” we do not dilute the process as to limit its returns. Significant attention is being paid to developing novel program designs that utilize technology and nonfacility-based programs – and in the end, there will be a balance struck between beneficial outcomes, program personalization, and proper patient selection for a given regimen.
Eric Gartman, MD, FCCP
Steering Committee Member
Thoracic Oncology
A new era in lung cancer diagnostics: Robotic-assisted bronchoscopy
Lung cancer screening leads to increased detection of early stage lung cancer (LC). The majority of nodules detected are peripherally located.
Image-guided bronchoscopic modalities, including radial probe endobronchial ultrasound (r-EBUS) and electromagnetic navigation bronchoscopy (ENB), allow diagnosis of peripheral nodules with a low rate of complications. Although a meta-analysis of image-guided bronchoscopic procedures reported a diagnostic yield of 70% (Wang Memoli JS, et al. Chest. 2012;142[2]:385), the diagnostic yield remains inferior to CT-guided biopsy. Robotic-assisted bronchoscopy (RAB) with four-way steering, 180 degrees of deflection in any direction and better access to peripheral airways may improve the diagnostic yield. Two FDA-approved platforms are commercially available. The Monarch System, (Auris Health) has a 3.2-mm outer diameter and a 1.2-mm working channel. Results from an ongoing prospective, multicenter study in 24 patients revealed successful localization of targeted lesion in 92%, with no significant adverse events (Chen, et al. Am J Respir Crit Care Med. 2019;199:A7304/NCT03727425; Clinical Trials. 2019. https://clinicaltrials.gov/ct2/show/NCT03727425).
The Ion Endoluminal System (Intuitive Surgical) has a 3.5-mm outer diameter and a 2.0-mm working channel. Preliminary data revealed 96.6% of target lesions were successfully reached, and no adverse events (Fielding et al. Chest. 2017;152[4]:A858). A prospective, multicenter randomized trial is currently ongoing (Clinical Trials. 2019. https://clinicaltrials.gov/ct2/show/NCT03893539).
The aim of bronchoscopic procedures is to safely and effectively diagnose early stage LC. RAB shows a great deal of potential in the future of LC diagnostics.
Priya Patel MD
Fellow-in-Training Member
Adnan Majid, MD
NetWork Member
This month in the journal CHEST®
Editor’s picks
ORIGINAL RESEARCH
The Saint Georges Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared to the classic definition. By Dr. V. Kim, et al.
Confocal laser endomicroscopy (CLE) as a guidance tool for pleural biopsies in malignant pleural mesothelioma. By Dr. L. Wijmans, et al.
Association of Angiotensin Modulators With the Course of Idiopathic Pulmonary Fibrosis. By Dr. M. Kreuter, et al.
Age-Stratified National Trends in Pulmonary Embolism Admissions. By Dr. E. D. Pauley, et al.
COMMENTARY
Solving the Opioid Crisis: Respiratory Depression by Opioids as Critical Endpoint.By Dr. G. Montandon and Dr. A. S. Slutsky.
Editor’s picks
Editor’s picks
ORIGINAL RESEARCH
The Saint Georges Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared to the classic definition. By Dr. V. Kim, et al.
Confocal laser endomicroscopy (CLE) as a guidance tool for pleural biopsies in malignant pleural mesothelioma. By Dr. L. Wijmans, et al.
Association of Angiotensin Modulators With the Course of Idiopathic Pulmonary Fibrosis. By Dr. M. Kreuter, et al.
Age-Stratified National Trends in Pulmonary Embolism Admissions. By Dr. E. D. Pauley, et al.
COMMENTARY
Solving the Opioid Crisis: Respiratory Depression by Opioids as Critical Endpoint.By Dr. G. Montandon and Dr. A. S. Slutsky.
ORIGINAL RESEARCH
The Saint Georges Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared to the classic definition. By Dr. V. Kim, et al.
Confocal laser endomicroscopy (CLE) as a guidance tool for pleural biopsies in malignant pleural mesothelioma. By Dr. L. Wijmans, et al.
Association of Angiotensin Modulators With the Course of Idiopathic Pulmonary Fibrosis. By Dr. M. Kreuter, et al.
Age-Stratified National Trends in Pulmonary Embolism Admissions. By Dr. E. D. Pauley, et al.
COMMENTARY
Solving the Opioid Crisis: Respiratory Depression by Opioids as Critical Endpoint.By Dr. G. Montandon and Dr. A. S. Slutsky.
E-cigarette-associated respiratory diseases: Ask your patients about vaping substances via e-cigarettes
E-cigarettes arrived in the U.S. market between 2005 and 2007. Vaping via e-cigarettes involves inhaling substances such as nicotine, flavorings, chemicals, and, sometimes, marijuana and/or other substances deep into the lungs. While the use of these devices is prevalent, the long-term effects are not known. We, as clinicians, need to specifically ask our patients about their use of substances via e-cigarettes because of alarming cases of severe, life-threatening respiratory illnesses recently being reported throughout the United States in young, otherwise healthy, individuals.
As of September 11, 2019, over 380 cases have been reported to the Centers for Disease Control and Prevention (CDC), where young, healthy people from 33 states and one US territory were hospitalized with severe respiratory disease. There have been at least six confirmed deaths and approximately one-third of those who survived required aggressive support with intubation and mechanical ventilation. The number of reported cases is rapidly rising (from 215 possible cases on August 27, 2019). The common theme in these cases is that every patient reported using an e-cigarette product within 90 days of the onset of symptoms, and most within the prior 2 weeks. By definition, other etiologies of respiratory failure, such as infections, collagen vascular, immunologic diseases, and malignancies were excluded.
Between 90% and 98% of patients presented to the hospital with respiratory symptoms, such as shortness of breath, cough, hemoptysis, and/or chest pain. The most common reported e-cigarette product exposure among these case patients is tetrahydrocannabinol, THC (in approximately 80% to 85%); however, some used only nicotine-based products (15% to 20%). In addition, approximately 45% to 50% reported using THC and nicotine-based products. One concerning fact that requires special attention is that some affected patients initially presented with nonrespiratory complaints, such as GI symptoms of nausea, vomiting, and/or diarrhea; constitutional symptoms such as fever (up to 104oF), fatigue, and/or weight loss; and neurologic symptoms such as headaches and even seizures. Many of these symptoms preceded the respiratory symptoms by up to 2 weeks. Therefore, a few of these patients initially presented without significant respiratory symptoms and with normal chest radiographs – but progressed over days to weeks to acute hypoxemic respiratory failure.
Up to 75% of the affected patients who ultimately required hospitalization for e-cigarette-associated respiratory disease initially presented to a primary care clinic or ED and were sent home due to nonspecific signs and symptoms, which mimic common viral illnesses. Therefore, it is critical for all health-care professionals to have a high clinical suspicion for e-cigarette-associated respiratory disease, particularly while more data are being gathered. When suspected, the CDC recommends asking patients about specific substances inhaled, the manufacturer, where the products/cartridges were obtained, type of device(s) used, and method used (ie, aerosolization, dabbing, dripping, etc).
The most common types of imaging and pathologic patterns attributed to e-cigarette use reported to date include lipoid pneumonia, diffuse alveolar damage, acute
respiratory distress syndrome (ARDS), diffuse alveolar hemorrhage (DAH), acute eosinophilic pneumonia, hypersensitivity pneumonitis, and organizing pneumonia. The most common patterns on imaging include basilar-predominant consolidation and ground-glass opacities with areas of subpleural sparing. In addition, approximately 10% to 15% of the reported cases had a spontaneous pneumothorax, pneumomediastinum, and/or associated pleural effusions. Bronchoscopy specimens, such as bronchoalveolar lavage (BAL) and transbronchial biopsies (TBBx), were often but not always obtained. In patients who underwent bronchoscopy; many were found to have lipid-laden alveolar macrophages. These findings were discovered by staining fresh (ie, those not placed in fixative) specimens from BAL and/or TBBx for lipids with oil red O or another stain to specifically detect fat within the samples. Other etiologies of these radiographic/pathologic patterns and conditions should be excluded, as listed above.
The clinical course varies widely among these reported cases of vaping and e-cigarette-associated respiratory diseases. A minority of the reported patients spontaneously improved, and others required significant supportive care – from supplemental oxygen to complete support with ECMO. Some were treated with systemic corticosteroids with a wide range of responses and with various dosages: from prednisone of 0.5 to 1 mg/kg up to pulse-dose steroids with 1 g methylprednisolone for 3 days with a slow taper.
The information and data reported about these e-cigarette-associated respiratory diseases are clearly evolving quickly and vary from center to center and state to state. All suspected cases should be reported to your state health department. Similar to other inhalational injuries, it is critical to monitor these patients following recovery from the acute illness to help determine the long-term pulmonary effects and clinical courses of these individuals. Offering assistance and treatment for addiction is also important in these patients to help reduce their chances of recurrent respiratory problems from ongoing exposure to these substances in e-cigarettes. The bottom line is that cases of e-cigarette-associated respiratory diseases are increasing rapidly throughout the United States. Therefore, we should all be vigilant about asking our patients about their use of these substances and providing clear and strong messages for each of our patients to avoid vaping any substances through e-cigarettes.
Dr. Adams is Professor of Medicine, Pulmonary/Critical Care Division, Distinguished Teaching Professor, UT Health San Antonio; Staff Physician, South Texas Veterans Health Care System, San Antonio, Texas
References
Centers for Disease Control and Prevention. Severe pulmonary disease associated with using e-cigarette products. Health Alert Network. August 30, 2019. CDCHAN-00421. .
https://emergency.cdc.gov/han/han00421.asp
Centers for Disease Control and Prevention. Outbreak of lung illness associated with using e-cigarette products. Investigation Notice. September 6, 2019. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
Henry TS et al. Imaging of vaping-associated lung disease. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1911995. [Epub ahead of print].
Layden JE et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614. [Epub ahead of print].
Maddock SD et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1912038. [Epub ahead of print].
E-cigarettes arrived in the U.S. market between 2005 and 2007. Vaping via e-cigarettes involves inhaling substances such as nicotine, flavorings, chemicals, and, sometimes, marijuana and/or other substances deep into the lungs. While the use of these devices is prevalent, the long-term effects are not known. We, as clinicians, need to specifically ask our patients about their use of substances via e-cigarettes because of alarming cases of severe, life-threatening respiratory illnesses recently being reported throughout the United States in young, otherwise healthy, individuals.
As of September 11, 2019, over 380 cases have been reported to the Centers for Disease Control and Prevention (CDC), where young, healthy people from 33 states and one US territory were hospitalized with severe respiratory disease. There have been at least six confirmed deaths and approximately one-third of those who survived required aggressive support with intubation and mechanical ventilation. The number of reported cases is rapidly rising (from 215 possible cases on August 27, 2019). The common theme in these cases is that every patient reported using an e-cigarette product within 90 days of the onset of symptoms, and most within the prior 2 weeks. By definition, other etiologies of respiratory failure, such as infections, collagen vascular, immunologic diseases, and malignancies were excluded.
Between 90% and 98% of patients presented to the hospital with respiratory symptoms, such as shortness of breath, cough, hemoptysis, and/or chest pain. The most common reported e-cigarette product exposure among these case patients is tetrahydrocannabinol, THC (in approximately 80% to 85%); however, some used only nicotine-based products (15% to 20%). In addition, approximately 45% to 50% reported using THC and nicotine-based products. One concerning fact that requires special attention is that some affected patients initially presented with nonrespiratory complaints, such as GI symptoms of nausea, vomiting, and/or diarrhea; constitutional symptoms such as fever (up to 104oF), fatigue, and/or weight loss; and neurologic symptoms such as headaches and even seizures. Many of these symptoms preceded the respiratory symptoms by up to 2 weeks. Therefore, a few of these patients initially presented without significant respiratory symptoms and with normal chest radiographs – but progressed over days to weeks to acute hypoxemic respiratory failure.
Up to 75% of the affected patients who ultimately required hospitalization for e-cigarette-associated respiratory disease initially presented to a primary care clinic or ED and were sent home due to nonspecific signs and symptoms, which mimic common viral illnesses. Therefore, it is critical for all health-care professionals to have a high clinical suspicion for e-cigarette-associated respiratory disease, particularly while more data are being gathered. When suspected, the CDC recommends asking patients about specific substances inhaled, the manufacturer, where the products/cartridges were obtained, type of device(s) used, and method used (ie, aerosolization, dabbing, dripping, etc).
The most common types of imaging and pathologic patterns attributed to e-cigarette use reported to date include lipoid pneumonia, diffuse alveolar damage, acute
respiratory distress syndrome (ARDS), diffuse alveolar hemorrhage (DAH), acute eosinophilic pneumonia, hypersensitivity pneumonitis, and organizing pneumonia. The most common patterns on imaging include basilar-predominant consolidation and ground-glass opacities with areas of subpleural sparing. In addition, approximately 10% to 15% of the reported cases had a spontaneous pneumothorax, pneumomediastinum, and/or associated pleural effusions. Bronchoscopy specimens, such as bronchoalveolar lavage (BAL) and transbronchial biopsies (TBBx), were often but not always obtained. In patients who underwent bronchoscopy; many were found to have lipid-laden alveolar macrophages. These findings were discovered by staining fresh (ie, those not placed in fixative) specimens from BAL and/or TBBx for lipids with oil red O or another stain to specifically detect fat within the samples. Other etiologies of these radiographic/pathologic patterns and conditions should be excluded, as listed above.
The clinical course varies widely among these reported cases of vaping and e-cigarette-associated respiratory diseases. A minority of the reported patients spontaneously improved, and others required significant supportive care – from supplemental oxygen to complete support with ECMO. Some were treated with systemic corticosteroids with a wide range of responses and with various dosages: from prednisone of 0.5 to 1 mg/kg up to pulse-dose steroids with 1 g methylprednisolone for 3 days with a slow taper.
The information and data reported about these e-cigarette-associated respiratory diseases are clearly evolving quickly and vary from center to center and state to state. All suspected cases should be reported to your state health department. Similar to other inhalational injuries, it is critical to monitor these patients following recovery from the acute illness to help determine the long-term pulmonary effects and clinical courses of these individuals. Offering assistance and treatment for addiction is also important in these patients to help reduce their chances of recurrent respiratory problems from ongoing exposure to these substances in e-cigarettes. The bottom line is that cases of e-cigarette-associated respiratory diseases are increasing rapidly throughout the United States. Therefore, we should all be vigilant about asking our patients about their use of these substances and providing clear and strong messages for each of our patients to avoid vaping any substances through e-cigarettes.
Dr. Adams is Professor of Medicine, Pulmonary/Critical Care Division, Distinguished Teaching Professor, UT Health San Antonio; Staff Physician, South Texas Veterans Health Care System, San Antonio, Texas
References
Centers for Disease Control and Prevention. Severe pulmonary disease associated with using e-cigarette products. Health Alert Network. August 30, 2019. CDCHAN-00421. .
https://emergency.cdc.gov/han/han00421.asp
Centers for Disease Control and Prevention. Outbreak of lung illness associated with using e-cigarette products. Investigation Notice. September 6, 2019. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
Henry TS et al. Imaging of vaping-associated lung disease. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1911995. [Epub ahead of print].
Layden JE et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614. [Epub ahead of print].
Maddock SD et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1912038. [Epub ahead of print].
E-cigarettes arrived in the U.S. market between 2005 and 2007. Vaping via e-cigarettes involves inhaling substances such as nicotine, flavorings, chemicals, and, sometimes, marijuana and/or other substances deep into the lungs. While the use of these devices is prevalent, the long-term effects are not known. We, as clinicians, need to specifically ask our patients about their use of substances via e-cigarettes because of alarming cases of severe, life-threatening respiratory illnesses recently being reported throughout the United States in young, otherwise healthy, individuals.
As of September 11, 2019, over 380 cases have been reported to the Centers for Disease Control and Prevention (CDC), where young, healthy people from 33 states and one US territory were hospitalized with severe respiratory disease. There have been at least six confirmed deaths and approximately one-third of those who survived required aggressive support with intubation and mechanical ventilation. The number of reported cases is rapidly rising (from 215 possible cases on August 27, 2019). The common theme in these cases is that every patient reported using an e-cigarette product within 90 days of the onset of symptoms, and most within the prior 2 weeks. By definition, other etiologies of respiratory failure, such as infections, collagen vascular, immunologic diseases, and malignancies were excluded.
Between 90% and 98% of patients presented to the hospital with respiratory symptoms, such as shortness of breath, cough, hemoptysis, and/or chest pain. The most common reported e-cigarette product exposure among these case patients is tetrahydrocannabinol, THC (in approximately 80% to 85%); however, some used only nicotine-based products (15% to 20%). In addition, approximately 45% to 50% reported using THC and nicotine-based products. One concerning fact that requires special attention is that some affected patients initially presented with nonrespiratory complaints, such as GI symptoms of nausea, vomiting, and/or diarrhea; constitutional symptoms such as fever (up to 104oF), fatigue, and/or weight loss; and neurologic symptoms such as headaches and even seizures. Many of these symptoms preceded the respiratory symptoms by up to 2 weeks. Therefore, a few of these patients initially presented without significant respiratory symptoms and with normal chest radiographs – but progressed over days to weeks to acute hypoxemic respiratory failure.
Up to 75% of the affected patients who ultimately required hospitalization for e-cigarette-associated respiratory disease initially presented to a primary care clinic or ED and were sent home due to nonspecific signs and symptoms, which mimic common viral illnesses. Therefore, it is critical for all health-care professionals to have a high clinical suspicion for e-cigarette-associated respiratory disease, particularly while more data are being gathered. When suspected, the CDC recommends asking patients about specific substances inhaled, the manufacturer, where the products/cartridges were obtained, type of device(s) used, and method used (ie, aerosolization, dabbing, dripping, etc).
The most common types of imaging and pathologic patterns attributed to e-cigarette use reported to date include lipoid pneumonia, diffuse alveolar damage, acute
respiratory distress syndrome (ARDS), diffuse alveolar hemorrhage (DAH), acute eosinophilic pneumonia, hypersensitivity pneumonitis, and organizing pneumonia. The most common patterns on imaging include basilar-predominant consolidation and ground-glass opacities with areas of subpleural sparing. In addition, approximately 10% to 15% of the reported cases had a spontaneous pneumothorax, pneumomediastinum, and/or associated pleural effusions. Bronchoscopy specimens, such as bronchoalveolar lavage (BAL) and transbronchial biopsies (TBBx), were often but not always obtained. In patients who underwent bronchoscopy; many were found to have lipid-laden alveolar macrophages. These findings were discovered by staining fresh (ie, those not placed in fixative) specimens from BAL and/or TBBx for lipids with oil red O or another stain to specifically detect fat within the samples. Other etiologies of these radiographic/pathologic patterns and conditions should be excluded, as listed above.
The clinical course varies widely among these reported cases of vaping and e-cigarette-associated respiratory diseases. A minority of the reported patients spontaneously improved, and others required significant supportive care – from supplemental oxygen to complete support with ECMO. Some were treated with systemic corticosteroids with a wide range of responses and with various dosages: from prednisone of 0.5 to 1 mg/kg up to pulse-dose steroids with 1 g methylprednisolone for 3 days with a slow taper.
The information and data reported about these e-cigarette-associated respiratory diseases are clearly evolving quickly and vary from center to center and state to state. All suspected cases should be reported to your state health department. Similar to other inhalational injuries, it is critical to monitor these patients following recovery from the acute illness to help determine the long-term pulmonary effects and clinical courses of these individuals. Offering assistance and treatment for addiction is also important in these patients to help reduce their chances of recurrent respiratory problems from ongoing exposure to these substances in e-cigarettes. The bottom line is that cases of e-cigarette-associated respiratory diseases are increasing rapidly throughout the United States. Therefore, we should all be vigilant about asking our patients about their use of these substances and providing clear and strong messages for each of our patients to avoid vaping any substances through e-cigarettes.
Dr. Adams is Professor of Medicine, Pulmonary/Critical Care Division, Distinguished Teaching Professor, UT Health San Antonio; Staff Physician, South Texas Veterans Health Care System, San Antonio, Texas
References
Centers for Disease Control and Prevention. Severe pulmonary disease associated with using e-cigarette products. Health Alert Network. August 30, 2019. CDCHAN-00421. .
https://emergency.cdc.gov/han/han00421.asp
Centers for Disease Control and Prevention. Outbreak of lung illness associated with using e-cigarette products. Investigation Notice. September 6, 2019. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
Henry TS et al. Imaging of vaping-associated lung disease. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1911995. [Epub ahead of print].
Layden JE et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614. [Epub ahead of print].
Maddock SD et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMc1912038. [Epub ahead of print].