User login
Lessons Learned From the Pediatric Overflow Planning Contingency Response Network: A Transdisciplinary Virtual Collaboration Addressing Health System Fragmentation and Disparity During the COVID-19 Pandemic
As the COVID-19 pandemic surged in March 2020 in the United States, it was clear that severe COVID-19 and rates of hospitalization were much higher in adults than in children.1 Pediatric facilities grappled with how to leverage empty beds and other underutilized human, clinical, and material resources to offset the overflowing adult facilities.2,3 Pediatricians agonized about how to identify adult patients for whom they could provide safe and effective care, not only as individual clinicians, but also with adequate support from their local pediatric facility and health system.
Maria* (*name changed) was a young adult whose experience with her local health system highlighted common and addressable issues that arose when pediatric facilities aimed to care for adult populations. Adult hospitals were already above capacity caring for acutely ill patients with COVID-19, and a local freestanding children’s hospital offered to offload young adult patients up to age 30 years. Maria, a 26-year-old, had just been transferred from an adult emergency department (ED) to the children’s hospital ED for management of postoperative pain after a recent appendectomy. There was concern for possible abscess formation, but no evidence of sepsis. During his oral presentation, a pediatric resident in the ED reported, “This patient has a history of drug abuse and should not be admitted to a children’s hospital. She has been demanding pain meds and I feel she would be better served at the adult hospital.”
At the intersection of these seemingly impossible questions, dually trained internal medicine and pediatrics (med-peds) physicians had a unique vantage point, as they were accustomed to bridging the divide between adult and pediatric medicine in their practices.
As POPCoRN members shared their challenges and institutional learnings, common themes were identified, such as management of intubated patients in non–intensive care unit (ICU) spaces; gaps in staffing with redeployment of residents and hospitalists; and dissemination of education, such as Advanced Cardiac Life Support (ACLS) webinars to frontline staff.
IDENTIFY THE “CORRECT” PATIENT POPULATION, BUT DO NOT LET PERFECTION BE A BARRIER TO PROGRESS
Many pediatric facilities reported perseveration over the adult age cutoff accepted to the pediatric facility, only to realize the initial arbitrary age cutoff usually did not encompass enough patients to benefit local adult health systems. Using only strict age cutoffs also created an unnecessary barrier to accepting otherwise appropriate adult patients (eg, adult patient with controlled hypertension and a soft tissue infection).
USE REPETITIVE STAKEHOLDER ANALYSIS TO ADAPT TO A RAPIDLY CHANGING ENVIRONMENT
The pandemic response was rapidly evolving and unpredictable. Planning required all affected parties at the table to effectively identify problems and solutions. Clinical and nonclinical groups were critical to planning operational logistics to provide safe care for adults in pediatric facilities.
COMMUNICATE WITH INTENTION AND TRANSPARENCY: WHEN LESS IS NOT MORE
Across care settings and training levels, the power of timely, honest, and transparent communication with leadership echoed throughout the network and could not be overemphasized. The cadence and modes of communication, while established by facility leaders, was best determined by explicitly asking team members for their needs. Often, leaders attempted to avoid communicating abrupt protocol changes to spare their teams additional stress and excessive correspondence. However, POPCoRN members found this approach often increased the perception among staff of a lack of transparency, which exacerbated feelings of discomfort and stress. While other specific examples of communication strategies are included in the POPCoRN guide, network members consistently noted that virtual open forums with leadership at regular intervals allowed teams to ask questions, raise concerns, and share ideas. In addition to open forums, leaders’ written communications regarding local medicolegal limitations and malpractice protection related to adult care should be distributed to staff. In Maria’s case, would provider discomfort and anxiety have been ameliorated with a proactive open forum to discuss the care of adults at the pediatric facility? Would that forum have called attention to staff educational and preparation needs around taking care of adults with a history substance use disorder? If so, this may have added a downstream benefit of decreasing effects of implicit bias amplified by stress.10
MAKE “JUST-IN-TIME” RESOURCES AVAILABLE FOR PEDIATRICIANS CARING FOR ADULT PATIENTS
DESIGN AN EMERGENCY RESPONSE SYSTEM FOR ADULT PATIENTS IN PEDIATRIC FACILITIES
CONCLUSION
Acknowledgments
Collaborators: All the collaborating authors listed below have contributed to the guide available in the appendix of the online version of this article, “Lessons Learned From COVID-19: A Practical Guide for Pediatric Facility Preparedness and Repurposing.” All the authors have provided consent to be listed.
Francisco Alvarez, MD, Stanford, California; Elizabeth Boggs, MD, MS, Aurora, Colorado; Rachel Boykan, MD, Stony Brook, New York; Alicia Caldwell, MD, Cincinnati, Ohio; Maryanne M. Chumpia, MD, MS, Torrance, California; Katharine N Clouser, MD, Hackensack, New Jersey; Alexandra L Coria, MD, Brooklyn, New York; Clare C Crosh, DO, Cincinnati, Ohio; Magna Dias, MD, Bridgeport, Connecticut; Laura N El-Hage, MD, Philadelphia, Pennsylvania; Jeff Foti, MD, Seattle, Washington; Mirna Giordano, MD, New York, New York; Sheena Gupta, MD, MBA, Evanston, Illinois; Laura Nell Hodo, MD, New York, New York; Ashley Jenkins, MD, MS, Rochester, New York; Anika Kumar, MD, Cleveland, Ohio; Merlin C Lowe, MD, Tuscon, Arizona; Brittany Middleton, MD, Pasadena, California; Sage Myers, MD, Philadelphia, Pennsylvania; Anik Patel, MD, Salt Lake City, Utah; Leah Ratner, MD, MS, Boston, Massachusetts; Shela Sridhar, MD, MPH, Boston, Massachusetts; Nathan Stehouwer, MD, Cleveland, Ohio; Julie Sylvester, DO, Mount Kisco, New York; Dava Szalda, MD, MSHP, Philadelphia, Pennsylvania; Heather Toth, MD, Milwaukee, Wisconsin; Krista Tuomela, MD, Milwaukee, Wisconsin; Ronald Williams, MD, Hershey, Pennsylvania.
1. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6):e20200702. https://doi.org/10.1542/peds.2020-0702
2. Osborn R, Doolittle B, Loyal J. When pediatric hospitalists took care of adults during the COVID-19 pandemic. Hosp Pediatr. 2021;11(1):e15-e18. https://doi.org/10.1542/hpeds.2020-001040
3. Yager PH, Whalen KA, Cummings BM. Repurposing a pediatric ICU for adults. N Engl J Med. 2020;382(22):e80. https://doi.org/10.1056/NEJMc2014819
4. Conway-Habes EE, Herbst BF Jr, Herbst LA, et al. Using quality improvement to introduce and standardize the National Early Warning Score (NEWS) for adult inpatients at a children’s hospital. Hosp Pediatr. 2017;7(3):156-163. https://doi.org/10.1542/hpeds.2016-0117
5. Kinnear B, O’Toole JK. Care of adults in children’s hospitals: acknowledging the aging elephant in the room. JAMA Pediatr. 2015;169(12):1081-1082. https://doi.org/10.1001/jamapediatrics.2015.2215
6. Szalda D, Steinway C, Greenberg A, et al. Developing a hospital-wide transition program for young adults with medical complexity. J Adolesc Health. 2019;65(4):476-482. https://doi.org/10.1016/j.jadohealth.2019.04.008
7. Jenkins A, Ratner L, Caldwell A, Sharma N, Uluer A, White C. Children’s hospitals caring for adults during a pandemic: pragmatic considerations and approaches. J Hosp Med. 2020;15(5):311-313. https://doi.org/10.12788/jhm.3432
8. Botwinick L, Bisognano M, Haraden C. Leadership Guide to Patient Safety. IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2006. Accessed January 20, 2021. http://www.ihi.org/resources/Pages/IHIWhitePapers/LeadershipGuidetoPatientSafetyWhitePaper.aspx
9. Essien UR, Eneanya ND, Crews DC. Prioritizing equity in a time of scarcity: the COVID-19 pandemic. J Gen Intern Med. 2020;35(9):2760-2762. https://doi.org/10.1007/s11606-020-05976-y
10. Yu R. Stress potentiates decision biases: a stress induced deliberation-to-intuition (SIDI) model. Neurobiol Stress. 2016;3:83-95. https://doi.org/10.1016/j.ynstr.2015.12.006
As the COVID-19 pandemic surged in March 2020 in the United States, it was clear that severe COVID-19 and rates of hospitalization were much higher in adults than in children.1 Pediatric facilities grappled with how to leverage empty beds and other underutilized human, clinical, and material resources to offset the overflowing adult facilities.2,3 Pediatricians agonized about how to identify adult patients for whom they could provide safe and effective care, not only as individual clinicians, but also with adequate support from their local pediatric facility and health system.
Maria* (*name changed) was a young adult whose experience with her local health system highlighted common and addressable issues that arose when pediatric facilities aimed to care for adult populations. Adult hospitals were already above capacity caring for acutely ill patients with COVID-19, and a local freestanding children’s hospital offered to offload young adult patients up to age 30 years. Maria, a 26-year-old, had just been transferred from an adult emergency department (ED) to the children’s hospital ED for management of postoperative pain after a recent appendectomy. There was concern for possible abscess formation, but no evidence of sepsis. During his oral presentation, a pediatric resident in the ED reported, “This patient has a history of drug abuse and should not be admitted to a children’s hospital. She has been demanding pain meds and I feel she would be better served at the adult hospital.”
At the intersection of these seemingly impossible questions, dually trained internal medicine and pediatrics (med-peds) physicians had a unique vantage point, as they were accustomed to bridging the divide between adult and pediatric medicine in their practices.
As POPCoRN members shared their challenges and institutional learnings, common themes were identified, such as management of intubated patients in non–intensive care unit (ICU) spaces; gaps in staffing with redeployment of residents and hospitalists; and dissemination of education, such as Advanced Cardiac Life Support (ACLS) webinars to frontline staff.
IDENTIFY THE “CORRECT” PATIENT POPULATION, BUT DO NOT LET PERFECTION BE A BARRIER TO PROGRESS
Many pediatric facilities reported perseveration over the adult age cutoff accepted to the pediatric facility, only to realize the initial arbitrary age cutoff usually did not encompass enough patients to benefit local adult health systems. Using only strict age cutoffs also created an unnecessary barrier to accepting otherwise appropriate adult patients (eg, adult patient with controlled hypertension and a soft tissue infection).
USE REPETITIVE STAKEHOLDER ANALYSIS TO ADAPT TO A RAPIDLY CHANGING ENVIRONMENT
The pandemic response was rapidly evolving and unpredictable. Planning required all affected parties at the table to effectively identify problems and solutions. Clinical and nonclinical groups were critical to planning operational logistics to provide safe care for adults in pediatric facilities.
COMMUNICATE WITH INTENTION AND TRANSPARENCY: WHEN LESS IS NOT MORE
Across care settings and training levels, the power of timely, honest, and transparent communication with leadership echoed throughout the network and could not be overemphasized. The cadence and modes of communication, while established by facility leaders, was best determined by explicitly asking team members for their needs. Often, leaders attempted to avoid communicating abrupt protocol changes to spare their teams additional stress and excessive correspondence. However, POPCoRN members found this approach often increased the perception among staff of a lack of transparency, which exacerbated feelings of discomfort and stress. While other specific examples of communication strategies are included in the POPCoRN guide, network members consistently noted that virtual open forums with leadership at regular intervals allowed teams to ask questions, raise concerns, and share ideas. In addition to open forums, leaders’ written communications regarding local medicolegal limitations and malpractice protection related to adult care should be distributed to staff. In Maria’s case, would provider discomfort and anxiety have been ameliorated with a proactive open forum to discuss the care of adults at the pediatric facility? Would that forum have called attention to staff educational and preparation needs around taking care of adults with a history substance use disorder? If so, this may have added a downstream benefit of decreasing effects of implicit bias amplified by stress.10
MAKE “JUST-IN-TIME” RESOURCES AVAILABLE FOR PEDIATRICIANS CARING FOR ADULT PATIENTS
DESIGN AN EMERGENCY RESPONSE SYSTEM FOR ADULT PATIENTS IN PEDIATRIC FACILITIES
CONCLUSION
Acknowledgments
Collaborators: All the collaborating authors listed below have contributed to the guide available in the appendix of the online version of this article, “Lessons Learned From COVID-19: A Practical Guide for Pediatric Facility Preparedness and Repurposing.” All the authors have provided consent to be listed.
Francisco Alvarez, MD, Stanford, California; Elizabeth Boggs, MD, MS, Aurora, Colorado; Rachel Boykan, MD, Stony Brook, New York; Alicia Caldwell, MD, Cincinnati, Ohio; Maryanne M. Chumpia, MD, MS, Torrance, California; Katharine N Clouser, MD, Hackensack, New Jersey; Alexandra L Coria, MD, Brooklyn, New York; Clare C Crosh, DO, Cincinnati, Ohio; Magna Dias, MD, Bridgeport, Connecticut; Laura N El-Hage, MD, Philadelphia, Pennsylvania; Jeff Foti, MD, Seattle, Washington; Mirna Giordano, MD, New York, New York; Sheena Gupta, MD, MBA, Evanston, Illinois; Laura Nell Hodo, MD, New York, New York; Ashley Jenkins, MD, MS, Rochester, New York; Anika Kumar, MD, Cleveland, Ohio; Merlin C Lowe, MD, Tuscon, Arizona; Brittany Middleton, MD, Pasadena, California; Sage Myers, MD, Philadelphia, Pennsylvania; Anik Patel, MD, Salt Lake City, Utah; Leah Ratner, MD, MS, Boston, Massachusetts; Shela Sridhar, MD, MPH, Boston, Massachusetts; Nathan Stehouwer, MD, Cleveland, Ohio; Julie Sylvester, DO, Mount Kisco, New York; Dava Szalda, MD, MSHP, Philadelphia, Pennsylvania; Heather Toth, MD, Milwaukee, Wisconsin; Krista Tuomela, MD, Milwaukee, Wisconsin; Ronald Williams, MD, Hershey, Pennsylvania.
As the COVID-19 pandemic surged in March 2020 in the United States, it was clear that severe COVID-19 and rates of hospitalization were much higher in adults than in children.1 Pediatric facilities grappled with how to leverage empty beds and other underutilized human, clinical, and material resources to offset the overflowing adult facilities.2,3 Pediatricians agonized about how to identify adult patients for whom they could provide safe and effective care, not only as individual clinicians, but also with adequate support from their local pediatric facility and health system.
Maria* (*name changed) was a young adult whose experience with her local health system highlighted common and addressable issues that arose when pediatric facilities aimed to care for adult populations. Adult hospitals were already above capacity caring for acutely ill patients with COVID-19, and a local freestanding children’s hospital offered to offload young adult patients up to age 30 years. Maria, a 26-year-old, had just been transferred from an adult emergency department (ED) to the children’s hospital ED for management of postoperative pain after a recent appendectomy. There was concern for possible abscess formation, but no evidence of sepsis. During his oral presentation, a pediatric resident in the ED reported, “This patient has a history of drug abuse and should not be admitted to a children’s hospital. She has been demanding pain meds and I feel she would be better served at the adult hospital.”
At the intersection of these seemingly impossible questions, dually trained internal medicine and pediatrics (med-peds) physicians had a unique vantage point, as they were accustomed to bridging the divide between adult and pediatric medicine in their practices.
As POPCoRN members shared their challenges and institutional learnings, common themes were identified, such as management of intubated patients in non–intensive care unit (ICU) spaces; gaps in staffing with redeployment of residents and hospitalists; and dissemination of education, such as Advanced Cardiac Life Support (ACLS) webinars to frontline staff.
IDENTIFY THE “CORRECT” PATIENT POPULATION, BUT DO NOT LET PERFECTION BE A BARRIER TO PROGRESS
Many pediatric facilities reported perseveration over the adult age cutoff accepted to the pediatric facility, only to realize the initial arbitrary age cutoff usually did not encompass enough patients to benefit local adult health systems. Using only strict age cutoffs also created an unnecessary barrier to accepting otherwise appropriate adult patients (eg, adult patient with controlled hypertension and a soft tissue infection).
USE REPETITIVE STAKEHOLDER ANALYSIS TO ADAPT TO A RAPIDLY CHANGING ENVIRONMENT
The pandemic response was rapidly evolving and unpredictable. Planning required all affected parties at the table to effectively identify problems and solutions. Clinical and nonclinical groups were critical to planning operational logistics to provide safe care for adults in pediatric facilities.
COMMUNICATE WITH INTENTION AND TRANSPARENCY: WHEN LESS IS NOT MORE
Across care settings and training levels, the power of timely, honest, and transparent communication with leadership echoed throughout the network and could not be overemphasized. The cadence and modes of communication, while established by facility leaders, was best determined by explicitly asking team members for their needs. Often, leaders attempted to avoid communicating abrupt protocol changes to spare their teams additional stress and excessive correspondence. However, POPCoRN members found this approach often increased the perception among staff of a lack of transparency, which exacerbated feelings of discomfort and stress. While other specific examples of communication strategies are included in the POPCoRN guide, network members consistently noted that virtual open forums with leadership at regular intervals allowed teams to ask questions, raise concerns, and share ideas. In addition to open forums, leaders’ written communications regarding local medicolegal limitations and malpractice protection related to adult care should be distributed to staff. In Maria’s case, would provider discomfort and anxiety have been ameliorated with a proactive open forum to discuss the care of adults at the pediatric facility? Would that forum have called attention to staff educational and preparation needs around taking care of adults with a history substance use disorder? If so, this may have added a downstream benefit of decreasing effects of implicit bias amplified by stress.10
MAKE “JUST-IN-TIME” RESOURCES AVAILABLE FOR PEDIATRICIANS CARING FOR ADULT PATIENTS
DESIGN AN EMERGENCY RESPONSE SYSTEM FOR ADULT PATIENTS IN PEDIATRIC FACILITIES
CONCLUSION
Acknowledgments
Collaborators: All the collaborating authors listed below have contributed to the guide available in the appendix of the online version of this article, “Lessons Learned From COVID-19: A Practical Guide for Pediatric Facility Preparedness and Repurposing.” All the authors have provided consent to be listed.
Francisco Alvarez, MD, Stanford, California; Elizabeth Boggs, MD, MS, Aurora, Colorado; Rachel Boykan, MD, Stony Brook, New York; Alicia Caldwell, MD, Cincinnati, Ohio; Maryanne M. Chumpia, MD, MS, Torrance, California; Katharine N Clouser, MD, Hackensack, New Jersey; Alexandra L Coria, MD, Brooklyn, New York; Clare C Crosh, DO, Cincinnati, Ohio; Magna Dias, MD, Bridgeport, Connecticut; Laura N El-Hage, MD, Philadelphia, Pennsylvania; Jeff Foti, MD, Seattle, Washington; Mirna Giordano, MD, New York, New York; Sheena Gupta, MD, MBA, Evanston, Illinois; Laura Nell Hodo, MD, New York, New York; Ashley Jenkins, MD, MS, Rochester, New York; Anika Kumar, MD, Cleveland, Ohio; Merlin C Lowe, MD, Tuscon, Arizona; Brittany Middleton, MD, Pasadena, California; Sage Myers, MD, Philadelphia, Pennsylvania; Anik Patel, MD, Salt Lake City, Utah; Leah Ratner, MD, MS, Boston, Massachusetts; Shela Sridhar, MD, MPH, Boston, Massachusetts; Nathan Stehouwer, MD, Cleveland, Ohio; Julie Sylvester, DO, Mount Kisco, New York; Dava Szalda, MD, MSHP, Philadelphia, Pennsylvania; Heather Toth, MD, Milwaukee, Wisconsin; Krista Tuomela, MD, Milwaukee, Wisconsin; Ronald Williams, MD, Hershey, Pennsylvania.
1. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6):e20200702. https://doi.org/10.1542/peds.2020-0702
2. Osborn R, Doolittle B, Loyal J. When pediatric hospitalists took care of adults during the COVID-19 pandemic. Hosp Pediatr. 2021;11(1):e15-e18. https://doi.org/10.1542/hpeds.2020-001040
3. Yager PH, Whalen KA, Cummings BM. Repurposing a pediatric ICU for adults. N Engl J Med. 2020;382(22):e80. https://doi.org/10.1056/NEJMc2014819
4. Conway-Habes EE, Herbst BF Jr, Herbst LA, et al. Using quality improvement to introduce and standardize the National Early Warning Score (NEWS) for adult inpatients at a children’s hospital. Hosp Pediatr. 2017;7(3):156-163. https://doi.org/10.1542/hpeds.2016-0117
5. Kinnear B, O’Toole JK. Care of adults in children’s hospitals: acknowledging the aging elephant in the room. JAMA Pediatr. 2015;169(12):1081-1082. https://doi.org/10.1001/jamapediatrics.2015.2215
6. Szalda D, Steinway C, Greenberg A, et al. Developing a hospital-wide transition program for young adults with medical complexity. J Adolesc Health. 2019;65(4):476-482. https://doi.org/10.1016/j.jadohealth.2019.04.008
7. Jenkins A, Ratner L, Caldwell A, Sharma N, Uluer A, White C. Children’s hospitals caring for adults during a pandemic: pragmatic considerations and approaches. J Hosp Med. 2020;15(5):311-313. https://doi.org/10.12788/jhm.3432
8. Botwinick L, Bisognano M, Haraden C. Leadership Guide to Patient Safety. IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2006. Accessed January 20, 2021. http://www.ihi.org/resources/Pages/IHIWhitePapers/LeadershipGuidetoPatientSafetyWhitePaper.aspx
9. Essien UR, Eneanya ND, Crews DC. Prioritizing equity in a time of scarcity: the COVID-19 pandemic. J Gen Intern Med. 2020;35(9):2760-2762. https://doi.org/10.1007/s11606-020-05976-y
10. Yu R. Stress potentiates decision biases: a stress induced deliberation-to-intuition (SIDI) model. Neurobiol Stress. 2016;3:83-95. https://doi.org/10.1016/j.ynstr.2015.12.006
1. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6):e20200702. https://doi.org/10.1542/peds.2020-0702
2. Osborn R, Doolittle B, Loyal J. When pediatric hospitalists took care of adults during the COVID-19 pandemic. Hosp Pediatr. 2021;11(1):e15-e18. https://doi.org/10.1542/hpeds.2020-001040
3. Yager PH, Whalen KA, Cummings BM. Repurposing a pediatric ICU for adults. N Engl J Med. 2020;382(22):e80. https://doi.org/10.1056/NEJMc2014819
4. Conway-Habes EE, Herbst BF Jr, Herbst LA, et al. Using quality improvement to introduce and standardize the National Early Warning Score (NEWS) for adult inpatients at a children’s hospital. Hosp Pediatr. 2017;7(3):156-163. https://doi.org/10.1542/hpeds.2016-0117
5. Kinnear B, O’Toole JK. Care of adults in children’s hospitals: acknowledging the aging elephant in the room. JAMA Pediatr. 2015;169(12):1081-1082. https://doi.org/10.1001/jamapediatrics.2015.2215
6. Szalda D, Steinway C, Greenberg A, et al. Developing a hospital-wide transition program for young adults with medical complexity. J Adolesc Health. 2019;65(4):476-482. https://doi.org/10.1016/j.jadohealth.2019.04.008
7. Jenkins A, Ratner L, Caldwell A, Sharma N, Uluer A, White C. Children’s hospitals caring for adults during a pandemic: pragmatic considerations and approaches. J Hosp Med. 2020;15(5):311-313. https://doi.org/10.12788/jhm.3432
8. Botwinick L, Bisognano M, Haraden C. Leadership Guide to Patient Safety. IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2006. Accessed January 20, 2021. http://www.ihi.org/resources/Pages/IHIWhitePapers/LeadershipGuidetoPatientSafetyWhitePaper.aspx
9. Essien UR, Eneanya ND, Crews DC. Prioritizing equity in a time of scarcity: the COVID-19 pandemic. J Gen Intern Med. 2020;35(9):2760-2762. https://doi.org/10.1007/s11606-020-05976-y
10. Yu R. Stress potentiates decision biases: a stress induced deliberation-to-intuition (SIDI) model. Neurobiol Stress. 2016;3:83-95. https://doi.org/10.1016/j.ynstr.2015.12.006
© 2021 Society of Hospital Medicine
Designing Quality Programs for Rural Hospitals
Population-based hospital payments provide incentives to reduce unnecessary healthcare use and a mechanism to finance population health investments. For hospitals, these payments provide stable revenue and flexibility in exchange for increased financial risk. The COVID-19 pandemic significantly reduced fee-for-service revenues, which has spurred provider interest in population-based payments, particularly from cash-strapped rural hospitals.
The Centers for Medicare & Medicaid Services (CMS) recently announced the launch of the Community Health Access and Rural Transformation (CHART) Model to test whether up-front, population-based payments improve access to high-quality care in rural communities and protect the financial stability of rural providers. This model follows the ongoing Pennsylvania Rural Health Model (PARHM), which offers similar payments to Pennsylvania’s rural hospitals. Prospective population-based hospital reimbursement appears to have helped Maryland’s hospitals survive the financial stress of the COVID-19 pandemic,1 and it is likely that the PARHM did the same for rural hospitals in Pennsylvania. Both the PARHM and the CHART Model place quality measurement and improvement at the core of payment reform, and for good reason. Capitation generates incentives for care stinting; linking prospective payments to quality measurement helps to ensure accountability. However, measuring the quality of rural healthcare is challenging. Rural health is different: Hospital size, payment mechanisms, and community health priorities are all distinct from those of metropolitan areas, which is why CMS exempts Critical Access Hospitals from Medicare’s core quality programs. Rural quality reporting programs could be established that address the unique aspects of rural healthcare.
As designers (JEF, DTL) of, and an advisor (ALS) for, a proposed pay-for-performance (P4P) program for the PARHM,2 we identified three central challenges in constructing and implementing P4P programs for rural hospitals, along with potential solutions. We hope that the lessons we learned can inform similar policy efforts.
First, many rural hospitals serve as stewards of community health resources. While metropolitan hospital systems can make targeted investments in population health, assigning accountability for health outcomes is challenging in cities where geographically overlapping provider systems compete for patients. In contrast, a rural hospital system with few or no competing providers is more naturally accountable for community health outcomes, especially if it owns most ambulatory clinics in its community. P4P programs could therefore reward rural hospitals for improving healthcare quality or health outcomes within their catchment areas. Like an accountable care organization (ACO), a rural hospital or hospital-based health system could be held accountable for appropriate screening for, and treatment of, uncontrolled hypertension, diabetes, or asthma, even without a network of community-based primary care providers that ACOs usually possess. Participants in the CHART Model’s Community Transformation Track, for example, select three community-level population health measures from four domains: substance use, chronic conditions, maternal health, and prevention. Accountability for community health outcomes is increasingly feasible because many larger rural hospitals have merged or been acquired.3
Second, small rural hospital patient volumes obscure the signal of true quality with statistical noise. Many common quality indicators, like risk-standardized mortality rates, are unreliable in rural settings with low patient volumes; in 2012-2013, the mean rural hospital daily census was seven inpatients.4,5 Payers and regulators have addressed this challenge by exempting rural hospitals from quality-reporting programs or by employing statistical techniques that diminish incentives to invest in improvement. CMS, for example, uses “shrinkage” estimators that adjust a hospital’s quality score toward a program-wide average, which makes it difficult to detect and reward performance improvement.4 Instead, rural P4P programs should use measures that are resistant to low patient volumes, such as the Measure Application Partnership’s (MAP) Core Set of Rural-Relevant Measures.6 Low volume–resistant measures include process and population-health outcome measures with naturally large denominators (eg, medication reconciliation), structural measures for which sample size is irrelevant (eg, nurse staffing ratios), and qualitative assessments of hospital adherence to best practices. CMS and other measure developers should also prioritize the creation of other rural-relevant, cross-cutting, low volume–resistant measures, like avoidance of deliriogenic medications in the elderly or initiation of treatment for substance use disorders, in consultation with rural stakeholders and the MAP Rural Health Workgroup. When extensive measurement noise is inevitable, public and private policymakers should eschew downside risk in rural P4P contracts.
Third, many rural hospitals have limited resources for measurement and improvement.7 While many well-resourced community hospitals have dedicated quality departments, quality directors in rural hospitals often have at least one other full-time job. Well-intentioned exemptions from P4P programs have left rural hospitals with limited experience with basic data collection and reporting, a handicap compounded by redundant and misaligned payor quality reporting requirements. To engage rural hospitals in quality improvement work, payors should coordinate to make participation in rural P4P programs as easy as possible. The adoption of a locally aligned set of healthcare quality measures by all payors in a region, like the PARHM’s proposed “all-payer quality program,” could substantially reduce administrative burden and motivate rural hospitals to enhance patient care and improve community health. In the CHART Model’s Community Transformation Track, for example, all public and private participating payers in each region must report on six quality measures: inpatient and emergency department visits for ambulatory care sensitive conditions, hospital-wide all-cause unplanned readmissions, and the Hospital Consumer Assessment of Health Care survey, as well as three community-chosen measures from the domains of substance use, maternal health, and prevention.8 As with all P4P programs, rural P4P programs should focus on a small number of meaningful measures, such as functional and clinical outcomes, complications, and patient experience, and feature relatively large rewards for improvement.9 The National Quality Forum recommends that rural programs avoid downside risk, reward improvement as well as achievement, and permit virtual provider groups.10 We would add that programs in rural communities ought to pair economic rewards with social recognition and comparison, offer technical assistance and opportunities for shared learning, and account for social as well as medical risk.
Many challenges to the adoption of rural P4P programs have been targeted through multi-stakeholder collaborations like the PARHM. Careful allocation of technical assistance resources may help address barriers such as comparing the performance of heterogeneous rural hospitals that vary in characteristics like size, affiliation with large health systems, or integration of ambulatory care services, which may affect hospital measurement capabilities and performance. Quality improvement efforts could be further bolstered through direct allocation of funds to the creation of virtual shared learning platforms, and by providing performance bonuses to groups of small hospitals that elect to engage in shared reporting.
The stakes are high for designing robust quality programs for rural hospitals. Although one in five Americans rely on them for healthcare, their rate of closure has accelerated in the past decade.11 CMS has made it clear that a sustainable system for financing rural health must be built around a commitment to quality measurement and improvement. While some rural provider organizations might be best served by participating in voluntary rural health networks and preexisting federal programs like the Medicare Beneficiary Quality Improvement Project, they should also have the opportunity to accept payments tied to quality, especially as growing numbers of rural hospitals are absorbed into larger healthcare systems. Adopting aligned sets of reliable and meaningful quality measures alongside population-based payments will help to create a sustainable future for rural hospitals.
Acknowledgment
We thank Mark Friedberg, MD, MPP, for his helpful comments on an earlier draft of this manuscript.
1. Peterson CL, Schumacher DN. How Maryland’s Total Cost of Care Model has helped hospitals manage the COVID-19 stress test. Health Affairs blog. October 7, 2020. Accessed July 15, 2021. https://www.healthaffairs.org/doi/10.1377/hblog20201005.677034/full/
2. Herzog MB, Fried JE, Liebers DT, MacKinney AC. Development of an all-payer quality program for the Pennsylvania Rural Health Model. J Rural Health. Published online December 4, 2020. https://doi.org/10.1111/jrh.12547
3. Williams D Jr, Reiter KL, Pink GH, Holmes GM, Song PH. Rural hospital mergers increased between 2005 and 2016—what did those hospitals look like? Inquiry. 2020;57:46958020935666. https://doi.org/10.1177/0046958020935666
4. Schwartz AL. Accuracy vs. incentives: a tradeoff for performance measurement. Am J Health Econ. Accepted February 8, 2021. https://doi.org/10.1086/714374
5. Freeman V, Thompson K, Howard HA, et al. The 21st Century Rural Hospital: A Chart Book. Cecil G. Sheps Center for Health Services Research. March 2015. https://www.shepscenter.unc.edu/product/21st-century-rural-hospital-chart-book/https://www.shepscenter.unc.edu/programs-projects/rural-health/projects/north-carolina-rural-health-research-and-policy-analysis-center/publications/
6. National Quality Forum. A core set of rural-relevant measures and measuring and improving access to care: 2018 recommendations from the MAP Rural Health Workgroup. August 31, 2018.
7. US Government Accountability Office. Medicare value-based payment models: participation challenges and available assistance for small and rural practices. December 9, 2016. Accessed July 15, 2021. https://www.gao.gov/products/gao-17-55
8. US Department of Health & Human Services. Community Health Access and Rural Transformation (CHART). Funding Opportunity Number: CMS-2G2-21-001. March 5, 2021. Accessed July 15, 2021. https://www.grants.gov/web/grants/view-opportunity.html?oppId=329062
9. Jha AK. Time to get serious about pay for performance. JAMA. 2013;309(4):347-348. https://doi.org/10.1001/jama.2012.196646
10. National Quality Forum. Performance measurement for rural low-volume providers. September 14, 2015. https://www.qualityforum.org/Publications/2015/09/Rural_Health_Final_Report.aspx
11. US Government Accountability Office. Rural hospital closures: number and characteristics of affected hospitals and contributing factors. GAO-18-634. August 29, 2018. https://www.gao.gov/assets/gao-18-634.pdf
Population-based hospital payments provide incentives to reduce unnecessary healthcare use and a mechanism to finance population health investments. For hospitals, these payments provide stable revenue and flexibility in exchange for increased financial risk. The COVID-19 pandemic significantly reduced fee-for-service revenues, which has spurred provider interest in population-based payments, particularly from cash-strapped rural hospitals.
The Centers for Medicare & Medicaid Services (CMS) recently announced the launch of the Community Health Access and Rural Transformation (CHART) Model to test whether up-front, population-based payments improve access to high-quality care in rural communities and protect the financial stability of rural providers. This model follows the ongoing Pennsylvania Rural Health Model (PARHM), which offers similar payments to Pennsylvania’s rural hospitals. Prospective population-based hospital reimbursement appears to have helped Maryland’s hospitals survive the financial stress of the COVID-19 pandemic,1 and it is likely that the PARHM did the same for rural hospitals in Pennsylvania. Both the PARHM and the CHART Model place quality measurement and improvement at the core of payment reform, and for good reason. Capitation generates incentives for care stinting; linking prospective payments to quality measurement helps to ensure accountability. However, measuring the quality of rural healthcare is challenging. Rural health is different: Hospital size, payment mechanisms, and community health priorities are all distinct from those of metropolitan areas, which is why CMS exempts Critical Access Hospitals from Medicare’s core quality programs. Rural quality reporting programs could be established that address the unique aspects of rural healthcare.
As designers (JEF, DTL) of, and an advisor (ALS) for, a proposed pay-for-performance (P4P) program for the PARHM,2 we identified three central challenges in constructing and implementing P4P programs for rural hospitals, along with potential solutions. We hope that the lessons we learned can inform similar policy efforts.
First, many rural hospitals serve as stewards of community health resources. While metropolitan hospital systems can make targeted investments in population health, assigning accountability for health outcomes is challenging in cities where geographically overlapping provider systems compete for patients. In contrast, a rural hospital system with few or no competing providers is more naturally accountable for community health outcomes, especially if it owns most ambulatory clinics in its community. P4P programs could therefore reward rural hospitals for improving healthcare quality or health outcomes within their catchment areas. Like an accountable care organization (ACO), a rural hospital or hospital-based health system could be held accountable for appropriate screening for, and treatment of, uncontrolled hypertension, diabetes, or asthma, even without a network of community-based primary care providers that ACOs usually possess. Participants in the CHART Model’s Community Transformation Track, for example, select three community-level population health measures from four domains: substance use, chronic conditions, maternal health, and prevention. Accountability for community health outcomes is increasingly feasible because many larger rural hospitals have merged or been acquired.3
Second, small rural hospital patient volumes obscure the signal of true quality with statistical noise. Many common quality indicators, like risk-standardized mortality rates, are unreliable in rural settings with low patient volumes; in 2012-2013, the mean rural hospital daily census was seven inpatients.4,5 Payers and regulators have addressed this challenge by exempting rural hospitals from quality-reporting programs or by employing statistical techniques that diminish incentives to invest in improvement. CMS, for example, uses “shrinkage” estimators that adjust a hospital’s quality score toward a program-wide average, which makes it difficult to detect and reward performance improvement.4 Instead, rural P4P programs should use measures that are resistant to low patient volumes, such as the Measure Application Partnership’s (MAP) Core Set of Rural-Relevant Measures.6 Low volume–resistant measures include process and population-health outcome measures with naturally large denominators (eg, medication reconciliation), structural measures for which sample size is irrelevant (eg, nurse staffing ratios), and qualitative assessments of hospital adherence to best practices. CMS and other measure developers should also prioritize the creation of other rural-relevant, cross-cutting, low volume–resistant measures, like avoidance of deliriogenic medications in the elderly or initiation of treatment for substance use disorders, in consultation with rural stakeholders and the MAP Rural Health Workgroup. When extensive measurement noise is inevitable, public and private policymakers should eschew downside risk in rural P4P contracts.
Third, many rural hospitals have limited resources for measurement and improvement.7 While many well-resourced community hospitals have dedicated quality departments, quality directors in rural hospitals often have at least one other full-time job. Well-intentioned exemptions from P4P programs have left rural hospitals with limited experience with basic data collection and reporting, a handicap compounded by redundant and misaligned payor quality reporting requirements. To engage rural hospitals in quality improvement work, payors should coordinate to make participation in rural P4P programs as easy as possible. The adoption of a locally aligned set of healthcare quality measures by all payors in a region, like the PARHM’s proposed “all-payer quality program,” could substantially reduce administrative burden and motivate rural hospitals to enhance patient care and improve community health. In the CHART Model’s Community Transformation Track, for example, all public and private participating payers in each region must report on six quality measures: inpatient and emergency department visits for ambulatory care sensitive conditions, hospital-wide all-cause unplanned readmissions, and the Hospital Consumer Assessment of Health Care survey, as well as three community-chosen measures from the domains of substance use, maternal health, and prevention.8 As with all P4P programs, rural P4P programs should focus on a small number of meaningful measures, such as functional and clinical outcomes, complications, and patient experience, and feature relatively large rewards for improvement.9 The National Quality Forum recommends that rural programs avoid downside risk, reward improvement as well as achievement, and permit virtual provider groups.10 We would add that programs in rural communities ought to pair economic rewards with social recognition and comparison, offer technical assistance and opportunities for shared learning, and account for social as well as medical risk.
Many challenges to the adoption of rural P4P programs have been targeted through multi-stakeholder collaborations like the PARHM. Careful allocation of technical assistance resources may help address barriers such as comparing the performance of heterogeneous rural hospitals that vary in characteristics like size, affiliation with large health systems, or integration of ambulatory care services, which may affect hospital measurement capabilities and performance. Quality improvement efforts could be further bolstered through direct allocation of funds to the creation of virtual shared learning platforms, and by providing performance bonuses to groups of small hospitals that elect to engage in shared reporting.
The stakes are high for designing robust quality programs for rural hospitals. Although one in five Americans rely on them for healthcare, their rate of closure has accelerated in the past decade.11 CMS has made it clear that a sustainable system for financing rural health must be built around a commitment to quality measurement and improvement. While some rural provider organizations might be best served by participating in voluntary rural health networks and preexisting federal programs like the Medicare Beneficiary Quality Improvement Project, they should also have the opportunity to accept payments tied to quality, especially as growing numbers of rural hospitals are absorbed into larger healthcare systems. Adopting aligned sets of reliable and meaningful quality measures alongside population-based payments will help to create a sustainable future for rural hospitals.
Acknowledgment
We thank Mark Friedberg, MD, MPP, for his helpful comments on an earlier draft of this manuscript.
Population-based hospital payments provide incentives to reduce unnecessary healthcare use and a mechanism to finance population health investments. For hospitals, these payments provide stable revenue and flexibility in exchange for increased financial risk. The COVID-19 pandemic significantly reduced fee-for-service revenues, which has spurred provider interest in population-based payments, particularly from cash-strapped rural hospitals.
The Centers for Medicare & Medicaid Services (CMS) recently announced the launch of the Community Health Access and Rural Transformation (CHART) Model to test whether up-front, population-based payments improve access to high-quality care in rural communities and protect the financial stability of rural providers. This model follows the ongoing Pennsylvania Rural Health Model (PARHM), which offers similar payments to Pennsylvania’s rural hospitals. Prospective population-based hospital reimbursement appears to have helped Maryland’s hospitals survive the financial stress of the COVID-19 pandemic,1 and it is likely that the PARHM did the same for rural hospitals in Pennsylvania. Both the PARHM and the CHART Model place quality measurement and improvement at the core of payment reform, and for good reason. Capitation generates incentives for care stinting; linking prospective payments to quality measurement helps to ensure accountability. However, measuring the quality of rural healthcare is challenging. Rural health is different: Hospital size, payment mechanisms, and community health priorities are all distinct from those of metropolitan areas, which is why CMS exempts Critical Access Hospitals from Medicare’s core quality programs. Rural quality reporting programs could be established that address the unique aspects of rural healthcare.
As designers (JEF, DTL) of, and an advisor (ALS) for, a proposed pay-for-performance (P4P) program for the PARHM,2 we identified three central challenges in constructing and implementing P4P programs for rural hospitals, along with potential solutions. We hope that the lessons we learned can inform similar policy efforts.
First, many rural hospitals serve as stewards of community health resources. While metropolitan hospital systems can make targeted investments in population health, assigning accountability for health outcomes is challenging in cities where geographically overlapping provider systems compete for patients. In contrast, a rural hospital system with few or no competing providers is more naturally accountable for community health outcomes, especially if it owns most ambulatory clinics in its community. P4P programs could therefore reward rural hospitals for improving healthcare quality or health outcomes within their catchment areas. Like an accountable care organization (ACO), a rural hospital or hospital-based health system could be held accountable for appropriate screening for, and treatment of, uncontrolled hypertension, diabetes, or asthma, even without a network of community-based primary care providers that ACOs usually possess. Participants in the CHART Model’s Community Transformation Track, for example, select three community-level population health measures from four domains: substance use, chronic conditions, maternal health, and prevention. Accountability for community health outcomes is increasingly feasible because many larger rural hospitals have merged or been acquired.3
Second, small rural hospital patient volumes obscure the signal of true quality with statistical noise. Many common quality indicators, like risk-standardized mortality rates, are unreliable in rural settings with low patient volumes; in 2012-2013, the mean rural hospital daily census was seven inpatients.4,5 Payers and regulators have addressed this challenge by exempting rural hospitals from quality-reporting programs or by employing statistical techniques that diminish incentives to invest in improvement. CMS, for example, uses “shrinkage” estimators that adjust a hospital’s quality score toward a program-wide average, which makes it difficult to detect and reward performance improvement.4 Instead, rural P4P programs should use measures that are resistant to low patient volumes, such as the Measure Application Partnership’s (MAP) Core Set of Rural-Relevant Measures.6 Low volume–resistant measures include process and population-health outcome measures with naturally large denominators (eg, medication reconciliation), structural measures for which sample size is irrelevant (eg, nurse staffing ratios), and qualitative assessments of hospital adherence to best practices. CMS and other measure developers should also prioritize the creation of other rural-relevant, cross-cutting, low volume–resistant measures, like avoidance of deliriogenic medications in the elderly or initiation of treatment for substance use disorders, in consultation with rural stakeholders and the MAP Rural Health Workgroup. When extensive measurement noise is inevitable, public and private policymakers should eschew downside risk in rural P4P contracts.
Third, many rural hospitals have limited resources for measurement and improvement.7 While many well-resourced community hospitals have dedicated quality departments, quality directors in rural hospitals often have at least one other full-time job. Well-intentioned exemptions from P4P programs have left rural hospitals with limited experience with basic data collection and reporting, a handicap compounded by redundant and misaligned payor quality reporting requirements. To engage rural hospitals in quality improvement work, payors should coordinate to make participation in rural P4P programs as easy as possible. The adoption of a locally aligned set of healthcare quality measures by all payors in a region, like the PARHM’s proposed “all-payer quality program,” could substantially reduce administrative burden and motivate rural hospitals to enhance patient care and improve community health. In the CHART Model’s Community Transformation Track, for example, all public and private participating payers in each region must report on six quality measures: inpatient and emergency department visits for ambulatory care sensitive conditions, hospital-wide all-cause unplanned readmissions, and the Hospital Consumer Assessment of Health Care survey, as well as three community-chosen measures from the domains of substance use, maternal health, and prevention.8 As with all P4P programs, rural P4P programs should focus on a small number of meaningful measures, such as functional and clinical outcomes, complications, and patient experience, and feature relatively large rewards for improvement.9 The National Quality Forum recommends that rural programs avoid downside risk, reward improvement as well as achievement, and permit virtual provider groups.10 We would add that programs in rural communities ought to pair economic rewards with social recognition and comparison, offer technical assistance and opportunities for shared learning, and account for social as well as medical risk.
Many challenges to the adoption of rural P4P programs have been targeted through multi-stakeholder collaborations like the PARHM. Careful allocation of technical assistance resources may help address barriers such as comparing the performance of heterogeneous rural hospitals that vary in characteristics like size, affiliation with large health systems, or integration of ambulatory care services, which may affect hospital measurement capabilities and performance. Quality improvement efforts could be further bolstered through direct allocation of funds to the creation of virtual shared learning platforms, and by providing performance bonuses to groups of small hospitals that elect to engage in shared reporting.
The stakes are high for designing robust quality programs for rural hospitals. Although one in five Americans rely on them for healthcare, their rate of closure has accelerated in the past decade.11 CMS has made it clear that a sustainable system for financing rural health must be built around a commitment to quality measurement and improvement. While some rural provider organizations might be best served by participating in voluntary rural health networks and preexisting federal programs like the Medicare Beneficiary Quality Improvement Project, they should also have the opportunity to accept payments tied to quality, especially as growing numbers of rural hospitals are absorbed into larger healthcare systems. Adopting aligned sets of reliable and meaningful quality measures alongside population-based payments will help to create a sustainable future for rural hospitals.
Acknowledgment
We thank Mark Friedberg, MD, MPP, for his helpful comments on an earlier draft of this manuscript.
1. Peterson CL, Schumacher DN. How Maryland’s Total Cost of Care Model has helped hospitals manage the COVID-19 stress test. Health Affairs blog. October 7, 2020. Accessed July 15, 2021. https://www.healthaffairs.org/doi/10.1377/hblog20201005.677034/full/
2. Herzog MB, Fried JE, Liebers DT, MacKinney AC. Development of an all-payer quality program for the Pennsylvania Rural Health Model. J Rural Health. Published online December 4, 2020. https://doi.org/10.1111/jrh.12547
3. Williams D Jr, Reiter KL, Pink GH, Holmes GM, Song PH. Rural hospital mergers increased between 2005 and 2016—what did those hospitals look like? Inquiry. 2020;57:46958020935666. https://doi.org/10.1177/0046958020935666
4. Schwartz AL. Accuracy vs. incentives: a tradeoff for performance measurement. Am J Health Econ. Accepted February 8, 2021. https://doi.org/10.1086/714374
5. Freeman V, Thompson K, Howard HA, et al. The 21st Century Rural Hospital: A Chart Book. Cecil G. Sheps Center for Health Services Research. March 2015. https://www.shepscenter.unc.edu/product/21st-century-rural-hospital-chart-book/https://www.shepscenter.unc.edu/programs-projects/rural-health/projects/north-carolina-rural-health-research-and-policy-analysis-center/publications/
6. National Quality Forum. A core set of rural-relevant measures and measuring and improving access to care: 2018 recommendations from the MAP Rural Health Workgroup. August 31, 2018.
7. US Government Accountability Office. Medicare value-based payment models: participation challenges and available assistance for small and rural practices. December 9, 2016. Accessed July 15, 2021. https://www.gao.gov/products/gao-17-55
8. US Department of Health & Human Services. Community Health Access and Rural Transformation (CHART). Funding Opportunity Number: CMS-2G2-21-001. March 5, 2021. Accessed July 15, 2021. https://www.grants.gov/web/grants/view-opportunity.html?oppId=329062
9. Jha AK. Time to get serious about pay for performance. JAMA. 2013;309(4):347-348. https://doi.org/10.1001/jama.2012.196646
10. National Quality Forum. Performance measurement for rural low-volume providers. September 14, 2015. https://www.qualityforum.org/Publications/2015/09/Rural_Health_Final_Report.aspx
11. US Government Accountability Office. Rural hospital closures: number and characteristics of affected hospitals and contributing factors. GAO-18-634. August 29, 2018. https://www.gao.gov/assets/gao-18-634.pdf
1. Peterson CL, Schumacher DN. How Maryland’s Total Cost of Care Model has helped hospitals manage the COVID-19 stress test. Health Affairs blog. October 7, 2020. Accessed July 15, 2021. https://www.healthaffairs.org/doi/10.1377/hblog20201005.677034/full/
2. Herzog MB, Fried JE, Liebers DT, MacKinney AC. Development of an all-payer quality program for the Pennsylvania Rural Health Model. J Rural Health. Published online December 4, 2020. https://doi.org/10.1111/jrh.12547
3. Williams D Jr, Reiter KL, Pink GH, Holmes GM, Song PH. Rural hospital mergers increased between 2005 and 2016—what did those hospitals look like? Inquiry. 2020;57:46958020935666. https://doi.org/10.1177/0046958020935666
4. Schwartz AL. Accuracy vs. incentives: a tradeoff for performance measurement. Am J Health Econ. Accepted February 8, 2021. https://doi.org/10.1086/714374
5. Freeman V, Thompson K, Howard HA, et al. The 21st Century Rural Hospital: A Chart Book. Cecil G. Sheps Center for Health Services Research. March 2015. https://www.shepscenter.unc.edu/product/21st-century-rural-hospital-chart-book/https://www.shepscenter.unc.edu/programs-projects/rural-health/projects/north-carolina-rural-health-research-and-policy-analysis-center/publications/
6. National Quality Forum. A core set of rural-relevant measures and measuring and improving access to care: 2018 recommendations from the MAP Rural Health Workgroup. August 31, 2018.
7. US Government Accountability Office. Medicare value-based payment models: participation challenges and available assistance for small and rural practices. December 9, 2016. Accessed July 15, 2021. https://www.gao.gov/products/gao-17-55
8. US Department of Health & Human Services. Community Health Access and Rural Transformation (CHART). Funding Opportunity Number: CMS-2G2-21-001. March 5, 2021. Accessed July 15, 2021. https://www.grants.gov/web/grants/view-opportunity.html?oppId=329062
9. Jha AK. Time to get serious about pay for performance. JAMA. 2013;309(4):347-348. https://doi.org/10.1001/jama.2012.196646
10. National Quality Forum. Performance measurement for rural low-volume providers. September 14, 2015. https://www.qualityforum.org/Publications/2015/09/Rural_Health_Final_Report.aspx
11. US Government Accountability Office. Rural hospital closures: number and characteristics of affected hospitals and contributing factors. GAO-18-634. August 29, 2018. https://www.gao.gov/assets/gao-18-634.pdf
© 2021 Society of Hospital Medicine
Moment vs Movement: Mission-Based Tweeting for Physician Advocacy
“We, the members of the world community of physicians, solemnly commit ourselves to . . . advocate for social, economic, educational and political changes that ameliorate suffering and contribute to human well-being.”
— American Medical Association Oath of Professional Responsibility. 1
As individuals and groups spread misinformation on social media platforms, there is a greater need for physician health advocacy.2 We have learned through the COVID-19 pandemic that rapidly evolving information requires public-facing health experts to address misinformation and explain why healthcare providers and experts make certain recommendations.2 Physicians recognize the potential for benefit from crowdsourcing education, positive publicity, and increasing their reach to a larger platform.3
However, despite social media’s need for such expertise and these recognized benefits, many physicians are hesitant to engage on social media, citing lack of time, interest, or the proper skill set to use it effectively.3 Additional barriers may include uncertainty about employer policies, fear of saying something inaccurate or unprofessional, or inadvertently breaching patient privacy.3 While these are valid concerns, a strategic approach to curating a social media presence focuses less on the moments created by provocative tweets and more on the movement the author wishes to amplify. Here, we propose a framework for effective physician advocacy using a strategy we term Mission-Based Tweeting (MBT).
MISSION-BASED TWEETING
Physicians can use Twitter to engage large audiences.4 MBT focuses an individual’s central message by providing a framework upon which to build such engagement.5 The conceptual framework for a meaningful social media strategy through MBT is anchored on the principle that the impact of our Twitter content is more valuable than the number of followers.6 Using this framework, users begin by creating and defining their identity while engaging in meaningful online interactions. Over time, these interactions will lead to generating influence related to their established identity, which can ultimately impact the social micro-society.6 While an individual’s social media impact can be determined and reinforced through MBT, it remains important to know that MBT is not exemplified in one specific tweet, but rather in the body of work shared by an individual that continuously reinforces the mission.
TWEETING FOR THE MOMENT VS FOR THE MOVEMENT: USING MBT FOR ADVOCACY
Advocacy typically involves using one’s voice to publicly support a specific interest. With that in mind, health advocacy can be divided into two categories: (1) agency, which involves advancing the health of individual patients within a system, and (2) activism, which acts to advance the health of communities or populations or change the structure of the healthcare system.7 While many physicians accept agency as part of their day-to-day job, activism is often more difficult. For example, physicians hoping to engage in health advocacy may be unable to travel to their state or federal legislature buildings, or their employers may restrict their ability to interact with elected officials. The emergence of social media and digital technology has lowered these barriers and created more accessible opportunities for physicians to engage in advocacy efforts.
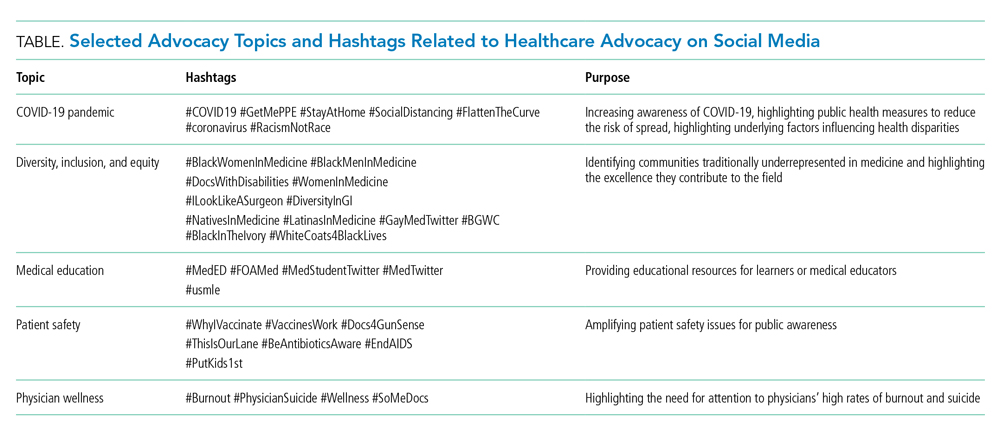
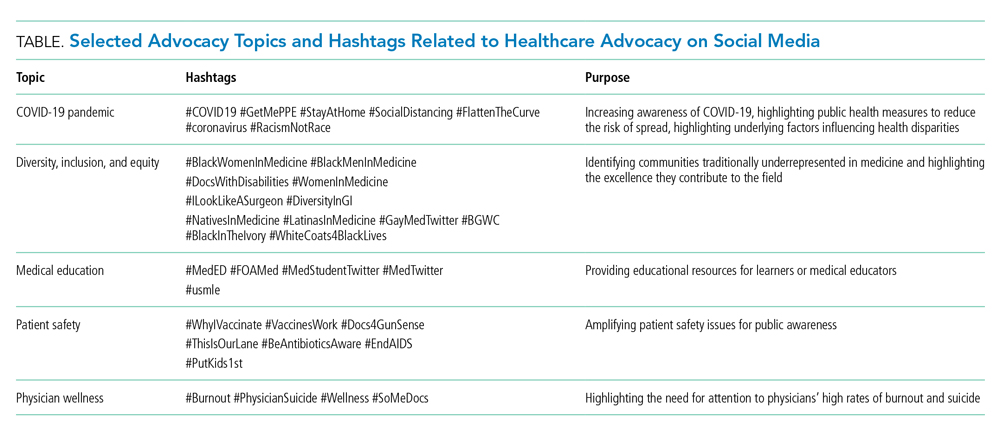
Social media can provide an opportunity for clinicians to engage with other healthcare professionals, creating movements that have far-reaching effects across the healthcare spectrum. These movements, often driven by common hashtags, have expanded greatly beyond their originators’ intent, thus demonstrating the power of social media for healthcare activism (Table).4 Physician advocacy can provide accurate information about medical conditions and treatments, dispel myths that may affect patient care, and draw attention to conditions that impact their ability to provide that care. For instance, physicians and medical students recently used Twitter during the COVID-19 pandemic to focus on the real consequences of lack of access to personal protective equipment during the pandemic (Table).8,9 In the past year, physicians have used Twitter to highlight how structural racism perpetuates racial disparities in COVID-19 and to call for action against police brutality and the killing of unarmed Black citizens. Such activism has led to media appearances and even congressional testimony—which has, in turn, provided even larger audiences for clinicians’ advocacy efforts.10 Physicians can also use MBT to advocate for the medical profession. Strategic, mission-based, social media campaigns have focused on including women; Black, Indigenous, and People of Color (BIPOC); doctors with disabilities; and LGBTQ+ physicians in the narrative of what a doctor looks like (Table).11,12
When physicians consider their personal mission statement as it applies to their social media presence, it allows them to connect to something bigger than themselves, while helping guide them away from engagements that do not align with their personal or professional values. In this manner, MBT harnesses an individual’s authenticity and helps build their personal branding, which may ultimately result in more opportunities to advance their mission. In our experience, the constant delivery of mission-based content can even accelerate one’s professional work, help amplify others’ successes and voices, and ultimately lead to more meaningful engagement and activism.
However, it is important to note that there are potential downsides to engaging on social media, particularly for women and BIPOC users. For example, in a recent online survey, almost a quarter of physicians who responded reported personal attacks on social media, with one in six female physicians reporting sexual harassment.13 This risk may increase as an individual’s visibility and reach increase.
DEVELOP YOUR MISSION STATEMENT
To aid in MBT, we have found it useful to define your personal mission statement, which should succinctly describe your core values, the specific population or cause you serve, and your overarching goals or ideals. For example, someone interested in advocating for health justice might have the following mission statement: “To create and support a healthcare workforce and graduate medical education environment that strives for excellence and values Inclusion, Diversity, Access, and Equity as not only important, but necessary, for excellence.”14 Developing a personal mission statement permits more focus in all activities, including clinical, educational, administrative, or scholarship, and allows one to succinctly communicate important values with others.15 Communicating your personal mission statement concisely can improve the quality of your interactions with others and allows you to more precisely define the qualitative and quantitative impact of your social media engagement.
ENGAGING TO AMPLIFY YOUR MISSION
There are several options for creating and delivering effective mission-driven content on Twitter.16 We propose the Five A’s of MBT (Authenticity is key, Amplify other voices, Accelerate your work, Avoid arguments, Always be professional) to provide a general guide to ensuring that your tweets honor your mission (Figure). While each factor is important, we consider authenticity the most important as it guides consistency of the message, addresses your mission, and invites discussion. In this manner, even when physicians tweet about lived experiences or scientific data that may make some individuals uncomfortable, authenticity can still lead to meaningful engagement.17

There is synergy between amplifying other voices and accelerating your own work, as both provide an opportunity to highlight your specific advocacy interest. In the earlier example, the physician advocating for health justice may create a thread highlighting inequities in COVID-19 vaccination, including their own data and that of other health justice scholars, and in doing so, provide an invaluable repository of references or speakers for a future project.
We caution that not everyone will agree with your mission, so avoiding arguments and remaining professional in these interactions is paramount. Furthermore, it is also possible that a physician’s mission and opinions may not align with those of their employer, so it is important for social media users to review and clarify their employer’s social media policies to avoid violations and related repercussions. Physicians should tweet as if they were speaking into a microphone on the record, and authenticity should ground them into projecting the same personality online as they would offline.
CONCLUSION
We believe that, by the very nature of their chosen careers, physicians should step into the tension of advocacy. We acknowledge that physicians who are otherwise vocal advocates in other areas of life may be reluctant to engage on social media. However, if the measure of “success” on Twitter is meaningful interaction, sharing knowledge, and amplifying other voices according to a specific personal mission, MBT can be a useful framework. This is a call to action for hesitant physicians to take a leap and explore this platform, and for those already using social media to reevaluate their use and reflect on their mission. Physicians have been gifted a megaphone that can be used to combat misinformation, advocate for patients and the healthcare community, and advance needed discussions to benefit those in society who cannot speak for themselves. We advocate for physicians to look beyond the moment of a tweet and consider how your voice can contribute to a movement.
Acknowledgments
The authors thank Dr Vineet Arora for her contribution to early concept development for this manuscript and the JHM editorial staff for their productive feedback and editorial comments.
1. Riddick FA Jr. The code of medical ethics of the American Medical Association. Ochsner J. 2003;5(2):6-10. https://doi.org/10.3201/eid2702.203139
2. Vraga EK, Bode L. Addressing COVID-19 misinformation on social media preemptively and responsively. Emerg Infect Dis. 2021;27(2):396-403. https://doi.org/10.3201/eid2702.203139
3. Campbell L, Evans Y, Pumper M, Moreno MA. Social media use by physicians: a qualitative study of the new frontier of medicine. BMC Med Inform Decis Mak. 2016;16:91. https://doi.org/10.1186/s12911-016-0327-y
4. Wetsman N. How Twitter is changing medical research. Nat Med. 2020;26(1):11-13. https://doi.org/10.1038/s41591-019-0697-7
5. Shapiro M. Episode 107: Vinny Arora & Charlie Wray on Social Media & CVs. Explore The Space Podcast. https://www.explorethespaceshow.com/podcasting/vinny-arora-charlie-wray-on-cvs-social-media/
6. Varghese T. i4 (i to the 4th) is a strategy for #SoMe. Accessed April 22, 2021. https://twitter.com/TomVargheseJr/status/1027181443712081920?s=20
7. Dobson S, Voyer S, Regehr G. Perspective: agency and activism: rethinking health advocacy in the medical profession. Acad Med. 2012;87(9):1161-1164. https://doi.org/10.1097/ACM.0b013e3182621c25
8. #GetMePPE. Accessed April 22, 2021. https://twitter.com/hashtag/getmeppe?f=live
9. Ouyang H. At the front lines of coronavirus, turning to social media. The New York Times. March 18, 2020. Accessed April 22, 2021. https://www.nytimes.com/2020/03/18/well/live/coronavirus-doctors-facebook-twitter-social-media-covid.html
10. Blackstock U. Combining social media advocacy with health policy advocacy. Accessed April 22, 2021. https://twitter.com/uche_blackstock/status/1270413367761666048?s=20
11. Meeks LM, Liao P, Kim N. Using Twitter to promote awareness of disabilities in medicine. Med Educ. 2019;53(5):525-526. https://doi.org/10.1111/medu.13836
12. Nolen L. To all the little brown girls out there “you can’t be what you can’t see but I hope you see me now and that you see yourself in me.” Accessed April 22, 2021. https://twitter.com/LashNolen/status/1160901502266777600?s=20.
13. Pendergrast TR, Jain S, Trueger NS, Gottlieb M, Woitowich NC, Arora VM. Prevalence of personal attacks and sexual harassment of physicians on social media. JAMA Intern Med. 2021;181(4):550-552. https://doi.org/10.1001/jamainternmed.2020.7235
14. Marcelin JR. Personal mission statement. Accessed July 6, 2021. https://www.unmc.edu/intmed/residencies-fellowships/residency/diverse-taskforce/index.html.
15. Li S-TT, Frohna JG, Bostwick SB. Using your personal mission statement to INSPIRE and achieve success. Acad Pediatr. 2017;17(2):107-109. https://doi.org/10.1016/j.acap.2016.11.010
16. Alton L. 7 tips for creating engaging content every day. Accessed April 22, 2021. https://business.twitter.com/en/blog/7-tips-creating-engaging-content-every-day.html
17. Boyd R. Is everyone reading this??! Accessed April 22, 2021. https://twitter.com/RheaBoydMD/status/1273006362679578625?s=20
“We, the members of the world community of physicians, solemnly commit ourselves to . . . advocate for social, economic, educational and political changes that ameliorate suffering and contribute to human well-being.”
— American Medical Association Oath of Professional Responsibility. 1
As individuals and groups spread misinformation on social media platforms, there is a greater need for physician health advocacy.2 We have learned through the COVID-19 pandemic that rapidly evolving information requires public-facing health experts to address misinformation and explain why healthcare providers and experts make certain recommendations.2 Physicians recognize the potential for benefit from crowdsourcing education, positive publicity, and increasing their reach to a larger platform.3
However, despite social media’s need for such expertise and these recognized benefits, many physicians are hesitant to engage on social media, citing lack of time, interest, or the proper skill set to use it effectively.3 Additional barriers may include uncertainty about employer policies, fear of saying something inaccurate or unprofessional, or inadvertently breaching patient privacy.3 While these are valid concerns, a strategic approach to curating a social media presence focuses less on the moments created by provocative tweets and more on the movement the author wishes to amplify. Here, we propose a framework for effective physician advocacy using a strategy we term Mission-Based Tweeting (MBT).
MISSION-BASED TWEETING
Physicians can use Twitter to engage large audiences.4 MBT focuses an individual’s central message by providing a framework upon which to build such engagement.5 The conceptual framework for a meaningful social media strategy through MBT is anchored on the principle that the impact of our Twitter content is more valuable than the number of followers.6 Using this framework, users begin by creating and defining their identity while engaging in meaningful online interactions. Over time, these interactions will lead to generating influence related to their established identity, which can ultimately impact the social micro-society.6 While an individual’s social media impact can be determined and reinforced through MBT, it remains important to know that MBT is not exemplified in one specific tweet, but rather in the body of work shared by an individual that continuously reinforces the mission.
TWEETING FOR THE MOMENT VS FOR THE MOVEMENT: USING MBT FOR ADVOCACY
Advocacy typically involves using one’s voice to publicly support a specific interest. With that in mind, health advocacy can be divided into two categories: (1) agency, which involves advancing the health of individual patients within a system, and (2) activism, which acts to advance the health of communities or populations or change the structure of the healthcare system.7 While many physicians accept agency as part of their day-to-day job, activism is often more difficult. For example, physicians hoping to engage in health advocacy may be unable to travel to their state or federal legislature buildings, or their employers may restrict their ability to interact with elected officials. The emergence of social media and digital technology has lowered these barriers and created more accessible opportunities for physicians to engage in advocacy efforts.
Social media can provide an opportunity for clinicians to engage with other healthcare professionals, creating movements that have far-reaching effects across the healthcare spectrum. These movements, often driven by common hashtags, have expanded greatly beyond their originators’ intent, thus demonstrating the power of social media for healthcare activism (Table).4 Physician advocacy can provide accurate information about medical conditions and treatments, dispel myths that may affect patient care, and draw attention to conditions that impact their ability to provide that care. For instance, physicians and medical students recently used Twitter during the COVID-19 pandemic to focus on the real consequences of lack of access to personal protective equipment during the pandemic (Table).8,9 In the past year, physicians have used Twitter to highlight how structural racism perpetuates racial disparities in COVID-19 and to call for action against police brutality and the killing of unarmed Black citizens. Such activism has led to media appearances and even congressional testimony—which has, in turn, provided even larger audiences for clinicians’ advocacy efforts.10 Physicians can also use MBT to advocate for the medical profession. Strategic, mission-based, social media campaigns have focused on including women; Black, Indigenous, and People of Color (BIPOC); doctors with disabilities; and LGBTQ+ physicians in the narrative of what a doctor looks like (Table).11,12
When physicians consider their personal mission statement as it applies to their social media presence, it allows them to connect to something bigger than themselves, while helping guide them away from engagements that do not align with their personal or professional values. In this manner, MBT harnesses an individual’s authenticity and helps build their personal branding, which may ultimately result in more opportunities to advance their mission. In our experience, the constant delivery of mission-based content can even accelerate one’s professional work, help amplify others’ successes and voices, and ultimately lead to more meaningful engagement and activism.
However, it is important to note that there are potential downsides to engaging on social media, particularly for women and BIPOC users. For example, in a recent online survey, almost a quarter of physicians who responded reported personal attacks on social media, with one in six female physicians reporting sexual harassment.13 This risk may increase as an individual’s visibility and reach increase.
DEVELOP YOUR MISSION STATEMENT
To aid in MBT, we have found it useful to define your personal mission statement, which should succinctly describe your core values, the specific population or cause you serve, and your overarching goals or ideals. For example, someone interested in advocating for health justice might have the following mission statement: “To create and support a healthcare workforce and graduate medical education environment that strives for excellence and values Inclusion, Diversity, Access, and Equity as not only important, but necessary, for excellence.”14 Developing a personal mission statement permits more focus in all activities, including clinical, educational, administrative, or scholarship, and allows one to succinctly communicate important values with others.15 Communicating your personal mission statement concisely can improve the quality of your interactions with others and allows you to more precisely define the qualitative and quantitative impact of your social media engagement.
ENGAGING TO AMPLIFY YOUR MISSION
There are several options for creating and delivering effective mission-driven content on Twitter.16 We propose the Five A’s of MBT (Authenticity is key, Amplify other voices, Accelerate your work, Avoid arguments, Always be professional) to provide a general guide to ensuring that your tweets honor your mission (Figure). While each factor is important, we consider authenticity the most important as it guides consistency of the message, addresses your mission, and invites discussion. In this manner, even when physicians tweet about lived experiences or scientific data that may make some individuals uncomfortable, authenticity can still lead to meaningful engagement.17

There is synergy between amplifying other voices and accelerating your own work, as both provide an opportunity to highlight your specific advocacy interest. In the earlier example, the physician advocating for health justice may create a thread highlighting inequities in COVID-19 vaccination, including their own data and that of other health justice scholars, and in doing so, provide an invaluable repository of references or speakers for a future project.
We caution that not everyone will agree with your mission, so avoiding arguments and remaining professional in these interactions is paramount. Furthermore, it is also possible that a physician’s mission and opinions may not align with those of their employer, so it is important for social media users to review and clarify their employer’s social media policies to avoid violations and related repercussions. Physicians should tweet as if they were speaking into a microphone on the record, and authenticity should ground them into projecting the same personality online as they would offline.
CONCLUSION
We believe that, by the very nature of their chosen careers, physicians should step into the tension of advocacy. We acknowledge that physicians who are otherwise vocal advocates in other areas of life may be reluctant to engage on social media. However, if the measure of “success” on Twitter is meaningful interaction, sharing knowledge, and amplifying other voices according to a specific personal mission, MBT can be a useful framework. This is a call to action for hesitant physicians to take a leap and explore this platform, and for those already using social media to reevaluate their use and reflect on their mission. Physicians have been gifted a megaphone that can be used to combat misinformation, advocate for patients and the healthcare community, and advance needed discussions to benefit those in society who cannot speak for themselves. We advocate for physicians to look beyond the moment of a tweet and consider how your voice can contribute to a movement.
Acknowledgments
The authors thank Dr Vineet Arora for her contribution to early concept development for this manuscript and the JHM editorial staff for their productive feedback and editorial comments.
“We, the members of the world community of physicians, solemnly commit ourselves to . . . advocate for social, economic, educational and political changes that ameliorate suffering and contribute to human well-being.”
— American Medical Association Oath of Professional Responsibility. 1
As individuals and groups spread misinformation on social media platforms, there is a greater need for physician health advocacy.2 We have learned through the COVID-19 pandemic that rapidly evolving information requires public-facing health experts to address misinformation and explain why healthcare providers and experts make certain recommendations.2 Physicians recognize the potential for benefit from crowdsourcing education, positive publicity, and increasing their reach to a larger platform.3
However, despite social media’s need for such expertise and these recognized benefits, many physicians are hesitant to engage on social media, citing lack of time, interest, or the proper skill set to use it effectively.3 Additional barriers may include uncertainty about employer policies, fear of saying something inaccurate or unprofessional, or inadvertently breaching patient privacy.3 While these are valid concerns, a strategic approach to curating a social media presence focuses less on the moments created by provocative tweets and more on the movement the author wishes to amplify. Here, we propose a framework for effective physician advocacy using a strategy we term Mission-Based Tweeting (MBT).
MISSION-BASED TWEETING
Physicians can use Twitter to engage large audiences.4 MBT focuses an individual’s central message by providing a framework upon which to build such engagement.5 The conceptual framework for a meaningful social media strategy through MBT is anchored on the principle that the impact of our Twitter content is more valuable than the number of followers.6 Using this framework, users begin by creating and defining their identity while engaging in meaningful online interactions. Over time, these interactions will lead to generating influence related to their established identity, which can ultimately impact the social micro-society.6 While an individual’s social media impact can be determined and reinforced through MBT, it remains important to know that MBT is not exemplified in one specific tweet, but rather in the body of work shared by an individual that continuously reinforces the mission.
TWEETING FOR THE MOMENT VS FOR THE MOVEMENT: USING MBT FOR ADVOCACY
Advocacy typically involves using one’s voice to publicly support a specific interest. With that in mind, health advocacy can be divided into two categories: (1) agency, which involves advancing the health of individual patients within a system, and (2) activism, which acts to advance the health of communities or populations or change the structure of the healthcare system.7 While many physicians accept agency as part of their day-to-day job, activism is often more difficult. For example, physicians hoping to engage in health advocacy may be unable to travel to their state or federal legislature buildings, or their employers may restrict their ability to interact with elected officials. The emergence of social media and digital technology has lowered these barriers and created more accessible opportunities for physicians to engage in advocacy efforts.
Social media can provide an opportunity for clinicians to engage with other healthcare professionals, creating movements that have far-reaching effects across the healthcare spectrum. These movements, often driven by common hashtags, have expanded greatly beyond their originators’ intent, thus demonstrating the power of social media for healthcare activism (Table).4 Physician advocacy can provide accurate information about medical conditions and treatments, dispel myths that may affect patient care, and draw attention to conditions that impact their ability to provide that care. For instance, physicians and medical students recently used Twitter during the COVID-19 pandemic to focus on the real consequences of lack of access to personal protective equipment during the pandemic (Table).8,9 In the past year, physicians have used Twitter to highlight how structural racism perpetuates racial disparities in COVID-19 and to call for action against police brutality and the killing of unarmed Black citizens. Such activism has led to media appearances and even congressional testimony—which has, in turn, provided even larger audiences for clinicians’ advocacy efforts.10 Physicians can also use MBT to advocate for the medical profession. Strategic, mission-based, social media campaigns have focused on including women; Black, Indigenous, and People of Color (BIPOC); doctors with disabilities; and LGBTQ+ physicians in the narrative of what a doctor looks like (Table).11,12
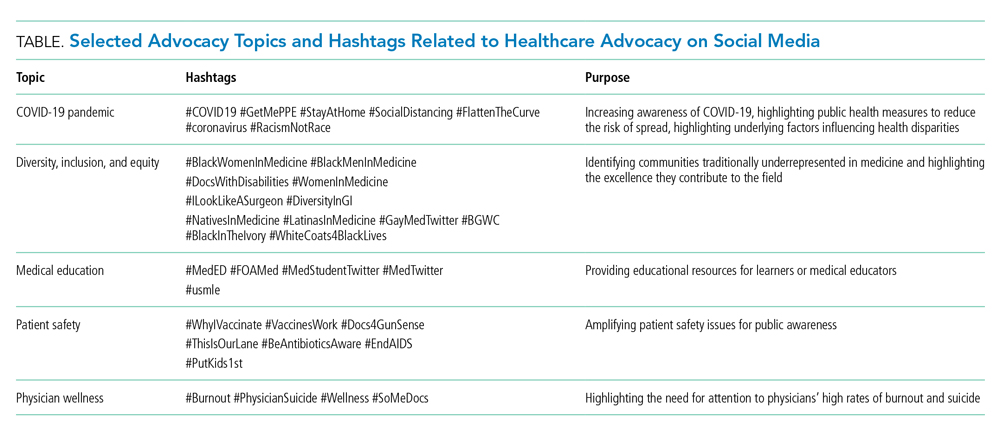
When physicians consider their personal mission statement as it applies to their social media presence, it allows them to connect to something bigger than themselves, while helping guide them away from engagements that do not align with their personal or professional values. In this manner, MBT harnesses an individual’s authenticity and helps build their personal branding, which may ultimately result in more opportunities to advance their mission. In our experience, the constant delivery of mission-based content can even accelerate one’s professional work, help amplify others’ successes and voices, and ultimately lead to more meaningful engagement and activism.
However, it is important to note that there are potential downsides to engaging on social media, particularly for women and BIPOC users. For example, in a recent online survey, almost a quarter of physicians who responded reported personal attacks on social media, with one in six female physicians reporting sexual harassment.13 This risk may increase as an individual’s visibility and reach increase.
DEVELOP YOUR MISSION STATEMENT
To aid in MBT, we have found it useful to define your personal mission statement, which should succinctly describe your core values, the specific population or cause you serve, and your overarching goals or ideals. For example, someone interested in advocating for health justice might have the following mission statement: “To create and support a healthcare workforce and graduate medical education environment that strives for excellence and values Inclusion, Diversity, Access, and Equity as not only important, but necessary, for excellence.”14 Developing a personal mission statement permits more focus in all activities, including clinical, educational, administrative, or scholarship, and allows one to succinctly communicate important values with others.15 Communicating your personal mission statement concisely can improve the quality of your interactions with others and allows you to more precisely define the qualitative and quantitative impact of your social media engagement.
ENGAGING TO AMPLIFY YOUR MISSION
There are several options for creating and delivering effective mission-driven content on Twitter.16 We propose the Five A’s of MBT (Authenticity is key, Amplify other voices, Accelerate your work, Avoid arguments, Always be professional) to provide a general guide to ensuring that your tweets honor your mission (Figure). While each factor is important, we consider authenticity the most important as it guides consistency of the message, addresses your mission, and invites discussion. In this manner, even when physicians tweet about lived experiences or scientific data that may make some individuals uncomfortable, authenticity can still lead to meaningful engagement.17

There is synergy between amplifying other voices and accelerating your own work, as both provide an opportunity to highlight your specific advocacy interest. In the earlier example, the physician advocating for health justice may create a thread highlighting inequities in COVID-19 vaccination, including their own data and that of other health justice scholars, and in doing so, provide an invaluable repository of references or speakers for a future project.
We caution that not everyone will agree with your mission, so avoiding arguments and remaining professional in these interactions is paramount. Furthermore, it is also possible that a physician’s mission and opinions may not align with those of their employer, so it is important for social media users to review and clarify their employer’s social media policies to avoid violations and related repercussions. Physicians should tweet as if they were speaking into a microphone on the record, and authenticity should ground them into projecting the same personality online as they would offline.
CONCLUSION
We believe that, by the very nature of their chosen careers, physicians should step into the tension of advocacy. We acknowledge that physicians who are otherwise vocal advocates in other areas of life may be reluctant to engage on social media. However, if the measure of “success” on Twitter is meaningful interaction, sharing knowledge, and amplifying other voices according to a specific personal mission, MBT can be a useful framework. This is a call to action for hesitant physicians to take a leap and explore this platform, and for those already using social media to reevaluate their use and reflect on their mission. Physicians have been gifted a megaphone that can be used to combat misinformation, advocate for patients and the healthcare community, and advance needed discussions to benefit those in society who cannot speak for themselves. We advocate for physicians to look beyond the moment of a tweet and consider how your voice can contribute to a movement.
Acknowledgments
The authors thank Dr Vineet Arora for her contribution to early concept development for this manuscript and the JHM editorial staff for their productive feedback and editorial comments.
1. Riddick FA Jr. The code of medical ethics of the American Medical Association. Ochsner J. 2003;5(2):6-10. https://doi.org/10.3201/eid2702.203139
2. Vraga EK, Bode L. Addressing COVID-19 misinformation on social media preemptively and responsively. Emerg Infect Dis. 2021;27(2):396-403. https://doi.org/10.3201/eid2702.203139
3. Campbell L, Evans Y, Pumper M, Moreno MA. Social media use by physicians: a qualitative study of the new frontier of medicine. BMC Med Inform Decis Mak. 2016;16:91. https://doi.org/10.1186/s12911-016-0327-y
4. Wetsman N. How Twitter is changing medical research. Nat Med. 2020;26(1):11-13. https://doi.org/10.1038/s41591-019-0697-7
5. Shapiro M. Episode 107: Vinny Arora & Charlie Wray on Social Media & CVs. Explore The Space Podcast. https://www.explorethespaceshow.com/podcasting/vinny-arora-charlie-wray-on-cvs-social-media/
6. Varghese T. i4 (i to the 4th) is a strategy for #SoMe. Accessed April 22, 2021. https://twitter.com/TomVargheseJr/status/1027181443712081920?s=20
7. Dobson S, Voyer S, Regehr G. Perspective: agency and activism: rethinking health advocacy in the medical profession. Acad Med. 2012;87(9):1161-1164. https://doi.org/10.1097/ACM.0b013e3182621c25
8. #GetMePPE. Accessed April 22, 2021. https://twitter.com/hashtag/getmeppe?f=live
9. Ouyang H. At the front lines of coronavirus, turning to social media. The New York Times. March 18, 2020. Accessed April 22, 2021. https://www.nytimes.com/2020/03/18/well/live/coronavirus-doctors-facebook-twitter-social-media-covid.html
10. Blackstock U. Combining social media advocacy with health policy advocacy. Accessed April 22, 2021. https://twitter.com/uche_blackstock/status/1270413367761666048?s=20
11. Meeks LM, Liao P, Kim N. Using Twitter to promote awareness of disabilities in medicine. Med Educ. 2019;53(5):525-526. https://doi.org/10.1111/medu.13836
12. Nolen L. To all the little brown girls out there “you can’t be what you can’t see but I hope you see me now and that you see yourself in me.” Accessed April 22, 2021. https://twitter.com/LashNolen/status/1160901502266777600?s=20.
13. Pendergrast TR, Jain S, Trueger NS, Gottlieb M, Woitowich NC, Arora VM. Prevalence of personal attacks and sexual harassment of physicians on social media. JAMA Intern Med. 2021;181(4):550-552. https://doi.org/10.1001/jamainternmed.2020.7235
14. Marcelin JR. Personal mission statement. Accessed July 6, 2021. https://www.unmc.edu/intmed/residencies-fellowships/residency/diverse-taskforce/index.html.
15. Li S-TT, Frohna JG, Bostwick SB. Using your personal mission statement to INSPIRE and achieve success. Acad Pediatr. 2017;17(2):107-109. https://doi.org/10.1016/j.acap.2016.11.010
16. Alton L. 7 tips for creating engaging content every day. Accessed April 22, 2021. https://business.twitter.com/en/blog/7-tips-creating-engaging-content-every-day.html
17. Boyd R. Is everyone reading this??! Accessed April 22, 2021. https://twitter.com/RheaBoydMD/status/1273006362679578625?s=20
1. Riddick FA Jr. The code of medical ethics of the American Medical Association. Ochsner J. 2003;5(2):6-10. https://doi.org/10.3201/eid2702.203139
2. Vraga EK, Bode L. Addressing COVID-19 misinformation on social media preemptively and responsively. Emerg Infect Dis. 2021;27(2):396-403. https://doi.org/10.3201/eid2702.203139
3. Campbell L, Evans Y, Pumper M, Moreno MA. Social media use by physicians: a qualitative study of the new frontier of medicine. BMC Med Inform Decis Mak. 2016;16:91. https://doi.org/10.1186/s12911-016-0327-y
4. Wetsman N. How Twitter is changing medical research. Nat Med. 2020;26(1):11-13. https://doi.org/10.1038/s41591-019-0697-7
5. Shapiro M. Episode 107: Vinny Arora & Charlie Wray on Social Media & CVs. Explore The Space Podcast. https://www.explorethespaceshow.com/podcasting/vinny-arora-charlie-wray-on-cvs-social-media/
6. Varghese T. i4 (i to the 4th) is a strategy for #SoMe. Accessed April 22, 2021. https://twitter.com/TomVargheseJr/status/1027181443712081920?s=20
7. Dobson S, Voyer S, Regehr G. Perspective: agency and activism: rethinking health advocacy in the medical profession. Acad Med. 2012;87(9):1161-1164. https://doi.org/10.1097/ACM.0b013e3182621c25
8. #GetMePPE. Accessed April 22, 2021. https://twitter.com/hashtag/getmeppe?f=live
9. Ouyang H. At the front lines of coronavirus, turning to social media. The New York Times. March 18, 2020. Accessed April 22, 2021. https://www.nytimes.com/2020/03/18/well/live/coronavirus-doctors-facebook-twitter-social-media-covid.html
10. Blackstock U. Combining social media advocacy with health policy advocacy. Accessed April 22, 2021. https://twitter.com/uche_blackstock/status/1270413367761666048?s=20
11. Meeks LM, Liao P, Kim N. Using Twitter to promote awareness of disabilities in medicine. Med Educ. 2019;53(5):525-526. https://doi.org/10.1111/medu.13836
12. Nolen L. To all the little brown girls out there “you can’t be what you can’t see but I hope you see me now and that you see yourself in me.” Accessed April 22, 2021. https://twitter.com/LashNolen/status/1160901502266777600?s=20.
13. Pendergrast TR, Jain S, Trueger NS, Gottlieb M, Woitowich NC, Arora VM. Prevalence of personal attacks and sexual harassment of physicians on social media. JAMA Intern Med. 2021;181(4):550-552. https://doi.org/10.1001/jamainternmed.2020.7235
14. Marcelin JR. Personal mission statement. Accessed July 6, 2021. https://www.unmc.edu/intmed/residencies-fellowships/residency/diverse-taskforce/index.html.
15. Li S-TT, Frohna JG, Bostwick SB. Using your personal mission statement to INSPIRE and achieve success. Acad Pediatr. 2017;17(2):107-109. https://doi.org/10.1016/j.acap.2016.11.010
16. Alton L. 7 tips for creating engaging content every day. Accessed April 22, 2021. https://business.twitter.com/en/blog/7-tips-creating-engaging-content-every-day.html
17. Boyd R. Is everyone reading this??! Accessed April 22, 2021. https://twitter.com/RheaBoydMD/status/1273006362679578625?s=20
© 2021 Society of Hospital Medicine
Drawing Down From Crisis: More Lessons From a Soldier
Last year, I wrote an article for the Journal of Hospital Medicine offering tips to healthcare providers in what was then an expanding COVID-19 environment.1 These lessons were drawn from my experiences during the “tough fights” and crisis situations of my military career, situations similar to what healthcare providers experienced during the pandemic.
Now, as vaccination rates rise and hospitalization rates fall, the nation and healthcare profession begin the transition to “normalcy.” What should healthcare professionals expect as they transition from a year of operating in a crisis to resumption of the habitual? What memories and lessons will linger from a long, tough fight against COVID-19, and how might physicians best approach the many post-crisis challenges they will surely face?
My military experiences inform the tips I offer to those in the medical profession. Both professions depend on adeptly leading and building a functional and effective organizational culture under trying circumstances. It may seem strange, but the challenges healthcare workers (HCWs) faced in fighting COVID-19 are comparable to what soldiers experience on a battlefield. And now, as citizens return to “normal” (however normal is defined), only naïve HCWs will believe they can simply resume their previous habits and practices. This part of the journey will present new challenges and unique opportunities.
Healthcare has changed…and so have you! Just like soldiers coming home from the battlefield face a necessarily new and different world, HCWs will also face changing circumstances, environments, and organizational requirements. Given this new landscape, I offer some of my lessons learned coming out of combat to help you adapt.
REFLECTIONS
Heading home from my last combat tour in Iraq, I found myself gazing out the aircraft window and pondering my personal experiences during a very long combat tour commanding a multinational task force. Pulling out my green soldier’s notebook, I rapidly scratched out some reflections on where I was, what I had learned, and what I needed to address personally and professionally. In talking with physicians in the healthcare organization where I now work, this emotional checklist seems to mirror some of the same thoughts they face coming out of the COVID-19 crisis.
Expect exhaustion. There’s a military axiom that “fatigue can make cowards of us all,” and while I don’t think I had succumbed to cowardice in battle, after 15 months in combat I was exhausted. Commanders in combat—or HCWs fighting a pandemic—face unrelenting demands from a variety of audiences. Leaders are asked to solve unsolvable problems, be at the right place at the right time with the right answers, have more energy than others, be upbeat, and exhibit behaviors that will motivate the “troops.” That’s true even if they’re exhausted and weary to the bone, serving on multiple teams, and attending endless meetings. There is also the common and unfortunate expectation that leaders should not take any time for themselves.
During the pandemic, most HCWs reported sleeping less, having little time to interact casually with others, and having less time for personal reflection, exercise, personal growth, or even prayer. My solution for addressing exhaustion was to develop a personal plan to address each one of these areas—mental, emotional, physical, spiritual—with a detailed rest and recovery strategy. I wrote my plan down, knowing that I would need to discuss this blueprint with both my employer and my spouse, who I suspected would have different ideas on what my schedule should look like after returning “home.” Healthcare providers have been through the same kinds of stresses and need to ask themselves: What recovery plan have I designed to help me overcome the fatigue I feel, and have I talked about this plan with the people who will be affected by it?
Take pride in what your teams accomplished. I was proud of how my teams had accomplished the impossible and how they had adapted to continually changing situations. Whenever military organizations know they’ll face the enemy in combat, they feel heightened anxiety, increased fear, and concern about the preparedness of their team. The Army, like any successful team, attempts to mitigate those emotions through training. During my reflections, I remembered the teams that came together to accomplish very tough missions. Some of those teams were those I had concerns about prior to deployment, but fortunately they often surprised me with their adaptability and successes in combat.
Leaders in healthcare can likely relate. Even in normal situations, organizational fault lines exist between physicians, nurses, and administrators. These fault lines may manifest as communication disconnects and distrust between different members who may not completely trust one another due to differences in training, culture, or role within the organization. But during a crisis, rifts dissipate and trust evolves as different cultures are forced to work together. Many healthcare organizations report that, during the COVID crisis, most personality conflicts, communication disconnects, and organizational dysfunctions receded, and organizations saw more and greater coordination and collaboration. Extensive research on leadership demonstrates that crises drive teams to communicate better and become more effective and efficient in accomplishing stated goals, resulting in team members who relish “being there” for one another like never before. These positive changes must be reinforced to ensure these newly formed high-performing teams do not revert back to work silos, which usually occurs due to distrust.
Just as important as pride in teams is the pride in the accomplishment of specific individuals during times of crisis. Diverse members of any organization deliver some of the best solutions to the toughest problems when they are included in the discussion, allowed to bring their ideas to the table, and rewarded for their actions (and their courage)! Just one example is given by Dr Sasha Shillcut as she describes the innovations and adaptations of the women physicians she observed in her organization during the COVID-19 crisis,2 and there are many examples of other organizations citing similar transformation in areas like telemedicine, emergency department procedures, and equipment design and use.3,4
Anticipate “survivor’s guilt.” During my three combat tours, 253 soldiers under my command or in my organization sacrificed their lives for the mission, and many more were wounded in action. There are times when bad dreams remind me of some of the circumstances surrounding the incidents that took the lives of those who died, and I often wake with a start and in a sweat. The first question I always ask myself in the middle of the night when this happens is, “Why did they die, and why did I survive?” That question is always followed by, “What might I have done differently to prevent those deaths?”
As we draw down from treating patients during the COVID-19 crisis, healthcare providers must also be wary of “survivor’s guilt.” Survivor’s guilt is a strong emotion for anyone who has survived a crisis, especially when their friends or loved ones have not. Healthcare providers have lost many patients, but they have also lost colleagues, friends, and family members. Because you are in the healing profession, many of you will question what more you could have done to prevent the loss of life. You likely won’t ever be completely satisfied with the answer, but I have a recommendation that may assuage your emotions.
In combat, we continually memorialized our fallen comrades in ceremonies that are attended by the entire unit. One of my commanders had an idea to keep pictures of those who had made the ultimate sacrifice, and on my desk is a box with the 253 pictures of those dedicated individuals who were killed in action under my command or in my unit. On the top of the box are the words “Make It Matter.” I look at those pictures often to remember them and their selfless service to the nation, and I often ask myself whether I am “making it matter” in my daily activities. Does your healthcare facility have plans for a memorial service for all those who died while in your care? Is there a special tribute in your hospital to those healthcare providers who paid the ultimate sacrifice in caring for patients? Most importantly, have you rededicated yourself to your profession, knowing that what you learned during the pandemic will help you be a better physician in the future, and do you have the knowledge that you are making a meaningful difference every day you serve in healthcare?
Relish being home. On that flight back to family, my excitement was palpable. But there were challenges too, as I knew I had to continue to focus on my team, my organization, and my profession. While images on the internet often show soldiers returning from war rushing into the arms of their loved ones, soldiers never leave the demands associated with wearing the cloth of the country. As a result, many marriages and families are damaged when one member who has been so singularly focused returns home and is still caught up in the demands of the job. They find it is difficult to pick up where they’ve left off, forgetting their family has also been under a different kind of intense stress.
These same challenges will face HCWs. Many of you voluntarily distanced yourself from family and friends due to a fear of transmitting the disease. Spouses and children underwent traumatic challenges in their jobs, holding together the household and piloting kids through schooling. My biggest recommendation is this: strive for a return to a healthy balance, be wary of any sharp edges that appear in your personality or in your relationships, and be open in communicating with those you love. Relying on friends, counselors, and mentors who can provide trusted advice—as well as therapy, if necessary—is not a sign of weakness, but a sign of strength and courage. The pandemic has affected our lives more than we can imagine, and “coming out” of the crisis will continue to test our humanity and civility like never before. Trust me on this one. I’ve been there.
RECOMMENDATIONS FOR POST-CRISIS ACTIONS
These reflections open us to issues physicians must address in the months after your “redeployment” from dealing with the pandemic. When soldiers redeploy from combat, every unit develops a plan to address personal and professional growth for individual members of the team. Additionally, leaders develop a plan to sustain performance and improve teams and organizational approaches. The objective? Polish the diamond from what we learned during the crisis, while preparing for those things that might detract from effectiveness in future crises. It’s an SOP (standard operating procedure) for military units to do these things. Is this approach also advisable for healthcare professionals and teams in responding to crises?
Crises increase stress on individuals and disrupt the functioning of organizations, but crises also provide phenomenal opportunities for growth.5 Adaptive organizations, be they military or healthcare, must take time to understand how the crises affected people and the organizational framework, while also preparing for potential future disruptions. While HCWs and their respective organizations are usually adept at learning from short-term emergencies (eg, limited disease outbreaks, natural disasters, mass-casualty events), they are less practiced in addressing crises that affect the profession for months. It has been a century since the medical profession has been faced with a global pandemic, but experts suggest other pandemics may be on the short-term horizon.6 We ought to use this past year of experiences to prepare for them.
Pay attention to your personal needs and the conditions of others on your team. After returning from combat, I was exhausted and stressed intellectually, physically, emotionally, and spiritually. From what I’ve seen, healthcare providers fit that same description, and the fatigue is palpable. Many of you have experienced extreme stress. I have experienced extremepost-traumatic stress, and it is important to understand that this will affect some on your team.7 In addition to addressing stress—and this is advice I give to all the physicians I know—find the time to get a physical examination. While the Army requires yearly physicals for all soldiers (especially generals!), most healthcare providers I know are shockingly deficient in taking the time to get a checkup from one of their colleagues. Commit to fixing that.
Reflect on what you have learned during this period. Take an afternoon with an adult beverage (if that’s your style) and reflect on what you learned and what others might learn from your unique experiences. Then, take some notes and shape your ideas. What did you experience? What adaptations did you or your team make during the pandemic? What worked and what didn’t? What things do you want to sustain in your practice and what things do you want to eliminate? What did you learn about the medical arts…or even about your Hippocratic Oath? If you have a mentor, share these thoughts with them; if you don’t have a mentor, find one and then share your thoughts with them. Get some outside feedback.
Assess team strengths and weaknesses. If you’re a formal physician leader (someone with a title and a position on your team), it’s your responsibility to provide feedback on both people and processes. If you’re an informal leader (someone who is a member of the team but doesn’t have specific leadership responsibilities outside your clinical role) and you don’t see this happening, volunteer to run the session for your formal leader and your organization. This session should last several hours and be held in a comfortable setting. You should prepare your team so they aren’t defensive about the points that may arise. Determine strengths and opportunities by asking for feedback on communication, behaviors, medical knowledge, emotional intelligence, and execution of tasks. Determine which processes and systems either worked or didn’t work, and either polish the approaches or drive change to improve systems as you get back to normal. Crises provide an opportunity to fix what’s broken while also reinforcing the things that worked in the crisis that might not be normal procedure. Don’t go back to old ways if those weren’t the things or the approaches you were using under critical conditions.
Encourage completion of an organization-wide after-action review (AAR). As I started writing this article, I watched CNN’s Dr Sanjay Gupta conduct a review of actions with the key physicians who contributed to the last administration’s response to the pandemic. In watching that session—and having conducted hundreds of AARs in my military career—there was discussion of obvious good and bad leadership and management procedures, process issues that needed to be addressed, and decision-making that might be applauded or questioned. Every healthcare organization ought to conduct a similar AAR, with a review of the most important aspects of actions and teamwork, the hospital’s operations, logistical preparation, and leader and organization procedures that demand to be addressed.
The successful conduct of any AAR requires asking (and getting answers to) four questions: What happened?; Why did it happen the way it did?; What needs to be fixed or “polished” in the processes, systems, or leadership approach?; and Who is responsible for ensuring the fixes or adjustments occur? The facilitator (and the key leaders of the organization) must ask the right questions, must be deeply involved in getting the right people to comment on the issues, and must “pin the rose” on someone who will be responsible for carrying through on the fixes. At the end of the AAR, after the key topics are discussed, with a plan for addressing each, the person in charge of the organization must publish an action plan with details for ensuring the fixes.
Like all citizens across our nation, my family is grateful for the skill and professionalism exhibited by clinicians and healthcare providers during this devastating pandemic. While we are all breathing a sigh of relief as we see the end in sight, true professionals must take the opportunity to learn and grow from this crisis and adapt. Hopefully, the reflections and recommendations in this article—things I learned from a different profession—will provide ideas to my new colleagues in healthcare.
1. Hertling M. Ten tips for a crisis: lessons from a soldier. J Hosp Med. 2020;15(5): 275-276. https://doi.org/10.12788/jhm.3424
2. Shillcut S. The inspiring women physicians of the COVID-19 pandemic. MedPage Today. April 9, 2020. Accessed July 7, 2021. https://www.kevinmd.com/blog/2020/04/the-insiring-women-physicians-of-the-covid-19-pandemic.html
3. Daley B. Three medical innovations fueled by COVID-19 that will outlast the pandemic. The Conversation. March 9, 2021. Accessed July 7, 2021. https://theconversation.com/3-medical-innovations-fueled-by-covid-19-that-will-outlast-the-pandemic-156464
4. Drees J, Dyrda L, Adams K. Ten big advancements in healthcare tech during the pandemic. Becker’s Health IT. July 6, 2020. Accessed July 7, 2021. https://www.beckershospitalreview.com/digital-transformation/10-big-advancements-in-healthcare-tech-during-the-pandemic.html
5. Wang J. Developing organizational learning capacity in crisis management. Adv Developing Hum Resources. 10(3):425-445. https://doi.org/10.1177/1523422308316464
6. Morens DM, Fauci AS. Emerging pandemic diseases: how we got COVID-19. Cell. 2020;182(5):1077-1092. https://doi.org/10.1016/j.cell.2020.08.021
7. What is posttraumatic stress disorder? American Psychiatric Association. Reviewed August 2020. Accessed July 7, 2021. https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
Last year, I wrote an article for the Journal of Hospital Medicine offering tips to healthcare providers in what was then an expanding COVID-19 environment.1 These lessons were drawn from my experiences during the “tough fights” and crisis situations of my military career, situations similar to what healthcare providers experienced during the pandemic.
Now, as vaccination rates rise and hospitalization rates fall, the nation and healthcare profession begin the transition to “normalcy.” What should healthcare professionals expect as they transition from a year of operating in a crisis to resumption of the habitual? What memories and lessons will linger from a long, tough fight against COVID-19, and how might physicians best approach the many post-crisis challenges they will surely face?
My military experiences inform the tips I offer to those in the medical profession. Both professions depend on adeptly leading and building a functional and effective organizational culture under trying circumstances. It may seem strange, but the challenges healthcare workers (HCWs) faced in fighting COVID-19 are comparable to what soldiers experience on a battlefield. And now, as citizens return to “normal” (however normal is defined), only naïve HCWs will believe they can simply resume their previous habits and practices. This part of the journey will present new challenges and unique opportunities.
Healthcare has changed…and so have you! Just like soldiers coming home from the battlefield face a necessarily new and different world, HCWs will also face changing circumstances, environments, and organizational requirements. Given this new landscape, I offer some of my lessons learned coming out of combat to help you adapt.
REFLECTIONS
Heading home from my last combat tour in Iraq, I found myself gazing out the aircraft window and pondering my personal experiences during a very long combat tour commanding a multinational task force. Pulling out my green soldier’s notebook, I rapidly scratched out some reflections on where I was, what I had learned, and what I needed to address personally and professionally. In talking with physicians in the healthcare organization where I now work, this emotional checklist seems to mirror some of the same thoughts they face coming out of the COVID-19 crisis.
Expect exhaustion. There’s a military axiom that “fatigue can make cowards of us all,” and while I don’t think I had succumbed to cowardice in battle, after 15 months in combat I was exhausted. Commanders in combat—or HCWs fighting a pandemic—face unrelenting demands from a variety of audiences. Leaders are asked to solve unsolvable problems, be at the right place at the right time with the right answers, have more energy than others, be upbeat, and exhibit behaviors that will motivate the “troops.” That’s true even if they’re exhausted and weary to the bone, serving on multiple teams, and attending endless meetings. There is also the common and unfortunate expectation that leaders should not take any time for themselves.
During the pandemic, most HCWs reported sleeping less, having little time to interact casually with others, and having less time for personal reflection, exercise, personal growth, or even prayer. My solution for addressing exhaustion was to develop a personal plan to address each one of these areas—mental, emotional, physical, spiritual—with a detailed rest and recovery strategy. I wrote my plan down, knowing that I would need to discuss this blueprint with both my employer and my spouse, who I suspected would have different ideas on what my schedule should look like after returning “home.” Healthcare providers have been through the same kinds of stresses and need to ask themselves: What recovery plan have I designed to help me overcome the fatigue I feel, and have I talked about this plan with the people who will be affected by it?
Take pride in what your teams accomplished. I was proud of how my teams had accomplished the impossible and how they had adapted to continually changing situations. Whenever military organizations know they’ll face the enemy in combat, they feel heightened anxiety, increased fear, and concern about the preparedness of their team. The Army, like any successful team, attempts to mitigate those emotions through training. During my reflections, I remembered the teams that came together to accomplish very tough missions. Some of those teams were those I had concerns about prior to deployment, but fortunately they often surprised me with their adaptability and successes in combat.
Leaders in healthcare can likely relate. Even in normal situations, organizational fault lines exist between physicians, nurses, and administrators. These fault lines may manifest as communication disconnects and distrust between different members who may not completely trust one another due to differences in training, culture, or role within the organization. But during a crisis, rifts dissipate and trust evolves as different cultures are forced to work together. Many healthcare organizations report that, during the COVID crisis, most personality conflicts, communication disconnects, and organizational dysfunctions receded, and organizations saw more and greater coordination and collaboration. Extensive research on leadership demonstrates that crises drive teams to communicate better and become more effective and efficient in accomplishing stated goals, resulting in team members who relish “being there” for one another like never before. These positive changes must be reinforced to ensure these newly formed high-performing teams do not revert back to work silos, which usually occurs due to distrust.
Just as important as pride in teams is the pride in the accomplishment of specific individuals during times of crisis. Diverse members of any organization deliver some of the best solutions to the toughest problems when they are included in the discussion, allowed to bring their ideas to the table, and rewarded for their actions (and their courage)! Just one example is given by Dr Sasha Shillcut as she describes the innovations and adaptations of the women physicians she observed in her organization during the COVID-19 crisis,2 and there are many examples of other organizations citing similar transformation in areas like telemedicine, emergency department procedures, and equipment design and use.3,4
Anticipate “survivor’s guilt.” During my three combat tours, 253 soldiers under my command or in my organization sacrificed their lives for the mission, and many more were wounded in action. There are times when bad dreams remind me of some of the circumstances surrounding the incidents that took the lives of those who died, and I often wake with a start and in a sweat. The first question I always ask myself in the middle of the night when this happens is, “Why did they die, and why did I survive?” That question is always followed by, “What might I have done differently to prevent those deaths?”
As we draw down from treating patients during the COVID-19 crisis, healthcare providers must also be wary of “survivor’s guilt.” Survivor’s guilt is a strong emotion for anyone who has survived a crisis, especially when their friends or loved ones have not. Healthcare providers have lost many patients, but they have also lost colleagues, friends, and family members. Because you are in the healing profession, many of you will question what more you could have done to prevent the loss of life. You likely won’t ever be completely satisfied with the answer, but I have a recommendation that may assuage your emotions.
In combat, we continually memorialized our fallen comrades in ceremonies that are attended by the entire unit. One of my commanders had an idea to keep pictures of those who had made the ultimate sacrifice, and on my desk is a box with the 253 pictures of those dedicated individuals who were killed in action under my command or in my unit. On the top of the box are the words “Make It Matter.” I look at those pictures often to remember them and their selfless service to the nation, and I often ask myself whether I am “making it matter” in my daily activities. Does your healthcare facility have plans for a memorial service for all those who died while in your care? Is there a special tribute in your hospital to those healthcare providers who paid the ultimate sacrifice in caring for patients? Most importantly, have you rededicated yourself to your profession, knowing that what you learned during the pandemic will help you be a better physician in the future, and do you have the knowledge that you are making a meaningful difference every day you serve in healthcare?
Relish being home. On that flight back to family, my excitement was palpable. But there were challenges too, as I knew I had to continue to focus on my team, my organization, and my profession. While images on the internet often show soldiers returning from war rushing into the arms of their loved ones, soldiers never leave the demands associated with wearing the cloth of the country. As a result, many marriages and families are damaged when one member who has been so singularly focused returns home and is still caught up in the demands of the job. They find it is difficult to pick up where they’ve left off, forgetting their family has also been under a different kind of intense stress.
These same challenges will face HCWs. Many of you voluntarily distanced yourself from family and friends due to a fear of transmitting the disease. Spouses and children underwent traumatic challenges in their jobs, holding together the household and piloting kids through schooling. My biggest recommendation is this: strive for a return to a healthy balance, be wary of any sharp edges that appear in your personality or in your relationships, and be open in communicating with those you love. Relying on friends, counselors, and mentors who can provide trusted advice—as well as therapy, if necessary—is not a sign of weakness, but a sign of strength and courage. The pandemic has affected our lives more than we can imagine, and “coming out” of the crisis will continue to test our humanity and civility like never before. Trust me on this one. I’ve been there.
RECOMMENDATIONS FOR POST-CRISIS ACTIONS
These reflections open us to issues physicians must address in the months after your “redeployment” from dealing with the pandemic. When soldiers redeploy from combat, every unit develops a plan to address personal and professional growth for individual members of the team. Additionally, leaders develop a plan to sustain performance and improve teams and organizational approaches. The objective? Polish the diamond from what we learned during the crisis, while preparing for those things that might detract from effectiveness in future crises. It’s an SOP (standard operating procedure) for military units to do these things. Is this approach also advisable for healthcare professionals and teams in responding to crises?
Crises increase stress on individuals and disrupt the functioning of organizations, but crises also provide phenomenal opportunities for growth.5 Adaptive organizations, be they military or healthcare, must take time to understand how the crises affected people and the organizational framework, while also preparing for potential future disruptions. While HCWs and their respective organizations are usually adept at learning from short-term emergencies (eg, limited disease outbreaks, natural disasters, mass-casualty events), they are less practiced in addressing crises that affect the profession for months. It has been a century since the medical profession has been faced with a global pandemic, but experts suggest other pandemics may be on the short-term horizon.6 We ought to use this past year of experiences to prepare for them.
Pay attention to your personal needs and the conditions of others on your team. After returning from combat, I was exhausted and stressed intellectually, physically, emotionally, and spiritually. From what I’ve seen, healthcare providers fit that same description, and the fatigue is palpable. Many of you have experienced extreme stress. I have experienced extremepost-traumatic stress, and it is important to understand that this will affect some on your team.7 In addition to addressing stress—and this is advice I give to all the physicians I know—find the time to get a physical examination. While the Army requires yearly physicals for all soldiers (especially generals!), most healthcare providers I know are shockingly deficient in taking the time to get a checkup from one of their colleagues. Commit to fixing that.
Reflect on what you have learned during this period. Take an afternoon with an adult beverage (if that’s your style) and reflect on what you learned and what others might learn from your unique experiences. Then, take some notes and shape your ideas. What did you experience? What adaptations did you or your team make during the pandemic? What worked and what didn’t? What things do you want to sustain in your practice and what things do you want to eliminate? What did you learn about the medical arts…or even about your Hippocratic Oath? If you have a mentor, share these thoughts with them; if you don’t have a mentor, find one and then share your thoughts with them. Get some outside feedback.
Assess team strengths and weaknesses. If you’re a formal physician leader (someone with a title and a position on your team), it’s your responsibility to provide feedback on both people and processes. If you’re an informal leader (someone who is a member of the team but doesn’t have specific leadership responsibilities outside your clinical role) and you don’t see this happening, volunteer to run the session for your formal leader and your organization. This session should last several hours and be held in a comfortable setting. You should prepare your team so they aren’t defensive about the points that may arise. Determine strengths and opportunities by asking for feedback on communication, behaviors, medical knowledge, emotional intelligence, and execution of tasks. Determine which processes and systems either worked or didn’t work, and either polish the approaches or drive change to improve systems as you get back to normal. Crises provide an opportunity to fix what’s broken while also reinforcing the things that worked in the crisis that might not be normal procedure. Don’t go back to old ways if those weren’t the things or the approaches you were using under critical conditions.
Encourage completion of an organization-wide after-action review (AAR). As I started writing this article, I watched CNN’s Dr Sanjay Gupta conduct a review of actions with the key physicians who contributed to the last administration’s response to the pandemic. In watching that session—and having conducted hundreds of AARs in my military career—there was discussion of obvious good and bad leadership and management procedures, process issues that needed to be addressed, and decision-making that might be applauded or questioned. Every healthcare organization ought to conduct a similar AAR, with a review of the most important aspects of actions and teamwork, the hospital’s operations, logistical preparation, and leader and organization procedures that demand to be addressed.
The successful conduct of any AAR requires asking (and getting answers to) four questions: What happened?; Why did it happen the way it did?; What needs to be fixed or “polished” in the processes, systems, or leadership approach?; and Who is responsible for ensuring the fixes or adjustments occur? The facilitator (and the key leaders of the organization) must ask the right questions, must be deeply involved in getting the right people to comment on the issues, and must “pin the rose” on someone who will be responsible for carrying through on the fixes. At the end of the AAR, after the key topics are discussed, with a plan for addressing each, the person in charge of the organization must publish an action plan with details for ensuring the fixes.
Like all citizens across our nation, my family is grateful for the skill and professionalism exhibited by clinicians and healthcare providers during this devastating pandemic. While we are all breathing a sigh of relief as we see the end in sight, true professionals must take the opportunity to learn and grow from this crisis and adapt. Hopefully, the reflections and recommendations in this article—things I learned from a different profession—will provide ideas to my new colleagues in healthcare.
Last year, I wrote an article for the Journal of Hospital Medicine offering tips to healthcare providers in what was then an expanding COVID-19 environment.1 These lessons were drawn from my experiences during the “tough fights” and crisis situations of my military career, situations similar to what healthcare providers experienced during the pandemic.
Now, as vaccination rates rise and hospitalization rates fall, the nation and healthcare profession begin the transition to “normalcy.” What should healthcare professionals expect as they transition from a year of operating in a crisis to resumption of the habitual? What memories and lessons will linger from a long, tough fight against COVID-19, and how might physicians best approach the many post-crisis challenges they will surely face?
My military experiences inform the tips I offer to those in the medical profession. Both professions depend on adeptly leading and building a functional and effective organizational culture under trying circumstances. It may seem strange, but the challenges healthcare workers (HCWs) faced in fighting COVID-19 are comparable to what soldiers experience on a battlefield. And now, as citizens return to “normal” (however normal is defined), only naïve HCWs will believe they can simply resume their previous habits and practices. This part of the journey will present new challenges and unique opportunities.
Healthcare has changed…and so have you! Just like soldiers coming home from the battlefield face a necessarily new and different world, HCWs will also face changing circumstances, environments, and organizational requirements. Given this new landscape, I offer some of my lessons learned coming out of combat to help you adapt.
REFLECTIONS
Heading home from my last combat tour in Iraq, I found myself gazing out the aircraft window and pondering my personal experiences during a very long combat tour commanding a multinational task force. Pulling out my green soldier’s notebook, I rapidly scratched out some reflections on where I was, what I had learned, and what I needed to address personally and professionally. In talking with physicians in the healthcare organization where I now work, this emotional checklist seems to mirror some of the same thoughts they face coming out of the COVID-19 crisis.
Expect exhaustion. There’s a military axiom that “fatigue can make cowards of us all,” and while I don’t think I had succumbed to cowardice in battle, after 15 months in combat I was exhausted. Commanders in combat—or HCWs fighting a pandemic—face unrelenting demands from a variety of audiences. Leaders are asked to solve unsolvable problems, be at the right place at the right time with the right answers, have more energy than others, be upbeat, and exhibit behaviors that will motivate the “troops.” That’s true even if they’re exhausted and weary to the bone, serving on multiple teams, and attending endless meetings. There is also the common and unfortunate expectation that leaders should not take any time for themselves.
During the pandemic, most HCWs reported sleeping less, having little time to interact casually with others, and having less time for personal reflection, exercise, personal growth, or even prayer. My solution for addressing exhaustion was to develop a personal plan to address each one of these areas—mental, emotional, physical, spiritual—with a detailed rest and recovery strategy. I wrote my plan down, knowing that I would need to discuss this blueprint with both my employer and my spouse, who I suspected would have different ideas on what my schedule should look like after returning “home.” Healthcare providers have been through the same kinds of stresses and need to ask themselves: What recovery plan have I designed to help me overcome the fatigue I feel, and have I talked about this plan with the people who will be affected by it?
Take pride in what your teams accomplished. I was proud of how my teams had accomplished the impossible and how they had adapted to continually changing situations. Whenever military organizations know they’ll face the enemy in combat, they feel heightened anxiety, increased fear, and concern about the preparedness of their team. The Army, like any successful team, attempts to mitigate those emotions through training. During my reflections, I remembered the teams that came together to accomplish very tough missions. Some of those teams were those I had concerns about prior to deployment, but fortunately they often surprised me with their adaptability and successes in combat.
Leaders in healthcare can likely relate. Even in normal situations, organizational fault lines exist between physicians, nurses, and administrators. These fault lines may manifest as communication disconnects and distrust between different members who may not completely trust one another due to differences in training, culture, or role within the organization. But during a crisis, rifts dissipate and trust evolves as different cultures are forced to work together. Many healthcare organizations report that, during the COVID crisis, most personality conflicts, communication disconnects, and organizational dysfunctions receded, and organizations saw more and greater coordination and collaboration. Extensive research on leadership demonstrates that crises drive teams to communicate better and become more effective and efficient in accomplishing stated goals, resulting in team members who relish “being there” for one another like never before. These positive changes must be reinforced to ensure these newly formed high-performing teams do not revert back to work silos, which usually occurs due to distrust.
Just as important as pride in teams is the pride in the accomplishment of specific individuals during times of crisis. Diverse members of any organization deliver some of the best solutions to the toughest problems when they are included in the discussion, allowed to bring their ideas to the table, and rewarded for their actions (and their courage)! Just one example is given by Dr Sasha Shillcut as she describes the innovations and adaptations of the women physicians she observed in her organization during the COVID-19 crisis,2 and there are many examples of other organizations citing similar transformation in areas like telemedicine, emergency department procedures, and equipment design and use.3,4
Anticipate “survivor’s guilt.” During my three combat tours, 253 soldiers under my command or in my organization sacrificed their lives for the mission, and many more were wounded in action. There are times when bad dreams remind me of some of the circumstances surrounding the incidents that took the lives of those who died, and I often wake with a start and in a sweat. The first question I always ask myself in the middle of the night when this happens is, “Why did they die, and why did I survive?” That question is always followed by, “What might I have done differently to prevent those deaths?”
As we draw down from treating patients during the COVID-19 crisis, healthcare providers must also be wary of “survivor’s guilt.” Survivor’s guilt is a strong emotion for anyone who has survived a crisis, especially when their friends or loved ones have not. Healthcare providers have lost many patients, but they have also lost colleagues, friends, and family members. Because you are in the healing profession, many of you will question what more you could have done to prevent the loss of life. You likely won’t ever be completely satisfied with the answer, but I have a recommendation that may assuage your emotions.
In combat, we continually memorialized our fallen comrades in ceremonies that are attended by the entire unit. One of my commanders had an idea to keep pictures of those who had made the ultimate sacrifice, and on my desk is a box with the 253 pictures of those dedicated individuals who were killed in action under my command or in my unit. On the top of the box are the words “Make It Matter.” I look at those pictures often to remember them and their selfless service to the nation, and I often ask myself whether I am “making it matter” in my daily activities. Does your healthcare facility have plans for a memorial service for all those who died while in your care? Is there a special tribute in your hospital to those healthcare providers who paid the ultimate sacrifice in caring for patients? Most importantly, have you rededicated yourself to your profession, knowing that what you learned during the pandemic will help you be a better physician in the future, and do you have the knowledge that you are making a meaningful difference every day you serve in healthcare?
Relish being home. On that flight back to family, my excitement was palpable. But there were challenges too, as I knew I had to continue to focus on my team, my organization, and my profession. While images on the internet often show soldiers returning from war rushing into the arms of their loved ones, soldiers never leave the demands associated with wearing the cloth of the country. As a result, many marriages and families are damaged when one member who has been so singularly focused returns home and is still caught up in the demands of the job. They find it is difficult to pick up where they’ve left off, forgetting their family has also been under a different kind of intense stress.
These same challenges will face HCWs. Many of you voluntarily distanced yourself from family and friends due to a fear of transmitting the disease. Spouses and children underwent traumatic challenges in their jobs, holding together the household and piloting kids through schooling. My biggest recommendation is this: strive for a return to a healthy balance, be wary of any sharp edges that appear in your personality or in your relationships, and be open in communicating with those you love. Relying on friends, counselors, and mentors who can provide trusted advice—as well as therapy, if necessary—is not a sign of weakness, but a sign of strength and courage. The pandemic has affected our lives more than we can imagine, and “coming out” of the crisis will continue to test our humanity and civility like never before. Trust me on this one. I’ve been there.
RECOMMENDATIONS FOR POST-CRISIS ACTIONS
These reflections open us to issues physicians must address in the months after your “redeployment” from dealing with the pandemic. When soldiers redeploy from combat, every unit develops a plan to address personal and professional growth for individual members of the team. Additionally, leaders develop a plan to sustain performance and improve teams and organizational approaches. The objective? Polish the diamond from what we learned during the crisis, while preparing for those things that might detract from effectiveness in future crises. It’s an SOP (standard operating procedure) for military units to do these things. Is this approach also advisable for healthcare professionals and teams in responding to crises?
Crises increase stress on individuals and disrupt the functioning of organizations, but crises also provide phenomenal opportunities for growth.5 Adaptive organizations, be they military or healthcare, must take time to understand how the crises affected people and the organizational framework, while also preparing for potential future disruptions. While HCWs and their respective organizations are usually adept at learning from short-term emergencies (eg, limited disease outbreaks, natural disasters, mass-casualty events), they are less practiced in addressing crises that affect the profession for months. It has been a century since the medical profession has been faced with a global pandemic, but experts suggest other pandemics may be on the short-term horizon.6 We ought to use this past year of experiences to prepare for them.
Pay attention to your personal needs and the conditions of others on your team. After returning from combat, I was exhausted and stressed intellectually, physically, emotionally, and spiritually. From what I’ve seen, healthcare providers fit that same description, and the fatigue is palpable. Many of you have experienced extreme stress. I have experienced extremepost-traumatic stress, and it is important to understand that this will affect some on your team.7 In addition to addressing stress—and this is advice I give to all the physicians I know—find the time to get a physical examination. While the Army requires yearly physicals for all soldiers (especially generals!), most healthcare providers I know are shockingly deficient in taking the time to get a checkup from one of their colleagues. Commit to fixing that.
Reflect on what you have learned during this period. Take an afternoon with an adult beverage (if that’s your style) and reflect on what you learned and what others might learn from your unique experiences. Then, take some notes and shape your ideas. What did you experience? What adaptations did you or your team make during the pandemic? What worked and what didn’t? What things do you want to sustain in your practice and what things do you want to eliminate? What did you learn about the medical arts…or even about your Hippocratic Oath? If you have a mentor, share these thoughts with them; if you don’t have a mentor, find one and then share your thoughts with them. Get some outside feedback.
Assess team strengths and weaknesses. If you’re a formal physician leader (someone with a title and a position on your team), it’s your responsibility to provide feedback on both people and processes. If you’re an informal leader (someone who is a member of the team but doesn’t have specific leadership responsibilities outside your clinical role) and you don’t see this happening, volunteer to run the session for your formal leader and your organization. This session should last several hours and be held in a comfortable setting. You should prepare your team so they aren’t defensive about the points that may arise. Determine strengths and opportunities by asking for feedback on communication, behaviors, medical knowledge, emotional intelligence, and execution of tasks. Determine which processes and systems either worked or didn’t work, and either polish the approaches or drive change to improve systems as you get back to normal. Crises provide an opportunity to fix what’s broken while also reinforcing the things that worked in the crisis that might not be normal procedure. Don’t go back to old ways if those weren’t the things or the approaches you were using under critical conditions.
Encourage completion of an organization-wide after-action review (AAR). As I started writing this article, I watched CNN’s Dr Sanjay Gupta conduct a review of actions with the key physicians who contributed to the last administration’s response to the pandemic. In watching that session—and having conducted hundreds of AARs in my military career—there was discussion of obvious good and bad leadership and management procedures, process issues that needed to be addressed, and decision-making that might be applauded or questioned. Every healthcare organization ought to conduct a similar AAR, with a review of the most important aspects of actions and teamwork, the hospital’s operations, logistical preparation, and leader and organization procedures that demand to be addressed.
The successful conduct of any AAR requires asking (and getting answers to) four questions: What happened?; Why did it happen the way it did?; What needs to be fixed or “polished” in the processes, systems, or leadership approach?; and Who is responsible for ensuring the fixes or adjustments occur? The facilitator (and the key leaders of the organization) must ask the right questions, must be deeply involved in getting the right people to comment on the issues, and must “pin the rose” on someone who will be responsible for carrying through on the fixes. At the end of the AAR, after the key topics are discussed, with a plan for addressing each, the person in charge of the organization must publish an action plan with details for ensuring the fixes.
Like all citizens across our nation, my family is grateful for the skill and professionalism exhibited by clinicians and healthcare providers during this devastating pandemic. While we are all breathing a sigh of relief as we see the end in sight, true professionals must take the opportunity to learn and grow from this crisis and adapt. Hopefully, the reflections and recommendations in this article—things I learned from a different profession—will provide ideas to my new colleagues in healthcare.
1. Hertling M. Ten tips for a crisis: lessons from a soldier. J Hosp Med. 2020;15(5): 275-276. https://doi.org/10.12788/jhm.3424
2. Shillcut S. The inspiring women physicians of the COVID-19 pandemic. MedPage Today. April 9, 2020. Accessed July 7, 2021. https://www.kevinmd.com/blog/2020/04/the-insiring-women-physicians-of-the-covid-19-pandemic.html
3. Daley B. Three medical innovations fueled by COVID-19 that will outlast the pandemic. The Conversation. March 9, 2021. Accessed July 7, 2021. https://theconversation.com/3-medical-innovations-fueled-by-covid-19-that-will-outlast-the-pandemic-156464
4. Drees J, Dyrda L, Adams K. Ten big advancements in healthcare tech during the pandemic. Becker’s Health IT. July 6, 2020. Accessed July 7, 2021. https://www.beckershospitalreview.com/digital-transformation/10-big-advancements-in-healthcare-tech-during-the-pandemic.html
5. Wang J. Developing organizational learning capacity in crisis management. Adv Developing Hum Resources. 10(3):425-445. https://doi.org/10.1177/1523422308316464
6. Morens DM, Fauci AS. Emerging pandemic diseases: how we got COVID-19. Cell. 2020;182(5):1077-1092. https://doi.org/10.1016/j.cell.2020.08.021
7. What is posttraumatic stress disorder? American Psychiatric Association. Reviewed August 2020. Accessed July 7, 2021. https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
1. Hertling M. Ten tips for a crisis: lessons from a soldier. J Hosp Med. 2020;15(5): 275-276. https://doi.org/10.12788/jhm.3424
2. Shillcut S. The inspiring women physicians of the COVID-19 pandemic. MedPage Today. April 9, 2020. Accessed July 7, 2021. https://www.kevinmd.com/blog/2020/04/the-insiring-women-physicians-of-the-covid-19-pandemic.html
3. Daley B. Three medical innovations fueled by COVID-19 that will outlast the pandemic. The Conversation. March 9, 2021. Accessed July 7, 2021. https://theconversation.com/3-medical-innovations-fueled-by-covid-19-that-will-outlast-the-pandemic-156464
4. Drees J, Dyrda L, Adams K. Ten big advancements in healthcare tech during the pandemic. Becker’s Health IT. July 6, 2020. Accessed July 7, 2021. https://www.beckershospitalreview.com/digital-transformation/10-big-advancements-in-healthcare-tech-during-the-pandemic.html
5. Wang J. Developing organizational learning capacity in crisis management. Adv Developing Hum Resources. 10(3):425-445. https://doi.org/10.1177/1523422308316464
6. Morens DM, Fauci AS. Emerging pandemic diseases: how we got COVID-19. Cell. 2020;182(5):1077-1092. https://doi.org/10.1016/j.cell.2020.08.021
7. What is posttraumatic stress disorder? American Psychiatric Association. Reviewed August 2020. Accessed July 7, 2021. https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
© 2021 Society of Hospital Medicine
Debriefing During a Mental Health Crisis
In the wake of the COVID-19 pandemic, hospitals across the country face a crisis in identifying resources for the surging needs of patients with mental health conditions. Compared with 2019, survey and utilization data from 2020 suggest an increase in suicidal ideation and other symptoms among adults,1 and an escalation in mental health-related visits to pediatric emergency departments, respectively.2 Unfortunately, mental health resources have dwindled during this period. Available inpatient psychiatric beds and 24-hour residential treatment beds—already on the decline over the past 5 years—have been massively affected by the pandemic due to capacity constraints and facility closures.3
These factors have placed general medical hospitals (hospitals) at the front lines of a mental health crisis4 for which most are ill prepared. Indeed, once a patient with acute mental health needs is “medically cleared,” they must wait for an available bed at a psychiatric or residential treatment facility.3 This waiting period often delays necessary patient care, as most consultation-liaison psychiatry models are not designed to provide intensive services.5
This waiting period can also place hospital staff in unfamiliar and potentially unsafe scenarios related to physical and psychological stressors. Staff may encounter patient behaviors that risk harm to patients and staff (ie, behavioral crisis events), which may require seclusion (ie, confinement to a locked room) or restraints (chemical, physical, and mechanical). Even in inpatient psychiatric units, an estimated 70% of nurses have been assaulted at least once during their career.6 Such violent behaviors and the interventions required to subdue them can be traumatizing for both patients and staff.7 In fact, the “cost of caring” may be higher for mental health nurses, who often suffer from secondary posttraumatic stress.8 Staff lacking mental health training may encounter additional stressors from feeling powerless to help their patients.
Facing this crisis, hospitals must develop a strategic response that encompasses the needs of both patients and staff. Beyond intensive interventions (eg, additional staffing resources), this response should include lower-effort interventions. In this perspective, we review two debriefing practices—clinical event debriefing and psychological debriefing—that hospitals can feasibly implement during this crisis. These respective practices can ensure safe and effective care of patients by reducing use of restraints and seclusion while also providing crucial support for staff.
CLINICAL EVENT DEBRIEFING
Broadly defined as a facilitated discussion of significant clinical events, clinical event debriefing (CED) can improve both individual and team performance in resuscitation events and patient outcomes.9-11 While CED is often utilized for clinical deterioration events, it can also apply to behavioral crises in a diversity of settings.6
In recent decades, researchers have developed several frameworks for reducing seclusion and restraint practices in psychiatric care settings.6 A common framework is Huckshorn’s Six Core Strategies,6,12,13 which can reduce seclusion and restraint use14 and is feasible to implement.15 This framework advocates for an immediate CED following behavioral crisis events. A unit supervisor or senior staff member not involved in the event should lead the CED, which has several goals. The first priorities, however, are ensuring the physical safety of all staff and returning the unit to normal operations. More broadly, the CED group should review event documentation and interview staff who were present at the time of the event. These processes can help identify antecedents as well as short- and long-term practices, systems, and environmental modifications to prevent reoccurence.12 However, little is known about this practice outside of inpatient psychiatric units.
Our pediatric hospital implemented a CED process in our medical behavioral unit (MBU), a 10-bed unit designed for patients with comorbid mental health needs requiring a higher level of psychosocial resources. The MBU is not an inpatient psychiatric unit, yet more than 50% of patients admitted to the MBU at any given time are hospitalized with a primary psychiatric diagnosis requiring intensive services due to a lack of resources in the community.
Preventing use of restraints is an institutional priority for all areas of our hospital. To reduce restraint use in the MBU, staff are asked to perform immediate CED following behavioral crisis events. This process involves both clinical (eg, nurses, physicians, psychiatric technicians) and nonclinical staff (eg, unit clerks, security officers). All staff involved in the event are invited to attend. A senior staff member not involved in the event typically organizes and leads the CED. The group uses a facilitative guide to (1) review the patient’s history; (2) identify potential triggers for the event; (3) reflect on areas of strength and weakness in unit response; (4) identify systems issues impacting the patient or the unit response; and (5) generate a strategy to prevent reoccurrence. The process is designed to take 5 to 10 minutes. The guide also serves as a data collection tool that unit leaders use to screen for generalizable learnings and improvement ideas (Appendix). For example, if a behavioral trigger is identified for a patient, unit leaders disseminate this information to create situational awareness and to ensure care plans are updated.
PSYCHOLOGICAL DEBRIEFING
Psychological debriefing is an application of Critical Incident Stress Management, a comprehensive approach that was developed in the 1970s to help emergency service workers process the thoughts and emotions arising from their exposure to trauma in their work.8,16 More recently, it has become a standard practice in many settings, including healthcare. Notably, psychological debriefing and event debriefing are often conflated. While not mutually exclusive, psychological debriefing has the unique aim of providing support to groups who work together in stressful situations.
Strategies for psychological debriefing are less well described in healthcare. However, our hospital has found it to be a useful tool for MBU staff. Operationally, this process takes the form of a weekly multidisciplinary team meeting with unit clinical staff. Typically, a psychologist or social worker initiates this meeting, which is held at a dedicated time and in a protected space. Discussion centers on patients who have been admitted to the unit for more than 30 days. A goal of the meeting is to review and update patient care plans, but there is also an important goal of emotional processing (Appendix).
In this meeting, staff reflect collectively on the unique stressors they encounter in their work, and they generate situational awareness and potential interventions for these stressors. The psychosocial providers often share recommendations, such as strategies to promote effective communication with patients and families. Peer support is a major component of this meeting and is often utilized to navigate stressful situations, such as disagreements with families regarding behavioral management. Staff also review and reinforce the Positive Behavioral Interventions and Supports framework—a preventive framework that can reduce seclusion and restraint use in pediatric psychiatric units, among other positive outcomes.17 This framework includes setting expectations for patients and families regarding behaviors on the unit. In reviewing these guidelines, staff are encouraged to recognize and report inappropriate behaviors (from patients or families) that can be traumatizing, especially over prolonged hospitalizations. This framework also provides a common language for staff to express behavioral expectations in a positive manner (eg, “Let’s use our walking feet” rather than “No running”). Overall, staff view this meeting as a resilience-building activity that empowers them in their routine work.
IMPLEMENTATION CONSIDERATIONS
While the MBU is a specialized unit with dedicated psychosocial resources, the debriefing practices we describe can be translated to multiple care settings. However, successful implementation relies on intentional process design. First, debriefing indications must be made clear to staff (eg, events of restraint). There should be a role or group accountable for organizing and leading debriefings, which should be held at a time that promotes participation from frontline staff,particularly for CED. Debriefings—especially psychological debriefings—should be held in a protected space. They should have a clear organization, such as use of a survey-based debriefing guide that allows for data collection. Importantly, there should be a unit or hospital leader accountable for disseminating learnings and improvement ideas to relevant staff and ensuring action items are completed. Finally, accountable leaders should evaluate the process’ feasibility, efficacy, and sustainability to inform implementation.
Hospitals must also consider how to train debriefing leaders to facilitate difficult conversations. Some hospitals may have formal communication training programs, but it may also be helpful to leverage the skills of social workers and psychosocial staff.
OTHER CONSIDERATIONS
Debriefing relies on a climate in which staff of diverse backgrounds and professional status feel comfortable speaking up. Psychological safety is critical in any crisis, and hospital leaders should consider how to make staff feel comfortable during this mental health crisis.18 Leaders must also be prepared to support staff beyond debriefing if resources are required for secondary posttraumatic stress, burnout, or compassion fatigue.8,19,20 Employee assistance programs may be a useful resource.
CONCLUSION
Debriefing practices can help hospitals contend with the unique challenges facing patients and staff in a mental health crisis. While debriefing may vary based on need and setting, hospitals should consider CED as a strategy for reducing seclusion and restraint use, which adversely impact patients and staff. Psychological debriefing can also help staff mitigate the psychosocial stressors of their work.
1. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049-1057. https://doi.org/10.15585/mmwr.mm6932a1
2. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1–October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1675-1680. https://doi.org/10.15585/mmwr.mm6945a3
3. Rapoport R. ‘Every day is an emergency’: The pandemic is worsening psychiatric bed shortages nationwide. Stat News. December 23, 2020. Accessed January 22, 2021. https://www.statnews.com/2020/12/23/mental-health-covid19-psychiatric-beds/
4. A step to ease the pandemic mental health crisis. Scientific American. February 1, 2021. Accessed April 14, 2021. https://www.scientificamerican.com/article/a-step-to-ease-the-pandemic-mental-health-crisis/
5. Sharpe M, Toynbee M, Walker J. Proactive Integrated Consultation-Liaison Psychiatry: A new service model for the psychiatric care of general hospital inpatients. Gen Hosp Psych. 2020;66:9-15. https://doi.org/10.1016/j.genhosppsych.2020.06.005
6. Mangaoil RA, Cleverley K, Peter E. Immediate staff debriefing following seclusions or restraint use in inpatient mental health settings: a scoping review. Clin Nurs Res. 2020;29(7):479-495. https://doi.org/10.1177/1054773818791085
7. Needham I, Abderhalden C, Zeller A, et al. The effect of a training course on nursing students’ attitudes toward, perceptions of, and confidence in managing patient aggression. J Nurs Educ. 2005;44:415-420.
8. Missouridou E. Secondary posttraumatic stress and nurses’ emotional responses to patient’s trauma. J Trauma Nurs. 2017;24(2):110-115. https://doi.org/10.1097/JTN.0000000000000274
9. Blankenship BAC, Fernandez RP, Joy BF, et al. Multidisciplinary review of code events in a heart center. Am J Crit Care. 2016;25(4):90-98. https://doi.org/10.4037/ajcc2016302
10. Wolfe H, Zebuhr C, Topjian AA, et al. Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes. Crit Care Med. 2014;42(7):1688-1695. https://doi.org/10.1097/CCM.0000000000000327
11. Tannenbaum SI, Cerasoli CP. Do team and individual debriefs enhance performance? A meta-analysis. Hum Factors. 2013;55(1):231-245. https://doi.org/10.1177/0018720812448394
12. Huckshorn KA. Reducing seclusion restraint in mental health use settings: core strategies for prevention. J Psychosoc Nurs Ment Health Serv. 2004;42:22-33.
13. Goulet MH, Larue C, Dumais A. Evaluation of seclusion and restraint reduction programs in mental health: a systematic review. Agress Violent Behav. 2017;34:139-146. https://doi.org/10.1016/j.avb.2017.01.019
14. Azeem MW, Aujila A, Rammerth M, et al, Effectiveness of six core strategies based on trauma informed care in reducing seclusions and restraints at a child and adolescent psychiatric hospital. J Child Adolesc Psychiatr Nurs. 2011;24:11-15. https://doi.org/10.1111/jcap.12190
15. Wieman DA, Camacho-Gonsalves T, Huckshorn KA, et al. Multisite study of an evidence-based practice to reduce seclusion and restraint in psychiatric inpatient facilities. Psychiatr Serv. 2014;65(3):345-351. https://doi.org/10.1176/appi.ps.201300210
16. Everly GS. A primer on critical incident stress management: what’s really in a name? Int J Emerg Ment Health. 1999;1(2):77-79.
17. Reynolds EK, Grados MA, Praglowski N, et al. Use of modified positive behavioral interventions and supports in a psychiatric inpatient unit for high-risk youths. Psychiatr Serv. 2016;67(5):570-573. https://doi.org/10.1176/appi.ps.201500039
18. Devaraj LR, Cooper C, Begin AS. Creating psychological safety on medical teams in times of crisis. J Hosp Med. 2021;16(1):47-49. https://doi.org/10.12788/jhm.3541
19. Bride BE, Radey M, Figley CR. Measuring compassion fatigue. Clin Soc Work J. 2007;35:155-163. https://doi.org/10.1007/s10615-007-0091-7
20. Figley CR. Compassion fatigue: psychotherapists’ lack of self care. J Clin Psychol. 2002;58(11):1433-1441. https://doi.org/10.1002/jclp.10090
In the wake of the COVID-19 pandemic, hospitals across the country face a crisis in identifying resources for the surging needs of patients with mental health conditions. Compared with 2019, survey and utilization data from 2020 suggest an increase in suicidal ideation and other symptoms among adults,1 and an escalation in mental health-related visits to pediatric emergency departments, respectively.2 Unfortunately, mental health resources have dwindled during this period. Available inpatient psychiatric beds and 24-hour residential treatment beds—already on the decline over the past 5 years—have been massively affected by the pandemic due to capacity constraints and facility closures.3
These factors have placed general medical hospitals (hospitals) at the front lines of a mental health crisis4 for which most are ill prepared. Indeed, once a patient with acute mental health needs is “medically cleared,” they must wait for an available bed at a psychiatric or residential treatment facility.3 This waiting period often delays necessary patient care, as most consultation-liaison psychiatry models are not designed to provide intensive services.5
This waiting period can also place hospital staff in unfamiliar and potentially unsafe scenarios related to physical and psychological stressors. Staff may encounter patient behaviors that risk harm to patients and staff (ie, behavioral crisis events), which may require seclusion (ie, confinement to a locked room) or restraints (chemical, physical, and mechanical). Even in inpatient psychiatric units, an estimated 70% of nurses have been assaulted at least once during their career.6 Such violent behaviors and the interventions required to subdue them can be traumatizing for both patients and staff.7 In fact, the “cost of caring” may be higher for mental health nurses, who often suffer from secondary posttraumatic stress.8 Staff lacking mental health training may encounter additional stressors from feeling powerless to help their patients.
Facing this crisis, hospitals must develop a strategic response that encompasses the needs of both patients and staff. Beyond intensive interventions (eg, additional staffing resources), this response should include lower-effort interventions. In this perspective, we review two debriefing practices—clinical event debriefing and psychological debriefing—that hospitals can feasibly implement during this crisis. These respective practices can ensure safe and effective care of patients by reducing use of restraints and seclusion while also providing crucial support for staff.
CLINICAL EVENT DEBRIEFING
Broadly defined as a facilitated discussion of significant clinical events, clinical event debriefing (CED) can improve both individual and team performance in resuscitation events and patient outcomes.9-11 While CED is often utilized for clinical deterioration events, it can also apply to behavioral crises in a diversity of settings.6
In recent decades, researchers have developed several frameworks for reducing seclusion and restraint practices in psychiatric care settings.6 A common framework is Huckshorn’s Six Core Strategies,6,12,13 which can reduce seclusion and restraint use14 and is feasible to implement.15 This framework advocates for an immediate CED following behavioral crisis events. A unit supervisor or senior staff member not involved in the event should lead the CED, which has several goals. The first priorities, however, are ensuring the physical safety of all staff and returning the unit to normal operations. More broadly, the CED group should review event documentation and interview staff who were present at the time of the event. These processes can help identify antecedents as well as short- and long-term practices, systems, and environmental modifications to prevent reoccurence.12 However, little is known about this practice outside of inpatient psychiatric units.
Our pediatric hospital implemented a CED process in our medical behavioral unit (MBU), a 10-bed unit designed for patients with comorbid mental health needs requiring a higher level of psychosocial resources. The MBU is not an inpatient psychiatric unit, yet more than 50% of patients admitted to the MBU at any given time are hospitalized with a primary psychiatric diagnosis requiring intensive services due to a lack of resources in the community.
Preventing use of restraints is an institutional priority for all areas of our hospital. To reduce restraint use in the MBU, staff are asked to perform immediate CED following behavioral crisis events. This process involves both clinical (eg, nurses, physicians, psychiatric technicians) and nonclinical staff (eg, unit clerks, security officers). All staff involved in the event are invited to attend. A senior staff member not involved in the event typically organizes and leads the CED. The group uses a facilitative guide to (1) review the patient’s history; (2) identify potential triggers for the event; (3) reflect on areas of strength and weakness in unit response; (4) identify systems issues impacting the patient or the unit response; and (5) generate a strategy to prevent reoccurrence. The process is designed to take 5 to 10 minutes. The guide also serves as a data collection tool that unit leaders use to screen for generalizable learnings and improvement ideas (Appendix). For example, if a behavioral trigger is identified for a patient, unit leaders disseminate this information to create situational awareness and to ensure care plans are updated.
PSYCHOLOGICAL DEBRIEFING
Psychological debriefing is an application of Critical Incident Stress Management, a comprehensive approach that was developed in the 1970s to help emergency service workers process the thoughts and emotions arising from their exposure to trauma in their work.8,16 More recently, it has become a standard practice in many settings, including healthcare. Notably, psychological debriefing and event debriefing are often conflated. While not mutually exclusive, psychological debriefing has the unique aim of providing support to groups who work together in stressful situations.
Strategies for psychological debriefing are less well described in healthcare. However, our hospital has found it to be a useful tool for MBU staff. Operationally, this process takes the form of a weekly multidisciplinary team meeting with unit clinical staff. Typically, a psychologist or social worker initiates this meeting, which is held at a dedicated time and in a protected space. Discussion centers on patients who have been admitted to the unit for more than 30 days. A goal of the meeting is to review and update patient care plans, but there is also an important goal of emotional processing (Appendix).
In this meeting, staff reflect collectively on the unique stressors they encounter in their work, and they generate situational awareness and potential interventions for these stressors. The psychosocial providers often share recommendations, such as strategies to promote effective communication with patients and families. Peer support is a major component of this meeting and is often utilized to navigate stressful situations, such as disagreements with families regarding behavioral management. Staff also review and reinforce the Positive Behavioral Interventions and Supports framework—a preventive framework that can reduce seclusion and restraint use in pediatric psychiatric units, among other positive outcomes.17 This framework includes setting expectations for patients and families regarding behaviors on the unit. In reviewing these guidelines, staff are encouraged to recognize and report inappropriate behaviors (from patients or families) that can be traumatizing, especially over prolonged hospitalizations. This framework also provides a common language for staff to express behavioral expectations in a positive manner (eg, “Let’s use our walking feet” rather than “No running”). Overall, staff view this meeting as a resilience-building activity that empowers them in their routine work.
IMPLEMENTATION CONSIDERATIONS
While the MBU is a specialized unit with dedicated psychosocial resources, the debriefing practices we describe can be translated to multiple care settings. However, successful implementation relies on intentional process design. First, debriefing indications must be made clear to staff (eg, events of restraint). There should be a role or group accountable for organizing and leading debriefings, which should be held at a time that promotes participation from frontline staff,particularly for CED. Debriefings—especially psychological debriefings—should be held in a protected space. They should have a clear organization, such as use of a survey-based debriefing guide that allows for data collection. Importantly, there should be a unit or hospital leader accountable for disseminating learnings and improvement ideas to relevant staff and ensuring action items are completed. Finally, accountable leaders should evaluate the process’ feasibility, efficacy, and sustainability to inform implementation.
Hospitals must also consider how to train debriefing leaders to facilitate difficult conversations. Some hospitals may have formal communication training programs, but it may also be helpful to leverage the skills of social workers and psychosocial staff.
OTHER CONSIDERATIONS
Debriefing relies on a climate in which staff of diverse backgrounds and professional status feel comfortable speaking up. Psychological safety is critical in any crisis, and hospital leaders should consider how to make staff feel comfortable during this mental health crisis.18 Leaders must also be prepared to support staff beyond debriefing if resources are required for secondary posttraumatic stress, burnout, or compassion fatigue.8,19,20 Employee assistance programs may be a useful resource.
CONCLUSION
Debriefing practices can help hospitals contend with the unique challenges facing patients and staff in a mental health crisis. While debriefing may vary based on need and setting, hospitals should consider CED as a strategy for reducing seclusion and restraint use, which adversely impact patients and staff. Psychological debriefing can also help staff mitigate the psychosocial stressors of their work.
In the wake of the COVID-19 pandemic, hospitals across the country face a crisis in identifying resources for the surging needs of patients with mental health conditions. Compared with 2019, survey and utilization data from 2020 suggest an increase in suicidal ideation and other symptoms among adults,1 and an escalation in mental health-related visits to pediatric emergency departments, respectively.2 Unfortunately, mental health resources have dwindled during this period. Available inpatient psychiatric beds and 24-hour residential treatment beds—already on the decline over the past 5 years—have been massively affected by the pandemic due to capacity constraints and facility closures.3
These factors have placed general medical hospitals (hospitals) at the front lines of a mental health crisis4 for which most are ill prepared. Indeed, once a patient with acute mental health needs is “medically cleared,” they must wait for an available bed at a psychiatric or residential treatment facility.3 This waiting period often delays necessary patient care, as most consultation-liaison psychiatry models are not designed to provide intensive services.5
This waiting period can also place hospital staff in unfamiliar and potentially unsafe scenarios related to physical and psychological stressors. Staff may encounter patient behaviors that risk harm to patients and staff (ie, behavioral crisis events), which may require seclusion (ie, confinement to a locked room) or restraints (chemical, physical, and mechanical). Even in inpatient psychiatric units, an estimated 70% of nurses have been assaulted at least once during their career.6 Such violent behaviors and the interventions required to subdue them can be traumatizing for both patients and staff.7 In fact, the “cost of caring” may be higher for mental health nurses, who often suffer from secondary posttraumatic stress.8 Staff lacking mental health training may encounter additional stressors from feeling powerless to help their patients.
Facing this crisis, hospitals must develop a strategic response that encompasses the needs of both patients and staff. Beyond intensive interventions (eg, additional staffing resources), this response should include lower-effort interventions. In this perspective, we review two debriefing practices—clinical event debriefing and psychological debriefing—that hospitals can feasibly implement during this crisis. These respective practices can ensure safe and effective care of patients by reducing use of restraints and seclusion while also providing crucial support for staff.
CLINICAL EVENT DEBRIEFING
Broadly defined as a facilitated discussion of significant clinical events, clinical event debriefing (CED) can improve both individual and team performance in resuscitation events and patient outcomes.9-11 While CED is often utilized for clinical deterioration events, it can also apply to behavioral crises in a diversity of settings.6
In recent decades, researchers have developed several frameworks for reducing seclusion and restraint practices in psychiatric care settings.6 A common framework is Huckshorn’s Six Core Strategies,6,12,13 which can reduce seclusion and restraint use14 and is feasible to implement.15 This framework advocates for an immediate CED following behavioral crisis events. A unit supervisor or senior staff member not involved in the event should lead the CED, which has several goals. The first priorities, however, are ensuring the physical safety of all staff and returning the unit to normal operations. More broadly, the CED group should review event documentation and interview staff who were present at the time of the event. These processes can help identify antecedents as well as short- and long-term practices, systems, and environmental modifications to prevent reoccurence.12 However, little is known about this practice outside of inpatient psychiatric units.
Our pediatric hospital implemented a CED process in our medical behavioral unit (MBU), a 10-bed unit designed for patients with comorbid mental health needs requiring a higher level of psychosocial resources. The MBU is not an inpatient psychiatric unit, yet more than 50% of patients admitted to the MBU at any given time are hospitalized with a primary psychiatric diagnosis requiring intensive services due to a lack of resources in the community.
Preventing use of restraints is an institutional priority for all areas of our hospital. To reduce restraint use in the MBU, staff are asked to perform immediate CED following behavioral crisis events. This process involves both clinical (eg, nurses, physicians, psychiatric technicians) and nonclinical staff (eg, unit clerks, security officers). All staff involved in the event are invited to attend. A senior staff member not involved in the event typically organizes and leads the CED. The group uses a facilitative guide to (1) review the patient’s history; (2) identify potential triggers for the event; (3) reflect on areas of strength and weakness in unit response; (4) identify systems issues impacting the patient or the unit response; and (5) generate a strategy to prevent reoccurrence. The process is designed to take 5 to 10 minutes. The guide also serves as a data collection tool that unit leaders use to screen for generalizable learnings and improvement ideas (Appendix). For example, if a behavioral trigger is identified for a patient, unit leaders disseminate this information to create situational awareness and to ensure care plans are updated.
PSYCHOLOGICAL DEBRIEFING
Psychological debriefing is an application of Critical Incident Stress Management, a comprehensive approach that was developed in the 1970s to help emergency service workers process the thoughts and emotions arising from their exposure to trauma in their work.8,16 More recently, it has become a standard practice in many settings, including healthcare. Notably, psychological debriefing and event debriefing are often conflated. While not mutually exclusive, psychological debriefing has the unique aim of providing support to groups who work together in stressful situations.
Strategies for psychological debriefing are less well described in healthcare. However, our hospital has found it to be a useful tool for MBU staff. Operationally, this process takes the form of a weekly multidisciplinary team meeting with unit clinical staff. Typically, a psychologist or social worker initiates this meeting, which is held at a dedicated time and in a protected space. Discussion centers on patients who have been admitted to the unit for more than 30 days. A goal of the meeting is to review and update patient care plans, but there is also an important goal of emotional processing (Appendix).
In this meeting, staff reflect collectively on the unique stressors they encounter in their work, and they generate situational awareness and potential interventions for these stressors. The psychosocial providers often share recommendations, such as strategies to promote effective communication with patients and families. Peer support is a major component of this meeting and is often utilized to navigate stressful situations, such as disagreements with families regarding behavioral management. Staff also review and reinforce the Positive Behavioral Interventions and Supports framework—a preventive framework that can reduce seclusion and restraint use in pediatric psychiatric units, among other positive outcomes.17 This framework includes setting expectations for patients and families regarding behaviors on the unit. In reviewing these guidelines, staff are encouraged to recognize and report inappropriate behaviors (from patients or families) that can be traumatizing, especially over prolonged hospitalizations. This framework also provides a common language for staff to express behavioral expectations in a positive manner (eg, “Let’s use our walking feet” rather than “No running”). Overall, staff view this meeting as a resilience-building activity that empowers them in their routine work.
IMPLEMENTATION CONSIDERATIONS
While the MBU is a specialized unit with dedicated psychosocial resources, the debriefing practices we describe can be translated to multiple care settings. However, successful implementation relies on intentional process design. First, debriefing indications must be made clear to staff (eg, events of restraint). There should be a role or group accountable for organizing and leading debriefings, which should be held at a time that promotes participation from frontline staff,particularly for CED. Debriefings—especially psychological debriefings—should be held in a protected space. They should have a clear organization, such as use of a survey-based debriefing guide that allows for data collection. Importantly, there should be a unit or hospital leader accountable for disseminating learnings and improvement ideas to relevant staff and ensuring action items are completed. Finally, accountable leaders should evaluate the process’ feasibility, efficacy, and sustainability to inform implementation.
Hospitals must also consider how to train debriefing leaders to facilitate difficult conversations. Some hospitals may have formal communication training programs, but it may also be helpful to leverage the skills of social workers and psychosocial staff.
OTHER CONSIDERATIONS
Debriefing relies on a climate in which staff of diverse backgrounds and professional status feel comfortable speaking up. Psychological safety is critical in any crisis, and hospital leaders should consider how to make staff feel comfortable during this mental health crisis.18 Leaders must also be prepared to support staff beyond debriefing if resources are required for secondary posttraumatic stress, burnout, or compassion fatigue.8,19,20 Employee assistance programs may be a useful resource.
CONCLUSION
Debriefing practices can help hospitals contend with the unique challenges facing patients and staff in a mental health crisis. While debriefing may vary based on need and setting, hospitals should consider CED as a strategy for reducing seclusion and restraint use, which adversely impact patients and staff. Psychological debriefing can also help staff mitigate the psychosocial stressors of their work.
1. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049-1057. https://doi.org/10.15585/mmwr.mm6932a1
2. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1–October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1675-1680. https://doi.org/10.15585/mmwr.mm6945a3
3. Rapoport R. ‘Every day is an emergency’: The pandemic is worsening psychiatric bed shortages nationwide. Stat News. December 23, 2020. Accessed January 22, 2021. https://www.statnews.com/2020/12/23/mental-health-covid19-psychiatric-beds/
4. A step to ease the pandemic mental health crisis. Scientific American. February 1, 2021. Accessed April 14, 2021. https://www.scientificamerican.com/article/a-step-to-ease-the-pandemic-mental-health-crisis/
5. Sharpe M, Toynbee M, Walker J. Proactive Integrated Consultation-Liaison Psychiatry: A new service model for the psychiatric care of general hospital inpatients. Gen Hosp Psych. 2020;66:9-15. https://doi.org/10.1016/j.genhosppsych.2020.06.005
6. Mangaoil RA, Cleverley K, Peter E. Immediate staff debriefing following seclusions or restraint use in inpatient mental health settings: a scoping review. Clin Nurs Res. 2020;29(7):479-495. https://doi.org/10.1177/1054773818791085
7. Needham I, Abderhalden C, Zeller A, et al. The effect of a training course on nursing students’ attitudes toward, perceptions of, and confidence in managing patient aggression. J Nurs Educ. 2005;44:415-420.
8. Missouridou E. Secondary posttraumatic stress and nurses’ emotional responses to patient’s trauma. J Trauma Nurs. 2017;24(2):110-115. https://doi.org/10.1097/JTN.0000000000000274
9. Blankenship BAC, Fernandez RP, Joy BF, et al. Multidisciplinary review of code events in a heart center. Am J Crit Care. 2016;25(4):90-98. https://doi.org/10.4037/ajcc2016302
10. Wolfe H, Zebuhr C, Topjian AA, et al. Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes. Crit Care Med. 2014;42(7):1688-1695. https://doi.org/10.1097/CCM.0000000000000327
11. Tannenbaum SI, Cerasoli CP. Do team and individual debriefs enhance performance? A meta-analysis. Hum Factors. 2013;55(1):231-245. https://doi.org/10.1177/0018720812448394
12. Huckshorn KA. Reducing seclusion restraint in mental health use settings: core strategies for prevention. J Psychosoc Nurs Ment Health Serv. 2004;42:22-33.
13. Goulet MH, Larue C, Dumais A. Evaluation of seclusion and restraint reduction programs in mental health: a systematic review. Agress Violent Behav. 2017;34:139-146. https://doi.org/10.1016/j.avb.2017.01.019
14. Azeem MW, Aujila A, Rammerth M, et al, Effectiveness of six core strategies based on trauma informed care in reducing seclusions and restraints at a child and adolescent psychiatric hospital. J Child Adolesc Psychiatr Nurs. 2011;24:11-15. https://doi.org/10.1111/jcap.12190
15. Wieman DA, Camacho-Gonsalves T, Huckshorn KA, et al. Multisite study of an evidence-based practice to reduce seclusion and restraint in psychiatric inpatient facilities. Psychiatr Serv. 2014;65(3):345-351. https://doi.org/10.1176/appi.ps.201300210
16. Everly GS. A primer on critical incident stress management: what’s really in a name? Int J Emerg Ment Health. 1999;1(2):77-79.
17. Reynolds EK, Grados MA, Praglowski N, et al. Use of modified positive behavioral interventions and supports in a psychiatric inpatient unit for high-risk youths. Psychiatr Serv. 2016;67(5):570-573. https://doi.org/10.1176/appi.ps.201500039
18. Devaraj LR, Cooper C, Begin AS. Creating psychological safety on medical teams in times of crisis. J Hosp Med. 2021;16(1):47-49. https://doi.org/10.12788/jhm.3541
19. Bride BE, Radey M, Figley CR. Measuring compassion fatigue. Clin Soc Work J. 2007;35:155-163. https://doi.org/10.1007/s10615-007-0091-7
20. Figley CR. Compassion fatigue: psychotherapists’ lack of self care. J Clin Psychol. 2002;58(11):1433-1441. https://doi.org/10.1002/jclp.10090
1. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049-1057. https://doi.org/10.15585/mmwr.mm6932a1
2. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1–October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1675-1680. https://doi.org/10.15585/mmwr.mm6945a3
3. Rapoport R. ‘Every day is an emergency’: The pandemic is worsening psychiatric bed shortages nationwide. Stat News. December 23, 2020. Accessed January 22, 2021. https://www.statnews.com/2020/12/23/mental-health-covid19-psychiatric-beds/
4. A step to ease the pandemic mental health crisis. Scientific American. February 1, 2021. Accessed April 14, 2021. https://www.scientificamerican.com/article/a-step-to-ease-the-pandemic-mental-health-crisis/
5. Sharpe M, Toynbee M, Walker J. Proactive Integrated Consultation-Liaison Psychiatry: A new service model for the psychiatric care of general hospital inpatients. Gen Hosp Psych. 2020;66:9-15. https://doi.org/10.1016/j.genhosppsych.2020.06.005
6. Mangaoil RA, Cleverley K, Peter E. Immediate staff debriefing following seclusions or restraint use in inpatient mental health settings: a scoping review. Clin Nurs Res. 2020;29(7):479-495. https://doi.org/10.1177/1054773818791085
7. Needham I, Abderhalden C, Zeller A, et al. The effect of a training course on nursing students’ attitudes toward, perceptions of, and confidence in managing patient aggression. J Nurs Educ. 2005;44:415-420.
8. Missouridou E. Secondary posttraumatic stress and nurses’ emotional responses to patient’s trauma. J Trauma Nurs. 2017;24(2):110-115. https://doi.org/10.1097/JTN.0000000000000274
9. Blankenship BAC, Fernandez RP, Joy BF, et al. Multidisciplinary review of code events in a heart center. Am J Crit Care. 2016;25(4):90-98. https://doi.org/10.4037/ajcc2016302
10. Wolfe H, Zebuhr C, Topjian AA, et al. Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes. Crit Care Med. 2014;42(7):1688-1695. https://doi.org/10.1097/CCM.0000000000000327
11. Tannenbaum SI, Cerasoli CP. Do team and individual debriefs enhance performance? A meta-analysis. Hum Factors. 2013;55(1):231-245. https://doi.org/10.1177/0018720812448394
12. Huckshorn KA. Reducing seclusion restraint in mental health use settings: core strategies for prevention. J Psychosoc Nurs Ment Health Serv. 2004;42:22-33.
13. Goulet MH, Larue C, Dumais A. Evaluation of seclusion and restraint reduction programs in mental health: a systematic review. Agress Violent Behav. 2017;34:139-146. https://doi.org/10.1016/j.avb.2017.01.019
14. Azeem MW, Aujila A, Rammerth M, et al, Effectiveness of six core strategies based on trauma informed care in reducing seclusions and restraints at a child and adolescent psychiatric hospital. J Child Adolesc Psychiatr Nurs. 2011;24:11-15. https://doi.org/10.1111/jcap.12190
15. Wieman DA, Camacho-Gonsalves T, Huckshorn KA, et al. Multisite study of an evidence-based practice to reduce seclusion and restraint in psychiatric inpatient facilities. Psychiatr Serv. 2014;65(3):345-351. https://doi.org/10.1176/appi.ps.201300210
16. Everly GS. A primer on critical incident stress management: what’s really in a name? Int J Emerg Ment Health. 1999;1(2):77-79.
17. Reynolds EK, Grados MA, Praglowski N, et al. Use of modified positive behavioral interventions and supports in a psychiatric inpatient unit for high-risk youths. Psychiatr Serv. 2016;67(5):570-573. https://doi.org/10.1176/appi.ps.201500039
18. Devaraj LR, Cooper C, Begin AS. Creating psychological safety on medical teams in times of crisis. J Hosp Med. 2021;16(1):47-49. https://doi.org/10.12788/jhm.3541
19. Bride BE, Radey M, Figley CR. Measuring compassion fatigue. Clin Soc Work J. 2007;35:155-163. https://doi.org/10.1007/s10615-007-0091-7
20. Figley CR. Compassion fatigue: psychotherapists’ lack of self care. J Clin Psychol. 2002;58(11):1433-1441. https://doi.org/10.1002/jclp.10090
© 2021 Society of Hospital Medicine
Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan
Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan

This work is licensed under a Creative Commons Attribution 4.0 International License
Since its inception in the mid-1990s, the hospitalist model of care has enjoyed robust growth in the United States, increasing to around 20,000 providers by the end of its first decade.1,2 Since then, it has far outstripped early predictions of adoption, currently standing at more than 50,000 hospitalist providers.2 Although driven by numerous factors, including system-based management needs, provision of inpatient care for unassigned patients, and demands for improved patient safety and satisfaction, this meteoric growth has been driven largely by cost pressures particular to the US healthcare system.1,2 Nonetheless, the growing complexity of healthcare systems, substantial fiscal pressures, and increasing healthcare demands from aging populations are worldwide challenges to which countries outside North America also seek solutions. Countries that have initiated hospitalist care have localized adoption, evolving the model to meet their unique fiscal and system-based needs and patients’ expectations.
While there has been keen interest in the hospitalist model in Asia, there has not yet been widespread adoption, despite numerous data demonstrating that this model is associated with lower length of stay (LOS), as well as lower costs and improved patient safety.3,4 This article explores hospitalist care adoption experiences in Singapore, Taiwan, Korea, and Japan, focusing on stakeholder demand for hospitalist care, respective adoption, outcomes, and associated challenges to date.
SINGAPORE
Stakeholder Demand for Hospitalist Care
Historically in Singapore, family physicians provided primary care and internal medicine subspecialists provided inpatient care.5 Present-day trends, including an aging population, increasing rates of chronic diseases, and multisystem health issues, have stressed the historical model, leading to care fragmentation, long LOS (>9 days), and reduced patient satisfaction.5,6 Additionally, as 80% of hospital care is government funded, public hospitals are under pressure to reduce healthcare expenditures.5
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
To meet patient needs and healthcare system challenges, the hospitalist model has evolved through several iterations in Singapore. The first model, implemented at Singapore General Hospital, utilized family physicians as hospitalists to coordinate inpatient care and integrate care between hospital and community settings.3,5 This model resulted in shorter LOS and reduced costs for patients cared for by family physician hospitalists.3 Despite these benefits, the family physician hospitalist model did not spread, partly due to biases favoring subspecialist care for hospitalized patients.7
The next iteration utilized general internal medicine (GIM) specialists. Traditionally, GIM specialists cared for a small number of low-acuity hospitalized patients. Recognizing the emerging need for holistic inpatient care, the Singapore Ministry of Health supported advances in generalist care, including a financial bonus and a revamped GIM training program. This spawned hospitalist-type models nationwide. At the National University Hospital (NUH), for example, GIM physicians were recruited to care for “specialty” patients in the acute medical unit and increase their ward coverage to include complex multimorbid patients. Additionally, NUH launched the enhanced complex care program, providing integrated inpatient and outpatient care to high-utilizing, complex patients. Overall, the NUH GIM division grew by 70% (faculty) and 60% (trainees) over 5 years. Currently, fueled by government enthusiasm for generalist care, hospitalist-type models are evident at newly minted hospitals across Singapore.
Although physicians act as hospitalists, the term hospitalist is not embraced in Singapore, thus limiting its potential to develop clinical- and system-improvement competencies and establish professional identity. This may be due to the strong UK-based cultural foundations and continued systemic bias favoring subspecialists.8
TAIWAN
Stakeholder Demand for Hospitalist Care
Under its national health insurance (NHI) system, Taiwan has relatively low copayments for medical services, with acute patients paying 10% of costs for a ≤30-day hospitalization, causing demand for inpatient care to remain strong.4,9 The NHI system has also led to increased numbers of patients accessing care in emergency departments (EDs), where costs may be as low as US $16 (NT $450), causing long waits for evaluation and transfer to wards.9,10 There remains an insufficient number of hospital-based physicians to manage this high patient volume, a situation exacerbated by low reimbursements.4
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
In order to address rising admissions, inefficient ED management, and physician shortages, a hospitalist care program was first introduced in Taiwan in 2002, followed by the establishment of a hospitalist-run ward in National Taiwan University Hospital in 2009.11 Subsequent studies from Taiwan have found that hospitalist-run wards had lower admission costs, shorter LOS, and more do-not-resuscitate consent, and also had similar in-hospital mortality and readmission rates compared to specialist-run wards.4,12 Reflecting these successes, the Taiwan Association of Hospital Medicine (TAHM) was established in 2018, and since January 2021, the Ministry of Health and Welfare of Taiwan has mandated hospital medicine programs as an accreditation requirement for all medical centers, with a dual role of educating residents and providing inpatient care.
Despite growing opportunities, Taiwan has seen a modest increase in the number of hospitalists, rising from three in 2009 to around 300 by January 2021. An indistinct professional identity and career path are the main barriers. Given this, TAHM is trying to strengthen hospitalist professionalism by introducing both hard and soft skills, such as utilizing point-of-care ultrasonography and implementing the concepts of Choosing Wisely® and shared decision-making.
KOREA
Stakeholder Demand for Hospitalist Care
Korea has experienced a chronic physician shortage, with just 2.4 physicians per 1,000 people (World Bank, 2017), leading to significant physician burnout. Designed to protect trainee well-being, the 2015 Improvement of Training Conditions and Status of Medical Residents Act limited resident work hours while reducing internal medicine and general surgery training periods, further exacerbating physician shortages.13 In addition, Korea’s current NHI system—including its’ healthcare insurance reimbursements scheme, established in 1989 when Korea’s per capita gross domestic product was less than US $5,000—provides low reimbursements to healthcare providers.14 Along with increased attention to patient safety and healthcare-related consumer expectations, the hospitalist system in Korea aims to maintain improvements to residents’ well-being, while increasing hospital revenue and meeting patient demand for improved services.14
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
Along with the Ministry of Health and Welfare, the Korean Health Insurance Review and Assessment Service launched a hospitalist pilot program in general medicine and surgery in 2016.15 Services for hospitalist-managed inpatients are charged on a new schedule covered by the NHI system, including facility fees, which are charged per diem, and separate hospitalist fees.14 New hospital medicine programs are utilized, in part, to recruit new physicians to manage a large volume of inpatients. Previous studies found that these new hospitalist care systems also improved patient safety, quality of care, and overall patient satisfaction, while being associated with shorter LOS and fewer unnecessary intensive care unit admissions.16,17 After a successful pilot, the revamped reimbursement system for hospitalist care officially started in January 2021.
Although Korea had only 250 registered hospitalists by August 2020, this is likely a substantial underestimate, as only hospital medicine teams with more than two hospitalists were allowed formal registration during the pilot period. Wider registration is currently underway for the new official reimbursement system.
JAPAN
Stakeholder Demand for Hospitalist Care
Hospitals in Japan are organized into highly compartmentalized subspecialties. Providing quality inpatient care to senior patients, who account for more than 28% of the population, and managing smooth transitions from hospital to long-term- care facilities remain challenging. In addition, given generous caps on maximum monthly out-of-pocket payments under its NHI system, LOS for Japanese hospitals are as long as 16.1 days.18 Nonetheless, given rising financial burdens associated with long-term care, hospitals are under government pressure to further shorten LOS and transition patients to local long-term-care facilities after treatment for acute symptoms.
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
To meet these challenges, an increasing number of Japanese hospitals have established departments of general medicine to triage and manage patients with multiple comorbidities and to coordinate patient care across relevant specialties. The Japanese Society of Hospital General Medicine (JSHGM) was established in 2010, and currently has 1,890 members from 896 medical institutions. In 2018, general medicine was recognized by the Japanese Board of Medical Specialties as a formal specialty for certification. Currently, JSHGM is working with the Japan Primary Care Association and other organizations to establish a specialty certification system for hospitalist physicians and raise awareness of hospital medicine. A Japanese study of elderly patients with chronic aspiration pneumonia found that care by hospitalists resulted in shorter LOS and lower costs than specialist care.19 Recently, hospitalists have played a central role in COVID-19 management, opening fever intake clinics and establishing collaborative guidelines with infectious disease experts and other specialists.
Yet, different from the prototypical hospitalist first defined by Wachter and Goldman, Japanese general medicine hospitalists continue to have substantial outpatient responsibilities, albeit in the hospital setting. Out of 81 university hospitals, 69 now have a department of hospital general medicine, though only 20 have inpatient services.20 In addition, a medical culture in which patients continue to see their surgery attendings long after surgery remains strong. Clear definitions regarding hospitalists’ roles need to be established, while promoting changes toward inpatient care for both patients and subspecialists.
DISCUSSION
The four Asian countries reviewed here have all established universal access to healthcare, with Taiwan, Korea, and Japan having strong NHI systems and Singapore providing significant healthcare subsidies for those in need. Nonetheless, they also face similar challenges, including the growing complexity of healthcare systems, substantial fiscal pressures, increased healthcare demands caused by aging populations, and increased expectations regarding stakeholder well-being. As such, these countries share common driving forces that are propelling the adoption of hospitalist care models, such as lack of a sufficient physician workforce on inpatient wards; need for extra resources to shorten ED wait times prior to inpatient admission; need for providing quality care to multimorbid senior patients across highly segmented hospital departments and coordinating medical services between hospitals and outpatient care facilities; and government pressure on cutting costs, especially by shortening inpatient LOS. Some common barriers among these Asian countries include unclear definitions of hospitalists’ roles and degree of collaboration with subspecialty departments, and social and systemic biases favoring subspecialty care for inpatients.
The four Asian countries reviewed here have chosen to adopt the hospitalist model as a supplement to already established, specialty-driven inpatient care systems; as such, further comparative outcome studies focusing on cost, care quality, and patient safety and satisfaction are warranted to bolster professional hospitalist roles, further facilitate government/policy-level support for hospital care systems, and promote future training and certification systems appropriate to each country’s unique healthcare system and medical culture. Similarly, evidence-driven educational outreach programs are warranted to facilitate patient understanding of the role of hospitalists in their care.For countries interested in establishing hospital medicine programs, the adoption experiences in Singapore, Taiwan, Korea, and Japan provide valuable insights regarding how to establish hospitalist models to meet country-specific healthcare challenges while successfully functioning in the context of their unique medical-system frameworks.
1. Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487-494. https://doi.org/10.1001/jama.287.4.487
2. Wachter RM, Goldman L. Zero to 50,000—the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
3. Lee KH, Yang Y, Yang KS, et al. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6:115-121. https://doi.org/10.1002/jhm.821
4. Shu CC, Lin JW, Lin YF, et al. Evaluating the performance of a hospitalist system in Taiwan: a pioneer study for nationwide health insurance in Asia. J Hosp Med. 2011;6(7):378-382. https://doi.org/ 10.1002/jhm.896
5. Lee KH. The hospitalist movement—a complex adaptive response to fragmentation of care in hospitals. Ann Acad Med Singap. 2008;37(2):145-150.
6. Ge L, Ya CW, Heng BH, Tan WS. Frailty and healthcare utilization across care settings among community-dwelling older adults in Singapore. BMC Geriatrics. 2020;20:389. https://doi.org/10.1186/s12877-020-01800-8
7. Lee KH. A historical perspective of the barriers to generalism. Aust Fam Physician. 2015;44(3):154-158.
8. Choo F. Alexandra Hospital provides patients with one-stop services under new care model. Updated December 14, 2018. Accessed March 26, 2021.https://www.straitstimes.com/singapore/health/alexandra-hospital-provides-patients-with-one-stop-services-under-new-care-model
9. National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. Medical services. Copayments. Updated December 28, 2020. Accessed March 26, 2021. https://www.nhi.gov.tw/English/Content_List.aspx?n=E5509C8FE29950EA&topn=1D1ECC54F86E9050
10. Tsai JCH, Chen WY, Liang YW. Nonemergent emergency department visits under the National Health Insurance in Taiwan. Health Policy. 2011;100:189-195. https://doi.org/10.1016/j.healthpol.2010.10.007
11. Taiwan Society of Hospital Medicine. The birth and growth of hospital medicine in Taiwan. Accessed March 26, 2021. https://www.hospitalist.org.tw/about_25.htm
12. Hsu NC, Huang CC, Shu CC, Yang MC. Implementation of a seven-day hospitalist program to improve the outcomes of the weekend admission: a retrospective before-after study in Taiwan. PLoS One. 2018;13(3):e0194833. https://doi.org/10.1371/journal.pone.0194833
13. Ministry of Health and Welfare, Statutes of the Republic of Korea. Act on the Improvement of Training Conditions and Status of Medical Residents. Accessed March 26, 2021. https://elaw.klri.re.kr/eng_mobile/viewer.do?hseq=49563&type=sogan&key=10
14. Chae W, Park EC, Lee KY, et al. Development and evolution of hospital medicine in Korea. J Hosp Med. 2021;16(4):247-250. https://doi.org/10.12788/jhm.3573
15. Oh SJ, Jung EJ. Prospects for the Korean model of the surgical hospitalist system. J Korean Med Assoc. 2020;63(5):236-239. https://doi.org/10.5124/jkma.2020.63.5.236
16. Ohn JH, Kim NH, Kim ES, et al. An acute medical unit in a Korean tertiary care hospital reduces the length of stay and waiting time in the emergency department. J Korean Med Sci. 2017;32:1917-1920. https://doi.org/10.3346/jkms.2017.32.12.1917
17. Lee JH, Kim AJ, Kyong TY, et al. Evaluating the outcome of multi-morbid patients cared for by hospitalists: a report of integrated medical model in Korea. J Korean Med Sci. 2019;34(25):e179. https://doi.org/10.3346/jkms.2019.34.e179
18. OECD. Length of hospital stay. Accessed March 26, 2021. https://doi.org/10.1787/8dda6b7a-en
19. Hamada O, Tsutsumi T, Miki A, et al. Impact of the hospitalist system in Japan on the quality of care and healthcare economics. Intern Med. 2019;58(23):3385-3391. https://doi.org/10.2169/internalmedicine.2872-19
20. Kawashima A. Report on general medicine’s effects on specialists and other healthcare staff in the context of inclusive local medical system. Chapter in Japanese. Accessed March 26, 2021.https://soshin.pcmed-tsukuba.jp/education/report/pdf/05_004.pdf
Since its inception in the mid-1990s, the hospitalist model of care has enjoyed robust growth in the United States, increasing to around 20,000 providers by the end of its first decade.1,2 Since then, it has far outstripped early predictions of adoption, currently standing at more than 50,000 hospitalist providers.2 Although driven by numerous factors, including system-based management needs, provision of inpatient care for unassigned patients, and demands for improved patient safety and satisfaction, this meteoric growth has been driven largely by cost pressures particular to the US healthcare system.1,2 Nonetheless, the growing complexity of healthcare systems, substantial fiscal pressures, and increasing healthcare demands from aging populations are worldwide challenges to which countries outside North America also seek solutions. Countries that have initiated hospitalist care have localized adoption, evolving the model to meet their unique fiscal and system-based needs and patients’ expectations.
While there has been keen interest in the hospitalist model in Asia, there has not yet been widespread adoption, despite numerous data demonstrating that this model is associated with lower length of stay (LOS), as well as lower costs and improved patient safety.3,4 This article explores hospitalist care adoption experiences in Singapore, Taiwan, Korea, and Japan, focusing on stakeholder demand for hospitalist care, respective adoption, outcomes, and associated challenges to date.
SINGAPORE
Stakeholder Demand for Hospitalist Care
Historically in Singapore, family physicians provided primary care and internal medicine subspecialists provided inpatient care.5 Present-day trends, including an aging population, increasing rates of chronic diseases, and multisystem health issues, have stressed the historical model, leading to care fragmentation, long LOS (>9 days), and reduced patient satisfaction.5,6 Additionally, as 80% of hospital care is government funded, public hospitals are under pressure to reduce healthcare expenditures.5
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
To meet patient needs and healthcare system challenges, the hospitalist model has evolved through several iterations in Singapore. The first model, implemented at Singapore General Hospital, utilized family physicians as hospitalists to coordinate inpatient care and integrate care between hospital and community settings.3,5 This model resulted in shorter LOS and reduced costs for patients cared for by family physician hospitalists.3 Despite these benefits, the family physician hospitalist model did not spread, partly due to biases favoring subspecialist care for hospitalized patients.7
The next iteration utilized general internal medicine (GIM) specialists. Traditionally, GIM specialists cared for a small number of low-acuity hospitalized patients. Recognizing the emerging need for holistic inpatient care, the Singapore Ministry of Health supported advances in generalist care, including a financial bonus and a revamped GIM training program. This spawned hospitalist-type models nationwide. At the National University Hospital (NUH), for example, GIM physicians were recruited to care for “specialty” patients in the acute medical unit and increase their ward coverage to include complex multimorbid patients. Additionally, NUH launched the enhanced complex care program, providing integrated inpatient and outpatient care to high-utilizing, complex patients. Overall, the NUH GIM division grew by 70% (faculty) and 60% (trainees) over 5 years. Currently, fueled by government enthusiasm for generalist care, hospitalist-type models are evident at newly minted hospitals across Singapore.
Although physicians act as hospitalists, the term hospitalist is not embraced in Singapore, thus limiting its potential to develop clinical- and system-improvement competencies and establish professional identity. This may be due to the strong UK-based cultural foundations and continued systemic bias favoring subspecialists.8
TAIWAN
Stakeholder Demand for Hospitalist Care
Under its national health insurance (NHI) system, Taiwan has relatively low copayments for medical services, with acute patients paying 10% of costs for a ≤30-day hospitalization, causing demand for inpatient care to remain strong.4,9 The NHI system has also led to increased numbers of patients accessing care in emergency departments (EDs), where costs may be as low as US $16 (NT $450), causing long waits for evaluation and transfer to wards.9,10 There remains an insufficient number of hospital-based physicians to manage this high patient volume, a situation exacerbated by low reimbursements.4
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
In order to address rising admissions, inefficient ED management, and physician shortages, a hospitalist care program was first introduced in Taiwan in 2002, followed by the establishment of a hospitalist-run ward in National Taiwan University Hospital in 2009.11 Subsequent studies from Taiwan have found that hospitalist-run wards had lower admission costs, shorter LOS, and more do-not-resuscitate consent, and also had similar in-hospital mortality and readmission rates compared to specialist-run wards.4,12 Reflecting these successes, the Taiwan Association of Hospital Medicine (TAHM) was established in 2018, and since January 2021, the Ministry of Health and Welfare of Taiwan has mandated hospital medicine programs as an accreditation requirement for all medical centers, with a dual role of educating residents and providing inpatient care.
Despite growing opportunities, Taiwan has seen a modest increase in the number of hospitalists, rising from three in 2009 to around 300 by January 2021. An indistinct professional identity and career path are the main barriers. Given this, TAHM is trying to strengthen hospitalist professionalism by introducing both hard and soft skills, such as utilizing point-of-care ultrasonography and implementing the concepts of Choosing Wisely® and shared decision-making.
KOREA
Stakeholder Demand for Hospitalist Care
Korea has experienced a chronic physician shortage, with just 2.4 physicians per 1,000 people (World Bank, 2017), leading to significant physician burnout. Designed to protect trainee well-being, the 2015 Improvement of Training Conditions and Status of Medical Residents Act limited resident work hours while reducing internal medicine and general surgery training periods, further exacerbating physician shortages.13 In addition, Korea’s current NHI system—including its’ healthcare insurance reimbursements scheme, established in 1989 when Korea’s per capita gross domestic product was less than US $5,000—provides low reimbursements to healthcare providers.14 Along with increased attention to patient safety and healthcare-related consumer expectations, the hospitalist system in Korea aims to maintain improvements to residents’ well-being, while increasing hospital revenue and meeting patient demand for improved services.14
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
Along with the Ministry of Health and Welfare, the Korean Health Insurance Review and Assessment Service launched a hospitalist pilot program in general medicine and surgery in 2016.15 Services for hospitalist-managed inpatients are charged on a new schedule covered by the NHI system, including facility fees, which are charged per diem, and separate hospitalist fees.14 New hospital medicine programs are utilized, in part, to recruit new physicians to manage a large volume of inpatients. Previous studies found that these new hospitalist care systems also improved patient safety, quality of care, and overall patient satisfaction, while being associated with shorter LOS and fewer unnecessary intensive care unit admissions.16,17 After a successful pilot, the revamped reimbursement system for hospitalist care officially started in January 2021.
Although Korea had only 250 registered hospitalists by August 2020, this is likely a substantial underestimate, as only hospital medicine teams with more than two hospitalists were allowed formal registration during the pilot period. Wider registration is currently underway for the new official reimbursement system.
JAPAN
Stakeholder Demand for Hospitalist Care
Hospitals in Japan are organized into highly compartmentalized subspecialties. Providing quality inpatient care to senior patients, who account for more than 28% of the population, and managing smooth transitions from hospital to long-term- care facilities remain challenging. In addition, given generous caps on maximum monthly out-of-pocket payments under its NHI system, LOS for Japanese hospitals are as long as 16.1 days.18 Nonetheless, given rising financial burdens associated with long-term care, hospitals are under government pressure to further shorten LOS and transition patients to local long-term-care facilities after treatment for acute symptoms.
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
To meet these challenges, an increasing number of Japanese hospitals have established departments of general medicine to triage and manage patients with multiple comorbidities and to coordinate patient care across relevant specialties. The Japanese Society of Hospital General Medicine (JSHGM) was established in 2010, and currently has 1,890 members from 896 medical institutions. In 2018, general medicine was recognized by the Japanese Board of Medical Specialties as a formal specialty for certification. Currently, JSHGM is working with the Japan Primary Care Association and other organizations to establish a specialty certification system for hospitalist physicians and raise awareness of hospital medicine. A Japanese study of elderly patients with chronic aspiration pneumonia found that care by hospitalists resulted in shorter LOS and lower costs than specialist care.19 Recently, hospitalists have played a central role in COVID-19 management, opening fever intake clinics and establishing collaborative guidelines with infectious disease experts and other specialists.
Yet, different from the prototypical hospitalist first defined by Wachter and Goldman, Japanese general medicine hospitalists continue to have substantial outpatient responsibilities, albeit in the hospital setting. Out of 81 university hospitals, 69 now have a department of hospital general medicine, though only 20 have inpatient services.20 In addition, a medical culture in which patients continue to see their surgery attendings long after surgery remains strong. Clear definitions regarding hospitalists’ roles need to be established, while promoting changes toward inpatient care for both patients and subspecialists.
DISCUSSION
The four Asian countries reviewed here have all established universal access to healthcare, with Taiwan, Korea, and Japan having strong NHI systems and Singapore providing significant healthcare subsidies for those in need. Nonetheless, they also face similar challenges, including the growing complexity of healthcare systems, substantial fiscal pressures, increased healthcare demands caused by aging populations, and increased expectations regarding stakeholder well-being. As such, these countries share common driving forces that are propelling the adoption of hospitalist care models, such as lack of a sufficient physician workforce on inpatient wards; need for extra resources to shorten ED wait times prior to inpatient admission; need for providing quality care to multimorbid senior patients across highly segmented hospital departments and coordinating medical services between hospitals and outpatient care facilities; and government pressure on cutting costs, especially by shortening inpatient LOS. Some common barriers among these Asian countries include unclear definitions of hospitalists’ roles and degree of collaboration with subspecialty departments, and social and systemic biases favoring subspecialty care for inpatients.
The four Asian countries reviewed here have chosen to adopt the hospitalist model as a supplement to already established, specialty-driven inpatient care systems; as such, further comparative outcome studies focusing on cost, care quality, and patient safety and satisfaction are warranted to bolster professional hospitalist roles, further facilitate government/policy-level support for hospital care systems, and promote future training and certification systems appropriate to each country’s unique healthcare system and medical culture. Similarly, evidence-driven educational outreach programs are warranted to facilitate patient understanding of the role of hospitalists in their care.For countries interested in establishing hospital medicine programs, the adoption experiences in Singapore, Taiwan, Korea, and Japan provide valuable insights regarding how to establish hospitalist models to meet country-specific healthcare challenges while successfully functioning in the context of their unique medical-system frameworks.
Since its inception in the mid-1990s, the hospitalist model of care has enjoyed robust growth in the United States, increasing to around 20,000 providers by the end of its first decade.1,2 Since then, it has far outstripped early predictions of adoption, currently standing at more than 50,000 hospitalist providers.2 Although driven by numerous factors, including system-based management needs, provision of inpatient care for unassigned patients, and demands for improved patient safety and satisfaction, this meteoric growth has been driven largely by cost pressures particular to the US healthcare system.1,2 Nonetheless, the growing complexity of healthcare systems, substantial fiscal pressures, and increasing healthcare demands from aging populations are worldwide challenges to which countries outside North America also seek solutions. Countries that have initiated hospitalist care have localized adoption, evolving the model to meet their unique fiscal and system-based needs and patients’ expectations.
While there has been keen interest in the hospitalist model in Asia, there has not yet been widespread adoption, despite numerous data demonstrating that this model is associated with lower length of stay (LOS), as well as lower costs and improved patient safety.3,4 This article explores hospitalist care adoption experiences in Singapore, Taiwan, Korea, and Japan, focusing on stakeholder demand for hospitalist care, respective adoption, outcomes, and associated challenges to date.
SINGAPORE
Stakeholder Demand for Hospitalist Care
Historically in Singapore, family physicians provided primary care and internal medicine subspecialists provided inpatient care.5 Present-day trends, including an aging population, increasing rates of chronic diseases, and multisystem health issues, have stressed the historical model, leading to care fragmentation, long LOS (>9 days), and reduced patient satisfaction.5,6 Additionally, as 80% of hospital care is government funded, public hospitals are under pressure to reduce healthcare expenditures.5
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
To meet patient needs and healthcare system challenges, the hospitalist model has evolved through several iterations in Singapore. The first model, implemented at Singapore General Hospital, utilized family physicians as hospitalists to coordinate inpatient care and integrate care between hospital and community settings.3,5 This model resulted in shorter LOS and reduced costs for patients cared for by family physician hospitalists.3 Despite these benefits, the family physician hospitalist model did not spread, partly due to biases favoring subspecialist care for hospitalized patients.7
The next iteration utilized general internal medicine (GIM) specialists. Traditionally, GIM specialists cared for a small number of low-acuity hospitalized patients. Recognizing the emerging need for holistic inpatient care, the Singapore Ministry of Health supported advances in generalist care, including a financial bonus and a revamped GIM training program. This spawned hospitalist-type models nationwide. At the National University Hospital (NUH), for example, GIM physicians were recruited to care for “specialty” patients in the acute medical unit and increase their ward coverage to include complex multimorbid patients. Additionally, NUH launched the enhanced complex care program, providing integrated inpatient and outpatient care to high-utilizing, complex patients. Overall, the NUH GIM division grew by 70% (faculty) and 60% (trainees) over 5 years. Currently, fueled by government enthusiasm for generalist care, hospitalist-type models are evident at newly minted hospitals across Singapore.
Although physicians act as hospitalists, the term hospitalist is not embraced in Singapore, thus limiting its potential to develop clinical- and system-improvement competencies and establish professional identity. This may be due to the strong UK-based cultural foundations and continued systemic bias favoring subspecialists.8
TAIWAN
Stakeholder Demand for Hospitalist Care
Under its national health insurance (NHI) system, Taiwan has relatively low copayments for medical services, with acute patients paying 10% of costs for a ≤30-day hospitalization, causing demand for inpatient care to remain strong.4,9 The NHI system has also led to increased numbers of patients accessing care in emergency departments (EDs), where costs may be as low as US $16 (NT $450), causing long waits for evaluation and transfer to wards.9,10 There remains an insufficient number of hospital-based physicians to manage this high patient volume, a situation exacerbated by low reimbursements.4
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
In order to address rising admissions, inefficient ED management, and physician shortages, a hospitalist care program was first introduced in Taiwan in 2002, followed by the establishment of a hospitalist-run ward in National Taiwan University Hospital in 2009.11 Subsequent studies from Taiwan have found that hospitalist-run wards had lower admission costs, shorter LOS, and more do-not-resuscitate consent, and also had similar in-hospital mortality and readmission rates compared to specialist-run wards.4,12 Reflecting these successes, the Taiwan Association of Hospital Medicine (TAHM) was established in 2018, and since January 2021, the Ministry of Health and Welfare of Taiwan has mandated hospital medicine programs as an accreditation requirement for all medical centers, with a dual role of educating residents and providing inpatient care.
Despite growing opportunities, Taiwan has seen a modest increase in the number of hospitalists, rising from three in 2009 to around 300 by January 2021. An indistinct professional identity and career path are the main barriers. Given this, TAHM is trying to strengthen hospitalist professionalism by introducing both hard and soft skills, such as utilizing point-of-care ultrasonography and implementing the concepts of Choosing Wisely® and shared decision-making.
KOREA
Stakeholder Demand for Hospitalist Care
Korea has experienced a chronic physician shortage, with just 2.4 physicians per 1,000 people (World Bank, 2017), leading to significant physician burnout. Designed to protect trainee well-being, the 2015 Improvement of Training Conditions and Status of Medical Residents Act limited resident work hours while reducing internal medicine and general surgery training periods, further exacerbating physician shortages.13 In addition, Korea’s current NHI system—including its’ healthcare insurance reimbursements scheme, established in 1989 when Korea’s per capita gross domestic product was less than US $5,000—provides low reimbursements to healthcare providers.14 Along with increased attention to patient safety and healthcare-related consumer expectations, the hospitalist system in Korea aims to maintain improvements to residents’ well-being, while increasing hospital revenue and meeting patient demand for improved services.14
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
Along with the Ministry of Health and Welfare, the Korean Health Insurance Review and Assessment Service launched a hospitalist pilot program in general medicine and surgery in 2016.15 Services for hospitalist-managed inpatients are charged on a new schedule covered by the NHI system, including facility fees, which are charged per diem, and separate hospitalist fees.14 New hospital medicine programs are utilized, in part, to recruit new physicians to manage a large volume of inpatients. Previous studies found that these new hospitalist care systems also improved patient safety, quality of care, and overall patient satisfaction, while being associated with shorter LOS and fewer unnecessary intensive care unit admissions.16,17 After a successful pilot, the revamped reimbursement system for hospitalist care officially started in January 2021.
Although Korea had only 250 registered hospitalists by August 2020, this is likely a substantial underestimate, as only hospital medicine teams with more than two hospitalists were allowed formal registration during the pilot period. Wider registration is currently underway for the new official reimbursement system.
JAPAN
Stakeholder Demand for Hospitalist Care
Hospitals in Japan are organized into highly compartmentalized subspecialties. Providing quality inpatient care to senior patients, who account for more than 28% of the population, and managing smooth transitions from hospital to long-term- care facilities remain challenging. In addition, given generous caps on maximum monthly out-of-pocket payments under its NHI system, LOS for Japanese hospitals are as long as 16.1 days.18 Nonetheless, given rising financial burdens associated with long-term care, hospitals are under government pressure to further shorten LOS and transition patients to local long-term-care facilities after treatment for acute symptoms.
Adoption of Hospitalist Care, Outcomes, and Challenges Faced
To meet these challenges, an increasing number of Japanese hospitals have established departments of general medicine to triage and manage patients with multiple comorbidities and to coordinate patient care across relevant specialties. The Japanese Society of Hospital General Medicine (JSHGM) was established in 2010, and currently has 1,890 members from 896 medical institutions. In 2018, general medicine was recognized by the Japanese Board of Medical Specialties as a formal specialty for certification. Currently, JSHGM is working with the Japan Primary Care Association and other organizations to establish a specialty certification system for hospitalist physicians and raise awareness of hospital medicine. A Japanese study of elderly patients with chronic aspiration pneumonia found that care by hospitalists resulted in shorter LOS and lower costs than specialist care.19 Recently, hospitalists have played a central role in COVID-19 management, opening fever intake clinics and establishing collaborative guidelines with infectious disease experts and other specialists.
Yet, different from the prototypical hospitalist first defined by Wachter and Goldman, Japanese general medicine hospitalists continue to have substantial outpatient responsibilities, albeit in the hospital setting. Out of 81 university hospitals, 69 now have a department of hospital general medicine, though only 20 have inpatient services.20 In addition, a medical culture in which patients continue to see their surgery attendings long after surgery remains strong. Clear definitions regarding hospitalists’ roles need to be established, while promoting changes toward inpatient care for both patients and subspecialists.
DISCUSSION
The four Asian countries reviewed here have all established universal access to healthcare, with Taiwan, Korea, and Japan having strong NHI systems and Singapore providing significant healthcare subsidies for those in need. Nonetheless, they also face similar challenges, including the growing complexity of healthcare systems, substantial fiscal pressures, increased healthcare demands caused by aging populations, and increased expectations regarding stakeholder well-being. As such, these countries share common driving forces that are propelling the adoption of hospitalist care models, such as lack of a sufficient physician workforce on inpatient wards; need for extra resources to shorten ED wait times prior to inpatient admission; need for providing quality care to multimorbid senior patients across highly segmented hospital departments and coordinating medical services between hospitals and outpatient care facilities; and government pressure on cutting costs, especially by shortening inpatient LOS. Some common barriers among these Asian countries include unclear definitions of hospitalists’ roles and degree of collaboration with subspecialty departments, and social and systemic biases favoring subspecialty care for inpatients.
The four Asian countries reviewed here have chosen to adopt the hospitalist model as a supplement to already established, specialty-driven inpatient care systems; as such, further comparative outcome studies focusing on cost, care quality, and patient safety and satisfaction are warranted to bolster professional hospitalist roles, further facilitate government/policy-level support for hospital care systems, and promote future training and certification systems appropriate to each country’s unique healthcare system and medical culture. Similarly, evidence-driven educational outreach programs are warranted to facilitate patient understanding of the role of hospitalists in their care.For countries interested in establishing hospital medicine programs, the adoption experiences in Singapore, Taiwan, Korea, and Japan provide valuable insights regarding how to establish hospitalist models to meet country-specific healthcare challenges while successfully functioning in the context of their unique medical-system frameworks.
1. Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487-494. https://doi.org/10.1001/jama.287.4.487
2. Wachter RM, Goldman L. Zero to 50,000—the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
3. Lee KH, Yang Y, Yang KS, et al. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6:115-121. https://doi.org/10.1002/jhm.821
4. Shu CC, Lin JW, Lin YF, et al. Evaluating the performance of a hospitalist system in Taiwan: a pioneer study for nationwide health insurance in Asia. J Hosp Med. 2011;6(7):378-382. https://doi.org/ 10.1002/jhm.896
5. Lee KH. The hospitalist movement—a complex adaptive response to fragmentation of care in hospitals. Ann Acad Med Singap. 2008;37(2):145-150.
6. Ge L, Ya CW, Heng BH, Tan WS. Frailty and healthcare utilization across care settings among community-dwelling older adults in Singapore. BMC Geriatrics. 2020;20:389. https://doi.org/10.1186/s12877-020-01800-8
7. Lee KH. A historical perspective of the barriers to generalism. Aust Fam Physician. 2015;44(3):154-158.
8. Choo F. Alexandra Hospital provides patients with one-stop services under new care model. Updated December 14, 2018. Accessed March 26, 2021.https://www.straitstimes.com/singapore/health/alexandra-hospital-provides-patients-with-one-stop-services-under-new-care-model
9. National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. Medical services. Copayments. Updated December 28, 2020. Accessed March 26, 2021. https://www.nhi.gov.tw/English/Content_List.aspx?n=E5509C8FE29950EA&topn=1D1ECC54F86E9050
10. Tsai JCH, Chen WY, Liang YW. Nonemergent emergency department visits under the National Health Insurance in Taiwan. Health Policy. 2011;100:189-195. https://doi.org/10.1016/j.healthpol.2010.10.007
11. Taiwan Society of Hospital Medicine. The birth and growth of hospital medicine in Taiwan. Accessed March 26, 2021. https://www.hospitalist.org.tw/about_25.htm
12. Hsu NC, Huang CC, Shu CC, Yang MC. Implementation of a seven-day hospitalist program to improve the outcomes of the weekend admission: a retrospective before-after study in Taiwan. PLoS One. 2018;13(3):e0194833. https://doi.org/10.1371/journal.pone.0194833
13. Ministry of Health and Welfare, Statutes of the Republic of Korea. Act on the Improvement of Training Conditions and Status of Medical Residents. Accessed March 26, 2021. https://elaw.klri.re.kr/eng_mobile/viewer.do?hseq=49563&type=sogan&key=10
14. Chae W, Park EC, Lee KY, et al. Development and evolution of hospital medicine in Korea. J Hosp Med. 2021;16(4):247-250. https://doi.org/10.12788/jhm.3573
15. Oh SJ, Jung EJ. Prospects for the Korean model of the surgical hospitalist system. J Korean Med Assoc. 2020;63(5):236-239. https://doi.org/10.5124/jkma.2020.63.5.236
16. Ohn JH, Kim NH, Kim ES, et al. An acute medical unit in a Korean tertiary care hospital reduces the length of stay and waiting time in the emergency department. J Korean Med Sci. 2017;32:1917-1920. https://doi.org/10.3346/jkms.2017.32.12.1917
17. Lee JH, Kim AJ, Kyong TY, et al. Evaluating the outcome of multi-morbid patients cared for by hospitalists: a report of integrated medical model in Korea. J Korean Med Sci. 2019;34(25):e179. https://doi.org/10.3346/jkms.2019.34.e179
18. OECD. Length of hospital stay. Accessed March 26, 2021. https://doi.org/10.1787/8dda6b7a-en
19. Hamada O, Tsutsumi T, Miki A, et al. Impact of the hospitalist system in Japan on the quality of care and healthcare economics. Intern Med. 2019;58(23):3385-3391. https://doi.org/10.2169/internalmedicine.2872-19
20. Kawashima A. Report on general medicine’s effects on specialists and other healthcare staff in the context of inclusive local medical system. Chapter in Japanese. Accessed March 26, 2021.https://soshin.pcmed-tsukuba.jp/education/report/pdf/05_004.pdf
1. Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487-494. https://doi.org/10.1001/jama.287.4.487
2. Wachter RM, Goldman L. Zero to 50,000—the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958
3. Lee KH, Yang Y, Yang KS, et al. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6:115-121. https://doi.org/10.1002/jhm.821
4. Shu CC, Lin JW, Lin YF, et al. Evaluating the performance of a hospitalist system in Taiwan: a pioneer study for nationwide health insurance in Asia. J Hosp Med. 2011;6(7):378-382. https://doi.org/ 10.1002/jhm.896
5. Lee KH. The hospitalist movement—a complex adaptive response to fragmentation of care in hospitals. Ann Acad Med Singap. 2008;37(2):145-150.
6. Ge L, Ya CW, Heng BH, Tan WS. Frailty and healthcare utilization across care settings among community-dwelling older adults in Singapore. BMC Geriatrics. 2020;20:389. https://doi.org/10.1186/s12877-020-01800-8
7. Lee KH. A historical perspective of the barriers to generalism. Aust Fam Physician. 2015;44(3):154-158.
8. Choo F. Alexandra Hospital provides patients with one-stop services under new care model. Updated December 14, 2018. Accessed March 26, 2021.https://www.straitstimes.com/singapore/health/alexandra-hospital-provides-patients-with-one-stop-services-under-new-care-model
9. National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. Medical services. Copayments. Updated December 28, 2020. Accessed March 26, 2021. https://www.nhi.gov.tw/English/Content_List.aspx?n=E5509C8FE29950EA&topn=1D1ECC54F86E9050
10. Tsai JCH, Chen WY, Liang YW. Nonemergent emergency department visits under the National Health Insurance in Taiwan. Health Policy. 2011;100:189-195. https://doi.org/10.1016/j.healthpol.2010.10.007
11. Taiwan Society of Hospital Medicine. The birth and growth of hospital medicine in Taiwan. Accessed March 26, 2021. https://www.hospitalist.org.tw/about_25.htm
12. Hsu NC, Huang CC, Shu CC, Yang MC. Implementation of a seven-day hospitalist program to improve the outcomes of the weekend admission: a retrospective before-after study in Taiwan. PLoS One. 2018;13(3):e0194833. https://doi.org/10.1371/journal.pone.0194833
13. Ministry of Health and Welfare, Statutes of the Republic of Korea. Act on the Improvement of Training Conditions and Status of Medical Residents. Accessed March 26, 2021. https://elaw.klri.re.kr/eng_mobile/viewer.do?hseq=49563&type=sogan&key=10
14. Chae W, Park EC, Lee KY, et al. Development and evolution of hospital medicine in Korea. J Hosp Med. 2021;16(4):247-250. https://doi.org/10.12788/jhm.3573
15. Oh SJ, Jung EJ. Prospects for the Korean model of the surgical hospitalist system. J Korean Med Assoc. 2020;63(5):236-239. https://doi.org/10.5124/jkma.2020.63.5.236
16. Ohn JH, Kim NH, Kim ES, et al. An acute medical unit in a Korean tertiary care hospital reduces the length of stay and waiting time in the emergency department. J Korean Med Sci. 2017;32:1917-1920. https://doi.org/10.3346/jkms.2017.32.12.1917
17. Lee JH, Kim AJ, Kyong TY, et al. Evaluating the outcome of multi-morbid patients cared for by hospitalists: a report of integrated medical model in Korea. J Korean Med Sci. 2019;34(25):e179. https://doi.org/10.3346/jkms.2019.34.e179
18. OECD. Length of hospital stay. Accessed March 26, 2021. https://doi.org/10.1787/8dda6b7a-en
19. Hamada O, Tsutsumi T, Miki A, et al. Impact of the hospitalist system in Japan on the quality of care and healthcare economics. Intern Med. 2019;58(23):3385-3391. https://doi.org/10.2169/internalmedicine.2872-19
20. Kawashima A. Report on general medicine’s effects on specialists and other healthcare staff in the context of inclusive local medical system. Chapter in Japanese. Accessed March 26, 2021.https://soshin.pcmed-tsukuba.jp/education/report/pdf/05_004.pdf
Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan

This work is licensed under a Creative Commons Attribution 4.0 International License
Adoption of Hospitalist Care in Asia: Experiences From Singapore, Taiwan, Korea, and Japan

This work is licensed under a Creative Commons Attribution 4.0 International License
© 2021 Society of Hospital Medicine
Trauma-Informed Transformation of Evaluation and Licensure for Physicians With Mental Illness
As a physician living with bipolar disorder, I am more intimately familiar with the psychiatric ward than I would like to admit. Despite a decade of medication and weekly therapy, I live with a disease which flares, not unlike many of the patients I care for.
–Justin L Bullock, MD, MPH
Mental health conditions are common among physicians. Approximately 28% of residents experience depression or depressive symptoms during their training,1 and many will not seek mental health care due to fear of medical licensing implications.2 These fears are well-founded. Executive directors of 13 of 35 state medical boards indicated that diagnosis of mental illness alone was sufficient for sanctioning physicians.3 Another study found that two-thirds of state licensing applications pose questions about providers’ mental health that violate the American with Disabilities Act.2 What happens when a physician discloses and trusts the system to support their mental health–related needs? We address this question through the story of one trainee (JLB) recounting his experience with help-seeking and a fitness-for-duty (FFD) evaluation and conclude with recommendations to improve FFD processes.
Once again, I found myself sitting on a sheetless hospital bed with a baggy hospital gown draping my bony shoulders as I described my aborted suicide attempt to an attending psychiatrist. After a brief pause, the psychiatrist told me that they did not want to cause problems for my medical license and would drop my psychiatric hold. Even though they were the third psychiatrist to say this to me, their words caught me off guard given my recent attempt. I believe these psychiatrists factored my medical career into their clinical care because they understood that the simple act of being psychiatrically hospitalized placed my medical career in peril. After I completed a month-long outpatient treatment program, a psychiatrist and therapist cleared me to return to work.
I feel no shame about living with bipolar disorder and have always been transparent with my institution; the reason behind my absence was no secret. But before I could return to work, my case had to be reviewed by my institution’s Physician Well-being Committee. This committee was presented to me as a group that would help determine how to best support my return to work. However, before I had an opportunity to speak with the committee, I was informed that I would have to undergo a formal FFD evaluation.
FITNESS FOR DUTY
A FFD evaluation is indicated when there are credible reports of physician impairment or professional misconduct. Its purpose is to ensure that physicians can perform their essential job functions and that they are not a risk to patient safety. The Federation of State Medical Boards cautions that illness should not be conflated with impairment.4 Indeed, physicians with mental illness can function safely, thrive, and benefit patients and peers, especially when accommodations or modification reduce workplace barriers.5,6
I can best describe FFD as a 2-month-long stigmatized interrogation. I was forced to provide hair, blood, and urine samples for drug tests, complete an extensive multi-day psychiatric interview—including questions about my childhood trauma—and given a personality test. I was asked to disclose all of my private mental health records and feared I would be penalized if I refused to answer any questions. Multiple people, including my program director, confirmed that there were no performance or professionalism concerns. My suicide attempt happened outside of work; in my eyes, I had a mental illness which had been appropriately treated, not a workplace issue. I voiced my concern that the committee discriminated against me based on my mental illness. The committee told me that their decision to conduct a FFD was warranted because I had a condition that could affect my cognition, despite the lack of evidence that it actually had. My institution’s Office for Prevention of Harassment and Discrimination concurred that this was legal practice.
All of this happened despite my transparency regarding my bipolar disorder. Before I began residency, I disclosed my illness to my institution’s disability office, and I requested and received workplace accommodations. I have appropriately called-out of work whenever I felt that my bipolar could interfere with my focus on patient care. I have been openly bipolar and at the same institution for 6 years. In that time, I have received multiple teaching awards and a graduation award for exemplifying the qualities of a true physician—all while managing bipolar flares, including four hospitalizations. To destigmatize mental illness, I have discussed suicidality and getting help multiple times in front of hundreds of medical students.
The FFD evaluation found no evidence of a substance use disorder, nonadherence to treatment, or danger to my patients. Despite no adverse findings, and a record of well-managed mental illness and ongoing treatment, if I wanted to return to residency, I had to sign an agreement stipulating frequent monitoring by a “case-manager” and worksite “mentor.” I felt stigmatized and penalized for getting help. As I spoke out publicly against this process, I learned that my FFD experience is neither unique nor uncommon. Mental illness is deeply stigmatized within medicine. As a gay Black bipolar man, I hold multiple marginalized identities that inform and shape my experiences, yet the FFD committee did not have a single psychiatrist nor a single Black member. Instead, to make decisions on my case, they relied on the recommendations of the external psychiatrist, who met me for two days. In addition to the therapy and medications I had been taking for years, in order to return to work, I had to agree to a new type of therapy for the remainder of residency. I was incredulous that my employers felt it was appropriate to dictate my specific psychiatric care when I already had my own providers and my own care plan. My voice was not heard in this process, and despite my objections and the institutional mentors who spoke up for me, the FFD committee would not permit me to work without agreeing to their unmodified terms.
RE-ENVISIONING PHYSICIAN EVALUATION
Institutions face the challenging task of simultaneously navigating physician illness, patient safety, and institutional liability. In our opinion, many institutions excessively scrutinize physicians with mental illness and initiate FFD evaluations for reasons that are disproportionately skewed toward minimizing institutional liability. Moreover, in the absence of demonstrated physician workplace impairment, institutions should have systems in place to work collaboratively with the physician to ensure that they have access to professional treatment and appropriate workplace accommodations. It is possible to be simultaneously disabled and completely competent; creative and supportive accommodation processes allow physicians with disabilities to thrive, and their patients to benefit from the care of a physician with personal experience navigating disability. If a physician’s mental illness, despite accommodations, begins to impact workplace safety, a FFD evaluation may be initiated; unfortunately, the FFD evaluation itself may become a source of further harm.
FFD EVALUATIONS' POTENTIAL TO HARM PHYSICIANS WITH MENTAL ILLNESS
FFD evaluations often situate the physician as incapable of managing their own mental illness, suggesting that they must be closely monitored and restricted even when physicians come forward independently.7 These beliefs and concurrent policies can propagate harmful, inaccurate biases against physicians who live with mental illness. These biases are compounded by the structural racism endemic in healthcare and academic medicine.8 Dehumanization in medicine adds fuel to this fire, projecting the ideal physician persona as an invulnerable, infallible superhuman who can witness intense suffering and work inhumane hours without impact upon the their mental health and well-being. Altogether, these factors increase fear and discourage help-seeking among physicians with mental illness (Appendix Figure), ultimately harming physicians and patients in the process.9 Given that the FFD process involves evaluation, treatment, surveillance, and restrictions for individuals with stigmatized health conditions, these processes risk amplifying the impacts of trauma, racism, and oppression unless specifically designed to be antiracist, anti-oppressive, and trauma-informed.
TRAUMA-INFORMED APPROACH TO FFD
To encourage physician help-seeking, especially for stigmatized conditions, we must dismantle systems that traumatize physicians with mental illness (Appendix Figure) and build systems that invite and support courageous vulnerability and help-seeking.5,6 Institutions can provide evaluation and oversight of physicians while also adopting trauma-informed care principles. A trauma-informed approach to FFD would ask: How can we create systems that are informed by a genuine understanding of suffering to promote healing and avoid re-traumatization? Trauma-informed care emphasizes safety, trustworthiness, transparency, cultural humility (an antiracist, anti-oppression framework), collaboration, peer support, and patient empowerment.10 FFD evaluations differ by institution and by state, with some being performed internally and others utilizing external state physician health programs. We believe our recommendations below apply independent of context (Table).
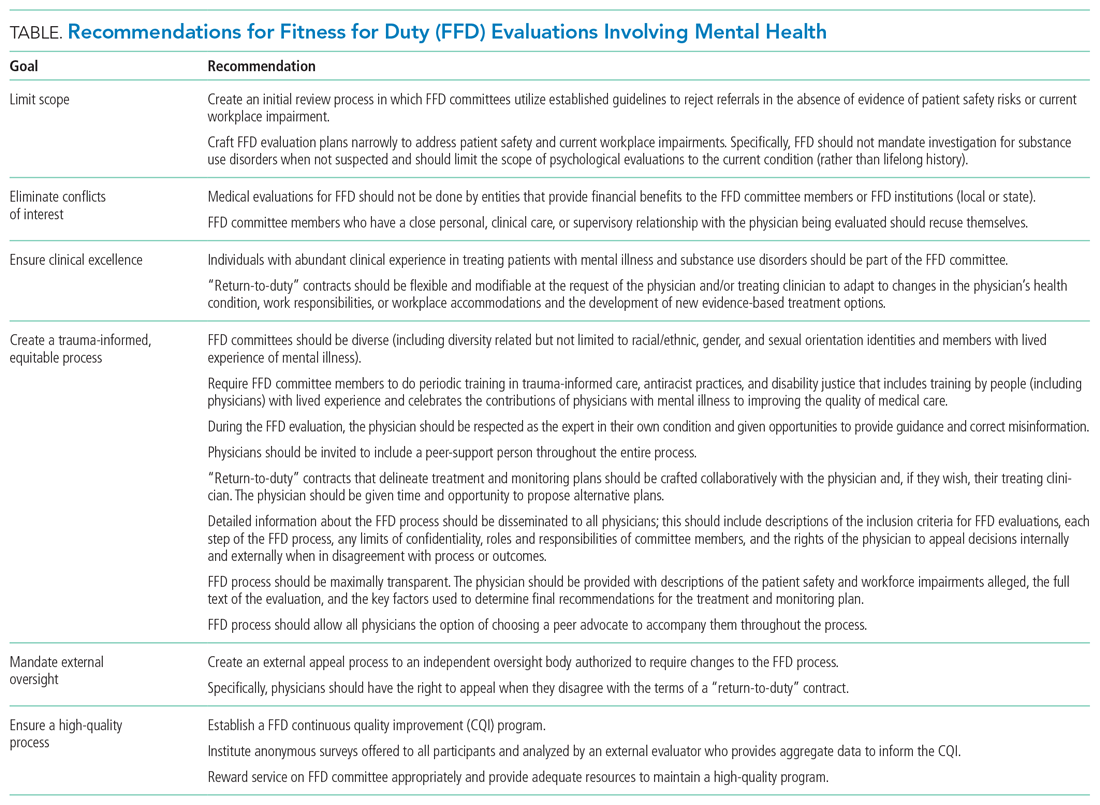
NECESSARY CHANGES
Institutional Changes
All institutions must publish a detailed description of the FFD process, including its purpose, the definition of impairment or potential impairment, and the steps of the FFD evaluation. The FFD evaluation should be as limited in scope as possible, without invasive inquiry about the physician’s life-long history. Physicians should be invited to include a peer-support person throughout the entire process. The FFD “return to work agreement” should incorporate meaningful input from the physician as the expert in their own experience and, if already in treatment, informed by their healthcare providers. Given the stigmatization of mental health conditions and inherent power differentials in FFD processes, it is paramount that committees be diverse (including but not limited to race/ethnicity, gender, sexual orientation, and mental illness) and comprised of physicians trained in trauma-informed processes who treat the conditions affecting the individual undergoing the FFD evaluation. Finally, trustworthiness requires accountability: We recommend that all FFD systems establish an external oversight body that is equipped to effect change in real time if a physician reports a potential process violation and that collects anonymous feedback from physicians to inform required continuous quality improvement.
State and Federal Changes
It is difficult to effect meaningful change without accurate measurement of physician suicide. Therefore, we recommend mandatory reporting of physician suicide and suspected suicide to publicly available, de-identified state registries. We call for each state medical licensing board to limit licensing questions to current impairment due to mental illness, substance use disorders, or other health condition, as recommended by the Federation of State Medical Boards.4 There is a critical need for federal legislation to fund improvements in workplace safety and enhanced access to mental health treatment on demand for physicians.
Especially in these extraordinary times, as physicians are being exposed to such high burdens of stress, suffering, loss, and moral injury, we must de-stigmatize mental illness, encourage help-seeking, and provide physicians struggling with mental illness with timely and compassionate support. By creating systems that are healing and supportive for physicians, we enhance healing for all.
Bipolar is my sun and my storm. As a physician, I am not ashamed of that. For my own health and that of my patients, I must work in a system where it is safe to come forward when I am struggling.
As I fought against what I felt was a toxic and injurious process, I was fortunate to not stand alone. More than 600 residents from 18 departments at my institution signed a petition in support of reforming the FFD process informed by my experience. My institution is in the early stages of responding to this display of strength and unity with a diverse taskforce dedicated to improving the Physician Well-being Committee and FFD process.
As I accompany my patients on their healing journeys, my own experience with recovery allows me to hold the hope of healing for them. My family, friends, mentors, and providers held these rays of hope for me when I was lost in my own darkness. I now know that being cured from disease is just one form of healing. My proximity to death grounds me as some of my patients approach the end of life. Notably, some of my primary care patients have read my story online and come to their appointments to tell me that they are proud to have me as their doctor, “bipolar and all.”
1. Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians a systematic review and meta-analysis. JAMA. 2015;314(22):2373-2383 . https://doi.org/10.1001/jama.2015.15845
2. Dyrbye LN, West CP, Sinsky CA, Goeders LE, Satele DV, Shanafelt TD. Medical Licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clin Proc. 2017;92(10):1486-1493. https://doi.org/10.1016/j.mayocp.2017.06.020
3. Hendin H, Reynolds C, Fox D, et al. Licensing and physician mental health: problems and possibilities. J Med Licens Discip. 2007;93(2):6-11.
4. Federation of State Medical Boards. Physician wellness and burnout: report and recommendations of the workgroup on physician wellness and burnout. 2018. Accessed February 6, 2021. https://www.fsmb.org/siteassets/advocacy/policies/policy-on-wellness-and-burnout.pdf
5. Kirch D. Physician mental health: my personal journey and professional plea. Acad Med. 2021;96(5):618-620. https://doi.org/10.1097/ACM.0000000000003942
6. Cho HL, Huang CJ. Why mental health–related stigma matters for physician wellbeing, burnout, and patient care. J Gen Intern Med. 2020;24:1-3. https://doi.org/10.1007/s11606-019-05173-6
7. Hill AB. Breaking the stigma - a physician’s perspective on self-care and recovery. N Engl J Med. 2017;376(12):1103-1105. https://doi.org/10.1056/NEJMp1615974
8. Grubbs V. Diversity, equity, and inclusion that matter. N Engl J Med. 2020;383(4):e25. https://doi.org/10.1056/NEJMpv2022639
9. Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54-62. https://doi.org/10.1001/archsurg.2010.292
10. Trauma-Informed Care Implementation Resource Center. Center for Healthcare Strategy. Accessed February 5, 2021. https://www.traumainformedcare.chcs.org/what-is-trauma-informed-care/
As a physician living with bipolar disorder, I am more intimately familiar with the psychiatric ward than I would like to admit. Despite a decade of medication and weekly therapy, I live with a disease which flares, not unlike many of the patients I care for.
–Justin L Bullock, MD, MPH
Mental health conditions are common among physicians. Approximately 28% of residents experience depression or depressive symptoms during their training,1 and many will not seek mental health care due to fear of medical licensing implications.2 These fears are well-founded. Executive directors of 13 of 35 state medical boards indicated that diagnosis of mental illness alone was sufficient for sanctioning physicians.3 Another study found that two-thirds of state licensing applications pose questions about providers’ mental health that violate the American with Disabilities Act.2 What happens when a physician discloses and trusts the system to support their mental health–related needs? We address this question through the story of one trainee (JLB) recounting his experience with help-seeking and a fitness-for-duty (FFD) evaluation and conclude with recommendations to improve FFD processes.
Once again, I found myself sitting on a sheetless hospital bed with a baggy hospital gown draping my bony shoulders as I described my aborted suicide attempt to an attending psychiatrist. After a brief pause, the psychiatrist told me that they did not want to cause problems for my medical license and would drop my psychiatric hold. Even though they were the third psychiatrist to say this to me, their words caught me off guard given my recent attempt. I believe these psychiatrists factored my medical career into their clinical care because they understood that the simple act of being psychiatrically hospitalized placed my medical career in peril. After I completed a month-long outpatient treatment program, a psychiatrist and therapist cleared me to return to work.
I feel no shame about living with bipolar disorder and have always been transparent with my institution; the reason behind my absence was no secret. But before I could return to work, my case had to be reviewed by my institution’s Physician Well-being Committee. This committee was presented to me as a group that would help determine how to best support my return to work. However, before I had an opportunity to speak with the committee, I was informed that I would have to undergo a formal FFD evaluation.
FITNESS FOR DUTY
A FFD evaluation is indicated when there are credible reports of physician impairment or professional misconduct. Its purpose is to ensure that physicians can perform their essential job functions and that they are not a risk to patient safety. The Federation of State Medical Boards cautions that illness should not be conflated with impairment.4 Indeed, physicians with mental illness can function safely, thrive, and benefit patients and peers, especially when accommodations or modification reduce workplace barriers.5,6
I can best describe FFD as a 2-month-long stigmatized interrogation. I was forced to provide hair, blood, and urine samples for drug tests, complete an extensive multi-day psychiatric interview—including questions about my childhood trauma—and given a personality test. I was asked to disclose all of my private mental health records and feared I would be penalized if I refused to answer any questions. Multiple people, including my program director, confirmed that there were no performance or professionalism concerns. My suicide attempt happened outside of work; in my eyes, I had a mental illness which had been appropriately treated, not a workplace issue. I voiced my concern that the committee discriminated against me based on my mental illness. The committee told me that their decision to conduct a FFD was warranted because I had a condition that could affect my cognition, despite the lack of evidence that it actually had. My institution’s Office for Prevention of Harassment and Discrimination concurred that this was legal practice.
All of this happened despite my transparency regarding my bipolar disorder. Before I began residency, I disclosed my illness to my institution’s disability office, and I requested and received workplace accommodations. I have appropriately called-out of work whenever I felt that my bipolar could interfere with my focus on patient care. I have been openly bipolar and at the same institution for 6 years. In that time, I have received multiple teaching awards and a graduation award for exemplifying the qualities of a true physician—all while managing bipolar flares, including four hospitalizations. To destigmatize mental illness, I have discussed suicidality and getting help multiple times in front of hundreds of medical students.
The FFD evaluation found no evidence of a substance use disorder, nonadherence to treatment, or danger to my patients. Despite no adverse findings, and a record of well-managed mental illness and ongoing treatment, if I wanted to return to residency, I had to sign an agreement stipulating frequent monitoring by a “case-manager” and worksite “mentor.” I felt stigmatized and penalized for getting help. As I spoke out publicly against this process, I learned that my FFD experience is neither unique nor uncommon. Mental illness is deeply stigmatized within medicine. As a gay Black bipolar man, I hold multiple marginalized identities that inform and shape my experiences, yet the FFD committee did not have a single psychiatrist nor a single Black member. Instead, to make decisions on my case, they relied on the recommendations of the external psychiatrist, who met me for two days. In addition to the therapy and medications I had been taking for years, in order to return to work, I had to agree to a new type of therapy for the remainder of residency. I was incredulous that my employers felt it was appropriate to dictate my specific psychiatric care when I already had my own providers and my own care plan. My voice was not heard in this process, and despite my objections and the institutional mentors who spoke up for me, the FFD committee would not permit me to work without agreeing to their unmodified terms.
RE-ENVISIONING PHYSICIAN EVALUATION
Institutions face the challenging task of simultaneously navigating physician illness, patient safety, and institutional liability. In our opinion, many institutions excessively scrutinize physicians with mental illness and initiate FFD evaluations for reasons that are disproportionately skewed toward minimizing institutional liability. Moreover, in the absence of demonstrated physician workplace impairment, institutions should have systems in place to work collaboratively with the physician to ensure that they have access to professional treatment and appropriate workplace accommodations. It is possible to be simultaneously disabled and completely competent; creative and supportive accommodation processes allow physicians with disabilities to thrive, and their patients to benefit from the care of a physician with personal experience navigating disability. If a physician’s mental illness, despite accommodations, begins to impact workplace safety, a FFD evaluation may be initiated; unfortunately, the FFD evaluation itself may become a source of further harm.
FFD EVALUATIONS' POTENTIAL TO HARM PHYSICIANS WITH MENTAL ILLNESS
FFD evaluations often situate the physician as incapable of managing their own mental illness, suggesting that they must be closely monitored and restricted even when physicians come forward independently.7 These beliefs and concurrent policies can propagate harmful, inaccurate biases against physicians who live with mental illness. These biases are compounded by the structural racism endemic in healthcare and academic medicine.8 Dehumanization in medicine adds fuel to this fire, projecting the ideal physician persona as an invulnerable, infallible superhuman who can witness intense suffering and work inhumane hours without impact upon the their mental health and well-being. Altogether, these factors increase fear and discourage help-seeking among physicians with mental illness (Appendix Figure), ultimately harming physicians and patients in the process.9 Given that the FFD process involves evaluation, treatment, surveillance, and restrictions for individuals with stigmatized health conditions, these processes risk amplifying the impacts of trauma, racism, and oppression unless specifically designed to be antiracist, anti-oppressive, and trauma-informed.
TRAUMA-INFORMED APPROACH TO FFD
To encourage physician help-seeking, especially for stigmatized conditions, we must dismantle systems that traumatize physicians with mental illness (Appendix Figure) and build systems that invite and support courageous vulnerability and help-seeking.5,6 Institutions can provide evaluation and oversight of physicians while also adopting trauma-informed care principles. A trauma-informed approach to FFD would ask: How can we create systems that are informed by a genuine understanding of suffering to promote healing and avoid re-traumatization? Trauma-informed care emphasizes safety, trustworthiness, transparency, cultural humility (an antiracist, anti-oppression framework), collaboration, peer support, and patient empowerment.10 FFD evaluations differ by institution and by state, with some being performed internally and others utilizing external state physician health programs. We believe our recommendations below apply independent of context (Table).
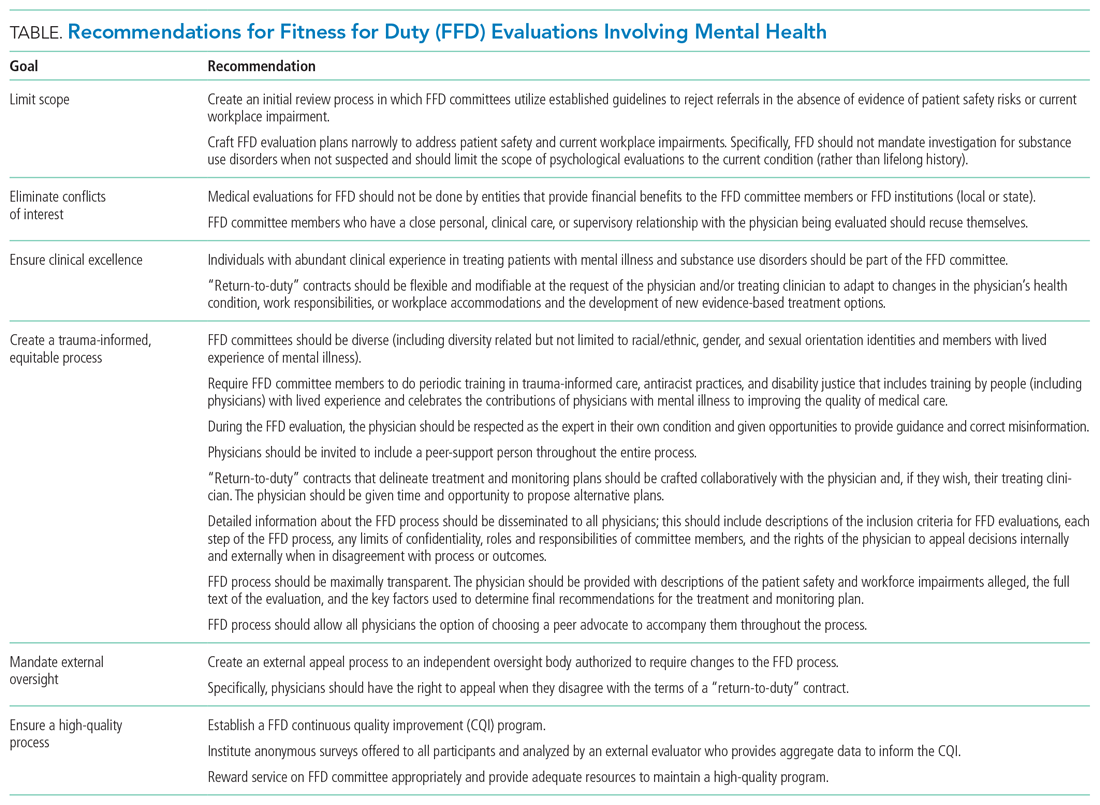
NECESSARY CHANGES
Institutional Changes
All institutions must publish a detailed description of the FFD process, including its purpose, the definition of impairment or potential impairment, and the steps of the FFD evaluation. The FFD evaluation should be as limited in scope as possible, without invasive inquiry about the physician’s life-long history. Physicians should be invited to include a peer-support person throughout the entire process. The FFD “return to work agreement” should incorporate meaningful input from the physician as the expert in their own experience and, if already in treatment, informed by their healthcare providers. Given the stigmatization of mental health conditions and inherent power differentials in FFD processes, it is paramount that committees be diverse (including but not limited to race/ethnicity, gender, sexual orientation, and mental illness) and comprised of physicians trained in trauma-informed processes who treat the conditions affecting the individual undergoing the FFD evaluation. Finally, trustworthiness requires accountability: We recommend that all FFD systems establish an external oversight body that is equipped to effect change in real time if a physician reports a potential process violation and that collects anonymous feedback from physicians to inform required continuous quality improvement.
State and Federal Changes
It is difficult to effect meaningful change without accurate measurement of physician suicide. Therefore, we recommend mandatory reporting of physician suicide and suspected suicide to publicly available, de-identified state registries. We call for each state medical licensing board to limit licensing questions to current impairment due to mental illness, substance use disorders, or other health condition, as recommended by the Federation of State Medical Boards.4 There is a critical need for federal legislation to fund improvements in workplace safety and enhanced access to mental health treatment on demand for physicians.
Especially in these extraordinary times, as physicians are being exposed to such high burdens of stress, suffering, loss, and moral injury, we must de-stigmatize mental illness, encourage help-seeking, and provide physicians struggling with mental illness with timely and compassionate support. By creating systems that are healing and supportive for physicians, we enhance healing for all.
Bipolar is my sun and my storm. As a physician, I am not ashamed of that. For my own health and that of my patients, I must work in a system where it is safe to come forward when I am struggling.
As I fought against what I felt was a toxic and injurious process, I was fortunate to not stand alone. More than 600 residents from 18 departments at my institution signed a petition in support of reforming the FFD process informed by my experience. My institution is in the early stages of responding to this display of strength and unity with a diverse taskforce dedicated to improving the Physician Well-being Committee and FFD process.
As I accompany my patients on their healing journeys, my own experience with recovery allows me to hold the hope of healing for them. My family, friends, mentors, and providers held these rays of hope for me when I was lost in my own darkness. I now know that being cured from disease is just one form of healing. My proximity to death grounds me as some of my patients approach the end of life. Notably, some of my primary care patients have read my story online and come to their appointments to tell me that they are proud to have me as their doctor, “bipolar and all.”
As a physician living with bipolar disorder, I am more intimately familiar with the psychiatric ward than I would like to admit. Despite a decade of medication and weekly therapy, I live with a disease which flares, not unlike many of the patients I care for.
–Justin L Bullock, MD, MPH
Mental health conditions are common among physicians. Approximately 28% of residents experience depression or depressive symptoms during their training,1 and many will not seek mental health care due to fear of medical licensing implications.2 These fears are well-founded. Executive directors of 13 of 35 state medical boards indicated that diagnosis of mental illness alone was sufficient for sanctioning physicians.3 Another study found that two-thirds of state licensing applications pose questions about providers’ mental health that violate the American with Disabilities Act.2 What happens when a physician discloses and trusts the system to support their mental health–related needs? We address this question through the story of one trainee (JLB) recounting his experience with help-seeking and a fitness-for-duty (FFD) evaluation and conclude with recommendations to improve FFD processes.
Once again, I found myself sitting on a sheetless hospital bed with a baggy hospital gown draping my bony shoulders as I described my aborted suicide attempt to an attending psychiatrist. After a brief pause, the psychiatrist told me that they did not want to cause problems for my medical license and would drop my psychiatric hold. Even though they were the third psychiatrist to say this to me, their words caught me off guard given my recent attempt. I believe these psychiatrists factored my medical career into their clinical care because they understood that the simple act of being psychiatrically hospitalized placed my medical career in peril. After I completed a month-long outpatient treatment program, a psychiatrist and therapist cleared me to return to work.
I feel no shame about living with bipolar disorder and have always been transparent with my institution; the reason behind my absence was no secret. But before I could return to work, my case had to be reviewed by my institution’s Physician Well-being Committee. This committee was presented to me as a group that would help determine how to best support my return to work. However, before I had an opportunity to speak with the committee, I was informed that I would have to undergo a formal FFD evaluation.
FITNESS FOR DUTY
A FFD evaluation is indicated when there are credible reports of physician impairment or professional misconduct. Its purpose is to ensure that physicians can perform their essential job functions and that they are not a risk to patient safety. The Federation of State Medical Boards cautions that illness should not be conflated with impairment.4 Indeed, physicians with mental illness can function safely, thrive, and benefit patients and peers, especially when accommodations or modification reduce workplace barriers.5,6
I can best describe FFD as a 2-month-long stigmatized interrogation. I was forced to provide hair, blood, and urine samples for drug tests, complete an extensive multi-day psychiatric interview—including questions about my childhood trauma—and given a personality test. I was asked to disclose all of my private mental health records and feared I would be penalized if I refused to answer any questions. Multiple people, including my program director, confirmed that there were no performance or professionalism concerns. My suicide attempt happened outside of work; in my eyes, I had a mental illness which had been appropriately treated, not a workplace issue. I voiced my concern that the committee discriminated against me based on my mental illness. The committee told me that their decision to conduct a FFD was warranted because I had a condition that could affect my cognition, despite the lack of evidence that it actually had. My institution’s Office for Prevention of Harassment and Discrimination concurred that this was legal practice.
All of this happened despite my transparency regarding my bipolar disorder. Before I began residency, I disclosed my illness to my institution’s disability office, and I requested and received workplace accommodations. I have appropriately called-out of work whenever I felt that my bipolar could interfere with my focus on patient care. I have been openly bipolar and at the same institution for 6 years. In that time, I have received multiple teaching awards and a graduation award for exemplifying the qualities of a true physician—all while managing bipolar flares, including four hospitalizations. To destigmatize mental illness, I have discussed suicidality and getting help multiple times in front of hundreds of medical students.
The FFD evaluation found no evidence of a substance use disorder, nonadherence to treatment, or danger to my patients. Despite no adverse findings, and a record of well-managed mental illness and ongoing treatment, if I wanted to return to residency, I had to sign an agreement stipulating frequent monitoring by a “case-manager” and worksite “mentor.” I felt stigmatized and penalized for getting help. As I spoke out publicly against this process, I learned that my FFD experience is neither unique nor uncommon. Mental illness is deeply stigmatized within medicine. As a gay Black bipolar man, I hold multiple marginalized identities that inform and shape my experiences, yet the FFD committee did not have a single psychiatrist nor a single Black member. Instead, to make decisions on my case, they relied on the recommendations of the external psychiatrist, who met me for two days. In addition to the therapy and medications I had been taking for years, in order to return to work, I had to agree to a new type of therapy for the remainder of residency. I was incredulous that my employers felt it was appropriate to dictate my specific psychiatric care when I already had my own providers and my own care plan. My voice was not heard in this process, and despite my objections and the institutional mentors who spoke up for me, the FFD committee would not permit me to work without agreeing to their unmodified terms.
RE-ENVISIONING PHYSICIAN EVALUATION
Institutions face the challenging task of simultaneously navigating physician illness, patient safety, and institutional liability. In our opinion, many institutions excessively scrutinize physicians with mental illness and initiate FFD evaluations for reasons that are disproportionately skewed toward minimizing institutional liability. Moreover, in the absence of demonstrated physician workplace impairment, institutions should have systems in place to work collaboratively with the physician to ensure that they have access to professional treatment and appropriate workplace accommodations. It is possible to be simultaneously disabled and completely competent; creative and supportive accommodation processes allow physicians with disabilities to thrive, and their patients to benefit from the care of a physician with personal experience navigating disability. If a physician’s mental illness, despite accommodations, begins to impact workplace safety, a FFD evaluation may be initiated; unfortunately, the FFD evaluation itself may become a source of further harm.
FFD EVALUATIONS' POTENTIAL TO HARM PHYSICIANS WITH MENTAL ILLNESS
FFD evaluations often situate the physician as incapable of managing their own mental illness, suggesting that they must be closely monitored and restricted even when physicians come forward independently.7 These beliefs and concurrent policies can propagate harmful, inaccurate biases against physicians who live with mental illness. These biases are compounded by the structural racism endemic in healthcare and academic medicine.8 Dehumanization in medicine adds fuel to this fire, projecting the ideal physician persona as an invulnerable, infallible superhuman who can witness intense suffering and work inhumane hours without impact upon the their mental health and well-being. Altogether, these factors increase fear and discourage help-seeking among physicians with mental illness (Appendix Figure), ultimately harming physicians and patients in the process.9 Given that the FFD process involves evaluation, treatment, surveillance, and restrictions for individuals with stigmatized health conditions, these processes risk amplifying the impacts of trauma, racism, and oppression unless specifically designed to be antiracist, anti-oppressive, and trauma-informed.
TRAUMA-INFORMED APPROACH TO FFD
To encourage physician help-seeking, especially for stigmatized conditions, we must dismantle systems that traumatize physicians with mental illness (Appendix Figure) and build systems that invite and support courageous vulnerability and help-seeking.5,6 Institutions can provide evaluation and oversight of physicians while also adopting trauma-informed care principles. A trauma-informed approach to FFD would ask: How can we create systems that are informed by a genuine understanding of suffering to promote healing and avoid re-traumatization? Trauma-informed care emphasizes safety, trustworthiness, transparency, cultural humility (an antiracist, anti-oppression framework), collaboration, peer support, and patient empowerment.10 FFD evaluations differ by institution and by state, with some being performed internally and others utilizing external state physician health programs. We believe our recommendations below apply independent of context (Table).
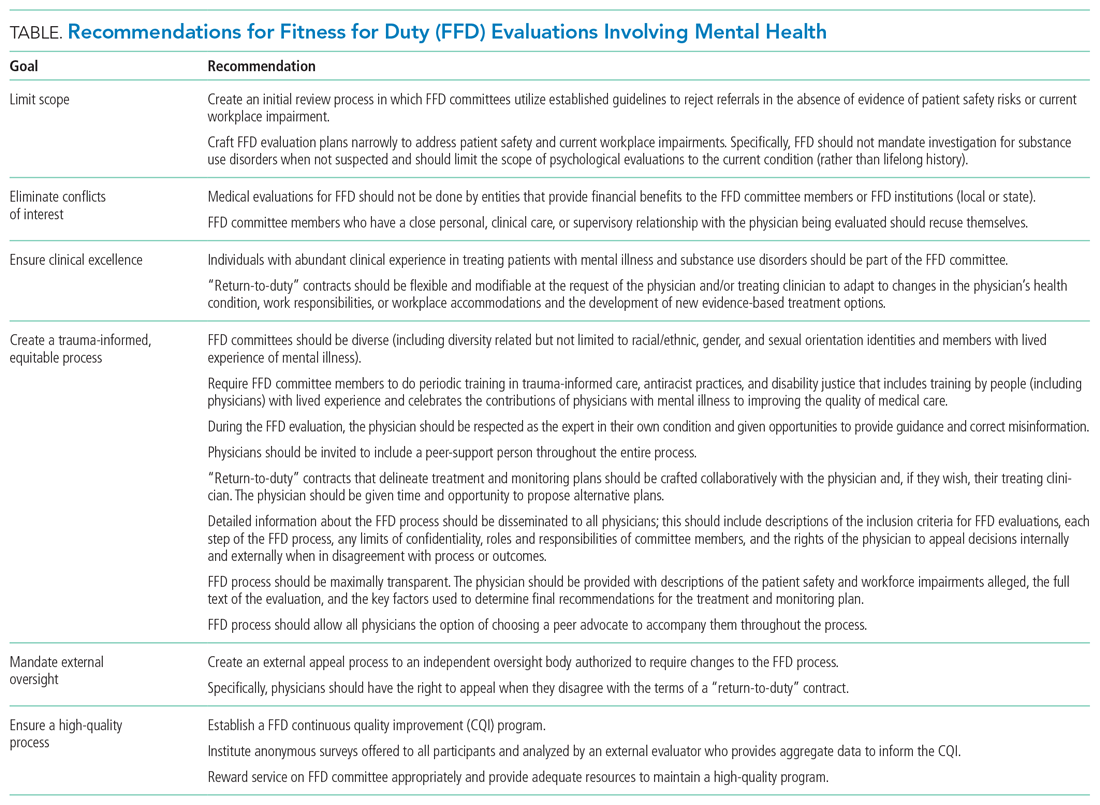
NECESSARY CHANGES
Institutional Changes
All institutions must publish a detailed description of the FFD process, including its purpose, the definition of impairment or potential impairment, and the steps of the FFD evaluation. The FFD evaluation should be as limited in scope as possible, without invasive inquiry about the physician’s life-long history. Physicians should be invited to include a peer-support person throughout the entire process. The FFD “return to work agreement” should incorporate meaningful input from the physician as the expert in their own experience and, if already in treatment, informed by their healthcare providers. Given the stigmatization of mental health conditions and inherent power differentials in FFD processes, it is paramount that committees be diverse (including but not limited to race/ethnicity, gender, sexual orientation, and mental illness) and comprised of physicians trained in trauma-informed processes who treat the conditions affecting the individual undergoing the FFD evaluation. Finally, trustworthiness requires accountability: We recommend that all FFD systems establish an external oversight body that is equipped to effect change in real time if a physician reports a potential process violation and that collects anonymous feedback from physicians to inform required continuous quality improvement.
State and Federal Changes
It is difficult to effect meaningful change without accurate measurement of physician suicide. Therefore, we recommend mandatory reporting of physician suicide and suspected suicide to publicly available, de-identified state registries. We call for each state medical licensing board to limit licensing questions to current impairment due to mental illness, substance use disorders, or other health condition, as recommended by the Federation of State Medical Boards.4 There is a critical need for federal legislation to fund improvements in workplace safety and enhanced access to mental health treatment on demand for physicians.
Especially in these extraordinary times, as physicians are being exposed to such high burdens of stress, suffering, loss, and moral injury, we must de-stigmatize mental illness, encourage help-seeking, and provide physicians struggling with mental illness with timely and compassionate support. By creating systems that are healing and supportive for physicians, we enhance healing for all.
Bipolar is my sun and my storm. As a physician, I am not ashamed of that. For my own health and that of my patients, I must work in a system where it is safe to come forward when I am struggling.
As I fought against what I felt was a toxic and injurious process, I was fortunate to not stand alone. More than 600 residents from 18 departments at my institution signed a petition in support of reforming the FFD process informed by my experience. My institution is in the early stages of responding to this display of strength and unity with a diverse taskforce dedicated to improving the Physician Well-being Committee and FFD process.
As I accompany my patients on their healing journeys, my own experience with recovery allows me to hold the hope of healing for them. My family, friends, mentors, and providers held these rays of hope for me when I was lost in my own darkness. I now know that being cured from disease is just one form of healing. My proximity to death grounds me as some of my patients approach the end of life. Notably, some of my primary care patients have read my story online and come to their appointments to tell me that they are proud to have me as their doctor, “bipolar and all.”
1. Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians a systematic review and meta-analysis. JAMA. 2015;314(22):2373-2383 . https://doi.org/10.1001/jama.2015.15845
2. Dyrbye LN, West CP, Sinsky CA, Goeders LE, Satele DV, Shanafelt TD. Medical Licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clin Proc. 2017;92(10):1486-1493. https://doi.org/10.1016/j.mayocp.2017.06.020
3. Hendin H, Reynolds C, Fox D, et al. Licensing and physician mental health: problems and possibilities. J Med Licens Discip. 2007;93(2):6-11.
4. Federation of State Medical Boards. Physician wellness and burnout: report and recommendations of the workgroup on physician wellness and burnout. 2018. Accessed February 6, 2021. https://www.fsmb.org/siteassets/advocacy/policies/policy-on-wellness-and-burnout.pdf
5. Kirch D. Physician mental health: my personal journey and professional plea. Acad Med. 2021;96(5):618-620. https://doi.org/10.1097/ACM.0000000000003942
6. Cho HL, Huang CJ. Why mental health–related stigma matters for physician wellbeing, burnout, and patient care. J Gen Intern Med. 2020;24:1-3. https://doi.org/10.1007/s11606-019-05173-6
7. Hill AB. Breaking the stigma - a physician’s perspective on self-care and recovery. N Engl J Med. 2017;376(12):1103-1105. https://doi.org/10.1056/NEJMp1615974
8. Grubbs V. Diversity, equity, and inclusion that matter. N Engl J Med. 2020;383(4):e25. https://doi.org/10.1056/NEJMpv2022639
9. Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54-62. https://doi.org/10.1001/archsurg.2010.292
10. Trauma-Informed Care Implementation Resource Center. Center for Healthcare Strategy. Accessed February 5, 2021. https://www.traumainformedcare.chcs.org/what-is-trauma-informed-care/
1. Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians a systematic review and meta-analysis. JAMA. 2015;314(22):2373-2383 . https://doi.org/10.1001/jama.2015.15845
2. Dyrbye LN, West CP, Sinsky CA, Goeders LE, Satele DV, Shanafelt TD. Medical Licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clin Proc. 2017;92(10):1486-1493. https://doi.org/10.1016/j.mayocp.2017.06.020
3. Hendin H, Reynolds C, Fox D, et al. Licensing and physician mental health: problems and possibilities. J Med Licens Discip. 2007;93(2):6-11.
4. Federation of State Medical Boards. Physician wellness and burnout: report and recommendations of the workgroup on physician wellness and burnout. 2018. Accessed February 6, 2021. https://www.fsmb.org/siteassets/advocacy/policies/policy-on-wellness-and-burnout.pdf
5. Kirch D. Physician mental health: my personal journey and professional plea. Acad Med. 2021;96(5):618-620. https://doi.org/10.1097/ACM.0000000000003942
6. Cho HL, Huang CJ. Why mental health–related stigma matters for physician wellbeing, burnout, and patient care. J Gen Intern Med. 2020;24:1-3. https://doi.org/10.1007/s11606-019-05173-6
7. Hill AB. Breaking the stigma - a physician’s perspective on self-care and recovery. N Engl J Med. 2017;376(12):1103-1105. https://doi.org/10.1056/NEJMp1615974
8. Grubbs V. Diversity, equity, and inclusion that matter. N Engl J Med. 2020;383(4):e25. https://doi.org/10.1056/NEJMpv2022639
9. Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54-62. https://doi.org/10.1001/archsurg.2010.292
10. Trauma-Informed Care Implementation Resource Center. Center for Healthcare Strategy. Accessed February 5, 2021. https://www.traumainformedcare.chcs.org/what-is-trauma-informed-care/
© 2021 Society of Hospital Medicine
End the Routine Shackling of Incarcerated Inpatients
The police shooting of Jacob Blake, an unarmed Wisconsin man, during an arrest in August 2020, led to more protests in a summer filled with calls against the unequal application of police force. Outrage grew as it was revealed that Blake, paralyzed from his waist down and not yet convicted of a crime, was still handcuffed to his hospital bed while receiving treatment.1 To many this seemed unusually cruel, but to those tasked with caring for incarcerated patients, it is all too familiar. Given the high rates of incarceration in the United States and the increased medical needs of this population, caring for those in custody is unavoidable for many physicians and hospitals. Though safety should be paramount, the universal application of metal handcuffs or leg cuffs by law enforcement officials, a process known as shackling, can lead to a variety of harms and should be abandoned.
BACKGROUND
The United States incarcerates more individuals both in total numbers and per capita than any other country in the world. This is currently believed to be more than two million people on any given day or more than 650 persons per 100,000 population.2 Incarceration occurs in jails, which are locally run facilities holding individuals on short sentences or those not yet convicted who are unable to afford bail before their trials (pretrial), or prisons, which are state and federally run facilities that house those with long sentences. When an incarcerated person experiences a medical emergency requiring hospitalization, they are either treated in the correctional facility or transferred to a local hospital for a higher level of care. Some hospitals are equipped with security measures similar to those of a correctional facility, with secure floors or wings dedicated solely to the care of the incarcerated. Secure units are more commonly seen in hospitals associated with prisons rather than local jails. Other hospitals house incarcerated patients in the same rooms as the public population, and thus movement is restricted by other means.3 Most commonly, this is done with a hard metal shackle resembling a handcuff with one end attached to the leg or wrist and the other end attached to the bed. Some agencies require more restraints, often requiring the use of wrist cuffs and leg cuffs concurrently for the entire duration of a patient’s hospitalization.4 In our experience, agencies apply these restraints universally, regardless of age, illness, mobility, or pretrial status.
Restraint practices are rooted in a concern for practitioner and public safety and bear merit. A patient from a correctional facility is usually guarded by just one officer in lieu of the multiple security measures at a jail or prison facility. Nonsecured hospitals have become sites of multiple escapes by incarcerated inpatients, given the lack of secured doors and the multiple movements during the admission and discharge processes.5 Furthermore, violence against hospital staff is now a focus issue in many hospitals and is no longer accepted as just “part of the job.” In several high-profile incidents, incarcerated inpatients have harmed staff, including one at our own institution, when an incarcerated patient held a makeshift weapon to a student’s throat.6
LEGAL CHALLENGES
The use of shackles during hospital visits has been challenged in US courts and routinely upheld. In one case, an incarcerated patient with renal failure received injuries after his leg edema was so severe that “at one point the shackles themselves were barely visible.”7 Though he was injured, the shackles were determined to have served a penological purpose outside of punishment, such as preventing escape, and the injuries were the result of the patient’s guards not following protocol. British courts have taken a different stance, ruling for an incarcerated patient who challenged the use of cuffs during three outpatient appointments and one inpatient admission.8 While the cuffs in the outpatient setting were deemed acceptable (as they were removed during the medical visit itself), they remained during the duration of the inpatient stay. This was deemed in violation of Title I/Article 3 of the Charter of Fundamental Rights of the European Union, Dignity/The right to integrity of the person. One area in US healthcare where shackling has been roundly condemned is the peripartum shackling of pregnant women. Though courts have had a mixed record to challenges, activism and advocacy have led to the banning of the practice in 23 states, though in most states significant exemptions exist.9 Through the First Step Act of 2018, the federal government banned peripartum shackling for all federal prisoners, but as most incarcerations are under state or local control, a considerable number of incarcerated pregnant women can legally be shackled during their deliveries.
RISKS OF SHACKLING
Legal and safety concerns aside, the shackling of incarcerated patients carries enormous risk. The use of medical restraints in hospitals has decreased over the past few decades, given their proven harms in increasing falls, exacerbating delirium, and increasing the risk of in-hospital death.10 There is no reason to believe that trading a soft medical restraint for a metal leg or wrist cuff would not confer the same risk. Additionally, metal law enforcement cuffs are not designed with patient safety in mind and have been known to cause specific nerve injuries, or handcuff neuropathy. This can occur when placement is too tight or when a patient struggles against them, as could happen with an agitated or delirious patient. The bar for removal, even briefly for an exam, is also much higher than that of a medical restraint, leading to a greater likelihood that certain aspects of the physical exam, such as gait or strength assessment, may not be adequately performed. In one small survey, British physicians reported often performing an exam while the patient was cuffed and with a guard in the room, despite country guidelines against both practices.11
Additionally, marginalized communities are disproportionately incarcerated and have a fraught and tenuous relationship with the healthcare system. Black patients routinely report greater mistrust than White patients in the outcomes of care and the motivations of physicians, in large part due to past and current discrimination and the medical community’s history of experimentation.12 A shackled patient may view a treating physician and hospital as complicit with the practice, rather than seeing the practice as something outside of their control. If a patient’s sole interaction with inpatient medicine involves shackling, it risks damaging whatever fragile physician-patient relationship may exist and could delay or limit care even further.
While the universal application of metal handcuffs or leg cuffs ensures low rates of escape or attacks on workers, it does so at the expense of vulnerable individuals. We have cared for an incarcerated elderly woman arrested for multiple traffic violations, a man with severe autism who slipped through the cracks of mental health diversion protocols and ended up in jail, and an arrested delirious man with severe alcohol withdrawal, all shackled with hard shackles on the wrists, legs, or in the final case, both. Safety and the rights of the vulnerable are not mutually exclusive, and we feel the following measures can protect both.
A WAY FORWARD
First, the universal application of shackles in the hospitalized incarcerated patient should end. If no alternative security measures are available for high-risk patients, correctional facilities must document their necessity as physicians and nurses are required to do for medical restraints. Hospitals should have processes in place for providers who feel unsafe with an unshackled patient or think a patient is unnecessarily shackled, and collegial discussions about shackling with law enforcement should be the norm. If safe to do so, shackles should routinely be removed for physical exams without question. Since law enforcement officials, rather than the hospitals, make the rules for shackling, this will take some degree of physician and administrative advocacy at the hospital level and legislative advocacy at the local and state levels.
Second, vulnerable populations, such as the elderly, those experiencing a mental health crisis, or others at risk for in-hospital delirium, should never be restrained with hard law enforcement cuffs. Restraint procedures should follow standard medical restraint procedures, and soft restraints should be used if at all possible. Given the high rates of psychiatric illness amongst the incarcerated and the role jails play in filling gaps in psychiatric care, medical admissions for those with mental illness are not rare occasions.
Finally, hospitals routinely taking care of an incarcerated population should seek to build secure units, a move that would dramatically reduce the need for shackling. In several cities, the primary referral hospitals for some of the largest jails in the country do not have units with the proper security to allow for freedom of movement, and thus, shackling persists. Creating secure units will take significant investment on the part of hospital and local authorities, but there is potential for decreasing costs due to consolidating supervision, which would lead to better patient outcomes given the above risks.
Advocating for the health of the incarcerated, even those who have not yet been convicted, is typically not a high priority for the general public. As inpatient physicians, we see the impact universal shackling has on some of our most vulnerable patients and should be their voice where they have none. Advocating for and implementing the above procedures will be a step toward improving patient care while maintaining safety.
1. Proctor C. Jacob Blake handcuffed to hospital bed, father says. Chicago Sun-Times. Updated August 27, 2020. Accessed December 29, 2020. chicago.suntimes.com/2020/8/27/21404463/jacob-blake-father-kenosha-police-shooting-hospital-bed-handcuffs
2. Maruschak LM, Minton TD. Correctional populations in the United States, 2017-2018. Bureau of Justice Statistics. August 2020. Accessed September 30, 2020. https://www.bjs.gov/content/pub/pdf/cpus1718.pdf
3. Huh K, Boucher A, Fehr S, McGaffey F, McKillop M, Schiff M. State prisons and the delivery of hospital care: how states set up and finance off-site care for incarcerated individuals. The Pew Charitable Trusts. July 2018. Accessed September 30, 2020. https://www.pewtrusts.org/-/media/assets/2018/07/prisons-and-hospital-care_report.pdf
4. Haber LA, Erickson HP, Ranji SR, Ortiz GM, Pratt LA. Acute care for patients who are incarcerated: a review. JAMA Intern Med. 2019;179(11):1561-1567. https://doi.org/10.1001/jamainternmed.2019.3881
5. Mikow-Porto VA, Smith TA. The IHSSF 2011 Prisoner Escape Study. J Healthc Prot Manage. 2011;27(2):38-58.
6. Lezon D, Blakinger K. Inmate shot by deputy after holding medical student at Ben Taub. Houston Chronicle. October 6, 2016. Accessed December 29, 2020. https://www.chron.com/news/houston-texas/article/Deputy-shoots-suspect-at-Ben-Taub-hopsital-9873972.php
7. Yearwood LT. Pregnant and shackled: why inmates are still giving birth cuffed and bound. The Guardian. January 24, 2020. Accessed December 29, 2020. theguardian.com/us-news/2020/jan/24/shackled-pregnant-women-prisoners-birth
8. Haslar v Megerman, 104 F.3d 178 (8th Cir. 1997).
9. FGP v Serco Plc and SSHD, EWHC 1804 (Admin) (2012).
10. Cleary K, Prescott K. The use of physical restraints in acute and long-term care: an updated review of the evidence, regulations, ethics, and legality. J Acute Care Phys Ther. 2015;6(1):8-15. https://doi.org/10.1097/JAT.0000000000000005
11. Tuite H, Browne K, O’Neill D. Prisoners in general hospitals: doctors’ attitudes and practice. BMJ. 2006;332(7540):548-549. https://doi.org/10.1136/bmj.332.7540.548-b
12. LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57(Suppl 1):146-161. https://doi.org/10.1177/1077558700057001S07
The police shooting of Jacob Blake, an unarmed Wisconsin man, during an arrest in August 2020, led to more protests in a summer filled with calls against the unequal application of police force. Outrage grew as it was revealed that Blake, paralyzed from his waist down and not yet convicted of a crime, was still handcuffed to his hospital bed while receiving treatment.1 To many this seemed unusually cruel, but to those tasked with caring for incarcerated patients, it is all too familiar. Given the high rates of incarceration in the United States and the increased medical needs of this population, caring for those in custody is unavoidable for many physicians and hospitals. Though safety should be paramount, the universal application of metal handcuffs or leg cuffs by law enforcement officials, a process known as shackling, can lead to a variety of harms and should be abandoned.
BACKGROUND
The United States incarcerates more individuals both in total numbers and per capita than any other country in the world. This is currently believed to be more than two million people on any given day or more than 650 persons per 100,000 population.2 Incarceration occurs in jails, which are locally run facilities holding individuals on short sentences or those not yet convicted who are unable to afford bail before their trials (pretrial), or prisons, which are state and federally run facilities that house those with long sentences. When an incarcerated person experiences a medical emergency requiring hospitalization, they are either treated in the correctional facility or transferred to a local hospital for a higher level of care. Some hospitals are equipped with security measures similar to those of a correctional facility, with secure floors or wings dedicated solely to the care of the incarcerated. Secure units are more commonly seen in hospitals associated with prisons rather than local jails. Other hospitals house incarcerated patients in the same rooms as the public population, and thus movement is restricted by other means.3 Most commonly, this is done with a hard metal shackle resembling a handcuff with one end attached to the leg or wrist and the other end attached to the bed. Some agencies require more restraints, often requiring the use of wrist cuffs and leg cuffs concurrently for the entire duration of a patient’s hospitalization.4 In our experience, agencies apply these restraints universally, regardless of age, illness, mobility, or pretrial status.
Restraint practices are rooted in a concern for practitioner and public safety and bear merit. A patient from a correctional facility is usually guarded by just one officer in lieu of the multiple security measures at a jail or prison facility. Nonsecured hospitals have become sites of multiple escapes by incarcerated inpatients, given the lack of secured doors and the multiple movements during the admission and discharge processes.5 Furthermore, violence against hospital staff is now a focus issue in many hospitals and is no longer accepted as just “part of the job.” In several high-profile incidents, incarcerated inpatients have harmed staff, including one at our own institution, when an incarcerated patient held a makeshift weapon to a student’s throat.6
LEGAL CHALLENGES
The use of shackles during hospital visits has been challenged in US courts and routinely upheld. In one case, an incarcerated patient with renal failure received injuries after his leg edema was so severe that “at one point the shackles themselves were barely visible.”7 Though he was injured, the shackles were determined to have served a penological purpose outside of punishment, such as preventing escape, and the injuries were the result of the patient’s guards not following protocol. British courts have taken a different stance, ruling for an incarcerated patient who challenged the use of cuffs during three outpatient appointments and one inpatient admission.8 While the cuffs in the outpatient setting were deemed acceptable (as they were removed during the medical visit itself), they remained during the duration of the inpatient stay. This was deemed in violation of Title I/Article 3 of the Charter of Fundamental Rights of the European Union, Dignity/The right to integrity of the person. One area in US healthcare where shackling has been roundly condemned is the peripartum shackling of pregnant women. Though courts have had a mixed record to challenges, activism and advocacy have led to the banning of the practice in 23 states, though in most states significant exemptions exist.9 Through the First Step Act of 2018, the federal government banned peripartum shackling for all federal prisoners, but as most incarcerations are under state or local control, a considerable number of incarcerated pregnant women can legally be shackled during their deliveries.
RISKS OF SHACKLING
Legal and safety concerns aside, the shackling of incarcerated patients carries enormous risk. The use of medical restraints in hospitals has decreased over the past few decades, given their proven harms in increasing falls, exacerbating delirium, and increasing the risk of in-hospital death.10 There is no reason to believe that trading a soft medical restraint for a metal leg or wrist cuff would not confer the same risk. Additionally, metal law enforcement cuffs are not designed with patient safety in mind and have been known to cause specific nerve injuries, or handcuff neuropathy. This can occur when placement is too tight or when a patient struggles against them, as could happen with an agitated or delirious patient. The bar for removal, even briefly for an exam, is also much higher than that of a medical restraint, leading to a greater likelihood that certain aspects of the physical exam, such as gait or strength assessment, may not be adequately performed. In one small survey, British physicians reported often performing an exam while the patient was cuffed and with a guard in the room, despite country guidelines against both practices.11
Additionally, marginalized communities are disproportionately incarcerated and have a fraught and tenuous relationship with the healthcare system. Black patients routinely report greater mistrust than White patients in the outcomes of care and the motivations of physicians, in large part due to past and current discrimination and the medical community’s history of experimentation.12 A shackled patient may view a treating physician and hospital as complicit with the practice, rather than seeing the practice as something outside of their control. If a patient’s sole interaction with inpatient medicine involves shackling, it risks damaging whatever fragile physician-patient relationship may exist and could delay or limit care even further.
While the universal application of metal handcuffs or leg cuffs ensures low rates of escape or attacks on workers, it does so at the expense of vulnerable individuals. We have cared for an incarcerated elderly woman arrested for multiple traffic violations, a man with severe autism who slipped through the cracks of mental health diversion protocols and ended up in jail, and an arrested delirious man with severe alcohol withdrawal, all shackled with hard shackles on the wrists, legs, or in the final case, both. Safety and the rights of the vulnerable are not mutually exclusive, and we feel the following measures can protect both.
A WAY FORWARD
First, the universal application of shackles in the hospitalized incarcerated patient should end. If no alternative security measures are available for high-risk patients, correctional facilities must document their necessity as physicians and nurses are required to do for medical restraints. Hospitals should have processes in place for providers who feel unsafe with an unshackled patient or think a patient is unnecessarily shackled, and collegial discussions about shackling with law enforcement should be the norm. If safe to do so, shackles should routinely be removed for physical exams without question. Since law enforcement officials, rather than the hospitals, make the rules for shackling, this will take some degree of physician and administrative advocacy at the hospital level and legislative advocacy at the local and state levels.
Second, vulnerable populations, such as the elderly, those experiencing a mental health crisis, or others at risk for in-hospital delirium, should never be restrained with hard law enforcement cuffs. Restraint procedures should follow standard medical restraint procedures, and soft restraints should be used if at all possible. Given the high rates of psychiatric illness amongst the incarcerated and the role jails play in filling gaps in psychiatric care, medical admissions for those with mental illness are not rare occasions.
Finally, hospitals routinely taking care of an incarcerated population should seek to build secure units, a move that would dramatically reduce the need for shackling. In several cities, the primary referral hospitals for some of the largest jails in the country do not have units with the proper security to allow for freedom of movement, and thus, shackling persists. Creating secure units will take significant investment on the part of hospital and local authorities, but there is potential for decreasing costs due to consolidating supervision, which would lead to better patient outcomes given the above risks.
Advocating for the health of the incarcerated, even those who have not yet been convicted, is typically not a high priority for the general public. As inpatient physicians, we see the impact universal shackling has on some of our most vulnerable patients and should be their voice where they have none. Advocating for and implementing the above procedures will be a step toward improving patient care while maintaining safety.
The police shooting of Jacob Blake, an unarmed Wisconsin man, during an arrest in August 2020, led to more protests in a summer filled with calls against the unequal application of police force. Outrage grew as it was revealed that Blake, paralyzed from his waist down and not yet convicted of a crime, was still handcuffed to his hospital bed while receiving treatment.1 To many this seemed unusually cruel, but to those tasked with caring for incarcerated patients, it is all too familiar. Given the high rates of incarceration in the United States and the increased medical needs of this population, caring for those in custody is unavoidable for many physicians and hospitals. Though safety should be paramount, the universal application of metal handcuffs or leg cuffs by law enforcement officials, a process known as shackling, can lead to a variety of harms and should be abandoned.
BACKGROUND
The United States incarcerates more individuals both in total numbers and per capita than any other country in the world. This is currently believed to be more than two million people on any given day or more than 650 persons per 100,000 population.2 Incarceration occurs in jails, which are locally run facilities holding individuals on short sentences or those not yet convicted who are unable to afford bail before their trials (pretrial), or prisons, which are state and federally run facilities that house those with long sentences. When an incarcerated person experiences a medical emergency requiring hospitalization, they are either treated in the correctional facility or transferred to a local hospital for a higher level of care. Some hospitals are equipped with security measures similar to those of a correctional facility, with secure floors or wings dedicated solely to the care of the incarcerated. Secure units are more commonly seen in hospitals associated with prisons rather than local jails. Other hospitals house incarcerated patients in the same rooms as the public population, and thus movement is restricted by other means.3 Most commonly, this is done with a hard metal shackle resembling a handcuff with one end attached to the leg or wrist and the other end attached to the bed. Some agencies require more restraints, often requiring the use of wrist cuffs and leg cuffs concurrently for the entire duration of a patient’s hospitalization.4 In our experience, agencies apply these restraints universally, regardless of age, illness, mobility, or pretrial status.
Restraint practices are rooted in a concern for practitioner and public safety and bear merit. A patient from a correctional facility is usually guarded by just one officer in lieu of the multiple security measures at a jail or prison facility. Nonsecured hospitals have become sites of multiple escapes by incarcerated inpatients, given the lack of secured doors and the multiple movements during the admission and discharge processes.5 Furthermore, violence against hospital staff is now a focus issue in many hospitals and is no longer accepted as just “part of the job.” In several high-profile incidents, incarcerated inpatients have harmed staff, including one at our own institution, when an incarcerated patient held a makeshift weapon to a student’s throat.6
LEGAL CHALLENGES
The use of shackles during hospital visits has been challenged in US courts and routinely upheld. In one case, an incarcerated patient with renal failure received injuries after his leg edema was so severe that “at one point the shackles themselves were barely visible.”7 Though he was injured, the shackles were determined to have served a penological purpose outside of punishment, such as preventing escape, and the injuries were the result of the patient’s guards not following protocol. British courts have taken a different stance, ruling for an incarcerated patient who challenged the use of cuffs during three outpatient appointments and one inpatient admission.8 While the cuffs in the outpatient setting were deemed acceptable (as they were removed during the medical visit itself), they remained during the duration of the inpatient stay. This was deemed in violation of Title I/Article 3 of the Charter of Fundamental Rights of the European Union, Dignity/The right to integrity of the person. One area in US healthcare where shackling has been roundly condemned is the peripartum shackling of pregnant women. Though courts have had a mixed record to challenges, activism and advocacy have led to the banning of the practice in 23 states, though in most states significant exemptions exist.9 Through the First Step Act of 2018, the federal government banned peripartum shackling for all federal prisoners, but as most incarcerations are under state or local control, a considerable number of incarcerated pregnant women can legally be shackled during their deliveries.
RISKS OF SHACKLING
Legal and safety concerns aside, the shackling of incarcerated patients carries enormous risk. The use of medical restraints in hospitals has decreased over the past few decades, given their proven harms in increasing falls, exacerbating delirium, and increasing the risk of in-hospital death.10 There is no reason to believe that trading a soft medical restraint for a metal leg or wrist cuff would not confer the same risk. Additionally, metal law enforcement cuffs are not designed with patient safety in mind and have been known to cause specific nerve injuries, or handcuff neuropathy. This can occur when placement is too tight or when a patient struggles against them, as could happen with an agitated or delirious patient. The bar for removal, even briefly for an exam, is also much higher than that of a medical restraint, leading to a greater likelihood that certain aspects of the physical exam, such as gait or strength assessment, may not be adequately performed. In one small survey, British physicians reported often performing an exam while the patient was cuffed and with a guard in the room, despite country guidelines against both practices.11
Additionally, marginalized communities are disproportionately incarcerated and have a fraught and tenuous relationship with the healthcare system. Black patients routinely report greater mistrust than White patients in the outcomes of care and the motivations of physicians, in large part due to past and current discrimination and the medical community’s history of experimentation.12 A shackled patient may view a treating physician and hospital as complicit with the practice, rather than seeing the practice as something outside of their control. If a patient’s sole interaction with inpatient medicine involves shackling, it risks damaging whatever fragile physician-patient relationship may exist and could delay or limit care even further.
While the universal application of metal handcuffs or leg cuffs ensures low rates of escape or attacks on workers, it does so at the expense of vulnerable individuals. We have cared for an incarcerated elderly woman arrested for multiple traffic violations, a man with severe autism who slipped through the cracks of mental health diversion protocols and ended up in jail, and an arrested delirious man with severe alcohol withdrawal, all shackled with hard shackles on the wrists, legs, or in the final case, both. Safety and the rights of the vulnerable are not mutually exclusive, and we feel the following measures can protect both.
A WAY FORWARD
First, the universal application of shackles in the hospitalized incarcerated patient should end. If no alternative security measures are available for high-risk patients, correctional facilities must document their necessity as physicians and nurses are required to do for medical restraints. Hospitals should have processes in place for providers who feel unsafe with an unshackled patient or think a patient is unnecessarily shackled, and collegial discussions about shackling with law enforcement should be the norm. If safe to do so, shackles should routinely be removed for physical exams without question. Since law enforcement officials, rather than the hospitals, make the rules for shackling, this will take some degree of physician and administrative advocacy at the hospital level and legislative advocacy at the local and state levels.
Second, vulnerable populations, such as the elderly, those experiencing a mental health crisis, or others at risk for in-hospital delirium, should never be restrained with hard law enforcement cuffs. Restraint procedures should follow standard medical restraint procedures, and soft restraints should be used if at all possible. Given the high rates of psychiatric illness amongst the incarcerated and the role jails play in filling gaps in psychiatric care, medical admissions for those with mental illness are not rare occasions.
Finally, hospitals routinely taking care of an incarcerated population should seek to build secure units, a move that would dramatically reduce the need for shackling. In several cities, the primary referral hospitals for some of the largest jails in the country do not have units with the proper security to allow for freedom of movement, and thus, shackling persists. Creating secure units will take significant investment on the part of hospital and local authorities, but there is potential for decreasing costs due to consolidating supervision, which would lead to better patient outcomes given the above risks.
Advocating for the health of the incarcerated, even those who have not yet been convicted, is typically not a high priority for the general public. As inpatient physicians, we see the impact universal shackling has on some of our most vulnerable patients and should be their voice where they have none. Advocating for and implementing the above procedures will be a step toward improving patient care while maintaining safety.
1. Proctor C. Jacob Blake handcuffed to hospital bed, father says. Chicago Sun-Times. Updated August 27, 2020. Accessed December 29, 2020. chicago.suntimes.com/2020/8/27/21404463/jacob-blake-father-kenosha-police-shooting-hospital-bed-handcuffs
2. Maruschak LM, Minton TD. Correctional populations in the United States, 2017-2018. Bureau of Justice Statistics. August 2020. Accessed September 30, 2020. https://www.bjs.gov/content/pub/pdf/cpus1718.pdf
3. Huh K, Boucher A, Fehr S, McGaffey F, McKillop M, Schiff M. State prisons and the delivery of hospital care: how states set up and finance off-site care for incarcerated individuals. The Pew Charitable Trusts. July 2018. Accessed September 30, 2020. https://www.pewtrusts.org/-/media/assets/2018/07/prisons-and-hospital-care_report.pdf
4. Haber LA, Erickson HP, Ranji SR, Ortiz GM, Pratt LA. Acute care for patients who are incarcerated: a review. JAMA Intern Med. 2019;179(11):1561-1567. https://doi.org/10.1001/jamainternmed.2019.3881
5. Mikow-Porto VA, Smith TA. The IHSSF 2011 Prisoner Escape Study. J Healthc Prot Manage. 2011;27(2):38-58.
6. Lezon D, Blakinger K. Inmate shot by deputy after holding medical student at Ben Taub. Houston Chronicle. October 6, 2016. Accessed December 29, 2020. https://www.chron.com/news/houston-texas/article/Deputy-shoots-suspect-at-Ben-Taub-hopsital-9873972.php
7. Yearwood LT. Pregnant and shackled: why inmates are still giving birth cuffed and bound. The Guardian. January 24, 2020. Accessed December 29, 2020. theguardian.com/us-news/2020/jan/24/shackled-pregnant-women-prisoners-birth
8. Haslar v Megerman, 104 F.3d 178 (8th Cir. 1997).
9. FGP v Serco Plc and SSHD, EWHC 1804 (Admin) (2012).
10. Cleary K, Prescott K. The use of physical restraints in acute and long-term care: an updated review of the evidence, regulations, ethics, and legality. J Acute Care Phys Ther. 2015;6(1):8-15. https://doi.org/10.1097/JAT.0000000000000005
11. Tuite H, Browne K, O’Neill D. Prisoners in general hospitals: doctors’ attitudes and practice. BMJ. 2006;332(7540):548-549. https://doi.org/10.1136/bmj.332.7540.548-b
12. LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57(Suppl 1):146-161. https://doi.org/10.1177/1077558700057001S07
1. Proctor C. Jacob Blake handcuffed to hospital bed, father says. Chicago Sun-Times. Updated August 27, 2020. Accessed December 29, 2020. chicago.suntimes.com/2020/8/27/21404463/jacob-blake-father-kenosha-police-shooting-hospital-bed-handcuffs
2. Maruschak LM, Minton TD. Correctional populations in the United States, 2017-2018. Bureau of Justice Statistics. August 2020. Accessed September 30, 2020. https://www.bjs.gov/content/pub/pdf/cpus1718.pdf
3. Huh K, Boucher A, Fehr S, McGaffey F, McKillop M, Schiff M. State prisons and the delivery of hospital care: how states set up and finance off-site care for incarcerated individuals. The Pew Charitable Trusts. July 2018. Accessed September 30, 2020. https://www.pewtrusts.org/-/media/assets/2018/07/prisons-and-hospital-care_report.pdf
4. Haber LA, Erickson HP, Ranji SR, Ortiz GM, Pratt LA. Acute care for patients who are incarcerated: a review. JAMA Intern Med. 2019;179(11):1561-1567. https://doi.org/10.1001/jamainternmed.2019.3881
5. Mikow-Porto VA, Smith TA. The IHSSF 2011 Prisoner Escape Study. J Healthc Prot Manage. 2011;27(2):38-58.
6. Lezon D, Blakinger K. Inmate shot by deputy after holding medical student at Ben Taub. Houston Chronicle. October 6, 2016. Accessed December 29, 2020. https://www.chron.com/news/houston-texas/article/Deputy-shoots-suspect-at-Ben-Taub-hopsital-9873972.php
7. Yearwood LT. Pregnant and shackled: why inmates are still giving birth cuffed and bound. The Guardian. January 24, 2020. Accessed December 29, 2020. theguardian.com/us-news/2020/jan/24/shackled-pregnant-women-prisoners-birth
8. Haslar v Megerman, 104 F.3d 178 (8th Cir. 1997).
9. FGP v Serco Plc and SSHD, EWHC 1804 (Admin) (2012).
10. Cleary K, Prescott K. The use of physical restraints in acute and long-term care: an updated review of the evidence, regulations, ethics, and legality. J Acute Care Phys Ther. 2015;6(1):8-15. https://doi.org/10.1097/JAT.0000000000000005
11. Tuite H, Browne K, O’Neill D. Prisoners in general hospitals: doctors’ attitudes and practice. BMJ. 2006;332(7540):548-549. https://doi.org/10.1136/bmj.332.7540.548-b
12. LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57(Suppl 1):146-161. https://doi.org/10.1177/1077558700057001S07
© 2021 Society of Hospital Medicine