User login
Le Petit Prince: Lessons From a Beloved Fable for Our Current Time
”Good evening,“ said the little prince politely.
”Good evening,“ said the snake.
”What planet have I fallen on?“ asked the little prince.
”On the planet Earth, in Africa,“ replied the snake.
”Oh… Then there are no people on Earth?”
”This is the desert. There are no people in the desert. The Earth is big,“ said the snake.
The little prince sat down on a stone and looked up at the sky.
”I wonder,“ he said, “if the stars are lit up so that each of us can find his own star again. Look at my planet. It is right above us… But how far away is it?” 1
Le Petit Prince is one of the twentieth century’s most widely read fables.1 Written in 1943 by the French aviator and novelist Antoine de Saint-Exupéry, it tells the story of a young prince who inhabits a small planet in outer space with his muse, a fragile and dainty rose. The prince loves his rose and goes to great lengths to protect her, but her constant needs prove too much for him to bear. One day he decides to leave her and sets out on a journey across the universe. Along the way he stops at several different planets and interacts with their sole inhabitants, each of whom performs a bizarre and arguably pointless activity. The prince leaves each planet confused and despondent—for no place or person has proven more inspiring than his own planet or rose—until he arrives on Earth, where he meets a snake, a fox, and the novel’s unnamed narrator. Their company is a welcome relief for the travel-weary prince, who learns important lessons about love, friendship, and “matters of consequence.” Toward the novel’s end, the snake promises to deliver the little prince home if he allows himself to be bitten. The prince obliges in order to be with his rose, and he soon disappears. The story concludes with the narrator looking up at the stars, wondering if the prince is somewhere among them.
One interpretation of Le Petit Prince is that life is more beautiful when the things that give it meaning are recognized and cherished, but there is a heavy irony behind this theme. The story was published during one of the lowest points in the Second World War, when France was still in the grips of its German oppressors. Saint-Exupéry himself had fled to the United States years earlier and composed Le Petit Prince during a time of personal upheaval. In short, nothing about the context of the book’s birth seemed to inspire its rosy message.
Now, almost 80 years after the first publication of Le Petit Prince, we find ourselves in a similarly jarring and unpredictable time. As calamitous global events unfold around us, it is difficult not to feel overwhelmed. For healthcare workers, the crush of patient care has made us feel vulnerable—first to a virus that might infect us and our loved ones, and second, to the overwhelming sense of despair when caring for patients who ultimately die despite our best efforts. Pandemics are a time of physical and social disruption, and while it has been 100 years since we experienced one like this, they are a repeated part of the history of life on our planet. What would the little prince see if he landed in our clinics, hospitals, nursing homes, testing centers, or vaccination facilities today? Would he observe patients saying good-bye to family members on tablets and cell phones because their loved ones are not allowed to visit in person? Would he see healthcare workers struggling to resuscitate dying patients in a crowded emergency department or intensive care unit? Would he see long lines of cars filled with people waiting for tests or vaccines? Would he see government officials and public health workers agonizing over decisions about steps that could reduce spread but impose economic hardship on many?
There has been much debate about whether Le Petit Prince is a children’s story or a message for adults disguised as a children’s fable. Perhaps the answer is that it is both, for many children’s stories were actually written for adults. Despite the fragility and delicacy of the book, there is clearly a haunting and deep irony inherent in what it is, in effect, a most savage critique of the world at war.
Two themes that emerge in the novel resonate widely now: isolation and death. Each character the little prince meets is alone, mirroring the long periods of social distancing we have experienced over the past year. And while death is never explicitly mentioned in the book, it seems to be lurking throughout, especially when the prince disappears from Earth after being bitten by the snake. Currently, we have almost become numb to the reported daily death counts—each one alone would have evoked outrage in more usual times. One might imagine that Saint-Exupéry wrote this fable in part to help people cope with the deaths of their loved ones.
And when you are comforted (time soothes all sorrows) you will be happy to have known me. You will always be my friend. You will want to laugh with me. And from time to time you will open your window, so, just for the pleasure of it ... And your friends will be astonished to see you laughing whilst gazing at the sky! And so you will say to them, “Yes, stars always make me laugh!”
Over the past year, both authors of this essay have seen people turn to Le Petit Prince to cope with death. One of us observed a daughter reading the book to her mother at her intensive care bedside on the day she died. The other received a copy as thanks from the wife of a young man who died after 18 months of punishing chemotherapy for sarcoma. Inside the cover was a picture of her husband and the inscription, “Please share this book with someone you love—it’s meant to be read out loud—and remember James.” And so I did, with my grandson Sebastian, who listened to the story with the imagination, wonder, and curiosity of a 6-year-old—he had many questions.
Perhaps the fable that has comforted our patients and their families during their time of despair can do the same for us. Like the prince, who returns to his rose after a difficult journey, we might find solace in the people and things that give our lives their deepest meaning. Thereafter, we might return, rejuvenated, to the clinics, emergency departments, and inpatient wards where our daily work must continue. While the scale of the problems around us makes it feel like any step we take towards preserving our hope will be moot, Le Petit Prince teaches us there is value in making the effort. And there is even a chance that we will find, to our surprise, and against our more cynical judgment, a small rose pushing itself up towards the light.
Acknowledgments
The authors thank Rita Charon (Columbia University), Pam Hartzband (Harvard University), Raphael Rush (University of Toronto), and Emily Silverman (University of California San Francisco) for their comments on earlier versions of this essay. None were compensated. We thank Sebastian, James’ wife, and our other patient’s daughter for giving permission to include them in the story.
1. de Saint-Exupéry A. The Little Prince. Harcourt Brace; 1961.
”Good evening,“ said the little prince politely.
”Good evening,“ said the snake.
”What planet have I fallen on?“ asked the little prince.
”On the planet Earth, in Africa,“ replied the snake.
”Oh… Then there are no people on Earth?”
”This is the desert. There are no people in the desert. The Earth is big,“ said the snake.
The little prince sat down on a stone and looked up at the sky.
”I wonder,“ he said, “if the stars are lit up so that each of us can find his own star again. Look at my planet. It is right above us… But how far away is it?” 1
Le Petit Prince is one of the twentieth century’s most widely read fables.1 Written in 1943 by the French aviator and novelist Antoine de Saint-Exupéry, it tells the story of a young prince who inhabits a small planet in outer space with his muse, a fragile and dainty rose. The prince loves his rose and goes to great lengths to protect her, but her constant needs prove too much for him to bear. One day he decides to leave her and sets out on a journey across the universe. Along the way he stops at several different planets and interacts with their sole inhabitants, each of whom performs a bizarre and arguably pointless activity. The prince leaves each planet confused and despondent—for no place or person has proven more inspiring than his own planet or rose—until he arrives on Earth, where he meets a snake, a fox, and the novel’s unnamed narrator. Their company is a welcome relief for the travel-weary prince, who learns important lessons about love, friendship, and “matters of consequence.” Toward the novel’s end, the snake promises to deliver the little prince home if he allows himself to be bitten. The prince obliges in order to be with his rose, and he soon disappears. The story concludes with the narrator looking up at the stars, wondering if the prince is somewhere among them.
One interpretation of Le Petit Prince is that life is more beautiful when the things that give it meaning are recognized and cherished, but there is a heavy irony behind this theme. The story was published during one of the lowest points in the Second World War, when France was still in the grips of its German oppressors. Saint-Exupéry himself had fled to the United States years earlier and composed Le Petit Prince during a time of personal upheaval. In short, nothing about the context of the book’s birth seemed to inspire its rosy message.
Now, almost 80 years after the first publication of Le Petit Prince, we find ourselves in a similarly jarring and unpredictable time. As calamitous global events unfold around us, it is difficult not to feel overwhelmed. For healthcare workers, the crush of patient care has made us feel vulnerable—first to a virus that might infect us and our loved ones, and second, to the overwhelming sense of despair when caring for patients who ultimately die despite our best efforts. Pandemics are a time of physical and social disruption, and while it has been 100 years since we experienced one like this, they are a repeated part of the history of life on our planet. What would the little prince see if he landed in our clinics, hospitals, nursing homes, testing centers, or vaccination facilities today? Would he observe patients saying good-bye to family members on tablets and cell phones because their loved ones are not allowed to visit in person? Would he see healthcare workers struggling to resuscitate dying patients in a crowded emergency department or intensive care unit? Would he see long lines of cars filled with people waiting for tests or vaccines? Would he see government officials and public health workers agonizing over decisions about steps that could reduce spread but impose economic hardship on many?
There has been much debate about whether Le Petit Prince is a children’s story or a message for adults disguised as a children’s fable. Perhaps the answer is that it is both, for many children’s stories were actually written for adults. Despite the fragility and delicacy of the book, there is clearly a haunting and deep irony inherent in what it is, in effect, a most savage critique of the world at war.
Two themes that emerge in the novel resonate widely now: isolation and death. Each character the little prince meets is alone, mirroring the long periods of social distancing we have experienced over the past year. And while death is never explicitly mentioned in the book, it seems to be lurking throughout, especially when the prince disappears from Earth after being bitten by the snake. Currently, we have almost become numb to the reported daily death counts—each one alone would have evoked outrage in more usual times. One might imagine that Saint-Exupéry wrote this fable in part to help people cope with the deaths of their loved ones.
And when you are comforted (time soothes all sorrows) you will be happy to have known me. You will always be my friend. You will want to laugh with me. And from time to time you will open your window, so, just for the pleasure of it ... And your friends will be astonished to see you laughing whilst gazing at the sky! And so you will say to them, “Yes, stars always make me laugh!”
Over the past year, both authors of this essay have seen people turn to Le Petit Prince to cope with death. One of us observed a daughter reading the book to her mother at her intensive care bedside on the day she died. The other received a copy as thanks from the wife of a young man who died after 18 months of punishing chemotherapy for sarcoma. Inside the cover was a picture of her husband and the inscription, “Please share this book with someone you love—it’s meant to be read out loud—and remember James.” And so I did, with my grandson Sebastian, who listened to the story with the imagination, wonder, and curiosity of a 6-year-old—he had many questions.
Perhaps the fable that has comforted our patients and their families during their time of despair can do the same for us. Like the prince, who returns to his rose after a difficult journey, we might find solace in the people and things that give our lives their deepest meaning. Thereafter, we might return, rejuvenated, to the clinics, emergency departments, and inpatient wards where our daily work must continue. While the scale of the problems around us makes it feel like any step we take towards preserving our hope will be moot, Le Petit Prince teaches us there is value in making the effort. And there is even a chance that we will find, to our surprise, and against our more cynical judgment, a small rose pushing itself up towards the light.
Acknowledgments
The authors thank Rita Charon (Columbia University), Pam Hartzband (Harvard University), Raphael Rush (University of Toronto), and Emily Silverman (University of California San Francisco) for their comments on earlier versions of this essay. None were compensated. We thank Sebastian, James’ wife, and our other patient’s daughter for giving permission to include them in the story.
”Good evening,“ said the little prince politely.
”Good evening,“ said the snake.
”What planet have I fallen on?“ asked the little prince.
”On the planet Earth, in Africa,“ replied the snake.
”Oh… Then there are no people on Earth?”
”This is the desert. There are no people in the desert. The Earth is big,“ said the snake.
The little prince sat down on a stone and looked up at the sky.
”I wonder,“ he said, “if the stars are lit up so that each of us can find his own star again. Look at my planet. It is right above us… But how far away is it?” 1
Le Petit Prince is one of the twentieth century’s most widely read fables.1 Written in 1943 by the French aviator and novelist Antoine de Saint-Exupéry, it tells the story of a young prince who inhabits a small planet in outer space with his muse, a fragile and dainty rose. The prince loves his rose and goes to great lengths to protect her, but her constant needs prove too much for him to bear. One day he decides to leave her and sets out on a journey across the universe. Along the way he stops at several different planets and interacts with their sole inhabitants, each of whom performs a bizarre and arguably pointless activity. The prince leaves each planet confused and despondent—for no place or person has proven more inspiring than his own planet or rose—until he arrives on Earth, where he meets a snake, a fox, and the novel’s unnamed narrator. Their company is a welcome relief for the travel-weary prince, who learns important lessons about love, friendship, and “matters of consequence.” Toward the novel’s end, the snake promises to deliver the little prince home if he allows himself to be bitten. The prince obliges in order to be with his rose, and he soon disappears. The story concludes with the narrator looking up at the stars, wondering if the prince is somewhere among them.
One interpretation of Le Petit Prince is that life is more beautiful when the things that give it meaning are recognized and cherished, but there is a heavy irony behind this theme. The story was published during one of the lowest points in the Second World War, when France was still in the grips of its German oppressors. Saint-Exupéry himself had fled to the United States years earlier and composed Le Petit Prince during a time of personal upheaval. In short, nothing about the context of the book’s birth seemed to inspire its rosy message.
Now, almost 80 years after the first publication of Le Petit Prince, we find ourselves in a similarly jarring and unpredictable time. As calamitous global events unfold around us, it is difficult not to feel overwhelmed. For healthcare workers, the crush of patient care has made us feel vulnerable—first to a virus that might infect us and our loved ones, and second, to the overwhelming sense of despair when caring for patients who ultimately die despite our best efforts. Pandemics are a time of physical and social disruption, and while it has been 100 years since we experienced one like this, they are a repeated part of the history of life on our planet. What would the little prince see if he landed in our clinics, hospitals, nursing homes, testing centers, or vaccination facilities today? Would he observe patients saying good-bye to family members on tablets and cell phones because their loved ones are not allowed to visit in person? Would he see healthcare workers struggling to resuscitate dying patients in a crowded emergency department or intensive care unit? Would he see long lines of cars filled with people waiting for tests or vaccines? Would he see government officials and public health workers agonizing over decisions about steps that could reduce spread but impose economic hardship on many?
There has been much debate about whether Le Petit Prince is a children’s story or a message for adults disguised as a children’s fable. Perhaps the answer is that it is both, for many children’s stories were actually written for adults. Despite the fragility and delicacy of the book, there is clearly a haunting and deep irony inherent in what it is, in effect, a most savage critique of the world at war.
Two themes that emerge in the novel resonate widely now: isolation and death. Each character the little prince meets is alone, mirroring the long periods of social distancing we have experienced over the past year. And while death is never explicitly mentioned in the book, it seems to be lurking throughout, especially when the prince disappears from Earth after being bitten by the snake. Currently, we have almost become numb to the reported daily death counts—each one alone would have evoked outrage in more usual times. One might imagine that Saint-Exupéry wrote this fable in part to help people cope with the deaths of their loved ones.
And when you are comforted (time soothes all sorrows) you will be happy to have known me. You will always be my friend. You will want to laugh with me. And from time to time you will open your window, so, just for the pleasure of it ... And your friends will be astonished to see you laughing whilst gazing at the sky! And so you will say to them, “Yes, stars always make me laugh!”
Over the past year, both authors of this essay have seen people turn to Le Petit Prince to cope with death. One of us observed a daughter reading the book to her mother at her intensive care bedside on the day she died. The other received a copy as thanks from the wife of a young man who died after 18 months of punishing chemotherapy for sarcoma. Inside the cover was a picture of her husband and the inscription, “Please share this book with someone you love—it’s meant to be read out loud—and remember James.” And so I did, with my grandson Sebastian, who listened to the story with the imagination, wonder, and curiosity of a 6-year-old—he had many questions.
Perhaps the fable that has comforted our patients and their families during their time of despair can do the same for us. Like the prince, who returns to his rose after a difficult journey, we might find solace in the people and things that give our lives their deepest meaning. Thereafter, we might return, rejuvenated, to the clinics, emergency departments, and inpatient wards where our daily work must continue. While the scale of the problems around us makes it feel like any step we take towards preserving our hope will be moot, Le Petit Prince teaches us there is value in making the effort. And there is even a chance that we will find, to our surprise, and against our more cynical judgment, a small rose pushing itself up towards the light.
Acknowledgments
The authors thank Rita Charon (Columbia University), Pam Hartzband (Harvard University), Raphael Rush (University of Toronto), and Emily Silverman (University of California San Francisco) for their comments on earlier versions of this essay. None were compensated. We thank Sebastian, James’ wife, and our other patient’s daughter for giving permission to include them in the story.
1. de Saint-Exupéry A. The Little Prince. Harcourt Brace; 1961.
1. de Saint-Exupéry A. The Little Prince. Harcourt Brace; 1961.
© 2021 Society of Hospital Medicine
Respiratory Illness Presenteeism in Academic Medicine: A Conceivable COVID-19 Culture Change for the Better
An intern is rotating on a medical ward in January 2018. Influenza is prevalent and hospital admissions are increasing daily. Despite receiving her influenza vaccine in October 2017, she develops fevers and myalgias. Due to time constraints, she does not get tested for influenza. She instead decides to work while sick to avoid payback of shifts.
She is now a hematology/oncology fellow in December 2020. She and her colleagues experienced the harrowing first wave of the COVID-19 pandemic. Unfortunately, community prevalence and hospital admissions are again rising. She adheres to mandatory masking and eye protection at work. Two days after attending a procedural workshop with lunch provided, she develops headache, myalgias, and sore throat. She contacts her supervisor, calls out sick, and initiates home isolation due to a positive result on a COVID-19 test performed through occupational health services (OHS). No patients are affected, but multiple colleagues are required to quarantine and others are pulled to provide coverage.
PRESENTEEISM
Presenteeism, the act of attending work despite personal illness, can adversely affect individuals and organizations.1 In a healthcare setting, transmissible illnesses contribute to complications in patients and missed workdays for staff. Prior to the pandemic, the rate of presenteeism among physicians was as high as 90%.2 Such presenteeism may have contributed to medical errors and decreased work efficiency.3,4 At our hospital in the Bronx, New York, a high annual prevalence of seasonal influenza fueled influenza clusters among patients and trainees, leading to presenteeism.
Our prior work on influenza-related practices in academic medicine revealed that 54% of trainees and 26% of program directors self-reported influenza-like illness (ILI) presenteeism. Drivers included desire to display a strong work ethic, desire not to burden colleagues, concern about colleagues’ negative perceptions, and knowledge gaps in influenza transmission.5
INFLUENCE OF THE COVID-19 PANDEMIC ON PRESENTEEISM
The COVID-19 pandemic has profoundly affected staffing models, infection prevention protocols, use of shared spaces, educational conferences, visitation policies, and other habitual healthcare practices. The experience of post-graduate training during a pandemic has resulted in important mindset and practice changes that may decrease presenteeism. However, health systems need robust mechanisms to accommodate appropriate work absences due to illness. We hypothesize that ILI/COVID-like illness presenteeism will decrease significantly for the following reasons, which will have positive and negative impacts on the organization and individual.
Shift in Accountability and Rewards
Our 2018 study revealed that presenteeism was motivated by a desire not to burden colleagues with extra clinical duties and to display conscientiousness. Despite a back-up call system, house staff were concerned about colleagues’ negative perceptions. Accountability was perceived as fulfilling one’s assigned clinical duties rather than protecting others from illness.
More recently, staff have experienced personal or family illness with COVID-19 or witnessed its rapid spread through the healthcare system. Forty-two percent (103 of 245) of our internal medicine residents had work absences resulting in 875 total missed workdays between February 29 and May 22, 2020. At the peak of the pandemic’s first wave in the spring of 2020, 16% (38 of 245) were out sick.6 We hypothesize that this experience resulted in a modified sense of accountability to peers and patients which manifested as a desire not to expose them to illness. Staying home while ill is now positively reinforced by supervisors, and presenteeism is recognized as harmful rather than commendable. However, increased utilization of the back-up call system to meet patient care demands is a secondary consequence.
Consequences of Exposures
While trainees and program faculty acknowledged that presenteeism puts patients and coworkers at risk,5 there was insufficient individual or institutional motivation to prevent it or fear its consequences pre-pandemic. An individual infected with influenza A may spread illness to one or two others, and several outpatient influenza treatments exist. Also, current trainees did not experience the prior respiratory viral pandemic (2009 H1N1 influenza A) as healthcare workers (HCWs).
In contrast, SARS-CoV-2 is more transmissible, with one infection resulting in two to three additional cases.7 Hence, mandatory quarantine and isolation policies are more stringent than those for influenza. While reinfection with SARS-CoV-2 is rare,8 HCWs can be exposed and quarantined multiple times, which potentially impacts paid sick leave for HCWs and elective-time for house staff pursuing fellowships. COVID-19 among HCWs also impacts secondary contacts, resulting in missed work and school days and strain on families. Hospital resource utilization for contact tracing and testing postexposure is significant. Unlike influenza, there are currently no oral antiviral treatments for outpatient COVID-19, and illness has been linked to chronic disabling symptoms.9 Finally, absences due to illness or quarantine may disrupt education, training, and fulfillment of competencies and experiences necessary for advancement.
We predict that these potentially sweeping consequences will reduce presenteeism. An important aspect of health system pandemic planning must include adequate staffing to account for work absences due to illness or quarantine.
Access to Occupational Health Services
Previously, staff reported barriers to seeking care from OHS. Therefore, this step was skipped, and HCWs managed their own symptoms, tested and treated each other for influenza, and returned to work at an arbitrary interval, without coordination with OHS protocols. OHS processes have since greatly improved. Employees with a COVID-19 exposure or concerning symptoms call the OHS hotline, are referred for same-day testing, and are given specific instructions regarding home quarantine or isolation and return to work. Follow-up to confirm fitness for duty is provided. In September 2020, an electronic screening tool assessing COVID-19 symptoms, exposures, and high-risk travel was implemented at our institution. Associates must present their clearance at hospital entrances.
Protection From Vaccine
Survey results indicated that all house staff and program faculty received the annual influenza vaccine.5 In New York State, public health regulations ensure a high rate of annual influenza vaccination among HCWs.10 It is possible that house staff did not perceive that ILI symptoms were caused by influenza after vaccination, and that vaccinated colleagues were at lower risk of illness. The influenza vaccine also has a well-established safety record, contributing to good uptake among HCWs.
At the time of writing of this article, HCWs have been prioritized for COVID-19 vaccination. Studies are in progress pertaining to the degree of protection after one dose, incidence of new infections after first and second doses, and secondary transmissions from vaccinated individuals. Vaccination is likely to influence HCW behaviors as well as occupational health policies. We suggest that the impact of COVID-19 vaccination on subsequent HCW presenteeism be given precedence in future studies.
Consistent Messaging and Communication
Prior to the pandemic, regular communication to staff on transmissible disease outbreaks scarcely occurred. Likewise, recurring training on infection prevention and personal protective equipment (PPE) protocols did not occur, and hospital policies regarding personal illness were not emphasized. Harms of presenteeism were infrequently addressed outside of nosocomial outbreaks. The pandemic has positively impacted communication from hospital leadership. Infection control and occupational health guidelines are continually revised and disseminated. Program directors send regular COVID-19 updates to trainees. The infectious diseases program director serves as a graduate medical education liaison to hospital leadership. All staff are regularly updated on evolving policies and given resources to assist with personal illness. While many positive practice changes have occurred, a decrease in presenteeism may exhaust sick coverage and compromise patient care. We suggest that health systems create safer work environments and ensure adequate staffing to accommodate illnesses and quarantines.
STRATEGIES TO CREATE SAFER WORK ENVIRONMENTS
- Conduct recurring staff PPE simulations spanning a range of communicable illnesses.
- Ensure adequate PPE for surge conditions.
- Implement occupancy limits for shared spaces, distanced seating, staggered mealtimes, plexiglass barriers, and portable air-filtration systems in rooms lacking windows.
- Invest in large-scale, serial testing of asymptomatic HCWs to identify early cases and enact quarantines prior to excess exposures.
STRATEGIES TO ADDRESS STAFFING CONSTRAINTS IN ACADEMIC MEDICAL CENTERS
- Adopt nonpunitive coverage systems, reducing presenteeism by removing expectations to “pay-back” colleagues later.
- Establish a third-party notification system, reducing strain on house staff to find coverage. This will enable strategic use of the jeopardy pool by training program leadership.
- Establish a backup coverage pool populated by hospitalists and third-year residents who have completed fellowship match. Ideally, health systems should be prepared to compensate physicians for extra shifts.
- Engage nondeployed physician assistants or nurse practitioners to provide coverage for residents on a per diem basis.
- At a federal level, funding for trainee workforce expansion can occur to ensure staffing redundancy. The appropriate number of trainees should be determined by program leadership, balancing surge needs with education and autonomy. Likewise, training extensions due to COVID-related absences or deployments away from research or electives should be federally funded.
- Inpatient and community COVID-19 surges can result in large-scale furloughs of HCWs; hospital leadership should expediently implement public health recommendations allowing fully immunized HCWs to work after exposures while maximally adhering to infection prevention protocols.
The COVID-19 pandemic has profoundly impacted academic medicine. It is imperative to explore solutions to balance workplace safety, education, and training with staffing constraints and patient care needs. Resource investment and executive leadership support are required to achieve this balance.
1. Webster RK, Liu R, Karimullina K, Hall I, Amlôt R, Rubin GJ. A systematic review of infectious illness Presenteeism: prevalence, reasons and risk factors. BMC Public Health. 2019;19:799. https://doi.org/10.1186/s12889-019-7138-x
2. Bergström G, Bodin L, Hagberg J, Aronsson G, Josephson M. Sickness presenteeism today, sickness absenteeism tomorrow? A prospective study on sickness presenteeism and future sickness absenteeism. J Occup Environ Med. 2009;51(6):629-638. https://doi.org/10.1097/JOM.0b013e3181a8281b
3. Al Nuhait M, Al Harbi K, Al Jarboa A, et al. Sickness presenteeism among health care providers in an academic tertiary care center in Riyadh. J Infect Public Health. 2017;10(6):711-715. https://doi.org/10.1016/j.jiph.2016.09.019
4. Brborovic H, Brborovic O. Patient safety culture shapes presenteeism and absenteeism: a cross-sectional study among Croatian healthcare workers. Arh Hig Rada Toksikol. 2017;68(3):185-189. https://doi.org/10.1515/aiht-2017-68-2957
5. Cowman K, Mittal J, Weston G, et al. Understanding drivers of influenza-like illness presenteeism within training programs: a survey of trainees and their program directors. Am J Infect Control. 2019;47(8):895-901. https://doi.org/10.1016/j.ajic.2019.02.004
6. Merkin R, Kruger A, Bhardwaj G, Kajita GR, Shapiro L, Galen BT. Internal medicine resident work absence during the COVID-19 pandemic at a large academic medical center in New York City. J Grad Med Educ. 2020;12(6):682-685. https://doi.org/10.4300/JGME-D-20-00657.1
7. Petersen E, Koopmans M, Go U, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis. 2020;20(9):e238-244. https://doi.org/10.1016/S1473-3099(20)30484-9
8. Reinfection with COVID-19. Centers for Disease Control and Prevention. Updated October 27, 2020. Accessed March 31, 2021. https://www.cdc.gov/coronavirus/2019-ncov/your-health/reinfection.html
9. Rubin R. As their numbers grow, COVID-19 “long haulers” stump experts. JAMA. 2020;324(14):1381-1383. https://doi.org/10.1001/jama.2020.17709
10. Regulation for prevention of influenza transmission by healthcare and residential facility and agency personnel. New York State Department of Health. Revised March 2021. Accessed December 7, 2020. https://www.health.ny.gov/diseases/communicable/influenza/seasonal/providers/prevention_of_influenza_transmission/
An intern is rotating on a medical ward in January 2018. Influenza is prevalent and hospital admissions are increasing daily. Despite receiving her influenza vaccine in October 2017, she develops fevers and myalgias. Due to time constraints, she does not get tested for influenza. She instead decides to work while sick to avoid payback of shifts.
She is now a hematology/oncology fellow in December 2020. She and her colleagues experienced the harrowing first wave of the COVID-19 pandemic. Unfortunately, community prevalence and hospital admissions are again rising. She adheres to mandatory masking and eye protection at work. Two days after attending a procedural workshop with lunch provided, she develops headache, myalgias, and sore throat. She contacts her supervisor, calls out sick, and initiates home isolation due to a positive result on a COVID-19 test performed through occupational health services (OHS). No patients are affected, but multiple colleagues are required to quarantine and others are pulled to provide coverage.
PRESENTEEISM
Presenteeism, the act of attending work despite personal illness, can adversely affect individuals and organizations.1 In a healthcare setting, transmissible illnesses contribute to complications in patients and missed workdays for staff. Prior to the pandemic, the rate of presenteeism among physicians was as high as 90%.2 Such presenteeism may have contributed to medical errors and decreased work efficiency.3,4 At our hospital in the Bronx, New York, a high annual prevalence of seasonal influenza fueled influenza clusters among patients and trainees, leading to presenteeism.
Our prior work on influenza-related practices in academic medicine revealed that 54% of trainees and 26% of program directors self-reported influenza-like illness (ILI) presenteeism. Drivers included desire to display a strong work ethic, desire not to burden colleagues, concern about colleagues’ negative perceptions, and knowledge gaps in influenza transmission.5
INFLUENCE OF THE COVID-19 PANDEMIC ON PRESENTEEISM
The COVID-19 pandemic has profoundly affected staffing models, infection prevention protocols, use of shared spaces, educational conferences, visitation policies, and other habitual healthcare practices. The experience of post-graduate training during a pandemic has resulted in important mindset and practice changes that may decrease presenteeism. However, health systems need robust mechanisms to accommodate appropriate work absences due to illness. We hypothesize that ILI/COVID-like illness presenteeism will decrease significantly for the following reasons, which will have positive and negative impacts on the organization and individual.
Shift in Accountability and Rewards
Our 2018 study revealed that presenteeism was motivated by a desire not to burden colleagues with extra clinical duties and to display conscientiousness. Despite a back-up call system, house staff were concerned about colleagues’ negative perceptions. Accountability was perceived as fulfilling one’s assigned clinical duties rather than protecting others from illness.
More recently, staff have experienced personal or family illness with COVID-19 or witnessed its rapid spread through the healthcare system. Forty-two percent (103 of 245) of our internal medicine residents had work absences resulting in 875 total missed workdays between February 29 and May 22, 2020. At the peak of the pandemic’s first wave in the spring of 2020, 16% (38 of 245) were out sick.6 We hypothesize that this experience resulted in a modified sense of accountability to peers and patients which manifested as a desire not to expose them to illness. Staying home while ill is now positively reinforced by supervisors, and presenteeism is recognized as harmful rather than commendable. However, increased utilization of the back-up call system to meet patient care demands is a secondary consequence.
Consequences of Exposures
While trainees and program faculty acknowledged that presenteeism puts patients and coworkers at risk,5 there was insufficient individual or institutional motivation to prevent it or fear its consequences pre-pandemic. An individual infected with influenza A may spread illness to one or two others, and several outpatient influenza treatments exist. Also, current trainees did not experience the prior respiratory viral pandemic (2009 H1N1 influenza A) as healthcare workers (HCWs).
In contrast, SARS-CoV-2 is more transmissible, with one infection resulting in two to three additional cases.7 Hence, mandatory quarantine and isolation policies are more stringent than those for influenza. While reinfection with SARS-CoV-2 is rare,8 HCWs can be exposed and quarantined multiple times, which potentially impacts paid sick leave for HCWs and elective-time for house staff pursuing fellowships. COVID-19 among HCWs also impacts secondary contacts, resulting in missed work and school days and strain on families. Hospital resource utilization for contact tracing and testing postexposure is significant. Unlike influenza, there are currently no oral antiviral treatments for outpatient COVID-19, and illness has been linked to chronic disabling symptoms.9 Finally, absences due to illness or quarantine may disrupt education, training, and fulfillment of competencies and experiences necessary for advancement.
We predict that these potentially sweeping consequences will reduce presenteeism. An important aspect of health system pandemic planning must include adequate staffing to account for work absences due to illness or quarantine.
Access to Occupational Health Services
Previously, staff reported barriers to seeking care from OHS. Therefore, this step was skipped, and HCWs managed their own symptoms, tested and treated each other for influenza, and returned to work at an arbitrary interval, without coordination with OHS protocols. OHS processes have since greatly improved. Employees with a COVID-19 exposure or concerning symptoms call the OHS hotline, are referred for same-day testing, and are given specific instructions regarding home quarantine or isolation and return to work. Follow-up to confirm fitness for duty is provided. In September 2020, an electronic screening tool assessing COVID-19 symptoms, exposures, and high-risk travel was implemented at our institution. Associates must present their clearance at hospital entrances.
Protection From Vaccine
Survey results indicated that all house staff and program faculty received the annual influenza vaccine.5 In New York State, public health regulations ensure a high rate of annual influenza vaccination among HCWs.10 It is possible that house staff did not perceive that ILI symptoms were caused by influenza after vaccination, and that vaccinated colleagues were at lower risk of illness. The influenza vaccine also has a well-established safety record, contributing to good uptake among HCWs.
At the time of writing of this article, HCWs have been prioritized for COVID-19 vaccination. Studies are in progress pertaining to the degree of protection after one dose, incidence of new infections after first and second doses, and secondary transmissions from vaccinated individuals. Vaccination is likely to influence HCW behaviors as well as occupational health policies. We suggest that the impact of COVID-19 vaccination on subsequent HCW presenteeism be given precedence in future studies.
Consistent Messaging and Communication
Prior to the pandemic, regular communication to staff on transmissible disease outbreaks scarcely occurred. Likewise, recurring training on infection prevention and personal protective equipment (PPE) protocols did not occur, and hospital policies regarding personal illness were not emphasized. Harms of presenteeism were infrequently addressed outside of nosocomial outbreaks. The pandemic has positively impacted communication from hospital leadership. Infection control and occupational health guidelines are continually revised and disseminated. Program directors send regular COVID-19 updates to trainees. The infectious diseases program director serves as a graduate medical education liaison to hospital leadership. All staff are regularly updated on evolving policies and given resources to assist with personal illness. While many positive practice changes have occurred, a decrease in presenteeism may exhaust sick coverage and compromise patient care. We suggest that health systems create safer work environments and ensure adequate staffing to accommodate illnesses and quarantines.
STRATEGIES TO CREATE SAFER WORK ENVIRONMENTS
- Conduct recurring staff PPE simulations spanning a range of communicable illnesses.
- Ensure adequate PPE for surge conditions.
- Implement occupancy limits for shared spaces, distanced seating, staggered mealtimes, plexiglass barriers, and portable air-filtration systems in rooms lacking windows.
- Invest in large-scale, serial testing of asymptomatic HCWs to identify early cases and enact quarantines prior to excess exposures.
STRATEGIES TO ADDRESS STAFFING CONSTRAINTS IN ACADEMIC MEDICAL CENTERS
- Adopt nonpunitive coverage systems, reducing presenteeism by removing expectations to “pay-back” colleagues later.
- Establish a third-party notification system, reducing strain on house staff to find coverage. This will enable strategic use of the jeopardy pool by training program leadership.
- Establish a backup coverage pool populated by hospitalists and third-year residents who have completed fellowship match. Ideally, health systems should be prepared to compensate physicians for extra shifts.
- Engage nondeployed physician assistants or nurse practitioners to provide coverage for residents on a per diem basis.
- At a federal level, funding for trainee workforce expansion can occur to ensure staffing redundancy. The appropriate number of trainees should be determined by program leadership, balancing surge needs with education and autonomy. Likewise, training extensions due to COVID-related absences or deployments away from research or electives should be federally funded.
- Inpatient and community COVID-19 surges can result in large-scale furloughs of HCWs; hospital leadership should expediently implement public health recommendations allowing fully immunized HCWs to work after exposures while maximally adhering to infection prevention protocols.
The COVID-19 pandemic has profoundly impacted academic medicine. It is imperative to explore solutions to balance workplace safety, education, and training with staffing constraints and patient care needs. Resource investment and executive leadership support are required to achieve this balance.
An intern is rotating on a medical ward in January 2018. Influenza is prevalent and hospital admissions are increasing daily. Despite receiving her influenza vaccine in October 2017, she develops fevers and myalgias. Due to time constraints, she does not get tested for influenza. She instead decides to work while sick to avoid payback of shifts.
She is now a hematology/oncology fellow in December 2020. She and her colleagues experienced the harrowing first wave of the COVID-19 pandemic. Unfortunately, community prevalence and hospital admissions are again rising. She adheres to mandatory masking and eye protection at work. Two days after attending a procedural workshop with lunch provided, she develops headache, myalgias, and sore throat. She contacts her supervisor, calls out sick, and initiates home isolation due to a positive result on a COVID-19 test performed through occupational health services (OHS). No patients are affected, but multiple colleagues are required to quarantine and others are pulled to provide coverage.
PRESENTEEISM
Presenteeism, the act of attending work despite personal illness, can adversely affect individuals and organizations.1 In a healthcare setting, transmissible illnesses contribute to complications in patients and missed workdays for staff. Prior to the pandemic, the rate of presenteeism among physicians was as high as 90%.2 Such presenteeism may have contributed to medical errors and decreased work efficiency.3,4 At our hospital in the Bronx, New York, a high annual prevalence of seasonal influenza fueled influenza clusters among patients and trainees, leading to presenteeism.
Our prior work on influenza-related practices in academic medicine revealed that 54% of trainees and 26% of program directors self-reported influenza-like illness (ILI) presenteeism. Drivers included desire to display a strong work ethic, desire not to burden colleagues, concern about colleagues’ negative perceptions, and knowledge gaps in influenza transmission.5
INFLUENCE OF THE COVID-19 PANDEMIC ON PRESENTEEISM
The COVID-19 pandemic has profoundly affected staffing models, infection prevention protocols, use of shared spaces, educational conferences, visitation policies, and other habitual healthcare practices. The experience of post-graduate training during a pandemic has resulted in important mindset and practice changes that may decrease presenteeism. However, health systems need robust mechanisms to accommodate appropriate work absences due to illness. We hypothesize that ILI/COVID-like illness presenteeism will decrease significantly for the following reasons, which will have positive and negative impacts on the organization and individual.
Shift in Accountability and Rewards
Our 2018 study revealed that presenteeism was motivated by a desire not to burden colleagues with extra clinical duties and to display conscientiousness. Despite a back-up call system, house staff were concerned about colleagues’ negative perceptions. Accountability was perceived as fulfilling one’s assigned clinical duties rather than protecting others from illness.
More recently, staff have experienced personal or family illness with COVID-19 or witnessed its rapid spread through the healthcare system. Forty-two percent (103 of 245) of our internal medicine residents had work absences resulting in 875 total missed workdays between February 29 and May 22, 2020. At the peak of the pandemic’s first wave in the spring of 2020, 16% (38 of 245) were out sick.6 We hypothesize that this experience resulted in a modified sense of accountability to peers and patients which manifested as a desire not to expose them to illness. Staying home while ill is now positively reinforced by supervisors, and presenteeism is recognized as harmful rather than commendable. However, increased utilization of the back-up call system to meet patient care demands is a secondary consequence.
Consequences of Exposures
While trainees and program faculty acknowledged that presenteeism puts patients and coworkers at risk,5 there was insufficient individual or institutional motivation to prevent it or fear its consequences pre-pandemic. An individual infected with influenza A may spread illness to one or two others, and several outpatient influenza treatments exist. Also, current trainees did not experience the prior respiratory viral pandemic (2009 H1N1 influenza A) as healthcare workers (HCWs).
In contrast, SARS-CoV-2 is more transmissible, with one infection resulting in two to three additional cases.7 Hence, mandatory quarantine and isolation policies are more stringent than those for influenza. While reinfection with SARS-CoV-2 is rare,8 HCWs can be exposed and quarantined multiple times, which potentially impacts paid sick leave for HCWs and elective-time for house staff pursuing fellowships. COVID-19 among HCWs also impacts secondary contacts, resulting in missed work and school days and strain on families. Hospital resource utilization for contact tracing and testing postexposure is significant. Unlike influenza, there are currently no oral antiviral treatments for outpatient COVID-19, and illness has been linked to chronic disabling symptoms.9 Finally, absences due to illness or quarantine may disrupt education, training, and fulfillment of competencies and experiences necessary for advancement.
We predict that these potentially sweeping consequences will reduce presenteeism. An important aspect of health system pandemic planning must include adequate staffing to account for work absences due to illness or quarantine.
Access to Occupational Health Services
Previously, staff reported barriers to seeking care from OHS. Therefore, this step was skipped, and HCWs managed their own symptoms, tested and treated each other for influenza, and returned to work at an arbitrary interval, without coordination with OHS protocols. OHS processes have since greatly improved. Employees with a COVID-19 exposure or concerning symptoms call the OHS hotline, are referred for same-day testing, and are given specific instructions regarding home quarantine or isolation and return to work. Follow-up to confirm fitness for duty is provided. In September 2020, an electronic screening tool assessing COVID-19 symptoms, exposures, and high-risk travel was implemented at our institution. Associates must present their clearance at hospital entrances.
Protection From Vaccine
Survey results indicated that all house staff and program faculty received the annual influenza vaccine.5 In New York State, public health regulations ensure a high rate of annual influenza vaccination among HCWs.10 It is possible that house staff did not perceive that ILI symptoms were caused by influenza after vaccination, and that vaccinated colleagues were at lower risk of illness. The influenza vaccine also has a well-established safety record, contributing to good uptake among HCWs.
At the time of writing of this article, HCWs have been prioritized for COVID-19 vaccination. Studies are in progress pertaining to the degree of protection after one dose, incidence of new infections after first and second doses, and secondary transmissions from vaccinated individuals. Vaccination is likely to influence HCW behaviors as well as occupational health policies. We suggest that the impact of COVID-19 vaccination on subsequent HCW presenteeism be given precedence in future studies.
Consistent Messaging and Communication
Prior to the pandemic, regular communication to staff on transmissible disease outbreaks scarcely occurred. Likewise, recurring training on infection prevention and personal protective equipment (PPE) protocols did not occur, and hospital policies regarding personal illness were not emphasized. Harms of presenteeism were infrequently addressed outside of nosocomial outbreaks. The pandemic has positively impacted communication from hospital leadership. Infection control and occupational health guidelines are continually revised and disseminated. Program directors send regular COVID-19 updates to trainees. The infectious diseases program director serves as a graduate medical education liaison to hospital leadership. All staff are regularly updated on evolving policies and given resources to assist with personal illness. While many positive practice changes have occurred, a decrease in presenteeism may exhaust sick coverage and compromise patient care. We suggest that health systems create safer work environments and ensure adequate staffing to accommodate illnesses and quarantines.
STRATEGIES TO CREATE SAFER WORK ENVIRONMENTS
- Conduct recurring staff PPE simulations spanning a range of communicable illnesses.
- Ensure adequate PPE for surge conditions.
- Implement occupancy limits for shared spaces, distanced seating, staggered mealtimes, plexiglass barriers, and portable air-filtration systems in rooms lacking windows.
- Invest in large-scale, serial testing of asymptomatic HCWs to identify early cases and enact quarantines prior to excess exposures.
STRATEGIES TO ADDRESS STAFFING CONSTRAINTS IN ACADEMIC MEDICAL CENTERS
- Adopt nonpunitive coverage systems, reducing presenteeism by removing expectations to “pay-back” colleagues later.
- Establish a third-party notification system, reducing strain on house staff to find coverage. This will enable strategic use of the jeopardy pool by training program leadership.
- Establish a backup coverage pool populated by hospitalists and third-year residents who have completed fellowship match. Ideally, health systems should be prepared to compensate physicians for extra shifts.
- Engage nondeployed physician assistants or nurse practitioners to provide coverage for residents on a per diem basis.
- At a federal level, funding for trainee workforce expansion can occur to ensure staffing redundancy. The appropriate number of trainees should be determined by program leadership, balancing surge needs with education and autonomy. Likewise, training extensions due to COVID-related absences or deployments away from research or electives should be federally funded.
- Inpatient and community COVID-19 surges can result in large-scale furloughs of HCWs; hospital leadership should expediently implement public health recommendations allowing fully immunized HCWs to work after exposures while maximally adhering to infection prevention protocols.
The COVID-19 pandemic has profoundly impacted academic medicine. It is imperative to explore solutions to balance workplace safety, education, and training with staffing constraints and patient care needs. Resource investment and executive leadership support are required to achieve this balance.
1. Webster RK, Liu R, Karimullina K, Hall I, Amlôt R, Rubin GJ. A systematic review of infectious illness Presenteeism: prevalence, reasons and risk factors. BMC Public Health. 2019;19:799. https://doi.org/10.1186/s12889-019-7138-x
2. Bergström G, Bodin L, Hagberg J, Aronsson G, Josephson M. Sickness presenteeism today, sickness absenteeism tomorrow? A prospective study on sickness presenteeism and future sickness absenteeism. J Occup Environ Med. 2009;51(6):629-638. https://doi.org/10.1097/JOM.0b013e3181a8281b
3. Al Nuhait M, Al Harbi K, Al Jarboa A, et al. Sickness presenteeism among health care providers in an academic tertiary care center in Riyadh. J Infect Public Health. 2017;10(6):711-715. https://doi.org/10.1016/j.jiph.2016.09.019
4. Brborovic H, Brborovic O. Patient safety culture shapes presenteeism and absenteeism: a cross-sectional study among Croatian healthcare workers. Arh Hig Rada Toksikol. 2017;68(3):185-189. https://doi.org/10.1515/aiht-2017-68-2957
5. Cowman K, Mittal J, Weston G, et al. Understanding drivers of influenza-like illness presenteeism within training programs: a survey of trainees and their program directors. Am J Infect Control. 2019;47(8):895-901. https://doi.org/10.1016/j.ajic.2019.02.004
6. Merkin R, Kruger A, Bhardwaj G, Kajita GR, Shapiro L, Galen BT. Internal medicine resident work absence during the COVID-19 pandemic at a large academic medical center in New York City. J Grad Med Educ. 2020;12(6):682-685. https://doi.org/10.4300/JGME-D-20-00657.1
7. Petersen E, Koopmans M, Go U, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis. 2020;20(9):e238-244. https://doi.org/10.1016/S1473-3099(20)30484-9
8. Reinfection with COVID-19. Centers for Disease Control and Prevention. Updated October 27, 2020. Accessed March 31, 2021. https://www.cdc.gov/coronavirus/2019-ncov/your-health/reinfection.html
9. Rubin R. As their numbers grow, COVID-19 “long haulers” stump experts. JAMA. 2020;324(14):1381-1383. https://doi.org/10.1001/jama.2020.17709
10. Regulation for prevention of influenza transmission by healthcare and residential facility and agency personnel. New York State Department of Health. Revised March 2021. Accessed December 7, 2020. https://www.health.ny.gov/diseases/communicable/influenza/seasonal/providers/prevention_of_influenza_transmission/
1. Webster RK, Liu R, Karimullina K, Hall I, Amlôt R, Rubin GJ. A systematic review of infectious illness Presenteeism: prevalence, reasons and risk factors. BMC Public Health. 2019;19:799. https://doi.org/10.1186/s12889-019-7138-x
2. Bergström G, Bodin L, Hagberg J, Aronsson G, Josephson M. Sickness presenteeism today, sickness absenteeism tomorrow? A prospective study on sickness presenteeism and future sickness absenteeism. J Occup Environ Med. 2009;51(6):629-638. https://doi.org/10.1097/JOM.0b013e3181a8281b
3. Al Nuhait M, Al Harbi K, Al Jarboa A, et al. Sickness presenteeism among health care providers in an academic tertiary care center in Riyadh. J Infect Public Health. 2017;10(6):711-715. https://doi.org/10.1016/j.jiph.2016.09.019
4. Brborovic H, Brborovic O. Patient safety culture shapes presenteeism and absenteeism: a cross-sectional study among Croatian healthcare workers. Arh Hig Rada Toksikol. 2017;68(3):185-189. https://doi.org/10.1515/aiht-2017-68-2957
5. Cowman K, Mittal J, Weston G, et al. Understanding drivers of influenza-like illness presenteeism within training programs: a survey of trainees and their program directors. Am J Infect Control. 2019;47(8):895-901. https://doi.org/10.1016/j.ajic.2019.02.004
6. Merkin R, Kruger A, Bhardwaj G, Kajita GR, Shapiro L, Galen BT. Internal medicine resident work absence during the COVID-19 pandemic at a large academic medical center in New York City. J Grad Med Educ. 2020;12(6):682-685. https://doi.org/10.4300/JGME-D-20-00657.1
7. Petersen E, Koopmans M, Go U, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis. 2020;20(9):e238-244. https://doi.org/10.1016/S1473-3099(20)30484-9
8. Reinfection with COVID-19. Centers for Disease Control and Prevention. Updated October 27, 2020. Accessed March 31, 2021. https://www.cdc.gov/coronavirus/2019-ncov/your-health/reinfection.html
9. Rubin R. As their numbers grow, COVID-19 “long haulers” stump experts. JAMA. 2020;324(14):1381-1383. https://doi.org/10.1001/jama.2020.17709
10. Regulation for prevention of influenza transmission by healthcare and residential facility and agency personnel. New York State Department of Health. Revised March 2021. Accessed December 7, 2020. https://www.health.ny.gov/diseases/communicable/influenza/seasonal/providers/prevention_of_influenza_transmission/
© 2021 Society of Hospital Medicine
Still Burning
A celebratory mood pervaded the last week of service for my ward team at the end of the academic year. As the attending, it was just another day, but it was hard not to be caught up in the general feeling of a milestone flying past. Like most days in a hospital, this one passed in a rhythm of alternating mundanity and crisis. Late in the afternoon, one of the residents called me to a bedside for help. Imagining that my diagnostic skills were urgently required, I took the stairs. The problem, as it turned out, was not strictly medical.
I could hear the yelling before I cleared the locked entry doors to the ward. It doesn’t really matter what the yelling was about, just that there is often yelling and there is always very little I can do about the root cause of it. As I stepped into the middle of the conflagration, I remembered the story an intern told me about the night earlier in the month when it fell to her to wheel the same patient’s intoxicated parent down to the emergency department. After sleeping it off, the parent was diagnosed with an “allergic reaction” and given a prescription for diphenhydramine. We all knew the diagnosis was fantasy, and yet we all went along with it because there was simply no help available for the root cause of the problem. State social services was already involved, and we had a “safety” plan in place for discharge. As meager as that may have been, we had done the best we could to balance the risk with the available resources… or so we told ourselves.
As a nation, we have chosen not to provide much of a social safety net for our citizens who suffer from addiction and/or mental illness and, most importantly, for those who’ve just not had a leg up on the economic ladder. As a hospital-based clinician, I know that people in distress lose their cool and yell sometimes. Ironically, they may yell most loudly at people who sincerely want to help, simply because others do not engage them. Medical schools don’t teach us how to handle the yelling, though many would say it is part of the hidden curriculum. One thing that distinguishes many pediatricians like myself is a willingness to listen to the yelling, to engage with it, and to try to help. Not surprisingly, our reputation around the hospital is that we skew a bit naive.
It is worth asking, though: Are pediatricians naive? Sure, we make funny faces. We clown. We baby-talk. Those things are largely true, but there are other true things about pediatricians. Chief among them is the fact that we come to know some of the worst things there are to know about human beings. Everybody knows people can be awful, but we know exactly how awful they are to defenseless children in precise detail. For instance, I’ve seen a 4-year-old who was repeatedly starved as a regular punishment. She was so hungry she ate her hair, which turned out to be lucky for her because it caused an intestinal blockage that led to the discovery of the abuse. I gave her an apple one day and she immediately hid it under her shirt. Where you see a scab on a child’s inner arm, I see a cigarette burn. I’ve resuscitated a baby whose parents dipped his pacifier in heroin to stop his crying—the remarkable part of the story being that it was heroin cooked in the hospital bathroom. And then there are the things that I cannot even bring myself to write down.
Carrying this knowledge hollows out a gap between pediatricians and the rest of the world. The divergence between our expectations of how a society should treat its children and the reality of our daily experience grinds away any naivete. The gap becomes a canyon for some of us. We live with the sense that nobody would believe the things we’ve seen, so we rarely talk about them. Years ago, I was testifying in a (for me) routine child-abuse case where this fact hit home. It is common for juries to disbelieve that a caregiver could do the things we allege. I say allege, but if you work as a pediatrician long enough, the space between allegation and fact narrows. It is simply pattern recognition to you—abuse happens so consistently that we accept it as a diagnostic category. The case in question was a submersion burn, which is an almost unmistakable pattern. The other piece of the story is that it happens to toddlers during toilet training as caregivers lose their self-control and punish children for soiling themselves. For me, simple pattern recognition; for the jury, simply unbelievable. We lost the case.
We are almost always losing the case as pediatricians. Spending on children makes up less than 10% of the federal budget, whereas spending on the elderly, including Social Security, Medicare, and the adult component of Medicaid, dominates that budget.1 Moreover, twice as many children as adults over age 65 are living in poverty in the United States. The Temporary Assistance for Needy Families program is often debated in this country and frequently criticized as wasteful. However, what is not debatable is that the allocated budget ($16.5 billion) hasn’t changed since 1996, resulting in a functional 40% decrease due to inflation.2 Life, for poor children, gets a little tougher every year.
After the resident and I wrapped up our day, we talked a little about how hard it is to witness some of the things you see in a children’s hospital. I could see the gap between her and the outside world widening right in front of me. In my weaker moments, I want to tell trainees like her to run while they can. I want to warn them that they don’t want to know so many of the things we’re going to teach them. I know how the story usually ends. I know that our country doesn’t promise children safety from social deprivation, hunger, or physical abuse. Instead, we’ve created the conditions for those things to occur at embarrassingly high rates, and we prosecute the unlucky after the fact. The children are simply collateral damage.
We stood at our patient’s bedside and tried to imagine a happy future. Even without his medical problems, he would likely need a major investment of resources in order to thrive. Where would those resources come from? I saw the hospital crib, metal bars on all sides and a thick plastic roof to prevent escape, as a metaphor. Later, I took the elevator down and overheard a snippet of conversation between two residents. One of them asked the other, “How do you know when you’ve burned out?” The other replied, “I don’t know, I guess when you’ve stopped burning.” Burnout is a hot topic in medicine, and some may assume the reasons are obvious: long hours and intellectually demanding work. In reality, those drivers may be less important than the repeated exposure to profound injustice inherent to the practice of medicine in our country.
As hospitalists, we address acute decompensation in our patients and send them back out into the world knowing there will soon be a next time. We also know that the next time might be preventable, if only … This cycle sometimes feels inexorable, but it can also prompt us to think about our obligation to work toward a more just society. We have to imagine a better future even as we struggle to believe it is on the way.
Most of our hospitals are trying to help. They have community-engagement programs, they purchase housing for homeless patients, they provide large amounts of uncompensated care and sometimes operate at a loss. Yet none of this addresses the root cause of the problem. Medicine, either in the form of an institution or a doctor, can’t replace a just society, but the truth of this fact does not mean we should not try.
Pediatrics has always been a field disposed toward advocacy. The origin of our largest professional organization in the United States was the intraprofessional conflict within the American Medical Association (AMA) over the Sheppard-Towner Act of 1921, one of this country’s first attempts to address the social determinants of health with legislation.3 The American Academy of Pediatrics was formed in 1930 after the AMA House of Delegates rebuked the Pediatric section for advocating for continuance of the act during the late 1920s.3 Perhaps what Pediatrics has to teach the rest of medicine is the necessity of making advocacy a part of our professional identity. And perhaps that’s the reason that so many pediatricians are still burning and not burned out.
1. Committee for a Responsible Federal Budget. Chartbook: budgeting for the next generation. October 11, 2018. Accessed February 2, 2021. http://www.crfb.org/papers/chartbook-budgeting-next-generation
2. Center on Budget and Policy Priorities. Policy basics: temporary assistance for needy families. Updated March 31, 2021. Accessed February 2, 2021. https://www.cbpp.org/research/family-income-support/temporary-assistance-for-needy-families
3. van Dyck PC. A history of child health equity legislation in the United States. Pediatrics. 2003;112(3 pt 2):727-730.
A celebratory mood pervaded the last week of service for my ward team at the end of the academic year. As the attending, it was just another day, but it was hard not to be caught up in the general feeling of a milestone flying past. Like most days in a hospital, this one passed in a rhythm of alternating mundanity and crisis. Late in the afternoon, one of the residents called me to a bedside for help. Imagining that my diagnostic skills were urgently required, I took the stairs. The problem, as it turned out, was not strictly medical.
I could hear the yelling before I cleared the locked entry doors to the ward. It doesn’t really matter what the yelling was about, just that there is often yelling and there is always very little I can do about the root cause of it. As I stepped into the middle of the conflagration, I remembered the story an intern told me about the night earlier in the month when it fell to her to wheel the same patient’s intoxicated parent down to the emergency department. After sleeping it off, the parent was diagnosed with an “allergic reaction” and given a prescription for diphenhydramine. We all knew the diagnosis was fantasy, and yet we all went along with it because there was simply no help available for the root cause of the problem. State social services was already involved, and we had a “safety” plan in place for discharge. As meager as that may have been, we had done the best we could to balance the risk with the available resources… or so we told ourselves.
As a nation, we have chosen not to provide much of a social safety net for our citizens who suffer from addiction and/or mental illness and, most importantly, for those who’ve just not had a leg up on the economic ladder. As a hospital-based clinician, I know that people in distress lose their cool and yell sometimes. Ironically, they may yell most loudly at people who sincerely want to help, simply because others do not engage them. Medical schools don’t teach us how to handle the yelling, though many would say it is part of the hidden curriculum. One thing that distinguishes many pediatricians like myself is a willingness to listen to the yelling, to engage with it, and to try to help. Not surprisingly, our reputation around the hospital is that we skew a bit naive.
It is worth asking, though: Are pediatricians naive? Sure, we make funny faces. We clown. We baby-talk. Those things are largely true, but there are other true things about pediatricians. Chief among them is the fact that we come to know some of the worst things there are to know about human beings. Everybody knows people can be awful, but we know exactly how awful they are to defenseless children in precise detail. For instance, I’ve seen a 4-year-old who was repeatedly starved as a regular punishment. She was so hungry she ate her hair, which turned out to be lucky for her because it caused an intestinal blockage that led to the discovery of the abuse. I gave her an apple one day and she immediately hid it under her shirt. Where you see a scab on a child’s inner arm, I see a cigarette burn. I’ve resuscitated a baby whose parents dipped his pacifier in heroin to stop his crying—the remarkable part of the story being that it was heroin cooked in the hospital bathroom. And then there are the things that I cannot even bring myself to write down.
Carrying this knowledge hollows out a gap between pediatricians and the rest of the world. The divergence between our expectations of how a society should treat its children and the reality of our daily experience grinds away any naivete. The gap becomes a canyon for some of us. We live with the sense that nobody would believe the things we’ve seen, so we rarely talk about them. Years ago, I was testifying in a (for me) routine child-abuse case where this fact hit home. It is common for juries to disbelieve that a caregiver could do the things we allege. I say allege, but if you work as a pediatrician long enough, the space between allegation and fact narrows. It is simply pattern recognition to you—abuse happens so consistently that we accept it as a diagnostic category. The case in question was a submersion burn, which is an almost unmistakable pattern. The other piece of the story is that it happens to toddlers during toilet training as caregivers lose their self-control and punish children for soiling themselves. For me, simple pattern recognition; for the jury, simply unbelievable. We lost the case.
We are almost always losing the case as pediatricians. Spending on children makes up less than 10% of the federal budget, whereas spending on the elderly, including Social Security, Medicare, and the adult component of Medicaid, dominates that budget.1 Moreover, twice as many children as adults over age 65 are living in poverty in the United States. The Temporary Assistance for Needy Families program is often debated in this country and frequently criticized as wasteful. However, what is not debatable is that the allocated budget ($16.5 billion) hasn’t changed since 1996, resulting in a functional 40% decrease due to inflation.2 Life, for poor children, gets a little tougher every year.
After the resident and I wrapped up our day, we talked a little about how hard it is to witness some of the things you see in a children’s hospital. I could see the gap between her and the outside world widening right in front of me. In my weaker moments, I want to tell trainees like her to run while they can. I want to warn them that they don’t want to know so many of the things we’re going to teach them. I know how the story usually ends. I know that our country doesn’t promise children safety from social deprivation, hunger, or physical abuse. Instead, we’ve created the conditions for those things to occur at embarrassingly high rates, and we prosecute the unlucky after the fact. The children are simply collateral damage.
We stood at our patient’s bedside and tried to imagine a happy future. Even without his medical problems, he would likely need a major investment of resources in order to thrive. Where would those resources come from? I saw the hospital crib, metal bars on all sides and a thick plastic roof to prevent escape, as a metaphor. Later, I took the elevator down and overheard a snippet of conversation between two residents. One of them asked the other, “How do you know when you’ve burned out?” The other replied, “I don’t know, I guess when you’ve stopped burning.” Burnout is a hot topic in medicine, and some may assume the reasons are obvious: long hours and intellectually demanding work. In reality, those drivers may be less important than the repeated exposure to profound injustice inherent to the practice of medicine in our country.
As hospitalists, we address acute decompensation in our patients and send them back out into the world knowing there will soon be a next time. We also know that the next time might be preventable, if only … This cycle sometimes feels inexorable, but it can also prompt us to think about our obligation to work toward a more just society. We have to imagine a better future even as we struggle to believe it is on the way.
Most of our hospitals are trying to help. They have community-engagement programs, they purchase housing for homeless patients, they provide large amounts of uncompensated care and sometimes operate at a loss. Yet none of this addresses the root cause of the problem. Medicine, either in the form of an institution or a doctor, can’t replace a just society, but the truth of this fact does not mean we should not try.
Pediatrics has always been a field disposed toward advocacy. The origin of our largest professional organization in the United States was the intraprofessional conflict within the American Medical Association (AMA) over the Sheppard-Towner Act of 1921, one of this country’s first attempts to address the social determinants of health with legislation.3 The American Academy of Pediatrics was formed in 1930 after the AMA House of Delegates rebuked the Pediatric section for advocating for continuance of the act during the late 1920s.3 Perhaps what Pediatrics has to teach the rest of medicine is the necessity of making advocacy a part of our professional identity. And perhaps that’s the reason that so many pediatricians are still burning and not burned out.
A celebratory mood pervaded the last week of service for my ward team at the end of the academic year. As the attending, it was just another day, but it was hard not to be caught up in the general feeling of a milestone flying past. Like most days in a hospital, this one passed in a rhythm of alternating mundanity and crisis. Late in the afternoon, one of the residents called me to a bedside for help. Imagining that my diagnostic skills were urgently required, I took the stairs. The problem, as it turned out, was not strictly medical.
I could hear the yelling before I cleared the locked entry doors to the ward. It doesn’t really matter what the yelling was about, just that there is often yelling and there is always very little I can do about the root cause of it. As I stepped into the middle of the conflagration, I remembered the story an intern told me about the night earlier in the month when it fell to her to wheel the same patient’s intoxicated parent down to the emergency department. After sleeping it off, the parent was diagnosed with an “allergic reaction” and given a prescription for diphenhydramine. We all knew the diagnosis was fantasy, and yet we all went along with it because there was simply no help available for the root cause of the problem. State social services was already involved, and we had a “safety” plan in place for discharge. As meager as that may have been, we had done the best we could to balance the risk with the available resources… or so we told ourselves.
As a nation, we have chosen not to provide much of a social safety net for our citizens who suffer from addiction and/or mental illness and, most importantly, for those who’ve just not had a leg up on the economic ladder. As a hospital-based clinician, I know that people in distress lose their cool and yell sometimes. Ironically, they may yell most loudly at people who sincerely want to help, simply because others do not engage them. Medical schools don’t teach us how to handle the yelling, though many would say it is part of the hidden curriculum. One thing that distinguishes many pediatricians like myself is a willingness to listen to the yelling, to engage with it, and to try to help. Not surprisingly, our reputation around the hospital is that we skew a bit naive.
It is worth asking, though: Are pediatricians naive? Sure, we make funny faces. We clown. We baby-talk. Those things are largely true, but there are other true things about pediatricians. Chief among them is the fact that we come to know some of the worst things there are to know about human beings. Everybody knows people can be awful, but we know exactly how awful they are to defenseless children in precise detail. For instance, I’ve seen a 4-year-old who was repeatedly starved as a regular punishment. She was so hungry she ate her hair, which turned out to be lucky for her because it caused an intestinal blockage that led to the discovery of the abuse. I gave her an apple one day and she immediately hid it under her shirt. Where you see a scab on a child’s inner arm, I see a cigarette burn. I’ve resuscitated a baby whose parents dipped his pacifier in heroin to stop his crying—the remarkable part of the story being that it was heroin cooked in the hospital bathroom. And then there are the things that I cannot even bring myself to write down.
Carrying this knowledge hollows out a gap between pediatricians and the rest of the world. The divergence between our expectations of how a society should treat its children and the reality of our daily experience grinds away any naivete. The gap becomes a canyon for some of us. We live with the sense that nobody would believe the things we’ve seen, so we rarely talk about them. Years ago, I was testifying in a (for me) routine child-abuse case where this fact hit home. It is common for juries to disbelieve that a caregiver could do the things we allege. I say allege, but if you work as a pediatrician long enough, the space between allegation and fact narrows. It is simply pattern recognition to you—abuse happens so consistently that we accept it as a diagnostic category. The case in question was a submersion burn, which is an almost unmistakable pattern. The other piece of the story is that it happens to toddlers during toilet training as caregivers lose their self-control and punish children for soiling themselves. For me, simple pattern recognition; for the jury, simply unbelievable. We lost the case.
We are almost always losing the case as pediatricians. Spending on children makes up less than 10% of the federal budget, whereas spending on the elderly, including Social Security, Medicare, and the adult component of Medicaid, dominates that budget.1 Moreover, twice as many children as adults over age 65 are living in poverty in the United States. The Temporary Assistance for Needy Families program is often debated in this country and frequently criticized as wasteful. However, what is not debatable is that the allocated budget ($16.5 billion) hasn’t changed since 1996, resulting in a functional 40% decrease due to inflation.2 Life, for poor children, gets a little tougher every year.
After the resident and I wrapped up our day, we talked a little about how hard it is to witness some of the things you see in a children’s hospital. I could see the gap between her and the outside world widening right in front of me. In my weaker moments, I want to tell trainees like her to run while they can. I want to warn them that they don’t want to know so many of the things we’re going to teach them. I know how the story usually ends. I know that our country doesn’t promise children safety from social deprivation, hunger, or physical abuse. Instead, we’ve created the conditions for those things to occur at embarrassingly high rates, and we prosecute the unlucky after the fact. The children are simply collateral damage.
We stood at our patient’s bedside and tried to imagine a happy future. Even without his medical problems, he would likely need a major investment of resources in order to thrive. Where would those resources come from? I saw the hospital crib, metal bars on all sides and a thick plastic roof to prevent escape, as a metaphor. Later, I took the elevator down and overheard a snippet of conversation between two residents. One of them asked the other, “How do you know when you’ve burned out?” The other replied, “I don’t know, I guess when you’ve stopped burning.” Burnout is a hot topic in medicine, and some may assume the reasons are obvious: long hours and intellectually demanding work. In reality, those drivers may be less important than the repeated exposure to profound injustice inherent to the practice of medicine in our country.
As hospitalists, we address acute decompensation in our patients and send them back out into the world knowing there will soon be a next time. We also know that the next time might be preventable, if only … This cycle sometimes feels inexorable, but it can also prompt us to think about our obligation to work toward a more just society. We have to imagine a better future even as we struggle to believe it is on the way.
Most of our hospitals are trying to help. They have community-engagement programs, they purchase housing for homeless patients, they provide large amounts of uncompensated care and sometimes operate at a loss. Yet none of this addresses the root cause of the problem. Medicine, either in the form of an institution or a doctor, can’t replace a just society, but the truth of this fact does not mean we should not try.
Pediatrics has always been a field disposed toward advocacy. The origin of our largest professional organization in the United States was the intraprofessional conflict within the American Medical Association (AMA) over the Sheppard-Towner Act of 1921, one of this country’s first attempts to address the social determinants of health with legislation.3 The American Academy of Pediatrics was formed in 1930 after the AMA House of Delegates rebuked the Pediatric section for advocating for continuance of the act during the late 1920s.3 Perhaps what Pediatrics has to teach the rest of medicine is the necessity of making advocacy a part of our professional identity. And perhaps that’s the reason that so many pediatricians are still burning and not burned out.
1. Committee for a Responsible Federal Budget. Chartbook: budgeting for the next generation. October 11, 2018. Accessed February 2, 2021. http://www.crfb.org/papers/chartbook-budgeting-next-generation
2. Center on Budget and Policy Priorities. Policy basics: temporary assistance for needy families. Updated March 31, 2021. Accessed February 2, 2021. https://www.cbpp.org/research/family-income-support/temporary-assistance-for-needy-families
3. van Dyck PC. A history of child health equity legislation in the United States. Pediatrics. 2003;112(3 pt 2):727-730.
1. Committee for a Responsible Federal Budget. Chartbook: budgeting for the next generation. October 11, 2018. Accessed February 2, 2021. http://www.crfb.org/papers/chartbook-budgeting-next-generation
2. Center on Budget and Policy Priorities. Policy basics: temporary assistance for needy families. Updated March 31, 2021. Accessed February 2, 2021. https://www.cbpp.org/research/family-income-support/temporary-assistance-for-needy-families
3. van Dyck PC. A history of child health equity legislation in the United States. Pediatrics. 2003;112(3 pt 2):727-730.
© 2021 Society of Hospital Medicine
Ableism and Quality of Life During the Coronavirus Pandemic
Michael Hickson was a 46-year-old with a severe acquired disability whose COVID-19 course involved multisystem organ failure, a court-appointed guardian, hospice care, discontinued fluids and tube feeds, and eventual death. While some details have been released by the hospital,1 the recorded conversation between Mr. Hickson’s wife and a treating physician has been shared widely in disability communities.
Physician: “Right now, his quality of life—he doesn’t have much of one.”
Spouse: “What do you mean? Because he’s paralyzed with a brain injury, he doesn’t have a quality of life?”
Physician: “Correct.”
As physiatrists—physicians for patients with disabilities—we heard those words with heavy hearts and sunken stomachs. We can only imagine the anger, fear, and betrayal felt by our patients and other people with disabilities. Or perhaps they feel vindicated, that the quiet sentiments were finally said out loud. The recording expresses what people with disabilities long suspected: physicians don’t always value the lives of persons with disabilities the way they value the nondisabled. Research confirms this.2-4 The privilege of the nondisabled is often expressed as “I would never want to live like that.” People make personal judgments about how they would feel in somebody else’s situation. The usually quiet sentiment, this time said aloud and recorded—“He doesn’t have much [quality of life]”—showed how physicians’ judgments and biases can have a grave impact on others, especially people with disabilities.
Stereotypes, assumptions, and biases about the quality of life of people with disabilities are pervasive throughout healthcare, resulting in the devaluation and disparate treatment of people with disabilities.5 Healthcare providers are not exempt from deficit-based perspectives about people with disabilities,6 and discrimination ensues when healthcare providers make critical decisions from these perspectives.5 Ableist biases are underrecognized among physicians, who often misperceive quality of life for people with disabilities as poor, and fail to recognize that medical judgments can be biased accordingly.5 Consequently, necessary care can be withheld or withdrawn inappropriately.5 An estimated 25% of adults in the United States self-report disability; furthermore, disability is highly correlated with age as well as socioeconomic disadvantages.7 There is also extensive evidence that, as a population, people with disabilities experience healthcare disparities.8 Bias against people with disabilities serves to both restrict and reduce access to healthcare.9
The consequences of the pandemic have disproportionally affected the Black community, in terms of both economic and disease burden. Mr. Hickson, a Black man with disabilities who contracted COVID-19, personifies the intersection of race and disability and demands our concern and attention as physicians. We must appreciate the intrinsic worth of all people and populations, and seek to understand and respect their capacity to be active agents in their own lives, making their own decisions about their quality of life. The lives of Black people have value, but movements such as Black Lives Matter have been needed to highlight this truth, and there still needs to be meaningful action beyond rhetoric. The lives of people with disabilities have value. Healthcare systems and providers similarly need to acknowledge and act in a way that honors the intrinsic worth of people with disabilities.
People with disabilities face long-standing systemic barriers to equitable healthcare,10 as do Black people. During the pandemic, widespread alarm was raised about individual and structural racism in medicine, just as numerous disability rights organizations raised concerns that ableism would lead to undertreatment during the COVID-19 crisis, worsening existing healthcare inequities. In response, the US Department of Health and Human Services Office for Civil Rights in Action released a bulletin that stated, “In this time of emergency, the laudable goal of providing care quickly and efficiently must be guided by the fundamental principles of fairness, equality, and compassion that animate our civil rights laws. This is particularly true with respect to the treatment of persons with disabilities during medical emergencies as they possess the same dignity and worth as everyone else.”11 Using the presence of disabilities to limit or deny a person’s access to health care constitutes a clear violation of nondiscrimination law.12 Hospitals and providers should not limit the care offered to people with disabilities because of their disabilities or utilize quality-of-life judgments when deciding whether or not to provide care.12 While the hospital where Michael Hickson died released a statement claiming that they did not consider his disability status as part of their treatment decision-making, the recorded words of the physician suggest otherwise.
The impact of our words and actions, and not the underlying intent, most affects patients’, families’, and communities’ trust in the institution of medicine, represented by individual providers. The hospital statement indicated “it was not medically possible to save [Mr. Hickson].”1 The phrase “not medically possible” ties Mr. Hickson’s case to one of futility; however, the recording was about quality of life, not futility. The National Council on Disability found that subjective quality-of-life assumptions influence medical futility decisions.5 While the intent of withdrawing care from Mr. Hickson may have been related to futility, the consequences of this decision are far-reaching as people with disabilities have reason to question whether someone else’s judgment about the quality and worth of their life will lead to loss of their life.
Emphasizing perceived quality of life in making treatment decisions, as was implied for Mr. Hickson, is not a rare event and is one that is likely more common when health systems are stressed. Despite having policies and procedures to follow, biases creep into treatment decisions. In Oregon, for example, multiple cases of disability discrimination during the pandemic were brought to the attention of the state Senate by Disability Rights Oregon.13,14
Physicians and healthcare leaders must consider the unique needs of the disability community through health equity efforts in the COVID-19 response. There must be universally accessible approaches when planning and implementing a COVID response to increase impact and ensure systems are reaching all underserved communities. For healthcare institutions and hospitals, disability equity must be emphasized in the development and implementation of COVID-19 policies. The exclusion of people with disabilities from decisions about people with disabilities is problematic. This systemic exclusion means that ableist beliefs and policies are often unchallenged.15 Including people with disabilities on committees creating crisis standards of care protocols or other policies that may purposefully or unintentionally discriminate against people with disabilities is an important step.16 Representation matters, and people with disabilities must be central in the development of all health equity strategies during a pandemic. Furthermore, when system-level decision algorithms exist that value the life of people with disabilities, clinician biases are minimized, leading to more equitable care.
Examples of strategies include accessible formats for essential COVID-19-related communications, such as American Sign Language, large print, or screen reading technology. We must acknowledge that necessary universal mask policies can generate communication barriers for people reading lips. Hospitals and clinics have rapidly expanded virtual care and telemedicine to improve access. This has enhanced access to care for many people with mobility disability, but can exacerbate disparities for those with vision, hearing, communication, or intellectual disability. To better manage this issue, tailored strategies, such as live closed captioning or digital patient navigators, can be implemented.
Additionally, a person with a disability has the legal right to be accompanied by a designated essential support person. Hospital visitor policies must become less restrictive or enable exceptions when a person with a disability requires their personal care attendant. When it comes to outcome data, it is important to highlight the need for better collection of disability data that can be used to identify inequities as well as monitor outcomes of treatment.
As previously acknowledged, people without disabilities tend to have negative attitudes (both implicit and explicit) toward people with disabilities. These attitudes are re-enforced by societal-level institutions, policies, and structures that marginalize people with disabilities.17 We call on all physicians and those working in healthcare to question their biases. When you consider quality of life in your decision-making, ask yourself, “whose life?” Recognize and honor the personal, social, and cultural contexts that affect how an individual experiences “quality of life.” Unless the answer to “whose life?” is your own or that of your incapacitated dependent, it is not your place to make “quality of life” judgments. You can and should describe potential outcomes at the physiological or activity level, but leave quality-of-life decisions where they belong—with the individual or their desi
Social media activity in the disability community indicates that Mr. Hickson’s story is perceived, regardless of the provider’s and healthcare system’s intentions, to be yet another breach of trust by the medical system. It is not the burden of the oppressed and betrayed to repair a broken relationship. It is our obligation, as individual physicians and the greater medical institution, to provide care that demonstrates the value and worth of people with disabilities. An imperative step toward equitable care for people with disabilities is to recognize and address our ableist biases.
1. Anderson D. Statement on the death of Michael Hickson. St David’s HealthCare. July 2, 2020. Accessed July 6, 2020. https://stdavids.com/about/newsroom/statement-on-the-death-of-michael-hickson
2. Amundson R. Disability, ideology, and quality of life: a bias in biomedical ethics. In: Wasserman D, Bickenbach J, Wachbroit R, eds. Quality of Life and Human Difference: Genetic Testing, Health Care, and Disability. Cambridge University Press; 2005:101-124.
3. Dunn DS. Outsider privileges can lead to insider disadvantages: some psychosocial aspects of ableism. J Soc Issues. 2019;75(3):665-682. https://doi.org/10.1111/josi.12331
4. Kothari S. Clinical (mis)judgments of quality of life after disability. J Clin Ethics. 2004;15:300-307.
5. National Council on Disability. Medical futility and disability bias: part of the bioethics and disability series. November 19, 2019. Accessed March 31, 2021. https://www.ncd.gov/sites/default/files/NCD_Medical_Futility_Report_508.pdf
6. Iezzoni LI, Rao SR, Ressalam J, et al. Physicians’ perceptions of people with disability and their health care. Health Aff (Millwood). 2021;40(2):297-306. https://doi.org/10.1377/hlthaff.2020.01452
7. Okoro CA, Hollis ND, Cyrus AC, Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(32):882-887. https://doi.org/10.15585/mmwr.mm6732a3
8. Meade MA, Mahmoudi E, Lee SY. The intersection of disability and healthcare disparities: a conceptual framework. Disabil Rehabil. 2015;37(7):632-641. https://doi.org/10.3109/09638288.2014.938176
9. Andrews EE, Ayers KB, Brown KS, Dunn DS, Pilarski CR. No body is expendable: medical rationing and disability justice during the COVID-19 pandemic. Am Psychol. Published online July 23, 2020. https://doi.org/10.1037/amp0000709
10. Savin K, Guidry-Grimes L. Confronting disability discrimination during the pandemic. The Hastings Center. April 2, 2020. Accessed March 31, 2021. https://www.thehastingscenter.org/confronting-disability-discrimination-during-the-pandemic/
11. Health and Human Services Office for Civil Rights in Action. Bulletin: civil rights, HIPAA, and the coronavirus disease 2019. March 28, 2020. Accessed March 31, 2021. https://www.hhs.gov/sites/default/files/ocr-bulletin-3-28-20.pdf
12. Preventing discrimination in the treatment of COVID-19 patients: the illegality of medical rationing on the basis of disability. Disability Rights Education & Defense Fund. March 25, 2020. Accessed March 31, 2021. https://dredf.org/wp-content/uploads/2020/03/DREDF-Policy-Statement-on-COVID-19-and-Medical-Rationing-3-25-2020.pdf
13. Oregon hospitals told not to withhold care because of a person’s disability. Transcript. Morning Edition. National Public Radio. December 21, 2020. Accessed March 31, 2021. https://www.npr.org/2020/12/21/948697808/oregon-hospitals-told-not-to-withhold-care-because-of-a-persons-disability
14. As hospitals fear being overwhelmed by COVID-19, do the disabled get the same access? Transcript. Morning Edition. National Public Radio. December 14, 2020. Accessed March 31, 2021. https://www.npr.org/2020/12/14/945056176/as-hospitals-fear-being-overwhelmed-by-covid-19-do-the-disabled-get-the-same-acc
15. Lund EM, Forber-Pratt AJ, Wilson C, Mona LR. The COVID-19 pandemic, stress, and trauma in the disability community: a call to action. Rehabil Psychol. 2020;65(4):313-322. https://doi.org/10.1037/rep0000368
16. Auriemma CL, Molinero AM, Houtrow AJ, Persad G, White DB, Halpern SD. Eliminating categorical exclusion criteria in crisis standards of care frameworks. Am J Bioeth. 2020;20(7):28-36. http://doi.org/10.1080/15265161.2020.1764141
17. Bogart KR, Dunn DS. Ableism special issue introduction. J Soc Issues. 2019;75(3):650-664. https://doi.org/10.1111/josi.12354
Michael Hickson was a 46-year-old with a severe acquired disability whose COVID-19 course involved multisystem organ failure, a court-appointed guardian, hospice care, discontinued fluids and tube feeds, and eventual death. While some details have been released by the hospital,1 the recorded conversation between Mr. Hickson’s wife and a treating physician has been shared widely in disability communities.
Physician: “Right now, his quality of life—he doesn’t have much of one.”
Spouse: “What do you mean? Because he’s paralyzed with a brain injury, he doesn’t have a quality of life?”
Physician: “Correct.”
As physiatrists—physicians for patients with disabilities—we heard those words with heavy hearts and sunken stomachs. We can only imagine the anger, fear, and betrayal felt by our patients and other people with disabilities. Or perhaps they feel vindicated, that the quiet sentiments were finally said out loud. The recording expresses what people with disabilities long suspected: physicians don’t always value the lives of persons with disabilities the way they value the nondisabled. Research confirms this.2-4 The privilege of the nondisabled is often expressed as “I would never want to live like that.” People make personal judgments about how they would feel in somebody else’s situation. The usually quiet sentiment, this time said aloud and recorded—“He doesn’t have much [quality of life]”—showed how physicians’ judgments and biases can have a grave impact on others, especially people with disabilities.
Stereotypes, assumptions, and biases about the quality of life of people with disabilities are pervasive throughout healthcare, resulting in the devaluation and disparate treatment of people with disabilities.5 Healthcare providers are not exempt from deficit-based perspectives about people with disabilities,6 and discrimination ensues when healthcare providers make critical decisions from these perspectives.5 Ableist biases are underrecognized among physicians, who often misperceive quality of life for people with disabilities as poor, and fail to recognize that medical judgments can be biased accordingly.5 Consequently, necessary care can be withheld or withdrawn inappropriately.5 An estimated 25% of adults in the United States self-report disability; furthermore, disability is highly correlated with age as well as socioeconomic disadvantages.7 There is also extensive evidence that, as a population, people with disabilities experience healthcare disparities.8 Bias against people with disabilities serves to both restrict and reduce access to healthcare.9
The consequences of the pandemic have disproportionally affected the Black community, in terms of both economic and disease burden. Mr. Hickson, a Black man with disabilities who contracted COVID-19, personifies the intersection of race and disability and demands our concern and attention as physicians. We must appreciate the intrinsic worth of all people and populations, and seek to understand and respect their capacity to be active agents in their own lives, making their own decisions about their quality of life. The lives of Black people have value, but movements such as Black Lives Matter have been needed to highlight this truth, and there still needs to be meaningful action beyond rhetoric. The lives of people with disabilities have value. Healthcare systems and providers similarly need to acknowledge and act in a way that honors the intrinsic worth of people with disabilities.
People with disabilities face long-standing systemic barriers to equitable healthcare,10 as do Black people. During the pandemic, widespread alarm was raised about individual and structural racism in medicine, just as numerous disability rights organizations raised concerns that ableism would lead to undertreatment during the COVID-19 crisis, worsening existing healthcare inequities. In response, the US Department of Health and Human Services Office for Civil Rights in Action released a bulletin that stated, “In this time of emergency, the laudable goal of providing care quickly and efficiently must be guided by the fundamental principles of fairness, equality, and compassion that animate our civil rights laws. This is particularly true with respect to the treatment of persons with disabilities during medical emergencies as they possess the same dignity and worth as everyone else.”11 Using the presence of disabilities to limit or deny a person’s access to health care constitutes a clear violation of nondiscrimination law.12 Hospitals and providers should not limit the care offered to people with disabilities because of their disabilities or utilize quality-of-life judgments when deciding whether or not to provide care.12 While the hospital where Michael Hickson died released a statement claiming that they did not consider his disability status as part of their treatment decision-making, the recorded words of the physician suggest otherwise.
The impact of our words and actions, and not the underlying intent, most affects patients’, families’, and communities’ trust in the institution of medicine, represented by individual providers. The hospital statement indicated “it was not medically possible to save [Mr. Hickson].”1 The phrase “not medically possible” ties Mr. Hickson’s case to one of futility; however, the recording was about quality of life, not futility. The National Council on Disability found that subjective quality-of-life assumptions influence medical futility decisions.5 While the intent of withdrawing care from Mr. Hickson may have been related to futility, the consequences of this decision are far-reaching as people with disabilities have reason to question whether someone else’s judgment about the quality and worth of their life will lead to loss of their life.
Emphasizing perceived quality of life in making treatment decisions, as was implied for Mr. Hickson, is not a rare event and is one that is likely more common when health systems are stressed. Despite having policies and procedures to follow, biases creep into treatment decisions. In Oregon, for example, multiple cases of disability discrimination during the pandemic were brought to the attention of the state Senate by Disability Rights Oregon.13,14
Physicians and healthcare leaders must consider the unique needs of the disability community through health equity efforts in the COVID-19 response. There must be universally accessible approaches when planning and implementing a COVID response to increase impact and ensure systems are reaching all underserved communities. For healthcare institutions and hospitals, disability equity must be emphasized in the development and implementation of COVID-19 policies. The exclusion of people with disabilities from decisions about people with disabilities is problematic. This systemic exclusion means that ableist beliefs and policies are often unchallenged.15 Including people with disabilities on committees creating crisis standards of care protocols or other policies that may purposefully or unintentionally discriminate against people with disabilities is an important step.16 Representation matters, and people with disabilities must be central in the development of all health equity strategies during a pandemic. Furthermore, when system-level decision algorithms exist that value the life of people with disabilities, clinician biases are minimized, leading to more equitable care.
Examples of strategies include accessible formats for essential COVID-19-related communications, such as American Sign Language, large print, or screen reading technology. We must acknowledge that necessary universal mask policies can generate communication barriers for people reading lips. Hospitals and clinics have rapidly expanded virtual care and telemedicine to improve access. This has enhanced access to care for many people with mobility disability, but can exacerbate disparities for those with vision, hearing, communication, or intellectual disability. To better manage this issue, tailored strategies, such as live closed captioning or digital patient navigators, can be implemented.
Additionally, a person with a disability has the legal right to be accompanied by a designated essential support person. Hospital visitor policies must become less restrictive or enable exceptions when a person with a disability requires their personal care attendant. When it comes to outcome data, it is important to highlight the need for better collection of disability data that can be used to identify inequities as well as monitor outcomes of treatment.
As previously acknowledged, people without disabilities tend to have negative attitudes (both implicit and explicit) toward people with disabilities. These attitudes are re-enforced by societal-level institutions, policies, and structures that marginalize people with disabilities.17 We call on all physicians and those working in healthcare to question their biases. When you consider quality of life in your decision-making, ask yourself, “whose life?” Recognize and honor the personal, social, and cultural contexts that affect how an individual experiences “quality of life.” Unless the answer to “whose life?” is your own or that of your incapacitated dependent, it is not your place to make “quality of life” judgments. You can and should describe potential outcomes at the physiological or activity level, but leave quality-of-life decisions where they belong—with the individual or their desi
Social media activity in the disability community indicates that Mr. Hickson’s story is perceived, regardless of the provider’s and healthcare system’s intentions, to be yet another breach of trust by the medical system. It is not the burden of the oppressed and betrayed to repair a broken relationship. It is our obligation, as individual physicians and the greater medical institution, to provide care that demonstrates the value and worth of people with disabilities. An imperative step toward equitable care for people with disabilities is to recognize and address our ableist biases.
Michael Hickson was a 46-year-old with a severe acquired disability whose COVID-19 course involved multisystem organ failure, a court-appointed guardian, hospice care, discontinued fluids and tube feeds, and eventual death. While some details have been released by the hospital,1 the recorded conversation between Mr. Hickson’s wife and a treating physician has been shared widely in disability communities.
Physician: “Right now, his quality of life—he doesn’t have much of one.”
Spouse: “What do you mean? Because he’s paralyzed with a brain injury, he doesn’t have a quality of life?”
Physician: “Correct.”
As physiatrists—physicians for patients with disabilities—we heard those words with heavy hearts and sunken stomachs. We can only imagine the anger, fear, and betrayal felt by our patients and other people with disabilities. Or perhaps they feel vindicated, that the quiet sentiments were finally said out loud. The recording expresses what people with disabilities long suspected: physicians don’t always value the lives of persons with disabilities the way they value the nondisabled. Research confirms this.2-4 The privilege of the nondisabled is often expressed as “I would never want to live like that.” People make personal judgments about how they would feel in somebody else’s situation. The usually quiet sentiment, this time said aloud and recorded—“He doesn’t have much [quality of life]”—showed how physicians’ judgments and biases can have a grave impact on others, especially people with disabilities.
Stereotypes, assumptions, and biases about the quality of life of people with disabilities are pervasive throughout healthcare, resulting in the devaluation and disparate treatment of people with disabilities.5 Healthcare providers are not exempt from deficit-based perspectives about people with disabilities,6 and discrimination ensues when healthcare providers make critical decisions from these perspectives.5 Ableist biases are underrecognized among physicians, who often misperceive quality of life for people with disabilities as poor, and fail to recognize that medical judgments can be biased accordingly.5 Consequently, necessary care can be withheld or withdrawn inappropriately.5 An estimated 25% of adults in the United States self-report disability; furthermore, disability is highly correlated with age as well as socioeconomic disadvantages.7 There is also extensive evidence that, as a population, people with disabilities experience healthcare disparities.8 Bias against people with disabilities serves to both restrict and reduce access to healthcare.9
The consequences of the pandemic have disproportionally affected the Black community, in terms of both economic and disease burden. Mr. Hickson, a Black man with disabilities who contracted COVID-19, personifies the intersection of race and disability and demands our concern and attention as physicians. We must appreciate the intrinsic worth of all people and populations, and seek to understand and respect their capacity to be active agents in their own lives, making their own decisions about their quality of life. The lives of Black people have value, but movements such as Black Lives Matter have been needed to highlight this truth, and there still needs to be meaningful action beyond rhetoric. The lives of people with disabilities have value. Healthcare systems and providers similarly need to acknowledge and act in a way that honors the intrinsic worth of people with disabilities.
People with disabilities face long-standing systemic barriers to equitable healthcare,10 as do Black people. During the pandemic, widespread alarm was raised about individual and structural racism in medicine, just as numerous disability rights organizations raised concerns that ableism would lead to undertreatment during the COVID-19 crisis, worsening existing healthcare inequities. In response, the US Department of Health and Human Services Office for Civil Rights in Action released a bulletin that stated, “In this time of emergency, the laudable goal of providing care quickly and efficiently must be guided by the fundamental principles of fairness, equality, and compassion that animate our civil rights laws. This is particularly true with respect to the treatment of persons with disabilities during medical emergencies as they possess the same dignity and worth as everyone else.”11 Using the presence of disabilities to limit or deny a person’s access to health care constitutes a clear violation of nondiscrimination law.12 Hospitals and providers should not limit the care offered to people with disabilities because of their disabilities or utilize quality-of-life judgments when deciding whether or not to provide care.12 While the hospital where Michael Hickson died released a statement claiming that they did not consider his disability status as part of their treatment decision-making, the recorded words of the physician suggest otherwise.
The impact of our words and actions, and not the underlying intent, most affects patients’, families’, and communities’ trust in the institution of medicine, represented by individual providers. The hospital statement indicated “it was not medically possible to save [Mr. Hickson].”1 The phrase “not medically possible” ties Mr. Hickson’s case to one of futility; however, the recording was about quality of life, not futility. The National Council on Disability found that subjective quality-of-life assumptions influence medical futility decisions.5 While the intent of withdrawing care from Mr. Hickson may have been related to futility, the consequences of this decision are far-reaching as people with disabilities have reason to question whether someone else’s judgment about the quality and worth of their life will lead to loss of their life.
Emphasizing perceived quality of life in making treatment decisions, as was implied for Mr. Hickson, is not a rare event and is one that is likely more common when health systems are stressed. Despite having policies and procedures to follow, biases creep into treatment decisions. In Oregon, for example, multiple cases of disability discrimination during the pandemic were brought to the attention of the state Senate by Disability Rights Oregon.13,14
Physicians and healthcare leaders must consider the unique needs of the disability community through health equity efforts in the COVID-19 response. There must be universally accessible approaches when planning and implementing a COVID response to increase impact and ensure systems are reaching all underserved communities. For healthcare institutions and hospitals, disability equity must be emphasized in the development and implementation of COVID-19 policies. The exclusion of people with disabilities from decisions about people with disabilities is problematic. This systemic exclusion means that ableist beliefs and policies are often unchallenged.15 Including people with disabilities on committees creating crisis standards of care protocols or other policies that may purposefully or unintentionally discriminate against people with disabilities is an important step.16 Representation matters, and people with disabilities must be central in the development of all health equity strategies during a pandemic. Furthermore, when system-level decision algorithms exist that value the life of people with disabilities, clinician biases are minimized, leading to more equitable care.
Examples of strategies include accessible formats for essential COVID-19-related communications, such as American Sign Language, large print, or screen reading technology. We must acknowledge that necessary universal mask policies can generate communication barriers for people reading lips. Hospitals and clinics have rapidly expanded virtual care and telemedicine to improve access. This has enhanced access to care for many people with mobility disability, but can exacerbate disparities for those with vision, hearing, communication, or intellectual disability. To better manage this issue, tailored strategies, such as live closed captioning or digital patient navigators, can be implemented.
Additionally, a person with a disability has the legal right to be accompanied by a designated essential support person. Hospital visitor policies must become less restrictive or enable exceptions when a person with a disability requires their personal care attendant. When it comes to outcome data, it is important to highlight the need for better collection of disability data that can be used to identify inequities as well as monitor outcomes of treatment.
As previously acknowledged, people without disabilities tend to have negative attitudes (both implicit and explicit) toward people with disabilities. These attitudes are re-enforced by societal-level institutions, policies, and structures that marginalize people with disabilities.17 We call on all physicians and those working in healthcare to question their biases. When you consider quality of life in your decision-making, ask yourself, “whose life?” Recognize and honor the personal, social, and cultural contexts that affect how an individual experiences “quality of life.” Unless the answer to “whose life?” is your own or that of your incapacitated dependent, it is not your place to make “quality of life” judgments. You can and should describe potential outcomes at the physiological or activity level, but leave quality-of-life decisions where they belong—with the individual or their desi
Social media activity in the disability community indicates that Mr. Hickson’s story is perceived, regardless of the provider’s and healthcare system’s intentions, to be yet another breach of trust by the medical system. It is not the burden of the oppressed and betrayed to repair a broken relationship. It is our obligation, as individual physicians and the greater medical institution, to provide care that demonstrates the value and worth of people with disabilities. An imperative step toward equitable care for people with disabilities is to recognize and address our ableist biases.
1. Anderson D. Statement on the death of Michael Hickson. St David’s HealthCare. July 2, 2020. Accessed July 6, 2020. https://stdavids.com/about/newsroom/statement-on-the-death-of-michael-hickson
2. Amundson R. Disability, ideology, and quality of life: a bias in biomedical ethics. In: Wasserman D, Bickenbach J, Wachbroit R, eds. Quality of Life and Human Difference: Genetic Testing, Health Care, and Disability. Cambridge University Press; 2005:101-124.
3. Dunn DS. Outsider privileges can lead to insider disadvantages: some psychosocial aspects of ableism. J Soc Issues. 2019;75(3):665-682. https://doi.org/10.1111/josi.12331
4. Kothari S. Clinical (mis)judgments of quality of life after disability. J Clin Ethics. 2004;15:300-307.
5. National Council on Disability. Medical futility and disability bias: part of the bioethics and disability series. November 19, 2019. Accessed March 31, 2021. https://www.ncd.gov/sites/default/files/NCD_Medical_Futility_Report_508.pdf
6. Iezzoni LI, Rao SR, Ressalam J, et al. Physicians’ perceptions of people with disability and their health care. Health Aff (Millwood). 2021;40(2):297-306. https://doi.org/10.1377/hlthaff.2020.01452
7. Okoro CA, Hollis ND, Cyrus AC, Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(32):882-887. https://doi.org/10.15585/mmwr.mm6732a3
8. Meade MA, Mahmoudi E, Lee SY. The intersection of disability and healthcare disparities: a conceptual framework. Disabil Rehabil. 2015;37(7):632-641. https://doi.org/10.3109/09638288.2014.938176
9. Andrews EE, Ayers KB, Brown KS, Dunn DS, Pilarski CR. No body is expendable: medical rationing and disability justice during the COVID-19 pandemic. Am Psychol. Published online July 23, 2020. https://doi.org/10.1037/amp0000709
10. Savin K, Guidry-Grimes L. Confronting disability discrimination during the pandemic. The Hastings Center. April 2, 2020. Accessed March 31, 2021. https://www.thehastingscenter.org/confronting-disability-discrimination-during-the-pandemic/
11. Health and Human Services Office for Civil Rights in Action. Bulletin: civil rights, HIPAA, and the coronavirus disease 2019. March 28, 2020. Accessed March 31, 2021. https://www.hhs.gov/sites/default/files/ocr-bulletin-3-28-20.pdf
12. Preventing discrimination in the treatment of COVID-19 patients: the illegality of medical rationing on the basis of disability. Disability Rights Education & Defense Fund. March 25, 2020. Accessed March 31, 2021. https://dredf.org/wp-content/uploads/2020/03/DREDF-Policy-Statement-on-COVID-19-and-Medical-Rationing-3-25-2020.pdf
13. Oregon hospitals told not to withhold care because of a person’s disability. Transcript. Morning Edition. National Public Radio. December 21, 2020. Accessed March 31, 2021. https://www.npr.org/2020/12/21/948697808/oregon-hospitals-told-not-to-withhold-care-because-of-a-persons-disability
14. As hospitals fear being overwhelmed by COVID-19, do the disabled get the same access? Transcript. Morning Edition. National Public Radio. December 14, 2020. Accessed March 31, 2021. https://www.npr.org/2020/12/14/945056176/as-hospitals-fear-being-overwhelmed-by-covid-19-do-the-disabled-get-the-same-acc
15. Lund EM, Forber-Pratt AJ, Wilson C, Mona LR. The COVID-19 pandemic, stress, and trauma in the disability community: a call to action. Rehabil Psychol. 2020;65(4):313-322. https://doi.org/10.1037/rep0000368
16. Auriemma CL, Molinero AM, Houtrow AJ, Persad G, White DB, Halpern SD. Eliminating categorical exclusion criteria in crisis standards of care frameworks. Am J Bioeth. 2020;20(7):28-36. http://doi.org/10.1080/15265161.2020.1764141
17. Bogart KR, Dunn DS. Ableism special issue introduction. J Soc Issues. 2019;75(3):650-664. https://doi.org/10.1111/josi.12354
1. Anderson D. Statement on the death of Michael Hickson. St David’s HealthCare. July 2, 2020. Accessed July 6, 2020. https://stdavids.com/about/newsroom/statement-on-the-death-of-michael-hickson
2. Amundson R. Disability, ideology, and quality of life: a bias in biomedical ethics. In: Wasserman D, Bickenbach J, Wachbroit R, eds. Quality of Life and Human Difference: Genetic Testing, Health Care, and Disability. Cambridge University Press; 2005:101-124.
3. Dunn DS. Outsider privileges can lead to insider disadvantages: some psychosocial aspects of ableism. J Soc Issues. 2019;75(3):665-682. https://doi.org/10.1111/josi.12331
4. Kothari S. Clinical (mis)judgments of quality of life after disability. J Clin Ethics. 2004;15:300-307.
5. National Council on Disability. Medical futility and disability bias: part of the bioethics and disability series. November 19, 2019. Accessed March 31, 2021. https://www.ncd.gov/sites/default/files/NCD_Medical_Futility_Report_508.pdf
6. Iezzoni LI, Rao SR, Ressalam J, et al. Physicians’ perceptions of people with disability and their health care. Health Aff (Millwood). 2021;40(2):297-306. https://doi.org/10.1377/hlthaff.2020.01452
7. Okoro CA, Hollis ND, Cyrus AC, Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(32):882-887. https://doi.org/10.15585/mmwr.mm6732a3
8. Meade MA, Mahmoudi E, Lee SY. The intersection of disability and healthcare disparities: a conceptual framework. Disabil Rehabil. 2015;37(7):632-641. https://doi.org/10.3109/09638288.2014.938176
9. Andrews EE, Ayers KB, Brown KS, Dunn DS, Pilarski CR. No body is expendable: medical rationing and disability justice during the COVID-19 pandemic. Am Psychol. Published online July 23, 2020. https://doi.org/10.1037/amp0000709
10. Savin K, Guidry-Grimes L. Confronting disability discrimination during the pandemic. The Hastings Center. April 2, 2020. Accessed March 31, 2021. https://www.thehastingscenter.org/confronting-disability-discrimination-during-the-pandemic/
11. Health and Human Services Office for Civil Rights in Action. Bulletin: civil rights, HIPAA, and the coronavirus disease 2019. March 28, 2020. Accessed March 31, 2021. https://www.hhs.gov/sites/default/files/ocr-bulletin-3-28-20.pdf
12. Preventing discrimination in the treatment of COVID-19 patients: the illegality of medical rationing on the basis of disability. Disability Rights Education & Defense Fund. March 25, 2020. Accessed March 31, 2021. https://dredf.org/wp-content/uploads/2020/03/DREDF-Policy-Statement-on-COVID-19-and-Medical-Rationing-3-25-2020.pdf
13. Oregon hospitals told not to withhold care because of a person’s disability. Transcript. Morning Edition. National Public Radio. December 21, 2020. Accessed March 31, 2021. https://www.npr.org/2020/12/21/948697808/oregon-hospitals-told-not-to-withhold-care-because-of-a-persons-disability
14. As hospitals fear being overwhelmed by COVID-19, do the disabled get the same access? Transcript. Morning Edition. National Public Radio. December 14, 2020. Accessed March 31, 2021. https://www.npr.org/2020/12/14/945056176/as-hospitals-fear-being-overwhelmed-by-covid-19-do-the-disabled-get-the-same-acc
15. Lund EM, Forber-Pratt AJ, Wilson C, Mona LR. The COVID-19 pandemic, stress, and trauma in the disability community: a call to action. Rehabil Psychol. 2020;65(4):313-322. https://doi.org/10.1037/rep0000368
16. Auriemma CL, Molinero AM, Houtrow AJ, Persad G, White DB, Halpern SD. Eliminating categorical exclusion criteria in crisis standards of care frameworks. Am J Bioeth. 2020;20(7):28-36. http://doi.org/10.1080/15265161.2020.1764141
17. Bogart KR, Dunn DS. Ableism special issue introduction. J Soc Issues. 2019;75(3):650-664. https://doi.org/10.1111/josi.12354
© 2021 Society of Hospital Medicine
Supporting Hospitals During a New Wave of COVID-19
The COVID-19 pandemic has put an extraordinary strain on US hospitals.1 In spring 2020, many hospitals had to quickly adapt to treat a surge of patients, and many more had to prepare for a potential surge. Creating reserve capacity meant halting outpatient care and elective surgeries, repurposing inpatient units, and increasing critical care staffing. Hospitals again face these difficult decisions, as COVID-19 resurges and variants of SARS-CoV-2 increasingly circulate, with large financial losses projected for 2021.2 Some large hospital systems may have the financial reserves to weather this storm, but the precarious situation facing others likely requires policy action.
Hospitals’ financial stress emanates from multiple quarters. First, revenue from elective inpatient procedures and outpatient care dropped dramatically, has not fully rebounded,3,4 and is not fully offset by revenue from COVID-19 care. Second, high unemployment may force up to 20% of commercially insured Americans into lower-reimbursing public insurance or the ranks of the uninsured, generating a projected $95 billion annual loss for hospitals.5 Third, under the current payment system, the costs of preparing for a pandemic are not directly reimbursed. Yet—whether or not they ultimately experienced a large COVID-19 caseload—hospitals’ surge preparation has involved purchasing vast quantities of protective personal equipment (PPE) and other supplies and equipment, hiring additional staff, building SARS-CoV-2 testing capacity, and expanding occupational health services. Many expenses persist as “the new normal”: admissions now require SARS-CoV-2 testing, additional staff and PPE, and often, a private room. Physical distancing requirements mean hospitals’ capacity—and thus, revenue—will remain reduced.
Private insurers, by and large, are not volunteering to cover these increased costs, and it is difficult for hospitals to pass them along. Payment terms in many contracts (eg, for Medicare) are not modifiable; even where they are, renegotiating takes time. To date, federal relief payments from the CARES Act do not fully reimburse COVID-19 losses—a particular problem for smaller and safety-net hospitals without large reserves.
This situation raises ethical concerns. For example, it is ethically relevant that COVID-19 resurgence and hospitalizations are linked to states’ decisions to reopen quickly to ease economic burdens on businesses and workers. One result has been to shift some of the pandemic’s economic burden to the healthcare sector. From a fairness perspective, there should be limits on the losses hospitals are forced to shoulder to maintain COVID-19 preparedness and services. Even if hospitals have reserves, spending them threatens funding for other essential activities, such as capital investment.
The current situation is also fraught with perverse incentives that could jeopardize safe care. With elective care remaining at risk of being reduced,6 pressure intensifies to deliver as many services as possible as quickly as possible, which may not align with patients’ best interests. Across hospitals that need to maximize volume to survive, a push to keep elective services open may emerge, even as COVID-19 prevalence may favor a shutdown. Hospitals with a heavy COVID-19 caseload may have greater difficulty reopening than competitors with lower caseloads, potentially impacting quality if patients seek elective care at lower-volume centers or in ways that disrupt continuity of care.
Ethical dilemmas are also raised by the delicate balancing of interests that hospitals have been engaging in among patient groups. How should they balance the needs of COVID-19 patients against potential harms to others who must delay care?
It is wrong to ask hospitals to make such choices when policy solutions are available. With the resurgence of COVID-19 must come a fresh, sustained program of federal financial relief for hospitals. While direct government support is the swiftest path, consideration should be given to the role of private insurers, which have benefited economically from the widespread deferment and forgoing of elective care. Voluntary or mandatory investments by insurers in helping hospitals survive the pandemic and weather the new normal are consonant with insurers’ commitment to providing their members access to high-quality healthcare.
The 200-page National Strategy document released by the Biden administration on January 21, 2021, promises some important assistance to hospitals.7 It includes plans to accelerate the production of PPE and other essential supplies using the Defense Production Act and other federal authorities, to rationalize nationwide distribution of these supplies and take steps to prevent price gouging, and to deploy federal personnel and assets to help surge critical-care personnel.
These steps, if fully funded and implemented, would bring welcome respite from some of the most vexing problems hospitals have encountered during COVID-19 surges. Yet, plans for direct financial relief for hospitals are strikingly absent from the National Strategy. Nor does the recently passed $1.9 trillion federal stimulus package provide dedicated funds for hospitals, though some funds earmarked for vaccine delivery may land at hospitals. These are consequential omissions in otherwise comprehensive, thoughtful pandemic response plans.
Future legislation should include an immediate revenue infusion to reimburse hospitals’ COVID-19 preparations and lost volume and a firm commitment of ongoing financial support for preparedness through the end of the pandemic at a level sufficient to offset COVID-19–related losses. Experience with the CARES Act also suggests specific lessons for statutory design: support for hospitals should be allocated based on actual COVID-19–related burden for preparation and care, unlike CARES Act grants that were allocated based on hospitals’ past revenue and Medicare billing. This resulted in some large payments to relatively well-off hospitals and scant support for others (eg, rural or safety-net hospitals) with substantial COVID-19–related losses, a misstep that should not be repeated.
Hospitals are an integral part of the nation’s public health system. In the context of a pandemic, they should not be forced to serve as a backstop for shortcomings in other parts of the system without assistance. They, and their mission during the pandemic, are too important to fail.
1. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
2. Coleman-Lochner L. Hospitals plead for bailout in face of runaway pandemic bills. February 26, 2021. Accessed March 25, 2021. https://www.bloomberg.com/news/articles/2021-02-26/hospitals-plead-for-bailout-in-face-of-runaway-pandemic-bills
3. American Hospital Association. Hospitals and health systems continue to face unprecedented financial challenges due to COVID-19. June 2020. Accessed February 5. 2021. https://www.aha.org/system/files/media/file/2020/06/aha-covid19-financial-impact-report.pdf
4. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood). 2020;39(11):2010-2017. https://doi.org/10.1377/hlthaff.2020.00980
5. Teasdale B, Schulman KA. Are U.S. hospitals still “recession-proof”? N Engl J Med. 2020;383(13):e82. https://doi.org/10.1056/NEJMp2018846
6. Meredith JW, High KP, Freischlag JA. Preserving elective surgeries in the COVID-19 pandemic and the future. JAMA. 2020;324(17):1725-1726. https://doi.org/10.1001/jama.2020.19594
7. Biden JR. National strategy for the COVID-19 response and pandemic preparedness. Bloomberg. January 2021. Accessed February 8, 2021. https://www.whitehouse.gov/wp-content/uploads/2021/01/National-Strategy-for-the-COVID-19-Response-and-Pandemic-Preparedness.pdf
The COVID-19 pandemic has put an extraordinary strain on US hospitals.1 In spring 2020, many hospitals had to quickly adapt to treat a surge of patients, and many more had to prepare for a potential surge. Creating reserve capacity meant halting outpatient care and elective surgeries, repurposing inpatient units, and increasing critical care staffing. Hospitals again face these difficult decisions, as COVID-19 resurges and variants of SARS-CoV-2 increasingly circulate, with large financial losses projected for 2021.2 Some large hospital systems may have the financial reserves to weather this storm, but the precarious situation facing others likely requires policy action.
Hospitals’ financial stress emanates from multiple quarters. First, revenue from elective inpatient procedures and outpatient care dropped dramatically, has not fully rebounded,3,4 and is not fully offset by revenue from COVID-19 care. Second, high unemployment may force up to 20% of commercially insured Americans into lower-reimbursing public insurance or the ranks of the uninsured, generating a projected $95 billion annual loss for hospitals.5 Third, under the current payment system, the costs of preparing for a pandemic are not directly reimbursed. Yet—whether or not they ultimately experienced a large COVID-19 caseload—hospitals’ surge preparation has involved purchasing vast quantities of protective personal equipment (PPE) and other supplies and equipment, hiring additional staff, building SARS-CoV-2 testing capacity, and expanding occupational health services. Many expenses persist as “the new normal”: admissions now require SARS-CoV-2 testing, additional staff and PPE, and often, a private room. Physical distancing requirements mean hospitals’ capacity—and thus, revenue—will remain reduced.
Private insurers, by and large, are not volunteering to cover these increased costs, and it is difficult for hospitals to pass them along. Payment terms in many contracts (eg, for Medicare) are not modifiable; even where they are, renegotiating takes time. To date, federal relief payments from the CARES Act do not fully reimburse COVID-19 losses—a particular problem for smaller and safety-net hospitals without large reserves.
This situation raises ethical concerns. For example, it is ethically relevant that COVID-19 resurgence and hospitalizations are linked to states’ decisions to reopen quickly to ease economic burdens on businesses and workers. One result has been to shift some of the pandemic’s economic burden to the healthcare sector. From a fairness perspective, there should be limits on the losses hospitals are forced to shoulder to maintain COVID-19 preparedness and services. Even if hospitals have reserves, spending them threatens funding for other essential activities, such as capital investment.
The current situation is also fraught with perverse incentives that could jeopardize safe care. With elective care remaining at risk of being reduced,6 pressure intensifies to deliver as many services as possible as quickly as possible, which may not align with patients’ best interests. Across hospitals that need to maximize volume to survive, a push to keep elective services open may emerge, even as COVID-19 prevalence may favor a shutdown. Hospitals with a heavy COVID-19 caseload may have greater difficulty reopening than competitors with lower caseloads, potentially impacting quality if patients seek elective care at lower-volume centers or in ways that disrupt continuity of care.
Ethical dilemmas are also raised by the delicate balancing of interests that hospitals have been engaging in among patient groups. How should they balance the needs of COVID-19 patients against potential harms to others who must delay care?
It is wrong to ask hospitals to make such choices when policy solutions are available. With the resurgence of COVID-19 must come a fresh, sustained program of federal financial relief for hospitals. While direct government support is the swiftest path, consideration should be given to the role of private insurers, which have benefited economically from the widespread deferment and forgoing of elective care. Voluntary or mandatory investments by insurers in helping hospitals survive the pandemic and weather the new normal are consonant with insurers’ commitment to providing their members access to high-quality healthcare.
The 200-page National Strategy document released by the Biden administration on January 21, 2021, promises some important assistance to hospitals.7 It includes plans to accelerate the production of PPE and other essential supplies using the Defense Production Act and other federal authorities, to rationalize nationwide distribution of these supplies and take steps to prevent price gouging, and to deploy federal personnel and assets to help surge critical-care personnel.
These steps, if fully funded and implemented, would bring welcome respite from some of the most vexing problems hospitals have encountered during COVID-19 surges. Yet, plans for direct financial relief for hospitals are strikingly absent from the National Strategy. Nor does the recently passed $1.9 trillion federal stimulus package provide dedicated funds for hospitals, though some funds earmarked for vaccine delivery may land at hospitals. These are consequential omissions in otherwise comprehensive, thoughtful pandemic response plans.
Future legislation should include an immediate revenue infusion to reimburse hospitals’ COVID-19 preparations and lost volume and a firm commitment of ongoing financial support for preparedness through the end of the pandemic at a level sufficient to offset COVID-19–related losses. Experience with the CARES Act also suggests specific lessons for statutory design: support for hospitals should be allocated based on actual COVID-19–related burden for preparation and care, unlike CARES Act grants that were allocated based on hospitals’ past revenue and Medicare billing. This resulted in some large payments to relatively well-off hospitals and scant support for others (eg, rural or safety-net hospitals) with substantial COVID-19–related losses, a misstep that should not be repeated.
Hospitals are an integral part of the nation’s public health system. In the context of a pandemic, they should not be forced to serve as a backstop for shortcomings in other parts of the system without assistance. They, and their mission during the pandemic, are too important to fail.
The COVID-19 pandemic has put an extraordinary strain on US hospitals.1 In spring 2020, many hospitals had to quickly adapt to treat a surge of patients, and many more had to prepare for a potential surge. Creating reserve capacity meant halting outpatient care and elective surgeries, repurposing inpatient units, and increasing critical care staffing. Hospitals again face these difficult decisions, as COVID-19 resurges and variants of SARS-CoV-2 increasingly circulate, with large financial losses projected for 2021.2 Some large hospital systems may have the financial reserves to weather this storm, but the precarious situation facing others likely requires policy action.
Hospitals’ financial stress emanates from multiple quarters. First, revenue from elective inpatient procedures and outpatient care dropped dramatically, has not fully rebounded,3,4 and is not fully offset by revenue from COVID-19 care. Second, high unemployment may force up to 20% of commercially insured Americans into lower-reimbursing public insurance or the ranks of the uninsured, generating a projected $95 billion annual loss for hospitals.5 Third, under the current payment system, the costs of preparing for a pandemic are not directly reimbursed. Yet—whether or not they ultimately experienced a large COVID-19 caseload—hospitals’ surge preparation has involved purchasing vast quantities of protective personal equipment (PPE) and other supplies and equipment, hiring additional staff, building SARS-CoV-2 testing capacity, and expanding occupational health services. Many expenses persist as “the new normal”: admissions now require SARS-CoV-2 testing, additional staff and PPE, and often, a private room. Physical distancing requirements mean hospitals’ capacity—and thus, revenue—will remain reduced.
Private insurers, by and large, are not volunteering to cover these increased costs, and it is difficult for hospitals to pass them along. Payment terms in many contracts (eg, for Medicare) are not modifiable; even where they are, renegotiating takes time. To date, federal relief payments from the CARES Act do not fully reimburse COVID-19 losses—a particular problem for smaller and safety-net hospitals without large reserves.
This situation raises ethical concerns. For example, it is ethically relevant that COVID-19 resurgence and hospitalizations are linked to states’ decisions to reopen quickly to ease economic burdens on businesses and workers. One result has been to shift some of the pandemic’s economic burden to the healthcare sector. From a fairness perspective, there should be limits on the losses hospitals are forced to shoulder to maintain COVID-19 preparedness and services. Even if hospitals have reserves, spending them threatens funding for other essential activities, such as capital investment.
The current situation is also fraught with perverse incentives that could jeopardize safe care. With elective care remaining at risk of being reduced,6 pressure intensifies to deliver as many services as possible as quickly as possible, which may not align with patients’ best interests. Across hospitals that need to maximize volume to survive, a push to keep elective services open may emerge, even as COVID-19 prevalence may favor a shutdown. Hospitals with a heavy COVID-19 caseload may have greater difficulty reopening than competitors with lower caseloads, potentially impacting quality if patients seek elective care at lower-volume centers or in ways that disrupt continuity of care.
Ethical dilemmas are also raised by the delicate balancing of interests that hospitals have been engaging in among patient groups. How should they balance the needs of COVID-19 patients against potential harms to others who must delay care?
It is wrong to ask hospitals to make such choices when policy solutions are available. With the resurgence of COVID-19 must come a fresh, sustained program of federal financial relief for hospitals. While direct government support is the swiftest path, consideration should be given to the role of private insurers, which have benefited economically from the widespread deferment and forgoing of elective care. Voluntary or mandatory investments by insurers in helping hospitals survive the pandemic and weather the new normal are consonant with insurers’ commitment to providing their members access to high-quality healthcare.
The 200-page National Strategy document released by the Biden administration on January 21, 2021, promises some important assistance to hospitals.7 It includes plans to accelerate the production of PPE and other essential supplies using the Defense Production Act and other federal authorities, to rationalize nationwide distribution of these supplies and take steps to prevent price gouging, and to deploy federal personnel and assets to help surge critical-care personnel.
These steps, if fully funded and implemented, would bring welcome respite from some of the most vexing problems hospitals have encountered during COVID-19 surges. Yet, plans for direct financial relief for hospitals are strikingly absent from the National Strategy. Nor does the recently passed $1.9 trillion federal stimulus package provide dedicated funds for hospitals, though some funds earmarked for vaccine delivery may land at hospitals. These are consequential omissions in otherwise comprehensive, thoughtful pandemic response plans.
Future legislation should include an immediate revenue infusion to reimburse hospitals’ COVID-19 preparations and lost volume and a firm commitment of ongoing financial support for preparedness through the end of the pandemic at a level sufficient to offset COVID-19–related losses. Experience with the CARES Act also suggests specific lessons for statutory design: support for hospitals should be allocated based on actual COVID-19–related burden for preparation and care, unlike CARES Act grants that were allocated based on hospitals’ past revenue and Medicare billing. This resulted in some large payments to relatively well-off hospitals and scant support for others (eg, rural or safety-net hospitals) with substantial COVID-19–related losses, a misstep that should not be repeated.
Hospitals are an integral part of the nation’s public health system. In the context of a pandemic, they should not be forced to serve as a backstop for shortcomings in other parts of the system without assistance. They, and their mission during the pandemic, are too important to fail.
1. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
2. Coleman-Lochner L. Hospitals plead for bailout in face of runaway pandemic bills. February 26, 2021. Accessed March 25, 2021. https://www.bloomberg.com/news/articles/2021-02-26/hospitals-plead-for-bailout-in-face-of-runaway-pandemic-bills
3. American Hospital Association. Hospitals and health systems continue to face unprecedented financial challenges due to COVID-19. June 2020. Accessed February 5. 2021. https://www.aha.org/system/files/media/file/2020/06/aha-covid19-financial-impact-report.pdf
4. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood). 2020;39(11):2010-2017. https://doi.org/10.1377/hlthaff.2020.00980
5. Teasdale B, Schulman KA. Are U.S. hospitals still “recession-proof”? N Engl J Med. 2020;383(13):e82. https://doi.org/10.1056/NEJMp2018846
6. Meredith JW, High KP, Freischlag JA. Preserving elective surgeries in the COVID-19 pandemic and the future. JAMA. 2020;324(17):1725-1726. https://doi.org/10.1001/jama.2020.19594
7. Biden JR. National strategy for the COVID-19 response and pandemic preparedness. Bloomberg. January 2021. Accessed February 8, 2021. https://www.whitehouse.gov/wp-content/uploads/2021/01/National-Strategy-for-the-COVID-19-Response-and-Pandemic-Preparedness.pdf
1. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
2. Coleman-Lochner L. Hospitals plead for bailout in face of runaway pandemic bills. February 26, 2021. Accessed March 25, 2021. https://www.bloomberg.com/news/articles/2021-02-26/hospitals-plead-for-bailout-in-face-of-runaway-pandemic-bills
3. American Hospital Association. Hospitals and health systems continue to face unprecedented financial challenges due to COVID-19. June 2020. Accessed February 5. 2021. https://www.aha.org/system/files/media/file/2020/06/aha-covid19-financial-impact-report.pdf
4. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood). 2020;39(11):2010-2017. https://doi.org/10.1377/hlthaff.2020.00980
5. Teasdale B, Schulman KA. Are U.S. hospitals still “recession-proof”? N Engl J Med. 2020;383(13):e82. https://doi.org/10.1056/NEJMp2018846
6. Meredith JW, High KP, Freischlag JA. Preserving elective surgeries in the COVID-19 pandemic and the future. JAMA. 2020;324(17):1725-1726. https://doi.org/10.1001/jama.2020.19594
7. Biden JR. National strategy for the COVID-19 response and pandemic preparedness. Bloomberg. January 2021. Accessed February 8, 2021. https://www.whitehouse.gov/wp-content/uploads/2021/01/National-Strategy-for-the-COVID-19-Response-and-Pandemic-Preparedness.pdf
© 2021 Society of Hospital Medicine
Limiting Patient Autonomy: Mandatory COVID-19 Diagnostic Testing
Despite the important clinical and public health implications of a COVID-19 diagnosis, respect for autonomy allows patients to decline testing without explanation and with impunity. Whether physicians believe a test is indicated for clinical care of an individual patient, prevention of nosocomial transmission, or the greater public health, patients may refuse. Such refusals may be increasing due to quarantine requirements, concerns regarding contact tracing, and the persistent absence of a curative treatment.1,2 Mass screening of all healthcare workers (HCWs) is being considered to prevent hospital transmission,3 and universal screening in nursing homes has thwarted outbreaks while providing data to facilitate resource allocation.4 Given these circumstances, patients’ absolute right to refuse a noninvasive test with the potential for multifaceted downstream benefit is worthy of reconsideration, in favor of mandatory testing. Mandatory testing confers numerous benefits, including mitigating risk to other patients and HCWs, who play a central role in pandemic response. Because infected HCWs may transmit the virus to patients, they also should undergo mandatory testing,3 particularly in the presence of symptoms, since nasal secretions increase the diagnostic yield of testing.5 Although pretest probability (as an estimate of disease prevalence) typically determines the testing strategy for admitted patients, model-based analyses suggest that testing every 3 days for HCWs or continuously hospitalized patients would nearly eliminate infectivity.6
Tools for assisting frustrated HCWs navigating patients’ right to refuse testing have been developed that incorporate education, clear communication, and conflict resolution.7 Such approaches are, however, only moderately successful, making the use of personal protective equipment (PPE) based on a default assumption of COVID-19 positivity common.8 The burden and disheartening waste created by low-yield PPE use among patients unwilling to be tested becomes particularly evident in the context of shortages. Such vexing, stressful shortages, as well as the dual responsibilities of hospitals as stewards of both individual patient and population health, serve as reminders that efficient allocation of resources must be valued alongside the autonomous rights of patients.9 Moreover, recent reports suggest that test avoidance is a growing problem.1,2 Refusal to accept testing may be rooted in anxiety, concerns about the consequences of a positive result (eg, inability to attend school or work), or a desire for self-determination.1,2 The hesitancy that leads to refusal may also arise from misinformation, poor public health messaging, distrust in the establishment, and unproductive considerations related to conscientious objection without foundation.2 Concepts of individual liberty that often underlie steadfast adherence to the principles of self-determination created opposition to masks that antagonized public health efforts to limit the spread of COVID-19. Although influencing inpatients’ behavior to benefit both the public and HCWs may be distinct from community settings, the attitudes that lead to test refusal and defiance of mask-related ordinances likely have substantial commonalities.
THE PATIENT ROLE IN HEALTHCARE DECISIONS
As a pillar of ethical
ANALOGOUS EXPERIENCES: ETHICAL LESSONS AND PRACTICAL IMPLICATIONS
In non-healthcare settings, the controversies surrounding vaccination and access to schools for unvaccinated children are perhaps the public and professional debate most analogous to COVID-19 testing refusal.12 Although policymakers may distinguish between testing and vaccination, these interventions similarly hold the potential to limit disease incidence and mitigate health impact. To preserve public health, most states prevent (with varied exemptions) unvaccinated children from attending schools. COVID-19 testing may in the future become a requirement for participation in group social activities, athletic competitions, or physical presence in the workplace to facilitate quarantining and/or targeted use of PPE for transmission risk reduction. Given the dramatic mitigation benefits accruable on college campuses,13 required testing for in-person learning has become common.
There are also parallels, and therefore lessons, to be drawn from experience in testing for HIV, although HIV-related stigma and devalued status of the marginalized populations initially infected impacted the broader societal view of HIV compared with COVID-19. For example, antenatal HIV screening of pregnant women is strongly recommended to facilitate interventions that reduce the chance of vertical transmission.14 The limitations of purely elective testing are one justification for the current standard of opt-out screening. However, in this case, the health complications of refusal are largely the burden of the fetus, over whose future the mother holds a great deal of choice and responsibility, irrespective of HIV status. The public health implications of HIV test refusal are far less immediate than for COVID-19 infection because there is no effective curative therapy for COVID-19 and spread occurs through nonintimate, unintentional, and unpredictable exposure.
Translating societal attitudes and practices into the healthcare setting to consider mandated COVID-19 testing requires additional considerations related to both patients and providers: (1) HCWs have committed to a set of values and professional obligations that include tasks requiring risks15; (2) the public expects HCWs to perform their duties according to a social contract that has few restrictions16; (3) limiting patient access to hospital care due to COVID-19 testing refusal would contradict and create conflicts related to professional conceptions of hospitals and physicians as patient agents15; and (4) patients who conscientiously object to testing may seek healthcare less diligently, which may lead to health decrements. The associated postponement of essential care may unduly burden the healthcare system, particularly in situations such as ambulatory care–sensitive conditions.
HEALTHCARE WORKER PROTECTION, PATIENT ACCESS, AND THE VALUE OF PARSIMONY
The extent to which the public health justification for mandatory testing extends to hospitalized patients to protect HCWs is ambiguous. HCWs are of enormous instrumental value and are therefore essential for the pandemic response and health of the broader population. Their protection may therefore justify curtailing informed consent for diagnostic testing. Downstream effects on the supply of frontline HCWs may be realized. Poor control over working conditions may negatively impact motivation among HCWs. In addition, they may feel disenfranchised while obligatorily taking personal risks in caring for patients unwilling to commit to the common good through diagnostic test consent. Hospitalized patients who refuse testing may remain patients under investigation (PUIs), thus requiring special respiratory precautions (SRP) throughout their hospitalization, thereby placing a persistent burden on those with responsibilities requiring patient contact.17 Repeatedly donning and doffing PPE may remind at-risk HCWs that a myriad of benefits may accrue from frequent, ubiquitous testing. Their motivation may be tempered by the demoralizing requirement to care for patients who will not consent to a simple test, knowing that an opportunity to diminish the burdens of this communicable disease that has taken the lives of many HCWs is being relinquished.
Although HCWs could use SRP universally, their selective application in rooms of known COVID-19–positive patients and those with temporary PUI status has several advantages.17 First, we learned that HIV testing on patients was helpful in enabling surgeons to selectively implement special precautions among infected patients rather than universally applied intensive precautions. Even in the setting of high rates of HIV infection and educational interventions, HCWs do not reliably apply protective measures included in universal precautions.18 In keeping with these experiences, limiting the number of patients on SRP will minimize the “precautions fatigue” that drives nonadherent behavior among HCWs.17 As a result, minimizing the proportion of patients on SRP through testing (and liberation from unnecessary precautions in most cases) will improve uptake of crucial hand hygiene practices and adoption of vigilant PPE use. Second, definitive knowledge of COVID-19 status will increase patient access to care because, whether by personal choice or policy, many HCWs limit in-person contact with patients who are or may be COVID-19 positive. For example, many inpatient dialysis units do not accept patients without a negative COVID-19 nasal swab. Physical therapists may delay or avoid seeing a PUI, which will pose challenges for efficient determination of discharge disposition. Third, selective use of SRP will limit the environmental impact of disposed PPE, which is neither recyclable nor biodegradable. Infectious or regulated biomedical waste products are a significant source of environmental pollution, and the World Health Organization has recommended parsimonious, selective use of PPE to minimize the adverse environmental consequences of biomedical waste products.
CONCLUSION
In summary, there are substantial justifications for mandatory testing for COVID-19 in the hospital for HCWs and patients, as has been successfully piloted in selected long-term care facilities. Patients who refuse to allow testing may have to accept that their care may be compromised. For preservation of HCW supply and maintenance of HCW morale, hospital policies should make explicit, without punishment or coercion, that HCWs may modify the care they provide to patients who refuse to consent to COVID-19 testing.
1. Morris NP. Refusing testing during a pandemic. Am J Public Health. 2020;110(9):1354-1355. https://doi.org/10.2105/AJPH.2020.305810
2. Rubin R. First it was masks; now some refuse testing for SARS-CoV-2. JAMA. 2020;324(20):2015-2016. https://doi.org/10.1001/jama.2020.22003
3. Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395(10234):1418-1420. https://doi.org/10.1016/S0140-6736(20)30917-X
4. McBee SM, Thomasson ED, Scott MA, et al. Notes from the field: universal statewide laboratory testing for SARS-CoV-2 in nursing homes—West Virginia, April 21–May 8, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(34):1177-1179. http://dx.doi.org/10.15585/mmwr.mm6934a4
5. Long DR, Gombar S, Hogan CA, et al. Occurrence and timing of subsequent severe acute respiratory syndrome coronavirus 2 reverse-transcription polymerase chain reaction positivity among initially negative patients. Clin Infect Dis. 2021;72(2):323-326. https://doi.org/10.1093/cid/ciaa722
6. Larremore DB, Wilder B, Lester E, et al. Test sensitivity is secondary to frequency and turnaround time for COVID-19 screening. Sci Adv. 2021;7(1):eabd5393. https://advances.sciencemag.org/content/7/1/eabd5393
7. Lu AC, Burgart AM. Elective surgery and COVID-19: a framework for the untested patient. Ann Surg. 2020;272(6):e291-e295. https://doi.org/10.1097/SLA.0000000000004474
8. Podboy A, Cholankeril G, Cianfichi L, Guzman E Jr, Ahmed A, Banerjee S. Implementation and impact of universal preprocedure testing of patients for COVID-19 before endoscopy. Gastroenterology. 2020;159(4):1586-1588. https://doi.org/10.1053/j.gastro.2020.06.022
9. O’Neill O. Some limits of informed consent. J Med Ethics. 2003;29(1):4-7. https://doi.org/10.1136/jme.29.1.4
10. Will JF. A brief historical and theoretical perspective on patient autonomy and medical decision making: part II: the autonomy model. Chest. 2011;139(6):1491-1497. https://doi.org/10.1378/chest.11-0516
11. Will JF. A brief historical and theoretical perspective on patient autonomy and medical decision making: part I: the beneficence model. Chest. 2011;139(3):669-673. https://doi.org/10.1378/chest.10-2532
12. Hendrix KS, Sturm LA, Zimet GD, Meslin EM. Ethics and childhood vaccination policy in the United States. Am J Public Health. 2016;106(2):273-278. https://doi.org/10.2105/AJPH.2015.302952
13. Losina E, Leifer V, Millham L, et al. College campuses and COVID-19 mitigation: clinical and economic value. Ann Intern Med. Published online December 21, 2020. https://doi.org/10.7326/M20-6558
14. Selph SS, Bougatsos C, Dana T, Grusing S, Chou R. Screening for HIV infection in pregnant women: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2019;321(23):2349-2360. https://doi.org/10.1001/jama.2019.2593
15. Dranove D, White WD. Agency and the organization of health care delivery. Inquiry. 1987;24(4):405-415.
16. Huber SJ, Wynia MK. When pestilence prevails...physician responsibilities in epidemics. Am J Bioeth. 2004;4(1):W5-W11. https://www.tandfonline.com/doi/abs/10.1162/152651604773067497
17. Ruhnke GW. COVID-19 diagnostic testing and the psychology of precautions fatigue. Cleve Clin J Med. 2020;88(1):19-21. https://doi.org/10.3949/ccjm.88a.20086
18. Freeman SW, Chambers CV. Compliance with universal precautions in a medical practice with a high rate of HIV infection. J Am Board Fam Pract. 1992;5(3):313-318.
Despite the important clinical and public health implications of a COVID-19 diagnosis, respect for autonomy allows patients to decline testing without explanation and with impunity. Whether physicians believe a test is indicated for clinical care of an individual patient, prevention of nosocomial transmission, or the greater public health, patients may refuse. Such refusals may be increasing due to quarantine requirements, concerns regarding contact tracing, and the persistent absence of a curative treatment.1,2 Mass screening of all healthcare workers (HCWs) is being considered to prevent hospital transmission,3 and universal screening in nursing homes has thwarted outbreaks while providing data to facilitate resource allocation.4 Given these circumstances, patients’ absolute right to refuse a noninvasive test with the potential for multifaceted downstream benefit is worthy of reconsideration, in favor of mandatory testing. Mandatory testing confers numerous benefits, including mitigating risk to other patients and HCWs, who play a central role in pandemic response. Because infected HCWs may transmit the virus to patients, they also should undergo mandatory testing,3 particularly in the presence of symptoms, since nasal secretions increase the diagnostic yield of testing.5 Although pretest probability (as an estimate of disease prevalence) typically determines the testing strategy for admitted patients, model-based analyses suggest that testing every 3 days for HCWs or continuously hospitalized patients would nearly eliminate infectivity.6
Tools for assisting frustrated HCWs navigating patients’ right to refuse testing have been developed that incorporate education, clear communication, and conflict resolution.7 Such approaches are, however, only moderately successful, making the use of personal protective equipment (PPE) based on a default assumption of COVID-19 positivity common.8 The burden and disheartening waste created by low-yield PPE use among patients unwilling to be tested becomes particularly evident in the context of shortages. Such vexing, stressful shortages, as well as the dual responsibilities of hospitals as stewards of both individual patient and population health, serve as reminders that efficient allocation of resources must be valued alongside the autonomous rights of patients.9 Moreover, recent reports suggest that test avoidance is a growing problem.1,2 Refusal to accept testing may be rooted in anxiety, concerns about the consequences of a positive result (eg, inability to attend school or work), or a desire for self-determination.1,2 The hesitancy that leads to refusal may also arise from misinformation, poor public health messaging, distrust in the establishment, and unproductive considerations related to conscientious objection without foundation.2 Concepts of individual liberty that often underlie steadfast adherence to the principles of self-determination created opposition to masks that antagonized public health efforts to limit the spread of COVID-19. Although influencing inpatients’ behavior to benefit both the public and HCWs may be distinct from community settings, the attitudes that lead to test refusal and defiance of mask-related ordinances likely have substantial commonalities.
THE PATIENT ROLE IN HEALTHCARE DECISIONS
As a pillar of ethical
ANALOGOUS EXPERIENCES: ETHICAL LESSONS AND PRACTICAL IMPLICATIONS
In non-healthcare settings, the controversies surrounding vaccination and access to schools for unvaccinated children are perhaps the public and professional debate most analogous to COVID-19 testing refusal.12 Although policymakers may distinguish between testing and vaccination, these interventions similarly hold the potential to limit disease incidence and mitigate health impact. To preserve public health, most states prevent (with varied exemptions) unvaccinated children from attending schools. COVID-19 testing may in the future become a requirement for participation in group social activities, athletic competitions, or physical presence in the workplace to facilitate quarantining and/or targeted use of PPE for transmission risk reduction. Given the dramatic mitigation benefits accruable on college campuses,13 required testing for in-person learning has become common.
There are also parallels, and therefore lessons, to be drawn from experience in testing for HIV, although HIV-related stigma and devalued status of the marginalized populations initially infected impacted the broader societal view of HIV compared with COVID-19. For example, antenatal HIV screening of pregnant women is strongly recommended to facilitate interventions that reduce the chance of vertical transmission.14 The limitations of purely elective testing are one justification for the current standard of opt-out screening. However, in this case, the health complications of refusal are largely the burden of the fetus, over whose future the mother holds a great deal of choice and responsibility, irrespective of HIV status. The public health implications of HIV test refusal are far less immediate than for COVID-19 infection because there is no effective curative therapy for COVID-19 and spread occurs through nonintimate, unintentional, and unpredictable exposure.
Translating societal attitudes and practices into the healthcare setting to consider mandated COVID-19 testing requires additional considerations related to both patients and providers: (1) HCWs have committed to a set of values and professional obligations that include tasks requiring risks15; (2) the public expects HCWs to perform their duties according to a social contract that has few restrictions16; (3) limiting patient access to hospital care due to COVID-19 testing refusal would contradict and create conflicts related to professional conceptions of hospitals and physicians as patient agents15; and (4) patients who conscientiously object to testing may seek healthcare less diligently, which may lead to health decrements. The associated postponement of essential care may unduly burden the healthcare system, particularly in situations such as ambulatory care–sensitive conditions.
HEALTHCARE WORKER PROTECTION, PATIENT ACCESS, AND THE VALUE OF PARSIMONY
The extent to which the public health justification for mandatory testing extends to hospitalized patients to protect HCWs is ambiguous. HCWs are of enormous instrumental value and are therefore essential for the pandemic response and health of the broader population. Their protection may therefore justify curtailing informed consent for diagnostic testing. Downstream effects on the supply of frontline HCWs may be realized. Poor control over working conditions may negatively impact motivation among HCWs. In addition, they may feel disenfranchised while obligatorily taking personal risks in caring for patients unwilling to commit to the common good through diagnostic test consent. Hospitalized patients who refuse testing may remain patients under investigation (PUIs), thus requiring special respiratory precautions (SRP) throughout their hospitalization, thereby placing a persistent burden on those with responsibilities requiring patient contact.17 Repeatedly donning and doffing PPE may remind at-risk HCWs that a myriad of benefits may accrue from frequent, ubiquitous testing. Their motivation may be tempered by the demoralizing requirement to care for patients who will not consent to a simple test, knowing that an opportunity to diminish the burdens of this communicable disease that has taken the lives of many HCWs is being relinquished.
Although HCWs could use SRP universally, their selective application in rooms of known COVID-19–positive patients and those with temporary PUI status has several advantages.17 First, we learned that HIV testing on patients was helpful in enabling surgeons to selectively implement special precautions among infected patients rather than universally applied intensive precautions. Even in the setting of high rates of HIV infection and educational interventions, HCWs do not reliably apply protective measures included in universal precautions.18 In keeping with these experiences, limiting the number of patients on SRP will minimize the “precautions fatigue” that drives nonadherent behavior among HCWs.17 As a result, minimizing the proportion of patients on SRP through testing (and liberation from unnecessary precautions in most cases) will improve uptake of crucial hand hygiene practices and adoption of vigilant PPE use. Second, definitive knowledge of COVID-19 status will increase patient access to care because, whether by personal choice or policy, many HCWs limit in-person contact with patients who are or may be COVID-19 positive. For example, many inpatient dialysis units do not accept patients without a negative COVID-19 nasal swab. Physical therapists may delay or avoid seeing a PUI, which will pose challenges for efficient determination of discharge disposition. Third, selective use of SRP will limit the environmental impact of disposed PPE, which is neither recyclable nor biodegradable. Infectious or regulated biomedical waste products are a significant source of environmental pollution, and the World Health Organization has recommended parsimonious, selective use of PPE to minimize the adverse environmental consequences of biomedical waste products.
CONCLUSION
In summary, there are substantial justifications for mandatory testing for COVID-19 in the hospital for HCWs and patients, as has been successfully piloted in selected long-term care facilities. Patients who refuse to allow testing may have to accept that their care may be compromised. For preservation of HCW supply and maintenance of HCW morale, hospital policies should make explicit, without punishment or coercion, that HCWs may modify the care they provide to patients who refuse to consent to COVID-19 testing.
Despite the important clinical and public health implications of a COVID-19 diagnosis, respect for autonomy allows patients to decline testing without explanation and with impunity. Whether physicians believe a test is indicated for clinical care of an individual patient, prevention of nosocomial transmission, or the greater public health, patients may refuse. Such refusals may be increasing due to quarantine requirements, concerns regarding contact tracing, and the persistent absence of a curative treatment.1,2 Mass screening of all healthcare workers (HCWs) is being considered to prevent hospital transmission,3 and universal screening in nursing homes has thwarted outbreaks while providing data to facilitate resource allocation.4 Given these circumstances, patients’ absolute right to refuse a noninvasive test with the potential for multifaceted downstream benefit is worthy of reconsideration, in favor of mandatory testing. Mandatory testing confers numerous benefits, including mitigating risk to other patients and HCWs, who play a central role in pandemic response. Because infected HCWs may transmit the virus to patients, they also should undergo mandatory testing,3 particularly in the presence of symptoms, since nasal secretions increase the diagnostic yield of testing.5 Although pretest probability (as an estimate of disease prevalence) typically determines the testing strategy for admitted patients, model-based analyses suggest that testing every 3 days for HCWs or continuously hospitalized patients would nearly eliminate infectivity.6
Tools for assisting frustrated HCWs navigating patients’ right to refuse testing have been developed that incorporate education, clear communication, and conflict resolution.7 Such approaches are, however, only moderately successful, making the use of personal protective equipment (PPE) based on a default assumption of COVID-19 positivity common.8 The burden and disheartening waste created by low-yield PPE use among patients unwilling to be tested becomes particularly evident in the context of shortages. Such vexing, stressful shortages, as well as the dual responsibilities of hospitals as stewards of both individual patient and population health, serve as reminders that efficient allocation of resources must be valued alongside the autonomous rights of patients.9 Moreover, recent reports suggest that test avoidance is a growing problem.1,2 Refusal to accept testing may be rooted in anxiety, concerns about the consequences of a positive result (eg, inability to attend school or work), or a desire for self-determination.1,2 The hesitancy that leads to refusal may also arise from misinformation, poor public health messaging, distrust in the establishment, and unproductive considerations related to conscientious objection without foundation.2 Concepts of individual liberty that often underlie steadfast adherence to the principles of self-determination created opposition to masks that antagonized public health efforts to limit the spread of COVID-19. Although influencing inpatients’ behavior to benefit both the public and HCWs may be distinct from community settings, the attitudes that lead to test refusal and defiance of mask-related ordinances likely have substantial commonalities.
THE PATIENT ROLE IN HEALTHCARE DECISIONS
As a pillar of ethical
ANALOGOUS EXPERIENCES: ETHICAL LESSONS AND PRACTICAL IMPLICATIONS
In non-healthcare settings, the controversies surrounding vaccination and access to schools for unvaccinated children are perhaps the public and professional debate most analogous to COVID-19 testing refusal.12 Although policymakers may distinguish between testing and vaccination, these interventions similarly hold the potential to limit disease incidence and mitigate health impact. To preserve public health, most states prevent (with varied exemptions) unvaccinated children from attending schools. COVID-19 testing may in the future become a requirement for participation in group social activities, athletic competitions, or physical presence in the workplace to facilitate quarantining and/or targeted use of PPE for transmission risk reduction. Given the dramatic mitigation benefits accruable on college campuses,13 required testing for in-person learning has become common.
There are also parallels, and therefore lessons, to be drawn from experience in testing for HIV, although HIV-related stigma and devalued status of the marginalized populations initially infected impacted the broader societal view of HIV compared with COVID-19. For example, antenatal HIV screening of pregnant women is strongly recommended to facilitate interventions that reduce the chance of vertical transmission.14 The limitations of purely elective testing are one justification for the current standard of opt-out screening. However, in this case, the health complications of refusal are largely the burden of the fetus, over whose future the mother holds a great deal of choice and responsibility, irrespective of HIV status. The public health implications of HIV test refusal are far less immediate than for COVID-19 infection because there is no effective curative therapy for COVID-19 and spread occurs through nonintimate, unintentional, and unpredictable exposure.
Translating societal attitudes and practices into the healthcare setting to consider mandated COVID-19 testing requires additional considerations related to both patients and providers: (1) HCWs have committed to a set of values and professional obligations that include tasks requiring risks15; (2) the public expects HCWs to perform their duties according to a social contract that has few restrictions16; (3) limiting patient access to hospital care due to COVID-19 testing refusal would contradict and create conflicts related to professional conceptions of hospitals and physicians as patient agents15; and (4) patients who conscientiously object to testing may seek healthcare less diligently, which may lead to health decrements. The associated postponement of essential care may unduly burden the healthcare system, particularly in situations such as ambulatory care–sensitive conditions.
HEALTHCARE WORKER PROTECTION, PATIENT ACCESS, AND THE VALUE OF PARSIMONY
The extent to which the public health justification for mandatory testing extends to hospitalized patients to protect HCWs is ambiguous. HCWs are of enormous instrumental value and are therefore essential for the pandemic response and health of the broader population. Their protection may therefore justify curtailing informed consent for diagnostic testing. Downstream effects on the supply of frontline HCWs may be realized. Poor control over working conditions may negatively impact motivation among HCWs. In addition, they may feel disenfranchised while obligatorily taking personal risks in caring for patients unwilling to commit to the common good through diagnostic test consent. Hospitalized patients who refuse testing may remain patients under investigation (PUIs), thus requiring special respiratory precautions (SRP) throughout their hospitalization, thereby placing a persistent burden on those with responsibilities requiring patient contact.17 Repeatedly donning and doffing PPE may remind at-risk HCWs that a myriad of benefits may accrue from frequent, ubiquitous testing. Their motivation may be tempered by the demoralizing requirement to care for patients who will not consent to a simple test, knowing that an opportunity to diminish the burdens of this communicable disease that has taken the lives of many HCWs is being relinquished.
Although HCWs could use SRP universally, their selective application in rooms of known COVID-19–positive patients and those with temporary PUI status has several advantages.17 First, we learned that HIV testing on patients was helpful in enabling surgeons to selectively implement special precautions among infected patients rather than universally applied intensive precautions. Even in the setting of high rates of HIV infection and educational interventions, HCWs do not reliably apply protective measures included in universal precautions.18 In keeping with these experiences, limiting the number of patients on SRP will minimize the “precautions fatigue” that drives nonadherent behavior among HCWs.17 As a result, minimizing the proportion of patients on SRP through testing (and liberation from unnecessary precautions in most cases) will improve uptake of crucial hand hygiene practices and adoption of vigilant PPE use. Second, definitive knowledge of COVID-19 status will increase patient access to care because, whether by personal choice or policy, many HCWs limit in-person contact with patients who are or may be COVID-19 positive. For example, many inpatient dialysis units do not accept patients without a negative COVID-19 nasal swab. Physical therapists may delay or avoid seeing a PUI, which will pose challenges for efficient determination of discharge disposition. Third, selective use of SRP will limit the environmental impact of disposed PPE, which is neither recyclable nor biodegradable. Infectious or regulated biomedical waste products are a significant source of environmental pollution, and the World Health Organization has recommended parsimonious, selective use of PPE to minimize the adverse environmental consequences of biomedical waste products.
CONCLUSION
In summary, there are substantial justifications for mandatory testing for COVID-19 in the hospital for HCWs and patients, as has been successfully piloted in selected long-term care facilities. Patients who refuse to allow testing may have to accept that their care may be compromised. For preservation of HCW supply and maintenance of HCW morale, hospital policies should make explicit, without punishment or coercion, that HCWs may modify the care they provide to patients who refuse to consent to COVID-19 testing.
1. Morris NP. Refusing testing during a pandemic. Am J Public Health. 2020;110(9):1354-1355. https://doi.org/10.2105/AJPH.2020.305810
2. Rubin R. First it was masks; now some refuse testing for SARS-CoV-2. JAMA. 2020;324(20):2015-2016. https://doi.org/10.1001/jama.2020.22003
3. Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395(10234):1418-1420. https://doi.org/10.1016/S0140-6736(20)30917-X
4. McBee SM, Thomasson ED, Scott MA, et al. Notes from the field: universal statewide laboratory testing for SARS-CoV-2 in nursing homes—West Virginia, April 21–May 8, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(34):1177-1179. http://dx.doi.org/10.15585/mmwr.mm6934a4
5. Long DR, Gombar S, Hogan CA, et al. Occurrence and timing of subsequent severe acute respiratory syndrome coronavirus 2 reverse-transcription polymerase chain reaction positivity among initially negative patients. Clin Infect Dis. 2021;72(2):323-326. https://doi.org/10.1093/cid/ciaa722
6. Larremore DB, Wilder B, Lester E, et al. Test sensitivity is secondary to frequency and turnaround time for COVID-19 screening. Sci Adv. 2021;7(1):eabd5393. https://advances.sciencemag.org/content/7/1/eabd5393
7. Lu AC, Burgart AM. Elective surgery and COVID-19: a framework for the untested patient. Ann Surg. 2020;272(6):e291-e295. https://doi.org/10.1097/SLA.0000000000004474
8. Podboy A, Cholankeril G, Cianfichi L, Guzman E Jr, Ahmed A, Banerjee S. Implementation and impact of universal preprocedure testing of patients for COVID-19 before endoscopy. Gastroenterology. 2020;159(4):1586-1588. https://doi.org/10.1053/j.gastro.2020.06.022
9. O’Neill O. Some limits of informed consent. J Med Ethics. 2003;29(1):4-7. https://doi.org/10.1136/jme.29.1.4
10. Will JF. A brief historical and theoretical perspective on patient autonomy and medical decision making: part II: the autonomy model. Chest. 2011;139(6):1491-1497. https://doi.org/10.1378/chest.11-0516
11. Will JF. A brief historical and theoretical perspective on patient autonomy and medical decision making: part I: the beneficence model. Chest. 2011;139(3):669-673. https://doi.org/10.1378/chest.10-2532
12. Hendrix KS, Sturm LA, Zimet GD, Meslin EM. Ethics and childhood vaccination policy in the United States. Am J Public Health. 2016;106(2):273-278. https://doi.org/10.2105/AJPH.2015.302952
13. Losina E, Leifer V, Millham L, et al. College campuses and COVID-19 mitigation: clinical and economic value. Ann Intern Med. Published online December 21, 2020. https://doi.org/10.7326/M20-6558
14. Selph SS, Bougatsos C, Dana T, Grusing S, Chou R. Screening for HIV infection in pregnant women: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2019;321(23):2349-2360. https://doi.org/10.1001/jama.2019.2593
15. Dranove D, White WD. Agency and the organization of health care delivery. Inquiry. 1987;24(4):405-415.
16. Huber SJ, Wynia MK. When pestilence prevails...physician responsibilities in epidemics. Am J Bioeth. 2004;4(1):W5-W11. https://www.tandfonline.com/doi/abs/10.1162/152651604773067497
17. Ruhnke GW. COVID-19 diagnostic testing and the psychology of precautions fatigue. Cleve Clin J Med. 2020;88(1):19-21. https://doi.org/10.3949/ccjm.88a.20086
18. Freeman SW, Chambers CV. Compliance with universal precautions in a medical practice with a high rate of HIV infection. J Am Board Fam Pract. 1992;5(3):313-318.
1. Morris NP. Refusing testing during a pandemic. Am J Public Health. 2020;110(9):1354-1355. https://doi.org/10.2105/AJPH.2020.305810
2. Rubin R. First it was masks; now some refuse testing for SARS-CoV-2. JAMA. 2020;324(20):2015-2016. https://doi.org/10.1001/jama.2020.22003
3. Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395(10234):1418-1420. https://doi.org/10.1016/S0140-6736(20)30917-X
4. McBee SM, Thomasson ED, Scott MA, et al. Notes from the field: universal statewide laboratory testing for SARS-CoV-2 in nursing homes—West Virginia, April 21–May 8, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(34):1177-1179. http://dx.doi.org/10.15585/mmwr.mm6934a4
5. Long DR, Gombar S, Hogan CA, et al. Occurrence and timing of subsequent severe acute respiratory syndrome coronavirus 2 reverse-transcription polymerase chain reaction positivity among initially negative patients. Clin Infect Dis. 2021;72(2):323-326. https://doi.org/10.1093/cid/ciaa722
6. Larremore DB, Wilder B, Lester E, et al. Test sensitivity is secondary to frequency and turnaround time for COVID-19 screening. Sci Adv. 2021;7(1):eabd5393. https://advances.sciencemag.org/content/7/1/eabd5393
7. Lu AC, Burgart AM. Elective surgery and COVID-19: a framework for the untested patient. Ann Surg. 2020;272(6):e291-e295. https://doi.org/10.1097/SLA.0000000000004474
8. Podboy A, Cholankeril G, Cianfichi L, Guzman E Jr, Ahmed A, Banerjee S. Implementation and impact of universal preprocedure testing of patients for COVID-19 before endoscopy. Gastroenterology. 2020;159(4):1586-1588. https://doi.org/10.1053/j.gastro.2020.06.022
9. O’Neill O. Some limits of informed consent. J Med Ethics. 2003;29(1):4-7. https://doi.org/10.1136/jme.29.1.4
10. Will JF. A brief historical and theoretical perspective on patient autonomy and medical decision making: part II: the autonomy model. Chest. 2011;139(6):1491-1497. https://doi.org/10.1378/chest.11-0516
11. Will JF. A brief historical and theoretical perspective on patient autonomy and medical decision making: part I: the beneficence model. Chest. 2011;139(3):669-673. https://doi.org/10.1378/chest.10-2532
12. Hendrix KS, Sturm LA, Zimet GD, Meslin EM. Ethics and childhood vaccination policy in the United States. Am J Public Health. 2016;106(2):273-278. https://doi.org/10.2105/AJPH.2015.302952
13. Losina E, Leifer V, Millham L, et al. College campuses and COVID-19 mitigation: clinical and economic value. Ann Intern Med. Published online December 21, 2020. https://doi.org/10.7326/M20-6558
14. Selph SS, Bougatsos C, Dana T, Grusing S, Chou R. Screening for HIV infection in pregnant women: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2019;321(23):2349-2360. https://doi.org/10.1001/jama.2019.2593
15. Dranove D, White WD. Agency and the organization of health care delivery. Inquiry. 1987;24(4):405-415.
16. Huber SJ, Wynia MK. When pestilence prevails...physician responsibilities in epidemics. Am J Bioeth. 2004;4(1):W5-W11. https://www.tandfonline.com/doi/abs/10.1162/152651604773067497
17. Ruhnke GW. COVID-19 diagnostic testing and the psychology of precautions fatigue. Cleve Clin J Med. 2020;88(1):19-21. https://doi.org/10.3949/ccjm.88a.20086
18. Freeman SW, Chambers CV. Compliance with universal precautions in a medical practice with a high rate of HIV infection. J Am Board Fam Pract. 1992;5(3):313-318.
© 2021 Society of Hospital Medicine
Striking While the Iron Is Hot: Using the Updated PHM Competencies in Time-Variable Training
In July 2020, the revision of The Pediatric Hospital Medicine Core Competencies was published, bringing to fruition three years of meticulous work.1 The working group produced 66 chapters outlining the knowledge, skills, and attitudes needed for competent pediatric hospitalist practice. The arrival of these competencies is especially prescient given pediatric hospital medicine’s (PHM’s) relatively new standing as an American Board of Medical Specialties certified subspecialty, as the competencies can serve as a guide for improvement of fellowship curricula, assessment systems, and faculty development. The competencies also represent an opportunity for PHM to take a bold step forward in the world of graduate medical education (GME) by realizing a key tenet of competency-based medical education (CBME)—competency-based, time-variable training (CBTVT), in which learners train until competence is achieved rather than for a predetermined duration.2,3 In this perspective, we describe how medical education in the United States adopted a time-based training paradigm (in which time-in-training is a surrogate for competence), how CBME has brought time-variable training to the fore, and how PHM has an opportunity to be on the leading edge of education innovation.
TIME-BASED TRAINING IN THE UNITED STATES
In the 1800s, during the time of the “Wild West,” medical education in the United States matched this moniker. There was little standardization across the multiple training pathways to become a practicing physician, including apprenticeships, lecture series, and university courses.4 Predictably, this led to significant heterogeneity in the quality of medical care that a patient of the day received. This problem became clearer as Americans traveled to Europe and witnessed more structured and rigorous training programs, only to return to the comparatively poor state of medical education back home.5 There was a clear need for curricular standardization.
In 1876, the American Medical College Association (which later became the Association of American Medical Colleges [AAMC]) was founded to meet this need, and in 1905 the Association adopted a set of minimum standards for medical training that included the now-familiar two years of basic sciences and two years of clinical training.6 Two subsequent national surveys in the United States were commissioned to evaluate whether medical schools met this new standard, with both surveys finding that roughly half of existing programs passed muster.7,8 As a result, nearly half of US medical schools had closed by 1920 in a crusade to standardize curricula and produce competent physicians. By the time the American Medical Association established initial standards for internship (an archetype of GME),4 time-based medical training was the dominant paradigm. This historical perspective highlights the rationale for standardization of education processes and curricula, particularly in terms of accountability to the American public. But heralded by the 1978 landmark paper by McGaghie et al,9 the paradigm began to shift in the late twentieth century from a focus on the process of physician training to outcomes.
CBME AND TIME VARIABILITY
In contrast to the process-focused model of the early 1900s, CBME starts by identifying patient and healthcare system needs, defining competencies required to meet those needs, and then designing curricular and assessment processes to help learners achieve those competencies.2 This outcomes-based approach grew as a response to calls for greater accountability to the public due to evidence that some graduates were unprepared for unsupervised practice, raising concerns that strictly time-based training was no longer defensible.10 CBME aims to mitigate these concerns by starting with desired outcomes of training and working backward to ensure those outcomes are met.
While many programs have attempted to implement CBME, most still rely heavily on time-in-training to determine competence. Learners participate in structured curricula and, unless they are extreme outliers, are deemed ready for unsupervised practice after a predetermined duration. This model presumes that competence and time are related in a fixed, predictable manner and that learners gain competence at a uniform rate. However, learners do not, in fact, progress uniformly. A study by Schumacher et al11 involving 23 pediatric residency programs showed significant interlearner variability in rates of entrustment (used as a surrogate for competence), leading the authors to call for time-variable training in GME. Significant interlearner variation in rates of competence attainment have been shown in other specialties as well.12 As more CBME studies on training outcomes emerge, the evidence is mounting that not all learners need the same duration of training to become competent providers. Time-in-training and competence attainment are not related in a fixed manner. As Dr Jason13 wrote in 1969, “By making time a constant, we make achievement a variable.” Variable achievement (competence, outcomes) was the very driver for medical education’s shift to a competency-based approach. If variable competence was not acceptable then, why should it be now? The goal of CBTVT is not shorter training, but rather flexible, individualized training both in terms of content and duration. While this also means some learners may need to extend their training, this should already be part of GME programs that are required to have remediation policies for learners who are not progressing as expected.
AN OPPORTUNITY FOR PHM
Time variability is an oft-cited tenet of CBME,2,3 but one that is being piloted by relatively few programs in the United States, mostly in undergraduate medical education (UME).14-16 The Education in Pediatrics Across the Continuum (EPAC), a consortium consisting of four institutions piloting CBTVT in UME,14 has shown early evidence of feasibility17 and that UME graduates from CBTVT programs enter residency with levels of competence similar to those of graduates of traditional time-based programs.18 We believe that PHM can take a step toward truly realizing CBME by implementing CBTVT in fellowship programs.
There are multiple reasons why this is an opportune time for PHM fellowships to consider CBTVT. First, PHM is a relatively new board-certified subspecialty with a recently revised set of core competencies1 that are likely to catalyze programmatic innovation. A key step in change management is building on previous efforts to generate more change.19 Programs can leverage the momentum from current and impending change initiatives to innovate and implement CBTVT. Second, the revised PHM competencies provide the first crucial step in implementing a CBME program by defining desired training outcomes necessary to deliver high-quality patient care. With PHM competencies now well defined, programs can focus on developing programs of assessment and corresponding faculty development, which can help deliver valid, defensible decisions about fellow competence.
Finally, PHM has a workforce that can support CBTVT. A major barrier to time-variable training in GME is the need for trainees-as-workforce. In many GME programs, residents and fellows provide a relatively inexpensive, renewable workforce. Trainees’ clinical rotations are often scheduled up to 1 year in advance to ensure care teams are fully staffed, particularly in the inpatient setting, creating a system where flexibility in training is impossible without creating gaps in clinical coverage. However, many PHM fellowships do not completely rely on fellows to cover clinical service lines. PHM fellows spend 32 weeks over 2 years in core clinical rotations with faculty supervision, in accordance with the Accreditation Council for Graduate Medical Education program requirements, both for 2- and 3-year programs. Some CBME experts estimate (based on previous and ongoing CBTVT pilots) that training duration is likely to vary by roughly 20% from current time-based practices when CBTVT is initially implemented.20 Thus, only a small number of clinical service weeks are likely to be affected. If a fellow were deemed ready for unsupervised practice before finishing 2 years of fellowship in a CBTVT program, the corresponding faculty supervisor could use the time previously assigned for supervision to pursue other priorities, such as education, scholarship, or quality improvement. Why provide supervision if a clinical competency committee has deemed a fellow ready for unsupervised practice? Some level of observation and formative feedback could continue, but full supervision would be redundant and unnecessary. CBTVT would allow for some fellows to experience the uncertainty that comes with unsupervised decision-making while still in an environment with trusted fellowship mentors and advisors.
STEPS TOWARD CHANGE
PHM fellowship programs likely cannot flip a switch to “turn on” CBTVT immediately, but they can take steps toward making the transition. Validity, or defensibility of decisions, will be crucial for assessment in CBTVT systems. Programs will need to develop robust assessment systems that collect myriad data to answer the question, “When is this learner competent to deliver high-quality care without supervision?” Programs can align assessment instruments, faculty-development initiatives, and clinical competency committee (CCC) processes with the 2020 PHM competencies to provide a defensible answer. Program leaders should then seek validity evidence, either in existing literature or through novel scholarly initiatives, to support these summative decisions. Engaging all fellowship stakeholders in transitions to CBTVT will be important and should include fellows, program directors, CCC members, clinical leadership, and members from accrediting and credentialing bodies.
CONCLUSION
As fellowship programs review and revise curricula and assessment systems around the updated PHM core competencies, they should also consider what changes are necessary to implement CBTVT. Time variability is not a novelty but, rather, is a corollary to the outcomes-based approach of CBME. PHM fellowships should strike while the iron is hot and build on current change initiatives prompted by the growth of our specialty to be leaders in CBTVT.
1. Maniscalco J, Gage S, Sofia Teferi M, Fisher ES. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
2. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638-645. https://doi.org/10.3109/0142159X.2010.501190
3. Lucey CR, Thibault GE, Ten Cate O. Competency-based, tme-variable education in the health professions: crossroads. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S1-S5. https://doi.org/10.1097/ACM.0000000000002080
4. Custers EJFM, Ten Cate O. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S49-S54. https://doi.org/10.1097/ACM.0000000000002079
5. Barr DA. Revolution or evolution? Putting the Flexner Report in context. Med Educ. 2011;45(1):17-22. https://doi.org/10.1111/j.1365-2923.2010.03850.x
6. Association of American Medical Colleges. Minutes of the Fifteenth Annual Meeting. April 10, 1905; Chicago, IL.
7. Bevan A. Council on Medical Education of the American Medical Association. JAMA. 1907;48(20):1701-1707.
8. Flexner A. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, Bulletin Number Four, 1910. Bull World Health Organ. 2002;80(7):594-602.
9. McGaghie WC, Sajid AW, Miller GE, et al. Competency-based curriculum development in medical education: an introduction. Public Health Pap. 1978;(68):11-91.
10. Frank JR, Snell L, Englander R, Holmboe ES, ICBME Collaborators. Implementing competency-based medical education: moving forward. Med Teach. 2017;39(6):568-573. https://doi.org/10.1080/0142159X.2017.1315069
11. Schumacher DJ, West DC, Schwartz A, et al. Longitudinal assessment of resident performance using entrustable professional activities. JAMA Netw Open. 2020;3(1):e1919316. https://doi.org/10.1001/jamanetworkopen.2019.19316
12. Warm EJ, Held J, Hellman M, et al. Entrusting observable practice activities and milestones over the 36 months of an internal medicine residency. Acad Med. 2016;91(10):1398-1405. https://doi.org/10.1097/ACM.0000000000001292
13. Jason H. Effective medical instruction: requirements and possibilities. In: Proceedings of a 1969 International Symposium on Medical Education. Medica; 1970:5-8.
14. Andrews JS, Bale JF Jr, Soep JB, et al. Education in Pediatrics Across the Continuum (EPAC): first steps toward realizing the dream of competency-based education. Acad Med. 2018;93(3):414-420. https://doi.org/10.1097/ACM.0000000000002020
15. Mejicano GC, Bumsted TN. Describing the journey and lessons learned implementing a competency-based, time-variable undergraduate medical education curriculum. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S42-S48. https://doi.org/10.1097/ACM.0000000000002068
16. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
17. Murray KE, Lane JL, Carraccio C, et al. Crossing the gap: using competency-based assessment to determine whether learners are ready for the undergraduate-to-graduate transition. Acad Med. 2019;94(3):338-345. https://doi.org/10.1097/ACM.0000000000002535
18. Schwartz A, Balmer DF, Borman-Shoap E, et al. Shared mental models among clinical competency committees in the context of time-variable, competency-based advancement to residency. Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S95-S102. https://doi.org/10.1097/ACM.0000000000003638
19. Kotter JP. Leading change: why transformation efforts fail. Harvard Business Review. May-June 1995. Accessed March 1, 2021. https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2
20. Schumacher DJ, Caretta-Weyer H, Busari J, et al. Competency-based time-variable training internationally: ensuring practical next steps. Med Teach. Forthcoming.
In July 2020, the revision of The Pediatric Hospital Medicine Core Competencies was published, bringing to fruition three years of meticulous work.1 The working group produced 66 chapters outlining the knowledge, skills, and attitudes needed for competent pediatric hospitalist practice. The arrival of these competencies is especially prescient given pediatric hospital medicine’s (PHM’s) relatively new standing as an American Board of Medical Specialties certified subspecialty, as the competencies can serve as a guide for improvement of fellowship curricula, assessment systems, and faculty development. The competencies also represent an opportunity for PHM to take a bold step forward in the world of graduate medical education (GME) by realizing a key tenet of competency-based medical education (CBME)—competency-based, time-variable training (CBTVT), in which learners train until competence is achieved rather than for a predetermined duration.2,3 In this perspective, we describe how medical education in the United States adopted a time-based training paradigm (in which time-in-training is a surrogate for competence), how CBME has brought time-variable training to the fore, and how PHM has an opportunity to be on the leading edge of education innovation.
TIME-BASED TRAINING IN THE UNITED STATES
In the 1800s, during the time of the “Wild West,” medical education in the United States matched this moniker. There was little standardization across the multiple training pathways to become a practicing physician, including apprenticeships, lecture series, and university courses.4 Predictably, this led to significant heterogeneity in the quality of medical care that a patient of the day received. This problem became clearer as Americans traveled to Europe and witnessed more structured and rigorous training programs, only to return to the comparatively poor state of medical education back home.5 There was a clear need for curricular standardization.
In 1876, the American Medical College Association (which later became the Association of American Medical Colleges [AAMC]) was founded to meet this need, and in 1905 the Association adopted a set of minimum standards for medical training that included the now-familiar two years of basic sciences and two years of clinical training.6 Two subsequent national surveys in the United States were commissioned to evaluate whether medical schools met this new standard, with both surveys finding that roughly half of existing programs passed muster.7,8 As a result, nearly half of US medical schools had closed by 1920 in a crusade to standardize curricula and produce competent physicians. By the time the American Medical Association established initial standards for internship (an archetype of GME),4 time-based medical training was the dominant paradigm. This historical perspective highlights the rationale for standardization of education processes and curricula, particularly in terms of accountability to the American public. But heralded by the 1978 landmark paper by McGaghie et al,9 the paradigm began to shift in the late twentieth century from a focus on the process of physician training to outcomes.
CBME AND TIME VARIABILITY
In contrast to the process-focused model of the early 1900s, CBME starts by identifying patient and healthcare system needs, defining competencies required to meet those needs, and then designing curricular and assessment processes to help learners achieve those competencies.2 This outcomes-based approach grew as a response to calls for greater accountability to the public due to evidence that some graduates were unprepared for unsupervised practice, raising concerns that strictly time-based training was no longer defensible.10 CBME aims to mitigate these concerns by starting with desired outcomes of training and working backward to ensure those outcomes are met.
While many programs have attempted to implement CBME, most still rely heavily on time-in-training to determine competence. Learners participate in structured curricula and, unless they are extreme outliers, are deemed ready for unsupervised practice after a predetermined duration. This model presumes that competence and time are related in a fixed, predictable manner and that learners gain competence at a uniform rate. However, learners do not, in fact, progress uniformly. A study by Schumacher et al11 involving 23 pediatric residency programs showed significant interlearner variability in rates of entrustment (used as a surrogate for competence), leading the authors to call for time-variable training in GME. Significant interlearner variation in rates of competence attainment have been shown in other specialties as well.12 As more CBME studies on training outcomes emerge, the evidence is mounting that not all learners need the same duration of training to become competent providers. Time-in-training and competence attainment are not related in a fixed manner. As Dr Jason13 wrote in 1969, “By making time a constant, we make achievement a variable.” Variable achievement (competence, outcomes) was the very driver for medical education’s shift to a competency-based approach. If variable competence was not acceptable then, why should it be now? The goal of CBTVT is not shorter training, but rather flexible, individualized training both in terms of content and duration. While this also means some learners may need to extend their training, this should already be part of GME programs that are required to have remediation policies for learners who are not progressing as expected.
AN OPPORTUNITY FOR PHM
Time variability is an oft-cited tenet of CBME,2,3 but one that is being piloted by relatively few programs in the United States, mostly in undergraduate medical education (UME).14-16 The Education in Pediatrics Across the Continuum (EPAC), a consortium consisting of four institutions piloting CBTVT in UME,14 has shown early evidence of feasibility17 and that UME graduates from CBTVT programs enter residency with levels of competence similar to those of graduates of traditional time-based programs.18 We believe that PHM can take a step toward truly realizing CBME by implementing CBTVT in fellowship programs.
There are multiple reasons why this is an opportune time for PHM fellowships to consider CBTVT. First, PHM is a relatively new board-certified subspecialty with a recently revised set of core competencies1 that are likely to catalyze programmatic innovation. A key step in change management is building on previous efforts to generate more change.19 Programs can leverage the momentum from current and impending change initiatives to innovate and implement CBTVT. Second, the revised PHM competencies provide the first crucial step in implementing a CBME program by defining desired training outcomes necessary to deliver high-quality patient care. With PHM competencies now well defined, programs can focus on developing programs of assessment and corresponding faculty development, which can help deliver valid, defensible decisions about fellow competence.
Finally, PHM has a workforce that can support CBTVT. A major barrier to time-variable training in GME is the need for trainees-as-workforce. In many GME programs, residents and fellows provide a relatively inexpensive, renewable workforce. Trainees’ clinical rotations are often scheduled up to 1 year in advance to ensure care teams are fully staffed, particularly in the inpatient setting, creating a system where flexibility in training is impossible without creating gaps in clinical coverage. However, many PHM fellowships do not completely rely on fellows to cover clinical service lines. PHM fellows spend 32 weeks over 2 years in core clinical rotations with faculty supervision, in accordance with the Accreditation Council for Graduate Medical Education program requirements, both for 2- and 3-year programs. Some CBME experts estimate (based on previous and ongoing CBTVT pilots) that training duration is likely to vary by roughly 20% from current time-based practices when CBTVT is initially implemented.20 Thus, only a small number of clinical service weeks are likely to be affected. If a fellow were deemed ready for unsupervised practice before finishing 2 years of fellowship in a CBTVT program, the corresponding faculty supervisor could use the time previously assigned for supervision to pursue other priorities, such as education, scholarship, or quality improvement. Why provide supervision if a clinical competency committee has deemed a fellow ready for unsupervised practice? Some level of observation and formative feedback could continue, but full supervision would be redundant and unnecessary. CBTVT would allow for some fellows to experience the uncertainty that comes with unsupervised decision-making while still in an environment with trusted fellowship mentors and advisors.
STEPS TOWARD CHANGE
PHM fellowship programs likely cannot flip a switch to “turn on” CBTVT immediately, but they can take steps toward making the transition. Validity, or defensibility of decisions, will be crucial for assessment in CBTVT systems. Programs will need to develop robust assessment systems that collect myriad data to answer the question, “When is this learner competent to deliver high-quality care without supervision?” Programs can align assessment instruments, faculty-development initiatives, and clinical competency committee (CCC) processes with the 2020 PHM competencies to provide a defensible answer. Program leaders should then seek validity evidence, either in existing literature or through novel scholarly initiatives, to support these summative decisions. Engaging all fellowship stakeholders in transitions to CBTVT will be important and should include fellows, program directors, CCC members, clinical leadership, and members from accrediting and credentialing bodies.
CONCLUSION
As fellowship programs review and revise curricula and assessment systems around the updated PHM core competencies, they should also consider what changes are necessary to implement CBTVT. Time variability is not a novelty but, rather, is a corollary to the outcomes-based approach of CBME. PHM fellowships should strike while the iron is hot and build on current change initiatives prompted by the growth of our specialty to be leaders in CBTVT.
In July 2020, the revision of The Pediatric Hospital Medicine Core Competencies was published, bringing to fruition three years of meticulous work.1 The working group produced 66 chapters outlining the knowledge, skills, and attitudes needed for competent pediatric hospitalist practice. The arrival of these competencies is especially prescient given pediatric hospital medicine’s (PHM’s) relatively new standing as an American Board of Medical Specialties certified subspecialty, as the competencies can serve as a guide for improvement of fellowship curricula, assessment systems, and faculty development. The competencies also represent an opportunity for PHM to take a bold step forward in the world of graduate medical education (GME) by realizing a key tenet of competency-based medical education (CBME)—competency-based, time-variable training (CBTVT), in which learners train until competence is achieved rather than for a predetermined duration.2,3 In this perspective, we describe how medical education in the United States adopted a time-based training paradigm (in which time-in-training is a surrogate for competence), how CBME has brought time-variable training to the fore, and how PHM has an opportunity to be on the leading edge of education innovation.
TIME-BASED TRAINING IN THE UNITED STATES
In the 1800s, during the time of the “Wild West,” medical education in the United States matched this moniker. There was little standardization across the multiple training pathways to become a practicing physician, including apprenticeships, lecture series, and university courses.4 Predictably, this led to significant heterogeneity in the quality of medical care that a patient of the day received. This problem became clearer as Americans traveled to Europe and witnessed more structured and rigorous training programs, only to return to the comparatively poor state of medical education back home.5 There was a clear need for curricular standardization.
In 1876, the American Medical College Association (which later became the Association of American Medical Colleges [AAMC]) was founded to meet this need, and in 1905 the Association adopted a set of minimum standards for medical training that included the now-familiar two years of basic sciences and two years of clinical training.6 Two subsequent national surveys in the United States were commissioned to evaluate whether medical schools met this new standard, with both surveys finding that roughly half of existing programs passed muster.7,8 As a result, nearly half of US medical schools had closed by 1920 in a crusade to standardize curricula and produce competent physicians. By the time the American Medical Association established initial standards for internship (an archetype of GME),4 time-based medical training was the dominant paradigm. This historical perspective highlights the rationale for standardization of education processes and curricula, particularly in terms of accountability to the American public. But heralded by the 1978 landmark paper by McGaghie et al,9 the paradigm began to shift in the late twentieth century from a focus on the process of physician training to outcomes.
CBME AND TIME VARIABILITY
In contrast to the process-focused model of the early 1900s, CBME starts by identifying patient and healthcare system needs, defining competencies required to meet those needs, and then designing curricular and assessment processes to help learners achieve those competencies.2 This outcomes-based approach grew as a response to calls for greater accountability to the public due to evidence that some graduates were unprepared for unsupervised practice, raising concerns that strictly time-based training was no longer defensible.10 CBME aims to mitigate these concerns by starting with desired outcomes of training and working backward to ensure those outcomes are met.
While many programs have attempted to implement CBME, most still rely heavily on time-in-training to determine competence. Learners participate in structured curricula and, unless they are extreme outliers, are deemed ready for unsupervised practice after a predetermined duration. This model presumes that competence and time are related in a fixed, predictable manner and that learners gain competence at a uniform rate. However, learners do not, in fact, progress uniformly. A study by Schumacher et al11 involving 23 pediatric residency programs showed significant interlearner variability in rates of entrustment (used as a surrogate for competence), leading the authors to call for time-variable training in GME. Significant interlearner variation in rates of competence attainment have been shown in other specialties as well.12 As more CBME studies on training outcomes emerge, the evidence is mounting that not all learners need the same duration of training to become competent providers. Time-in-training and competence attainment are not related in a fixed manner. As Dr Jason13 wrote in 1969, “By making time a constant, we make achievement a variable.” Variable achievement (competence, outcomes) was the very driver for medical education’s shift to a competency-based approach. If variable competence was not acceptable then, why should it be now? The goal of CBTVT is not shorter training, but rather flexible, individualized training both in terms of content and duration. While this also means some learners may need to extend their training, this should already be part of GME programs that are required to have remediation policies for learners who are not progressing as expected.
AN OPPORTUNITY FOR PHM
Time variability is an oft-cited tenet of CBME,2,3 but one that is being piloted by relatively few programs in the United States, mostly in undergraduate medical education (UME).14-16 The Education in Pediatrics Across the Continuum (EPAC), a consortium consisting of four institutions piloting CBTVT in UME,14 has shown early evidence of feasibility17 and that UME graduates from CBTVT programs enter residency with levels of competence similar to those of graduates of traditional time-based programs.18 We believe that PHM can take a step toward truly realizing CBME by implementing CBTVT in fellowship programs.
There are multiple reasons why this is an opportune time for PHM fellowships to consider CBTVT. First, PHM is a relatively new board-certified subspecialty with a recently revised set of core competencies1 that are likely to catalyze programmatic innovation. A key step in change management is building on previous efforts to generate more change.19 Programs can leverage the momentum from current and impending change initiatives to innovate and implement CBTVT. Second, the revised PHM competencies provide the first crucial step in implementing a CBME program by defining desired training outcomes necessary to deliver high-quality patient care. With PHM competencies now well defined, programs can focus on developing programs of assessment and corresponding faculty development, which can help deliver valid, defensible decisions about fellow competence.
Finally, PHM has a workforce that can support CBTVT. A major barrier to time-variable training in GME is the need for trainees-as-workforce. In many GME programs, residents and fellows provide a relatively inexpensive, renewable workforce. Trainees’ clinical rotations are often scheduled up to 1 year in advance to ensure care teams are fully staffed, particularly in the inpatient setting, creating a system where flexibility in training is impossible without creating gaps in clinical coverage. However, many PHM fellowships do not completely rely on fellows to cover clinical service lines. PHM fellows spend 32 weeks over 2 years in core clinical rotations with faculty supervision, in accordance with the Accreditation Council for Graduate Medical Education program requirements, both for 2- and 3-year programs. Some CBME experts estimate (based on previous and ongoing CBTVT pilots) that training duration is likely to vary by roughly 20% from current time-based practices when CBTVT is initially implemented.20 Thus, only a small number of clinical service weeks are likely to be affected. If a fellow were deemed ready for unsupervised practice before finishing 2 years of fellowship in a CBTVT program, the corresponding faculty supervisor could use the time previously assigned for supervision to pursue other priorities, such as education, scholarship, or quality improvement. Why provide supervision if a clinical competency committee has deemed a fellow ready for unsupervised practice? Some level of observation and formative feedback could continue, but full supervision would be redundant and unnecessary. CBTVT would allow for some fellows to experience the uncertainty that comes with unsupervised decision-making while still in an environment with trusted fellowship mentors and advisors.
STEPS TOWARD CHANGE
PHM fellowship programs likely cannot flip a switch to “turn on” CBTVT immediately, but they can take steps toward making the transition. Validity, or defensibility of decisions, will be crucial for assessment in CBTVT systems. Programs will need to develop robust assessment systems that collect myriad data to answer the question, “When is this learner competent to deliver high-quality care without supervision?” Programs can align assessment instruments, faculty-development initiatives, and clinical competency committee (CCC) processes with the 2020 PHM competencies to provide a defensible answer. Program leaders should then seek validity evidence, either in existing literature or through novel scholarly initiatives, to support these summative decisions. Engaging all fellowship stakeholders in transitions to CBTVT will be important and should include fellows, program directors, CCC members, clinical leadership, and members from accrediting and credentialing bodies.
CONCLUSION
As fellowship programs review and revise curricula and assessment systems around the updated PHM core competencies, they should also consider what changes are necessary to implement CBTVT. Time variability is not a novelty but, rather, is a corollary to the outcomes-based approach of CBME. PHM fellowships should strike while the iron is hot and build on current change initiatives prompted by the growth of our specialty to be leaders in CBTVT.
1. Maniscalco J, Gage S, Sofia Teferi M, Fisher ES. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
2. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638-645. https://doi.org/10.3109/0142159X.2010.501190
3. Lucey CR, Thibault GE, Ten Cate O. Competency-based, tme-variable education in the health professions: crossroads. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S1-S5. https://doi.org/10.1097/ACM.0000000000002080
4. Custers EJFM, Ten Cate O. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S49-S54. https://doi.org/10.1097/ACM.0000000000002079
5. Barr DA. Revolution or evolution? Putting the Flexner Report in context. Med Educ. 2011;45(1):17-22. https://doi.org/10.1111/j.1365-2923.2010.03850.x
6. Association of American Medical Colleges. Minutes of the Fifteenth Annual Meeting. April 10, 1905; Chicago, IL.
7. Bevan A. Council on Medical Education of the American Medical Association. JAMA. 1907;48(20):1701-1707.
8. Flexner A. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, Bulletin Number Four, 1910. Bull World Health Organ. 2002;80(7):594-602.
9. McGaghie WC, Sajid AW, Miller GE, et al. Competency-based curriculum development in medical education: an introduction. Public Health Pap. 1978;(68):11-91.
10. Frank JR, Snell L, Englander R, Holmboe ES, ICBME Collaborators. Implementing competency-based medical education: moving forward. Med Teach. 2017;39(6):568-573. https://doi.org/10.1080/0142159X.2017.1315069
11. Schumacher DJ, West DC, Schwartz A, et al. Longitudinal assessment of resident performance using entrustable professional activities. JAMA Netw Open. 2020;3(1):e1919316. https://doi.org/10.1001/jamanetworkopen.2019.19316
12. Warm EJ, Held J, Hellman M, et al. Entrusting observable practice activities and milestones over the 36 months of an internal medicine residency. Acad Med. 2016;91(10):1398-1405. https://doi.org/10.1097/ACM.0000000000001292
13. Jason H. Effective medical instruction: requirements and possibilities. In: Proceedings of a 1969 International Symposium on Medical Education. Medica; 1970:5-8.
14. Andrews JS, Bale JF Jr, Soep JB, et al. Education in Pediatrics Across the Continuum (EPAC): first steps toward realizing the dream of competency-based education. Acad Med. 2018;93(3):414-420. https://doi.org/10.1097/ACM.0000000000002020
15. Mejicano GC, Bumsted TN. Describing the journey and lessons learned implementing a competency-based, time-variable undergraduate medical education curriculum. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S42-S48. https://doi.org/10.1097/ACM.0000000000002068
16. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
17. Murray KE, Lane JL, Carraccio C, et al. Crossing the gap: using competency-based assessment to determine whether learners are ready for the undergraduate-to-graduate transition. Acad Med. 2019;94(3):338-345. https://doi.org/10.1097/ACM.0000000000002535
18. Schwartz A, Balmer DF, Borman-Shoap E, et al. Shared mental models among clinical competency committees in the context of time-variable, competency-based advancement to residency. Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S95-S102. https://doi.org/10.1097/ACM.0000000000003638
19. Kotter JP. Leading change: why transformation efforts fail. Harvard Business Review. May-June 1995. Accessed March 1, 2021. https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2
20. Schumacher DJ, Caretta-Weyer H, Busari J, et al. Competency-based time-variable training internationally: ensuring practical next steps. Med Teach. Forthcoming.
1. Maniscalco J, Gage S, Sofia Teferi M, Fisher ES. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
2. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638-645. https://doi.org/10.3109/0142159X.2010.501190
3. Lucey CR, Thibault GE, Ten Cate O. Competency-based, tme-variable education in the health professions: crossroads. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S1-S5. https://doi.org/10.1097/ACM.0000000000002080
4. Custers EJFM, Ten Cate O. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S49-S54. https://doi.org/10.1097/ACM.0000000000002079
5. Barr DA. Revolution or evolution? Putting the Flexner Report in context. Med Educ. 2011;45(1):17-22. https://doi.org/10.1111/j.1365-2923.2010.03850.x
6. Association of American Medical Colleges. Minutes of the Fifteenth Annual Meeting. April 10, 1905; Chicago, IL.
7. Bevan A. Council on Medical Education of the American Medical Association. JAMA. 1907;48(20):1701-1707.
8. Flexner A. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, Bulletin Number Four, 1910. Bull World Health Organ. 2002;80(7):594-602.
9. McGaghie WC, Sajid AW, Miller GE, et al. Competency-based curriculum development in medical education: an introduction. Public Health Pap. 1978;(68):11-91.
10. Frank JR, Snell L, Englander R, Holmboe ES, ICBME Collaborators. Implementing competency-based medical education: moving forward. Med Teach. 2017;39(6):568-573. https://doi.org/10.1080/0142159X.2017.1315069
11. Schumacher DJ, West DC, Schwartz A, et al. Longitudinal assessment of resident performance using entrustable professional activities. JAMA Netw Open. 2020;3(1):e1919316. https://doi.org/10.1001/jamanetworkopen.2019.19316
12. Warm EJ, Held J, Hellman M, et al. Entrusting observable practice activities and milestones over the 36 months of an internal medicine residency. Acad Med. 2016;91(10):1398-1405. https://doi.org/10.1097/ACM.0000000000001292
13. Jason H. Effective medical instruction: requirements and possibilities. In: Proceedings of a 1969 International Symposium on Medical Education. Medica; 1970:5-8.
14. Andrews JS, Bale JF Jr, Soep JB, et al. Education in Pediatrics Across the Continuum (EPAC): first steps toward realizing the dream of competency-based education. Acad Med. 2018;93(3):414-420. https://doi.org/10.1097/ACM.0000000000002020
15. Mejicano GC, Bumsted TN. Describing the journey and lessons learned implementing a competency-based, time-variable undergraduate medical education curriculum. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S42-S48. https://doi.org/10.1097/ACM.0000000000002068
16. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
17. Murray KE, Lane JL, Carraccio C, et al. Crossing the gap: using competency-based assessment to determine whether learners are ready for the undergraduate-to-graduate transition. Acad Med. 2019;94(3):338-345. https://doi.org/10.1097/ACM.0000000000002535
18. Schwartz A, Balmer DF, Borman-Shoap E, et al. Shared mental models among clinical competency committees in the context of time-variable, competency-based advancement to residency. Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S95-S102. https://doi.org/10.1097/ACM.0000000000003638
19. Kotter JP. Leading change: why transformation efforts fail. Harvard Business Review. May-June 1995. Accessed March 1, 2021. https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2
20. Schumacher DJ, Caretta-Weyer H, Busari J, et al. Competency-based time-variable training internationally: ensuring practical next steps. Med Teach. Forthcoming.
© 2021 Society of Hospital Medicine
Development and Evolution of Hospital Medicine in Korea
The healthcare system in South Korea (Korea) is evolving. Korea began developing a national health insurance system for the entire population in 1989, and implementation took 12 years. The healthcare insurance premium was set in 1989 when the Korean gross domestic product (GDP) per capita was less than $5,000 USD. Since then, the incremental rise in healthcare insurance premiums, approximately 6% of the typical Korean income, has been relatively small considering the economic growth of Korea.1-3 The success and rapid adoption of national health insurance in Korea revealed unanticipated problems in three specific areas: low individual contributions relative to costs of care, low levels of reimbursement to providers, and incomplete coverage of medical services, which then require out-of-pocket payments (typically 20% of the inpatient care fee).4 Additionally, while little attention has been paid to quality and safety in the past, the nation has come to recognize the importance of these considerations,5 particularly with regard to patient expectations for and consumption of medical care and the consequent demand for better services from the medical community and government.6
Healthcare constitutes about 7.5% of Korea’s GDP. In contrast, healthcare spending accounts for about 17.7% of US GDP and about 8.8% of the GDP of member nations of the Organisation for Economic Co-operation and Development (OECD) in aggregate. Additionally, Korea has a longer length of hospital stay (16.5 days vs 7.3 days for OECD countries) and fewer practicing physicians (1.1 per 1,000 persons vs 1.9 per 1,000 for OECD countries). Therefore, the average cumulative annual patient hospital days per physician is 2,394 days in Korea, three times higher than that in the OECD countries.7 Furthermore, the number of physicians providing hospital care in Korea has remained relatively low.8
Despite recent growth in the total number of practicing physicians, the number of hospital-based physicians remains insufficient to cover admitted patients. The pressure for hospital-based physicians to serve large numbers of patients to generate sufficient revenue has deterred growth of more physicians focused on inpatient care.6 In order to operate the hospital, doctors must see as many patients as possible because physicians are reimbursed primarily by an inpatient care fee rather than by type or extent of care provided. Therefore, this low fee schedule makes it difficult to provide good quality inpatient care while simultaneously trying to increase accessibility. The costs of testing and treatment are reimbursed through a separate fee schedule.
THE NEED FOR A HOSPITALIST SYSTEM IN KOREA
The Korean government enacted two new policies regarding medical school graduates and residents that led to implementation of a hospitalist system. The first policy created a quota of medical residents to match the total number of medical school graduates.9 Before the new regulation, the number of medical resident positions exceeded the number of medical school graduates by 20%, which led to a shortage of resident applicants in “unpopular” medical specialties or departments. These specialties (eg, general surgery, obstetrics and gynecology, urology) have a lower fee schedule, which leads to lower wages while having very high workloads. The decrease in the number of available medical resident positions results in greater workloads for physicians providing inpatient care. These changes, including the shortage of a resident workforce, led to a burgeoning hospital-based attending physician workforce to care for hospitalized patients.
The other policy, created in December 2015 and known as the Act on the Improvement of Training Conditions and Status of Medical Residents, was enacted to improve working conditions for residents by limiting their working hours to 80 or fewer per week.10 These work-hour restrictions made it nearly impossible to provide 24-hour inpatient care depending solely on residents.10-12 This policy increased the need for hospitalists in Korea, similar to that of the US Accreditation Council for Graduate Medical Education in 2003, which limited resident work hours. Because of these changes, the hospitalist model was introduced to manage the growing volume of inpatients at teaching hospitals.13
The institutional implementation of the Korean hospitalist system was catalyzed by the need to solve current problems such as patient safety, healthcare quality, and residents’ well-being.8,14 Therefore, the hospitalist system was designed and implemented to meet the needs of patients, medical professionals, and hospitals.6,8,14 Furthermore, under the universal health insurance system in Korea, institutional implementation also meant creating a new set of fee schedules for hospitalists. The Korean hospitalist system reflects the nuances and challenges faced by the Korean healthcare system.5
DESIGN, IMPLEMENTATION, AND EVALUATION
A council was formed to implement a hospitalist model suitable for Korea. The council was composed of five groups: the Korean Association of Internal Medicine, Korean Surgical Society, Korean Medical Association, Korean Hospital Association, and Korean Academy of Medical Sciences. The Korean Association of Internal Medicine and the Korean Surgical Society were involved in creating a new medical discipline because their members provided a disproportionate amount of inpatient care and were most often responsible for hospital patient safety and quality care. Along with the support of the council, the Ministry of Health and Welfare began to realize the high demand on inpatient care and requested an official proposal to broaden the hospitalist model, with two conditions. First, the government requested a unified proposal from the medical community that reflected the collective voices of individual stakeholders, with an expectation that the new system would focus on patient safety and healthcare quality across all specialties. Second, the proposal had to be detailed and include a specific fee schedule for hospitalist services.
Before implementing a national hospitalist system, we conducted a pilot study supported by funding from the council. This first study, the Korean Hospitalist System Operation and Evaluation Research (September 2015 to August 2016)14, was designed to (a) determine hospitalist needs (eg, rotation schedule, salary, working conditions) for this new profession, (b) determine the necessary number of hospitalists and appropriate fee schedules to cover salary and benefits, and (c) provide Korean hospitalist models with operational methods to facilitate implementation at individual institutions. The council and research team selected four hospitals for the privately funded pilot study (Table). These hospitals already had an inpatient care system managed by specialists prior to the pilot study, so major changes in patient care and hospital operations were not required.
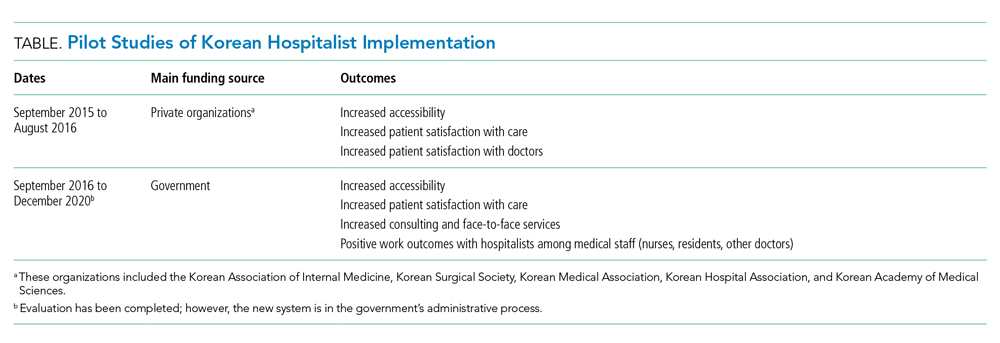
The pilot study demonstrated improvements in patient satisfaction, medical service quality, and patient safety.8,14,15 As a result, fees billed from hospitalist services were now covered by national health insurance; previously, they were not covered by any inpatient care fee or bundled service fee. The next study (phase 2) was then conducted to evaluate the national implementation of the hospitalist system and its outcomes. The first phase defined criteria for monitoring and evaluating the institutionalized hospitalist system in Korea. The second phase, initiated in September 2016, evaluated how the implemented system could be expanded nationwide. The government was actively involved in the study; 31 of 344 (9%) general hospitals were selected and able to apply the hospitalist fee schedule for care of patients who were admitted to the hospitalist ward.
To investigate the effect of the hospitalist system, we measured the satisfaction of patients and medical providers (eg, specialists, residents, and nurses). The outcomes were number of doctors’ calls to hospitalists and to other specialties, duration of time required to address medical problems, number of contacts with the hospitalist (residents or other physicians in the control group), and time spent with hospitalized patients. In addition, we analyzed claims costs and the operating costs for implementing the system within each hospital (Table).
The new set of fee schedules was created specifically for hospitalist care services so hospitals could now claim separate inpatient care fees and hospitalist fees. The standard hospitalist fee schedule is applied only to patients who are on hospitalist-led wards. The fee schedule has two criteria: The hospitalist ward must have 50 beds which are assigned to hospitalists only, and each hospitalist ward has a team of five hospitalists. A maximum of 25 patients could be assigned to an individual hospitalist. However, fees can be adjusted based on individual hospital operation and management after government approval.
Under the national insurance system, the fee schedule is essential to obtain reimbursement for provided services. As a new medical profession, it is important to have the institutional implementation of the hospitalist system. In contrast to those in the United States, inpatients in Korea pay inpatient care fees only, which are charged per day. Therefore, reducing the length of stay without increasing patient volume does not financially benefit the hospital.
DEFINITION OF A KOREAN HOSPITALIST AND SCOPE OF PRACTICE
The definition of a Korean hospitalist was carefully developed, and a reimbursement system for hospitalists was created within the Korean healthcare system. All hospitalists are medical specialists who have completed advanced education and clinical training in their specialty area (internal medicine or surgery). Creating a definition of a hospitalist and a standard fee schedule was necessary for national incorporation of this new approach. The model must also be accepted by related parties, including healthcare professionals such as hospital executives, nonhospitalist doctors, and nurses. Therefore, the system has a minimum of two requirements to operate at the hospital level, and the remaining factors can be modified by individual hospitals to protect the new discipline within the healthcare system. First, hospitalist services are provided only to hospitalist patients. To establish the new system, limiting the patient range to a specific group was necessary to prevent abuse of human-based resources within the hospital. Second, hospitalists must be stationed near the hospitalist ward to enhance accessibility, patient safety, and healthcare quality. In other words, a hospitalist provides services to hospitalized patients who paid the hospitalist fee, and the hospitalist does not provide care beyond the hospitalist ward (eg, they cannot provide outpatient consultation or provide care on other wards).
INPATIENT CARE REIMBURSEMENT BEFORE AND AFTER IMPLEMENTATION
Korean national health insurance is the universal health insurance under a single insurer (ie, the government). Therefore, all Korean citizens have national health insurance. Individuals can choose to have additional health insurance (private insurance) if they wish to pay an out-of-pocket fee with their additional private insurance. In Korea, the inpatient care fee includes all fees to provide care for the patient during hospital stays, such as the physician fee, facility fee, and consultation fee. The inpatient care fee schedule is charged per day including all the inpatient care composition. The claim and reimbursement system is different in Korea in that the hospital as a whole submits the claim for reimbursement. There is no separate claim from physicians, lab technicians, or facilities. Doctors provide care to patients and are then paid for the services in terms of salaries. Since the original inpatient care fee schedule was low and insufficient, it was difficult to provide high-quality care. Also, resources for spending on inpatient care management was limited. So a new system to improve inpatient care was needed. Implementing the hospitalist system in Korea led to the creation of a new fee schedule specifically for hospitalists so that hospitals could claim hospitalist fees on top of inpatient care fees when the patient was cared for by the hospitalist. The additional fees in the hospitalist fee schedule allow safe and high-quality care to be provided for patients during hospital stays.
KOREAN HOSPITAL MEDICINE TODAY
The Korean hospitalist system has been implemented for 3 years with the government’s active involvement, with approximately 250 specialists working as hospitalists as of August 2020. Importantly, Korean hospitalists are not limited to internal medicine specialists; in fact, several different specialties practice as hospitalists, including surgeons and other medical specialists, who account for 20% and 30% of the hospitalist workforce, respectively. Since the system’s implementation, all inpatient care and management is now transferred to specialists from residents in hospitalist wards. This change has increased patient safety and care quality. At the beginning of the pilot study, the concept of a “hospitalist” was new in Korea and the public did not know who a hospitalist was nor what a hospitalist did. However, after 3 years, patients now seek hospitalist care.
CONCLUSION
National implementation of the hospitalist model represents a key paradigm shift in the Korean healthcare system. The Korean hospitalist system is the result of the hospitals’, doctors’, and patients’ desire for higher-quality care. We expect to see growth of hospitalists in Korea and provision of better, safer, and more efficient inpatient care across specialties, payers, and government. Since we are at the early stage of the system, further efforts to support implementation are required. We hope our implementation process of a new medical system could serve as a model for other countries who are seeking to adopt hospitalist systems within their current healthcare paradigms.
Acknowledgments
The authors thank the medical professionals, government officers, and other professionals who put great effort into the implementation of the Korean Hospitalist System.
1. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009;24(1):63-71. https://doi.org/10.1093/heapol/czn037
2. Song YJ. The South Korean health care system. JMAJ. 2009;52(3):206-209.
3. Park YH, Park E-C. Healthcare policy. In: Preventive Medicine and Public Health. Vol 3.Gyechuk; 2017:821-833.
4. Park E-C, Lee TJ, Jun BY, Jung SH, Jeong HS. Health security. In: Preventive Medicine and Public Health. Vol 3. Gyechuk; 2017:888-897.
5. Jang S-I, Jang S-y, Park E-C. Trends of US hospitalist and suggestions for introduction of Korean hospitalist. Korean J Med. 2015;89(1):1-5. http://doi.org/10.3904/kjm.2015.89.1.1
6. Jang S-I. Korean hospitalist system implementation and development strategies based on pilot studies. J Korean Med Assoc. 2019;62(11):558-563. http://doi.org/10.5124/jkma.2019.62.11.558
7. OECD. Health at a Glance 2017: OECD indicators. OECD iLibrary. 2017. Accessed September 27, 2019. https://doi.org/10.1787/health_glance-2017-en
8. Jang S-I, Park E-C, Nam JM, et al. A study on the implementation and the evaluation of Korean Hospitalist System to improve the quality of hospitalization (Phase 2). Institute of Health Services Research, Yonsei University; 2018.
9. Koh DY. Political strategies to enhance medical residents. Health Policy. Vol 37. Seoul National University Hospital; 2014.
10. Act on the Improvement of Training Conditions and Status of Medical Residents. Vol No. 16260: Ministry of Health and Welfare; 2015.
11. Eom JS. Operating the hospitalist system. J Korean Med Assoc. 2016;59(5):342-344. http://doi.org/10.5124/jkma.2016.59.5.342
12. Kim S-S. Working conditions of interns/residents and patient safety: Painful training might not be authentic. J Korean Med Assoc. 2016;59(2):82-84. http://dx.doi.org/10.5124/jkma.2016.59.2.82
13. Oshimura J, Sperring J, Bauer BD, Rauch DA. Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299-303. https://doi.org/10.1002/jhm.952
14. Park E-C, Lee SG, Kim T-H, et al. A study on the implementation and the evaluation of Korean Hospitalist System to improve the quality of hospitalization (Phase 1). Institute of Health Services Research, Yonsei University; 2016.
15. Jang S-I, Jung E-J, Park SK, Chae W, Kim Y-K. A study on the feasibility of the Korean hospitalist system and cost estimation. Ministry of Health and Welfare, Institute of Health Service Research Yonsei University; 2019.
The healthcare system in South Korea (Korea) is evolving. Korea began developing a national health insurance system for the entire population in 1989, and implementation took 12 years. The healthcare insurance premium was set in 1989 when the Korean gross domestic product (GDP) per capita was less than $5,000 USD. Since then, the incremental rise in healthcare insurance premiums, approximately 6% of the typical Korean income, has been relatively small considering the economic growth of Korea.1-3 The success and rapid adoption of national health insurance in Korea revealed unanticipated problems in three specific areas: low individual contributions relative to costs of care, low levels of reimbursement to providers, and incomplete coverage of medical services, which then require out-of-pocket payments (typically 20% of the inpatient care fee).4 Additionally, while little attention has been paid to quality and safety in the past, the nation has come to recognize the importance of these considerations,5 particularly with regard to patient expectations for and consumption of medical care and the consequent demand for better services from the medical community and government.6
Healthcare constitutes about 7.5% of Korea’s GDP. In contrast, healthcare spending accounts for about 17.7% of US GDP and about 8.8% of the GDP of member nations of the Organisation for Economic Co-operation and Development (OECD) in aggregate. Additionally, Korea has a longer length of hospital stay (16.5 days vs 7.3 days for OECD countries) and fewer practicing physicians (1.1 per 1,000 persons vs 1.9 per 1,000 for OECD countries). Therefore, the average cumulative annual patient hospital days per physician is 2,394 days in Korea, three times higher than that in the OECD countries.7 Furthermore, the number of physicians providing hospital care in Korea has remained relatively low.8
Despite recent growth in the total number of practicing physicians, the number of hospital-based physicians remains insufficient to cover admitted patients. The pressure for hospital-based physicians to serve large numbers of patients to generate sufficient revenue has deterred growth of more physicians focused on inpatient care.6 In order to operate the hospital, doctors must see as many patients as possible because physicians are reimbursed primarily by an inpatient care fee rather than by type or extent of care provided. Therefore, this low fee schedule makes it difficult to provide good quality inpatient care while simultaneously trying to increase accessibility. The costs of testing and treatment are reimbursed through a separate fee schedule.
THE NEED FOR A HOSPITALIST SYSTEM IN KOREA
The Korean government enacted two new policies regarding medical school graduates and residents that led to implementation of a hospitalist system. The first policy created a quota of medical residents to match the total number of medical school graduates.9 Before the new regulation, the number of medical resident positions exceeded the number of medical school graduates by 20%, which led to a shortage of resident applicants in “unpopular” medical specialties or departments. These specialties (eg, general surgery, obstetrics and gynecology, urology) have a lower fee schedule, which leads to lower wages while having very high workloads. The decrease in the number of available medical resident positions results in greater workloads for physicians providing inpatient care. These changes, including the shortage of a resident workforce, led to a burgeoning hospital-based attending physician workforce to care for hospitalized patients.
The other policy, created in December 2015 and known as the Act on the Improvement of Training Conditions and Status of Medical Residents, was enacted to improve working conditions for residents by limiting their working hours to 80 or fewer per week.10 These work-hour restrictions made it nearly impossible to provide 24-hour inpatient care depending solely on residents.10-12 This policy increased the need for hospitalists in Korea, similar to that of the US Accreditation Council for Graduate Medical Education in 2003, which limited resident work hours. Because of these changes, the hospitalist model was introduced to manage the growing volume of inpatients at teaching hospitals.13
The institutional implementation of the Korean hospitalist system was catalyzed by the need to solve current problems such as patient safety, healthcare quality, and residents’ well-being.8,14 Therefore, the hospitalist system was designed and implemented to meet the needs of patients, medical professionals, and hospitals.6,8,14 Furthermore, under the universal health insurance system in Korea, institutional implementation also meant creating a new set of fee schedules for hospitalists. The Korean hospitalist system reflects the nuances and challenges faced by the Korean healthcare system.5
DESIGN, IMPLEMENTATION, AND EVALUATION
A council was formed to implement a hospitalist model suitable for Korea. The council was composed of five groups: the Korean Association of Internal Medicine, Korean Surgical Society, Korean Medical Association, Korean Hospital Association, and Korean Academy of Medical Sciences. The Korean Association of Internal Medicine and the Korean Surgical Society were involved in creating a new medical discipline because their members provided a disproportionate amount of inpatient care and were most often responsible for hospital patient safety and quality care. Along with the support of the council, the Ministry of Health and Welfare began to realize the high demand on inpatient care and requested an official proposal to broaden the hospitalist model, with two conditions. First, the government requested a unified proposal from the medical community that reflected the collective voices of individual stakeholders, with an expectation that the new system would focus on patient safety and healthcare quality across all specialties. Second, the proposal had to be detailed and include a specific fee schedule for hospitalist services.
Before implementing a national hospitalist system, we conducted a pilot study supported by funding from the council. This first study, the Korean Hospitalist System Operation and Evaluation Research (September 2015 to August 2016)14, was designed to (a) determine hospitalist needs (eg, rotation schedule, salary, working conditions) for this new profession, (b) determine the necessary number of hospitalists and appropriate fee schedules to cover salary and benefits, and (c) provide Korean hospitalist models with operational methods to facilitate implementation at individual institutions. The council and research team selected four hospitals for the privately funded pilot study (Table). These hospitals already had an inpatient care system managed by specialists prior to the pilot study, so major changes in patient care and hospital operations were not required.
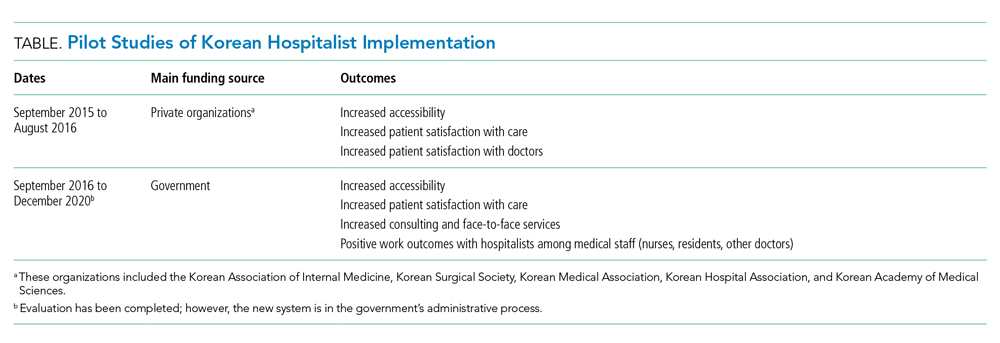
The pilot study demonstrated improvements in patient satisfaction, medical service quality, and patient safety.8,14,15 As a result, fees billed from hospitalist services were now covered by national health insurance; previously, they were not covered by any inpatient care fee or bundled service fee. The next study (phase 2) was then conducted to evaluate the national implementation of the hospitalist system and its outcomes. The first phase defined criteria for monitoring and evaluating the institutionalized hospitalist system in Korea. The second phase, initiated in September 2016, evaluated how the implemented system could be expanded nationwide. The government was actively involved in the study; 31 of 344 (9%) general hospitals were selected and able to apply the hospitalist fee schedule for care of patients who were admitted to the hospitalist ward.
To investigate the effect of the hospitalist system, we measured the satisfaction of patients and medical providers (eg, specialists, residents, and nurses). The outcomes were number of doctors’ calls to hospitalists and to other specialties, duration of time required to address medical problems, number of contacts with the hospitalist (residents or other physicians in the control group), and time spent with hospitalized patients. In addition, we analyzed claims costs and the operating costs for implementing the system within each hospital (Table).
The new set of fee schedules was created specifically for hospitalist care services so hospitals could now claim separate inpatient care fees and hospitalist fees. The standard hospitalist fee schedule is applied only to patients who are on hospitalist-led wards. The fee schedule has two criteria: The hospitalist ward must have 50 beds which are assigned to hospitalists only, and each hospitalist ward has a team of five hospitalists. A maximum of 25 patients could be assigned to an individual hospitalist. However, fees can be adjusted based on individual hospital operation and management after government approval.
Under the national insurance system, the fee schedule is essential to obtain reimbursement for provided services. As a new medical profession, it is important to have the institutional implementation of the hospitalist system. In contrast to those in the United States, inpatients in Korea pay inpatient care fees only, which are charged per day. Therefore, reducing the length of stay without increasing patient volume does not financially benefit the hospital.
DEFINITION OF A KOREAN HOSPITALIST AND SCOPE OF PRACTICE
The definition of a Korean hospitalist was carefully developed, and a reimbursement system for hospitalists was created within the Korean healthcare system. All hospitalists are medical specialists who have completed advanced education and clinical training in their specialty area (internal medicine or surgery). Creating a definition of a hospitalist and a standard fee schedule was necessary for national incorporation of this new approach. The model must also be accepted by related parties, including healthcare professionals such as hospital executives, nonhospitalist doctors, and nurses. Therefore, the system has a minimum of two requirements to operate at the hospital level, and the remaining factors can be modified by individual hospitals to protect the new discipline within the healthcare system. First, hospitalist services are provided only to hospitalist patients. To establish the new system, limiting the patient range to a specific group was necessary to prevent abuse of human-based resources within the hospital. Second, hospitalists must be stationed near the hospitalist ward to enhance accessibility, patient safety, and healthcare quality. In other words, a hospitalist provides services to hospitalized patients who paid the hospitalist fee, and the hospitalist does not provide care beyond the hospitalist ward (eg, they cannot provide outpatient consultation or provide care on other wards).
INPATIENT CARE REIMBURSEMENT BEFORE AND AFTER IMPLEMENTATION
Korean national health insurance is the universal health insurance under a single insurer (ie, the government). Therefore, all Korean citizens have national health insurance. Individuals can choose to have additional health insurance (private insurance) if they wish to pay an out-of-pocket fee with their additional private insurance. In Korea, the inpatient care fee includes all fees to provide care for the patient during hospital stays, such as the physician fee, facility fee, and consultation fee. The inpatient care fee schedule is charged per day including all the inpatient care composition. The claim and reimbursement system is different in Korea in that the hospital as a whole submits the claim for reimbursement. There is no separate claim from physicians, lab technicians, or facilities. Doctors provide care to patients and are then paid for the services in terms of salaries. Since the original inpatient care fee schedule was low and insufficient, it was difficult to provide high-quality care. Also, resources for spending on inpatient care management was limited. So a new system to improve inpatient care was needed. Implementing the hospitalist system in Korea led to the creation of a new fee schedule specifically for hospitalists so that hospitals could claim hospitalist fees on top of inpatient care fees when the patient was cared for by the hospitalist. The additional fees in the hospitalist fee schedule allow safe and high-quality care to be provided for patients during hospital stays.
KOREAN HOSPITAL MEDICINE TODAY
The Korean hospitalist system has been implemented for 3 years with the government’s active involvement, with approximately 250 specialists working as hospitalists as of August 2020. Importantly, Korean hospitalists are not limited to internal medicine specialists; in fact, several different specialties practice as hospitalists, including surgeons and other medical specialists, who account for 20% and 30% of the hospitalist workforce, respectively. Since the system’s implementation, all inpatient care and management is now transferred to specialists from residents in hospitalist wards. This change has increased patient safety and care quality. At the beginning of the pilot study, the concept of a “hospitalist” was new in Korea and the public did not know who a hospitalist was nor what a hospitalist did. However, after 3 years, patients now seek hospitalist care.
CONCLUSION
National implementation of the hospitalist model represents a key paradigm shift in the Korean healthcare system. The Korean hospitalist system is the result of the hospitals’, doctors’, and patients’ desire for higher-quality care. We expect to see growth of hospitalists in Korea and provision of better, safer, and more efficient inpatient care across specialties, payers, and government. Since we are at the early stage of the system, further efforts to support implementation are required. We hope our implementation process of a new medical system could serve as a model for other countries who are seeking to adopt hospitalist systems within their current healthcare paradigms.
Acknowledgments
The authors thank the medical professionals, government officers, and other professionals who put great effort into the implementation of the Korean Hospitalist System.
The healthcare system in South Korea (Korea) is evolving. Korea began developing a national health insurance system for the entire population in 1989, and implementation took 12 years. The healthcare insurance premium was set in 1989 when the Korean gross domestic product (GDP) per capita was less than $5,000 USD. Since then, the incremental rise in healthcare insurance premiums, approximately 6% of the typical Korean income, has been relatively small considering the economic growth of Korea.1-3 The success and rapid adoption of national health insurance in Korea revealed unanticipated problems in three specific areas: low individual contributions relative to costs of care, low levels of reimbursement to providers, and incomplete coverage of medical services, which then require out-of-pocket payments (typically 20% of the inpatient care fee).4 Additionally, while little attention has been paid to quality and safety in the past, the nation has come to recognize the importance of these considerations,5 particularly with regard to patient expectations for and consumption of medical care and the consequent demand for better services from the medical community and government.6
Healthcare constitutes about 7.5% of Korea’s GDP. In contrast, healthcare spending accounts for about 17.7% of US GDP and about 8.8% of the GDP of member nations of the Organisation for Economic Co-operation and Development (OECD) in aggregate. Additionally, Korea has a longer length of hospital stay (16.5 days vs 7.3 days for OECD countries) and fewer practicing physicians (1.1 per 1,000 persons vs 1.9 per 1,000 for OECD countries). Therefore, the average cumulative annual patient hospital days per physician is 2,394 days in Korea, three times higher than that in the OECD countries.7 Furthermore, the number of physicians providing hospital care in Korea has remained relatively low.8
Despite recent growth in the total number of practicing physicians, the number of hospital-based physicians remains insufficient to cover admitted patients. The pressure for hospital-based physicians to serve large numbers of patients to generate sufficient revenue has deterred growth of more physicians focused on inpatient care.6 In order to operate the hospital, doctors must see as many patients as possible because physicians are reimbursed primarily by an inpatient care fee rather than by type or extent of care provided. Therefore, this low fee schedule makes it difficult to provide good quality inpatient care while simultaneously trying to increase accessibility. The costs of testing and treatment are reimbursed through a separate fee schedule.
THE NEED FOR A HOSPITALIST SYSTEM IN KOREA
The Korean government enacted two new policies regarding medical school graduates and residents that led to implementation of a hospitalist system. The first policy created a quota of medical residents to match the total number of medical school graduates.9 Before the new regulation, the number of medical resident positions exceeded the number of medical school graduates by 20%, which led to a shortage of resident applicants in “unpopular” medical specialties or departments. These specialties (eg, general surgery, obstetrics and gynecology, urology) have a lower fee schedule, which leads to lower wages while having very high workloads. The decrease in the number of available medical resident positions results in greater workloads for physicians providing inpatient care. These changes, including the shortage of a resident workforce, led to a burgeoning hospital-based attending physician workforce to care for hospitalized patients.
The other policy, created in December 2015 and known as the Act on the Improvement of Training Conditions and Status of Medical Residents, was enacted to improve working conditions for residents by limiting their working hours to 80 or fewer per week.10 These work-hour restrictions made it nearly impossible to provide 24-hour inpatient care depending solely on residents.10-12 This policy increased the need for hospitalists in Korea, similar to that of the US Accreditation Council for Graduate Medical Education in 2003, which limited resident work hours. Because of these changes, the hospitalist model was introduced to manage the growing volume of inpatients at teaching hospitals.13
The institutional implementation of the Korean hospitalist system was catalyzed by the need to solve current problems such as patient safety, healthcare quality, and residents’ well-being.8,14 Therefore, the hospitalist system was designed and implemented to meet the needs of patients, medical professionals, and hospitals.6,8,14 Furthermore, under the universal health insurance system in Korea, institutional implementation also meant creating a new set of fee schedules for hospitalists. The Korean hospitalist system reflects the nuances and challenges faced by the Korean healthcare system.5
DESIGN, IMPLEMENTATION, AND EVALUATION
A council was formed to implement a hospitalist model suitable for Korea. The council was composed of five groups: the Korean Association of Internal Medicine, Korean Surgical Society, Korean Medical Association, Korean Hospital Association, and Korean Academy of Medical Sciences. The Korean Association of Internal Medicine and the Korean Surgical Society were involved in creating a new medical discipline because their members provided a disproportionate amount of inpatient care and were most often responsible for hospital patient safety and quality care. Along with the support of the council, the Ministry of Health and Welfare began to realize the high demand on inpatient care and requested an official proposal to broaden the hospitalist model, with two conditions. First, the government requested a unified proposal from the medical community that reflected the collective voices of individual stakeholders, with an expectation that the new system would focus on patient safety and healthcare quality across all specialties. Second, the proposal had to be detailed and include a specific fee schedule for hospitalist services.
Before implementing a national hospitalist system, we conducted a pilot study supported by funding from the council. This first study, the Korean Hospitalist System Operation and Evaluation Research (September 2015 to August 2016)14, was designed to (a) determine hospitalist needs (eg, rotation schedule, salary, working conditions) for this new profession, (b) determine the necessary number of hospitalists and appropriate fee schedules to cover salary and benefits, and (c) provide Korean hospitalist models with operational methods to facilitate implementation at individual institutions. The council and research team selected four hospitals for the privately funded pilot study (Table). These hospitals already had an inpatient care system managed by specialists prior to the pilot study, so major changes in patient care and hospital operations were not required.
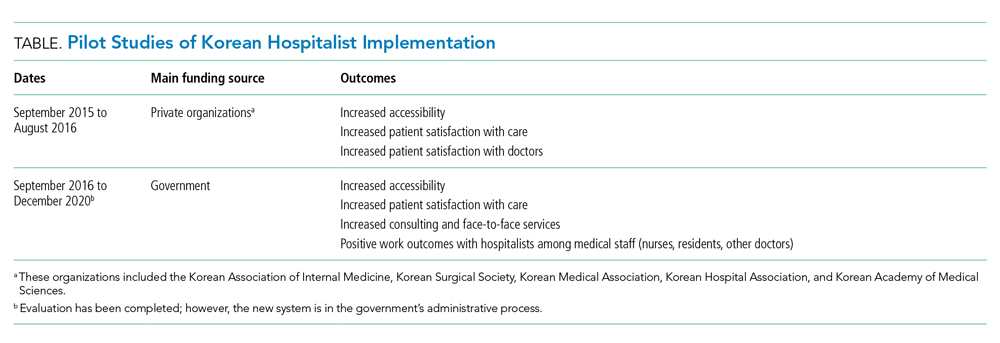
The pilot study demonstrated improvements in patient satisfaction, medical service quality, and patient safety.8,14,15 As a result, fees billed from hospitalist services were now covered by national health insurance; previously, they were not covered by any inpatient care fee or bundled service fee. The next study (phase 2) was then conducted to evaluate the national implementation of the hospitalist system and its outcomes. The first phase defined criteria for monitoring and evaluating the institutionalized hospitalist system in Korea. The second phase, initiated in September 2016, evaluated how the implemented system could be expanded nationwide. The government was actively involved in the study; 31 of 344 (9%) general hospitals were selected and able to apply the hospitalist fee schedule for care of patients who were admitted to the hospitalist ward.
To investigate the effect of the hospitalist system, we measured the satisfaction of patients and medical providers (eg, specialists, residents, and nurses). The outcomes were number of doctors’ calls to hospitalists and to other specialties, duration of time required to address medical problems, number of contacts with the hospitalist (residents or other physicians in the control group), and time spent with hospitalized patients. In addition, we analyzed claims costs and the operating costs for implementing the system within each hospital (Table).
The new set of fee schedules was created specifically for hospitalist care services so hospitals could now claim separate inpatient care fees and hospitalist fees. The standard hospitalist fee schedule is applied only to patients who are on hospitalist-led wards. The fee schedule has two criteria: The hospitalist ward must have 50 beds which are assigned to hospitalists only, and each hospitalist ward has a team of five hospitalists. A maximum of 25 patients could be assigned to an individual hospitalist. However, fees can be adjusted based on individual hospital operation and management after government approval.
Under the national insurance system, the fee schedule is essential to obtain reimbursement for provided services. As a new medical profession, it is important to have the institutional implementation of the hospitalist system. In contrast to those in the United States, inpatients in Korea pay inpatient care fees only, which are charged per day. Therefore, reducing the length of stay without increasing patient volume does not financially benefit the hospital.
DEFINITION OF A KOREAN HOSPITALIST AND SCOPE OF PRACTICE
The definition of a Korean hospitalist was carefully developed, and a reimbursement system for hospitalists was created within the Korean healthcare system. All hospitalists are medical specialists who have completed advanced education and clinical training in their specialty area (internal medicine or surgery). Creating a definition of a hospitalist and a standard fee schedule was necessary for national incorporation of this new approach. The model must also be accepted by related parties, including healthcare professionals such as hospital executives, nonhospitalist doctors, and nurses. Therefore, the system has a minimum of two requirements to operate at the hospital level, and the remaining factors can be modified by individual hospitals to protect the new discipline within the healthcare system. First, hospitalist services are provided only to hospitalist patients. To establish the new system, limiting the patient range to a specific group was necessary to prevent abuse of human-based resources within the hospital. Second, hospitalists must be stationed near the hospitalist ward to enhance accessibility, patient safety, and healthcare quality. In other words, a hospitalist provides services to hospitalized patients who paid the hospitalist fee, and the hospitalist does not provide care beyond the hospitalist ward (eg, they cannot provide outpatient consultation or provide care on other wards).
INPATIENT CARE REIMBURSEMENT BEFORE AND AFTER IMPLEMENTATION
Korean national health insurance is the universal health insurance under a single insurer (ie, the government). Therefore, all Korean citizens have national health insurance. Individuals can choose to have additional health insurance (private insurance) if they wish to pay an out-of-pocket fee with their additional private insurance. In Korea, the inpatient care fee includes all fees to provide care for the patient during hospital stays, such as the physician fee, facility fee, and consultation fee. The inpatient care fee schedule is charged per day including all the inpatient care composition. The claim and reimbursement system is different in Korea in that the hospital as a whole submits the claim for reimbursement. There is no separate claim from physicians, lab technicians, or facilities. Doctors provide care to patients and are then paid for the services in terms of salaries. Since the original inpatient care fee schedule was low and insufficient, it was difficult to provide high-quality care. Also, resources for spending on inpatient care management was limited. So a new system to improve inpatient care was needed. Implementing the hospitalist system in Korea led to the creation of a new fee schedule specifically for hospitalists so that hospitals could claim hospitalist fees on top of inpatient care fees when the patient was cared for by the hospitalist. The additional fees in the hospitalist fee schedule allow safe and high-quality care to be provided for patients during hospital stays.
KOREAN HOSPITAL MEDICINE TODAY
The Korean hospitalist system has been implemented for 3 years with the government’s active involvement, with approximately 250 specialists working as hospitalists as of August 2020. Importantly, Korean hospitalists are not limited to internal medicine specialists; in fact, several different specialties practice as hospitalists, including surgeons and other medical specialists, who account for 20% and 30% of the hospitalist workforce, respectively. Since the system’s implementation, all inpatient care and management is now transferred to specialists from residents in hospitalist wards. This change has increased patient safety and care quality. At the beginning of the pilot study, the concept of a “hospitalist” was new in Korea and the public did not know who a hospitalist was nor what a hospitalist did. However, after 3 years, patients now seek hospitalist care.
CONCLUSION
National implementation of the hospitalist model represents a key paradigm shift in the Korean healthcare system. The Korean hospitalist system is the result of the hospitals’, doctors’, and patients’ desire for higher-quality care. We expect to see growth of hospitalists in Korea and provision of better, safer, and more efficient inpatient care across specialties, payers, and government. Since we are at the early stage of the system, further efforts to support implementation are required. We hope our implementation process of a new medical system could serve as a model for other countries who are seeking to adopt hospitalist systems within their current healthcare paradigms.
Acknowledgments
The authors thank the medical professionals, government officers, and other professionals who put great effort into the implementation of the Korean Hospitalist System.
1. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009;24(1):63-71. https://doi.org/10.1093/heapol/czn037
2. Song YJ. The South Korean health care system. JMAJ. 2009;52(3):206-209.
3. Park YH, Park E-C. Healthcare policy. In: Preventive Medicine and Public Health. Vol 3.Gyechuk; 2017:821-833.
4. Park E-C, Lee TJ, Jun BY, Jung SH, Jeong HS. Health security. In: Preventive Medicine and Public Health. Vol 3. Gyechuk; 2017:888-897.
5. Jang S-I, Jang S-y, Park E-C. Trends of US hospitalist and suggestions for introduction of Korean hospitalist. Korean J Med. 2015;89(1):1-5. http://doi.org/10.3904/kjm.2015.89.1.1
6. Jang S-I. Korean hospitalist system implementation and development strategies based on pilot studies. J Korean Med Assoc. 2019;62(11):558-563. http://doi.org/10.5124/jkma.2019.62.11.558
7. OECD. Health at a Glance 2017: OECD indicators. OECD iLibrary. 2017. Accessed September 27, 2019. https://doi.org/10.1787/health_glance-2017-en
8. Jang S-I, Park E-C, Nam JM, et al. A study on the implementation and the evaluation of Korean Hospitalist System to improve the quality of hospitalization (Phase 2). Institute of Health Services Research, Yonsei University; 2018.
9. Koh DY. Political strategies to enhance medical residents. Health Policy. Vol 37. Seoul National University Hospital; 2014.
10. Act on the Improvement of Training Conditions and Status of Medical Residents. Vol No. 16260: Ministry of Health and Welfare; 2015.
11. Eom JS. Operating the hospitalist system. J Korean Med Assoc. 2016;59(5):342-344. http://doi.org/10.5124/jkma.2016.59.5.342
12. Kim S-S. Working conditions of interns/residents and patient safety: Painful training might not be authentic. J Korean Med Assoc. 2016;59(2):82-84. http://dx.doi.org/10.5124/jkma.2016.59.2.82
13. Oshimura J, Sperring J, Bauer BD, Rauch DA. Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299-303. https://doi.org/10.1002/jhm.952
14. Park E-C, Lee SG, Kim T-H, et al. A study on the implementation and the evaluation of Korean Hospitalist System to improve the quality of hospitalization (Phase 1). Institute of Health Services Research, Yonsei University; 2016.
15. Jang S-I, Jung E-J, Park SK, Chae W, Kim Y-K. A study on the feasibility of the Korean hospitalist system and cost estimation. Ministry of Health and Welfare, Institute of Health Service Research Yonsei University; 2019.
1. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009;24(1):63-71. https://doi.org/10.1093/heapol/czn037
2. Song YJ. The South Korean health care system. JMAJ. 2009;52(3):206-209.
3. Park YH, Park E-C. Healthcare policy. In: Preventive Medicine and Public Health. Vol 3.Gyechuk; 2017:821-833.
4. Park E-C, Lee TJ, Jun BY, Jung SH, Jeong HS. Health security. In: Preventive Medicine and Public Health. Vol 3. Gyechuk; 2017:888-897.
5. Jang S-I, Jang S-y, Park E-C. Trends of US hospitalist and suggestions for introduction of Korean hospitalist. Korean J Med. 2015;89(1):1-5. http://doi.org/10.3904/kjm.2015.89.1.1
6. Jang S-I. Korean hospitalist system implementation and development strategies based on pilot studies. J Korean Med Assoc. 2019;62(11):558-563. http://doi.org/10.5124/jkma.2019.62.11.558
7. OECD. Health at a Glance 2017: OECD indicators. OECD iLibrary. 2017. Accessed September 27, 2019. https://doi.org/10.1787/health_glance-2017-en
8. Jang S-I, Park E-C, Nam JM, et al. A study on the implementation and the evaluation of Korean Hospitalist System to improve the quality of hospitalization (Phase 2). Institute of Health Services Research, Yonsei University; 2018.
9. Koh DY. Political strategies to enhance medical residents. Health Policy. Vol 37. Seoul National University Hospital; 2014.
10. Act on the Improvement of Training Conditions and Status of Medical Residents. Vol No. 16260: Ministry of Health and Welfare; 2015.
11. Eom JS. Operating the hospitalist system. J Korean Med Assoc. 2016;59(5):342-344. http://doi.org/10.5124/jkma.2016.59.5.342
12. Kim S-S. Working conditions of interns/residents and patient safety: Painful training might not be authentic. J Korean Med Assoc. 2016;59(2):82-84. http://dx.doi.org/10.5124/jkma.2016.59.2.82
13. Oshimura J, Sperring J, Bauer BD, Rauch DA. Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299-303. https://doi.org/10.1002/jhm.952
14. Park E-C, Lee SG, Kim T-H, et al. A study on the implementation and the evaluation of Korean Hospitalist System to improve the quality of hospitalization (Phase 1). Institute of Health Services Research, Yonsei University; 2016.
15. Jang S-I, Jung E-J, Park SK, Chae W, Kim Y-K. A study on the feasibility of the Korean hospitalist system and cost estimation. Ministry of Health and Welfare, Institute of Health Service Research Yonsei University; 2019.
© 2021 Society of Hospital Medicine