User login
Improving transitions for elderly patients
Transitions are always a time of concern for hospitalists, and the transition from hospital to skilled nursing facilities (SNF) is no exception.
“During the transition and in the 30 days after discharge from the hospital to a SNF, patients are at high risk for death, rehospitalization, and high-cost health care,” said Amber Moore, MD, MPH, a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School. “Elderly adults are especially vulnerable because of impairments that may prevent them from participating in the discharge process and an increase in the risk that information is lost or incomplete during the care transition.”
To address this, she and several other physicians studied a novel video-conference program called Extension for Community Health Outcomes–Care Transitions (ECHO-CT) that connects an interdisciplinary hospital-based team with clinicians at SNFs to help reduce patient mortality, hospital readmission, skilled nursing facility length of stay, and 30-day health care costs.
The results of their study suggest that this intervention significantly decreased SNF length of stay, readmission rate, and costs of care, she says; the model they used is reproducible and has the potential to significantly improve care of these patients. “Our model was hospitalist run and is a mechanism to help hospitalists improve care to their patients during the transition time and beyond,” Dr. Moore said. “Furthermore, in participating in this model, hospitalists have the opportunity to better understand the challenges that face their patients after discharge and learn from postacute care providers.”
Ideally, she would like to see the model spread to other hospitals; she says hospitalists are well positioned to set up this program at their institution. “I also hope that our study highlights the incredible opportunity for improvement in the care of patients during transition from hospital to SNF and encourages hospitalists to look for innovative ways to improve care at this transition,” she said.
Reference
Moore AB, Krupp JE, Dufour AB, et al. Improving transitions to post-acute care for elderly patients using a novel video-conferencing program: ECHO-Care transitions. Am J Med. 2017 Oct;130(10):1199-204. Accessed June 6, 2017.
Transitions are always a time of concern for hospitalists, and the transition from hospital to skilled nursing facilities (SNF) is no exception.
“During the transition and in the 30 days after discharge from the hospital to a SNF, patients are at high risk for death, rehospitalization, and high-cost health care,” said Amber Moore, MD, MPH, a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School. “Elderly adults are especially vulnerable because of impairments that may prevent them from participating in the discharge process and an increase in the risk that information is lost or incomplete during the care transition.”
To address this, she and several other physicians studied a novel video-conference program called Extension for Community Health Outcomes–Care Transitions (ECHO-CT) that connects an interdisciplinary hospital-based team with clinicians at SNFs to help reduce patient mortality, hospital readmission, skilled nursing facility length of stay, and 30-day health care costs.
The results of their study suggest that this intervention significantly decreased SNF length of stay, readmission rate, and costs of care, she says; the model they used is reproducible and has the potential to significantly improve care of these patients. “Our model was hospitalist run and is a mechanism to help hospitalists improve care to their patients during the transition time and beyond,” Dr. Moore said. “Furthermore, in participating in this model, hospitalists have the opportunity to better understand the challenges that face their patients after discharge and learn from postacute care providers.”
Ideally, she would like to see the model spread to other hospitals; she says hospitalists are well positioned to set up this program at their institution. “I also hope that our study highlights the incredible opportunity for improvement in the care of patients during transition from hospital to SNF and encourages hospitalists to look for innovative ways to improve care at this transition,” she said.
Reference
Moore AB, Krupp JE, Dufour AB, et al. Improving transitions to post-acute care for elderly patients using a novel video-conferencing program: ECHO-Care transitions. Am J Med. 2017 Oct;130(10):1199-204. Accessed June 6, 2017.
Transitions are always a time of concern for hospitalists, and the transition from hospital to skilled nursing facilities (SNF) is no exception.
“During the transition and in the 30 days after discharge from the hospital to a SNF, patients are at high risk for death, rehospitalization, and high-cost health care,” said Amber Moore, MD, MPH, a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School. “Elderly adults are especially vulnerable because of impairments that may prevent them from participating in the discharge process and an increase in the risk that information is lost or incomplete during the care transition.”
To address this, she and several other physicians studied a novel video-conference program called Extension for Community Health Outcomes–Care Transitions (ECHO-CT) that connects an interdisciplinary hospital-based team with clinicians at SNFs to help reduce patient mortality, hospital readmission, skilled nursing facility length of stay, and 30-day health care costs.
The results of their study suggest that this intervention significantly decreased SNF length of stay, readmission rate, and costs of care, she says; the model they used is reproducible and has the potential to significantly improve care of these patients. “Our model was hospitalist run and is a mechanism to help hospitalists improve care to their patients during the transition time and beyond,” Dr. Moore said. “Furthermore, in participating in this model, hospitalists have the opportunity to better understand the challenges that face their patients after discharge and learn from postacute care providers.”
Ideally, she would like to see the model spread to other hospitals; she says hospitalists are well positioned to set up this program at their institution. “I also hope that our study highlights the incredible opportunity for improvement in the care of patients during transition from hospital to SNF and encourages hospitalists to look for innovative ways to improve care at this transition,” she said.
Reference
Moore AB, Krupp JE, Dufour AB, et al. Improving transitions to post-acute care for elderly patients using a novel video-conferencing program: ECHO-Care transitions. Am J Med. 2017 Oct;130(10):1199-204. Accessed June 6, 2017.
Scheduling patterns in hospital medicine
For years, the Society of Hospital Medicine has been asking hospital medicine programs about operational metrics in order to understand and catalog how they are functioning and evolving. After compensation, the scheduling patterns that hospital medicine groups (HMGs) are using is the most reviewed item in the report.
When hospital medicine first started, 7 days working followed by 7 days off (7-on-7-off) quickly became vogue. No one really knows how this happened, but it was most likely due to the fact that hospital medicine most closely resembled emergency medicine and scheduling similar to emergency medicine seemed to make sense (that is, 14 shifts per month). That along with the assumption that continuity of care was critical in inpatient care and would improve quality most likely resulted in the popularity of the 7-on-7-off schedule.
In the most recent survey in 2016, HMGs were once again asked to comment on how they schedule. Groups were able to choose from five scheduling options:
1. Seven days on followed by 7 days off
2. Other fixed rotation block schedules (such as 5-on 5-off; or 10-on 5-off)
3. Monday to Friday with rotating weekend coverage
4. Variable schedule
5. Other
Looking at HMG programs that serve only adult populations, a majority of them (48%) follow a fixed rotating schedule either 7 days on followed by 7 days off, or some other fixed schedule, while 31% of programs that responded stated that they used a Monday to Friday schedule. Looking at the programs as a whole, it would seem that the 7-on-7-off schedule was quickly losing popularity while the Monday to Friday schedule was increasingly being used. However, this broad generalization doesn’t really give you the full picture.
Upon analyzing the data further, we see some distinct differences arise based on program size. Small programs (fewer than 10 full-time employees [FTEs]) are much more likely to schedule a Monday to Friday schedule than any other model, whereas only a handful of large programs (greater than 20 FTEs) schedule in this way, rather choosing to use a 7-on-7-off schedule.
The last survey was done in 2014 and a lot has changed since then. Significantly more programs responded in 2016, compared with 2014 (530 vs. 355) and the majority of this increase was made of up smaller programs (fewer than 10 FTEs). Programs with four or fewer FTEs, compared with the prior survey, increased by over 400% (37 programs in 2014 vs. 151 programs in 2016). Overall, programs with fewer than 10 FTEs constituted over 50% of the total programs that responded in 2016 (whereas they made up only a third in 2014). This was particularly significant since size of the program was the one variable that determined how a program might schedule – other factors like geographic region, academic status, or primary hospital GME status did not show significant variance in how groups scheduled.
The second major change that occurred is that these same small programs (those with fewer than 10 FTEs) moved overwhelmingly to a Monday to Friday schedule. In 2014, only 3% of small programs scheduled using a Monday to Friday pattern, but in 2016 almost 50% of small programs reported scheduling in this way. This change in the overall composition of programs, with small programs now making up over 50% of the programs that reported, and the specific change in how small programs schedule results in a noteworthy decrease of programs using a 7 days on followed by 7 days off (7-on-7-off) schedule (53.8% in 2014 and only 38.1% in 2016), and a corresponding increase in the number of programs that schedule using a Monday to Friday schedule (4% in 2014 to 31% in 2016).
In distinct contrast to programs with fewer than 10 FTEs, a very similar number of programs with greater than 20 FTEs reported in 2016 as in 2014 – there was no increase in this subgroup. I’m not clear at this time if this is because there is truly no increase in the number of large programs nationally, or if there is another factor causing larger programs to under-report. The large programs that did report data in 2016 continue to utilize a 7-on-7-off schedule or another fixed rotating block schedule more than 50% of the time. In fact, the utilization of one of these two scheduling patterns increased slightly from 2014 to 2016 (from 52% to 58%). Those that did not use one of the prior mentioned scheduling patterns were most likely to schedule with a variable schedule. A Monday to Friday schedule was almost never used in programs of this size and showed no significant change from 2014 to 2016.
This snapshot highlights the changing landscape in hospital medicine. Hospital medicine is penetrating more and more into smaller and smaller hospitals, and has even made it into critical access hospitals. As recently as 5-10 years ago, it was felt that these hospitals were too small to have a hospital medicine program. This is likely one of the reasons for the increase in programs with four or fewer FTEs. There has also been increasing discontent with the 7-on-7-off schedule, which many feel is leading to burnout. Dr. Bob Wachter famously said during the closing plenary of the 2016 Society of Hospital Medicine Annual Meeting that the 7-on-7-off schedule was “a mistake.” Despite this brewing discontent, larger programs have not changed their scheduling patterns, likely because finding a another scheduling pattern that is effective, supports high-quality care, and is sustainable for such a large group is challenging.
Many people will say that there are as many different types of hospital medicine programs as there are hospital medicine programs. This is true for scheduling as for other aspects of hospital medicine operations. As we continue to grow and evolve as an industry, scheduling patterns will continue to change and evolve as well. For now, two patterns are emerging – smaller programs are utilizing a Monday to Friday schedule and larger programs are utilizing a 7-on-7-off schedule. Only time will tell if these scheduling patterns persist or continue to evolve.
Dr. George is a board certified internal medicine physician and practicing hospitalist with over 15 years of experience in hospital medicine. She has been actively involved in the Society of Hospital Medicine and has participated in and chaired multiple committees and task forces. She is currently executive vice president and chief medical officer of Hospital Medicine at Schumacher Clinical Partners, a national provider of emergency medicine and hospital medicine services. She lives in the northwest suburbs of Chicago with her family.
For years, the Society of Hospital Medicine has been asking hospital medicine programs about operational metrics in order to understand and catalog how they are functioning and evolving. After compensation, the scheduling patterns that hospital medicine groups (HMGs) are using is the most reviewed item in the report.
When hospital medicine first started, 7 days working followed by 7 days off (7-on-7-off) quickly became vogue. No one really knows how this happened, but it was most likely due to the fact that hospital medicine most closely resembled emergency medicine and scheduling similar to emergency medicine seemed to make sense (that is, 14 shifts per month). That along with the assumption that continuity of care was critical in inpatient care and would improve quality most likely resulted in the popularity of the 7-on-7-off schedule.
In the most recent survey in 2016, HMGs were once again asked to comment on how they schedule. Groups were able to choose from five scheduling options:
1. Seven days on followed by 7 days off
2. Other fixed rotation block schedules (such as 5-on 5-off; or 10-on 5-off)
3. Monday to Friday with rotating weekend coverage
4. Variable schedule
5. Other
Looking at HMG programs that serve only adult populations, a majority of them (48%) follow a fixed rotating schedule either 7 days on followed by 7 days off, or some other fixed schedule, while 31% of programs that responded stated that they used a Monday to Friday schedule. Looking at the programs as a whole, it would seem that the 7-on-7-off schedule was quickly losing popularity while the Monday to Friday schedule was increasingly being used. However, this broad generalization doesn’t really give you the full picture.
Upon analyzing the data further, we see some distinct differences arise based on program size. Small programs (fewer than 10 full-time employees [FTEs]) are much more likely to schedule a Monday to Friday schedule than any other model, whereas only a handful of large programs (greater than 20 FTEs) schedule in this way, rather choosing to use a 7-on-7-off schedule.
The last survey was done in 2014 and a lot has changed since then. Significantly more programs responded in 2016, compared with 2014 (530 vs. 355) and the majority of this increase was made of up smaller programs (fewer than 10 FTEs). Programs with four or fewer FTEs, compared with the prior survey, increased by over 400% (37 programs in 2014 vs. 151 programs in 2016). Overall, programs with fewer than 10 FTEs constituted over 50% of the total programs that responded in 2016 (whereas they made up only a third in 2014). This was particularly significant since size of the program was the one variable that determined how a program might schedule – other factors like geographic region, academic status, or primary hospital GME status did not show significant variance in how groups scheduled.
The second major change that occurred is that these same small programs (those with fewer than 10 FTEs) moved overwhelmingly to a Monday to Friday schedule. In 2014, only 3% of small programs scheduled using a Monday to Friday pattern, but in 2016 almost 50% of small programs reported scheduling in this way. This change in the overall composition of programs, with small programs now making up over 50% of the programs that reported, and the specific change in how small programs schedule results in a noteworthy decrease of programs using a 7 days on followed by 7 days off (7-on-7-off) schedule (53.8% in 2014 and only 38.1% in 2016), and a corresponding increase in the number of programs that schedule using a Monday to Friday schedule (4% in 2014 to 31% in 2016).
In distinct contrast to programs with fewer than 10 FTEs, a very similar number of programs with greater than 20 FTEs reported in 2016 as in 2014 – there was no increase in this subgroup. I’m not clear at this time if this is because there is truly no increase in the number of large programs nationally, or if there is another factor causing larger programs to under-report. The large programs that did report data in 2016 continue to utilize a 7-on-7-off schedule or another fixed rotating block schedule more than 50% of the time. In fact, the utilization of one of these two scheduling patterns increased slightly from 2014 to 2016 (from 52% to 58%). Those that did not use one of the prior mentioned scheduling patterns were most likely to schedule with a variable schedule. A Monday to Friday schedule was almost never used in programs of this size and showed no significant change from 2014 to 2016.
This snapshot highlights the changing landscape in hospital medicine. Hospital medicine is penetrating more and more into smaller and smaller hospitals, and has even made it into critical access hospitals. As recently as 5-10 years ago, it was felt that these hospitals were too small to have a hospital medicine program. This is likely one of the reasons for the increase in programs with four or fewer FTEs. There has also been increasing discontent with the 7-on-7-off schedule, which many feel is leading to burnout. Dr. Bob Wachter famously said during the closing plenary of the 2016 Society of Hospital Medicine Annual Meeting that the 7-on-7-off schedule was “a mistake.” Despite this brewing discontent, larger programs have not changed their scheduling patterns, likely because finding a another scheduling pattern that is effective, supports high-quality care, and is sustainable for such a large group is challenging.
Many people will say that there are as many different types of hospital medicine programs as there are hospital medicine programs. This is true for scheduling as for other aspects of hospital medicine operations. As we continue to grow and evolve as an industry, scheduling patterns will continue to change and evolve as well. For now, two patterns are emerging – smaller programs are utilizing a Monday to Friday schedule and larger programs are utilizing a 7-on-7-off schedule. Only time will tell if these scheduling patterns persist or continue to evolve.
Dr. George is a board certified internal medicine physician and practicing hospitalist with over 15 years of experience in hospital medicine. She has been actively involved in the Society of Hospital Medicine and has participated in and chaired multiple committees and task forces. She is currently executive vice president and chief medical officer of Hospital Medicine at Schumacher Clinical Partners, a national provider of emergency medicine and hospital medicine services. She lives in the northwest suburbs of Chicago with her family.
For years, the Society of Hospital Medicine has been asking hospital medicine programs about operational metrics in order to understand and catalog how they are functioning and evolving. After compensation, the scheduling patterns that hospital medicine groups (HMGs) are using is the most reviewed item in the report.
When hospital medicine first started, 7 days working followed by 7 days off (7-on-7-off) quickly became vogue. No one really knows how this happened, but it was most likely due to the fact that hospital medicine most closely resembled emergency medicine and scheduling similar to emergency medicine seemed to make sense (that is, 14 shifts per month). That along with the assumption that continuity of care was critical in inpatient care and would improve quality most likely resulted in the popularity of the 7-on-7-off schedule.
In the most recent survey in 2016, HMGs were once again asked to comment on how they schedule. Groups were able to choose from five scheduling options:
1. Seven days on followed by 7 days off
2. Other fixed rotation block schedules (such as 5-on 5-off; or 10-on 5-off)
3. Monday to Friday with rotating weekend coverage
4. Variable schedule
5. Other
Looking at HMG programs that serve only adult populations, a majority of them (48%) follow a fixed rotating schedule either 7 days on followed by 7 days off, or some other fixed schedule, while 31% of programs that responded stated that they used a Monday to Friday schedule. Looking at the programs as a whole, it would seem that the 7-on-7-off schedule was quickly losing popularity while the Monday to Friday schedule was increasingly being used. However, this broad generalization doesn’t really give you the full picture.
Upon analyzing the data further, we see some distinct differences arise based on program size. Small programs (fewer than 10 full-time employees [FTEs]) are much more likely to schedule a Monday to Friday schedule than any other model, whereas only a handful of large programs (greater than 20 FTEs) schedule in this way, rather choosing to use a 7-on-7-off schedule.
The last survey was done in 2014 and a lot has changed since then. Significantly more programs responded in 2016, compared with 2014 (530 vs. 355) and the majority of this increase was made of up smaller programs (fewer than 10 FTEs). Programs with four or fewer FTEs, compared with the prior survey, increased by over 400% (37 programs in 2014 vs. 151 programs in 2016). Overall, programs with fewer than 10 FTEs constituted over 50% of the total programs that responded in 2016 (whereas they made up only a third in 2014). This was particularly significant since size of the program was the one variable that determined how a program might schedule – other factors like geographic region, academic status, or primary hospital GME status did not show significant variance in how groups scheduled.
The second major change that occurred is that these same small programs (those with fewer than 10 FTEs) moved overwhelmingly to a Monday to Friday schedule. In 2014, only 3% of small programs scheduled using a Monday to Friday pattern, but in 2016 almost 50% of small programs reported scheduling in this way. This change in the overall composition of programs, with small programs now making up over 50% of the programs that reported, and the specific change in how small programs schedule results in a noteworthy decrease of programs using a 7 days on followed by 7 days off (7-on-7-off) schedule (53.8% in 2014 and only 38.1% in 2016), and a corresponding increase in the number of programs that schedule using a Monday to Friday schedule (4% in 2014 to 31% in 2016).
In distinct contrast to programs with fewer than 10 FTEs, a very similar number of programs with greater than 20 FTEs reported in 2016 as in 2014 – there was no increase in this subgroup. I’m not clear at this time if this is because there is truly no increase in the number of large programs nationally, or if there is another factor causing larger programs to under-report. The large programs that did report data in 2016 continue to utilize a 7-on-7-off schedule or another fixed rotating block schedule more than 50% of the time. In fact, the utilization of one of these two scheduling patterns increased slightly from 2014 to 2016 (from 52% to 58%). Those that did not use one of the prior mentioned scheduling patterns were most likely to schedule with a variable schedule. A Monday to Friday schedule was almost never used in programs of this size and showed no significant change from 2014 to 2016.
This snapshot highlights the changing landscape in hospital medicine. Hospital medicine is penetrating more and more into smaller and smaller hospitals, and has even made it into critical access hospitals. As recently as 5-10 years ago, it was felt that these hospitals were too small to have a hospital medicine program. This is likely one of the reasons for the increase in programs with four or fewer FTEs. There has also been increasing discontent with the 7-on-7-off schedule, which many feel is leading to burnout. Dr. Bob Wachter famously said during the closing plenary of the 2016 Society of Hospital Medicine Annual Meeting that the 7-on-7-off schedule was “a mistake.” Despite this brewing discontent, larger programs have not changed their scheduling patterns, likely because finding a another scheduling pattern that is effective, supports high-quality care, and is sustainable for such a large group is challenging.
Many people will say that there are as many different types of hospital medicine programs as there are hospital medicine programs. This is true for scheduling as for other aspects of hospital medicine operations. As we continue to grow and evolve as an industry, scheduling patterns will continue to change and evolve as well. For now, two patterns are emerging – smaller programs are utilizing a Monday to Friday schedule and larger programs are utilizing a 7-on-7-off schedule. Only time will tell if these scheduling patterns persist or continue to evolve.
Dr. George is a board certified internal medicine physician and practicing hospitalist with over 15 years of experience in hospital medicine. She has been actively involved in the Society of Hospital Medicine and has participated in and chaired multiple committees and task forces. She is currently executive vice president and chief medical officer of Hospital Medicine at Schumacher Clinical Partners, a national provider of emergency medicine and hospital medicine services. She lives in the northwest suburbs of Chicago with her family.
Pediatric hospitalists take on the challenge of antibiotic stewardship
When Carol Glaser, MD, was in training, the philosophy around antibiotic prescribing often went something like this: “Ten days of antibiotics is good, but let’s do a few more days just to be sure,” she said.
Today, however, the new mantra is “less is more.” Dr. Glaser is an experienced pediatric infectious disease physician and the lead physician for pediatric antimicrobial stewardship at The Permanente Medical Group, Kaiser Permanente, at the Oakland (Calif.) Medical Center. While antibiotic stewardship is an issue relevant to nearly all hospitalists, for pediatric patients, the considerations can be unique and particularly serious.
Dr. Shah, a pediatric infectious disease physician at Cincinnati Children’s Hospital, spoke last spring at HM17, the Society of Hospital Medicine’s annual meeting. His talk drew from issues raised on pediatric hospital medicine electronic mailing lists and from audience questions. These centered on decisions regarding the use of intravenous versus oral antibiotics for pediatric patients – or what he refers to as intravenous-to-oral conversion – as well as antibiotic treatment duration.
“For many conditions in pediatrics, we used to treat with intravenous antibiotics initially – and sometimes for the entire course – and now we’re using oral antibiotics for the entire course,” Dr. Shah said. He noted that urinary tract infections were once treated with IV antibiotics in the hospital but are now routinely treated orally in an outpatient setting.
Dr. Shah cited two studies, both of which he coauthored as part of the Pediatric Research in Inpatient Settings Network, which compared intravenous versus oral antibiotics treatments given after discharge: The first, published in JAMA Pediatrics in 2014, examined treatment for osteomyelitis, while the second, which focused on complicated pneumonia, was published in Pediatrics in 2016.1,2
Both were observational, retrospective studies involving more than 2,000 children across more than 30 hospitals. The JAMA Pediatrics study found that roughly half of the patients were discharged with a peripherally inserted central catheter (PICC) line, and half were prescribed oral antibiotics. In some hospitals, 100% of patients were sent home with a PICC line, and in others, all children were sent home on oral antibiotics. Although treatment failure rates were the same for both groups, 15% of the patients sent home with a PICC line had to return to the emergency department because of PICC-related complications. Some were hospitalized.1
The Pediatrics study found less variation in PICC versus oral antibiotic use across hospitals for patients with complicated pneumonia, but the treatment failure rate was slightly higher for PICC patients at 3.2%, compared with 2.6% for those on oral antibiotics. This difference, however, was not statistically significant. PICC-related complications were observed in 7.1% of patients with PICC lines also were more likely to experience adverse drug reactions, compared with patients on oral antibiotics.2
“PICC lines have some advantages, particularly when children are unable or unwilling to take oral antibiotics, but they also have risks” said Dr. Shah. “If outcomes are equivalent, why would you subject patients to the risks of a catheter? And, every time they get a fever at home with a PICC line, they need urgent evaluation for the possibility of a catheter-associated bacterial infection. There is an emotional cost, as well, to taking care of catheters in the home setting.”
Additionally, economic pressures are compelling hospitals to reduce costs and resource utilization while maintaining or improving the quality of care, Dr. Shah pointed out. “Hospitalists do many things well, and quality improvement is one of those areas. That approach really aligns with antimicrobial stewardship, and there is greater incentive with episode-based payment models and financial penalties for excess readmissions. Reducing post-discharge IV antibiotic use aligns with stewardship goals and reduces the likelihood of hospital readmissions.”
The hospital medicine division at Dr. Shah’s hospital helped assemble a multidisciplinary team involving emergency physicians, pharmacists, nursing staff, hospitalists, and infectious disease physicians to encourage the use of appropriate, narrow-spectrum antibiotics and reduce the duration of antibiotic therapies. For example, skin and soft-tissue infections that were once treated for 10-14 days are now sufficiently treated in 5-7days. These efforts to improve outcomes through better adherence to evidence-based practices, including better stewardship, earned the team the SHM Teamwork in Quality Improvement Award in 2014.
“Quality improvement is really about changing the system, and hospitalists, who excel in QI, are poised to help drive antimicrobial stewardship efforts,” Dr. Shah said.
At Oakland Medical Center, Dr. Glaser helped implement handshake rounds, an idea they adopted from a group in Colorado. Every day, with every patient, the antimicrobial stewardship team meets with representatives of the teams – pediatric intensive care, the wards, the NICU, and others – to review antibiotic treatment plans for the choice of antimicrobial drug, for the duration of treatment, and for specific conditions. “We work really closely with hospitalists and our strong pediatric pharmacy team every day to ask: ‘Do we have the right dose? Do we really need to use this antibiotic?’ ” Dr. Glaser said.
Last year, she also worked to incorporate antimicrobial stewardship principles into the hospital’s residency program. “I think the most important thing we’re doing is changing the culture,” she said. “For these young physicians, we’re giving them the knowledge to empower them rather than telling them what to do and giving them a better, fundamental understanding of infectious disease.”
For instance, most pediatric respiratory illnesses are caused by a virus, yet physicians will still prescribe antibiotics for a host of reasons – including the expectations of parents, the guesswork that can go into diagnosing a young patient who cannot describe what is wrong, and the fear that children will get sicker if an antibiotic is not started early.
“A lot of it is figuring out the best approach with the least amount of side effects but covering what we need to cover for a given patient,” she said.
A number of physicians from Dr. Glaser’s team presented stewardship data from their hospital at the July 2017 Pediatric Hospital Medicine meeting in Nashville, demonstrating that, overall, they are using fewer antibiotics and that fewer of those used are broad spectrum. This satisfies the “pillars of stewardship,” Dr. Glaser said. Use antibiotics only when you need them, use them only as long as you need, and then make sure you use the most narrow-spectrum antibiotic you possibly can, she said.
Oakland Medical Center has benefited from a strong commitment to antimicrobial stewardship efforts, Dr. Glaser said, noting that many programs may lack such support, a problem that can be one of the biggest hurdles antimicrobial stewardship efforts face. The support at her hospital “has been an immense help in getting our program to where it is today.”
References
1. Keren R, Shah SS, Srivastava R, et al. Comparative effectiveness of intravenous vs oral antibiotics for postdischarge treatment of acute osteomyelitis in children. JAMA Pediatr. 2015 Feb:169(2):120-8.
2. Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016 Dec;138(6). pii: e20161692.
When Carol Glaser, MD, was in training, the philosophy around antibiotic prescribing often went something like this: “Ten days of antibiotics is good, but let’s do a few more days just to be sure,” she said.
Today, however, the new mantra is “less is more.” Dr. Glaser is an experienced pediatric infectious disease physician and the lead physician for pediatric antimicrobial stewardship at The Permanente Medical Group, Kaiser Permanente, at the Oakland (Calif.) Medical Center. While antibiotic stewardship is an issue relevant to nearly all hospitalists, for pediatric patients, the considerations can be unique and particularly serious.
Dr. Shah, a pediatric infectious disease physician at Cincinnati Children’s Hospital, spoke last spring at HM17, the Society of Hospital Medicine’s annual meeting. His talk drew from issues raised on pediatric hospital medicine electronic mailing lists and from audience questions. These centered on decisions regarding the use of intravenous versus oral antibiotics for pediatric patients – or what he refers to as intravenous-to-oral conversion – as well as antibiotic treatment duration.
“For many conditions in pediatrics, we used to treat with intravenous antibiotics initially – and sometimes for the entire course – and now we’re using oral antibiotics for the entire course,” Dr. Shah said. He noted that urinary tract infections were once treated with IV antibiotics in the hospital but are now routinely treated orally in an outpatient setting.
Dr. Shah cited two studies, both of which he coauthored as part of the Pediatric Research in Inpatient Settings Network, which compared intravenous versus oral antibiotics treatments given after discharge: The first, published in JAMA Pediatrics in 2014, examined treatment for osteomyelitis, while the second, which focused on complicated pneumonia, was published in Pediatrics in 2016.1,2
Both were observational, retrospective studies involving more than 2,000 children across more than 30 hospitals. The JAMA Pediatrics study found that roughly half of the patients were discharged with a peripherally inserted central catheter (PICC) line, and half were prescribed oral antibiotics. In some hospitals, 100% of patients were sent home with a PICC line, and in others, all children were sent home on oral antibiotics. Although treatment failure rates were the same for both groups, 15% of the patients sent home with a PICC line had to return to the emergency department because of PICC-related complications. Some were hospitalized.1
The Pediatrics study found less variation in PICC versus oral antibiotic use across hospitals for patients with complicated pneumonia, but the treatment failure rate was slightly higher for PICC patients at 3.2%, compared with 2.6% for those on oral antibiotics. This difference, however, was not statistically significant. PICC-related complications were observed in 7.1% of patients with PICC lines also were more likely to experience adverse drug reactions, compared with patients on oral antibiotics.2
“PICC lines have some advantages, particularly when children are unable or unwilling to take oral antibiotics, but they also have risks” said Dr. Shah. “If outcomes are equivalent, why would you subject patients to the risks of a catheter? And, every time they get a fever at home with a PICC line, they need urgent evaluation for the possibility of a catheter-associated bacterial infection. There is an emotional cost, as well, to taking care of catheters in the home setting.”
Additionally, economic pressures are compelling hospitals to reduce costs and resource utilization while maintaining or improving the quality of care, Dr. Shah pointed out. “Hospitalists do many things well, and quality improvement is one of those areas. That approach really aligns with antimicrobial stewardship, and there is greater incentive with episode-based payment models and financial penalties for excess readmissions. Reducing post-discharge IV antibiotic use aligns with stewardship goals and reduces the likelihood of hospital readmissions.”
The hospital medicine division at Dr. Shah’s hospital helped assemble a multidisciplinary team involving emergency physicians, pharmacists, nursing staff, hospitalists, and infectious disease physicians to encourage the use of appropriate, narrow-spectrum antibiotics and reduce the duration of antibiotic therapies. For example, skin and soft-tissue infections that were once treated for 10-14 days are now sufficiently treated in 5-7days. These efforts to improve outcomes through better adherence to evidence-based practices, including better stewardship, earned the team the SHM Teamwork in Quality Improvement Award in 2014.
“Quality improvement is really about changing the system, and hospitalists, who excel in QI, are poised to help drive antimicrobial stewardship efforts,” Dr. Shah said.
At Oakland Medical Center, Dr. Glaser helped implement handshake rounds, an idea they adopted from a group in Colorado. Every day, with every patient, the antimicrobial stewardship team meets with representatives of the teams – pediatric intensive care, the wards, the NICU, and others – to review antibiotic treatment plans for the choice of antimicrobial drug, for the duration of treatment, and for specific conditions. “We work really closely with hospitalists and our strong pediatric pharmacy team every day to ask: ‘Do we have the right dose? Do we really need to use this antibiotic?’ ” Dr. Glaser said.
Last year, she also worked to incorporate antimicrobial stewardship principles into the hospital’s residency program. “I think the most important thing we’re doing is changing the culture,” she said. “For these young physicians, we’re giving them the knowledge to empower them rather than telling them what to do and giving them a better, fundamental understanding of infectious disease.”
For instance, most pediatric respiratory illnesses are caused by a virus, yet physicians will still prescribe antibiotics for a host of reasons – including the expectations of parents, the guesswork that can go into diagnosing a young patient who cannot describe what is wrong, and the fear that children will get sicker if an antibiotic is not started early.
“A lot of it is figuring out the best approach with the least amount of side effects but covering what we need to cover for a given patient,” she said.
A number of physicians from Dr. Glaser’s team presented stewardship data from their hospital at the July 2017 Pediatric Hospital Medicine meeting in Nashville, demonstrating that, overall, they are using fewer antibiotics and that fewer of those used are broad spectrum. This satisfies the “pillars of stewardship,” Dr. Glaser said. Use antibiotics only when you need them, use them only as long as you need, and then make sure you use the most narrow-spectrum antibiotic you possibly can, she said.
Oakland Medical Center has benefited from a strong commitment to antimicrobial stewardship efforts, Dr. Glaser said, noting that many programs may lack such support, a problem that can be one of the biggest hurdles antimicrobial stewardship efforts face. The support at her hospital “has been an immense help in getting our program to where it is today.”
References
1. Keren R, Shah SS, Srivastava R, et al. Comparative effectiveness of intravenous vs oral antibiotics for postdischarge treatment of acute osteomyelitis in children. JAMA Pediatr. 2015 Feb:169(2):120-8.
2. Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016 Dec;138(6). pii: e20161692.
When Carol Glaser, MD, was in training, the philosophy around antibiotic prescribing often went something like this: “Ten days of antibiotics is good, but let’s do a few more days just to be sure,” she said.
Today, however, the new mantra is “less is more.” Dr. Glaser is an experienced pediatric infectious disease physician and the lead physician for pediatric antimicrobial stewardship at The Permanente Medical Group, Kaiser Permanente, at the Oakland (Calif.) Medical Center. While antibiotic stewardship is an issue relevant to nearly all hospitalists, for pediatric patients, the considerations can be unique and particularly serious.
Dr. Shah, a pediatric infectious disease physician at Cincinnati Children’s Hospital, spoke last spring at HM17, the Society of Hospital Medicine’s annual meeting. His talk drew from issues raised on pediatric hospital medicine electronic mailing lists and from audience questions. These centered on decisions regarding the use of intravenous versus oral antibiotics for pediatric patients – or what he refers to as intravenous-to-oral conversion – as well as antibiotic treatment duration.
“For many conditions in pediatrics, we used to treat with intravenous antibiotics initially – and sometimes for the entire course – and now we’re using oral antibiotics for the entire course,” Dr. Shah said. He noted that urinary tract infections were once treated with IV antibiotics in the hospital but are now routinely treated orally in an outpatient setting.
Dr. Shah cited two studies, both of which he coauthored as part of the Pediatric Research in Inpatient Settings Network, which compared intravenous versus oral antibiotics treatments given after discharge: The first, published in JAMA Pediatrics in 2014, examined treatment for osteomyelitis, while the second, which focused on complicated pneumonia, was published in Pediatrics in 2016.1,2
Both were observational, retrospective studies involving more than 2,000 children across more than 30 hospitals. The JAMA Pediatrics study found that roughly half of the patients were discharged with a peripherally inserted central catheter (PICC) line, and half were prescribed oral antibiotics. In some hospitals, 100% of patients were sent home with a PICC line, and in others, all children were sent home on oral antibiotics. Although treatment failure rates were the same for both groups, 15% of the patients sent home with a PICC line had to return to the emergency department because of PICC-related complications. Some were hospitalized.1
The Pediatrics study found less variation in PICC versus oral antibiotic use across hospitals for patients with complicated pneumonia, but the treatment failure rate was slightly higher for PICC patients at 3.2%, compared with 2.6% for those on oral antibiotics. This difference, however, was not statistically significant. PICC-related complications were observed in 7.1% of patients with PICC lines also were more likely to experience adverse drug reactions, compared with patients on oral antibiotics.2
“PICC lines have some advantages, particularly when children are unable or unwilling to take oral antibiotics, but they also have risks” said Dr. Shah. “If outcomes are equivalent, why would you subject patients to the risks of a catheter? And, every time they get a fever at home with a PICC line, they need urgent evaluation for the possibility of a catheter-associated bacterial infection. There is an emotional cost, as well, to taking care of catheters in the home setting.”
Additionally, economic pressures are compelling hospitals to reduce costs and resource utilization while maintaining or improving the quality of care, Dr. Shah pointed out. “Hospitalists do many things well, and quality improvement is one of those areas. That approach really aligns with antimicrobial stewardship, and there is greater incentive with episode-based payment models and financial penalties for excess readmissions. Reducing post-discharge IV antibiotic use aligns with stewardship goals and reduces the likelihood of hospital readmissions.”
The hospital medicine division at Dr. Shah’s hospital helped assemble a multidisciplinary team involving emergency physicians, pharmacists, nursing staff, hospitalists, and infectious disease physicians to encourage the use of appropriate, narrow-spectrum antibiotics and reduce the duration of antibiotic therapies. For example, skin and soft-tissue infections that were once treated for 10-14 days are now sufficiently treated in 5-7days. These efforts to improve outcomes through better adherence to evidence-based practices, including better stewardship, earned the team the SHM Teamwork in Quality Improvement Award in 2014.
“Quality improvement is really about changing the system, and hospitalists, who excel in QI, are poised to help drive antimicrobial stewardship efforts,” Dr. Shah said.
At Oakland Medical Center, Dr. Glaser helped implement handshake rounds, an idea they adopted from a group in Colorado. Every day, with every patient, the antimicrobial stewardship team meets with representatives of the teams – pediatric intensive care, the wards, the NICU, and others – to review antibiotic treatment plans for the choice of antimicrobial drug, for the duration of treatment, and for specific conditions. “We work really closely with hospitalists and our strong pediatric pharmacy team every day to ask: ‘Do we have the right dose? Do we really need to use this antibiotic?’ ” Dr. Glaser said.
Last year, she also worked to incorporate antimicrobial stewardship principles into the hospital’s residency program. “I think the most important thing we’re doing is changing the culture,” she said. “For these young physicians, we’re giving them the knowledge to empower them rather than telling them what to do and giving them a better, fundamental understanding of infectious disease.”
For instance, most pediatric respiratory illnesses are caused by a virus, yet physicians will still prescribe antibiotics for a host of reasons – including the expectations of parents, the guesswork that can go into diagnosing a young patient who cannot describe what is wrong, and the fear that children will get sicker if an antibiotic is not started early.
“A lot of it is figuring out the best approach with the least amount of side effects but covering what we need to cover for a given patient,” she said.
A number of physicians from Dr. Glaser’s team presented stewardship data from their hospital at the July 2017 Pediatric Hospital Medicine meeting in Nashville, demonstrating that, overall, they are using fewer antibiotics and that fewer of those used are broad spectrum. This satisfies the “pillars of stewardship,” Dr. Glaser said. Use antibiotics only when you need them, use them only as long as you need, and then make sure you use the most narrow-spectrum antibiotic you possibly can, she said.
Oakland Medical Center has benefited from a strong commitment to antimicrobial stewardship efforts, Dr. Glaser said, noting that many programs may lack such support, a problem that can be one of the biggest hurdles antimicrobial stewardship efforts face. The support at her hospital “has been an immense help in getting our program to where it is today.”
References
1. Keren R, Shah SS, Srivastava R, et al. Comparative effectiveness of intravenous vs oral antibiotics for postdischarge treatment of acute osteomyelitis in children. JAMA Pediatr. 2015 Feb:169(2):120-8.
2. Shah SS, Srivastava R, Wu S, et al. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016 Dec;138(6). pii: e20161692.
Readmission rates linked to hospital quality measures
Poorer-performing hospitals have higher readmission rates than better-performing hospitals for patients with similar diagnoses, a study shows.
Lead author Harlan M. Krumholz, MD, of Yale University, New Haven, Conn., and his colleagues analyzed Centers for Medicare and Medicaid Services hospital-wide readmission data and divided data from July 2014 through June 2015 into two random samples. Researchers used the first sample to calculate the risk-standardized readmission rate within 30 days for each hospital and classified hospitals into performance quartiles, with a lower readmission rate indicating better performance. The second study sample included patients who had two admissions for similar diagnoses at different hospitals that occurred more than 1 month and less than 1 year apart. Researchers compared the observed readmission rates among patients who had been admitted to hospitals in different performance quartiles. The analysis included all discharges occurring from July 1, 2014, through June 30, 2015, from short-term acute care or critical access hospitals in the United States involving Medicare patients who were aged 65 years or older.
Results found that among the patients hospitalized more than once for similar diagnoses at different hospitals, the readmission rate was significantly higher among patients admitted to the worst-performing quartile of hospitals than among those admitted to the best-performing quartile (absolute difference in readmission rate, 2.0 percentage points; 95% confidence interval, 0.4-3.5; P = .001) (N Engl J Med. 2017. doi: 10.1056/NEJMsa1702321). The differences in the comparisons of the other quartiles were smaller and not significant, according to the study. 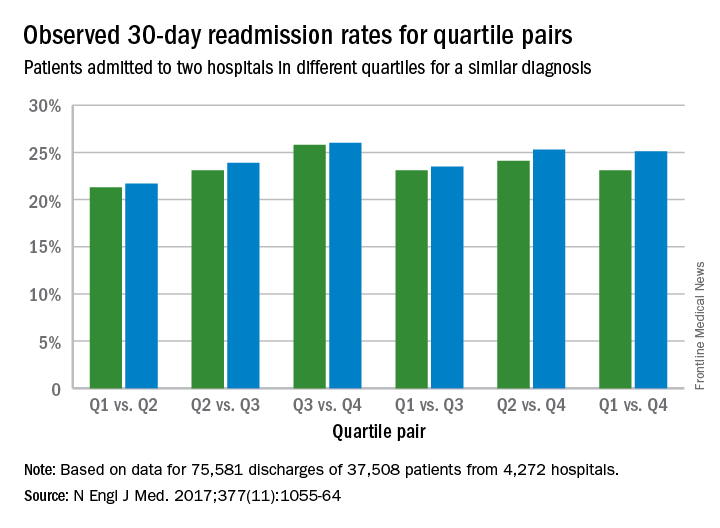
The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors, study authors concluded.
“This study addresses a persistent concern that national readmission measures may reflect differences in unmeasured factors rather than in hospital performance,” they said. “The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors. By studying patients who were admitted twice within 1 year with similar diagnoses to different hospitals, this study design was able to isolate hospital signals of performance while minimizing differences among the patients. In these cases, because the same patients had similar admissions at two hospitals, the characteristics of the patients, including their level of social disadvantage, level of education, or degree of underlying illness, were broadly the same. The alignment of the differences that we observed with the results of the CMS hospital-wide readmission measure also adds to evidence that the readmission measure classifies true differences in performance.”
Dr. Krumholz and seven coauthors reported receiving support from contracts with the Center for Medicare and Medicaid Services to develop and reevaluate performance measures that are used for public reporting.
[email protected]
On Twitter @legal_med
The Hospital Readmission Reduction Program (HRRP) was established in 2011 by a provision in the Affordable Care Act (ACA) requiring Medicare to reduce payments to hospitals with relatively high readmission rates for patients in traditional Medicare. Since the inception of the HRRP, readmission rates have declined across all measured diagnostic categories resulting in estimates of 565,000 fewer Medicare readmissions through 2015.1 These reductions seem to be driven by penalties demonstrated by the fact that readmissions fell more quickly at hospitals that had readmission penalties than at other hospitals. Although the severity and fairness of the penalties can be debated, the HRRP has been successful in achieving the goal of reducing readmissions.
Despite these declines seen in most hospitals, readmission rates have not declined among all hospitals. Hospitals that have higher proportions of low-income Medicare patients have not had as significant reduction in readmissions as their counterparts.2 One of the biggest complaints leveled at the HRRP program is that it is indifferent to the socioeconomic circumstances of a hospital’s patient population. In many of these hospitals, efforts to reduce readmissions have been seen as futile exercises in a patient population with complex social needs.
A study published in the journal Health Affairs found that socioeconomic factors do appear to drive many of the difference in readmission rates between safety net hospitals and their more prosperous peers. However, it also suggested that hospital performance may play a factor as well.3
The NEJM article, Hospital-Readmission Risk – Isolating Hospital Effects from Patient Effects confirms this. This well-designed review determined that hospitals, independent of a patient’s socioeconomic status, had an impact on the likelihood of patient being readmitted. The more complicated question of what higher functioning hospitals did to reduce readmissions was not addressed. It is certain that some hospitals will face greater challenges in reducing readmissions. It is difficult to determine which socioeconomic factors play the biggest role in driving readmission rates and even more difficult to change them. This study also demonstrates that despite challenging conditions, reductions in readmissions can occur.
As the primary focus and leader of health care in most communities, hospitals are best equipped to reach into the community and to develop successful transition programs that limit readmissions and begin to addressee complex social needs. Of course this must be a coordinated effort among many groups, but the hospital and its organization is in the right position to take a leading role. It is essential that hospitalists, who are on the front lines of this process, play a significant role.Many hospitals with patients who have complex needs are rising to the occasion. Motivated by the HRRP, unique innovations to improve care transitions out of hospitals are being developed. Hospitals that are serving low socioeconomic populations are finding innovative ways to reduce readmissions. These include identifying high-risk social conditions driving readmissions, intensive discharge planning, and deploying community health care workers. A key component of this has been addressing the opioid epidemic.Despite some opposition, the HHRP has worked by aligning financial incentives with good health care. The program was successful not by developing complicated metrics, but rather by simply providing financial incentives for good care and then allowing innovation to develop independently. Hopefully this study further promotes these efforts
Kevin Conrad, MD, is medical director of community affairs and healthy policy at Ochsner Health System, New Orleans.
References
1. Zuckerman RB et al. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016 April 21;374:1543-1551.
2. Jencks SF et al. Hospitalizations among patients in the Medicare Fee-for-Service Program. N Engl J Med. 2009.360(14):1418-1428; Epstein AM et al. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011. 365(24):2287-2295.
3. Kahn C et al. Assessing Medicare’s hospital Pay-for-Performance programs and whether they are achieving their goals. Health Affairs. 2015 Aug;34(8).
The Hospital Readmission Reduction Program (HRRP) was established in 2011 by a provision in the Affordable Care Act (ACA) requiring Medicare to reduce payments to hospitals with relatively high readmission rates for patients in traditional Medicare. Since the inception of the HRRP, readmission rates have declined across all measured diagnostic categories resulting in estimates of 565,000 fewer Medicare readmissions through 2015.1 These reductions seem to be driven by penalties demonstrated by the fact that readmissions fell more quickly at hospitals that had readmission penalties than at other hospitals. Although the severity and fairness of the penalties can be debated, the HRRP has been successful in achieving the goal of reducing readmissions.
Despite these declines seen in most hospitals, readmission rates have not declined among all hospitals. Hospitals that have higher proportions of low-income Medicare patients have not had as significant reduction in readmissions as their counterparts.2 One of the biggest complaints leveled at the HRRP program is that it is indifferent to the socioeconomic circumstances of a hospital’s patient population. In many of these hospitals, efforts to reduce readmissions have been seen as futile exercises in a patient population with complex social needs.
A study published in the journal Health Affairs found that socioeconomic factors do appear to drive many of the difference in readmission rates between safety net hospitals and their more prosperous peers. However, it also suggested that hospital performance may play a factor as well.3
The NEJM article, Hospital-Readmission Risk – Isolating Hospital Effects from Patient Effects confirms this. This well-designed review determined that hospitals, independent of a patient’s socioeconomic status, had an impact on the likelihood of patient being readmitted. The more complicated question of what higher functioning hospitals did to reduce readmissions was not addressed. It is certain that some hospitals will face greater challenges in reducing readmissions. It is difficult to determine which socioeconomic factors play the biggest role in driving readmission rates and even more difficult to change them. This study also demonstrates that despite challenging conditions, reductions in readmissions can occur.
As the primary focus and leader of health care in most communities, hospitals are best equipped to reach into the community and to develop successful transition programs that limit readmissions and begin to addressee complex social needs. Of course this must be a coordinated effort among many groups, but the hospital and its organization is in the right position to take a leading role. It is essential that hospitalists, who are on the front lines of this process, play a significant role.Many hospitals with patients who have complex needs are rising to the occasion. Motivated by the HRRP, unique innovations to improve care transitions out of hospitals are being developed. Hospitals that are serving low socioeconomic populations are finding innovative ways to reduce readmissions. These include identifying high-risk social conditions driving readmissions, intensive discharge planning, and deploying community health care workers. A key component of this has been addressing the opioid epidemic.Despite some opposition, the HHRP has worked by aligning financial incentives with good health care. The program was successful not by developing complicated metrics, but rather by simply providing financial incentives for good care and then allowing innovation to develop independently. Hopefully this study further promotes these efforts
Kevin Conrad, MD, is medical director of community affairs and healthy policy at Ochsner Health System, New Orleans.
References
1. Zuckerman RB et al. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016 April 21;374:1543-1551.
2. Jencks SF et al. Hospitalizations among patients in the Medicare Fee-for-Service Program. N Engl J Med. 2009.360(14):1418-1428; Epstein AM et al. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011. 365(24):2287-2295.
3. Kahn C et al. Assessing Medicare’s hospital Pay-for-Performance programs and whether they are achieving their goals. Health Affairs. 2015 Aug;34(8).
The Hospital Readmission Reduction Program (HRRP) was established in 2011 by a provision in the Affordable Care Act (ACA) requiring Medicare to reduce payments to hospitals with relatively high readmission rates for patients in traditional Medicare. Since the inception of the HRRP, readmission rates have declined across all measured diagnostic categories resulting in estimates of 565,000 fewer Medicare readmissions through 2015.1 These reductions seem to be driven by penalties demonstrated by the fact that readmissions fell more quickly at hospitals that had readmission penalties than at other hospitals. Although the severity and fairness of the penalties can be debated, the HRRP has been successful in achieving the goal of reducing readmissions.
Despite these declines seen in most hospitals, readmission rates have not declined among all hospitals. Hospitals that have higher proportions of low-income Medicare patients have not had as significant reduction in readmissions as their counterparts.2 One of the biggest complaints leveled at the HRRP program is that it is indifferent to the socioeconomic circumstances of a hospital’s patient population. In many of these hospitals, efforts to reduce readmissions have been seen as futile exercises in a patient population with complex social needs.
A study published in the journal Health Affairs found that socioeconomic factors do appear to drive many of the difference in readmission rates between safety net hospitals and their more prosperous peers. However, it also suggested that hospital performance may play a factor as well.3
The NEJM article, Hospital-Readmission Risk – Isolating Hospital Effects from Patient Effects confirms this. This well-designed review determined that hospitals, independent of a patient’s socioeconomic status, had an impact on the likelihood of patient being readmitted. The more complicated question of what higher functioning hospitals did to reduce readmissions was not addressed. It is certain that some hospitals will face greater challenges in reducing readmissions. It is difficult to determine which socioeconomic factors play the biggest role in driving readmission rates and even more difficult to change them. This study also demonstrates that despite challenging conditions, reductions in readmissions can occur.
As the primary focus and leader of health care in most communities, hospitals are best equipped to reach into the community and to develop successful transition programs that limit readmissions and begin to addressee complex social needs. Of course this must be a coordinated effort among many groups, but the hospital and its organization is in the right position to take a leading role. It is essential that hospitalists, who are on the front lines of this process, play a significant role.Many hospitals with patients who have complex needs are rising to the occasion. Motivated by the HRRP, unique innovations to improve care transitions out of hospitals are being developed. Hospitals that are serving low socioeconomic populations are finding innovative ways to reduce readmissions. These include identifying high-risk social conditions driving readmissions, intensive discharge planning, and deploying community health care workers. A key component of this has been addressing the opioid epidemic.Despite some opposition, the HHRP has worked by aligning financial incentives with good health care. The program was successful not by developing complicated metrics, but rather by simply providing financial incentives for good care and then allowing innovation to develop independently. Hopefully this study further promotes these efforts
Kevin Conrad, MD, is medical director of community affairs and healthy policy at Ochsner Health System, New Orleans.
References
1. Zuckerman RB et al. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016 April 21;374:1543-1551.
2. Jencks SF et al. Hospitalizations among patients in the Medicare Fee-for-Service Program. N Engl J Med. 2009.360(14):1418-1428; Epstein AM et al. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011. 365(24):2287-2295.
3. Kahn C et al. Assessing Medicare’s hospital Pay-for-Performance programs and whether they are achieving their goals. Health Affairs. 2015 Aug;34(8).
Poorer-performing hospitals have higher readmission rates than better-performing hospitals for patients with similar diagnoses, a study shows.
Lead author Harlan M. Krumholz, MD, of Yale University, New Haven, Conn., and his colleagues analyzed Centers for Medicare and Medicaid Services hospital-wide readmission data and divided data from July 2014 through June 2015 into two random samples. Researchers used the first sample to calculate the risk-standardized readmission rate within 30 days for each hospital and classified hospitals into performance quartiles, with a lower readmission rate indicating better performance. The second study sample included patients who had two admissions for similar diagnoses at different hospitals that occurred more than 1 month and less than 1 year apart. Researchers compared the observed readmission rates among patients who had been admitted to hospitals in different performance quartiles. The analysis included all discharges occurring from July 1, 2014, through June 30, 2015, from short-term acute care or critical access hospitals in the United States involving Medicare patients who were aged 65 years or older.
Results found that among the patients hospitalized more than once for similar diagnoses at different hospitals, the readmission rate was significantly higher among patients admitted to the worst-performing quartile of hospitals than among those admitted to the best-performing quartile (absolute difference in readmission rate, 2.0 percentage points; 95% confidence interval, 0.4-3.5; P = .001) (N Engl J Med. 2017. doi: 10.1056/NEJMsa1702321). The differences in the comparisons of the other quartiles were smaller and not significant, according to the study. 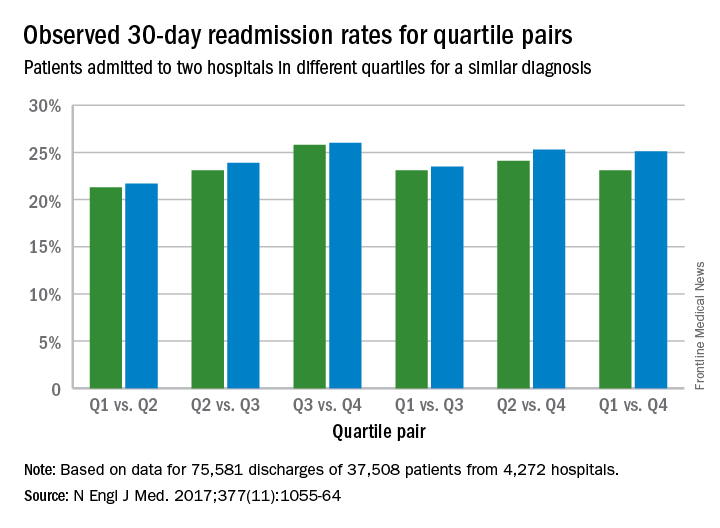
The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors, study authors concluded.
“This study addresses a persistent concern that national readmission measures may reflect differences in unmeasured factors rather than in hospital performance,” they said. “The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors. By studying patients who were admitted twice within 1 year with similar diagnoses to different hospitals, this study design was able to isolate hospital signals of performance while minimizing differences among the patients. In these cases, because the same patients had similar admissions at two hospitals, the characteristics of the patients, including their level of social disadvantage, level of education, or degree of underlying illness, were broadly the same. The alignment of the differences that we observed with the results of the CMS hospital-wide readmission measure also adds to evidence that the readmission measure classifies true differences in performance.”
Dr. Krumholz and seven coauthors reported receiving support from contracts with the Center for Medicare and Medicaid Services to develop and reevaluate performance measures that are used for public reporting.
[email protected]
On Twitter @legal_med
Poorer-performing hospitals have higher readmission rates than better-performing hospitals for patients with similar diagnoses, a study shows.
Lead author Harlan M. Krumholz, MD, of Yale University, New Haven, Conn., and his colleagues analyzed Centers for Medicare and Medicaid Services hospital-wide readmission data and divided data from July 2014 through June 2015 into two random samples. Researchers used the first sample to calculate the risk-standardized readmission rate within 30 days for each hospital and classified hospitals into performance quartiles, with a lower readmission rate indicating better performance. The second study sample included patients who had two admissions for similar diagnoses at different hospitals that occurred more than 1 month and less than 1 year apart. Researchers compared the observed readmission rates among patients who had been admitted to hospitals in different performance quartiles. The analysis included all discharges occurring from July 1, 2014, through June 30, 2015, from short-term acute care or critical access hospitals in the United States involving Medicare patients who were aged 65 years or older.
Results found that among the patients hospitalized more than once for similar diagnoses at different hospitals, the readmission rate was significantly higher among patients admitted to the worst-performing quartile of hospitals than among those admitted to the best-performing quartile (absolute difference in readmission rate, 2.0 percentage points; 95% confidence interval, 0.4-3.5; P = .001) (N Engl J Med. 2017. doi: 10.1056/NEJMsa1702321). The differences in the comparisons of the other quartiles were smaller and not significant, according to the study. 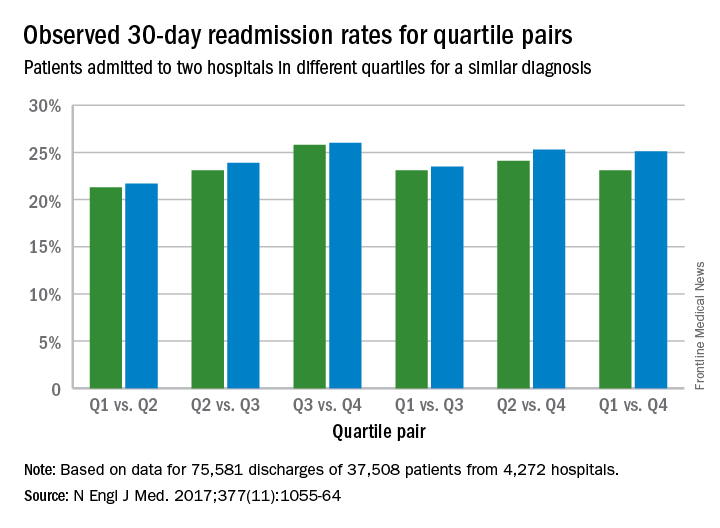
The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors, study authors concluded.
“This study addresses a persistent concern that national readmission measures may reflect differences in unmeasured factors rather than in hospital performance,” they said. “The findings suggest that hospital quality contributes at least in part to readmission rates, independent of patient factors. By studying patients who were admitted twice within 1 year with similar diagnoses to different hospitals, this study design was able to isolate hospital signals of performance while minimizing differences among the patients. In these cases, because the same patients had similar admissions at two hospitals, the characteristics of the patients, including their level of social disadvantage, level of education, or degree of underlying illness, were broadly the same. The alignment of the differences that we observed with the results of the CMS hospital-wide readmission measure also adds to evidence that the readmission measure classifies true differences in performance.”
Dr. Krumholz and seven coauthors reported receiving support from contracts with the Center for Medicare and Medicaid Services to develop and reevaluate performance measures that are used for public reporting.
[email protected]
On Twitter @legal_med
Key clinical point:
Major finding: The readmission rate was significantly higher among patients admitted to the worst-performing quartile of hospitals than among those admitted to the best-performing quartile (absolute difference in readmission rate, 2.0 percentage points).
Data source: Analysis of Centers for Medicare and Medicaid Services hospital-wide readmission data from July 2014 through June 2015.
Disclosures: Dr. Krumholz and seven coauthors reported receiving support from contracts with the Center for Medicare and Medicaid Services to develop and reevaluate performance measures that are used for public reporting.
Thinking about the basic science of quality improvement
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I reviewed recent literature about my research topic, which is clinical pathways for hospitalized injection drug users due to injection-related infection sequelae and came up with my research proposal. As part of a scholarly pursuit, I believe having a theoretical background of quality improvement to be important. Before further diving into the research topic, I also generated a small reading list of the “basic science” of quality improvement, which covers topics of general operational science and those in health care applications.
What makes standardization in health care difficult? In my operations class at Tuck School of Business, we watched a video showing former Soviet Union ophthalmologists performing “assembly line” cataract surgery. It includes multiple surgeons sitting around multiple rotating tables, each surgeon performing exactly one step of the cataract surgery. I recall all my classmates were amused by the video, because it appeared both impractical (as one surgeon was almost chasing the table) as well as slightly de-humanizing. In the health care setting, standardization can be difficult. The service is intrinsically complex, it is difficult to define processes and to measure outcomes, and standardization can create tension secondary to physician autonomy and organizational culture.
In service delivery, the person (the patient in health care organizations) is part of the production process. Patients by nature are not standard inputs. They assume different pre-existing conditions and have different preferences for clinical and non-clinical services/processes. The medical service itself, consisting of both clinical and operational processes, sometimes can be difficult to qualify and measure. A hospital can control patient flow by managing appointment and beds allocation. Clinical pathways can be defined for different diseases. However, patients can encounter undiscovered diseases or complications during the treatment, making the clinical service different and unpredictable.
Lastly standardization can encounter resistance from physicians and other health care providers. “Patients are not cars” is a phrase commonly used when discussing standardization. A health care organization needs to have not only tools, but also the cultural and managerial foundations to carry out changes. I am looking forward to using this project opportunity to further explore the local application of quality improvement.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I reviewed recent literature about my research topic, which is clinical pathways for hospitalized injection drug users due to injection-related infection sequelae and came up with my research proposal. As part of a scholarly pursuit, I believe having a theoretical background of quality improvement to be important. Before further diving into the research topic, I also generated a small reading list of the “basic science” of quality improvement, which covers topics of general operational science and those in health care applications.
What makes standardization in health care difficult? In my operations class at Tuck School of Business, we watched a video showing former Soviet Union ophthalmologists performing “assembly line” cataract surgery. It includes multiple surgeons sitting around multiple rotating tables, each surgeon performing exactly one step of the cataract surgery. I recall all my classmates were amused by the video, because it appeared both impractical (as one surgeon was almost chasing the table) as well as slightly de-humanizing. In the health care setting, standardization can be difficult. The service is intrinsically complex, it is difficult to define processes and to measure outcomes, and standardization can create tension secondary to physician autonomy and organizational culture.
In service delivery, the person (the patient in health care organizations) is part of the production process. Patients by nature are not standard inputs. They assume different pre-existing conditions and have different preferences for clinical and non-clinical services/processes. The medical service itself, consisting of both clinical and operational processes, sometimes can be difficult to qualify and measure. A hospital can control patient flow by managing appointment and beds allocation. Clinical pathways can be defined for different diseases. However, patients can encounter undiscovered diseases or complications during the treatment, making the clinical service different and unpredictable.
Lastly standardization can encounter resistance from physicians and other health care providers. “Patients are not cars” is a phrase commonly used when discussing standardization. A health care organization needs to have not only tools, but also the cultural and managerial foundations to carry out changes. I am looking forward to using this project opportunity to further explore the local application of quality improvement.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform health care and revolutionize patient care. The program has been expanded for the 2017-18 year, offering two options for students to receive funding and engage in scholarly work during their first, second and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I reviewed recent literature about my research topic, which is clinical pathways for hospitalized injection drug users due to injection-related infection sequelae and came up with my research proposal. As part of a scholarly pursuit, I believe having a theoretical background of quality improvement to be important. Before further diving into the research topic, I also generated a small reading list of the “basic science” of quality improvement, which covers topics of general operational science and those in health care applications.
What makes standardization in health care difficult? In my operations class at Tuck School of Business, we watched a video showing former Soviet Union ophthalmologists performing “assembly line” cataract surgery. It includes multiple surgeons sitting around multiple rotating tables, each surgeon performing exactly one step of the cataract surgery. I recall all my classmates were amused by the video, because it appeared both impractical (as one surgeon was almost chasing the table) as well as slightly de-humanizing. In the health care setting, standardization can be difficult. The service is intrinsically complex, it is difficult to define processes and to measure outcomes, and standardization can create tension secondary to physician autonomy and organizational culture.
In service delivery, the person (the patient in health care organizations) is part of the production process. Patients by nature are not standard inputs. They assume different pre-existing conditions and have different preferences for clinical and non-clinical services/processes. The medical service itself, consisting of both clinical and operational processes, sometimes can be difficult to qualify and measure. A hospital can control patient flow by managing appointment and beds allocation. Clinical pathways can be defined for different diseases. However, patients can encounter undiscovered diseases or complications during the treatment, making the clinical service different and unpredictable.
Lastly standardization can encounter resistance from physicians and other health care providers. “Patients are not cars” is a phrase commonly used when discussing standardization. A health care organization needs to have not only tools, but also the cultural and managerial foundations to carry out changes. I am looking forward to using this project opportunity to further explore the local application of quality improvement.
Yun Li is an MD/MBA student attending Geisel School of Medicine and Tuck School of Business at Dartmouth. She obtained her Bachelor of Arts degree from Hanover College double-majoring in Economics and Biological Chemistry. Ms. Li participated in research in injury epidemiology and genetics, and has conducted studies on traditional Tibetan medicine, rural health, health NGOs, and digital health. Her career interest is practicing hospital medicine and geriatrics as a clinician/administrator, either in the US or China. Ms. Li is a student member of the Society of Hospital Medicine.
Upfront preparation key to QI projects
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I am currently working with my mentor, Ian Jenkins, MD, an attending in the Division of Hospital Medicine at the University of California, San Diego, to begin preliminary data collection for our project to cut catheter-associated urinary tract infections (CAUTI). The project time line is on track, and we hope to have things up and running in the next month.
Up to this point, we have been working to identify the most relevant data to collect to best explore our outcome variable. A key goal for our project is to show that increased education measures can ultimately lead to reductions in patient harm. Rather than directly measuring harm reduction, we have settled on tracking the closely identified process measure of the number of inappropriate Foley catheters removed. This measure is potentially more accessible for health care providers than measuring CAUTI rates would be because individual CAUTI events are rare.
In addition to starting data collection, I am quickly learning that conducting a quality improvement project requires a large amount of upfront preparation. Namely, it requires not only identifying the outcome measures you would like to track but also prospectively strategizing about how to track this measure to facilitate future data presentation and publication. Dr. Jenkins has been instrumental as a resource for bouncing off various ideas regarding how to streamline data collection and presentation. He has also been valuable in helping me to identify appropriate units for data collection and teaching me to be forward thinking regarding the best way to collect data for my project. This has truly saved me a significant amount of time and increased the project’s efficiency.
Outside of data collection, we have continued to engage as many stakeholders as we can to ensure the success of the project. Because our project was deemed high priority because of the high CAUTI rates at UCSD, we engaged higher-level hospital administrators who could be onboard with the project, as well as provide their own input to improve project’s effects. Separately, we have continued to collaborate directly with nursing and physician staff to not only share our ongoing project with them but also directly engage them in the project so we can better ensure that the project is not only theoretically palatable but will be realistically implemented as well.
A quality improvement project certainly presents its own unique set of challenges, but I am truly enjoying collaborating and troubleshooting in hopes of ultimately improving patient care.
Victor Ekuta is a third-year medical student at UC San Diego.
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I am currently working with my mentor, Ian Jenkins, MD, an attending in the Division of Hospital Medicine at the University of California, San Diego, to begin preliminary data collection for our project to cut catheter-associated urinary tract infections (CAUTI). The project time line is on track, and we hope to have things up and running in the next month.
Up to this point, we have been working to identify the most relevant data to collect to best explore our outcome variable. A key goal for our project is to show that increased education measures can ultimately lead to reductions in patient harm. Rather than directly measuring harm reduction, we have settled on tracking the closely identified process measure of the number of inappropriate Foley catheters removed. This measure is potentially more accessible for health care providers than measuring CAUTI rates would be because individual CAUTI events are rare.
In addition to starting data collection, I am quickly learning that conducting a quality improvement project requires a large amount of upfront preparation. Namely, it requires not only identifying the outcome measures you would like to track but also prospectively strategizing about how to track this measure to facilitate future data presentation and publication. Dr. Jenkins has been instrumental as a resource for bouncing off various ideas regarding how to streamline data collection and presentation. He has also been valuable in helping me to identify appropriate units for data collection and teaching me to be forward thinking regarding the best way to collect data for my project. This has truly saved me a significant amount of time and increased the project’s efficiency.
Outside of data collection, we have continued to engage as many stakeholders as we can to ensure the success of the project. Because our project was deemed high priority because of the high CAUTI rates at UCSD, we engaged higher-level hospital administrators who could be onboard with the project, as well as provide their own input to improve project’s effects. Separately, we have continued to collaborate directly with nursing and physician staff to not only share our ongoing project with them but also directly engage them in the project so we can better ensure that the project is not only theoretically palatable but will be realistically implemented as well.
A quality improvement project certainly presents its own unique set of challenges, but I am truly enjoying collaborating and troubleshooting in hopes of ultimately improving patient care.
Victor Ekuta is a third-year medical student at UC San Diego.
Editor’s note: The Society of Hospital Medicine’s (SHM’s) Physician in Training Committee launched a scholarship program in 2015 for medical students to help transform healthcare and revolutionize patient care. The program has been expanded for the 2017-2018 year, offering two options for students to receive funding and engage in scholarly work during their first, second, and third years of medical school. As a part of the longitudinal (18-month) program, recipients are required to write about their experience on a monthly basis.
I am currently working with my mentor, Ian Jenkins, MD, an attending in the Division of Hospital Medicine at the University of California, San Diego, to begin preliminary data collection for our project to cut catheter-associated urinary tract infections (CAUTI). The project time line is on track, and we hope to have things up and running in the next month.
Up to this point, we have been working to identify the most relevant data to collect to best explore our outcome variable. A key goal for our project is to show that increased education measures can ultimately lead to reductions in patient harm. Rather than directly measuring harm reduction, we have settled on tracking the closely identified process measure of the number of inappropriate Foley catheters removed. This measure is potentially more accessible for health care providers than measuring CAUTI rates would be because individual CAUTI events are rare.
In addition to starting data collection, I am quickly learning that conducting a quality improvement project requires a large amount of upfront preparation. Namely, it requires not only identifying the outcome measures you would like to track but also prospectively strategizing about how to track this measure to facilitate future data presentation and publication. Dr. Jenkins has been instrumental as a resource for bouncing off various ideas regarding how to streamline data collection and presentation. He has also been valuable in helping me to identify appropriate units for data collection and teaching me to be forward thinking regarding the best way to collect data for my project. This has truly saved me a significant amount of time and increased the project’s efficiency.
Outside of data collection, we have continued to engage as many stakeholders as we can to ensure the success of the project. Because our project was deemed high priority because of the high CAUTI rates at UCSD, we engaged higher-level hospital administrators who could be onboard with the project, as well as provide their own input to improve project’s effects. Separately, we have continued to collaborate directly with nursing and physician staff to not only share our ongoing project with them but also directly engage them in the project so we can better ensure that the project is not only theoretically palatable but will be realistically implemented as well.
A quality improvement project certainly presents its own unique set of challenges, but I am truly enjoying collaborating and troubleshooting in hopes of ultimately improving patient care.
Victor Ekuta is a third-year medical student at UC San Diego.
Everything We Say And Do: The physician patient
Editor’s note: “Everything We Say and Do” provides readers with thoughtful and actionable communication tactics that can positively impact patients’ experience of care. In the next series of columns, physicians will share how their experiences as patients have shaped their professional approach.
In May 2007, I received my acceptance letter for medical school. One month later, I was diagnosed with cancer.
The clinic visit was only supposed to be a routine postoperative follow-up after a simple cyst resection. I really hoped that my doctor was mistaken as he walked me through what to expect, and when he was finished, the desperate look in my eyes demanded answers.
After I fully absorbed the initial shock of the grave news, I eventually found the strength to analyze the situation at hand. Ultimately, I adopted a more positive outlook and fought cancer head on. Contending with cancer while tackling the rigors of medical school was tedious, but despite the hardships, my experience catalyzed my determination and molded my personality as a physician.
What I say and do
I employ active listening and practice patience, especially when it comes to family members.
As both a cancer survivor and a physician, I am able to integrate empathy and diligence by putting myself in my patients’ shoes. My experience in a hospital bed during medical school granted me an extremely intriguing perspective towards medicine.
Why I do it
When I was a patient, the most crucial thing to my family was information. Most physicians did not take the time to explain my course of care, which elevated my family’s angst and anxiety. The experience taught me the importance of patience and communication.
But there were good examples. I still remember the physician who comforted my mother and assuaged her concerns. She held my mother’s hand and showed empathy. When my mother cried, she cried. That physician taught me that it was acceptable for physicians to express emotions.
When my surgeon rounded on me in the morning after my procedure, she was not wearing a white coat, which made her appear relatable. Her contagious confidence and humble demeanor were endorsement enough for her capabilities, showing me that a physician’s persona supersedes the conventional coat.
How I do it
I try to put myself in my patients’ shoes. I rejoice with them. I mourn with them. My uninhibited display of emotions affirms empathy. I dissolve all barriers by not wearing a white coat and ask my patients for a partnership. After all, I once walked miles in those shoes.
Dr. Sharma is a chief hospitalist for Sound Physicians at the Sierra Campus of The Hospitals of Providence, El Paso, Texas. She is a columnist for the El Paso Times and the medical contributor for KVIA Channel 7 ABC News. Her work has appeared on kevinmd.com, Thrive Global, and in El Paso magazine.
Editor’s note: “Everything We Say and Do” provides readers with thoughtful and actionable communication tactics that can positively impact patients’ experience of care. In the next series of columns, physicians will share how their experiences as patients have shaped their professional approach.
In May 2007, I received my acceptance letter for medical school. One month later, I was diagnosed with cancer.
The clinic visit was only supposed to be a routine postoperative follow-up after a simple cyst resection. I really hoped that my doctor was mistaken as he walked me through what to expect, and when he was finished, the desperate look in my eyes demanded answers.
After I fully absorbed the initial shock of the grave news, I eventually found the strength to analyze the situation at hand. Ultimately, I adopted a more positive outlook and fought cancer head on. Contending with cancer while tackling the rigors of medical school was tedious, but despite the hardships, my experience catalyzed my determination and molded my personality as a physician.
What I say and do
I employ active listening and practice patience, especially when it comes to family members.
As both a cancer survivor and a physician, I am able to integrate empathy and diligence by putting myself in my patients’ shoes. My experience in a hospital bed during medical school granted me an extremely intriguing perspective towards medicine.
Why I do it
When I was a patient, the most crucial thing to my family was information. Most physicians did not take the time to explain my course of care, which elevated my family’s angst and anxiety. The experience taught me the importance of patience and communication.
But there were good examples. I still remember the physician who comforted my mother and assuaged her concerns. She held my mother’s hand and showed empathy. When my mother cried, she cried. That physician taught me that it was acceptable for physicians to express emotions.
When my surgeon rounded on me in the morning after my procedure, she was not wearing a white coat, which made her appear relatable. Her contagious confidence and humble demeanor were endorsement enough for her capabilities, showing me that a physician’s persona supersedes the conventional coat.
How I do it
I try to put myself in my patients’ shoes. I rejoice with them. I mourn with them. My uninhibited display of emotions affirms empathy. I dissolve all barriers by not wearing a white coat and ask my patients for a partnership. After all, I once walked miles in those shoes.
Dr. Sharma is a chief hospitalist for Sound Physicians at the Sierra Campus of The Hospitals of Providence, El Paso, Texas. She is a columnist for the El Paso Times and the medical contributor for KVIA Channel 7 ABC News. Her work has appeared on kevinmd.com, Thrive Global, and in El Paso magazine.
Editor’s note: “Everything We Say and Do” provides readers with thoughtful and actionable communication tactics that can positively impact patients’ experience of care. In the next series of columns, physicians will share how their experiences as patients have shaped their professional approach.
In May 2007, I received my acceptance letter for medical school. One month later, I was diagnosed with cancer.
The clinic visit was only supposed to be a routine postoperative follow-up after a simple cyst resection. I really hoped that my doctor was mistaken as he walked me through what to expect, and when he was finished, the desperate look in my eyes demanded answers.
After I fully absorbed the initial shock of the grave news, I eventually found the strength to analyze the situation at hand. Ultimately, I adopted a more positive outlook and fought cancer head on. Contending with cancer while tackling the rigors of medical school was tedious, but despite the hardships, my experience catalyzed my determination and molded my personality as a physician.
What I say and do
I employ active listening and practice patience, especially when it comes to family members.
As both a cancer survivor and a physician, I am able to integrate empathy and diligence by putting myself in my patients’ shoes. My experience in a hospital bed during medical school granted me an extremely intriguing perspective towards medicine.
Why I do it
When I was a patient, the most crucial thing to my family was information. Most physicians did not take the time to explain my course of care, which elevated my family’s angst and anxiety. The experience taught me the importance of patience and communication.
But there were good examples. I still remember the physician who comforted my mother and assuaged her concerns. She held my mother’s hand and showed empathy. When my mother cried, she cried. That physician taught me that it was acceptable for physicians to express emotions.
When my surgeon rounded on me in the morning after my procedure, she was not wearing a white coat, which made her appear relatable. Her contagious confidence and humble demeanor were endorsement enough for her capabilities, showing me that a physician’s persona supersedes the conventional coat.
How I do it
I try to put myself in my patients’ shoes. I rejoice with them. I mourn with them. My uninhibited display of emotions affirms empathy. I dissolve all barriers by not wearing a white coat and ask my patients for a partnership. After all, I once walked miles in those shoes.
Dr. Sharma is a chief hospitalist for Sound Physicians at the Sierra Campus of The Hospitals of Providence, El Paso, Texas. She is a columnist for the El Paso Times and the medical contributor for KVIA Channel 7 ABC News. Her work has appeared on kevinmd.com, Thrive Global, and in El Paso magazine.
Sneak Peek: The Hospital Leader blog – Sept. 2017
Wrongful Life
There have been recent discussions in the lay media about a growing trend of litigation cases focused not on the “right to live,” but rather on the “right to die.” These cases have involved patients who received aggressive treatment, despite having documentation of their wishes not to receive such aggressive treatment. Although unsettling, it is not surprising that this issue has arisen, given the national conversations about the exorbitant cost of care at the end of life in the United States, and the frequency with which patients do not receive end-of-life care that is concordant with their wishes.
These conversations have spurred providers and patients to discuss and document their wishes, via advanced care directives and/or POLST orders (Physicians Orders for Life Sustaining Treatment). There is now even a national day devoted to advanced care decision making (National Healthcare Decisions Day).
But for situations where the paperwork is clear, and the patient actually does receive undesired aggressive care, more plaintiff attorneys are taking on these cases of the “right to die,” since now more people are recognizing and accepting that unwanted life is a type of harm.
This brings to light two important considerations in how we use advanced care planning documentation:
1. These documents should be treated as dynamic decision-making documents, not static documents that are filled out and filed at a single point in time. Patient wishes can and do change due to a variety of factors; any changes should be repeatedly sought to ensure consistency with care plans.
2. These documents should be the start of a conversation, not the end of a conversation. Written documentation can still be wrought with ambiguity; a conversation about the document can help clarify desires and ensure that wishes and care plans match.
In our ongoing desire to “do no harm,” overtreatment is increasingly being recognized by patients and families as a type of harm. To avoid these potentially catastrophic situations, we should all use advanced care documentation as the start of a careful conversation about goals of care and treatment choices. Hospitalists should work with their interprofessional team members (for example, case managers, social workers, nurse navigators, and so on) to make sure every patient has, or is at least working on, advance care directives, and guide the patient and family in decision-making that puts them at ease. With our patients, we can help ensure concordance between their end-of-life wishes and our care plans.
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
Follow You, Follow Me by Tracy Cardin, ACNP-BC, SFHM
SHM Movers & Shakers, Hospital Silos & JHM Research in HM News by Felicia Steele
Wrongful Life
There have been recent discussions in the lay media about a growing trend of litigation cases focused not on the “right to live,” but rather on the “right to die.” These cases have involved patients who received aggressive treatment, despite having documentation of their wishes not to receive such aggressive treatment. Although unsettling, it is not surprising that this issue has arisen, given the national conversations about the exorbitant cost of care at the end of life in the United States, and the frequency with which patients do not receive end-of-life care that is concordant with their wishes.
These conversations have spurred providers and patients to discuss and document their wishes, via advanced care directives and/or POLST orders (Physicians Orders for Life Sustaining Treatment). There is now even a national day devoted to advanced care decision making (National Healthcare Decisions Day).
But for situations where the paperwork is clear, and the patient actually does receive undesired aggressive care, more plaintiff attorneys are taking on these cases of the “right to die,” since now more people are recognizing and accepting that unwanted life is a type of harm.
This brings to light two important considerations in how we use advanced care planning documentation:
1. These documents should be treated as dynamic decision-making documents, not static documents that are filled out and filed at a single point in time. Patient wishes can and do change due to a variety of factors; any changes should be repeatedly sought to ensure consistency with care plans.
2. These documents should be the start of a conversation, not the end of a conversation. Written documentation can still be wrought with ambiguity; a conversation about the document can help clarify desires and ensure that wishes and care plans match.
In our ongoing desire to “do no harm,” overtreatment is increasingly being recognized by patients and families as a type of harm. To avoid these potentially catastrophic situations, we should all use advanced care documentation as the start of a careful conversation about goals of care and treatment choices. Hospitalists should work with their interprofessional team members (for example, case managers, social workers, nurse navigators, and so on) to make sure every patient has, or is at least working on, advance care directives, and guide the patient and family in decision-making that puts them at ease. With our patients, we can help ensure concordance between their end-of-life wishes and our care plans.
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
Follow You, Follow Me by Tracy Cardin, ACNP-BC, SFHM
SHM Movers & Shakers, Hospital Silos & JHM Research in HM News by Felicia Steele
Wrongful Life
There have been recent discussions in the lay media about a growing trend of litigation cases focused not on the “right to live,” but rather on the “right to die.” These cases have involved patients who received aggressive treatment, despite having documentation of their wishes not to receive such aggressive treatment. Although unsettling, it is not surprising that this issue has arisen, given the national conversations about the exorbitant cost of care at the end of life in the United States, and the frequency with which patients do not receive end-of-life care that is concordant with their wishes.
These conversations have spurred providers and patients to discuss and document their wishes, via advanced care directives and/or POLST orders (Physicians Orders for Life Sustaining Treatment). There is now even a national day devoted to advanced care decision making (National Healthcare Decisions Day).
But for situations where the paperwork is clear, and the patient actually does receive undesired aggressive care, more plaintiff attorneys are taking on these cases of the “right to die,” since now more people are recognizing and accepting that unwanted life is a type of harm.
This brings to light two important considerations in how we use advanced care planning documentation:
1. These documents should be treated as dynamic decision-making documents, not static documents that are filled out and filed at a single point in time. Patient wishes can and do change due to a variety of factors; any changes should be repeatedly sought to ensure consistency with care plans.
2. These documents should be the start of a conversation, not the end of a conversation. Written documentation can still be wrought with ambiguity; a conversation about the document can help clarify desires and ensure that wishes and care plans match.
In our ongoing desire to “do no harm,” overtreatment is increasingly being recognized by patients and families as a type of harm. To avoid these potentially catastrophic situations, we should all use advanced care documentation as the start of a careful conversation about goals of care and treatment choices. Hospitalists should work with their interprofessional team members (for example, case managers, social workers, nurse navigators, and so on) to make sure every patient has, or is at least working on, advance care directives, and guide the patient and family in decision-making that puts them at ease. With our patients, we can help ensure concordance between their end-of-life wishes and our care plans.
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
Follow You, Follow Me by Tracy Cardin, ACNP-BC, SFHM
SHM Movers & Shakers, Hospital Silos & JHM Research in HM News by Felicia Steele
New hospitalist unit has stellar patient satisfaction scores
It’s very unusual for hospitalists to achieve top quartile performance on the Physician Communication domain of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. This is the story of a group that did just that for patients on one unit of a large hospital.
I’m not sure how reproducible this would be at other hospitals, or even on other units in the same hospital, and wonder whether performance will stay at this remarkably high level much longer than the current 5-month track record of success. Even so, five months of success suggests they’re on to something.
There is another hospitalist group at that hospital, but I’m discussing work done only by MedOne hospitalists, who together with hospital personnel, developed what they call the Comprehensive Medical Unit (CMU). Their goal was to involve multiple disciplines and use Lean principles to design a new approach to care on 5-Orange, a 20-bed unit in OhioHealth’s Riverside Methodist Hospital in Columbus. The CMU model went live in October 2016.
MedOne Hospital Physicians is a private hospitalist group of 35 physicians and 12 advanced practice clinicians, which comprise nurse practitioners (NPs) and physician assistants (PAs), constituting 46 full-time–equivalent clinical staffing. The group contracts with Riverside, which has approximately 710 staffed beds. MedOne also works in area skilled nursing facilities, helps a long-term acute care and rehabilitation hospital, and provides support to two other hospitals that are not part of OhioHealth.
Features of the model
At its core, this model is a variation of the increasingly common combination of geographically assigned hospitalists (who in this case don’t have patients elsewhere in the hospital) and multidisciplinary rounds (that is, the physician and NP hospitalists make bedside rounds with a nurse and pharmacist). But their model also incorporates a few less-common features.
Only 4 of the 35 MedOne hospitalists are eligible to provide care on the CMU, and each still spends a significant portion of time in the regular hospitalist rotation working in the rest of the hospital. These doctors weren’t selected as the highest performers or because they had the best patient satisfaction track record. Instead, five MedOne doctors volunteered to work on the unit, and four were chosen. A MedOne hospitalist NP also works on the unit, since any NP in the group is eligible to work there.
This is a hospitalist-only unit; no non–hospitalist patients are placed on the unit. There is no deliberate attempt to assign patients to the unit based on how sick they are or complicated their cases are. All are general medicine patients, including up to six intermediate care patients (e.g., “ICU step-down” patients requiring mask ventilation, etc.). While configured for 20 patients, the unit can flex to as many as 24 patients and has done so numerous times. The hospitalists (physician and NP combined) have averaged 18.9 daily encounters since the CMU opened.
Nurse staffing on the unit was reconfigured to comprise bedside nurses – known as Clinical Nurses (CNs) – and more experienced RNs – in the role of Comprehensive Charge Nurses (CCNs), who attend rounds and coordinate the patients’ hospitalizations rather than doing bedside care. 5-Orange has one more Charge Nurse than is typical for other units in the hospital, so total RN-to-patient staffing levels and nurse staffing costs are higher. But the CNs care for the same number of patients as do their counterparts in other hospital units.
In order to try to discharge patients early in the day, the NP sees only the patients who are being discharged, while the physician makes all other visits. When possible, I think it’s best to minimize the incidence of a provider’s first visit with a patient being a discharge visit; this may increase the risk of misunderstandings and errors. Instead, in this model, the physician working on the CMU will already know the patient from the preceding days and will be on the unit and readily accessible to the NP all day, which might mitigate some of these concerns.
Outcomes
I think the most notable outcome is the top quartile patient satisfaction scores from the 37 patients cared for on the unit who returned a survey, some of whom have asked to return to the CMU if they’re hospitalized again. Specifically, 86% of responses were “top box,” which places the hospitalists at the 84th percentile of performance for all hospitals. Physician Communication scores on the HCAHPS survey for hospitalists on other units at this hospital are in the bottom deciles, which is more typical for hospitalists.
Length of stay is half a day shorter than comparable units with similar readmission rates, and more patients are discharged earlier in the day. The four hospitalists who work on the unit report higher satisfaction, in part because they get an average of only 1 page a day – compared with the typical 15-40 pages their colleagues get working elsewhere in the hospital.
Cautions
I’m not sure why the MedOne model has yielded such impressive patient satisfaction and other results. While there are some relatively unique features of their model – only four hospitalists are eligible to work there and nursing roles have been reconfigured – I wouldn’t expect these to yield such remarkable results. So far, they have roughly 5 months of data and just 37 returned patient satisfaction surveys, so it’s possible that random variation and/or the Hawthorne effect are playing a meaningful role. It will be really informative to see their outcomes a year or 2 from now and to gauge how they fare if and when they implement the same model in other units of the hospital.
I suspect MedOne’s precise configuration for staffing and roles of nurses, NPs, and physicians is important, but I’m guessing the most valuable thing they implemented was the creation of a powerful sense of teamwork and shared purpose among those working on the unit. The interpersonal bonding and feeling of shared purpose that likely occurred as they worked to devise and go live with the model, as well as the tremendous satisfaction at seeing their early results, have probably led to terrific enthusiasm within their team.
That enthusiasm may be the key ingredient contributing to their early success.
Dr. Nelson has been working in clinical practice as a hospitalist since 1988. He is a cofounder and past president of Society of Hospital Medicine and a principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice-management courses. Contact him at [email protected]
It’s very unusual for hospitalists to achieve top quartile performance on the Physician Communication domain of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. This is the story of a group that did just that for patients on one unit of a large hospital.
I’m not sure how reproducible this would be at other hospitals, or even on other units in the same hospital, and wonder whether performance will stay at this remarkably high level much longer than the current 5-month track record of success. Even so, five months of success suggests they’re on to something.
There is another hospitalist group at that hospital, but I’m discussing work done only by MedOne hospitalists, who together with hospital personnel, developed what they call the Comprehensive Medical Unit (CMU). Their goal was to involve multiple disciplines and use Lean principles to design a new approach to care on 5-Orange, a 20-bed unit in OhioHealth’s Riverside Methodist Hospital in Columbus. The CMU model went live in October 2016.
MedOne Hospital Physicians is a private hospitalist group of 35 physicians and 12 advanced practice clinicians, which comprise nurse practitioners (NPs) and physician assistants (PAs), constituting 46 full-time–equivalent clinical staffing. The group contracts with Riverside, which has approximately 710 staffed beds. MedOne also works in area skilled nursing facilities, helps a long-term acute care and rehabilitation hospital, and provides support to two other hospitals that are not part of OhioHealth.
Features of the model
At its core, this model is a variation of the increasingly common combination of geographically assigned hospitalists (who in this case don’t have patients elsewhere in the hospital) and multidisciplinary rounds (that is, the physician and NP hospitalists make bedside rounds with a nurse and pharmacist). But their model also incorporates a few less-common features.
Only 4 of the 35 MedOne hospitalists are eligible to provide care on the CMU, and each still spends a significant portion of time in the regular hospitalist rotation working in the rest of the hospital. These doctors weren’t selected as the highest performers or because they had the best patient satisfaction track record. Instead, five MedOne doctors volunteered to work on the unit, and four were chosen. A MedOne hospitalist NP also works on the unit, since any NP in the group is eligible to work there.
This is a hospitalist-only unit; no non–hospitalist patients are placed on the unit. There is no deliberate attempt to assign patients to the unit based on how sick they are or complicated their cases are. All are general medicine patients, including up to six intermediate care patients (e.g., “ICU step-down” patients requiring mask ventilation, etc.). While configured for 20 patients, the unit can flex to as many as 24 patients and has done so numerous times. The hospitalists (physician and NP combined) have averaged 18.9 daily encounters since the CMU opened.
Nurse staffing on the unit was reconfigured to comprise bedside nurses – known as Clinical Nurses (CNs) – and more experienced RNs – in the role of Comprehensive Charge Nurses (CCNs), who attend rounds and coordinate the patients’ hospitalizations rather than doing bedside care. 5-Orange has one more Charge Nurse than is typical for other units in the hospital, so total RN-to-patient staffing levels and nurse staffing costs are higher. But the CNs care for the same number of patients as do their counterparts in other hospital units.
In order to try to discharge patients early in the day, the NP sees only the patients who are being discharged, while the physician makes all other visits. When possible, I think it’s best to minimize the incidence of a provider’s first visit with a patient being a discharge visit; this may increase the risk of misunderstandings and errors. Instead, in this model, the physician working on the CMU will already know the patient from the preceding days and will be on the unit and readily accessible to the NP all day, which might mitigate some of these concerns.
Outcomes
I think the most notable outcome is the top quartile patient satisfaction scores from the 37 patients cared for on the unit who returned a survey, some of whom have asked to return to the CMU if they’re hospitalized again. Specifically, 86% of responses were “top box,” which places the hospitalists at the 84th percentile of performance for all hospitals. Physician Communication scores on the HCAHPS survey for hospitalists on other units at this hospital are in the bottom deciles, which is more typical for hospitalists.
Length of stay is half a day shorter than comparable units with similar readmission rates, and more patients are discharged earlier in the day. The four hospitalists who work on the unit report higher satisfaction, in part because they get an average of only 1 page a day – compared with the typical 15-40 pages their colleagues get working elsewhere in the hospital.
Cautions
I’m not sure why the MedOne model has yielded such impressive patient satisfaction and other results. While there are some relatively unique features of their model – only four hospitalists are eligible to work there and nursing roles have been reconfigured – I wouldn’t expect these to yield such remarkable results. So far, they have roughly 5 months of data and just 37 returned patient satisfaction surveys, so it’s possible that random variation and/or the Hawthorne effect are playing a meaningful role. It will be really informative to see their outcomes a year or 2 from now and to gauge how they fare if and when they implement the same model in other units of the hospital.
I suspect MedOne’s precise configuration for staffing and roles of nurses, NPs, and physicians is important, but I’m guessing the most valuable thing they implemented was the creation of a powerful sense of teamwork and shared purpose among those working on the unit. The interpersonal bonding and feeling of shared purpose that likely occurred as they worked to devise and go live with the model, as well as the tremendous satisfaction at seeing their early results, have probably led to terrific enthusiasm within their team.
That enthusiasm may be the key ingredient contributing to their early success.
Dr. Nelson has been working in clinical practice as a hospitalist since 1988. He is a cofounder and past president of Society of Hospital Medicine and a principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice-management courses. Contact him at [email protected]
It’s very unusual for hospitalists to achieve top quartile performance on the Physician Communication domain of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. This is the story of a group that did just that for patients on one unit of a large hospital.
I’m not sure how reproducible this would be at other hospitals, or even on other units in the same hospital, and wonder whether performance will stay at this remarkably high level much longer than the current 5-month track record of success. Even so, five months of success suggests they’re on to something.
There is another hospitalist group at that hospital, but I’m discussing work done only by MedOne hospitalists, who together with hospital personnel, developed what they call the Comprehensive Medical Unit (CMU). Their goal was to involve multiple disciplines and use Lean principles to design a new approach to care on 5-Orange, a 20-bed unit in OhioHealth’s Riverside Methodist Hospital in Columbus. The CMU model went live in October 2016.
MedOne Hospital Physicians is a private hospitalist group of 35 physicians and 12 advanced practice clinicians, which comprise nurse practitioners (NPs) and physician assistants (PAs), constituting 46 full-time–equivalent clinical staffing. The group contracts with Riverside, which has approximately 710 staffed beds. MedOne also works in area skilled nursing facilities, helps a long-term acute care and rehabilitation hospital, and provides support to two other hospitals that are not part of OhioHealth.
Features of the model
At its core, this model is a variation of the increasingly common combination of geographically assigned hospitalists (who in this case don’t have patients elsewhere in the hospital) and multidisciplinary rounds (that is, the physician and NP hospitalists make bedside rounds with a nurse and pharmacist). But their model also incorporates a few less-common features.
Only 4 of the 35 MedOne hospitalists are eligible to provide care on the CMU, and each still spends a significant portion of time in the regular hospitalist rotation working in the rest of the hospital. These doctors weren’t selected as the highest performers or because they had the best patient satisfaction track record. Instead, five MedOne doctors volunteered to work on the unit, and four were chosen. A MedOne hospitalist NP also works on the unit, since any NP in the group is eligible to work there.
This is a hospitalist-only unit; no non–hospitalist patients are placed on the unit. There is no deliberate attempt to assign patients to the unit based on how sick they are or complicated their cases are. All are general medicine patients, including up to six intermediate care patients (e.g., “ICU step-down” patients requiring mask ventilation, etc.). While configured for 20 patients, the unit can flex to as many as 24 patients and has done so numerous times. The hospitalists (physician and NP combined) have averaged 18.9 daily encounters since the CMU opened.
Nurse staffing on the unit was reconfigured to comprise bedside nurses – known as Clinical Nurses (CNs) – and more experienced RNs – in the role of Comprehensive Charge Nurses (CCNs), who attend rounds and coordinate the patients’ hospitalizations rather than doing bedside care. 5-Orange has one more Charge Nurse than is typical for other units in the hospital, so total RN-to-patient staffing levels and nurse staffing costs are higher. But the CNs care for the same number of patients as do their counterparts in other hospital units.
In order to try to discharge patients early in the day, the NP sees only the patients who are being discharged, while the physician makes all other visits. When possible, I think it’s best to minimize the incidence of a provider’s first visit with a patient being a discharge visit; this may increase the risk of misunderstandings and errors. Instead, in this model, the physician working on the CMU will already know the patient from the preceding days and will be on the unit and readily accessible to the NP all day, which might mitigate some of these concerns.
Outcomes
I think the most notable outcome is the top quartile patient satisfaction scores from the 37 patients cared for on the unit who returned a survey, some of whom have asked to return to the CMU if they’re hospitalized again. Specifically, 86% of responses were “top box,” which places the hospitalists at the 84th percentile of performance for all hospitals. Physician Communication scores on the HCAHPS survey for hospitalists on other units at this hospital are in the bottom deciles, which is more typical for hospitalists.
Length of stay is half a day shorter than comparable units with similar readmission rates, and more patients are discharged earlier in the day. The four hospitalists who work on the unit report higher satisfaction, in part because they get an average of only 1 page a day – compared with the typical 15-40 pages their colleagues get working elsewhere in the hospital.
Cautions
I’m not sure why the MedOne model has yielded such impressive patient satisfaction and other results. While there are some relatively unique features of their model – only four hospitalists are eligible to work there and nursing roles have been reconfigured – I wouldn’t expect these to yield such remarkable results. So far, they have roughly 5 months of data and just 37 returned patient satisfaction surveys, so it’s possible that random variation and/or the Hawthorne effect are playing a meaningful role. It will be really informative to see their outcomes a year or 2 from now and to gauge how they fare if and when they implement the same model in other units of the hospital.
I suspect MedOne’s precise configuration for staffing and roles of nurses, NPs, and physicians is important, but I’m guessing the most valuable thing they implemented was the creation of a powerful sense of teamwork and shared purpose among those working on the unit. The interpersonal bonding and feeling of shared purpose that likely occurred as they worked to devise and go live with the model, as well as the tremendous satisfaction at seeing their early results, have probably led to terrific enthusiasm within their team.
That enthusiasm may be the key ingredient contributing to their early success.
Dr. Nelson has been working in clinical practice as a hospitalist since 1988. He is a cofounder and past president of Society of Hospital Medicine and a principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice-management courses. Contact him at [email protected]
QI enthusiast to QI leader: Jonathan Bae, MD, SFHM
Editor’s Note: This SHM series highlights the professional pathways of quality improvement leaders. This month features the story of Jonathan Bae, MD, SFHM, associate chief medical officer for patient and clinical quality at Duke University Health System, Durham, N.C.
With a father and two sisters in medicine, Jonathan Bae was destined to become a physician – or something completely different, as he explains.
“Either outcome is common when you have a parent who is a doctor,” said Dr. Bae, who has two siblings who chose a different career path. But while Dr. Bae’s desire to be a clinician was set at an early age, his interest in quality improvement work came much later.
Twelve years ago, Dr. Bae matched in Duke’s Medicine-Pediatrics residency program because he wanted to be well equipped to treat patients across the age spectrum. Completing residency in 2009, Dr. Bae enjoyed providing clinical care as a hospitalist, but discovered that he also enjoyed teaching. To enhance his skills as a clinician educator, Dr. Bae enrolled in the Academic Hospitalist Academy, where the curriculum introduced him to quality improvement and patient safety, and some aspects of hospital administration. “Jeff Glasheen’s talk on the drivers of medicine, and how to find your unique voice and identity … brought together my interest in education and quality work,” Dr. Bae recalled.
“I left the meeting energized with new information, and then the opportunity came up to lead a QI initiative here,” he said. The project focused on improving improve care delivery to diabetic patients, specifically the completion of foot exams. “We saw our rates of screening go from less than 50% to greater than 80%,” Dr. Bae said. “I found it to be extremely gratifying to be involved in implementing changes that could lead to care improvement for patients.”
Once Dr. Bae made his interests in QI work known to colleagues and administrators, the projects came readily. Following his chief residency year, Dr. Bae remained with Duke Medicine Residency Program as an associate program director for QI, “which was a great platform for doing project work that aligned my interests in teaching and doing QI work,” he said. In addition to developing a residency curriculum in QI, Dr. Bae initiated a program to incentivize GME trainees across the health system in performance metrics such as readmissions, patient satisfaction, hand hygiene, and safety event reporting. The outcomes, Dr. Bae said, “have had an improved quality and safety impact on our organization.”
From there, Dr. Bae initiated multiple projects focused on reducing readmissions and mortality. Currently, he is standardizing the mortality review process across three hospitals in Duke’s health system. Consistent methodology and language will allow for more accurate analysis and comparison of factors contributing to patient mortality in the system, Dr. Bae said, adding, “We have already learned a lot about care delivery and operations, and measures that can be taken to reduce gaps in care delivery and keep patients safe.”
Looking back on the days when he only thought about providing care, Dr. Bae said, “my world view has changed but my desire to change the world hasn’t. I now do more quality work because I find it so gratifying. In the QI space, I’m affecting not one, but many people at a time.”
He encourages hospitalists with similar interests to seek out colleagues and leaders – internal and external to their institutions – that will help them initiate and implement projects that feed their passions. Getting to know the QI basics is the simple part, Dr. Bae said.
“There’s no magic behind PDSA cycles or models of improvement,” he said. “It’s the team and people you pull together that makes a project successful.”
His current work centers on understanding and building health care provider resiliency at Duke. “I feel this … is going to make a tremendous difference for our organization,” Dr. Bae said. “The system should be designed to promote well-being, not just prevent burnout.”
Claudia Stahl is content manager at the Society of Hospital Medicine.
Editor’s Note: This SHM series highlights the professional pathways of quality improvement leaders. This month features the story of Jonathan Bae, MD, SFHM, associate chief medical officer for patient and clinical quality at Duke University Health System, Durham, N.C.
With a father and two sisters in medicine, Jonathan Bae was destined to become a physician – or something completely different, as he explains.
“Either outcome is common when you have a parent who is a doctor,” said Dr. Bae, who has two siblings who chose a different career path. But while Dr. Bae’s desire to be a clinician was set at an early age, his interest in quality improvement work came much later.
Twelve years ago, Dr. Bae matched in Duke’s Medicine-Pediatrics residency program because he wanted to be well equipped to treat patients across the age spectrum. Completing residency in 2009, Dr. Bae enjoyed providing clinical care as a hospitalist, but discovered that he also enjoyed teaching. To enhance his skills as a clinician educator, Dr. Bae enrolled in the Academic Hospitalist Academy, where the curriculum introduced him to quality improvement and patient safety, and some aspects of hospital administration. “Jeff Glasheen’s talk on the drivers of medicine, and how to find your unique voice and identity … brought together my interest in education and quality work,” Dr. Bae recalled.
“I left the meeting energized with new information, and then the opportunity came up to lead a QI initiative here,” he said. The project focused on improving improve care delivery to diabetic patients, specifically the completion of foot exams. “We saw our rates of screening go from less than 50% to greater than 80%,” Dr. Bae said. “I found it to be extremely gratifying to be involved in implementing changes that could lead to care improvement for patients.”
Once Dr. Bae made his interests in QI work known to colleagues and administrators, the projects came readily. Following his chief residency year, Dr. Bae remained with Duke Medicine Residency Program as an associate program director for QI, “which was a great platform for doing project work that aligned my interests in teaching and doing QI work,” he said. In addition to developing a residency curriculum in QI, Dr. Bae initiated a program to incentivize GME trainees across the health system in performance metrics such as readmissions, patient satisfaction, hand hygiene, and safety event reporting. The outcomes, Dr. Bae said, “have had an improved quality and safety impact on our organization.”
From there, Dr. Bae initiated multiple projects focused on reducing readmissions and mortality. Currently, he is standardizing the mortality review process across three hospitals in Duke’s health system. Consistent methodology and language will allow for more accurate analysis and comparison of factors contributing to patient mortality in the system, Dr. Bae said, adding, “We have already learned a lot about care delivery and operations, and measures that can be taken to reduce gaps in care delivery and keep patients safe.”
Looking back on the days when he only thought about providing care, Dr. Bae said, “my world view has changed but my desire to change the world hasn’t. I now do more quality work because I find it so gratifying. In the QI space, I’m affecting not one, but many people at a time.”
He encourages hospitalists with similar interests to seek out colleagues and leaders – internal and external to their institutions – that will help them initiate and implement projects that feed their passions. Getting to know the QI basics is the simple part, Dr. Bae said.
“There’s no magic behind PDSA cycles or models of improvement,” he said. “It’s the team and people you pull together that makes a project successful.”
His current work centers on understanding and building health care provider resiliency at Duke. “I feel this … is going to make a tremendous difference for our organization,” Dr. Bae said. “The system should be designed to promote well-being, not just prevent burnout.”
Claudia Stahl is content manager at the Society of Hospital Medicine.
Editor’s Note: This SHM series highlights the professional pathways of quality improvement leaders. This month features the story of Jonathan Bae, MD, SFHM, associate chief medical officer for patient and clinical quality at Duke University Health System, Durham, N.C.
With a father and two sisters in medicine, Jonathan Bae was destined to become a physician – or something completely different, as he explains.
“Either outcome is common when you have a parent who is a doctor,” said Dr. Bae, who has two siblings who chose a different career path. But while Dr. Bae’s desire to be a clinician was set at an early age, his interest in quality improvement work came much later.
Twelve years ago, Dr. Bae matched in Duke’s Medicine-Pediatrics residency program because he wanted to be well equipped to treat patients across the age spectrum. Completing residency in 2009, Dr. Bae enjoyed providing clinical care as a hospitalist, but discovered that he also enjoyed teaching. To enhance his skills as a clinician educator, Dr. Bae enrolled in the Academic Hospitalist Academy, where the curriculum introduced him to quality improvement and patient safety, and some aspects of hospital administration. “Jeff Glasheen’s talk on the drivers of medicine, and how to find your unique voice and identity … brought together my interest in education and quality work,” Dr. Bae recalled.
“I left the meeting energized with new information, and then the opportunity came up to lead a QI initiative here,” he said. The project focused on improving improve care delivery to diabetic patients, specifically the completion of foot exams. “We saw our rates of screening go from less than 50% to greater than 80%,” Dr. Bae said. “I found it to be extremely gratifying to be involved in implementing changes that could lead to care improvement for patients.”
Once Dr. Bae made his interests in QI work known to colleagues and administrators, the projects came readily. Following his chief residency year, Dr. Bae remained with Duke Medicine Residency Program as an associate program director for QI, “which was a great platform for doing project work that aligned my interests in teaching and doing QI work,” he said. In addition to developing a residency curriculum in QI, Dr. Bae initiated a program to incentivize GME trainees across the health system in performance metrics such as readmissions, patient satisfaction, hand hygiene, and safety event reporting. The outcomes, Dr. Bae said, “have had an improved quality and safety impact on our organization.”
From there, Dr. Bae initiated multiple projects focused on reducing readmissions and mortality. Currently, he is standardizing the mortality review process across three hospitals in Duke’s health system. Consistent methodology and language will allow for more accurate analysis and comparison of factors contributing to patient mortality in the system, Dr. Bae said, adding, “We have already learned a lot about care delivery and operations, and measures that can be taken to reduce gaps in care delivery and keep patients safe.”
Looking back on the days when he only thought about providing care, Dr. Bae said, “my world view has changed but my desire to change the world hasn’t. I now do more quality work because I find it so gratifying. In the QI space, I’m affecting not one, but many people at a time.”
He encourages hospitalists with similar interests to seek out colleagues and leaders – internal and external to their institutions – that will help them initiate and implement projects that feed their passions. Getting to know the QI basics is the simple part, Dr. Bae said.
“There’s no magic behind PDSA cycles or models of improvement,” he said. “It’s the team and people you pull together that makes a project successful.”
His current work centers on understanding and building health care provider resiliency at Duke. “I feel this … is going to make a tremendous difference for our organization,” Dr. Bae said. “The system should be designed to promote well-being, not just prevent burnout.”
Claudia Stahl is content manager at the Society of Hospital Medicine.