User login
Does U.S. Healthcare Need More Diverse Leadership?
Throughout its history, the United States has been a nation of immigrants. From the early colonial settlements to the mid-20th century, most immigrants came from Western European countries. Since 1965, when the Immigration and Nationality Act abolished national-origin quotas, the diversity of immigrants has increased. “By the year 2043,” says Tomás León, president and CEO of the Institute for Diversity in Health Management in Chicago, “we will be a country where the majority of our population is comprised of racial and ethnic minorities.”
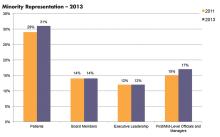
Those changing demographics, cited from the U.S. Census Bureau’s projections, already are evidenced in hospital patient populations. According to a benchmarking survey sponsored by the institute, which is an affiliate of the American Hospital Association, the percentage of minority patients seen in hospitals grew from 29% to 31% of patient census between 2011 and 2013.1 And yet, the survey found this increasing diversity is not currently reflected in leadership positions. During the same time period, underrepresented racial and ethnic minorities (UREM) on hospital boards of directors (14%) and in C-suite positions (14%) remained flat (see Figure 1).
Gender disparities in healthcare and academic leadership also have been slow to change. Periodic surveys conducted by the American College of Healthcare Executives indicate that women comprise only 11% of healthcare CEOs in the U.S.2 And despite the fact that women make up half of all medical students (and one-third of full-time faculty), the Association of American Medical Colleges (AAMC) finds that women still trail men when it comes to attaining full professorship and decanal positions at their academic institutions.3
The Hospitalist interviewed medical directors, researchers, diversity management professionals, and hospitalists to ascertain current solutions being pursued to narrow the gaps in leadership diversity.
Why Diversity in Leadership Matters
Eric E. Howell, MD, MHM, chief of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in the Hopkins School of Medicine in Baltimore, believes there is a need to encourage the advancement to leadership positions for female and UREM physicians.
“In medicine, it’s really about service. If we are really here for our patients, we need representation of diversity in our faculty and leadership,” says Dr. Howell, a past SHM president and faculty member of SHM’s Leadership Academy since its inception in 2005. In addition, he says, “Diversity adds incredible strength to an organization and adds to the richness of the ideas and solutions to overcome challenging problems.”
With the implementation of the Affordable Care Act, formerly uninsured people are now accessing the healthcare system; many are bilingual and bicultural, notes George A. Zeppenfeldt-Cestero, president and CEO, Association of Hispanic Healthcare Executives.
“You want to make sure that providers, whether they are physicians, nurses, dentists, or health executives that drive policy issues, are also reflective of that population throughout the organization,” he says. “The real definition of diversity is making sure you have diversity in all layers of the workforce, including the C-suite.”
León points to the coming “seismic demographic shifts” and wonders if healthcare is ready to become more reflective of the communities it serves.
“Increasing diversity in healthcare leadership and governance is essential for the delivery and provision of culturally competent care,” León says. “Now, more than ever, it’s important that we collectively accelerate progress in this area.”
Advancing in Academic and Hospital Medicine
Might hospital medicine offer additional opportunities for women and minorities to advance into leadership positions? Hospitalist Flora Kisuule, MD, SFHM, assistant professor of medicine at Johns Hopkins School of Medicine and associate division director of the Collaborative Inpatient Medicine Service (CIMS) at Johns Hopkins Bayview Medical Center, believes this may be the case. She was with Dr. Howell’s group when he needed to fill the associate director position.
“My advancement speaks to hospital medicine and the fact that we are growing as a field,” she says. “Because of that, opportunities are presenting themselves.”
Dr. Kisuule’s ability to thrive in her position speaks to her professionalism but also to a number of other intentional factors: Dr. Howell’s continuing sponsorship to include her in leadership opportunities, an emergency call system for parents with sick children, and a women’s task force whose agenda calls for transparency in hiring and advancement.
Intentional Structure Change
Cardiologist Hannah A. Valantine, MD, recognizes the importance of addressing the lack of women and people from unrepresented groups in the Science, Technology, Engineering, and Mathematics (STEM) workforce. While at Stanford University School of Medicine, she developed and put into place a set of strategies to understand and mitigate the drivers of gender imbalance. Since then, Dr. Valantine was recruited to bring her expertise to the National Institutes of Health in Bethesda, Md., where she is the inaugural chief officer for scientific workforce diversity. In this role, she is committed “to promoting biomedical workforce diversity as an opportunity, not a problem.”
Dr. Valantine is pushing NIH to pursue a wide range of evidence-based programming to eliminate career-transition barriers that keep women and individuals from underrepresented groups from attaining spots in the top echelons of science and health leadership. She believes that applying scientific rigor to the issue of workforce diversity can lead to quantifiable, translatable, and repeatable methods for recruitment and retention of talent in the biomedical workforce (see “Building Blocks").
Before joining NIH, Dr. Valantine and her colleagues at Stanford surveyed gender composition and faculty satisfaction several years after initiating a multifaceted intervention to boost recruitment and development of women faculty.4 After making a visible commitment of resources to support faculty, with special attention to women, Stanford rose from below to above national benchmarks in the representation of women among faculty. Yet significant work remains to be done, Dr. Valantine says. Her work predicts that the estimated time to achieve 50% occupancy of full professorships by women nationally approaches 50 years—“far too long using current approaches.”
In a separate review article, Dr. Valantine and co-author Christy Sandborg, MD, described the Stanford University School of Medicine Academic Biomedical Career Customization (ABCC) model, which was adapted from Deloitte’s Mass Career Customization framework and allows for development of individual career plans that span a faculty member’s total career, not just a year or two at a time. Long-term planning can enable better alignment between the work culture and values of the workforce, which will improve the outlook for women faculty, Dr. Valantine says.
The issues of work-life balance may actually be generational, Dr. Valantine explains. Veteran hospitalist Janet Nagamine, MD, BSN, SFHM, of Santa Clara, Calif., agrees.
“Nowadays, men as well as women are looking for work-life balance,” she says.
In hospital medicine, Dr. Nagamine points out, the structural changes required to effect a work-life balance for hospital leaders are often difficult to achieve.
“As productivity surveys show, HM group leaders are putting in as many RVUs as the staff,” the former SHM board member says. “There is no dedicated time for administrative duties.”
Construct a Pipeline
Barriers to advancement often are particular to characteristics of diverse populations. For example, the AAMC’s report on the U.S. physician workforce documents that in African-American physicians 40 and younger, women outnumber their male counterparts. Therefore, in the association’s Diversity in Medical Education: Facts and Figures 2012 report, the executive summary points out the need to strengthen the medical education pipeline to increase the number of African-American males who enter the premed track.
Despite the fast-growing percentage of Latino and Hispanic populations in the United States, the shortage of Latino/Hispanic physicians increased from 1980 to 2010. Latinos/Hispanics are greatly underrepresented in the medical student, resident, and faculty populations, according to John Paul Sánchez, MD, MPH, assistant dean for diversity and inclusion in the Office for Diversity and Community Engagement at Rutgers, The State University of New Jersey. Likewise, Zeppenfeldt-Cestero believes that efforts must begin much earlier with Latino and other minority and underrepresented students.
“We have to make sure our students pursue the STEM disciplines and that they also later have the education and preparation to be competitive at the MBA or MPH levels,” he says.
Dr. Sánchez, an associate professor of emergency medicine and a diversity activist since his med school days, is the recipient of last year’s Association of Hispanic Healthcare Executives’ academic leader of the year award. Since September 2014, he has been involved with Building the Next Generation of Academic Physicians Inc., which collaborates with more than 40 medical schools across the country. The initiative offers conferences designed to develop diverse medical students’ and residents’ interest in pursuing academic medicine. Open to all medical students and residents, the conference curriculum is tailored for women, UREMs, and trainees who identify as lesbian, gay, bisexual, or transgender (LGBT), he says. Seven conferences were held in 2015, 10 are planned for this year, and seven for 2017.
Healthcare Leadership Gaps
Despite their omnipresence in healthcare, there is a dearth of women in chief executive and governance roles, as has been noted by both the American College of Healthcare Executives and the National Center for Healthcare Leadership. As with academic leadership positions, the leadership gap in the administrative sector does not seem to be due to a lack of women entering graduate programs in health administration. On the contrary, since the mid-1980s women have comprised 50% to 60% of graduate students.
“This is absolutely not a pipeline issue,” says Christy Harris Lemak, PhD, FACHE, professor and chair of the Department of Health Services Administration at the University of Alabama at Birmingham School of Health Professions and lead investigator of the National Center for Healthcare Leadership’s study of women in healthcare executive positions. Other factors come into play.
In the study, she and her co-authors queried female healthcare CEOs to ascertain the critical career inflection points that led to their success.6 Those who were strategic about their careers, sought out mentors, and voiced their intentions about pursuing leadership positions were more likely to be successful in those efforts. However, individual career efforts must be coupled with overall organizational commitment to fostering inclusion (see “Path to the Top: Strategic Advice for Women").
Hospitals and healthcare organizations must pursue the development of human capital (and the diversity of their leaders) in a systematic way. “We recommended [in the study] that organizations set expectations that leaders who mentor other potential leaders be rewarded in the same way as those who hit financial targets or readmission rate targets,” Dr. Lemak says.
Leadership matters, agrees Deborah J. Bowen, FACHE, CAE, president and CEO of Chicago-based American College of Healthcare Executives.
“I think we’re getting a little smarter. Organizational leaders and trustees have a better understanding that talent development is one of the most important jobs,” she says. “If you don’t have the right people in the right places making good decisions on behalf of the patients and the populations in the communities they’re serving, the rest falls apart.”
Nuances of Mentoring
Many conversations about encouraging diversity in healthcare leadership converge around the role of effective mentoring and sponsorship. A substantial body of research supports the impact of mentoring on retention, research productivity, career satisfaction, and career development for women. It’s important to ensure that the institutional culture is geared toward mentoring junior faculty, says Jessie Kimbrough Marshall, MD, MPH, assistant professor in the Division of General Medicine Hospitalist Program at the University of Michigan Health System in Ann Arbor (UMHS).
Several of our sources pointed out that leaders must learn how to be effective mentors. More attention is being given to enhancing leaders’ mentorship skills. One example is at the Institute for Diversity in Health Management, which conducts an intensive 12-month certificate in diversity management program for practitioners. León says the program fosters ongoing networking and support through the American Leadership Council on Diversity in Healthcare by building leadership competencies.
Dr. Valantine points out that mentoring is hardly a one-style-fits-all proposition but that it is a crucial element to creating and retaining diversity. She says it should be viewed “much more broadly than it is today, and it should focus beyond the trainer-trainee relationship.”
The process is a two-way street. Denege Ward, MD, hospitalist, assistant professor of internal medicine, and director of the medical short stay unit at UMHS, says minorities need to be ready to take a leap of faith.
“Underrepresented faculty and staff should take the risk of possible failure in challenging situations but learn from it and do better and not succumb to fear in face of challenges,” Dr. Ward says.
Although mentoring is one important component in building diversity in academic medicine, Dr. Sánchez asserts that role models, champions, and sponsors are equally important.
“In addition and separate from role models, there must be in place policies and procedures that promote a climate for diverse individuals to succeed,” he says. “What’s needed is an institutional vision and strategic plan that recognizes the importance of diversity. [It] has to become a core principle.”
Dr. Marshall echoes that refrain, noting the recruitment and retention of a diverse set of leaders will take time and intentionality. She is actively engaged in organizing annual meeting mentoring panels at the Society of General Internal Medicine.
“There are still quite a few barriers for women and minorities to advance into hospital leadership roles,” she says. “We still have a long way to go. However, I’m seeing more women and people of color get into these positions. The numbers are increasing, and that encourages me.” TH
Gretchen Henkel is a freelance writer in California.
References
- Institute for Diversity in Health Management. The state of health care diversity and disparities: a benchmarking study of U.S. hospitals. Available at: http://www.diversityconnection.org/diversityconnection/leadership-conferences/Benchmarking-Survey.jsp?fll=S11.
- Top issues confronting hospitals in 2015. American College of Healthcare Executives website. Available at: https://www.ache.org/pubs/research/ceoissues.cfm. Accessed March 5, 2016.
- Association of American Medical Colleges. Diversity in the physician workforce: facts & figures 2014. Available at: http://aamcdiversityfactsandfigures.org/.
- Valantine HA, Grewal D, Ku MC, et al. The gender gap in academic medicine: comparing results from a multifaceted intervention for Stanford faculty to peer and national cohorts. Acad Med. 2014;89(6):904-911.
- Valantine H, Sandborg CI. Changing the culture of academic medicine to eliminate the gender leadership gap: 50/50 by 2020. Acad Med. 2013;88(10):1411-1413.
- Sexton DW, Lemak CH, Wainio JA. Career inflection points of women who successfully achieved the hospital CEO position. J Healthc Manag. 2014;59(5):367-383.
Throughout its history, the United States has been a nation of immigrants. From the early colonial settlements to the mid-20th century, most immigrants came from Western European countries. Since 1965, when the Immigration and Nationality Act abolished national-origin quotas, the diversity of immigrants has increased. “By the year 2043,” says Tomás León, president and CEO of the Institute for Diversity in Health Management in Chicago, “we will be a country where the majority of our population is comprised of racial and ethnic minorities.”
Those changing demographics, cited from the U.S. Census Bureau’s projections, already are evidenced in hospital patient populations. According to a benchmarking survey sponsored by the institute, which is an affiliate of the American Hospital Association, the percentage of minority patients seen in hospitals grew from 29% to 31% of patient census between 2011 and 2013.1 And yet, the survey found this increasing diversity is not currently reflected in leadership positions. During the same time period, underrepresented racial and ethnic minorities (UREM) on hospital boards of directors (14%) and in C-suite positions (14%) remained flat (see Figure 1).
Gender disparities in healthcare and academic leadership also have been slow to change. Periodic surveys conducted by the American College of Healthcare Executives indicate that women comprise only 11% of healthcare CEOs in the U.S.2 And despite the fact that women make up half of all medical students (and one-third of full-time faculty), the Association of American Medical Colleges (AAMC) finds that women still trail men when it comes to attaining full professorship and decanal positions at their academic institutions.3
The Hospitalist interviewed medical directors, researchers, diversity management professionals, and hospitalists to ascertain current solutions being pursued to narrow the gaps in leadership diversity.
Why Diversity in Leadership Matters
Eric E. Howell, MD, MHM, chief of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in the Hopkins School of Medicine in Baltimore, believes there is a need to encourage the advancement to leadership positions for female and UREM physicians.
“In medicine, it’s really about service. If we are really here for our patients, we need representation of diversity in our faculty and leadership,” says Dr. Howell, a past SHM president and faculty member of SHM’s Leadership Academy since its inception in 2005. In addition, he says, “Diversity adds incredible strength to an organization and adds to the richness of the ideas and solutions to overcome challenging problems.”
With the implementation of the Affordable Care Act, formerly uninsured people are now accessing the healthcare system; many are bilingual and bicultural, notes George A. Zeppenfeldt-Cestero, president and CEO, Association of Hispanic Healthcare Executives.
“You want to make sure that providers, whether they are physicians, nurses, dentists, or health executives that drive policy issues, are also reflective of that population throughout the organization,” he says. “The real definition of diversity is making sure you have diversity in all layers of the workforce, including the C-suite.”
León points to the coming “seismic demographic shifts” and wonders if healthcare is ready to become more reflective of the communities it serves.
“Increasing diversity in healthcare leadership and governance is essential for the delivery and provision of culturally competent care,” León says. “Now, more than ever, it’s important that we collectively accelerate progress in this area.”
Advancing in Academic and Hospital Medicine
Might hospital medicine offer additional opportunities for women and minorities to advance into leadership positions? Hospitalist Flora Kisuule, MD, SFHM, assistant professor of medicine at Johns Hopkins School of Medicine and associate division director of the Collaborative Inpatient Medicine Service (CIMS) at Johns Hopkins Bayview Medical Center, believes this may be the case. She was with Dr. Howell’s group when he needed to fill the associate director position.
“My advancement speaks to hospital medicine and the fact that we are growing as a field,” she says. “Because of that, opportunities are presenting themselves.”
Dr. Kisuule’s ability to thrive in her position speaks to her professionalism but also to a number of other intentional factors: Dr. Howell’s continuing sponsorship to include her in leadership opportunities, an emergency call system for parents with sick children, and a women’s task force whose agenda calls for transparency in hiring and advancement.
Intentional Structure Change
Cardiologist Hannah A. Valantine, MD, recognizes the importance of addressing the lack of women and people from unrepresented groups in the Science, Technology, Engineering, and Mathematics (STEM) workforce. While at Stanford University School of Medicine, she developed and put into place a set of strategies to understand and mitigate the drivers of gender imbalance. Since then, Dr. Valantine was recruited to bring her expertise to the National Institutes of Health in Bethesda, Md., where she is the inaugural chief officer for scientific workforce diversity. In this role, she is committed “to promoting biomedical workforce diversity as an opportunity, not a problem.”
Dr. Valantine is pushing NIH to pursue a wide range of evidence-based programming to eliminate career-transition barriers that keep women and individuals from underrepresented groups from attaining spots in the top echelons of science and health leadership. She believes that applying scientific rigor to the issue of workforce diversity can lead to quantifiable, translatable, and repeatable methods for recruitment and retention of talent in the biomedical workforce (see “Building Blocks").
Before joining NIH, Dr. Valantine and her colleagues at Stanford surveyed gender composition and faculty satisfaction several years after initiating a multifaceted intervention to boost recruitment and development of women faculty.4 After making a visible commitment of resources to support faculty, with special attention to women, Stanford rose from below to above national benchmarks in the representation of women among faculty. Yet significant work remains to be done, Dr. Valantine says. Her work predicts that the estimated time to achieve 50% occupancy of full professorships by women nationally approaches 50 years—“far too long using current approaches.”
In a separate review article, Dr. Valantine and co-author Christy Sandborg, MD, described the Stanford University School of Medicine Academic Biomedical Career Customization (ABCC) model, which was adapted from Deloitte’s Mass Career Customization framework and allows for development of individual career plans that span a faculty member’s total career, not just a year or two at a time. Long-term planning can enable better alignment between the work culture and values of the workforce, which will improve the outlook for women faculty, Dr. Valantine says.
The issues of work-life balance may actually be generational, Dr. Valantine explains. Veteran hospitalist Janet Nagamine, MD, BSN, SFHM, of Santa Clara, Calif., agrees.
“Nowadays, men as well as women are looking for work-life balance,” she says.
In hospital medicine, Dr. Nagamine points out, the structural changes required to effect a work-life balance for hospital leaders are often difficult to achieve.
“As productivity surveys show, HM group leaders are putting in as many RVUs as the staff,” the former SHM board member says. “There is no dedicated time for administrative duties.”
Construct a Pipeline
Barriers to advancement often are particular to characteristics of diverse populations. For example, the AAMC’s report on the U.S. physician workforce documents that in African-American physicians 40 and younger, women outnumber their male counterparts. Therefore, in the association’s Diversity in Medical Education: Facts and Figures 2012 report, the executive summary points out the need to strengthen the medical education pipeline to increase the number of African-American males who enter the premed track.
Despite the fast-growing percentage of Latino and Hispanic populations in the United States, the shortage of Latino/Hispanic physicians increased from 1980 to 2010. Latinos/Hispanics are greatly underrepresented in the medical student, resident, and faculty populations, according to John Paul Sánchez, MD, MPH, assistant dean for diversity and inclusion in the Office for Diversity and Community Engagement at Rutgers, The State University of New Jersey. Likewise, Zeppenfeldt-Cestero believes that efforts must begin much earlier with Latino and other minority and underrepresented students.
“We have to make sure our students pursue the STEM disciplines and that they also later have the education and preparation to be competitive at the MBA or MPH levels,” he says.
Dr. Sánchez, an associate professor of emergency medicine and a diversity activist since his med school days, is the recipient of last year’s Association of Hispanic Healthcare Executives’ academic leader of the year award. Since September 2014, he has been involved with Building the Next Generation of Academic Physicians Inc., which collaborates with more than 40 medical schools across the country. The initiative offers conferences designed to develop diverse medical students’ and residents’ interest in pursuing academic medicine. Open to all medical students and residents, the conference curriculum is tailored for women, UREMs, and trainees who identify as lesbian, gay, bisexual, or transgender (LGBT), he says. Seven conferences were held in 2015, 10 are planned for this year, and seven for 2017.
Healthcare Leadership Gaps
Despite their omnipresence in healthcare, there is a dearth of women in chief executive and governance roles, as has been noted by both the American College of Healthcare Executives and the National Center for Healthcare Leadership. As with academic leadership positions, the leadership gap in the administrative sector does not seem to be due to a lack of women entering graduate programs in health administration. On the contrary, since the mid-1980s women have comprised 50% to 60% of graduate students.
“This is absolutely not a pipeline issue,” says Christy Harris Lemak, PhD, FACHE, professor and chair of the Department of Health Services Administration at the University of Alabama at Birmingham School of Health Professions and lead investigator of the National Center for Healthcare Leadership’s study of women in healthcare executive positions. Other factors come into play.
In the study, she and her co-authors queried female healthcare CEOs to ascertain the critical career inflection points that led to their success.6 Those who were strategic about their careers, sought out mentors, and voiced their intentions about pursuing leadership positions were more likely to be successful in those efforts. However, individual career efforts must be coupled with overall organizational commitment to fostering inclusion (see “Path to the Top: Strategic Advice for Women").
Hospitals and healthcare organizations must pursue the development of human capital (and the diversity of their leaders) in a systematic way. “We recommended [in the study] that organizations set expectations that leaders who mentor other potential leaders be rewarded in the same way as those who hit financial targets or readmission rate targets,” Dr. Lemak says.
Leadership matters, agrees Deborah J. Bowen, FACHE, CAE, president and CEO of Chicago-based American College of Healthcare Executives.
“I think we’re getting a little smarter. Organizational leaders and trustees have a better understanding that talent development is one of the most important jobs,” she says. “If you don’t have the right people in the right places making good decisions on behalf of the patients and the populations in the communities they’re serving, the rest falls apart.”
Nuances of Mentoring
Many conversations about encouraging diversity in healthcare leadership converge around the role of effective mentoring and sponsorship. A substantial body of research supports the impact of mentoring on retention, research productivity, career satisfaction, and career development for women. It’s important to ensure that the institutional culture is geared toward mentoring junior faculty, says Jessie Kimbrough Marshall, MD, MPH, assistant professor in the Division of General Medicine Hospitalist Program at the University of Michigan Health System in Ann Arbor (UMHS).
Several of our sources pointed out that leaders must learn how to be effective mentors. More attention is being given to enhancing leaders’ mentorship skills. One example is at the Institute for Diversity in Health Management, which conducts an intensive 12-month certificate in diversity management program for practitioners. León says the program fosters ongoing networking and support through the American Leadership Council on Diversity in Healthcare by building leadership competencies.
Dr. Valantine points out that mentoring is hardly a one-style-fits-all proposition but that it is a crucial element to creating and retaining diversity. She says it should be viewed “much more broadly than it is today, and it should focus beyond the trainer-trainee relationship.”
The process is a two-way street. Denege Ward, MD, hospitalist, assistant professor of internal medicine, and director of the medical short stay unit at UMHS, says minorities need to be ready to take a leap of faith.
“Underrepresented faculty and staff should take the risk of possible failure in challenging situations but learn from it and do better and not succumb to fear in face of challenges,” Dr. Ward says.
Although mentoring is one important component in building diversity in academic medicine, Dr. Sánchez asserts that role models, champions, and sponsors are equally important.
“In addition and separate from role models, there must be in place policies and procedures that promote a climate for diverse individuals to succeed,” he says. “What’s needed is an institutional vision and strategic plan that recognizes the importance of diversity. [It] has to become a core principle.”
Dr. Marshall echoes that refrain, noting the recruitment and retention of a diverse set of leaders will take time and intentionality. She is actively engaged in organizing annual meeting mentoring panels at the Society of General Internal Medicine.
“There are still quite a few barriers for women and minorities to advance into hospital leadership roles,” she says. “We still have a long way to go. However, I’m seeing more women and people of color get into these positions. The numbers are increasing, and that encourages me.” TH
Gretchen Henkel is a freelance writer in California.
References
- Institute for Diversity in Health Management. The state of health care diversity and disparities: a benchmarking study of U.S. hospitals. Available at: http://www.diversityconnection.org/diversityconnection/leadership-conferences/Benchmarking-Survey.jsp?fll=S11.
- Top issues confronting hospitals in 2015. American College of Healthcare Executives website. Available at: https://www.ache.org/pubs/research/ceoissues.cfm. Accessed March 5, 2016.
- Association of American Medical Colleges. Diversity in the physician workforce: facts & figures 2014. Available at: http://aamcdiversityfactsandfigures.org/.
- Valantine HA, Grewal D, Ku MC, et al. The gender gap in academic medicine: comparing results from a multifaceted intervention for Stanford faculty to peer and national cohorts. Acad Med. 2014;89(6):904-911.
- Valantine H, Sandborg CI. Changing the culture of academic medicine to eliminate the gender leadership gap: 50/50 by 2020. Acad Med. 2013;88(10):1411-1413.
- Sexton DW, Lemak CH, Wainio JA. Career inflection points of women who successfully achieved the hospital CEO position. J Healthc Manag. 2014;59(5):367-383.
Throughout its history, the United States has been a nation of immigrants. From the early colonial settlements to the mid-20th century, most immigrants came from Western European countries. Since 1965, when the Immigration and Nationality Act abolished national-origin quotas, the diversity of immigrants has increased. “By the year 2043,” says Tomás León, president and CEO of the Institute for Diversity in Health Management in Chicago, “we will be a country where the majority of our population is comprised of racial and ethnic minorities.”
Those changing demographics, cited from the U.S. Census Bureau’s projections, already are evidenced in hospital patient populations. According to a benchmarking survey sponsored by the institute, which is an affiliate of the American Hospital Association, the percentage of minority patients seen in hospitals grew from 29% to 31% of patient census between 2011 and 2013.1 And yet, the survey found this increasing diversity is not currently reflected in leadership positions. During the same time period, underrepresented racial and ethnic minorities (UREM) on hospital boards of directors (14%) and in C-suite positions (14%) remained flat (see Figure 1).
Gender disparities in healthcare and academic leadership also have been slow to change. Periodic surveys conducted by the American College of Healthcare Executives indicate that women comprise only 11% of healthcare CEOs in the U.S.2 And despite the fact that women make up half of all medical students (and one-third of full-time faculty), the Association of American Medical Colleges (AAMC) finds that women still trail men when it comes to attaining full professorship and decanal positions at their academic institutions.3
The Hospitalist interviewed medical directors, researchers, diversity management professionals, and hospitalists to ascertain current solutions being pursued to narrow the gaps in leadership diversity.
Why Diversity in Leadership Matters
Eric E. Howell, MD, MHM, chief of the Division of Hospital Medicine at Johns Hopkins Bayview Medical Center in the Hopkins School of Medicine in Baltimore, believes there is a need to encourage the advancement to leadership positions for female and UREM physicians.
“In medicine, it’s really about service. If we are really here for our patients, we need representation of diversity in our faculty and leadership,” says Dr. Howell, a past SHM president and faculty member of SHM’s Leadership Academy since its inception in 2005. In addition, he says, “Diversity adds incredible strength to an organization and adds to the richness of the ideas and solutions to overcome challenging problems.”
With the implementation of the Affordable Care Act, formerly uninsured people are now accessing the healthcare system; many are bilingual and bicultural, notes George A. Zeppenfeldt-Cestero, president and CEO, Association of Hispanic Healthcare Executives.
“You want to make sure that providers, whether they are physicians, nurses, dentists, or health executives that drive policy issues, are also reflective of that population throughout the organization,” he says. “The real definition of diversity is making sure you have diversity in all layers of the workforce, including the C-suite.”
León points to the coming “seismic demographic shifts” and wonders if healthcare is ready to become more reflective of the communities it serves.
“Increasing diversity in healthcare leadership and governance is essential for the delivery and provision of culturally competent care,” León says. “Now, more than ever, it’s important that we collectively accelerate progress in this area.”
Advancing in Academic and Hospital Medicine
Might hospital medicine offer additional opportunities for women and minorities to advance into leadership positions? Hospitalist Flora Kisuule, MD, SFHM, assistant professor of medicine at Johns Hopkins School of Medicine and associate division director of the Collaborative Inpatient Medicine Service (CIMS) at Johns Hopkins Bayview Medical Center, believes this may be the case. She was with Dr. Howell’s group when he needed to fill the associate director position.
“My advancement speaks to hospital medicine and the fact that we are growing as a field,” she says. “Because of that, opportunities are presenting themselves.”
Dr. Kisuule’s ability to thrive in her position speaks to her professionalism but also to a number of other intentional factors: Dr. Howell’s continuing sponsorship to include her in leadership opportunities, an emergency call system for parents with sick children, and a women’s task force whose agenda calls for transparency in hiring and advancement.
Intentional Structure Change
Cardiologist Hannah A. Valantine, MD, recognizes the importance of addressing the lack of women and people from unrepresented groups in the Science, Technology, Engineering, and Mathematics (STEM) workforce. While at Stanford University School of Medicine, she developed and put into place a set of strategies to understand and mitigate the drivers of gender imbalance. Since then, Dr. Valantine was recruited to bring her expertise to the National Institutes of Health in Bethesda, Md., where she is the inaugural chief officer for scientific workforce diversity. In this role, she is committed “to promoting biomedical workforce diversity as an opportunity, not a problem.”
Dr. Valantine is pushing NIH to pursue a wide range of evidence-based programming to eliminate career-transition barriers that keep women and individuals from underrepresented groups from attaining spots in the top echelons of science and health leadership. She believes that applying scientific rigor to the issue of workforce diversity can lead to quantifiable, translatable, and repeatable methods for recruitment and retention of talent in the biomedical workforce (see “Building Blocks").
Before joining NIH, Dr. Valantine and her colleagues at Stanford surveyed gender composition and faculty satisfaction several years after initiating a multifaceted intervention to boost recruitment and development of women faculty.4 After making a visible commitment of resources to support faculty, with special attention to women, Stanford rose from below to above national benchmarks in the representation of women among faculty. Yet significant work remains to be done, Dr. Valantine says. Her work predicts that the estimated time to achieve 50% occupancy of full professorships by women nationally approaches 50 years—“far too long using current approaches.”
In a separate review article, Dr. Valantine and co-author Christy Sandborg, MD, described the Stanford University School of Medicine Academic Biomedical Career Customization (ABCC) model, which was adapted from Deloitte’s Mass Career Customization framework and allows for development of individual career plans that span a faculty member’s total career, not just a year or two at a time. Long-term planning can enable better alignment between the work culture and values of the workforce, which will improve the outlook for women faculty, Dr. Valantine says.
The issues of work-life balance may actually be generational, Dr. Valantine explains. Veteran hospitalist Janet Nagamine, MD, BSN, SFHM, of Santa Clara, Calif., agrees.
“Nowadays, men as well as women are looking for work-life balance,” she says.
In hospital medicine, Dr. Nagamine points out, the structural changes required to effect a work-life balance for hospital leaders are often difficult to achieve.
“As productivity surveys show, HM group leaders are putting in as many RVUs as the staff,” the former SHM board member says. “There is no dedicated time for administrative duties.”
Construct a Pipeline
Barriers to advancement often are particular to characteristics of diverse populations. For example, the AAMC’s report on the U.S. physician workforce documents that in African-American physicians 40 and younger, women outnumber their male counterparts. Therefore, in the association’s Diversity in Medical Education: Facts and Figures 2012 report, the executive summary points out the need to strengthen the medical education pipeline to increase the number of African-American males who enter the premed track.
Despite the fast-growing percentage of Latino and Hispanic populations in the United States, the shortage of Latino/Hispanic physicians increased from 1980 to 2010. Latinos/Hispanics are greatly underrepresented in the medical student, resident, and faculty populations, according to John Paul Sánchez, MD, MPH, assistant dean for diversity and inclusion in the Office for Diversity and Community Engagement at Rutgers, The State University of New Jersey. Likewise, Zeppenfeldt-Cestero believes that efforts must begin much earlier with Latino and other minority and underrepresented students.
“We have to make sure our students pursue the STEM disciplines and that they also later have the education and preparation to be competitive at the MBA or MPH levels,” he says.
Dr. Sánchez, an associate professor of emergency medicine and a diversity activist since his med school days, is the recipient of last year’s Association of Hispanic Healthcare Executives’ academic leader of the year award. Since September 2014, he has been involved with Building the Next Generation of Academic Physicians Inc., which collaborates with more than 40 medical schools across the country. The initiative offers conferences designed to develop diverse medical students’ and residents’ interest in pursuing academic medicine. Open to all medical students and residents, the conference curriculum is tailored for women, UREMs, and trainees who identify as lesbian, gay, bisexual, or transgender (LGBT), he says. Seven conferences were held in 2015, 10 are planned for this year, and seven for 2017.
Healthcare Leadership Gaps
Despite their omnipresence in healthcare, there is a dearth of women in chief executive and governance roles, as has been noted by both the American College of Healthcare Executives and the National Center for Healthcare Leadership. As with academic leadership positions, the leadership gap in the administrative sector does not seem to be due to a lack of women entering graduate programs in health administration. On the contrary, since the mid-1980s women have comprised 50% to 60% of graduate students.
“This is absolutely not a pipeline issue,” says Christy Harris Lemak, PhD, FACHE, professor and chair of the Department of Health Services Administration at the University of Alabama at Birmingham School of Health Professions and lead investigator of the National Center for Healthcare Leadership’s study of women in healthcare executive positions. Other factors come into play.
In the study, she and her co-authors queried female healthcare CEOs to ascertain the critical career inflection points that led to their success.6 Those who were strategic about their careers, sought out mentors, and voiced their intentions about pursuing leadership positions were more likely to be successful in those efforts. However, individual career efforts must be coupled with overall organizational commitment to fostering inclusion (see “Path to the Top: Strategic Advice for Women").
Hospitals and healthcare organizations must pursue the development of human capital (and the diversity of their leaders) in a systematic way. “We recommended [in the study] that organizations set expectations that leaders who mentor other potential leaders be rewarded in the same way as those who hit financial targets or readmission rate targets,” Dr. Lemak says.
Leadership matters, agrees Deborah J. Bowen, FACHE, CAE, president and CEO of Chicago-based American College of Healthcare Executives.
“I think we’re getting a little smarter. Organizational leaders and trustees have a better understanding that talent development is one of the most important jobs,” she says. “If you don’t have the right people in the right places making good decisions on behalf of the patients and the populations in the communities they’re serving, the rest falls apart.”
Nuances of Mentoring
Many conversations about encouraging diversity in healthcare leadership converge around the role of effective mentoring and sponsorship. A substantial body of research supports the impact of mentoring on retention, research productivity, career satisfaction, and career development for women. It’s important to ensure that the institutional culture is geared toward mentoring junior faculty, says Jessie Kimbrough Marshall, MD, MPH, assistant professor in the Division of General Medicine Hospitalist Program at the University of Michigan Health System in Ann Arbor (UMHS).
Several of our sources pointed out that leaders must learn how to be effective mentors. More attention is being given to enhancing leaders’ mentorship skills. One example is at the Institute for Diversity in Health Management, which conducts an intensive 12-month certificate in diversity management program for practitioners. León says the program fosters ongoing networking and support through the American Leadership Council on Diversity in Healthcare by building leadership competencies.
Dr. Valantine points out that mentoring is hardly a one-style-fits-all proposition but that it is a crucial element to creating and retaining diversity. She says it should be viewed “much more broadly than it is today, and it should focus beyond the trainer-trainee relationship.”
The process is a two-way street. Denege Ward, MD, hospitalist, assistant professor of internal medicine, and director of the medical short stay unit at UMHS, says minorities need to be ready to take a leap of faith.
“Underrepresented faculty and staff should take the risk of possible failure in challenging situations but learn from it and do better and not succumb to fear in face of challenges,” Dr. Ward says.
Although mentoring is one important component in building diversity in academic medicine, Dr. Sánchez asserts that role models, champions, and sponsors are equally important.
“In addition and separate from role models, there must be in place policies and procedures that promote a climate for diverse individuals to succeed,” he says. “What’s needed is an institutional vision and strategic plan that recognizes the importance of diversity. [It] has to become a core principle.”
Dr. Marshall echoes that refrain, noting the recruitment and retention of a diverse set of leaders will take time and intentionality. She is actively engaged in organizing annual meeting mentoring panels at the Society of General Internal Medicine.
“There are still quite a few barriers for women and minorities to advance into hospital leadership roles,” she says. “We still have a long way to go. However, I’m seeing more women and people of color get into these positions. The numbers are increasing, and that encourages me.” TH
Gretchen Henkel is a freelance writer in California.
References
- Institute for Diversity in Health Management. The state of health care diversity and disparities: a benchmarking study of U.S. hospitals. Available at: http://www.diversityconnection.org/diversityconnection/leadership-conferences/Benchmarking-Survey.jsp?fll=S11.
- Top issues confronting hospitals in 2015. American College of Healthcare Executives website. Available at: https://www.ache.org/pubs/research/ceoissues.cfm. Accessed March 5, 2016.
- Association of American Medical Colleges. Diversity in the physician workforce: facts & figures 2014. Available at: http://aamcdiversityfactsandfigures.org/.
- Valantine HA, Grewal D, Ku MC, et al. The gender gap in academic medicine: comparing results from a multifaceted intervention for Stanford faculty to peer and national cohorts. Acad Med. 2014;89(6):904-911.
- Valantine H, Sandborg CI. Changing the culture of academic medicine to eliminate the gender leadership gap: 50/50 by 2020. Acad Med. 2013;88(10):1411-1413.
- Sexton DW, Lemak CH, Wainio JA. Career inflection points of women who successfully achieved the hospital CEO position. J Healthc Manag. 2014;59(5):367-383.
Public Opinion about Healthcare Reform Becomes More Positive
Reference
1. Jacobs LR, Mettler S. Liking health reform but turned off by toxic politics [published online ahead of print April 2016]. Health Aff. doi:10.1377/hlthaff.2015.1313.
Reference
1. Jacobs LR, Mettler S. Liking health reform but turned off by toxic politics [published online ahead of print April 2016]. Health Aff. doi:10.1377/hlthaff.2015.1313.
Reference
1. Jacobs LR, Mettler S. Liking health reform but turned off by toxic politics [published online ahead of print April 2016]. Health Aff. doi:10.1377/hlthaff.2015.1313.
Tips for Improving Early Discharge Rates
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
New Community-Based Palliative Care Certification to Launch
The industry’s first certification for home health and hospices that provide top-caliber community-based palliative care services in the patient’s place of residence is being launched by The Joint Commission.
“As healthcare continues to evolve and the Affordable Care Act is beginning to impact the industry, one of the things that has come to light is that many patients over the years have experienced unnecessary hospitalization admissions when the management of their disease stage really required palliative care,” says Margherita Labson, RN, MSHSA, CPHQ, executive director of The Joint Commission’s Home Care Program. “For those of us in the home care environment in the community, we’ve always tried to manage this, but the current models of care didn’t really meet the needs of these patients because the Medicare benefit is an episodic payment program that’s built for rehab and restoration, not for maintenance.”
The Joint Commission’s new program, she says, provides value to patients, results in a lower rate of a necessary readmission, and contributes to patient satisfaction and improved outcomes of care.
Surveys for Community-Based Palliative Care (CBPC) Certification will begin on July 1. Certification is awarded for a three-year period, and the certification’s framework helps providers design, deliver, and validate patient-centered care and services. Key CBPC certification requirements include:
- A robust interdisciplinary care team
- Customized, comprehensive care plans
- After-hours care and services
- Use of evidence-based clinical practice guidelines
- A defined hand-off communications process
“This helps to address perhaps one of the key frustrations of hospitalists: the repeated readmissions of patients struggling with serious chronic illnesses,” Labson says. “It helps reduce the number of inappropriate hospital admissions and allows the hospitalist to focus on the admission and successful management of those patients that are appropriate for hospital intervention or acute-care intervention at that point.”
The industry’s first certification for home health and hospices that provide top-caliber community-based palliative care services in the patient’s place of residence is being launched by The Joint Commission.
“As healthcare continues to evolve and the Affordable Care Act is beginning to impact the industry, one of the things that has come to light is that many patients over the years have experienced unnecessary hospitalization admissions when the management of their disease stage really required palliative care,” says Margherita Labson, RN, MSHSA, CPHQ, executive director of The Joint Commission’s Home Care Program. “For those of us in the home care environment in the community, we’ve always tried to manage this, but the current models of care didn’t really meet the needs of these patients because the Medicare benefit is an episodic payment program that’s built for rehab and restoration, not for maintenance.”
The Joint Commission’s new program, she says, provides value to patients, results in a lower rate of a necessary readmission, and contributes to patient satisfaction and improved outcomes of care.
Surveys for Community-Based Palliative Care (CBPC) Certification will begin on July 1. Certification is awarded for a three-year period, and the certification’s framework helps providers design, deliver, and validate patient-centered care and services. Key CBPC certification requirements include:
- A robust interdisciplinary care team
- Customized, comprehensive care plans
- After-hours care and services
- Use of evidence-based clinical practice guidelines
- A defined hand-off communications process
“This helps to address perhaps one of the key frustrations of hospitalists: the repeated readmissions of patients struggling with serious chronic illnesses,” Labson says. “It helps reduce the number of inappropriate hospital admissions and allows the hospitalist to focus on the admission and successful management of those patients that are appropriate for hospital intervention or acute-care intervention at that point.”
The industry’s first certification for home health and hospices that provide top-caliber community-based palliative care services in the patient’s place of residence is being launched by The Joint Commission.
“As healthcare continues to evolve and the Affordable Care Act is beginning to impact the industry, one of the things that has come to light is that many patients over the years have experienced unnecessary hospitalization admissions when the management of their disease stage really required palliative care,” says Margherita Labson, RN, MSHSA, CPHQ, executive director of The Joint Commission’s Home Care Program. “For those of us in the home care environment in the community, we’ve always tried to manage this, but the current models of care didn’t really meet the needs of these patients because the Medicare benefit is an episodic payment program that’s built for rehab and restoration, not for maintenance.”
The Joint Commission’s new program, she says, provides value to patients, results in a lower rate of a necessary readmission, and contributes to patient satisfaction and improved outcomes of care.
Surveys for Community-Based Palliative Care (CBPC) Certification will begin on July 1. Certification is awarded for a three-year period, and the certification’s framework helps providers design, deliver, and validate patient-centered care and services. Key CBPC certification requirements include:
- A robust interdisciplinary care team
- Customized, comprehensive care plans
- After-hours care and services
- Use of evidence-based clinical practice guidelines
- A defined hand-off communications process
“This helps to address perhaps one of the key frustrations of hospitalists: the repeated readmissions of patients struggling with serious chronic illnesses,” Labson says. “It helps reduce the number of inappropriate hospital admissions and allows the hospitalist to focus on the admission and successful management of those patients that are appropriate for hospital intervention or acute-care intervention at that point.”
Early Follow-up Can Reduce Readmission Rates
Heart failure patients who had early follow-up (within seven days of discharge) with general medicine or cardiology providers had a lower risk of being readmitted to the hospital within 30 days, according to a study from Kaiser Permanente published in the journal Medical Care.
“We found that follow-up within the first seven days post-discharge—mostly done through in-person clinic visits—was independently associated with a 19% lower chance of readmission, whereas initial follow-up after seven days was not significantly associated with readmission,” says lead researcher Keane K. Lee, MD, MS, a cardiologist and research scientist with Kaiser Permanente. “Perhaps as important, we also observed that telephone visits, mostly done by non-physician providers, within seven days after hospital discharge were associated with a non-statistically significant trend toward lower 30-day readmission rates, even after carefully accounting for potential differences between patients.
“This finding that telephone visits could reduce readmissions has never been reported and has potentially important implications. Contact by telephone with non-physicians may be more convenient for patients and family members and be more practical and cost-effective when implemented on a large scale.”
Dr. Lee suggests hospitalists have a role in creating a system to reliably arrange this follow-up.
“Hospitalists serve as a key part of the process to help patients transition successfully from the hospital back home,” Dr. Lee says.
Reference
- Lee KK, Yang J, Hernandez AF, Steimle AE, Go S. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365-372.
Heart failure patients who had early follow-up (within seven days of discharge) with general medicine or cardiology providers had a lower risk of being readmitted to the hospital within 30 days, according to a study from Kaiser Permanente published in the journal Medical Care.
“We found that follow-up within the first seven days post-discharge—mostly done through in-person clinic visits—was independently associated with a 19% lower chance of readmission, whereas initial follow-up after seven days was not significantly associated with readmission,” says lead researcher Keane K. Lee, MD, MS, a cardiologist and research scientist with Kaiser Permanente. “Perhaps as important, we also observed that telephone visits, mostly done by non-physician providers, within seven days after hospital discharge were associated with a non-statistically significant trend toward lower 30-day readmission rates, even after carefully accounting for potential differences between patients.
“This finding that telephone visits could reduce readmissions has never been reported and has potentially important implications. Contact by telephone with non-physicians may be more convenient for patients and family members and be more practical and cost-effective when implemented on a large scale.”
Dr. Lee suggests hospitalists have a role in creating a system to reliably arrange this follow-up.
“Hospitalists serve as a key part of the process to help patients transition successfully from the hospital back home,” Dr. Lee says.
Reference
- Lee KK, Yang J, Hernandez AF, Steimle AE, Go S. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365-372.
Heart failure patients who had early follow-up (within seven days of discharge) with general medicine or cardiology providers had a lower risk of being readmitted to the hospital within 30 days, according to a study from Kaiser Permanente published in the journal Medical Care.
“We found that follow-up within the first seven days post-discharge—mostly done through in-person clinic visits—was independently associated with a 19% lower chance of readmission, whereas initial follow-up after seven days was not significantly associated with readmission,” says lead researcher Keane K. Lee, MD, MS, a cardiologist and research scientist with Kaiser Permanente. “Perhaps as important, we also observed that telephone visits, mostly done by non-physician providers, within seven days after hospital discharge were associated with a non-statistically significant trend toward lower 30-day readmission rates, even after carefully accounting for potential differences between patients.
“This finding that telephone visits could reduce readmissions has never been reported and has potentially important implications. Contact by telephone with non-physicians may be more convenient for patients and family members and be more practical and cost-effective when implemented on a large scale.”
Dr. Lee suggests hospitalists have a role in creating a system to reliably arrange this follow-up.
“Hospitalists serve as a key part of the process to help patients transition successfully from the hospital back home,” Dr. Lee says.
Reference
- Lee KK, Yang J, Hernandez AF, Steimle AE, Go S. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365-372.
Barriers to Achieving High Reliability
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.
Is Email an Endangered Species?
And yet despite the seemingly definitive place email communication holds for hospitalists—for messages to one another, missives to hospital administrators, instructions to patients, and myriad other uses—there are those who often wonder if email is outmoded. In a world bent on text messaging, Facebook, Twitter, Skype, Vine, Periscope, and Google Talk (not to mention dozens of lesser-known services and a seemingly endless string of startups aiming to be the proverbial next big thing), is email old-fashioned or ineffective?
In a word, no.
But that doesn’t mean email is the only communication method in a hospitalist’s toolbox or the best one for every situation. Physicians and communication experts interviewed by The Hospitalist agree that email has a function and isn’t going anywhere anytime soon. However, that function is dependent on trust, urgency, formality, and relationships.
“It has a place in communication, especially for busy hospitals, but the key is to figure out what is that place,” says Vineet Arora, MD, MAPP, FHM, a hospitalist at the University of Chicago, who has spoken at SHM annual meetings on how hospitalists communicate. “All of the information that is coming to you is in a push-pull model … There is information that you want pushed to you because it’s important and you want to see it. And then there is information that you want to pull because perhaps you know it relates to a patient in front of you … Where does email fit into it?”
Communications consultant A.J. Moore, associate professor of communication at Rider University in Lawrenceville, N.J., put it even more bluntly when assuring that email isn’t going anywhere.
“Research shows, and I know I do it myself, the first thing I do in the morning when I pick up my phone is check my email,” he says. “People often check their email before they check the weather, before they check social media.
“Sure, there are other places to go, there’s other ways of communicating. But I still think that email is the center point. It’s the starting line for your communication.”
A Modus for the Medium
Hospitalist Aaron Jacobs, MD, associate chief medical information officer at University of New Mexico Hospital in Albuquerque, appreciates the academic discussion over the future of email, but he also knows he uses it every day. To him, there are several factors that go into choosing which medium he uses for a particular message.
“It depends on the situation and the message you are sending,” says Dr. Jacobs, associate professor in the Department of Pediatrics at the University of New Mexico School of Medicine. “If I’m friends with the pediatric nephrologist, I may text him a quick question about a [glomerular filtration rate] or a clinical question. But if I’m not on those terms with another subspecialist, I wouldn’t do that.
“There’s definitely a relationship aspect that is relevant.”
Another factor in choosing to send an email versus a text message versus a tweet is timing. In the days when email was the only alternative to in-person communication or a phone call, the electronic message was the fastest way to reach a person. It was the best way to hold a synchronous conversation. But in today’s era of smartphones, tablets, and even wristwatches that have instant access, email is no longer the fastest option. In fact, email today is best tailored to asynchronous conversations, Dr. Arora says.
“Texting is really more invasive. It’s more demanding of the recipient’s time in an immediate sort of way,” Dr. Jacobs says. “With email, you’re basically saying, ‘Please take a look at this at your convenience, and when you can, write me back.’ In contrast, when people send text messages, they’re typically expecting a response in minutes. This may seem logical and trivial, but it can also be disruptive. Since some texts are urgent, all texts must at least initially be treated as such.”
The urgency that comes with a text message or a direct message on Facebook or Twitter is the flip side of the formality that comes with an email, says Moore.
“Email has more of a professional connotation to it than a Facebook message,” Moore says. “Even if I work with somebody, even if I’m Facebook friends with somebody and that person is one door away from me, if it is a work conversation, I am going to send them an email.”
Formality is the delineation between social media and what Moore half-jokingly calls “professional media.” And while in some ways technology gaps can often be a generational difference, Moore doesn’t see email usage through that prism and certainly not when he’s interacting with the young adults in his classes.
“I look at myself as a professor, and I have that formal relationship with younger people being students. They could find me on social media. There’s nothing preventing them,” he says. “But still they reach out to me via email, and I communicate with them via email.”
That being said, a generational gap does exist that can cause older physicians to refrain from embracing newer technologies that could be effective alternatives to email, says Howard Landa, chief medical information officer of the Alameda Health System in Oakland, Calif., and vice chairman of the board of advisors for the Association of Medical Directors of Information Systems. Many communication tools (Shortmail, Fridge, Apple Mail) either were discontinued, wrapped into larger technologies, or never became mainstream enough to be worthwhile. So the idea that some technologies won’t catch on discourages some from using anything but email.
“The younger we are, the easier the changes are and the more receptive we are to change,” Landa says. “We have seen a lot of flash-in-the-pan technology, snake oil, new ideas that go crazy for [a while]. They get to the top in the hype cycle, they drop to the bottom of the pit in the depression, and then they never move.
“With the older physicians, I think there is a reluctance to try something just because it’s new, whereas with the younger docs, there is every week a new technology that I want to try because I am willing to go through 20 of them before I find one that works. They have more energy and are more open to it.”
Security Is Job One
The safety of email is a major reason that many continually question its fate. In a broad sense, that is the natural question when a technology is new, says Ben Compaine, director of the fellows program at the Columbia University Institute for Tele-Information and a lecturer in the D’Amore-McKim School of Business at Northeastern University in Boston.
“There are always people who will find something to fear,” Compaine says. “Like when ATMs came along, there was stuff being written about safety concerns: ‘People will go to an ATM, and someone just holds them up and gets their money.’ It’s happened, but given the hundreds of millions of transactions that go on, you don’t throw out the baby with the bathwater.”
Dr. Arora cautions that the difference for hospitalists is that when a safety mistake is made with email, it can constitute a violation of the Health Insurance Portability and Accountability Act (HIPAA). And while those mistakes can happen innocently enough on social media or via text messaging, she says email issues are the most common.
“I’ve seen HIPAA violations where a patient would send an email to a doctor and the doctor would reply all to all of the [hospitalists] in their group saying, ‘Can anyone help me answer this question?’” she says. “So the forward email and forward and reply all are the most dangerous features because you have to know what you are forwarding and would that person want it shared with everybody.”
Landa believes that part of the problem with the efficacy of email is that it’s become so fast and so easy that people don’t take their time thinking about the impact of each email. Dr. Arora agrees and suggests hospitalists think carefully about what is in an email, particularly when it involves patient information.
“Share the minimum necessary information with a minimum number of people to try to accomplish what you are trying to do,” she adds. “That way, you are not clogging the inbox of everybody involved.”
Another potential pitfall to the efficacy of email is the “lost in translation” phenomenon, Landa says.
“How many times have you written am email and someone misinterpreted sarcasm or a joke or a particular word or a phrase and got upset because of what they thought you were saying?” he says. “I think that when you talk about the synchronous and rapid-fire style of the forms of communication, I think you elevate the risk by an order of magnitude. That’s the reason we have developed all the emoticons and all the visual references that are out there—to make sure that people don’t misinterpret what we’re saying.”
What’s Old Is New
So if hospitalists and communications experts believe email retains a place in the way information is conveyed, why is the question of its impending death a continuing parlor game for some?
“Because there’s always something new,” Moore says. “Because Messenger on Facebook looks a little bit flashier than email. Because now we have Periscope. Now we have Twitter. Now we have different types of platforms that message within each other. They all look flashier.”
But, in essence, each is simply a somewhat more modernized version, more bells and whistles, Moore says. He likes to compare it to the U.S. Postal Service. As technology progressed and communication became more real-time in ways well beyond telephone conversations, many pundits forecasted the end of what is derisively called snail mail, itself an admission of the speed and efficacy of electronic mail.
“You could make the analogy between the death of email and the death of the U.S. mail,” Moore says. “Ten years ago, people were writing this article about the death of the U.S. mail. And it certainly changed. Yes, there are less letters and less traffic and less parcels that the post office sends. But it’s still there. It’s not going away; it’s just adapting in a certain way.
“If you want to pinpoint a time that there is ‘the death of email,’ I think the death of the U.S. mail comes before it.” TH
Richard Quinn is a freelance writer in New Jersey.
And yet despite the seemingly definitive place email communication holds for hospitalists—for messages to one another, missives to hospital administrators, instructions to patients, and myriad other uses—there are those who often wonder if email is outmoded. In a world bent on text messaging, Facebook, Twitter, Skype, Vine, Periscope, and Google Talk (not to mention dozens of lesser-known services and a seemingly endless string of startups aiming to be the proverbial next big thing), is email old-fashioned or ineffective?
In a word, no.
But that doesn’t mean email is the only communication method in a hospitalist’s toolbox or the best one for every situation. Physicians and communication experts interviewed by The Hospitalist agree that email has a function and isn’t going anywhere anytime soon. However, that function is dependent on trust, urgency, formality, and relationships.
“It has a place in communication, especially for busy hospitals, but the key is to figure out what is that place,” says Vineet Arora, MD, MAPP, FHM, a hospitalist at the University of Chicago, who has spoken at SHM annual meetings on how hospitalists communicate. “All of the information that is coming to you is in a push-pull model … There is information that you want pushed to you because it’s important and you want to see it. And then there is information that you want to pull because perhaps you know it relates to a patient in front of you … Where does email fit into it?”
Communications consultant A.J. Moore, associate professor of communication at Rider University in Lawrenceville, N.J., put it even more bluntly when assuring that email isn’t going anywhere.
“Research shows, and I know I do it myself, the first thing I do in the morning when I pick up my phone is check my email,” he says. “People often check their email before they check the weather, before they check social media.
“Sure, there are other places to go, there’s other ways of communicating. But I still think that email is the center point. It’s the starting line for your communication.”
A Modus for the Medium
Hospitalist Aaron Jacobs, MD, associate chief medical information officer at University of New Mexico Hospital in Albuquerque, appreciates the academic discussion over the future of email, but he also knows he uses it every day. To him, there are several factors that go into choosing which medium he uses for a particular message.
“It depends on the situation and the message you are sending,” says Dr. Jacobs, associate professor in the Department of Pediatrics at the University of New Mexico School of Medicine. “If I’m friends with the pediatric nephrologist, I may text him a quick question about a [glomerular filtration rate] or a clinical question. But if I’m not on those terms with another subspecialist, I wouldn’t do that.
“There’s definitely a relationship aspect that is relevant.”
Another factor in choosing to send an email versus a text message versus a tweet is timing. In the days when email was the only alternative to in-person communication or a phone call, the electronic message was the fastest way to reach a person. It was the best way to hold a synchronous conversation. But in today’s era of smartphones, tablets, and even wristwatches that have instant access, email is no longer the fastest option. In fact, email today is best tailored to asynchronous conversations, Dr. Arora says.
“Texting is really more invasive. It’s more demanding of the recipient’s time in an immediate sort of way,” Dr. Jacobs says. “With email, you’re basically saying, ‘Please take a look at this at your convenience, and when you can, write me back.’ In contrast, when people send text messages, they’re typically expecting a response in minutes. This may seem logical and trivial, but it can also be disruptive. Since some texts are urgent, all texts must at least initially be treated as such.”
The urgency that comes with a text message or a direct message on Facebook or Twitter is the flip side of the formality that comes with an email, says Moore.
“Email has more of a professional connotation to it than a Facebook message,” Moore says. “Even if I work with somebody, even if I’m Facebook friends with somebody and that person is one door away from me, if it is a work conversation, I am going to send them an email.”
Formality is the delineation between social media and what Moore half-jokingly calls “professional media.” And while in some ways technology gaps can often be a generational difference, Moore doesn’t see email usage through that prism and certainly not when he’s interacting with the young adults in his classes.
“I look at myself as a professor, and I have that formal relationship with younger people being students. They could find me on social media. There’s nothing preventing them,” he says. “But still they reach out to me via email, and I communicate with them via email.”
That being said, a generational gap does exist that can cause older physicians to refrain from embracing newer technologies that could be effective alternatives to email, says Howard Landa, chief medical information officer of the Alameda Health System in Oakland, Calif., and vice chairman of the board of advisors for the Association of Medical Directors of Information Systems. Many communication tools (Shortmail, Fridge, Apple Mail) either were discontinued, wrapped into larger technologies, or never became mainstream enough to be worthwhile. So the idea that some technologies won’t catch on discourages some from using anything but email.
“The younger we are, the easier the changes are and the more receptive we are to change,” Landa says. “We have seen a lot of flash-in-the-pan technology, snake oil, new ideas that go crazy for [a while]. They get to the top in the hype cycle, they drop to the bottom of the pit in the depression, and then they never move.
“With the older physicians, I think there is a reluctance to try something just because it’s new, whereas with the younger docs, there is every week a new technology that I want to try because I am willing to go through 20 of them before I find one that works. They have more energy and are more open to it.”
Security Is Job One
The safety of email is a major reason that many continually question its fate. In a broad sense, that is the natural question when a technology is new, says Ben Compaine, director of the fellows program at the Columbia University Institute for Tele-Information and a lecturer in the D’Amore-McKim School of Business at Northeastern University in Boston.
“There are always people who will find something to fear,” Compaine says. “Like when ATMs came along, there was stuff being written about safety concerns: ‘People will go to an ATM, and someone just holds them up and gets their money.’ It’s happened, but given the hundreds of millions of transactions that go on, you don’t throw out the baby with the bathwater.”
Dr. Arora cautions that the difference for hospitalists is that when a safety mistake is made with email, it can constitute a violation of the Health Insurance Portability and Accountability Act (HIPAA). And while those mistakes can happen innocently enough on social media or via text messaging, she says email issues are the most common.
“I’ve seen HIPAA violations where a patient would send an email to a doctor and the doctor would reply all to all of the [hospitalists] in their group saying, ‘Can anyone help me answer this question?’” she says. “So the forward email and forward and reply all are the most dangerous features because you have to know what you are forwarding and would that person want it shared with everybody.”
Landa believes that part of the problem with the efficacy of email is that it’s become so fast and so easy that people don’t take their time thinking about the impact of each email. Dr. Arora agrees and suggests hospitalists think carefully about what is in an email, particularly when it involves patient information.
“Share the minimum necessary information with a minimum number of people to try to accomplish what you are trying to do,” she adds. “That way, you are not clogging the inbox of everybody involved.”
Another potential pitfall to the efficacy of email is the “lost in translation” phenomenon, Landa says.
“How many times have you written am email and someone misinterpreted sarcasm or a joke or a particular word or a phrase and got upset because of what they thought you were saying?” he says. “I think that when you talk about the synchronous and rapid-fire style of the forms of communication, I think you elevate the risk by an order of magnitude. That’s the reason we have developed all the emoticons and all the visual references that are out there—to make sure that people don’t misinterpret what we’re saying.”
What’s Old Is New
So if hospitalists and communications experts believe email retains a place in the way information is conveyed, why is the question of its impending death a continuing parlor game for some?
“Because there’s always something new,” Moore says. “Because Messenger on Facebook looks a little bit flashier than email. Because now we have Periscope. Now we have Twitter. Now we have different types of platforms that message within each other. They all look flashier.”
But, in essence, each is simply a somewhat more modernized version, more bells and whistles, Moore says. He likes to compare it to the U.S. Postal Service. As technology progressed and communication became more real-time in ways well beyond telephone conversations, many pundits forecasted the end of what is derisively called snail mail, itself an admission of the speed and efficacy of electronic mail.
“You could make the analogy between the death of email and the death of the U.S. mail,” Moore says. “Ten years ago, people were writing this article about the death of the U.S. mail. And it certainly changed. Yes, there are less letters and less traffic and less parcels that the post office sends. But it’s still there. It’s not going away; it’s just adapting in a certain way.
“If you want to pinpoint a time that there is ‘the death of email,’ I think the death of the U.S. mail comes before it.” TH
Richard Quinn is a freelance writer in New Jersey.
And yet despite the seemingly definitive place email communication holds for hospitalists—for messages to one another, missives to hospital administrators, instructions to patients, and myriad other uses—there are those who often wonder if email is outmoded. In a world bent on text messaging, Facebook, Twitter, Skype, Vine, Periscope, and Google Talk (not to mention dozens of lesser-known services and a seemingly endless string of startups aiming to be the proverbial next big thing), is email old-fashioned or ineffective?
In a word, no.
But that doesn’t mean email is the only communication method in a hospitalist’s toolbox or the best one for every situation. Physicians and communication experts interviewed by The Hospitalist agree that email has a function and isn’t going anywhere anytime soon. However, that function is dependent on trust, urgency, formality, and relationships.
“It has a place in communication, especially for busy hospitals, but the key is to figure out what is that place,” says Vineet Arora, MD, MAPP, FHM, a hospitalist at the University of Chicago, who has spoken at SHM annual meetings on how hospitalists communicate. “All of the information that is coming to you is in a push-pull model … There is information that you want pushed to you because it’s important and you want to see it. And then there is information that you want to pull because perhaps you know it relates to a patient in front of you … Where does email fit into it?”
Communications consultant A.J. Moore, associate professor of communication at Rider University in Lawrenceville, N.J., put it even more bluntly when assuring that email isn’t going anywhere.
“Research shows, and I know I do it myself, the first thing I do in the morning when I pick up my phone is check my email,” he says. “People often check their email before they check the weather, before they check social media.
“Sure, there are other places to go, there’s other ways of communicating. But I still think that email is the center point. It’s the starting line for your communication.”
A Modus for the Medium
Hospitalist Aaron Jacobs, MD, associate chief medical information officer at University of New Mexico Hospital in Albuquerque, appreciates the academic discussion over the future of email, but he also knows he uses it every day. To him, there are several factors that go into choosing which medium he uses for a particular message.
“It depends on the situation and the message you are sending,” says Dr. Jacobs, associate professor in the Department of Pediatrics at the University of New Mexico School of Medicine. “If I’m friends with the pediatric nephrologist, I may text him a quick question about a [glomerular filtration rate] or a clinical question. But if I’m not on those terms with another subspecialist, I wouldn’t do that.
“There’s definitely a relationship aspect that is relevant.”
Another factor in choosing to send an email versus a text message versus a tweet is timing. In the days when email was the only alternative to in-person communication or a phone call, the electronic message was the fastest way to reach a person. It was the best way to hold a synchronous conversation. But in today’s era of smartphones, tablets, and even wristwatches that have instant access, email is no longer the fastest option. In fact, email today is best tailored to asynchronous conversations, Dr. Arora says.
“Texting is really more invasive. It’s more demanding of the recipient’s time in an immediate sort of way,” Dr. Jacobs says. “With email, you’re basically saying, ‘Please take a look at this at your convenience, and when you can, write me back.’ In contrast, when people send text messages, they’re typically expecting a response in minutes. This may seem logical and trivial, but it can also be disruptive. Since some texts are urgent, all texts must at least initially be treated as such.”
The urgency that comes with a text message or a direct message on Facebook or Twitter is the flip side of the formality that comes with an email, says Moore.
“Email has more of a professional connotation to it than a Facebook message,” Moore says. “Even if I work with somebody, even if I’m Facebook friends with somebody and that person is one door away from me, if it is a work conversation, I am going to send them an email.”
Formality is the delineation between social media and what Moore half-jokingly calls “professional media.” And while in some ways technology gaps can often be a generational difference, Moore doesn’t see email usage through that prism and certainly not when he’s interacting with the young adults in his classes.
“I look at myself as a professor, and I have that formal relationship with younger people being students. They could find me on social media. There’s nothing preventing them,” he says. “But still they reach out to me via email, and I communicate with them via email.”
That being said, a generational gap does exist that can cause older physicians to refrain from embracing newer technologies that could be effective alternatives to email, says Howard Landa, chief medical information officer of the Alameda Health System in Oakland, Calif., and vice chairman of the board of advisors for the Association of Medical Directors of Information Systems. Many communication tools (Shortmail, Fridge, Apple Mail) either were discontinued, wrapped into larger technologies, or never became mainstream enough to be worthwhile. So the idea that some technologies won’t catch on discourages some from using anything but email.
“The younger we are, the easier the changes are and the more receptive we are to change,” Landa says. “We have seen a lot of flash-in-the-pan technology, snake oil, new ideas that go crazy for [a while]. They get to the top in the hype cycle, they drop to the bottom of the pit in the depression, and then they never move.
“With the older physicians, I think there is a reluctance to try something just because it’s new, whereas with the younger docs, there is every week a new technology that I want to try because I am willing to go through 20 of them before I find one that works. They have more energy and are more open to it.”
Security Is Job One
The safety of email is a major reason that many continually question its fate. In a broad sense, that is the natural question when a technology is new, says Ben Compaine, director of the fellows program at the Columbia University Institute for Tele-Information and a lecturer in the D’Amore-McKim School of Business at Northeastern University in Boston.
“There are always people who will find something to fear,” Compaine says. “Like when ATMs came along, there was stuff being written about safety concerns: ‘People will go to an ATM, and someone just holds them up and gets their money.’ It’s happened, but given the hundreds of millions of transactions that go on, you don’t throw out the baby with the bathwater.”
Dr. Arora cautions that the difference for hospitalists is that when a safety mistake is made with email, it can constitute a violation of the Health Insurance Portability and Accountability Act (HIPAA). And while those mistakes can happen innocently enough on social media or via text messaging, she says email issues are the most common.
“I’ve seen HIPAA violations where a patient would send an email to a doctor and the doctor would reply all to all of the [hospitalists] in their group saying, ‘Can anyone help me answer this question?’” she says. “So the forward email and forward and reply all are the most dangerous features because you have to know what you are forwarding and would that person want it shared with everybody.”
Landa believes that part of the problem with the efficacy of email is that it’s become so fast and so easy that people don’t take their time thinking about the impact of each email. Dr. Arora agrees and suggests hospitalists think carefully about what is in an email, particularly when it involves patient information.
“Share the minimum necessary information with a minimum number of people to try to accomplish what you are trying to do,” she adds. “That way, you are not clogging the inbox of everybody involved.”
Another potential pitfall to the efficacy of email is the “lost in translation” phenomenon, Landa says.
“How many times have you written am email and someone misinterpreted sarcasm or a joke or a particular word or a phrase and got upset because of what they thought you were saying?” he says. “I think that when you talk about the synchronous and rapid-fire style of the forms of communication, I think you elevate the risk by an order of magnitude. That’s the reason we have developed all the emoticons and all the visual references that are out there—to make sure that people don’t misinterpret what we’re saying.”
What’s Old Is New
So if hospitalists and communications experts believe email retains a place in the way information is conveyed, why is the question of its impending death a continuing parlor game for some?
“Because there’s always something new,” Moore says. “Because Messenger on Facebook looks a little bit flashier than email. Because now we have Periscope. Now we have Twitter. Now we have different types of platforms that message within each other. They all look flashier.”
But, in essence, each is simply a somewhat more modernized version, more bells and whistles, Moore says. He likes to compare it to the U.S. Postal Service. As technology progressed and communication became more real-time in ways well beyond telephone conversations, many pundits forecasted the end of what is derisively called snail mail, itself an admission of the speed and efficacy of electronic mail.
“You could make the analogy between the death of email and the death of the U.S. mail,” Moore says. “Ten years ago, people were writing this article about the death of the U.S. mail. And it certainly changed. Yes, there are less letters and less traffic and less parcels that the post office sends. But it’s still there. It’s not going away; it’s just adapting in a certain way.
“If you want to pinpoint a time that there is ‘the death of email,’ I think the death of the U.S. mail comes before it.” TH
Richard Quinn is a freelance writer in New Jersey.
Benefits of Hospital-Wide Mortality Reviews
Most divisions within a hospital will have a morbidity or mortality round where they review deaths that occurred in that department, but doing that on an institution-wide level is unusual and important. “It gives a totally different viewpoint,” he says. “When it’s a couple highly selected patients whose cases you examine, you really don’t have an idea at the end if the problems you identified are systemwide issues in your institution.”
The major issue the study identified was an inadequate discussion of goals of care. “This was often a patient who was dying, and in retrospect, it was clear that they were at high risk for death, but there had been no discussion with the patient about prognosis or about symptom management,” Dr. Kobewka says. “It seemed that care was directed at prolonging life. When we looked back at the case, that wasn’t realistic. That accounted for 25% of the quality issues that we identified: The discussion of prognosis and goals of care was inadequate or even absent all together. I think every hospital needs to think about those discussions and how and where and when we have them.”
Another revelation from the study: Errors in care are common but also underdiscussed. “When a physician is aware that maybe there was an error in care, it’s easy for there to be guilt and secrecy,” Dr. Kobewka says. “This is just a reminder that it’s common, and we need an open discussion about it. We need high-level, institution-wide systems to help us with this, but even at the individual provider level, this discussion needs to happen. Any quality improvement process needs engagement of frontline staff.”
Reference
- Kobewka DM, van Walraven C, Turnbull J, Worthington J, Calder L, Forster A. Quality gaps identified through mortality review [published online ahead of print February 8, 2016]. BMJ Qual Saf. doi:10.1136/bmjqs-2015-004735.
Most divisions within a hospital will have a morbidity or mortality round where they review deaths that occurred in that department, but doing that on an institution-wide level is unusual and important. “It gives a totally different viewpoint,” he says. “When it’s a couple highly selected patients whose cases you examine, you really don’t have an idea at the end if the problems you identified are systemwide issues in your institution.”
The major issue the study identified was an inadequate discussion of goals of care. “This was often a patient who was dying, and in retrospect, it was clear that they were at high risk for death, but there had been no discussion with the patient about prognosis or about symptom management,” Dr. Kobewka says. “It seemed that care was directed at prolonging life. When we looked back at the case, that wasn’t realistic. That accounted for 25% of the quality issues that we identified: The discussion of prognosis and goals of care was inadequate or even absent all together. I think every hospital needs to think about those discussions and how and where and when we have them.”
Another revelation from the study: Errors in care are common but also underdiscussed. “When a physician is aware that maybe there was an error in care, it’s easy for there to be guilt and secrecy,” Dr. Kobewka says. “This is just a reminder that it’s common, and we need an open discussion about it. We need high-level, institution-wide systems to help us with this, but even at the individual provider level, this discussion needs to happen. Any quality improvement process needs engagement of frontline staff.”
Reference
- Kobewka DM, van Walraven C, Turnbull J, Worthington J, Calder L, Forster A. Quality gaps identified through mortality review [published online ahead of print February 8, 2016]. BMJ Qual Saf. doi:10.1136/bmjqs-2015-004735.
Most divisions within a hospital will have a morbidity or mortality round where they review deaths that occurred in that department, but doing that on an institution-wide level is unusual and important. “It gives a totally different viewpoint,” he says. “When it’s a couple highly selected patients whose cases you examine, you really don’t have an idea at the end if the problems you identified are systemwide issues in your institution.”
The major issue the study identified was an inadequate discussion of goals of care. “This was often a patient who was dying, and in retrospect, it was clear that they were at high risk for death, but there had been no discussion with the patient about prognosis or about symptom management,” Dr. Kobewka says. “It seemed that care was directed at prolonging life. When we looked back at the case, that wasn’t realistic. That accounted for 25% of the quality issues that we identified: The discussion of prognosis and goals of care was inadequate or even absent all together. I think every hospital needs to think about those discussions and how and where and when we have them.”
Another revelation from the study: Errors in care are common but also underdiscussed. “When a physician is aware that maybe there was an error in care, it’s easy for there to be guilt and secrecy,” Dr. Kobewka says. “This is just a reminder that it’s common, and we need an open discussion about it. We need high-level, institution-wide systems to help us with this, but even at the individual provider level, this discussion needs to happen. Any quality improvement process needs engagement of frontline staff.”
Reference
- Kobewka DM, van Walraven C, Turnbull J, Worthington J, Calder L, Forster A. Quality gaps identified through mortality review [published online ahead of print February 8, 2016]. BMJ Qual Saf. doi:10.1136/bmjqs-2015-004735.
8 Lessons for Hospitalists Turned Entrepreneurs
If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

If you are a hospitalist, you are an entrepreneur almost by definition. All hospitalists are continuously engaged in improving the hospital experience for our patients. For some of us, the inner entrepreneur may grow to a point where we seriously consider a part-time or full-time commitment to an entrepreneurial dream. Combining our years of immersion in hospital patient care with an inventive streak can be a potent recipe for an innovative product or service idea.
It may be that the burgeoning startup scene in healthcare has inspired your dream. From coast to coast, there are startup incubators such as Rock Health, Healthbox, Blueprint Health, StartUp Health, Health Wildcatters, The Iron Yard, and TechSpring. These outfits support entrepreneurs with mentorship, funding, workspace, and/or information, such as how to deal with HIPAA or the FDA. Most of us have had at least a passing fascination with Steve Jobs–type characters, individuals who changed the world through their vision and force of will or who just seemed to enjoy a freedom that those who work for “The Man” will never know.
A few years ago, I caught the entrepreneurial bug. Initially, I continued with my day job and worked nights and weekends on my side project. Eventually, I made the leap to work full-time at an early-stage healthcare company. Since then, I’ve spent a lot of time trying to improve my new practice as a full-time entrepreneur, working as hard as ever, trying to be an effective innovator. Every day seems to bring new lessons—some more hard-earned than others—and there’s a lifetime of them still ahead. I’d like to share some of the insights I have learned on this journey. By the way, I still make time for patient care since that remains a priority for me.
Patience Is a Virtue, but Persistence and Positivity Count Even More
As Henry David Thoreau wrote, “Go confidently in the direction of your dreams.” Don’t postpone action indefinitely just because there are obstacles. Stop making excuses, make a start, and build momentum every day. Commit.
Becoming an entrepreneur is a long-term effort fueled by dedication and optimism, but first you have to make a start. You can’t win if you don’t play.
Action and Learning Matter More than Ideation
Start with your idea and a rough plan, but above all, believe in yourself, especially your ability to problem-solve. Many of the qualities that have fueled our success as physicians—precision, thoughtfulness, error aversion, and compulsiveness—might be constraints in a startup environment. Startups are hostile places for perfectionists and those who require complete information before proceeding. Have a bias for action and become comfortable with ambiguity. Entrepreneurs turn little things into big things by making progress every day.
Perhaps contrary to what we learn as physicians, entrepreneurs understand progress is measured more by authentic learning than by getting particular results. Entrepreneurs must quickly learn how to fail. In fact, progress often resembles multiple experiments that allow you to fail (and learn) faster. For entrepreneurs, perfection truly is the enemy of the good.
Learn, make adjustments, and progress will follow.
Guidance Is More Valuable than Money
Commercializing an idea is a challenging proposition. First-timers need advice, support, and help. For advice, find a mentor who has successfully launched a startup. Most of the successful people I know have had the wisdom or good fortune to have a mentor to provide guidance.
Startup incubators can be another source of support. Nearly all large cities and many medium and small cities now have business incubators or accelerators. Attend an event and get involved. They will provide many of the tools you will need to get started.
There are lots of opportunities for innovation in healthcare. But commercializing an idea will be one of the most challenging things you’ll ever do. Surround yourself with people who have skills that complement yours. Physician entrepreneurs need to be part of a viable team.
Sell, Sell, Sell
In business, as in life, “we’re all in sales.” We sell our ideas, our work product, ourselves. Even as physicians we have to sell patients and colleagues on our thought processes to be successful. Successful entrepreneurs are comfortable selling and put their best foot forward when trying to recruit a resource or persuade a potential customer.
Conflicts of Interest
“There is no interest without conflict.” If you look hard enough, you’ll see that we all have conflicts of interest. The key is to recognize them and disclose them. Of course, there are certain conflicts that are deal breakers. They must be avoided. If you remain employed, most of them are spelled out in your employer’s conflict of interest and intellectual property policies.
HIPAA Is an Innovation Killer
If your idea involves technology or services that address protected health information, become a HIPAA savant as soon as possible. The good news is that if you can effectively navigate the HIPAA challenge, you will have an advantage over your competitors.
Pure ‘Tech’ Plays Are Difficult
If you want to try to build the next killer app for healthcare and hope it will go viral, good luck. Based on my experience, it is difficult to get market traction with a pure technology offering. The strategy with a higher likelihood of success is to provide services with a technology platform that supports those services. As a provider of a service, you can provide immediate value to the customer and become “sticky” as you build your business (and software).
Enjoy the Journey, No Matter What
At first, you will be propelled by irrational exuberance and a passion for the greatness of your idea. That’s not only a good thing, it’s a requirement. But becoming a successful entrepreneur is a heavy haul down a long road of hard work and execution. Enjoying the journey is crucial since, beyond that, there are no guarantees. But life is short, so maybe you also value a career with no regrets. Take a chance and enjoy the ride.
Being a physician entrepreneur is not for everyone. But for those who take the plunge, it can be one of the most fulfilling, exciting, and meaningful journeys one could imagine. TH
Author note: I’d like to thank Dr. Jason Stein and Joe Miller for their helpful comments on this column.

Benefits of Earlier Palliative Care
Offering palliative care early to hospitalized patients with multiple serious conditions could improve care and help reduce healthcare spending, according to “Palliative Care Teams’ Cost-Saving Effect Is Larger for Cancer Patients with Higher Numbers of Comorbidities,” published in Health Affairs. When adults with advanced cancer (excluding those with dementia) received a palliative care consultation within two days of admission, costs were 22% lower for patients with a comorbidity score of 2 to 3 and 32% lower for those with a score of 4 or higher.
Reference
- May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53.
Quick Byte
Efforts to shift provider payment from fee-for-service to more risk-based alternatives are proceeding slowly: Nearly 95% of all 2013 physician office visits were reimbursed as fee-for-service.
Reference
- Zuvekas SH, Cohen JW. Fee-for-service, while much maligned, remains the dominant payment method for physician visits. Health Aff. 2016;35(3):411-414. doi:10.1377/hlthaff.2015.1291.
Offering palliative care early to hospitalized patients with multiple serious conditions could improve care and help reduce healthcare spending, according to “Palliative Care Teams’ Cost-Saving Effect Is Larger for Cancer Patients with Higher Numbers of Comorbidities,” published in Health Affairs. When adults with advanced cancer (excluding those with dementia) received a palliative care consultation within two days of admission, costs were 22% lower for patients with a comorbidity score of 2 to 3 and 32% lower for those with a score of 4 or higher.
Reference
- May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53.
Quick Byte
Efforts to shift provider payment from fee-for-service to more risk-based alternatives are proceeding slowly: Nearly 95% of all 2013 physician office visits were reimbursed as fee-for-service.
Reference
- Zuvekas SH, Cohen JW. Fee-for-service, while much maligned, remains the dominant payment method for physician visits. Health Aff. 2016;35(3):411-414. doi:10.1377/hlthaff.2015.1291.
Offering palliative care early to hospitalized patients with multiple serious conditions could improve care and help reduce healthcare spending, according to “Palliative Care Teams’ Cost-Saving Effect Is Larger for Cancer Patients with Higher Numbers of Comorbidities,” published in Health Affairs. When adults with advanced cancer (excluding those with dementia) received a palliative care consultation within two days of admission, costs were 22% lower for patients with a comorbidity score of 2 to 3 and 32% lower for those with a score of 4 or higher.
Reference
- May P, Garrido MM, Cassel JB, et al. Palliative care teams’ cost-saving effect is larger for cancer patients with higher numbers of comorbidities. Health Aff. 2016;35(1):44-53.
Quick Byte
Efforts to shift provider payment from fee-for-service to more risk-based alternatives are proceeding slowly: Nearly 95% of all 2013 physician office visits were reimbursed as fee-for-service.
Reference
- Zuvekas SH, Cohen JW. Fee-for-service, while much maligned, remains the dominant payment method for physician visits. Health Aff. 2016;35(3):411-414. doi:10.1377/hlthaff.2015.1291.