User login
Adjustment for characteristics not used by Medicare reduces hospital variations in readmission rates
Clinical question: Can differences in hospital readmission rates be explained by patient characteristics not accounted for by Medicare?
Background: In its Pay for Performance program, Medicare ties payments to readmission rates but adjusts these rates only for limited patient characteristics. Hospitals serving higher-risk patients have received greater penalties. These programs may have the unintended consequence of penalizing hospitals that provide care to higher-risk patients.
Study design: Observational study.
Setting: Medicare admissions claims from 2013 through 2014 in 2,215 hospitals.
Synopsis: Using Medicare claims for admission and linked U.S. census data, the study assessed several clinical and social characteristics not currently used for risk adjustment. A sample of 1,169,014 index admissions among 1,003,664 unique beneficiaries was analyzed. The study compared rates with and without these additional adjustments.
Additional adjustments reduced overall variation in hospital readmission by 9.6%, changed rates upward or downward by 0.4%-0.7% for the 10% of hospitals most affected by the readjustments, and they would be expected to reduce penalties by 52%, 46%, and 41% for hospitals with the largest 1%, 5%, and 10% of penalty reductions, respectively.
Bottom line: Hospitals serving higher-risk patients may be penalized because of the patients they serve rather that the quality of care they provide.
Citation: Roberts ET et al. Assessment of the effect of adjustment for patient characteristics on hospital readmission rates: Implications for Pay for Performance. JAMA Intern Med. 2018;178(11)1498-1507.
Dr. Asuen is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Can differences in hospital readmission rates be explained by patient characteristics not accounted for by Medicare?
Background: In its Pay for Performance program, Medicare ties payments to readmission rates but adjusts these rates only for limited patient characteristics. Hospitals serving higher-risk patients have received greater penalties. These programs may have the unintended consequence of penalizing hospitals that provide care to higher-risk patients.
Study design: Observational study.
Setting: Medicare admissions claims from 2013 through 2014 in 2,215 hospitals.
Synopsis: Using Medicare claims for admission and linked U.S. census data, the study assessed several clinical and social characteristics not currently used for risk adjustment. A sample of 1,169,014 index admissions among 1,003,664 unique beneficiaries was analyzed. The study compared rates with and without these additional adjustments.
Additional adjustments reduced overall variation in hospital readmission by 9.6%, changed rates upward or downward by 0.4%-0.7% for the 10% of hospitals most affected by the readjustments, and they would be expected to reduce penalties by 52%, 46%, and 41% for hospitals with the largest 1%, 5%, and 10% of penalty reductions, respectively.
Bottom line: Hospitals serving higher-risk patients may be penalized because of the patients they serve rather that the quality of care they provide.
Citation: Roberts ET et al. Assessment of the effect of adjustment for patient characteristics on hospital readmission rates: Implications for Pay for Performance. JAMA Intern Med. 2018;178(11)1498-1507.
Dr. Asuen is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Can differences in hospital readmission rates be explained by patient characteristics not accounted for by Medicare?
Background: In its Pay for Performance program, Medicare ties payments to readmission rates but adjusts these rates only for limited patient characteristics. Hospitals serving higher-risk patients have received greater penalties. These programs may have the unintended consequence of penalizing hospitals that provide care to higher-risk patients.
Study design: Observational study.
Setting: Medicare admissions claims from 2013 through 2014 in 2,215 hospitals.
Synopsis: Using Medicare claims for admission and linked U.S. census data, the study assessed several clinical and social characteristics not currently used for risk adjustment. A sample of 1,169,014 index admissions among 1,003,664 unique beneficiaries was analyzed. The study compared rates with and without these additional adjustments.
Additional adjustments reduced overall variation in hospital readmission by 9.6%, changed rates upward or downward by 0.4%-0.7% for the 10% of hospitals most affected by the readjustments, and they would be expected to reduce penalties by 52%, 46%, and 41% for hospitals with the largest 1%, 5%, and 10% of penalty reductions, respectively.
Bottom line: Hospitals serving higher-risk patients may be penalized because of the patients they serve rather that the quality of care they provide.
Citation: Roberts ET et al. Assessment of the effect of adjustment for patient characteristics on hospital readmission rates: Implications for Pay for Performance. JAMA Intern Med. 2018;178(11)1498-1507.
Dr. Asuen is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
Becoming a high-value care physician
‘Culture shift’ comes from collective efforts
It’s Monday morning, and Mrs. Jones still has abdominal pain. Your ward team decides to order a CT. On chart review you notice she’s had three other abdominal CTs for the same indication this year. How did this happen? What should you do?
High-value care has been defined by the Institute of Medicine as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.”1 With an estimated $700 billion dollars – 30% of medical expenditures – spent on wasted care, there are rising calls for a transformational shift.2
You are now asked to consider not just everything you can do for a patient, but also the benefits, harms, and costs associated with those choices. But where to start? We recommend that trainees integrate these tips for high-value care into their routine practice.
1. Use evidence-based resources that highlight value
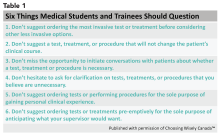
A great place to begin is the “Six Things Medical Students and Trainees Should Question,” originally published in Academic Medicine and created by Choosing Wisely Canada™. Recommendations range from avoiding tests or treatments that will not change a patient’s clinical course to holding off on ordering tests solely based on what you assume your preceptor will want (see the full list in Table 1).3
Other ways to avoid low-value care include following the United States Choosing Wisely™ campaign, which has collected more than 500 specialty society recommendations. Likewise, the American College of Radiology Appropriateness Criteria are designed to assist providers with ordering the appropriate imaging tests (for a more extensive list see Table 2).
2. Express your clinical reasoning
One driver of health care expenditures that is especially prevalent in academia is the pressure to demonstrate knowledge by recommending extensive testing. While these tests may rule out obscure diagnoses, they often do not change management.
You can still demonstrate a mastery of your patients’ care by expressing your thought process overtly. For instance, “I considered secondary causes of the patient’s severe hypertension but felt it was most reasonable to first treat her pain and restart her home medications before pursuing a larger work-up. If the patient’s blood pressure remains elevated and she is hypokalemic, we could consider testing for hyperaldosteronism.” If you explain why you think a diagnosis is less likely and order tests accordingly, others will be encouraged to consider value in their own medical decision making.
3. Hone your communication skills
One of the most cited reasons for providing unnecessary care is the time required to discuss treatment plans with patients – it’s much faster to just order the test than to explain why it isn’t needed. Research, however, shows that these cost conversations take 68 seconds on average.4 Costs of Care (see Table 2) has an excellent video series that highlights how effective communication allows for shared decision making, which promotes both patient engagement and helps avoid wasteful care.
Physicians’ first instincts are often defensive when a patient asks for care we perceive as unnecessary. However, exploring what the patient hopes to gain from said test or treatment frequently reveals concern for a specific, missed diagnosis or complication. Addressing this underlying fear, rather than defending your ordering patterns, can create improved rapport and may serve to provide more reassurance than a test ever could.5
As a physician-in-training, try to observe others having these conversations and take every opportunity to practice. By focusing on this key skill set, you will increase your comfort with in-depth discussions on the value of care.
4. Get involved in a project related to high-value care
While you are developing your own practice patterns, you may be inspired to tackle areas of overuse and underuse at a more systemwide level. If your hospital does not have a committee for high-value care, perhaps a quality improvement leader can support your ideas to launch a project or participate in an ongoing initiative. Physicians-in-training have been identified as crucial to these projects’ success – your frontline insight can highlight potential problems and the nuances of workflow that are key to effective solutions.6
5. Embrace lifelong learning and reflection
The process of becoming a physician and of practicing high-value care is not a sprint but a marathon. Multiple barriers to high-value care exist, and you may feel these pressures differently at various points in your career. These include malpractice concerns, addressing patient expectations, and the desire to take action “just to be safe.”6
Interestingly, fear of malpractice does not seem to dissipate in areas where tort reform has provided stronger provider protections.7 Practitioners may also inaccurately assume a patient’s desire for additional work-up or treatment.8 Furthermore, be aware of the role of “commission bias” by which a provider regrets not doing something that could have helped a previous patient. This regret can prove to be a stronger motivator than the potential harm related to unnecessary diagnostic tests or treatments.9
While these barriers cannot be removed easily, learners and providers can practice active reflection by examining their own fears, biases, and motivations before and after they order additional testing or treatment.
As a physician-in-training, you may feel that your decisions do not have a major impact on the health care system as a whole. However, the culture shift needed to “bend the cost curve” will come from the collective efforts of individuals like you. Practicing high-value care is not just a matter of ordering fewer tests – appropriate ordering of an expensive test that expedites a diagnosis may be more cost-effective and enhance the quality of care provided. Increasing your own awareness of both necessary and unnecessary practices is a major step toward realizing system change. Your efforts to resist and reform the medical culture that propagates low value care will encourage your colleagues to follow suit.
Dr. Lacy is assistant professor and associate clerkship director at the University of New Mexico, Albuquerque, as well as division director of high-value care for the division of hospital medicine. Dr. Goetz is assistant professor at Rush University Medical Center, Chicago. They met as 2015 Copello Fellows at the National Physician Alliance. Both have been involved in numerous high-value care initiatives, curricular development, and medical education at their respective institutions.
References
1. Committee on the Learning Health Care System in America, Institute of Medicine. “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Edited by Smith M, Saunders R, Stuckhardt L, and McGinnis JM. (Washington: National Academies Press, 2013). http://www.ncbi.nlm.nih.gov/books/NBK207225/.
2. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513-6.
3. Lakhani A et al. Choosing Wisely for Medical Education: Six things medical students and trainees should question. Acad Med. 2016 Oct;91(10):1374-8.
4. Hunter WG et al. Patient-physician discussions about costs: Definitions and impact on cost conversation incidence estimates. BMC Health Serv Res. 2016;16:108.
5. van Ravesteijn H et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012;86(1):3-8.
6. Moriates C, Wong BM. High-value care programmes from the bottom-up… and the top-down. BMJ Qual Saf. 2016;25(11):821-3.
7. Snyder Sulmasy L, Weinberger SE. Better care is the best defense: High-value clinical practice vs. defensive medicine. Cleve Clin J Med. 2014;81(8):464-7.
8. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: Patients’ preferences matter. BMJ. 2012;345:e6572.
9. Scott IA. Cognitive challenges to minimising low value care. Intern Med J. 2017;47(9):1079-1083.
‘Culture shift’ comes from collective efforts
‘Culture shift’ comes from collective efforts
It’s Monday morning, and Mrs. Jones still has abdominal pain. Your ward team decides to order a CT. On chart review you notice she’s had three other abdominal CTs for the same indication this year. How did this happen? What should you do?
High-value care has been defined by the Institute of Medicine as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.”1 With an estimated $700 billion dollars – 30% of medical expenditures – spent on wasted care, there are rising calls for a transformational shift.2
You are now asked to consider not just everything you can do for a patient, but also the benefits, harms, and costs associated with those choices. But where to start? We recommend that trainees integrate these tips for high-value care into their routine practice.
1. Use evidence-based resources that highlight value
A great place to begin is the “Six Things Medical Students and Trainees Should Question,” originally published in Academic Medicine and created by Choosing Wisely Canada™. Recommendations range from avoiding tests or treatments that will not change a patient’s clinical course to holding off on ordering tests solely based on what you assume your preceptor will want (see the full list in Table 1).3
Other ways to avoid low-value care include following the United States Choosing Wisely™ campaign, which has collected more than 500 specialty society recommendations. Likewise, the American College of Radiology Appropriateness Criteria are designed to assist providers with ordering the appropriate imaging tests (for a more extensive list see Table 2).
2. Express your clinical reasoning
One driver of health care expenditures that is especially prevalent in academia is the pressure to demonstrate knowledge by recommending extensive testing. While these tests may rule out obscure diagnoses, they often do not change management.
You can still demonstrate a mastery of your patients’ care by expressing your thought process overtly. For instance, “I considered secondary causes of the patient’s severe hypertension but felt it was most reasonable to first treat her pain and restart her home medications before pursuing a larger work-up. If the patient’s blood pressure remains elevated and she is hypokalemic, we could consider testing for hyperaldosteronism.” If you explain why you think a diagnosis is less likely and order tests accordingly, others will be encouraged to consider value in their own medical decision making.
3. Hone your communication skills
One of the most cited reasons for providing unnecessary care is the time required to discuss treatment plans with patients – it’s much faster to just order the test than to explain why it isn’t needed. Research, however, shows that these cost conversations take 68 seconds on average.4 Costs of Care (see Table 2) has an excellent video series that highlights how effective communication allows for shared decision making, which promotes both patient engagement and helps avoid wasteful care.
Physicians’ first instincts are often defensive when a patient asks for care we perceive as unnecessary. However, exploring what the patient hopes to gain from said test or treatment frequently reveals concern for a specific, missed diagnosis or complication. Addressing this underlying fear, rather than defending your ordering patterns, can create improved rapport and may serve to provide more reassurance than a test ever could.5
As a physician-in-training, try to observe others having these conversations and take every opportunity to practice. By focusing on this key skill set, you will increase your comfort with in-depth discussions on the value of care.
4. Get involved in a project related to high-value care
While you are developing your own practice patterns, you may be inspired to tackle areas of overuse and underuse at a more systemwide level. If your hospital does not have a committee for high-value care, perhaps a quality improvement leader can support your ideas to launch a project or participate in an ongoing initiative. Physicians-in-training have been identified as crucial to these projects’ success – your frontline insight can highlight potential problems and the nuances of workflow that are key to effective solutions.6
5. Embrace lifelong learning and reflection
The process of becoming a physician and of practicing high-value care is not a sprint but a marathon. Multiple barriers to high-value care exist, and you may feel these pressures differently at various points in your career. These include malpractice concerns, addressing patient expectations, and the desire to take action “just to be safe.”6
Interestingly, fear of malpractice does not seem to dissipate in areas where tort reform has provided stronger provider protections.7 Practitioners may also inaccurately assume a patient’s desire for additional work-up or treatment.8 Furthermore, be aware of the role of “commission bias” by which a provider regrets not doing something that could have helped a previous patient. This regret can prove to be a stronger motivator than the potential harm related to unnecessary diagnostic tests or treatments.9
While these barriers cannot be removed easily, learners and providers can practice active reflection by examining their own fears, biases, and motivations before and after they order additional testing or treatment.
As a physician-in-training, you may feel that your decisions do not have a major impact on the health care system as a whole. However, the culture shift needed to “bend the cost curve” will come from the collective efforts of individuals like you. Practicing high-value care is not just a matter of ordering fewer tests – appropriate ordering of an expensive test that expedites a diagnosis may be more cost-effective and enhance the quality of care provided. Increasing your own awareness of both necessary and unnecessary practices is a major step toward realizing system change. Your efforts to resist and reform the medical culture that propagates low value care will encourage your colleagues to follow suit.
Dr. Lacy is assistant professor and associate clerkship director at the University of New Mexico, Albuquerque, as well as division director of high-value care for the division of hospital medicine. Dr. Goetz is assistant professor at Rush University Medical Center, Chicago. They met as 2015 Copello Fellows at the National Physician Alliance. Both have been involved in numerous high-value care initiatives, curricular development, and medical education at their respective institutions.
References
1. Committee on the Learning Health Care System in America, Institute of Medicine. “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Edited by Smith M, Saunders R, Stuckhardt L, and McGinnis JM. (Washington: National Academies Press, 2013). http://www.ncbi.nlm.nih.gov/books/NBK207225/.
2. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513-6.
3. Lakhani A et al. Choosing Wisely for Medical Education: Six things medical students and trainees should question. Acad Med. 2016 Oct;91(10):1374-8.
4. Hunter WG et al. Patient-physician discussions about costs: Definitions and impact on cost conversation incidence estimates. BMC Health Serv Res. 2016;16:108.
5. van Ravesteijn H et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012;86(1):3-8.
6. Moriates C, Wong BM. High-value care programmes from the bottom-up… and the top-down. BMJ Qual Saf. 2016;25(11):821-3.
7. Snyder Sulmasy L, Weinberger SE. Better care is the best defense: High-value clinical practice vs. defensive medicine. Cleve Clin J Med. 2014;81(8):464-7.
8. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: Patients’ preferences matter. BMJ. 2012;345:e6572.
9. Scott IA. Cognitive challenges to minimising low value care. Intern Med J. 2017;47(9):1079-1083.
It’s Monday morning, and Mrs. Jones still has abdominal pain. Your ward team decides to order a CT. On chart review you notice she’s had three other abdominal CTs for the same indication this year. How did this happen? What should you do?
High-value care has been defined by the Institute of Medicine as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.”1 With an estimated $700 billion dollars – 30% of medical expenditures – spent on wasted care, there are rising calls for a transformational shift.2
You are now asked to consider not just everything you can do for a patient, but also the benefits, harms, and costs associated with those choices. But where to start? We recommend that trainees integrate these tips for high-value care into their routine practice.
1. Use evidence-based resources that highlight value
A great place to begin is the “Six Things Medical Students and Trainees Should Question,” originally published in Academic Medicine and created by Choosing Wisely Canada™. Recommendations range from avoiding tests or treatments that will not change a patient’s clinical course to holding off on ordering tests solely based on what you assume your preceptor will want (see the full list in Table 1).3
Other ways to avoid low-value care include following the United States Choosing Wisely™ campaign, which has collected more than 500 specialty society recommendations. Likewise, the American College of Radiology Appropriateness Criteria are designed to assist providers with ordering the appropriate imaging tests (for a more extensive list see Table 2).
2. Express your clinical reasoning
One driver of health care expenditures that is especially prevalent in academia is the pressure to demonstrate knowledge by recommending extensive testing. While these tests may rule out obscure diagnoses, they often do not change management.
You can still demonstrate a mastery of your patients’ care by expressing your thought process overtly. For instance, “I considered secondary causes of the patient’s severe hypertension but felt it was most reasonable to first treat her pain and restart her home medications before pursuing a larger work-up. If the patient’s blood pressure remains elevated and she is hypokalemic, we could consider testing for hyperaldosteronism.” If you explain why you think a diagnosis is less likely and order tests accordingly, others will be encouraged to consider value in their own medical decision making.
3. Hone your communication skills
One of the most cited reasons for providing unnecessary care is the time required to discuss treatment plans with patients – it’s much faster to just order the test than to explain why it isn’t needed. Research, however, shows that these cost conversations take 68 seconds on average.4 Costs of Care (see Table 2) has an excellent video series that highlights how effective communication allows for shared decision making, which promotes both patient engagement and helps avoid wasteful care.
Physicians’ first instincts are often defensive when a patient asks for care we perceive as unnecessary. However, exploring what the patient hopes to gain from said test or treatment frequently reveals concern for a specific, missed diagnosis or complication. Addressing this underlying fear, rather than defending your ordering patterns, can create improved rapport and may serve to provide more reassurance than a test ever could.5
As a physician-in-training, try to observe others having these conversations and take every opportunity to practice. By focusing on this key skill set, you will increase your comfort with in-depth discussions on the value of care.
4. Get involved in a project related to high-value care
While you are developing your own practice patterns, you may be inspired to tackle areas of overuse and underuse at a more systemwide level. If your hospital does not have a committee for high-value care, perhaps a quality improvement leader can support your ideas to launch a project or participate in an ongoing initiative. Physicians-in-training have been identified as crucial to these projects’ success – your frontline insight can highlight potential problems and the nuances of workflow that are key to effective solutions.6
5. Embrace lifelong learning and reflection
The process of becoming a physician and of practicing high-value care is not a sprint but a marathon. Multiple barriers to high-value care exist, and you may feel these pressures differently at various points in your career. These include malpractice concerns, addressing patient expectations, and the desire to take action “just to be safe.”6
Interestingly, fear of malpractice does not seem to dissipate in areas where tort reform has provided stronger provider protections.7 Practitioners may also inaccurately assume a patient’s desire for additional work-up or treatment.8 Furthermore, be aware of the role of “commission bias” by which a provider regrets not doing something that could have helped a previous patient. This regret can prove to be a stronger motivator than the potential harm related to unnecessary diagnostic tests or treatments.9
While these barriers cannot be removed easily, learners and providers can practice active reflection by examining their own fears, biases, and motivations before and after they order additional testing or treatment.
As a physician-in-training, you may feel that your decisions do not have a major impact on the health care system as a whole. However, the culture shift needed to “bend the cost curve” will come from the collective efforts of individuals like you. Practicing high-value care is not just a matter of ordering fewer tests – appropriate ordering of an expensive test that expedites a diagnosis may be more cost-effective and enhance the quality of care provided. Increasing your own awareness of both necessary and unnecessary practices is a major step toward realizing system change. Your efforts to resist and reform the medical culture that propagates low value care will encourage your colleagues to follow suit.
Dr. Lacy is assistant professor and associate clerkship director at the University of New Mexico, Albuquerque, as well as division director of high-value care for the division of hospital medicine. Dr. Goetz is assistant professor at Rush University Medical Center, Chicago. They met as 2015 Copello Fellows at the National Physician Alliance. Both have been involved in numerous high-value care initiatives, curricular development, and medical education at their respective institutions.
References
1. Committee on the Learning Health Care System in America, Institute of Medicine. “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Edited by Smith M, Saunders R, Stuckhardt L, and McGinnis JM. (Washington: National Academies Press, 2013). http://www.ncbi.nlm.nih.gov/books/NBK207225/.
2. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513-6.
3. Lakhani A et al. Choosing Wisely for Medical Education: Six things medical students and trainees should question. Acad Med. 2016 Oct;91(10):1374-8.
4. Hunter WG et al. Patient-physician discussions about costs: Definitions and impact on cost conversation incidence estimates. BMC Health Serv Res. 2016;16:108.
5. van Ravesteijn H et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012;86(1):3-8.
6. Moriates C, Wong BM. High-value care programmes from the bottom-up… and the top-down. BMJ Qual Saf. 2016;25(11):821-3.
7. Snyder Sulmasy L, Weinberger SE. Better care is the best defense: High-value clinical practice vs. defensive medicine. Cleve Clin J Med. 2014;81(8):464-7.
8. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: Patients’ preferences matter. BMJ. 2012;345:e6572.
9. Scott IA. Cognitive challenges to minimising low value care. Intern Med J. 2017;47(9):1079-1083.
Physician burnout may be jeopardizing patient care
Clinical question: Is physician burnout associated with more patient safety issues, low professionalism, or poor patient satisfaction?
Background: Burnout is common among physicians and has a negative effect on their personal lives. It is unclear whether physician burnout is associated with poor outcomes for patients.
Study design: Meta-analysis.
Setting: Forty-seven published studies from 19 countries assessing inpatient and outpatient physicians and the relationship between physician burnout and patient care.
Synopsis: After a systematic review of the published literature, 47 studies were included to pool data from 42,473 physicians. Study subjects included residents, early-career and late-career physicians, and both hospital and outpatient physicians. All studies used validated measures of physician burnout.
Burnout was associated with a two-fold increased risk of physician-reported safety incidents (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), low professionalism (OR, 2.31; 95% CI, 1.87-2.85), and likelihood of low patient-reported satisfaction (OR, 2.28; 95% CI, 1.42-3.68). There were no significant differences in these results based on country of origin of the study. Early-career physicians were more likely to have burnout associated with low professionalism than were late-career physicians.
Of the components of burnout, depersonalization was most strongly associated with these negative outcomes. Interestingly, the increased risk of patient safety incidents was associated with physician-reported, but not health care system–reported, patient safety outcomes. This raises concerns that the health care systems may not be capturing “near misses” in their metrics.
Bottom line: Physician burnout doubles the risk of being involved in a patient safety incident, low professionalism, and poor patient satisfaction.
Citation: Panagioti M et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction. JAMA Intern Med. 2018;178(10):1317-30.
Dr. Gabriel is assistant professor of medicine and director of Pre-operative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Is physician burnout associated with more patient safety issues, low professionalism, or poor patient satisfaction?
Background: Burnout is common among physicians and has a negative effect on their personal lives. It is unclear whether physician burnout is associated with poor outcomes for patients.
Study design: Meta-analysis.
Setting: Forty-seven published studies from 19 countries assessing inpatient and outpatient physicians and the relationship between physician burnout and patient care.
Synopsis: After a systematic review of the published literature, 47 studies were included to pool data from 42,473 physicians. Study subjects included residents, early-career and late-career physicians, and both hospital and outpatient physicians. All studies used validated measures of physician burnout.
Burnout was associated with a two-fold increased risk of physician-reported safety incidents (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), low professionalism (OR, 2.31; 95% CI, 1.87-2.85), and likelihood of low patient-reported satisfaction (OR, 2.28; 95% CI, 1.42-3.68). There were no significant differences in these results based on country of origin of the study. Early-career physicians were more likely to have burnout associated with low professionalism than were late-career physicians.
Of the components of burnout, depersonalization was most strongly associated with these negative outcomes. Interestingly, the increased risk of patient safety incidents was associated with physician-reported, but not health care system–reported, patient safety outcomes. This raises concerns that the health care systems may not be capturing “near misses” in their metrics.
Bottom line: Physician burnout doubles the risk of being involved in a patient safety incident, low professionalism, and poor patient satisfaction.
Citation: Panagioti M et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction. JAMA Intern Med. 2018;178(10):1317-30.
Dr. Gabriel is assistant professor of medicine and director of Pre-operative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Is physician burnout associated with more patient safety issues, low professionalism, or poor patient satisfaction?
Background: Burnout is common among physicians and has a negative effect on their personal lives. It is unclear whether physician burnout is associated with poor outcomes for patients.
Study design: Meta-analysis.
Setting: Forty-seven published studies from 19 countries assessing inpatient and outpatient physicians and the relationship between physician burnout and patient care.
Synopsis: After a systematic review of the published literature, 47 studies were included to pool data from 42,473 physicians. Study subjects included residents, early-career and late-career physicians, and both hospital and outpatient physicians. All studies used validated measures of physician burnout.
Burnout was associated with a two-fold increased risk of physician-reported safety incidents (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), low professionalism (OR, 2.31; 95% CI, 1.87-2.85), and likelihood of low patient-reported satisfaction (OR, 2.28; 95% CI, 1.42-3.68). There were no significant differences in these results based on country of origin of the study. Early-career physicians were more likely to have burnout associated with low professionalism than were late-career physicians.
Of the components of burnout, depersonalization was most strongly associated with these negative outcomes. Interestingly, the increased risk of patient safety incidents was associated with physician-reported, but not health care system–reported, patient safety outcomes. This raises concerns that the health care systems may not be capturing “near misses” in their metrics.
Bottom line: Physician burnout doubles the risk of being involved in a patient safety incident, low professionalism, and poor patient satisfaction.
Citation: Panagioti M et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction. JAMA Intern Med. 2018;178(10):1317-30.
Dr. Gabriel is assistant professor of medicine and director of Pre-operative Medicine and Medicine Consult Service in the division of hospital medicine at Mount Sinai Hospital, New York.
Creating better performance incentives
P4P programs suffer from several flaws
Many performance improvement programs try to create a higher value health system by incentivizing physicians and health systems to behave in particular ways. These have often been pay-for-performance programs that offer bonuses or impose penalties depending on how providers perform on various metrics.
“In theory, this makes sense,” said Dhruv Khullar, MD, MPP, lead author of a JAMA article about the future of incentives, and assistant professor at Weill Cornell Medicine in New York. “But in practice, these programs have not been successful in consistently improving quality, and sometimes they have been counterproductive. In our article, we argued that focusing too narrowly on financial rewards is not the right strategy to improve health system performance – and is sometimes at odds with the physician professionalism and what really motivates most clinicians.”
Pay-for-performance programs suffer from several fundamental flaws: they focus too narrowly on financial incentives and use centralized accountability instead of local culture, for example, Dr. Khullar said.
“A better future state would involve capitalizing on physician professionalism through nonfinancial rewards, resources for quality improvement, team-based assessments, and emphasizing continuous learning and organizational culture,” he noted. Performance programs would take a more global view of clinical care by emphasizing culture, teams, trust, and learning. Such a system would allow hospitalists and other physicians to worry less about meeting specific metrics and focus more on providing high-quality care to their patients.
“I would hope physicians, payers, and administrators would reconsider some previously held beliefs about quality improvement, especially the idea that better quality requires giving people bonus payments or imposing financial penalties,” Dr. Khullar said. “We believe the next wave of performance improvement programs should entertain other paths to better quality, which are more in line with human motivation and physician professionalism.”
Reference
1. Khullar D, Wolfson D, Casalino LP. Professionalism, Performance, and the Future of Physician Incentives. JAMA. 2018 Nov 26 (Epub ahead of print). doi: 10.1001/jama.2018.17719. Accessed Dec. 11, 2018.
P4P programs suffer from several flaws
P4P programs suffer from several flaws
Many performance improvement programs try to create a higher value health system by incentivizing physicians and health systems to behave in particular ways. These have often been pay-for-performance programs that offer bonuses or impose penalties depending on how providers perform on various metrics.
“In theory, this makes sense,” said Dhruv Khullar, MD, MPP, lead author of a JAMA article about the future of incentives, and assistant professor at Weill Cornell Medicine in New York. “But in practice, these programs have not been successful in consistently improving quality, and sometimes they have been counterproductive. In our article, we argued that focusing too narrowly on financial rewards is not the right strategy to improve health system performance – and is sometimes at odds with the physician professionalism and what really motivates most clinicians.”
Pay-for-performance programs suffer from several fundamental flaws: they focus too narrowly on financial incentives and use centralized accountability instead of local culture, for example, Dr. Khullar said.
“A better future state would involve capitalizing on physician professionalism through nonfinancial rewards, resources for quality improvement, team-based assessments, and emphasizing continuous learning and organizational culture,” he noted. Performance programs would take a more global view of clinical care by emphasizing culture, teams, trust, and learning. Such a system would allow hospitalists and other physicians to worry less about meeting specific metrics and focus more on providing high-quality care to their patients.
“I would hope physicians, payers, and administrators would reconsider some previously held beliefs about quality improvement, especially the idea that better quality requires giving people bonus payments or imposing financial penalties,” Dr. Khullar said. “We believe the next wave of performance improvement programs should entertain other paths to better quality, which are more in line with human motivation and physician professionalism.”
Reference
1. Khullar D, Wolfson D, Casalino LP. Professionalism, Performance, and the Future of Physician Incentives. JAMA. 2018 Nov 26 (Epub ahead of print). doi: 10.1001/jama.2018.17719. Accessed Dec. 11, 2018.
Many performance improvement programs try to create a higher value health system by incentivizing physicians and health systems to behave in particular ways. These have often been pay-for-performance programs that offer bonuses or impose penalties depending on how providers perform on various metrics.
“In theory, this makes sense,” said Dhruv Khullar, MD, MPP, lead author of a JAMA article about the future of incentives, and assistant professor at Weill Cornell Medicine in New York. “But in practice, these programs have not been successful in consistently improving quality, and sometimes they have been counterproductive. In our article, we argued that focusing too narrowly on financial rewards is not the right strategy to improve health system performance – and is sometimes at odds with the physician professionalism and what really motivates most clinicians.”
Pay-for-performance programs suffer from several fundamental flaws: they focus too narrowly on financial incentives and use centralized accountability instead of local culture, for example, Dr. Khullar said.
“A better future state would involve capitalizing on physician professionalism through nonfinancial rewards, resources for quality improvement, team-based assessments, and emphasizing continuous learning and organizational culture,” he noted. Performance programs would take a more global view of clinical care by emphasizing culture, teams, trust, and learning. Such a system would allow hospitalists and other physicians to worry less about meeting specific metrics and focus more on providing high-quality care to their patients.
“I would hope physicians, payers, and administrators would reconsider some previously held beliefs about quality improvement, especially the idea that better quality requires giving people bonus payments or imposing financial penalties,” Dr. Khullar said. “We believe the next wave of performance improvement programs should entertain other paths to better quality, which are more in line with human motivation and physician professionalism.”
Reference
1. Khullar D, Wolfson D, Casalino LP. Professionalism, Performance, and the Future of Physician Incentives. JAMA. 2018 Nov 26 (Epub ahead of print). doi: 10.1001/jama.2018.17719. Accessed Dec. 11, 2018.
Reducing adverse drug reactions
Easing the inpatient/outpatient transition
Adverse drug reactions are a problem hospitalists encounter often. An estimated 9% of hospital admissions in older adults are the result of adverse drug reactions, and up to one in five adults experience an adverse drug reaction during hospitalization.
“Many interventions have been tried to solve this problem, and certain of them have worked, but to date we don’t have any great solutions that meaningfully impact the rate of these events in a way that’s feasible in most health care environments, so any efforts to reduce the burden of these problems in older adults could be hugely beneficial,” said Michael Steinman, MD, author of an editorial highlighting a new approach.
His editorial in BMJ Quality & Safety cites research on the Pharm2Pharm program, implemented in six Hawaiian hospitals, in which hospital-based pharmacists identified inpatients at high risk of medication misadventures with criteria such as use of multiple medications, presence of high-risk medications such as warfarin or glucose-lowering drugs, and a history of previous acute care use resulting from medication-related problems. The hospital pharmacist would then meet with the patient to reconcile medications and facilitate a coordinated hand-off to a community pharmacist, who would meet with the patient after discharge.
In addition to a 36% reduction in the rate of medication-related hospitalizations, the intervention generated an estimated savings of $6.6 million per year in avoided hospitalizations.
There are two major takeaways, said Dr. Steinman, who is based in the division of geriatrics at the University of California, San Francisco: It’s critical to focus on transitions and coordination between inpatient and outpatient care to address medication-related problems, and pharmacists can be extremely helpful in that.
“Decisions about drug therapy in the hospital may seem reasonable in the short term but often won’t stick in the long term unless there is a coordinated care that can help ensure appropriate follow-through once patients return home,” Dr. Steinman said. “The study that the editorial references is a systems intervention that hospitalists can advocate for in their own institutions, but in the immediate day-to-day, trying to ensure solid coordination of medication management from the inpatient to outpatient setting is likely to be very helpful for their patients.”
The long-term outcomes of hospitalized patients are largely influenced by getting them set up with appropriate community resources and supports once they leave the hospital, he added, and the hospital can play a critical role in putting these pieces into place.
Reference
1. Steinman MA. Reducing hospital admissions for adverse drug events through coordinated pharmacist care: learning from Hawai’i without a field trip. BMJ Qual Saf. Epub 2018 Nov 24. doi: 10.1136/bmjqs-2018-008815. Accessed Dec. 11, 2018.
Easing the inpatient/outpatient transition
Easing the inpatient/outpatient transition
Adverse drug reactions are a problem hospitalists encounter often. An estimated 9% of hospital admissions in older adults are the result of adverse drug reactions, and up to one in five adults experience an adverse drug reaction during hospitalization.
“Many interventions have been tried to solve this problem, and certain of them have worked, but to date we don’t have any great solutions that meaningfully impact the rate of these events in a way that’s feasible in most health care environments, so any efforts to reduce the burden of these problems in older adults could be hugely beneficial,” said Michael Steinman, MD, author of an editorial highlighting a new approach.
His editorial in BMJ Quality & Safety cites research on the Pharm2Pharm program, implemented in six Hawaiian hospitals, in which hospital-based pharmacists identified inpatients at high risk of medication misadventures with criteria such as use of multiple medications, presence of high-risk medications such as warfarin or glucose-lowering drugs, and a history of previous acute care use resulting from medication-related problems. The hospital pharmacist would then meet with the patient to reconcile medications and facilitate a coordinated hand-off to a community pharmacist, who would meet with the patient after discharge.
In addition to a 36% reduction in the rate of medication-related hospitalizations, the intervention generated an estimated savings of $6.6 million per year in avoided hospitalizations.
There are two major takeaways, said Dr. Steinman, who is based in the division of geriatrics at the University of California, San Francisco: It’s critical to focus on transitions and coordination between inpatient and outpatient care to address medication-related problems, and pharmacists can be extremely helpful in that.
“Decisions about drug therapy in the hospital may seem reasonable in the short term but often won’t stick in the long term unless there is a coordinated care that can help ensure appropriate follow-through once patients return home,” Dr. Steinman said. “The study that the editorial references is a systems intervention that hospitalists can advocate for in their own institutions, but in the immediate day-to-day, trying to ensure solid coordination of medication management from the inpatient to outpatient setting is likely to be very helpful for their patients.”
The long-term outcomes of hospitalized patients are largely influenced by getting them set up with appropriate community resources and supports once they leave the hospital, he added, and the hospital can play a critical role in putting these pieces into place.
Reference
1. Steinman MA. Reducing hospital admissions for adverse drug events through coordinated pharmacist care: learning from Hawai’i without a field trip. BMJ Qual Saf. Epub 2018 Nov 24. doi: 10.1136/bmjqs-2018-008815. Accessed Dec. 11, 2018.
Adverse drug reactions are a problem hospitalists encounter often. An estimated 9% of hospital admissions in older adults are the result of adverse drug reactions, and up to one in five adults experience an adverse drug reaction during hospitalization.
“Many interventions have been tried to solve this problem, and certain of them have worked, but to date we don’t have any great solutions that meaningfully impact the rate of these events in a way that’s feasible in most health care environments, so any efforts to reduce the burden of these problems in older adults could be hugely beneficial,” said Michael Steinman, MD, author of an editorial highlighting a new approach.
His editorial in BMJ Quality & Safety cites research on the Pharm2Pharm program, implemented in six Hawaiian hospitals, in which hospital-based pharmacists identified inpatients at high risk of medication misadventures with criteria such as use of multiple medications, presence of high-risk medications such as warfarin or glucose-lowering drugs, and a history of previous acute care use resulting from medication-related problems. The hospital pharmacist would then meet with the patient to reconcile medications and facilitate a coordinated hand-off to a community pharmacist, who would meet with the patient after discharge.
In addition to a 36% reduction in the rate of medication-related hospitalizations, the intervention generated an estimated savings of $6.6 million per year in avoided hospitalizations.
There are two major takeaways, said Dr. Steinman, who is based in the division of geriatrics at the University of California, San Francisco: It’s critical to focus on transitions and coordination between inpatient and outpatient care to address medication-related problems, and pharmacists can be extremely helpful in that.
“Decisions about drug therapy in the hospital may seem reasonable in the short term but often won’t stick in the long term unless there is a coordinated care that can help ensure appropriate follow-through once patients return home,” Dr. Steinman said. “The study that the editorial references is a systems intervention that hospitalists can advocate for in their own institutions, but in the immediate day-to-day, trying to ensure solid coordination of medication management from the inpatient to outpatient setting is likely to be very helpful for their patients.”
The long-term outcomes of hospitalized patients are largely influenced by getting them set up with appropriate community resources and supports once they leave the hospital, he added, and the hospital can play a critical role in putting these pieces into place.
Reference
1. Steinman MA. Reducing hospital admissions for adverse drug events through coordinated pharmacist care: learning from Hawai’i without a field trip. BMJ Qual Saf. Epub 2018 Nov 24. doi: 10.1136/bmjqs-2018-008815. Accessed Dec. 11, 2018.
Bringing QI training to an IM residency program
Consider a formal step-wise curriculum
For current and future hospitalists, there’s no doubt that knowledge of quality improvement (QI) fundamentals is an important component of a successful practice. One physician team set out to provide their trainees with that QI foundation and described the results.
“We believed that implementing a formal step-wise QI curriculum would not only meet the Accreditation Council of Graduate Medical Education (ACGME) requirements, but also increase residents’ knowledge of QI fundamentals and ultimately establish a culture of continuous improvement aiming to provide high-value care to our health care consumers,” said lead author J. Colt Cowdell, MD, MBA, of Mayo Clinic in Jacksonville, Fla.
Prior to any interventions, the team surveyed internal medicine residents regarding three unique patient scenarios and scored their answers. Residents were then assigned to one of five unique QI projects for the academic year in combination with a structured didactic QI curriculum.
After the structured progressive curriculum, in combination with team-based QI projects, residents were surveyed again. Results showed not only increased QI knowledge, but also improved patient safety and reduced waste.
“Keys to successful implementation included a thorough explanation of the need for this curriculum to the learners and ensuring that QI teams were multidisciplinary – residents, QI experts, nurses, techs, pharmacy, administrators, etc.,” said Dr. Cowdell.
For hospitalists in an academic setting, this work can provide a framework to incorporate QI into their residency programs. “I hope, if they have a passion for QI, they would seek out opportunities to mentor residents and help lead multidisciplinary team-based projects,” Dr. Cowdell said.
Reference
1. Cowdell, JC; Trautman, C; Lewis, M; Dawson, N. Integration of a Novel Quality Improvement Curriculum into an Internal Medicine Residency Program. Abstract published at Hospital Medicine 2018; April 8-11; Orlando, Fla. Abstract 54. https://www.shmabstracts.com/abstract/integration-of-a-novel-quality-improvement-curriculum-into-an-internal-medicine-residency-program/. Accessed Dec. 11, 2018.
Consider a formal step-wise curriculum
Consider a formal step-wise curriculum
For current and future hospitalists, there’s no doubt that knowledge of quality improvement (QI) fundamentals is an important component of a successful practice. One physician team set out to provide their trainees with that QI foundation and described the results.
“We believed that implementing a formal step-wise QI curriculum would not only meet the Accreditation Council of Graduate Medical Education (ACGME) requirements, but also increase residents’ knowledge of QI fundamentals and ultimately establish a culture of continuous improvement aiming to provide high-value care to our health care consumers,” said lead author J. Colt Cowdell, MD, MBA, of Mayo Clinic in Jacksonville, Fla.
Prior to any interventions, the team surveyed internal medicine residents regarding three unique patient scenarios and scored their answers. Residents were then assigned to one of five unique QI projects for the academic year in combination with a structured didactic QI curriculum.
After the structured progressive curriculum, in combination with team-based QI projects, residents were surveyed again. Results showed not only increased QI knowledge, but also improved patient safety and reduced waste.
“Keys to successful implementation included a thorough explanation of the need for this curriculum to the learners and ensuring that QI teams were multidisciplinary – residents, QI experts, nurses, techs, pharmacy, administrators, etc.,” said Dr. Cowdell.
For hospitalists in an academic setting, this work can provide a framework to incorporate QI into their residency programs. “I hope, if they have a passion for QI, they would seek out opportunities to mentor residents and help lead multidisciplinary team-based projects,” Dr. Cowdell said.
Reference
1. Cowdell, JC; Trautman, C; Lewis, M; Dawson, N. Integration of a Novel Quality Improvement Curriculum into an Internal Medicine Residency Program. Abstract published at Hospital Medicine 2018; April 8-11; Orlando, Fla. Abstract 54. https://www.shmabstracts.com/abstract/integration-of-a-novel-quality-improvement-curriculum-into-an-internal-medicine-residency-program/. Accessed Dec. 11, 2018.
For current and future hospitalists, there’s no doubt that knowledge of quality improvement (QI) fundamentals is an important component of a successful practice. One physician team set out to provide their trainees with that QI foundation and described the results.
“We believed that implementing a formal step-wise QI curriculum would not only meet the Accreditation Council of Graduate Medical Education (ACGME) requirements, but also increase residents’ knowledge of QI fundamentals and ultimately establish a culture of continuous improvement aiming to provide high-value care to our health care consumers,” said lead author J. Colt Cowdell, MD, MBA, of Mayo Clinic in Jacksonville, Fla.
Prior to any interventions, the team surveyed internal medicine residents regarding three unique patient scenarios and scored their answers. Residents were then assigned to one of five unique QI projects for the academic year in combination with a structured didactic QI curriculum.
After the structured progressive curriculum, in combination with team-based QI projects, residents were surveyed again. Results showed not only increased QI knowledge, but also improved patient safety and reduced waste.
“Keys to successful implementation included a thorough explanation of the need for this curriculum to the learners and ensuring that QI teams were multidisciplinary – residents, QI experts, nurses, techs, pharmacy, administrators, etc.,” said Dr. Cowdell.
For hospitalists in an academic setting, this work can provide a framework to incorporate QI into their residency programs. “I hope, if they have a passion for QI, they would seek out opportunities to mentor residents and help lead multidisciplinary team-based projects,” Dr. Cowdell said.
Reference
1. Cowdell, JC; Trautman, C; Lewis, M; Dawson, N. Integration of a Novel Quality Improvement Curriculum into an Internal Medicine Residency Program. Abstract published at Hospital Medicine 2018; April 8-11; Orlando, Fla. Abstract 54. https://www.shmabstracts.com/abstract/integration-of-a-novel-quality-improvement-curriculum-into-an-internal-medicine-residency-program/. Accessed Dec. 11, 2018.
Following the path of leadership
VA Hospitalist Dr. Matthew Tuck
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
VA Hospitalist Dr. Matthew Tuck
VA Hospitalist Dr. Matthew Tuck
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
For Matthew Tuck, MD, MEd, FACP, associate section chief for hospital medicine at the Veterans Affairs Medical Center (VAMC) in Washington, leadership is something that hospitalists can and should be learning at every opportunity.
Some of the best insights about effective leadership, teamwork, and process improvement come from the business world and have been slower to infiltrate into hospital settings and hospitalist groups, he says. But Dr. Tuck has tried to take advantage of numerous opportunities for leadership development in his own career.
He has been a hospitalist since 2010 and is part of a group of 13 physicians, all of whom carry clinical, teaching, and research responsibilities while pursuing a variety of education, quality improvement, and performance improvement topics.
“My chair has been generous about giving me time to do teaching and research and to pursue opportunities for career development,” he said. The Washington VAMC works with four affiliate medical schools in the area, and its six daily hospital medicine services are all 100% teaching services with assigned residents and interns.
Dr. Tuck divides his professional time roughly one-third each between clinical – seeing patients 5 months a year on a consultative or inpatient basis with resident teams; administrative in a variety of roles; and research. He has academic appointments at the George Washington University (GWU) School of Medicine and at the Uniformed Services University of Health Sciences in Bethesda, Md. He developed the coursework for teaching evidence-based medicine to first- and second-year medical students at GWU.
He is also part of a large research consortium with five sites and $7.5 million in funding over 5 years from NIH’s National Institute on Minority Health and Health Disparities to study how genetic information from African American patients can predict their response to cardiovascular medications. He serves as the study’s site Principal Investigator at the VAMC.
Opportunities to advance his leadership skills have included the VA’s Aspiring Leaders Program and Leadership Development Mentoring Program, which teach leadership skills on topical subjects such as teaching, communications skills, and finance. The Master Teacher Leadership Development Program for medical faculty at GWU, where he attended medical school and did his internship and residency, offers six intensive, classroom-based 8-week courses over a 1-year period. They cover various topical subjects with faculty from the business world teaching principles of leadership. The program includes a mentoring action plan for participants and leads to a graduate certificate in leadership development from GWU’s Graduate School of Education and Human Development at the end of the year’s studies.
Dr. Tuck credits completing this kind of coursework for his current position of leadership in the VA and he tries to share what he has learned with the medical students he teaches.
“When I was starting out as a physician, I never received training in how to lead a team. I found myself trying to get everything done for my patients while teaching my learners, and I really struggled for the first couple of years to manage these competing demands on my time,” he said.
Now, on the first day of a new clinical rotation, he meets one-on-one with his residents to set out goals and expectations. “I say: ‘This is how I want rounds to be run. What are your expectations?’ That way we make sure we’re collaborating as a team. I don’t know that medical school prepares you for this kind of teamwork. Unless you bring a background in business, you can really struggle.”
Interest in hospital medicine
“Throughout our medical training we do a variety of rotations and clerkships. I found myself falling in love with all of them – surgery, psychiatry, obstetrics, and gynecology,” Dr. Tuck explained, as he reflected on how he ended up in hospital medicine. “As someone who was interested in all of these different fields of medicine, I considered myself a true medical generalist. And in hospitalized patients, who struggle with all of the different issues that bring them to the hospital, I saw a compilation of all my experiences in residency training combined in one setting.”
Hospital medicine was a relatively young field at that time, with few academic hospitalists, he said. “But I had good mentors who encouraged me to pursue my educational, research, and administrative interests. My affinity for the VA was also largely due to my training. We worked in multiple settings – academic, community-based, National Institutes of Health, and at the VA.”
Dr. Tuck said that, of all the settings in which he practiced, he felt the VA truly trained him best to be a doctor. “The experience made me feel like a holistic practitioner,” he said. “The system allowed me to take the best care of my patients, since I didn’t have to worry about whether I could make needed referrals to specialists. Very early in my internship year we were seeing very sick patients with multiple comorbidities, but it was easy to get a social worker or case manager involved, compared to other settings, which can be more difficult to navigate.”
While the VA is a “great health system,” Dr. Tuck said, the challenge is learning how to work with its bureaucracy. “If you don’t know how the system works, it can seem to get in your way.” But overall, he said, the VA functions well and compares favorably with private sector hospitals and health systems. That was also the conclusion of a recent study in the Journal of General Internal Medicine, which compared the quality of outpatient and inpatient care in VA and non-VA settings using recent performance measure data.1 The authors concluded that the VA system performed similarly or better than non-VA health care on most nationally recognized measures of inpatient and outpatient care quality, although there is wide variation between VA facilities.
Working with the team
Another major interest for Dr. Tuck is team-based learning, which also grew out of his GWU leadership certificate course work on teaching teams and team development. He is working on a draft paper for publication with coauthor Patrick Rendon, MD, associate program director for the University of New Mexico’s internal medicine residency program, building on the group development stage theory – “Forming/Storming/Norming/Performing” – developed by Tuckman and Jenson.2
The theory offers 12 tips for optimizing inpatient ward team performance, such as getting the learners to buy in at an early stage of a project. “Everyone I talk to about our research is eager to learn how to apply these principles. I don’t think we’re unique at this center. We’re constantly rotating learners through the program. If you apply these principles, you can get learners to be more efficient starting from the first day,” he said.
The current inpatient team model at the Washington VAMC involves a broadly representative team from nursing, case management, social work, the business office, medical coding, utilization management, and administration that convenes every morning to discuss patient navigation and difficult discharges. “Everyone sits around a big table, and the six hospital medicine teams rotate through every fifteen minutes to review their patients’ admitting diagnoses, barriers to discharge and plans of care.”
At the patient’s bedside, a Focused Interdisciplinary Team (FIT) model, which Dr. Tuck helped to implement, incorporates a four-step process with clearly defined roles for the attending, nurse, pharmacist, and case manager or social worker. “Since implementation, our data show overall reductions in lengths of stay,” he said.
Dr. Tuck urges other hospitalists to pursue opportunities available to them to develop their leadership skills. “Look to your professional societies such as the Society of General Internal Medicine (SGIM) or SHM.” For example, SGIM’s Academic Hospitalist Commission, which he cochairs, provides a voice on the national stage for academic hospitalists and cosponsors with SHM an annual Academic Hospitalist Academy to support career development for junior academic hospitalists as educational leaders. Since 2016, its Distinguished Professor of Hospital Medicine recognizes a professor of hospital medicine to give a plenary address at the SGIM national meeting.
SGIM’s SCHOLAR Project, a subgroup of its Academic Hospitalist Commission, has worked to identify features of successful academic hospitalist programs, with the results published in the Journal of Hospital Medicine.3
“We learned that what sets successful programs apart is their leadership – as well as protected time for scholarly pursuits,” he said. “We’re all leaders in this field, whether we view ourselves that way or not.”
References
1. Price RA et al. Comparing quality of care in Veterans Affairs and Non–Veterans Affairs settings. J Gen Intern Med. 2018 Oct;33(10):1631-38.
2. Tuckman B, Jensen M. Stages of small group development revisited. Group and Organizational Studies. 1977;2:419-427.
3. Seymann GB et al. Features of successful academic hospitalist programs: Insights from the SCHOLAR (Successful hospitalists in academics and research) project. J Hosp Med. 2016 Oct;11(10):708-13.
HM19: Things we do for no reason
The pediatric version
Presenters
Amit K. Pahwa, MD, FAAP; Nicola Orlov, MD, MPH, FAAP
Workshop title
Things we do for no reason (pediatrics)
Session summary
As he began by stating the Institute of Medicine definition of high-value care (HVC), Amit K. Pahwa, MD, of Johns Hopkins Medicine, Baltimore, described HVC as the best care for the patient, with the optimal result for the circumstances, at the right price. But few pediatric residency programs provide education regarding HVC, with only 11% providing a formal HVC curriculum, as found by a survey of pediatric program directors and chief residents in a study published in 2017.
Dr. Pahwa then provided examples of cases in which HVC could be optimized, including reducing rebound bilirubin levels in neonatal hyperbilirubinemia, giving nasogastric feeds instead of IV hydration in bronchiolitis, reducing unnecessary vital sign checks, and providing apple juice supplemented with liquids of choice instead of more expensive oral electrolyte solutions.
Nicola Orlov, MD, of the University of Chicago presented another illustrative case which highlighted the need to reduce vital sign frequency when appropriate. This was linked to her work at Comer Children’s Hospital on reducing nighttime sleep disruptions in hospitalized children, as part of the SIESTA (Sleep for Inpatients: Empowering Staff to Act) study. This led to a significant reduction in nurse/physician interruptions during the study period.
Key takeaways for HM
- High-value care (HVC) is a key focus of systems improvement in the field of pediatric hospital medicine.
- Educational efforts for all levels of learners is inadequate currently, and needs to be augmented.
- Quality improvement projects to promote HVC can lead not only to reduced costs, but improved quality and patient experience.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
The pediatric version
The pediatric version
Presenters
Amit K. Pahwa, MD, FAAP; Nicola Orlov, MD, MPH, FAAP
Workshop title
Things we do for no reason (pediatrics)
Session summary
As he began by stating the Institute of Medicine definition of high-value care (HVC), Amit K. Pahwa, MD, of Johns Hopkins Medicine, Baltimore, described HVC as the best care for the patient, with the optimal result for the circumstances, at the right price. But few pediatric residency programs provide education regarding HVC, with only 11% providing a formal HVC curriculum, as found by a survey of pediatric program directors and chief residents in a study published in 2017.
Dr. Pahwa then provided examples of cases in which HVC could be optimized, including reducing rebound bilirubin levels in neonatal hyperbilirubinemia, giving nasogastric feeds instead of IV hydration in bronchiolitis, reducing unnecessary vital sign checks, and providing apple juice supplemented with liquids of choice instead of more expensive oral electrolyte solutions.
Nicola Orlov, MD, of the University of Chicago presented another illustrative case which highlighted the need to reduce vital sign frequency when appropriate. This was linked to her work at Comer Children’s Hospital on reducing nighttime sleep disruptions in hospitalized children, as part of the SIESTA (Sleep for Inpatients: Empowering Staff to Act) study. This led to a significant reduction in nurse/physician interruptions during the study period.
Key takeaways for HM
- High-value care (HVC) is a key focus of systems improvement in the field of pediatric hospital medicine.
- Educational efforts for all levels of learners is inadequate currently, and needs to be augmented.
- Quality improvement projects to promote HVC can lead not only to reduced costs, but improved quality and patient experience.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
Presenters
Amit K. Pahwa, MD, FAAP; Nicola Orlov, MD, MPH, FAAP
Workshop title
Things we do for no reason (pediatrics)
Session summary
As he began by stating the Institute of Medicine definition of high-value care (HVC), Amit K. Pahwa, MD, of Johns Hopkins Medicine, Baltimore, described HVC as the best care for the patient, with the optimal result for the circumstances, at the right price. But few pediatric residency programs provide education regarding HVC, with only 11% providing a formal HVC curriculum, as found by a survey of pediatric program directors and chief residents in a study published in 2017.
Dr. Pahwa then provided examples of cases in which HVC could be optimized, including reducing rebound bilirubin levels in neonatal hyperbilirubinemia, giving nasogastric feeds instead of IV hydration in bronchiolitis, reducing unnecessary vital sign checks, and providing apple juice supplemented with liquids of choice instead of more expensive oral electrolyte solutions.
Nicola Orlov, MD, of the University of Chicago presented another illustrative case which highlighted the need to reduce vital sign frequency when appropriate. This was linked to her work at Comer Children’s Hospital on reducing nighttime sleep disruptions in hospitalized children, as part of the SIESTA (Sleep for Inpatients: Empowering Staff to Act) study. This led to a significant reduction in nurse/physician interruptions during the study period.
Key takeaways for HM
- High-value care (HVC) is a key focus of systems improvement in the field of pediatric hospital medicine.
- Educational efforts for all levels of learners is inadequate currently, and needs to be augmented.
- Quality improvement projects to promote HVC can lead not only to reduced costs, but improved quality and patient experience.
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
Lower rates of patient satisfaction may predict readmission
Clinical question: Do higher rates of patient satisfaction lead to lower rates of hospital readmission?
Background: Readmissions account for 32.1% of total health care expenditures in the United States, of which 15%-20% are considered potentially preventable. Multiple studies have examined a variety of possible indicators of readmission, but rarely has patient perspective prior to discharge been examined.
Study design: Thematic interview and questionnaire.
Setting: Two inpatient medical units at Massachusetts General Hospital, Boston.
Synopsis: 846 patients were enrolled during their index admission with 201 of these patients being readmitted within 30 days of discharge. During the index admission, the patients completed a questionnaire developed by the authors and underwent a formal, thematic interview with identification of core domains performed by trained research coordinators. The primary outcome was 30-day readmission. Readmitted patients were less likely to have reported being “very satisfied” with their overall care (67.7% vs. 76.4%; P = .045) and were less likely to have reported that physicians “always listened” to them (65.7% vs. 73.2%; P = .048). Interestingly, if health care providers discussed the possible need for help after hospital stay, the patient had an increased risk of readmission (adjusted odds ratio, 1.56; 95% confidence interval, 1.02-2.39; P = .04) and patients who predicted they were “very likely” to require readmission were not more likely to be readmitted (aOR, 1.35; 95% CI, 0.83-2.19; P = .22). The major limitations of this study are that researchers interviewed only English-speaking patients who were able to participate in an in-depth interview and survey, perhaps resulting in a healthier-patient bias, as well as an inability to capture hospital admission at other institutions. Additionally, these patients are drawn from a tertiary-care service designed to care for medically complex cases and may not be generalizable to larger populations.
Bottom line: Lower rates of 30-day hospital readmission were associated with higher rates of patient satisfaction and a higher level of patient perception that providers were listening to them.
Citation: Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 2018 Sep;27:683-90.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
Clinical question: Do higher rates of patient satisfaction lead to lower rates of hospital readmission?
Background: Readmissions account for 32.1% of total health care expenditures in the United States, of which 15%-20% are considered potentially preventable. Multiple studies have examined a variety of possible indicators of readmission, but rarely has patient perspective prior to discharge been examined.
Study design: Thematic interview and questionnaire.
Setting: Two inpatient medical units at Massachusetts General Hospital, Boston.
Synopsis: 846 patients were enrolled during their index admission with 201 of these patients being readmitted within 30 days of discharge. During the index admission, the patients completed a questionnaire developed by the authors and underwent a formal, thematic interview with identification of core domains performed by trained research coordinators. The primary outcome was 30-day readmission. Readmitted patients were less likely to have reported being “very satisfied” with their overall care (67.7% vs. 76.4%; P = .045) and were less likely to have reported that physicians “always listened” to them (65.7% vs. 73.2%; P = .048). Interestingly, if health care providers discussed the possible need for help after hospital stay, the patient had an increased risk of readmission (adjusted odds ratio, 1.56; 95% confidence interval, 1.02-2.39; P = .04) and patients who predicted they were “very likely” to require readmission were not more likely to be readmitted (aOR, 1.35; 95% CI, 0.83-2.19; P = .22). The major limitations of this study are that researchers interviewed only English-speaking patients who were able to participate in an in-depth interview and survey, perhaps resulting in a healthier-patient bias, as well as an inability to capture hospital admission at other institutions. Additionally, these patients are drawn from a tertiary-care service designed to care for medically complex cases and may not be generalizable to larger populations.
Bottom line: Lower rates of 30-day hospital readmission were associated with higher rates of patient satisfaction and a higher level of patient perception that providers were listening to them.
Citation: Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 2018 Sep;27:683-90.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
Clinical question: Do higher rates of patient satisfaction lead to lower rates of hospital readmission?
Background: Readmissions account for 32.1% of total health care expenditures in the United States, of which 15%-20% are considered potentially preventable. Multiple studies have examined a variety of possible indicators of readmission, but rarely has patient perspective prior to discharge been examined.
Study design: Thematic interview and questionnaire.
Setting: Two inpatient medical units at Massachusetts General Hospital, Boston.
Synopsis: 846 patients were enrolled during their index admission with 201 of these patients being readmitted within 30 days of discharge. During the index admission, the patients completed a questionnaire developed by the authors and underwent a formal, thematic interview with identification of core domains performed by trained research coordinators. The primary outcome was 30-day readmission. Readmitted patients were less likely to have reported being “very satisfied” with their overall care (67.7% vs. 76.4%; P = .045) and were less likely to have reported that physicians “always listened” to them (65.7% vs. 73.2%; P = .048). Interestingly, if health care providers discussed the possible need for help after hospital stay, the patient had an increased risk of readmission (adjusted odds ratio, 1.56; 95% confidence interval, 1.02-2.39; P = .04) and patients who predicted they were “very likely” to require readmission were not more likely to be readmitted (aOR, 1.35; 95% CI, 0.83-2.19; P = .22). The major limitations of this study are that researchers interviewed only English-speaking patients who were able to participate in an in-depth interview and survey, perhaps resulting in a healthier-patient bias, as well as an inability to capture hospital admission at other institutions. Additionally, these patients are drawn from a tertiary-care service designed to care for medically complex cases and may not be generalizable to larger populations.
Bottom line: Lower rates of 30-day hospital readmission were associated with higher rates of patient satisfaction and a higher level of patient perception that providers were listening to them.
Citation: Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 2018 Sep;27:683-90.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
Culture: An unseen force in the hospital workplace
Parallels from the airline industry
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.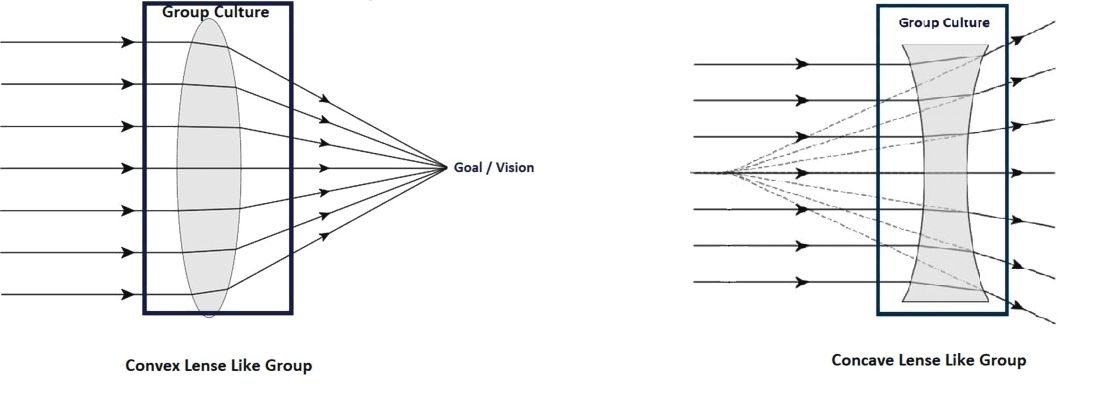
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.
Parallels from the airline industry
Parallels from the airline industry
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.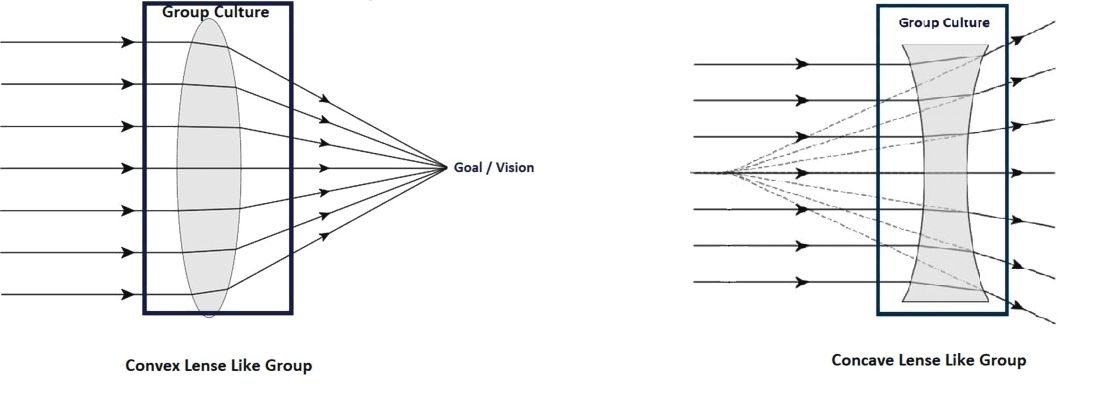
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.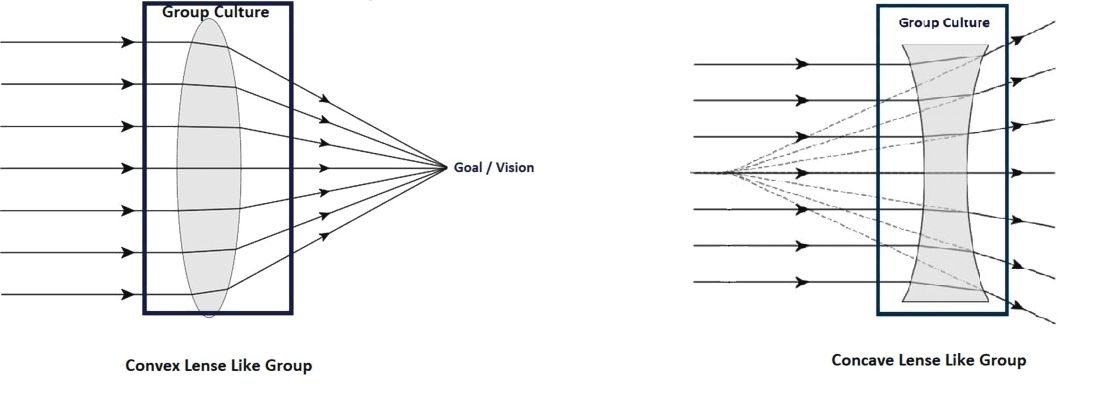
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.