User login
2016 Humanitarian Award
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
Everything We Say & Do: What PFACs reveal about patient experience
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable tactics that have great potential to positively impact patients’ experience of care.
Patient and Family Advisory Councils (PFACs) provide a tool for understanding the patient perspective and are utilized nationwide. These councils, typically consisting of former and current patients and/or their family members, meet on a regular basis to advise provider communities on a wide range of care-related matters. At my institution, Beth Israel Deaconess Medical Center, our PFAC has weighed in on a wide range of issues, such as how to conduct effective nursing rounds and the best methods for supporting patients with disabilities.
Most recently, we have utilized an innovative approach to both understanding the patient experience and capitalizing on the expertise of our PFAC members. Modeled after a program developed at the Dartmouth-Hitchcock Medical Center, we have trained members of our PFAC to interview inpatients at the bedside about their experience. Time-sensitive information is immediately reported back to the nurse manager, who responds with real-time solutions. Oftentimes, problems can be easily resolved using the right communication, or just providing the “listening ear” of someone to whom the patient relates.
In addition, the information is aggregated to provide us with a broad-based perspective of the patient experience at BIDMC. For example, we found that our patients often discuss issues with volunteers that they have not addressed with providers, suggesting they may at times feel more comfortable disclosing concerns to people outside of their medical team.
The Society of Hospital Medicine (SHM) also recognizes the central role of the patient’s voice in quality medical care. Through the work of its Patient Experience Committee, SHM has convened a nationwide “virtual” PFAC consisting of leaders of PFACs from medical facilities across the country. Members of the SHM PFAC share questions posed by SHM’s committees with their constituents, and the responses are reported back to the Patient Experience Committee.
What lessons have we learned from the SHM PFAC? Make no assumptions. While some of us have been patients ourselves and all of us interact with patients, our ability to understand the patient perspective is blurred by the lenses of medical training, system constraints, and the pressures of the challenging work that we do.
It is often impossible to predict the response when you question a patient about his or her experience. For example, the first question we asked SHM’s nationwide PFAC was: “What is one thing that a hospitalist could do to improve the patient experience?” The most common response we received was: “What is a hospitalist?” These responses suggest that we (hospitalists) need to redirect our efforts in a way that we had not anticipated, with a focus on clarifying who we are and what we do.
Other, more predictable themes emerged as well. Our patients want consistency and continuity throughout their hospitalization. They value a good bedside manner and want us to engage in sensitivity training. They ask us to work on minimizing errors and ensuring accountability both during hospitalization as well as pre- and post hospitalization.
Ultimately we hope that the SHM PFAC will be utilized by all of SHM’s committees, allowing for the patient experience to be a common thread woven through all SHM initiatives.
Amber Moore, MD, MPH, is a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School.
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable tactics that have great potential to positively impact patients’ experience of care.
Patient and Family Advisory Councils (PFACs) provide a tool for understanding the patient perspective and are utilized nationwide. These councils, typically consisting of former and current patients and/or their family members, meet on a regular basis to advise provider communities on a wide range of care-related matters. At my institution, Beth Israel Deaconess Medical Center, our PFAC has weighed in on a wide range of issues, such as how to conduct effective nursing rounds and the best methods for supporting patients with disabilities.
Most recently, we have utilized an innovative approach to both understanding the patient experience and capitalizing on the expertise of our PFAC members. Modeled after a program developed at the Dartmouth-Hitchcock Medical Center, we have trained members of our PFAC to interview inpatients at the bedside about their experience. Time-sensitive information is immediately reported back to the nurse manager, who responds with real-time solutions. Oftentimes, problems can be easily resolved using the right communication, or just providing the “listening ear” of someone to whom the patient relates.
In addition, the information is aggregated to provide us with a broad-based perspective of the patient experience at BIDMC. For example, we found that our patients often discuss issues with volunteers that they have not addressed with providers, suggesting they may at times feel more comfortable disclosing concerns to people outside of their medical team.
The Society of Hospital Medicine (SHM) also recognizes the central role of the patient’s voice in quality medical care. Through the work of its Patient Experience Committee, SHM has convened a nationwide “virtual” PFAC consisting of leaders of PFACs from medical facilities across the country. Members of the SHM PFAC share questions posed by SHM’s committees with their constituents, and the responses are reported back to the Patient Experience Committee.
What lessons have we learned from the SHM PFAC? Make no assumptions. While some of us have been patients ourselves and all of us interact with patients, our ability to understand the patient perspective is blurred by the lenses of medical training, system constraints, and the pressures of the challenging work that we do.
It is often impossible to predict the response when you question a patient about his or her experience. For example, the first question we asked SHM’s nationwide PFAC was: “What is one thing that a hospitalist could do to improve the patient experience?” The most common response we received was: “What is a hospitalist?” These responses suggest that we (hospitalists) need to redirect our efforts in a way that we had not anticipated, with a focus on clarifying who we are and what we do.
Other, more predictable themes emerged as well. Our patients want consistency and continuity throughout their hospitalization. They value a good bedside manner and want us to engage in sensitivity training. They ask us to work on minimizing errors and ensuring accountability both during hospitalization as well as pre- and post hospitalization.
Ultimately we hope that the SHM PFAC will be utilized by all of SHM’s committees, allowing for the patient experience to be a common thread woven through all SHM initiatives.
Amber Moore, MD, MPH, is a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School.
Editor’s note: “Everything We Say and Do” is an informational series developed by the Society of Hospital Medicine’s Patient Experience Committee to provide readers with thoughtful and actionable tactics that have great potential to positively impact patients’ experience of care.
Patient and Family Advisory Councils (PFACs) provide a tool for understanding the patient perspective and are utilized nationwide. These councils, typically consisting of former and current patients and/or their family members, meet on a regular basis to advise provider communities on a wide range of care-related matters. At my institution, Beth Israel Deaconess Medical Center, our PFAC has weighed in on a wide range of issues, such as how to conduct effective nursing rounds and the best methods for supporting patients with disabilities.
Most recently, we have utilized an innovative approach to both understanding the patient experience and capitalizing on the expertise of our PFAC members. Modeled after a program developed at the Dartmouth-Hitchcock Medical Center, we have trained members of our PFAC to interview inpatients at the bedside about their experience. Time-sensitive information is immediately reported back to the nurse manager, who responds with real-time solutions. Oftentimes, problems can be easily resolved using the right communication, or just providing the “listening ear” of someone to whom the patient relates.
In addition, the information is aggregated to provide us with a broad-based perspective of the patient experience at BIDMC. For example, we found that our patients often discuss issues with volunteers that they have not addressed with providers, suggesting they may at times feel more comfortable disclosing concerns to people outside of their medical team.
The Society of Hospital Medicine (SHM) also recognizes the central role of the patient’s voice in quality medical care. Through the work of its Patient Experience Committee, SHM has convened a nationwide “virtual” PFAC consisting of leaders of PFACs from medical facilities across the country. Members of the SHM PFAC share questions posed by SHM’s committees with their constituents, and the responses are reported back to the Patient Experience Committee.
What lessons have we learned from the SHM PFAC? Make no assumptions. While some of us have been patients ourselves and all of us interact with patients, our ability to understand the patient perspective is blurred by the lenses of medical training, system constraints, and the pressures of the challenging work that we do.
It is often impossible to predict the response when you question a patient about his or her experience. For example, the first question we asked SHM’s nationwide PFAC was: “What is one thing that a hospitalist could do to improve the patient experience?” The most common response we received was: “What is a hospitalist?” These responses suggest that we (hospitalists) need to redirect our efforts in a way that we had not anticipated, with a focus on clarifying who we are and what we do.
Other, more predictable themes emerged as well. Our patients want consistency and continuity throughout their hospitalization. They value a good bedside manner and want us to engage in sensitivity training. They ask us to work on minimizing errors and ensuring accountability both during hospitalization as well as pre- and post hospitalization.
Ultimately we hope that the SHM PFAC will be utilized by all of SHM’s committees, allowing for the patient experience to be a common thread woven through all SHM initiatives.
Amber Moore, MD, MPH, is a hospitalist at Beth Israel Deaconess Medical Center, and instructor of medicine, Harvard Medical School.
Hospitalists trained in family medicine seek critical care training pathway
A nationwide shortage of intensivists has more hospitalists stepping into the critical care arena, but not all with the level of preparation and comfort of David Aymond, MD, a Louisiana-based hospitalist trained in family medicine (HTFM).
Dr. Aymond gained his ICU experience in a fellowship with the University of Alabama, where hospitalists also “were responsible for ICU patients,” he said. Years later, as an employee of both small and large hospitals with busy ICU services, and a faculty member for a family medicine residency with a busy ICU, Dr. Aymond moves seamlessly between roles.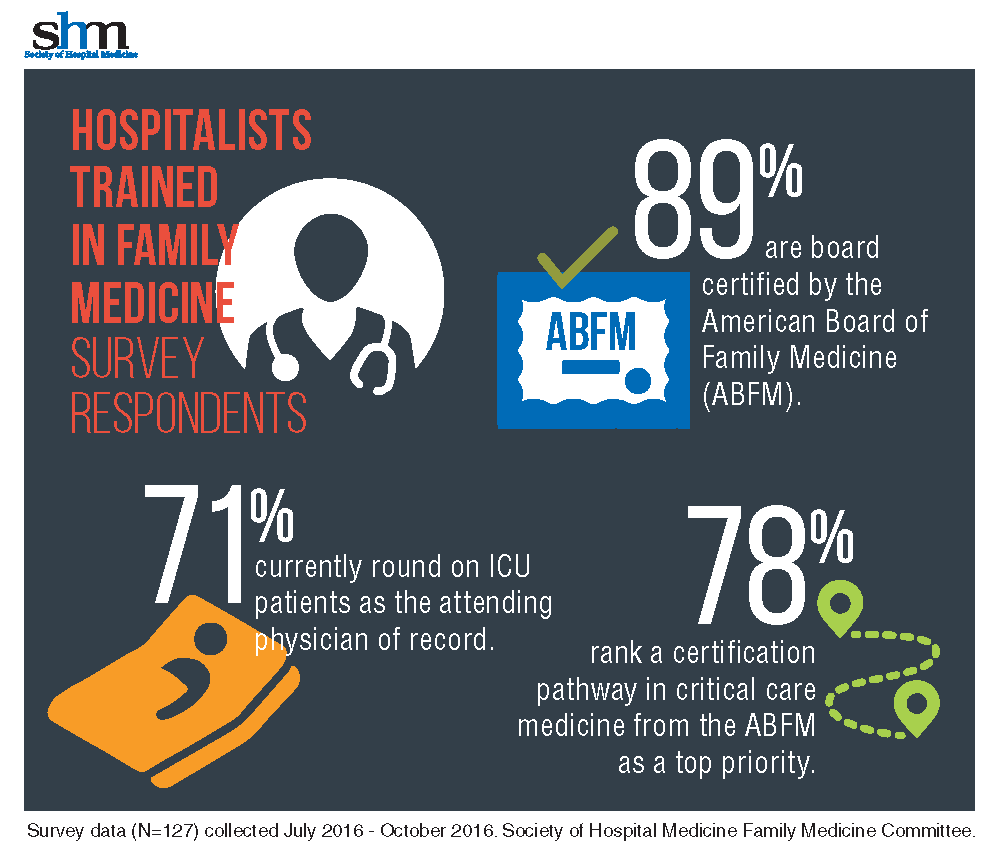
“It was eye-opening to learn how many [HTFM] are not only caring for patients in the ICU, but also are requesting additional training,” said Dr. Aymond, a member of the SHM Family Medicine Committee. “A critical care pathway would provide them with a level of expertise already available to physicians in internal medicine, emergency medicine, and surgery.”
With 71% of HTFM reporting that they round on ICU as the attending physician, the strong endorsement (78%) for critical care certification is not surprising.
“I am currently practicing as a full time intensivist and take consults from other providers, yet I only have a certificate from fellowship, no formal board certification in critical care,” noted a survey respondent.
Other participants stated, “it makes perfect sense to have a pathway to critical care if both family medicine and internal medicine coexist as hospitalists,” that certification is “imperative at rural and underserved hospitals,” and also “helpful for those …who work in larger hospitals and take care of critically ill patients.” More than half of those surveyed want the Family Medicine Committee to work with ABFM to create the pathway.
The majority (87%) of the HTFM survey respondents are certified by the ABFM, and 8% have attained Recognition of Focused Practice in Hospital Medicine. Common pathways for additional credentialing include SHM’s Fellow of Hospital Medicine program (38%), a fellowship in hospital medicine (19%), and certification in hospice and palliative care (15%). More than 38% reported “other qualifications,” such as years of work experience, certification by the American Osteopathic Board of Family Physicians, and prior training in internal medicine.
The survey also found that certification differences in internal medicine and family medicine hospitalists, which may have posed employment obstacles in the past for HTFM, are not as much of an issue.
“The critical care pathway is the bigger concern,” Dr. Aymond said.
SHM’s Family Medicine Committee will be working on a proposal to ABFM to create the training pathway in the coming months. Dr. Aymond wants intensivists to know that this not an attempt to encroach on their professional domain, “but an opportunity to fill the existing professional gap.
Family medicine physicians are already providing critical care services, so a pathway to obtain formal training makes sense,” he adds. “If a family medicine doc completes the fellowship and takes it back to a residency program [the residents] will be more prepared for their potential careers in hospital and ICU medicine and much more comfortable with high-acuity patients.”
Claudia Stahl is SHM’s content manager.
A nationwide shortage of intensivists has more hospitalists stepping into the critical care arena, but not all with the level of preparation and comfort of David Aymond, MD, a Louisiana-based hospitalist trained in family medicine (HTFM).
Dr. Aymond gained his ICU experience in a fellowship with the University of Alabama, where hospitalists also “were responsible for ICU patients,” he said. Years later, as an employee of both small and large hospitals with busy ICU services, and a faculty member for a family medicine residency with a busy ICU, Dr. Aymond moves seamlessly between roles.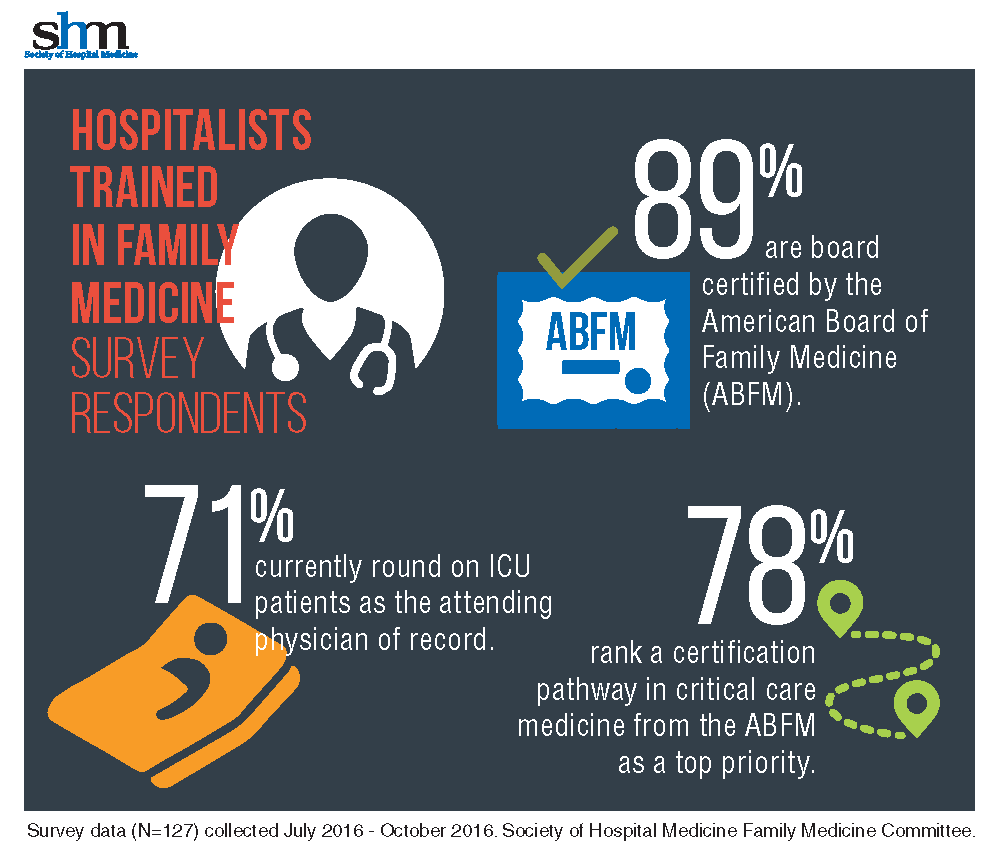
“It was eye-opening to learn how many [HTFM] are not only caring for patients in the ICU, but also are requesting additional training,” said Dr. Aymond, a member of the SHM Family Medicine Committee. “A critical care pathway would provide them with a level of expertise already available to physicians in internal medicine, emergency medicine, and surgery.”
With 71% of HTFM reporting that they round on ICU as the attending physician, the strong endorsement (78%) for critical care certification is not surprising.
“I am currently practicing as a full time intensivist and take consults from other providers, yet I only have a certificate from fellowship, no formal board certification in critical care,” noted a survey respondent.
Other participants stated, “it makes perfect sense to have a pathway to critical care if both family medicine and internal medicine coexist as hospitalists,” that certification is “imperative at rural and underserved hospitals,” and also “helpful for those …who work in larger hospitals and take care of critically ill patients.” More than half of those surveyed want the Family Medicine Committee to work with ABFM to create the pathway.
The majority (87%) of the HTFM survey respondents are certified by the ABFM, and 8% have attained Recognition of Focused Practice in Hospital Medicine. Common pathways for additional credentialing include SHM’s Fellow of Hospital Medicine program (38%), a fellowship in hospital medicine (19%), and certification in hospice and palliative care (15%). More than 38% reported “other qualifications,” such as years of work experience, certification by the American Osteopathic Board of Family Physicians, and prior training in internal medicine.
The survey also found that certification differences in internal medicine and family medicine hospitalists, which may have posed employment obstacles in the past for HTFM, are not as much of an issue.
“The critical care pathway is the bigger concern,” Dr. Aymond said.
SHM’s Family Medicine Committee will be working on a proposal to ABFM to create the training pathway in the coming months. Dr. Aymond wants intensivists to know that this not an attempt to encroach on their professional domain, “but an opportunity to fill the existing professional gap.
Family medicine physicians are already providing critical care services, so a pathway to obtain formal training makes sense,” he adds. “If a family medicine doc completes the fellowship and takes it back to a residency program [the residents] will be more prepared for their potential careers in hospital and ICU medicine and much more comfortable with high-acuity patients.”
Claudia Stahl is SHM’s content manager.
A nationwide shortage of intensivists has more hospitalists stepping into the critical care arena, but not all with the level of preparation and comfort of David Aymond, MD, a Louisiana-based hospitalist trained in family medicine (HTFM).
Dr. Aymond gained his ICU experience in a fellowship with the University of Alabama, where hospitalists also “were responsible for ICU patients,” he said. Years later, as an employee of both small and large hospitals with busy ICU services, and a faculty member for a family medicine residency with a busy ICU, Dr. Aymond moves seamlessly between roles.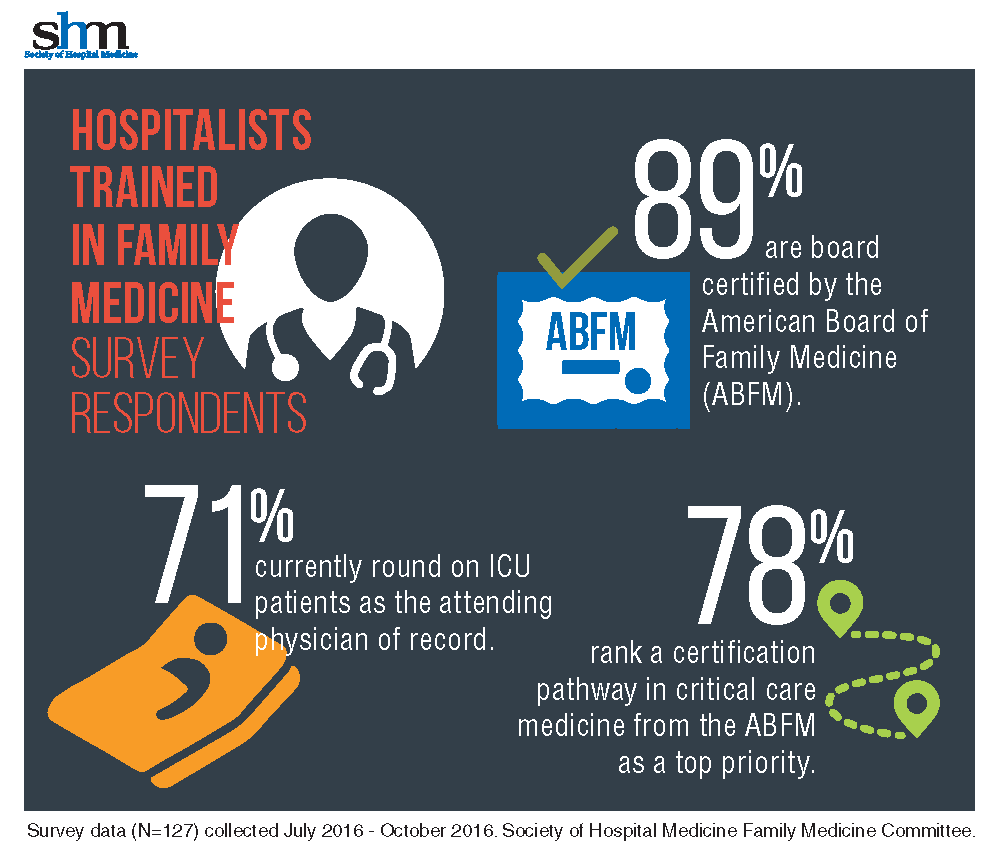
“It was eye-opening to learn how many [HTFM] are not only caring for patients in the ICU, but also are requesting additional training,” said Dr. Aymond, a member of the SHM Family Medicine Committee. “A critical care pathway would provide them with a level of expertise already available to physicians in internal medicine, emergency medicine, and surgery.”
With 71% of HTFM reporting that they round on ICU as the attending physician, the strong endorsement (78%) for critical care certification is not surprising.
“I am currently practicing as a full time intensivist and take consults from other providers, yet I only have a certificate from fellowship, no formal board certification in critical care,” noted a survey respondent.
Other participants stated, “it makes perfect sense to have a pathway to critical care if both family medicine and internal medicine coexist as hospitalists,” that certification is “imperative at rural and underserved hospitals,” and also “helpful for those …who work in larger hospitals and take care of critically ill patients.” More than half of those surveyed want the Family Medicine Committee to work with ABFM to create the pathway.
The majority (87%) of the HTFM survey respondents are certified by the ABFM, and 8% have attained Recognition of Focused Practice in Hospital Medicine. Common pathways for additional credentialing include SHM’s Fellow of Hospital Medicine program (38%), a fellowship in hospital medicine (19%), and certification in hospice and palliative care (15%). More than 38% reported “other qualifications,” such as years of work experience, certification by the American Osteopathic Board of Family Physicians, and prior training in internal medicine.
The survey also found that certification differences in internal medicine and family medicine hospitalists, which may have posed employment obstacles in the past for HTFM, are not as much of an issue.
“The critical care pathway is the bigger concern,” Dr. Aymond said.
SHM’s Family Medicine Committee will be working on a proposal to ABFM to create the training pathway in the coming months. Dr. Aymond wants intensivists to know that this not an attempt to encroach on their professional domain, “but an opportunity to fill the existing professional gap.
Family medicine physicians are already providing critical care services, so a pathway to obtain formal training makes sense,” he adds. “If a family medicine doc completes the fellowship and takes it back to a residency program [the residents] will be more prepared for their potential careers in hospital and ICU medicine and much more comfortable with high-acuity patients.”
Claudia Stahl is SHM’s content manager.
Sneak Peek: The Hospital Leader Blog
Editor’s note: This article first appeared on “The Hospital Leader” blog. Read the full post at hospitalleader.org.
In December, I wrote a letter to hospital executives, urging them to deliberately invest their own personal time and effort in fostering hospitalist well-being. I suggested several actions that leaders can take to enhance hospitalist job satisfaction and reduce the risk of burnout and turnover.
Following publication of that post, I heard from several hospital executives and was pleasantly surprised that they all responded positively to my message. Several execs told me that they gained valuable new insights about their hospitalists’ challenges and needs; others said they planned to take action on one or more of my suggestions that had never occurred to them before.
Their feedback reinforced my belief that most hospital leaders actually do care a lot about promoting healthy, stable, and sustainable hospitalist programs, but the hospital leaders I talked with also had some messages for their hospitalist colleagues, and I think it’s important to share them in the spirit of fostering a healthy exchange of perspectives. Your hospital’s leaders would be delighted and encouraged if you engaged them in dialogue about these issues.
Help us help you
Several hospital leaders told me that their hospitalists grumble about being treated by the medical staff (and even nurses) like second-class citizens or glorified residents. Those same hospitalists, however, routinely show up for work dressed in scrubs and tennis shoes rather than professional attire. They rarely come in early when it’s busy or invest more time than is absolutely needed to see the patients on their list, making it easy for others to dismiss them as shift workers.
Hospitalists, they say, are unwilling to come in on their own time to attend a medical staff meeting, something other doctors do as a matter of course. And instead of interacting as social peers with other physicians when opportunity arises (i.e., in the cafeteria or doctors’ lounge), the hospitalists just grab food and head back to eat together in their work room.
The executives said they want to help enhance the stature of their hospitalists within the medical staff, but the Here’s a typical comment:
“[Hospitalists] also need to be willing to participate in hospital and system committees. Although this may require them to interrupt their workflow and stay late on some days they are working or come in on days off, they will never garner the respect of their colleagues if they are unwilling to do so.”
Read the full post at hospitalleader.org.
Leslie Flores is a hospital medicine consultant and member of SHM’s Practice Analysis Committee.
Also on The Hospital Leader. . .
• Creating Value through Crowdsourcing & Finding ‘Value’ in the New Year, by Vineet Arora, MD, MPP, FHM
• BREAKING NEWS: “Physicians Deemed Unnecessary”; Social Worker Promoted to Hospital CEO, by Jordan Messler, MD, SFHM
• ER Docs and Out-of-Network Billing: Are We in the Same Boat?, by Brad Flansbaum, DO, MPH, MHM
• The Best Way to Die?, by David Brabeck, MD
Editor’s note: This article first appeared on “The Hospital Leader” blog. Read the full post at hospitalleader.org.
In December, I wrote a letter to hospital executives, urging them to deliberately invest their own personal time and effort in fostering hospitalist well-being. I suggested several actions that leaders can take to enhance hospitalist job satisfaction and reduce the risk of burnout and turnover.
Following publication of that post, I heard from several hospital executives and was pleasantly surprised that they all responded positively to my message. Several execs told me that they gained valuable new insights about their hospitalists’ challenges and needs; others said they planned to take action on one or more of my suggestions that had never occurred to them before.
Their feedback reinforced my belief that most hospital leaders actually do care a lot about promoting healthy, stable, and sustainable hospitalist programs, but the hospital leaders I talked with also had some messages for their hospitalist colleagues, and I think it’s important to share them in the spirit of fostering a healthy exchange of perspectives. Your hospital’s leaders would be delighted and encouraged if you engaged them in dialogue about these issues.
Help us help you
Several hospital leaders told me that their hospitalists grumble about being treated by the medical staff (and even nurses) like second-class citizens or glorified residents. Those same hospitalists, however, routinely show up for work dressed in scrubs and tennis shoes rather than professional attire. They rarely come in early when it’s busy or invest more time than is absolutely needed to see the patients on their list, making it easy for others to dismiss them as shift workers.
Hospitalists, they say, are unwilling to come in on their own time to attend a medical staff meeting, something other doctors do as a matter of course. And instead of interacting as social peers with other physicians when opportunity arises (i.e., in the cafeteria or doctors’ lounge), the hospitalists just grab food and head back to eat together in their work room.
The executives said they want to help enhance the stature of their hospitalists within the medical staff, but the Here’s a typical comment:
“[Hospitalists] also need to be willing to participate in hospital and system committees. Although this may require them to interrupt their workflow and stay late on some days they are working or come in on days off, they will never garner the respect of their colleagues if they are unwilling to do so.”
Read the full post at hospitalleader.org.
Leslie Flores is a hospital medicine consultant and member of SHM’s Practice Analysis Committee.
Also on The Hospital Leader. . .
• Creating Value through Crowdsourcing & Finding ‘Value’ in the New Year, by Vineet Arora, MD, MPP, FHM
• BREAKING NEWS: “Physicians Deemed Unnecessary”; Social Worker Promoted to Hospital CEO, by Jordan Messler, MD, SFHM
• ER Docs and Out-of-Network Billing: Are We in the Same Boat?, by Brad Flansbaum, DO, MPH, MHM
• The Best Way to Die?, by David Brabeck, MD
Editor’s note: This article first appeared on “The Hospital Leader” blog. Read the full post at hospitalleader.org.
In December, I wrote a letter to hospital executives, urging them to deliberately invest their own personal time and effort in fostering hospitalist well-being. I suggested several actions that leaders can take to enhance hospitalist job satisfaction and reduce the risk of burnout and turnover.
Following publication of that post, I heard from several hospital executives and was pleasantly surprised that they all responded positively to my message. Several execs told me that they gained valuable new insights about their hospitalists’ challenges and needs; others said they planned to take action on one or more of my suggestions that had never occurred to them before.
Their feedback reinforced my belief that most hospital leaders actually do care a lot about promoting healthy, stable, and sustainable hospitalist programs, but the hospital leaders I talked with also had some messages for their hospitalist colleagues, and I think it’s important to share them in the spirit of fostering a healthy exchange of perspectives. Your hospital’s leaders would be delighted and encouraged if you engaged them in dialogue about these issues.
Help us help you
Several hospital leaders told me that their hospitalists grumble about being treated by the medical staff (and even nurses) like second-class citizens or glorified residents. Those same hospitalists, however, routinely show up for work dressed in scrubs and tennis shoes rather than professional attire. They rarely come in early when it’s busy or invest more time than is absolutely needed to see the patients on their list, making it easy for others to dismiss them as shift workers.
Hospitalists, they say, are unwilling to come in on their own time to attend a medical staff meeting, something other doctors do as a matter of course. And instead of interacting as social peers with other physicians when opportunity arises (i.e., in the cafeteria or doctors’ lounge), the hospitalists just grab food and head back to eat together in their work room.
The executives said they want to help enhance the stature of their hospitalists within the medical staff, but the Here’s a typical comment:
“[Hospitalists] also need to be willing to participate in hospital and system committees. Although this may require them to interrupt their workflow and stay late on some days they are working or come in on days off, they will never garner the respect of their colleagues if they are unwilling to do so.”
Read the full post at hospitalleader.org.
Leslie Flores is a hospital medicine consultant and member of SHM’s Practice Analysis Committee.
Also on The Hospital Leader. . .
• Creating Value through Crowdsourcing & Finding ‘Value’ in the New Year, by Vineet Arora, MD, MPP, FHM
• BREAKING NEWS: “Physicians Deemed Unnecessary”; Social Worker Promoted to Hospital CEO, by Jordan Messler, MD, SFHM
• ER Docs and Out-of-Network Billing: Are We in the Same Boat?, by Brad Flansbaum, DO, MPH, MHM
• The Best Way to Die?, by David Brabeck, MD
Scholar grants help future hospitalists explore career pathways
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Everything We Say and Do: Use familiar terminology to allay patients’ fears
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM ’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I clearly explain diagnoses and treatment plans in plain terms.
Why I do it
We hear repeatedly from patients and families that a major source of their fear comes from “not knowing.” Fear of the unknown. If our patients and their families do not understand the message we are trying to communicate, these fears will be realized. It is our responsibility to explain their medical situation(s) to them in plain terms that they can comprehend, so as to allay those fears and enable them to become active, informed participants in their care.
How I do it
I start by reminding myself that I want to treat each patient as I would want a member of my own family to be treated. No one else in my family is in the medical field, so this means I must avoid medical terminology and use more familiar, everyday phrases. For example, I say “heart doctor” or “lung doctor” instead of “cardiologist” or “pulmonologist.” I also prefer “sonogram” to “ultrasound” because most people have heard that term in relation to a pregnancy. Even “EEG” and “EKG” need more plain descriptions.
I also try to use common, relatable analogies when explaining diseases. My favorite is to describe COPD (or any restrictive lung disease) like an old, hard sponge as compared with normal lungs, which are like a new, soft sponge.
I use the Teach-Back Method (which has already been well-discussed in this column by Dr. Trina Dorrah) to check for comprehension. If there are still issues with my message not being received as I had hoped, then I try again to find the terminology or an analogy that will connect with that patient.
Hopefully, using familiar, relatable language in this manner gives my patients and their families a better understanding of their diagnoses and care plans, quells their fears, and enhances their experience.
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla., and a member of SHM's Patient Experience Committee.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM ’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I clearly explain diagnoses and treatment plans in plain terms.
Why I do it
We hear repeatedly from patients and families that a major source of their fear comes from “not knowing.” Fear of the unknown. If our patients and their families do not understand the message we are trying to communicate, these fears will be realized. It is our responsibility to explain their medical situation(s) to them in plain terms that they can comprehend, so as to allay those fears and enable them to become active, informed participants in their care.
How I do it
I start by reminding myself that I want to treat each patient as I would want a member of my own family to be treated. No one else in my family is in the medical field, so this means I must avoid medical terminology and use more familiar, everyday phrases. For example, I say “heart doctor” or “lung doctor” instead of “cardiologist” or “pulmonologist.” I also prefer “sonogram” to “ultrasound” because most people have heard that term in relation to a pregnancy. Even “EEG” and “EKG” need more plain descriptions.
I also try to use common, relatable analogies when explaining diseases. My favorite is to describe COPD (or any restrictive lung disease) like an old, hard sponge as compared with normal lungs, which are like a new, soft sponge.
I use the Teach-Back Method (which has already been well-discussed in this column by Dr. Trina Dorrah) to check for comprehension. If there are still issues with my message not being received as I had hoped, then I try again to find the terminology or an analogy that will connect with that patient.
Hopefully, using familiar, relatable language in this manner gives my patients and their families a better understanding of their diagnoses and care plans, quells their fears, and enhances their experience.
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla., and a member of SHM's Patient Experience Committee.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM ’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I clearly explain diagnoses and treatment plans in plain terms.
Why I do it
We hear repeatedly from patients and families that a major source of their fear comes from “not knowing.” Fear of the unknown. If our patients and their families do not understand the message we are trying to communicate, these fears will be realized. It is our responsibility to explain their medical situation(s) to them in plain terms that they can comprehend, so as to allay those fears and enable them to become active, informed participants in their care.
How I do it
I start by reminding myself that I want to treat each patient as I would want a member of my own family to be treated. No one else in my family is in the medical field, so this means I must avoid medical terminology and use more familiar, everyday phrases. For example, I say “heart doctor” or “lung doctor” instead of “cardiologist” or “pulmonologist.” I also prefer “sonogram” to “ultrasound” because most people have heard that term in relation to a pregnancy. Even “EEG” and “EKG” need more plain descriptions.
I also try to use common, relatable analogies when explaining diseases. My favorite is to describe COPD (or any restrictive lung disease) like an old, hard sponge as compared with normal lungs, which are like a new, soft sponge.
I use the Teach-Back Method (which has already been well-discussed in this column by Dr. Trina Dorrah) to check for comprehension. If there are still issues with my message not being received as I had hoped, then I try again to find the terminology or an analogy that will connect with that patient.
Hopefully, using familiar, relatable language in this manner gives my patients and their families a better understanding of their diagnoses and care plans, quells their fears, and enhances their experience.
Dr. Sharp is a chief hospitalist with Sound Physicians at UF Health in Jacksonville, Fla., and a member of SHM's Patient Experience Committee.
Trending at SHM
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Sneak Peek: The Hospital Leader blog
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
Editor’s note: First published on The Hospital Leader blog under the title, “How I Realized QI Could Be a Dirty Word.”
With the recent election, there has been a new recognition of the various “bubbles” we all seem to be living in. It reminds me of the parable I like to often mention, popularized by the late great writer David Foster Wallace: Two fish were swimming along when an older fish swam by, nodded his head at them and said, “Mornin’ boys, how’s the water?” The two young fish nod back and swim for a bit, then one turns to the other and says, “What the hell is water?”
Imagine the hard reality that hit me when I read this quote from a resident: “Truly, the first thing I think of when I hear [QI] is going to make more work for residents.”
Wait – is QI actually a dirty word for other residents and physicians?
The quote comes from an Academic Medicine study titled “ ‘It Feels Like a Lot of Extra Work’: Resident Attitudes About Quality Improvement and Implications for an Effective Learning Health Care System.” I read on, and it got worse.
“This hasn’t really made any difference to the patients. Like this checklist we do on rounds, like I don’t know. Maybe it has.”
And, by far, most concerning: “There’s like the central line protocols … If you suspect that anybody has any type of bacteremia, you don’t do a blood culture; you just do a urine culture and pull the lines … we just don’t even test for it because the quality improvement then like marks you off.”
Wow.
That is some harsh truth about unintended consequences right there. (Also, apparently us kids of the 1990s still say “like” a lot, which is, like, not very professional and also like kinda grating.)
The residents in this study were from the University of Utah, Salt Lake City – an institution I frequently– and publicly – admire for their incredible progress on systematically introducing value improvement into their practice.
What can we do?
Read the full post at hospitalleader.org.
Also on The Hospital Leader…
- THIS Is What Teamwork Looks Like, by Danielle Scheurer, MD, MSCR, SFHM
- The Medicaid Overhaul and How Hospitals and Their Providers Could Be Hardest Hit, by Brad Flansbaum, DO, MPH, MHM
- Count Me – and My Intuition – In, by Tracy Cardin, ACNP-BC, SFHM
SHM launches Chapter Development Fund to enhance reach, impact of chapters
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
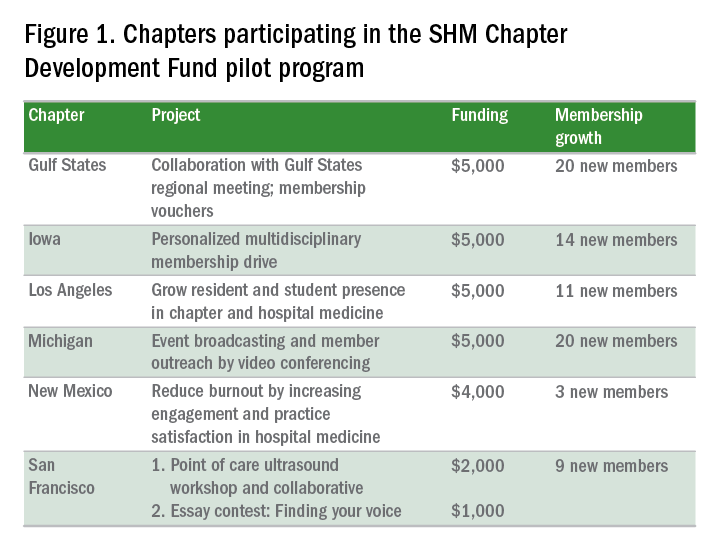
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
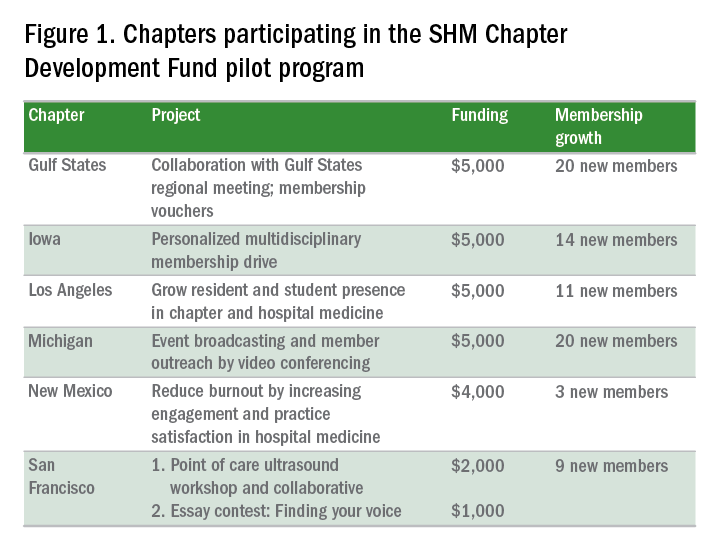
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
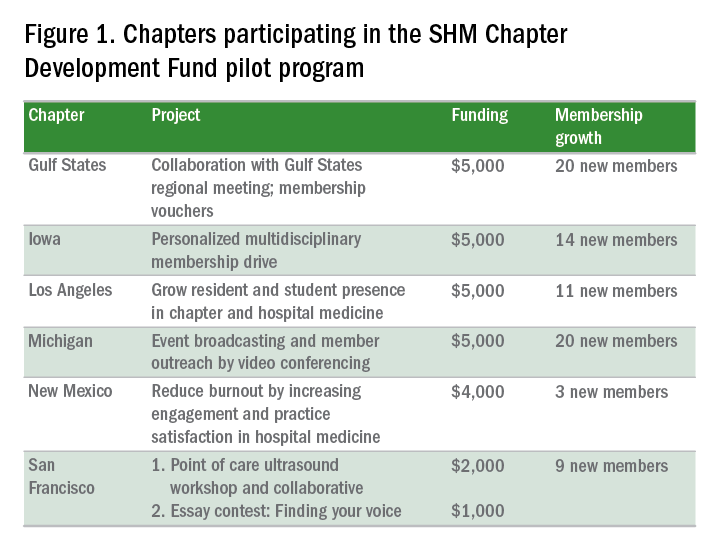
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
SHM Practice Administrators’ Mentor Program benefits both parties
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.















