User login
DVT risk higher in cardiac and vascular surgery
WASHINGTON - Cardiac and vascular surgery patients are at higher risk for deep vein thrombosis than are general surgery patients, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective analysis of 2,669,772 patients with a median age of 64 years, 43% of whom were males, in the ACS-National Surgical Quality Improvement Program (NSQIP) during 2005-2009, Dr. Faisal Aziz of Penn State Hershey (Pa.) Heart and Vascular Institute and his colleagues sought to determine the actual rate of deep vein thrombosis (DVT) during revascularization procedures, compared with general surgery.
The researchers sorted patients according to DVT risk factors such as age, gender, body mass index over 40 kg/m2, and whether the surgery was acute. They then assessed intraoperative factors such as total time to completion and the American Society of Anesthesiology score. They then considered the postoperative factors associated with DVT, such as blood transfusions, return to the operating room, deep wound infection, cardiac arrest, and mortality.
There were 18,512 incidences of DVT, equaling 0.69% of all patients studied. Of those, 0.66% occurred during general surgery, 2.08% occurred during cardiac surgery, and 1% occurred during vascular surgery.
"The implications of our study are that, contrary to popular belief, the incidence of postop DVT is actually higher after cardiac surgery and vascular surgery procedures," he said.
The cardiac surgery procedures associated with the highest DVT incidence rate were tricuspid valve replacement (8%), thoracic endovascular aortic repair (5%), thoracic aortic graft replacement (4%), and pericardial window (4%).
In a comparison of cardiac procedures, tricuspid valve replacement vs. aortic valve replacement had a risk ratio of 3.5 (P < .001). In tricuspid valve replacement vs. coronary artery bypass, the former had a risk ratio of 11.24 (P < .001).
Vascular surgeries with the highest DVT incidence rates were peripheral bypass (1%), amputation (trans-metatarsal, 0.75%; below knee, 1%; above the knee, 1%), and ruptured aortic aneurysms (3.5%).
Comparatively, in ruptured endovascular aneurysm repair (EVAR) vs. elective EVAR, the risk ratio was 3.55 (P < .001). In abdominal aortic aneurysm (AAA) repair, ruptured vs. elective surgeries had a risk ratio of 2.37 (P < .001).
Compared with 80% of general surgery patients, 74% of cardiac surgery patients were 70 years or older (relative risk, 1.12; P = .13); 86% of vascular surgery patients were 70 years or older (RR, 1.1; P < .05).
Male gender was an associated risk factor in 49% of general surgery patients, compared with 70% for cardiac patients (RR, 1.4; P < .001) and 51% for vascular patients (RR, 1.1; P < .001).
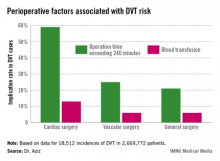
Intra- and postoperative factors associated with DVT risk included operation times exceeding 240 minutes and previous DVT. Compared with 21% of general surgery patients, operation time was implicated in 59% of cardiac surgery patients (relative risk, 2.72; P < .001) and 25% of vascular surgery patients (RR, 1.14; P <.001). Blood transfusions affected 13% of cardiac surgery patients (RR, 2.3; P < .001), 6% of vascular surgery patients (RR, 1.3; P < .001), and 6% of general surgery patients.
Compared with 24% for general surgery patients, returning to the operating room was implicated in 27% of cardiac patients (RR, 1.4; P = .27) and 32% of vascular surgery patients (RR, 1.3; P < .001).
"Procedures and perioperative factors associated with high risk of postoperative DVT should be identified, and adequate DVT prophylaxis should be ensured for these patients," Dr. Aziz concluded.
He had no disclosures.
WASHINGTON - Cardiac and vascular surgery patients are at higher risk for deep vein thrombosis than are general surgery patients, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective analysis of 2,669,772 patients with a median age of 64 years, 43% of whom were males, in the ACS-National Surgical Quality Improvement Program (NSQIP) during 2005-2009, Dr. Faisal Aziz of Penn State Hershey (Pa.) Heart and Vascular Institute and his colleagues sought to determine the actual rate of deep vein thrombosis (DVT) during revascularization procedures, compared with general surgery.
The researchers sorted patients according to DVT risk factors such as age, gender, body mass index over 40 kg/m2, and whether the surgery was acute. They then assessed intraoperative factors such as total time to completion and the American Society of Anesthesiology score. They then considered the postoperative factors associated with DVT, such as blood transfusions, return to the operating room, deep wound infection, cardiac arrest, and mortality.
There were 18,512 incidences of DVT, equaling 0.69% of all patients studied. Of those, 0.66% occurred during general surgery, 2.08% occurred during cardiac surgery, and 1% occurred during vascular surgery.
"The implications of our study are that, contrary to popular belief, the incidence of postop DVT is actually higher after cardiac surgery and vascular surgery procedures," he said.
The cardiac surgery procedures associated with the highest DVT incidence rate were tricuspid valve replacement (8%), thoracic endovascular aortic repair (5%), thoracic aortic graft replacement (4%), and pericardial window (4%).
In a comparison of cardiac procedures, tricuspid valve replacement vs. aortic valve replacement had a risk ratio of 3.5 (P < .001). In tricuspid valve replacement vs. coronary artery bypass, the former had a risk ratio of 11.24 (P < .001).
Vascular surgeries with the highest DVT incidence rates were peripheral bypass (1%), amputation (trans-metatarsal, 0.75%; below knee, 1%; above the knee, 1%), and ruptured aortic aneurysms (3.5%).
Comparatively, in ruptured endovascular aneurysm repair (EVAR) vs. elective EVAR, the risk ratio was 3.55 (P < .001). In abdominal aortic aneurysm (AAA) repair, ruptured vs. elective surgeries had a risk ratio of 2.37 (P < .001).
Compared with 80% of general surgery patients, 74% of cardiac surgery patients were 70 years or older (relative risk, 1.12; P = .13); 86% of vascular surgery patients were 70 years or older (RR, 1.1; P < .05).
Male gender was an associated risk factor in 49% of general surgery patients, compared with 70% for cardiac patients (RR, 1.4; P < .001) and 51% for vascular patients (RR, 1.1; P < .001).
Intra- and postoperative factors associated with DVT risk included operation times exceeding 240 minutes and previous DVT. Compared with 21% of general surgery patients, operation time was implicated in 59% of cardiac surgery patients (relative risk, 2.72; P < .001) and 25% of vascular surgery patients (RR, 1.14; P <.001). Blood transfusions affected 13% of cardiac surgery patients (RR, 2.3; P < .001), 6% of vascular surgery patients (RR, 1.3; P < .001), and 6% of general surgery patients.
Compared with 24% for general surgery patients, returning to the operating room was implicated in 27% of cardiac patients (RR, 1.4; P = .27) and 32% of vascular surgery patients (RR, 1.3; P < .001).
"Procedures and perioperative factors associated with high risk of postoperative DVT should be identified, and adequate DVT prophylaxis should be ensured for these patients," Dr. Aziz concluded.
He had no disclosures.
WASHINGTON - Cardiac and vascular surgery patients are at higher risk for deep vein thrombosis than are general surgery patients, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective analysis of 2,669,772 patients with a median age of 64 years, 43% of whom were males, in the ACS-National Surgical Quality Improvement Program (NSQIP) during 2005-2009, Dr. Faisal Aziz of Penn State Hershey (Pa.) Heart and Vascular Institute and his colleagues sought to determine the actual rate of deep vein thrombosis (DVT) during revascularization procedures, compared with general surgery.
The researchers sorted patients according to DVT risk factors such as age, gender, body mass index over 40 kg/m2, and whether the surgery was acute. They then assessed intraoperative factors such as total time to completion and the American Society of Anesthesiology score. They then considered the postoperative factors associated with DVT, such as blood transfusions, return to the operating room, deep wound infection, cardiac arrest, and mortality.
There were 18,512 incidences of DVT, equaling 0.69% of all patients studied. Of those, 0.66% occurred during general surgery, 2.08% occurred during cardiac surgery, and 1% occurred during vascular surgery.
"The implications of our study are that, contrary to popular belief, the incidence of postop DVT is actually higher after cardiac surgery and vascular surgery procedures," he said.
The cardiac surgery procedures associated with the highest DVT incidence rate were tricuspid valve replacement (8%), thoracic endovascular aortic repair (5%), thoracic aortic graft replacement (4%), and pericardial window (4%).
In a comparison of cardiac procedures, tricuspid valve replacement vs. aortic valve replacement had a risk ratio of 3.5 (P < .001). In tricuspid valve replacement vs. coronary artery bypass, the former had a risk ratio of 11.24 (P < .001).
Vascular surgeries with the highest DVT incidence rates were peripheral bypass (1%), amputation (trans-metatarsal, 0.75%; below knee, 1%; above the knee, 1%), and ruptured aortic aneurysms (3.5%).
Comparatively, in ruptured endovascular aneurysm repair (EVAR) vs. elective EVAR, the risk ratio was 3.55 (P < .001). In abdominal aortic aneurysm (AAA) repair, ruptured vs. elective surgeries had a risk ratio of 2.37 (P < .001).
Compared with 80% of general surgery patients, 74% of cardiac surgery patients were 70 years or older (relative risk, 1.12; P = .13); 86% of vascular surgery patients were 70 years or older (RR, 1.1; P < .05).
Male gender was an associated risk factor in 49% of general surgery patients, compared with 70% for cardiac patients (RR, 1.4; P < .001) and 51% for vascular patients (RR, 1.1; P < .001).
Intra- and postoperative factors associated with DVT risk included operation times exceeding 240 minutes and previous DVT. Compared with 21% of general surgery patients, operation time was implicated in 59% of cardiac surgery patients (relative risk, 2.72; P < .001) and 25% of vascular surgery patients (RR, 1.14; P <.001). Blood transfusions affected 13% of cardiac surgery patients (RR, 2.3; P < .001), 6% of vascular surgery patients (RR, 1.3; P < .001), and 6% of general surgery patients.
Compared with 24% for general surgery patients, returning to the operating room was implicated in 27% of cardiac patients (RR, 1.4; P = .27) and 32% of vascular surgery patients (RR, 1.3; P < .001).
"Procedures and perioperative factors associated with high risk of postoperative DVT should be identified, and adequate DVT prophylaxis should be ensured for these patients," Dr. Aziz concluded.
He had no disclosures.
Mitral valve repair seen as no better than replacement
Mitral valve repair was no better than chordal-sparing mitral valve replacement in the first randomized clinical trial attempting to settle the controversy over which procedure is superior for treating functional ischemic mitral regurgitation, which was simultaneously reported at the annual scientific sessions of the American Heart Association and online in the New England Journal of Medicine.
In the past few years, the use of mitral valve repair has far exceeded that of mitral valve replacement for this indication, largely on the basis of reports that the repair procedure yields lower operative mortality, improved left ventricular function, and higher long-term survival rates. In particular, a 2011 meta-analysis found a 35% lower relative risk of death in the long term with mitral valve repair, compared with replacement, said Dr. Michael A. Acker and his associates in the Cardiothoracic Surgical Trials Network (CTSN).
But in their multicenter study directly comparing the two procedures in 251 patients with severe functional ischemic mitral regurgitation, there was no significant difference between the surgeries in left ventricular end-systolic volume index at 1 year, nor in mortality at either 1 month or 1 year.
Moreover, study participants who underwent mitral valve repair showed a disturbing excess in the rate of recurrence of mitral regurgitation at 1 year, with a rate that was 30 percentage points higher than that among patients who underwent mitral valve replacement. "This lack of durability in correction of mitral regurgitation is disconcerting, given its reported association with further progression and long-term negative outcomes," said Dr. Acker of the division of cardiovascular surgery, University of Pennsylvania, Philadelphia, and his associates.
Functional ischemic mitral regurgitation, a "high-prevalence" condition affecting an estimated 2-3 million Americans, differs from primary degenerative mitral regurgitation in that the valve leaflets themselves remain normal while the defect occurs in the myocardium. "Ischemic mitral regurgitation is a consequence of adverse left ventricular remodeling after myocardial injury, with enlargement of the left ventricular chamber and mitral annulus, apical and lateral migration of the papillary muscles, leaflet retethering, and reduced closing forces. These processes lead to malcoaptation of the leaflets and variable degrees of mitral regurgitation that can fluctuate dynamically as a function of volume status, afterload, heart rhythm, and residual ischemia," the researchers said.
Current guidelines recommend mitral valve repair or chordal-sparing mitral valve replacement for severe regurgitation unresponsive to medical therapy, but do not specify which procedure is preferred because there is no conclusive evidence demonstrating the superiority of one over the other. "Recently, the field has embraced mitral valve repair over replacement," even without such evidence, Dr. Acker and his colleagues said.
The CTSN performed this study at 22 medical centers to assess the relative benefits of the two surgeries, with 126 patients randomized to undergo mitral valve repair and 125 to undergo replacement that included complete preservation of the subvalvular apparatus.
The primary endpoint was the degree of LV reverse remodeling, as measured by the left ventricular end-systolic volume index (LVESVI) on transthoracic echocardiography, at 1 year. The mean LVESVI was not significantly different between the repair group (54.6 mL per square meter) and the replacement group (60.7 mL per square meter), reflecting decreases of 6.6 mL per square meter and 6.8 mL per square meter, respectively, the investigators said (N. Engl. J. Med. 2013 [doi:10.1056/NEJMoa1312808]).
The median between group difference in the change in LVESVI score after surgery also was not clinically significant. However, 32.6% of patients who underwent mitral valve repair had a recurrence of regurgitation within 1 year, compared with only 2.3% of those who had mitral valve replacement. Three patients in the repair group required reoperation, compared with none in the replacement group.
There were no significant differences in cumulative mortality, 30-day postoperative mortality, or 1-year mortality between the two groups, and no significant difference in a composite endpoint of major adverse cardiac or cerebrovascular events.
Rates of serious adverse events were similar, and the durations of hospitalization were similar between the two study groups, as were rates of readmission. All measures of quality of life and functional status on two assessment tools were similar.
"Our findings contradict much of the published literature on this topic, which reports several advantages to mitral valve repair over replacement, including lower operative mortality, improved left ventricular function, and higher rates of long-term survival," Dr. Acker and his associates noted.
The evolution of the valve replacement procedure, which now includes chordal sparing, "may account for the improved results we observed, as compared with previous studies, since the retention of the internal architectural support of the left ventricle may preserve contractile efficiency and reduce left ventricular dilatation and dysfunction," they said.
Dr. Acker reported no conflicts.
Mitral valve repair was no better than chordal-sparing mitral valve replacement in the first randomized clinical trial attempting to settle the controversy over which procedure is superior for treating functional ischemic mitral regurgitation, which was simultaneously reported at the annual scientific sessions of the American Heart Association and online in the New England Journal of Medicine.
In the past few years, the use of mitral valve repair has far exceeded that of mitral valve replacement for this indication, largely on the basis of reports that the repair procedure yields lower operative mortality, improved left ventricular function, and higher long-term survival rates. In particular, a 2011 meta-analysis found a 35% lower relative risk of death in the long term with mitral valve repair, compared with replacement, said Dr. Michael A. Acker and his associates in the Cardiothoracic Surgical Trials Network (CTSN).
But in their multicenter study directly comparing the two procedures in 251 patients with severe functional ischemic mitral regurgitation, there was no significant difference between the surgeries in left ventricular end-systolic volume index at 1 year, nor in mortality at either 1 month or 1 year.
Moreover, study participants who underwent mitral valve repair showed a disturbing excess in the rate of recurrence of mitral regurgitation at 1 year, with a rate that was 30 percentage points higher than that among patients who underwent mitral valve replacement. "This lack of durability in correction of mitral regurgitation is disconcerting, given its reported association with further progression and long-term negative outcomes," said Dr. Acker of the division of cardiovascular surgery, University of Pennsylvania, Philadelphia, and his associates.
Functional ischemic mitral regurgitation, a "high-prevalence" condition affecting an estimated 2-3 million Americans, differs from primary degenerative mitral regurgitation in that the valve leaflets themselves remain normal while the defect occurs in the myocardium. "Ischemic mitral regurgitation is a consequence of adverse left ventricular remodeling after myocardial injury, with enlargement of the left ventricular chamber and mitral annulus, apical and lateral migration of the papillary muscles, leaflet retethering, and reduced closing forces. These processes lead to malcoaptation of the leaflets and variable degrees of mitral regurgitation that can fluctuate dynamically as a function of volume status, afterload, heart rhythm, and residual ischemia," the researchers said.
Current guidelines recommend mitral valve repair or chordal-sparing mitral valve replacement for severe regurgitation unresponsive to medical therapy, but do not specify which procedure is preferred because there is no conclusive evidence demonstrating the superiority of one over the other. "Recently, the field has embraced mitral valve repair over replacement," even without such evidence, Dr. Acker and his colleagues said.
The CTSN performed this study at 22 medical centers to assess the relative benefits of the two surgeries, with 126 patients randomized to undergo mitral valve repair and 125 to undergo replacement that included complete preservation of the subvalvular apparatus.
The primary endpoint was the degree of LV reverse remodeling, as measured by the left ventricular end-systolic volume index (LVESVI) on transthoracic echocardiography, at 1 year. The mean LVESVI was not significantly different between the repair group (54.6 mL per square meter) and the replacement group (60.7 mL per square meter), reflecting decreases of 6.6 mL per square meter and 6.8 mL per square meter, respectively, the investigators said (N. Engl. J. Med. 2013 [doi:10.1056/NEJMoa1312808]).
The median between group difference in the change in LVESVI score after surgery also was not clinically significant. However, 32.6% of patients who underwent mitral valve repair had a recurrence of regurgitation within 1 year, compared with only 2.3% of those who had mitral valve replacement. Three patients in the repair group required reoperation, compared with none in the replacement group.
There were no significant differences in cumulative mortality, 30-day postoperative mortality, or 1-year mortality between the two groups, and no significant difference in a composite endpoint of major adverse cardiac or cerebrovascular events.
Rates of serious adverse events were similar, and the durations of hospitalization were similar between the two study groups, as were rates of readmission. All measures of quality of life and functional status on two assessment tools were similar.
"Our findings contradict much of the published literature on this topic, which reports several advantages to mitral valve repair over replacement, including lower operative mortality, improved left ventricular function, and higher rates of long-term survival," Dr. Acker and his associates noted.
The evolution of the valve replacement procedure, which now includes chordal sparing, "may account for the improved results we observed, as compared with previous studies, since the retention of the internal architectural support of the left ventricle may preserve contractile efficiency and reduce left ventricular dilatation and dysfunction," they said.
Dr. Acker reported no conflicts.
Mitral valve repair was no better than chordal-sparing mitral valve replacement in the first randomized clinical trial attempting to settle the controversy over which procedure is superior for treating functional ischemic mitral regurgitation, which was simultaneously reported at the annual scientific sessions of the American Heart Association and online in the New England Journal of Medicine.
In the past few years, the use of mitral valve repair has far exceeded that of mitral valve replacement for this indication, largely on the basis of reports that the repair procedure yields lower operative mortality, improved left ventricular function, and higher long-term survival rates. In particular, a 2011 meta-analysis found a 35% lower relative risk of death in the long term with mitral valve repair, compared with replacement, said Dr. Michael A. Acker and his associates in the Cardiothoracic Surgical Trials Network (CTSN).
But in their multicenter study directly comparing the two procedures in 251 patients with severe functional ischemic mitral regurgitation, there was no significant difference between the surgeries in left ventricular end-systolic volume index at 1 year, nor in mortality at either 1 month or 1 year.
Moreover, study participants who underwent mitral valve repair showed a disturbing excess in the rate of recurrence of mitral regurgitation at 1 year, with a rate that was 30 percentage points higher than that among patients who underwent mitral valve replacement. "This lack of durability in correction of mitral regurgitation is disconcerting, given its reported association with further progression and long-term negative outcomes," said Dr. Acker of the division of cardiovascular surgery, University of Pennsylvania, Philadelphia, and his associates.
Functional ischemic mitral regurgitation, a "high-prevalence" condition affecting an estimated 2-3 million Americans, differs from primary degenerative mitral regurgitation in that the valve leaflets themselves remain normal while the defect occurs in the myocardium. "Ischemic mitral regurgitation is a consequence of adverse left ventricular remodeling after myocardial injury, with enlargement of the left ventricular chamber and mitral annulus, apical and lateral migration of the papillary muscles, leaflet retethering, and reduced closing forces. These processes lead to malcoaptation of the leaflets and variable degrees of mitral regurgitation that can fluctuate dynamically as a function of volume status, afterload, heart rhythm, and residual ischemia," the researchers said.
Current guidelines recommend mitral valve repair or chordal-sparing mitral valve replacement for severe regurgitation unresponsive to medical therapy, but do not specify which procedure is preferred because there is no conclusive evidence demonstrating the superiority of one over the other. "Recently, the field has embraced mitral valve repair over replacement," even without such evidence, Dr. Acker and his colleagues said.
The CTSN performed this study at 22 medical centers to assess the relative benefits of the two surgeries, with 126 patients randomized to undergo mitral valve repair and 125 to undergo replacement that included complete preservation of the subvalvular apparatus.
The primary endpoint was the degree of LV reverse remodeling, as measured by the left ventricular end-systolic volume index (LVESVI) on transthoracic echocardiography, at 1 year. The mean LVESVI was not significantly different between the repair group (54.6 mL per square meter) and the replacement group (60.7 mL per square meter), reflecting decreases of 6.6 mL per square meter and 6.8 mL per square meter, respectively, the investigators said (N. Engl. J. Med. 2013 [doi:10.1056/NEJMoa1312808]).
The median between group difference in the change in LVESVI score after surgery also was not clinically significant. However, 32.6% of patients who underwent mitral valve repair had a recurrence of regurgitation within 1 year, compared with only 2.3% of those who had mitral valve replacement. Three patients in the repair group required reoperation, compared with none in the replacement group.
There were no significant differences in cumulative mortality, 30-day postoperative mortality, or 1-year mortality between the two groups, and no significant difference in a composite endpoint of major adverse cardiac or cerebrovascular events.
Rates of serious adverse events were similar, and the durations of hospitalization were similar between the two study groups, as were rates of readmission. All measures of quality of life and functional status on two assessment tools were similar.
"Our findings contradict much of the published literature on this topic, which reports several advantages to mitral valve repair over replacement, including lower operative mortality, improved left ventricular function, and higher rates of long-term survival," Dr. Acker and his associates noted.
The evolution of the valve replacement procedure, which now includes chordal sparing, "may account for the improved results we observed, as compared with previous studies, since the retention of the internal architectural support of the left ventricle may preserve contractile efficiency and reduce left ventricular dilatation and dysfunction," they said.
Dr. Acker reported no conflicts.
Major Finding: The primary end point ? the degree of LV reverse remodeling, as measured by the left ventricular end-systolic volume index on transthoracic echocardiography at 1 year ? was not significantly different between the repair group (54.6 mL per square meter) and the replacement group (60.7 mL per square meter).
Data Source: A randomized clinical trial involving 126 patients with severe functional ischemic mitral regurgitation who underwent mitral valve repair and 125 who underwent chordal-sparing mitral valve replacement, and who were followed for 1 year.
Disclosures: This study was funded by the National Heart, Lung, and Blood Institute, the National Institute of Neurological Diseases and Stroke, and the Canadian Institutes of Health Research. Dr. Acker and his associates reported no financial conflicts of interest.
CoreValve Extreme Risk study is promising
SAN FRANCISCO – Trans-catheter aortic valve replacement with the self-expanding CoreValve in patients at extreme surgical risk significantly reduced the rate of death or major stroke at 1 year, from 43% to 26%, in a 487-patient pivotal trial.
The CoreValve Extreme Risk study gathered data from a registry of patients with symptomatic severe aortic stenosis who attempted an iliofemoral implantation procedure with the CoreValve at 40 U.S. sites. Results were compared with an "objective performance goal" derived from two sources: a meta-analysis of five contemporary balloon valvuloplasty series that found a 43% mortality and major stroke rate at 1 year, and the 1-year rate from the PARTNER B trial in inoperable patients (Placement of Aortic Transcatheter Valves, Cohort B), which was 50% but had a lower confidence bound of 43%.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The performance-goal comparison was necessary in the current study because randomizing these patients to medical therapy in a control group is no longer an acceptable option in the United States, Dr. Jeffrey J. Popma said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The 1-year all-cause mortality rate was 24%, and the cardiovascular mortality was 18%, reported Dr. Popma, professor of medicine at Harvard Medical School, Boston.
Two percent of patients developed a major stroke within 1 month and 4% did so within 1 year.
Data from a continued access study involving another 830 extreme-risk patients who received the CoreValve through an iliofemoral approach are showing even better results, with a 16% rate of mortality or major stroke at 6 months.
Among secondary endpoints at 1 year in the main study, 7% of patients developed any kind of stroke, 2% had an MI, 2% needed reintervention, 41% had bleeding that met Valve Academic Research Consortium criteria, 8% had major vascular complications, and 27% required implantation of a permanent pacemaker, Dr. Popma reported at the meeting, cosponsored by the American College of Cardiology. Ninety percent of patients improved by at least one New York Heart Association functional class and 60% improved by at least two classes at 1 year of follow-up.
Paravalvular regurgitation of any severity was seen in 53% of patients 1 month after implantation and in 33% at 1 year. Moderate paravalvular leakage (PVL) affected 9% at 1 month and 4% at 1 year, and severe PVL affected 1.6% at 1 month and no patients at 1 year, Dr. Popma said. Among the 11% of patients with moderate PVL at 1 month, 80% of those who survived to 1 year had a reduction in leakage over time.
"We believe that’s why we did not find an association in the study between mild or moderate aortic regurgitation with respect to late-term mortality," though mortality risk was substantially higher with severe regurgitation, he said. One-year mortality rates were 86% with severe PVL and 24% with either moderate or mild PVL, compared with 18% in patients with no PVL.
The improvement in PVL rates over time may be due to use of CT angiography to select appropriate valve sizes for patients and continued expansion of the self-expanding frame over time. "That’s a remarkable finding, and it needs to be confirmed," Dr. Popma said.
The study focused on patients whose severe frailty, comorbidity, or disability put them at extreme risk of at least a 50% chance of death or irreversible morbidity within 30 days had they undergone surgical aortic valve replacement. A second U.S. pivotal trial of the CoreValve is focusing on patients at high (but not extreme) risk.
Most of the sites in the study had no experience with CoreValve before this study, Dr. Michael J. Mack noted at a press briefing. "The results are outstanding, but especially putting it in that light," said Dr. Mack, a member of the steering committee for the PARTNER trial.
Dr. Popma reported financial ties with Medtronic, which sponsored the study and makes CoreValve.
This is a brilliantly executed, rigorously performed study. After doing sham-control studies, as we did, in these extreme-risk patients, it’s difficult to do a randomized trial. I think these investigators did they best that they could. Using a performance goal standard was the right thing to do.

|
| Dr. Martin B. Leon |
I think that the results are good. It’s always difficult to compare study to study. They’re at different points in time, and we learn things over time. The CoreValve device is a lower-profile device, so there were fewer vascular complications, there was less major bleeding. Those things, in fact, can have an impact on 1-year mortality. The overall 1-year mortality was lower than in PARTNER. In PARTNER by intention to treat the mortality rate was 30.7%, and in the CoreValve study it was in the low 20% range. I think that that’s encouraging.
The stroke rates are encouraging. The pacemaker rates are predictable; it’s a by-product of the specific device. The importance of that is debatable, but it’s not really a concern. It was anticipated.
The paravalvular leakage (PVL) rate is interesting. Many studies with CoreValve suggest that either moderate or severe PVL is associated with an increase in late mortality, if not at 1 year later. It’s not a huge sample size; maybe over time with different definitions of PVL we’d begin to see that.
I am surprised by the 30-day to 1-year data that suggest a reduced PVL rate. I can understand how a self-expanding platform might change in the first 30 days; I can’t quite understand how it would change between 1 month and 12 months in a way that PVL would go down.
Martin B. Leon, M.D., is director of the Center for Interventional Vascular Therapy at Columbia University, New York, and served as principal investigator of the PARTNER trial of the competing Sapien valve.
This is a brilliantly executed, rigorously performed study. After doing sham-control studies, as we did, in these extreme-risk patients, it’s difficult to do a randomized trial. I think these investigators did they best that they could. Using a performance goal standard was the right thing to do.

|
| Dr. Martin B. Leon |
I think that the results are good. It’s always difficult to compare study to study. They’re at different points in time, and we learn things over time. The CoreValve device is a lower-profile device, so there were fewer vascular complications, there was less major bleeding. Those things, in fact, can have an impact on 1-year mortality. The overall 1-year mortality was lower than in PARTNER. In PARTNER by intention to treat the mortality rate was 30.7%, and in the CoreValve study it was in the low 20% range. I think that that’s encouraging.
The stroke rates are encouraging. The pacemaker rates are predictable; it’s a by-product of the specific device. The importance of that is debatable, but it’s not really a concern. It was anticipated.
The paravalvular leakage (PVL) rate is interesting. Many studies with CoreValve suggest that either moderate or severe PVL is associated with an increase in late mortality, if not at 1 year later. It’s not a huge sample size; maybe over time with different definitions of PVL we’d begin to see that.
I am surprised by the 30-day to 1-year data that suggest a reduced PVL rate. I can understand how a self-expanding platform might change in the first 30 days; I can’t quite understand how it would change between 1 month and 12 months in a way that PVL would go down.
Martin B. Leon, M.D., is director of the Center for Interventional Vascular Therapy at Columbia University, New York, and served as principal investigator of the PARTNER trial of the competing Sapien valve.
This is a brilliantly executed, rigorously performed study. After doing sham-control studies, as we did, in these extreme-risk patients, it’s difficult to do a randomized trial. I think these investigators did they best that they could. Using a performance goal standard was the right thing to do.

|
| Dr. Martin B. Leon |
I think that the results are good. It’s always difficult to compare study to study. They’re at different points in time, and we learn things over time. The CoreValve device is a lower-profile device, so there were fewer vascular complications, there was less major bleeding. Those things, in fact, can have an impact on 1-year mortality. The overall 1-year mortality was lower than in PARTNER. In PARTNER by intention to treat the mortality rate was 30.7%, and in the CoreValve study it was in the low 20% range. I think that that’s encouraging.
The stroke rates are encouraging. The pacemaker rates are predictable; it’s a by-product of the specific device. The importance of that is debatable, but it’s not really a concern. It was anticipated.
The paravalvular leakage (PVL) rate is interesting. Many studies with CoreValve suggest that either moderate or severe PVL is associated with an increase in late mortality, if not at 1 year later. It’s not a huge sample size; maybe over time with different definitions of PVL we’d begin to see that.
I am surprised by the 30-day to 1-year data that suggest a reduced PVL rate. I can understand how a self-expanding platform might change in the first 30 days; I can’t quite understand how it would change between 1 month and 12 months in a way that PVL would go down.
Martin B. Leon, M.D., is director of the Center for Interventional Vascular Therapy at Columbia University, New York, and served as principal investigator of the PARTNER trial of the competing Sapien valve.
SAN FRANCISCO – Trans-catheter aortic valve replacement with the self-expanding CoreValve in patients at extreme surgical risk significantly reduced the rate of death or major stroke at 1 year, from 43% to 26%, in a 487-patient pivotal trial.
The CoreValve Extreme Risk study gathered data from a registry of patients with symptomatic severe aortic stenosis who attempted an iliofemoral implantation procedure with the CoreValve at 40 U.S. sites. Results were compared with an "objective performance goal" derived from two sources: a meta-analysis of five contemporary balloon valvuloplasty series that found a 43% mortality and major stroke rate at 1 year, and the 1-year rate from the PARTNER B trial in inoperable patients (Placement of Aortic Transcatheter Valves, Cohort B), which was 50% but had a lower confidence bound of 43%.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The performance-goal comparison was necessary in the current study because randomizing these patients to medical therapy in a control group is no longer an acceptable option in the United States, Dr. Jeffrey J. Popma said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The 1-year all-cause mortality rate was 24%, and the cardiovascular mortality was 18%, reported Dr. Popma, professor of medicine at Harvard Medical School, Boston.
Two percent of patients developed a major stroke within 1 month and 4% did so within 1 year.
Data from a continued access study involving another 830 extreme-risk patients who received the CoreValve through an iliofemoral approach are showing even better results, with a 16% rate of mortality or major stroke at 6 months.
Among secondary endpoints at 1 year in the main study, 7% of patients developed any kind of stroke, 2% had an MI, 2% needed reintervention, 41% had bleeding that met Valve Academic Research Consortium criteria, 8% had major vascular complications, and 27% required implantation of a permanent pacemaker, Dr. Popma reported at the meeting, cosponsored by the American College of Cardiology. Ninety percent of patients improved by at least one New York Heart Association functional class and 60% improved by at least two classes at 1 year of follow-up.
Paravalvular regurgitation of any severity was seen in 53% of patients 1 month after implantation and in 33% at 1 year. Moderate paravalvular leakage (PVL) affected 9% at 1 month and 4% at 1 year, and severe PVL affected 1.6% at 1 month and no patients at 1 year, Dr. Popma said. Among the 11% of patients with moderate PVL at 1 month, 80% of those who survived to 1 year had a reduction in leakage over time.
"We believe that’s why we did not find an association in the study between mild or moderate aortic regurgitation with respect to late-term mortality," though mortality risk was substantially higher with severe regurgitation, he said. One-year mortality rates were 86% with severe PVL and 24% with either moderate or mild PVL, compared with 18% in patients with no PVL.
The improvement in PVL rates over time may be due to use of CT angiography to select appropriate valve sizes for patients and continued expansion of the self-expanding frame over time. "That’s a remarkable finding, and it needs to be confirmed," Dr. Popma said.
The study focused on patients whose severe frailty, comorbidity, or disability put them at extreme risk of at least a 50% chance of death or irreversible morbidity within 30 days had they undergone surgical aortic valve replacement. A second U.S. pivotal trial of the CoreValve is focusing on patients at high (but not extreme) risk.
Most of the sites in the study had no experience with CoreValve before this study, Dr. Michael J. Mack noted at a press briefing. "The results are outstanding, but especially putting it in that light," said Dr. Mack, a member of the steering committee for the PARTNER trial.
Dr. Popma reported financial ties with Medtronic, which sponsored the study and makes CoreValve.
SAN FRANCISCO – Trans-catheter aortic valve replacement with the self-expanding CoreValve in patients at extreme surgical risk significantly reduced the rate of death or major stroke at 1 year, from 43% to 26%, in a 487-patient pivotal trial.
The CoreValve Extreme Risk study gathered data from a registry of patients with symptomatic severe aortic stenosis who attempted an iliofemoral implantation procedure with the CoreValve at 40 U.S. sites. Results were compared with an "objective performance goal" derived from two sources: a meta-analysis of five contemporary balloon valvuloplasty series that found a 43% mortality and major stroke rate at 1 year, and the 1-year rate from the PARTNER B trial in inoperable patients (Placement of Aortic Transcatheter Valves, Cohort B), which was 50% but had a lower confidence bound of 43%.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The performance-goal comparison was necessary in the current study because randomizing these patients to medical therapy in a control group is no longer an acceptable option in the United States, Dr. Jeffrey J. Popma said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The 1-year all-cause mortality rate was 24%, and the cardiovascular mortality was 18%, reported Dr. Popma, professor of medicine at Harvard Medical School, Boston.
Two percent of patients developed a major stroke within 1 month and 4% did so within 1 year.
Data from a continued access study involving another 830 extreme-risk patients who received the CoreValve through an iliofemoral approach are showing even better results, with a 16% rate of mortality or major stroke at 6 months.
Among secondary endpoints at 1 year in the main study, 7% of patients developed any kind of stroke, 2% had an MI, 2% needed reintervention, 41% had bleeding that met Valve Academic Research Consortium criteria, 8% had major vascular complications, and 27% required implantation of a permanent pacemaker, Dr. Popma reported at the meeting, cosponsored by the American College of Cardiology. Ninety percent of patients improved by at least one New York Heart Association functional class and 60% improved by at least two classes at 1 year of follow-up.
Paravalvular regurgitation of any severity was seen in 53% of patients 1 month after implantation and in 33% at 1 year. Moderate paravalvular leakage (PVL) affected 9% at 1 month and 4% at 1 year, and severe PVL affected 1.6% at 1 month and no patients at 1 year, Dr. Popma said. Among the 11% of patients with moderate PVL at 1 month, 80% of those who survived to 1 year had a reduction in leakage over time.
"We believe that’s why we did not find an association in the study between mild or moderate aortic regurgitation with respect to late-term mortality," though mortality risk was substantially higher with severe regurgitation, he said. One-year mortality rates were 86% with severe PVL and 24% with either moderate or mild PVL, compared with 18% in patients with no PVL.
The improvement in PVL rates over time may be due to use of CT angiography to select appropriate valve sizes for patients and continued expansion of the self-expanding frame over time. "That’s a remarkable finding, and it needs to be confirmed," Dr. Popma said.
The study focused on patients whose severe frailty, comorbidity, or disability put them at extreme risk of at least a 50% chance of death or irreversible morbidity within 30 days had they undergone surgical aortic valve replacement. A second U.S. pivotal trial of the CoreValve is focusing on patients at high (but not extreme) risk.
Most of the sites in the study had no experience with CoreValve before this study, Dr. Michael J. Mack noted at a press briefing. "The results are outstanding, but especially putting it in that light," said Dr. Mack, a member of the steering committee for the PARTNER trial.
Dr. Popma reported financial ties with Medtronic, which sponsored the study and makes CoreValve.
Major finding: The rate of all-cause mortality or stroke at 1 year was 26%, compared with an objective performance goal of 43%.
Data source: Study of registry data on 487 patients with symptomatic severe aortic stenosis and attempted CoreValve implantation via iliofemoral access.
Disclosures: Dr. Popma reported financial associations with Medtronic, which sponsored the study and makes CoreValve, and with six other companies.
Ten-year outcomes for ablation in atrial fibrillation impressive
DALLAS - At 10 years after their procedures, the rate of freedom from atrial fibrillation and atrial tachycardia was 87% in 513 patients who underwent pulmonary vein antrum isolation for drug-refractory paroxysmal atrial fibrillation at a single high-volume center in Texas.
After a single radiofrequency ablation procedure, 59% of patients remained arrhythmia free for the full decade and another 28% of the cohort was rendered arrhythmia free after an average of two repeat ablation procedures, Dr. Pasquale Santangeli reported at the American Heart Association scientific sessions.
A particularly striking finding in this series was the low 4% rate of recurrent atrial arrhythmias during years 3-6 of follow-up, and the 5% rate between years 6 and 10. Those late recurrence rates are much lower than those in previous reports from other centers. The likely explanation lies in the fact that electrophysiologists at the Austin center routinely extended their pulmonary vein antrum isolation to the posterior wall and performed empiric isolation of the superior vena cava in all patients. Other centers reporting long-term outcomes generally performed segmental or less extensive antral isolation, observed Dr. Santangeli of the Texas Cardiac Arrhythmia Institute at St. David?s Medical Center in Austin, Tex., and the University of Foggia (Italy).
Follow-up, including Holter monitoring, was performed every 3 months during year 1 and every 6-9 months thereafter. The rate of recurrent atrial arrhythmia was 21% at 1 year and 11% during years 1-3.
All patients with a recurrence were offered a repeat procedure, and 74% of them underwent repeat ablation. Reconnection in the pulmonary vein antrum was found in 31% of patients at the time of their first repeat procedure and in no patients who underwent a second repeat ablation.
Patients with recurrent atrial arrhythmia after two failed procedures underwent a high-dose isoproterenol challenge to identify nonpulmonary vein triggers, which were then targeted for ablation. The predictors of very late recurrence due to nonpulmonary vein triggers were increased left atrial size, obesity, and female gender.
Dr. Santangeli reported having no financial conflicts in connection with this study, which was honored as the top presentation by an early career investigator in the core area of heart rhythm disorders and resuscitation science at the annual meeting.
DALLAS - At 10 years after their procedures, the rate of freedom from atrial fibrillation and atrial tachycardia was 87% in 513 patients who underwent pulmonary vein antrum isolation for drug-refractory paroxysmal atrial fibrillation at a single high-volume center in Texas.
After a single radiofrequency ablation procedure, 59% of patients remained arrhythmia free for the full decade and another 28% of the cohort was rendered arrhythmia free after an average of two repeat ablation procedures, Dr. Pasquale Santangeli reported at the American Heart Association scientific sessions.
A particularly striking finding in this series was the low 4% rate of recurrent atrial arrhythmias during years 3-6 of follow-up, and the 5% rate between years 6 and 10. Those late recurrence rates are much lower than those in previous reports from other centers. The likely explanation lies in the fact that electrophysiologists at the Austin center routinely extended their pulmonary vein antrum isolation to the posterior wall and performed empiric isolation of the superior vena cava in all patients. Other centers reporting long-term outcomes generally performed segmental or less extensive antral isolation, observed Dr. Santangeli of the Texas Cardiac Arrhythmia Institute at St. David?s Medical Center in Austin, Tex., and the University of Foggia (Italy).
Follow-up, including Holter monitoring, was performed every 3 months during year 1 and every 6-9 months thereafter. The rate of recurrent atrial arrhythmia was 21% at 1 year and 11% during years 1-3.
All patients with a recurrence were offered a repeat procedure, and 74% of them underwent repeat ablation. Reconnection in the pulmonary vein antrum was found in 31% of patients at the time of their first repeat procedure and in no patients who underwent a second repeat ablation.
Patients with recurrent atrial arrhythmia after two failed procedures underwent a high-dose isoproterenol challenge to identify nonpulmonary vein triggers, which were then targeted for ablation. The predictors of very late recurrence due to nonpulmonary vein triggers were increased left atrial size, obesity, and female gender.
Dr. Santangeli reported having no financial conflicts in connection with this study, which was honored as the top presentation by an early career investigator in the core area of heart rhythm disorders and resuscitation science at the annual meeting.
DALLAS - At 10 years after their procedures, the rate of freedom from atrial fibrillation and atrial tachycardia was 87% in 513 patients who underwent pulmonary vein antrum isolation for drug-refractory paroxysmal atrial fibrillation at a single high-volume center in Texas.
After a single radiofrequency ablation procedure, 59% of patients remained arrhythmia free for the full decade and another 28% of the cohort was rendered arrhythmia free after an average of two repeat ablation procedures, Dr. Pasquale Santangeli reported at the American Heart Association scientific sessions.
A particularly striking finding in this series was the low 4% rate of recurrent atrial arrhythmias during years 3-6 of follow-up, and the 5% rate between years 6 and 10. Those late recurrence rates are much lower than those in previous reports from other centers. The likely explanation lies in the fact that electrophysiologists at the Austin center routinely extended their pulmonary vein antrum isolation to the posterior wall and performed empiric isolation of the superior vena cava in all patients. Other centers reporting long-term outcomes generally performed segmental or less extensive antral isolation, observed Dr. Santangeli of the Texas Cardiac Arrhythmia Institute at St. David?s Medical Center in Austin, Tex., and the University of Foggia (Italy).
Follow-up, including Holter monitoring, was performed every 3 months during year 1 and every 6-9 months thereafter. The rate of recurrent atrial arrhythmia was 21% at 1 year and 11% during years 1-3.
All patients with a recurrence were offered a repeat procedure, and 74% of them underwent repeat ablation. Reconnection in the pulmonary vein antrum was found in 31% of patients at the time of their first repeat procedure and in no patients who underwent a second repeat ablation.
Patients with recurrent atrial arrhythmia after two failed procedures underwent a high-dose isoproterenol challenge to identify nonpulmonary vein triggers, which were then targeted for ablation. The predictors of very late recurrence due to nonpulmonary vein triggers were increased left atrial size, obesity, and female gender.
Dr. Santangeli reported having no financial conflicts in connection with this study, which was honored as the top presentation by an early career investigator in the core area of heart rhythm disorders and resuscitation science at the annual meeting.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: A decade after 513 patients underwent extensive pulmonary vein antrum isolation for drug-resistant paroxysmal atrial fibrillation, 87% were free of atrial fibrillation/atrial tachycardia, including 59% with single-procedure arrhythmia-free survival.
Data source: A retrospective case series involving 513 patients who underwent pulmonary vein antrum isolation during 2000-2002 at a single high-volume center.
Disclosures: The presenter reported having no financial conflicts.
Transradial PCI seems feasible in women
SAN FRANCISCO – Rates of bleeding or vascular complications in women undergoing percutaneous coronary intervention were 59% lower using radial access, compared with femoral access, a difference that did not reach statistical significance in a randomized study of 1,787 patients.
Bleeding or vascular complications within 72 hours or at hospital discharge were seen in 1.2% of 345 women who had transradial percutaneous coronary intervention (PCI) and 2.9% of 345 women who had transfemoral PCI, Dr. Sunil V. Rao reported at the Trans-catheter Cardiovascular Therapeutics annual meeting.
Although that difference was not statistically significant in this prespecified analysis of patients who actually underwent PCI, the rate of bleeding and vascular complications was significantly lower for the group randomized to radial access in an analysis of the whole cohort, regardless of whether they had PCI or just diagnostic catheterization. Bleeding and vascular complication rates were 0.6% in those randomized to radial access and 1.7% in those randomized to femoral access.
In both the PCI cohort and the total cohort, significantly more women in the radial group needed to cross over to femoral access for PCI compared with the crossover rate in the femoral group. In the PCI cohort, 6.1% of the radial group crossed over, as did 1.7% of the femoral group. In the total cohort, crossover was needed in 6.7% of the radial group and 1.9% of the femoral group, said Dr. Rao of Duke University, Durham, N.C. The main reason for crossover from radial to femoral access was radial artery spasm, in 43% of cases.
The Study of Access Site for Enhancement of PCI for Women (SAFE-PCI) leveraged data from the National Cardiovascular Data Registry’s CathPCI Registry from 60 institutions on adult women undergoing elective or urgent PCI or undergoing diagnostic angiography to evaluate ischemic symptoms with the possibility of PCI. The primary outcome measure was Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding events and vascular complications requiring intervention.
The investigators had planned to randomize 3,000 women to obtain 1,800 who underwent PCI, but a routine review after randomizing 1,120 patients suggested that the trial would be too small to show a difference because of lower-than-expected bleeding rates. Because no harm was noted in either the radial or femoral group, the investigators continued until they had enough patients for a quality-of-life substudy, then prematurely discontinued the trial.
The reduction in bleeding with the radial approach was similar to reductions seen in previous studies, Dr. Rao said at the meeting, cosponsored by the American College of Cardiology. The conversion rate from radial to femoral access was similar to the 7.6% rate reported in a prior trial (Lancet 2011;377:1409-20).
Compared with men, women have an increased risk for bleeding from antithrombotic therapy and from femoral access for PCI. Radial access can decrease bleeding risk, but trans-radial PCI has been less common in women, in part because they have smaller radial arteries.
The current trial’s results suggest that "an initial strategy of radial access is reasonable and may be preferred by some operators for women undergoing cardiac catheterization or PCI, with the recognition that a proportion of patients will require conversion to femoral access," he said.
Women preferred the radial approach over femoral access in the study, he added.
The results could be looked at as a glass half empty or half full, Dr. Roxana Mehran said as the discussant of the study at the meeting. She served on the executive committee of the SAFE-PCI trial.
In the eyes of a purist statistician, the results show no significant evidence that radial access prevents bleeding or vascular complications, the primary endpoint, said Dr. Mehran, professor of medicine and director of interventional cardiovascular research at Mount Sinai School of Medicine, New York.
From a clinician’s viewpoint, however, the estimates of benefit from radial access in the overall cohort and the PCI cohort were similar, yielding approximately a 60% reduction in bleeding with radial access, she noted. "The study provides evidence, albeit not conclusive, for greater efficacy with radial access in women," she said.
The crossover rates suggest that for every bleeding event or vascular complication prevented in the radial access group, three patients would cross over. "While there’s a higher crossover from [the] radial to the femoral approach, it’s reasonable and intuitive to begin with the radial approach in women," she said, "especially in those women at high risk for bleeding."
Dr. Rao has been a consultant for the Medicines Co., which helped fund the trial, and for AstraZeneca. Dr. Mehran reported financial associations with these companies and with Abbott Vascular and Daiichi-Sankyo/Eli Lilly & Co., which also funded the trial. Other funders of the study included Terumo Medical, Medtronic, ACIST Medical Systems, and Guerbet. Dr. Mehran also reported financial associations with nine other medical companies.
I don’t think we have the data to say that this is a positive study or that we should change our practice because of these results. It’s an incomplete study, so we really don’t have the data. We need to think about why we didn’t have the anticipated enrollment and why the bleeding rate was lower than expected in the femoral access group. Those are the things that I think led to the futility. But it’s not really a negative trial. We simply don’t know whether radial access will be better in high-risk women undergoing PCI. It’s promising, and it makes all the sense in the world because of the bleeding risk in women.
Dr. Alice K. Jacobs is a professor of medicine and director of the cardiac catheterization laboratory and interventional cardiology at Boston University. She gave these remarks at a press briefing. Dr. Jacobs reported having no relevant financial disclosures.
I don’t think we have the data to say that this is a positive study or that we should change our practice because of these results. It’s an incomplete study, so we really don’t have the data. We need to think about why we didn’t have the anticipated enrollment and why the bleeding rate was lower than expected in the femoral access group. Those are the things that I think led to the futility. But it’s not really a negative trial. We simply don’t know whether radial access will be better in high-risk women undergoing PCI. It’s promising, and it makes all the sense in the world because of the bleeding risk in women.
Dr. Alice K. Jacobs is a professor of medicine and director of the cardiac catheterization laboratory and interventional cardiology at Boston University. She gave these remarks at a press briefing. Dr. Jacobs reported having no relevant financial disclosures.
I don’t think we have the data to say that this is a positive study or that we should change our practice because of these results. It’s an incomplete study, so we really don’t have the data. We need to think about why we didn’t have the anticipated enrollment and why the bleeding rate was lower than expected in the femoral access group. Those are the things that I think led to the futility. But it’s not really a negative trial. We simply don’t know whether radial access will be better in high-risk women undergoing PCI. It’s promising, and it makes all the sense in the world because of the bleeding risk in women.
Dr. Alice K. Jacobs is a professor of medicine and director of the cardiac catheterization laboratory and interventional cardiology at Boston University. She gave these remarks at a press briefing. Dr. Jacobs reported having no relevant financial disclosures.
SAN FRANCISCO – Rates of bleeding or vascular complications in women undergoing percutaneous coronary intervention were 59% lower using radial access, compared with femoral access, a difference that did not reach statistical significance in a randomized study of 1,787 patients.
Bleeding or vascular complications within 72 hours or at hospital discharge were seen in 1.2% of 345 women who had transradial percutaneous coronary intervention (PCI) and 2.9% of 345 women who had transfemoral PCI, Dr. Sunil V. Rao reported at the Trans-catheter Cardiovascular Therapeutics annual meeting.
Although that difference was not statistically significant in this prespecified analysis of patients who actually underwent PCI, the rate of bleeding and vascular complications was significantly lower for the group randomized to radial access in an analysis of the whole cohort, regardless of whether they had PCI or just diagnostic catheterization. Bleeding and vascular complication rates were 0.6% in those randomized to radial access and 1.7% in those randomized to femoral access.
In both the PCI cohort and the total cohort, significantly more women in the radial group needed to cross over to femoral access for PCI compared with the crossover rate in the femoral group. In the PCI cohort, 6.1% of the radial group crossed over, as did 1.7% of the femoral group. In the total cohort, crossover was needed in 6.7% of the radial group and 1.9% of the femoral group, said Dr. Rao of Duke University, Durham, N.C. The main reason for crossover from radial to femoral access was radial artery spasm, in 43% of cases.
The Study of Access Site for Enhancement of PCI for Women (SAFE-PCI) leveraged data from the National Cardiovascular Data Registry’s CathPCI Registry from 60 institutions on adult women undergoing elective or urgent PCI or undergoing diagnostic angiography to evaluate ischemic symptoms with the possibility of PCI. The primary outcome measure was Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding events and vascular complications requiring intervention.
The investigators had planned to randomize 3,000 women to obtain 1,800 who underwent PCI, but a routine review after randomizing 1,120 patients suggested that the trial would be too small to show a difference because of lower-than-expected bleeding rates. Because no harm was noted in either the radial or femoral group, the investigators continued until they had enough patients for a quality-of-life substudy, then prematurely discontinued the trial.
The reduction in bleeding with the radial approach was similar to reductions seen in previous studies, Dr. Rao said at the meeting, cosponsored by the American College of Cardiology. The conversion rate from radial to femoral access was similar to the 7.6% rate reported in a prior trial (Lancet 2011;377:1409-20).
Compared with men, women have an increased risk for bleeding from antithrombotic therapy and from femoral access for PCI. Radial access can decrease bleeding risk, but trans-radial PCI has been less common in women, in part because they have smaller radial arteries.
The current trial’s results suggest that "an initial strategy of radial access is reasonable and may be preferred by some operators for women undergoing cardiac catheterization or PCI, with the recognition that a proportion of patients will require conversion to femoral access," he said.
Women preferred the radial approach over femoral access in the study, he added.
The results could be looked at as a glass half empty or half full, Dr. Roxana Mehran said as the discussant of the study at the meeting. She served on the executive committee of the SAFE-PCI trial.
In the eyes of a purist statistician, the results show no significant evidence that radial access prevents bleeding or vascular complications, the primary endpoint, said Dr. Mehran, professor of medicine and director of interventional cardiovascular research at Mount Sinai School of Medicine, New York.
From a clinician’s viewpoint, however, the estimates of benefit from radial access in the overall cohort and the PCI cohort were similar, yielding approximately a 60% reduction in bleeding with radial access, she noted. "The study provides evidence, albeit not conclusive, for greater efficacy with radial access in women," she said.
The crossover rates suggest that for every bleeding event or vascular complication prevented in the radial access group, three patients would cross over. "While there’s a higher crossover from [the] radial to the femoral approach, it’s reasonable and intuitive to begin with the radial approach in women," she said, "especially in those women at high risk for bleeding."
Dr. Rao has been a consultant for the Medicines Co., which helped fund the trial, and for AstraZeneca. Dr. Mehran reported financial associations with these companies and with Abbott Vascular and Daiichi-Sankyo/Eli Lilly & Co., which also funded the trial. Other funders of the study included Terumo Medical, Medtronic, ACIST Medical Systems, and Guerbet. Dr. Mehran also reported financial associations with nine other medical companies.
SAN FRANCISCO – Rates of bleeding or vascular complications in women undergoing percutaneous coronary intervention were 59% lower using radial access, compared with femoral access, a difference that did not reach statistical significance in a randomized study of 1,787 patients.
Bleeding or vascular complications within 72 hours or at hospital discharge were seen in 1.2% of 345 women who had transradial percutaneous coronary intervention (PCI) and 2.9% of 345 women who had transfemoral PCI, Dr. Sunil V. Rao reported at the Trans-catheter Cardiovascular Therapeutics annual meeting.
Although that difference was not statistically significant in this prespecified analysis of patients who actually underwent PCI, the rate of bleeding and vascular complications was significantly lower for the group randomized to radial access in an analysis of the whole cohort, regardless of whether they had PCI or just diagnostic catheterization. Bleeding and vascular complication rates were 0.6% in those randomized to radial access and 1.7% in those randomized to femoral access.
In both the PCI cohort and the total cohort, significantly more women in the radial group needed to cross over to femoral access for PCI compared with the crossover rate in the femoral group. In the PCI cohort, 6.1% of the radial group crossed over, as did 1.7% of the femoral group. In the total cohort, crossover was needed in 6.7% of the radial group and 1.9% of the femoral group, said Dr. Rao of Duke University, Durham, N.C. The main reason for crossover from radial to femoral access was radial artery spasm, in 43% of cases.
The Study of Access Site for Enhancement of PCI for Women (SAFE-PCI) leveraged data from the National Cardiovascular Data Registry’s CathPCI Registry from 60 institutions on adult women undergoing elective or urgent PCI or undergoing diagnostic angiography to evaluate ischemic symptoms with the possibility of PCI. The primary outcome measure was Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding events and vascular complications requiring intervention.
The investigators had planned to randomize 3,000 women to obtain 1,800 who underwent PCI, but a routine review after randomizing 1,120 patients suggested that the trial would be too small to show a difference because of lower-than-expected bleeding rates. Because no harm was noted in either the radial or femoral group, the investigators continued until they had enough patients for a quality-of-life substudy, then prematurely discontinued the trial.
The reduction in bleeding with the radial approach was similar to reductions seen in previous studies, Dr. Rao said at the meeting, cosponsored by the American College of Cardiology. The conversion rate from radial to femoral access was similar to the 7.6% rate reported in a prior trial (Lancet 2011;377:1409-20).
Compared with men, women have an increased risk for bleeding from antithrombotic therapy and from femoral access for PCI. Radial access can decrease bleeding risk, but trans-radial PCI has been less common in women, in part because they have smaller radial arteries.
The current trial’s results suggest that "an initial strategy of radial access is reasonable and may be preferred by some operators for women undergoing cardiac catheterization or PCI, with the recognition that a proportion of patients will require conversion to femoral access," he said.
Women preferred the radial approach over femoral access in the study, he added.
The results could be looked at as a glass half empty or half full, Dr. Roxana Mehran said as the discussant of the study at the meeting. She served on the executive committee of the SAFE-PCI trial.
In the eyes of a purist statistician, the results show no significant evidence that radial access prevents bleeding or vascular complications, the primary endpoint, said Dr. Mehran, professor of medicine and director of interventional cardiovascular research at Mount Sinai School of Medicine, New York.
From a clinician’s viewpoint, however, the estimates of benefit from radial access in the overall cohort and the PCI cohort were similar, yielding approximately a 60% reduction in bleeding with radial access, she noted. "The study provides evidence, albeit not conclusive, for greater efficacy with radial access in women," she said.
The crossover rates suggest that for every bleeding event or vascular complication prevented in the radial access group, three patients would cross over. "While there’s a higher crossover from [the] radial to the femoral approach, it’s reasonable and intuitive to begin with the radial approach in women," she said, "especially in those women at high risk for bleeding."
Dr. Rao has been a consultant for the Medicines Co., which helped fund the trial, and for AstraZeneca. Dr. Mehran reported financial associations with these companies and with Abbott Vascular and Daiichi-Sankyo/Eli Lilly & Co., which also funded the trial. Other funders of the study included Terumo Medical, Medtronic, ACIST Medical Systems, and Guerbet. Dr. Mehran also reported financial associations with nine other medical companies.
Major finding: Rates of bleeding or vascular complications were 1.2% using radial access and 2.9% using femoral access in the PCI subgroup and 6.7% and 1.9%, respectively, in the entire cohort.
Data source: A randomized study of 1,787 women undergoing definite or possible PCI at 60 institutions.
Disclosures: Dr. Rao has been a consultant for the Medicines Co., which helped fund the trial, and for AstraZeneca. Dr. Mehran reported financial associations with these companies and with Abbott Vascular and Daiichi-Sankyo/Eli Lilly & Co., which also funded the trial. Other funders of the study included Abbott Vascular, Daiichi-Sankyo/Eli Lilly & Co., Terumo Medical, Medtronic, ACIST Medical Systems, and Guerbet. Dr. Mehran also reported financial associations with nine other medical companies.
How to foil post-CABG aspirin resistance
AMSTERDAM (IMNG) – Giving low-dose aspirin four times per day in the first days after coronary artery bypass graft surgery suppresses serum thromboxane levels far more effectively than does conventional once-daily dosing at 325 mg, according to a randomized trial.
The clinical implication of this finding is that more frequent dosing of aspirin may prevent the serious problem of premature vein graft failure from the development of aspirin resistance in the postoperative period, although at this point this is a hypothesis that requires testing in a future study, Dr. Jeremy S. Paikin said at the annual congress of the European Society of Cardiology.
He reported on 110 on-pump coronary artery bypass graft (CABG) patients randomized on postoperative day 1 to aspirin either at 81 mg four times daily, the standard 325 mg once daily, or to 81 mg once daily.
The primary study endpoint was the serum thromboxane level on the morning of postoperative day 4. The median level was 13.3 ng/mL in the group on aspirin at 81 mg once daily, 3.4 ng/mL with 325 mg once daily, and significantly lower at 1.1 ng/mL in patients on 81 mg four times daily.
"With 81 mg QD [four times daily], there’s almost complete suppression of serum thromboxane throughout the course of the hospital stay," according to Dr. Paikin of McMaster University, Hamilton, Ont.
Aspirin is known to prevent CABG graft failure, but its effectiveness is limited by the not-infrequent development of aspirin hyporesponsiveness in the postoperative period. The underlying mechanism involved in this aspirin resistance was previously unknown; however, in their randomized trial Dr. Paikin and coinvestigators established that the hyporesponsiveness is caused at least in part by increased platelet turnover in the postoperative period. The investigators showed that platelet turnover per day was increased two- to threefold in the week after CABG, compared with presurgical levels, a finding Dr. Paikin termed "quite exciting."
Recognizing that administration of any drug four times daily raises formidable adherence obstacles, he and his coworkers are just about to start a clinical trial looking at twice-daily aspirin dosing post CABG. They’re also interested in drawing a firm evidentiary connection between serum thromboxane levels and risk of premature graft failure.
Dr. Paikin reported having no financial conflicts of interest.
AMSTERDAM (IMNG) – Giving low-dose aspirin four times per day in the first days after coronary artery bypass graft surgery suppresses serum thromboxane levels far more effectively than does conventional once-daily dosing at 325 mg, according to a randomized trial.
The clinical implication of this finding is that more frequent dosing of aspirin may prevent the serious problem of premature vein graft failure from the development of aspirin resistance in the postoperative period, although at this point this is a hypothesis that requires testing in a future study, Dr. Jeremy S. Paikin said at the annual congress of the European Society of Cardiology.
He reported on 110 on-pump coronary artery bypass graft (CABG) patients randomized on postoperative day 1 to aspirin either at 81 mg four times daily, the standard 325 mg once daily, or to 81 mg once daily.
The primary study endpoint was the serum thromboxane level on the morning of postoperative day 4. The median level was 13.3 ng/mL in the group on aspirin at 81 mg once daily, 3.4 ng/mL with 325 mg once daily, and significantly lower at 1.1 ng/mL in patients on 81 mg four times daily.
"With 81 mg QD [four times daily], there’s almost complete suppression of serum thromboxane throughout the course of the hospital stay," according to Dr. Paikin of McMaster University, Hamilton, Ont.
Aspirin is known to prevent CABG graft failure, but its effectiveness is limited by the not-infrequent development of aspirin hyporesponsiveness in the postoperative period. The underlying mechanism involved in this aspirin resistance was previously unknown; however, in their randomized trial Dr. Paikin and coinvestigators established that the hyporesponsiveness is caused at least in part by increased platelet turnover in the postoperative period. The investigators showed that platelet turnover per day was increased two- to threefold in the week after CABG, compared with presurgical levels, a finding Dr. Paikin termed "quite exciting."
Recognizing that administration of any drug four times daily raises formidable adherence obstacles, he and his coworkers are just about to start a clinical trial looking at twice-daily aspirin dosing post CABG. They’re also interested in drawing a firm evidentiary connection between serum thromboxane levels and risk of premature graft failure.
Dr. Paikin reported having no financial conflicts of interest.
AMSTERDAM (IMNG) – Giving low-dose aspirin four times per day in the first days after coronary artery bypass graft surgery suppresses serum thromboxane levels far more effectively than does conventional once-daily dosing at 325 mg, according to a randomized trial.
The clinical implication of this finding is that more frequent dosing of aspirin may prevent the serious problem of premature vein graft failure from the development of aspirin resistance in the postoperative period, although at this point this is a hypothesis that requires testing in a future study, Dr. Jeremy S. Paikin said at the annual congress of the European Society of Cardiology.
He reported on 110 on-pump coronary artery bypass graft (CABG) patients randomized on postoperative day 1 to aspirin either at 81 mg four times daily, the standard 325 mg once daily, or to 81 mg once daily.
The primary study endpoint was the serum thromboxane level on the morning of postoperative day 4. The median level was 13.3 ng/mL in the group on aspirin at 81 mg once daily, 3.4 ng/mL with 325 mg once daily, and significantly lower at 1.1 ng/mL in patients on 81 mg four times daily.
"With 81 mg QD [four times daily], there’s almost complete suppression of serum thromboxane throughout the course of the hospital stay," according to Dr. Paikin of McMaster University, Hamilton, Ont.
Aspirin is known to prevent CABG graft failure, but its effectiveness is limited by the not-infrequent development of aspirin hyporesponsiveness in the postoperative period. The underlying mechanism involved in this aspirin resistance was previously unknown; however, in their randomized trial Dr. Paikin and coinvestigators established that the hyporesponsiveness is caused at least in part by increased platelet turnover in the postoperative period. The investigators showed that platelet turnover per day was increased two- to threefold in the week after CABG, compared with presurgical levels, a finding Dr. Paikin termed "quite exciting."
Recognizing that administration of any drug four times daily raises formidable adherence obstacles, he and his coworkers are just about to start a clinical trial looking at twice-daily aspirin dosing post CABG. They’re also interested in drawing a firm evidentiary connection between serum thromboxane levels and risk of premature graft failure.
Dr. Paikin reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2013
Major finding: The median serum thromboxane level on the morning of post CABG day 4 was 13.3 ng/mL in the group on aspirin at 81 mg once daily, 3.4 ng/mL with 325 mg once daily, and significantly lower at 1.1 ng/mL in patients on 81 mg four times daily.
Data source: A randomized clinical trial in which 110 patients who underwent on-pump CABG surgery were randomized on postoperative day 1 to aspirin at either 81 mg four times daily, 325 mg once daily, or 81 mg once daily.
Disclosures: The study presenter reported having no financial conflicts.
Losartan effective in Marfan syndrome
AMSTERDAM – Daily losartan significantly slowed the aortic root dilatation rate in adults with Marfan syndrome in a 3-year randomized clinical trial.
"I think we can be positive about this treatment. We can now recommend losartan in clinical practice," Dr. Maarten Groenink said at the annual congress of the European Society of Cardiology.
The COMPARE (Cozaar in Marfan Patients Reduces Aortic Enlargement) trial included 218 patients at all four university Marfan centers in the Netherlands. Patients were randomized to oral losartan at a target dose of 100 mg/day or no losartan in addition to standard-of-care treatment with beta-blockers. Roughly half of the patients in the losartan group were unable to tolerate the full dose of losartan in addition to a beta-blocker; those patients were maintained on losartan at 50 mg/day. Aortic root diameter was measured by MRI at enrollment and after 3 years of prospective follow-up. The aortic dilatation rate was significantly lower in the losartan group than in controls both in the patients with a native root and in those who had undergone aortic root replacement surgery, reported Dr. Groenink, a cardiologist at the Academic Medical Center, Amsterdam.
There were no aortic dissections in the losartan group and two in the control arm. Elective aortic replacement surgery was performed in a similar number of patients in both groups.
Blood pressure was lower in the losartan group, yet blood pressure didn’t correlate with the aortic dilatation rate. Dr. Groenink speculated that losartan’s chief mechanism of benefit in Marfan syndrome is its ability to curb overexpression of transforming growth factor-beta, which weakens the structure of the media layer of the aortic wall. He said it’s unknown whether losartan’s benefits are specific to that drug or are a class effect.
Ongoing clinical trials are evaluating losartan in children and adolescents with Marfan syndrome, he said, adding that there is a solid rationale for beginning treatment as early in life as possible. "I believe the adverse effects on the aortic wall in Marfan syndrome are caused by the fibrillin defect but also by wear and tear due to cyclic stress by the beating heart. So you can hypothesize that the earlier you start treatment, the better," he explained.
The prevalence of Marfan syndrome has been estimated at 1 in 5,000, but Dr. Groenink suspects the syndrome may actually be more common than that.
Simultaneous with Dr. Groenink’s presentation at the ESC, the COMPARE results were published online (Eur. Heart J. 2013 [doi:10.1093/eurheartj/eht334]).
Dr. Groenink reported having no disclosures.

|
| Dr. John Gordon Harold |
COMPARE is a very important study whose results are going to mean a paradigm shift for the management of Marfan syndrome.
It is intriguing to consider that the benefits of losartan might possibly also extend to patients with thoracic aortic disease in general, a worthy topic for future investigation.
Dr. John Gordon Harold is with Cedars-Sinai Heart Institute, Los Angeles, and president of the American College of Cardiology. He had no relevant financial disclosures.

|
| Dr. John Gordon Harold |
COMPARE is a very important study whose results are going to mean a paradigm shift for the management of Marfan syndrome.
It is intriguing to consider that the benefits of losartan might possibly also extend to patients with thoracic aortic disease in general, a worthy topic for future investigation.
Dr. John Gordon Harold is with Cedars-Sinai Heart Institute, Los Angeles, and president of the American College of Cardiology. He had no relevant financial disclosures.

|
| Dr. John Gordon Harold |
COMPARE is a very important study whose results are going to mean a paradigm shift for the management of Marfan syndrome.
It is intriguing to consider that the benefits of losartan might possibly also extend to patients with thoracic aortic disease in general, a worthy topic for future investigation.
Dr. John Gordon Harold is with Cedars-Sinai Heart Institute, Los Angeles, and president of the American College of Cardiology. He had no relevant financial disclosures.
AMSTERDAM – Daily losartan significantly slowed the aortic root dilatation rate in adults with Marfan syndrome in a 3-year randomized clinical trial.
"I think we can be positive about this treatment. We can now recommend losartan in clinical practice," Dr. Maarten Groenink said at the annual congress of the European Society of Cardiology.
The COMPARE (Cozaar in Marfan Patients Reduces Aortic Enlargement) trial included 218 patients at all four university Marfan centers in the Netherlands. Patients were randomized to oral losartan at a target dose of 100 mg/day or no losartan in addition to standard-of-care treatment with beta-blockers. Roughly half of the patients in the losartan group were unable to tolerate the full dose of losartan in addition to a beta-blocker; those patients were maintained on losartan at 50 mg/day. Aortic root diameter was measured by MRI at enrollment and after 3 years of prospective follow-up. The aortic dilatation rate was significantly lower in the losartan group than in controls both in the patients with a native root and in those who had undergone aortic root replacement surgery, reported Dr. Groenink, a cardiologist at the Academic Medical Center, Amsterdam.
There were no aortic dissections in the losartan group and two in the control arm. Elective aortic replacement surgery was performed in a similar number of patients in both groups.
Blood pressure was lower in the losartan group, yet blood pressure didn’t correlate with the aortic dilatation rate. Dr. Groenink speculated that losartan’s chief mechanism of benefit in Marfan syndrome is its ability to curb overexpression of transforming growth factor-beta, which weakens the structure of the media layer of the aortic wall. He said it’s unknown whether losartan’s benefits are specific to that drug or are a class effect.
Ongoing clinical trials are evaluating losartan in children and adolescents with Marfan syndrome, he said, adding that there is a solid rationale for beginning treatment as early in life as possible. "I believe the adverse effects on the aortic wall in Marfan syndrome are caused by the fibrillin defect but also by wear and tear due to cyclic stress by the beating heart. So you can hypothesize that the earlier you start treatment, the better," he explained.
The prevalence of Marfan syndrome has been estimated at 1 in 5,000, but Dr. Groenink suspects the syndrome may actually be more common than that.
Simultaneous with Dr. Groenink’s presentation at the ESC, the COMPARE results were published online (Eur. Heart J. 2013 [doi:10.1093/eurheartj/eht334]).
Dr. Groenink reported having no disclosures.
AMSTERDAM – Daily losartan significantly slowed the aortic root dilatation rate in adults with Marfan syndrome in a 3-year randomized clinical trial.
"I think we can be positive about this treatment. We can now recommend losartan in clinical practice," Dr. Maarten Groenink said at the annual congress of the European Society of Cardiology.
The COMPARE (Cozaar in Marfan Patients Reduces Aortic Enlargement) trial included 218 patients at all four university Marfan centers in the Netherlands. Patients were randomized to oral losartan at a target dose of 100 mg/day or no losartan in addition to standard-of-care treatment with beta-blockers. Roughly half of the patients in the losartan group were unable to tolerate the full dose of losartan in addition to a beta-blocker; those patients were maintained on losartan at 50 mg/day. Aortic root diameter was measured by MRI at enrollment and after 3 years of prospective follow-up. The aortic dilatation rate was significantly lower in the losartan group than in controls both in the patients with a native root and in those who had undergone aortic root replacement surgery, reported Dr. Groenink, a cardiologist at the Academic Medical Center, Amsterdam.
There were no aortic dissections in the losartan group and two in the control arm. Elective aortic replacement surgery was performed in a similar number of patients in both groups.
Blood pressure was lower in the losartan group, yet blood pressure didn’t correlate with the aortic dilatation rate. Dr. Groenink speculated that losartan’s chief mechanism of benefit in Marfan syndrome is its ability to curb overexpression of transforming growth factor-beta, which weakens the structure of the media layer of the aortic wall. He said it’s unknown whether losartan’s benefits are specific to that drug or are a class effect.
Ongoing clinical trials are evaluating losartan in children and adolescents with Marfan syndrome, he said, adding that there is a solid rationale for beginning treatment as early in life as possible. "I believe the adverse effects on the aortic wall in Marfan syndrome are caused by the fibrillin defect but also by wear and tear due to cyclic stress by the beating heart. So you can hypothesize that the earlier you start treatment, the better," he explained.
The prevalence of Marfan syndrome has been estimated at 1 in 5,000, but Dr. Groenink suspects the syndrome may actually be more common than that.
Simultaneous with Dr. Groenink’s presentation at the ESC, the COMPARE results were published online (Eur. Heart J. 2013 [doi:10.1093/eurheartj/eht334]).
Dr. Groenink reported having no disclosures.
Major finding: The rate of aortic root enlargement during 3 years of prospective follow-up was 0.77 mm in losartan-treated patients with Marfan syndrome, significantly less than the 1.35 mm in patients on standard-of-care treatment with no losartan.
Data source: The COMPARE trial was a randomized, prospective, open-label multicenter study in which 218 patients with Marfan syndrome were randomized to losartan at a target dose of 100 mg or to no losartan and followed for 3 years with the aortic root dilatation rate as measured by MRI the primary endpoint.
Disclosures: The COMPARE trial was supported by the Dutch Heart Association. Dr. Groenink reported having no financial conflicts.
Nix new anticoagulants with mechanical valves
AMSTERDAM -- The complete failure of the oral direct thrombin inhibitor dabigatran in the RE-ALIGN trial spells big trouble for efforts to use the novel oral factor Xa inhibitors for anticoagulation in patients with a mechanical heart valve, RE-ALIGN steering committee cochair Dr. Frans Van de Werf cautioned at the annual congress of the European Society of Cardiology.
"It would not be wise for a cardiologist to prescribe these agents for a patient with a mechanical heart valve," declared Dr. Van de Werf, professor and chairman of the department of cardiovascular medicine at the Catholic University at Leuven (Belgium).
Dabigatran (Pradaxa) is approved as a more effective and convenient alternative to warfarin for prevention of stroke and other systemic embolism in patients with nonvalvular atrial fibrillation. RE-ALIGN (Randomized, Phase II Study to Evaluate the Safety and Pharmacokinetics of Oral Dabigatran Etexilate in Patients After Heart Valve Replacement) was an effort to expand the drug's indications to include prevention of thromboembolic events in patients with mechanical heart valves.
The study was halted prematurely late last year when an interim analysis showed that dabigatran was both less safe and less protective than standard warfarin therapy. Shortly afterward, the Food and Drug Administration and the European regulatory agency warned that dabigatran is contraindicated in patients with mechanical heart valves. Dr. Van de Werf's report in Amsterdam, however, was the first presentation of the actual data.
RE-ALIGN was stopped after 252 patients with mechanical heart valves had been randomized 2:1 to dabigatran or warfarin. Dabigatran dosing was adjusted on the basis of creatinine clearance to achieve a trough plasma level of at least 50 ng/mL.
The study halt came in response to an interim analysis showing a 5% stroke rate in the dabigatran group, compared with 0% with warfarin. This was accompanied by a 4% rate of major bleeding with dabigatran, compared with 2% with warfarin, and a 27% rate of any bleeding with dabigatran versus 12% with warfarin. All dabigatran-treated patients with major bleeding had pericardial bleeding and were in the subgroup of participants who started on the direct thrombin inhibitor within 7 days post surgery.
Other unwelcome outcomes in the interim analysis included a 2% MI rate and 3% rate of valve thrombosis without symptoms in the dabigatran group, versus no such events in the warfarin arm.
"Overall, this study was clearly negative: more thrombotic events and more bleeding complications in spite of adjusting the dose of dabigatran based upon renal function," Dr. Van de Werf observed.
Simultaneous with his presentation of the RE-ALIGN findings at the ESC congress in Amsterdam, the results were published online (N. Engl. J. Med. 2013 Sept. 1 [doi:10.1056/NEJMoa1300615]).
In an accompanying editorial, Dr. Elaine M. Hylek of Boston University said the most likely explanation for the disappointing results in RE-ALIGN was that blood levels of dabigatran were inadequate (N. Engl. J. Med. 2013 Sept. 1 [doi:10.1056/NEJMe1310399]).
Dr. Van de Werf, however, rejected that as unlikely. Given that there were excesses of both thromboembolic and bleeding events, other dosing regimens would surely have sent rates of one type of complication or the other even higher, he argued.
Instead, he and his coinvestigators believe that the most likely explanation for the negative results lies in the differences in the mechanisms of action of dabigatran and warfarin. Dabigatran acts near the tail end of the coagulation cascade, on thrombin. In patients with a mechanical heart valve, thrombin is generated by exposure of blood to the artificial surface of the valve leaflets, activating what is known as the contact pathway of coagulation. Thrombin also is generated by the release of tissue factor from tissues injured during the valve surgery. Warfarin acts at both the contact pathway and tissue injury levels; dabigatran doesn't address either.
The novel oral factor Xa inhibitors don't act at the contact pathway and tissue injury levels, either, which is why Dr. Van de Werf cautioned against their off-label use in patients with a mechanical valve.
Discussant Dr. Alec Vahanian said that he "fully agrees" with Dr. Van de Werf's interpretation that the negative results most likely stemmed from dabigatran's absence of efficacy on the contact pathway.
"It sounds from this study that there is no future for dabigatran with this indication. We should not give this agent to a patient with a mechanical prosthesis, and personally I would extend that further and say we should not give this agent to patients with a bioprosthesis or other high-risk patients with severe valve disease. We don't have the evidence for that yet," said Dr. Vahanian, head of cardiology at Bichat Hospital, Paris.
Patients with a mechanical heart valve constitute a challenging population at extreme thromboembolic risk, but Dr. Vahanian offered a comforting prediction: "We are nearing the end of the era of mechanical prosthetic valves," he declared. "Patients are getting older, bioprostheses are getting better, and valve repair techniques are improving."
Dr. Harry R. Buller took issue with Dr. Van de Werf's blanket prediction that the factor Xa inhibitors will prove similarly unsafe and ineffective in patients with mechanical valves, as was dabigatran.
"We still need to find that out. One molecule of factor Xa generates about 1,000 thrombin molecules, so inhibiting coagulation at the level of Xa might actually be effective. What you see with dabigatran is inhibition at the very last stages of the whole coagulation cascade, when there are millions and millions of molecules of thrombin. That's quite difficult. If you do it higher up in the cascade it might work," argued Dr. Buller, chairman of the department of vascular medicine at the Academic Medical Center, Amsterdam.
"Would you take that risk?" challenged Dr. Van de Werf.
"I know there are people taking that risk. I love studies; I would study it," Dr. Buller replied.
Session cochair Dr. Keith A.A. Fox of the University of Edinburgh posed a provocative question to Dr. Van de Werf: "Would you extrapolate these RE-ALIGN data to a patient in atrial fibrillation with a bioprosthetic valve?"
"It's a difficult question," Dr. Van de Werf replied. "In principle, you could give one of the novel anticoagulants approved for atrial fibrillation, including dabigatran, because it is assumed there is no indication for oral anticoagulation for the bioprosthetic valve. I'm not saying you necessarily should do that. If the patient is doing well on warfarin, I don't see the need to switch to one of the new anticoagulants."
RE-ALIGN was supported by Boehringer Ingelheim. Dr. Van de Werf reported receiving research grants and speakers' fees from the company. Dr. Buller, Dr. Fox, and Dr. Vahanian reported no relevant financial interests.
AMSTERDAM -- The complete failure of the oral direct thrombin inhibitor dabigatran in the RE-ALIGN trial spells big trouble for efforts to use the novel oral factor Xa inhibitors for anticoagulation in patients with a mechanical heart valve, RE-ALIGN steering committee cochair Dr. Frans Van de Werf cautioned at the annual congress of the European Society of Cardiology.
"It would not be wise for a cardiologist to prescribe these agents for a patient with a mechanical heart valve," declared Dr. Van de Werf, professor and chairman of the department of cardiovascular medicine at the Catholic University at Leuven (Belgium).
Dabigatran (Pradaxa) is approved as a more effective and convenient alternative to warfarin for prevention of stroke and other systemic embolism in patients with nonvalvular atrial fibrillation. RE-ALIGN (Randomized, Phase II Study to Evaluate the Safety and Pharmacokinetics of Oral Dabigatran Etexilate in Patients After Heart Valve Replacement) was an effort to expand the drug's indications to include prevention of thromboembolic events in patients with mechanical heart valves.
The study was halted prematurely late last year when an interim analysis showed that dabigatran was both less safe and less protective than standard warfarin therapy. Shortly afterward, the Food and Drug Administration and the European regulatory agency warned that dabigatran is contraindicated in patients with mechanical heart valves. Dr. Van de Werf's report in Amsterdam, however, was the first presentation of the actual data.
RE-ALIGN was stopped after 252 patients with mechanical heart valves had been randomized 2:1 to dabigatran or warfarin. Dabigatran dosing was adjusted on the basis of creatinine clearance to achieve a trough plasma level of at least 50 ng/mL.
The study halt came in response to an interim analysis showing a 5% stroke rate in the dabigatran group, compared with 0% with warfarin. This was accompanied by a 4% rate of major bleeding with dabigatran, compared with 2% with warfarin, and a 27% rate of any bleeding with dabigatran versus 12% with warfarin. All dabigatran-treated patients with major bleeding had pericardial bleeding and were in the subgroup of participants who started on the direct thrombin inhibitor within 7 days post surgery.
Other unwelcome outcomes in the interim analysis included a 2% MI rate and 3% rate of valve thrombosis without symptoms in the dabigatran group, versus no such events in the warfarin arm.
"Overall, this study was clearly negative: more thrombotic events and more bleeding complications in spite of adjusting the dose of dabigatran based upon renal function," Dr. Van de Werf observed.
Simultaneous with his presentation of the RE-ALIGN findings at the ESC congress in Amsterdam, the results were published online (N. Engl. J. Med. 2013 Sept. 1 [doi:10.1056/NEJMoa1300615]).
In an accompanying editorial, Dr. Elaine M. Hylek of Boston University said the most likely explanation for the disappointing results in RE-ALIGN was that blood levels of dabigatran were inadequate (N. Engl. J. Med. 2013 Sept. 1 [doi:10.1056/NEJMe1310399]).
Dr. Van de Werf, however, rejected that as unlikely. Given that there were excesses of both thromboembolic and bleeding events, other dosing regimens would surely have sent rates of one type of complication or the other even higher, he argued.
Instead, he and his coinvestigators believe that the most likely explanation for the negative results lies in the differences in the mechanisms of action of dabigatran and warfarin. Dabigatran acts near the tail end of the coagulation cascade, on thrombin. In patients with a mechanical heart valve, thrombin is generated by exposure of blood to the artificial surface of the valve leaflets, activating what is known as the contact pathway of coagulation. Thrombin also is generated by the release of tissue factor from tissues injured during the valve surgery. Warfarin acts at both the contact pathway and tissue injury levels; dabigatran doesn't address either.
The novel oral factor Xa inhibitors don't act at the contact pathway and tissue injury levels, either, which is why Dr. Van de Werf cautioned against their off-label use in patients with a mechanical valve.
Discussant Dr. Alec Vahanian said that he "fully agrees" with Dr. Van de Werf's interpretation that the negative results most likely stemmed from dabigatran's absence of efficacy on the contact pathway.
"It sounds from this study that there is no future for dabigatran with this indication. We should not give this agent to a patient with a mechanical prosthesis, and personally I would extend that further and say we should not give this agent to patients with a bioprosthesis or other high-risk patients with severe valve disease. We don't have the evidence for that yet," said Dr. Vahanian, head of cardiology at Bichat Hospital, Paris.
Patients with a mechanical heart valve constitute a challenging population at extreme thromboembolic risk, but Dr. Vahanian offered a comforting prediction: "We are nearing the end of the era of mechanical prosthetic valves," he declared. "Patients are getting older, bioprostheses are getting better, and valve repair techniques are improving."
Dr. Harry R. Buller took issue with Dr. Van de Werf's blanket prediction that the factor Xa inhibitors will prove similarly unsafe and ineffective in patients with mechanical valves, as was dabigatran.
"We still need to find that out. One molecule of factor Xa generates about 1,000 thrombin molecules, so inhibiting coagulation at the level of Xa might actually be effective. What you see with dabigatran is inhibition at the very last stages of the whole coagulation cascade, when there are millions and millions of molecules of thrombin. That's quite difficult. If you do it higher up in the cascade it might work," argued Dr. Buller, chairman of the department of vascular medicine at the Academic Medical Center, Amsterdam.
"Would you take that risk?" challenged Dr. Van de Werf.
"I know there are people taking that risk. I love studies; I would study it," Dr. Buller replied.
Session cochair Dr. Keith A.A. Fox of the University of Edinburgh posed a provocative question to Dr. Van de Werf: "Would you extrapolate these RE-ALIGN data to a patient in atrial fibrillation with a bioprosthetic valve?"
"It's a difficult question," Dr. Van de Werf replied. "In principle, you could give one of the novel anticoagulants approved for atrial fibrillation, including dabigatran, because it is assumed there is no indication for oral anticoagulation for the bioprosthetic valve. I'm not saying you necessarily should do that. If the patient is doing well on warfarin, I don't see the need to switch to one of the new anticoagulants."
RE-ALIGN was supported by Boehringer Ingelheim. Dr. Van de Werf reported receiving research grants and speakers' fees from the company. Dr. Buller, Dr. Fox, and Dr. Vahanian reported no relevant financial interests.
AMSTERDAM -- The complete failure of the oral direct thrombin inhibitor dabigatran in the RE-ALIGN trial spells big trouble for efforts to use the novel oral factor Xa inhibitors for anticoagulation in patients with a mechanical heart valve, RE-ALIGN steering committee cochair Dr. Frans Van de Werf cautioned at the annual congress of the European Society of Cardiology.
"It would not be wise for a cardiologist to prescribe these agents for a patient with a mechanical heart valve," declared Dr. Van de Werf, professor and chairman of the department of cardiovascular medicine at the Catholic University at Leuven (Belgium).
Dabigatran (Pradaxa) is approved as a more effective and convenient alternative to warfarin for prevention of stroke and other systemic embolism in patients with nonvalvular atrial fibrillation. RE-ALIGN (Randomized, Phase II Study to Evaluate the Safety and Pharmacokinetics of Oral Dabigatran Etexilate in Patients After Heart Valve Replacement) was an effort to expand the drug's indications to include prevention of thromboembolic events in patients with mechanical heart valves.
The study was halted prematurely late last year when an interim analysis showed that dabigatran was both less safe and less protective than standard warfarin therapy. Shortly afterward, the Food and Drug Administration and the European regulatory agency warned that dabigatran is contraindicated in patients with mechanical heart valves. Dr. Van de Werf's report in Amsterdam, however, was the first presentation of the actual data.
RE-ALIGN was stopped after 252 patients with mechanical heart valves had been randomized 2:1 to dabigatran or warfarin. Dabigatran dosing was adjusted on the basis of creatinine clearance to achieve a trough plasma level of at least 50 ng/mL.
The study halt came in response to an interim analysis showing a 5% stroke rate in the dabigatran group, compared with 0% with warfarin. This was accompanied by a 4% rate of major bleeding with dabigatran, compared with 2% with warfarin, and a 27% rate of any bleeding with dabigatran versus 12% with warfarin. All dabigatran-treated patients with major bleeding had pericardial bleeding and were in the subgroup of participants who started on the direct thrombin inhibitor within 7 days post surgery.
Other unwelcome outcomes in the interim analysis included a 2% MI rate and 3% rate of valve thrombosis without symptoms in the dabigatran group, versus no such events in the warfarin arm.
"Overall, this study was clearly negative: more thrombotic events and more bleeding complications in spite of adjusting the dose of dabigatran based upon renal function," Dr. Van de Werf observed.
Simultaneous with his presentation of the RE-ALIGN findings at the ESC congress in Amsterdam, the results were published online (N. Engl. J. Med. 2013 Sept. 1 [doi:10.1056/NEJMoa1300615]).
In an accompanying editorial, Dr. Elaine M. Hylek of Boston University said the most likely explanation for the disappointing results in RE-ALIGN was that blood levels of dabigatran were inadequate (N. Engl. J. Med. 2013 Sept. 1 [doi:10.1056/NEJMe1310399]).
Dr. Van de Werf, however, rejected that as unlikely. Given that there were excesses of both thromboembolic and bleeding events, other dosing regimens would surely have sent rates of one type of complication or the other even higher, he argued.
Instead, he and his coinvestigators believe that the most likely explanation for the negative results lies in the differences in the mechanisms of action of dabigatran and warfarin. Dabigatran acts near the tail end of the coagulation cascade, on thrombin. In patients with a mechanical heart valve, thrombin is generated by exposure of blood to the artificial surface of the valve leaflets, activating what is known as the contact pathway of coagulation. Thrombin also is generated by the release of tissue factor from tissues injured during the valve surgery. Warfarin acts at both the contact pathway and tissue injury levels; dabigatran doesn't address either.
The novel oral factor Xa inhibitors don't act at the contact pathway and tissue injury levels, either, which is why Dr. Van de Werf cautioned against their off-label use in patients with a mechanical valve.
Discussant Dr. Alec Vahanian said that he "fully agrees" with Dr. Van de Werf's interpretation that the negative results most likely stemmed from dabigatran's absence of efficacy on the contact pathway.
"It sounds from this study that there is no future for dabigatran with this indication. We should not give this agent to a patient with a mechanical prosthesis, and personally I would extend that further and say we should not give this agent to patients with a bioprosthesis or other high-risk patients with severe valve disease. We don't have the evidence for that yet," said Dr. Vahanian, head of cardiology at Bichat Hospital, Paris.
Patients with a mechanical heart valve constitute a challenging population at extreme thromboembolic risk, but Dr. Vahanian offered a comforting prediction: "We are nearing the end of the era of mechanical prosthetic valves," he declared. "Patients are getting older, bioprostheses are getting better, and valve repair techniques are improving."
Dr. Harry R. Buller took issue with Dr. Van de Werf's blanket prediction that the factor Xa inhibitors will prove similarly unsafe and ineffective in patients with mechanical valves, as was dabigatran.
"We still need to find that out. One molecule of factor Xa generates about 1,000 thrombin molecules, so inhibiting coagulation at the level of Xa might actually be effective. What you see with dabigatran is inhibition at the very last stages of the whole coagulation cascade, when there are millions and millions of molecules of thrombin. That's quite difficult. If you do it higher up in the cascade it might work," argued Dr. Buller, chairman of the department of vascular medicine at the Academic Medical Center, Amsterdam.
"Would you take that risk?" challenged Dr. Van de Werf.
"I know there are people taking that risk. I love studies; I would study it," Dr. Buller replied.
Session cochair Dr. Keith A.A. Fox of the University of Edinburgh posed a provocative question to Dr. Van de Werf: "Would you extrapolate these RE-ALIGN data to a patient in atrial fibrillation with a bioprosthetic valve?"
"It's a difficult question," Dr. Van de Werf replied. "In principle, you could give one of the novel anticoagulants approved for atrial fibrillation, including dabigatran, because it is assumed there is no indication for oral anticoagulation for the bioprosthetic valve. I'm not saying you necessarily should do that. If the patient is doing well on warfarin, I don't see the need to switch to one of the new anticoagulants."
RE-ALIGN was supported by Boehringer Ingelheim. Dr. Van de Werf reported receiving research grants and speakers' fees from the company. Dr. Buller, Dr. Fox, and Dr. Vahanian reported no relevant financial interests.
Surgery vs. waiting for flail leaflets
In patients with asymptomatic or minimally symptomatic mitral valve regurgitation as a result of flail mitral leaflets, early surgery yields better survival, lower risk of heart failure, and equivalent rates of atrial fibrillation, compared with watchful waiting, according to a report published online on August 13 in JAMA.
Overall long-term mortality is approximately 40% lower and HF risk approximately 60% lower for early surgery vs. watchful waiting. These benefits persist for up to 20 years and are seen across every important subgroup of patients, said Dr. Rakesh M. Suri of the Mayo Clinic, Rochester, Minn., and his associates.
These are the findings of a series of analyses of data from an international registry of consecutive patients diagnosed in routine clinical practice – the largest study in the world of the comparative effectiveness of early surgery vs. watchful waiting in patients without traditional indications for immediate surgery. The study results "emanate from institutions that together provide a very high rate of mitral valve repair (more than 90%) with low operative mortality, emphasizing that such results might also be achieved in routine practice at many advanced repair centers," the investigators noted.
Despite the safety and efficacy of current surgical correction of flail mitral leaflets, clinicians disagree as to the best approach for patients who have no or minimal HF symptoms, a left ventricular ejection fraction of 60% or more, and a left ventricular end-systolic diameter of 40 mm or more. Those who support watchful waiting consider the consequences of uncorrected mitral regurgitation to be benign, especially when weighed against the potential morbidity and mortality of early surgical intervention. North American guidelines favor early surgery while European guidelines favor watchful waiting.
The Mitral Regurgitation International Database (MIDA) – a registry of patients at two tertiary care centers in France, two in Italy, one in Belgium, and one in the United States – provided an ideal study population to compare the two approaches. For their study, Dr. Suri and his associates examined data for 1,021 of these patients who had been diagnosed in 1980-2004 and followed for up to 25 years (mean follow-up, 10.3 years).
This study included only patients who had no ischemic mitral regurgitation and no significant concomitant aortic valve disease, congenital heart disease, mitral stenosis, or previous valve surgery.
A total of 446 of these patients underwent early surgery (within 30 days of diagnosis) and 575 had watchful waiting at the discretion of their treating physicians. Importantly, 339 (59%) of the watchful-waiting group eventually were advised by their cardiologists to undergo valve repair, at a median of 1.65 years after diagnosis.
Overall, there were 319 deaths during follow-up.
The primary end points of this study were all-cause mortality at 5, 10, and 20 years.
In the initial, unadjusted analysis, survival was 95%, 86%, and 63%, respectively, with early surgery. In contrast, survival was significantly lower with watchful waiting, at 84% at 5 years, 69% at 10 years, and 41% at 20 years, the researchers said (JAMA 2013; 310:609-16).
The large survival benefit with early surgery was confirmed in a multivariable analysis that adjusted for patient age, sex, comorbidities, and the presence of subtle symptoms.
To account for differences between the two study groups in the propensity to undergo surgery, the investigators performed an analysis of the data in a set of 648 patients who were matched for age, comorbidities, and other factors. This analysis also showed a similar and distinct survival advantage with early surgery. Several subgroup analyses also confirmed the results.
Secondary end points were the incidence of heart failure and the onset of new atrial fibrillation during follow-up.
A total of 167 patients had at least one episode of HF. The rates were 7% with early surgery and 23% with watchful waiting at 10 years, and 10% vs. 35% at 20 years, showing a clear advantage for early surgery.
This strong advantage persisted in further analyses of the propensity-matched patients and in all other subgroups examined, at all time points examined.
New-onset AF developed in 227 patients overall. The rate was slightly higher in the early-surgery group during the immediate postoperative period but decreased thereafter and was equivalent between the two study groups at 5, 10, and 20 years.
"Long-term, the results are coherent by all methods used (direct comparison, adjusted comparison, propensity score matching, inverse probability weighing) that early surgical correction of mitral valve regurgitation was associated with a significant survival benefit (total mortality decrement of approximately 40%) and diminished HF risk (reduction of approximately 60%)," Dr. Suri and his associates wrote.
Dr. Suri reported ties to Edwards Lifesciences, Sorin Group, St. Jude Medical, and Abbott.
In patients with asymptomatic or minimally symptomatic mitral valve regurgitation as a result of flail mitral leaflets, early surgery yields better survival, lower risk of heart failure, and equivalent rates of atrial fibrillation, compared with watchful waiting, according to a report published online on August 13 in JAMA.
Overall long-term mortality is approximately 40% lower and HF risk approximately 60% lower for early surgery vs. watchful waiting. These benefits persist for up to 20 years and are seen across every important subgroup of patients, said Dr. Rakesh M. Suri of the Mayo Clinic, Rochester, Minn., and his associates.
These are the findings of a series of analyses of data from an international registry of consecutive patients diagnosed in routine clinical practice – the largest study in the world of the comparative effectiveness of early surgery vs. watchful waiting in patients without traditional indications for immediate surgery. The study results "emanate from institutions that together provide a very high rate of mitral valve repair (more than 90%) with low operative mortality, emphasizing that such results might also be achieved in routine practice at many advanced repair centers," the investigators noted.
Despite the safety and efficacy of current surgical correction of flail mitral leaflets, clinicians disagree as to the best approach for patients who have no or minimal HF symptoms, a left ventricular ejection fraction of 60% or more, and a left ventricular end-systolic diameter of 40 mm or more. Those who support watchful waiting consider the consequences of uncorrected mitral regurgitation to be benign, especially when weighed against the potential morbidity and mortality of early surgical intervention. North American guidelines favor early surgery while European guidelines favor watchful waiting.
The Mitral Regurgitation International Database (MIDA) – a registry of patients at two tertiary care centers in France, two in Italy, one in Belgium, and one in the United States – provided an ideal study population to compare the two approaches. For their study, Dr. Suri and his associates examined data for 1,021 of these patients who had been diagnosed in 1980-2004 and followed for up to 25 years (mean follow-up, 10.3 years).
This study included only patients who had no ischemic mitral regurgitation and no significant concomitant aortic valve disease, congenital heart disease, mitral stenosis, or previous valve surgery.
A total of 446 of these patients underwent early surgery (within 30 days of diagnosis) and 575 had watchful waiting at the discretion of their treating physicians. Importantly, 339 (59%) of the watchful-waiting group eventually were advised by their cardiologists to undergo valve repair, at a median of 1.65 years after diagnosis.
Overall, there were 319 deaths during follow-up.
The primary end points of this study were all-cause mortality at 5, 10, and 20 years.
In the initial, unadjusted analysis, survival was 95%, 86%, and 63%, respectively, with early surgery. In contrast, survival was significantly lower with watchful waiting, at 84% at 5 years, 69% at 10 years, and 41% at 20 years, the researchers said (JAMA 2013; 310:609-16).
The large survival benefit with early surgery was confirmed in a multivariable analysis that adjusted for patient age, sex, comorbidities, and the presence of subtle symptoms.
To account for differences between the two study groups in the propensity to undergo surgery, the investigators performed an analysis of the data in a set of 648 patients who were matched for age, comorbidities, and other factors. This analysis also showed a similar and distinct survival advantage with early surgery. Several subgroup analyses also confirmed the results.
Secondary end points were the incidence of heart failure and the onset of new atrial fibrillation during follow-up.
A total of 167 patients had at least one episode of HF. The rates were 7% with early surgery and 23% with watchful waiting at 10 years, and 10% vs. 35% at 20 years, showing a clear advantage for early surgery.
This strong advantage persisted in further analyses of the propensity-matched patients and in all other subgroups examined, at all time points examined.
New-onset AF developed in 227 patients overall. The rate was slightly higher in the early-surgery group during the immediate postoperative period but decreased thereafter and was equivalent between the two study groups at 5, 10, and 20 years.
"Long-term, the results are coherent by all methods used (direct comparison, adjusted comparison, propensity score matching, inverse probability weighing) that early surgical correction of mitral valve regurgitation was associated with a significant survival benefit (total mortality decrement of approximately 40%) and diminished HF risk (reduction of approximately 60%)," Dr. Suri and his associates wrote.
Dr. Suri reported ties to Edwards Lifesciences, Sorin Group, St. Jude Medical, and Abbott.
In patients with asymptomatic or minimally symptomatic mitral valve regurgitation as a result of flail mitral leaflets, early surgery yields better survival, lower risk of heart failure, and equivalent rates of atrial fibrillation, compared with watchful waiting, according to a report published online on August 13 in JAMA.
Overall long-term mortality is approximately 40% lower and HF risk approximately 60% lower for early surgery vs. watchful waiting. These benefits persist for up to 20 years and are seen across every important subgroup of patients, said Dr. Rakesh M. Suri of the Mayo Clinic, Rochester, Minn., and his associates.
These are the findings of a series of analyses of data from an international registry of consecutive patients diagnosed in routine clinical practice – the largest study in the world of the comparative effectiveness of early surgery vs. watchful waiting in patients without traditional indications for immediate surgery. The study results "emanate from institutions that together provide a very high rate of mitral valve repair (more than 90%) with low operative mortality, emphasizing that such results might also be achieved in routine practice at many advanced repair centers," the investigators noted.
Despite the safety and efficacy of current surgical correction of flail mitral leaflets, clinicians disagree as to the best approach for patients who have no or minimal HF symptoms, a left ventricular ejection fraction of 60% or more, and a left ventricular end-systolic diameter of 40 mm or more. Those who support watchful waiting consider the consequences of uncorrected mitral regurgitation to be benign, especially when weighed against the potential morbidity and mortality of early surgical intervention. North American guidelines favor early surgery while European guidelines favor watchful waiting.
The Mitral Regurgitation International Database (MIDA) – a registry of patients at two tertiary care centers in France, two in Italy, one in Belgium, and one in the United States – provided an ideal study population to compare the two approaches. For their study, Dr. Suri and his associates examined data for 1,021 of these patients who had been diagnosed in 1980-2004 and followed for up to 25 years (mean follow-up, 10.3 years).
This study included only patients who had no ischemic mitral regurgitation and no significant concomitant aortic valve disease, congenital heart disease, mitral stenosis, or previous valve surgery.
A total of 446 of these patients underwent early surgery (within 30 days of diagnosis) and 575 had watchful waiting at the discretion of their treating physicians. Importantly, 339 (59%) of the watchful-waiting group eventually were advised by their cardiologists to undergo valve repair, at a median of 1.65 years after diagnosis.
Overall, there were 319 deaths during follow-up.
The primary end points of this study were all-cause mortality at 5, 10, and 20 years.
In the initial, unadjusted analysis, survival was 95%, 86%, and 63%, respectively, with early surgery. In contrast, survival was significantly lower with watchful waiting, at 84% at 5 years, 69% at 10 years, and 41% at 20 years, the researchers said (JAMA 2013; 310:609-16).
The large survival benefit with early surgery was confirmed in a multivariable analysis that adjusted for patient age, sex, comorbidities, and the presence of subtle symptoms.
To account for differences between the two study groups in the propensity to undergo surgery, the investigators performed an analysis of the data in a set of 648 patients who were matched for age, comorbidities, and other factors. This analysis also showed a similar and distinct survival advantage with early surgery. Several subgroup analyses also confirmed the results.
Secondary end points were the incidence of heart failure and the onset of new atrial fibrillation during follow-up.
A total of 167 patients had at least one episode of HF. The rates were 7% with early surgery and 23% with watchful waiting at 10 years, and 10% vs. 35% at 20 years, showing a clear advantage for early surgery.
This strong advantage persisted in further analyses of the propensity-matched patients and in all other subgroups examined, at all time points examined.
New-onset AF developed in 227 patients overall. The rate was slightly higher in the early-surgery group during the immediate postoperative period but decreased thereafter and was equivalent between the two study groups at 5, 10, and 20 years.
"Long-term, the results are coherent by all methods used (direct comparison, adjusted comparison, propensity score matching, inverse probability weighing) that early surgical correction of mitral valve regurgitation was associated with a significant survival benefit (total mortality decrement of approximately 40%) and diminished HF risk (reduction of approximately 60%)," Dr. Suri and his associates wrote.
Dr. Suri reported ties to Edwards Lifesciences, Sorin Group, St. Jude Medical, and Abbott.
Major finding: Survival at 5, 10, and 20 years was 95%, 86%, and 63%, respectively, with early surgery, compared with 84%, 69%, and 41%, respectively, with watchful waiting.
Data source: Serial analyses of data on 1,021 patients with asymptomatic or minimally symptomatic mitral valve regurgitation caused by flail mitral leaflets who were advised to undergo early repair (446 subjects) or watchful waiting (575 subjects) and were followed for up to 25 years.
Disclosures: Dr. Suri reported ties to Edwards Lifesciences, Sorin Group, St. Jude Medical, and Abbott. His associates reported ties to Edwards Lifesciences, Valtech, and Abbott Vascular.
Aortic valve-sparing surgery shows durability
MINNEAPOLIS – Despite the complexity of aortic valve–sparing techniques, early outcomes and 1-year survival were similar to those achieved with valve replacing during root replacement surgery in patients with Marfan syndrome in a prospective registry study.
Major adverse valve-related events (MAVREs) at 1 year were also comparable, although there was an increase, of course, in aortic valve regurgitation with valve sparing (7% vs. 0%), Dr. Joseph S. Coselli said at the annual meeting of the American Association for Thoracic Surgery.
"Follow-up is needed for this particular incident because we don’t know exactly what’s going to happen to these 2-plus aortic regurgitations," he said. "It’s quite possible they may remain stable over a long period of time and don’t represent a failure of the concept."
In an initial report from the international registry, valve-sparing techniques were the most common, and provided comparable 30-day outcomes in 151 patients (J. Thorac. Cardiovasc. Surg. 2009;137:1124-32).
The current analysis involved 316 patients, aged 4-70 years, who underwent aortic valve–sparing (AVS) (N = 239) or aortic valve–replacing (AVR) (N = 63 mechanical and 14 tissue) root replacement surgery at 19 centers between March 2005 and November 2010. The type of operation was determined by clinical factors, and by surgeon and patient preference. AVR surgery was considered the only option in 17% of patients. At 1 year, clinical follow-up was complete in 98% and imaging follow-up in 93%.
"Interestingly, when we started out this particular collection of patients, over 30% were receiving aortic valve replacement, but toward the end of this observational study, late 2010, virtually almost all patients were receiving aortic valve sparing," said Dr. Coselli, chief of adult cardiac surgery at Baylor College of Medicine, Texas Heart Institute, Houston.
AVS patients were younger (33 vs. 39 years); had smaller sinuses of Valsalva (49 vs. 53 mm); and had less acute dissection (3% vs. 9%), chronic dissection (3% vs. 12%), and previous cardiovascular surgery (5% vs. 14%).
Aortic-sparing techniques required significantly longer cardiopulmonary bypass time (195 vs. 152 minutes) and aortic clamp time (156 vs. 115 minutes), but cut ICU time from 46 hours with AVR surgery to 26 hours, ventilator support time from 12 to 8 hours, and hospital length of stay from 7 to 6 days, Dr. Coselli reported.
At 30 days, MAVREs were reported in 6 patients in the AVR group and 15 in the AVS group (P = .4), with no differences in nonstructural dysfunction (1 vs. 7), embolism (1 vs. 3), or bleeding (2 vs. 3 events).
Two AVS patients required early reoperation: One required same-day reintervention because of coronary artery kinking after a Florida sleeve procedure, and the second needed reintervention because of a coronary pseudoaneurysm 6 days after a David-V procedure, he said. Two early deaths occurred, one in each group, but neither was valve related.
One-year survival rates were 98% after AVS surgery and 97% after AVR surgery (4 vs. 2 deaths; P = .06).
At 1 year, MAVREs occurred in 8 AVR and 35 AVS patients (P = .5). There was no significant difference between AVR and AVS in freedom from valve-related death (1 vs. 2), embolism (2 vs. 4 events), reintervention (0 vs. 1), endocarditis (1 vs. 0), valve thrombosis (0 both), or valve-related morbidity (7 vs. 28), Dr. Coselli said.
The AVS group had significantly more nonstructural dysfunction/structural valve deterioration (23 events vs. 1 event; P = .04), but significantly less bleeding (3 vs. 5 events; P = .01).
In a Cox regression analysis at 1 year, the type of surgery was not associated with overall survival, MAVREs, or any other valve-related outcome, he said.
Dr. Coselli reported research support from St. Jude Medical; an educational grant, consultancy, and royalties from Vascutek Terumo; and research support, speaking for, and steering committee membership with Medtronic. Two coauthors reported consultant/advisory board participation with Medtronic or Edwards Lifesciences.
MINNEAPOLIS – Despite the complexity of aortic valve–sparing techniques, early outcomes and 1-year survival were similar to those achieved with valve replacing during root replacement surgery in patients with Marfan syndrome in a prospective registry study.
Major adverse valve-related events (MAVREs) at 1 year were also comparable, although there was an increase, of course, in aortic valve regurgitation with valve sparing (7% vs. 0%), Dr. Joseph S. Coselli said at the annual meeting of the American Association for Thoracic Surgery.
"Follow-up is needed for this particular incident because we don’t know exactly what’s going to happen to these 2-plus aortic regurgitations," he said. "It’s quite possible they may remain stable over a long period of time and don’t represent a failure of the concept."
In an initial report from the international registry, valve-sparing techniques were the most common, and provided comparable 30-day outcomes in 151 patients (J. Thorac. Cardiovasc. Surg. 2009;137:1124-32).
The current analysis involved 316 patients, aged 4-70 years, who underwent aortic valve–sparing (AVS) (N = 239) or aortic valve–replacing (AVR) (N = 63 mechanical and 14 tissue) root replacement surgery at 19 centers between March 2005 and November 2010. The type of operation was determined by clinical factors, and by surgeon and patient preference. AVR surgery was considered the only option in 17% of patients. At 1 year, clinical follow-up was complete in 98% and imaging follow-up in 93%.
"Interestingly, when we started out this particular collection of patients, over 30% were receiving aortic valve replacement, but toward the end of this observational study, late 2010, virtually almost all patients were receiving aortic valve sparing," said Dr. Coselli, chief of adult cardiac surgery at Baylor College of Medicine, Texas Heart Institute, Houston.
AVS patients were younger (33 vs. 39 years); had smaller sinuses of Valsalva (49 vs. 53 mm); and had less acute dissection (3% vs. 9%), chronic dissection (3% vs. 12%), and previous cardiovascular surgery (5% vs. 14%).
Aortic-sparing techniques required significantly longer cardiopulmonary bypass time (195 vs. 152 minutes) and aortic clamp time (156 vs. 115 minutes), but cut ICU time from 46 hours with AVR surgery to 26 hours, ventilator support time from 12 to 8 hours, and hospital length of stay from 7 to 6 days, Dr. Coselli reported.
At 30 days, MAVREs were reported in 6 patients in the AVR group and 15 in the AVS group (P = .4), with no differences in nonstructural dysfunction (1 vs. 7), embolism (1 vs. 3), or bleeding (2 vs. 3 events).
Two AVS patients required early reoperation: One required same-day reintervention because of coronary artery kinking after a Florida sleeve procedure, and the second needed reintervention because of a coronary pseudoaneurysm 6 days after a David-V procedure, he said. Two early deaths occurred, one in each group, but neither was valve related.
One-year survival rates were 98% after AVS surgery and 97% after AVR surgery (4 vs. 2 deaths; P = .06).
At 1 year, MAVREs occurred in 8 AVR and 35 AVS patients (P = .5). There was no significant difference between AVR and AVS in freedom from valve-related death (1 vs. 2), embolism (2 vs. 4 events), reintervention (0 vs. 1), endocarditis (1 vs. 0), valve thrombosis (0 both), or valve-related morbidity (7 vs. 28), Dr. Coselli said.
The AVS group had significantly more nonstructural dysfunction/structural valve deterioration (23 events vs. 1 event; P = .04), but significantly less bleeding (3 vs. 5 events; P = .01).
In a Cox regression analysis at 1 year, the type of surgery was not associated with overall survival, MAVREs, or any other valve-related outcome, he said.
Dr. Coselli reported research support from St. Jude Medical; an educational grant, consultancy, and royalties from Vascutek Terumo; and research support, speaking for, and steering committee membership with Medtronic. Two coauthors reported consultant/advisory board participation with Medtronic or Edwards Lifesciences.
MINNEAPOLIS – Despite the complexity of aortic valve–sparing techniques, early outcomes and 1-year survival were similar to those achieved with valve replacing during root replacement surgery in patients with Marfan syndrome in a prospective registry study.
Major adverse valve-related events (MAVREs) at 1 year were also comparable, although there was an increase, of course, in aortic valve regurgitation with valve sparing (7% vs. 0%), Dr. Joseph S. Coselli said at the annual meeting of the American Association for Thoracic Surgery.
"Follow-up is needed for this particular incident because we don’t know exactly what’s going to happen to these 2-plus aortic regurgitations," he said. "It’s quite possible they may remain stable over a long period of time and don’t represent a failure of the concept."
In an initial report from the international registry, valve-sparing techniques were the most common, and provided comparable 30-day outcomes in 151 patients (J. Thorac. Cardiovasc. Surg. 2009;137:1124-32).
The current analysis involved 316 patients, aged 4-70 years, who underwent aortic valve–sparing (AVS) (N = 239) or aortic valve–replacing (AVR) (N = 63 mechanical and 14 tissue) root replacement surgery at 19 centers between March 2005 and November 2010. The type of operation was determined by clinical factors, and by surgeon and patient preference. AVR surgery was considered the only option in 17% of patients. At 1 year, clinical follow-up was complete in 98% and imaging follow-up in 93%.
"Interestingly, when we started out this particular collection of patients, over 30% were receiving aortic valve replacement, but toward the end of this observational study, late 2010, virtually almost all patients were receiving aortic valve sparing," said Dr. Coselli, chief of adult cardiac surgery at Baylor College of Medicine, Texas Heart Institute, Houston.
AVS patients were younger (33 vs. 39 years); had smaller sinuses of Valsalva (49 vs. 53 mm); and had less acute dissection (3% vs. 9%), chronic dissection (3% vs. 12%), and previous cardiovascular surgery (5% vs. 14%).
Aortic-sparing techniques required significantly longer cardiopulmonary bypass time (195 vs. 152 minutes) and aortic clamp time (156 vs. 115 minutes), but cut ICU time from 46 hours with AVR surgery to 26 hours, ventilator support time from 12 to 8 hours, and hospital length of stay from 7 to 6 days, Dr. Coselli reported.
At 30 days, MAVREs were reported in 6 patients in the AVR group and 15 in the AVS group (P = .4), with no differences in nonstructural dysfunction (1 vs. 7), embolism (1 vs. 3), or bleeding (2 vs. 3 events).
Two AVS patients required early reoperation: One required same-day reintervention because of coronary artery kinking after a Florida sleeve procedure, and the second needed reintervention because of a coronary pseudoaneurysm 6 days after a David-V procedure, he said. Two early deaths occurred, one in each group, but neither was valve related.
One-year survival rates were 98% after AVS surgery and 97% after AVR surgery (4 vs. 2 deaths; P = .06).
At 1 year, MAVREs occurred in 8 AVR and 35 AVS patients (P = .5). There was no significant difference between AVR and AVS in freedom from valve-related death (1 vs. 2), embolism (2 vs. 4 events), reintervention (0 vs. 1), endocarditis (1 vs. 0), valve thrombosis (0 both), or valve-related morbidity (7 vs. 28), Dr. Coselli said.
The AVS group had significantly more nonstructural dysfunction/structural valve deterioration (23 events vs. 1 event; P = .04), but significantly less bleeding (3 vs. 5 events; P = .01).
In a Cox regression analysis at 1 year, the type of surgery was not associated with overall survival, MAVREs, or any other valve-related outcome, he said.
Dr. Coselli reported research support from St. Jude Medical; an educational grant, consultancy, and royalties from Vascutek Terumo; and research support, speaking for, and steering committee membership with Medtronic. Two coauthors reported consultant/advisory board participation with Medtronic or Edwards Lifesciences.
AT THE AATS ANNUAL MEETING