User login
Nivolumab linked to CNS disorder in case report
Autoimmune encephalitis may be a potentially severe complication of immune checkpoint inhibitor therapy, a case report suggests.
The recently published report describes a 53-year-old man with B-cell non-Hodgkin lymphoma who presented with double vision, ataxia, impaired speech, and mild cognitive dysfunction following treatment with the immune checkpoint inhibitor nivolumab.
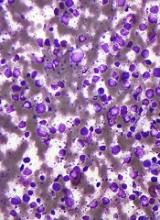
Neuropathologic examination of a biopsied brain lesion found on cranial MRI showed a T cell–dominated inflammatory process thought to be autoimmune in origin, according to Herwig Strik, MD, of the department of neurology at Philipps University of Marburg (Germany), and his colleagues (Eur J Cancer. 2017 Oct 16. doi: 10.1016/j.ejca.2017.09.026).
After the patient stopped taking nivolumab and the inflammatory process was treated, his “clinical neurological and radiological status remained stable but disabling with fluctuating dysarthria and ataxia,” Dr. Strik and his colleagues wrote.
“Since these novel anticancer agents are increasingly used, this severe complication should be recognized soon and treatment should be terminated to avoid chronification,” they said in the report.
Nivolumab and other checkpoint inhibitors are known to have autoimmune side effects in some cases that can affect the pulmonary, gastrointestinal, and endocrine systems, the authors said.
Several previous case reports have detailed encephalitis occurring in cancer patients receiving nivolumab, the combination of nivolumab plus the immune checkpoint inhibitor ipilimumab, or ipilimumab alone. The authors said they believe that this case report is the first to describe multifocal CNS inflammation following nivolumab treatment for systemic lymphoma.
The patient was diagnosed with B-cell non-Hodgkin lymphoma in 2005, according to the case report. He was first treated in 2009 with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone), followed by stem cell apheresis, radioimmunotherapy, and rituximab; he then received R-DHAP (rituximab, dexamethasone, high-dose cytarabine, and cisplatin) in August 2014, followed by autologous stem cell transplantation in October of that year. The patient started nivolumab maintenance therapy in February 2015 but started experiencing neurological symptoms that eventually led to ending nivolumab treatment in September 2015.
The patient’s lymphoma relapsed in June 2016. “The disabling neurological symptoms and his personal situation, however, worsened the patient’s depressive symptoms so severely that he went abroad to commit assisted suicide,” wrote Dr. Strik and his colleagues.
The authors proposed the term “immune checkpoint inhibitor–associated CNS autoimmune disorder (ICICAD)” to describe the inflammatory condition described in the case report.
They declared no conflicts of interest related to the case report and did not receive grant support for conducting the research described in it.
Autoimmune encephalitis may be a potentially severe complication of immune checkpoint inhibitor therapy, a case report suggests.
The recently published report describes a 53-year-old man with B-cell non-Hodgkin lymphoma who presented with double vision, ataxia, impaired speech, and mild cognitive dysfunction following treatment with the immune checkpoint inhibitor nivolumab.
Neuropathologic examination of a biopsied brain lesion found on cranial MRI showed a T cell–dominated inflammatory process thought to be autoimmune in origin, according to Herwig Strik, MD, of the department of neurology at Philipps University of Marburg (Germany), and his colleagues (Eur J Cancer. 2017 Oct 16. doi: 10.1016/j.ejca.2017.09.026).
After the patient stopped taking nivolumab and the inflammatory process was treated, his “clinical neurological and radiological status remained stable but disabling with fluctuating dysarthria and ataxia,” Dr. Strik and his colleagues wrote.
“Since these novel anticancer agents are increasingly used, this severe complication should be recognized soon and treatment should be terminated to avoid chronification,” they said in the report.
Nivolumab and other checkpoint inhibitors are known to have autoimmune side effects in some cases that can affect the pulmonary, gastrointestinal, and endocrine systems, the authors said.
Several previous case reports have detailed encephalitis occurring in cancer patients receiving nivolumab, the combination of nivolumab plus the immune checkpoint inhibitor ipilimumab, or ipilimumab alone. The authors said they believe that this case report is the first to describe multifocal CNS inflammation following nivolumab treatment for systemic lymphoma.
The patient was diagnosed with B-cell non-Hodgkin lymphoma in 2005, according to the case report. He was first treated in 2009 with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone), followed by stem cell apheresis, radioimmunotherapy, and rituximab; he then received R-DHAP (rituximab, dexamethasone, high-dose cytarabine, and cisplatin) in August 2014, followed by autologous stem cell transplantation in October of that year. The patient started nivolumab maintenance therapy in February 2015 but started experiencing neurological symptoms that eventually led to ending nivolumab treatment in September 2015.
The patient’s lymphoma relapsed in June 2016. “The disabling neurological symptoms and his personal situation, however, worsened the patient’s depressive symptoms so severely that he went abroad to commit assisted suicide,” wrote Dr. Strik and his colleagues.
The authors proposed the term “immune checkpoint inhibitor–associated CNS autoimmune disorder (ICICAD)” to describe the inflammatory condition described in the case report.
They declared no conflicts of interest related to the case report and did not receive grant support for conducting the research described in it.
Autoimmune encephalitis may be a potentially severe complication of immune checkpoint inhibitor therapy, a case report suggests.
The recently published report describes a 53-year-old man with B-cell non-Hodgkin lymphoma who presented with double vision, ataxia, impaired speech, and mild cognitive dysfunction following treatment with the immune checkpoint inhibitor nivolumab.
Neuropathologic examination of a biopsied brain lesion found on cranial MRI showed a T cell–dominated inflammatory process thought to be autoimmune in origin, according to Herwig Strik, MD, of the department of neurology at Philipps University of Marburg (Germany), and his colleagues (Eur J Cancer. 2017 Oct 16. doi: 10.1016/j.ejca.2017.09.026).
After the patient stopped taking nivolumab and the inflammatory process was treated, his “clinical neurological and radiological status remained stable but disabling with fluctuating dysarthria and ataxia,” Dr. Strik and his colleagues wrote.
“Since these novel anticancer agents are increasingly used, this severe complication should be recognized soon and treatment should be terminated to avoid chronification,” they said in the report.
Nivolumab and other checkpoint inhibitors are known to have autoimmune side effects in some cases that can affect the pulmonary, gastrointestinal, and endocrine systems, the authors said.
Several previous case reports have detailed encephalitis occurring in cancer patients receiving nivolumab, the combination of nivolumab plus the immune checkpoint inhibitor ipilimumab, or ipilimumab alone. The authors said they believe that this case report is the first to describe multifocal CNS inflammation following nivolumab treatment for systemic lymphoma.
The patient was diagnosed with B-cell non-Hodgkin lymphoma in 2005, according to the case report. He was first treated in 2009 with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone), followed by stem cell apheresis, radioimmunotherapy, and rituximab; he then received R-DHAP (rituximab, dexamethasone, high-dose cytarabine, and cisplatin) in August 2014, followed by autologous stem cell transplantation in October of that year. The patient started nivolumab maintenance therapy in February 2015 but started experiencing neurological symptoms that eventually led to ending nivolumab treatment in September 2015.
The patient’s lymphoma relapsed in June 2016. “The disabling neurological symptoms and his personal situation, however, worsened the patient’s depressive symptoms so severely that he went abroad to commit assisted suicide,” wrote Dr. Strik and his colleagues.
The authors proposed the term “immune checkpoint inhibitor–associated CNS autoimmune disorder (ICICAD)” to describe the inflammatory condition described in the case report.
They declared no conflicts of interest related to the case report and did not receive grant support for conducting the research described in it.
FROM THE EUROPEAN JOURNAL OF CANCER
Key clinical point: Autoimmune encephalitis may be a potential complication of checkpoint inhibitor therapy.
Major finding: A patient with B-cell non-Hodgkin lymphoma presented with double vision, ataxia, impaired speech, and mild cognitive dysfunction following treatment with nivolumab. Examination of a brain lesion showed a T cell–dominated inflammatory process thought to be autoimmune in origin.
Data source: A case report of a 53-year-old man with B-cell non-Hodgkin lymphoma (B-NHL) who received nivolumab maintenance treatment.
Disclosures: The authors declared no conflicts of interest and did not receive grant support for the research.
FDA approves drug to treat rel/ref MCL
The US Food and Drug Administration (FDA) has granted accelerated approval to the BTK inhibitor acalabrutinib (Calquence, formerly ACP-196).
The drug is now approved to treat adults with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s accelerated approval pathway is used for drugs intended to treat serious conditions where there is unmet medical need and when said drugs have demonstrated effects that suggest they will provide a clinical benefit to patients.
This means further study is required to verify and describe the anticipated clinical benefits of acalabrutinib, which was approved based on the overall response rate observed in a phase 2 trial.
The company developing acalabrutinib, AstraZeneca Pharmaceuticals LP, is currently conducting the necessary additional research.
The FDA previously granted AstraZeneca priority review, breakthrough therapy, and orphan drug designations for acalabrutinib as a treatment for MCL.
Phase 2 trial
The FDA approved acalabrutinib based on results of the phase 2 ACE-LY-004 trial. This single-arm trial enrolled 124 adults with relapsed or refractory MCL.
According to AstraZeneca, acalabrutinib produced an overall response rate of 80%, with 40% of patients achieving a complete response and 40% experiencing a partial response.
The most common adverse events (AEs) of any grade (occurring in at least 20% of patients) were anemia (46%), thrombocytopenia (44%), headache (39%), neutropenia (36%), diarrhea (31%), fatigue (28%), myalgia (21%), and bruising (21%).
Dosage reductions due to AEs occurred in 1.6% of patients. Discontinuations due to AEs occurred in 6.5% of patients. Increases in creatinine 1.5 to 3 times the upper limit of normal occurred in 4.8% of patients.
According to AstraZeneca, full results from ACE-LY-004 have been submitted for presentation at an upcoming medical meeting.
This will be the first MCL trial data to be presented from the acalabrutinib development program, which includes both monotherapy and combination therapies in hematologic and solid tumor malignancies. ![]()
The US Food and Drug Administration (FDA) has granted accelerated approval to the BTK inhibitor acalabrutinib (Calquence, formerly ACP-196).
The drug is now approved to treat adults with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s accelerated approval pathway is used for drugs intended to treat serious conditions where there is unmet medical need and when said drugs have demonstrated effects that suggest they will provide a clinical benefit to patients.
This means further study is required to verify and describe the anticipated clinical benefits of acalabrutinib, which was approved based on the overall response rate observed in a phase 2 trial.
The company developing acalabrutinib, AstraZeneca Pharmaceuticals LP, is currently conducting the necessary additional research.
The FDA previously granted AstraZeneca priority review, breakthrough therapy, and orphan drug designations for acalabrutinib as a treatment for MCL.
Phase 2 trial
The FDA approved acalabrutinib based on results of the phase 2 ACE-LY-004 trial. This single-arm trial enrolled 124 adults with relapsed or refractory MCL.
According to AstraZeneca, acalabrutinib produced an overall response rate of 80%, with 40% of patients achieving a complete response and 40% experiencing a partial response.
The most common adverse events (AEs) of any grade (occurring in at least 20% of patients) were anemia (46%), thrombocytopenia (44%), headache (39%), neutropenia (36%), diarrhea (31%), fatigue (28%), myalgia (21%), and bruising (21%).
Dosage reductions due to AEs occurred in 1.6% of patients. Discontinuations due to AEs occurred in 6.5% of patients. Increases in creatinine 1.5 to 3 times the upper limit of normal occurred in 4.8% of patients.
According to AstraZeneca, full results from ACE-LY-004 have been submitted for presentation at an upcoming medical meeting.
This will be the first MCL trial data to be presented from the acalabrutinib development program, which includes both monotherapy and combination therapies in hematologic and solid tumor malignancies. ![]()
The US Food and Drug Administration (FDA) has granted accelerated approval to the BTK inhibitor acalabrutinib (Calquence, formerly ACP-196).
The drug is now approved to treat adults with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s accelerated approval pathway is used for drugs intended to treat serious conditions where there is unmet medical need and when said drugs have demonstrated effects that suggest they will provide a clinical benefit to patients.
This means further study is required to verify and describe the anticipated clinical benefits of acalabrutinib, which was approved based on the overall response rate observed in a phase 2 trial.
The company developing acalabrutinib, AstraZeneca Pharmaceuticals LP, is currently conducting the necessary additional research.
The FDA previously granted AstraZeneca priority review, breakthrough therapy, and orphan drug designations for acalabrutinib as a treatment for MCL.
Phase 2 trial
The FDA approved acalabrutinib based on results of the phase 2 ACE-LY-004 trial. This single-arm trial enrolled 124 adults with relapsed or refractory MCL.
According to AstraZeneca, acalabrutinib produced an overall response rate of 80%, with 40% of patients achieving a complete response and 40% experiencing a partial response.
The most common adverse events (AEs) of any grade (occurring in at least 20% of patients) were anemia (46%), thrombocytopenia (44%), headache (39%), neutropenia (36%), diarrhea (31%), fatigue (28%), myalgia (21%), and bruising (21%).
Dosage reductions due to AEs occurred in 1.6% of patients. Discontinuations due to AEs occurred in 6.5% of patients. Increases in creatinine 1.5 to 3 times the upper limit of normal occurred in 4.8% of patients.
According to AstraZeneca, full results from ACE-LY-004 have been submitted for presentation at an upcoming medical meeting.
This will be the first MCL trial data to be presented from the acalabrutinib development program, which includes both monotherapy and combination therapies in hematologic and solid tumor malignancies. ![]()
CCSs more likely to stay at jobs to keep health insurance
Survey results suggest childhood cancer survivors (CCSs) in the US are more likely than individuals without a history of cancer to experience “job lock,” or staying at a job to keep work-related health insurance.
CCSs are also more likely than individuals without a history of cancer to report problems paying medical bills and being denied health insurance.
Anne Kirchhoff, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City, and her colleagues reported these findings in JAMA Oncology.
The researchers analyzed 394 CCSs from pediatric oncology institutions across the US, along with 128 of their siblings who had no history of cancer. All study participants worked 35 hours or more per week.
The most common cancer diagnosis among CCSs was leukemia (35.4%), followed by Hodgkin lymphoma (14.9%). Most patients had undergone chemotherapy (77.2%), radiotherapy (63.9%), and surgery (81.1%).
Overall, sociodemographic and clinical characteristics were similar between CCSs and siblings. However, CCSs were more likely than siblings to have severe, disabling, or life-threatening chronic conditions—33.9% and 17.7%, respectively (P<0.001).
Most CCSs (88.0%) and siblings (88.5%) had employer-sponsored health insurance. Three percent of siblings and 5.3% of CCSs had individual insurance; 1.9% and 2.3%, respectively, had public insurance; and 6.7% and 4.4%, respectively, were uninsured.
Results
CCSs were more likely than siblings to report:
- Job lock—23.2% and 16.9%, respectively (P=0.16)
- Problems paying medical bills—20.1% and 12.9%, respectively (P=0.09)
- Denial of health insurance—13.4% and 1.8%, respectively (P<0.001).
In a multivariable analysis, insurance denial remained significantly more common among CCSs than siblings (relative risk [RR]=7.38).
In another multivariable analysis, 38% of CCSs with a previous insurance denial reported job lock, compared with 20% of those who never experienced insurance denial (RR=1.60). And 44% of CCSs who reported problems paying their medical bills also reported job lock, compared to 16% of those who had no problems paying medical bills (RR=2.43).
The researchers also found that female CCSs (RR=1.70) and CCSs with severe, disabling, or life-threatening chronic conditions (RR=1.72) were more likely to report job lock.
“This information gives us a feel for high-risk groups of survivors who may need more information about insurance,” Dr Kirchhoff said. “Many people experience a gap in education and literacy around insurance, and it’s important for people to understand their options—even those who are employed and consistently had access to insurance through work. We want to know what their concerns are so we can help patients and survivors. Getting healthcare should not be a worry for cancer survivors.”
“Survivors have been through a lot when they were younger and understand the importance of making sure they can get healthcare when they need it. I think a lot of them also saw what their parents and families went through in terms of the financial stress and burden of dealing with a health crisis. So they’re just primed to understand the importance of health insurance.”
Dr Kirchhoff noted that this study was conducted as the Affordable Care Act was rolling out. Therefore, she would like to do a follow-up study to see if the insurance exchanges and Medicaid expansion lessened job-related insurance worries. ![]()
Survey results suggest childhood cancer survivors (CCSs) in the US are more likely than individuals without a history of cancer to experience “job lock,” or staying at a job to keep work-related health insurance.
CCSs are also more likely than individuals without a history of cancer to report problems paying medical bills and being denied health insurance.
Anne Kirchhoff, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City, and her colleagues reported these findings in JAMA Oncology.
The researchers analyzed 394 CCSs from pediatric oncology institutions across the US, along with 128 of their siblings who had no history of cancer. All study participants worked 35 hours or more per week.
The most common cancer diagnosis among CCSs was leukemia (35.4%), followed by Hodgkin lymphoma (14.9%). Most patients had undergone chemotherapy (77.2%), radiotherapy (63.9%), and surgery (81.1%).
Overall, sociodemographic and clinical characteristics were similar between CCSs and siblings. However, CCSs were more likely than siblings to have severe, disabling, or life-threatening chronic conditions—33.9% and 17.7%, respectively (P<0.001).
Most CCSs (88.0%) and siblings (88.5%) had employer-sponsored health insurance. Three percent of siblings and 5.3% of CCSs had individual insurance; 1.9% and 2.3%, respectively, had public insurance; and 6.7% and 4.4%, respectively, were uninsured.
Results
CCSs were more likely than siblings to report:
- Job lock—23.2% and 16.9%, respectively (P=0.16)
- Problems paying medical bills—20.1% and 12.9%, respectively (P=0.09)
- Denial of health insurance—13.4% and 1.8%, respectively (P<0.001).
In a multivariable analysis, insurance denial remained significantly more common among CCSs than siblings (relative risk [RR]=7.38).
In another multivariable analysis, 38% of CCSs with a previous insurance denial reported job lock, compared with 20% of those who never experienced insurance denial (RR=1.60). And 44% of CCSs who reported problems paying their medical bills also reported job lock, compared to 16% of those who had no problems paying medical bills (RR=2.43).
The researchers also found that female CCSs (RR=1.70) and CCSs with severe, disabling, or life-threatening chronic conditions (RR=1.72) were more likely to report job lock.
“This information gives us a feel for high-risk groups of survivors who may need more information about insurance,” Dr Kirchhoff said. “Many people experience a gap in education and literacy around insurance, and it’s important for people to understand their options—even those who are employed and consistently had access to insurance through work. We want to know what their concerns are so we can help patients and survivors. Getting healthcare should not be a worry for cancer survivors.”
“Survivors have been through a lot when they were younger and understand the importance of making sure they can get healthcare when they need it. I think a lot of them also saw what their parents and families went through in terms of the financial stress and burden of dealing with a health crisis. So they’re just primed to understand the importance of health insurance.”
Dr Kirchhoff noted that this study was conducted as the Affordable Care Act was rolling out. Therefore, she would like to do a follow-up study to see if the insurance exchanges and Medicaid expansion lessened job-related insurance worries. ![]()
Survey results suggest childhood cancer survivors (CCSs) in the US are more likely than individuals without a history of cancer to experience “job lock,” or staying at a job to keep work-related health insurance.
CCSs are also more likely than individuals without a history of cancer to report problems paying medical bills and being denied health insurance.
Anne Kirchhoff, PhD, of Huntsman Cancer Institute at the University of Utah in Salt Lake City, and her colleagues reported these findings in JAMA Oncology.
The researchers analyzed 394 CCSs from pediatric oncology institutions across the US, along with 128 of their siblings who had no history of cancer. All study participants worked 35 hours or more per week.
The most common cancer diagnosis among CCSs was leukemia (35.4%), followed by Hodgkin lymphoma (14.9%). Most patients had undergone chemotherapy (77.2%), radiotherapy (63.9%), and surgery (81.1%).
Overall, sociodemographic and clinical characteristics were similar between CCSs and siblings. However, CCSs were more likely than siblings to have severe, disabling, or life-threatening chronic conditions—33.9% and 17.7%, respectively (P<0.001).
Most CCSs (88.0%) and siblings (88.5%) had employer-sponsored health insurance. Three percent of siblings and 5.3% of CCSs had individual insurance; 1.9% and 2.3%, respectively, had public insurance; and 6.7% and 4.4%, respectively, were uninsured.
Results
CCSs were more likely than siblings to report:
- Job lock—23.2% and 16.9%, respectively (P=0.16)
- Problems paying medical bills—20.1% and 12.9%, respectively (P=0.09)
- Denial of health insurance—13.4% and 1.8%, respectively (P<0.001).
In a multivariable analysis, insurance denial remained significantly more common among CCSs than siblings (relative risk [RR]=7.38).
In another multivariable analysis, 38% of CCSs with a previous insurance denial reported job lock, compared with 20% of those who never experienced insurance denial (RR=1.60). And 44% of CCSs who reported problems paying their medical bills also reported job lock, compared to 16% of those who had no problems paying medical bills (RR=2.43).
The researchers also found that female CCSs (RR=1.70) and CCSs with severe, disabling, or life-threatening chronic conditions (RR=1.72) were more likely to report job lock.
“This information gives us a feel for high-risk groups of survivors who may need more information about insurance,” Dr Kirchhoff said. “Many people experience a gap in education and literacy around insurance, and it’s important for people to understand their options—even those who are employed and consistently had access to insurance through work. We want to know what their concerns are so we can help patients and survivors. Getting healthcare should not be a worry for cancer survivors.”
“Survivors have been through a lot when they were younger and understand the importance of making sure they can get healthcare when they need it. I think a lot of them also saw what their parents and families went through in terms of the financial stress and burden of dealing with a health crisis. So they’re just primed to understand the importance of health insurance.”
Dr Kirchhoff noted that this study was conducted as the Affordable Care Act was rolling out. Therefore, she would like to do a follow-up study to see if the insurance exchanges and Medicaid expansion lessened job-related insurance worries. ![]()
Drug receives breakthrough designation for DLBCL
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to MOR208, an Fc-enhanced monoclonal antibody directed against CD19.
The designation is for MOR208 to be used in combination with lenalidomide to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who are not eligible for high-dose chemotherapy and autologous stem cell transplant.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The breakthrough designation for MOR208 is based on preliminary data from the ongoing phase 2 L-MIND study (NCT02399085).
In this trial, researchers are evaluating MOR208 in combination with lenalidomide in patients with relapsed/refractory DLBCL who are ineligible for high-dose chemotherapy and autologous stem cell transplant.
Preliminary data from this trial were presented at ASCO 2017.* Of the 44 patients enrolled at the data cut-off, 34 were evaluable for efficacy.
The objective response rate was 56% (19/34), and the complete response rate was 32% (11/34). Sixteen of the 19 responders were still on study at the data cut-off point.
The most frequent adverse events of grade 3 or higher were neutropenia (32%), thrombocytopenia (9%), and leukopenia (9%). As of the data cut-off, 27% of patients required a reduction of the lenalidomide dose due to side effects.
“We expect to report further data from our ongoing phase 2 L-MIND trial with MOR208 plus lenalidomide at this year’s American Society of Hematology conference in December,” said Malte Peters, chief development officer of MorphoSys AG, the company developing MOR208.
“In addition, we are currently evaluating MOR208 in combination with bendamustine in our phase 3 B-MIND trial.”
The B-MIND study is designed to compare MOR208 plus bendamustine to rituximab plus bendamustine in patients with relapsed/refractory DLBCL who are not eligible for high-dose chemotherapy and autologous stem cell transplant. ![]()
*Data in the abstract differ from the data presented at the meeting.
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to MOR208, an Fc-enhanced monoclonal antibody directed against CD19.
The designation is for MOR208 to be used in combination with lenalidomide to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who are not eligible for high-dose chemotherapy and autologous stem cell transplant.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The breakthrough designation for MOR208 is based on preliminary data from the ongoing phase 2 L-MIND study (NCT02399085).
In this trial, researchers are evaluating MOR208 in combination with lenalidomide in patients with relapsed/refractory DLBCL who are ineligible for high-dose chemotherapy and autologous stem cell transplant.
Preliminary data from this trial were presented at ASCO 2017.* Of the 44 patients enrolled at the data cut-off, 34 were evaluable for efficacy.
The objective response rate was 56% (19/34), and the complete response rate was 32% (11/34). Sixteen of the 19 responders were still on study at the data cut-off point.
The most frequent adverse events of grade 3 or higher were neutropenia (32%), thrombocytopenia (9%), and leukopenia (9%). As of the data cut-off, 27% of patients required a reduction of the lenalidomide dose due to side effects.
“We expect to report further data from our ongoing phase 2 L-MIND trial with MOR208 plus lenalidomide at this year’s American Society of Hematology conference in December,” said Malte Peters, chief development officer of MorphoSys AG, the company developing MOR208.
“In addition, we are currently evaluating MOR208 in combination with bendamustine in our phase 3 B-MIND trial.”
The B-MIND study is designed to compare MOR208 plus bendamustine to rituximab plus bendamustine in patients with relapsed/refractory DLBCL who are not eligible for high-dose chemotherapy and autologous stem cell transplant. ![]()
*Data in the abstract differ from the data presented at the meeting.
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to MOR208, an Fc-enhanced monoclonal antibody directed against CD19.
The designation is for MOR208 to be used in combination with lenalidomide to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who are not eligible for high-dose chemotherapy and autologous stem cell transplant.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The breakthrough designation for MOR208 is based on preliminary data from the ongoing phase 2 L-MIND study (NCT02399085).
In this trial, researchers are evaluating MOR208 in combination with lenalidomide in patients with relapsed/refractory DLBCL who are ineligible for high-dose chemotherapy and autologous stem cell transplant.
Preliminary data from this trial were presented at ASCO 2017.* Of the 44 patients enrolled at the data cut-off, 34 were evaluable for efficacy.
The objective response rate was 56% (19/34), and the complete response rate was 32% (11/34). Sixteen of the 19 responders were still on study at the data cut-off point.
The most frequent adverse events of grade 3 or higher were neutropenia (32%), thrombocytopenia (9%), and leukopenia (9%). As of the data cut-off, 27% of patients required a reduction of the lenalidomide dose due to side effects.
“We expect to report further data from our ongoing phase 2 L-MIND trial with MOR208 plus lenalidomide at this year’s American Society of Hematology conference in December,” said Malte Peters, chief development officer of MorphoSys AG, the company developing MOR208.
“In addition, we are currently evaluating MOR208 in combination with bendamustine in our phase 3 B-MIND trial.”
The B-MIND study is designed to compare MOR208 plus bendamustine to rituximab plus bendamustine in patients with relapsed/refractory DLBCL who are not eligible for high-dose chemotherapy and autologous stem cell transplant. ![]()
*Data in the abstract differ from the data presented at the meeting.
EMA recommends orphan designation for G100 to treat FL
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended orphan designation for G100 for the treatment of follicular lymphoma (FL).
G100 contains the synthetic small molecule toll-like receptor-4 agonist glucopyranosyl lipid A.
G100 works by activating innate and adaptive immunity in the tumor microenvironment to generate an immune response against the tumor’s pre-existing antigens.
Clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The induction of local and systemic immune responses has been shown in preclinical studies to result in local and abscopal tumor control.
Immune Design, the company developing G100, is currently evaluating G100 plus local radiation, with or without pembrolizumab, in a phase 1/2 trial of FL patients.
Results from this trial were presented at the 2017 ASCO Annual Meeting (abstract 7537). Nine patients who received G100 (3 patients each at the 5, 10, or 20 μg dose) with radiation (but not pembrolizumab) were evaluable for safety and efficacy.
The overall response rate was 44%, and all of these were partial responses (n=4). Thirty-three percent of patients had stable disease (n=3).
Among the responders, tumor regression ranged from 58% to 89%, which included up to 56% shrinkage of abscopal sites. Tumor biopsies showed increased inflammatory responses and T-cell infiltrates in abscopal tumors.
An additional 13 patients treated at the 10 μg dose were evaluable for safety. There were no dose-limiting toxicities, serious adverse events (AEs), or grade 3/4 AEs observed.
Common AEs included injection site disorders, abdominal pain/discomfort, nausea, pruritus, and decrease in lymphocytes.
Immune Design said that, if this trial produces a sufficiently robust clinical benefit for patients, the company may pursue FL as the first indication for regulatory approval of G100.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission. ![]()
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended orphan designation for G100 for the treatment of follicular lymphoma (FL).
G100 contains the synthetic small molecule toll-like receptor-4 agonist glucopyranosyl lipid A.
G100 works by activating innate and adaptive immunity in the tumor microenvironment to generate an immune response against the tumor’s pre-existing antigens.
Clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The induction of local and systemic immune responses has been shown in preclinical studies to result in local and abscopal tumor control.
Immune Design, the company developing G100, is currently evaluating G100 plus local radiation, with or without pembrolizumab, in a phase 1/2 trial of FL patients.
Results from this trial were presented at the 2017 ASCO Annual Meeting (abstract 7537). Nine patients who received G100 (3 patients each at the 5, 10, or 20 μg dose) with radiation (but not pembrolizumab) were evaluable for safety and efficacy.
The overall response rate was 44%, and all of these were partial responses (n=4). Thirty-three percent of patients had stable disease (n=3).
Among the responders, tumor regression ranged from 58% to 89%, which included up to 56% shrinkage of abscopal sites. Tumor biopsies showed increased inflammatory responses and T-cell infiltrates in abscopal tumors.
An additional 13 patients treated at the 10 μg dose were evaluable for safety. There were no dose-limiting toxicities, serious adverse events (AEs), or grade 3/4 AEs observed.
Common AEs included injection site disorders, abdominal pain/discomfort, nausea, pruritus, and decrease in lymphocytes.
Immune Design said that, if this trial produces a sufficiently robust clinical benefit for patients, the company may pursue FL as the first indication for regulatory approval of G100.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission. ![]()
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended orphan designation for G100 for the treatment of follicular lymphoma (FL).
G100 contains the synthetic small molecule toll-like receptor-4 agonist glucopyranosyl lipid A.
G100 works by activating innate and adaptive immunity in the tumor microenvironment to generate an immune response against the tumor’s pre-existing antigens.
Clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The induction of local and systemic immune responses has been shown in preclinical studies to result in local and abscopal tumor control.
Immune Design, the company developing G100, is currently evaluating G100 plus local radiation, with or without pembrolizumab, in a phase 1/2 trial of FL patients.
Results from this trial were presented at the 2017 ASCO Annual Meeting (abstract 7537). Nine patients who received G100 (3 patients each at the 5, 10, or 20 μg dose) with radiation (but not pembrolizumab) were evaluable for safety and efficacy.
The overall response rate was 44%, and all of these were partial responses (n=4). Thirty-three percent of patients had stable disease (n=3).
Among the responders, tumor regression ranged from 58% to 89%, which included up to 56% shrinkage of abscopal sites. Tumor biopsies showed increased inflammatory responses and T-cell infiltrates in abscopal tumors.
An additional 13 patients treated at the 10 μg dose were evaluable for safety. There were no dose-limiting toxicities, serious adverse events (AEs), or grade 3/4 AEs observed.
Common AEs included injection site disorders, abdominal pain/discomfort, nausea, pruritus, and decrease in lymphocytes.
Immune Design said that, if this trial produces a sufficiently robust clinical benefit for patients, the company may pursue FL as the first indication for regulatory approval of G100.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission. ![]()
Rituximab improves salvage in elderly B-cell lymphoma patients
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
FROM ANNALS OF ONCOLOGY
Key clinical point: Rituximab improved salvage therapy for elderly patients with aggressive-B-cell lymphoma who relapsed after CHOP or R-CHOP.
Major finding: Rituximab as part of a salvage regimen improved the 2-year survival rate from 20.7% to 46.8% (P less than .001).
Data source: Retrospective analysis including 297 elderly patients in the RICOVER-60 trial who had progressive, persistent, or relapsed lymphoma.
Disclosures: Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
New assay may aid diagnosis, treatment of DLBCL
A new assay may help improve the diagnosis and treatment of diffuse large B-cell lymphoma (DLBCL), according to researchers.
The gene expression signature assay can be used to classify subtypes of DLBCL and may enhance disease management by helping to match tumors with the appropriate targeted therapy.
Researchers described the assay in the Journal of Molecular Diagnostics.
The assay is a novel gene expression profiling DLBCL classifier based on reverse transcriptase multiplex ligation-dependent probe amplification (RT-MLPA).
It can simultaneously evaluate the expression of 21 markers, allowing differentiation of the 3 subtypes of DLBCL—germinal center B-cell-like (GCB), activated B-cell-like (ABC), and primary mediastinal B-cell lymphoma (PMBL)—as well as other individualized disease characteristics, such as Epstein-Barr infection status.
Researchers used the RT-MLPA assay to test 150 samples from DLBCL patients. Forty-two percent of the samples were the ABC subtype, 37% the GCB subtype, and 10% molecular PMBL. Eleven percent of the samples could not be classified.
Overall, the RT-MLPA assay correctly assigned 85.0% of the cases into the expected subtypes, compared to 78.8% of samples assigned via immunohistochemistry.
The RT-MLPA assay was also able to detect the MYD88 L265P mutation, one of the most common genetic abnormalities found in ABC DLBCLs. This information can influence treatment, since the presence of the mutation is thought to be predictive of ibrutinib sensitivity.
The researchers said RT-MLPA is a robust, efficient, rapid, and cost-effective alternative to current methods used in the clinic to establish the cell-of-origin classification of DLBCLs.
RT-MLPA requires only common laboratory equipment and can be applied to formalin-fixed, paraffin-embedded samples. Other types of diagnostic methods may not provide the level of detail needed and may also be limited by poor reproducibility and lack of adaptability to routine use in standard laboratories.
“Because we have provided the classification algorithms, other laboratories will be able to verify our results and adjust the procedures to suit their environment,” said study author Philippe Ruminy, PhD, of the Henri Becquerel Cancer Treatment Center, INSERM U1245 in Rouen, France.
“It is our hope that the assay we have developed, which addresses an important recommendation of the recent WHO classifications, will contribute to better management of these tumors and improved patient outcomes.” ![]()
A new assay may help improve the diagnosis and treatment of diffuse large B-cell lymphoma (DLBCL), according to researchers.
The gene expression signature assay can be used to classify subtypes of DLBCL and may enhance disease management by helping to match tumors with the appropriate targeted therapy.
Researchers described the assay in the Journal of Molecular Diagnostics.
The assay is a novel gene expression profiling DLBCL classifier based on reverse transcriptase multiplex ligation-dependent probe amplification (RT-MLPA).
It can simultaneously evaluate the expression of 21 markers, allowing differentiation of the 3 subtypes of DLBCL—germinal center B-cell-like (GCB), activated B-cell-like (ABC), and primary mediastinal B-cell lymphoma (PMBL)—as well as other individualized disease characteristics, such as Epstein-Barr infection status.
Researchers used the RT-MLPA assay to test 150 samples from DLBCL patients. Forty-two percent of the samples were the ABC subtype, 37% the GCB subtype, and 10% molecular PMBL. Eleven percent of the samples could not be classified.
Overall, the RT-MLPA assay correctly assigned 85.0% of the cases into the expected subtypes, compared to 78.8% of samples assigned via immunohistochemistry.
The RT-MLPA assay was also able to detect the MYD88 L265P mutation, one of the most common genetic abnormalities found in ABC DLBCLs. This information can influence treatment, since the presence of the mutation is thought to be predictive of ibrutinib sensitivity.
The researchers said RT-MLPA is a robust, efficient, rapid, and cost-effective alternative to current methods used in the clinic to establish the cell-of-origin classification of DLBCLs.
RT-MLPA requires only common laboratory equipment and can be applied to formalin-fixed, paraffin-embedded samples. Other types of diagnostic methods may not provide the level of detail needed and may also be limited by poor reproducibility and lack of adaptability to routine use in standard laboratories.
“Because we have provided the classification algorithms, other laboratories will be able to verify our results and adjust the procedures to suit their environment,” said study author Philippe Ruminy, PhD, of the Henri Becquerel Cancer Treatment Center, INSERM U1245 in Rouen, France.
“It is our hope that the assay we have developed, which addresses an important recommendation of the recent WHO classifications, will contribute to better management of these tumors and improved patient outcomes.” ![]()
A new assay may help improve the diagnosis and treatment of diffuse large B-cell lymphoma (DLBCL), according to researchers.
The gene expression signature assay can be used to classify subtypes of DLBCL and may enhance disease management by helping to match tumors with the appropriate targeted therapy.
Researchers described the assay in the Journal of Molecular Diagnostics.
The assay is a novel gene expression profiling DLBCL classifier based on reverse transcriptase multiplex ligation-dependent probe amplification (RT-MLPA).
It can simultaneously evaluate the expression of 21 markers, allowing differentiation of the 3 subtypes of DLBCL—germinal center B-cell-like (GCB), activated B-cell-like (ABC), and primary mediastinal B-cell lymphoma (PMBL)—as well as other individualized disease characteristics, such as Epstein-Barr infection status.
Researchers used the RT-MLPA assay to test 150 samples from DLBCL patients. Forty-two percent of the samples were the ABC subtype, 37% the GCB subtype, and 10% molecular PMBL. Eleven percent of the samples could not be classified.
Overall, the RT-MLPA assay correctly assigned 85.0% of the cases into the expected subtypes, compared to 78.8% of samples assigned via immunohistochemistry.
The RT-MLPA assay was also able to detect the MYD88 L265P mutation, one of the most common genetic abnormalities found in ABC DLBCLs. This information can influence treatment, since the presence of the mutation is thought to be predictive of ibrutinib sensitivity.
The researchers said RT-MLPA is a robust, efficient, rapid, and cost-effective alternative to current methods used in the clinic to establish the cell-of-origin classification of DLBCLs.
RT-MLPA requires only common laboratory equipment and can be applied to formalin-fixed, paraffin-embedded samples. Other types of diagnostic methods may not provide the level of detail needed and may also be limited by poor reproducibility and lack of adaptability to routine use in standard laboratories.
“Because we have provided the classification algorithms, other laboratories will be able to verify our results and adjust the procedures to suit their environment,” said study author Philippe Ruminy, PhD, of the Henri Becquerel Cancer Treatment Center, INSERM U1245 in Rouen, France.
“It is our hope that the assay we have developed, which addresses an important recommendation of the recent WHO classifications, will contribute to better management of these tumors and improved patient outcomes.” ![]()
FDA approves second CAR-T therapy
A second chimeric antigen receptor (CAR) T-cell therapy has gained FDA approval, this time for the treatment of large B-cell lymphoma in adults.
“Today marks another milestone in the development of a whole new scientific paradigm for the treatment of serious diseases,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “This approval demonstrates the continued momentum of this promising new area of medicine, and we’re committed to supporting and helping expedite the development of these products.”
Approval was based on ZUMA-1, a multicenter clinical trial of 101 adults with refractory or relapsed large B-cell lymphoma. Almost three-quarters (72%) of patients responded, including 51% who achieved complete remission.
CAR-T therapy can cause severe, life-threatening side effects, most notably cytokine release syndrome (CRS) and neurologic toxicities, for which axicabtagene ciloleucel will carry a boxed warning and will come with a risk evaluation and mitigation strategy (REMS), according to the FDA.
The list price for a single treatment of axicabtagene ciloleucel is $373,000, according to the manufacturer.
“We will soon release a comprehensive policy to address how we plan to support the development of cell-based regenerative medicine,” Dr. Gottlieb said in a statement. “That policy will also clarify how we will apply our expedited programs to breakthrough products that use CAR-T cells and other gene therapies. We remain committed to supporting the efficient development of safe and effective treatments that leverage these new scientific platforms.”
Axicabtagene ciloleucel was developed by Kite Pharma, which was acquired recently by Gilead Sciences.
[email protected]
On Twitter @denisefulton
A second chimeric antigen receptor (CAR) T-cell therapy has gained FDA approval, this time for the treatment of large B-cell lymphoma in adults.
“Today marks another milestone in the development of a whole new scientific paradigm for the treatment of serious diseases,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “This approval demonstrates the continued momentum of this promising new area of medicine, and we’re committed to supporting and helping expedite the development of these products.”
Approval was based on ZUMA-1, a multicenter clinical trial of 101 adults with refractory or relapsed large B-cell lymphoma. Almost three-quarters (72%) of patients responded, including 51% who achieved complete remission.
CAR-T therapy can cause severe, life-threatening side effects, most notably cytokine release syndrome (CRS) and neurologic toxicities, for which axicabtagene ciloleucel will carry a boxed warning and will come with a risk evaluation and mitigation strategy (REMS), according to the FDA.
The list price for a single treatment of axicabtagene ciloleucel is $373,000, according to the manufacturer.
“We will soon release a comprehensive policy to address how we plan to support the development of cell-based regenerative medicine,” Dr. Gottlieb said in a statement. “That policy will also clarify how we will apply our expedited programs to breakthrough products that use CAR-T cells and other gene therapies. We remain committed to supporting the efficient development of safe and effective treatments that leverage these new scientific platforms.”
Axicabtagene ciloleucel was developed by Kite Pharma, which was acquired recently by Gilead Sciences.
[email protected]
On Twitter @denisefulton
A second chimeric antigen receptor (CAR) T-cell therapy has gained FDA approval, this time for the treatment of large B-cell lymphoma in adults.
“Today marks another milestone in the development of a whole new scientific paradigm for the treatment of serious diseases,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “This approval demonstrates the continued momentum of this promising new area of medicine, and we’re committed to supporting and helping expedite the development of these products.”
Approval was based on ZUMA-1, a multicenter clinical trial of 101 adults with refractory or relapsed large B-cell lymphoma. Almost three-quarters (72%) of patients responded, including 51% who achieved complete remission.
CAR-T therapy can cause severe, life-threatening side effects, most notably cytokine release syndrome (CRS) and neurologic toxicities, for which axicabtagene ciloleucel will carry a boxed warning and will come with a risk evaluation and mitigation strategy (REMS), according to the FDA.
The list price for a single treatment of axicabtagene ciloleucel is $373,000, according to the manufacturer.
“We will soon release a comprehensive policy to address how we plan to support the development of cell-based regenerative medicine,” Dr. Gottlieb said in a statement. “That policy will also clarify how we will apply our expedited programs to breakthrough products that use CAR-T cells and other gene therapies. We remain committed to supporting the efficient development of safe and effective treatments that leverage these new scientific platforms.”
Axicabtagene ciloleucel was developed by Kite Pharma, which was acquired recently by Gilead Sciences.
[email protected]
On Twitter @denisefulton
CAR T-cell therapy approved to treat lymphomas
The US Food and Drug Administration (FDA) has approved axicabtagene ciloleucel (Yescarta™, formerly KTE-C19) for use in adults with relapsed or refractory large B-cell lymphoma who have received 2 or more lines of systemic therapy.
Axicabtagene ciloleucel is the first chimeric antigen receptor (CAR) T-cell therapy approved to treat lymphomas.
The approval encompasses diffuse large B-cell lymphoma not otherwise specified, primary mediastinal large B-cell lymphoma, high-grade B-cell lymphoma, and transformed follicular lymphoma.
Axicabtagene ciloleucel is not approved to treat primary central nervous system lymphoma.
The FDA’s approval of axicabtagene ciloleucel was based on results from the phase 2 ZUMA-1 trial. Updated results from this trial were presented at the AACR Annual Meeting 2017.
Risks
Axicabtagene ciloleucel has a Boxed Warning in its product label noting that the therapy can cause cytokine release syndrome (CRS) and neurologic toxicities. Full prescribing information for axicabtagene ciloleucel is available at https://www.yescarta.com/.
Because of the risk of CRS and neurologic toxicities, axicabtagene ciloleucel was approved with a risk evaluation and mitigation strategy (REMS), which includes elements to assure safe use. The FDA is requiring that hospitals and clinics that dispense axicabtagene ciloleucel be specially certified.
As part of that certification, staff who prescribe, dispense, or administer axicabtagene ciloleucel are required to be trained to recognize and manage CRS and nervous system toxicities. In addition, patients must be informed of the potential serious side effects associated with axicabtagene ciloleucel and of the importance of promptly returning to the treatment site if side effects develop.
Additional information about the REMS program can be found at https://www.yescartarems.com/.
To further evaluate the long-term safety of axicabtagene ciloleucel, the FDA is requiring the manufacturer—Kite, a Gilead company—to conduct a post-marketing observational study of patients treated with axicabtagene ciloleucel.
Access and cost
The list price of axicabtagene ciloleucel is $373,000.
The product will be manufactured in Kite’s commercial manufacturing facility in El Segundo, California.
In 2017, Kite established a multi-disciplinary field team focused on providing education and logistics training for medical centers. Now, this team has provided final site certification to 16 centers, enabling them to make axicabtagene ciloleucel available to appropriate patients.
Kite is working to train staff at more than 30 additional centers, with an eventual target of 70 to 90 centers across the US. The latest information on authorized centers is available at https://www.yescarta.com/authorized-treatment-centers/. ![]()
The US Food and Drug Administration (FDA) has approved axicabtagene ciloleucel (Yescarta™, formerly KTE-C19) for use in adults with relapsed or refractory large B-cell lymphoma who have received 2 or more lines of systemic therapy.
Axicabtagene ciloleucel is the first chimeric antigen receptor (CAR) T-cell therapy approved to treat lymphomas.
The approval encompasses diffuse large B-cell lymphoma not otherwise specified, primary mediastinal large B-cell lymphoma, high-grade B-cell lymphoma, and transformed follicular lymphoma.
Axicabtagene ciloleucel is not approved to treat primary central nervous system lymphoma.
The FDA’s approval of axicabtagene ciloleucel was based on results from the phase 2 ZUMA-1 trial. Updated results from this trial were presented at the AACR Annual Meeting 2017.
Risks
Axicabtagene ciloleucel has a Boxed Warning in its product label noting that the therapy can cause cytokine release syndrome (CRS) and neurologic toxicities. Full prescribing information for axicabtagene ciloleucel is available at https://www.yescarta.com/.
Because of the risk of CRS and neurologic toxicities, axicabtagene ciloleucel was approved with a risk evaluation and mitigation strategy (REMS), which includes elements to assure safe use. The FDA is requiring that hospitals and clinics that dispense axicabtagene ciloleucel be specially certified.
As part of that certification, staff who prescribe, dispense, or administer axicabtagene ciloleucel are required to be trained to recognize and manage CRS and nervous system toxicities. In addition, patients must be informed of the potential serious side effects associated with axicabtagene ciloleucel and of the importance of promptly returning to the treatment site if side effects develop.
Additional information about the REMS program can be found at https://www.yescartarems.com/.
To further evaluate the long-term safety of axicabtagene ciloleucel, the FDA is requiring the manufacturer—Kite, a Gilead company—to conduct a post-marketing observational study of patients treated with axicabtagene ciloleucel.
Access and cost
The list price of axicabtagene ciloleucel is $373,000.
The product will be manufactured in Kite’s commercial manufacturing facility in El Segundo, California.
In 2017, Kite established a multi-disciplinary field team focused on providing education and logistics training for medical centers. Now, this team has provided final site certification to 16 centers, enabling them to make axicabtagene ciloleucel available to appropriate patients.
Kite is working to train staff at more than 30 additional centers, with an eventual target of 70 to 90 centers across the US. The latest information on authorized centers is available at https://www.yescarta.com/authorized-treatment-centers/. ![]()
The US Food and Drug Administration (FDA) has approved axicabtagene ciloleucel (Yescarta™, formerly KTE-C19) for use in adults with relapsed or refractory large B-cell lymphoma who have received 2 or more lines of systemic therapy.
Axicabtagene ciloleucel is the first chimeric antigen receptor (CAR) T-cell therapy approved to treat lymphomas.
The approval encompasses diffuse large B-cell lymphoma not otherwise specified, primary mediastinal large B-cell lymphoma, high-grade B-cell lymphoma, and transformed follicular lymphoma.
Axicabtagene ciloleucel is not approved to treat primary central nervous system lymphoma.
The FDA’s approval of axicabtagene ciloleucel was based on results from the phase 2 ZUMA-1 trial. Updated results from this trial were presented at the AACR Annual Meeting 2017.
Risks
Axicabtagene ciloleucel has a Boxed Warning in its product label noting that the therapy can cause cytokine release syndrome (CRS) and neurologic toxicities. Full prescribing information for axicabtagene ciloleucel is available at https://www.yescarta.com/.
Because of the risk of CRS and neurologic toxicities, axicabtagene ciloleucel was approved with a risk evaluation and mitigation strategy (REMS), which includes elements to assure safe use. The FDA is requiring that hospitals and clinics that dispense axicabtagene ciloleucel be specially certified.
As part of that certification, staff who prescribe, dispense, or administer axicabtagene ciloleucel are required to be trained to recognize and manage CRS and nervous system toxicities. In addition, patients must be informed of the potential serious side effects associated with axicabtagene ciloleucel and of the importance of promptly returning to the treatment site if side effects develop.
Additional information about the REMS program can be found at https://www.yescartarems.com/.
To further evaluate the long-term safety of axicabtagene ciloleucel, the FDA is requiring the manufacturer—Kite, a Gilead company—to conduct a post-marketing observational study of patients treated with axicabtagene ciloleucel.
Access and cost
The list price of axicabtagene ciloleucel is $373,000.
The product will be manufactured in Kite’s commercial manufacturing facility in El Segundo, California.
In 2017, Kite established a multi-disciplinary field team focused on providing education and logistics training for medical centers. Now, this team has provided final site certification to 16 centers, enabling them to make axicabtagene ciloleucel available to appropriate patients.
Kite is working to train staff at more than 30 additional centers, with an eventual target of 70 to 90 centers across the US. The latest information on authorized centers is available at https://www.yescarta.com/authorized-treatment-centers/. ![]()
Natural selection opportunities tied to cancer rates
Countries with the lowest opportunities for natural selection have higher cancer rates than countries with the highest opportunities for natural selection, according to a study published in Evolutionary Applications.
Researchers said this is because modern medicine is enabling people to survive cancers, and their genetic backgrounds are passing from one generation to the next.
The team said the rate of some cancers has doubled and even quadrupled over the past 100 to 150 years, and human evolution has moved away from “survival of the fittest.”
“Modern medicine has enabled the human species to live much longer than would otherwise be expected in the natural world,” said study author Maciej Henneberg, PhD, DSc, of the University of Adelaide in South Australia.
“Besides the obvious benefits that modern medicine gives, it also brings with it an unexpected side-effect—allowing genetic material to be passed from one generation to the next that predisposes people to have poor health, such as type 1 diabetes or cancer.”
“Because of the quality of our healthcare in western society, we have almost removed natural selection as the ‘janitor of the gene pool.’ Unfortunately, the accumulation of genetic mutations over time and across multiple generations is like a delayed death sentence.”
Country comparison
The researchers studied global cancer data from the World Health Organization as well as other health and socioeconomic data from the United Nations and the World Bank of 173 countries. The team compared the top 10 countries with the highest opportunities for natural selection to the 10 countries with the lowest opportunities for natural selection.
“We looked at countries that offered the greatest opportunity to survive cancer compared with those that didn’t,” said study author Wenpeng You, a PhD student at the University of Adelaide. “This does not only take into account factors such as socioeconomic status, urbanization, and quality of medical services but also low mortality and fertility rates, which are the 2 distinguishing features in the ‘better’ world.”
“Countries with low mortality rates may allow more people with cancer genetic background to reproduce and pass cancer genes/mutations to the next generation. Meanwhile, low fertility rates in these countries may not be able to have diverse biological variations to provide the opportunity for selecting a naturally fit population—for example, people without or with less cancer genetic background. Low mortality rate and low fertility rate in the ‘better’ world may have formed a self-reinforcing cycle which has accumulated cancer genetic background at a greater rate than previously thought.”
Based on the researchers’ analysis, the 20 countries are:
| Lowest opportunities for natural selection | Highest opportunities for natural selection |
| Iceland | Burkina Faso |
| Singapore | Chad |
| Japan | Central African Republic |
| Switzerland | Afghanistan |
| Sweden | Somalia |
| Luxembourg | Sierra Leone |
| Germany | Democratic Republic of the Congo |
| Italy | Guinea-Bissau |
| Cyprus | Burundi |
| Andorra | Cameroon |
Cancer incidence
The researchers found the rates of most cancers were higher in the 10 countries with the lowest opportunities for natural selection. The incidence of all cancers was 2.326 times higher in the low-opportunity countries than the high-opportunity ones.
The increased incidences of hematologic malignancies were as follows:
- Non-Hodgkin lymphoma—2.019 times higher in the low-opportunity countries
- Hodgkin lymphoma—3.314 times higher in the low-opportunity countries
- Leukemia—3.574 times higher in the low-opportunity countries
- Multiple myeloma—4.257 times higher in the low-opportunity countries .
Dr Henneberg said that, having removed natural selection as the “janitor of the gene pool,” our modern society is faced with a controversial issue.
“It may be that the only way humankind can be rid of cancer once and for all is through genetic engineering—to repair our genes and take cancer out of the equation,” he said. ![]()
Countries with the lowest opportunities for natural selection have higher cancer rates than countries with the highest opportunities for natural selection, according to a study published in Evolutionary Applications.
Researchers said this is because modern medicine is enabling people to survive cancers, and their genetic backgrounds are passing from one generation to the next.
The team said the rate of some cancers has doubled and even quadrupled over the past 100 to 150 years, and human evolution has moved away from “survival of the fittest.”
“Modern medicine has enabled the human species to live much longer than would otherwise be expected in the natural world,” said study author Maciej Henneberg, PhD, DSc, of the University of Adelaide in South Australia.
“Besides the obvious benefits that modern medicine gives, it also brings with it an unexpected side-effect—allowing genetic material to be passed from one generation to the next that predisposes people to have poor health, such as type 1 diabetes or cancer.”
“Because of the quality of our healthcare in western society, we have almost removed natural selection as the ‘janitor of the gene pool.’ Unfortunately, the accumulation of genetic mutations over time and across multiple generations is like a delayed death sentence.”
Country comparison
The researchers studied global cancer data from the World Health Organization as well as other health and socioeconomic data from the United Nations and the World Bank of 173 countries. The team compared the top 10 countries with the highest opportunities for natural selection to the 10 countries with the lowest opportunities for natural selection.
“We looked at countries that offered the greatest opportunity to survive cancer compared with those that didn’t,” said study author Wenpeng You, a PhD student at the University of Adelaide. “This does not only take into account factors such as socioeconomic status, urbanization, and quality of medical services but also low mortality and fertility rates, which are the 2 distinguishing features in the ‘better’ world.”
“Countries with low mortality rates may allow more people with cancer genetic background to reproduce and pass cancer genes/mutations to the next generation. Meanwhile, low fertility rates in these countries may not be able to have diverse biological variations to provide the opportunity for selecting a naturally fit population—for example, people without or with less cancer genetic background. Low mortality rate and low fertility rate in the ‘better’ world may have formed a self-reinforcing cycle which has accumulated cancer genetic background at a greater rate than previously thought.”
Based on the researchers’ analysis, the 20 countries are:
| Lowest opportunities for natural selection | Highest opportunities for natural selection |
| Iceland | Burkina Faso |
| Singapore | Chad |
| Japan | Central African Republic |
| Switzerland | Afghanistan |
| Sweden | Somalia |
| Luxembourg | Sierra Leone |
| Germany | Democratic Republic of the Congo |
| Italy | Guinea-Bissau |
| Cyprus | Burundi |
| Andorra | Cameroon |
Cancer incidence
The researchers found the rates of most cancers were higher in the 10 countries with the lowest opportunities for natural selection. The incidence of all cancers was 2.326 times higher in the low-opportunity countries than the high-opportunity ones.
The increased incidences of hematologic malignancies were as follows:
- Non-Hodgkin lymphoma—2.019 times higher in the low-opportunity countries
- Hodgkin lymphoma—3.314 times higher in the low-opportunity countries
- Leukemia—3.574 times higher in the low-opportunity countries
- Multiple myeloma—4.257 times higher in the low-opportunity countries .
Dr Henneberg said that, having removed natural selection as the “janitor of the gene pool,” our modern society is faced with a controversial issue.
“It may be that the only way humankind can be rid of cancer once and for all is through genetic engineering—to repair our genes and take cancer out of the equation,” he said. ![]()
Countries with the lowest opportunities for natural selection have higher cancer rates than countries with the highest opportunities for natural selection, according to a study published in Evolutionary Applications.
Researchers said this is because modern medicine is enabling people to survive cancers, and their genetic backgrounds are passing from one generation to the next.
The team said the rate of some cancers has doubled and even quadrupled over the past 100 to 150 years, and human evolution has moved away from “survival of the fittest.”
“Modern medicine has enabled the human species to live much longer than would otherwise be expected in the natural world,” said study author Maciej Henneberg, PhD, DSc, of the University of Adelaide in South Australia.
“Besides the obvious benefits that modern medicine gives, it also brings with it an unexpected side-effect—allowing genetic material to be passed from one generation to the next that predisposes people to have poor health, such as type 1 diabetes or cancer.”
“Because of the quality of our healthcare in western society, we have almost removed natural selection as the ‘janitor of the gene pool.’ Unfortunately, the accumulation of genetic mutations over time and across multiple generations is like a delayed death sentence.”
Country comparison
The researchers studied global cancer data from the World Health Organization as well as other health and socioeconomic data from the United Nations and the World Bank of 173 countries. The team compared the top 10 countries with the highest opportunities for natural selection to the 10 countries with the lowest opportunities for natural selection.
“We looked at countries that offered the greatest opportunity to survive cancer compared with those that didn’t,” said study author Wenpeng You, a PhD student at the University of Adelaide. “This does not only take into account factors such as socioeconomic status, urbanization, and quality of medical services but also low mortality and fertility rates, which are the 2 distinguishing features in the ‘better’ world.”
“Countries with low mortality rates may allow more people with cancer genetic background to reproduce and pass cancer genes/mutations to the next generation. Meanwhile, low fertility rates in these countries may not be able to have diverse biological variations to provide the opportunity for selecting a naturally fit population—for example, people without or with less cancer genetic background. Low mortality rate and low fertility rate in the ‘better’ world may have formed a self-reinforcing cycle which has accumulated cancer genetic background at a greater rate than previously thought.”
Based on the researchers’ analysis, the 20 countries are:
| Lowest opportunities for natural selection | Highest opportunities for natural selection |
| Iceland | Burkina Faso |
| Singapore | Chad |
| Japan | Central African Republic |
| Switzerland | Afghanistan |
| Sweden | Somalia |
| Luxembourg | Sierra Leone |
| Germany | Democratic Republic of the Congo |
| Italy | Guinea-Bissau |
| Cyprus | Burundi |
| Andorra | Cameroon |
Cancer incidence
The researchers found the rates of most cancers were higher in the 10 countries with the lowest opportunities for natural selection. The incidence of all cancers was 2.326 times higher in the low-opportunity countries than the high-opportunity ones.
The increased incidences of hematologic malignancies were as follows:
- Non-Hodgkin lymphoma—2.019 times higher in the low-opportunity countries
- Hodgkin lymphoma—3.314 times higher in the low-opportunity countries
- Leukemia—3.574 times higher in the low-opportunity countries
- Multiple myeloma—4.257 times higher in the low-opportunity countries .
Dr Henneberg said that, having removed natural selection as the “janitor of the gene pool,” our modern society is faced with a controversial issue.
“It may be that the only way humankind can be rid of cancer once and for all is through genetic engineering—to repair our genes and take cancer out of the equation,” he said.