User login
Children with Acute Hematogenous Osteomyelitis Have Similar Outcomes When Discharged with Oral Antibiotics versus Prolonged IV Antibiotics and Escape PICC Complications
Clinical question: After hospitalization for acute hematogenous osteomyelitis (AHOM), do children discharged with oral antibiotics have similar clinical outcomes compared to those discharged with home IV antibiotics?
Background: AHOM occurs in one in 5,000 children yearly and makes up approximately 1% of pediatric hospitalizations in the U.S.1 The incidence of AHOM might be increasing in some communities, concurrent with the increasing prevalence of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA).2 Uncomplicated AHOM typically is defined as osteomyelitis not associated with trauma, with less than 14 days of symptoms and not requiring surgical intervention beyond diagnostic sampling.1 Most recent published studies support a seven-day inpatient course of IV antibiotics for uncomplicated AHOM, followed by 21 to 28 days of oral therapy for patients who continue to improve clinically.1 Significant variability exists in practice, with a recent study of free-standing children’s hospitals showing rates of transition to oral antibiotics after hospitalization for AHOM ranging from approximately 10% to more than 90%.3
Study design: Multi-center, retrospective, cohort study.
Setting: Thirty-eight U.S. children’s hospitals.
Synopsis: Researchers used clinical and billing data from the Pediatric Health Information System (PHIS) to identify children between the ages of two months and 18 years over a 48-month period who were discharged with a diagnosis of acute or unspecified osteomyelitis based on ICD-9-CM coding.
PHIS is a database of administrative, billing, and clinical details derived from hospitalizations at 44 U.S. children’s hospitals.
Exclusions from the study were numerous, and included:
- Hospitalization in the six months prior with acute, unspecified, or chronic osteomyelitis;
- Chronic cardiac, hematologic, immunologic, oncologic, or respiratory conditions that would increase the risk of treatment failure;
- Transfer either to or from the hospital at any point during hospitalization;
- More than one site of osteomyelitis;
- Length of stay of less than two or more than 14 days;
- Inability to take antibiotics orally or enterally;
- Malabsorption disorders;
- Primary diagnosis of cellulitis or septic arthritis;
- Orthopedic hardware or bone fractures;
- Prolonged immobilization or developed pressure ulcers; and
- Osteomyelitis of the head, face, and orbits.
Local physicians and research assistants at each hospital site reviewed medical records to confirm the validity of the ICD-9-CM diagnosis, determine the post-discharge antibiotic details, review for return ED visits or readmission within six months, and extract culture results. Primary outcome was treatment failure, defined as revisit to the ED or readmission for a change in antibiotic treatment (type, dosage, or prolongation), drainage of abscess, debridement, bone biopsy, or conversion to PICC route. Secondary outcomes included a return to ED or rehospitalization for adverse drug reactions (vomiting/diarrhea, dehydration, C. difficile infection, allergic reactions, drug-induced neutropenia, acute kidney injury) or PICC complication (fever evaluation, PICC site infection, blood stream infection, sepsis, thrombosis, breakage, repair, adjustment, manipulation, or PICC removal).
Of 8,555 patients from 38 hospitals who satisfied inclusion criteria, 2,060 patients from 36 hospitals remained after application of exclusion criteria, with 1,005 receiving antibiotics orally and 1,055 via a peripherally inserted central catheter (PICC) upon discharge. Median length of stay was six days, and the percentage of patients discharged on oral antibiotics ranged widely at the hospital level, from zero to 100%. Patients were most commonly discharged on clindamycin (50%) and cephalexin (37%) in the oral cohort, and clindamycin (36%) and cefazolin (33%) in the PICC cohort.
The rate of treatment failure was similar in unmatched analyses of the oral cohort (5%) versus the PICC cohort (6%). This similarity persisted in across-hospital and within-hospital matched analyses. Rates of adverse drug reactions were low (<4%) in both groups, but 15% of the PICC cohort returned to the ED or were readmitted for a PICC complication.
Bottom line: Previously healthy children hospitalized with a single focus of AHOM have similarly low rates of treatment failure whether discharged on oral- or PICC-administered antibiotics. Patients discharged with PICC-administered antibiotics suffer from a higher rate of return ED visit or readmission due to PICC-related complications.

References
- Majewski J, Del Vecchio M, Aronoff S. Route and length of therapy of acute uncomplicated hematogenous osteomyelitis: do we have the answers yet? Hosp Pediatr. 2014;4(1):44-47.
- Arnold SR, Elias D, Buckingham SC, et al. Changing patterns of acute hematogenous osteomyelitis and septic arthritis: emergence of community-associated methicillin-resistant Staphylococcus aureus. J Pediatr Orthop. 2006;26(6):703-708.
- Zaoutis T, Localio AR, Leckerman K, Saddlemire S, Bertoch D, Keren R. Prolonged intravenous therapy versus eraly transtion to oral antimicrobial therapy for acute osteomyelitis in children. Pediatrics. 2009;123(2):636-642.
Clinical question: After hospitalization for acute hematogenous osteomyelitis (AHOM), do children discharged with oral antibiotics have similar clinical outcomes compared to those discharged with home IV antibiotics?
Background: AHOM occurs in one in 5,000 children yearly and makes up approximately 1% of pediatric hospitalizations in the U.S.1 The incidence of AHOM might be increasing in some communities, concurrent with the increasing prevalence of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA).2 Uncomplicated AHOM typically is defined as osteomyelitis not associated with trauma, with less than 14 days of symptoms and not requiring surgical intervention beyond diagnostic sampling.1 Most recent published studies support a seven-day inpatient course of IV antibiotics for uncomplicated AHOM, followed by 21 to 28 days of oral therapy for patients who continue to improve clinically.1 Significant variability exists in practice, with a recent study of free-standing children’s hospitals showing rates of transition to oral antibiotics after hospitalization for AHOM ranging from approximately 10% to more than 90%.3
Study design: Multi-center, retrospective, cohort study.
Setting: Thirty-eight U.S. children’s hospitals.
Synopsis: Researchers used clinical and billing data from the Pediatric Health Information System (PHIS) to identify children between the ages of two months and 18 years over a 48-month period who were discharged with a diagnosis of acute or unspecified osteomyelitis based on ICD-9-CM coding.
PHIS is a database of administrative, billing, and clinical details derived from hospitalizations at 44 U.S. children’s hospitals.
Exclusions from the study were numerous, and included:
- Hospitalization in the six months prior with acute, unspecified, or chronic osteomyelitis;
- Chronic cardiac, hematologic, immunologic, oncologic, or respiratory conditions that would increase the risk of treatment failure;
- Transfer either to or from the hospital at any point during hospitalization;
- More than one site of osteomyelitis;
- Length of stay of less than two or more than 14 days;
- Inability to take antibiotics orally or enterally;
- Malabsorption disorders;
- Primary diagnosis of cellulitis or septic arthritis;
- Orthopedic hardware or bone fractures;
- Prolonged immobilization or developed pressure ulcers; and
- Osteomyelitis of the head, face, and orbits.
Local physicians and research assistants at each hospital site reviewed medical records to confirm the validity of the ICD-9-CM diagnosis, determine the post-discharge antibiotic details, review for return ED visits or readmission within six months, and extract culture results. Primary outcome was treatment failure, defined as revisit to the ED or readmission for a change in antibiotic treatment (type, dosage, or prolongation), drainage of abscess, debridement, bone biopsy, or conversion to PICC route. Secondary outcomes included a return to ED or rehospitalization for adverse drug reactions (vomiting/diarrhea, dehydration, C. difficile infection, allergic reactions, drug-induced neutropenia, acute kidney injury) or PICC complication (fever evaluation, PICC site infection, blood stream infection, sepsis, thrombosis, breakage, repair, adjustment, manipulation, or PICC removal).
Of 8,555 patients from 38 hospitals who satisfied inclusion criteria, 2,060 patients from 36 hospitals remained after application of exclusion criteria, with 1,005 receiving antibiotics orally and 1,055 via a peripherally inserted central catheter (PICC) upon discharge. Median length of stay was six days, and the percentage of patients discharged on oral antibiotics ranged widely at the hospital level, from zero to 100%. Patients were most commonly discharged on clindamycin (50%) and cephalexin (37%) in the oral cohort, and clindamycin (36%) and cefazolin (33%) in the PICC cohort.
The rate of treatment failure was similar in unmatched analyses of the oral cohort (5%) versus the PICC cohort (6%). This similarity persisted in across-hospital and within-hospital matched analyses. Rates of adverse drug reactions were low (<4%) in both groups, but 15% of the PICC cohort returned to the ED or were readmitted for a PICC complication.
Bottom line: Previously healthy children hospitalized with a single focus of AHOM have similarly low rates of treatment failure whether discharged on oral- or PICC-administered antibiotics. Patients discharged with PICC-administered antibiotics suffer from a higher rate of return ED visit or readmission due to PICC-related complications.

References
- Majewski J, Del Vecchio M, Aronoff S. Route and length of therapy of acute uncomplicated hematogenous osteomyelitis: do we have the answers yet? Hosp Pediatr. 2014;4(1):44-47.
- Arnold SR, Elias D, Buckingham SC, et al. Changing patterns of acute hematogenous osteomyelitis and septic arthritis: emergence of community-associated methicillin-resistant Staphylococcus aureus. J Pediatr Orthop. 2006;26(6):703-708.
- Zaoutis T, Localio AR, Leckerman K, Saddlemire S, Bertoch D, Keren R. Prolonged intravenous therapy versus eraly transtion to oral antimicrobial therapy for acute osteomyelitis in children. Pediatrics. 2009;123(2):636-642.
Clinical question: After hospitalization for acute hematogenous osteomyelitis (AHOM), do children discharged with oral antibiotics have similar clinical outcomes compared to those discharged with home IV antibiotics?
Background: AHOM occurs in one in 5,000 children yearly and makes up approximately 1% of pediatric hospitalizations in the U.S.1 The incidence of AHOM might be increasing in some communities, concurrent with the increasing prevalence of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA).2 Uncomplicated AHOM typically is defined as osteomyelitis not associated with trauma, with less than 14 days of symptoms and not requiring surgical intervention beyond diagnostic sampling.1 Most recent published studies support a seven-day inpatient course of IV antibiotics for uncomplicated AHOM, followed by 21 to 28 days of oral therapy for patients who continue to improve clinically.1 Significant variability exists in practice, with a recent study of free-standing children’s hospitals showing rates of transition to oral antibiotics after hospitalization for AHOM ranging from approximately 10% to more than 90%.3
Study design: Multi-center, retrospective, cohort study.
Setting: Thirty-eight U.S. children’s hospitals.
Synopsis: Researchers used clinical and billing data from the Pediatric Health Information System (PHIS) to identify children between the ages of two months and 18 years over a 48-month period who were discharged with a diagnosis of acute or unspecified osteomyelitis based on ICD-9-CM coding.
PHIS is a database of administrative, billing, and clinical details derived from hospitalizations at 44 U.S. children’s hospitals.
Exclusions from the study were numerous, and included:
- Hospitalization in the six months prior with acute, unspecified, or chronic osteomyelitis;
- Chronic cardiac, hematologic, immunologic, oncologic, or respiratory conditions that would increase the risk of treatment failure;
- Transfer either to or from the hospital at any point during hospitalization;
- More than one site of osteomyelitis;
- Length of stay of less than two or more than 14 days;
- Inability to take antibiotics orally or enterally;
- Malabsorption disorders;
- Primary diagnosis of cellulitis or septic arthritis;
- Orthopedic hardware or bone fractures;
- Prolonged immobilization or developed pressure ulcers; and
- Osteomyelitis of the head, face, and orbits.
Local physicians and research assistants at each hospital site reviewed medical records to confirm the validity of the ICD-9-CM diagnosis, determine the post-discharge antibiotic details, review for return ED visits or readmission within six months, and extract culture results. Primary outcome was treatment failure, defined as revisit to the ED or readmission for a change in antibiotic treatment (type, dosage, or prolongation), drainage of abscess, debridement, bone biopsy, or conversion to PICC route. Secondary outcomes included a return to ED or rehospitalization for adverse drug reactions (vomiting/diarrhea, dehydration, C. difficile infection, allergic reactions, drug-induced neutropenia, acute kidney injury) or PICC complication (fever evaluation, PICC site infection, blood stream infection, sepsis, thrombosis, breakage, repair, adjustment, manipulation, or PICC removal).
Of 8,555 patients from 38 hospitals who satisfied inclusion criteria, 2,060 patients from 36 hospitals remained after application of exclusion criteria, with 1,005 receiving antibiotics orally and 1,055 via a peripherally inserted central catheter (PICC) upon discharge. Median length of stay was six days, and the percentage of patients discharged on oral antibiotics ranged widely at the hospital level, from zero to 100%. Patients were most commonly discharged on clindamycin (50%) and cephalexin (37%) in the oral cohort, and clindamycin (36%) and cefazolin (33%) in the PICC cohort.
The rate of treatment failure was similar in unmatched analyses of the oral cohort (5%) versus the PICC cohort (6%). This similarity persisted in across-hospital and within-hospital matched analyses. Rates of adverse drug reactions were low (<4%) in both groups, but 15% of the PICC cohort returned to the ED or were readmitted for a PICC complication.
Bottom line: Previously healthy children hospitalized with a single focus of AHOM have similarly low rates of treatment failure whether discharged on oral- or PICC-administered antibiotics. Patients discharged with PICC-administered antibiotics suffer from a higher rate of return ED visit or readmission due to PICC-related complications.

References
- Majewski J, Del Vecchio M, Aronoff S. Route and length of therapy of acute uncomplicated hematogenous osteomyelitis: do we have the answers yet? Hosp Pediatr. 2014;4(1):44-47.
- Arnold SR, Elias D, Buckingham SC, et al. Changing patterns of acute hematogenous osteomyelitis and septic arthritis: emergence of community-associated methicillin-resistant Staphylococcus aureus. J Pediatr Orthop. 2006;26(6):703-708.
- Zaoutis T, Localio AR, Leckerman K, Saddlemire S, Bertoch D, Keren R. Prolonged intravenous therapy versus eraly transtion to oral antimicrobial therapy for acute osteomyelitis in children. Pediatrics. 2009;123(2):636-642.
Procalcitonin-Based Algorithm Does Not Reduce Antibiotic Use in the ICU
Clinical question
Can a procalcitonin-based algorithm reduce antibiotic use in critically ill patients?
Bottom line
A procalcitonin-based algorithm using a 0.1 ng/mL cutoff does not significantly decrease the duration of antibiotic treatment in critically ill patients nor does it reduce length of stay or number of deaths. The rate of decline in the procalcitonin level over the first 72 hours, however, does serve as an independent predictor of short-term and long-term all-cause mortality. (LOE = 1b-)
Reference
Study design: Randomized controlled trial (nonblinded)
Funding source: Foundation
Allocation: Concealed
Setting: Inpatient (ICU only)
Synopsis
Procalcitonin (PCT) is a sepsis biomarker that has been utilized to guide antibiotic use in different patient populations. In this study, the authors tested a PCT-algorithm using a 0.1 ng/mL cut-off to reduce antibiotic exposure in critically ill patients. Patients newly admitted to intensive care units (ICUs) who were receiving antibiotics for suspected infections were randomized, using concealed allocation, to receive PCT-guided care (n = 196) or standard care (n = 198). All patients had PCT levels drawn daily until discharge from the ICU or up to a maximum of 7 days. In the PCT group, antibiotics were stopped if PCT levels were negative (< 0.1 ng/mL), if PCT levels were borderline (0.1 - 0.25 ng/mL) and infection was unlikely, or if PCT levels decreased more than 90% from baseline values. In the standard care group, the treating clinician determined antibiotic use without knowledge of the PCT results. Baseline characteristics of the 2 groups were similar with regard to severity-of-disease scores and baseline PCT values. There was high compliance with the PCT algorithm, with less than 3% of study days when the algorithm was not followed. There was no significant difference detected between the 2 groups for the primary outcome of time to antibiotic cessation. However, duration of antibiotic use was longer than expected in the control group (11 days actual vs 9 days expected), so the study may have been underpowered to detect an expected 25% reduction. Nevertheless, the 2 groups were similar with regard to ICU and hospital lengths of stay, as well as ICU, hospital, and 90-day mortality rates. Of note, the rate of decline in PCT level over the first 72 hours was an independent predictor of hospital mortality and 90-day mortality, with a slower decline corresponding to a higher mortality.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Can a procalcitonin-based algorithm reduce antibiotic use in critically ill patients?
Bottom line
A procalcitonin-based algorithm using a 0.1 ng/mL cutoff does not significantly decrease the duration of antibiotic treatment in critically ill patients nor does it reduce length of stay or number of deaths. The rate of decline in the procalcitonin level over the first 72 hours, however, does serve as an independent predictor of short-term and long-term all-cause mortality. (LOE = 1b-)
Reference
Study design: Randomized controlled trial (nonblinded)
Funding source: Foundation
Allocation: Concealed
Setting: Inpatient (ICU only)
Synopsis
Procalcitonin (PCT) is a sepsis biomarker that has been utilized to guide antibiotic use in different patient populations. In this study, the authors tested a PCT-algorithm using a 0.1 ng/mL cut-off to reduce antibiotic exposure in critically ill patients. Patients newly admitted to intensive care units (ICUs) who were receiving antibiotics for suspected infections were randomized, using concealed allocation, to receive PCT-guided care (n = 196) or standard care (n = 198). All patients had PCT levels drawn daily until discharge from the ICU or up to a maximum of 7 days. In the PCT group, antibiotics were stopped if PCT levels were negative (< 0.1 ng/mL), if PCT levels were borderline (0.1 - 0.25 ng/mL) and infection was unlikely, or if PCT levels decreased more than 90% from baseline values. In the standard care group, the treating clinician determined antibiotic use without knowledge of the PCT results. Baseline characteristics of the 2 groups were similar with regard to severity-of-disease scores and baseline PCT values. There was high compliance with the PCT algorithm, with less than 3% of study days when the algorithm was not followed. There was no significant difference detected between the 2 groups for the primary outcome of time to antibiotic cessation. However, duration of antibiotic use was longer than expected in the control group (11 days actual vs 9 days expected), so the study may have been underpowered to detect an expected 25% reduction. Nevertheless, the 2 groups were similar with regard to ICU and hospital lengths of stay, as well as ICU, hospital, and 90-day mortality rates. Of note, the rate of decline in PCT level over the first 72 hours was an independent predictor of hospital mortality and 90-day mortality, with a slower decline corresponding to a higher mortality.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Can a procalcitonin-based algorithm reduce antibiotic use in critically ill patients?
Bottom line
A procalcitonin-based algorithm using a 0.1 ng/mL cutoff does not significantly decrease the duration of antibiotic treatment in critically ill patients nor does it reduce length of stay or number of deaths. The rate of decline in the procalcitonin level over the first 72 hours, however, does serve as an independent predictor of short-term and long-term all-cause mortality. (LOE = 1b-)
Reference
Study design: Randomized controlled trial (nonblinded)
Funding source: Foundation
Allocation: Concealed
Setting: Inpatient (ICU only)
Synopsis
Procalcitonin (PCT) is a sepsis biomarker that has been utilized to guide antibiotic use in different patient populations. In this study, the authors tested a PCT-algorithm using a 0.1 ng/mL cut-off to reduce antibiotic exposure in critically ill patients. Patients newly admitted to intensive care units (ICUs) who were receiving antibiotics for suspected infections were randomized, using concealed allocation, to receive PCT-guided care (n = 196) or standard care (n = 198). All patients had PCT levels drawn daily until discharge from the ICU or up to a maximum of 7 days. In the PCT group, antibiotics were stopped if PCT levels were negative (< 0.1 ng/mL), if PCT levels were borderline (0.1 - 0.25 ng/mL) and infection was unlikely, or if PCT levels decreased more than 90% from baseline values. In the standard care group, the treating clinician determined antibiotic use without knowledge of the PCT results. Baseline characteristics of the 2 groups were similar with regard to severity-of-disease scores and baseline PCT values. There was high compliance with the PCT algorithm, with less than 3% of study days when the algorithm was not followed. There was no significant difference detected between the 2 groups for the primary outcome of time to antibiotic cessation. However, duration of antibiotic use was longer than expected in the control group (11 days actual vs 9 days expected), so the study may have been underpowered to detect an expected 25% reduction. Nevertheless, the 2 groups were similar with regard to ICU and hospital lengths of stay, as well as ICU, hospital, and 90-day mortality rates. Of note, the rate of decline in PCT level over the first 72 hours was an independent predictor of hospital mortality and 90-day mortality, with a slower decline corresponding to a higher mortality.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Antibiotic Therapy Guidelines for Pediatric Pneumonia Helpful, Not Hurtful
Hospitalists need not fear negative consequences when prescribing guideline-recommended antibiotic therapy for children hospitalized with community-acquired pneumonia (CAP), according to a recent study conducted at Cincinnati Children’s Hospital Medical Center (CCHMC).
"Guideline-recommended therapy for pediatric pneumonia did not result in different outcomes than nonrecommended [largely cephalosporin] therapy," lead author and CCHMC-based hospitalist Joanna Thomson MD, MPH, says in an email to The Hospitalist.
Published in the Journal of Hospital Medicine, the study followed the outcomes of 168 pediatric inpatients ages 3 months to 18 years who were prescribed empiric guideline-recommended therapy, which advises using an aminopenicillin first rather than a broad-spectrum antibiotic. The study focused on patients’ outcomes, specifically length of stay (LOS), total cost of hospitalization, and inpatient pharmacy costs, and found no difference in LOS or costs for patients treated according to guidelines compared with those whose treatment varied from the recommendations.
"Given growing concerns regarding antimicrobial resistance, it is pretty easy to extrapolate the benefits of using narrow-spectrum therapy, but we wanted to make sure that it wasn't resulting in negative unintended consequences," Dr. Thomson says. "Indeed, use of guideline-recommended therapy did not change our outcomes."
However, most patients hospitalized with CAP do not currently receive guideline-recommended therapy, according to Dr. Thomson. CCHMC had been one of those institutions overprescribing cephalosporin, with nearly 70% of children admitted with pneumonia receiving the antibiotic. That practice has since changed, she notes.
"The majority of hospitalized patients in the U.S. still receive broad-spectrum cephalosporins," Dr. Thomson says. "I suspect that this may partially be due to fears of unintended negative consequences. We should all be good stewards and prescribe guideline-recommended therapy whenever possible."
Visit our website for more information on antibiotic prescription practices.
Hospitalists need not fear negative consequences when prescribing guideline-recommended antibiotic therapy for children hospitalized with community-acquired pneumonia (CAP), according to a recent study conducted at Cincinnati Children’s Hospital Medical Center (CCHMC).
"Guideline-recommended therapy for pediatric pneumonia did not result in different outcomes than nonrecommended [largely cephalosporin] therapy," lead author and CCHMC-based hospitalist Joanna Thomson MD, MPH, says in an email to The Hospitalist.
Published in the Journal of Hospital Medicine, the study followed the outcomes of 168 pediatric inpatients ages 3 months to 18 years who were prescribed empiric guideline-recommended therapy, which advises using an aminopenicillin first rather than a broad-spectrum antibiotic. The study focused on patients’ outcomes, specifically length of stay (LOS), total cost of hospitalization, and inpatient pharmacy costs, and found no difference in LOS or costs for patients treated according to guidelines compared with those whose treatment varied from the recommendations.
"Given growing concerns regarding antimicrobial resistance, it is pretty easy to extrapolate the benefits of using narrow-spectrum therapy, but we wanted to make sure that it wasn't resulting in negative unintended consequences," Dr. Thomson says. "Indeed, use of guideline-recommended therapy did not change our outcomes."
However, most patients hospitalized with CAP do not currently receive guideline-recommended therapy, according to Dr. Thomson. CCHMC had been one of those institutions overprescribing cephalosporin, with nearly 70% of children admitted with pneumonia receiving the antibiotic. That practice has since changed, she notes.
"The majority of hospitalized patients in the U.S. still receive broad-spectrum cephalosporins," Dr. Thomson says. "I suspect that this may partially be due to fears of unintended negative consequences. We should all be good stewards and prescribe guideline-recommended therapy whenever possible."
Visit our website for more information on antibiotic prescription practices.
Hospitalists need not fear negative consequences when prescribing guideline-recommended antibiotic therapy for children hospitalized with community-acquired pneumonia (CAP), according to a recent study conducted at Cincinnati Children’s Hospital Medical Center (CCHMC).
"Guideline-recommended therapy for pediatric pneumonia did not result in different outcomes than nonrecommended [largely cephalosporin] therapy," lead author and CCHMC-based hospitalist Joanna Thomson MD, MPH, says in an email to The Hospitalist.
Published in the Journal of Hospital Medicine, the study followed the outcomes of 168 pediatric inpatients ages 3 months to 18 years who were prescribed empiric guideline-recommended therapy, which advises using an aminopenicillin first rather than a broad-spectrum antibiotic. The study focused on patients’ outcomes, specifically length of stay (LOS), total cost of hospitalization, and inpatient pharmacy costs, and found no difference in LOS or costs for patients treated according to guidelines compared with those whose treatment varied from the recommendations.
"Given growing concerns regarding antimicrobial resistance, it is pretty easy to extrapolate the benefits of using narrow-spectrum therapy, but we wanted to make sure that it wasn't resulting in negative unintended consequences," Dr. Thomson says. "Indeed, use of guideline-recommended therapy did not change our outcomes."
However, most patients hospitalized with CAP do not currently receive guideline-recommended therapy, according to Dr. Thomson. CCHMC had been one of those institutions overprescribing cephalosporin, with nearly 70% of children admitted with pneumonia receiving the antibiotic. That practice has since changed, she notes.
"The majority of hospitalized patients in the U.S. still receive broad-spectrum cephalosporins," Dr. Thomson says. "I suspect that this may partially be due to fears of unintended negative consequences. We should all be good stewards and prescribe guideline-recommended therapy whenever possible."
Visit our website for more information on antibiotic prescription practices.
Antibiotic Overprescribing Sparks Call for Stronger Stewardship
Antibiotic overprescription remains a problem in the U.S. and abroad and shows no signs of slowing. A study published in the October 2014 issue of JAMA reports that nearly half of all hospitalized patients receive antibiotics, and the drugs most commonly prescribed are broad-spectrum antibiotics, which have been linked with promoting the spread of antibiotic-resistant bacteria. Based on a one-day prevalence survey of more than 11,000 patients in 183 U.S. hospitals in 2011, the study notes that half of inpatients prescribed antibiotics received two or more of them. The CDC estimates that 20% to 50% of all antibiotics prescribed in U.S. hospitals are either unnecessary or inappropriate, and many of them count adverse drug reactions among their side effects .
While a growing body of evidence suggests that hospital-based antibiotic stewardship programs can optimize treatment, reduce antibacterial side effects, and save money, a study published September 2014 in JAMA says those benefits may be lost post-discharge. Results of a randomized trial of an outpatient antimicrobial stewardship intervention found that an initial 50% reduction in antibiotic prescriptions was lost when their targeted interventions ceased.
“These data suggest that audit and feedback was a vital element of this intervention and that antimicrobial stewardship requires continued, active efforts to sustain initial improvements,” says lead author Jeffrey S. Gerber, MD, PhD, CHCP, attending physician in infectious diseases at the Children’s Hospital of Philadelphia.
The federal government has taken a three-pronged approach to the problem: a report from the President’s Council of Advisors on Science and Technology with recommendations for monitoring superbugs and slowing their spread; an executive order issued by President Obama on September 18, 2014 with a commitment to “accelerate scientific research and facilitate the development of new antibacterial drugs;” and the creation of a national task force charged with designing a national strategy to combat antibiotic overuse by February 2015.
The President’s Council report notes that bacteria are becoming resistant to antibiotics in large part because these drugs are overprescribed to patients and overused in animals raised for food. The report recommends the CDC develop rules by 2017 requiring hospitals and nursing homes to implement best practices for antibiotic use.
Antibiotic overprescription remains a problem in the U.S. and abroad and shows no signs of slowing. A study published in the October 2014 issue of JAMA reports that nearly half of all hospitalized patients receive antibiotics, and the drugs most commonly prescribed are broad-spectrum antibiotics, which have been linked with promoting the spread of antibiotic-resistant bacteria. Based on a one-day prevalence survey of more than 11,000 patients in 183 U.S. hospitals in 2011, the study notes that half of inpatients prescribed antibiotics received two or more of them. The CDC estimates that 20% to 50% of all antibiotics prescribed in U.S. hospitals are either unnecessary or inappropriate, and many of them count adverse drug reactions among their side effects .
While a growing body of evidence suggests that hospital-based antibiotic stewardship programs can optimize treatment, reduce antibacterial side effects, and save money, a study published September 2014 in JAMA says those benefits may be lost post-discharge. Results of a randomized trial of an outpatient antimicrobial stewardship intervention found that an initial 50% reduction in antibiotic prescriptions was lost when their targeted interventions ceased.
“These data suggest that audit and feedback was a vital element of this intervention and that antimicrobial stewardship requires continued, active efforts to sustain initial improvements,” says lead author Jeffrey S. Gerber, MD, PhD, CHCP, attending physician in infectious diseases at the Children’s Hospital of Philadelphia.
The federal government has taken a three-pronged approach to the problem: a report from the President’s Council of Advisors on Science and Technology with recommendations for monitoring superbugs and slowing their spread; an executive order issued by President Obama on September 18, 2014 with a commitment to “accelerate scientific research and facilitate the development of new antibacterial drugs;” and the creation of a national task force charged with designing a national strategy to combat antibiotic overuse by February 2015.
The President’s Council report notes that bacteria are becoming resistant to antibiotics in large part because these drugs are overprescribed to patients and overused in animals raised for food. The report recommends the CDC develop rules by 2017 requiring hospitals and nursing homes to implement best practices for antibiotic use.
Antibiotic overprescription remains a problem in the U.S. and abroad and shows no signs of slowing. A study published in the October 2014 issue of JAMA reports that nearly half of all hospitalized patients receive antibiotics, and the drugs most commonly prescribed are broad-spectrum antibiotics, which have been linked with promoting the spread of antibiotic-resistant bacteria. Based on a one-day prevalence survey of more than 11,000 patients in 183 U.S. hospitals in 2011, the study notes that half of inpatients prescribed antibiotics received two or more of them. The CDC estimates that 20% to 50% of all antibiotics prescribed in U.S. hospitals are either unnecessary or inappropriate, and many of them count adverse drug reactions among their side effects .
While a growing body of evidence suggests that hospital-based antibiotic stewardship programs can optimize treatment, reduce antibacterial side effects, and save money, a study published September 2014 in JAMA says those benefits may be lost post-discharge. Results of a randomized trial of an outpatient antimicrobial stewardship intervention found that an initial 50% reduction in antibiotic prescriptions was lost when their targeted interventions ceased.
“These data suggest that audit and feedback was a vital element of this intervention and that antimicrobial stewardship requires continued, active efforts to sustain initial improvements,” says lead author Jeffrey S. Gerber, MD, PhD, CHCP, attending physician in infectious diseases at the Children’s Hospital of Philadelphia.
The federal government has taken a three-pronged approach to the problem: a report from the President’s Council of Advisors on Science and Technology with recommendations for monitoring superbugs and slowing their spread; an executive order issued by President Obama on September 18, 2014 with a commitment to “accelerate scientific research and facilitate the development of new antibacterial drugs;” and the creation of a national task force charged with designing a national strategy to combat antibiotic overuse by February 2015.
The President’s Council report notes that bacteria are becoming resistant to antibiotics in large part because these drugs are overprescribed to patients and overused in animals raised for food. The report recommends the CDC develop rules by 2017 requiring hospitals and nursing homes to implement best practices for antibiotic use.
When Should You Decolonize Methicillin-Resistant Staphylococcus aureus (MRSA) in Hospitalized Patients?
Case
A 45-year-old previously healthy female was admitted to the ICU with sepsis caused by community-acquired pneumonia. Per hospital policy, all patients admitted to the ICU are screened for MRSA colonization. If the nasal screen is positive, contact isolation is initiated and the hospital’s MRSA decolonization protocol is implemented. Her nasal screen was positive for MRSA.
Overview
MRSA infections are associated with significant morbidity and mortality, and death occurs in almost 5% of patients who develop a MRSA infection. In 2005, invasive MRSA was responsible for approximately 278,000 hospitalizations and 19,000 deaths. MRSA is a common cause of healthcare-associated infections (HAIs) and is the most common pathogen in surgical site infections (SSIs) and ventilator-associated pneumonias. The cost of treating MRSA infections is substantial; in 2003, $14.5 billion was spent on MRSA-related hospitalizations.
It is well known that MRSA colonization is a risk factor for the subsequent development of a MRSA infection. This risk persists over time, and approximately 25% of individuals who are colonized with MRSA for more than one year will develop a late-onset MRSA infection.1 It is estimated that between 0.8% and 6% of people in the U.S. are asymptomatically colonized with MRSA.
One infection control strategy for reducing the transmission of MRSA among hospitalized patients involves screening for the presence of this organism and then placing colonized and/or infected patients in isolation; however, there is considerable controversy about which patients should be screened.
An additional element of many infection control strategies involves MRSA decolonization, but there is uncertainty about which patients benefit from it and significant variability in its reported success rates.2 Additionally, several studies have indicated that MRSA decolonization is only temporary and that patients become recolonized over time.
Treatment
It is estimated that 10% to 20% of MRSA carriers will develop an infection while they are hospitalized. Furthermore, even after they have been discharged from the hospital, their risk for developing a MRSA infection persists.
Most patients who develop a MRSA infection have been colonized prior to infection, and these patients usually develop an infection caused by the same strain as the colonization. In view of this fact, a primary goal of decolonization is reducing the likelihood of “auto-infection.” Another goal of decolonization is reducing the transmission of MRSA to other patients.
In order to determine whether MRSA colonization is present, patients undergo screening, and specimens are collected from the nares using nasal swabs. Specimens from extranasal sites, such as the groin, are sometimes also obtained for screening. These screening tests are usually done with either cultures or polymerase chain reaction testing.
There is significant variability in the details of screening and decolonization protocols among different healthcare facilities. Typically, the screening test costs more than the agents used for decolonization. Partly for this reason, some facilities forego screening altogether, instead treating all patients with a decolonization regimen; however, there is concern that administering decolonizing medications to all patients would lead to the unnecessary treatment of large numbers of patients. Such widespread use of the decolonizing agents might promote the development of resistance to these medications.
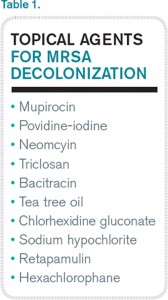
Medications. Decolonization typically involves the use of a topical antibiotic, most commonly mupirocin, which is applied to the nares. This may be used in conjunction with an oral antimicrobial agent. While the nares are the anatomical locations most commonly colonized by MRSA, extranasal colonization occurs in 50% of those who are nasally colonized.
Of the topical medications available for decolonization, mupirocin has the highest efficacy, with eradication of MRSA and methicillin-sensitive Staphylococcus aureus (MSSA) colonization ranging from 81% to 93%. To increase the likelihood of successful decolonization, an antiseptic agent, such as chlorhexidine gluconate, may also be applied to the skin. Chlorhexidine gluconate is also commonly used to prevent other HAIs.
Neomycin is sometimes used for decolonization, but its efficacy for this purpose is questionable. There are also concerns about resistance, but it may be an option in cases of documented mupirocin resistance. Preparations that contain tea tree oil appear to be more effective for decolonization of skin sites than for nasal decolonization. Table 1 lists the topical antibiotics and antiseptics that may be utilized for decolonization, while Table 2 lists the oral medications that can be used for this purpose. Table 3 lists investigational agents being evaluated for their ability to decolonize patients.
It has been suggested that the patients who might derive the most benefit from decolonization are those at increased risk for developing a MRSA infection during a specific time interval. This would include patients who are admitted to the ICU for an acute illness and cardiothoracic surgery patients. A benefit from decolonization has also been observed in hemodialysis patients, who have an incidence of invasive MRSA infections 100 times greater than the general population. Otherwise, there are no data to support the routine use of decolonization in nonsurgical patients.
It is not uncommon for hospitals to screen patients admitted to the ICU for MRSA nasal colonization; in fact, screening is mandatory in nine states. If the nasal screen is positive, contact precautions are instituted. The decision about whether or not to initiate a decolonization protocol varies among different ICUs, but most do not carry out universal decolonization.
Some studies show decolonization is beneficial for ICU patients. These studies include a large cluster-randomized trial called REDUCE MRSA,3 which took place in 43 hospitals and involved 74,256 patients in 74 ICUs. The study showed that universal (i.e., without screening) decolonization using mupirocin and chlorhexidine was effective in reducing rates of MRSA clinical isolates, as well as bloodstream infection from any pathogen. Other studies have demonstrated benefits from the decolonization of ICU patients.4,5
Surgical Site Infections. Meanwhile, SSIs are often associated with increased mortality rates and substantial healthcare costs, including increased hospital lengths of stay and readmission rates. Staphylococcus aureus is the pathogen most commonly isolated from SSIs. In surgical patients, colonization with MRSA is associated with an elevated rate of MRSA SSIs. The goal of decolonization in surgical patients is not to permanently eliminate MRSA but to prevent SSIs by suppressing the presence of this organism for a relatively brief duration.
There is evidence that decolonization reduces SSIs for cardiothoracic surgeries.6 For these patients, it is cost effective to screen for nasal carriage of MRSA and then treat carriers with a combination of pre-operative mupirocin and chlorhexidine. It may be reasonable to delay cardiothoracic surgery in colonized patients who will require implantation of prosthetic material until they complete MRSA decolonization.
In addition to reducing the risk of auto-infection, another goal of decolonization is limiting the possibility of transmission of MRSA from a colonized patient to a susceptible individual; however, there are only limited data available that measure the efficacy of decolonization for preventing transmission.
Concerns about the potential hazards of decolonization therapy have impacted its widespread implementation. The biggest concern is that patients may develop resistance to the antimicrobial agents used for decolonization, particularly if they are used at increased frequency. Mupirocin resistance monitoring is valuable, but, unfortunately, the susceptibility of Staphylococcus aureus to mupirocin is not routinely evaluated, so the prevalence of mupirocin resistance in local strains is often unknown. Another concern about decolonization is the cost of screening and decolonizing patients.
Back to the Case
The patient in this case required admission to an ICU and, based on the results of the REDUCE MRSA clinical trial, she would likely benefit from undergoing decolonization to reduce her risk of both MRSA-positive clinical cultures and bloodstream infections caused by any pathogen.
Bottom Line
Decolonization is beneficial for patients at increased risk of developing a MRSA infection during a specific period, such as patients admitted to the ICU and those undergoing cardiothoracic surgery.
Dr. Clarke is assistant professor in the division of hospital medicine at Emory University Hospital and a faculty member in the Emory University Department of Medicine, both in Atlanta.
References
- Dow G, Field D, Mancuso M, Allard J. Decolonization of methicillin-resistant Staphylococcus aureus during routine hospital care: Efficacy and long-term follow-up. Can J Infect Dis Med Microbiol. 2010;21(1):38-44.
- Simor AE. Staphylococcal decolonisation: An effective strategy for prevention of infection? Lancet Infect Dis. 2011;11(12):952-962.
- Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;368(24):2255-2265.
- Fraser T, Fatica C, Scarpelli M, et al. Decrease in Staphylococcus aureus colonization and hospital-acquired infection in a medical intensive care unit after institution of an active surveillance and decolonization program. Infect Control Hosp Epidemiol. 2010;31(8):779-783.
- Robotham J, Graves N, Cookson B, et al. Screening, isolation, and decolonisation strategies in the control of methicillin-resistant Staphylococcus aureus in intensive care units: Cost effectiveness evaluation. BMJ. 2011;343:d5694.
- Schweizer M, Perencevich E, McDanel J, et al. Effectiveness of a bundled intervention of decolonization and prophylaxis to decrease Gram positive surgical site infections after cardiac or orthopedic surgery: Systematic review and meta-analysis. BMJ. 2013;346:f2743.
Case
A 45-year-old previously healthy female was admitted to the ICU with sepsis caused by community-acquired pneumonia. Per hospital policy, all patients admitted to the ICU are screened for MRSA colonization. If the nasal screen is positive, contact isolation is initiated and the hospital’s MRSA decolonization protocol is implemented. Her nasal screen was positive for MRSA.
Overview
MRSA infections are associated with significant morbidity and mortality, and death occurs in almost 5% of patients who develop a MRSA infection. In 2005, invasive MRSA was responsible for approximately 278,000 hospitalizations and 19,000 deaths. MRSA is a common cause of healthcare-associated infections (HAIs) and is the most common pathogen in surgical site infections (SSIs) and ventilator-associated pneumonias. The cost of treating MRSA infections is substantial; in 2003, $14.5 billion was spent on MRSA-related hospitalizations.
It is well known that MRSA colonization is a risk factor for the subsequent development of a MRSA infection. This risk persists over time, and approximately 25% of individuals who are colonized with MRSA for more than one year will develop a late-onset MRSA infection.1 It is estimated that between 0.8% and 6% of people in the U.S. are asymptomatically colonized with MRSA.
One infection control strategy for reducing the transmission of MRSA among hospitalized patients involves screening for the presence of this organism and then placing colonized and/or infected patients in isolation; however, there is considerable controversy about which patients should be screened.
An additional element of many infection control strategies involves MRSA decolonization, but there is uncertainty about which patients benefit from it and significant variability in its reported success rates.2 Additionally, several studies have indicated that MRSA decolonization is only temporary and that patients become recolonized over time.
Treatment
It is estimated that 10% to 20% of MRSA carriers will develop an infection while they are hospitalized. Furthermore, even after they have been discharged from the hospital, their risk for developing a MRSA infection persists.
Most patients who develop a MRSA infection have been colonized prior to infection, and these patients usually develop an infection caused by the same strain as the colonization. In view of this fact, a primary goal of decolonization is reducing the likelihood of “auto-infection.” Another goal of decolonization is reducing the transmission of MRSA to other patients.
In order to determine whether MRSA colonization is present, patients undergo screening, and specimens are collected from the nares using nasal swabs. Specimens from extranasal sites, such as the groin, are sometimes also obtained for screening. These screening tests are usually done with either cultures or polymerase chain reaction testing.
There is significant variability in the details of screening and decolonization protocols among different healthcare facilities. Typically, the screening test costs more than the agents used for decolonization. Partly for this reason, some facilities forego screening altogether, instead treating all patients with a decolonization regimen; however, there is concern that administering decolonizing medications to all patients would lead to the unnecessary treatment of large numbers of patients. Such widespread use of the decolonizing agents might promote the development of resistance to these medications.
Medications. Decolonization typically involves the use of a topical antibiotic, most commonly mupirocin, which is applied to the nares. This may be used in conjunction with an oral antimicrobial agent. While the nares are the anatomical locations most commonly colonized by MRSA, extranasal colonization occurs in 50% of those who are nasally colonized.
Of the topical medications available for decolonization, mupirocin has the highest efficacy, with eradication of MRSA and methicillin-sensitive Staphylococcus aureus (MSSA) colonization ranging from 81% to 93%. To increase the likelihood of successful decolonization, an antiseptic agent, such as chlorhexidine gluconate, may also be applied to the skin. Chlorhexidine gluconate is also commonly used to prevent other HAIs.
Neomycin is sometimes used for decolonization, but its efficacy for this purpose is questionable. There are also concerns about resistance, but it may be an option in cases of documented mupirocin resistance. Preparations that contain tea tree oil appear to be more effective for decolonization of skin sites than for nasal decolonization. Table 1 lists the topical antibiotics and antiseptics that may be utilized for decolonization, while Table 2 lists the oral medications that can be used for this purpose. Table 3 lists investigational agents being evaluated for their ability to decolonize patients.
It has been suggested that the patients who might derive the most benefit from decolonization are those at increased risk for developing a MRSA infection during a specific time interval. This would include patients who are admitted to the ICU for an acute illness and cardiothoracic surgery patients. A benefit from decolonization has also been observed in hemodialysis patients, who have an incidence of invasive MRSA infections 100 times greater than the general population. Otherwise, there are no data to support the routine use of decolonization in nonsurgical patients.
It is not uncommon for hospitals to screen patients admitted to the ICU for MRSA nasal colonization; in fact, screening is mandatory in nine states. If the nasal screen is positive, contact precautions are instituted. The decision about whether or not to initiate a decolonization protocol varies among different ICUs, but most do not carry out universal decolonization.
Some studies show decolonization is beneficial for ICU patients. These studies include a large cluster-randomized trial called REDUCE MRSA,3 which took place in 43 hospitals and involved 74,256 patients in 74 ICUs. The study showed that universal (i.e., without screening) decolonization using mupirocin and chlorhexidine was effective in reducing rates of MRSA clinical isolates, as well as bloodstream infection from any pathogen. Other studies have demonstrated benefits from the decolonization of ICU patients.4,5
Surgical Site Infections. Meanwhile, SSIs are often associated with increased mortality rates and substantial healthcare costs, including increased hospital lengths of stay and readmission rates. Staphylococcus aureus is the pathogen most commonly isolated from SSIs. In surgical patients, colonization with MRSA is associated with an elevated rate of MRSA SSIs. The goal of decolonization in surgical patients is not to permanently eliminate MRSA but to prevent SSIs by suppressing the presence of this organism for a relatively brief duration.
There is evidence that decolonization reduces SSIs for cardiothoracic surgeries.6 For these patients, it is cost effective to screen for nasal carriage of MRSA and then treat carriers with a combination of pre-operative mupirocin and chlorhexidine. It may be reasonable to delay cardiothoracic surgery in colonized patients who will require implantation of prosthetic material until they complete MRSA decolonization.
In addition to reducing the risk of auto-infection, another goal of decolonization is limiting the possibility of transmission of MRSA from a colonized patient to a susceptible individual; however, there are only limited data available that measure the efficacy of decolonization for preventing transmission.
Concerns about the potential hazards of decolonization therapy have impacted its widespread implementation. The biggest concern is that patients may develop resistance to the antimicrobial agents used for decolonization, particularly if they are used at increased frequency. Mupirocin resistance monitoring is valuable, but, unfortunately, the susceptibility of Staphylococcus aureus to mupirocin is not routinely evaluated, so the prevalence of mupirocin resistance in local strains is often unknown. Another concern about decolonization is the cost of screening and decolonizing patients.
Back to the Case
The patient in this case required admission to an ICU and, based on the results of the REDUCE MRSA clinical trial, she would likely benefit from undergoing decolonization to reduce her risk of both MRSA-positive clinical cultures and bloodstream infections caused by any pathogen.
Bottom Line
Decolonization is beneficial for patients at increased risk of developing a MRSA infection during a specific period, such as patients admitted to the ICU and those undergoing cardiothoracic surgery.
Dr. Clarke is assistant professor in the division of hospital medicine at Emory University Hospital and a faculty member in the Emory University Department of Medicine, both in Atlanta.
References
- Dow G, Field D, Mancuso M, Allard J. Decolonization of methicillin-resistant Staphylococcus aureus during routine hospital care: Efficacy and long-term follow-up. Can J Infect Dis Med Microbiol. 2010;21(1):38-44.
- Simor AE. Staphylococcal decolonisation: An effective strategy for prevention of infection? Lancet Infect Dis. 2011;11(12):952-962.
- Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;368(24):2255-2265.
- Fraser T, Fatica C, Scarpelli M, et al. Decrease in Staphylococcus aureus colonization and hospital-acquired infection in a medical intensive care unit after institution of an active surveillance and decolonization program. Infect Control Hosp Epidemiol. 2010;31(8):779-783.
- Robotham J, Graves N, Cookson B, et al. Screening, isolation, and decolonisation strategies in the control of methicillin-resistant Staphylococcus aureus in intensive care units: Cost effectiveness evaluation. BMJ. 2011;343:d5694.
- Schweizer M, Perencevich E, McDanel J, et al. Effectiveness of a bundled intervention of decolonization and prophylaxis to decrease Gram positive surgical site infections after cardiac or orthopedic surgery: Systematic review and meta-analysis. BMJ. 2013;346:f2743.
Case
A 45-year-old previously healthy female was admitted to the ICU with sepsis caused by community-acquired pneumonia. Per hospital policy, all patients admitted to the ICU are screened for MRSA colonization. If the nasal screen is positive, contact isolation is initiated and the hospital’s MRSA decolonization protocol is implemented. Her nasal screen was positive for MRSA.
Overview
MRSA infections are associated with significant morbidity and mortality, and death occurs in almost 5% of patients who develop a MRSA infection. In 2005, invasive MRSA was responsible for approximately 278,000 hospitalizations and 19,000 deaths. MRSA is a common cause of healthcare-associated infections (HAIs) and is the most common pathogen in surgical site infections (SSIs) and ventilator-associated pneumonias. The cost of treating MRSA infections is substantial; in 2003, $14.5 billion was spent on MRSA-related hospitalizations.
It is well known that MRSA colonization is a risk factor for the subsequent development of a MRSA infection. This risk persists over time, and approximately 25% of individuals who are colonized with MRSA for more than one year will develop a late-onset MRSA infection.1 It is estimated that between 0.8% and 6% of people in the U.S. are asymptomatically colonized with MRSA.
One infection control strategy for reducing the transmission of MRSA among hospitalized patients involves screening for the presence of this organism and then placing colonized and/or infected patients in isolation; however, there is considerable controversy about which patients should be screened.
An additional element of many infection control strategies involves MRSA decolonization, but there is uncertainty about which patients benefit from it and significant variability in its reported success rates.2 Additionally, several studies have indicated that MRSA decolonization is only temporary and that patients become recolonized over time.
Treatment
It is estimated that 10% to 20% of MRSA carriers will develop an infection while they are hospitalized. Furthermore, even after they have been discharged from the hospital, their risk for developing a MRSA infection persists.
Most patients who develop a MRSA infection have been colonized prior to infection, and these patients usually develop an infection caused by the same strain as the colonization. In view of this fact, a primary goal of decolonization is reducing the likelihood of “auto-infection.” Another goal of decolonization is reducing the transmission of MRSA to other patients.
In order to determine whether MRSA colonization is present, patients undergo screening, and specimens are collected from the nares using nasal swabs. Specimens from extranasal sites, such as the groin, are sometimes also obtained for screening. These screening tests are usually done with either cultures or polymerase chain reaction testing.
There is significant variability in the details of screening and decolonization protocols among different healthcare facilities. Typically, the screening test costs more than the agents used for decolonization. Partly for this reason, some facilities forego screening altogether, instead treating all patients with a decolonization regimen; however, there is concern that administering decolonizing medications to all patients would lead to the unnecessary treatment of large numbers of patients. Such widespread use of the decolonizing agents might promote the development of resistance to these medications.
Medications. Decolonization typically involves the use of a topical antibiotic, most commonly mupirocin, which is applied to the nares. This may be used in conjunction with an oral antimicrobial agent. While the nares are the anatomical locations most commonly colonized by MRSA, extranasal colonization occurs in 50% of those who are nasally colonized.
Of the topical medications available for decolonization, mupirocin has the highest efficacy, with eradication of MRSA and methicillin-sensitive Staphylococcus aureus (MSSA) colonization ranging from 81% to 93%. To increase the likelihood of successful decolonization, an antiseptic agent, such as chlorhexidine gluconate, may also be applied to the skin. Chlorhexidine gluconate is also commonly used to prevent other HAIs.
Neomycin is sometimes used for decolonization, but its efficacy for this purpose is questionable. There are also concerns about resistance, but it may be an option in cases of documented mupirocin resistance. Preparations that contain tea tree oil appear to be more effective for decolonization of skin sites than for nasal decolonization. Table 1 lists the topical antibiotics and antiseptics that may be utilized for decolonization, while Table 2 lists the oral medications that can be used for this purpose. Table 3 lists investigational agents being evaluated for their ability to decolonize patients.
It has been suggested that the patients who might derive the most benefit from decolonization are those at increased risk for developing a MRSA infection during a specific time interval. This would include patients who are admitted to the ICU for an acute illness and cardiothoracic surgery patients. A benefit from decolonization has also been observed in hemodialysis patients, who have an incidence of invasive MRSA infections 100 times greater than the general population. Otherwise, there are no data to support the routine use of decolonization in nonsurgical patients.
It is not uncommon for hospitals to screen patients admitted to the ICU for MRSA nasal colonization; in fact, screening is mandatory in nine states. If the nasal screen is positive, contact precautions are instituted. The decision about whether or not to initiate a decolonization protocol varies among different ICUs, but most do not carry out universal decolonization.
Some studies show decolonization is beneficial for ICU patients. These studies include a large cluster-randomized trial called REDUCE MRSA,3 which took place in 43 hospitals and involved 74,256 patients in 74 ICUs. The study showed that universal (i.e., without screening) decolonization using mupirocin and chlorhexidine was effective in reducing rates of MRSA clinical isolates, as well as bloodstream infection from any pathogen. Other studies have demonstrated benefits from the decolonization of ICU patients.4,5
Surgical Site Infections. Meanwhile, SSIs are often associated with increased mortality rates and substantial healthcare costs, including increased hospital lengths of stay and readmission rates. Staphylococcus aureus is the pathogen most commonly isolated from SSIs. In surgical patients, colonization with MRSA is associated with an elevated rate of MRSA SSIs. The goal of decolonization in surgical patients is not to permanently eliminate MRSA but to prevent SSIs by suppressing the presence of this organism for a relatively brief duration.
There is evidence that decolonization reduces SSIs for cardiothoracic surgeries.6 For these patients, it is cost effective to screen for nasal carriage of MRSA and then treat carriers with a combination of pre-operative mupirocin and chlorhexidine. It may be reasonable to delay cardiothoracic surgery in colonized patients who will require implantation of prosthetic material until they complete MRSA decolonization.
In addition to reducing the risk of auto-infection, another goal of decolonization is limiting the possibility of transmission of MRSA from a colonized patient to a susceptible individual; however, there are only limited data available that measure the efficacy of decolonization for preventing transmission.
Concerns about the potential hazards of decolonization therapy have impacted its widespread implementation. The biggest concern is that patients may develop resistance to the antimicrobial agents used for decolonization, particularly if they are used at increased frequency. Mupirocin resistance monitoring is valuable, but, unfortunately, the susceptibility of Staphylococcus aureus to mupirocin is not routinely evaluated, so the prevalence of mupirocin resistance in local strains is often unknown. Another concern about decolonization is the cost of screening and decolonizing patients.
Back to the Case
The patient in this case required admission to an ICU and, based on the results of the REDUCE MRSA clinical trial, she would likely benefit from undergoing decolonization to reduce her risk of both MRSA-positive clinical cultures and bloodstream infections caused by any pathogen.
Bottom Line
Decolonization is beneficial for patients at increased risk of developing a MRSA infection during a specific period, such as patients admitted to the ICU and those undergoing cardiothoracic surgery.
Dr. Clarke is assistant professor in the division of hospital medicine at Emory University Hospital and a faculty member in the Emory University Department of Medicine, both in Atlanta.
References
- Dow G, Field D, Mancuso M, Allard J. Decolonization of methicillin-resistant Staphylococcus aureus during routine hospital care: Efficacy and long-term follow-up. Can J Infect Dis Med Microbiol. 2010;21(1):38-44.
- Simor AE. Staphylococcal decolonisation: An effective strategy for prevention of infection? Lancet Infect Dis. 2011;11(12):952-962.
- Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;368(24):2255-2265.
- Fraser T, Fatica C, Scarpelli M, et al. Decrease in Staphylococcus aureus colonization and hospital-acquired infection in a medical intensive care unit after institution of an active surveillance and decolonization program. Infect Control Hosp Epidemiol. 2010;31(8):779-783.
- Robotham J, Graves N, Cookson B, et al. Screening, isolation, and decolonisation strategies in the control of methicillin-resistant Staphylococcus aureus in intensive care units: Cost effectiveness evaluation. BMJ. 2011;343:d5694.
- Schweizer M, Perencevich E, McDanel J, et al. Effectiveness of a bundled intervention of decolonization and prophylaxis to decrease Gram positive surgical site infections after cardiac or orthopedic surgery: Systematic review and meta-analysis. BMJ. 2013;346:f2743.
Antibiotic Prophylaxis Might Prevent Recurrent UTIs
Clinical question: Does antibiotic prophylaxis prevent future episodes of urinary tract infections?
Background: Recurrent urinary tract infections (UTI) in children might be associated with renal scarring and subsequent clinical consequences associated with long-term morbidity. Historically, antibiotic prophylaxis has been recommended for children who might have risk factors for recurrent infection, most commonly vesicoureteral reflux. However, scars may be present in the absence of known risk factors and upon first UTI. The efficacy of antibiotic prophylaxis in preventing recurrent UTIs is unclear.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: Four centers in Australia.
Synopsis: The study looked at 576 children under the age of 18 with a history of at least one symptomatic UTI. The patients were randomized to receive trimethoprim-sulfamethoxazole (TMP-SMX) or placebo for 12 months. Children with vesicoureteral reflux were included, but those with known neurologic, skeletal, or urologic predispositions were excluded.
Thirteen percent of patients in the antibiotic group developed a UTI compared with 19% of patients in the placebo group (P=0.02). The authors calculate that at 12 months, 14 patients would need to be treated to prevent one UTI.
This study was unable to enroll the planned number of children but remained adequately powered to show a reduction in the primary outcome (rate of symptomatic UTI). However, a significant number of patients (approximately 28%) in each arm stopped taking the medication, the majority for undisclosed reasons. Despite an intention-to-treat analysis, this degree of dropout raises questions about the true effect size. Additionally, this study does not answer the more important clinical question regarding the effect of prophylaxis on potential future renal damage, specifically in children with vesicoureteral reflux.
Bottom line: Antibiotic prophylaxis might be modestly effective in preventing recurrent UTIs.
Citation: Craig JC, Simpson JM, Williams GJ, et al. Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med. 2009;361(18):1748-1759.
Clinical question: Does antibiotic prophylaxis prevent future episodes of urinary tract infections?
Background: Recurrent urinary tract infections (UTI) in children might be associated with renal scarring and subsequent clinical consequences associated with long-term morbidity. Historically, antibiotic prophylaxis has been recommended for children who might have risk factors for recurrent infection, most commonly vesicoureteral reflux. However, scars may be present in the absence of known risk factors and upon first UTI. The efficacy of antibiotic prophylaxis in preventing recurrent UTIs is unclear.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: Four centers in Australia.
Synopsis: The study looked at 576 children under the age of 18 with a history of at least one symptomatic UTI. The patients were randomized to receive trimethoprim-sulfamethoxazole (TMP-SMX) or placebo for 12 months. Children with vesicoureteral reflux were included, but those with known neurologic, skeletal, or urologic predispositions were excluded.
Thirteen percent of patients in the antibiotic group developed a UTI compared with 19% of patients in the placebo group (P=0.02). The authors calculate that at 12 months, 14 patients would need to be treated to prevent one UTI.
This study was unable to enroll the planned number of children but remained adequately powered to show a reduction in the primary outcome (rate of symptomatic UTI). However, a significant number of patients (approximately 28%) in each arm stopped taking the medication, the majority for undisclosed reasons. Despite an intention-to-treat analysis, this degree of dropout raises questions about the true effect size. Additionally, this study does not answer the more important clinical question regarding the effect of prophylaxis on potential future renal damage, specifically in children with vesicoureteral reflux.
Bottom line: Antibiotic prophylaxis might be modestly effective in preventing recurrent UTIs.
Citation: Craig JC, Simpson JM, Williams GJ, et al. Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med. 2009;361(18):1748-1759.
Clinical question: Does antibiotic prophylaxis prevent future episodes of urinary tract infections?
Background: Recurrent urinary tract infections (UTI) in children might be associated with renal scarring and subsequent clinical consequences associated with long-term morbidity. Historically, antibiotic prophylaxis has been recommended for children who might have risk factors for recurrent infection, most commonly vesicoureteral reflux. However, scars may be present in the absence of known risk factors and upon first UTI. The efficacy of antibiotic prophylaxis in preventing recurrent UTIs is unclear.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: Four centers in Australia.
Synopsis: The study looked at 576 children under the age of 18 with a history of at least one symptomatic UTI. The patients were randomized to receive trimethoprim-sulfamethoxazole (TMP-SMX) or placebo for 12 months. Children with vesicoureteral reflux were included, but those with known neurologic, skeletal, or urologic predispositions were excluded.
Thirteen percent of patients in the antibiotic group developed a UTI compared with 19% of patients in the placebo group (P=0.02). The authors calculate that at 12 months, 14 patients would need to be treated to prevent one UTI.
This study was unable to enroll the planned number of children but remained adequately powered to show a reduction in the primary outcome (rate of symptomatic UTI). However, a significant number of patients (approximately 28%) in each arm stopped taking the medication, the majority for undisclosed reasons. Despite an intention-to-treat analysis, this degree of dropout raises questions about the true effect size. Additionally, this study does not answer the more important clinical question regarding the effect of prophylaxis on potential future renal damage, specifically in children with vesicoureteral reflux.
Bottom line: Antibiotic prophylaxis might be modestly effective in preventing recurrent UTIs.
Citation: Craig JC, Simpson JM, Williams GJ, et al. Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med. 2009;361(18):1748-1759.
Antibiotic Resistance Threats in the United States, 2013
Clinical question: What antibiotic-resistant bacteria are the greatest threats for the next 10 years?
Background: Two million people suffer antibiotic-resistant infections yearly, and 23,000 die each year as a result. Most of these infections occur in the community, but deaths usually occur in healthcare settings. Cost estimates vary but may be as high as $20 billion in excess direct healthcare costs.
Study design: The CDC used several different surveys and databanks, including the National Antimicrobial Resistance Monitoring System, to collect data. The threat level for antibiotic-resistant bacteria was determined using several factors: clinical impact, economic impact, incidence, 10-year projection of incidence, transmissibility, availability of effective antibiotics, and barriers to prevention.
Setting: United States.
Synopsis: The CDC has three classifications of antibiotic-resistant bacteria: urgent, serious, and concerning. Urgent threats are high-consequence, antibiotic-resistant threats because of significant risks identified across several criteria. These threats might not currently be widespread but have the potential to become so and require urgent public health attention to identify infections and to limit transmission. They include carbapenem-resistant Enterobacteriaceae, drug-resistant Neisseria gonorrhoeae, and Clostridium difficile (does not have true resistance, but is a consequence of antibiotic overuse).
Serious threats are significant antibiotic-resistant threats. These threats will worsen and might become urgent without ongoing public health monitoring and prevention activities. They include multidrug-resistant Acinetobacter, drug-resistant Campylobacter, fluconazole-resistant Candida (a fungus), extended-spectrum β-lactamase-producing Enterobacteriaceae, vancomycin-resistant Enterococcus, multidrug-resistant Pseudomonas aeruginosa, drug-resistant non-typhoidal Salmonella, drug-resistant Salmonella Typhimurium, drug-resistant Shigella, methicillin-resistant Staphylococcus aureus, drug-resistant Streptococcus pneumonia, and drug-resistant tuberculosis.
Concerning threats are bacteria for which the threat of antibiotic resistance is low, and/ or there are multiple therapeutic options for resistant infections. These bacterial pathogens cause severe illness. Threats in this category require monitoring and, in some cases, rapid incident or outbreak response. These include vancomycin-resistant Staphylococcus aureus, erythromycin-resistant Group A Streptococcus, and clindamycin-resistant Group B Streptococcus. Research has shown patients with resistant infections have significantly longer hospital stays, delayed recuperation, long-term disability, and higher mortality. As resistance to current antibiotics occurs, providers are forced to use antibiotics that are more toxic, more expensive, and less effective.
The CDC recommends four core actions to fight antibiotic resistance:
- Preventing infections from occurring and preventing resistant bacteria from spreading (immunization, infection control, screening, treatment, and education);
- Tracking resistant bacteria;
- Improving the use of antibiotics (antibiotic stewardship); and
- Promoting the development of new antibiotics and new diagnostic tests for resistant bacteria.
Bottom line: Antibiotics are a limited resource. The more antibiotics are used today, the less likely they will continue to be effective in the future. The CDC lists 18 antibiotic-resistant organisms as urgent, serious, or concerning and recommends actions to combat the spread of current organisms and emergence of new antibiotic organisms.
Citation: Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. CDC website. September 16, 2013. Available at: www.cdc.gov/drugresistance/threat-report-2013. Accessed Nov. 30, 2013.
Clinical question: What antibiotic-resistant bacteria are the greatest threats for the next 10 years?
Background: Two million people suffer antibiotic-resistant infections yearly, and 23,000 die each year as a result. Most of these infections occur in the community, but deaths usually occur in healthcare settings. Cost estimates vary but may be as high as $20 billion in excess direct healthcare costs.
Study design: The CDC used several different surveys and databanks, including the National Antimicrobial Resistance Monitoring System, to collect data. The threat level for antibiotic-resistant bacteria was determined using several factors: clinical impact, economic impact, incidence, 10-year projection of incidence, transmissibility, availability of effective antibiotics, and barriers to prevention.
Setting: United States.
Synopsis: The CDC has three classifications of antibiotic-resistant bacteria: urgent, serious, and concerning. Urgent threats are high-consequence, antibiotic-resistant threats because of significant risks identified across several criteria. These threats might not currently be widespread but have the potential to become so and require urgent public health attention to identify infections and to limit transmission. They include carbapenem-resistant Enterobacteriaceae, drug-resistant Neisseria gonorrhoeae, and Clostridium difficile (does not have true resistance, but is a consequence of antibiotic overuse).
Serious threats are significant antibiotic-resistant threats. These threats will worsen and might become urgent without ongoing public health monitoring and prevention activities. They include multidrug-resistant Acinetobacter, drug-resistant Campylobacter, fluconazole-resistant Candida (a fungus), extended-spectrum β-lactamase-producing Enterobacteriaceae, vancomycin-resistant Enterococcus, multidrug-resistant Pseudomonas aeruginosa, drug-resistant non-typhoidal Salmonella, drug-resistant Salmonella Typhimurium, drug-resistant Shigella, methicillin-resistant Staphylococcus aureus, drug-resistant Streptococcus pneumonia, and drug-resistant tuberculosis.
Concerning threats are bacteria for which the threat of antibiotic resistance is low, and/ or there are multiple therapeutic options for resistant infections. These bacterial pathogens cause severe illness. Threats in this category require monitoring and, in some cases, rapid incident or outbreak response. These include vancomycin-resistant Staphylococcus aureus, erythromycin-resistant Group A Streptococcus, and clindamycin-resistant Group B Streptococcus. Research has shown patients with resistant infections have significantly longer hospital stays, delayed recuperation, long-term disability, and higher mortality. As resistance to current antibiotics occurs, providers are forced to use antibiotics that are more toxic, more expensive, and less effective.
The CDC recommends four core actions to fight antibiotic resistance:
- Preventing infections from occurring and preventing resistant bacteria from spreading (immunization, infection control, screening, treatment, and education);
- Tracking resistant bacteria;
- Improving the use of antibiotics (antibiotic stewardship); and
- Promoting the development of new antibiotics and new diagnostic tests for resistant bacteria.
Bottom line: Antibiotics are a limited resource. The more antibiotics are used today, the less likely they will continue to be effective in the future. The CDC lists 18 antibiotic-resistant organisms as urgent, serious, or concerning and recommends actions to combat the spread of current organisms and emergence of new antibiotic organisms.
Citation: Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. CDC website. September 16, 2013. Available at: www.cdc.gov/drugresistance/threat-report-2013. Accessed Nov. 30, 2013.
Clinical question: What antibiotic-resistant bacteria are the greatest threats for the next 10 years?
Background: Two million people suffer antibiotic-resistant infections yearly, and 23,000 die each year as a result. Most of these infections occur in the community, but deaths usually occur in healthcare settings. Cost estimates vary but may be as high as $20 billion in excess direct healthcare costs.
Study design: The CDC used several different surveys and databanks, including the National Antimicrobial Resistance Monitoring System, to collect data. The threat level for antibiotic-resistant bacteria was determined using several factors: clinical impact, economic impact, incidence, 10-year projection of incidence, transmissibility, availability of effective antibiotics, and barriers to prevention.
Setting: United States.
Synopsis: The CDC has three classifications of antibiotic-resistant bacteria: urgent, serious, and concerning. Urgent threats are high-consequence, antibiotic-resistant threats because of significant risks identified across several criteria. These threats might not currently be widespread but have the potential to become so and require urgent public health attention to identify infections and to limit transmission. They include carbapenem-resistant Enterobacteriaceae, drug-resistant Neisseria gonorrhoeae, and Clostridium difficile (does not have true resistance, but is a consequence of antibiotic overuse).
Serious threats are significant antibiotic-resistant threats. These threats will worsen and might become urgent without ongoing public health monitoring and prevention activities. They include multidrug-resistant Acinetobacter, drug-resistant Campylobacter, fluconazole-resistant Candida (a fungus), extended-spectrum β-lactamase-producing Enterobacteriaceae, vancomycin-resistant Enterococcus, multidrug-resistant Pseudomonas aeruginosa, drug-resistant non-typhoidal Salmonella, drug-resistant Salmonella Typhimurium, drug-resistant Shigella, methicillin-resistant Staphylococcus aureus, drug-resistant Streptococcus pneumonia, and drug-resistant tuberculosis.
Concerning threats are bacteria for which the threat of antibiotic resistance is low, and/ or there are multiple therapeutic options for resistant infections. These bacterial pathogens cause severe illness. Threats in this category require monitoring and, in some cases, rapid incident or outbreak response. These include vancomycin-resistant Staphylococcus aureus, erythromycin-resistant Group A Streptococcus, and clindamycin-resistant Group B Streptococcus. Research has shown patients with resistant infections have significantly longer hospital stays, delayed recuperation, long-term disability, and higher mortality. As resistance to current antibiotics occurs, providers are forced to use antibiotics that are more toxic, more expensive, and less effective.
The CDC recommends four core actions to fight antibiotic resistance:
- Preventing infections from occurring and preventing resistant bacteria from spreading (immunization, infection control, screening, treatment, and education);
- Tracking resistant bacteria;
- Improving the use of antibiotics (antibiotic stewardship); and
- Promoting the development of new antibiotics and new diagnostic tests for resistant bacteria.
Bottom line: Antibiotics are a limited resource. The more antibiotics are used today, the less likely they will continue to be effective in the future. The CDC lists 18 antibiotic-resistant organisms as urgent, serious, or concerning and recommends actions to combat the spread of current organisms and emergence of new antibiotic organisms.
Citation: Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. CDC website. September 16, 2013. Available at: www.cdc.gov/drugresistance/threat-report-2013. Accessed Nov. 30, 2013.
Once-Weekly Antibiotic Might Be Effective for Treatment of Acute Bacterial Skin Infections
Background: Acute bacterial skin infections are common and often require hospitalization for intravenous antibiotic administration. Treatment covering gram-positive bacteria usually is indicated. Dalbavancin is effective against gram-positives, including MRSA. Its long half-life makes it an attractive alternative to other commonly used antibiotics, which require more frequent dosing.
Study design: Phase 3, double-blinded RCT.
Setting: Multiple international centers.
Synopsis: Researchers randomized 1,312 patients with acute bacterial skin and skin-structure infections with signs of systemic infection requiring intravenous antibiotics to receive dalbavancin on days one and eight, with placebo on other days, or several doses of vancomycin with an option to switch to oral linezolid. The primary endpoint was cessation of spread of erythema and temperature of =37.6°C at 48–72 hours. Secondary endpoints included a decrease in lesion area of =20% at 48–72 hours and clinical success at end of therapy (determined by clinical and historical features). Results of the primary endpoint were similar with dalbavancin and vancomycin-linezolid groups (79.7% and 79.8%, respectively) and were within 10 percentage points of noninferiority. The secondary endpoints were similar between both groups. Limitations of the study were the early primary endpoint, lack of noninferiority analysis of the secondary endpoints, and cost-effective analysis.
Bottom line: Once-weekly dalbavancin appears to be similarly efficacious to intravenous vancomycin in the treatment of acute bacterial skin infections in terms of outcomes within 48–72 hours of therapy and might provide an alternative to continued inpatient hospitalization for intravenous antibiotics in stable patients.
Citation: Boucher HW, Wilcox M, Talbot GH, Puttagunta S, Das AF, Dunne MW. Once-weekly dalbavancin versus daily conventional therapy for skin infection. N Engl J Med. 2014;370(23):2169-2179.
Background: Acute bacterial skin infections are common and often require hospitalization for intravenous antibiotic administration. Treatment covering gram-positive bacteria usually is indicated. Dalbavancin is effective against gram-positives, including MRSA. Its long half-life makes it an attractive alternative to other commonly used antibiotics, which require more frequent dosing.
Study design: Phase 3, double-blinded RCT.
Setting: Multiple international centers.
Synopsis: Researchers randomized 1,312 patients with acute bacterial skin and skin-structure infections with signs of systemic infection requiring intravenous antibiotics to receive dalbavancin on days one and eight, with placebo on other days, or several doses of vancomycin with an option to switch to oral linezolid. The primary endpoint was cessation of spread of erythema and temperature of =37.6°C at 48–72 hours. Secondary endpoints included a decrease in lesion area of =20% at 48–72 hours and clinical success at end of therapy (determined by clinical and historical features). Results of the primary endpoint were similar with dalbavancin and vancomycin-linezolid groups (79.7% and 79.8%, respectively) and were within 10 percentage points of noninferiority. The secondary endpoints were similar between both groups. Limitations of the study were the early primary endpoint, lack of noninferiority analysis of the secondary endpoints, and cost-effective analysis.
Bottom line: Once-weekly dalbavancin appears to be similarly efficacious to intravenous vancomycin in the treatment of acute bacterial skin infections in terms of outcomes within 48–72 hours of therapy and might provide an alternative to continued inpatient hospitalization for intravenous antibiotics in stable patients.
Citation: Boucher HW, Wilcox M, Talbot GH, Puttagunta S, Das AF, Dunne MW. Once-weekly dalbavancin versus daily conventional therapy for skin infection. N Engl J Med. 2014;370(23):2169-2179.
Background: Acute bacterial skin infections are common and often require hospitalization for intravenous antibiotic administration. Treatment covering gram-positive bacteria usually is indicated. Dalbavancin is effective against gram-positives, including MRSA. Its long half-life makes it an attractive alternative to other commonly used antibiotics, which require more frequent dosing.
Study design: Phase 3, double-blinded RCT.
Setting: Multiple international centers.
Synopsis: Researchers randomized 1,312 patients with acute bacterial skin and skin-structure infections with signs of systemic infection requiring intravenous antibiotics to receive dalbavancin on days one and eight, with placebo on other days, or several doses of vancomycin with an option to switch to oral linezolid. The primary endpoint was cessation of spread of erythema and temperature of =37.6°C at 48–72 hours. Secondary endpoints included a decrease in lesion area of =20% at 48–72 hours and clinical success at end of therapy (determined by clinical and historical features). Results of the primary endpoint were similar with dalbavancin and vancomycin-linezolid groups (79.7% and 79.8%, respectively) and were within 10 percentage points of noninferiority. The secondary endpoints were similar between both groups. Limitations of the study were the early primary endpoint, lack of noninferiority analysis of the secondary endpoints, and cost-effective analysis.
Bottom line: Once-weekly dalbavancin appears to be similarly efficacious to intravenous vancomycin in the treatment of acute bacterial skin infections in terms of outcomes within 48–72 hours of therapy and might provide an alternative to continued inpatient hospitalization for intravenous antibiotics in stable patients.
Citation: Boucher HW, Wilcox M, Talbot GH, Puttagunta S, Das AF, Dunne MW. Once-weekly dalbavancin versus daily conventional therapy for skin infection. N Engl J Med. 2014;370(23):2169-2179.
De-Escalating Antibiotics in Sepsis
Clinical question: Does tailoring antibiotics based on known pathogens impact mortality for patients with severe sepsis or shock?
Background: In patients with sepsis, the use of early empiric antibiotics reduces morbidity and mortality. De-escalation therapy refers to narrowing the broad-spectrum antibiotics once the pathogen and sensitivities are known; however, no randomized controlled studies have assessed the impact of this therapy on critically ill patients.
Study design: Prospective observational study.
Setting: Academic hospital ICU in Spain.
Synopsis: From January 2008 to May 2012, 628 adult patients were treated empirically with broad-spectrum antibiotics. De-escalation was applied to 219 patients (34.9%). Outcomes measured were ICU mortality, hospital mortality, and 90-day mortality in patients who received de-escalation therapy, patients whose antibiotics were not changed, and patients for whom antibiotics were escalated.
The in-hospital mortality rate was 27.4% in patients who were de-escalated, 32.6% in the unchanged group, and 42.9% in the escalation group. ICU and 90-day mortality were lower in the de-escalation group. De-escalation was more commonly used in medical than in surgical patients.
This study is limited because it is not a randomized controlled study and was single-centered, so it might only be applicable on the larger scale. Also, multi-drug resistant organisms were not evaluated.
Overall, it is safe to narrow empiric antibiotics in severe sepsis and shock when the pathogen and sensitivities are known.
Bottom line: De-escalation of antibiotics in severe sepsis and septic shock is associated with a lower mortality.
Citation: Garnacho-Montero J, Gutierrez-Pizarraya A, Escoresca-Ortega A, et al. De-escalation of empirical therapy is associated with lower mortality in patients with severe sepsis and septic shock. Intensive Care Med. 2014;40(1):32-40.
Clinical question: Does tailoring antibiotics based on known pathogens impact mortality for patients with severe sepsis or shock?
Background: In patients with sepsis, the use of early empiric antibiotics reduces morbidity and mortality. De-escalation therapy refers to narrowing the broad-spectrum antibiotics once the pathogen and sensitivities are known; however, no randomized controlled studies have assessed the impact of this therapy on critically ill patients.
Study design: Prospective observational study.
Setting: Academic hospital ICU in Spain.
Synopsis: From January 2008 to May 2012, 628 adult patients were treated empirically with broad-spectrum antibiotics. De-escalation was applied to 219 patients (34.9%). Outcomes measured were ICU mortality, hospital mortality, and 90-day mortality in patients who received de-escalation therapy, patients whose antibiotics were not changed, and patients for whom antibiotics were escalated.
The in-hospital mortality rate was 27.4% in patients who were de-escalated, 32.6% in the unchanged group, and 42.9% in the escalation group. ICU and 90-day mortality were lower in the de-escalation group. De-escalation was more commonly used in medical than in surgical patients.
This study is limited because it is not a randomized controlled study and was single-centered, so it might only be applicable on the larger scale. Also, multi-drug resistant organisms were not evaluated.
Overall, it is safe to narrow empiric antibiotics in severe sepsis and shock when the pathogen and sensitivities are known.
Bottom line: De-escalation of antibiotics in severe sepsis and septic shock is associated with a lower mortality.
Citation: Garnacho-Montero J, Gutierrez-Pizarraya A, Escoresca-Ortega A, et al. De-escalation of empirical therapy is associated with lower mortality in patients with severe sepsis and septic shock. Intensive Care Med. 2014;40(1):32-40.
Clinical question: Does tailoring antibiotics based on known pathogens impact mortality for patients with severe sepsis or shock?
Background: In patients with sepsis, the use of early empiric antibiotics reduces morbidity and mortality. De-escalation therapy refers to narrowing the broad-spectrum antibiotics once the pathogen and sensitivities are known; however, no randomized controlled studies have assessed the impact of this therapy on critically ill patients.
Study design: Prospective observational study.
Setting: Academic hospital ICU in Spain.
Synopsis: From January 2008 to May 2012, 628 adult patients were treated empirically with broad-spectrum antibiotics. De-escalation was applied to 219 patients (34.9%). Outcomes measured were ICU mortality, hospital mortality, and 90-day mortality in patients who received de-escalation therapy, patients whose antibiotics were not changed, and patients for whom antibiotics were escalated.
The in-hospital mortality rate was 27.4% in patients who were de-escalated, 32.6% in the unchanged group, and 42.9% in the escalation group. ICU and 90-day mortality were lower in the de-escalation group. De-escalation was more commonly used in medical than in surgical patients.
This study is limited because it is not a randomized controlled study and was single-centered, so it might only be applicable on the larger scale. Also, multi-drug resistant organisms were not evaluated.
Overall, it is safe to narrow empiric antibiotics in severe sepsis and shock when the pathogen and sensitivities are known.
Bottom line: De-escalation of antibiotics in severe sepsis and septic shock is associated with a lower mortality.
Citation: Garnacho-Montero J, Gutierrez-Pizarraya A, Escoresca-Ortega A, et al. De-escalation of empirical therapy is associated with lower mortality in patients with severe sepsis and septic shock. Intensive Care Med. 2014;40(1):32-40.
Antibiotic Algorithm Can Guide Therapy in Healthcare-Associated Pneumonia
Clinical question: Can an algorithm based on risk for multidrug-resistant (MDR) organisms and illness severity guide antibiotic selection in healthcare-associated pneumonia (HCAP)?
Background: The 2005 American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) guidelines identify patients with HCAP as those with recent contact with a healthcare environment, including nursing homes and hemodialysis; however, previous studies have shown that not all patients with healthcare contact have equal risk for MDR organisms.
Study design: Prospective cohort study.
Setting: Japan, multi-center.
Synopsis: Of the 445 enrolled patients, 124 were diagnosed with community-acquired pneumonia (CAP) and 321 with HCAP. Patients with HCAP were classified based on severity of illness or MDR pathogen risk factors (immune suppression, hospitalization within the last 90 days, poor functional status, and antibiotics within the past six months). Patients with low risk (0-1 factors) for MDR organisms were treated for CAP, and patients with high risk (≥2 factors) or moderate risk (≥1 factor) for severe illness were treated for HCAP.
HCAP patients had a higher 30-day mortality rate (13.7% vs. 5.6%, P=0.017), but mortality rate was less in the patients at low risk for MDR pathogens (8.6% vs. 18.2%, P=0.012). Of the HCAP patients, only 7.1% received inappropriate therapy (pathogen resistant to initial antibiotic regimen), and treatment failure was 19.3%.
Appropriateness of initial empiric therapy was determined not to be a mortality risk; however, this trial might be limited by its location, because Japan appears to have fewer MDR pathogens than the U.S.
Bottom line: A treatment algorithm based on risk for MDR organisms and severity of illness can be used to guide empiric antibiotic therapy in patients with HCAP, and, ideally, to reduce excessive use of broad-spectrum antibiotics.
Citation: Maruyama T, Fujisawa T, Okuno M, et al. A new strategy for healthcare-associated pneumonia: a 2-year prospective multicenter cohort study using risk factors for multidrug-resistant pathogens to select initial empiric therapy. Clin Infect Dis. 2013;57(10):1373-1383.
Clinical question: Can an algorithm based on risk for multidrug-resistant (MDR) organisms and illness severity guide antibiotic selection in healthcare-associated pneumonia (HCAP)?
Background: The 2005 American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) guidelines identify patients with HCAP as those with recent contact with a healthcare environment, including nursing homes and hemodialysis; however, previous studies have shown that not all patients with healthcare contact have equal risk for MDR organisms.
Study design: Prospective cohort study.
Setting: Japan, multi-center.
Synopsis: Of the 445 enrolled patients, 124 were diagnosed with community-acquired pneumonia (CAP) and 321 with HCAP. Patients with HCAP were classified based on severity of illness or MDR pathogen risk factors (immune suppression, hospitalization within the last 90 days, poor functional status, and antibiotics within the past six months). Patients with low risk (0-1 factors) for MDR organisms were treated for CAP, and patients with high risk (≥2 factors) or moderate risk (≥1 factor) for severe illness were treated for HCAP.
HCAP patients had a higher 30-day mortality rate (13.7% vs. 5.6%, P=0.017), but mortality rate was less in the patients at low risk for MDR pathogens (8.6% vs. 18.2%, P=0.012). Of the HCAP patients, only 7.1% received inappropriate therapy (pathogen resistant to initial antibiotic regimen), and treatment failure was 19.3%.
Appropriateness of initial empiric therapy was determined not to be a mortality risk; however, this trial might be limited by its location, because Japan appears to have fewer MDR pathogens than the U.S.
Bottom line: A treatment algorithm based on risk for MDR organisms and severity of illness can be used to guide empiric antibiotic therapy in patients with HCAP, and, ideally, to reduce excessive use of broad-spectrum antibiotics.
Citation: Maruyama T, Fujisawa T, Okuno M, et al. A new strategy for healthcare-associated pneumonia: a 2-year prospective multicenter cohort study using risk factors for multidrug-resistant pathogens to select initial empiric therapy. Clin Infect Dis. 2013;57(10):1373-1383.
Clinical question: Can an algorithm based on risk for multidrug-resistant (MDR) organisms and illness severity guide antibiotic selection in healthcare-associated pneumonia (HCAP)?
Background: The 2005 American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) guidelines identify patients with HCAP as those with recent contact with a healthcare environment, including nursing homes and hemodialysis; however, previous studies have shown that not all patients with healthcare contact have equal risk for MDR organisms.
Study design: Prospective cohort study.
Setting: Japan, multi-center.
Synopsis: Of the 445 enrolled patients, 124 were diagnosed with community-acquired pneumonia (CAP) and 321 with HCAP. Patients with HCAP were classified based on severity of illness or MDR pathogen risk factors (immune suppression, hospitalization within the last 90 days, poor functional status, and antibiotics within the past six months). Patients with low risk (0-1 factors) for MDR organisms were treated for CAP, and patients with high risk (≥2 factors) or moderate risk (≥1 factor) for severe illness were treated for HCAP.
HCAP patients had a higher 30-day mortality rate (13.7% vs. 5.6%, P=0.017), but mortality rate was less in the patients at low risk for MDR pathogens (8.6% vs. 18.2%, P=0.012). Of the HCAP patients, only 7.1% received inappropriate therapy (pathogen resistant to initial antibiotic regimen), and treatment failure was 19.3%.
Appropriateness of initial empiric therapy was determined not to be a mortality risk; however, this trial might be limited by its location, because Japan appears to have fewer MDR pathogens than the U.S.
Bottom line: A treatment algorithm based on risk for MDR organisms and severity of illness can be used to guide empiric antibiotic therapy in patients with HCAP, and, ideally, to reduce excessive use of broad-spectrum antibiotics.
Citation: Maruyama T, Fujisawa T, Okuno M, et al. A new strategy for healthcare-associated pneumonia: a 2-year prospective multicenter cohort study using risk factors for multidrug-resistant pathogens to select initial empiric therapy. Clin Infect Dis. 2013;57(10):1373-1383.