User login
Novartis CAR T-cell therapy adds a lymphoma indication
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.
FDA approves CAR T-cell therapy for lymphoma
The US Food and Drug Administration (FDA) has approved tisagenlecleucel (Kymriah®) for its second indication.
The chimeric antigen receptor (CAR) T-cell therapy is now approved to treat adults with relapsed or refractory large B-cell lymphoma after 2 or more lines of systemic therapy.
This includes patients with diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma.
The application for tisagenlecleucel in B-cell lymphoma was granted priority review. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
Tisagenlecleucel is also FDA-approved to treat patients age 25 and younger who have B-cell precursor acute lymphoblastic leukemia that is refractory or in second or later relapse.
Access to tisagenlecleucel
The prescribing information for tisagenlecleucel includes a boxed warning detailing the risk of cytokine release syndrome (CRS) and neurological toxicities for patients receiving tisagenlecleucel.
Because of these risks, tisagenlecleucel is only available through a Risk Evaluation and Mitigation Strategy (REMS) program. The REMS program serves to inform and educate healthcare professionals about the risks associated with tisagenlecleucel treatment.
Novartis, the company marketing tisagenlecleucel, has established a network of certified treatment centers throughout the US. Staff at these centers are trained on the use of tisagenlecleucel and appropriate patient care.
Tisagenlecleucel is manufactured at a Novartis facility in Morris Plains, New Jersey. In the US, the target turnaround time for manufacturing tisagenlecleucel is 22 days.
Tisagenlecleucel costs $475,000 for a single course of treatment. However, Novartis said it is collaborating with the US Centers for Medicare and Medicaid Services on the creation of an appropriate value-based pricing approach.
The company also has a program called KYMRIAH CARES™, which offers financial assistance to eligible patients to help them gain access to tisagenlecleucel.
Phase 2 trial
The FDA approval of tisagenlecleucel for adults with relapsed/refractory B-cell lymphoma is based on results of the phase 2 JULIET trial.
The prescribing information for tisagenlecleucel includes data on 106 patients treated on this trial.
Only 68 of these patients were evaluable for efficacy. They had a median age of 56 (range, 22 to 74), and 71% were male.
Seventy-eight percent of patients had primary DLBCL not otherwise specified, and 22% had DLBCL following transformation from follicular lymphoma. Seventeen percent had high grade DLBCL.
Fifty-six percent of patients had refractory disease, and 44% had relapsed after their last therapy. The median number of prior therapies was 3 (range, 1 to 6), and 44% of patients had undergone autologous transplant.
Ninety percent of patients received lymphodepleting chemotherapy (66% fludarabine and 24% bendamustine) prior to tisagenlecleucel, and 10% did not. The median dose of tisagenlecleucel was 3.5 × 108 CAR+ T cells (range, 1.0 to 5.2 × 108).
The overall response rate was 50%, with 32% of patients achieving a complete response and 18% achieving a partial response. The median duration of response was not reached with a median follow-up of 9.4 months.
In all 106 patients infused with tisagenlecleucel, the most common grade 3/4 adverse events were infections (25%), CRS (23%), neurologic events (18%), febrile neutropenia (17%), encephalopathy (11%), lymphopenia (94%), neutropenia (81%), leukopenia (77%), anemia (58%), thrombocytopenia (54%), hypophosphatemia (24%), hypokalemia (12%), and hyponatremia (11%).
Three patients died within 30 days of tisagenlecleucel infusion. All of them had CRS and either stable or progressive disease. One of these patients developed bowel necrosis.
One patient died of infection. There were no deaths attributed to neurological events, and no fatal cases of cerebral edema.
The US Food and Drug Administration (FDA) has approved tisagenlecleucel (Kymriah®) for its second indication.
The chimeric antigen receptor (CAR) T-cell therapy is now approved to treat adults with relapsed or refractory large B-cell lymphoma after 2 or more lines of systemic therapy.
This includes patients with diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma.
The application for tisagenlecleucel in B-cell lymphoma was granted priority review. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
Tisagenlecleucel is also FDA-approved to treat patients age 25 and younger who have B-cell precursor acute lymphoblastic leukemia that is refractory or in second or later relapse.
Access to tisagenlecleucel
The prescribing information for tisagenlecleucel includes a boxed warning detailing the risk of cytokine release syndrome (CRS) and neurological toxicities for patients receiving tisagenlecleucel.
Because of these risks, tisagenlecleucel is only available through a Risk Evaluation and Mitigation Strategy (REMS) program. The REMS program serves to inform and educate healthcare professionals about the risks associated with tisagenlecleucel treatment.
Novartis, the company marketing tisagenlecleucel, has established a network of certified treatment centers throughout the US. Staff at these centers are trained on the use of tisagenlecleucel and appropriate patient care.
Tisagenlecleucel is manufactured at a Novartis facility in Morris Plains, New Jersey. In the US, the target turnaround time for manufacturing tisagenlecleucel is 22 days.
Tisagenlecleucel costs $475,000 for a single course of treatment. However, Novartis said it is collaborating with the US Centers for Medicare and Medicaid Services on the creation of an appropriate value-based pricing approach.
The company also has a program called KYMRIAH CARES™, which offers financial assistance to eligible patients to help them gain access to tisagenlecleucel.
Phase 2 trial
The FDA approval of tisagenlecleucel for adults with relapsed/refractory B-cell lymphoma is based on results of the phase 2 JULIET trial.
The prescribing information for tisagenlecleucel includes data on 106 patients treated on this trial.
Only 68 of these patients were evaluable for efficacy. They had a median age of 56 (range, 22 to 74), and 71% were male.
Seventy-eight percent of patients had primary DLBCL not otherwise specified, and 22% had DLBCL following transformation from follicular lymphoma. Seventeen percent had high grade DLBCL.
Fifty-six percent of patients had refractory disease, and 44% had relapsed after their last therapy. The median number of prior therapies was 3 (range, 1 to 6), and 44% of patients had undergone autologous transplant.
Ninety percent of patients received lymphodepleting chemotherapy (66% fludarabine and 24% bendamustine) prior to tisagenlecleucel, and 10% did not. The median dose of tisagenlecleucel was 3.5 × 108 CAR+ T cells (range, 1.0 to 5.2 × 108).
The overall response rate was 50%, with 32% of patients achieving a complete response and 18% achieving a partial response. The median duration of response was not reached with a median follow-up of 9.4 months.
In all 106 patients infused with tisagenlecleucel, the most common grade 3/4 adverse events were infections (25%), CRS (23%), neurologic events (18%), febrile neutropenia (17%), encephalopathy (11%), lymphopenia (94%), neutropenia (81%), leukopenia (77%), anemia (58%), thrombocytopenia (54%), hypophosphatemia (24%), hypokalemia (12%), and hyponatremia (11%).
Three patients died within 30 days of tisagenlecleucel infusion. All of them had CRS and either stable or progressive disease. One of these patients developed bowel necrosis.
One patient died of infection. There were no deaths attributed to neurological events, and no fatal cases of cerebral edema.
The US Food and Drug Administration (FDA) has approved tisagenlecleucel (Kymriah®) for its second indication.
The chimeric antigen receptor (CAR) T-cell therapy is now approved to treat adults with relapsed or refractory large B-cell lymphoma after 2 or more lines of systemic therapy.
This includes patients with diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma.
The application for tisagenlecleucel in B-cell lymphoma was granted priority review. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
Tisagenlecleucel is also FDA-approved to treat patients age 25 and younger who have B-cell precursor acute lymphoblastic leukemia that is refractory or in second or later relapse.
Access to tisagenlecleucel
The prescribing information for tisagenlecleucel includes a boxed warning detailing the risk of cytokine release syndrome (CRS) and neurological toxicities for patients receiving tisagenlecleucel.
Because of these risks, tisagenlecleucel is only available through a Risk Evaluation and Mitigation Strategy (REMS) program. The REMS program serves to inform and educate healthcare professionals about the risks associated with tisagenlecleucel treatment.
Novartis, the company marketing tisagenlecleucel, has established a network of certified treatment centers throughout the US. Staff at these centers are trained on the use of tisagenlecleucel and appropriate patient care.
Tisagenlecleucel is manufactured at a Novartis facility in Morris Plains, New Jersey. In the US, the target turnaround time for manufacturing tisagenlecleucel is 22 days.
Tisagenlecleucel costs $475,000 for a single course of treatment. However, Novartis said it is collaborating with the US Centers for Medicare and Medicaid Services on the creation of an appropriate value-based pricing approach.
The company also has a program called KYMRIAH CARES™, which offers financial assistance to eligible patients to help them gain access to tisagenlecleucel.
Phase 2 trial
The FDA approval of tisagenlecleucel for adults with relapsed/refractory B-cell lymphoma is based on results of the phase 2 JULIET trial.
The prescribing information for tisagenlecleucel includes data on 106 patients treated on this trial.
Only 68 of these patients were evaluable for efficacy. They had a median age of 56 (range, 22 to 74), and 71% were male.
Seventy-eight percent of patients had primary DLBCL not otherwise specified, and 22% had DLBCL following transformation from follicular lymphoma. Seventeen percent had high grade DLBCL.
Fifty-six percent of patients had refractory disease, and 44% had relapsed after their last therapy. The median number of prior therapies was 3 (range, 1 to 6), and 44% of patients had undergone autologous transplant.
Ninety percent of patients received lymphodepleting chemotherapy (66% fludarabine and 24% bendamustine) prior to tisagenlecleucel, and 10% did not. The median dose of tisagenlecleucel was 3.5 × 108 CAR+ T cells (range, 1.0 to 5.2 × 108).
The overall response rate was 50%, with 32% of patients achieving a complete response and 18% achieving a partial response. The median duration of response was not reached with a median follow-up of 9.4 months.
In all 106 patients infused with tisagenlecleucel, the most common grade 3/4 adverse events were infections (25%), CRS (23%), neurologic events (18%), febrile neutropenia (17%), encephalopathy (11%), lymphopenia (94%), neutropenia (81%), leukopenia (77%), anemia (58%), thrombocytopenia (54%), hypophosphatemia (24%), hypokalemia (12%), and hyponatremia (11%).
Three patients died within 30 days of tisagenlecleucel infusion. All of them had CRS and either stable or progressive disease. One of these patients developed bowel necrosis.
One patient died of infection. There were no deaths attributed to neurological events, and no fatal cases of cerebral edema.
Background color a dermoscopic clue to cutaneous B-cell lymphoma
A salmon-colored background and prominent serpentine blood vessels are two characteristic features of primary cutaneous B-cell lymphoma (PCBCL) that can be identified dermoscopically and may aid diagnosis, researchers say.
In the January issue of the Journal of the European Academy of Dermatology and Venereology, researchers reported the results of a retrospective observational study using the dermoscopic images of 58 biopsy-confirmed primary cutaneous B-cell lymphoma lesions in 51 patients.
While all the lesions were nonpigmented, 46 (79.3%) of them showed salmon- or yellow- to orange- colored background areas. More than three-quarters of the lesions also featured prominent blood vessels (77.6%), the majority of which were serpentine in nature.
, while only 8.6% of the lesions showed neither feature.
Of the 58 lesions, the authors selected 17 to be evaluated by two dermoscopy experts who were blinded to the diagnosis. In 70.6% of these cases they included cutaneous B-cell lymphoma in the differential diagnosis, while other diagnoses included spider bite (58.8%), basal cell carcinoma (52.9%), amelanotic melanoma (47.1%), and scar/keloid (47.1%). Overall, the two experts did not agree on almost 30% of the suggested differential diagnoses.
“The presentation of cutaneous lymphomas in general and of PCBCLs in particular can be nonspecific, and a biopsy is essential for a definitive diagnosis,” wrote Shamir Geller, MD, of the dermatology service at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
The 58 PCBCLs analyzed were among 172 biopsy-proven PCBCL lesions in the study, which were newly diagnosed and whose pathology reports included the clinical differential diagnosis in the pathology requisition slip, in patients referred to the cancer center between 1992 and 2016. In only 16.3% of these cases, the clinician suspected cutaneous lymphoma. Skin malignancies were suspected in 54.7% of cases, with the leading diagnosis being basal cell carcinoma in 17.4% of cases. Basal cell carcinoma was considered in nearly one-third of lesions, particularly those on the head and neck.
Nonneoplastic conditions suspected by clinicians included cyst in 21.5% of cases, granulomatous processes in 15.7%, and infectious disease in 4.7%.
The authors commented that a low index of suspicion for skin lymphoma was seen regardless of the subtype or site.
“While dermoscopy offers a bridge between the naked eye examination and the histopathological appearance, cutaneous lymphoma is diagnosed on a cellular level using histopathology, immunohistochemistry and molecular studies,” they wrote. “Therefore, dermoscopy may serve as an ancillary tool in PCBCL; however, it cannot be diagnostic.”
The study was supported in part by the National Institutes of Health/National Cancer Institute Cancer Center. Dr. Geller is a recipient of a grant from the American Physicians and Friends For Medicine in Israel. No conflicts of interest were declared.
SOURCE: Geller S et al. J Eur Acad Dermatol Venereol. 2018 Jan;32(1):53-6.
A salmon-colored background and prominent serpentine blood vessels are two characteristic features of primary cutaneous B-cell lymphoma (PCBCL) that can be identified dermoscopically and may aid diagnosis, researchers say.
In the January issue of the Journal of the European Academy of Dermatology and Venereology, researchers reported the results of a retrospective observational study using the dermoscopic images of 58 biopsy-confirmed primary cutaneous B-cell lymphoma lesions in 51 patients.
While all the lesions were nonpigmented, 46 (79.3%) of them showed salmon- or yellow- to orange- colored background areas. More than three-quarters of the lesions also featured prominent blood vessels (77.6%), the majority of which were serpentine in nature.
, while only 8.6% of the lesions showed neither feature.
Of the 58 lesions, the authors selected 17 to be evaluated by two dermoscopy experts who were blinded to the diagnosis. In 70.6% of these cases they included cutaneous B-cell lymphoma in the differential diagnosis, while other diagnoses included spider bite (58.8%), basal cell carcinoma (52.9%), amelanotic melanoma (47.1%), and scar/keloid (47.1%). Overall, the two experts did not agree on almost 30% of the suggested differential diagnoses.
“The presentation of cutaneous lymphomas in general and of PCBCLs in particular can be nonspecific, and a biopsy is essential for a definitive diagnosis,” wrote Shamir Geller, MD, of the dermatology service at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
The 58 PCBCLs analyzed were among 172 biopsy-proven PCBCL lesions in the study, which were newly diagnosed and whose pathology reports included the clinical differential diagnosis in the pathology requisition slip, in patients referred to the cancer center between 1992 and 2016. In only 16.3% of these cases, the clinician suspected cutaneous lymphoma. Skin malignancies were suspected in 54.7% of cases, with the leading diagnosis being basal cell carcinoma in 17.4% of cases. Basal cell carcinoma was considered in nearly one-third of lesions, particularly those on the head and neck.
Nonneoplastic conditions suspected by clinicians included cyst in 21.5% of cases, granulomatous processes in 15.7%, and infectious disease in 4.7%.
The authors commented that a low index of suspicion for skin lymphoma was seen regardless of the subtype or site.
“While dermoscopy offers a bridge between the naked eye examination and the histopathological appearance, cutaneous lymphoma is diagnosed on a cellular level using histopathology, immunohistochemistry and molecular studies,” they wrote. “Therefore, dermoscopy may serve as an ancillary tool in PCBCL; however, it cannot be diagnostic.”
The study was supported in part by the National Institutes of Health/National Cancer Institute Cancer Center. Dr. Geller is a recipient of a grant from the American Physicians and Friends For Medicine in Israel. No conflicts of interest were declared.
SOURCE: Geller S et al. J Eur Acad Dermatol Venereol. 2018 Jan;32(1):53-6.
A salmon-colored background and prominent serpentine blood vessels are two characteristic features of primary cutaneous B-cell lymphoma (PCBCL) that can be identified dermoscopically and may aid diagnosis, researchers say.
In the January issue of the Journal of the European Academy of Dermatology and Venereology, researchers reported the results of a retrospective observational study using the dermoscopic images of 58 biopsy-confirmed primary cutaneous B-cell lymphoma lesions in 51 patients.
While all the lesions were nonpigmented, 46 (79.3%) of them showed salmon- or yellow- to orange- colored background areas. More than three-quarters of the lesions also featured prominent blood vessels (77.6%), the majority of which were serpentine in nature.
, while only 8.6% of the lesions showed neither feature.
Of the 58 lesions, the authors selected 17 to be evaluated by two dermoscopy experts who were blinded to the diagnosis. In 70.6% of these cases they included cutaneous B-cell lymphoma in the differential diagnosis, while other diagnoses included spider bite (58.8%), basal cell carcinoma (52.9%), amelanotic melanoma (47.1%), and scar/keloid (47.1%). Overall, the two experts did not agree on almost 30% of the suggested differential diagnoses.
“The presentation of cutaneous lymphomas in general and of PCBCLs in particular can be nonspecific, and a biopsy is essential for a definitive diagnosis,” wrote Shamir Geller, MD, of the dermatology service at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
The 58 PCBCLs analyzed were among 172 biopsy-proven PCBCL lesions in the study, which were newly diagnosed and whose pathology reports included the clinical differential diagnosis in the pathology requisition slip, in patients referred to the cancer center between 1992 and 2016. In only 16.3% of these cases, the clinician suspected cutaneous lymphoma. Skin malignancies were suspected in 54.7% of cases, with the leading diagnosis being basal cell carcinoma in 17.4% of cases. Basal cell carcinoma was considered in nearly one-third of lesions, particularly those on the head and neck.
Nonneoplastic conditions suspected by clinicians included cyst in 21.5% of cases, granulomatous processes in 15.7%, and infectious disease in 4.7%.
The authors commented that a low index of suspicion for skin lymphoma was seen regardless of the subtype or site.
“While dermoscopy offers a bridge between the naked eye examination and the histopathological appearance, cutaneous lymphoma is diagnosed on a cellular level using histopathology, immunohistochemistry and molecular studies,” they wrote. “Therefore, dermoscopy may serve as an ancillary tool in PCBCL; however, it cannot be diagnostic.”
The study was supported in part by the National Institutes of Health/National Cancer Institute Cancer Center. Dr. Geller is a recipient of a grant from the American Physicians and Friends For Medicine in Israel. No conflicts of interest were declared.
SOURCE: Geller S et al. J Eur Acad Dermatol Venereol. 2018 Jan;32(1):53-6.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Key clinical point: A salmon-colored background and prominent serpentine blood vessels are two characteristic dermoscopic features of primary cutaneous B-cell lymphoma (PCBCL).
Major finding: Nearly 80% of PCBCLs had a salmon-colored background on dermoscopy.
Data source: A retrospective observational study that analyzed 172 biopsy-proven PCBCLs, including 58 PCBCL dermoscopic images.
Disclosures: The study was supported by the NIH/NCI Cancer Center. The lead author received a grant from the American Physicians and Friends for Medicine in Israel. No conflicts of interest were declared.
Source: Geller S et al. J Eur Acad Dermatol Venereol. 2018 Jan;32(1):53-6.
VIDEO: CAR T cell axi-cel drives B-cell lymphomas into remission
ATLANTA – In the ZUMA-1 trial, more than one-third of patients with refractory large B-cell lymphomas treated with the chimeric antigen receptor (CAR) T-cell product axicabtagene ciloleucel (Yescarta; axi-cel) had durable responses, with some patients having complete responses lasting more than 1 year after a single infusion.
Updated combined phase 1 and 2 results in 108 patients with diffuse large B-cell lymphoma, primary mediastinal B-cell lymphoma, or transformed follicular lymphoma showed an objective response rate of 82% of patients – including 58% showing complete responses – after a median follow-up of 15.4 months.
In a video interview at the annual meeting of the American Society of Hematology, Sattva S. Neelapu, MD, from the University of Texas MD Anderson Cancer Center in Houston discusses the use of CAR T cells directed against the CD19 antigen in patients with relapsed/refractory B-cell lymphomas and describes efforts to improve responses while managing adverse events common to CAR T-cell therapies, notably cytokine release syndrome.
ZUMA-1 is supported by Kite Pharma, which developed axicabtagene ciloleucel, and the Leukemia & Lymphoma Society’s Therapy Acceleration Program. Dr. Neelapu reported receiving advisory board fees from the company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – In the ZUMA-1 trial, more than one-third of patients with refractory large B-cell lymphomas treated with the chimeric antigen receptor (CAR) T-cell product axicabtagene ciloleucel (Yescarta; axi-cel) had durable responses, with some patients having complete responses lasting more than 1 year after a single infusion.
Updated combined phase 1 and 2 results in 108 patients with diffuse large B-cell lymphoma, primary mediastinal B-cell lymphoma, or transformed follicular lymphoma showed an objective response rate of 82% of patients – including 58% showing complete responses – after a median follow-up of 15.4 months.
In a video interview at the annual meeting of the American Society of Hematology, Sattva S. Neelapu, MD, from the University of Texas MD Anderson Cancer Center in Houston discusses the use of CAR T cells directed against the CD19 antigen in patients with relapsed/refractory B-cell lymphomas and describes efforts to improve responses while managing adverse events common to CAR T-cell therapies, notably cytokine release syndrome.
ZUMA-1 is supported by Kite Pharma, which developed axicabtagene ciloleucel, and the Leukemia & Lymphoma Society’s Therapy Acceleration Program. Dr. Neelapu reported receiving advisory board fees from the company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – In the ZUMA-1 trial, more than one-third of patients with refractory large B-cell lymphomas treated with the chimeric antigen receptor (CAR) T-cell product axicabtagene ciloleucel (Yescarta; axi-cel) had durable responses, with some patients having complete responses lasting more than 1 year after a single infusion.
Updated combined phase 1 and 2 results in 108 patients with diffuse large B-cell lymphoma, primary mediastinal B-cell lymphoma, or transformed follicular lymphoma showed an objective response rate of 82% of patients – including 58% showing complete responses – after a median follow-up of 15.4 months.
In a video interview at the annual meeting of the American Society of Hematology, Sattva S. Neelapu, MD, from the University of Texas MD Anderson Cancer Center in Houston discusses the use of CAR T cells directed against the CD19 antigen in patients with relapsed/refractory B-cell lymphomas and describes efforts to improve responses while managing adverse events common to CAR T-cell therapies, notably cytokine release syndrome.
ZUMA-1 is supported by Kite Pharma, which developed axicabtagene ciloleucel, and the Leukemia & Lymphoma Society’s Therapy Acceleration Program. Dr. Neelapu reported receiving advisory board fees from the company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM ASH 2017
Updated ZUMA-1 data show durable CAR-T responses in B-cell lymphomas
ATLANTA – More than one-third of patients with refractory large B-cell lymphomas treated with the chimeric antigen receptor (CAR) T-cell product axicabtagene ciloleucel (Yescarta), often called axi-cel, had durable responses, with some patients having complete responses lasting more than 1 year after a single infusion, according to investigators in the ZUMA-1 trial.
Updated combined phase 1 and phase 2 results in 108 patients with diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), or transformed follicular lymphoma (TFL) showed an objective response rate (ORR) of 82%, including 58% complete responses, after a median follow-up of 15.4 months, reported Sattva S. Neelapu, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Axi-cel is highly effective in patients with large B-cell lymphoma who otherwise have no curative treatment options,” he said in a briefing at the annual meeting of the American Society of Hematology, prior to his presentation of the data in an oral session.
The trial results were also published simultaneously in the New England Journal of Medicine.As previously reported, in the multicenter phase 2 ZUMA-1 trial, 111 patients with treatment refractory DLBCL, PMBCL, or TFL were enrolled and treated with axi-cel at a target dose of 2 x 106 cells/kg, following a conditioning regimen with low-dose cyclophosphamide and fludarabine.
The median patient age was 58 years. Patients had stage III or IV disease, 48% had International Prognostic Index scores of 3-4, 76% had disease that was refractory to third-line therapies or beyond, and 21% had disease that relapsed within 12 months of an autologous bone marrow transplant
Axi-cel was successfully manufactured with sufficient cells for transfusion in all but one of the 111 patients, and 101 patients eventually received infusions in phase 2 (modified intention-to-treat population). The average turnaround time from apheresis to the clinical site was 17 days.
Dr. Neelapu also presented data on seven patients enrolled in phase 1; the data were combined with the phase 2 results for an updated analysis of those patients who had at least 1 year of follow-up.
The phase 2 trial met its primary endpoint at the time of the primary analysis, with an 82% ORR, consisting of 54% complete responses and 28% partial responses at a median follow-up of 8.7 months.
In the updated analysis, the ORR and respective remission rates were 82%, 58%, and 34%, at a median of 15.4 months follow-up.
The median duration of response in the updated analysis was 11.1 months. The median duration of complete responses had not been reached at the time of data cutoff in August 2017. The median duration of partial responses was 1.9 months.
At the 15.4-month mark, 42% of patients remained free of disease progression, and 56% were alive, with the median overall survival not yet reached.
The treatment had generally acceptable toxicities, with only 13% of patients in phase 2 experiencing grade 3 or greater cytokine release syndrome (CRS), although one patient with CRS died from hemophagocytic lymphohistiocytosis, and one with CRS died from cardiac arrest. Grade 3 or greater neurologic events occurred in 28% of patients, and included encephalopathy, confusional state, aphasia, and somnolence.
The events were generally reversible, and the rates of each declined over time. The use of tocilizumab or steroids to control adverse events did not have a negative effect on responses.
Since the primary analysis with at least 6 months of follow-up, there have been no new axi-cel–related cases of CRS, neurologic events, or deaths.
Dr. Neelapu also presented safety data on serious adverse events occurring more than 6 months after therapy in 10 patients who developed symptoms after the data cutoff.
Grade 3 events in these patients included lung infection, recurrent upper respiratory viral infection, and rotavirus infection, pneumonias, atrial fibrillation with rapid ventricular response, lung infection, febrile neutropenia, and influenza B infection. One patient had grade 4 sepsis.
In an editorial accompanying the study in the New England Journal of Medicine, Eric Tran, PhD, and Walter J. Urba, MD, PhD, from the Earle A. Chiles Research Institute and the Providence Portland (Ore.) Medical Center, and Dan L. Longo, MD, deputy editor of the journal, praised ZUMA-1 as “a landmark study because it involved 22 institutions and showed that a personalized gene-engineered T-cell product could be rapidly generated at a centralized cell-manufacturing facility and safely administered to patients at transplantation-capable medical centers.”
They noted, however, that about half of all patients with relapsed or refractory large B-cell lymphomas will not have durable responses to CAR T-cell therapy directed against CD19, and that new strategies will be needed to improve responses (N Engl J Med. 2017 Dec 10; doi: 10.1056/NEJMe1714680).
In the question and answer session at the end of the briefing, Dr. Neelapu said the preliminary observations of mechanisms of relapse or disease progression in some patients may be related to the loss of the CD19 antigen, which occurs in about one-third of patients who experience relapse, and to high expression of the programmed death ligand-1, which can potentially inhibit CAR-T cell function. A clinical trial is currently underway to evaluate potential strategies for improving response rates to CAR-T therapies, he said.
ZUMA-1 is supported by Kite Pharma and the Leukemia and Lymphoma Society Therapy Acceleration Program. Dr. Neelapu reported receiving advisory board fees from the company. Myriad coauthors also reported financial relationship with multiple companies.
SOURCE: Neelapu S et al. ASH 2017 Abstract 578.
ATLANTA – More than one-third of patients with refractory large B-cell lymphomas treated with the chimeric antigen receptor (CAR) T-cell product axicabtagene ciloleucel (Yescarta), often called axi-cel, had durable responses, with some patients having complete responses lasting more than 1 year after a single infusion, according to investigators in the ZUMA-1 trial.
Updated combined phase 1 and phase 2 results in 108 patients with diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), or transformed follicular lymphoma (TFL) showed an objective response rate (ORR) of 82%, including 58% complete responses, after a median follow-up of 15.4 months, reported Sattva S. Neelapu, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Axi-cel is highly effective in patients with large B-cell lymphoma who otherwise have no curative treatment options,” he said in a briefing at the annual meeting of the American Society of Hematology, prior to his presentation of the data in an oral session.
The trial results were also published simultaneously in the New England Journal of Medicine.As previously reported, in the multicenter phase 2 ZUMA-1 trial, 111 patients with treatment refractory DLBCL, PMBCL, or TFL were enrolled and treated with axi-cel at a target dose of 2 x 106 cells/kg, following a conditioning regimen with low-dose cyclophosphamide and fludarabine.
The median patient age was 58 years. Patients had stage III or IV disease, 48% had International Prognostic Index scores of 3-4, 76% had disease that was refractory to third-line therapies or beyond, and 21% had disease that relapsed within 12 months of an autologous bone marrow transplant
Axi-cel was successfully manufactured with sufficient cells for transfusion in all but one of the 111 patients, and 101 patients eventually received infusions in phase 2 (modified intention-to-treat population). The average turnaround time from apheresis to the clinical site was 17 days.
Dr. Neelapu also presented data on seven patients enrolled in phase 1; the data were combined with the phase 2 results for an updated analysis of those patients who had at least 1 year of follow-up.
The phase 2 trial met its primary endpoint at the time of the primary analysis, with an 82% ORR, consisting of 54% complete responses and 28% partial responses at a median follow-up of 8.7 months.
In the updated analysis, the ORR and respective remission rates were 82%, 58%, and 34%, at a median of 15.4 months follow-up.
The median duration of response in the updated analysis was 11.1 months. The median duration of complete responses had not been reached at the time of data cutoff in August 2017. The median duration of partial responses was 1.9 months.
At the 15.4-month mark, 42% of patients remained free of disease progression, and 56% were alive, with the median overall survival not yet reached.
The treatment had generally acceptable toxicities, with only 13% of patients in phase 2 experiencing grade 3 or greater cytokine release syndrome (CRS), although one patient with CRS died from hemophagocytic lymphohistiocytosis, and one with CRS died from cardiac arrest. Grade 3 or greater neurologic events occurred in 28% of patients, and included encephalopathy, confusional state, aphasia, and somnolence.
The events were generally reversible, and the rates of each declined over time. The use of tocilizumab or steroids to control adverse events did not have a negative effect on responses.
Since the primary analysis with at least 6 months of follow-up, there have been no new axi-cel–related cases of CRS, neurologic events, or deaths.
Dr. Neelapu also presented safety data on serious adverse events occurring more than 6 months after therapy in 10 patients who developed symptoms after the data cutoff.
Grade 3 events in these patients included lung infection, recurrent upper respiratory viral infection, and rotavirus infection, pneumonias, atrial fibrillation with rapid ventricular response, lung infection, febrile neutropenia, and influenza B infection. One patient had grade 4 sepsis.
In an editorial accompanying the study in the New England Journal of Medicine, Eric Tran, PhD, and Walter J. Urba, MD, PhD, from the Earle A. Chiles Research Institute and the Providence Portland (Ore.) Medical Center, and Dan L. Longo, MD, deputy editor of the journal, praised ZUMA-1 as “a landmark study because it involved 22 institutions and showed that a personalized gene-engineered T-cell product could be rapidly generated at a centralized cell-manufacturing facility and safely administered to patients at transplantation-capable medical centers.”
They noted, however, that about half of all patients with relapsed or refractory large B-cell lymphomas will not have durable responses to CAR T-cell therapy directed against CD19, and that new strategies will be needed to improve responses (N Engl J Med. 2017 Dec 10; doi: 10.1056/NEJMe1714680).
In the question and answer session at the end of the briefing, Dr. Neelapu said the preliminary observations of mechanisms of relapse or disease progression in some patients may be related to the loss of the CD19 antigen, which occurs in about one-third of patients who experience relapse, and to high expression of the programmed death ligand-1, which can potentially inhibit CAR-T cell function. A clinical trial is currently underway to evaluate potential strategies for improving response rates to CAR-T therapies, he said.
ZUMA-1 is supported by Kite Pharma and the Leukemia and Lymphoma Society Therapy Acceleration Program. Dr. Neelapu reported receiving advisory board fees from the company. Myriad coauthors also reported financial relationship with multiple companies.
SOURCE: Neelapu S et al. ASH 2017 Abstract 578.
ATLANTA – More than one-third of patients with refractory large B-cell lymphomas treated with the chimeric antigen receptor (CAR) T-cell product axicabtagene ciloleucel (Yescarta), often called axi-cel, had durable responses, with some patients having complete responses lasting more than 1 year after a single infusion, according to investigators in the ZUMA-1 trial.
Updated combined phase 1 and phase 2 results in 108 patients with diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), or transformed follicular lymphoma (TFL) showed an objective response rate (ORR) of 82%, including 58% complete responses, after a median follow-up of 15.4 months, reported Sattva S. Neelapu, MD, from the University of Texas MD Anderson Cancer Center in Houston.
“Axi-cel is highly effective in patients with large B-cell lymphoma who otherwise have no curative treatment options,” he said in a briefing at the annual meeting of the American Society of Hematology, prior to his presentation of the data in an oral session.
The trial results were also published simultaneously in the New England Journal of Medicine.As previously reported, in the multicenter phase 2 ZUMA-1 trial, 111 patients with treatment refractory DLBCL, PMBCL, or TFL were enrolled and treated with axi-cel at a target dose of 2 x 106 cells/kg, following a conditioning regimen with low-dose cyclophosphamide and fludarabine.
The median patient age was 58 years. Patients had stage III or IV disease, 48% had International Prognostic Index scores of 3-4, 76% had disease that was refractory to third-line therapies or beyond, and 21% had disease that relapsed within 12 months of an autologous bone marrow transplant
Axi-cel was successfully manufactured with sufficient cells for transfusion in all but one of the 111 patients, and 101 patients eventually received infusions in phase 2 (modified intention-to-treat population). The average turnaround time from apheresis to the clinical site was 17 days.
Dr. Neelapu also presented data on seven patients enrolled in phase 1; the data were combined with the phase 2 results for an updated analysis of those patients who had at least 1 year of follow-up.
The phase 2 trial met its primary endpoint at the time of the primary analysis, with an 82% ORR, consisting of 54% complete responses and 28% partial responses at a median follow-up of 8.7 months.
In the updated analysis, the ORR and respective remission rates were 82%, 58%, and 34%, at a median of 15.4 months follow-up.
The median duration of response in the updated analysis was 11.1 months. The median duration of complete responses had not been reached at the time of data cutoff in August 2017. The median duration of partial responses was 1.9 months.
At the 15.4-month mark, 42% of patients remained free of disease progression, and 56% were alive, with the median overall survival not yet reached.
The treatment had generally acceptable toxicities, with only 13% of patients in phase 2 experiencing grade 3 or greater cytokine release syndrome (CRS), although one patient with CRS died from hemophagocytic lymphohistiocytosis, and one with CRS died from cardiac arrest. Grade 3 or greater neurologic events occurred in 28% of patients, and included encephalopathy, confusional state, aphasia, and somnolence.
The events were generally reversible, and the rates of each declined over time. The use of tocilizumab or steroids to control adverse events did not have a negative effect on responses.
Since the primary analysis with at least 6 months of follow-up, there have been no new axi-cel–related cases of CRS, neurologic events, or deaths.
Dr. Neelapu also presented safety data on serious adverse events occurring more than 6 months after therapy in 10 patients who developed symptoms after the data cutoff.
Grade 3 events in these patients included lung infection, recurrent upper respiratory viral infection, and rotavirus infection, pneumonias, atrial fibrillation with rapid ventricular response, lung infection, febrile neutropenia, and influenza B infection. One patient had grade 4 sepsis.
In an editorial accompanying the study in the New England Journal of Medicine, Eric Tran, PhD, and Walter J. Urba, MD, PhD, from the Earle A. Chiles Research Institute and the Providence Portland (Ore.) Medical Center, and Dan L. Longo, MD, deputy editor of the journal, praised ZUMA-1 as “a landmark study because it involved 22 institutions and showed that a personalized gene-engineered T-cell product could be rapidly generated at a centralized cell-manufacturing facility and safely administered to patients at transplantation-capable medical centers.”
They noted, however, that about half of all patients with relapsed or refractory large B-cell lymphomas will not have durable responses to CAR T-cell therapy directed against CD19, and that new strategies will be needed to improve responses (N Engl J Med. 2017 Dec 10; doi: 10.1056/NEJMe1714680).
In the question and answer session at the end of the briefing, Dr. Neelapu said the preliminary observations of mechanisms of relapse or disease progression in some patients may be related to the loss of the CD19 antigen, which occurs in about one-third of patients who experience relapse, and to high expression of the programmed death ligand-1, which can potentially inhibit CAR-T cell function. A clinical trial is currently underway to evaluate potential strategies for improving response rates to CAR-T therapies, he said.
ZUMA-1 is supported by Kite Pharma and the Leukemia and Lymphoma Society Therapy Acceleration Program. Dr. Neelapu reported receiving advisory board fees from the company. Myriad coauthors also reported financial relationship with multiple companies.
SOURCE: Neelapu S et al. ASH 2017 Abstract 578.
REPORTING FROM ASH 2017
Key clinical point:.
Major finding: The objective response rate was 82%, including 58% complete responses at a median of 15.4 months of follow-up.
Data source: Update analysis of phase 1 and 2 data from the ZUMA-1 trial in 108 patients with large B-cell lymphomas.
Disclosures: ZUMA-1 is supported by Kite Pharma and the Leukemia and Lymphoma Society Therapy Acceleration Program. Dr. Neelapu reported receiving advisory board fees from the company. Myriad coauthors also reported financial relationship with multiple companies.
Source: Neelapu S et al. ASH 2017 Abstract 578
Rituximab improves salvage in elderly B-cell lymphoma patients
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
FROM ANNALS OF ONCOLOGY
Key clinical point: Rituximab improved salvage therapy for elderly patients with aggressive-B-cell lymphoma who relapsed after CHOP or R-CHOP.
Major finding: Rituximab as part of a salvage regimen improved the 2-year survival rate from 20.7% to 46.8% (P less than .001).
Data source: Retrospective analysis including 297 elderly patients in the RICOVER-60 trial who had progressive, persistent, or relapsed lymphoma.
Disclosures: Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
Adding bortezomib to R-CHOP didn’t improve survival in diffuse large B-cell lymphoma
, findings from the phase-2 PYRAMID trial showed.
When the proteasome inhibitor bortezomib was combined with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in patients with previously untreated non–germinal center B-cell–like (non-GCB) DLBCL, a significant improvement in progression-free survival (PFS) was not observed.
There also was no increase in 2-year PFS among patients treated with the combination of bortezomib plus R-CHOP (VR-CHOP), according to findings from the open-label, randomized study published in the Journal of Clinical Oncology (2017 Sep 1. doi: 10.1200/JCO.2017.73.2784).
“A potential reason for the lack of benefit with VR-CHOP was that only two doses of bortezomib were given per 21-day cycle, whereas the standard schedule for bortezomib in multiple myeloma is four doses per cycle on days 1, 4, 8, and 11,” wrote John P. Leonard, MD, of Weill Cornell Medicine and New York Presbyterian Hospital, New York, and his colleagues. “In this study, treatment duration was limited to six 21-day cycles of R-CHOP.”
The authors noted that previous research has demonstrated the feasibility of using VR-CHOP and similar immunochemotherapy regimens in DLBCL. In the current PYRAMID (Personalized Lymphoma Therapy: Randomized Study of Proteasome Inhibition in Non-GCB DLBCL) phase 2 trial, VR-CHOP was compared with R-CHOP in 206 patients with previously untreated non-GCB DLBCL who were selected by real-time subtyping conducted or confirmed at a central laboratory that used the Hans algorithm.
The cohort was randomized to receive six 21-day cycles of standard R-CHOP alone or R-CHOP plus bortezomib 1.3 mg/m2 intravenously on days 1 and 4, and the primary endpoint was PFS.
The hazard ratio (HR) for PFS was 0.73 (90% confidence interval, 0.43-1.24) and favored VR-CHOP (P = .611), while the median PFS was not reached in either group. At 2 years, PFS was 77.6% with R-CHOP, versus 82.0% with VR-CHOP.
Among patients with high-intermediate/high International Prognostic Index (IPI) risk, those rates were 65.1% with R-CHOP, versus 72.4% with VR-CHOP (HR, 0.67; 90% CI, 0.34-1.29; P = .606). For those patients at low/low-intermediate IPI risk, the rates were 90.0% for R-CHOP, versus 88.9% for VR-CHOP (HR, 0.85; 90% CI, 0.35-2.10; P = .958).
The overall response rate was 98% for R-CHOP patients and 96% for VR-CHOP, with complete response rates of 49% and 56%, respectively.
Time to progression rates at 2 years were 79.8% for R-CHOP, versus 83.0% with VR-CHOP (HR, 0.79; 90% CI, 0.45-1.37; P = .767). While median overall survival was not reached in either arm, the HR for the entire cohort was 0.75 (90% CI, 0.38-1.45; P = .763). Two-year overall survival was 88.4% and 93.0%, respectively.
In the high-intermediate/high IPI score group, 2-year overall survival was 79.2% with R-CHOP, versus 92.1% with VR-CHOP (HR, 0.62; 90% CI, 0.25-1.42; P = .638), and for those with low/low-intermediate IPI risk scores, 97.7% versus 93.8% (HR, 1.02; 90% CI, 0.34-3.27; P = .999).
Millennium Pharmaceuticals supported the study. Dr. Leonard and several of the coauthors reported relationships with industry.
, findings from the phase-2 PYRAMID trial showed.
When the proteasome inhibitor bortezomib was combined with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in patients with previously untreated non–germinal center B-cell–like (non-GCB) DLBCL, a significant improvement in progression-free survival (PFS) was not observed.
There also was no increase in 2-year PFS among patients treated with the combination of bortezomib plus R-CHOP (VR-CHOP), according to findings from the open-label, randomized study published in the Journal of Clinical Oncology (2017 Sep 1. doi: 10.1200/JCO.2017.73.2784).
“A potential reason for the lack of benefit with VR-CHOP was that only two doses of bortezomib were given per 21-day cycle, whereas the standard schedule for bortezomib in multiple myeloma is four doses per cycle on days 1, 4, 8, and 11,” wrote John P. Leonard, MD, of Weill Cornell Medicine and New York Presbyterian Hospital, New York, and his colleagues. “In this study, treatment duration was limited to six 21-day cycles of R-CHOP.”
The authors noted that previous research has demonstrated the feasibility of using VR-CHOP and similar immunochemotherapy regimens in DLBCL. In the current PYRAMID (Personalized Lymphoma Therapy: Randomized Study of Proteasome Inhibition in Non-GCB DLBCL) phase 2 trial, VR-CHOP was compared with R-CHOP in 206 patients with previously untreated non-GCB DLBCL who were selected by real-time subtyping conducted or confirmed at a central laboratory that used the Hans algorithm.
The cohort was randomized to receive six 21-day cycles of standard R-CHOP alone or R-CHOP plus bortezomib 1.3 mg/m2 intravenously on days 1 and 4, and the primary endpoint was PFS.
The hazard ratio (HR) for PFS was 0.73 (90% confidence interval, 0.43-1.24) and favored VR-CHOP (P = .611), while the median PFS was not reached in either group. At 2 years, PFS was 77.6% with R-CHOP, versus 82.0% with VR-CHOP.
Among patients with high-intermediate/high International Prognostic Index (IPI) risk, those rates were 65.1% with R-CHOP, versus 72.4% with VR-CHOP (HR, 0.67; 90% CI, 0.34-1.29; P = .606). For those patients at low/low-intermediate IPI risk, the rates were 90.0% for R-CHOP, versus 88.9% for VR-CHOP (HR, 0.85; 90% CI, 0.35-2.10; P = .958).
The overall response rate was 98% for R-CHOP patients and 96% for VR-CHOP, with complete response rates of 49% and 56%, respectively.
Time to progression rates at 2 years were 79.8% for R-CHOP, versus 83.0% with VR-CHOP (HR, 0.79; 90% CI, 0.45-1.37; P = .767). While median overall survival was not reached in either arm, the HR for the entire cohort was 0.75 (90% CI, 0.38-1.45; P = .763). Two-year overall survival was 88.4% and 93.0%, respectively.
In the high-intermediate/high IPI score group, 2-year overall survival was 79.2% with R-CHOP, versus 92.1% with VR-CHOP (HR, 0.62; 90% CI, 0.25-1.42; P = .638), and for those with low/low-intermediate IPI risk scores, 97.7% versus 93.8% (HR, 1.02; 90% CI, 0.34-3.27; P = .999).
Millennium Pharmaceuticals supported the study. Dr. Leonard and several of the coauthors reported relationships with industry.
, findings from the phase-2 PYRAMID trial showed.
When the proteasome inhibitor bortezomib was combined with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in patients with previously untreated non–germinal center B-cell–like (non-GCB) DLBCL, a significant improvement in progression-free survival (PFS) was not observed.
There also was no increase in 2-year PFS among patients treated with the combination of bortezomib plus R-CHOP (VR-CHOP), according to findings from the open-label, randomized study published in the Journal of Clinical Oncology (2017 Sep 1. doi: 10.1200/JCO.2017.73.2784).
“A potential reason for the lack of benefit with VR-CHOP was that only two doses of bortezomib were given per 21-day cycle, whereas the standard schedule for bortezomib in multiple myeloma is four doses per cycle on days 1, 4, 8, and 11,” wrote John P. Leonard, MD, of Weill Cornell Medicine and New York Presbyterian Hospital, New York, and his colleagues. “In this study, treatment duration was limited to six 21-day cycles of R-CHOP.”
The authors noted that previous research has demonstrated the feasibility of using VR-CHOP and similar immunochemotherapy regimens in DLBCL. In the current PYRAMID (Personalized Lymphoma Therapy: Randomized Study of Proteasome Inhibition in Non-GCB DLBCL) phase 2 trial, VR-CHOP was compared with R-CHOP in 206 patients with previously untreated non-GCB DLBCL who were selected by real-time subtyping conducted or confirmed at a central laboratory that used the Hans algorithm.
The cohort was randomized to receive six 21-day cycles of standard R-CHOP alone or R-CHOP plus bortezomib 1.3 mg/m2 intravenously on days 1 and 4, and the primary endpoint was PFS.
The hazard ratio (HR) for PFS was 0.73 (90% confidence interval, 0.43-1.24) and favored VR-CHOP (P = .611), while the median PFS was not reached in either group. At 2 years, PFS was 77.6% with R-CHOP, versus 82.0% with VR-CHOP.
Among patients with high-intermediate/high International Prognostic Index (IPI) risk, those rates were 65.1% with R-CHOP, versus 72.4% with VR-CHOP (HR, 0.67; 90% CI, 0.34-1.29; P = .606). For those patients at low/low-intermediate IPI risk, the rates were 90.0% for R-CHOP, versus 88.9% for VR-CHOP (HR, 0.85; 90% CI, 0.35-2.10; P = .958).
The overall response rate was 98% for R-CHOP patients and 96% for VR-CHOP, with complete response rates of 49% and 56%, respectively.
Time to progression rates at 2 years were 79.8% for R-CHOP, versus 83.0% with VR-CHOP (HR, 0.79; 90% CI, 0.45-1.37; P = .767). While median overall survival was not reached in either arm, the HR for the entire cohort was 0.75 (90% CI, 0.38-1.45; P = .763). Two-year overall survival was 88.4% and 93.0%, respectively.
In the high-intermediate/high IPI score group, 2-year overall survival was 79.2% with R-CHOP, versus 92.1% with VR-CHOP (HR, 0.62; 90% CI, 0.25-1.42; P = .638), and for those with low/low-intermediate IPI risk scores, 97.7% versus 93.8% (HR, 1.02; 90% CI, 0.34-3.27; P = .999).
Millennium Pharmaceuticals supported the study. Dr. Leonard and several of the coauthors reported relationships with industry.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Bortezomib combined with R-CHOP did not improve outcomes significantly in diffuse large B-cell lymphoma.
Major finding: Two-year progression-free survival was 77.6% with R-CHOP, compared with 82.0% with VR-CHOP, a nonsignificant difference.
Data source: An open-label, randomized, phase 2 trial that compared VR-CHOP to R-CHOP in 206 patients with previously untreated non-GCB DLBCL.
Disclosures: Millennium Pharmaceuticals funded the study. Dr. Leonard and several of the coauthors reported relationships with industry.
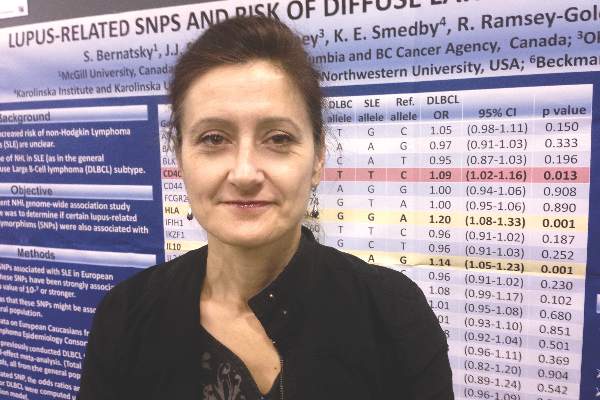
Lupus and diffuse large B-cell lymphoma share genetic risk
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
SAN FRANCISCO – Single-nucleotide polymorphisms in genes for interleukin 10 and human leukocyte antigen are significantly associated with both systemic lupus erythematosus (SLE) and diffuse large B-cell lymphoma, according to a meta-analysis of data from three genome-wide association studies.
The findings add to existing data that exonerates immunosuppressive medications as the main causes of lymphoma in patients with SLE, said lead investigator Dr. Sasha Bernatsky of McGill University, Montreal, in an interview. “People with lupus may have a slight increase in risk for lymphoma because of genetic factors, which would be reassuring,” she said. “It may even mean that if you take your baseline risk of lupus and you control the inflammation, perhaps you can modify that small increase in risk of lymphoma and make it more like the risk in the general population.”
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, with an incidence of about one case in 3,000 person-years in the general population and about one case in 1,000 person-years in patients with SLE, Dr. Bernatsky noted. To look for shared genetic risk factors for both diseases, she and her colleagues analyzed pooled data from three genome-wide association studies conducted by the International Lymphoma Epidemiology Consortium. Using data from 3,857 patients with DLBCL and 7,666 controls, the investigators calculated the odds of DLBCL for each of 28 SNPs that are known genetic risk variants for SLE. “If there’s an overlap there, that might be the key,” Dr. Bernatsky said at the annual meeting of the American College of Rheumatology.
In fact, two SLE-related SNPs were clearly linked to an increased risk for DLBCL – rs3024505, a variant allele of the gene for interleukin 10 on chromosome 1 (odds ratio, 1.14; 95% confidence interval, 1.05-1.23; P = .001), and rs1270942, a variant of the gene for human leukocyte antigen on chromosome 6 (OR, 1.2; 95% CI, 1.08-1.33; P = .0007). Both SNPs seem plausible – interleukin 10 induces the bcl-2 protein, which prevents the spontaneous death of germinal center B cells, and some evidence has linked HLA polymorphisms to DLBCL, Dr. Bernatsky said.
The study also linked two other SLE-related SNPs to increased risk for DLBCL, although the associations were not as strong. The first was rs4810485 on the CD40 gene (OR, 1.09; 95% CI, 1.02-1.16; P = .013), and the second was rs2205960 on the TNFSF4 gene, which encodes a cytokine from the tumor necrosis factor–superfamily (OR, 1.08; 95% CI, 1.02-1.15; P = .044). “These findings kind of make sense, because tumor necrosis factor is a very important inflammatory cytokine, and CD40 is a lymphocyte marker,” Dr. Bernatsky said. “It is possible that some genetic factor that controls their expression or function might be associated with lymphoma.”
Rheumatologists have long debated why patients with lupus are at increased risk for lymphoma, and have repeatedly asked whether immunomodulatory drugs are to blame. “We can exercise some caution, but still be aware that most people who use these drugs never end up developing cancer,” Dr. Bernatsky emphasized. In past studies, the absolute risk of lymphoma in patients with SLE remained below 1%, and those patients who did develop lymphoma often had never received drugs such as azathioprine, she noted. The exception was cyclophosphamide, which caused various severe adverse effects, including blood cancers (Ann Rheum Dis. 2013 Jan 8. doi: 10.1136/annrheumdis-2012-202099). “Although we need to use cyclophosphamide for very severe cases of autoimmune disease, it’s clearly a drug that we should use almost as a last resort,” she said.
The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Two genetic risk variants for systemic lupus erythematosus also were clearly linked to risk of diffuse large B-cell lymphoma.
Major finding: The single-nucleotide polymorphisms were rs3024505 on chromosome 1 (OR, 1.14; P = .001), and rs1270942 on chromosome 6 (OR, 1.2; P = .0007).
Data source: A fixed-effect meta-analysis of 28 SLE-related SNPs from 3,857 patients with diffuse large B-cell lymphoma and 7,666 controls.
Disclosures: The study was funded by the Canadian Institutes for Health Research; the Fonds du recherche du Québec; Santé, the Research Institute of the McGill University Health Centre; and the Singer Family Fund for Lupus Research. Dr. Bernatsky and her coinvestigators had no disclosures.
Routine imaging for diffuse large B-cell lymphoma offers no survival benefit
A population-based comparison of patients with diffuse large B-cell lymphoma (DLBCL) in first complete remission indicated that routine imaging surveillance did not improve outcomes, researchers reported.
Overall survival was similar for Danish and Swedish populations who received similar follow-up care, except that routine imaging surveillance is the standard of care in Denmark, but not in Sweden. The 3-year overall survival for Danish and Swedish patients was 92% and 91%, respectively.
Outcomes grouped by international prognostic index (IPI) also showed no significant differences between populations (J Clin Oncol. 2015 Oct 5, doi:10.1200/jco.2015.62.0229.).
“An imaging-based follow-up strategy does not improve postremission [overall survival] for DLBCL,” wrote Dr. Tarec Christoffer El-Galaly, of Aalborg University Hospital, Denmark, and colleagues.
They observed that aside from using IPI as risk stratification, the study “also points to baseline [lactate dehyrogenase] as a single discriminator of patients with high versus low risk of progression,” (Hazard ratio, 3.12; 95% CI, 1.78-5.48; P less than .01).
The retrospective study examined records of patients with DLBCL from Sweden (n=696) and Denmark (n=525) who achieved first complete remission after first-line therapy with R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) and CHOP-like regimens from 2007 to 2012. The proportion of patients with IPI greater than two were similar for both groups, though more Danish patients received radiotherapy compared with their Swedish counterparts (35% v. 9%).
Standard follow-up care after first complete remission is similar in Denmark and Sweden and typically includes symptom assessment, clinical examination, and blood tests at 3- to 4-month intervals for 2 years, and 6-month intervals in the third year. After 3 years, Swedish patients are seen annually for 2 years and then follow-up is ended for most patients. In Denmark, 6-month checks are continued until 5 years and then follow-up is usually ended. However, in Denmark guidelines support routine computerized tomography (CT) scans of the neck, abdomen, and thorax every 6 months for 2 years, which is not encouraged by guidelines in Sweden.
Early relapse detection aims to improve survival, and although low disease burden is associated with durable survival in patients treated for relapsed DLBCL, most studies show similar outcomes for imaging versus non-imaging detection. Additionally, previous retrospective studies that have reported survival differences based on relapse detection method are prone to lead-time bias, according to the researchers.
Given that a majority of patients with recurrent DLBCL experience symptoms before relapse, that elevated lactate dehyrogenase or abnormal physical examination may raise suspicion, and that exposure to ionizing radiation from medical imaging can lead to radiation-induced cancers, “routine imaging for DLBCL in first [complete remission] is not recommended,” the authors wrote.
The research was supported in part by the North Denmark Region. Dr. El-Galaly and coauthors reported having no financial disclosures.
The best way to determine the effectiveness of surveillance imaging would be a randomized trial including patients with diffuse large B-cell lymphoma (DLBCL) after first complete remission, but it is unlikely that such a study will be done. The study by El-Galaly et al may be the next best approach. Taking advantage of the fact that neighboring countries Denmark and Sweden have opposite policies for surveillance imaging but otherwise similar follow-up visit schedules and testing, the authors identified factors that predicted relapse (e.g., age greater than 60 years and elevated LDH), and they found that routine surveillance imaging had no impact on outcome. The study presents the strongest argument yet published against routine surveillance imaging.
The two other outstanding issues of routine surveillance are long-term safety and cost benefit. The study by El-Galaly et al, in combination with several other reports, suggests that routine surveillance imaging, in the absence of new or suspicious symptoms, physical findings, or change in laboratory results, is unlikely to benefit patients, may add to the patient’s stress, may cause long-term health problems, and incurs substantial economic cost.
Dr. James O. Armitage and Dr. Julie M. Vose are both at the University of Nebraska, Omaha. Dr. Armitage disclosed a leadership role with Tesaro and consulting or advisory roles with GlaxoSmithKline, Roche, Spectrum Pharmaceuticals, ZIOPHARM Oncology, Conatus, and Celgene. Dr. Vose reported honoraria from Sanofi-Aventis and Seattle Genetics; consulting or advisory roles with Bioconnections; and institutional research funding from Spectrum Pharmaceuticals, Bristol-Myers Squibb, Celgene, Genentech, GlaxoSmithKline, Incyte, Janssen Biotech, Pharmacyclics, Acerta, and Kite Pharma. These remarks were adapted from their accompanying editorial (J Clin Oncol. 2015 Oct 5, doi:10.1200/jco.2015.63.5946).
The best way to determine the effectiveness of surveillance imaging would be a randomized trial including patients with diffuse large B-cell lymphoma (DLBCL) after first complete remission, but it is unlikely that such a study will be done. The study by El-Galaly et al may be the next best approach. Taking advantage of the fact that neighboring countries Denmark and Sweden have opposite policies for surveillance imaging but otherwise similar follow-up visit schedules and testing, the authors identified factors that predicted relapse (e.g., age greater than 60 years and elevated LDH), and they found that routine surveillance imaging had no impact on outcome. The study presents the strongest argument yet published against routine surveillance imaging.
The two other outstanding issues of routine surveillance are long-term safety and cost benefit. The study by El-Galaly et al, in combination with several other reports, suggests that routine surveillance imaging, in the absence of new or suspicious symptoms, physical findings, or change in laboratory results, is unlikely to benefit patients, may add to the patient’s stress, may cause long-term health problems, and incurs substantial economic cost.
Dr. James O. Armitage and Dr. Julie M. Vose are both at the University of Nebraska, Omaha. Dr. Armitage disclosed a leadership role with Tesaro and consulting or advisory roles with GlaxoSmithKline, Roche, Spectrum Pharmaceuticals, ZIOPHARM Oncology, Conatus, and Celgene. Dr. Vose reported honoraria from Sanofi-Aventis and Seattle Genetics; consulting or advisory roles with Bioconnections; and institutional research funding from Spectrum Pharmaceuticals, Bristol-Myers Squibb, Celgene, Genentech, GlaxoSmithKline, Incyte, Janssen Biotech, Pharmacyclics, Acerta, and Kite Pharma. These remarks were adapted from their accompanying editorial (J Clin Oncol. 2015 Oct 5, doi:10.1200/jco.2015.63.5946).
The best way to determine the effectiveness of surveillance imaging would be a randomized trial including patients with diffuse large B-cell lymphoma (DLBCL) after first complete remission, but it is unlikely that such a study will be done. The study by El-Galaly et al may be the next best approach. Taking advantage of the fact that neighboring countries Denmark and Sweden have opposite policies for surveillance imaging but otherwise similar follow-up visit schedules and testing, the authors identified factors that predicted relapse (e.g., age greater than 60 years and elevated LDH), and they found that routine surveillance imaging had no impact on outcome. The study presents the strongest argument yet published against routine surveillance imaging.
The two other outstanding issues of routine surveillance are long-term safety and cost benefit. The study by El-Galaly et al, in combination with several other reports, suggests that routine surveillance imaging, in the absence of new or suspicious symptoms, physical findings, or change in laboratory results, is unlikely to benefit patients, may add to the patient’s stress, may cause long-term health problems, and incurs substantial economic cost.
Dr. James O. Armitage and Dr. Julie M. Vose are both at the University of Nebraska, Omaha. Dr. Armitage disclosed a leadership role with Tesaro and consulting or advisory roles with GlaxoSmithKline, Roche, Spectrum Pharmaceuticals, ZIOPHARM Oncology, Conatus, and Celgene. Dr. Vose reported honoraria from Sanofi-Aventis and Seattle Genetics; consulting or advisory roles with Bioconnections; and institutional research funding from Spectrum Pharmaceuticals, Bristol-Myers Squibb, Celgene, Genentech, GlaxoSmithKline, Incyte, Janssen Biotech, Pharmacyclics, Acerta, and Kite Pharma. These remarks were adapted from their accompanying editorial (J Clin Oncol. 2015 Oct 5, doi:10.1200/jco.2015.63.5946).
A population-based comparison of patients with diffuse large B-cell lymphoma (DLBCL) in first complete remission indicated that routine imaging surveillance did not improve outcomes, researchers reported.
Overall survival was similar for Danish and Swedish populations who received similar follow-up care, except that routine imaging surveillance is the standard of care in Denmark, but not in Sweden. The 3-year overall survival for Danish and Swedish patients was 92% and 91%, respectively.
Outcomes grouped by international prognostic index (IPI) also showed no significant differences between populations (J Clin Oncol. 2015 Oct 5, doi:10.1200/jco.2015.62.0229.).
“An imaging-based follow-up strategy does not improve postremission [overall survival] for DLBCL,” wrote Dr. Tarec Christoffer El-Galaly, of Aalborg University Hospital, Denmark, and colleagues.
They observed that aside from using IPI as risk stratification, the study “also points to baseline [lactate dehyrogenase] as a single discriminator of patients with high versus low risk of progression,” (Hazard ratio, 3.12; 95% CI, 1.78-5.48; P less than .01).
The retrospective study examined records of patients with DLBCL from Sweden (n=696) and Denmark (n=525) who achieved first complete remission after first-line therapy with R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) and CHOP-like regimens from 2007 to 2012. The proportion of patients with IPI greater than two were similar for both groups, though more Danish patients received radiotherapy compared with their Swedish counterparts (35% v. 9%).
Standard follow-up care after first complete remission is similar in Denmark and Sweden and typically includes symptom assessment, clinical examination, and blood tests at 3- to 4-month intervals for 2 years, and 6-month intervals in the third year. After 3 years, Swedish patients are seen annually for 2 years and then follow-up is ended for most patients. In Denmark, 6-month checks are continued until 5 years and then follow-up is usually ended. However, in Denmark guidelines support routine computerized tomography (CT) scans of the neck, abdomen, and thorax every 6 months for 2 years, which is not encouraged by guidelines in Sweden.
Early relapse detection aims to improve survival, and although low disease burden is associated with durable survival in patients treated for relapsed DLBCL, most studies show similar outcomes for imaging versus non-imaging detection. Additionally, previous retrospective studies that have reported survival differences based on relapse detection method are prone to lead-time bias, according to the researchers.
Given that a majority of patients with recurrent DLBCL experience symptoms before relapse, that elevated lactate dehyrogenase or abnormal physical examination may raise suspicion, and that exposure to ionizing radiation from medical imaging can lead to radiation-induced cancers, “routine imaging for DLBCL in first [complete remission] is not recommended,” the authors wrote.
The research was supported in part by the North Denmark Region. Dr. El-Galaly and coauthors reported having no financial disclosures.
A population-based comparison of patients with diffuse large B-cell lymphoma (DLBCL) in first complete remission indicated that routine imaging surveillance did not improve outcomes, researchers reported.
Overall survival was similar for Danish and Swedish populations who received similar follow-up care, except that routine imaging surveillance is the standard of care in Denmark, but not in Sweden. The 3-year overall survival for Danish and Swedish patients was 92% and 91%, respectively.
Outcomes grouped by international prognostic index (IPI) also showed no significant differences between populations (J Clin Oncol. 2015 Oct 5, doi:10.1200/jco.2015.62.0229.).
“An imaging-based follow-up strategy does not improve postremission [overall survival] for DLBCL,” wrote Dr. Tarec Christoffer El-Galaly, of Aalborg University Hospital, Denmark, and colleagues.
They observed that aside from using IPI as risk stratification, the study “also points to baseline [lactate dehyrogenase] as a single discriminator of patients with high versus low risk of progression,” (Hazard ratio, 3.12; 95% CI, 1.78-5.48; P less than .01).
The retrospective study examined records of patients with DLBCL from Sweden (n=696) and Denmark (n=525) who achieved first complete remission after first-line therapy with R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) and CHOP-like regimens from 2007 to 2012. The proportion of patients with IPI greater than two were similar for both groups, though more Danish patients received radiotherapy compared with their Swedish counterparts (35% v. 9%).
Standard follow-up care after first complete remission is similar in Denmark and Sweden and typically includes symptom assessment, clinical examination, and blood tests at 3- to 4-month intervals for 2 years, and 6-month intervals in the third year. After 3 years, Swedish patients are seen annually for 2 years and then follow-up is ended for most patients. In Denmark, 6-month checks are continued until 5 years and then follow-up is usually ended. However, in Denmark guidelines support routine computerized tomography (CT) scans of the neck, abdomen, and thorax every 6 months for 2 years, which is not encouraged by guidelines in Sweden.
Early relapse detection aims to improve survival, and although low disease burden is associated with durable survival in patients treated for relapsed DLBCL, most studies show similar outcomes for imaging versus non-imaging detection. Additionally, previous retrospective studies that have reported survival differences based on relapse detection method are prone to lead-time bias, according to the researchers.
Given that a majority of patients with recurrent DLBCL experience symptoms before relapse, that elevated lactate dehyrogenase or abnormal physical examination may raise suspicion, and that exposure to ionizing radiation from medical imaging can lead to radiation-induced cancers, “routine imaging for DLBCL in first [complete remission] is not recommended,” the authors wrote.
The research was supported in part by the North Denmark Region. Dr. El-Galaly and coauthors reported having no financial disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:Danish patients with diffuse large B-cell lymphoma (DLBCL) who received routine imaging during follow up had similar survival to Swedish patients who did not undergo routine imaging surveillance.
Major finding: After first complete remission, the 3-year overall survival for Danish and Swedish patients was 92% and 91%, respectively.
Data source: Population-based study of 525 Danish patients and 696 Swedish patients with DLBCL who achieved first complete remission after R-CHOP/CHOP-like first-line therapies from 2007 to 2012.
Disclosures: The research was supported in part by the North Denmark Region. Dr. El-Galaly and coauthors reported having no financial disclosures.
How B-cell lymphoma evades NK cells

Image by Joshua Strokes
Researchers say they have determined how lymphoma cells evade natural killer (NK) cells, and this discovery has revealed potential solutions to the problem.
The team found that NK-cell activation and a second, “triggering” event are both necessary for NK cells to exhibit cytotoxicity in the presence of B-cell lymphoma.
Previous research demonstrated this 2-step process in vitro. Now, researchers have shown that it occurs in vivo.
Dr Ralph Mocikat, of Helmholtz Zentrum München in Munich, Germany, and his colleagues described this research in the European Journal of Immunology.
The team conducted experiments using transplantable tumors, a λ-myc-transgenic model of endogenously arising lymphoma that mimics human Burkitt lymphoma, and mice deficient in the NK group 2 D (NKG2D) receptor.
The experiments showed that NK cells could eliminate lymphoma cells after receiving 2 signals. The first was NK-cell activation, which gave rise to IFN-γ expression.
The researchers found that NK cells could be activated in the presence of MHC class Ilow tumor cells or by injecting bone marrow-derived dendritic cells. Previous research had shown that interleukin 2 (IL-2) and IL-15 could activate NK cells.
The second step involved the NKG2D receptor and its ligands. NKG2D ligands are located on the surface of tumor cells and bind to NK cells. The researchers found that, if these ligands are down-regulated, the NK cells cannot carry out cytotoxic activity.
However, the team found they could increase NKG2D ligand levels. They introduced bortezomib to the tumor cell line 291 and saw a roughly 4-fold increase in NKG2D ligand levels.
“Our results show that the transfer of NK cells is a possible strategic option to treat B-cell lymphoma,” Dr Mocikat said. “According to our findings, this therapeutic approach can be optimized when transferred NK cells are already activated in vitro prior to their injection, thus bypassing the missing activation potential in the tumor microenvironment. An additional injection of IFN-γ or of antibodies against IL-10 could further support the immune activity.” ![]()

Image by Joshua Strokes
Researchers say they have determined how lymphoma cells evade natural killer (NK) cells, and this discovery has revealed potential solutions to the problem.
The team found that NK-cell activation and a second, “triggering” event are both necessary for NK cells to exhibit cytotoxicity in the presence of B-cell lymphoma.
Previous research demonstrated this 2-step process in vitro. Now, researchers have shown that it occurs in vivo.
Dr Ralph Mocikat, of Helmholtz Zentrum München in Munich, Germany, and his colleagues described this research in the European Journal of Immunology.
The team conducted experiments using transplantable tumors, a λ-myc-transgenic model of endogenously arising lymphoma that mimics human Burkitt lymphoma, and mice deficient in the NK group 2 D (NKG2D) receptor.
The experiments showed that NK cells could eliminate lymphoma cells after receiving 2 signals. The first was NK-cell activation, which gave rise to IFN-γ expression.
The researchers found that NK cells could be activated in the presence of MHC class Ilow tumor cells or by injecting bone marrow-derived dendritic cells. Previous research had shown that interleukin 2 (IL-2) and IL-15 could activate NK cells.
The second step involved the NKG2D receptor and its ligands. NKG2D ligands are located on the surface of tumor cells and bind to NK cells. The researchers found that, if these ligands are down-regulated, the NK cells cannot carry out cytotoxic activity.
However, the team found they could increase NKG2D ligand levels. They introduced bortezomib to the tumor cell line 291 and saw a roughly 4-fold increase in NKG2D ligand levels.
“Our results show that the transfer of NK cells is a possible strategic option to treat B-cell lymphoma,” Dr Mocikat said. “According to our findings, this therapeutic approach can be optimized when transferred NK cells are already activated in vitro prior to their injection, thus bypassing the missing activation potential in the tumor microenvironment. An additional injection of IFN-γ or of antibodies against IL-10 could further support the immune activity.” ![]()

Image by Joshua Strokes
Researchers say they have determined how lymphoma cells evade natural killer (NK) cells, and this discovery has revealed potential solutions to the problem.
The team found that NK-cell activation and a second, “triggering” event are both necessary for NK cells to exhibit cytotoxicity in the presence of B-cell lymphoma.
Previous research demonstrated this 2-step process in vitro. Now, researchers have shown that it occurs in vivo.
Dr Ralph Mocikat, of Helmholtz Zentrum München in Munich, Germany, and his colleagues described this research in the European Journal of Immunology.
The team conducted experiments using transplantable tumors, a λ-myc-transgenic model of endogenously arising lymphoma that mimics human Burkitt lymphoma, and mice deficient in the NK group 2 D (NKG2D) receptor.
The experiments showed that NK cells could eliminate lymphoma cells after receiving 2 signals. The first was NK-cell activation, which gave rise to IFN-γ expression.
The researchers found that NK cells could be activated in the presence of MHC class Ilow tumor cells or by injecting bone marrow-derived dendritic cells. Previous research had shown that interleukin 2 (IL-2) and IL-15 could activate NK cells.
The second step involved the NKG2D receptor and its ligands. NKG2D ligands are located on the surface of tumor cells and bind to NK cells. The researchers found that, if these ligands are down-regulated, the NK cells cannot carry out cytotoxic activity.
However, the team found they could increase NKG2D ligand levels. They introduced bortezomib to the tumor cell line 291 and saw a roughly 4-fold increase in NKG2D ligand levels.
“Our results show that the transfer of NK cells is a possible strategic option to treat B-cell lymphoma,” Dr Mocikat said. “According to our findings, this therapeutic approach can be optimized when transferred NK cells are already activated in vitro prior to their injection, thus bypassing the missing activation potential in the tumor microenvironment. An additional injection of IFN-γ or of antibodies against IL-10 could further support the immune activity.” ![]()