User login
Prior maternal gastric bypass surgery tied to fewer birth defects
according to data from a cohort study of 2,921 women with a history of gastric bypass surgery and 30,573 matched controls.
“Obesity is associated with poor glucose control, which is teratogenic. Bariatric surgery results in weight loss and glucose normalization but is also associated with nutritional deficiencies and substance abuse, which could cause birth defects as hypothesized based on case series,” wrote Martin Neovius, PhD, of Karolinska Institutet, Stockholm, Sweden, and colleagues.
To determine the risk of birth defects for infants born to women after gastric bypass surgery, the researchers used the Swedish Medical Birth Register to identify singleton infants born between 2007 and 2014 to women who underwent Roux-en-Y gastric bypass surgery and matched controls. The findings were published in a research letter in JAMA.
In the surgery group, the mean interval from surgery to conception was 1.6 years, and the mean weight loss was 40 kg for these women. In addition, the use of diabetes drugs decreased from 10% before surgery to 2% during the 6 months before conception.
Overall, major birth defects occurred in 3% of infants in the gastric bypass groups versus 5% of infants in the control group (risk ratio, 0.67). No neural tube defects occurred in the surgery group and 20 cases of neural tube defects were noted in the control group.
The study was limited by several factors including the lack of data on pregnancy termination, exclusion of stillbirths, and inability to analyze individual birth defects because of small numbers, the researchers noted.
Nonetheless, the results suggest that “a mechanism could be that surgery-induced improvements in glucose metabolism, and potentially other beneficial physiologic changes, led to a reduction of major birth defect risk to a level similar to that of the general population,” they said.
Dr. Neovius disclosed advisory board fees from Itrim and Ethicon Johnson & Johnson. Three coauthors reported grants or other fees from a variety of pharmaceutical companies. The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health, by the Swedish Research Council, and by the Swedish Research Council for Health, Working Life, and Welfare.
SOURCE: Neovius M et al. JAMA. 2019 Oct 15; 322:1515-17.
according to data from a cohort study of 2,921 women with a history of gastric bypass surgery and 30,573 matched controls.
“Obesity is associated with poor glucose control, which is teratogenic. Bariatric surgery results in weight loss and glucose normalization but is also associated with nutritional deficiencies and substance abuse, which could cause birth defects as hypothesized based on case series,” wrote Martin Neovius, PhD, of Karolinska Institutet, Stockholm, Sweden, and colleagues.
To determine the risk of birth defects for infants born to women after gastric bypass surgery, the researchers used the Swedish Medical Birth Register to identify singleton infants born between 2007 and 2014 to women who underwent Roux-en-Y gastric bypass surgery and matched controls. The findings were published in a research letter in JAMA.
In the surgery group, the mean interval from surgery to conception was 1.6 years, and the mean weight loss was 40 kg for these women. In addition, the use of diabetes drugs decreased from 10% before surgery to 2% during the 6 months before conception.
Overall, major birth defects occurred in 3% of infants in the gastric bypass groups versus 5% of infants in the control group (risk ratio, 0.67). No neural tube defects occurred in the surgery group and 20 cases of neural tube defects were noted in the control group.
The study was limited by several factors including the lack of data on pregnancy termination, exclusion of stillbirths, and inability to analyze individual birth defects because of small numbers, the researchers noted.
Nonetheless, the results suggest that “a mechanism could be that surgery-induced improvements in glucose metabolism, and potentially other beneficial physiologic changes, led to a reduction of major birth defect risk to a level similar to that of the general population,” they said.
Dr. Neovius disclosed advisory board fees from Itrim and Ethicon Johnson & Johnson. Three coauthors reported grants or other fees from a variety of pharmaceutical companies. The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health, by the Swedish Research Council, and by the Swedish Research Council for Health, Working Life, and Welfare.
SOURCE: Neovius M et al. JAMA. 2019 Oct 15; 322:1515-17.
according to data from a cohort study of 2,921 women with a history of gastric bypass surgery and 30,573 matched controls.
“Obesity is associated with poor glucose control, which is teratogenic. Bariatric surgery results in weight loss and glucose normalization but is also associated with nutritional deficiencies and substance abuse, which could cause birth defects as hypothesized based on case series,” wrote Martin Neovius, PhD, of Karolinska Institutet, Stockholm, Sweden, and colleagues.
To determine the risk of birth defects for infants born to women after gastric bypass surgery, the researchers used the Swedish Medical Birth Register to identify singleton infants born between 2007 and 2014 to women who underwent Roux-en-Y gastric bypass surgery and matched controls. The findings were published in a research letter in JAMA.
In the surgery group, the mean interval from surgery to conception was 1.6 years, and the mean weight loss was 40 kg for these women. In addition, the use of diabetes drugs decreased from 10% before surgery to 2% during the 6 months before conception.
Overall, major birth defects occurred in 3% of infants in the gastric bypass groups versus 5% of infants in the control group (risk ratio, 0.67). No neural tube defects occurred in the surgery group and 20 cases of neural tube defects were noted in the control group.
The study was limited by several factors including the lack of data on pregnancy termination, exclusion of stillbirths, and inability to analyze individual birth defects because of small numbers, the researchers noted.
Nonetheless, the results suggest that “a mechanism could be that surgery-induced improvements in glucose metabolism, and potentially other beneficial physiologic changes, led to a reduction of major birth defect risk to a level similar to that of the general population,” they said.
Dr. Neovius disclosed advisory board fees from Itrim and Ethicon Johnson & Johnson. Three coauthors reported grants or other fees from a variety of pharmaceutical companies. The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health, by the Swedish Research Council, and by the Swedish Research Council for Health, Working Life, and Welfare.
SOURCE: Neovius M et al. JAMA. 2019 Oct 15; 322:1515-17.
FROM JAMA
Key clinical point: Infants whose mothers previously underwent gastric bypass surgery had a lower risk of birth defects than did the infants of matched controls.
Major finding: Major birth defects occurred in 3% of infants whose mothers had gastric bypass surgery, compared with 5% of infants born to control women.
Study details: The data come from a cohort study of 2,921 women with history of gastric bypass surgery and 30,573 matched controls.
Disclosures: Dr. Neovius disclosed advisory board fees from Itrim and Ethicon Johnson & Johnson. Three coauthors reported grants or other fees from a variety of pharmaceutical companies. The study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health, by the Swedish Research Council, and by the Swedish Research Council for Health, Working Life, and Welfare.
Source: Neovius M et al. JAMA. 2019 Oct 15; 322:1515-17.
Weight loss surgery linked to lower CV event risk in diabetes
, compared with nonsurgical management, according to data presented at the annual congress of the European Society of Cardiology.
The retrospective cohort study, simultaneously published in JAMA, looked at outcomes in 13,722 individuals with type 2 diabetes and obesity, 2,287 of whom underwent metabolic surgery and the rest of the matched cohort receiving usual care.
At 8 years of follow-up, the cumulative incidence of the primary endpoint – a composite of first occurrence of all-cause mortality, coronary artery events, cerebrovascular events, heart failure, nephropathy, and atrial fibrillation – was 30.8% in the weight loss–surgery group and 47.7% in the nonsurgical-control group, representing a 39% lower risk with weight loss surgery (P less than .001).
The analysis failed to find any interaction with sex, age, body mass index (BMI), HbA1c level, estimated glomerular filtration rate, or use of insulin, sulfonylureas, or lipid-lowering medications.
Metabolic surgery was also associated with a significantly lower cumulative incidence of myocardial infarction, ischemic stroke and mortality than usual care (17% vs. 27.6%).
In particular, researchers saw a significant 41% reduction in the risk of death at eight years in the surgical group compared to usual care (10% vs. 17.8%), a 62% reduction in the risk of heart failure, a 31% reduction in the risk of coronary artery disease, and a 60% reduction in nephropathy risk. Metabolic surgery was also associated with a 33% reduction in cerebrovascular disease risk, and a 22% lower risk of atrial fibrillation.
In the group that underwent metabolic surgery, mean bodyweight at 8 years was reduced by 29.1 kg, compared with 8.7 kg in the control group. At baseline, 75% of the metabolic surgery group had a BMI of 40 kg/m2 or above, 20% had a BMI between 35-39.9, and 5% had a BMI between 30-34.9.
The surgery was also associated with significantly greater reductions in HbA1c, and in the use of noninsulin diabetes medications, insulin, antihypertensive medications, lipid-lowering therapies, and aspirin.
The most common surgical weight loss procedure was Roux-en-Y gastric bypass (63%), followed by sleeve gastrectomy (32%), and adjustable gastric banding (5%). Five patients underwent duodenal switch.
In the 90 days after surgery, 3% of patients experienced bleeding that required transfusion, 2.5% experienced pulmonary adverse events, 1% experienced venous thromboembolism, 0.7% experienced cardiac events, and 0.2% experienced renal failure that required dialysis. There were also 15 deaths (0.7%) in the surgical group, and 4.8% of patients required abdominal surgical intervention.
“We speculate that the lower rate of [major adverse cardiovascular events] after metabolic surgery observed in this study may be related to substantial and sustained weight loss with subsequent improvement in metabolic, structural, hemodynamic, and neurohormonal abnormalities,” wrote Ali Aminian, MD, of the Bariatric and Metabolic Institute at the Cleveland Clinic, and coauthors.
“Although large and sustained surgically induced weight loss has profound physiologic effects, a growing body of evidence indicates that some of the beneficial metabolic and neurohormonal changes that occur after metabolic surgical procedures are related to anatomical changes in the gastrointestinal tract that are partially independent of weight loss,” they wrote.
The authors, however, were also keen to point out that their study was observational, and should therefore be considered “hypothesis generating.” While the two study groups were matched on 37 baseline covariates, those in the surgical group did have a higher body weight, higher BMI, higher rates of dyslipidemia, and higher rates of hypertension.
“The findings from this observational study must be confirmed in randomized clinical trials,” they noted.
The study was partly funded by Medtronic, and one author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Five authors declared funding and support from private industry, including from Medtronic, and one author declared institutional grants.
SOURCE: Aminian A et al. JAMA 2019, Sept 2. DOI: 10.1001/jama.2019.14231.
Despite a focus on reducing macrovascular events in individuals with type 2 diabetes, none of the major randomized controlled trials of glucose-lowering interventions that support current treatment guidelines have achieved this outcome. This study of bariatric surgery in obese patients with diabetes, however, does show reductions in major adverse cardiovascular events, although these outcomes should be interpreted with caution because of their observational nature and imprecise matching of the study groups.
Despite this, the many known benefits associated with bariatric surgery–induced weight loss suggest that for carefully selected, motivated patients with obesity and type 2 diabetes – who have been unable to lose weight by other means – this could be the preferred treatment option.
Dr. Edward H. Livingston is the deputy editor of JAMA and with the department of surgery at the University of California, Los Angeles. These comments are adapted from an accompanying editorial (JAMA 2019, Sept 2. DOI:10.1001/jama.2019.14577). No conflicts of interest were declared.
Despite a focus on reducing macrovascular events in individuals with type 2 diabetes, none of the major randomized controlled trials of glucose-lowering interventions that support current treatment guidelines have achieved this outcome. This study of bariatric surgery in obese patients with diabetes, however, does show reductions in major adverse cardiovascular events, although these outcomes should be interpreted with caution because of their observational nature and imprecise matching of the study groups.
Despite this, the many known benefits associated with bariatric surgery–induced weight loss suggest that for carefully selected, motivated patients with obesity and type 2 diabetes – who have been unable to lose weight by other means – this could be the preferred treatment option.
Dr. Edward H. Livingston is the deputy editor of JAMA and with the department of surgery at the University of California, Los Angeles. These comments are adapted from an accompanying editorial (JAMA 2019, Sept 2. DOI:10.1001/jama.2019.14577). No conflicts of interest were declared.
Despite a focus on reducing macrovascular events in individuals with type 2 diabetes, none of the major randomized controlled trials of glucose-lowering interventions that support current treatment guidelines have achieved this outcome. This study of bariatric surgery in obese patients with diabetes, however, does show reductions in major adverse cardiovascular events, although these outcomes should be interpreted with caution because of their observational nature and imprecise matching of the study groups.
Despite this, the many known benefits associated with bariatric surgery–induced weight loss suggest that for carefully selected, motivated patients with obesity and type 2 diabetes – who have been unable to lose weight by other means – this could be the preferred treatment option.
Dr. Edward H. Livingston is the deputy editor of JAMA and with the department of surgery at the University of California, Los Angeles. These comments are adapted from an accompanying editorial (JAMA 2019, Sept 2. DOI:10.1001/jama.2019.14577). No conflicts of interest were declared.
, compared with nonsurgical management, according to data presented at the annual congress of the European Society of Cardiology.
The retrospective cohort study, simultaneously published in JAMA, looked at outcomes in 13,722 individuals with type 2 diabetes and obesity, 2,287 of whom underwent metabolic surgery and the rest of the matched cohort receiving usual care.
At 8 years of follow-up, the cumulative incidence of the primary endpoint – a composite of first occurrence of all-cause mortality, coronary artery events, cerebrovascular events, heart failure, nephropathy, and atrial fibrillation – was 30.8% in the weight loss–surgery group and 47.7% in the nonsurgical-control group, representing a 39% lower risk with weight loss surgery (P less than .001).
The analysis failed to find any interaction with sex, age, body mass index (BMI), HbA1c level, estimated glomerular filtration rate, or use of insulin, sulfonylureas, or lipid-lowering medications.
Metabolic surgery was also associated with a significantly lower cumulative incidence of myocardial infarction, ischemic stroke and mortality than usual care (17% vs. 27.6%).
In particular, researchers saw a significant 41% reduction in the risk of death at eight years in the surgical group compared to usual care (10% vs. 17.8%), a 62% reduction in the risk of heart failure, a 31% reduction in the risk of coronary artery disease, and a 60% reduction in nephropathy risk. Metabolic surgery was also associated with a 33% reduction in cerebrovascular disease risk, and a 22% lower risk of atrial fibrillation.
In the group that underwent metabolic surgery, mean bodyweight at 8 years was reduced by 29.1 kg, compared with 8.7 kg in the control group. At baseline, 75% of the metabolic surgery group had a BMI of 40 kg/m2 or above, 20% had a BMI between 35-39.9, and 5% had a BMI between 30-34.9.
The surgery was also associated with significantly greater reductions in HbA1c, and in the use of noninsulin diabetes medications, insulin, antihypertensive medications, lipid-lowering therapies, and aspirin.
The most common surgical weight loss procedure was Roux-en-Y gastric bypass (63%), followed by sleeve gastrectomy (32%), and adjustable gastric banding (5%). Five patients underwent duodenal switch.
In the 90 days after surgery, 3% of patients experienced bleeding that required transfusion, 2.5% experienced pulmonary adverse events, 1% experienced venous thromboembolism, 0.7% experienced cardiac events, and 0.2% experienced renal failure that required dialysis. There were also 15 deaths (0.7%) in the surgical group, and 4.8% of patients required abdominal surgical intervention.
“We speculate that the lower rate of [major adverse cardiovascular events] after metabolic surgery observed in this study may be related to substantial and sustained weight loss with subsequent improvement in metabolic, structural, hemodynamic, and neurohormonal abnormalities,” wrote Ali Aminian, MD, of the Bariatric and Metabolic Institute at the Cleveland Clinic, and coauthors.
“Although large and sustained surgically induced weight loss has profound physiologic effects, a growing body of evidence indicates that some of the beneficial metabolic and neurohormonal changes that occur after metabolic surgical procedures are related to anatomical changes in the gastrointestinal tract that are partially independent of weight loss,” they wrote.
The authors, however, were also keen to point out that their study was observational, and should therefore be considered “hypothesis generating.” While the two study groups were matched on 37 baseline covariates, those in the surgical group did have a higher body weight, higher BMI, higher rates of dyslipidemia, and higher rates of hypertension.
“The findings from this observational study must be confirmed in randomized clinical trials,” they noted.
The study was partly funded by Medtronic, and one author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Five authors declared funding and support from private industry, including from Medtronic, and one author declared institutional grants.
SOURCE: Aminian A et al. JAMA 2019, Sept 2. DOI: 10.1001/jama.2019.14231.
, compared with nonsurgical management, according to data presented at the annual congress of the European Society of Cardiology.
The retrospective cohort study, simultaneously published in JAMA, looked at outcomes in 13,722 individuals with type 2 diabetes and obesity, 2,287 of whom underwent metabolic surgery and the rest of the matched cohort receiving usual care.
At 8 years of follow-up, the cumulative incidence of the primary endpoint – a composite of first occurrence of all-cause mortality, coronary artery events, cerebrovascular events, heart failure, nephropathy, and atrial fibrillation – was 30.8% in the weight loss–surgery group and 47.7% in the nonsurgical-control group, representing a 39% lower risk with weight loss surgery (P less than .001).
The analysis failed to find any interaction with sex, age, body mass index (BMI), HbA1c level, estimated glomerular filtration rate, or use of insulin, sulfonylureas, or lipid-lowering medications.
Metabolic surgery was also associated with a significantly lower cumulative incidence of myocardial infarction, ischemic stroke and mortality than usual care (17% vs. 27.6%).
In particular, researchers saw a significant 41% reduction in the risk of death at eight years in the surgical group compared to usual care (10% vs. 17.8%), a 62% reduction in the risk of heart failure, a 31% reduction in the risk of coronary artery disease, and a 60% reduction in nephropathy risk. Metabolic surgery was also associated with a 33% reduction in cerebrovascular disease risk, and a 22% lower risk of atrial fibrillation.
In the group that underwent metabolic surgery, mean bodyweight at 8 years was reduced by 29.1 kg, compared with 8.7 kg in the control group. At baseline, 75% of the metabolic surgery group had a BMI of 40 kg/m2 or above, 20% had a BMI between 35-39.9, and 5% had a BMI between 30-34.9.
The surgery was also associated with significantly greater reductions in HbA1c, and in the use of noninsulin diabetes medications, insulin, antihypertensive medications, lipid-lowering therapies, and aspirin.
The most common surgical weight loss procedure was Roux-en-Y gastric bypass (63%), followed by sleeve gastrectomy (32%), and adjustable gastric banding (5%). Five patients underwent duodenal switch.
In the 90 days after surgery, 3% of patients experienced bleeding that required transfusion, 2.5% experienced pulmonary adverse events, 1% experienced venous thromboembolism, 0.7% experienced cardiac events, and 0.2% experienced renal failure that required dialysis. There were also 15 deaths (0.7%) in the surgical group, and 4.8% of patients required abdominal surgical intervention.
“We speculate that the lower rate of [major adverse cardiovascular events] after metabolic surgery observed in this study may be related to substantial and sustained weight loss with subsequent improvement in metabolic, structural, hemodynamic, and neurohormonal abnormalities,” wrote Ali Aminian, MD, of the Bariatric and Metabolic Institute at the Cleveland Clinic, and coauthors.
“Although large and sustained surgically induced weight loss has profound physiologic effects, a growing body of evidence indicates that some of the beneficial metabolic and neurohormonal changes that occur after metabolic surgical procedures are related to anatomical changes in the gastrointestinal tract that are partially independent of weight loss,” they wrote.
The authors, however, were also keen to point out that their study was observational, and should therefore be considered “hypothesis generating.” While the two study groups were matched on 37 baseline covariates, those in the surgical group did have a higher body weight, higher BMI, higher rates of dyslipidemia, and higher rates of hypertension.
“The findings from this observational study must be confirmed in randomized clinical trials,” they noted.
The study was partly funded by Medtronic, and one author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Five authors declared funding and support from private industry, including from Medtronic, and one author declared institutional grants.
SOURCE: Aminian A et al. JAMA 2019, Sept 2. DOI: 10.1001/jama.2019.14231.
AT THE ESC CONGRESS 2019
Key clinical point: Bariatric surgery may reduce the risk of cardiovascular events in people with type 2 diabetes.
Major finding: Bariatric surgery is associated with a 39% reduction in risk of major cardiovascular events.
Study details: Retrospective cohort study in 13,722 individuals with type 2 diabetes and obesity.
Disclosures: The study was partly funded by Medtronic, and one author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Five authors declared funding and support from private industry, including from Medtronic, and one author declared institutional grants.
Source: Aminian A et al. JAMA 2019, September 2. DOI: 10.1001/jama.2019.14231.
Adding drugs to gastric balloons increases weight loss
SAN DIEGO – In a multicenter study involving four academic medical centers, the addition of weight loss drugs to intragastric balloons resulted in better weight loss 12 months after balloon placement.
In a video interview at the annual Digestive Disease Week, study investigator Reem Sharaiha, MD, explained that one of the drawbacks of intragastric balloons is that, although they produce weight loss for the 6 or 12 months that they are in place, patients tend to regain that weight after they are removed. The study, involving 111 patients, was designed to determine whether the addition of weight loss drugs could mitigate this effect and improve weight loss, said Dr. Sharaiha of Weill Cornell Medical Center, New York.
Adding drugs such as metformin or weight loss drugs tailored to patients’ particular weight issues (cravings, anxiety, or fast gastric emptying) at the 3- or 6-month mark while the intragastric balloon was in place helped patients continue losing weight after balloon removal. At 12 months, the percentage of total body weight lost was significantly greater in the intragastric balloon group with concurrent pharmacotherapy (21.4% vs. 13.1%).
SOURCE: Shah SL et al. DDW 2019, Abstract 1105.
SAN DIEGO – In a multicenter study involving four academic medical centers, the addition of weight loss drugs to intragastric balloons resulted in better weight loss 12 months after balloon placement.
In a video interview at the annual Digestive Disease Week, study investigator Reem Sharaiha, MD, explained that one of the drawbacks of intragastric balloons is that, although they produce weight loss for the 6 or 12 months that they are in place, patients tend to regain that weight after they are removed. The study, involving 111 patients, was designed to determine whether the addition of weight loss drugs could mitigate this effect and improve weight loss, said Dr. Sharaiha of Weill Cornell Medical Center, New York.
Adding drugs such as metformin or weight loss drugs tailored to patients’ particular weight issues (cravings, anxiety, or fast gastric emptying) at the 3- or 6-month mark while the intragastric balloon was in place helped patients continue losing weight after balloon removal. At 12 months, the percentage of total body weight lost was significantly greater in the intragastric balloon group with concurrent pharmacotherapy (21.4% vs. 13.1%).
SOURCE: Shah SL et al. DDW 2019, Abstract 1105.
SAN DIEGO – In a multicenter study involving four academic medical centers, the addition of weight loss drugs to intragastric balloons resulted in better weight loss 12 months after balloon placement.
In a video interview at the annual Digestive Disease Week, study investigator Reem Sharaiha, MD, explained that one of the drawbacks of intragastric balloons is that, although they produce weight loss for the 6 or 12 months that they are in place, patients tend to regain that weight after they are removed. The study, involving 111 patients, was designed to determine whether the addition of weight loss drugs could mitigate this effect and improve weight loss, said Dr. Sharaiha of Weill Cornell Medical Center, New York.
Adding drugs such as metformin or weight loss drugs tailored to patients’ particular weight issues (cravings, anxiety, or fast gastric emptying) at the 3- or 6-month mark while the intragastric balloon was in place helped patients continue losing weight after balloon removal. At 12 months, the percentage of total body weight lost was significantly greater in the intragastric balloon group with concurrent pharmacotherapy (21.4% vs. 13.1%).
SOURCE: Shah SL et al. DDW 2019, Abstract 1105.
REPORTING FROM DDW 2019
Diabetes, hypertension remission more prevalent in adolescents than adults after gastric bypass
according to two related studies of 5-year outcomes after Roux-en-Y gastric bypass.
However, despite adolescents’ better outcomes for diabetes and hypertension, their rate of abdominal reoperations was significantly higher during the 5-year follow-up period, and at 2 years post surgery, they were found to have low ferritin levels. The rates of death were similar in the two groups at 5 years.
“We have documented similar and durable weight loss after gastric bypass in adolescents and adults, but important differences between these cohorts were observed in specific health outcomes,” wrote Thomas H. Inge, MD, PhD, of the University of Colorado at Denver, Aurora, and his coauthors. The study was published in the New England Journal of Medicine.
To evaluate and compare outcomes after bariatric surgery, the researchers undertook the Teen–Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study and the LABS study. The two were related but independent observational studies of postsurgery patient cohorts. The Teen-LABS study included 161 adolescents with severe obesity, and the LABS study included 396 adults who reported becoming obese during adolescence.
At 5-year follow-up, there was no significant difference in mean percentage weight change between adolescents (−26%; 95% confidence interval, −29 to −23) and adults (−29%; 95% CI, −31 to −27; P = .08). Adolescents were more likely than were adults to have remission of type 2 diabetes (86% vs. 53%, respectively; risk ratio, 1.27; 95% CI, 1.03 to 1.57; P = .03) as well as hypertension (68% vs. 41%; risk ratio, 1.51; 95% CI, 1.21 to 1.88; P less than .001).
In addition, 20% of adolescents and 16% of adults underwent intra-abdominal procedures within 5 years of surgery, with cholecystectomy being the most common, followed by surgery for bowel obstruction or hernia repair, and gastrostomy. At 2 years, ferritin levels were lower in adolescents than in adults (48% of patients vs. 29%, respectively). Five-year ferritin levels were not assessed.
In all, three adolescents (1.9%) and seven adults (1.8%) died over the 5-year period. Among the adolescents, one patient with type 1 diabetes died 3 years after surgery from complications after a hypoglycemic episode, and the other two deaths, both 4 years after surgery, were consistent with overdose. Among the adults, three of the deaths occurred within 3 weeks of surgery and were related to gastric bypass, two were of indeterminate cause (at 11 months and 5 years after surgery), one was by suicide at 3 years, and one was from colon cancer at 4 years.
The authors acknowledged the limitations of their study, including its observational design, low counts for some of the outcomes, and a lack of nonsurgical controls. They also noted potential unmeasured biases in the adult cohort, including the effects of weight cycling and inaccuracies in recalling adolescent weight issues.
The study and several of its authors were supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases. Several authors reported receiving grants, honoraria, and consulting fees from medical technology and pharmaceutical companies.
SOURCE: Inge TH et al. N Engl J Med. 2019 May 16. doi: 10.1056/NEJMoa1813909.
For obese adolescents, making a decision with lifelong consequences, as is the case with bariatric surgery, should still be handled on a case-by-case basis, according to Ted D. Adams, PhD, of the University of Utah, Salt Lake City.
In general, treatment approaches for children and adults differ because of their physiological and psychological differences, but that does not apply in the case of obesity, wrote Dr. Adams, who noted the similarities in obesity across age groups. In addition, he said, most adolescents who are obese remain obese into adulthood, and obese adults who were obese when they were younger face worse outcomes than do those who become obese in adulthood.
As such, this study from Dr. Inge and his colleagues is clinically important given the prevalence of obesity in the United States and a step in the right direction. However, Dr. Adams acknowledged concerns over certain elements, including the higher rate of abdominal reoperations in adolescents during the 5-year postsurgery period.
For now, a case-by-case basis remains his recommendation. “More complete data will be required to fully inform clinicians, parents, and adolescents whether to embark on surgical intervention or to postpone it,” he wrote, adding that “the 5-year data look promising but ... the lifetime outcome is unknown.”
These comments are adapted from an editorial (N Engl J Med. 2019 May 16. doi: 10.1056/NEJMe1905778 ). Dr. Adams reported receiving grants from the National Institute of Diabetes and Digestive and Kidney Diseases as well as the Intermountain Research Foundation and Ethicon Endo-Surgery, a subsidiary of Johnson & Johnson.
For obese adolescents, making a decision with lifelong consequences, as is the case with bariatric surgery, should still be handled on a case-by-case basis, according to Ted D. Adams, PhD, of the University of Utah, Salt Lake City.
In general, treatment approaches for children and adults differ because of their physiological and psychological differences, but that does not apply in the case of obesity, wrote Dr. Adams, who noted the similarities in obesity across age groups. In addition, he said, most adolescents who are obese remain obese into adulthood, and obese adults who were obese when they were younger face worse outcomes than do those who become obese in adulthood.
As such, this study from Dr. Inge and his colleagues is clinically important given the prevalence of obesity in the United States and a step in the right direction. However, Dr. Adams acknowledged concerns over certain elements, including the higher rate of abdominal reoperations in adolescents during the 5-year postsurgery period.
For now, a case-by-case basis remains his recommendation. “More complete data will be required to fully inform clinicians, parents, and adolescents whether to embark on surgical intervention or to postpone it,” he wrote, adding that “the 5-year data look promising but ... the lifetime outcome is unknown.”
These comments are adapted from an editorial (N Engl J Med. 2019 May 16. doi: 10.1056/NEJMe1905778 ). Dr. Adams reported receiving grants from the National Institute of Diabetes and Digestive and Kidney Diseases as well as the Intermountain Research Foundation and Ethicon Endo-Surgery, a subsidiary of Johnson & Johnson.
For obese adolescents, making a decision with lifelong consequences, as is the case with bariatric surgery, should still be handled on a case-by-case basis, according to Ted D. Adams, PhD, of the University of Utah, Salt Lake City.
In general, treatment approaches for children and adults differ because of their physiological and psychological differences, but that does not apply in the case of obesity, wrote Dr. Adams, who noted the similarities in obesity across age groups. In addition, he said, most adolescents who are obese remain obese into adulthood, and obese adults who were obese when they were younger face worse outcomes than do those who become obese in adulthood.
As such, this study from Dr. Inge and his colleagues is clinically important given the prevalence of obesity in the United States and a step in the right direction. However, Dr. Adams acknowledged concerns over certain elements, including the higher rate of abdominal reoperations in adolescents during the 5-year postsurgery period.
For now, a case-by-case basis remains his recommendation. “More complete data will be required to fully inform clinicians, parents, and adolescents whether to embark on surgical intervention or to postpone it,” he wrote, adding that “the 5-year data look promising but ... the lifetime outcome is unknown.”
These comments are adapted from an editorial (N Engl J Med. 2019 May 16. doi: 10.1056/NEJMe1905778 ). Dr. Adams reported receiving grants from the National Institute of Diabetes and Digestive and Kidney Diseases as well as the Intermountain Research Foundation and Ethicon Endo-Surgery, a subsidiary of Johnson & Johnson.
according to two related studies of 5-year outcomes after Roux-en-Y gastric bypass.
However, despite adolescents’ better outcomes for diabetes and hypertension, their rate of abdominal reoperations was significantly higher during the 5-year follow-up period, and at 2 years post surgery, they were found to have low ferritin levels. The rates of death were similar in the two groups at 5 years.
“We have documented similar and durable weight loss after gastric bypass in adolescents and adults, but important differences between these cohorts were observed in specific health outcomes,” wrote Thomas H. Inge, MD, PhD, of the University of Colorado at Denver, Aurora, and his coauthors. The study was published in the New England Journal of Medicine.
To evaluate and compare outcomes after bariatric surgery, the researchers undertook the Teen–Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study and the LABS study. The two were related but independent observational studies of postsurgery patient cohorts. The Teen-LABS study included 161 adolescents with severe obesity, and the LABS study included 396 adults who reported becoming obese during adolescence.
At 5-year follow-up, there was no significant difference in mean percentage weight change between adolescents (−26%; 95% confidence interval, −29 to −23) and adults (−29%; 95% CI, −31 to −27; P = .08). Adolescents were more likely than were adults to have remission of type 2 diabetes (86% vs. 53%, respectively; risk ratio, 1.27; 95% CI, 1.03 to 1.57; P = .03) as well as hypertension (68% vs. 41%; risk ratio, 1.51; 95% CI, 1.21 to 1.88; P less than .001).
In addition, 20% of adolescents and 16% of adults underwent intra-abdominal procedures within 5 years of surgery, with cholecystectomy being the most common, followed by surgery for bowel obstruction or hernia repair, and gastrostomy. At 2 years, ferritin levels were lower in adolescents than in adults (48% of patients vs. 29%, respectively). Five-year ferritin levels were not assessed.
In all, three adolescents (1.9%) and seven adults (1.8%) died over the 5-year period. Among the adolescents, one patient with type 1 diabetes died 3 years after surgery from complications after a hypoglycemic episode, and the other two deaths, both 4 years after surgery, were consistent with overdose. Among the adults, three of the deaths occurred within 3 weeks of surgery and were related to gastric bypass, two were of indeterminate cause (at 11 months and 5 years after surgery), one was by suicide at 3 years, and one was from colon cancer at 4 years.
The authors acknowledged the limitations of their study, including its observational design, low counts for some of the outcomes, and a lack of nonsurgical controls. They also noted potential unmeasured biases in the adult cohort, including the effects of weight cycling and inaccuracies in recalling adolescent weight issues.
The study and several of its authors were supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases. Several authors reported receiving grants, honoraria, and consulting fees from medical technology and pharmaceutical companies.
SOURCE: Inge TH et al. N Engl J Med. 2019 May 16. doi: 10.1056/NEJMoa1813909.
according to two related studies of 5-year outcomes after Roux-en-Y gastric bypass.
However, despite adolescents’ better outcomes for diabetes and hypertension, their rate of abdominal reoperations was significantly higher during the 5-year follow-up period, and at 2 years post surgery, they were found to have low ferritin levels. The rates of death were similar in the two groups at 5 years.
“We have documented similar and durable weight loss after gastric bypass in adolescents and adults, but important differences between these cohorts were observed in specific health outcomes,” wrote Thomas H. Inge, MD, PhD, of the University of Colorado at Denver, Aurora, and his coauthors. The study was published in the New England Journal of Medicine.
To evaluate and compare outcomes after bariatric surgery, the researchers undertook the Teen–Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study and the LABS study. The two were related but independent observational studies of postsurgery patient cohorts. The Teen-LABS study included 161 adolescents with severe obesity, and the LABS study included 396 adults who reported becoming obese during adolescence.
At 5-year follow-up, there was no significant difference in mean percentage weight change between adolescents (−26%; 95% confidence interval, −29 to −23) and adults (−29%; 95% CI, −31 to −27; P = .08). Adolescents were more likely than were adults to have remission of type 2 diabetes (86% vs. 53%, respectively; risk ratio, 1.27; 95% CI, 1.03 to 1.57; P = .03) as well as hypertension (68% vs. 41%; risk ratio, 1.51; 95% CI, 1.21 to 1.88; P less than .001).
In addition, 20% of adolescents and 16% of adults underwent intra-abdominal procedures within 5 years of surgery, with cholecystectomy being the most common, followed by surgery for bowel obstruction or hernia repair, and gastrostomy. At 2 years, ferritin levels were lower in adolescents than in adults (48% of patients vs. 29%, respectively). Five-year ferritin levels were not assessed.
In all, three adolescents (1.9%) and seven adults (1.8%) died over the 5-year period. Among the adolescents, one patient with type 1 diabetes died 3 years after surgery from complications after a hypoglycemic episode, and the other two deaths, both 4 years after surgery, were consistent with overdose. Among the adults, three of the deaths occurred within 3 weeks of surgery and were related to gastric bypass, two were of indeterminate cause (at 11 months and 5 years after surgery), one was by suicide at 3 years, and one was from colon cancer at 4 years.
The authors acknowledged the limitations of their study, including its observational design, low counts for some of the outcomes, and a lack of nonsurgical controls. They also noted potential unmeasured biases in the adult cohort, including the effects of weight cycling and inaccuracies in recalling adolescent weight issues.
The study and several of its authors were supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases. Several authors reported receiving grants, honoraria, and consulting fees from medical technology and pharmaceutical companies.
SOURCE: Inge TH et al. N Engl J Med. 2019 May 16. doi: 10.1056/NEJMoa1813909.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Bariatric surgery found to be effective in IBD patients
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
REPORTING FROM DDW 2019
PPI metabolism may be altered in about one-third of bariatric surgery candidates
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
REPORTING FROM DDW 2019
Sustainable weight loss seen 5 years after endoscopic sleeve gastroplasty

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.
FROM DDW 2019
Key clinical point: Endoscopic sleeve gastroplasty is an effective, minimally invasive weight-loss procedure that results in significant total body weight loss.
Major finding: Between 1 and 5 years after endoscopic sleeve gastroplasty, patients lost 15%-20% of their total body weight.
Study details: A retrospective study of prospectively collected data on 203 patients.
Disclosures: Dr. Sharaiha reported having no financial disclosures.
Study identifies predictors of bariatric surgery attrition
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
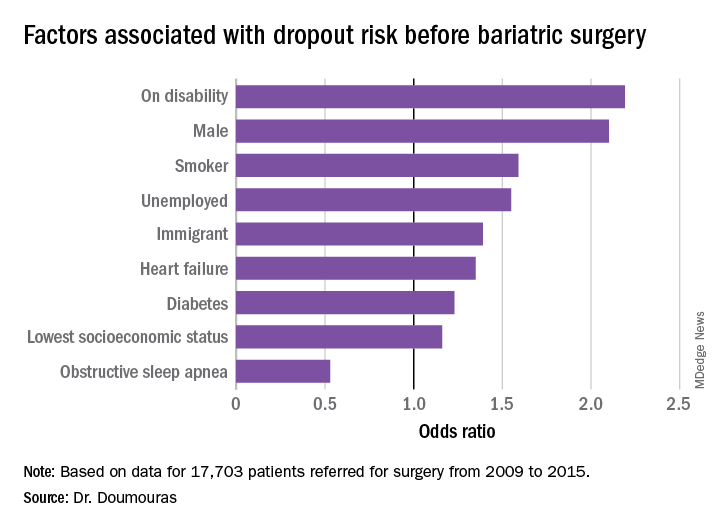
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
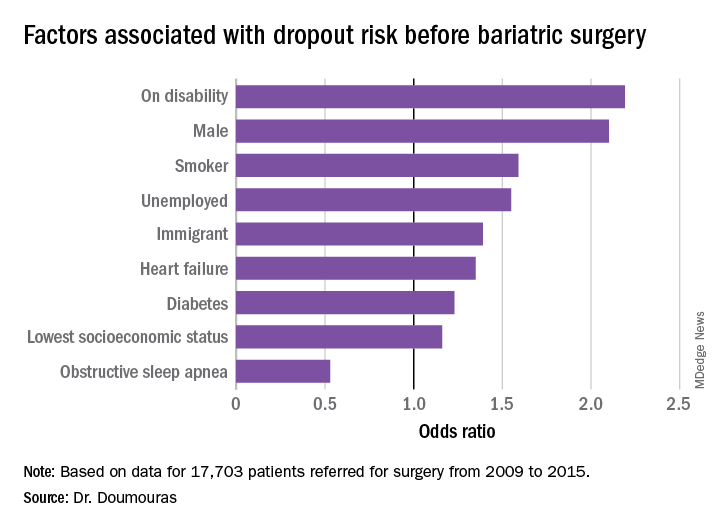
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
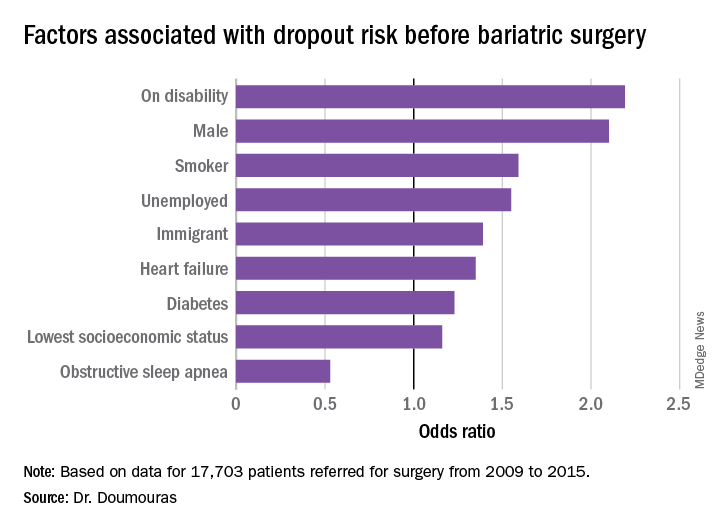
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
REPORTING FROM SAGES 2019
Study finds inconsistencies in MBSAQIP database
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
REPORTING FROM SAGES 2019
Study: Surgeon post-SG reflux rates vary widely
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
REPORTING FROM SAGES 2019





