User login
Hemoglobin nanoparticles could serve as blood substitute
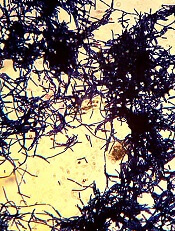
A new type of hemoglobin-based oxygen carrier has shown early promise as a potential blood substitute, according to researchers.
The team created nanoparticles consisting of bovine hemoglobin coated with the polymer polydopamine (PDA).
Lab tests showed that hemoglobin-PDA nanoparticles effectively carried oxygen, caused minimal cell damage, and acted as antioxidants, scavenging for potentially damaging free radicals and reactive oxygen species (ROS).
Hong Zhou, PhD, of the Beijing Institute of Transfusion Medicine in China, and colleagues reported these results in Biomacromolecules.
Past attempts to develop chemically modified hemoglobin as a blood substitute have been hindered by the formation of methemoglobin.
Methemoglobin doesn’t bind oxygen and therefore decreases the amount of oxygen blood delivers in the body. In addition, the generation of methemoglobin produces hydrogen peroxide, which leads to cell damage.
Dr Zhou and colleagues wanted to see if packaging hemoglobin in a benign envelope could prevent these problems. So the team developed a one-step method for wrapping hemoglobin—extracted from bovine red cells—in PDA.
The researchers said their simple preparation method meant the nanoparticles maintained the integrity of hemoglobin’s chemical structure without introducing any toxic reagent.
In addition, the PDA coating allowed hemoglobin to maintain its oxygen-carrying ability by preventing the formation of methemoglobin.
The researchers found the hemoglobin-PDA nanoparticles to have “excellent antioxidant capacity,” as they scavenged free radicals. The team said the ABTS+ radical scavenging rate reached 89%, and the DPPH radical scavenging rate reached 49%.
The hemoglobin-PDA nanoparticles also demonstrated antioxidant capacity by suppressing ROS generation. They reduced hydrogen peroxide-induced ROS generation in H9c2 cells.
Furthermore, the hemoglobin-PDA nanoparticles had little effect on blood constituents and cell viability.
The researchers found the nanoparticles had minimal effects on platelet aggregation, hemolysis in red blood cells, and coagulation processes.
And the nanoparticles had no significant cytotoxic effects on human umbilical vein endothelial cells.
The researchers therefore concluded that their hemoglobin-PDA nanoparticles represent “promising progress” for hemoglobin-based oxygen carriers. ![]()
A new type of hemoglobin-based oxygen carrier has shown early promise as a potential blood substitute, according to researchers.
The team created nanoparticles consisting of bovine hemoglobin coated with the polymer polydopamine (PDA).
Lab tests showed that hemoglobin-PDA nanoparticles effectively carried oxygen, caused minimal cell damage, and acted as antioxidants, scavenging for potentially damaging free radicals and reactive oxygen species (ROS).
Hong Zhou, PhD, of the Beijing Institute of Transfusion Medicine in China, and colleagues reported these results in Biomacromolecules.
Past attempts to develop chemically modified hemoglobin as a blood substitute have been hindered by the formation of methemoglobin.
Methemoglobin doesn’t bind oxygen and therefore decreases the amount of oxygen blood delivers in the body. In addition, the generation of methemoglobin produces hydrogen peroxide, which leads to cell damage.
Dr Zhou and colleagues wanted to see if packaging hemoglobin in a benign envelope could prevent these problems. So the team developed a one-step method for wrapping hemoglobin—extracted from bovine red cells—in PDA.
The researchers said their simple preparation method meant the nanoparticles maintained the integrity of hemoglobin’s chemical structure without introducing any toxic reagent.
In addition, the PDA coating allowed hemoglobin to maintain its oxygen-carrying ability by preventing the formation of methemoglobin.
The researchers found the hemoglobin-PDA nanoparticles to have “excellent antioxidant capacity,” as they scavenged free radicals. The team said the ABTS+ radical scavenging rate reached 89%, and the DPPH radical scavenging rate reached 49%.
The hemoglobin-PDA nanoparticles also demonstrated antioxidant capacity by suppressing ROS generation. They reduced hydrogen peroxide-induced ROS generation in H9c2 cells.
Furthermore, the hemoglobin-PDA nanoparticles had little effect on blood constituents and cell viability.
The researchers found the nanoparticles had minimal effects on platelet aggregation, hemolysis in red blood cells, and coagulation processes.
And the nanoparticles had no significant cytotoxic effects on human umbilical vein endothelial cells.
The researchers therefore concluded that their hemoglobin-PDA nanoparticles represent “promising progress” for hemoglobin-based oxygen carriers. ![]()
A new type of hemoglobin-based oxygen carrier has shown early promise as a potential blood substitute, according to researchers.
The team created nanoparticles consisting of bovine hemoglobin coated with the polymer polydopamine (PDA).
Lab tests showed that hemoglobin-PDA nanoparticles effectively carried oxygen, caused minimal cell damage, and acted as antioxidants, scavenging for potentially damaging free radicals and reactive oxygen species (ROS).
Hong Zhou, PhD, of the Beijing Institute of Transfusion Medicine in China, and colleagues reported these results in Biomacromolecules.
Past attempts to develop chemically modified hemoglobin as a blood substitute have been hindered by the formation of methemoglobin.
Methemoglobin doesn’t bind oxygen and therefore decreases the amount of oxygen blood delivers in the body. In addition, the generation of methemoglobin produces hydrogen peroxide, which leads to cell damage.
Dr Zhou and colleagues wanted to see if packaging hemoglobin in a benign envelope could prevent these problems. So the team developed a one-step method for wrapping hemoglobin—extracted from bovine red cells—in PDA.
The researchers said their simple preparation method meant the nanoparticles maintained the integrity of hemoglobin’s chemical structure without introducing any toxic reagent.
In addition, the PDA coating allowed hemoglobin to maintain its oxygen-carrying ability by preventing the formation of methemoglobin.
The researchers found the hemoglobin-PDA nanoparticles to have “excellent antioxidant capacity,” as they scavenged free radicals. The team said the ABTS+ radical scavenging rate reached 89%, and the DPPH radical scavenging rate reached 49%.
The hemoglobin-PDA nanoparticles also demonstrated antioxidant capacity by suppressing ROS generation. They reduced hydrogen peroxide-induced ROS generation in H9c2 cells.
Furthermore, the hemoglobin-PDA nanoparticles had little effect on blood constituents and cell viability.
The researchers found the nanoparticles had minimal effects on platelet aggregation, hemolysis in red blood cells, and coagulation processes.
And the nanoparticles had no significant cytotoxic effects on human umbilical vein endothelial cells.
The researchers therefore concluded that their hemoglobin-PDA nanoparticles represent “promising progress” for hemoglobin-based oxygen carriers. ![]()
FDA clears test for individual WBD platelet units
The US Food and Drug Administration (FDA) has granted new clearance for Verax Biomedical’s Platelet PGD® Test.
This qualitative immunoassay is designed to detect aerobic and anaerobic Gram-positive and Gram-negative bacteria in platelets.
The test is now cleared for use on single units of leukocyte-reduced or non-leukocyte-reduced whole blood-derived (WBD) platelets in plasma.
The Platelet PGD Test was previously cleared by the FDA as a safety measure to be used following testing with a growth-based, quality control (QC) test for platelet components that is cleared by the FDA.
For this indication, the Platelet PGD Test can be used within 24 hours of transfusion on:
- Leukocyte-reduced apheresis platelets suspended in plasma
- Leukocyte-reduced apheresis platelets suspended in platelet additive solution C and plasma
- Pre-storage pools of up to 6 leukocyte-reduced WBD platelets suspended in plasma.
When used as a safety measure, the Platelet PGD Test can extend the dating of apheresis platelets in plasma from 5 to 7 days.
The Platelet PGD Test also has FDA clearance as a QC test for use on pools of up to 6 units of leukocyte-reduced and non-leukocyte-reduced WBD platelets suspended in plasma that are pooled within 4 hours of transfusion.
The latest FDA clearance extends this use to individual units of WBD platelets in plasma.
“[The new clearance] has been requested by current users of PGD as well as being outlined as a need in pending FDA Draft Guidance to address the risk of bacterial contamination in platelets,” said Jim Lousararian, chief executive officer of Verax Biomedical.
According to the company, the new clearance is intended to help reduce the risk of bacterial contamination for pediatric patients receiving platelet transfusions.
“Pediatric patients pose unique challenges in transfusion medicine,” said Paul Mintz, MD, chief medical officer of Verax Biomedical.
“They require small platelet doses and possess fragile immune systems. PGD testing individual WBD units for transfusion makes it practical to provide bacterially tested platelets to this most vulnerable group of patients.”
Multicenter study
The Verax PGD® test was evaluated in a 2-year study including 18 US hospitals. The results were published in Transfusion in 2011.
The objective of the study was to evaluate the test’s ability to detect bacterially contaminated units in the US apheresis inventory that tested negative for contamination by existing growth-based QC tests.
A total of 9 contaminated units were detected by PGD and confirmed as bacterially contaminated in a population of 27,620 leukocyte-reduced apheresis units (1:3,069 doses tested).
All 9 units had previously tested negative by growth-based QC methods applied earlier in unit life in conformance with all applicable AABB and CAP standards for bacterial testing.
Researchers said the study clearly demonstrated the ability of the Platelet PGD Test to detect and interdict contaminated units missed by current QC testing methods. ![]()
The US Food and Drug Administration (FDA) has granted new clearance for Verax Biomedical’s Platelet PGD® Test.
This qualitative immunoassay is designed to detect aerobic and anaerobic Gram-positive and Gram-negative bacteria in platelets.
The test is now cleared for use on single units of leukocyte-reduced or non-leukocyte-reduced whole blood-derived (WBD) platelets in plasma.
The Platelet PGD Test was previously cleared by the FDA as a safety measure to be used following testing with a growth-based, quality control (QC) test for platelet components that is cleared by the FDA.
For this indication, the Platelet PGD Test can be used within 24 hours of transfusion on:
- Leukocyte-reduced apheresis platelets suspended in plasma
- Leukocyte-reduced apheresis platelets suspended in platelet additive solution C and plasma
- Pre-storage pools of up to 6 leukocyte-reduced WBD platelets suspended in plasma.
When used as a safety measure, the Platelet PGD Test can extend the dating of apheresis platelets in plasma from 5 to 7 days.
The Platelet PGD Test also has FDA clearance as a QC test for use on pools of up to 6 units of leukocyte-reduced and non-leukocyte-reduced WBD platelets suspended in plasma that are pooled within 4 hours of transfusion.
The latest FDA clearance extends this use to individual units of WBD platelets in plasma.
“[The new clearance] has been requested by current users of PGD as well as being outlined as a need in pending FDA Draft Guidance to address the risk of bacterial contamination in platelets,” said Jim Lousararian, chief executive officer of Verax Biomedical.
According to the company, the new clearance is intended to help reduce the risk of bacterial contamination for pediatric patients receiving platelet transfusions.
“Pediatric patients pose unique challenges in transfusion medicine,” said Paul Mintz, MD, chief medical officer of Verax Biomedical.
“They require small platelet doses and possess fragile immune systems. PGD testing individual WBD units for transfusion makes it practical to provide bacterially tested platelets to this most vulnerable group of patients.”
Multicenter study
The Verax PGD® test was evaluated in a 2-year study including 18 US hospitals. The results were published in Transfusion in 2011.
The objective of the study was to evaluate the test’s ability to detect bacterially contaminated units in the US apheresis inventory that tested negative for contamination by existing growth-based QC tests.
A total of 9 contaminated units were detected by PGD and confirmed as bacterially contaminated in a population of 27,620 leukocyte-reduced apheresis units (1:3,069 doses tested).
All 9 units had previously tested negative by growth-based QC methods applied earlier in unit life in conformance with all applicable AABB and CAP standards for bacterial testing.
Researchers said the study clearly demonstrated the ability of the Platelet PGD Test to detect and interdict contaminated units missed by current QC testing methods. ![]()
The US Food and Drug Administration (FDA) has granted new clearance for Verax Biomedical’s Platelet PGD® Test.
This qualitative immunoassay is designed to detect aerobic and anaerobic Gram-positive and Gram-negative bacteria in platelets.
The test is now cleared for use on single units of leukocyte-reduced or non-leukocyte-reduced whole blood-derived (WBD) platelets in plasma.
The Platelet PGD Test was previously cleared by the FDA as a safety measure to be used following testing with a growth-based, quality control (QC) test for platelet components that is cleared by the FDA.
For this indication, the Platelet PGD Test can be used within 24 hours of transfusion on:
- Leukocyte-reduced apheresis platelets suspended in plasma
- Leukocyte-reduced apheresis platelets suspended in platelet additive solution C and plasma
- Pre-storage pools of up to 6 leukocyte-reduced WBD platelets suspended in plasma.
When used as a safety measure, the Platelet PGD Test can extend the dating of apheresis platelets in plasma from 5 to 7 days.
The Platelet PGD Test also has FDA clearance as a QC test for use on pools of up to 6 units of leukocyte-reduced and non-leukocyte-reduced WBD platelets suspended in plasma that are pooled within 4 hours of transfusion.
The latest FDA clearance extends this use to individual units of WBD platelets in plasma.
“[The new clearance] has been requested by current users of PGD as well as being outlined as a need in pending FDA Draft Guidance to address the risk of bacterial contamination in platelets,” said Jim Lousararian, chief executive officer of Verax Biomedical.
According to the company, the new clearance is intended to help reduce the risk of bacterial contamination for pediatric patients receiving platelet transfusions.
“Pediatric patients pose unique challenges in transfusion medicine,” said Paul Mintz, MD, chief medical officer of Verax Biomedical.
“They require small platelet doses and possess fragile immune systems. PGD testing individual WBD units for transfusion makes it practical to provide bacterially tested platelets to this most vulnerable group of patients.”
Multicenter study
The Verax PGD® test was evaluated in a 2-year study including 18 US hospitals. The results were published in Transfusion in 2011.
The objective of the study was to evaluate the test’s ability to detect bacterially contaminated units in the US apheresis inventory that tested negative for contamination by existing growth-based QC tests.
A total of 9 contaminated units were detected by PGD and confirmed as bacterially contaminated in a population of 27,620 leukocyte-reduced apheresis units (1:3,069 doses tested).
All 9 units had previously tested negative by growth-based QC methods applied earlier in unit life in conformance with all applicable AABB and CAP standards for bacterial testing.
Researchers said the study clearly demonstrated the ability of the Platelet PGD Test to detect and interdict contaminated units missed by current QC testing methods. ![]()
FDA authorizes use of first fully automated Zika IgM test
The US Food and Drug Administration (FDA) has granted emergency use authorization (EUA) for DiaSorin Incorporated’s LIAISON® XL Zika Capture IgM assay, the first fully automated serology assay for the detection of Zika virus infection.
The LIAISON® XL Zika Capture IgM assay is intended for the presumptive qualitative detection of Zika virus IgM antibodies in human sera.
The FDA’s decision to grant an EUA means the LIAISON® XL Zika Capture IgM assay can be used to test serum samples collected from individuals meeting criteria for Zika virus testing set forth by the US Centers for Disease Control and Prevention.
This includes clinical criteria—such as a history of clinical signs and symptoms associated with Zika virus infection—and/or epidemiological criteria—such as a history of residence in or travel to a geographic region with active Zika transmission.
Specimens used with the LIAISON® XL Zika Capture IgM assay should be collected between 8 days and 10 weeks after the onset of symptoms or risk of exposure to Zika.
The assay is intended for use in US laboratories that are certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. §263a, to perform high-complexity tests, or by similarly qualified non-US laboratories, pursuant to section 564 of the Federal Food, Drug, and Cosmetic Act (21 U.S.C. § 360bbb-3).
Where there are presumptive Zika IgM positive and presumptive recent Zika positive results from the LIAISON® XL Zika Capture IgM assay, confirmation of the presence of anti-Zika IgM antibodies requires additional testing and/or consideration alongside test results for other patient-matched specimens using the latest CDC testing algorithms for the diagnosis of Zika virus infection.
More information on the LIAISON® XL Zika Capture IgM assay and other Zika assays granted EUAs can be found on the FDA’s EUA page.
Funding for the LIAISON® XL Zika Capture IgM assay was provided by the US Department of Health and Human Services, which granted DiaSorin a $2.6 million contract in the fall of 2016.
About the EUA
The EUA does not mean the LIAISON® XL Zika Capture IgM assay is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency.
The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
This means the LIAISON® XL Zika Capture IgM assay is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner. ![]()
The US Food and Drug Administration (FDA) has granted emergency use authorization (EUA) for DiaSorin Incorporated’s LIAISON® XL Zika Capture IgM assay, the first fully automated serology assay for the detection of Zika virus infection.
The LIAISON® XL Zika Capture IgM assay is intended for the presumptive qualitative detection of Zika virus IgM antibodies in human sera.
The FDA’s decision to grant an EUA means the LIAISON® XL Zika Capture IgM assay can be used to test serum samples collected from individuals meeting criteria for Zika virus testing set forth by the US Centers for Disease Control and Prevention.
This includes clinical criteria—such as a history of clinical signs and symptoms associated with Zika virus infection—and/or epidemiological criteria—such as a history of residence in or travel to a geographic region with active Zika transmission.
Specimens used with the LIAISON® XL Zika Capture IgM assay should be collected between 8 days and 10 weeks after the onset of symptoms or risk of exposure to Zika.
The assay is intended for use in US laboratories that are certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. §263a, to perform high-complexity tests, or by similarly qualified non-US laboratories, pursuant to section 564 of the Federal Food, Drug, and Cosmetic Act (21 U.S.C. § 360bbb-3).
Where there are presumptive Zika IgM positive and presumptive recent Zika positive results from the LIAISON® XL Zika Capture IgM assay, confirmation of the presence of anti-Zika IgM antibodies requires additional testing and/or consideration alongside test results for other patient-matched specimens using the latest CDC testing algorithms for the diagnosis of Zika virus infection.
More information on the LIAISON® XL Zika Capture IgM assay and other Zika assays granted EUAs can be found on the FDA’s EUA page.
Funding for the LIAISON® XL Zika Capture IgM assay was provided by the US Department of Health and Human Services, which granted DiaSorin a $2.6 million contract in the fall of 2016.
About the EUA
The EUA does not mean the LIAISON® XL Zika Capture IgM assay is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency.
The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
This means the LIAISON® XL Zika Capture IgM assay is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner. ![]()
The US Food and Drug Administration (FDA) has granted emergency use authorization (EUA) for DiaSorin Incorporated’s LIAISON® XL Zika Capture IgM assay, the first fully automated serology assay for the detection of Zika virus infection.
The LIAISON® XL Zika Capture IgM assay is intended for the presumptive qualitative detection of Zika virus IgM antibodies in human sera.
The FDA’s decision to grant an EUA means the LIAISON® XL Zika Capture IgM assay can be used to test serum samples collected from individuals meeting criteria for Zika virus testing set forth by the US Centers for Disease Control and Prevention.
This includes clinical criteria—such as a history of clinical signs and symptoms associated with Zika virus infection—and/or epidemiological criteria—such as a history of residence in or travel to a geographic region with active Zika transmission.
Specimens used with the LIAISON® XL Zika Capture IgM assay should be collected between 8 days and 10 weeks after the onset of symptoms or risk of exposure to Zika.
The assay is intended for use in US laboratories that are certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. §263a, to perform high-complexity tests, or by similarly qualified non-US laboratories, pursuant to section 564 of the Federal Food, Drug, and Cosmetic Act (21 U.S.C. § 360bbb-3).
Where there are presumptive Zika IgM positive and presumptive recent Zika positive results from the LIAISON® XL Zika Capture IgM assay, confirmation of the presence of anti-Zika IgM antibodies requires additional testing and/or consideration alongside test results for other patient-matched specimens using the latest CDC testing algorithms for the diagnosis of Zika virus infection.
More information on the LIAISON® XL Zika Capture IgM assay and other Zika assays granted EUAs can be found on the FDA’s EUA page.
Funding for the LIAISON® XL Zika Capture IgM assay was provided by the US Department of Health and Human Services, which granted DiaSorin a $2.6 million contract in the fall of 2016.
About the EUA
The EUA does not mean the LIAISON® XL Zika Capture IgM assay is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency.
The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
This means the LIAISON® XL Zika Capture IgM assay is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner. ![]()
EC publishes guides on patient blood management
The European Commission (EC) has published guides intended to help hospitals and national authorities implement patient blood management (PBM) programs throughout the European Union.
The EC said its guide for hospitals is intended to help them implement PBM in a practical way, building on already recognized best practices.
The guide is the result of the combined expertise of clinicians and PBM professionals and the experience gathered from a 30-month pilot program implementing PBM in 5 European teaching hospitals.
The EC said this guide is relevant for all medical professionals and organizations involved in caring for patients suffering from anemia, blood loss, and medical conditions that might require transfusion.
The EC’s other PBM guide is intended for national authorities. It lists 10 “essential public health operations,” which encompass a range of activities authorities can engage in to aid the implementation of PBM in their health systems.
The essential public health operations (and examples of activities) are:
- Surveillance—eg, continuously collect patient-level data on anemia, transfusion, and outcomes to measure and guide the implementation of PBM as a standard of care
- Monitoring—eg, recommend the monitoring and flagging of too liberal blood component utilization to prevent health hazards
- Health protection—eg, develop information and education materials for clinicians, quality and safety managers, and hospital administrators
- Health promotion—eg, promote awareness of iron deficiency and iron deficiency anemia
- Disease prevention—eg, create a sense of urgency for PBM as a new evidence-based standard of care through professional training and education
- Governance—eg, create and institute a national PBM steering committee under the authority of the Ministry of Health
- Workforce, equipment, and facilities—eg, provide hospital facilities for PBM
- Organization and funding—eg, organize reallocation of funds and resources toward PBM
- Communication—eg, provide PBM webpage sections for patients, health professionals, and health administrators
- Research—eg, conduct PBM-related studies focusing on patient outcomes, cost-effectiveness, etc.
The EC said the publication of their PBM guides is timely, as the journal Transfusion recently published results from a 5-year PBM program in Western Australia, which is the world’s largest PBM program to date. The program included 605,046 patients admitted to 4 major adult tertiary-care hospitals.
The use of blood products was reduced by 41% during the study period. The program also resulted in a 28% reduction in hospital mortality, a 15% reduction in the average hospital length of stay, a 21% decrease in hospital-acquired infections, and a 31% decrease in the incidence of heart attack or stroke. ![]()
The European Commission (EC) has published guides intended to help hospitals and national authorities implement patient blood management (PBM) programs throughout the European Union.
The EC said its guide for hospitals is intended to help them implement PBM in a practical way, building on already recognized best practices.
The guide is the result of the combined expertise of clinicians and PBM professionals and the experience gathered from a 30-month pilot program implementing PBM in 5 European teaching hospitals.
The EC said this guide is relevant for all medical professionals and organizations involved in caring for patients suffering from anemia, blood loss, and medical conditions that might require transfusion.
The EC’s other PBM guide is intended for national authorities. It lists 10 “essential public health operations,” which encompass a range of activities authorities can engage in to aid the implementation of PBM in their health systems.
The essential public health operations (and examples of activities) are:
- Surveillance—eg, continuously collect patient-level data on anemia, transfusion, and outcomes to measure and guide the implementation of PBM as a standard of care
- Monitoring—eg, recommend the monitoring and flagging of too liberal blood component utilization to prevent health hazards
- Health protection—eg, develop information and education materials for clinicians, quality and safety managers, and hospital administrators
- Health promotion—eg, promote awareness of iron deficiency and iron deficiency anemia
- Disease prevention—eg, create a sense of urgency for PBM as a new evidence-based standard of care through professional training and education
- Governance—eg, create and institute a national PBM steering committee under the authority of the Ministry of Health
- Workforce, equipment, and facilities—eg, provide hospital facilities for PBM
- Organization and funding—eg, organize reallocation of funds and resources toward PBM
- Communication—eg, provide PBM webpage sections for patients, health professionals, and health administrators
- Research—eg, conduct PBM-related studies focusing on patient outcomes, cost-effectiveness, etc.
The EC said the publication of their PBM guides is timely, as the journal Transfusion recently published results from a 5-year PBM program in Western Australia, which is the world’s largest PBM program to date. The program included 605,046 patients admitted to 4 major adult tertiary-care hospitals.
The use of blood products was reduced by 41% during the study period. The program also resulted in a 28% reduction in hospital mortality, a 15% reduction in the average hospital length of stay, a 21% decrease in hospital-acquired infections, and a 31% decrease in the incidence of heart attack or stroke. ![]()
The European Commission (EC) has published guides intended to help hospitals and national authorities implement patient blood management (PBM) programs throughout the European Union.
The EC said its guide for hospitals is intended to help them implement PBM in a practical way, building on already recognized best practices.
The guide is the result of the combined expertise of clinicians and PBM professionals and the experience gathered from a 30-month pilot program implementing PBM in 5 European teaching hospitals.
The EC said this guide is relevant for all medical professionals and organizations involved in caring for patients suffering from anemia, blood loss, and medical conditions that might require transfusion.
The EC’s other PBM guide is intended for national authorities. It lists 10 “essential public health operations,” which encompass a range of activities authorities can engage in to aid the implementation of PBM in their health systems.
The essential public health operations (and examples of activities) are:
- Surveillance—eg, continuously collect patient-level data on anemia, transfusion, and outcomes to measure and guide the implementation of PBM as a standard of care
- Monitoring—eg, recommend the monitoring and flagging of too liberal blood component utilization to prevent health hazards
- Health protection—eg, develop information and education materials for clinicians, quality and safety managers, and hospital administrators
- Health promotion—eg, promote awareness of iron deficiency and iron deficiency anemia
- Disease prevention—eg, create a sense of urgency for PBM as a new evidence-based standard of care through professional training and education
- Governance—eg, create and institute a national PBM steering committee under the authority of the Ministry of Health
- Workforce, equipment, and facilities—eg, provide hospital facilities for PBM
- Organization and funding—eg, organize reallocation of funds and resources toward PBM
- Communication—eg, provide PBM webpage sections for patients, health professionals, and health administrators
- Research—eg, conduct PBM-related studies focusing on patient outcomes, cost-effectiveness, etc.
The EC said the publication of their PBM guides is timely, as the journal Transfusion recently published results from a 5-year PBM program in Western Australia, which is the world’s largest PBM program to date. The program included 605,046 patients admitted to 4 major adult tertiary-care hospitals.
The use of blood products was reduced by 41% during the study period. The program also resulted in a 28% reduction in hospital mortality, a 15% reduction in the average hospital length of stay, a 21% decrease in hospital-acquired infections, and a 31% decrease in the incidence of heart attack or stroke. ![]()
Studies support Zika screening in entire US blood supply
Results from a pair of studies suggest it is necessary to test for Zika virus in all blood donated in the US, even blood collected outside areas of active Zika transmission.
Last year, the US Food and Drug Administration recommended that all states and US territories screen donated whole blood and blood components for the Zika virus.
Two studies published in Transfusion support that recommendation by revealing the presence of blood donors who tested positive for Zika and may have acquired the infection via travel or sexual contact.
In the first study, researchers screened donor plasma samples using the cobas Zika test. Some of the researchers are employees/contractors of Roche Molecular Systems, Inc., which developed the test.
The study included 358,786 blood donations made in US states. Plasma samples from 23 of the donors were reactive on the first test.
For these cases, the testing lab performed repeat tests with cobas Zika. The lab also simulated minipool testing by diluting a donor sample 1:6 with Zika-negative human plasma. In addition, the reactive samples were sent out for alternate nucleic acid testing and serology testing.
The additional tests suggested 14 of the samples were positive for the Zika virus.
Ten of the 14 donors said they had traveled to an area of active Zika transmission within 90 days of their donation, and 3 of the 10 donors also had a sexual exposure risk. The median time from the end of the donors’ travel to their donation was 25 days (range, 6-71).
Three donors had not traveled to an area of active Zika transmission outside the US, but they lived in Miami-Dade County and were thought to have contracted the virus there.
For the remaining donor, there was no information on travel or sexual exposure risk.
The researchers said minipool testing likely would have identified half of the Zika-positive donations, as only 7 of the 14 donations with probable Zika virus infection were detectable via the simulated minipool testing.
The team also said the estimated specificity of the cobas Zika test was 99.997%.
In the second study, researchers screened donor plasma samples using the Procleix Zika virus assay. Some of the researchers are employees/contractors of Hologic, Inc., and Grifols Diagnostic Solutions, Inc., the companies that co-developed the assay.
The study included 466,834 blood donations in the US (outside of Puerto Rico and Florida). Twenty donor samples were reactive on the initial test.
These 20 samples (and additional samples from these donors) underwent subsequent testing with the Procleix Zika virus assay, real-time polymerase chain reaction, and Zika virus IgG and IgM capture ELISAs.
According to subsequent tests, 5 donors were reactive for Zika virus RNA. All of these donations were collected outside areas of active Zika transmission, but all 5 donors had traveled to areas of active transmission.
The researchers said the estimated specificity of the Procleix Zika virus assay was 99.997%.
The team also reported transfusion of an apheresis platelet donation from 1 of the 5 Zika-positive donors. The recipient of this product did not develop Zika infection, which suggests these units may not be infectious.
However, other researchers previously reported what they believed to be transmission of the Zika virus via platelet transfusion. ![]()
Results from a pair of studies suggest it is necessary to test for Zika virus in all blood donated in the US, even blood collected outside areas of active Zika transmission.
Last year, the US Food and Drug Administration recommended that all states and US territories screen donated whole blood and blood components for the Zika virus.
Two studies published in Transfusion support that recommendation by revealing the presence of blood donors who tested positive for Zika and may have acquired the infection via travel or sexual contact.
In the first study, researchers screened donor plasma samples using the cobas Zika test. Some of the researchers are employees/contractors of Roche Molecular Systems, Inc., which developed the test.
The study included 358,786 blood donations made in US states. Plasma samples from 23 of the donors were reactive on the first test.
For these cases, the testing lab performed repeat tests with cobas Zika. The lab also simulated minipool testing by diluting a donor sample 1:6 with Zika-negative human plasma. In addition, the reactive samples were sent out for alternate nucleic acid testing and serology testing.
The additional tests suggested 14 of the samples were positive for the Zika virus.
Ten of the 14 donors said they had traveled to an area of active Zika transmission within 90 days of their donation, and 3 of the 10 donors also had a sexual exposure risk. The median time from the end of the donors’ travel to their donation was 25 days (range, 6-71).
Three donors had not traveled to an area of active Zika transmission outside the US, but they lived in Miami-Dade County and were thought to have contracted the virus there.
For the remaining donor, there was no information on travel or sexual exposure risk.
The researchers said minipool testing likely would have identified half of the Zika-positive donations, as only 7 of the 14 donations with probable Zika virus infection were detectable via the simulated minipool testing.
The team also said the estimated specificity of the cobas Zika test was 99.997%.
In the second study, researchers screened donor plasma samples using the Procleix Zika virus assay. Some of the researchers are employees/contractors of Hologic, Inc., and Grifols Diagnostic Solutions, Inc., the companies that co-developed the assay.
The study included 466,834 blood donations in the US (outside of Puerto Rico and Florida). Twenty donor samples were reactive on the initial test.
These 20 samples (and additional samples from these donors) underwent subsequent testing with the Procleix Zika virus assay, real-time polymerase chain reaction, and Zika virus IgG and IgM capture ELISAs.
According to subsequent tests, 5 donors were reactive for Zika virus RNA. All of these donations were collected outside areas of active Zika transmission, but all 5 donors had traveled to areas of active transmission.
The researchers said the estimated specificity of the Procleix Zika virus assay was 99.997%.
The team also reported transfusion of an apheresis platelet donation from 1 of the 5 Zika-positive donors. The recipient of this product did not develop Zika infection, which suggests these units may not be infectious.
However, other researchers previously reported what they believed to be transmission of the Zika virus via platelet transfusion. ![]()
Results from a pair of studies suggest it is necessary to test for Zika virus in all blood donated in the US, even blood collected outside areas of active Zika transmission.
Last year, the US Food and Drug Administration recommended that all states and US territories screen donated whole blood and blood components for the Zika virus.
Two studies published in Transfusion support that recommendation by revealing the presence of blood donors who tested positive for Zika and may have acquired the infection via travel or sexual contact.
In the first study, researchers screened donor plasma samples using the cobas Zika test. Some of the researchers are employees/contractors of Roche Molecular Systems, Inc., which developed the test.
The study included 358,786 blood donations made in US states. Plasma samples from 23 of the donors were reactive on the first test.
For these cases, the testing lab performed repeat tests with cobas Zika. The lab also simulated minipool testing by diluting a donor sample 1:6 with Zika-negative human plasma. In addition, the reactive samples were sent out for alternate nucleic acid testing and serology testing.
The additional tests suggested 14 of the samples were positive for the Zika virus.
Ten of the 14 donors said they had traveled to an area of active Zika transmission within 90 days of their donation, and 3 of the 10 donors also had a sexual exposure risk. The median time from the end of the donors’ travel to their donation was 25 days (range, 6-71).
Three donors had not traveled to an area of active Zika transmission outside the US, but they lived in Miami-Dade County and were thought to have contracted the virus there.
For the remaining donor, there was no information on travel or sexual exposure risk.
The researchers said minipool testing likely would have identified half of the Zika-positive donations, as only 7 of the 14 donations with probable Zika virus infection were detectable via the simulated minipool testing.
The team also said the estimated specificity of the cobas Zika test was 99.997%.
In the second study, researchers screened donor plasma samples using the Procleix Zika virus assay. Some of the researchers are employees/contractors of Hologic, Inc., and Grifols Diagnostic Solutions, Inc., the companies that co-developed the assay.
The study included 466,834 blood donations in the US (outside of Puerto Rico and Florida). Twenty donor samples were reactive on the initial test.
These 20 samples (and additional samples from these donors) underwent subsequent testing with the Procleix Zika virus assay, real-time polymerase chain reaction, and Zika virus IgG and IgM capture ELISAs.
According to subsequent tests, 5 donors were reactive for Zika virus RNA. All of these donations were collected outside areas of active Zika transmission, but all 5 donors had traveled to areas of active transmission.
The researchers said the estimated specificity of the Procleix Zika virus assay was 99.997%.
The team also reported transfusion of an apheresis platelet donation from 1 of the 5 Zika-positive donors. The recipient of this product did not develop Zika infection, which suggests these units may not be infectious.
However, other researchers previously reported what they believed to be transmission of the Zika virus via platelet transfusion. ![]()
Donor screening assays more sensitive than diagnostic assays for Zika
New research suggests assays used to screen donated blood for the Zika virus are more sensitive than assays used to help physicians diagnose Zika infection.
The study showed that donor screening assays could detect Zika virus RNA with greater sensitivity than diagnostic real-time polymerase chain reaction (RT-PCR) assays.
However, the evidence also indicated that increasing the volume of blood analyzed can increase the sensitivity of diagnostic assays.
This research was published in Transfusion in a special issue focusing on Zika and other transfusion-transmitted viruses.
The researchers compared 17 nucleic acid amplification technology assays used at 11 different labs. (Some of the 17 assays were actually the same assays used at different labs.)
One of the donor screening assays was the Procleix Zika virus assay, which was co-developed by Hologic, Inc. and Grifols Diagnostic Solutions, Inc. and used at Hologic.
The other donor screening assay was the cobas Zika test, which was developed by Roche Molecular Systems, Inc. and used in the company’s lab.
The RT-PCR diagnostic assays included the US Centers for Disease Control and Prevention’s (CDC) Singleplex (1087, 4481) and Trioplex assays—both low input (LI) and high input (HI)—which were used at the CDC labs in Puerto Rico (PR) and Fort Collins (FC).
Modified versions of the CDC’s assays were also used at the Blood Systems Research Institute (BSRI) in San Francisco, the University of California (UC) Davis, the Institut Louis Malarde (ILM) in French Polynesia, and 2 labs in Brazil—Fundação Pró-Sangue and Laboratório Richet.
The US Food and Drug Administration (FDA) used its own RT-PCR test, and the Etablissement Francais du Sang (EFS) in France used the Altona RealStar ZIKV RT-PCR assay.
Results
The various assays were used on plasma samples positive for 2 different strains of Zika virus—1 from Brazil and 1 from French Polynesia—as well as Zika-negative control samples.
The researchers found the donor screening assays provided comparable sensitivity and were more sensitive than each of the diagnostic RT-PCR assays.
So the team compared results with the 2 donor screening assays combined to results with the RT-PCR assays, which they grouped into 9 categories based on similar intended applications, methodologies, and results.
The 95% limit of detection (LOD95) and 50% limit of detection (LOD50) for the assays were as follows.
| Donor screening assays | CDC PR Trioplex-LI | CDC PR Trioplex-HI | CDC FC 1087-LI | CDC FC 1087-HI | BSRI/UC Davis | FDA | EFS | ILM | Brazil labs | |
| Brazil LOD95 | 13.7 | 540 | 22.8 | 220 | 43.9 | 2189 | 6343 | 312 | 107 | 165 |
| Brazil LOD50 | 2.5 | 411 | 19.6 | 43.9 | 32.3 | 326 | 523 | 46.3 | 19.6 | 124 |
| French Polynesia LOD95 | 17.9 | 1529 | 28.8 | 205 | 20.3 | 1102 | 4918 | 466 | 135 | 1351 |
| French Polynesia LOD50 | 2.5 | 123 | 24.8 | 152 | 15.1 | 81.7 | 321 | 49.6 | 24.8 | 248 |
The researchers noted that the donor screening assays were about 10-fold to 100-fold more sensitive than the standard input RT-PCR assays.
However, the CDC’s assays were performed with low and high inputs of plasma. And increasing the sample input volume increased the limit of detection by 10-fold to 30-fold.
“The results of this study, that evaluated 17 Zika virus assays in 11 laboratories and documented excellent sensitivity of the 2 donor screening assays manufactured by Roche and Grifols, were critical to support the decision by the US Food and Drug Administration and blood industry to implement investigational screening of donors in Puerto Rico in April 2016 and the entire US by the end of 2016,” said study author Michael Busch, MD, PhD, of BSRI.
“Given the sensitivity of these assays, the FDA approved clinical trials using individual donation screening and rescinded earlier policies precluding transfusion of blood collected in Puerto Rico and deferral from donation by donors who had traveled to Zika risk countries throughout the US. This screening has detected over 350 infected blood donations in Puerto Rico and dozens of infected donations in the continental US.” ![]()
New research suggests assays used to screen donated blood for the Zika virus are more sensitive than assays used to help physicians diagnose Zika infection.
The study showed that donor screening assays could detect Zika virus RNA with greater sensitivity than diagnostic real-time polymerase chain reaction (RT-PCR) assays.
However, the evidence also indicated that increasing the volume of blood analyzed can increase the sensitivity of diagnostic assays.
This research was published in Transfusion in a special issue focusing on Zika and other transfusion-transmitted viruses.
The researchers compared 17 nucleic acid amplification technology assays used at 11 different labs. (Some of the 17 assays were actually the same assays used at different labs.)
One of the donor screening assays was the Procleix Zika virus assay, which was co-developed by Hologic, Inc. and Grifols Diagnostic Solutions, Inc. and used at Hologic.
The other donor screening assay was the cobas Zika test, which was developed by Roche Molecular Systems, Inc. and used in the company’s lab.
The RT-PCR diagnostic assays included the US Centers for Disease Control and Prevention’s (CDC) Singleplex (1087, 4481) and Trioplex assays—both low input (LI) and high input (HI)—which were used at the CDC labs in Puerto Rico (PR) and Fort Collins (FC).
Modified versions of the CDC’s assays were also used at the Blood Systems Research Institute (BSRI) in San Francisco, the University of California (UC) Davis, the Institut Louis Malarde (ILM) in French Polynesia, and 2 labs in Brazil—Fundação Pró-Sangue and Laboratório Richet.
The US Food and Drug Administration (FDA) used its own RT-PCR test, and the Etablissement Francais du Sang (EFS) in France used the Altona RealStar ZIKV RT-PCR assay.
Results
The various assays were used on plasma samples positive for 2 different strains of Zika virus—1 from Brazil and 1 from French Polynesia—as well as Zika-negative control samples.
The researchers found the donor screening assays provided comparable sensitivity and were more sensitive than each of the diagnostic RT-PCR assays.
So the team compared results with the 2 donor screening assays combined to results with the RT-PCR assays, which they grouped into 9 categories based on similar intended applications, methodologies, and results.
The 95% limit of detection (LOD95) and 50% limit of detection (LOD50) for the assays were as follows.
| Donor screening assays | CDC PR Trioplex-LI | CDC PR Trioplex-HI | CDC FC 1087-LI | CDC FC 1087-HI | BSRI/UC Davis | FDA | EFS | ILM | Brazil labs | |
| Brazil LOD95 | 13.7 | 540 | 22.8 | 220 | 43.9 | 2189 | 6343 | 312 | 107 | 165 |
| Brazil LOD50 | 2.5 | 411 | 19.6 | 43.9 | 32.3 | 326 | 523 | 46.3 | 19.6 | 124 |
| French Polynesia LOD95 | 17.9 | 1529 | 28.8 | 205 | 20.3 | 1102 | 4918 | 466 | 135 | 1351 |
| French Polynesia LOD50 | 2.5 | 123 | 24.8 | 152 | 15.1 | 81.7 | 321 | 49.6 | 24.8 | 248 |
The researchers noted that the donor screening assays were about 10-fold to 100-fold more sensitive than the standard input RT-PCR assays.
However, the CDC’s assays were performed with low and high inputs of plasma. And increasing the sample input volume increased the limit of detection by 10-fold to 30-fold.
“The results of this study, that evaluated 17 Zika virus assays in 11 laboratories and documented excellent sensitivity of the 2 donor screening assays manufactured by Roche and Grifols, were critical to support the decision by the US Food and Drug Administration and blood industry to implement investigational screening of donors in Puerto Rico in April 2016 and the entire US by the end of 2016,” said study author Michael Busch, MD, PhD, of BSRI.
“Given the sensitivity of these assays, the FDA approved clinical trials using individual donation screening and rescinded earlier policies precluding transfusion of blood collected in Puerto Rico and deferral from donation by donors who had traveled to Zika risk countries throughout the US. This screening has detected over 350 infected blood donations in Puerto Rico and dozens of infected donations in the continental US.” ![]()
New research suggests assays used to screen donated blood for the Zika virus are more sensitive than assays used to help physicians diagnose Zika infection.
The study showed that donor screening assays could detect Zika virus RNA with greater sensitivity than diagnostic real-time polymerase chain reaction (RT-PCR) assays.
However, the evidence also indicated that increasing the volume of blood analyzed can increase the sensitivity of diagnostic assays.
This research was published in Transfusion in a special issue focusing on Zika and other transfusion-transmitted viruses.
The researchers compared 17 nucleic acid amplification technology assays used at 11 different labs. (Some of the 17 assays were actually the same assays used at different labs.)
One of the donor screening assays was the Procleix Zika virus assay, which was co-developed by Hologic, Inc. and Grifols Diagnostic Solutions, Inc. and used at Hologic.
The other donor screening assay was the cobas Zika test, which was developed by Roche Molecular Systems, Inc. and used in the company’s lab.
The RT-PCR diagnostic assays included the US Centers for Disease Control and Prevention’s (CDC) Singleplex (1087, 4481) and Trioplex assays—both low input (LI) and high input (HI)—which were used at the CDC labs in Puerto Rico (PR) and Fort Collins (FC).
Modified versions of the CDC’s assays were also used at the Blood Systems Research Institute (BSRI) in San Francisco, the University of California (UC) Davis, the Institut Louis Malarde (ILM) in French Polynesia, and 2 labs in Brazil—Fundação Pró-Sangue and Laboratório Richet.
The US Food and Drug Administration (FDA) used its own RT-PCR test, and the Etablissement Francais du Sang (EFS) in France used the Altona RealStar ZIKV RT-PCR assay.
Results
The various assays were used on plasma samples positive for 2 different strains of Zika virus—1 from Brazil and 1 from French Polynesia—as well as Zika-negative control samples.
The researchers found the donor screening assays provided comparable sensitivity and were more sensitive than each of the diagnostic RT-PCR assays.
So the team compared results with the 2 donor screening assays combined to results with the RT-PCR assays, which they grouped into 9 categories based on similar intended applications, methodologies, and results.
The 95% limit of detection (LOD95) and 50% limit of detection (LOD50) for the assays were as follows.
| Donor screening assays | CDC PR Trioplex-LI | CDC PR Trioplex-HI | CDC FC 1087-LI | CDC FC 1087-HI | BSRI/UC Davis | FDA | EFS | ILM | Brazil labs | |
| Brazil LOD95 | 13.7 | 540 | 22.8 | 220 | 43.9 | 2189 | 6343 | 312 | 107 | 165 |
| Brazil LOD50 | 2.5 | 411 | 19.6 | 43.9 | 32.3 | 326 | 523 | 46.3 | 19.6 | 124 |
| French Polynesia LOD95 | 17.9 | 1529 | 28.8 | 205 | 20.3 | 1102 | 4918 | 466 | 135 | 1351 |
| French Polynesia LOD50 | 2.5 | 123 | 24.8 | 152 | 15.1 | 81.7 | 321 | 49.6 | 24.8 | 248 |
The researchers noted that the donor screening assays were about 10-fold to 100-fold more sensitive than the standard input RT-PCR assays.
However, the CDC’s assays were performed with low and high inputs of plasma. And increasing the sample input volume increased the limit of detection by 10-fold to 30-fold.
“The results of this study, that evaluated 17 Zika virus assays in 11 laboratories and documented excellent sensitivity of the 2 donor screening assays manufactured by Roche and Grifols, were critical to support the decision by the US Food and Drug Administration and blood industry to implement investigational screening of donors in Puerto Rico in April 2016 and the entire US by the end of 2016,” said study author Michael Busch, MD, PhD, of BSRI.
“Given the sensitivity of these assays, the FDA approved clinical trials using individual donation screening and rescinded earlier policies precluding transfusion of blood collected in Puerto Rico and deferral from donation by donors who had traveled to Zika risk countries throughout the US. This screening has detected over 350 infected blood donations in Puerto Rico and dozens of infected donations in the continental US.” ![]()
Team devises new way to manufacture RBCs
Researchers say they have generated the first human immortalized adult erythroid line that provides a sustainable supply of erythroid cells.
The team says this cell line, known as Bristol Erythroid Line Adult (BEL-A), is the first erythroid line to fully recapitulate normal erythropoiesis.
It produced mature reticulocytes that proved functionally and molecularly similar to adult reticulocytes cultured in vitro.
In addition, in vivo survival rates of BEL-A reticulocytes were similar to the survival rates of red blood cells (RBCs) from adult donors.
The researchers described their generation and testing of the BEL-A line in Nature Communications.
“Previous approaches to producing red blood cells have relied on various sources of stem cells, which can only presently produce very limited quantities,” said study author Jan Frayne, PhD, of the University of Bristol in the UK.
“By taking an alternative approach, we have generated the first human immortalized adult erythroid line (Bristol Erythroid Line Adult or BEL-A), and in doing so, have demonstrated a feasible way to sustainably manufacture red cells for clinical use from in vitro culture.”
Dr Frayne and her colleagues began with CD34+ cells from adult bone marrow. The researchers transduced these cells with an HPV16-E6/E7 construct and maintained them in the primary medium of the team’s erythroid culture system for 4 days.
On day 5, the researchers transferred the cells to an expansion medium containing doxycycline. After 190 days of continuous proliferation, the cells were frozen for storage.
Some cells were frozen throughout this time period as well, and all of the samples re-established efficiently in culture after thawing.
The researchers said these immortalized BEL-A cells were pro- to early basophilic erythroblasts, and there was no change in morphology over time.
After 100 days in continuous culture, the researchers transferred BEL-A cells to the primary erythroid culture medium containing doxycycline. The cells remained there for 6 days and were then moved to a medium without doxycycline to induce differentiation to mature erythroblasts and reticulocytes.
The researchers said the BEL-A cells exhibited an “unchanged ability to differentiate,” and were consistently able to expand.
The team also noted that BEL-A reticulocytes were similar to normal adult reticulocytes. The cells had similar diameters, comparable deformability indexes, and they bound and released oxygen in the same way.
The researchers tested the in vivo survival of BEL-A reticulocytes as well. They transfused BEL-A reticulocytes and donor RBCs into macrophage-depleted NSG mice. There was no difference in survival between the 2 cell types.
Dr Frayne and her colleagues said their results suggest immortalized erythroid lines can be used for the manufacture of RBCs for clinical use and for the study of erythropoiesis. ![]()
Researchers say they have generated the first human immortalized adult erythroid line that provides a sustainable supply of erythroid cells.
The team says this cell line, known as Bristol Erythroid Line Adult (BEL-A), is the first erythroid line to fully recapitulate normal erythropoiesis.
It produced mature reticulocytes that proved functionally and molecularly similar to adult reticulocytes cultured in vitro.
In addition, in vivo survival rates of BEL-A reticulocytes were similar to the survival rates of red blood cells (RBCs) from adult donors.
The researchers described their generation and testing of the BEL-A line in Nature Communications.
“Previous approaches to producing red blood cells have relied on various sources of stem cells, which can only presently produce very limited quantities,” said study author Jan Frayne, PhD, of the University of Bristol in the UK.
“By taking an alternative approach, we have generated the first human immortalized adult erythroid line (Bristol Erythroid Line Adult or BEL-A), and in doing so, have demonstrated a feasible way to sustainably manufacture red cells for clinical use from in vitro culture.”
Dr Frayne and her colleagues began with CD34+ cells from adult bone marrow. The researchers transduced these cells with an HPV16-E6/E7 construct and maintained them in the primary medium of the team’s erythroid culture system for 4 days.
On day 5, the researchers transferred the cells to an expansion medium containing doxycycline. After 190 days of continuous proliferation, the cells were frozen for storage.
Some cells were frozen throughout this time period as well, and all of the samples re-established efficiently in culture after thawing.
The researchers said these immortalized BEL-A cells were pro- to early basophilic erythroblasts, and there was no change in morphology over time.
After 100 days in continuous culture, the researchers transferred BEL-A cells to the primary erythroid culture medium containing doxycycline. The cells remained there for 6 days and were then moved to a medium without doxycycline to induce differentiation to mature erythroblasts and reticulocytes.
The researchers said the BEL-A cells exhibited an “unchanged ability to differentiate,” and were consistently able to expand.
The team also noted that BEL-A reticulocytes were similar to normal adult reticulocytes. The cells had similar diameters, comparable deformability indexes, and they bound and released oxygen in the same way.
The researchers tested the in vivo survival of BEL-A reticulocytes as well. They transfused BEL-A reticulocytes and donor RBCs into macrophage-depleted NSG mice. There was no difference in survival between the 2 cell types.
Dr Frayne and her colleagues said their results suggest immortalized erythroid lines can be used for the manufacture of RBCs for clinical use and for the study of erythropoiesis. ![]()
Researchers say they have generated the first human immortalized adult erythroid line that provides a sustainable supply of erythroid cells.
The team says this cell line, known as Bristol Erythroid Line Adult (BEL-A), is the first erythroid line to fully recapitulate normal erythropoiesis.
It produced mature reticulocytes that proved functionally and molecularly similar to adult reticulocytes cultured in vitro.
In addition, in vivo survival rates of BEL-A reticulocytes were similar to the survival rates of red blood cells (RBCs) from adult donors.
The researchers described their generation and testing of the BEL-A line in Nature Communications.
“Previous approaches to producing red blood cells have relied on various sources of stem cells, which can only presently produce very limited quantities,” said study author Jan Frayne, PhD, of the University of Bristol in the UK.
“By taking an alternative approach, we have generated the first human immortalized adult erythroid line (Bristol Erythroid Line Adult or BEL-A), and in doing so, have demonstrated a feasible way to sustainably manufacture red cells for clinical use from in vitro culture.”
Dr Frayne and her colleagues began with CD34+ cells from adult bone marrow. The researchers transduced these cells with an HPV16-E6/E7 construct and maintained them in the primary medium of the team’s erythroid culture system for 4 days.
On day 5, the researchers transferred the cells to an expansion medium containing doxycycline. After 190 days of continuous proliferation, the cells were frozen for storage.
Some cells were frozen throughout this time period as well, and all of the samples re-established efficiently in culture after thawing.
The researchers said these immortalized BEL-A cells were pro- to early basophilic erythroblasts, and there was no change in morphology over time.
After 100 days in continuous culture, the researchers transferred BEL-A cells to the primary erythroid culture medium containing doxycycline. The cells remained there for 6 days and were then moved to a medium without doxycycline to induce differentiation to mature erythroblasts and reticulocytes.
The researchers said the BEL-A cells exhibited an “unchanged ability to differentiate,” and were consistently able to expand.
The team also noted that BEL-A reticulocytes were similar to normal adult reticulocytes. The cells had similar diameters, comparable deformability indexes, and they bound and released oxygen in the same way.
The researchers tested the in vivo survival of BEL-A reticulocytes as well. They transfused BEL-A reticulocytes and donor RBCs into macrophage-depleted NSG mice. There was no difference in survival between the 2 cell types.
Dr Frayne and her colleagues said their results suggest immortalized erythroid lines can be used for the manufacture of RBCs for clinical use and for the study of erythropoiesis.
Team develops paper-based test for blood typing
Researchers say they have created a paper-based assay that provides “rapid and reliable” blood typing.
The team used this test to analyze 3550 blood samples and observed a more than 99.9% accuracy rate.
The test was able to classify samples into the common ABO and Rh blood groups in less than 30 seconds.
With slightly more time (but still in less than 2 minutes), the assay was able to identify multiple rare blood types.
Hong Zhang, of Southwest Hospital, Third Military Medical University in Chongqing, China, and colleagues described this test in Science Translational Medicine.
To create the test, the researchers took advantage of chemical reactions between blood serum proteins and the dye bromocreosol green.
The team applied a small sample of whole blood onto a test-strip containing antibodies that recognized different blood group antigens.
The results appeared as visual color changes—teal if a blood group antigen was present in a sample and brown if not.
The researchers also incorporated a separation membrane to isolate plasma from whole blood, which allowed them to simultaneously identify specific blood cell antigens and detect antibodies in plasma based on how the blood cells clumped together (also known as forward and reverse typing), without a centrifuge.
The team said the rapid turnaround time of this test could be ideal for resource-limited situations, such as war zones, remote areas, and during emergencies.
Researchers say they have created a paper-based assay that provides “rapid and reliable” blood typing.
The team used this test to analyze 3550 blood samples and observed a more than 99.9% accuracy rate.
The test was able to classify samples into the common ABO and Rh blood groups in less than 30 seconds.
With slightly more time (but still in less than 2 minutes), the assay was able to identify multiple rare blood types.
Hong Zhang, of Southwest Hospital, Third Military Medical University in Chongqing, China, and colleagues described this test in Science Translational Medicine.
To create the test, the researchers took advantage of chemical reactions between blood serum proteins and the dye bromocreosol green.
The team applied a small sample of whole blood onto a test-strip containing antibodies that recognized different blood group antigens.
The results appeared as visual color changes—teal if a blood group antigen was present in a sample and brown if not.
The researchers also incorporated a separation membrane to isolate plasma from whole blood, which allowed them to simultaneously identify specific blood cell antigens and detect antibodies in plasma based on how the blood cells clumped together (also known as forward and reverse typing), without a centrifuge.
The team said the rapid turnaround time of this test could be ideal for resource-limited situations, such as war zones, remote areas, and during emergencies.
Researchers say they have created a paper-based assay that provides “rapid and reliable” blood typing.
The team used this test to analyze 3550 blood samples and observed a more than 99.9% accuracy rate.
The test was able to classify samples into the common ABO and Rh blood groups in less than 30 seconds.
With slightly more time (but still in less than 2 minutes), the assay was able to identify multiple rare blood types.
Hong Zhang, of Southwest Hospital, Third Military Medical University in Chongqing, China, and colleagues described this test in Science Translational Medicine.
To create the test, the researchers took advantage of chemical reactions between blood serum proteins and the dye bromocreosol green.
The team applied a small sample of whole blood onto a test-strip containing antibodies that recognized different blood group antigens.
The results appeared as visual color changes—teal if a blood group antigen was present in a sample and brown if not.
The researchers also incorporated a separation membrane to isolate plasma from whole blood, which allowed them to simultaneously identify specific blood cell antigens and detect antibodies in plasma based on how the blood cells clumped together (also known as forward and reverse typing), without a centrifuge.
The team said the rapid turnaround time of this test could be ideal for resource-limited situations, such as war zones, remote areas, and during emergencies.
Transfusion practice may harm certain patients
A retrospective study indicates that a high transfusion ratio of fresh frozen plasma (FFP) to red blood cells (RBCs) may not be beneficial for surgical patients who do not have traumatic injuries.
In fact, the data suggest a high FFP:RBC ratio may be harmful for some of these patients.
“The strategy of giving patients requiring massive transfusion greater amounts of fresh frozen plasma, relative to the amount of red blood cells, has spilled over from trauma patients into unstudied patient populations,” said Daniel Dante Yeh, MD, of Massachusetts General Hospital in Boston.
“This may have important consequences, since our results suggest that certain populations may be harmed by this practice.”
Dr Yeh and his colleagues reported these results in JAMA Surgery.
The researchers reviewed all massive transfusions performed at Massachusetts General Hospital from January 1, 2009, through December 31, 2012.
A transfusion qualified as “massive” if at least 10 units of RBCs were given in the first 24 hours after a patient’s admission to the operating room, emergency department, or intensive care unit.
The researchers included all patients who received massive transfusions during the study period and survived more than 30 minutes after hospital arrival.
According to these criteria, there were 865 massive transfusion events. The total number of units transfused was 16,569 for RBCs, 13,933 for FFP, 5228 for cryoprecipitate, and 22,635 for platelets.
A majority of the massive transfusion recipients were not trauma patients (88.7%). Most of the transfusions were performed for intraoperative bleeding (62.9%).
The researchers compared patients who survived at least 30 days from hospital arrival to those who did not. Patients who died were older and received more RBCs (P<0.001), FFP (P<0.001), and cryoprecipitate (P=0.008).
However, the FFP:RBC ratios of survivors and non-survivors were similar. The median was 1:1.5 for survivors and 1:1.4 for non-survivors (P=0.43).
Patients without trauma
Among all non-trauma patients (n=767), there was no significant difference in the adjusted odds ratio (aOR) for 30-day mortality between patients who received a transfusion with a high FFP:RBC ratio and those who received one with a low FFP:RBC ratio (aOR=1.10, P=0.65). (The analysis was adjusted for patient age and total units of RBCs transfused.)
Among patients undergoing vascular surgery, those who received transfusions with a high FFP:RBC ratio were less likely to die within 30 days than those who received transfusions with a low FFP:RBC ratio (aOR=0.16, P=0.02).
However, among general surgery and medical service patients, those receiving transfusions with a high FFP:RBC ratio were more likely to die within 30 days than those receiving low-ratio transfusions. The aOR was 4.27 (P=0.02) for general surgery and 8.48 (P=0.02) for medicine.
“Finding evidence of increased mortality in some patients was surprising because that is directly contradictory to what is expected and intended,” Dr Yeh said. “Avoiding unnecessary FFP transfusion is important because there have been reports that associated the use of excess FFP with worse outcomes among patients that required less-than-massive transfusions.”
“Because our study is retrospective, it can only point to the need for further research. Ratio-based transfusion has been studied in trauma patients, most recently in a landmark, multicenter, randomized study called the PROPRR trial. Similar studies now need to be performed in non-trauma patients before the approach can be accepted as standard practice here at MGH [Massachusetts General Hospital] and elsewhere.” ![]()
A retrospective study indicates that a high transfusion ratio of fresh frozen plasma (FFP) to red blood cells (RBCs) may not be beneficial for surgical patients who do not have traumatic injuries.
In fact, the data suggest a high FFP:RBC ratio may be harmful for some of these patients.
“The strategy of giving patients requiring massive transfusion greater amounts of fresh frozen plasma, relative to the amount of red blood cells, has spilled over from trauma patients into unstudied patient populations,” said Daniel Dante Yeh, MD, of Massachusetts General Hospital in Boston.
“This may have important consequences, since our results suggest that certain populations may be harmed by this practice.”
Dr Yeh and his colleagues reported these results in JAMA Surgery.
The researchers reviewed all massive transfusions performed at Massachusetts General Hospital from January 1, 2009, through December 31, 2012.
A transfusion qualified as “massive” if at least 10 units of RBCs were given in the first 24 hours after a patient’s admission to the operating room, emergency department, or intensive care unit.
The researchers included all patients who received massive transfusions during the study period and survived more than 30 minutes after hospital arrival.
According to these criteria, there were 865 massive transfusion events. The total number of units transfused was 16,569 for RBCs, 13,933 for FFP, 5228 for cryoprecipitate, and 22,635 for platelets.
A majority of the massive transfusion recipients were not trauma patients (88.7%). Most of the transfusions were performed for intraoperative bleeding (62.9%).
The researchers compared patients who survived at least 30 days from hospital arrival to those who did not. Patients who died were older and received more RBCs (P<0.001), FFP (P<0.001), and cryoprecipitate (P=0.008).
However, the FFP:RBC ratios of survivors and non-survivors were similar. The median was 1:1.5 for survivors and 1:1.4 for non-survivors (P=0.43).
Patients without trauma
Among all non-trauma patients (n=767), there was no significant difference in the adjusted odds ratio (aOR) for 30-day mortality between patients who received a transfusion with a high FFP:RBC ratio and those who received one with a low FFP:RBC ratio (aOR=1.10, P=0.65). (The analysis was adjusted for patient age and total units of RBCs transfused.)
Among patients undergoing vascular surgery, those who received transfusions with a high FFP:RBC ratio were less likely to die within 30 days than those who received transfusions with a low FFP:RBC ratio (aOR=0.16, P=0.02).
However, among general surgery and medical service patients, those receiving transfusions with a high FFP:RBC ratio were more likely to die within 30 days than those receiving low-ratio transfusions. The aOR was 4.27 (P=0.02) for general surgery and 8.48 (P=0.02) for medicine.
“Finding evidence of increased mortality in some patients was surprising because that is directly contradictory to what is expected and intended,” Dr Yeh said. “Avoiding unnecessary FFP transfusion is important because there have been reports that associated the use of excess FFP with worse outcomes among patients that required less-than-massive transfusions.”
“Because our study is retrospective, it can only point to the need for further research. Ratio-based transfusion has been studied in trauma patients, most recently in a landmark, multicenter, randomized study called the PROPRR trial. Similar studies now need to be performed in non-trauma patients before the approach can be accepted as standard practice here at MGH [Massachusetts General Hospital] and elsewhere.” ![]()
A retrospective study indicates that a high transfusion ratio of fresh frozen plasma (FFP) to red blood cells (RBCs) may not be beneficial for surgical patients who do not have traumatic injuries.
In fact, the data suggest a high FFP:RBC ratio may be harmful for some of these patients.
“The strategy of giving patients requiring massive transfusion greater amounts of fresh frozen plasma, relative to the amount of red blood cells, has spilled over from trauma patients into unstudied patient populations,” said Daniel Dante Yeh, MD, of Massachusetts General Hospital in Boston.
“This may have important consequences, since our results suggest that certain populations may be harmed by this practice.”
Dr Yeh and his colleagues reported these results in JAMA Surgery.
The researchers reviewed all massive transfusions performed at Massachusetts General Hospital from January 1, 2009, through December 31, 2012.
A transfusion qualified as “massive” if at least 10 units of RBCs were given in the first 24 hours after a patient’s admission to the operating room, emergency department, or intensive care unit.
The researchers included all patients who received massive transfusions during the study period and survived more than 30 minutes after hospital arrival.
According to these criteria, there were 865 massive transfusion events. The total number of units transfused was 16,569 for RBCs, 13,933 for FFP, 5228 for cryoprecipitate, and 22,635 for platelets.
A majority of the massive transfusion recipients were not trauma patients (88.7%). Most of the transfusions were performed for intraoperative bleeding (62.9%).
The researchers compared patients who survived at least 30 days from hospital arrival to those who did not. Patients who died were older and received more RBCs (P<0.001), FFP (P<0.001), and cryoprecipitate (P=0.008).
However, the FFP:RBC ratios of survivors and non-survivors were similar. The median was 1:1.5 for survivors and 1:1.4 for non-survivors (P=0.43).
Patients without trauma
Among all non-trauma patients (n=767), there was no significant difference in the adjusted odds ratio (aOR) for 30-day mortality between patients who received a transfusion with a high FFP:RBC ratio and those who received one with a low FFP:RBC ratio (aOR=1.10, P=0.65). (The analysis was adjusted for patient age and total units of RBCs transfused.)
Among patients undergoing vascular surgery, those who received transfusions with a high FFP:RBC ratio were less likely to die within 30 days than those who received transfusions with a low FFP:RBC ratio (aOR=0.16, P=0.02).
However, among general surgery and medical service patients, those receiving transfusions with a high FFP:RBC ratio were more likely to die within 30 days than those receiving low-ratio transfusions. The aOR was 4.27 (P=0.02) for general surgery and 8.48 (P=0.02) for medicine.
“Finding evidence of increased mortality in some patients was surprising because that is directly contradictory to what is expected and intended,” Dr Yeh said. “Avoiding unnecessary FFP transfusion is important because there have been reports that associated the use of excess FFP with worse outcomes among patients that required less-than-massive transfusions.”
“Because our study is retrospective, it can only point to the need for further research. Ratio-based transfusion has been studied in trauma patients, most recently in a landmark, multicenter, randomized study called the PROPRR trial. Similar studies now need to be performed in non-trauma patients before the approach can be accepted as standard practice here at MGH [Massachusetts General Hospital] and elsewhere.” ![]()
FDA clears push-button blood draw device
The US Food and Drug Administration (FDA) has granted 510(k) clearance for a push-button blood collection device called TAP.
It provides “virtually painless, simple, and fast” blood collection, according to Seventh Sense Biosystems, Inc., the company marketing the device.
The FDA clearance allows healthcare workers to use TAP only for the collection of capillary blood for hemoglobin A1c testing.
However, Seventh Sense Biosystems said it is working with the FDA to expand the use of TAP to add additional tests, as well as at-home blood collection.
How TAP works
The TAP device is placed on a patient’s upper arm, and blood collection starts with the press of a button. The process typically takes 2 to 3 minutes.
When TAP is placed on the arm, the base of the device generates a seal with the skin to create a vacuum. When the user presses the button, TAP deploys microneedles that puncture the skin above the dermis.
The vacuum draws capillary blood out of the micropunctures and through microfluidic channels into a collection chamber prefilled with lithium heparin.
TAP collects up to 100 μL of blood. To transfer the blood to an analyzer, a precision pipette is placed in an access port at the bottom of the device.
Seventh Sense Biosystems said it will launch TAP over the coming months. For up-to-date information, visit www.7sbio.com. ![]()
The US Food and Drug Administration (FDA) has granted 510(k) clearance for a push-button blood collection device called TAP.
It provides “virtually painless, simple, and fast” blood collection, according to Seventh Sense Biosystems, Inc., the company marketing the device.
The FDA clearance allows healthcare workers to use TAP only for the collection of capillary blood for hemoglobin A1c testing.
However, Seventh Sense Biosystems said it is working with the FDA to expand the use of TAP to add additional tests, as well as at-home blood collection.
How TAP works
The TAP device is placed on a patient’s upper arm, and blood collection starts with the press of a button. The process typically takes 2 to 3 minutes.
When TAP is placed on the arm, the base of the device generates a seal with the skin to create a vacuum. When the user presses the button, TAP deploys microneedles that puncture the skin above the dermis.
The vacuum draws capillary blood out of the micropunctures and through microfluidic channels into a collection chamber prefilled with lithium heparin.
TAP collects up to 100 μL of blood. To transfer the blood to an analyzer, a precision pipette is placed in an access port at the bottom of the device.
Seventh Sense Biosystems said it will launch TAP over the coming months. For up-to-date information, visit www.7sbio.com. ![]()
The US Food and Drug Administration (FDA) has granted 510(k) clearance for a push-button blood collection device called TAP.
It provides “virtually painless, simple, and fast” blood collection, according to Seventh Sense Biosystems, Inc., the company marketing the device.
The FDA clearance allows healthcare workers to use TAP only for the collection of capillary blood for hemoglobin A1c testing.
However, Seventh Sense Biosystems said it is working with the FDA to expand the use of TAP to add additional tests, as well as at-home blood collection.
How TAP works
The TAP device is placed on a patient’s upper arm, and blood collection starts with the press of a button. The process typically takes 2 to 3 minutes.
When TAP is placed on the arm, the base of the device generates a seal with the skin to create a vacuum. When the user presses the button, TAP deploys microneedles that puncture the skin above the dermis.
The vacuum draws capillary blood out of the micropunctures and through microfluidic channels into a collection chamber prefilled with lithium heparin.
TAP collects up to 100 μL of blood. To transfer the blood to an analyzer, a precision pipette is placed in an access port at the bottom of the device.
Seventh Sense Biosystems said it will launch TAP over the coming months. For up-to-date information, visit www.7sbio.com. ![]()