User login
STS releases public surgical outcomes report
The Society of Thoracic Surgeons has released a public online report of national surgical outcomes from its Congenital Heart Surgery Database, the association has announced.
The STS report focuses on pediatric and congenital cardiac malformations, and includes 4-year observed, expected, and risk-adjusted mortality rates, the society said in a statement.
Twenty-five sites participated in the first round of STS public online reporting, similar to the observed participation in the first round of public reporting in the STS Adult Cardiac Surgery Database, which started in 2010.
“Reporting hospital surgical outcomes using risk-adjusted analysis is extremely important because it allows for a fair assessment, on a level playing field, of outcomes across hospitals that treat different populations of patients,” Dr. Marshall L. Jacobs, STS CHSD Task Force chair, said in the statement.
For more information, visit http://www.sts.org/quality-research-patient-safety/sts-public-reporting-online.
The Society of Thoracic Surgeons has released a public online report of national surgical outcomes from its Congenital Heart Surgery Database, the association has announced.
The STS report focuses on pediatric and congenital cardiac malformations, and includes 4-year observed, expected, and risk-adjusted mortality rates, the society said in a statement.
Twenty-five sites participated in the first round of STS public online reporting, similar to the observed participation in the first round of public reporting in the STS Adult Cardiac Surgery Database, which started in 2010.
“Reporting hospital surgical outcomes using risk-adjusted analysis is extremely important because it allows for a fair assessment, on a level playing field, of outcomes across hospitals that treat different populations of patients,” Dr. Marshall L. Jacobs, STS CHSD Task Force chair, said in the statement.
For more information, visit http://www.sts.org/quality-research-patient-safety/sts-public-reporting-online.
The Society of Thoracic Surgeons has released a public online report of national surgical outcomes from its Congenital Heart Surgery Database, the association has announced.
The STS report focuses on pediatric and congenital cardiac malformations, and includes 4-year observed, expected, and risk-adjusted mortality rates, the society said in a statement.
Twenty-five sites participated in the first round of STS public online reporting, similar to the observed participation in the first round of public reporting in the STS Adult Cardiac Surgery Database, which started in 2010.
“Reporting hospital surgical outcomes using risk-adjusted analysis is extremely important because it allows for a fair assessment, on a level playing field, of outcomes across hospitals that treat different populations of patients,” Dr. Marshall L. Jacobs, STS CHSD Task Force chair, said in the statement.
For more information, visit http://www.sts.org/quality-research-patient-safety/sts-public-reporting-online.
Anatomy of VSD in outflow tract defects indicates a continuum and has surgical relevance
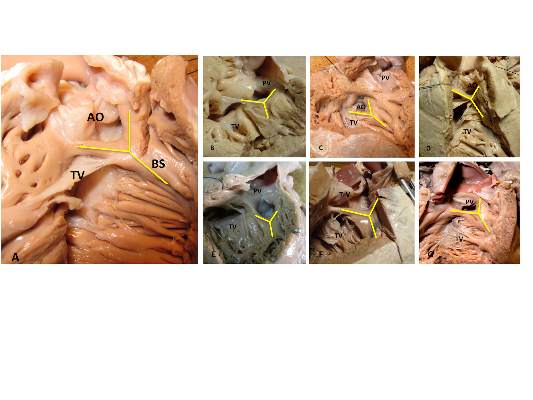
The outlet ventricular septal defect is a cornerstone of the outflow tract defects and exists on a continuum that is anatomically different from the isolated central perimembranous VSD, according to the results of an observational study of 277 preserved heart specimens with isolated outlet ventricular septal defect without subpulmonary stenosis.
“In all of the specimens studied, the VSD always opened in the outlet of the right ventricle, cradled between the two limbs of the septal band, irrespective of the presence or absence of a fibrous continuity between the aortic and tricuspid valves, and the presence of an outlet septum,” according to the report published in the March issue of the Journal of Thoracic and Cardiovascular Surgery by Dr. Meriem Mostefa-Kara of the Paris Descartes University and her colleagues.
The 277 specimens comprised 19 with isolated ventricular septal defect; 71 with tetralogy of Fallot (TOF); 51 with TOF with pulmonary atresia (PA); 54 with common arterial trunk (CAT); 65 with double-outlet right ventricle (DORV), with subaortic, doubly committed, or subpulmonary ventricular septal defect; and 17 with interrupted aortic arch (IAA) type B (doi:10.1016/j.jtcvs.2014.11.087).
Previous studies have shown that all malalignment defects include a VSD because of the malalignment and the absence of fusion between the outlet septum and the rest of the ventricular septum, and all authors agree that this VSD is cradled between the two limbs of the septal band, according to the researchers.
They found such an outlet VSD in all of the heart specimens studied, Dr. Mostefa-Kara and her colleagues added. In addition, they found that its anatomic variants were distributed differently according to the defect involved. This was especially true when focusing of the posteroinferior rim and particularly on the aortic-tricuspid fibrous continuity. In addition, this continuity occurred with different frequency among the various outflow tract defects studied.
They found the highest rate of continuity in isolated outlet VSD, then decreasing progressively from TOF to TOF-PA, then DORV, becoming “exceedingly rare” in CAT and absent in IAA type B.
The researchers also analyzed 26 hearts with isolated central perimembranous VSD from their anatomic collection and compared these with the outlet VSD hearts. All 26 of these VSDs were located behind the septal leaflet of the tricuspid valve, under the posteroinferior limb of the septal band, and NOT between the two limbs of the septal band as was the case with the outlet VSDs.
This led them to state that there was a “blatant anatomical difference between the these two types of VSDs,” and pointed out the risk of confusion. “The presence of a fibrous continuity at the posteroinferior rim of the VSD is important for the surgeon, because it makes the conduction axis vulnerable during surgery and therefore must be described specifically in the preoperative assessment of the defect,” they warned.
“This anatomic approach places the outlet VSD as a cornerstone of the outflow tract defects, anatomically different from the isolated central perimembranous VSD. This may help us to better understand the anatomy of the VSDs and to clarify their classification and terminology,” Dr. Mostefa-Kara and her colleagues concluded.
The study was sponsored by the French Society of Cardiology. The authors reported having no relevant disclosures.
The Paris researchers’ study is important for several reasons, according to the invited editorial commentary by Dr. Robert H. Anderson (doi:10.1016/j,jtcvs.2014.12.003). “First, it shows that careful examination of archives of autopsied hearts can still provide new information. Second, to provide all the information required to achieve safe and secure surgical closures of channels between the ventricles, they emphasize that knowledge is required how the defect opens toward the right ventricle and regarding the boundaries around which the surgeon will place a patch to restore septal integrity. The location of the defect relative to the right ventricle is geography. The details of the margins of the channel requiring closure represent its geometry. In earlier years, investigators tended to use either the geography or the geometry to provide their definitions, or else they accorded priority to one of these features. Both features are surgically important.” In addition, “as the Parisian investigators stress, it is not sufficient simply to state that a defect is perimembranous. We should now be distinguishing between perimembranous defects opening centrally, those that open to the outlet of the right ventricle between the limbs of the septal band, and those that can open to the right ventricular inlet. Another important feature of their research is the presence or absence of septal malalignment.”
Dr. Anderson is a professorial fellow at the Institute of Genetic Medicine, Newcastle University, Newcastle-upon-Tyne, England.
The Paris researchers’ study is important for several reasons, according to the invited editorial commentary by Dr. Robert H. Anderson (doi:10.1016/j,jtcvs.2014.12.003). “First, it shows that careful examination of archives of autopsied hearts can still provide new information. Second, to provide all the information required to achieve safe and secure surgical closures of channels between the ventricles, they emphasize that knowledge is required how the defect opens toward the right ventricle and regarding the boundaries around which the surgeon will place a patch to restore septal integrity. The location of the defect relative to the right ventricle is geography. The details of the margins of the channel requiring closure represent its geometry. In earlier years, investigators tended to use either the geography or the geometry to provide their definitions, or else they accorded priority to one of these features. Both features are surgically important.” In addition, “as the Parisian investigators stress, it is not sufficient simply to state that a defect is perimembranous. We should now be distinguishing between perimembranous defects opening centrally, those that open to the outlet of the right ventricle between the limbs of the septal band, and those that can open to the right ventricular inlet. Another important feature of their research is the presence or absence of septal malalignment.”
Dr. Anderson is a professorial fellow at the Institute of Genetic Medicine, Newcastle University, Newcastle-upon-Tyne, England.
The Paris researchers’ study is important for several reasons, according to the invited editorial commentary by Dr. Robert H. Anderson (doi:10.1016/j,jtcvs.2014.12.003). “First, it shows that careful examination of archives of autopsied hearts can still provide new information. Second, to provide all the information required to achieve safe and secure surgical closures of channels between the ventricles, they emphasize that knowledge is required how the defect opens toward the right ventricle and regarding the boundaries around which the surgeon will place a patch to restore septal integrity. The location of the defect relative to the right ventricle is geography. The details of the margins of the channel requiring closure represent its geometry. In earlier years, investigators tended to use either the geography or the geometry to provide their definitions, or else they accorded priority to one of these features. Both features are surgically important.” In addition, “as the Parisian investigators stress, it is not sufficient simply to state that a defect is perimembranous. We should now be distinguishing between perimembranous defects opening centrally, those that open to the outlet of the right ventricle between the limbs of the septal band, and those that can open to the right ventricular inlet. Another important feature of their research is the presence or absence of septal malalignment.”
Dr. Anderson is a professorial fellow at the Institute of Genetic Medicine, Newcastle University, Newcastle-upon-Tyne, England.
The outlet ventricular septal defect is a cornerstone of the outflow tract defects and exists on a continuum that is anatomically different from the isolated central perimembranous VSD, according to the results of an observational study of 277 preserved heart specimens with isolated outlet ventricular septal defect without subpulmonary stenosis.
“In all of the specimens studied, the VSD always opened in the outlet of the right ventricle, cradled between the two limbs of the septal band, irrespective of the presence or absence of a fibrous continuity between the aortic and tricuspid valves, and the presence of an outlet septum,” according to the report published in the March issue of the Journal of Thoracic and Cardiovascular Surgery by Dr. Meriem Mostefa-Kara of the Paris Descartes University and her colleagues.
The 277 specimens comprised 19 with isolated ventricular septal defect; 71 with tetralogy of Fallot (TOF); 51 with TOF with pulmonary atresia (PA); 54 with common arterial trunk (CAT); 65 with double-outlet right ventricle (DORV), with subaortic, doubly committed, or subpulmonary ventricular septal defect; and 17 with interrupted aortic arch (IAA) type B (doi:10.1016/j.jtcvs.2014.11.087).
Previous studies have shown that all malalignment defects include a VSD because of the malalignment and the absence of fusion between the outlet septum and the rest of the ventricular septum, and all authors agree that this VSD is cradled between the two limbs of the septal band, according to the researchers.
They found such an outlet VSD in all of the heart specimens studied, Dr. Mostefa-Kara and her colleagues added. In addition, they found that its anatomic variants were distributed differently according to the defect involved. This was especially true when focusing of the posteroinferior rim and particularly on the aortic-tricuspid fibrous continuity. In addition, this continuity occurred with different frequency among the various outflow tract defects studied.
They found the highest rate of continuity in isolated outlet VSD, then decreasing progressively from TOF to TOF-PA, then DORV, becoming “exceedingly rare” in CAT and absent in IAA type B.
The researchers also analyzed 26 hearts with isolated central perimembranous VSD from their anatomic collection and compared these with the outlet VSD hearts. All 26 of these VSDs were located behind the septal leaflet of the tricuspid valve, under the posteroinferior limb of the septal band, and NOT between the two limbs of the septal band as was the case with the outlet VSDs.
This led them to state that there was a “blatant anatomical difference between the these two types of VSDs,” and pointed out the risk of confusion. “The presence of a fibrous continuity at the posteroinferior rim of the VSD is important for the surgeon, because it makes the conduction axis vulnerable during surgery and therefore must be described specifically in the preoperative assessment of the defect,” they warned.
“This anatomic approach places the outlet VSD as a cornerstone of the outflow tract defects, anatomically different from the isolated central perimembranous VSD. This may help us to better understand the anatomy of the VSDs and to clarify their classification and terminology,” Dr. Mostefa-Kara and her colleagues concluded.
The study was sponsored by the French Society of Cardiology. The authors reported having no relevant disclosures.
The outlet ventricular septal defect is a cornerstone of the outflow tract defects and exists on a continuum that is anatomically different from the isolated central perimembranous VSD, according to the results of an observational study of 277 preserved heart specimens with isolated outlet ventricular septal defect without subpulmonary stenosis.
“In all of the specimens studied, the VSD always opened in the outlet of the right ventricle, cradled between the two limbs of the septal band, irrespective of the presence or absence of a fibrous continuity between the aortic and tricuspid valves, and the presence of an outlet septum,” according to the report published in the March issue of the Journal of Thoracic and Cardiovascular Surgery by Dr. Meriem Mostefa-Kara of the Paris Descartes University and her colleagues.
The 277 specimens comprised 19 with isolated ventricular septal defect; 71 with tetralogy of Fallot (TOF); 51 with TOF with pulmonary atresia (PA); 54 with common arterial trunk (CAT); 65 with double-outlet right ventricle (DORV), with subaortic, doubly committed, or subpulmonary ventricular septal defect; and 17 with interrupted aortic arch (IAA) type B (doi:10.1016/j.jtcvs.2014.11.087).
Previous studies have shown that all malalignment defects include a VSD because of the malalignment and the absence of fusion between the outlet septum and the rest of the ventricular septum, and all authors agree that this VSD is cradled between the two limbs of the septal band, according to the researchers.
They found such an outlet VSD in all of the heart specimens studied, Dr. Mostefa-Kara and her colleagues added. In addition, they found that its anatomic variants were distributed differently according to the defect involved. This was especially true when focusing of the posteroinferior rim and particularly on the aortic-tricuspid fibrous continuity. In addition, this continuity occurred with different frequency among the various outflow tract defects studied.
They found the highest rate of continuity in isolated outlet VSD, then decreasing progressively from TOF to TOF-PA, then DORV, becoming “exceedingly rare” in CAT and absent in IAA type B.
The researchers also analyzed 26 hearts with isolated central perimembranous VSD from their anatomic collection and compared these with the outlet VSD hearts. All 26 of these VSDs were located behind the septal leaflet of the tricuspid valve, under the posteroinferior limb of the septal band, and NOT between the two limbs of the septal band as was the case with the outlet VSDs.
This led them to state that there was a “blatant anatomical difference between the these two types of VSDs,” and pointed out the risk of confusion. “The presence of a fibrous continuity at the posteroinferior rim of the VSD is important for the surgeon, because it makes the conduction axis vulnerable during surgery and therefore must be described specifically in the preoperative assessment of the defect,” they warned.
“This anatomic approach places the outlet VSD as a cornerstone of the outflow tract defects, anatomically different from the isolated central perimembranous VSD. This may help us to better understand the anatomy of the VSDs and to clarify their classification and terminology,” Dr. Mostefa-Kara and her colleagues concluded.
The study was sponsored by the French Society of Cardiology. The authors reported having no relevant disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The presence of a fibrous continuity at the postinferior rim of the VSD is important for the surgeon because it makes the conduction axis vulnerable during surgery and therefore must be described specifically in the preoperative assessment.
Major finding: The outlet VSD is a cornerstone of the outflow tract defects and exists on a continuum that is anatomically different from the isolated central perimembranous VSD.
Data source: The researchers examined 277 preserved heart specimens with isolated outlet ventricular septal defect.
Disclosures: The study was sponsored by the French Society of Cardiology. The authors reported having no relevant disclosures.
Confronting aspirin unresponsiveness in congenital heart surgery
Thrombosis occurs in up to 15% of pediatric patients following cardiac surgery, and is associated with increased mortality. Although aspirin is commonly administered to pediatric patients after high-risk congenital cardiac surgery to reduce thrombosis risk, aspirin responsiveness is rarely assessed, according to Dr. Sirisha Emani and colleagues .
“In our observational study, aspirin unresponsiveness occurred in approximately 11% of patients undergoing specific high-risk cardiac procedures, and postoperative thrombosis was associated with aspirin unresponsiveness in this patient population,” said Dr. Emani.
In order to determine whether inadequate response to aspirin was associated with increased risk of thrombosis following high-risk procedures, the researchers performed a prospective analysis of 62 patients undergoing congenital cardiac surgical procedures involving placement of prosthetic material into the circulation or coronary artery manipulation who received aspirin.
Response to aspirin was determined using the Verify Now system at least 48 hours following administration. Patients were prospectively monitored for development of thrombosis events by imaging (echocardiogram, cardiac catheterization, MRI) and review of clinical events (shunt thrombosis, stroke, or limb ischemia) until the time of hospital discharge.
Aspirin responsiveness was tested a median of 2 days after initiation of therapy. The rate of aspirin unresponsiveness (Aspirin Responsive Unit, ARU greater than 550) was 7/62 (11.3%) in all patients and was highest in patients less than 5 kg who received 20.25 mg aspirin. Thrombosis events were demonstrated in 7 patients (11.3%). Thrombosis was observed in 6 (86%) of 7 patients who were unresponsive to aspirin as opposed to 1 (2%) of 54 patients who were responsive to aspirin, a significant difference. In two neonates who were unresponsive at 20.25 and 40.5 mg of aspirin, increase in dosage to 40.5 and 81 mg, respectively, resulted in an aspirin response, suggesting insufficiency rather than true unresponsiveness.
“Monitoring of aspirin therapy and consideration of dose adjustment or alternative agents for unresponsive patients may be justified and warrants further investigation in a prospective trial,” concluded Dr. Emani.

|
Dr. Robert Jaquiss |
Aspirin is sometimes used in pediatric cardiac surgical patients with either therapeutic or prophylactic intent, and the anticipated anti-platelet activity is simply assumed to follow. This study demonstrates that in children, this assumption may be flawed in as many as 11% of patients. Furthermore, in those patients in whom the assumption of efficacy was wrong, thrombosis was alarmingly common. This information should be of concern to physicians and surgeons who prescribe aspirin for children with cardiovascular abnormalities, and certainly merits further study.
Dr. Robert Jaquiss is chief of pediatric heart surgery, Duke University Medical Center, Durham, N.C.

|
Dr. Robert Jaquiss |
Aspirin is sometimes used in pediatric cardiac surgical patients with either therapeutic or prophylactic intent, and the anticipated anti-platelet activity is simply assumed to follow. This study demonstrates that in children, this assumption may be flawed in as many as 11% of patients. Furthermore, in those patients in whom the assumption of efficacy was wrong, thrombosis was alarmingly common. This information should be of concern to physicians and surgeons who prescribe aspirin for children with cardiovascular abnormalities, and certainly merits further study.
Dr. Robert Jaquiss is chief of pediatric heart surgery, Duke University Medical Center, Durham, N.C.

|
Dr. Robert Jaquiss |
Aspirin is sometimes used in pediatric cardiac surgical patients with either therapeutic or prophylactic intent, and the anticipated anti-platelet activity is simply assumed to follow. This study demonstrates that in children, this assumption may be flawed in as many as 11% of patients. Furthermore, in those patients in whom the assumption of efficacy was wrong, thrombosis was alarmingly common. This information should be of concern to physicians and surgeons who prescribe aspirin for children with cardiovascular abnormalities, and certainly merits further study.
Dr. Robert Jaquiss is chief of pediatric heart surgery, Duke University Medical Center, Durham, N.C.
Thrombosis occurs in up to 15% of pediatric patients following cardiac surgery, and is associated with increased mortality. Although aspirin is commonly administered to pediatric patients after high-risk congenital cardiac surgery to reduce thrombosis risk, aspirin responsiveness is rarely assessed, according to Dr. Sirisha Emani and colleagues .
“In our observational study, aspirin unresponsiveness occurred in approximately 11% of patients undergoing specific high-risk cardiac procedures, and postoperative thrombosis was associated with aspirin unresponsiveness in this patient population,” said Dr. Emani.
In order to determine whether inadequate response to aspirin was associated with increased risk of thrombosis following high-risk procedures, the researchers performed a prospective analysis of 62 patients undergoing congenital cardiac surgical procedures involving placement of prosthetic material into the circulation or coronary artery manipulation who received aspirin.
Response to aspirin was determined using the Verify Now system at least 48 hours following administration. Patients were prospectively monitored for development of thrombosis events by imaging (echocardiogram, cardiac catheterization, MRI) and review of clinical events (shunt thrombosis, stroke, or limb ischemia) until the time of hospital discharge.
Aspirin responsiveness was tested a median of 2 days after initiation of therapy. The rate of aspirin unresponsiveness (Aspirin Responsive Unit, ARU greater than 550) was 7/62 (11.3%) in all patients and was highest in patients less than 5 kg who received 20.25 mg aspirin. Thrombosis events were demonstrated in 7 patients (11.3%). Thrombosis was observed in 6 (86%) of 7 patients who were unresponsive to aspirin as opposed to 1 (2%) of 54 patients who were responsive to aspirin, a significant difference. In two neonates who were unresponsive at 20.25 and 40.5 mg of aspirin, increase in dosage to 40.5 and 81 mg, respectively, resulted in an aspirin response, suggesting insufficiency rather than true unresponsiveness.
“Monitoring of aspirin therapy and consideration of dose adjustment or alternative agents for unresponsive patients may be justified and warrants further investigation in a prospective trial,” concluded Dr. Emani.
Thrombosis occurs in up to 15% of pediatric patients following cardiac surgery, and is associated with increased mortality. Although aspirin is commonly administered to pediatric patients after high-risk congenital cardiac surgery to reduce thrombosis risk, aspirin responsiveness is rarely assessed, according to Dr. Sirisha Emani and colleagues .
“In our observational study, aspirin unresponsiveness occurred in approximately 11% of patients undergoing specific high-risk cardiac procedures, and postoperative thrombosis was associated with aspirin unresponsiveness in this patient population,” said Dr. Emani.
In order to determine whether inadequate response to aspirin was associated with increased risk of thrombosis following high-risk procedures, the researchers performed a prospective analysis of 62 patients undergoing congenital cardiac surgical procedures involving placement of prosthetic material into the circulation or coronary artery manipulation who received aspirin.
Response to aspirin was determined using the Verify Now system at least 48 hours following administration. Patients were prospectively monitored for development of thrombosis events by imaging (echocardiogram, cardiac catheterization, MRI) and review of clinical events (shunt thrombosis, stroke, or limb ischemia) until the time of hospital discharge.
Aspirin responsiveness was tested a median of 2 days after initiation of therapy. The rate of aspirin unresponsiveness (Aspirin Responsive Unit, ARU greater than 550) was 7/62 (11.3%) in all patients and was highest in patients less than 5 kg who received 20.25 mg aspirin. Thrombosis events were demonstrated in 7 patients (11.3%). Thrombosis was observed in 6 (86%) of 7 patients who were unresponsive to aspirin as opposed to 1 (2%) of 54 patients who were responsive to aspirin, a significant difference. In two neonates who were unresponsive at 20.25 and 40.5 mg of aspirin, increase in dosage to 40.5 and 81 mg, respectively, resulted in an aspirin response, suggesting insufficiency rather than true unresponsiveness.
“Monitoring of aspirin therapy and consideration of dose adjustment or alternative agents for unresponsive patients may be justified and warrants further investigation in a prospective trial,” concluded Dr. Emani.
Efficacy, safety seen with transcatheter pulmonary valve
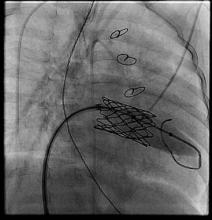
WASHINGTON - A transcatheter pulmonary valve system that provides a new right ventricle to pulmonary artery conduit to congenital heart disease patients without the need for open heart surgery performed a little better in a real-world registry at 10 U.S. centers than it had in the pivotal trial that led to the system's 2010 FDA approval.
The new results "confirm the strong performance of the Melody transcatheter pulmonary valve achieved by real-world providers with results comparable to the U.S. investigational device exemption [IDE] trial," Dr. Aimee K. Armstrong said at the annual meeting of the American College of Cardiology. The "high level" of 97% freedom from transcatheter pulmonary valve (TPV) dysfunction at 1 year "was better than in the IDE trial," where the level reached 94%, noted Dr. Armstrong of the University of Michigan in Ann Arbor.
The registry study, which the FDA mandated when it approved the Melody valve in 2010, ran during July 2010 to July 2012 at 10 U.S. centers that had not participated in the pivotal trial. The 99 patients who received an implant that stayed in place for at least 1 day ranged from 5 to 45 years old, with an average age of 20 years. Although patient follow-up averaged 22 months, the study's primary endpoint was acceptable hemodynamic function within the conduit at 6 months, with a prespecified performance goal of 75% of patients achieving this outcome. The outcome actually occurred in 97% of the 90 evaluable patients at 6 months, and in 88% of all 99 patients who received a conduit. The difference between each of these rates and the performance goal was statistically significant, Dr. Armstrong said.
The transcatheter valve showed excellent performance by other criteria as well. Acceptable hemodynamic function continued through 1 year in 94% of the 87 implanted patients with evaluable data at 12 months, which translated to 83% of the entire 99 patients in the implanted group. Severe or moderate pulmonary valve regurgitation existed in 85% of the patients before treatment; after treatment no patient had severe or moderate regurgitation, and after 1 year 63% had no regurgitation, 24% had trace, and 12% had mild regurgitation (figures total 99% because of rounding). The 1-year rate of 97% of patients free from dysfunction of their implanted valve appeared to surpass the 94% rate seen in the pivotal trial (Circulation 2010;122:507-16).
The results also showed that high right ventricular pressure prior to valve placement was the only variable independently associated with subsequent valve dysfunction. "Patients who go into the procedure with a very stenotic conduit are probably at higher risk for transcatheter pulmonary valve dysfunction down the road," she said.
The study was sponsored by Medtronic, which markets the Melody transcatheter pulmonary valve. Dr. Armstrong said she has received research funding from Medtronic and Edwards Lifesciences.

|
| Dr. Robert Jaquiss |
This study is an important post-approval demonstration that the excellent early results obtained in the original IDE trial in the United States can be reproduced or even exceeded with a broader rollout of the Melody valve to many more centers. The next set of data, which is eagerly anticipated, is the mid-term and longer results for the Melody valve, which will begin to answer questions about the durability of valve competence. Additional information about the performance of the valve in alternative anatomic settings, such as in failing stented bioprostheses - so-called "valve-in-valve" usage - is also beginning to accumulate.
Dr. Robert Jaquiss is professor of surgery and pediatrics and chief of pediatric heart surgery at Duke University School of Medicine and an associate medical editor for Vascular Specialist.

|
| Dr. Robert Jaquiss |
This study is an important post-approval demonstration that the excellent early results obtained in the original IDE trial in the United States can be reproduced or even exceeded with a broader rollout of the Melody valve to many more centers. The next set of data, which is eagerly anticipated, is the mid-term and longer results for the Melody valve, which will begin to answer questions about the durability of valve competence. Additional information about the performance of the valve in alternative anatomic settings, such as in failing stented bioprostheses - so-called "valve-in-valve" usage - is also beginning to accumulate.
Dr. Robert Jaquiss is professor of surgery and pediatrics and chief of pediatric heart surgery at Duke University School of Medicine and an associate medical editor for Vascular Specialist.

|
| Dr. Robert Jaquiss |
This study is an important post-approval demonstration that the excellent early results obtained in the original IDE trial in the United States can be reproduced or even exceeded with a broader rollout of the Melody valve to many more centers. The next set of data, which is eagerly anticipated, is the mid-term and longer results for the Melody valve, which will begin to answer questions about the durability of valve competence. Additional information about the performance of the valve in alternative anatomic settings, such as in failing stented bioprostheses - so-called "valve-in-valve" usage - is also beginning to accumulate.
Dr. Robert Jaquiss is professor of surgery and pediatrics and chief of pediatric heart surgery at Duke University School of Medicine and an associate medical editor for Vascular Specialist.
WASHINGTON - A transcatheter pulmonary valve system that provides a new right ventricle to pulmonary artery conduit to congenital heart disease patients without the need for open heart surgery performed a little better in a real-world registry at 10 U.S. centers than it had in the pivotal trial that led to the system's 2010 FDA approval.
The new results "confirm the strong performance of the Melody transcatheter pulmonary valve achieved by real-world providers with results comparable to the U.S. investigational device exemption [IDE] trial," Dr. Aimee K. Armstrong said at the annual meeting of the American College of Cardiology. The "high level" of 97% freedom from transcatheter pulmonary valve (TPV) dysfunction at 1 year "was better than in the IDE trial," where the level reached 94%, noted Dr. Armstrong of the University of Michigan in Ann Arbor.
The registry study, which the FDA mandated when it approved the Melody valve in 2010, ran during July 2010 to July 2012 at 10 U.S. centers that had not participated in the pivotal trial. The 99 patients who received an implant that stayed in place for at least 1 day ranged from 5 to 45 years old, with an average age of 20 years. Although patient follow-up averaged 22 months, the study's primary endpoint was acceptable hemodynamic function within the conduit at 6 months, with a prespecified performance goal of 75% of patients achieving this outcome. The outcome actually occurred in 97% of the 90 evaluable patients at 6 months, and in 88% of all 99 patients who received a conduit. The difference between each of these rates and the performance goal was statistically significant, Dr. Armstrong said.
The transcatheter valve showed excellent performance by other criteria as well. Acceptable hemodynamic function continued through 1 year in 94% of the 87 implanted patients with evaluable data at 12 months, which translated to 83% of the entire 99 patients in the implanted group. Severe or moderate pulmonary valve regurgitation existed in 85% of the patients before treatment; after treatment no patient had severe or moderate regurgitation, and after 1 year 63% had no regurgitation, 24% had trace, and 12% had mild regurgitation (figures total 99% because of rounding). The 1-year rate of 97% of patients free from dysfunction of their implanted valve appeared to surpass the 94% rate seen in the pivotal trial (Circulation 2010;122:507-16).
The results also showed that high right ventricular pressure prior to valve placement was the only variable independently associated with subsequent valve dysfunction. "Patients who go into the procedure with a very stenotic conduit are probably at higher risk for transcatheter pulmonary valve dysfunction down the road," she said.
The study was sponsored by Medtronic, which markets the Melody transcatheter pulmonary valve. Dr. Armstrong said she has received research funding from Medtronic and Edwards Lifesciences.
WASHINGTON - A transcatheter pulmonary valve system that provides a new right ventricle to pulmonary artery conduit to congenital heart disease patients without the need for open heart surgery performed a little better in a real-world registry at 10 U.S. centers than it had in the pivotal trial that led to the system's 2010 FDA approval.
The new results "confirm the strong performance of the Melody transcatheter pulmonary valve achieved by real-world providers with results comparable to the U.S. investigational device exemption [IDE] trial," Dr. Aimee K. Armstrong said at the annual meeting of the American College of Cardiology. The "high level" of 97% freedom from transcatheter pulmonary valve (TPV) dysfunction at 1 year "was better than in the IDE trial," where the level reached 94%, noted Dr. Armstrong of the University of Michigan in Ann Arbor.
The registry study, which the FDA mandated when it approved the Melody valve in 2010, ran during July 2010 to July 2012 at 10 U.S. centers that had not participated in the pivotal trial. The 99 patients who received an implant that stayed in place for at least 1 day ranged from 5 to 45 years old, with an average age of 20 years. Although patient follow-up averaged 22 months, the study's primary endpoint was acceptable hemodynamic function within the conduit at 6 months, with a prespecified performance goal of 75% of patients achieving this outcome. The outcome actually occurred in 97% of the 90 evaluable patients at 6 months, and in 88% of all 99 patients who received a conduit. The difference between each of these rates and the performance goal was statistically significant, Dr. Armstrong said.
The transcatheter valve showed excellent performance by other criteria as well. Acceptable hemodynamic function continued through 1 year in 94% of the 87 implanted patients with evaluable data at 12 months, which translated to 83% of the entire 99 patients in the implanted group. Severe or moderate pulmonary valve regurgitation existed in 85% of the patients before treatment; after treatment no patient had severe or moderate regurgitation, and after 1 year 63% had no regurgitation, 24% had trace, and 12% had mild regurgitation (figures total 99% because of rounding). The 1-year rate of 97% of patients free from dysfunction of their implanted valve appeared to surpass the 94% rate seen in the pivotal trial (Circulation 2010;122:507-16).
The results also showed that high right ventricular pressure prior to valve placement was the only variable independently associated with subsequent valve dysfunction. "Patients who go into the procedure with a very stenotic conduit are probably at higher risk for transcatheter pulmonary valve dysfunction down the road," she said.
The study was sponsored by Medtronic, which markets the Melody transcatheter pulmonary valve. Dr. Armstrong said she has received research funding from Medtronic and Edwards Lifesciences.
Key clinical point: The Melody transcatheter pulmonary valve system worked as well in a real world registry as it did in its pivotal trial as a conduit between the right ventricle and pulmonary artery.
Major finding: Acceptable hemodynamic function at 6 months occurred in 88% of implanted patients, significantly surpassing the 75% performance goal.
Data source: A series of 99 patients who received a transcatheter pulmonary valve at any of 10 participating U.S. centers.
Disclosures: The study was sponsored by Medtronic, which markets the Melody transcatheter pulmonary valve. Dr. Armstrong said that she has received consultant fees and honoraria from Siemens Healthcare and St. Jude Medical, and has received research funding from Medtronic and Edwards Lifesciences.
Subclinical seizures a risk during cardiac surgery
TORONTO – Routine EEG monitoring after surgery with cardiopulmonary bypass in neonates revealed a seizure incidence of 8% in a recent study. In most cases (85%), seizure activity was detectable only on EEG and would not have been identified or treated without EEG monitoring, reported Dr. Maryam Y. Naim, of Children’s Hospital of Philadelphia, during the AATS Annual Meeting.
Of concern, status epilepticus was noted in 62% of neonates with seizures, and mortality was higher in babies with seizures versus those without (38% vs. 3%; P less than .01). "Postoperative seizures are associated with worse neurological outcomes," said Dr. Naim. In addition to being a biomarker of underlying brain injury, there is some evidence that the seizures themselves may cause secondary brain injury.
A total of 161 neonates had 48-hours of EEG monitoring begun within 6 hours of cardiac surgery with CPB. The median gestational age of the cohort was 39 weeks, 16% were premature, and 13% had identified genetic defects. The median age at surgery was 5 days. Deep hypothermic circulatory arrest was used in 48% of surgeries (median time, 48 minutes), 16% had open chest with delayed sternal closure, and 9% had a cardiac arrest.
Seizures were detected in 13 (8%), with a median onset of 20 hours after return to the cardiac ICU (CICU) from surgery. Seizures were subclinical, or EEG only, in 11 patients (85%), electroclinical in the other 2 (15%), and status epilepticus was seen in 8 (62%). When seizures occurred, the patient was treated with antiseizure medications. Abnormal vital signs or movements suggestive of seizure activity were noted at the bedside; although such events were recorded in 32 patients (22%), none had EEG correlates consistent with seizure activity.
"Neonates with all types of heart disease had seizures ... " said Dr. Naim. " ... with a highest percentage occurring in those with single ventricles and arch obstruction."
Neuroimaging studies were reviewed by a neurologist to determine any association between injury and seizure location. Although neonates with and without seizures had similar CICU lengths of stay, mortality was higher in those with seizures (38% vs. 3%; P less than .01). No predictors of seizures were identified on multivariable analysis.
"Based on these data, we are continuing routine postoperative EEG monitoring in all neonates following surgery with CPB," she said.
While not discredited in any way, Dr. Naim’s data were met with a fair amount of pushback from the gathered group of pediatric cardiothoracic surgical experts. An informal poll of the audience showed that 80%-90% do not routinely monitor neonates for seizures post-CPB despite ACNS recommendations, and several of the comments questioned the technical and financial feasibility of routine EEG monitoring.
Said the invited discussant, Dr. Frank Pigula, a cardiac surgeon from Boston Children’s Hospital, "In all the groups that have studied this, in all patients who have had a seizure, there were documented brain abnormalities. So, the ways I picture these data are that a seizure is a sign of an underlying brain injury, much like a fever is a sign of an underlying infection.
"And you’ve made a good case for the routine postoperative surveillance for seizures; I’m sure everyone would agree that treating seizures is a good thing, but is there any evidence showing us that the early identification and treatment of seizures improves outcomes, either developmental delays or mortality?
In response, Dr. Naim noted that all the CHOP seizure sufferers were treated, whether they had EEG only or clinical seizures, and, at the 4-year mark, they are showing fewer neurodevelopmental issues than previous cohorts of untreated neonates.
"I think one thing that is very concerning is emerging evidence that the seizures themselves cause secondary brain injury," she said.
Dr. Naim and Dr. Pigula reported having no financial disclosures.
TORONTO – Routine EEG monitoring after surgery with cardiopulmonary bypass in neonates revealed a seizure incidence of 8% in a recent study. In most cases (85%), seizure activity was detectable only on EEG and would not have been identified or treated without EEG monitoring, reported Dr. Maryam Y. Naim, of Children’s Hospital of Philadelphia, during the AATS Annual Meeting.
Of concern, status epilepticus was noted in 62% of neonates with seizures, and mortality was higher in babies with seizures versus those without (38% vs. 3%; P less than .01). "Postoperative seizures are associated with worse neurological outcomes," said Dr. Naim. In addition to being a biomarker of underlying brain injury, there is some evidence that the seizures themselves may cause secondary brain injury.
A total of 161 neonates had 48-hours of EEG monitoring begun within 6 hours of cardiac surgery with CPB. The median gestational age of the cohort was 39 weeks, 16% were premature, and 13% had identified genetic defects. The median age at surgery was 5 days. Deep hypothermic circulatory arrest was used in 48% of surgeries (median time, 48 minutes), 16% had open chest with delayed sternal closure, and 9% had a cardiac arrest.
Seizures were detected in 13 (8%), with a median onset of 20 hours after return to the cardiac ICU (CICU) from surgery. Seizures were subclinical, or EEG only, in 11 patients (85%), electroclinical in the other 2 (15%), and status epilepticus was seen in 8 (62%). When seizures occurred, the patient was treated with antiseizure medications. Abnormal vital signs or movements suggestive of seizure activity were noted at the bedside; although such events were recorded in 32 patients (22%), none had EEG correlates consistent with seizure activity.
"Neonates with all types of heart disease had seizures ... " said Dr. Naim. " ... with a highest percentage occurring in those with single ventricles and arch obstruction."
Neuroimaging studies were reviewed by a neurologist to determine any association between injury and seizure location. Although neonates with and without seizures had similar CICU lengths of stay, mortality was higher in those with seizures (38% vs. 3%; P less than .01). No predictors of seizures were identified on multivariable analysis.
"Based on these data, we are continuing routine postoperative EEG monitoring in all neonates following surgery with CPB," she said.
While not discredited in any way, Dr. Naim’s data were met with a fair amount of pushback from the gathered group of pediatric cardiothoracic surgical experts. An informal poll of the audience showed that 80%-90% do not routinely monitor neonates for seizures post-CPB despite ACNS recommendations, and several of the comments questioned the technical and financial feasibility of routine EEG monitoring.
Said the invited discussant, Dr. Frank Pigula, a cardiac surgeon from Boston Children’s Hospital, "In all the groups that have studied this, in all patients who have had a seizure, there were documented brain abnormalities. So, the ways I picture these data are that a seizure is a sign of an underlying brain injury, much like a fever is a sign of an underlying infection.
"And you’ve made a good case for the routine postoperative surveillance for seizures; I’m sure everyone would agree that treating seizures is a good thing, but is there any evidence showing us that the early identification and treatment of seizures improves outcomes, either developmental delays or mortality?
In response, Dr. Naim noted that all the CHOP seizure sufferers were treated, whether they had EEG only or clinical seizures, and, at the 4-year mark, they are showing fewer neurodevelopmental issues than previous cohorts of untreated neonates.
"I think one thing that is very concerning is emerging evidence that the seizures themselves cause secondary brain injury," she said.
Dr. Naim and Dr. Pigula reported having no financial disclosures.
TORONTO – Routine EEG monitoring after surgery with cardiopulmonary bypass in neonates revealed a seizure incidence of 8% in a recent study. In most cases (85%), seizure activity was detectable only on EEG and would not have been identified or treated without EEG monitoring, reported Dr. Maryam Y. Naim, of Children’s Hospital of Philadelphia, during the AATS Annual Meeting.
Of concern, status epilepticus was noted in 62% of neonates with seizures, and mortality was higher in babies with seizures versus those without (38% vs. 3%; P less than .01). "Postoperative seizures are associated with worse neurological outcomes," said Dr. Naim. In addition to being a biomarker of underlying brain injury, there is some evidence that the seizures themselves may cause secondary brain injury.
A total of 161 neonates had 48-hours of EEG monitoring begun within 6 hours of cardiac surgery with CPB. The median gestational age of the cohort was 39 weeks, 16% were premature, and 13% had identified genetic defects. The median age at surgery was 5 days. Deep hypothermic circulatory arrest was used in 48% of surgeries (median time, 48 minutes), 16% had open chest with delayed sternal closure, and 9% had a cardiac arrest.
Seizures were detected in 13 (8%), with a median onset of 20 hours after return to the cardiac ICU (CICU) from surgery. Seizures were subclinical, or EEG only, in 11 patients (85%), electroclinical in the other 2 (15%), and status epilepticus was seen in 8 (62%). When seizures occurred, the patient was treated with antiseizure medications. Abnormal vital signs or movements suggestive of seizure activity were noted at the bedside; although such events were recorded in 32 patients (22%), none had EEG correlates consistent with seizure activity.
"Neonates with all types of heart disease had seizures ... " said Dr. Naim. " ... with a highest percentage occurring in those with single ventricles and arch obstruction."
Neuroimaging studies were reviewed by a neurologist to determine any association between injury and seizure location. Although neonates with and without seizures had similar CICU lengths of stay, mortality was higher in those with seizures (38% vs. 3%; P less than .01). No predictors of seizures were identified on multivariable analysis.
"Based on these data, we are continuing routine postoperative EEG monitoring in all neonates following surgery with CPB," she said.
While not discredited in any way, Dr. Naim’s data were met with a fair amount of pushback from the gathered group of pediatric cardiothoracic surgical experts. An informal poll of the audience showed that 80%-90% do not routinely monitor neonates for seizures post-CPB despite ACNS recommendations, and several of the comments questioned the technical and financial feasibility of routine EEG monitoring.
Said the invited discussant, Dr. Frank Pigula, a cardiac surgeon from Boston Children’s Hospital, "In all the groups that have studied this, in all patients who have had a seizure, there were documented brain abnormalities. So, the ways I picture these data are that a seizure is a sign of an underlying brain injury, much like a fever is a sign of an underlying infection.
"And you’ve made a good case for the routine postoperative surveillance for seizures; I’m sure everyone would agree that treating seizures is a good thing, but is there any evidence showing us that the early identification and treatment of seizures improves outcomes, either developmental delays or mortality?
In response, Dr. Naim noted that all the CHOP seizure sufferers were treated, whether they had EEG only or clinical seizures, and, at the 4-year mark, they are showing fewer neurodevelopmental issues than previous cohorts of untreated neonates.
"I think one thing that is very concerning is emerging evidence that the seizures themselves cause secondary brain injury," she said.
Dr. Naim and Dr. Pigula reported having no financial disclosures.
Delayed revisions led to worse congenital outcomes
In previous studies on patients under 6 months of age undergoing a wide range of congenital cardiac operations, Dr. Meena Nathan and her colleagues at Boston Children’s Hospital found that immediate revisions of procedures intraoperatively that resulted in adequate anatomic correction of residual defects did not affect outcomes, but that delayed revisions of residual lesions resulted in worse patient outcomes.
Dr. Nathan presented the results of a larger prospective cohort of patients that she and her colleagues studied who were followed from index surgery to discharge from January 2011 to September 2013.
Patients were divided into four groups: a) intraoperative revisions of residual lesion, b) delayed postoperative revision of residual lesions during the same hospital stay, c) both intraoperative and delayed (BOTH) revision of residual lesions, d) and no revisions (neither intraoperative nor postoperative revision), Dr. Nathan said at the annual meeting of the American Association for Thoracic Surgery.
They used linear and logistic regression to compare the outcomes mortality, complications (excluding unplanned postoperative reinterventions) and postoperative hospital length of stay across the four groups (using patients who had intraoperative revisions only as reference group).
"We adjusted for baseline patient risk including age, prematurity, presence of extracardiac anomalies, and RACHS-1 risk category, each of which could contribute to the difference in outcomes," according to Dr. Nathan.
"In addition, to allow inclusion of all patients in the risk-adjusted analyses, we added two additional categories to the RACHS-1 categories: all patients less than 18 years of age with non–RACHS-1 categorizable procedures, and adults greater than 18 years who are not eligible for RACHS-1 risk adjustment," Dr. Nathan added.
A total of 2,427 patients were discharged after congenital cardiac operations during the time period studied.
As might be expected, on multivariable modeling, adjusting for other significant patient factors, the no-revisions group fared better than the other three groups. The intraoperative revision group had significantly lower postoperative length of stay and complication rates when compared to the delayed postoperative revision and the BOTH group, but they showed no significant differences in mortality compared to these two groups.
On subgroup analysis of the intraoperative revision group, 86% left the hospital with an optimal or adequate repair on discharge echocardiogram, Dr. Nathan added.
"We found that the intraoperative correction of residual lesions results in a shorter length of stay and lower complications when compared to those patients who underwent delayed postoperative revision of residual lesion," she concluded.
Dr. Nathan reported that she had no relevant disclosures.
In previous studies on patients under 6 months of age undergoing a wide range of congenital cardiac operations, Dr. Meena Nathan and her colleagues at Boston Children’s Hospital found that immediate revisions of procedures intraoperatively that resulted in adequate anatomic correction of residual defects did not affect outcomes, but that delayed revisions of residual lesions resulted in worse patient outcomes.
Dr. Nathan presented the results of a larger prospective cohort of patients that she and her colleagues studied who were followed from index surgery to discharge from January 2011 to September 2013.
Patients were divided into four groups: a) intraoperative revisions of residual lesion, b) delayed postoperative revision of residual lesions during the same hospital stay, c) both intraoperative and delayed (BOTH) revision of residual lesions, d) and no revisions (neither intraoperative nor postoperative revision), Dr. Nathan said at the annual meeting of the American Association for Thoracic Surgery.
They used linear and logistic regression to compare the outcomes mortality, complications (excluding unplanned postoperative reinterventions) and postoperative hospital length of stay across the four groups (using patients who had intraoperative revisions only as reference group).
"We adjusted for baseline patient risk including age, prematurity, presence of extracardiac anomalies, and RACHS-1 risk category, each of which could contribute to the difference in outcomes," according to Dr. Nathan.
"In addition, to allow inclusion of all patients in the risk-adjusted analyses, we added two additional categories to the RACHS-1 categories: all patients less than 18 years of age with non–RACHS-1 categorizable procedures, and adults greater than 18 years who are not eligible for RACHS-1 risk adjustment," Dr. Nathan added.
A total of 2,427 patients were discharged after congenital cardiac operations during the time period studied.
As might be expected, on multivariable modeling, adjusting for other significant patient factors, the no-revisions group fared better than the other three groups. The intraoperative revision group had significantly lower postoperative length of stay and complication rates when compared to the delayed postoperative revision and the BOTH group, but they showed no significant differences in mortality compared to these two groups.
On subgroup analysis of the intraoperative revision group, 86% left the hospital with an optimal or adequate repair on discharge echocardiogram, Dr. Nathan added.
"We found that the intraoperative correction of residual lesions results in a shorter length of stay and lower complications when compared to those patients who underwent delayed postoperative revision of residual lesion," she concluded.
Dr. Nathan reported that she had no relevant disclosures.
In previous studies on patients under 6 months of age undergoing a wide range of congenital cardiac operations, Dr. Meena Nathan and her colleagues at Boston Children’s Hospital found that immediate revisions of procedures intraoperatively that resulted in adequate anatomic correction of residual defects did not affect outcomes, but that delayed revisions of residual lesions resulted in worse patient outcomes.
Dr. Nathan presented the results of a larger prospective cohort of patients that she and her colleagues studied who were followed from index surgery to discharge from January 2011 to September 2013.
Patients were divided into four groups: a) intraoperative revisions of residual lesion, b) delayed postoperative revision of residual lesions during the same hospital stay, c) both intraoperative and delayed (BOTH) revision of residual lesions, d) and no revisions (neither intraoperative nor postoperative revision), Dr. Nathan said at the annual meeting of the American Association for Thoracic Surgery.
They used linear and logistic regression to compare the outcomes mortality, complications (excluding unplanned postoperative reinterventions) and postoperative hospital length of stay across the four groups (using patients who had intraoperative revisions only as reference group).
"We adjusted for baseline patient risk including age, prematurity, presence of extracardiac anomalies, and RACHS-1 risk category, each of which could contribute to the difference in outcomes," according to Dr. Nathan.
"In addition, to allow inclusion of all patients in the risk-adjusted analyses, we added two additional categories to the RACHS-1 categories: all patients less than 18 years of age with non–RACHS-1 categorizable procedures, and adults greater than 18 years who are not eligible for RACHS-1 risk adjustment," Dr. Nathan added.
A total of 2,427 patients were discharged after congenital cardiac operations during the time period studied.
As might be expected, on multivariable modeling, adjusting for other significant patient factors, the no-revisions group fared better than the other three groups. The intraoperative revision group had significantly lower postoperative length of stay and complication rates when compared to the delayed postoperative revision and the BOTH group, but they showed no significant differences in mortality compared to these two groups.
On subgroup analysis of the intraoperative revision group, 86% left the hospital with an optimal or adequate repair on discharge echocardiogram, Dr. Nathan added.
"We found that the intraoperative correction of residual lesions results in a shorter length of stay and lower complications when compared to those patients who underwent delayed postoperative revision of residual lesion," she concluded.
Dr. Nathan reported that she had no relevant disclosures.
Mitral replacement may grow with infant
NEW YORK – Physicians at Boston Children’s Hospital replaced the mitral valves of eight infants with irreparable mitral valve disease with a valve that offers the opportunity of sequential expansion as the child grows, according to Dr. Sitaram M. Emani. The results were presented at the 2013 Mitral Valve Conclave earlier this year.
"The Melody valve retains its competence if you expand it before putting it in. We asked whether the valve retains the ability to maintain competence even if expansion is performed after implantation as the patient grows," said Dr. Emani, a pediatric cardiac surgeon at Boston Children’s Hospital.
According to Dr. Emani, the current options for infants with damaged mitral valves that are beyond repair are replacement with mechanical or bioprosthetic valves or the Ross mitral procedure. Perhaps the main disadvantage of these options is the lack of a prosthetic valve small enough for an infant, one that is less than 12 mm in diameter. Another problem is the possibility of stenosis developing as the child grows, since the diameters of the prosthetics are fixed. Other drawbacks are that supra-annular fixation is generally associated with poor outcomes and that annular fixation limits the ability to upsize at reoperation.
The Melody valve is an externally stented bovine jugular vein graft that was designed for transcatheter pulmonary valve replacement. In this study, the valve was inserted surgically. The valve maintains competence over a range of sizes up to 22 mm. Although this valve is not approved for use for mitral valve replacement, the hope of using such a prosthetic is that it can be enlarged in the catheterization laboratory as the child grows.
Dr. Emani did a retrospective study of his experience with the Melody valve for mitral valve replacement in eight infants less than 12 months of age. The median age at implantation was 6 months (range, 1-9 months). Four infants had an atrioventricular canal (AVC) defect and four had congenital mitral valve stenosis. Most of the children had two prior operations for mitral valve repair. The longest follow-up to date has been 2 years.
At a median follow-up of 8 months, regurgitation on the echocardiogram was considered to be mild or less in all patients. The median gradient was 3 mm Hg (range, 2-7 mm Hg) on the immediate postoperative echocardiogram. Three patients developed a mild paravalvular leak; one of these patients had undergone aggressive stent resection, a modification Dr. Emani does not recommend. One patient developed left ventricular outflow tract obstruction (LVOTO), which Dr. Emani attributed to the lack of distal stent fixation in this patient. Another patient with an AVC defect developed complete heart block.
One patient who died 3 days postoperatively had heterotaxy, severe mitral regurgitation, and prior ventricular failure on extracorporeal membrane oxygenation support. That patient had undergone valve implantation as a last resort.
Three patients underwent sequential expansion about 6 months after implantation. After valve expansion, the median balloon size was 12 mm, ranging from 12 to 16 mm. None of the patients developed worsening valvular function and all had relief of obstruction. Transcatheter intervention was used to correct a paravalvular leak in one patient and to treat a left ventricular outflow tract problem in another. None of the patients developed endocarditis or a strut fracture, "although I worry about strut fracture if aggressive stent resection and manipulation is performed," he said at the meeting, which was sponsored by the AATS.
Dr. Emani offered some procedural tips. First, the Melody valve must be optimized for surgical implantation in infants. The length of the valve must be reduced by trimming it to reduce the chance of LVOTO or pulmonary vein obstruction. He recommends sizing the valves by echocardiogram and fixating the distal stent to the inferior free wall of the ventricle.
He reported that friction of the stent against the annulus prevents leakage. Early on he used a pericardial cuff to anchor to the annulus, particularly in patients who had undergone failed AVC repair. He tries to preserve at least part of the anterior leaflet to facilitate suture placement and create a "stand-off" from the LVOTO.
Dr. Emani also advised limiting intraoperative dilation to no more than 1 mm greater than the measured annulus. "Try not to overdilate at implantation to avoid heart block, LVOTO, and coronary compression. The nice thing is you don’t have to decide then and there what size you want. You can go back to the cath lab and, under direct visualization with the coronary view, you can dilate it under more controlled circumstances.
"The hope is that we will be able to dilate these valves as the patients grow into adolescence. If we can dilate them up to 22 mm, hopefully we will decrease the number of repeat replacements, delay the time to reoperation, and perhaps modify our thresholds for tolerating significant disease after unsuccessful repairs."
Dr. Emani reported no disclosures.
NEW YORK – Physicians at Boston Children’s Hospital replaced the mitral valves of eight infants with irreparable mitral valve disease with a valve that offers the opportunity of sequential expansion as the child grows, according to Dr. Sitaram M. Emani. The results were presented at the 2013 Mitral Valve Conclave earlier this year.
"The Melody valve retains its competence if you expand it before putting it in. We asked whether the valve retains the ability to maintain competence even if expansion is performed after implantation as the patient grows," said Dr. Emani, a pediatric cardiac surgeon at Boston Children’s Hospital.
According to Dr. Emani, the current options for infants with damaged mitral valves that are beyond repair are replacement with mechanical or bioprosthetic valves or the Ross mitral procedure. Perhaps the main disadvantage of these options is the lack of a prosthetic valve small enough for an infant, one that is less than 12 mm in diameter. Another problem is the possibility of stenosis developing as the child grows, since the diameters of the prosthetics are fixed. Other drawbacks are that supra-annular fixation is generally associated with poor outcomes and that annular fixation limits the ability to upsize at reoperation.
The Melody valve is an externally stented bovine jugular vein graft that was designed for transcatheter pulmonary valve replacement. In this study, the valve was inserted surgically. The valve maintains competence over a range of sizes up to 22 mm. Although this valve is not approved for use for mitral valve replacement, the hope of using such a prosthetic is that it can be enlarged in the catheterization laboratory as the child grows.
Dr. Emani did a retrospective study of his experience with the Melody valve for mitral valve replacement in eight infants less than 12 months of age. The median age at implantation was 6 months (range, 1-9 months). Four infants had an atrioventricular canal (AVC) defect and four had congenital mitral valve stenosis. Most of the children had two prior operations for mitral valve repair. The longest follow-up to date has been 2 years.
At a median follow-up of 8 months, regurgitation on the echocardiogram was considered to be mild or less in all patients. The median gradient was 3 mm Hg (range, 2-7 mm Hg) on the immediate postoperative echocardiogram. Three patients developed a mild paravalvular leak; one of these patients had undergone aggressive stent resection, a modification Dr. Emani does not recommend. One patient developed left ventricular outflow tract obstruction (LVOTO), which Dr. Emani attributed to the lack of distal stent fixation in this patient. Another patient with an AVC defect developed complete heart block.
One patient who died 3 days postoperatively had heterotaxy, severe mitral regurgitation, and prior ventricular failure on extracorporeal membrane oxygenation support. That patient had undergone valve implantation as a last resort.
Three patients underwent sequential expansion about 6 months after implantation. After valve expansion, the median balloon size was 12 mm, ranging from 12 to 16 mm. None of the patients developed worsening valvular function and all had relief of obstruction. Transcatheter intervention was used to correct a paravalvular leak in one patient and to treat a left ventricular outflow tract problem in another. None of the patients developed endocarditis or a strut fracture, "although I worry about strut fracture if aggressive stent resection and manipulation is performed," he said at the meeting, which was sponsored by the AATS.
Dr. Emani offered some procedural tips. First, the Melody valve must be optimized for surgical implantation in infants. The length of the valve must be reduced by trimming it to reduce the chance of LVOTO or pulmonary vein obstruction. He recommends sizing the valves by echocardiogram and fixating the distal stent to the inferior free wall of the ventricle.
He reported that friction of the stent against the annulus prevents leakage. Early on he used a pericardial cuff to anchor to the annulus, particularly in patients who had undergone failed AVC repair. He tries to preserve at least part of the anterior leaflet to facilitate suture placement and create a "stand-off" from the LVOTO.
Dr. Emani also advised limiting intraoperative dilation to no more than 1 mm greater than the measured annulus. "Try not to overdilate at implantation to avoid heart block, LVOTO, and coronary compression. The nice thing is you don’t have to decide then and there what size you want. You can go back to the cath lab and, under direct visualization with the coronary view, you can dilate it under more controlled circumstances.
"The hope is that we will be able to dilate these valves as the patients grow into adolescence. If we can dilate them up to 22 mm, hopefully we will decrease the number of repeat replacements, delay the time to reoperation, and perhaps modify our thresholds for tolerating significant disease after unsuccessful repairs."
Dr. Emani reported no disclosures.
NEW YORK – Physicians at Boston Children’s Hospital replaced the mitral valves of eight infants with irreparable mitral valve disease with a valve that offers the opportunity of sequential expansion as the child grows, according to Dr. Sitaram M. Emani. The results were presented at the 2013 Mitral Valve Conclave earlier this year.
"The Melody valve retains its competence if you expand it before putting it in. We asked whether the valve retains the ability to maintain competence even if expansion is performed after implantation as the patient grows," said Dr. Emani, a pediatric cardiac surgeon at Boston Children’s Hospital.
According to Dr. Emani, the current options for infants with damaged mitral valves that are beyond repair are replacement with mechanical or bioprosthetic valves or the Ross mitral procedure. Perhaps the main disadvantage of these options is the lack of a prosthetic valve small enough for an infant, one that is less than 12 mm in diameter. Another problem is the possibility of stenosis developing as the child grows, since the diameters of the prosthetics are fixed. Other drawbacks are that supra-annular fixation is generally associated with poor outcomes and that annular fixation limits the ability to upsize at reoperation.
The Melody valve is an externally stented bovine jugular vein graft that was designed for transcatheter pulmonary valve replacement. In this study, the valve was inserted surgically. The valve maintains competence over a range of sizes up to 22 mm. Although this valve is not approved for use for mitral valve replacement, the hope of using such a prosthetic is that it can be enlarged in the catheterization laboratory as the child grows.
Dr. Emani did a retrospective study of his experience with the Melody valve for mitral valve replacement in eight infants less than 12 months of age. The median age at implantation was 6 months (range, 1-9 months). Four infants had an atrioventricular canal (AVC) defect and four had congenital mitral valve stenosis. Most of the children had two prior operations for mitral valve repair. The longest follow-up to date has been 2 years.
At a median follow-up of 8 months, regurgitation on the echocardiogram was considered to be mild or less in all patients. The median gradient was 3 mm Hg (range, 2-7 mm Hg) on the immediate postoperative echocardiogram. Three patients developed a mild paravalvular leak; one of these patients had undergone aggressive stent resection, a modification Dr. Emani does not recommend. One patient developed left ventricular outflow tract obstruction (LVOTO), which Dr. Emani attributed to the lack of distal stent fixation in this patient. Another patient with an AVC defect developed complete heart block.
One patient who died 3 days postoperatively had heterotaxy, severe mitral regurgitation, and prior ventricular failure on extracorporeal membrane oxygenation support. That patient had undergone valve implantation as a last resort.
Three patients underwent sequential expansion about 6 months after implantation. After valve expansion, the median balloon size was 12 mm, ranging from 12 to 16 mm. None of the patients developed worsening valvular function and all had relief of obstruction. Transcatheter intervention was used to correct a paravalvular leak in one patient and to treat a left ventricular outflow tract problem in another. None of the patients developed endocarditis or a strut fracture, "although I worry about strut fracture if aggressive stent resection and manipulation is performed," he said at the meeting, which was sponsored by the AATS.
Dr. Emani offered some procedural tips. First, the Melody valve must be optimized for surgical implantation in infants. The length of the valve must be reduced by trimming it to reduce the chance of LVOTO or pulmonary vein obstruction. He recommends sizing the valves by echocardiogram and fixating the distal stent to the inferior free wall of the ventricle.
He reported that friction of the stent against the annulus prevents leakage. Early on he used a pericardial cuff to anchor to the annulus, particularly in patients who had undergone failed AVC repair. He tries to preserve at least part of the anterior leaflet to facilitate suture placement and create a "stand-off" from the LVOTO.
Dr. Emani also advised limiting intraoperative dilation to no more than 1 mm greater than the measured annulus. "Try not to overdilate at implantation to avoid heart block, LVOTO, and coronary compression. The nice thing is you don’t have to decide then and there what size you want. You can go back to the cath lab and, under direct visualization with the coronary view, you can dilate it under more controlled circumstances.
"The hope is that we will be able to dilate these valves as the patients grow into adolescence. If we can dilate them up to 22 mm, hopefully we will decrease the number of repeat replacements, delay the time to reoperation, and perhaps modify our thresholds for tolerating significant disease after unsuccessful repairs."
Dr. Emani reported no disclosures.
Risks for poorer outcomes of ASO for TGA
Neoaortic root dilation and neoaortic valve regurgitation are common complications in infants with transposition of the great arteries who undergo an arterial switch operation for repair, and the risk of developing these changes in the neoaorta increases over time, according to the results of a retrospective database study of patients at Children’s Hospital of Wisconsin.
In addition, when dilation occurs, the dimensions may progressively enlarge over time, making it important to maintain lifelong surveillance of this population.
Although perioperative mortality and long-term survival (assessed up to 30 years) has improved in more recent eras for use of an arterial switch operation (ASO) for transposition of the great arteries (TGA), these long-term studies have also shown important late complications that may contribute to late morbidity and the need for reoperation, according to Dr. Jennifer G. Co-Vu and her colleagues at the Medical College of Wisconsin, Milwaukee.
They performed their study to determine the prevalence of neoaortic root dilation and neoaortic valve regurgitation in patients treated at their institution and to determine risk factors involved in the development of these late complications.
Out of 247 patients with TGA treated with an ASO at the hospital, there were 124 patients who had at least one available postoperative transthoracic echocardiogram at least 1 year after the ASO. Median age of these patients was 0.2 months at the time of their ASO and 7.2 years at their last follow-up; 71% were boys (Ann. Thorac. Surg. 2013;95:1654-9).
Retrospective measurements of the neoaortic annulus and root were performed on all available transthoracic echocardiograms and the severity of neoaortic valve regurgitation was determined by assessing the width of the color Doppler jet of regurgitation measured at the level of the valve in the parasternal long-axis view. A jet width of 1-4 mm was defined as trivial to mild; 4-6 mm was defined as moderate; and greater than 6 mm indicated severe regurgitation, according to the researchers. Significant regurgitation was defined as moderate or severe. Significant neoaortic annulus dilation was defined as a z score of 2.5 or greater.
They evaluated potential risk factors for the development of neoaortic root dilation, annulus dilation, and neoaortic valve regurgitation.
Significant neoaortic root dilation developed in 88 of 124 (66%) of the patients during follow-up, with the probability of being free from a root diameter z score of 2.5 or greater of 84%, 67%, 47%, and 32% at 1, 5, 10, and 15 years, respectively. Significant risk factors predicting neoaortic root dilation using multivariate analysis were a history of double outlet right ventricle (DORV), previous pulmonary artery (PA) banding, and length of follow-up. A history of ventricular septal defect (VSD), coarctation, left ventricular outflow tract obstruction, and age at ASO were not significant risk factors.
Significant annulus dilation occurred in 54% of patients, with significant risk factors including a history of VSD, history of DORV, and the presence of a dilated neoaortic root. History of PA banding and length of follow-up were not significant. Moderate or severe neoaortic valve regurgitation occurred in 17 of 124 (14%) of the patients, with a probability of being free of these levels of regurgitation of 96%, 92%, 89%, and 75% at 1, 5, 10, and 15 years, respectively. The significant risk factors for regurgitation were history of DORV, VSD, left ventricular outflow tract obstruction, and length of follow-up. No patient in the series required reintervention on the neoaorta.
The authors had no disclosures.
Most people living with congenital heart disease are now adults. Unfortunately the majority of these adults, for unclear reasons, are not receiving expert care by congenital heart specialists. Perhaps some of these adults have a misperception that they are cured. Dr. Co-Vu and coauthors at the Medical College of Wisconsin confirm that the highly successful arterial switch operation is not a "cure."
| Dr. Williams |
Their important, carefully executed echo study demonstrates important progressive increases in measured diameters of the neoaortic annulus and neoaortic root over the first 15 years of life. The
authors point out that the dilation has not as yet led to a need for reintervention, and the late prevalence of neoaortic regurgitation is not high, although it too is slowly increasing over time. Their message is a clarion call for lifelong clinical surveillance following an arterial switch operation – a message that should be applied to all patients with congenital heart disease.
Dr. William G. Williams is executive director of the Congenital Heart Surgeons’ Society Data Center, Toronto, and emeritus professor of surgery, University of Toronto, and an associate medical editor for Thoracic Surgery News.
Most people living with congenital heart disease are now adults. Unfortunately the majority of these adults, for unclear reasons, are not receiving expert care by congenital heart specialists. Perhaps some of these adults have a misperception that they are cured. Dr. Co-Vu and coauthors at the Medical College of Wisconsin confirm that the highly successful arterial switch operation is not a "cure."
| Dr. Williams |
Their important, carefully executed echo study demonstrates important progressive increases in measured diameters of the neoaortic annulus and neoaortic root over the first 15 years of life. The
authors point out that the dilation has not as yet led to a need for reintervention, and the late prevalence of neoaortic regurgitation is not high, although it too is slowly increasing over time. Their message is a clarion call for lifelong clinical surveillance following an arterial switch operation – a message that should be applied to all patients with congenital heart disease.
Dr. William G. Williams is executive director of the Congenital Heart Surgeons’ Society Data Center, Toronto, and emeritus professor of surgery, University of Toronto, and an associate medical editor for Thoracic Surgery News.
Most people living with congenital heart disease are now adults. Unfortunately the majority of these adults, for unclear reasons, are not receiving expert care by congenital heart specialists. Perhaps some of these adults have a misperception that they are cured. Dr. Co-Vu and coauthors at the Medical College of Wisconsin confirm that the highly successful arterial switch operation is not a "cure."
| Dr. Williams |
Their important, carefully executed echo study demonstrates important progressive increases in measured diameters of the neoaortic annulus and neoaortic root over the first 15 years of life. The
authors point out that the dilation has not as yet led to a need for reintervention, and the late prevalence of neoaortic regurgitation is not high, although it too is slowly increasing over time. Their message is a clarion call for lifelong clinical surveillance following an arterial switch operation – a message that should be applied to all patients with congenital heart disease.
Dr. William G. Williams is executive director of the Congenital Heart Surgeons’ Society Data Center, Toronto, and emeritus professor of surgery, University of Toronto, and an associate medical editor for Thoracic Surgery News.
Neoaortic root dilation and neoaortic valve regurgitation are common complications in infants with transposition of the great arteries who undergo an arterial switch operation for repair, and the risk of developing these changes in the neoaorta increases over time, according to the results of a retrospective database study of patients at Children’s Hospital of Wisconsin.
In addition, when dilation occurs, the dimensions may progressively enlarge over time, making it important to maintain lifelong surveillance of this population.
Although perioperative mortality and long-term survival (assessed up to 30 years) has improved in more recent eras for use of an arterial switch operation (ASO) for transposition of the great arteries (TGA), these long-term studies have also shown important late complications that may contribute to late morbidity and the need for reoperation, according to Dr. Jennifer G. Co-Vu and her colleagues at the Medical College of Wisconsin, Milwaukee.
They performed their study to determine the prevalence of neoaortic root dilation and neoaortic valve regurgitation in patients treated at their institution and to determine risk factors involved in the development of these late complications.
Out of 247 patients with TGA treated with an ASO at the hospital, there were 124 patients who had at least one available postoperative transthoracic echocardiogram at least 1 year after the ASO. Median age of these patients was 0.2 months at the time of their ASO and 7.2 years at their last follow-up; 71% were boys (Ann. Thorac. Surg. 2013;95:1654-9).
Retrospective measurements of the neoaortic annulus and root were performed on all available transthoracic echocardiograms and the severity of neoaortic valve regurgitation was determined by assessing the width of the color Doppler jet of regurgitation measured at the level of the valve in the parasternal long-axis view. A jet width of 1-4 mm was defined as trivial to mild; 4-6 mm was defined as moderate; and greater than 6 mm indicated severe regurgitation, according to the researchers. Significant regurgitation was defined as moderate or severe. Significant neoaortic annulus dilation was defined as a z score of 2.5 or greater.
They evaluated potential risk factors for the development of neoaortic root dilation, annulus dilation, and neoaortic valve regurgitation.
Significant neoaortic root dilation developed in 88 of 124 (66%) of the patients during follow-up, with the probability of being free from a root diameter z score of 2.5 or greater of 84%, 67%, 47%, and 32% at 1, 5, 10, and 15 years, respectively. Significant risk factors predicting neoaortic root dilation using multivariate analysis were a history of double outlet right ventricle (DORV), previous pulmonary artery (PA) banding, and length of follow-up. A history of ventricular septal defect (VSD), coarctation, left ventricular outflow tract obstruction, and age at ASO were not significant risk factors.
Significant annulus dilation occurred in 54% of patients, with significant risk factors including a history of VSD, history of DORV, and the presence of a dilated neoaortic root. History of PA banding and length of follow-up were not significant. Moderate or severe neoaortic valve regurgitation occurred in 17 of 124 (14%) of the patients, with a probability of being free of these levels of regurgitation of 96%, 92%, 89%, and 75% at 1, 5, 10, and 15 years, respectively. The significant risk factors for regurgitation were history of DORV, VSD, left ventricular outflow tract obstruction, and length of follow-up. No patient in the series required reintervention on the neoaorta.
The authors had no disclosures.
Neoaortic root dilation and neoaortic valve regurgitation are common complications in infants with transposition of the great arteries who undergo an arterial switch operation for repair, and the risk of developing these changes in the neoaorta increases over time, according to the results of a retrospective database study of patients at Children’s Hospital of Wisconsin.
In addition, when dilation occurs, the dimensions may progressively enlarge over time, making it important to maintain lifelong surveillance of this population.
Although perioperative mortality and long-term survival (assessed up to 30 years) has improved in more recent eras for use of an arterial switch operation (ASO) for transposition of the great arteries (TGA), these long-term studies have also shown important late complications that may contribute to late morbidity and the need for reoperation, according to Dr. Jennifer G. Co-Vu and her colleagues at the Medical College of Wisconsin, Milwaukee.
They performed their study to determine the prevalence of neoaortic root dilation and neoaortic valve regurgitation in patients treated at their institution and to determine risk factors involved in the development of these late complications.
Out of 247 patients with TGA treated with an ASO at the hospital, there were 124 patients who had at least one available postoperative transthoracic echocardiogram at least 1 year after the ASO. Median age of these patients was 0.2 months at the time of their ASO and 7.2 years at their last follow-up; 71% were boys (Ann. Thorac. Surg. 2013;95:1654-9).
Retrospective measurements of the neoaortic annulus and root were performed on all available transthoracic echocardiograms and the severity of neoaortic valve regurgitation was determined by assessing the width of the color Doppler jet of regurgitation measured at the level of the valve in the parasternal long-axis view. A jet width of 1-4 mm was defined as trivial to mild; 4-6 mm was defined as moderate; and greater than 6 mm indicated severe regurgitation, according to the researchers. Significant regurgitation was defined as moderate or severe. Significant neoaortic annulus dilation was defined as a z score of 2.5 or greater.
They evaluated potential risk factors for the development of neoaortic root dilation, annulus dilation, and neoaortic valve regurgitation.
Significant neoaortic root dilation developed in 88 of 124 (66%) of the patients during follow-up, with the probability of being free from a root diameter z score of 2.5 or greater of 84%, 67%, 47%, and 32% at 1, 5, 10, and 15 years, respectively. Significant risk factors predicting neoaortic root dilation using multivariate analysis were a history of double outlet right ventricle (DORV), previous pulmonary artery (PA) banding, and length of follow-up. A history of ventricular septal defect (VSD), coarctation, left ventricular outflow tract obstruction, and age at ASO were not significant risk factors.
Significant annulus dilation occurred in 54% of patients, with significant risk factors including a history of VSD, history of DORV, and the presence of a dilated neoaortic root. History of PA banding and length of follow-up were not significant. Moderate or severe neoaortic valve regurgitation occurred in 17 of 124 (14%) of the patients, with a probability of being free of these levels of regurgitation of 96%, 92%, 89%, and 75% at 1, 5, 10, and 15 years, respectively. The significant risk factors for regurgitation were history of DORV, VSD, left ventricular outflow tract obstruction, and length of follow-up. No patient in the series required reintervention on the neoaorta.
The authors had no disclosures.
Fontan reoperation mortality unexpectedly high in multicenter analysis
MINNEAPOLIS – Early mortality is substantially higher than initially thought for Fontan revision or conversion, the most common reoperation in adults with congenital heart disease.
Discharge mortality was 10.1% among adults undergoing a Fontan redo from 2007 to 2011 in an analysis of the STS-CHSD (Society of Thoracic Surgeons Congenital Heart Surgery Database), encompassing more than 90% of heart surgeries in the United States.
When Fontan conversion was first described in a single-center series, however, discharge mortality was less than 1% (Ann. Thorac. Surg. 2007;84:1457-65), observed Dr. Jeffrey P. Jacobs, chair of the STS-CHSD, and a cardiovascular surgeon with All Children’s Hospital, Johns Hopkins Medicine, St. Petersburg, Fla.
"This point really exemplifies the power of multi-institution data and exemplifies that the published literature reflecting an excellence experience at one center, may not reflect the reality of what is going on across the country or across the world," he said at the annual meeting of the American Association for Thoracic Surgery.
The STS-CHSD includes 108 congenital heart surgery hospitals in North America, 105 in the United States and 3 in Canada, or 84% of programs in the United States.
The investigators identified 92,603 index cardiac operations in the database from 2007-2011, after excluding those with missing data and patients weighing 2,500 g or less undergoing patent ductus arteriosus ligation as their primary procedure.
In all, 30,673 (33%) had one or more prior cardiopulmonary bypass cardiothoracic operation, which was used as a surrogate for reoperation.
Discharge mortality was 3.98% with no prior bypass cardiothoracic operations, 2.38% with one, 1.67% with two, 2.41% with three, 3.31% with four, 4.08% with five, and 5.07% with six or more reoperations, Dr. Jacobs said.
Mean length of stay was 14.8 days for the index procedure and increased in a stepwise manner from 10.8 days with one prior surgery to 14.07 with six or more surgeries.
Fontan (total cavopulmonary connection, external conduit) was the most common reoperation performed among all patients and had the highest discharge mortality whether it was fenestrated (1.8% among 1,870 patients) or nonfenestrated (1.6% among 1,403 patients).
Discharge mortality was lower among all patients for bidirectional cavopulmonary anastomosis (1.3%), pulmonic valve replacement (0.4%), conduit reoperation (0.8%), pacemaker procedure (0.3%), and permanent pacemaker implantation (1.4%).
The number of neonates dying before discharge was alarmingly high for various operations including total anomalous pulmonary venous connection repair (55.6%), pulmonary artery banding (36.4%), and the Norwood procedure (21.6%), but Dr. Jacobs cautioned that these reoperations are very rare events occurring in 18, 11, and 37 cases, respectively.
In contrast, discharge mortality among infants reached a high of 2.6% for a hemi-Fontan reoperation (8 deaths/311 procedures) and was half that for bidirectional cavopulmonary anastomosis, the most common reoperation among infants (29 deaths/2,271 procedures).
Discharge mortality for reoperations among children, aged 1-18 years, in the United States also remained below 2%, he said. The highest rate was 1.7% for a Fontan redo (TCPC, external conduit, fenestrated), the most common operation, performed in 1,852 children.
Finally, there were no double-digit discharge mortality rates among adults, save for the bloated 10.1% reported for Fontan revision or conversion. Rates were low for arrhythmia surgery–atrial surgical ablation (3.4%), right ventricle to pulmonary artery conduit placement (3.3%), permanent pacemaker implantation (2%), conduit reoperation (1.6%), pulmonic valve replacement (0.3%), and pacemaker procedure (0.2%).
Science tells us what we can do, guidelines what we should do, and registries what we are actually doing, Dr. Jacobs concluded.
Dr. Jacobs is chair of the STS Congenital Heart Surgery Database Taskforce; STS Task Force on Longitudinal Follow-Up and Linked Registries; and the STS Public Reporting Task Force.
MINNEAPOLIS – Early mortality is substantially higher than initially thought for Fontan revision or conversion, the most common reoperation in adults with congenital heart disease.
Discharge mortality was 10.1% among adults undergoing a Fontan redo from 2007 to 2011 in an analysis of the STS-CHSD (Society of Thoracic Surgeons Congenital Heart Surgery Database), encompassing more than 90% of heart surgeries in the United States.
When Fontan conversion was first described in a single-center series, however, discharge mortality was less than 1% (Ann. Thorac. Surg. 2007;84:1457-65), observed Dr. Jeffrey P. Jacobs, chair of the STS-CHSD, and a cardiovascular surgeon with All Children’s Hospital, Johns Hopkins Medicine, St. Petersburg, Fla.
"This point really exemplifies the power of multi-institution data and exemplifies that the published literature reflecting an excellence experience at one center, may not reflect the reality of what is going on across the country or across the world," he said at the annual meeting of the American Association for Thoracic Surgery.
The STS-CHSD includes 108 congenital heart surgery hospitals in North America, 105 in the United States and 3 in Canada, or 84% of programs in the United States.
The investigators identified 92,603 index cardiac operations in the database from 2007-2011, after excluding those with missing data and patients weighing 2,500 g or less undergoing patent ductus arteriosus ligation as their primary procedure.
In all, 30,673 (33%) had one or more prior cardiopulmonary bypass cardiothoracic operation, which was used as a surrogate for reoperation.
Discharge mortality was 3.98% with no prior bypass cardiothoracic operations, 2.38% with one, 1.67% with two, 2.41% with three, 3.31% with four, 4.08% with five, and 5.07% with six or more reoperations, Dr. Jacobs said.
Mean length of stay was 14.8 days for the index procedure and increased in a stepwise manner from 10.8 days with one prior surgery to 14.07 with six or more surgeries.
Fontan (total cavopulmonary connection, external conduit) was the most common reoperation performed among all patients and had the highest discharge mortality whether it was fenestrated (1.8% among 1,870 patients) or nonfenestrated (1.6% among 1,403 patients).
Discharge mortality was lower among all patients for bidirectional cavopulmonary anastomosis (1.3%), pulmonic valve replacement (0.4%), conduit reoperation (0.8%), pacemaker procedure (0.3%), and permanent pacemaker implantation (1.4%).
The number of neonates dying before discharge was alarmingly high for various operations including total anomalous pulmonary venous connection repair (55.6%), pulmonary artery banding (36.4%), and the Norwood procedure (21.6%), but Dr. Jacobs cautioned that these reoperations are very rare events occurring in 18, 11, and 37 cases, respectively.
In contrast, discharge mortality among infants reached a high of 2.6% for a hemi-Fontan reoperation (8 deaths/311 procedures) and was half that for bidirectional cavopulmonary anastomosis, the most common reoperation among infants (29 deaths/2,271 procedures).
Discharge mortality for reoperations among children, aged 1-18 years, in the United States also remained below 2%, he said. The highest rate was 1.7% for a Fontan redo (TCPC, external conduit, fenestrated), the most common operation, performed in 1,852 children.
Finally, there were no double-digit discharge mortality rates among adults, save for the bloated 10.1% reported for Fontan revision or conversion. Rates were low for arrhythmia surgery–atrial surgical ablation (3.4%), right ventricle to pulmonary artery conduit placement (3.3%), permanent pacemaker implantation (2%), conduit reoperation (1.6%), pulmonic valve replacement (0.3%), and pacemaker procedure (0.2%).
Science tells us what we can do, guidelines what we should do, and registries what we are actually doing, Dr. Jacobs concluded.
Dr. Jacobs is chair of the STS Congenital Heart Surgery Database Taskforce; STS Task Force on Longitudinal Follow-Up and Linked Registries; and the STS Public Reporting Task Force.
MINNEAPOLIS – Early mortality is substantially higher than initially thought for Fontan revision or conversion, the most common reoperation in adults with congenital heart disease.
Discharge mortality was 10.1% among adults undergoing a Fontan redo from 2007 to 2011 in an analysis of the STS-CHSD (Society of Thoracic Surgeons Congenital Heart Surgery Database), encompassing more than 90% of heart surgeries in the United States.
When Fontan conversion was first described in a single-center series, however, discharge mortality was less than 1% (Ann. Thorac. Surg. 2007;84:1457-65), observed Dr. Jeffrey P. Jacobs, chair of the STS-CHSD, and a cardiovascular surgeon with All Children’s Hospital, Johns Hopkins Medicine, St. Petersburg, Fla.
"This point really exemplifies the power of multi-institution data and exemplifies that the published literature reflecting an excellence experience at one center, may not reflect the reality of what is going on across the country or across the world," he said at the annual meeting of the American Association for Thoracic Surgery.
The STS-CHSD includes 108 congenital heart surgery hospitals in North America, 105 in the United States and 3 in Canada, or 84% of programs in the United States.
The investigators identified 92,603 index cardiac operations in the database from 2007-2011, after excluding those with missing data and patients weighing 2,500 g or less undergoing patent ductus arteriosus ligation as their primary procedure.
In all, 30,673 (33%) had one or more prior cardiopulmonary bypass cardiothoracic operation, which was used as a surrogate for reoperation.
Discharge mortality was 3.98% with no prior bypass cardiothoracic operations, 2.38% with one, 1.67% with two, 2.41% with three, 3.31% with four, 4.08% with five, and 5.07% with six or more reoperations, Dr. Jacobs said.
Mean length of stay was 14.8 days for the index procedure and increased in a stepwise manner from 10.8 days with one prior surgery to 14.07 with six or more surgeries.
Fontan (total cavopulmonary connection, external conduit) was the most common reoperation performed among all patients and had the highest discharge mortality whether it was fenestrated (1.8% among 1,870 patients) or nonfenestrated (1.6% among 1,403 patients).
Discharge mortality was lower among all patients for bidirectional cavopulmonary anastomosis (1.3%), pulmonic valve replacement (0.4%), conduit reoperation (0.8%), pacemaker procedure (0.3%), and permanent pacemaker implantation (1.4%).
The number of neonates dying before discharge was alarmingly high for various operations including total anomalous pulmonary venous connection repair (55.6%), pulmonary artery banding (36.4%), and the Norwood procedure (21.6%), but Dr. Jacobs cautioned that these reoperations are very rare events occurring in 18, 11, and 37 cases, respectively.
In contrast, discharge mortality among infants reached a high of 2.6% for a hemi-Fontan reoperation (8 deaths/311 procedures) and was half that for bidirectional cavopulmonary anastomosis, the most common reoperation among infants (29 deaths/2,271 procedures).
Discharge mortality for reoperations among children, aged 1-18 years, in the United States also remained below 2%, he said. The highest rate was 1.7% for a Fontan redo (TCPC, external conduit, fenestrated), the most common operation, performed in 1,852 children.
Finally, there were no double-digit discharge mortality rates among adults, save for the bloated 10.1% reported for Fontan revision or conversion. Rates were low for arrhythmia surgery–atrial surgical ablation (3.4%), right ventricle to pulmonary artery conduit placement (3.3%), permanent pacemaker implantation (2%), conduit reoperation (1.6%), pulmonic valve replacement (0.3%), and pacemaker procedure (0.2%).
Science tells us what we can do, guidelines what we should do, and registries what we are actually doing, Dr. Jacobs concluded.
Dr. Jacobs is chair of the STS Congenital Heart Surgery Database Taskforce; STS Task Force on Longitudinal Follow-Up and Linked Registries; and the STS Public Reporting Task Force.
Neonates at highest risk for Ebstein’s malformation treatment
LOS ANGELES – Neonates in particular are at risk for poor outcomes from Ebstein’s malformation, showing significantly higher mortality than infants, children, and adults, according to a database study presented by Dr. Ryan R. Davies at the annual meeting of the Society of Thoracic Surgeons.
Ebstein’s malformation is a rare congenital cardiac anomaly. Surgery for Ebstein’s involves a range of procedures, and with low institutional volumes, the only available data on treatment have been limited to individual reports demonstrating highly variable approaches.
Dr. Davies of the Nemours/A.I. duPont Hospital for Children, Wilmington, Del., and his colleagues performed a retrospective study of procedures performed on patients with a primary diagnosis of Ebstein’s malformation (2002-2009) in the STS Congenital Heart Surgery Database.
A total of 595 operations on patients with Ebstein’s were included: 116 on neonates (19%), 122 on infants (21%), 264 on children (44%), and 93 on adults (16%). The authors found that average annual institutional case volumes were low (median, 1 case/year), and procedures varied according to age. Neonates had a high rate of palliative procedures: tricuspid valve (TV) closure (16%) and systemic-to-pulmonary shunts with or without TV closure (37%) and isolated TV closure (8.6%), with Ebstein’s repair or TV valvuloplasty performed in 32%.
Infants usually underwent superior cavopulmonary connections (52%).
Among older patients, procedures were mostly in three categories: TV surgery (children, 55%; adults, 69%), arrhythmia procedures (children, 9%; adults, 17%), and Fontan (children, 16%). In-hospital mortality was higher among neonatal patients (23%) than in infants (4%), children (0.8%), and adults (1.1%).
Among neonates, 36 subsequent procedures were performed during the same hospitalization in 27 patients (23%); including TV closure (11%); shunt (15%); Ebstein’s repair (17%) or TV replacement (15%); and heart transplantation (7.4%). Mortality was similar among neonates who had a second procedure and those who did not (27% vs. 23%, respectively). ECMO (extracorporeal membrane oxygenation) was used in 9% of neonates but in less than 2% of patients in other age groups.
"This study represents a broad overview of the diverse options for surgical treatment of Ebstein’s anomaly. It shows the challenges faced in caring for extremely ill neonatal patients. We have also shown that repair of Ebstein’s anomaly is performed infrequently at most centers, limiting the ability of individual series to define optimal management strategies," Dr. Davies said in an interview.
"Unfortunately, currently available databases do not contain information that may be important in defining such strategies (both surgical and nonsurgical), including anatomic and physiologic variables – whether they are neonates presenting in severe heart failure or older patients presenting for tricuspid valve repair or replacement," he added.
"We feel that in this setting, a prospective multi-institutional study would be of significant value. It should include operative and nonoperative patients, as well as precise diagnostic information and procedural details, to evaluate long-term outcomes including survival, reoperation and other reinterventions, as well as neurodevelopmental outcomes, functional health status, and quality of life," Dr. Davies concluded.
Dr. Davies and his colleagues reported having no relevant disclosures.
LOS ANGELES – Neonates in particular are at risk for poor outcomes from Ebstein’s malformation, showing significantly higher mortality than infants, children, and adults, according to a database study presented by Dr. Ryan R. Davies at the annual meeting of the Society of Thoracic Surgeons.
Ebstein’s malformation is a rare congenital cardiac anomaly. Surgery for Ebstein’s involves a range of procedures, and with low institutional volumes, the only available data on treatment have been limited to individual reports demonstrating highly variable approaches.
Dr. Davies of the Nemours/A.I. duPont Hospital for Children, Wilmington, Del., and his colleagues performed a retrospective study of procedures performed on patients with a primary diagnosis of Ebstein’s malformation (2002-2009) in the STS Congenital Heart Surgery Database.
A total of 595 operations on patients with Ebstein’s were included: 116 on neonates (19%), 122 on infants (21%), 264 on children (44%), and 93 on adults (16%). The authors found that average annual institutional case volumes were low (median, 1 case/year), and procedures varied according to age. Neonates had a high rate of palliative procedures: tricuspid valve (TV) closure (16%) and systemic-to-pulmonary shunts with or without TV closure (37%) and isolated TV closure (8.6%), with Ebstein’s repair or TV valvuloplasty performed in 32%.
Infants usually underwent superior cavopulmonary connections (52%).
Among older patients, procedures were mostly in three categories: TV surgery (children, 55%; adults, 69%), arrhythmia procedures (children, 9%; adults, 17%), and Fontan (children, 16%). In-hospital mortality was higher among neonatal patients (23%) than in infants (4%), children (0.8%), and adults (1.1%).
Among neonates, 36 subsequent procedures were performed during the same hospitalization in 27 patients (23%); including TV closure (11%); shunt (15%); Ebstein’s repair (17%) or TV replacement (15%); and heart transplantation (7.4%). Mortality was similar among neonates who had a second procedure and those who did not (27% vs. 23%, respectively). ECMO (extracorporeal membrane oxygenation) was used in 9% of neonates but in less than 2% of patients in other age groups.
"This study represents a broad overview of the diverse options for surgical treatment of Ebstein’s anomaly. It shows the challenges faced in caring for extremely ill neonatal patients. We have also shown that repair of Ebstein’s anomaly is performed infrequently at most centers, limiting the ability of individual series to define optimal management strategies," Dr. Davies said in an interview.
"Unfortunately, currently available databases do not contain information that may be important in defining such strategies (both surgical and nonsurgical), including anatomic and physiologic variables – whether they are neonates presenting in severe heart failure or older patients presenting for tricuspid valve repair or replacement," he added.
"We feel that in this setting, a prospective multi-institutional study would be of significant value. It should include operative and nonoperative patients, as well as precise diagnostic information and procedural details, to evaluate long-term outcomes including survival, reoperation and other reinterventions, as well as neurodevelopmental outcomes, functional health status, and quality of life," Dr. Davies concluded.
Dr. Davies and his colleagues reported having no relevant disclosures.
LOS ANGELES – Neonates in particular are at risk for poor outcomes from Ebstein’s malformation, showing significantly higher mortality than infants, children, and adults, according to a database study presented by Dr. Ryan R. Davies at the annual meeting of the Society of Thoracic Surgeons.
Ebstein’s malformation is a rare congenital cardiac anomaly. Surgery for Ebstein’s involves a range of procedures, and with low institutional volumes, the only available data on treatment have been limited to individual reports demonstrating highly variable approaches.
Dr. Davies of the Nemours/A.I. duPont Hospital for Children, Wilmington, Del., and his colleagues performed a retrospective study of procedures performed on patients with a primary diagnosis of Ebstein’s malformation (2002-2009) in the STS Congenital Heart Surgery Database.
A total of 595 operations on patients with Ebstein’s were included: 116 on neonates (19%), 122 on infants (21%), 264 on children (44%), and 93 on adults (16%). The authors found that average annual institutional case volumes were low (median, 1 case/year), and procedures varied according to age. Neonates had a high rate of palliative procedures: tricuspid valve (TV) closure (16%) and systemic-to-pulmonary shunts with or without TV closure (37%) and isolated TV closure (8.6%), with Ebstein’s repair or TV valvuloplasty performed in 32%.
Infants usually underwent superior cavopulmonary connections (52%).
Among older patients, procedures were mostly in three categories: TV surgery (children, 55%; adults, 69%), arrhythmia procedures (children, 9%; adults, 17%), and Fontan (children, 16%). In-hospital mortality was higher among neonatal patients (23%) than in infants (4%), children (0.8%), and adults (1.1%).
Among neonates, 36 subsequent procedures were performed during the same hospitalization in 27 patients (23%); including TV closure (11%); shunt (15%); Ebstein’s repair (17%) or TV replacement (15%); and heart transplantation (7.4%). Mortality was similar among neonates who had a second procedure and those who did not (27% vs. 23%, respectively). ECMO (extracorporeal membrane oxygenation) was used in 9% of neonates but in less than 2% of patients in other age groups.
"This study represents a broad overview of the diverse options for surgical treatment of Ebstein’s anomaly. It shows the challenges faced in caring for extremely ill neonatal patients. We have also shown that repair of Ebstein’s anomaly is performed infrequently at most centers, limiting the ability of individual series to define optimal management strategies," Dr. Davies said in an interview.
"Unfortunately, currently available databases do not contain information that may be important in defining such strategies (both surgical and nonsurgical), including anatomic and physiologic variables – whether they are neonates presenting in severe heart failure or older patients presenting for tricuspid valve repair or replacement," he added.
"We feel that in this setting, a prospective multi-institutional study would be of significant value. It should include operative and nonoperative patients, as well as precise diagnostic information and procedural details, to evaluate long-term outcomes including survival, reoperation and other reinterventions, as well as neurodevelopmental outcomes, functional health status, and quality of life," Dr. Davies concluded.
Dr. Davies and his colleagues reported having no relevant disclosures.
AT THE STS ANNUAL MEETING
Major Finding: In-hospital mortality was higher among neonatal patients (23%) than in infants (4%), children (0.8%), and adults (1.1%).
Data Source: A retrospective database analysis of 595 operations on patients with Ebstein’s malformation.
Disclosures: Dr. Davies and his colleagues reported having no relevant disclosures.