User login
Drug allows for treatment-free periods in PV
ATLANTA—Results of a phase 1 study suggest patients with polycythemia vera (PV) can achieve extended treatment-free periods after receiving idasanutlin.
Six of 12 patients who received the drug were able to have a treatment holiday—4 patients for 1 month, 1 for 2 to 3 consecutive months, and 1 for more than 3 consecutive months.
Four patients achieved a complete response (CR) and 3 a partial response (PR), for an overall response rate (ORR) of 58%.
There were no dose-limiting toxicities (DLTs) in the trial.
John Mascarenhas, MD, of Icahn School of Medicine at Mount Sinai in New York, New York, reported these results at the 2017 ASH Annual Meeting as abstract 254.*
The study was supported by Roche and funded by the National Cancer Institute, PDRC, and a grant from the Leukemia and Lymphoma Society.
Study rationale
Patients with PV have higher levels of MDM2 in their CD34+ cells compared to normal CD34+ cells. Nutlins block the interaction between p53 and MDM2, thus activating the p53 pathway.
Investigators previously found that low doses of nutlin and pegylated IFNα 2a promoted apoptosis in PV CD34+ cells.
And treatment with the combination reduced the numbers of JAK2V617-positive cells transplanted into immune-deficient NOD/SCID mice.
So Dr Mascarenhas and his colleagues undertook a study (NCT02407080) to evaluate the toxicity, safety, and tolerability of the MDM2 antagonist idasanutlin in patients with PV and essential thrombocythemia (ET).
The investigators hypothesized that since overexpression of MDM2 negatively regulates wild-type p53 function in primary PV cells, idasanutlin therapy, either alone or in combination with low-dose peg-IFN, could result in selective reduction or elimination of the myeloproliferative neoplasm cells in PV patients.
Study design
The investigators evaluated 2 dose levels of idasanutlin—100 mg daily and 150 mg daily on days 1 to 5, repeated every 28 days. The first cycle was 56 days to allow investigators to evaluate any DLTs.
Dr Mascarenhas pointed out that the dose is 1/6 of that being evaluated in acute myeloid leukemia.
Investigators defined a DLT as a non-hematologic adverse event (AE) of grade 3 or higher or a hematologic AE of grade 2 or higher thrombocytopenia or grade 3 or higher neutropenia or anemia.
If patients did not achieve at least a PR by the end of cycle 3 of single-agent therapy, they could proceed to Part B of the study and receive idasanutlin with pegylated IFN.
After cycle 3, dosing was dependent upon patients hitting a hematocrit greater than 42% and/or platelet counts greater than 400,000.
“So you had to meet parameters, which means that if you did meet parameters, you could get a treatment holiday,” Dr Mascarenhas explained.
Patients were eligible if they had JAK2V617F-positive PV or ET confirmed by WHO diagnostic criteria.
They had to have high-risk disease, be older than 60, and have a history of thrombosis. They also had to be either intolerant or resistant to at least one prior treatment, including hydroxyurea, interferon, or anagrelide.
Patients were excluded if they had post-ET/PV myelofibrosis, blast phase disease, acute thrombosis within 3 months of screening, or uncontrolled inter-current illness.
Baseline patient characteristics
Eleven of the 12 patients enrolled had PV, and 1 had ET. Their median age was 63.5, and 7 were female. Their median duration of disease was 43.9 months (range, 14.9–154.3), 3 had previous thrombosis, and 10 had prior hydroxyurea therapy.
They had a median leukocyte count of 11.3 x 109/L, median hemoglobin levels of 13.6 g/dL, median hematocrit of 42.3%, and median platelet levels of 443.5 x 109/L.
They all had the JAK2V617F mutation. Some patients had additional mutations, including TET2, DNMT3A, ASXL1, CBL, and EZH2, among others.
“One patient had an inactivating p53 mutation,” Dr Mascarenhas said. “I didn’t know this when we put her on study. . . , but this is an interesting part of the study. So remember, one patient had an inactivating p53 mutation in a trial where I’m using a drug that interrupts wild-type p53-MDM2 interaction.”
Efficacy
Plasma MIC-1 levels were significantly increased (P=0.004) in PV patients following treatment with idasanutlin at day 5 compared to day 1. MIC-1 is a secreted protein strongly induced by activated p53.
“Some patients didn’t need to be treated every month,” Dr Mascarenhas said. “They got treatment holidays. That’s unique. I don’t usually see that in the treatments that we give. In fact, this one person here, after 3 cycles, didn’t need to be re-treated for 9 months.”
In the 100 mg cohort (n=6), patients received a median of 8 cycles of idasanutlin (range, 7-13) and were on study for a median of 34.1 weeks (range, 29.0–127.3). One patient experienced a treatment holiday of 1 month, and another patient had a treatment holiday of more than 3 consecutive months.
In the 150 mg cohort (n=6), patients received a median of 9.5 cycles of therapy (range, 5–17) and were on study for a median of 52.1 weeks (range, 23.1–72.9). Three patients experienced a 1-month treatment holiday, and 1 patient had a 2- to 3-month treatment holiday.
In total, 6 patients continued the single-agent regimen, and 4 proceeded to the combination treatment with pegylated IFN.
Reasons for discontinuation were patient refusal and investigator decision.
The ORR (CR + PR) for both dose cohorts with single-agent idasanutlin was 58%. One patient was not evaluable, 4 had no response, 3 had a PR, and 4 had a CR.
In the combination portion of the study, the ORR was 50%. One patient was not evaluable, 1 had no response, 1 had a PR, and 1 had a CR.
“The 1 non-responder in Part B,” Dr Mascarenhas noted, “was the p53-mutated patient. Makes sense.”
The ORR for both the single-agent and combination parts of the study was 75%.
Eight of 12 patients had a 50% reduction in total symptom score from baseline, which is considered clinically meaningful, according to Dr Mascarenhas.
“What’s also interesting,” he pointed out, “[ is that] patients who didn’t obtain a response also enjoyed symptom benefit.”
Patients had a median 43% reduction in JAK2 mutation from baseline.
“One patient had nearly 92% reduction in JAK2V617F,” Dr Mascarenhas said. “One patient had a 60% increase. But guess what? That was the p53-mutated patient. Makes sense.”
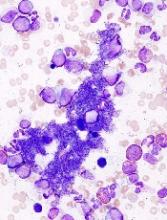
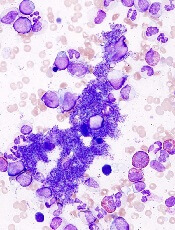
Bone morphology showed reduction in marrow hypercellularity and normalization of megakaryocyte atypia and clustering.
Safety
There were no DLTs with either dose of idasanutlin.
“This was a well-tolerated drug,” Dr Mascarenhas said.
Three patients experienced grade 3 non-hematologic treatment-emergent AEs, all at 100 mg, of fatigue (1 patient), headache (1 patient), and pain (1 patient).
No grade 4 non-hematologic treatment-emergent AEs occurred at either dose, and investigators observed no hematologic AE of any grade.
Investigators also observed no grade 3–4 gastrointestinal (GI) treatment-emergent AEs. Constipation (91.7%), nausea (75%), and diarrhea (66.7%) were the most frequent grade 1 or 2 events. Patients received GI prophylaxis upfront with ondansetron, lorazepam, or dexamethasone.
Because of the safety profile and manageable GI toxicity, the higher dose of idasanutlin was chosen as the recommended phase 2 dose.
A global, multicenter, single-arm, phase 2 trial with idasanutlin in patients with hydroxyurea-resistant or -intolerant PV is underway. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Results of a phase 1 study suggest patients with polycythemia vera (PV) can achieve extended treatment-free periods after receiving idasanutlin.
Six of 12 patients who received the drug were able to have a treatment holiday—4 patients for 1 month, 1 for 2 to 3 consecutive months, and 1 for more than 3 consecutive months.
Four patients achieved a complete response (CR) and 3 a partial response (PR), for an overall response rate (ORR) of 58%.
There were no dose-limiting toxicities (DLTs) in the trial.
John Mascarenhas, MD, of Icahn School of Medicine at Mount Sinai in New York, New York, reported these results at the 2017 ASH Annual Meeting as abstract 254.*
The study was supported by Roche and funded by the National Cancer Institute, PDRC, and a grant from the Leukemia and Lymphoma Society.
Study rationale
Patients with PV have higher levels of MDM2 in their CD34+ cells compared to normal CD34+ cells. Nutlins block the interaction between p53 and MDM2, thus activating the p53 pathway.
Investigators previously found that low doses of nutlin and pegylated IFNα 2a promoted apoptosis in PV CD34+ cells.
And treatment with the combination reduced the numbers of JAK2V617-positive cells transplanted into immune-deficient NOD/SCID mice.
So Dr Mascarenhas and his colleagues undertook a study (NCT02407080) to evaluate the toxicity, safety, and tolerability of the MDM2 antagonist idasanutlin in patients with PV and essential thrombocythemia (ET).
The investigators hypothesized that since overexpression of MDM2 negatively regulates wild-type p53 function in primary PV cells, idasanutlin therapy, either alone or in combination with low-dose peg-IFN, could result in selective reduction or elimination of the myeloproliferative neoplasm cells in PV patients.
Study design
The investigators evaluated 2 dose levels of idasanutlin—100 mg daily and 150 mg daily on days 1 to 5, repeated every 28 days. The first cycle was 56 days to allow investigators to evaluate any DLTs.
Dr Mascarenhas pointed out that the dose is 1/6 of that being evaluated in acute myeloid leukemia.
Investigators defined a DLT as a non-hematologic adverse event (AE) of grade 3 or higher or a hematologic AE of grade 2 or higher thrombocytopenia or grade 3 or higher neutropenia or anemia.
If patients did not achieve at least a PR by the end of cycle 3 of single-agent therapy, they could proceed to Part B of the study and receive idasanutlin with pegylated IFN.
After cycle 3, dosing was dependent upon patients hitting a hematocrit greater than 42% and/or platelet counts greater than 400,000.
“So you had to meet parameters, which means that if you did meet parameters, you could get a treatment holiday,” Dr Mascarenhas explained.
Patients were eligible if they had JAK2V617F-positive PV or ET confirmed by WHO diagnostic criteria.
They had to have high-risk disease, be older than 60, and have a history of thrombosis. They also had to be either intolerant or resistant to at least one prior treatment, including hydroxyurea, interferon, or anagrelide.
Patients were excluded if they had post-ET/PV myelofibrosis, blast phase disease, acute thrombosis within 3 months of screening, or uncontrolled inter-current illness.
Baseline patient characteristics
Eleven of the 12 patients enrolled had PV, and 1 had ET. Their median age was 63.5, and 7 were female. Their median duration of disease was 43.9 months (range, 14.9–154.3), 3 had previous thrombosis, and 10 had prior hydroxyurea therapy.
They had a median leukocyte count of 11.3 x 109/L, median hemoglobin levels of 13.6 g/dL, median hematocrit of 42.3%, and median platelet levels of 443.5 x 109/L.
They all had the JAK2V617F mutation. Some patients had additional mutations, including TET2, DNMT3A, ASXL1, CBL, and EZH2, among others.
“One patient had an inactivating p53 mutation,” Dr Mascarenhas said. “I didn’t know this when we put her on study. . . , but this is an interesting part of the study. So remember, one patient had an inactivating p53 mutation in a trial where I’m using a drug that interrupts wild-type p53-MDM2 interaction.”
Efficacy
Plasma MIC-1 levels were significantly increased (P=0.004) in PV patients following treatment with idasanutlin at day 5 compared to day 1. MIC-1 is a secreted protein strongly induced by activated p53.
“Some patients didn’t need to be treated every month,” Dr Mascarenhas said. “They got treatment holidays. That’s unique. I don’t usually see that in the treatments that we give. In fact, this one person here, after 3 cycles, didn’t need to be re-treated for 9 months.”
In the 100 mg cohort (n=6), patients received a median of 8 cycles of idasanutlin (range, 7-13) and were on study for a median of 34.1 weeks (range, 29.0–127.3). One patient experienced a treatment holiday of 1 month, and another patient had a treatment holiday of more than 3 consecutive months.
In the 150 mg cohort (n=6), patients received a median of 9.5 cycles of therapy (range, 5–17) and were on study for a median of 52.1 weeks (range, 23.1–72.9). Three patients experienced a 1-month treatment holiday, and 1 patient had a 2- to 3-month treatment holiday.
In total, 6 patients continued the single-agent regimen, and 4 proceeded to the combination treatment with pegylated IFN.
Reasons for discontinuation were patient refusal and investigator decision.
The ORR (CR + PR) for both dose cohorts with single-agent idasanutlin was 58%. One patient was not evaluable, 4 had no response, 3 had a PR, and 4 had a CR.
In the combination portion of the study, the ORR was 50%. One patient was not evaluable, 1 had no response, 1 had a PR, and 1 had a CR.
“The 1 non-responder in Part B,” Dr Mascarenhas noted, “was the p53-mutated patient. Makes sense.”
The ORR for both the single-agent and combination parts of the study was 75%.
Eight of 12 patients had a 50% reduction in total symptom score from baseline, which is considered clinically meaningful, according to Dr Mascarenhas.
“What’s also interesting,” he pointed out, “[ is that] patients who didn’t obtain a response also enjoyed symptom benefit.”
Patients had a median 43% reduction in JAK2 mutation from baseline.
“One patient had nearly 92% reduction in JAK2V617F,” Dr Mascarenhas said. “One patient had a 60% increase. But guess what? That was the p53-mutated patient. Makes sense.”
Bone morphology showed reduction in marrow hypercellularity and normalization of megakaryocyte atypia and clustering.
Safety
There were no DLTs with either dose of idasanutlin.
“This was a well-tolerated drug,” Dr Mascarenhas said.
Three patients experienced grade 3 non-hematologic treatment-emergent AEs, all at 100 mg, of fatigue (1 patient), headache (1 patient), and pain (1 patient).
No grade 4 non-hematologic treatment-emergent AEs occurred at either dose, and investigators observed no hematologic AE of any grade.
Investigators also observed no grade 3–4 gastrointestinal (GI) treatment-emergent AEs. Constipation (91.7%), nausea (75%), and diarrhea (66.7%) were the most frequent grade 1 or 2 events. Patients received GI prophylaxis upfront with ondansetron, lorazepam, or dexamethasone.
Because of the safety profile and manageable GI toxicity, the higher dose of idasanutlin was chosen as the recommended phase 2 dose.
A global, multicenter, single-arm, phase 2 trial with idasanutlin in patients with hydroxyurea-resistant or -intolerant PV is underway. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Results of a phase 1 study suggest patients with polycythemia vera (PV) can achieve extended treatment-free periods after receiving idasanutlin.
Six of 12 patients who received the drug were able to have a treatment holiday—4 patients for 1 month, 1 for 2 to 3 consecutive months, and 1 for more than 3 consecutive months.
Four patients achieved a complete response (CR) and 3 a partial response (PR), for an overall response rate (ORR) of 58%.
There were no dose-limiting toxicities (DLTs) in the trial.
John Mascarenhas, MD, of Icahn School of Medicine at Mount Sinai in New York, New York, reported these results at the 2017 ASH Annual Meeting as abstract 254.*
The study was supported by Roche and funded by the National Cancer Institute, PDRC, and a grant from the Leukemia and Lymphoma Society.
Study rationale
Patients with PV have higher levels of MDM2 in their CD34+ cells compared to normal CD34+ cells. Nutlins block the interaction between p53 and MDM2, thus activating the p53 pathway.
Investigators previously found that low doses of nutlin and pegylated IFNα 2a promoted apoptosis in PV CD34+ cells.
And treatment with the combination reduced the numbers of JAK2V617-positive cells transplanted into immune-deficient NOD/SCID mice.
So Dr Mascarenhas and his colleagues undertook a study (NCT02407080) to evaluate the toxicity, safety, and tolerability of the MDM2 antagonist idasanutlin in patients with PV and essential thrombocythemia (ET).
The investigators hypothesized that since overexpression of MDM2 negatively regulates wild-type p53 function in primary PV cells, idasanutlin therapy, either alone or in combination with low-dose peg-IFN, could result in selective reduction or elimination of the myeloproliferative neoplasm cells in PV patients.
Study design
The investigators evaluated 2 dose levels of idasanutlin—100 mg daily and 150 mg daily on days 1 to 5, repeated every 28 days. The first cycle was 56 days to allow investigators to evaluate any DLTs.
Dr Mascarenhas pointed out that the dose is 1/6 of that being evaluated in acute myeloid leukemia.
Investigators defined a DLT as a non-hematologic adverse event (AE) of grade 3 or higher or a hematologic AE of grade 2 or higher thrombocytopenia or grade 3 or higher neutropenia or anemia.
If patients did not achieve at least a PR by the end of cycle 3 of single-agent therapy, they could proceed to Part B of the study and receive idasanutlin with pegylated IFN.
After cycle 3, dosing was dependent upon patients hitting a hematocrit greater than 42% and/or platelet counts greater than 400,000.
“So you had to meet parameters, which means that if you did meet parameters, you could get a treatment holiday,” Dr Mascarenhas explained.
Patients were eligible if they had JAK2V617F-positive PV or ET confirmed by WHO diagnostic criteria.
They had to have high-risk disease, be older than 60, and have a history of thrombosis. They also had to be either intolerant or resistant to at least one prior treatment, including hydroxyurea, interferon, or anagrelide.
Patients were excluded if they had post-ET/PV myelofibrosis, blast phase disease, acute thrombosis within 3 months of screening, or uncontrolled inter-current illness.
Baseline patient characteristics
Eleven of the 12 patients enrolled had PV, and 1 had ET. Their median age was 63.5, and 7 were female. Their median duration of disease was 43.9 months (range, 14.9–154.3), 3 had previous thrombosis, and 10 had prior hydroxyurea therapy.
They had a median leukocyte count of 11.3 x 109/L, median hemoglobin levels of 13.6 g/dL, median hematocrit of 42.3%, and median platelet levels of 443.5 x 109/L.
They all had the JAK2V617F mutation. Some patients had additional mutations, including TET2, DNMT3A, ASXL1, CBL, and EZH2, among others.
“One patient had an inactivating p53 mutation,” Dr Mascarenhas said. “I didn’t know this when we put her on study. . . , but this is an interesting part of the study. So remember, one patient had an inactivating p53 mutation in a trial where I’m using a drug that interrupts wild-type p53-MDM2 interaction.”
Efficacy
Plasma MIC-1 levels were significantly increased (P=0.004) in PV patients following treatment with idasanutlin at day 5 compared to day 1. MIC-1 is a secreted protein strongly induced by activated p53.
“Some patients didn’t need to be treated every month,” Dr Mascarenhas said. “They got treatment holidays. That’s unique. I don’t usually see that in the treatments that we give. In fact, this one person here, after 3 cycles, didn’t need to be re-treated for 9 months.”
In the 100 mg cohort (n=6), patients received a median of 8 cycles of idasanutlin (range, 7-13) and were on study for a median of 34.1 weeks (range, 29.0–127.3). One patient experienced a treatment holiday of 1 month, and another patient had a treatment holiday of more than 3 consecutive months.
In the 150 mg cohort (n=6), patients received a median of 9.5 cycles of therapy (range, 5–17) and were on study for a median of 52.1 weeks (range, 23.1–72.9). Three patients experienced a 1-month treatment holiday, and 1 patient had a 2- to 3-month treatment holiday.
In total, 6 patients continued the single-agent regimen, and 4 proceeded to the combination treatment with pegylated IFN.
Reasons for discontinuation were patient refusal and investigator decision.
The ORR (CR + PR) for both dose cohorts with single-agent idasanutlin was 58%. One patient was not evaluable, 4 had no response, 3 had a PR, and 4 had a CR.
In the combination portion of the study, the ORR was 50%. One patient was not evaluable, 1 had no response, 1 had a PR, and 1 had a CR.
“The 1 non-responder in Part B,” Dr Mascarenhas noted, “was the p53-mutated patient. Makes sense.”
The ORR for both the single-agent and combination parts of the study was 75%.
Eight of 12 patients had a 50% reduction in total symptom score from baseline, which is considered clinically meaningful, according to Dr Mascarenhas.
“What’s also interesting,” he pointed out, “[ is that] patients who didn’t obtain a response also enjoyed symptom benefit.”
Patients had a median 43% reduction in JAK2 mutation from baseline.
“One patient had nearly 92% reduction in JAK2V617F,” Dr Mascarenhas said. “One patient had a 60% increase. But guess what? That was the p53-mutated patient. Makes sense.”
Bone morphology showed reduction in marrow hypercellularity and normalization of megakaryocyte atypia and clustering.
Safety
There were no DLTs with either dose of idasanutlin.
“This was a well-tolerated drug,” Dr Mascarenhas said.
Three patients experienced grade 3 non-hematologic treatment-emergent AEs, all at 100 mg, of fatigue (1 patient), headache (1 patient), and pain (1 patient).
No grade 4 non-hematologic treatment-emergent AEs occurred at either dose, and investigators observed no hematologic AE of any grade.
Investigators also observed no grade 3–4 gastrointestinal (GI) treatment-emergent AEs. Constipation (91.7%), nausea (75%), and diarrhea (66.7%) were the most frequent grade 1 or 2 events. Patients received GI prophylaxis upfront with ondansetron, lorazepam, or dexamethasone.
Because of the safety profile and manageable GI toxicity, the higher dose of idasanutlin was chosen as the recommended phase 2 dose.
A global, multicenter, single-arm, phase 2 trial with idasanutlin in patients with hydroxyurea-resistant or -intolerant PV is underway. ![]()
*Data in the presentation differ from the abstract.
Allo-HSCT leads to long-term survival in MF
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
ATLANTA—One of the largest single-center studies of fludarabine/melphalan-based allogeneic hematopoietic stem cell transplant (allo-HSCT) for patients with myelofibrosis (MF) shows excellent overall survival (OS) with a low risk of relapse, according to investigators.
Allo-HSCT is the only potential curative treatment modality for MF.
However, it is associated with risks of transplant-related morbidity and mortality from graft-versus-host disease (GVHD), infection, graft rejection, and regimen-related toxicities.
This necessitates careful patient selection and intense peri-transplant management, said study investigator Haris Ali, MD, of the City of Hope Medical Center in Duarte, California.
He noted that there has been a 5-fold increase in allo-HSCT in the last 2 decades, mainly among older patients, due to the increase in reduced-intensity conditioning.
At the 2017 ASH Annual Meeting (in abstract 199), Dr Ali reported on a cohort of 110 MF patients who underwent allo-HSCT with fludarabine/melphalan conditioning at City of Hope between 2004 and 2017.
The patients, 58 with primary MF and 52 with secondary MF, were without prior acute leukemic transformation. They were a median age of 58.5 at the time of transplant, with a median interval of 15.2 months from MF diagnosis.
Virtually all (n=107) received peripheral blood stem cells, and 3 were transplanted with bone marrow as the stem cell source. Forty-nine allo-HSCT donors were matched related, 32 were matched unrelated, 27 were mismatched unrelated, 1 was mismatched relative, and 1 was haploidentical family.
Three-quarters of the patients had intermediate-2 or high-risk disease. Of the 110 patients, 16 had splenectomy prior to allo-HSCT. All but 2 patients engrafted.
After a median follow-up of 56.8 months, the 2-year OS rate was 74%, and the 5-year OS rate was 65%.
Non-relapse mortality at 2 years was 12%. At 5 years, it was 24%.
“The risk of non-relapse mortality was acceptable, considering the relatively older age of a large subset of patients; nearly half were over age 60 at allo-HSCT,” Dr Ali said.
In a univariate analysis, mismatched donors and matched unrelated donors were significantly associated with worse OS compared with matched related donors.
The cumulative incidence of relapse was 17% at 2 years and 5 years.
Splenectomy prior to transplant was associated with higher relapse risk, Dr Ali noted.
“Cytogenetic abnormalities were not associated with transplant relapse or other outcomes in our cohort,” he added.
Mutational changes are being tested in pre-transplant samples and will be reported at a later date.
The incidence of grade 2-4 and 3-4 acute GVHD at 100 days was 45% and 17%, respectively.
At 36 months, the cumulative incidence of all chronic GVHD was 66%. For extensive chronic GVHD, it was 59%.
“Interestingly, prior use of ruxolitinib increased the risk of grade 3-4 acute GVHD, possibly due to known inflammatory cytokine rebound,” Dr Ali said.
Extended use of ruxolitinib until day 30 or longer is currently being evaluated in a prospective trial at City of Hope (NCT02917096).
Dr Ali disclosed consulting fees from Incyte. ![]()
Ruxolitinib improves survival for MF patients in CP-e
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures. ![]()
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures. ![]()
ATLANTA—A new study suggests the JAK2 inhibitor ruxolitinib has the potential to significantly improve survival in patients who have chronic phase (CP) myelofibrosis (MF), with or without elevated blasts.
In this retrospective study, researchers found evidence to suggest that MF patients in CP with elevated blasts (CP-e) should be considered a high-risk group.
However, ruxolitinib significantly improved overall survival (OS) in CP-e patients—who had 5% to 9% blasts in the bone marrow or peripheral blood—and in patients with CP and less than 5% blasts.
On the other hand, ruxolitinib had no impact on the rate of progression to acute myeloid leukemia (AML) in CP or CP-e patients.
Lucia Masarova, MD, of The University of Texas MD Anderson Cancer Center in Houston, presented these findings at the 2017 ASH Annual Meeting (abstract 201).
Clinical characteristics of MF CP-e patients are not well described, and the outcome of available therapy in this population is largely unknown. Therefore, Dr Masarova and her colleagues set out to evaluate the effects of ruxolitinib on CP-e patients.
The team conducted a retrospective chart review of 1199 MF patients, 832 with primary MF, 169 with post-essential thrombocythemia MF, and 198 with post-polycythemia vera MF. About two-thirds of the patients were newly diagnosed.
The majority of patients (85%, n=1020) were in CP with less than 5% blasts, 10% (n=123) were in CP-e, and 5% (n=56) were in accelerated phase (AP, 10% to 19% blasts).
CP-e patients had similar clinical characteristics as patients in AP. Both groups had higher white blood cell counts; lower hemoglobin and platelets; and more frequent splenomegaly, systemic symptoms, and presence of abnormal and unfavorable karyotype than CP patients.
Among the 1030 treated patients, ruxolitinib was used in 30% (n=328), including 28% of CP patients (n=289), 27% of CP-e patients (n=33), and 11% of AP patients (n=6). The median treatment duration was about 22 months in the CP and CP-e groups.
After a median follow-up of 27 months, half the patients studied had died.
“Patients in the [CP-e] group had similar OS as those in AP, which was inferior to patients in CP,” Dr Masarova said.
The median OS was 48 months for the entire cohort, 56 months in the CP group, 34 months in the CP-e group, and 23 months in the AP group.
One-year OS rates were 86% for the CP group, 73% for the CP-e group, and 65% for the AP group. Five-year OS rates were 46%, 24%, and 21%, respectively.
CP and CP-e patients had superior OS if they had received ruxolitinib.
Among CP patients, the median OS was 61 months in those who received ruxolitinib and 54 months in those who did not (hazard ratio=0.85, P=0.002).
Among CP-e patients, the median OS was 54 months in those who received ruxolitinib and 27 months in those who did not (hazard ratio=0.50, P=0.001).
Ruxolitinib had no impact on OS in AP patients, which was 23 months with or without the drug. However, Dr Masarova noted that the AP patient numbers were small.
Progression to AML occurred in 9% of patients overall (n=139), 9% in the CP group, 20% in the CP-e group, and 39% in the AP group.
Ruxolitinib had no impact on the rate of AML progression, which was 9% in CP patients, with and without the drug.
In CP-e patients, AML progression occurred in 22% of those who received ruxolitinib and 18% of those who did not.
“The [CP-e] patients are similar to AP patients, with adverse clinical characteristics, inferior OS, and a 20% to 40% AML rate,” Dr Masarova said. “Ruxolitinib improves survival of [CP-e] patients, which is similar to CP patients on the drug.”
CP-e patients should be considered a high-risk population, she said, adding “we need to find new, better treatments for these patients.”
Dr Masarova had no disclosures. ![]()
CHMP recommends generic drug for ET
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation. ![]()
Plek2 may be therapeutic target in MPNs
New research suggests plecktrin-2 (Plek2) may be a therapeutic target for myeloproliferative neoplasms (MPNs).
Plek2 was previously shown to be involved in red blood cell production.
Now, researchers have found Plek2 is upregulated in patients with JAK2V617F-positive MPNs.
And loss of Plek2 ameliorated JAK2V617F-induced myeloproliferative phenotypes in a mouse model.
Peng Ji, MD, PhD, of Northwestern University in Chicago, Illinois, and his colleagues conducted this research and reported the results in The Journal of Clinical Investigation.
The researchers found that Plek2 was significantly upregulated in patients with JAK2V617F-positive MPNs, including myelofibrosis, essential thrombocythemia, and polycythemia vera.
Plek2 was also upregulated in myeloid, lymphoid, and erythroid cells in a JAK2V617F hematopoietic-specific knock-in mouse model that mimics the pathogenesis of MPNs.
The researchers assessed the effects of turning off Plek2 in this model and found that loss of Plek2 significantly reverted neutrophilia and thrombocytosis, partially reverted reticulocytosis, mildly reduced red blood cell count, significantly reduced megakaryocyte numbers and clusters, and reduced spleen size.
Loss of Plek2 also reduced red blood cell mass, which was the main contributing factor in the reversion of vascular occlusions, according to the researchers. The team detected “widespread vascular occlusions” in mice with Plek2, but mice without Plek2 had “relatively clear vasculature.”
“The risk of thrombosis was not completely cured because there are other factors aside from pleckstrin-2, but we saw a very dramatic amelioration in blood clotting,” Dr Ji said.
Finally, loss of Plek2 improved survival. All mice with Plek2 died at around 30 weeks, but more than 80% of the mice without Plek2 survived beyond 40 weeks.
Dr Ji and his colleagues hope to build upon these findings by developing a Plek2 inhibitor.
“We are looking for a molecule that can bind with pleckstrin-2 and block its functions,” Dr Ji said. “We’ve already screened compounds, and we have about 40 we are testing right now.”
“Mice with pleckstrin-2 deactivated experienced fewer side effects compared to mice without JAK2, so we believe the pleckstrin-2 inhibitor will generate fewer side effects as well.” ![]()
New research suggests plecktrin-2 (Plek2) may be a therapeutic target for myeloproliferative neoplasms (MPNs).
Plek2 was previously shown to be involved in red blood cell production.
Now, researchers have found Plek2 is upregulated in patients with JAK2V617F-positive MPNs.
And loss of Plek2 ameliorated JAK2V617F-induced myeloproliferative phenotypes in a mouse model.
Peng Ji, MD, PhD, of Northwestern University in Chicago, Illinois, and his colleagues conducted this research and reported the results in The Journal of Clinical Investigation.
The researchers found that Plek2 was significantly upregulated in patients with JAK2V617F-positive MPNs, including myelofibrosis, essential thrombocythemia, and polycythemia vera.
Plek2 was also upregulated in myeloid, lymphoid, and erythroid cells in a JAK2V617F hematopoietic-specific knock-in mouse model that mimics the pathogenesis of MPNs.
The researchers assessed the effects of turning off Plek2 in this model and found that loss of Plek2 significantly reverted neutrophilia and thrombocytosis, partially reverted reticulocytosis, mildly reduced red blood cell count, significantly reduced megakaryocyte numbers and clusters, and reduced spleen size.
Loss of Plek2 also reduced red blood cell mass, which was the main contributing factor in the reversion of vascular occlusions, according to the researchers. The team detected “widespread vascular occlusions” in mice with Plek2, but mice without Plek2 had “relatively clear vasculature.”
“The risk of thrombosis was not completely cured because there are other factors aside from pleckstrin-2, but we saw a very dramatic amelioration in blood clotting,” Dr Ji said.
Finally, loss of Plek2 improved survival. All mice with Plek2 died at around 30 weeks, but more than 80% of the mice without Plek2 survived beyond 40 weeks.
Dr Ji and his colleagues hope to build upon these findings by developing a Plek2 inhibitor.
“We are looking for a molecule that can bind with pleckstrin-2 and block its functions,” Dr Ji said. “We’ve already screened compounds, and we have about 40 we are testing right now.”
“Mice with pleckstrin-2 deactivated experienced fewer side effects compared to mice without JAK2, so we believe the pleckstrin-2 inhibitor will generate fewer side effects as well.” ![]()
New research suggests plecktrin-2 (Plek2) may be a therapeutic target for myeloproliferative neoplasms (MPNs).
Plek2 was previously shown to be involved in red blood cell production.
Now, researchers have found Plek2 is upregulated in patients with JAK2V617F-positive MPNs.
And loss of Plek2 ameliorated JAK2V617F-induced myeloproliferative phenotypes in a mouse model.
Peng Ji, MD, PhD, of Northwestern University in Chicago, Illinois, and his colleagues conducted this research and reported the results in The Journal of Clinical Investigation.
The researchers found that Plek2 was significantly upregulated in patients with JAK2V617F-positive MPNs, including myelofibrosis, essential thrombocythemia, and polycythemia vera.
Plek2 was also upregulated in myeloid, lymphoid, and erythroid cells in a JAK2V617F hematopoietic-specific knock-in mouse model that mimics the pathogenesis of MPNs.
The researchers assessed the effects of turning off Plek2 in this model and found that loss of Plek2 significantly reverted neutrophilia and thrombocytosis, partially reverted reticulocytosis, mildly reduced red blood cell count, significantly reduced megakaryocyte numbers and clusters, and reduced spleen size.
Loss of Plek2 also reduced red blood cell mass, which was the main contributing factor in the reversion of vascular occlusions, according to the researchers. The team detected “widespread vascular occlusions” in mice with Plek2, but mice without Plek2 had “relatively clear vasculature.”
“The risk of thrombosis was not completely cured because there are other factors aside from pleckstrin-2, but we saw a very dramatic amelioration in blood clotting,” Dr Ji said.
Finally, loss of Plek2 improved survival. All mice with Plek2 died at around 30 weeks, but more than 80% of the mice without Plek2 survived beyond 40 weeks.
Dr Ji and his colleagues hope to build upon these findings by developing a Plek2 inhibitor.
“We are looking for a molecule that can bind with pleckstrin-2 and block its functions,” Dr Ji said. “We’ve already screened compounds, and we have about 40 we are testing right now.”
“Mice with pleckstrin-2 deactivated experienced fewer side effects compared to mice without JAK2, so we believe the pleckstrin-2 inhibitor will generate fewer side effects as well.” ![]()
FDA approves first treatment for ECD
The US Food and Drug Administration (FDA) has expanded the approved use of vemurafenib (Zelboraf) to include the treatment of adults who have Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug was already approved by the FDA to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation, as detected by an FDA-approved test.
Now, vemurafenib is the first FDA-approved treatment for ECD.
The FDA previously granted vemurafenib orphan drug and breakthrough therapy designations for this indication, and the supplemental new drug application for vemurafenib in ECD received priority review.
“Today’s approval of Zelboraf for patients with ECD demonstrates how we can apply knowledge of the underlying genetic characteristics of certain malignancies to other cancers,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“This product was first approved in 2011 to treat certain patients with melanoma that harbor the BRAF V600E mutation, and we are now bringing the therapy to patients with a rare cancer with no approved therapies.”
The application for vemurafenib in ECD was supported by data from the phase 2 VE-BASKET study. Initial results from this study were published in NEJM in August 2015.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
In the 22 patients with ECD, the best overall response rate was 54.5%. Eleven patients experienced a partial response, and 1 patient achieved a complete response.
The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events (>50%) were joint pain, rash, hair loss, fatigue, change in heart rhythm, and skin tags. The most common grade 3 or higher adverse events (≥10%) were new skin cancers, high blood pressure, rash, and joint pain. ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of vemurafenib (Zelboraf) to include the treatment of adults who have Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug was already approved by the FDA to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation, as detected by an FDA-approved test.
Now, vemurafenib is the first FDA-approved treatment for ECD.
The FDA previously granted vemurafenib orphan drug and breakthrough therapy designations for this indication, and the supplemental new drug application for vemurafenib in ECD received priority review.
“Today’s approval of Zelboraf for patients with ECD demonstrates how we can apply knowledge of the underlying genetic characteristics of certain malignancies to other cancers,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“This product was first approved in 2011 to treat certain patients with melanoma that harbor the BRAF V600E mutation, and we are now bringing the therapy to patients with a rare cancer with no approved therapies.”
The application for vemurafenib in ECD was supported by data from the phase 2 VE-BASKET study. Initial results from this study were published in NEJM in August 2015.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
In the 22 patients with ECD, the best overall response rate was 54.5%. Eleven patients experienced a partial response, and 1 patient achieved a complete response.
The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events (>50%) were joint pain, rash, hair loss, fatigue, change in heart rhythm, and skin tags. The most common grade 3 or higher adverse events (≥10%) were new skin cancers, high blood pressure, rash, and joint pain. ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of vemurafenib (Zelboraf) to include the treatment of adults who have Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug was already approved by the FDA to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation, as detected by an FDA-approved test.
Now, vemurafenib is the first FDA-approved treatment for ECD.
The FDA previously granted vemurafenib orphan drug and breakthrough therapy designations for this indication, and the supplemental new drug application for vemurafenib in ECD received priority review.
“Today’s approval of Zelboraf for patients with ECD demonstrates how we can apply knowledge of the underlying genetic characteristics of certain malignancies to other cancers,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“This product was first approved in 2011 to treat certain patients with melanoma that harbor the BRAF V600E mutation, and we are now bringing the therapy to patients with a rare cancer with no approved therapies.”
The application for vemurafenib in ECD was supported by data from the phase 2 VE-BASKET study. Initial results from this study were published in NEJM in August 2015.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
In the 22 patients with ECD, the best overall response rate was 54.5%. Eleven patients experienced a partial response, and 1 patient achieved a complete response.
The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events (>50%) were joint pain, rash, hair loss, fatigue, change in heart rhythm, and skin tags. The most common grade 3 or higher adverse events (≥10%) were new skin cancers, high blood pressure, rash, and joint pain. ![]()
NCCN releases new guidelines for patients with MPNs
The National Comprehensive Cancer Network® (NCCN) has released new guidelines for patients with myeloproliferative neoplasms (MPNs).
The guidelines include information on the diagnosis and treatment of polycythemia vera, essential thrombocythemia, and myelofibrosis.
NCCN Guidelines for Patients® are written in plain language and include tools such as suggested questions for doctors, a glossary of terms, and medical illustrations of anatomy, tests, and treatment.
NCCN also provides accompanying Quick Guide™ sheets, which are short summaries of key points in the guidelines.
The patient guidelines and Quick Guide sheet for MPNs are available to read and download for free from the NCCN website and via the NCCN Patient Guides for Cancer mobile app. Printed editions can be ordered from Amazon.com for a fee.
“As a physician, I find it makes a difference when patients and caregivers have access to the information they need when making treatment decisions, to complement what they’re hearing from me,” said Brady L. Stein, MD, an associate professor at Northwestern University in Chicago, Illinois, and a member of the NCCN Clinical Practice Guidelines in Oncology Panel for MPN.
“Sitting in the hematologists’ office can be an overwhelming experience. These patient guidelines provide the most comprehensive at-home resource available for people with these rare diseases. They cover everything from basic explanations to complicated decision-making around diagnostic confirmation, supportive care techniques, treatment sequencing, adverse effects, and more.”
NCCN also has patient guidelines on acute lymphoblastic leukemia, adolescents and young adults with cancer, chronic lymphocytic leukemia, chronic myelogenous leukemia*, distress/supportive care, Hodgkin lymphoma, multiple myeloma*, myelodysplastic syndromes*, nausea and vomiting/supportive care, non-Hodgkin lymphomas, Waldenström’s macroglobulinemia, and a range of solid tumor malignancies. ![]()
*Guidelines with new updates coming soon.
The National Comprehensive Cancer Network® (NCCN) has released new guidelines for patients with myeloproliferative neoplasms (MPNs).
The guidelines include information on the diagnosis and treatment of polycythemia vera, essential thrombocythemia, and myelofibrosis.
NCCN Guidelines for Patients® are written in plain language and include tools such as suggested questions for doctors, a glossary of terms, and medical illustrations of anatomy, tests, and treatment.
NCCN also provides accompanying Quick Guide™ sheets, which are short summaries of key points in the guidelines.
The patient guidelines and Quick Guide sheet for MPNs are available to read and download for free from the NCCN website and via the NCCN Patient Guides for Cancer mobile app. Printed editions can be ordered from Amazon.com for a fee.
“As a physician, I find it makes a difference when patients and caregivers have access to the information they need when making treatment decisions, to complement what they’re hearing from me,” said Brady L. Stein, MD, an associate professor at Northwestern University in Chicago, Illinois, and a member of the NCCN Clinical Practice Guidelines in Oncology Panel for MPN.
“Sitting in the hematologists’ office can be an overwhelming experience. These patient guidelines provide the most comprehensive at-home resource available for people with these rare diseases. They cover everything from basic explanations to complicated decision-making around diagnostic confirmation, supportive care techniques, treatment sequencing, adverse effects, and more.”
NCCN also has patient guidelines on acute lymphoblastic leukemia, adolescents and young adults with cancer, chronic lymphocytic leukemia, chronic myelogenous leukemia*, distress/supportive care, Hodgkin lymphoma, multiple myeloma*, myelodysplastic syndromes*, nausea and vomiting/supportive care, non-Hodgkin lymphomas, Waldenström’s macroglobulinemia, and a range of solid tumor malignancies. ![]()
*Guidelines with new updates coming soon.
The National Comprehensive Cancer Network® (NCCN) has released new guidelines for patients with myeloproliferative neoplasms (MPNs).
The guidelines include information on the diagnosis and treatment of polycythemia vera, essential thrombocythemia, and myelofibrosis.
NCCN Guidelines for Patients® are written in plain language and include tools such as suggested questions for doctors, a glossary of terms, and medical illustrations of anatomy, tests, and treatment.
NCCN also provides accompanying Quick Guide™ sheets, which are short summaries of key points in the guidelines.
The patient guidelines and Quick Guide sheet for MPNs are available to read and download for free from the NCCN website and via the NCCN Patient Guides for Cancer mobile app. Printed editions can be ordered from Amazon.com for a fee.
“As a physician, I find it makes a difference when patients and caregivers have access to the information they need when making treatment decisions, to complement what they’re hearing from me,” said Brady L. Stein, MD, an associate professor at Northwestern University in Chicago, Illinois, and a member of the NCCN Clinical Practice Guidelines in Oncology Panel for MPN.
“Sitting in the hematologists’ office can be an overwhelming experience. These patient guidelines provide the most comprehensive at-home resource available for people with these rare diseases. They cover everything from basic explanations to complicated decision-making around diagnostic confirmation, supportive care techniques, treatment sequencing, adverse effects, and more.”
NCCN also has patient guidelines on acute lymphoblastic leukemia, adolescents and young adults with cancer, chronic lymphocytic leukemia, chronic myelogenous leukemia*, distress/supportive care, Hodgkin lymphoma, multiple myeloma*, myelodysplastic syndromes*, nausea and vomiting/supportive care, non-Hodgkin lymphomas, Waldenström’s macroglobulinemia, and a range of solid tumor malignancies.
*Guidelines with new updates coming soon.
JAK inhibitors face off in myelofibrosis trial
Results of the SIMPLIFY-1 study revealed how 2 JAK inhibitors—momelotinib and ruxolitinib—compared to one another in myelofibrosis (MF) patients who were previously JAK-inhibitor-naïve.
Momelotinib proved noninferior to ruxolitinib when it came to spleen reduction but not symptom response.
On the other hand, momelotinib was more effective than ruxolitinib in reducing transfusion dependence.
The overall incidence of adverse events (AEs) was similar between the treatment arms.
However, patients receiving momelotinib were more likely to experience AEs leading to treatment discontinuation.
Ruben A. Mesa, MD, of Mayo Clinic Cancer Center in Phoenix, Arizona, and his colleagues reported these results in the Journal of Clinical Oncology. The study was sponsored by Gilead Sciences.
SIMPLIFY-1 was a phase 3, double-blind, active-controlled study. It enrolled 432 patients with symptomatic intermediate-1-risk MF, intermediate-2-risk MF, or high-risk MF.
These JAK-inhibitor-naïve patients were randomized to receive 24 weeks of treatment with momelotinib (n=215, 200 mg once daily) or ruxolitinib (n=217, 20 mg twice a day or per label). After that, all patients could receive open-label momelotinib.
The researchers said baseline characteristics were similar between the treatment arms. In the overall cohort, most patients were white (82.6%), male (56.5%), 65 or older (57.2%), and had primary MF (56.5%).
In all, 376 patients completed 24 weeks of treatment—175 in the momelotinib arm and 201 in the ruxolitinib arm. And 368 patients proceeded to the open-label phase of the study—171 from the momelotinib arm and 197 from the ruxolitinib arm (who switched to momelotinib).
Efficacy
The primary efficacy endpoint was spleen response rate at 24 weeks, which was defined as the proportion of patients achieving at least a 35% reduction in spleen volume.
This endpoint was achieved by a similar proportion of patients in both treatment arms—26.5% in the momelotinib arm and 29% in the ruxolitinib arm. This met the criteria for noninferiority (P=0.011).
On the other hand, noninferiority was not met for total symptom score, which was the proportion of patients achieving at least a 50% reduction in MF symptoms. This endpoint was achieved by 28.4% in the momelotinib arm and 42.2% in the ruxolitinib arm (P=0.98 for noninferiority).
A greater proportion of patients were transfusion-independent at week 24 in the momelotinib arm than the ruxolitinib arm—66.5% and 49.3%, respectively (nominal P<0.001).
The median rate of red blood cell transfusion was 0 units per month in the momelotinib arm and 0.4 units per month in the ruxolitinib arm (nominal P<0.001).
Safety
Most patients had at least 1 AE—92.1% in the momelotinib arm and 95.4% in the ruxolitinib arm. Grade 3 or higher AEs occurred in 35.5% and 43.5%, respectively.
Serious AEs occurred in 22.9% and 18.1%, respectively. AEs leading to treatment discontinuation occurred in 13.1% and 5.6%, respectively.
Treatment-emergent AEs occurring in at least 10% of patients in either treatment arm (momelotinib and ruxolitinib, respectively) were thrombocytopenia (18.7% and 29.2%), diarrhea (17.8% and 19.9%), headache (17.3% and 19.9%), dizziness (15.9% and 11.6%), nausea (15.9% and 3.7%), fatigue (14.5% and 12.0%), anemia (13.6% and 38%), abdominal pain (10.3% and 11.1%), and peripheral neuropathy (10.3% and 4.6%).
The most common grade 3/4 AEs in the momelotinib arm were thrombocytopenia (7.0%), anemia (5.6%), diarrhea (2.8%), hypertension (2.8%), and neutropenia (2.8%).
The most common grade 3/4 AEs in the ruxolitinib arm were anemia (23.1%), neutropenia (4.6%), thrombocytopenia (4.6%), and hypertension (4.2%).
There were 7 deaths in the momelotinib arm. The causes of death were listed as enteritis, mesenteric vein thrombosis, death, sudden death, sepsis, renal failure, and aortic dissection.
There were 7 deaths in the ruxolitinib arm as well. The causes of death were melena, sepsis, pneumonia, head injury, acute myeloid leukemia, recurrent mantle cell lymphoma, and coma.
Transformation to acute myeloid leukemia occurred in 1 patient in the momelotinib arm (grade 4) and 2 patients in the ruxolitinib arm (grade 3 and grade 5).
Results of the SIMPLIFY-1 study revealed how 2 JAK inhibitors—momelotinib and ruxolitinib—compared to one another in myelofibrosis (MF) patients who were previously JAK-inhibitor-naïve.
Momelotinib proved noninferior to ruxolitinib when it came to spleen reduction but not symptom response.
On the other hand, momelotinib was more effective than ruxolitinib in reducing transfusion dependence.
The overall incidence of adverse events (AEs) was similar between the treatment arms.
However, patients receiving momelotinib were more likely to experience AEs leading to treatment discontinuation.
Ruben A. Mesa, MD, of Mayo Clinic Cancer Center in Phoenix, Arizona, and his colleagues reported these results in the Journal of Clinical Oncology. The study was sponsored by Gilead Sciences.
SIMPLIFY-1 was a phase 3, double-blind, active-controlled study. It enrolled 432 patients with symptomatic intermediate-1-risk MF, intermediate-2-risk MF, or high-risk MF.
These JAK-inhibitor-naïve patients were randomized to receive 24 weeks of treatment with momelotinib (n=215, 200 mg once daily) or ruxolitinib (n=217, 20 mg twice a day or per label). After that, all patients could receive open-label momelotinib.
The researchers said baseline characteristics were similar between the treatment arms. In the overall cohort, most patients were white (82.6%), male (56.5%), 65 or older (57.2%), and had primary MF (56.5%).
In all, 376 patients completed 24 weeks of treatment—175 in the momelotinib arm and 201 in the ruxolitinib arm. And 368 patients proceeded to the open-label phase of the study—171 from the momelotinib arm and 197 from the ruxolitinib arm (who switched to momelotinib).
Efficacy
The primary efficacy endpoint was spleen response rate at 24 weeks, which was defined as the proportion of patients achieving at least a 35% reduction in spleen volume.
This endpoint was achieved by a similar proportion of patients in both treatment arms—26.5% in the momelotinib arm and 29% in the ruxolitinib arm. This met the criteria for noninferiority (P=0.011).
On the other hand, noninferiority was not met for total symptom score, which was the proportion of patients achieving at least a 50% reduction in MF symptoms. This endpoint was achieved by 28.4% in the momelotinib arm and 42.2% in the ruxolitinib arm (P=0.98 for noninferiority).
A greater proportion of patients were transfusion-independent at week 24 in the momelotinib arm than the ruxolitinib arm—66.5% and 49.3%, respectively (nominal P<0.001).
The median rate of red blood cell transfusion was 0 units per month in the momelotinib arm and 0.4 units per month in the ruxolitinib arm (nominal P<0.001).
Safety
Most patients had at least 1 AE—92.1% in the momelotinib arm and 95.4% in the ruxolitinib arm. Grade 3 or higher AEs occurred in 35.5% and 43.5%, respectively.
Serious AEs occurred in 22.9% and 18.1%, respectively. AEs leading to treatment discontinuation occurred in 13.1% and 5.6%, respectively.
Treatment-emergent AEs occurring in at least 10% of patients in either treatment arm (momelotinib and ruxolitinib, respectively) were thrombocytopenia (18.7% and 29.2%), diarrhea (17.8% and 19.9%), headache (17.3% and 19.9%), dizziness (15.9% and 11.6%), nausea (15.9% and 3.7%), fatigue (14.5% and 12.0%), anemia (13.6% and 38%), abdominal pain (10.3% and 11.1%), and peripheral neuropathy (10.3% and 4.6%).
The most common grade 3/4 AEs in the momelotinib arm were thrombocytopenia (7.0%), anemia (5.6%), diarrhea (2.8%), hypertension (2.8%), and neutropenia (2.8%).
The most common grade 3/4 AEs in the ruxolitinib arm were anemia (23.1%), neutropenia (4.6%), thrombocytopenia (4.6%), and hypertension (4.2%).
There were 7 deaths in the momelotinib arm. The causes of death were listed as enteritis, mesenteric vein thrombosis, death, sudden death, sepsis, renal failure, and aortic dissection.
There were 7 deaths in the ruxolitinib arm as well. The causes of death were melena, sepsis, pneumonia, head injury, acute myeloid leukemia, recurrent mantle cell lymphoma, and coma.
Transformation to acute myeloid leukemia occurred in 1 patient in the momelotinib arm (grade 4) and 2 patients in the ruxolitinib arm (grade 3 and grade 5).
Results of the SIMPLIFY-1 study revealed how 2 JAK inhibitors—momelotinib and ruxolitinib—compared to one another in myelofibrosis (MF) patients who were previously JAK-inhibitor-naïve.
Momelotinib proved noninferior to ruxolitinib when it came to spleen reduction but not symptom response.
On the other hand, momelotinib was more effective than ruxolitinib in reducing transfusion dependence.
The overall incidence of adverse events (AEs) was similar between the treatment arms.
However, patients receiving momelotinib were more likely to experience AEs leading to treatment discontinuation.
Ruben A. Mesa, MD, of Mayo Clinic Cancer Center in Phoenix, Arizona, and his colleagues reported these results in the Journal of Clinical Oncology. The study was sponsored by Gilead Sciences.
SIMPLIFY-1 was a phase 3, double-blind, active-controlled study. It enrolled 432 patients with symptomatic intermediate-1-risk MF, intermediate-2-risk MF, or high-risk MF.
These JAK-inhibitor-naïve patients were randomized to receive 24 weeks of treatment with momelotinib (n=215, 200 mg once daily) or ruxolitinib (n=217, 20 mg twice a day or per label). After that, all patients could receive open-label momelotinib.
The researchers said baseline characteristics were similar between the treatment arms. In the overall cohort, most patients were white (82.6%), male (56.5%), 65 or older (57.2%), and had primary MF (56.5%).
In all, 376 patients completed 24 weeks of treatment—175 in the momelotinib arm and 201 in the ruxolitinib arm. And 368 patients proceeded to the open-label phase of the study—171 from the momelotinib arm and 197 from the ruxolitinib arm (who switched to momelotinib).
Efficacy
The primary efficacy endpoint was spleen response rate at 24 weeks, which was defined as the proportion of patients achieving at least a 35% reduction in spleen volume.
This endpoint was achieved by a similar proportion of patients in both treatment arms—26.5% in the momelotinib arm and 29% in the ruxolitinib arm. This met the criteria for noninferiority (P=0.011).
On the other hand, noninferiority was not met for total symptom score, which was the proportion of patients achieving at least a 50% reduction in MF symptoms. This endpoint was achieved by 28.4% in the momelotinib arm and 42.2% in the ruxolitinib arm (P=0.98 for noninferiority).
A greater proportion of patients were transfusion-independent at week 24 in the momelotinib arm than the ruxolitinib arm—66.5% and 49.3%, respectively (nominal P<0.001).
The median rate of red blood cell transfusion was 0 units per month in the momelotinib arm and 0.4 units per month in the ruxolitinib arm (nominal P<0.001).
Safety
Most patients had at least 1 AE—92.1% in the momelotinib arm and 95.4% in the ruxolitinib arm. Grade 3 or higher AEs occurred in 35.5% and 43.5%, respectively.
Serious AEs occurred in 22.9% and 18.1%, respectively. AEs leading to treatment discontinuation occurred in 13.1% and 5.6%, respectively.
Treatment-emergent AEs occurring in at least 10% of patients in either treatment arm (momelotinib and ruxolitinib, respectively) were thrombocytopenia (18.7% and 29.2%), diarrhea (17.8% and 19.9%), headache (17.3% and 19.9%), dizziness (15.9% and 11.6%), nausea (15.9% and 3.7%), fatigue (14.5% and 12.0%), anemia (13.6% and 38%), abdominal pain (10.3% and 11.1%), and peripheral neuropathy (10.3% and 4.6%).
The most common grade 3/4 AEs in the momelotinib arm were thrombocytopenia (7.0%), anemia (5.6%), diarrhea (2.8%), hypertension (2.8%), and neutropenia (2.8%).
The most common grade 3/4 AEs in the ruxolitinib arm were anemia (23.1%), neutropenia (4.6%), thrombocytopenia (4.6%), and hypertension (4.2%).
There were 7 deaths in the momelotinib arm. The causes of death were listed as enteritis, mesenteric vein thrombosis, death, sudden death, sepsis, renal failure, and aortic dissection.
There were 7 deaths in the ruxolitinib arm as well. The causes of death were melena, sepsis, pneumonia, head injury, acute myeloid leukemia, recurrent mantle cell lymphoma, and coma.
Transformation to acute myeloid leukemia occurred in 1 patient in the momelotinib arm (grade 4) and 2 patients in the ruxolitinib arm (grade 3 and grade 5).
CHMP recommends approval of generic imatinib
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases.
Methotrexate could treat myeloproliferative neoplasms
Methotrexate (MTX) may be a feasible treatment option for myeloproliferative neoplasms (MPNs), according to preclinical research published in Haematologica.
Researchers tested low-dose MTX in mouse models that mimic human MPNs—essential thrombocythemia (ET) and polycythemia vera (PV).
The team found that MTX inhibited the JAK/STAT pathway, normalized some blood counts, and reduced splenomegaly in these mice.
“We have now shown pretty conclusively that we can use this approach to treat mouse models of human MPNs, results which provide a much more tangible prospect of success in humans,” said study author Martin Zeidler, PhD, of the University of Sheffield in Sheffield, UK.
Dr Zeidler and his colleagues tested MTX in transgenic mice whose endogenous JAK2 locus had been replaced by the human JAK2 V617F allele. These mice develop ET-like disease when heterozygous and PV-like disease when homozygous.
The researchers first treated wild-type mice and hJAK2 V617F age-matched littermates with either MTX or vehicle control for 28 days. The results indicated that low-dose MTX inhibits the JAK/STAT pathway.
The team then compared MTX and ruxolitinib in hJAK2 V617F-expressing mice.
MTX reduced hemoglobin levels, red blood cell counts, and hematocrit levels in heterozygous and homozygous hJAK2 V617F mice.
MTX also normalized white cell counts in heterozygous and homozygous mice, but platelet numbers and mean corpuscular volume were not significantly affected by treatment.
The researchers said MTX was as effective as ruxolitinib in these mice, but MTX treatment doesn’t result in general myelosuppression.
When the team analyzed bone marrow in the MTX-treated hJAK2 V617F mice, they found no reduction in cellularity or differentiation in any of the 3 hematopoietic lineages.
The researchers noted that homozygous mice have erythrocytic and megakaryocytic hyperplasia and polylobated nuclei in a proportion of megakaryocytes, and these phenotypes are subjectively reduced in MTX-treated mice. This suggests a disease-specific effect of MTX, rather than non-specific myelosuppression.
Both MTX and ruxolitinib reduced splenomegaly in hJAK2 V617F mice.
However, the researchers said they observed “modest increases” in reticulocyte numbers and spleen size in wild-type mice treated with MTX. These mice also had “slight increases” in pSTAT5 and PIM1 mRNA levels, but these same changes did not occur in hJAK2 V617F mice.
The researchers therefore concluded that a “detailed molecular analysis” of the interactions between MTX and wild-type JAK2 is needed.
The team is also hoping to start testing MTX in a clinical trial early next year, as these preclinical results suggest the drug could be effective in patients with ET or PV. And this might make MTX a low-cost alternative to therapies currently used to treat MPNs.
“Repurposing MTX has the potential to provide a new, molecularly targeted treatment for MPN patients within a budget accessible to healthcare systems throughout the world—a development that may ultimately provide substantial clinical and health economic benefits,” Dr Zeidler said.
Methotrexate (MTX) may be a feasible treatment option for myeloproliferative neoplasms (MPNs), according to preclinical research published in Haematologica.
Researchers tested low-dose MTX in mouse models that mimic human MPNs—essential thrombocythemia (ET) and polycythemia vera (PV).
The team found that MTX inhibited the JAK/STAT pathway, normalized some blood counts, and reduced splenomegaly in these mice.
“We have now shown pretty conclusively that we can use this approach to treat mouse models of human MPNs, results which provide a much more tangible prospect of success in humans,” said study author Martin Zeidler, PhD, of the University of Sheffield in Sheffield, UK.
Dr Zeidler and his colleagues tested MTX in transgenic mice whose endogenous JAK2 locus had been replaced by the human JAK2 V617F allele. These mice develop ET-like disease when heterozygous and PV-like disease when homozygous.
The researchers first treated wild-type mice and hJAK2 V617F age-matched littermates with either MTX or vehicle control for 28 days. The results indicated that low-dose MTX inhibits the JAK/STAT pathway.
The team then compared MTX and ruxolitinib in hJAK2 V617F-expressing mice.
MTX reduced hemoglobin levels, red blood cell counts, and hematocrit levels in heterozygous and homozygous hJAK2 V617F mice.
MTX also normalized white cell counts in heterozygous and homozygous mice, but platelet numbers and mean corpuscular volume were not significantly affected by treatment.
The researchers said MTX was as effective as ruxolitinib in these mice, but MTX treatment doesn’t result in general myelosuppression.
When the team analyzed bone marrow in the MTX-treated hJAK2 V617F mice, they found no reduction in cellularity or differentiation in any of the 3 hematopoietic lineages.
The researchers noted that homozygous mice have erythrocytic and megakaryocytic hyperplasia and polylobated nuclei in a proportion of megakaryocytes, and these phenotypes are subjectively reduced in MTX-treated mice. This suggests a disease-specific effect of MTX, rather than non-specific myelosuppression.
Both MTX and ruxolitinib reduced splenomegaly in hJAK2 V617F mice.
However, the researchers said they observed “modest increases” in reticulocyte numbers and spleen size in wild-type mice treated with MTX. These mice also had “slight increases” in pSTAT5 and PIM1 mRNA levels, but these same changes did not occur in hJAK2 V617F mice.
The researchers therefore concluded that a “detailed molecular analysis” of the interactions between MTX and wild-type JAK2 is needed.
The team is also hoping to start testing MTX in a clinical trial early next year, as these preclinical results suggest the drug could be effective in patients with ET or PV. And this might make MTX a low-cost alternative to therapies currently used to treat MPNs.
“Repurposing MTX has the potential to provide a new, molecularly targeted treatment for MPN patients within a budget accessible to healthcare systems throughout the world—a development that may ultimately provide substantial clinical and health economic benefits,” Dr Zeidler said.
Methotrexate (MTX) may be a feasible treatment option for myeloproliferative neoplasms (MPNs), according to preclinical research published in Haematologica.
Researchers tested low-dose MTX in mouse models that mimic human MPNs—essential thrombocythemia (ET) and polycythemia vera (PV).
The team found that MTX inhibited the JAK/STAT pathway, normalized some blood counts, and reduced splenomegaly in these mice.
“We have now shown pretty conclusively that we can use this approach to treat mouse models of human MPNs, results which provide a much more tangible prospect of success in humans,” said study author Martin Zeidler, PhD, of the University of Sheffield in Sheffield, UK.
Dr Zeidler and his colleagues tested MTX in transgenic mice whose endogenous JAK2 locus had been replaced by the human JAK2 V617F allele. These mice develop ET-like disease when heterozygous and PV-like disease when homozygous.
The researchers first treated wild-type mice and hJAK2 V617F age-matched littermates with either MTX or vehicle control for 28 days. The results indicated that low-dose MTX inhibits the JAK/STAT pathway.
The team then compared MTX and ruxolitinib in hJAK2 V617F-expressing mice.
MTX reduced hemoglobin levels, red blood cell counts, and hematocrit levels in heterozygous and homozygous hJAK2 V617F mice.
MTX also normalized white cell counts in heterozygous and homozygous mice, but platelet numbers and mean corpuscular volume were not significantly affected by treatment.
The researchers said MTX was as effective as ruxolitinib in these mice, but MTX treatment doesn’t result in general myelosuppression.
When the team analyzed bone marrow in the MTX-treated hJAK2 V617F mice, they found no reduction in cellularity or differentiation in any of the 3 hematopoietic lineages.
The researchers noted that homozygous mice have erythrocytic and megakaryocytic hyperplasia and polylobated nuclei in a proportion of megakaryocytes, and these phenotypes are subjectively reduced in MTX-treated mice. This suggests a disease-specific effect of MTX, rather than non-specific myelosuppression.
Both MTX and ruxolitinib reduced splenomegaly in hJAK2 V617F mice.
However, the researchers said they observed “modest increases” in reticulocyte numbers and spleen size in wild-type mice treated with MTX. These mice also had “slight increases” in pSTAT5 and PIM1 mRNA levels, but these same changes did not occur in hJAK2 V617F mice.
The researchers therefore concluded that a “detailed molecular analysis” of the interactions between MTX and wild-type JAK2 is needed.
The team is also hoping to start testing MTX in a clinical trial early next year, as these preclinical results suggest the drug could be effective in patients with ET or PV. And this might make MTX a low-cost alternative to therapies currently used to treat MPNs.
“Repurposing MTX has the potential to provide a new, molecularly targeted treatment for MPN patients within a budget accessible to healthcare systems throughout the world—a development that may ultimately provide substantial clinical and health economic benefits,” Dr Zeidler said.