User login
EMA recommends orphan designation for G100 to treat FL
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended orphan designation for G100 for the treatment of follicular lymphoma (FL).
G100 contains the synthetic small molecule toll-like receptor-4 agonist glucopyranosyl lipid A.
G100 works by activating innate and adaptive immunity in the tumor microenvironment to generate an immune response against the tumor’s pre-existing antigens.
Clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The induction of local and systemic immune responses has been shown in preclinical studies to result in local and abscopal tumor control.
Immune Design, the company developing G100, is currently evaluating G100 plus local radiation, with or without pembrolizumab, in a phase 1/2 trial of FL patients.
Results from this trial were presented at the 2017 ASCO Annual Meeting (abstract 7537). Nine patients who received G100 (3 patients each at the 5, 10, or 20 μg dose) with radiation (but not pembrolizumab) were evaluable for safety and efficacy.
The overall response rate was 44%, and all of these were partial responses (n=4). Thirty-three percent of patients had stable disease (n=3).
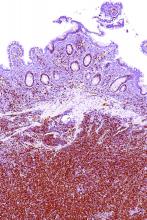
Among the responders, tumor regression ranged from 58% to 89%, which included up to 56% shrinkage of abscopal sites. Tumor biopsies showed increased inflammatory responses and T-cell infiltrates in abscopal tumors.
An additional 13 patients treated at the 10 μg dose were evaluable for safety. There were no dose-limiting toxicities, serious adverse events (AEs), or grade 3/4 AEs observed.
Common AEs included injection site disorders, abdominal pain/discomfort, nausea, pruritus, and decrease in lymphocytes.
Immune Design said that, if this trial produces a sufficiently robust clinical benefit for patients, the company may pursue FL as the first indication for regulatory approval of G100.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission. ![]()
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended orphan designation for G100 for the treatment of follicular lymphoma (FL).
G100 contains the synthetic small molecule toll-like receptor-4 agonist glucopyranosyl lipid A.
G100 works by activating innate and adaptive immunity in the tumor microenvironment to generate an immune response against the tumor’s pre-existing antigens.
Clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The induction of local and systemic immune responses has been shown in preclinical studies to result in local and abscopal tumor control.
Immune Design, the company developing G100, is currently evaluating G100 plus local radiation, with or without pembrolizumab, in a phase 1/2 trial of FL patients.
Results from this trial were presented at the 2017 ASCO Annual Meeting (abstract 7537). Nine patients who received G100 (3 patients each at the 5, 10, or 20 μg dose) with radiation (but not pembrolizumab) were evaluable for safety and efficacy.
The overall response rate was 44%, and all of these were partial responses (n=4). Thirty-three percent of patients had stable disease (n=3).
Among the responders, tumor regression ranged from 58% to 89%, which included up to 56% shrinkage of abscopal sites. Tumor biopsies showed increased inflammatory responses and T-cell infiltrates in abscopal tumors.
An additional 13 patients treated at the 10 μg dose were evaluable for safety. There were no dose-limiting toxicities, serious adverse events (AEs), or grade 3/4 AEs observed.
Common AEs included injection site disorders, abdominal pain/discomfort, nausea, pruritus, and decrease in lymphocytes.
Immune Design said that, if this trial produces a sufficiently robust clinical benefit for patients, the company may pursue FL as the first indication for regulatory approval of G100.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission. ![]()
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has recommended orphan designation for G100 for the treatment of follicular lymphoma (FL).
G100 contains the synthetic small molecule toll-like receptor-4 agonist glucopyranosyl lipid A.
G100 works by activating innate and adaptive immunity in the tumor microenvironment to generate an immune response against the tumor’s pre-existing antigens.
Clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The induction of local and systemic immune responses has been shown in preclinical studies to result in local and abscopal tumor control.
Immune Design, the company developing G100, is currently evaluating G100 plus local radiation, with or without pembrolizumab, in a phase 1/2 trial of FL patients.
Results from this trial were presented at the 2017 ASCO Annual Meeting (abstract 7537). Nine patients who received G100 (3 patients each at the 5, 10, or 20 μg dose) with radiation (but not pembrolizumab) were evaluable for safety and efficacy.
The overall response rate was 44%, and all of these were partial responses (n=4). Thirty-three percent of patients had stable disease (n=3).
Among the responders, tumor regression ranged from 58% to 89%, which included up to 56% shrinkage of abscopal sites. Tumor biopsies showed increased inflammatory responses and T-cell infiltrates in abscopal tumors.
An additional 13 patients treated at the 10 μg dose were evaluable for safety. There were no dose-limiting toxicities, serious adverse events (AEs), or grade 3/4 AEs observed.
Common AEs included injection site disorders, abdominal pain/discomfort, nausea, pruritus, and decrease in lymphocytes.
Immune Design said that, if this trial produces a sufficiently robust clinical benefit for patients, the company may pursue FL as the first indication for regulatory approval of G100.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission. ![]()
Obinutuzumab edges out rituximab for PFS in follicular lymphoma
In a head-to-head trial of anti-CD20 monoclonal antibodies in first-line therapy for follicular lymphoma, obinutuzumab-based chemotherapy was associated with slightly but significantly better progression-free survival than rituximab-based therapy, but at the cost of higher toxicities, including severe adverse events.
Among 1,202 patients with follicular lymphoma followed for a median of 34.5 months, the estimated 3-year rate of progression-free survival (PFS) for patients randomized to obinutuzumab-based chemotherapy and maintenance was 80%, compared with 73.3% for patients randomized to rituximab chemotherapy and maintenance. Response rates and overall survival were similar between the treatment groups, Robert Marcus, MB, BS, of King’s College Hospital, London, and his coinvestigators reported in the GALLIUM trial.
They acknowledged, however, that there were substantial differences between the treatment groups in the cumulative doses of obinutuzumab (Gazyva) and rituximab (Rituxan and others), which could have affected the relative efficacy of each regimen.
In addition, while patients were randomly assigned to one monoclonal antibody or the other, the choice of chemotherapy regimens, while standardized, was left to the discretion of investigators at each treatment site, another factor that might have influenced outcomes.
The investigators reported the results of a preplanned interim efficacy analysis. They compared obinutuzumab or rituximab plus chemotherapy in patients with indolent non-Hodgkin lymphoma, but the trial was powered to detect a PFS difference only in patients with follicular lymphoma. Patients who had a clinical response to induction therapy went on to maintenance therapy with the same monoclonal antibody.
In all, 1,202 patients with follicular lymphoma were enrolled and randomized, 601 in each arm, to receive induction with either intravenous obinutuzumab 1,000 mg on days 1, 8, and 15 of cycle 1 and on day 1 of subsequent cycles, or rituximab 375 mg/m2 on day 1 of each cycle for six or eight cycles, depending on the accompanying chemotherapy regimen. The regimens used were either CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), CVP (cyclophosphamide, vincristine, and prednisone), or bendamustine.
Patients with partial or complete responses were then maintained on the same monoclonal antibody they had received during induction, either obinutuzumab 1,000 mg or rituximab 375 mg/m2 every 2 months for 2 years, or until disease progression. Patients were not allowed to be crossed over to the other maintenance therapy.
Patients with stable disease after induction continued to be followed, but did not receive maintenance therapy.
The interim analysis was performed after 245 of 370 anticipated events (disease progression, relapse, or death) had occurred. At that time, the independent data and safety monitoring committee recommended full analysis of the trial data, and the sponsor agreed.
After a median follow-up of 34.5 months, an intention-to-treat analysis showed that the investigator-assessed, estimated 3-year rate of PFS was 80.0% in the obinutuzumab arm, compared with 73.3%; in the rituximab arm. This translated into a hazard ratio (HR) for progression, relapse, or death of 0.66 (P = .001). An independent review committee calculated a HR favoring obinutuzumab of 0.71 (P = .01).
Estimated 3-year overall survival rates were not significantly different at 94% and 92.1%, respectively.
Overall response rates were similar between the groups, at 88.5% with obinutuzumab group and 86.9% with rituximab, a difference that was not significant.
Obinutuzumab was associated with a higher rate of prespecified events of special interest, including infections, cardiac events, second neoplasms, infusion-related events, neutropenia, and thrombocytopenia.
Adverse events deemed to be related to the antibodies occurred in 59.3% of patients on obinutuzumab, and 48.9% of patients on rituximab.
There were more frequent grade 3 or 4 adverse events and deaths with obinutuzumab, occurring in 74.6% of patients vs. 67.8% on rituximab. Fatal adverse events occurred in 4% and 3.4% of patients, respectively.
A total of 81 patients died during the trial, including 35 in the obinutuzumab group and 46 in the rituximab group.
F. Hoffmann–La Roche supported the trial. Dr. Marcus disclosed consulting fees and lecture fees from Takeda Pharmaceuticals and travel support, consulting fees, and lecture fees from Roche. The majority of coauthors disclosed similar relationships.
Should obinutuzumab replace rituximab as the standard antibody in the treatment of patients receiving chemoimmunotherapy regimens for follicular lymphoma? Results from this trial would suggest that there might be no advantage for an obinutuzumab-containing chemoimmunotherapy regimen if maintenance treatment was not planned. Even with maintenance therapy, there is no evidence from this trial of an overall survival benefit with obinutuzumab. These findings, combined with the higher rate of toxic effects and, presumably, the higher cost of obinutuzumab, raise important questions regarding the advantage of its use. This issue is complicated further because it is possible that giving rituximab at a dose of 1,000 mg might reduce or eliminate any difference in progression-free survival – that is, if the difference is primarily a dose effect.
When the data on minimal residual disease are made available, the case in favor of obinutuzumab may appear to be more compelling if indeed a higher proportion of patients who received obinutuzumab have minimal residual disease status at some point in treatment and remain in remission longer than those who received rituximab. At the moment, the competition between these agents looks too close to call.
These comments are excerpted from an editorial (N Engl J Med. 2017 Oct 5;377;14:1389-90) by James O. Armitage, MD, University of Nebraska, Omaha, and Dan L. Longo, MD, Dana-Farber Cancer Institute, Boston. Dr. Armitage reported personal fees from Conatus, Samus Therapeutics, and Tesaro. Dr. Longo reported no relevant disclosures. He is deputy editor of The New England Journal of Medicine.
Should obinutuzumab replace rituximab as the standard antibody in the treatment of patients receiving chemoimmunotherapy regimens for follicular lymphoma? Results from this trial would suggest that there might be no advantage for an obinutuzumab-containing chemoimmunotherapy regimen if maintenance treatment was not planned. Even with maintenance therapy, there is no evidence from this trial of an overall survival benefit with obinutuzumab. These findings, combined with the higher rate of toxic effects and, presumably, the higher cost of obinutuzumab, raise important questions regarding the advantage of its use. This issue is complicated further because it is possible that giving rituximab at a dose of 1,000 mg might reduce or eliminate any difference in progression-free survival – that is, if the difference is primarily a dose effect.
When the data on minimal residual disease are made available, the case in favor of obinutuzumab may appear to be more compelling if indeed a higher proportion of patients who received obinutuzumab have minimal residual disease status at some point in treatment and remain in remission longer than those who received rituximab. At the moment, the competition between these agents looks too close to call.
These comments are excerpted from an editorial (N Engl J Med. 2017 Oct 5;377;14:1389-90) by James O. Armitage, MD, University of Nebraska, Omaha, and Dan L. Longo, MD, Dana-Farber Cancer Institute, Boston. Dr. Armitage reported personal fees from Conatus, Samus Therapeutics, and Tesaro. Dr. Longo reported no relevant disclosures. He is deputy editor of The New England Journal of Medicine.
Should obinutuzumab replace rituximab as the standard antibody in the treatment of patients receiving chemoimmunotherapy regimens for follicular lymphoma? Results from this trial would suggest that there might be no advantage for an obinutuzumab-containing chemoimmunotherapy regimen if maintenance treatment was not planned. Even with maintenance therapy, there is no evidence from this trial of an overall survival benefit with obinutuzumab. These findings, combined with the higher rate of toxic effects and, presumably, the higher cost of obinutuzumab, raise important questions regarding the advantage of its use. This issue is complicated further because it is possible that giving rituximab at a dose of 1,000 mg might reduce or eliminate any difference in progression-free survival – that is, if the difference is primarily a dose effect.
When the data on minimal residual disease are made available, the case in favor of obinutuzumab may appear to be more compelling if indeed a higher proportion of patients who received obinutuzumab have minimal residual disease status at some point in treatment and remain in remission longer than those who received rituximab. At the moment, the competition between these agents looks too close to call.
These comments are excerpted from an editorial (N Engl J Med. 2017 Oct 5;377;14:1389-90) by James O. Armitage, MD, University of Nebraska, Omaha, and Dan L. Longo, MD, Dana-Farber Cancer Institute, Boston. Dr. Armitage reported personal fees from Conatus, Samus Therapeutics, and Tesaro. Dr. Longo reported no relevant disclosures. He is deputy editor of The New England Journal of Medicine.
In a head-to-head trial of anti-CD20 monoclonal antibodies in first-line therapy for follicular lymphoma, obinutuzumab-based chemotherapy was associated with slightly but significantly better progression-free survival than rituximab-based therapy, but at the cost of higher toxicities, including severe adverse events.
Among 1,202 patients with follicular lymphoma followed for a median of 34.5 months, the estimated 3-year rate of progression-free survival (PFS) for patients randomized to obinutuzumab-based chemotherapy and maintenance was 80%, compared with 73.3% for patients randomized to rituximab chemotherapy and maintenance. Response rates and overall survival were similar between the treatment groups, Robert Marcus, MB, BS, of King’s College Hospital, London, and his coinvestigators reported in the GALLIUM trial.
They acknowledged, however, that there were substantial differences between the treatment groups in the cumulative doses of obinutuzumab (Gazyva) and rituximab (Rituxan and others), which could have affected the relative efficacy of each regimen.
In addition, while patients were randomly assigned to one monoclonal antibody or the other, the choice of chemotherapy regimens, while standardized, was left to the discretion of investigators at each treatment site, another factor that might have influenced outcomes.
The investigators reported the results of a preplanned interim efficacy analysis. They compared obinutuzumab or rituximab plus chemotherapy in patients with indolent non-Hodgkin lymphoma, but the trial was powered to detect a PFS difference only in patients with follicular lymphoma. Patients who had a clinical response to induction therapy went on to maintenance therapy with the same monoclonal antibody.
In all, 1,202 patients with follicular lymphoma were enrolled and randomized, 601 in each arm, to receive induction with either intravenous obinutuzumab 1,000 mg on days 1, 8, and 15 of cycle 1 and on day 1 of subsequent cycles, or rituximab 375 mg/m2 on day 1 of each cycle for six or eight cycles, depending on the accompanying chemotherapy regimen. The regimens used were either CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), CVP (cyclophosphamide, vincristine, and prednisone), or bendamustine.
Patients with partial or complete responses were then maintained on the same monoclonal antibody they had received during induction, either obinutuzumab 1,000 mg or rituximab 375 mg/m2 every 2 months for 2 years, or until disease progression. Patients were not allowed to be crossed over to the other maintenance therapy.
Patients with stable disease after induction continued to be followed, but did not receive maintenance therapy.
The interim analysis was performed after 245 of 370 anticipated events (disease progression, relapse, or death) had occurred. At that time, the independent data and safety monitoring committee recommended full analysis of the trial data, and the sponsor agreed.
After a median follow-up of 34.5 months, an intention-to-treat analysis showed that the investigator-assessed, estimated 3-year rate of PFS was 80.0% in the obinutuzumab arm, compared with 73.3%; in the rituximab arm. This translated into a hazard ratio (HR) for progression, relapse, or death of 0.66 (P = .001). An independent review committee calculated a HR favoring obinutuzumab of 0.71 (P = .01).
Estimated 3-year overall survival rates were not significantly different at 94% and 92.1%, respectively.
Overall response rates were similar between the groups, at 88.5% with obinutuzumab group and 86.9% with rituximab, a difference that was not significant.
Obinutuzumab was associated with a higher rate of prespecified events of special interest, including infections, cardiac events, second neoplasms, infusion-related events, neutropenia, and thrombocytopenia.
Adverse events deemed to be related to the antibodies occurred in 59.3% of patients on obinutuzumab, and 48.9% of patients on rituximab.
There were more frequent grade 3 or 4 adverse events and deaths with obinutuzumab, occurring in 74.6% of patients vs. 67.8% on rituximab. Fatal adverse events occurred in 4% and 3.4% of patients, respectively.
A total of 81 patients died during the trial, including 35 in the obinutuzumab group and 46 in the rituximab group.
F. Hoffmann–La Roche supported the trial. Dr. Marcus disclosed consulting fees and lecture fees from Takeda Pharmaceuticals and travel support, consulting fees, and lecture fees from Roche. The majority of coauthors disclosed similar relationships.
In a head-to-head trial of anti-CD20 monoclonal antibodies in first-line therapy for follicular lymphoma, obinutuzumab-based chemotherapy was associated with slightly but significantly better progression-free survival than rituximab-based therapy, but at the cost of higher toxicities, including severe adverse events.
Among 1,202 patients with follicular lymphoma followed for a median of 34.5 months, the estimated 3-year rate of progression-free survival (PFS) for patients randomized to obinutuzumab-based chemotherapy and maintenance was 80%, compared with 73.3% for patients randomized to rituximab chemotherapy and maintenance. Response rates and overall survival were similar between the treatment groups, Robert Marcus, MB, BS, of King’s College Hospital, London, and his coinvestigators reported in the GALLIUM trial.
They acknowledged, however, that there were substantial differences between the treatment groups in the cumulative doses of obinutuzumab (Gazyva) and rituximab (Rituxan and others), which could have affected the relative efficacy of each regimen.
In addition, while patients were randomly assigned to one monoclonal antibody or the other, the choice of chemotherapy regimens, while standardized, was left to the discretion of investigators at each treatment site, another factor that might have influenced outcomes.
The investigators reported the results of a preplanned interim efficacy analysis. They compared obinutuzumab or rituximab plus chemotherapy in patients with indolent non-Hodgkin lymphoma, but the trial was powered to detect a PFS difference only in patients with follicular lymphoma. Patients who had a clinical response to induction therapy went on to maintenance therapy with the same monoclonal antibody.
In all, 1,202 patients with follicular lymphoma were enrolled and randomized, 601 in each arm, to receive induction with either intravenous obinutuzumab 1,000 mg on days 1, 8, and 15 of cycle 1 and on day 1 of subsequent cycles, or rituximab 375 mg/m2 on day 1 of each cycle for six or eight cycles, depending on the accompanying chemotherapy regimen. The regimens used were either CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), CVP (cyclophosphamide, vincristine, and prednisone), or bendamustine.
Patients with partial or complete responses were then maintained on the same monoclonal antibody they had received during induction, either obinutuzumab 1,000 mg or rituximab 375 mg/m2 every 2 months for 2 years, or until disease progression. Patients were not allowed to be crossed over to the other maintenance therapy.
Patients with stable disease after induction continued to be followed, but did not receive maintenance therapy.
The interim analysis was performed after 245 of 370 anticipated events (disease progression, relapse, or death) had occurred. At that time, the independent data and safety monitoring committee recommended full analysis of the trial data, and the sponsor agreed.
After a median follow-up of 34.5 months, an intention-to-treat analysis showed that the investigator-assessed, estimated 3-year rate of PFS was 80.0% in the obinutuzumab arm, compared with 73.3%; in the rituximab arm. This translated into a hazard ratio (HR) for progression, relapse, or death of 0.66 (P = .001). An independent review committee calculated a HR favoring obinutuzumab of 0.71 (P = .01).
Estimated 3-year overall survival rates were not significantly different at 94% and 92.1%, respectively.
Overall response rates were similar between the groups, at 88.5% with obinutuzumab group and 86.9% with rituximab, a difference that was not significant.
Obinutuzumab was associated with a higher rate of prespecified events of special interest, including infections, cardiac events, second neoplasms, infusion-related events, neutropenia, and thrombocytopenia.
Adverse events deemed to be related to the antibodies occurred in 59.3% of patients on obinutuzumab, and 48.9% of patients on rituximab.
There were more frequent grade 3 or 4 adverse events and deaths with obinutuzumab, occurring in 74.6% of patients vs. 67.8% on rituximab. Fatal adverse events occurred in 4% and 3.4% of patients, respectively.
A total of 81 patients died during the trial, including 35 in the obinutuzumab group and 46 in the rituximab group.
F. Hoffmann–La Roche supported the trial. Dr. Marcus disclosed consulting fees and lecture fees from Takeda Pharmaceuticals and travel support, consulting fees, and lecture fees from Roche. The majority of coauthors disclosed similar relationships.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Obinutuzumab-based chemotherapy and maintenance was associated with better progression-free survival, but not overall survival, compared with rituximab-based chemotherapy and maintenance.
Major finding: Three-year progression-free survival was 80% with obinutuzumab, vs. 73.3% with rituximab.
Data source: Interim analysis of a randomized phase 3, open-label trial of 1,202 patients with follicular lymphoma.
Disclosures: F. Hoffmann–La Roche supported the trial. Dr. Marcus disclosed consulting fees and lecture fees from Takeda Pharmaceuticals and travel support, consulting fees, and lecture fees from Roche. The majority of coauthors disclosed similar relationships.
VCR regimen showed efficacy in mantle cell and indolent lymphomas
The combination of bortezomib, cladribine, and rituximab (VCR) was an effective treatment regimen for patients with CD20-positive mantle cell lymphoma (MCL) and indolent non-Hodgkin’s lymphoma (iNHL), based on results of a recent phase 2, open-label study.
The overall response rate was 92% in the single-center, 24-patient study. The 2-year progression-free survival (PFS) was 82% and 54%, respectively, for MCL and iNHL patients; PFS was 80% for treatment-naive patients and 57% for those with refractory/recalcitrant disease, according to Soham D. Puvvada, MD, of the University of Arizona Cancer Center in Tucson, and her associates.
Two-year overall survival was 91% for MCL and 69% for iNHL patients. Median time to progression was 34.5 months, and median PFS had not been reached at 2 years, according to the researchers.
While the study (NCT00980395) was small and limited by its single-center design, the VCR combination “has encouraging activity in both MCL and iNHL and could be compared to standard therapies in future studies,” the researchers wrote. “For MCL in particular, we believe a noninferiority comparison to standard therapies would be justified by our results.”
Adverse events were most commonly hematologic, and three patients experienced febrile neutropenia, data show.
“Although hematological toxicity can be an issue, the regimen provides an alternative option in transplant ineligible relapsed/refractory MCL and iNHL,” wrote Dr. Puvvada and her colleagues. The study was published in Clinical Lymphoma, Myeloma & Leukemia (doi: 10.1016/j.clml.2017.09.001).
The researchers studied the combination of bortezomib, the proteasome inhibitor initially approved for relapsed/refractory MCL, cladribine, which has shown activity and promising response rates in patients with indolent lymphomas, and rituximab in patients with CD20-positive mantle cell or indolent lymphoma.
Patients with follicular lymphomas were eligible to be included in the study if they had received at least one previous line of therapy. All other participants could be treatment naive or have relapsed after previous treatment.
Of the 24 patients enrolled, 11 had MCL, 5 had follicular lymphoma, 4 had marginal zone lymphoma, 3 had lymphoplasmacytic lymphoma, and 1 had small lymphocytic lymphoma.
The VCR regimen, given every 28 days for no more than six cycles, included rituximab at 375 mg/m2 given intravenously on day 1 of each cycle, cladribine 4 mg/m2 given intravenously over 2 hours on days 1 through 5, and bortezomib 1.3 mg/m2 given intravenously on days 1 and 4. Patients received a median of five cycles of therapy.
Adverse events of grade 3 or greater occurred in 14 patients (58%); 8 patients had leukopenia, 6 had thrombocytopenia, 5 had fatigue, and 5 had neutropenia, which included febrile neutropenia in 3 patients.
With a median follow-up of 38.5 months, overall response rate for VCR was 96%. Complete responses occurred in 8 of 23 evaluable patients (35%) and partial responses in 14 more patients (61%).
The combination of bortezomib, cladribine, and rituximab (VCR) was an effective treatment regimen for patients with CD20-positive mantle cell lymphoma (MCL) and indolent non-Hodgkin’s lymphoma (iNHL), based on results of a recent phase 2, open-label study.
The overall response rate was 92% in the single-center, 24-patient study. The 2-year progression-free survival (PFS) was 82% and 54%, respectively, for MCL and iNHL patients; PFS was 80% for treatment-naive patients and 57% for those with refractory/recalcitrant disease, according to Soham D. Puvvada, MD, of the University of Arizona Cancer Center in Tucson, and her associates.
Two-year overall survival was 91% for MCL and 69% for iNHL patients. Median time to progression was 34.5 months, and median PFS had not been reached at 2 years, according to the researchers.
While the study (NCT00980395) was small and limited by its single-center design, the VCR combination “has encouraging activity in both MCL and iNHL and could be compared to standard therapies in future studies,” the researchers wrote. “For MCL in particular, we believe a noninferiority comparison to standard therapies would be justified by our results.”
Adverse events were most commonly hematologic, and three patients experienced febrile neutropenia, data show.
“Although hematological toxicity can be an issue, the regimen provides an alternative option in transplant ineligible relapsed/refractory MCL and iNHL,” wrote Dr. Puvvada and her colleagues. The study was published in Clinical Lymphoma, Myeloma & Leukemia (doi: 10.1016/j.clml.2017.09.001).
The researchers studied the combination of bortezomib, the proteasome inhibitor initially approved for relapsed/refractory MCL, cladribine, which has shown activity and promising response rates in patients with indolent lymphomas, and rituximab in patients with CD20-positive mantle cell or indolent lymphoma.
Patients with follicular lymphomas were eligible to be included in the study if they had received at least one previous line of therapy. All other participants could be treatment naive or have relapsed after previous treatment.
Of the 24 patients enrolled, 11 had MCL, 5 had follicular lymphoma, 4 had marginal zone lymphoma, 3 had lymphoplasmacytic lymphoma, and 1 had small lymphocytic lymphoma.
The VCR regimen, given every 28 days for no more than six cycles, included rituximab at 375 mg/m2 given intravenously on day 1 of each cycle, cladribine 4 mg/m2 given intravenously over 2 hours on days 1 through 5, and bortezomib 1.3 mg/m2 given intravenously on days 1 and 4. Patients received a median of five cycles of therapy.
Adverse events of grade 3 or greater occurred in 14 patients (58%); 8 patients had leukopenia, 6 had thrombocytopenia, 5 had fatigue, and 5 had neutropenia, which included febrile neutropenia in 3 patients.
With a median follow-up of 38.5 months, overall response rate for VCR was 96%. Complete responses occurred in 8 of 23 evaluable patients (35%) and partial responses in 14 more patients (61%).
The combination of bortezomib, cladribine, and rituximab (VCR) was an effective treatment regimen for patients with CD20-positive mantle cell lymphoma (MCL) and indolent non-Hodgkin’s lymphoma (iNHL), based on results of a recent phase 2, open-label study.
The overall response rate was 92% in the single-center, 24-patient study. The 2-year progression-free survival (PFS) was 82% and 54%, respectively, for MCL and iNHL patients; PFS was 80% for treatment-naive patients and 57% for those with refractory/recalcitrant disease, according to Soham D. Puvvada, MD, of the University of Arizona Cancer Center in Tucson, and her associates.
Two-year overall survival was 91% for MCL and 69% for iNHL patients. Median time to progression was 34.5 months, and median PFS had not been reached at 2 years, according to the researchers.
While the study (NCT00980395) was small and limited by its single-center design, the VCR combination “has encouraging activity in both MCL and iNHL and could be compared to standard therapies in future studies,” the researchers wrote. “For MCL in particular, we believe a noninferiority comparison to standard therapies would be justified by our results.”
Adverse events were most commonly hematologic, and three patients experienced febrile neutropenia, data show.
“Although hematological toxicity can be an issue, the regimen provides an alternative option in transplant ineligible relapsed/refractory MCL and iNHL,” wrote Dr. Puvvada and her colleagues. The study was published in Clinical Lymphoma, Myeloma & Leukemia (doi: 10.1016/j.clml.2017.09.001).
The researchers studied the combination of bortezomib, the proteasome inhibitor initially approved for relapsed/refractory MCL, cladribine, which has shown activity and promising response rates in patients with indolent lymphomas, and rituximab in patients with CD20-positive mantle cell or indolent lymphoma.
Patients with follicular lymphomas were eligible to be included in the study if they had received at least one previous line of therapy. All other participants could be treatment naive or have relapsed after previous treatment.
Of the 24 patients enrolled, 11 had MCL, 5 had follicular lymphoma, 4 had marginal zone lymphoma, 3 had lymphoplasmacytic lymphoma, and 1 had small lymphocytic lymphoma.
The VCR regimen, given every 28 days for no more than six cycles, included rituximab at 375 mg/m2 given intravenously on day 1 of each cycle, cladribine 4 mg/m2 given intravenously over 2 hours on days 1 through 5, and bortezomib 1.3 mg/m2 given intravenously on days 1 and 4. Patients received a median of five cycles of therapy.
Adverse events of grade 3 or greater occurred in 14 patients (58%); 8 patients had leukopenia, 6 had thrombocytopenia, 5 had fatigue, and 5 had neutropenia, which included febrile neutropenia in 3 patients.
With a median follow-up of 38.5 months, overall response rate for VCR was 96%. Complete responses occurred in 8 of 23 evaluable patients (35%) and partial responses in 14 more patients (61%).
FROM LYMPHOMA, MYELOMA & LEUKEMIA
Key clinical point:
Major finding: The overall response rate was 92%, with a 2-year PFS of 82% and 54% for patients with mantle cell lymphoma (MCL) and indolent non-Hodgkin’s lymphoma (iNHL), respectively. Adverse events were most commonly hematologic, and three patients experienced febrile neutropenia.
Data source: A phase 2, open-label study including 24 patients with mantle cell or indolent lymphomas.
Disclosures: No disclosures were reported in the accepted manuscript.
Newer blood cancer drugs may not improve OS, QOL
A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

EC expands approval of obinutuzumab in FL
The European Commission (EC) has expanded the marketing authorization for obinutuzumab (Gazyvaro).
The drug is now approved for use in combination with chemotherapy to treat patients with previously untreated, advanced follicular lymphoma (FL). Patients who respond to this treatment can then receive obinutuzumab maintenance.
This is the third EC approval for obinutuzumab.
The drug was first approved by the EC in 2014 to be used in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia and comorbidities that make them unsuitable for full-dose fludarabine-based therapy.
In 2016, the EC approved obinutuzumab in combination with bendamustine, followed by obinutuzumab maintenance, in FL patients who did not respond to, or who progressed during or up to 6 months after, treatment with rituximab or a rituximab-containing regimen.
The EC’s latest approval of obinutuzumab is based on results of the phase 3 GALLIUM trial, which were presented at the 2016 ASH Annual Meeting.
The study enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%). ![]()
The European Commission (EC) has expanded the marketing authorization for obinutuzumab (Gazyvaro).
The drug is now approved for use in combination with chemotherapy to treat patients with previously untreated, advanced follicular lymphoma (FL). Patients who respond to this treatment can then receive obinutuzumab maintenance.
This is the third EC approval for obinutuzumab.
The drug was first approved by the EC in 2014 to be used in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia and comorbidities that make them unsuitable for full-dose fludarabine-based therapy.
In 2016, the EC approved obinutuzumab in combination with bendamustine, followed by obinutuzumab maintenance, in FL patients who did not respond to, or who progressed during or up to 6 months after, treatment with rituximab or a rituximab-containing regimen.
The EC’s latest approval of obinutuzumab is based on results of the phase 3 GALLIUM trial, which were presented at the 2016 ASH Annual Meeting.
The study enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%). ![]()
The European Commission (EC) has expanded the marketing authorization for obinutuzumab (Gazyvaro).
The drug is now approved for use in combination with chemotherapy to treat patients with previously untreated, advanced follicular lymphoma (FL). Patients who respond to this treatment can then receive obinutuzumab maintenance.
This is the third EC approval for obinutuzumab.
The drug was first approved by the EC in 2014 to be used in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia and comorbidities that make them unsuitable for full-dose fludarabine-based therapy.
In 2016, the EC approved obinutuzumab in combination with bendamustine, followed by obinutuzumab maintenance, in FL patients who did not respond to, or who progressed during or up to 6 months after, treatment with rituximab or a rituximab-containing regimen.
The EC’s latest approval of obinutuzumab is based on results of the phase 3 GALLIUM trial, which were presented at the 2016 ASH Annual Meeting.
The study enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%). ![]()
FDA grants accelerated approval to copanlisib for relapsed follicular lymphoma
The Food and Drug Administration has granted accelerated approval to copanlisib (Aliqopa) for the treatment of adults with relapsed follicular lymphoma who have received at least two prior treatments.
Approval of the kinase inhibitor was based on an overall response rate of 59% in a single-arm trial of 104 patients with follicular B-cell non-Hodgkin lymphoma who had relapsed disease following at least two prior treatments. These patients had a complete or partial response for a median 12.2 months.
“For patients with relapsed follicular lymphoma, the cancer often comes back even after multiple treatments,” Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research said in the press release. “Options are limited for these patients and today’s approval provides an additional choice for treatment, filling an unmet need for them,” he said.
The Food and Drug Administration has granted accelerated approval to copanlisib (Aliqopa) for the treatment of adults with relapsed follicular lymphoma who have received at least two prior treatments.
Approval of the kinase inhibitor was based on an overall response rate of 59% in a single-arm trial of 104 patients with follicular B-cell non-Hodgkin lymphoma who had relapsed disease following at least two prior treatments. These patients had a complete or partial response for a median 12.2 months.
“For patients with relapsed follicular lymphoma, the cancer often comes back even after multiple treatments,” Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research said in the press release. “Options are limited for these patients and today’s approval provides an additional choice for treatment, filling an unmet need for them,” he said.
The Food and Drug Administration has granted accelerated approval to copanlisib (Aliqopa) for the treatment of adults with relapsed follicular lymphoma who have received at least two prior treatments.
Approval of the kinase inhibitor was based on an overall response rate of 59% in a single-arm trial of 104 patients with follicular B-cell non-Hodgkin lymphoma who had relapsed disease following at least two prior treatments. These patients had a complete or partial response for a median 12.2 months.
“For patients with relapsed follicular lymphoma, the cancer often comes back even after multiple treatments,” Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research said in the press release. “Options are limited for these patients and today’s approval provides an additional choice for treatment, filling an unmet need for them,” he said.
Trials of atezolizumab placed on partial hold
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
FDA approves drug to treat relapsed FL
The US Food and Drug Administration (FDA) has granted accelerated approval to copanlisib (Aliqopa), an intravenous PI3K inhibitor developed by Bayer.
The drug is now approved to treat adults with relapsed follicular lymphoma (FL) who have received at least 2 prior systemic therapies.
Copanlisib received accelerated approval from the FDA because it has not yet shown a clinical benefit in these patients.
The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit.
Continued approval of copanlisib for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA previously granted copanlisib priority review, fast track designation, and orphan drug designation.
According to Bayer, copanlisib is now available. The prescribing information is available for download here.
In addition, Bayer has created the Aliqopa™ Resource Connections (ARCTM) Program, which includes resources to help patients navigate the insurance process and identify sources of financial assistance.
The program offers free medication to patients who are uninsured or underinsured and meet the eligibility criteria. It includes a $0 co-pay program for covered patients.
Phase 2 results
The FDA’s approval of copanlisib is based on data from the phase 2 CHRONOS-1 trial. Data from this trial were presented at the AACR Annual Meeting 2017 and the 2017 ASCO Annual Meeting.
The trial included 104 patients with FL who had relapsed after at least 2 prior systemic therapies.
The median duration of treatment with copanlisib was 22 weeks (range, 1-105). Thirty-three patients (32%) were still on treatment at last follow-up.
The overall response rate was 59%, with 14% of patients achieving a complete response. The median duration of response was 12.2 months (range, 0+ to 22.6).
The most common treatment-emergent adverse events (in ≥25% of patients) were diarrhea (34% all grades, 5% ≥grade 3), reduced neutrophil count (30% all grades, 24% ≥grade 3), fatigue (30% all grades, 2% ≥grade 3), and fever (25% all grades, 4% ≥grade 3).
There were 6 deaths, and 3 of them were attributed to copanlisib. One patient died of lung infection, 1 died of respiratory failure, and 1 died of a thromboembolic event. ![]()
The US Food and Drug Administration (FDA) has granted accelerated approval to copanlisib (Aliqopa), an intravenous PI3K inhibitor developed by Bayer.
The drug is now approved to treat adults with relapsed follicular lymphoma (FL) who have received at least 2 prior systemic therapies.
Copanlisib received accelerated approval from the FDA because it has not yet shown a clinical benefit in these patients.
The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit.
Continued approval of copanlisib for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA previously granted copanlisib priority review, fast track designation, and orphan drug designation.
According to Bayer, copanlisib is now available. The prescribing information is available for download here.
In addition, Bayer has created the Aliqopa™ Resource Connections (ARCTM) Program, which includes resources to help patients navigate the insurance process and identify sources of financial assistance.
The program offers free medication to patients who are uninsured or underinsured and meet the eligibility criteria. It includes a $0 co-pay program for covered patients.
Phase 2 results
The FDA’s approval of copanlisib is based on data from the phase 2 CHRONOS-1 trial. Data from this trial were presented at the AACR Annual Meeting 2017 and the 2017 ASCO Annual Meeting.
The trial included 104 patients with FL who had relapsed after at least 2 prior systemic therapies.
The median duration of treatment with copanlisib was 22 weeks (range, 1-105). Thirty-three patients (32%) were still on treatment at last follow-up.
The overall response rate was 59%, with 14% of patients achieving a complete response. The median duration of response was 12.2 months (range, 0+ to 22.6).
The most common treatment-emergent adverse events (in ≥25% of patients) were diarrhea (34% all grades, 5% ≥grade 3), reduced neutrophil count (30% all grades, 24% ≥grade 3), fatigue (30% all grades, 2% ≥grade 3), and fever (25% all grades, 4% ≥grade 3).
There were 6 deaths, and 3 of them were attributed to copanlisib. One patient died of lung infection, 1 died of respiratory failure, and 1 died of a thromboembolic event. ![]()
The US Food and Drug Administration (FDA) has granted accelerated approval to copanlisib (Aliqopa), an intravenous PI3K inhibitor developed by Bayer.
The drug is now approved to treat adults with relapsed follicular lymphoma (FL) who have received at least 2 prior systemic therapies.
Copanlisib received accelerated approval from the FDA because it has not yet shown a clinical benefit in these patients.
The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit.
Continued approval of copanlisib for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA previously granted copanlisib priority review, fast track designation, and orphan drug designation.
According to Bayer, copanlisib is now available. The prescribing information is available for download here.
In addition, Bayer has created the Aliqopa™ Resource Connections (ARCTM) Program, which includes resources to help patients navigate the insurance process and identify sources of financial assistance.
The program offers free medication to patients who are uninsured or underinsured and meet the eligibility criteria. It includes a $0 co-pay program for covered patients.
Phase 2 results
The FDA’s approval of copanlisib is based on data from the phase 2 CHRONOS-1 trial. Data from this trial were presented at the AACR Annual Meeting 2017 and the 2017 ASCO Annual Meeting.
The trial included 104 patients with FL who had relapsed after at least 2 prior systemic therapies.
The median duration of treatment with copanlisib was 22 weeks (range, 1-105). Thirty-three patients (32%) were still on treatment at last follow-up.
The overall response rate was 59%, with 14% of patients achieving a complete response. The median duration of response was 12.2 months (range, 0+ to 22.6).
The most common treatment-emergent adverse events (in ≥25% of patients) were diarrhea (34% all grades, 5% ≥grade 3), reduced neutrophil count (30% all grades, 24% ≥grade 3), fatigue (30% all grades, 2% ≥grade 3), and fever (25% all grades, 4% ≥grade 3).
There were 6 deaths, and 3 of them were attributed to copanlisib. One patient died of lung infection, 1 died of respiratory failure, and 1 died of a thromboembolic event. ![]()
Immune status linked to outcomes of CAR T-cell therapy
MAINZ/FRANKFURT, GERMANY—Outcomes of treatment with a third-generation chimeric antigen receptor (CAR) T-cell therapy are associated with a patient’s immune status, according to a phase 1/2a trial.
The CD19-specific CAR T-cell therapy produced a complete response (CR) in 6 of 15 patients with relapsed/refractory CD19-positive leukemia or lymphoma.
Though all responders eventually relapsed, 4 patients—including 2 with stable disease (SD) after treatment—responded to subsequent therapy and are still alive, 1 of them beyond 36 months.
An analysis of blood samples taken throughout the study revealed that a patient’s immune status was associated with treatment failure and overall survival.
Tanja Lövgren, PhD, of Uppsala University in Sweden, and her colleagues presented these findings at the Third CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference: Translating Science into Survival (abstract B156).
“CD19-specific CAR T-cell therapy has yielded remarkable response rates for patients who have B-cell acute lymphoblastic leukemia,” Dr Lövgren said. “However, many patients relapse.”
“In addition, response rates are more variable for patients who have other CD19-positive B-cell malignancies, and many patients experience serious adverse events. We set out to investigate the safety and effectiveness of a third-generation CD19-specific CAR T-cell therapy and to identify potential biomarkers of treatment outcome.”
Dr Lövgren and her colleagues studied 15 patients (ages 24-72) who had relapsed or refractory CD19-positive B-cell malignancies:
- Six patients with diffuse large B-cell lymphoma (DLBCL), including 3 cases that were transformed from follicular lymphoma (FL)
- Four patients with pre-B acute lymphoblastic leukemia (ALL)
- Two patients with mantle cell lymphoma (MCL)
- Two patients with chronic lymphocytic leukemia (CLL)
- One patient with FL transformed from Burkitt lymphoma.
Eleven patients received preconditioning with cyclophosphamide (500 mg/m2) and fludarabine (3 doses at 25 mg/m2).
All patients received CAR T cells at 1 x 108, 2 x 107, or 2 x 108 cells/m2. These were autologous, CD19-targeting CAR T cells with 3 intracellular signaling domains derived from CD3 zeta, CD28, and 4-1BB.
The researchers assessed tumor responses via bone marrow/blood analysis and/or radiology, depending on the type of malignancy. The team also collected blood samples before CAR T-cell infusion and at multiple times after infusion.
Efficacy and safety
Six patients achieved a CR to treatment—3 with DLBCL (1 transformed), 2 with ALL, and 1 with CLL. Two patients had SD—1 with MCL and 1 with CLL. The remaining patients progressed.
All patients with a CR eventually relapsed. The median duration of CR was 5 months (range, 3-24 months).
Four patients—2 complete responders and 2 with SD—responded well to subsequent therapy and are still alive with 27 to 36 months of follow-up. This includes 1 patient with DLBCL, 1 with MCL, and 2 with CLL.
Four patients had serious adverse events. Three had cytokine-release syndrome, and 2 had neurological toxicity.
All cases of cytokine-release syndrome resolved after treatment with corticosteroids/anti-IL6R therapy. The neurological toxicity resolved spontaneously.
Immune status
An analysis of the blood samples taken throughout the study showed that high levels of monocytic myeloid-derived suppressor cells (MDSCs) prior to treatment was associated with decreased overall survival. In addition, increased levels of MDSCs after treatment preceded treatment failure.
Furthermore, high plasma levels of immunosuppressive factors—such as PD-L1 and PD-L2—after treatment were associated with decreased overall survival.
High plasma levels of biomarkers of an immunostimulatory environment—including IL-12, DC-LAMP, TRAIL, and FasL—before the administration of CAR T-cell therapy was associated with increased overall survival.
“[A]n immunostimulatory environment was associated with improved overall survival, while immunosuppressive cells and factors were associated with treatment failure and decreased overall survival,” Dr Lövgren said.
“We are hoping to follow up this study with another clinical trial that will combine CAR T-cell therapy with chemotherapy known to decrease the number of monocytic myeloid-derived suppressive cells. We are also looking to further optimize the CAR T-cell therapy.”
Dr Lövgren said the main limitations of this study are that it only included 15 patients, the patients had several different malignancies, and some patients may have been too sick to respond to any treatment.
This study was supported by funds from AFA Insurance AB, the Swedish Cancer Society, the Swedish Research Council, the Lions Fund at Uppsala University Hospital, and the Swedish State Support for Clinical Research. Dr Lövgren declared no conflicts of interest. ![]()
MAINZ/FRANKFURT, GERMANY—Outcomes of treatment with a third-generation chimeric antigen receptor (CAR) T-cell therapy are associated with a patient’s immune status, according to a phase 1/2a trial.
The CD19-specific CAR T-cell therapy produced a complete response (CR) in 6 of 15 patients with relapsed/refractory CD19-positive leukemia or lymphoma.
Though all responders eventually relapsed, 4 patients—including 2 with stable disease (SD) after treatment—responded to subsequent therapy and are still alive, 1 of them beyond 36 months.
An analysis of blood samples taken throughout the study revealed that a patient’s immune status was associated with treatment failure and overall survival.
Tanja Lövgren, PhD, of Uppsala University in Sweden, and her colleagues presented these findings at the Third CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference: Translating Science into Survival (abstract B156).
“CD19-specific CAR T-cell therapy has yielded remarkable response rates for patients who have B-cell acute lymphoblastic leukemia,” Dr Lövgren said. “However, many patients relapse.”
“In addition, response rates are more variable for patients who have other CD19-positive B-cell malignancies, and many patients experience serious adverse events. We set out to investigate the safety and effectiveness of a third-generation CD19-specific CAR T-cell therapy and to identify potential biomarkers of treatment outcome.”
Dr Lövgren and her colleagues studied 15 patients (ages 24-72) who had relapsed or refractory CD19-positive B-cell malignancies:
- Six patients with diffuse large B-cell lymphoma (DLBCL), including 3 cases that were transformed from follicular lymphoma (FL)
- Four patients with pre-B acute lymphoblastic leukemia (ALL)
- Two patients with mantle cell lymphoma (MCL)
- Two patients with chronic lymphocytic leukemia (CLL)
- One patient with FL transformed from Burkitt lymphoma.
Eleven patients received preconditioning with cyclophosphamide (500 mg/m2) and fludarabine (3 doses at 25 mg/m2).
All patients received CAR T cells at 1 x 108, 2 x 107, or 2 x 108 cells/m2. These were autologous, CD19-targeting CAR T cells with 3 intracellular signaling domains derived from CD3 zeta, CD28, and 4-1BB.
The researchers assessed tumor responses via bone marrow/blood analysis and/or radiology, depending on the type of malignancy. The team also collected blood samples before CAR T-cell infusion and at multiple times after infusion.
Efficacy and safety
Six patients achieved a CR to treatment—3 with DLBCL (1 transformed), 2 with ALL, and 1 with CLL. Two patients had SD—1 with MCL and 1 with CLL. The remaining patients progressed.
All patients with a CR eventually relapsed. The median duration of CR was 5 months (range, 3-24 months).
Four patients—2 complete responders and 2 with SD—responded well to subsequent therapy and are still alive with 27 to 36 months of follow-up. This includes 1 patient with DLBCL, 1 with MCL, and 2 with CLL.
Four patients had serious adverse events. Three had cytokine-release syndrome, and 2 had neurological toxicity.
All cases of cytokine-release syndrome resolved after treatment with corticosteroids/anti-IL6R therapy. The neurological toxicity resolved spontaneously.
Immune status
An analysis of the blood samples taken throughout the study showed that high levels of monocytic myeloid-derived suppressor cells (MDSCs) prior to treatment was associated with decreased overall survival. In addition, increased levels of MDSCs after treatment preceded treatment failure.
Furthermore, high plasma levels of immunosuppressive factors—such as PD-L1 and PD-L2—after treatment were associated with decreased overall survival.
High plasma levels of biomarkers of an immunostimulatory environment—including IL-12, DC-LAMP, TRAIL, and FasL—before the administration of CAR T-cell therapy was associated with increased overall survival.
“[A]n immunostimulatory environment was associated with improved overall survival, while immunosuppressive cells and factors were associated with treatment failure and decreased overall survival,” Dr Lövgren said.
“We are hoping to follow up this study with another clinical trial that will combine CAR T-cell therapy with chemotherapy known to decrease the number of monocytic myeloid-derived suppressive cells. We are also looking to further optimize the CAR T-cell therapy.”
Dr Lövgren said the main limitations of this study are that it only included 15 patients, the patients had several different malignancies, and some patients may have been too sick to respond to any treatment.
This study was supported by funds from AFA Insurance AB, the Swedish Cancer Society, the Swedish Research Council, the Lions Fund at Uppsala University Hospital, and the Swedish State Support for Clinical Research. Dr Lövgren declared no conflicts of interest. ![]()
MAINZ/FRANKFURT, GERMANY—Outcomes of treatment with a third-generation chimeric antigen receptor (CAR) T-cell therapy are associated with a patient’s immune status, according to a phase 1/2a trial.
The CD19-specific CAR T-cell therapy produced a complete response (CR) in 6 of 15 patients with relapsed/refractory CD19-positive leukemia or lymphoma.
Though all responders eventually relapsed, 4 patients—including 2 with stable disease (SD) after treatment—responded to subsequent therapy and are still alive, 1 of them beyond 36 months.
An analysis of blood samples taken throughout the study revealed that a patient’s immune status was associated with treatment failure and overall survival.
Tanja Lövgren, PhD, of Uppsala University in Sweden, and her colleagues presented these findings at the Third CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference: Translating Science into Survival (abstract B156).
“CD19-specific CAR T-cell therapy has yielded remarkable response rates for patients who have B-cell acute lymphoblastic leukemia,” Dr Lövgren said. “However, many patients relapse.”
“In addition, response rates are more variable for patients who have other CD19-positive B-cell malignancies, and many patients experience serious adverse events. We set out to investigate the safety and effectiveness of a third-generation CD19-specific CAR T-cell therapy and to identify potential biomarkers of treatment outcome.”
Dr Lövgren and her colleagues studied 15 patients (ages 24-72) who had relapsed or refractory CD19-positive B-cell malignancies:
- Six patients with diffuse large B-cell lymphoma (DLBCL), including 3 cases that were transformed from follicular lymphoma (FL)
- Four patients with pre-B acute lymphoblastic leukemia (ALL)
- Two patients with mantle cell lymphoma (MCL)
- Two patients with chronic lymphocytic leukemia (CLL)
- One patient with FL transformed from Burkitt lymphoma.
Eleven patients received preconditioning with cyclophosphamide (500 mg/m2) and fludarabine (3 doses at 25 mg/m2).
All patients received CAR T cells at 1 x 108, 2 x 107, or 2 x 108 cells/m2. These were autologous, CD19-targeting CAR T cells with 3 intracellular signaling domains derived from CD3 zeta, CD28, and 4-1BB.
The researchers assessed tumor responses via bone marrow/blood analysis and/or radiology, depending on the type of malignancy. The team also collected blood samples before CAR T-cell infusion and at multiple times after infusion.
Efficacy and safety
Six patients achieved a CR to treatment—3 with DLBCL (1 transformed), 2 with ALL, and 1 with CLL. Two patients had SD—1 with MCL and 1 with CLL. The remaining patients progressed.
All patients with a CR eventually relapsed. The median duration of CR was 5 months (range, 3-24 months).
Four patients—2 complete responders and 2 with SD—responded well to subsequent therapy and are still alive with 27 to 36 months of follow-up. This includes 1 patient with DLBCL, 1 with MCL, and 2 with CLL.
Four patients had serious adverse events. Three had cytokine-release syndrome, and 2 had neurological toxicity.
All cases of cytokine-release syndrome resolved after treatment with corticosteroids/anti-IL6R therapy. The neurological toxicity resolved spontaneously.
Immune status
An analysis of the blood samples taken throughout the study showed that high levels of monocytic myeloid-derived suppressor cells (MDSCs) prior to treatment was associated with decreased overall survival. In addition, increased levels of MDSCs after treatment preceded treatment failure.
Furthermore, high plasma levels of immunosuppressive factors—such as PD-L1 and PD-L2—after treatment were associated with decreased overall survival.
High plasma levels of biomarkers of an immunostimulatory environment—including IL-12, DC-LAMP, TRAIL, and FasL—before the administration of CAR T-cell therapy was associated with increased overall survival.
“[A]n immunostimulatory environment was associated with improved overall survival, while immunosuppressive cells and factors were associated with treatment failure and decreased overall survival,” Dr Lövgren said.
“We are hoping to follow up this study with another clinical trial that will combine CAR T-cell therapy with chemotherapy known to decrease the number of monocytic myeloid-derived suppressive cells. We are also looking to further optimize the CAR T-cell therapy.”
Dr Lövgren said the main limitations of this study are that it only included 15 patients, the patients had several different malignancies, and some patients may have been too sick to respond to any treatment.
This study was supported by funds from AFA Insurance AB, the Swedish Cancer Society, the Swedish Research Council, the Lions Fund at Uppsala University Hospital, and the Swedish State Support for Clinical Research. Dr Lövgren declared no conflicts of interest. ![]()
Biosimilar matches rituximab in large follicular lymphoma trial
MADRID – The biosimilar GP2013 met the criteria for therapeutic equivalence to rituximab in a large comparator trial of previously untreated patients with aggressive follicular lymphoma.
Based on results presented at the European Society for Medical Oncology Congress, “there is absolutely no difference in the objective response rates for GP2013 and rituximab,” the primary endpoint of the trial, reported Wojciech Jurczak, MD, PhD, head of lymphoma, department of hematology, Jagiellonian University, Krakow, Poland.
Dr. Jurczak characterized the double-blind, randomized phase 3 trial ASSIST_FL (NCT01419665) as the “largest biosimilar trial in hematology.” For the study, 629 patients with previously untreated, advanced-stage follicular lymphoma were randomized to GP2013 and the conventional regimen of cyclophosphamide, vincristine, and prednisone (G-CVP) or rituximab and the same three-agent regimen (R-CVP). Each regimen was given for eight cycles followed by maintenance monotherapy with the assigned monoclonal antibody for up to 2 years.
The primary endpoint, objective response rate (ORR), was 87.1% and 87.5% for G-CVP and R-CVP, respectively. There were no differences in ORR among the subgroups evaluated, which included patients aged 60 years and older vs. younger patients, presence or absence of bulky disease, high or low FLIPI (Follicular Lymphoma International Prognostic Index) score, gender, and the geographic region where treatment was given.
Safety was a secondary endpoint evaluated at the end of eight cycles and again after a year of maintenance therapy. The proportion of patients with any adverse event and the proportion with grade 3 or greater adverse events were not statistically different at any time point. There were also no significant differences in any of the other secondary endpoints evaluated, which included pharmacokinetic, pharmacodynamic, and immune measures.
The results are consistent with those of a related randomized bioequivalence trial comparing GP2013 and rituximab in 312 patients with rheumatoid arthritis (Ann Rheum Dis. 2017;76:1598-1602). The primary endpoint in that trial was area-under-the-curve serum concentration time.
The two studies are mutually reinforcing, and “the ASSIST_FL trial ends the story. We have the totality of evidence that GP2013 can be considered a biosimilar,” said Dr. Jurczak, who anticipates “major price differences” for this agent relative to rituximab.
“We may, based on the results of the follicular lymphoma trial, use the biosimilar in all registered indications for rituximab,” said Dr. Jurczak. This is also the conclusion of the European Medicine Agency, which approved this agent in June 2017 for all rituximab indications.
In explaining the process for approval of biosimilars, Dr. Jurczak emphasized that demonstrating bioequivalence is not the same as the approval process for a new therapeutic agent, for which regulatory agents require a demonstration of efficacy on a meaningful clinical endpoint, such as progression-free survival. For biosimilars, it is not necessary to show clinical benefits. Biosimilars must demonstrate the same biological activity, and ORR is considered an acceptable measure.
The ESMO-invited discussant, Michele Ghielmini, MD, PhD, medical director at the Oncology Institute of Southern Switzerland, Bellinzona, agreed. “We can reasonably speculate that (when rituximab and the biosimilar are associated with the same) response rate, they will lead to the same clinical benefits.”
MADRID – The biosimilar GP2013 met the criteria for therapeutic equivalence to rituximab in a large comparator trial of previously untreated patients with aggressive follicular lymphoma.
Based on results presented at the European Society for Medical Oncology Congress, “there is absolutely no difference in the objective response rates for GP2013 and rituximab,” the primary endpoint of the trial, reported Wojciech Jurczak, MD, PhD, head of lymphoma, department of hematology, Jagiellonian University, Krakow, Poland.
Dr. Jurczak characterized the double-blind, randomized phase 3 trial ASSIST_FL (NCT01419665) as the “largest biosimilar trial in hematology.” For the study, 629 patients with previously untreated, advanced-stage follicular lymphoma were randomized to GP2013 and the conventional regimen of cyclophosphamide, vincristine, and prednisone (G-CVP) or rituximab and the same three-agent regimen (R-CVP). Each regimen was given for eight cycles followed by maintenance monotherapy with the assigned monoclonal antibody for up to 2 years.
The primary endpoint, objective response rate (ORR), was 87.1% and 87.5% for G-CVP and R-CVP, respectively. There were no differences in ORR among the subgroups evaluated, which included patients aged 60 years and older vs. younger patients, presence or absence of bulky disease, high or low FLIPI (Follicular Lymphoma International Prognostic Index) score, gender, and the geographic region where treatment was given.
Safety was a secondary endpoint evaluated at the end of eight cycles and again after a year of maintenance therapy. The proportion of patients with any adverse event and the proportion with grade 3 or greater adverse events were not statistically different at any time point. There were also no significant differences in any of the other secondary endpoints evaluated, which included pharmacokinetic, pharmacodynamic, and immune measures.
The results are consistent with those of a related randomized bioequivalence trial comparing GP2013 and rituximab in 312 patients with rheumatoid arthritis (Ann Rheum Dis. 2017;76:1598-1602). The primary endpoint in that trial was area-under-the-curve serum concentration time.
The two studies are mutually reinforcing, and “the ASSIST_FL trial ends the story. We have the totality of evidence that GP2013 can be considered a biosimilar,” said Dr. Jurczak, who anticipates “major price differences” for this agent relative to rituximab.
“We may, based on the results of the follicular lymphoma trial, use the biosimilar in all registered indications for rituximab,” said Dr. Jurczak. This is also the conclusion of the European Medicine Agency, which approved this agent in June 2017 for all rituximab indications.
In explaining the process for approval of biosimilars, Dr. Jurczak emphasized that demonstrating bioequivalence is not the same as the approval process for a new therapeutic agent, for which regulatory agents require a demonstration of efficacy on a meaningful clinical endpoint, such as progression-free survival. For biosimilars, it is not necessary to show clinical benefits. Biosimilars must demonstrate the same biological activity, and ORR is considered an acceptable measure.
The ESMO-invited discussant, Michele Ghielmini, MD, PhD, medical director at the Oncology Institute of Southern Switzerland, Bellinzona, agreed. “We can reasonably speculate that (when rituximab and the biosimilar are associated with the same) response rate, they will lead to the same clinical benefits.”
MADRID – The biosimilar GP2013 met the criteria for therapeutic equivalence to rituximab in a large comparator trial of previously untreated patients with aggressive follicular lymphoma.
Based on results presented at the European Society for Medical Oncology Congress, “there is absolutely no difference in the objective response rates for GP2013 and rituximab,” the primary endpoint of the trial, reported Wojciech Jurczak, MD, PhD, head of lymphoma, department of hematology, Jagiellonian University, Krakow, Poland.
Dr. Jurczak characterized the double-blind, randomized phase 3 trial ASSIST_FL (NCT01419665) as the “largest biosimilar trial in hematology.” For the study, 629 patients with previously untreated, advanced-stage follicular lymphoma were randomized to GP2013 and the conventional regimen of cyclophosphamide, vincristine, and prednisone (G-CVP) or rituximab and the same three-agent regimen (R-CVP). Each regimen was given for eight cycles followed by maintenance monotherapy with the assigned monoclonal antibody for up to 2 years.
The primary endpoint, objective response rate (ORR), was 87.1% and 87.5% for G-CVP and R-CVP, respectively. There were no differences in ORR among the subgroups evaluated, which included patients aged 60 years and older vs. younger patients, presence or absence of bulky disease, high or low FLIPI (Follicular Lymphoma International Prognostic Index) score, gender, and the geographic region where treatment was given.
Safety was a secondary endpoint evaluated at the end of eight cycles and again after a year of maintenance therapy. The proportion of patients with any adverse event and the proportion with grade 3 or greater adverse events were not statistically different at any time point. There were also no significant differences in any of the other secondary endpoints evaluated, which included pharmacokinetic, pharmacodynamic, and immune measures.
The results are consistent with those of a related randomized bioequivalence trial comparing GP2013 and rituximab in 312 patients with rheumatoid arthritis (Ann Rheum Dis. 2017;76:1598-1602). The primary endpoint in that trial was area-under-the-curve serum concentration time.
The two studies are mutually reinforcing, and “the ASSIST_FL trial ends the story. We have the totality of evidence that GP2013 can be considered a biosimilar,” said Dr. Jurczak, who anticipates “major price differences” for this agent relative to rituximab.
“We may, based on the results of the follicular lymphoma trial, use the biosimilar in all registered indications for rituximab,” said Dr. Jurczak. This is also the conclusion of the European Medicine Agency, which approved this agent in June 2017 for all rituximab indications.
In explaining the process for approval of biosimilars, Dr. Jurczak emphasized that demonstrating bioequivalence is not the same as the approval process for a new therapeutic agent, for which regulatory agents require a demonstration of efficacy on a meaningful clinical endpoint, such as progression-free survival. For biosimilars, it is not necessary to show clinical benefits. Biosimilars must demonstrate the same biological activity, and ORR is considered an acceptable measure.
The ESMO-invited discussant, Michele Ghielmini, MD, PhD, medical director at the Oncology Institute of Southern Switzerland, Bellinzona, agreed. “We can reasonably speculate that (when rituximab and the biosimilar are associated with the same) response rate, they will lead to the same clinical benefits.”
AT ESMO 2017
Key clinical point:
Major finding: The objective response rates were 87.1% and 87.5% for G-CVP and R-CVP.
Data source: Double-blind, multicenter randomized trial of 629 patients with previously untreated, advanced-stage follicular lymphoma.
Disclosures: Dr. Jurczak reported financial relationships with Sandoz.