User login
Adding rituximab to reduced intensity conditioning boosts PFS
ORLANDO – Rituximab conferred a significant progression-free survival benefit in reduced intensity conditioning regimens for patients with B-cell non-Hodgkin lymphoma who underwent allogeneic hematopoietic cell transplantation, based on data from the Center for International Blood & Marrow Transplant Research.
Further, higher cumulative rituximab doses appeared to confer a benefit in overall survival.
Rituximab is frequently a component of reduced intensity conditioning (RIC) regimens in allogeneic hematopoietic cell transplantation (HCT), but there has been a “paucity of comparative data” for rituximab-containing (R-RIC) versus non–R-RIC conditioning regimens for allogeneic transplant patients, Narendranath Epperla, MD, of the Medical College of Wisconsin, Milwaukee, said during the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
Using data from the Center for International Blood & Marrow Transplant Research, Dr. Epperla and his colleagues identified 1,022 patients who received rituximab and 379 patients who did not with diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, and marginal zone lymphoma. The patients received their first RIC or non-myeloablative allogeneic HCT between 2008 and 2014. The donors were matched, and either related or 8x8 allele-matched unrelated; the graft source could be bone marrow or peripheral blood. Graft versus host disease (GVHD) suppression was calcineurin inhibitor based.
Patients who had received myeloablative conditioning, or who had received radioimmunotherapy or alemtuzumab were excluded, as were those who received alternative donor allografts.
Dr. Epperla and his colleagues factored in patient and disease characteristics, as well as differences in transplant regimen, in determining the adjusted cumulative incidence of relapse or progression, as well as the incidence of nonrelapse mortality.
In the multivariable analysis, overall survival did not differ between the R-RIC and the non–R-RIC cohorts (relative risk [RR] of all-cause mortality, R-RIC = 0.83, 95% CI 0.67-1.03, P = .09).
Based on the cumulative dose of rituximab that patients had received, though, “we noted that patients who got higher doses of rituximab had lower risk of nonrelapse mortality,” Dr. Epperla said. “Higher cumulative doses of rituximab seem to confer overall survival benefit.” This was true even though the higher rituximab doses had no significant effect on the risk of therapy failure, nonrelapse mortality, or the risk of progression/relapse.
When the cumulative rituximab dose was 2,000 to 3,375 mg/m2, the hazard ratio for all-cause mortality fell to 0.43 compared to a cumulative rituximab dose of less than 1,000 mg/m2 (95% confidence interval [CI] 0.21-0.90, P = .02).
Among the R-RIC group, there was a nonsignificant trend toward reduced risk of progression or relapse (relative risk of progression/relapse, R-RIC = 0.79, 95% CI 0.63-1.01, P = .055). However, the R-RIC group fared significantly better in terms of progression-free survival (RR of PFS, R-RIC = 0.76, 95% CI 0.62-0.92, P = .006).
After transplant, patients in the R-RIC group were no more likely than those in the non–R-RIC group to experience chronic GVHD (RR of GVHD, R-RIC = 1.15, 95% CI 0.96-1.39, P = .13). There was no difference in the adjusted curves of nonrelapse mortality between the groups (RR of nonrelapse mortality, R-RIC = 0.90, 95% CI 0.67-1.22, P = .51).
Also, there were no fatal cytopenias in the R-RIC arm, although the literature warrants some concern for increased risk of infection with rituximab, Dr. Epperla said.
At baseline, there were no significant differences in demographic characteristics between the nonrituximab and rituximab arms of the study population. More than 90% of patients were white, and 65% were male; the median age was 57 years (range, 18-74).
Patients had been diagnosed about 3 years before receiving HCT; about 60% of patients had a baseline Karnofsky performance score greater than 90, and the HCT comorbidity index was 2. About 86% of patients were chemosensitive, and patients in both study arms had received a median of three prior lines of therapy.
There were some differences in conditioning regimens between the two groups. “There were a significantly higher number of patients in the nonrituximab group who received fludarabine/busulfan, while there were a significantly high number in the rituximab group who received a fludarabine/cyclophosphamide-based conditioning regimen,” Dr. Epperla said. Follicular lymphomas were more common in the R-RIC arm, while diffuse large B-cell lymphomas were seen more in the non–R-RIC arm.
Given the survival benefit and similar rates of chronic GVHD seen in the retrospective analysis, a prospective, randomized head-to-head trial of R-RIC versus non–R-RIC is warranted, Dr. Epperla concluded.
During the postpresentation discussion, Dr. Epperla acknowledged the variability of the lymphomas in the study, but that there was no significant statistical effect of specific histologies on the findings in a subgroup analysis. Dr. Epperla added that the chemosensitivity status at transplant was checked to account for patient exposure to rituximab before RIC, and that there was no effect of prior rituximab exposure on the outcomes examined.
Dr. Epperla reported no conflicts of interest.
[email protected]
On Twitter @karioakes
ORLANDO – Rituximab conferred a significant progression-free survival benefit in reduced intensity conditioning regimens for patients with B-cell non-Hodgkin lymphoma who underwent allogeneic hematopoietic cell transplantation, based on data from the Center for International Blood & Marrow Transplant Research.
Further, higher cumulative rituximab doses appeared to confer a benefit in overall survival.
Rituximab is frequently a component of reduced intensity conditioning (RIC) regimens in allogeneic hematopoietic cell transplantation (HCT), but there has been a “paucity of comparative data” for rituximab-containing (R-RIC) versus non–R-RIC conditioning regimens for allogeneic transplant patients, Narendranath Epperla, MD, of the Medical College of Wisconsin, Milwaukee, said during the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
Using data from the Center for International Blood & Marrow Transplant Research, Dr. Epperla and his colleagues identified 1,022 patients who received rituximab and 379 patients who did not with diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, and marginal zone lymphoma. The patients received their first RIC or non-myeloablative allogeneic HCT between 2008 and 2014. The donors were matched, and either related or 8x8 allele-matched unrelated; the graft source could be bone marrow or peripheral blood. Graft versus host disease (GVHD) suppression was calcineurin inhibitor based.
Patients who had received myeloablative conditioning, or who had received radioimmunotherapy or alemtuzumab were excluded, as were those who received alternative donor allografts.
Dr. Epperla and his colleagues factored in patient and disease characteristics, as well as differences in transplant regimen, in determining the adjusted cumulative incidence of relapse or progression, as well as the incidence of nonrelapse mortality.
In the multivariable analysis, overall survival did not differ between the R-RIC and the non–R-RIC cohorts (relative risk [RR] of all-cause mortality, R-RIC = 0.83, 95% CI 0.67-1.03, P = .09).
Based on the cumulative dose of rituximab that patients had received, though, “we noted that patients who got higher doses of rituximab had lower risk of nonrelapse mortality,” Dr. Epperla said. “Higher cumulative doses of rituximab seem to confer overall survival benefit.” This was true even though the higher rituximab doses had no significant effect on the risk of therapy failure, nonrelapse mortality, or the risk of progression/relapse.
When the cumulative rituximab dose was 2,000 to 3,375 mg/m2, the hazard ratio for all-cause mortality fell to 0.43 compared to a cumulative rituximab dose of less than 1,000 mg/m2 (95% confidence interval [CI] 0.21-0.90, P = .02).
Among the R-RIC group, there was a nonsignificant trend toward reduced risk of progression or relapse (relative risk of progression/relapse, R-RIC = 0.79, 95% CI 0.63-1.01, P = .055). However, the R-RIC group fared significantly better in terms of progression-free survival (RR of PFS, R-RIC = 0.76, 95% CI 0.62-0.92, P = .006).
After transplant, patients in the R-RIC group were no more likely than those in the non–R-RIC group to experience chronic GVHD (RR of GVHD, R-RIC = 1.15, 95% CI 0.96-1.39, P = .13). There was no difference in the adjusted curves of nonrelapse mortality between the groups (RR of nonrelapse mortality, R-RIC = 0.90, 95% CI 0.67-1.22, P = .51).
Also, there were no fatal cytopenias in the R-RIC arm, although the literature warrants some concern for increased risk of infection with rituximab, Dr. Epperla said.
At baseline, there were no significant differences in demographic characteristics between the nonrituximab and rituximab arms of the study population. More than 90% of patients were white, and 65% were male; the median age was 57 years (range, 18-74).
Patients had been diagnosed about 3 years before receiving HCT; about 60% of patients had a baseline Karnofsky performance score greater than 90, and the HCT comorbidity index was 2. About 86% of patients were chemosensitive, and patients in both study arms had received a median of three prior lines of therapy.
There were some differences in conditioning regimens between the two groups. “There were a significantly higher number of patients in the nonrituximab group who received fludarabine/busulfan, while there were a significantly high number in the rituximab group who received a fludarabine/cyclophosphamide-based conditioning regimen,” Dr. Epperla said. Follicular lymphomas were more common in the R-RIC arm, while diffuse large B-cell lymphomas were seen more in the non–R-RIC arm.
Given the survival benefit and similar rates of chronic GVHD seen in the retrospective analysis, a prospective, randomized head-to-head trial of R-RIC versus non–R-RIC is warranted, Dr. Epperla concluded.
During the postpresentation discussion, Dr. Epperla acknowledged the variability of the lymphomas in the study, but that there was no significant statistical effect of specific histologies on the findings in a subgroup analysis. Dr. Epperla added that the chemosensitivity status at transplant was checked to account for patient exposure to rituximab before RIC, and that there was no effect of prior rituximab exposure on the outcomes examined.
Dr. Epperla reported no conflicts of interest.
[email protected]
On Twitter @karioakes
ORLANDO – Rituximab conferred a significant progression-free survival benefit in reduced intensity conditioning regimens for patients with B-cell non-Hodgkin lymphoma who underwent allogeneic hematopoietic cell transplantation, based on data from the Center for International Blood & Marrow Transplant Research.
Further, higher cumulative rituximab doses appeared to confer a benefit in overall survival.
Rituximab is frequently a component of reduced intensity conditioning (RIC) regimens in allogeneic hematopoietic cell transplantation (HCT), but there has been a “paucity of comparative data” for rituximab-containing (R-RIC) versus non–R-RIC conditioning regimens for allogeneic transplant patients, Narendranath Epperla, MD, of the Medical College of Wisconsin, Milwaukee, said during the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
Using data from the Center for International Blood & Marrow Transplant Research, Dr. Epperla and his colleagues identified 1,022 patients who received rituximab and 379 patients who did not with diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, and marginal zone lymphoma. The patients received their first RIC or non-myeloablative allogeneic HCT between 2008 and 2014. The donors were matched, and either related or 8x8 allele-matched unrelated; the graft source could be bone marrow or peripheral blood. Graft versus host disease (GVHD) suppression was calcineurin inhibitor based.
Patients who had received myeloablative conditioning, or who had received radioimmunotherapy or alemtuzumab were excluded, as were those who received alternative donor allografts.
Dr. Epperla and his colleagues factored in patient and disease characteristics, as well as differences in transplant regimen, in determining the adjusted cumulative incidence of relapse or progression, as well as the incidence of nonrelapse mortality.
In the multivariable analysis, overall survival did not differ between the R-RIC and the non–R-RIC cohorts (relative risk [RR] of all-cause mortality, R-RIC = 0.83, 95% CI 0.67-1.03, P = .09).
Based on the cumulative dose of rituximab that patients had received, though, “we noted that patients who got higher doses of rituximab had lower risk of nonrelapse mortality,” Dr. Epperla said. “Higher cumulative doses of rituximab seem to confer overall survival benefit.” This was true even though the higher rituximab doses had no significant effect on the risk of therapy failure, nonrelapse mortality, or the risk of progression/relapse.
When the cumulative rituximab dose was 2,000 to 3,375 mg/m2, the hazard ratio for all-cause mortality fell to 0.43 compared to a cumulative rituximab dose of less than 1,000 mg/m2 (95% confidence interval [CI] 0.21-0.90, P = .02).
Among the R-RIC group, there was a nonsignificant trend toward reduced risk of progression or relapse (relative risk of progression/relapse, R-RIC = 0.79, 95% CI 0.63-1.01, P = .055). However, the R-RIC group fared significantly better in terms of progression-free survival (RR of PFS, R-RIC = 0.76, 95% CI 0.62-0.92, P = .006).
After transplant, patients in the R-RIC group were no more likely than those in the non–R-RIC group to experience chronic GVHD (RR of GVHD, R-RIC = 1.15, 95% CI 0.96-1.39, P = .13). There was no difference in the adjusted curves of nonrelapse mortality between the groups (RR of nonrelapse mortality, R-RIC = 0.90, 95% CI 0.67-1.22, P = .51).
Also, there were no fatal cytopenias in the R-RIC arm, although the literature warrants some concern for increased risk of infection with rituximab, Dr. Epperla said.
At baseline, there were no significant differences in demographic characteristics between the nonrituximab and rituximab arms of the study population. More than 90% of patients were white, and 65% were male; the median age was 57 years (range, 18-74).
Patients had been diagnosed about 3 years before receiving HCT; about 60% of patients had a baseline Karnofsky performance score greater than 90, and the HCT comorbidity index was 2. About 86% of patients were chemosensitive, and patients in both study arms had received a median of three prior lines of therapy.
There were some differences in conditioning regimens between the two groups. “There were a significantly higher number of patients in the nonrituximab group who received fludarabine/busulfan, while there were a significantly high number in the rituximab group who received a fludarabine/cyclophosphamide-based conditioning regimen,” Dr. Epperla said. Follicular lymphomas were more common in the R-RIC arm, while diffuse large B-cell lymphomas were seen more in the non–R-RIC arm.
Given the survival benefit and similar rates of chronic GVHD seen in the retrospective analysis, a prospective, randomized head-to-head trial of R-RIC versus non–R-RIC is warranted, Dr. Epperla concluded.
During the postpresentation discussion, Dr. Epperla acknowledged the variability of the lymphomas in the study, but that there was no significant statistical effect of specific histologies on the findings in a subgroup analysis. Dr. Epperla added that the chemosensitivity status at transplant was checked to account for patient exposure to rituximab before RIC, and that there was no effect of prior rituximab exposure on the outcomes examined.
Dr. Epperla reported no conflicts of interest.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: Patients with rituximab-containing RIC regimens had better progression-free survival (PFS; relative risk of PFS, non–R-RIC=1, R-RIC=076, 95% CI 0.62-092, P = .006).
Data source: Retrospective review of 1,022 allogeneic HCT B-cell non-Hodgkin lymphoma patients who received rituximab and 379 who did not.
Disclosures: The data were obtained from the Center for International Blood & Marrow Transplant Research. Dr. Epperla reported no disclosures.
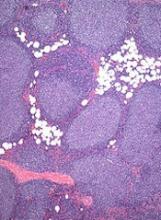
Potential therapeutic strategy for BL, DLBCL
Preclinical research has revealed a potential strategy for treating Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL).
Investigators discovered that miR-28 inhibits the growth of B-cell lymphomas, but this microRNA is often lost in these lymphomas.
Re-expressing miR-28 in mouse models of BL and DLBCL inhibited tumor growth, which supports the potential of synthetic miR-28 analogs for the treatment of these lymphomas.
In fact, the investigators believe their work could lead to the development of the first miRNA analog therapy for the treatment of B-cell lymphoma and provide the basis for clinical trials.
Almudena Ramiro, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues described the work in Blood.
The team characterized the function of miR-28 in the biology of mature B lymphocytes and in the development of lymphomas associated with this cell type.
The investigators found that miR-28 regulates the terminal differentiation of B lymphocytes, a fundamental process in the biology of these cells that generates memory B lymphocytes and highly specific plasma cells.
But the team found that miR-28 expression is lost in several germinal center-derived lymphoma subtypes, including BL, DLBCL, follicular lymphoma, and chronic lymphocytic leukemia.
In vitro experiments showed that miR-28 expression dampens B-cell receptor signaling and diminishes the proliferation and survival of primary B cells and lymphoma cells.
And in vivo experiments showed that re-establishing miR-28 expression slows tumor growth in DLBCL and BL.
The investigators re-expressed miR-28 in xenograft models of BL and DLBCL via the use of viral vectors or synthetic molecules and found that both methods blocked tumor growth. The same effect was observed in mice with established BL tumors.
Dr Ramiro and her colleagues said these results reveal the therapeutic potential of miR-28 and provide ample justification for the initiation of clinical trials of miR-28-based therapies to treat B-cell lymphomas. ![]()
Preclinical research has revealed a potential strategy for treating Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL).
Investigators discovered that miR-28 inhibits the growth of B-cell lymphomas, but this microRNA is often lost in these lymphomas.
Re-expressing miR-28 in mouse models of BL and DLBCL inhibited tumor growth, which supports the potential of synthetic miR-28 analogs for the treatment of these lymphomas.
In fact, the investigators believe their work could lead to the development of the first miRNA analog therapy for the treatment of B-cell lymphoma and provide the basis for clinical trials.
Almudena Ramiro, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues described the work in Blood.
The team characterized the function of miR-28 in the biology of mature B lymphocytes and in the development of lymphomas associated with this cell type.
The investigators found that miR-28 regulates the terminal differentiation of B lymphocytes, a fundamental process in the biology of these cells that generates memory B lymphocytes and highly specific plasma cells.
But the team found that miR-28 expression is lost in several germinal center-derived lymphoma subtypes, including BL, DLBCL, follicular lymphoma, and chronic lymphocytic leukemia.
In vitro experiments showed that miR-28 expression dampens B-cell receptor signaling and diminishes the proliferation and survival of primary B cells and lymphoma cells.
And in vivo experiments showed that re-establishing miR-28 expression slows tumor growth in DLBCL and BL.
The investigators re-expressed miR-28 in xenograft models of BL and DLBCL via the use of viral vectors or synthetic molecules and found that both methods blocked tumor growth. The same effect was observed in mice with established BL tumors.
Dr Ramiro and her colleagues said these results reveal the therapeutic potential of miR-28 and provide ample justification for the initiation of clinical trials of miR-28-based therapies to treat B-cell lymphomas. ![]()
Preclinical research has revealed a potential strategy for treating Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL).
Investigators discovered that miR-28 inhibits the growth of B-cell lymphomas, but this microRNA is often lost in these lymphomas.
Re-expressing miR-28 in mouse models of BL and DLBCL inhibited tumor growth, which supports the potential of synthetic miR-28 analogs for the treatment of these lymphomas.
In fact, the investigators believe their work could lead to the development of the first miRNA analog therapy for the treatment of B-cell lymphoma and provide the basis for clinical trials.
Almudena Ramiro, PhD, of Centro Nacional de Investigaciones Cardiovasculares in Madrid, Spain, and her colleagues described the work in Blood.
The team characterized the function of miR-28 in the biology of mature B lymphocytes and in the development of lymphomas associated with this cell type.
The investigators found that miR-28 regulates the terminal differentiation of B lymphocytes, a fundamental process in the biology of these cells that generates memory B lymphocytes and highly specific plasma cells.
But the team found that miR-28 expression is lost in several germinal center-derived lymphoma subtypes, including BL, DLBCL, follicular lymphoma, and chronic lymphocytic leukemia.
In vitro experiments showed that miR-28 expression dampens B-cell receptor signaling and diminishes the proliferation and survival of primary B cells and lymphoma cells.
And in vivo experiments showed that re-establishing miR-28 expression slows tumor growth in DLBCL and BL.
The investigators re-expressed miR-28 in xenograft models of BL and DLBCL via the use of viral vectors or synthetic molecules and found that both methods blocked tumor growth. The same effect was observed in mice with established BL tumors.
Dr Ramiro and her colleagues said these results reveal the therapeutic potential of miR-28 and provide ample justification for the initiation of clinical trials of miR-28-based therapies to treat B-cell lymphomas. ![]()
Drug granted orphan status for follicular lymphoma
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
The US Food and Drug Administration (FDA) has granted orphan designation to G100 for the treatment of follicular lymphoma.
G100 is a synthetic small-molecule toll-like receptor-4 agonist, glucopyranosyl lipid A, formulated in a stable emulsion.
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent rare diseases/disorders affecting fewer than 200,000 people in the US.
Orphan designation provides companies with certain incentives to develop products for rare diseases. This includes a 50% tax break on research and development, a fee waiver, access to federal grants, and 7 years of market exclusivity if the product is approved.
G100 is being developed by Immune Design. The company says G100 works by leveraging the activation of innate and adaptive immunity in the tumor microenvironment to create an immune response against the tumor’s pre-existing antigens.
According to Immune Design, clinical and preclinical data have demonstrated G100’s ability to activate tumor-infiltrating lymphocytes, macrophages, and dendritic cells, and promote antigen-presentation and the recruitment of T cells to the tumor.
The ensuing induction of local and systemic immune responses has been shown to result in local and abscopal tumor control in preclinical studies.
In fact, G100, when combined with local radiation, demonstrated efficacy against A20 lymphoma in mice. This research was presented in a poster at the 2016 ASH Annual Meeting (abstract 4166).
In this study, investigators evaluated the immune response and therapeutic effects of intratumoral G100 alone, local radiation alone, and concomitant G100 and local radiation in mice with A20 lymphoma.
The investigators said the combination therapy demonstrated:
- Synergistic antitumor effects in both injected as well as uninjected tumors (abscopal effects)
- Synergistic induction of pro-inflammatory cytokine and chemokine environment, as well as induction of genes governing antigen processing and presentation
- Increased infiltration of T cells, including CD4 and CD8 T cells, in treated tumors.
In contrast, tumors that received only radiation had significantly lower T-cell levels than untreated tumors.
“These findings highlight the potential beneficial effect that immunotherapy with G100 could provide when given with radiation by modulating the tumor microenvironment to generate a systemic, durable, T-cell anti-tumor response,” said study investigator Ramesh Rengan, MD, of the University of Washington in Seattle.
“As shown in this model, G100 may hold potential as a treatment for lymphoma patients.”
To test that theory, Immune Design is conducting a phase 1/2 trial of G100 given with local radiation or the anti-PD-1 agent pembrolizumab to patients with follicular lymphoma. ![]()
Factors linked to B-NHL in Palestinians, Israelis
New research has revealed factors that may increase the risk of B-cell non-Hodgkin lymphoma (B-NHL) in Israelis and Palestinians.
This large-scale, epidemiological study indicated that each group had its own unique risk factors.
However, in both groups, recreational sun exposure, black hair-dye use, a history of hospitalization for infection, and having a first-degree relative with a hematopoietic malignancy were all associated with B-NHL.
A team of Palestinian and Israeli researchers reported these findings in PLOS ONE.
The researchers noted that Israelis and Palestinians share the same ecosystem but differ in terms of lifestyle, health behaviors, and medical systems. Yet both populations report high incidences of NHL.
To gain some insight into this phenomenon, the team conducted a study examining risk factors for B-NHL and its subtypes in these two populations.
The researchers looked at medical history, environmental factors, and lifestyle factors in 823 B-NHL patients and 808 healthy controls.
There were 516 Israeli Jews with B-NHL and 307 Palestinian Arabs with B-NHL. The mean age at diagnosis was 60 and 51, respectively.
The proportion of patients with diffuse large B-cell lymphoma was 71% of Palestinian Arabs and 41% of Israeli Jews. The proportion of patients with follicular lymphoma was 14% and 28%, respectively. And the proportion of patients with marginal zone lymphoma was 2% and 14%, respectively.
Using data from questionnaires, pathology review, serology, and genotyping, the researchers uncovered potential risk factors for B-NHL common to both populations and other factors unique to each population.
Results
The data showed that, in both Palestinian Arabs and Israeli Jews, B-NHL was associated with:
- Recreational sun exposure (odds ratio [OR]=1.4)
- Black hair-dye use (OR=1.70)
- A history of hospitalization for infection (OR=1.68)
- Having a first-degree relative with a hematopoietic malignancy (OR=1.69).
Smoking was associated with follicular lymphoma in both populations (OR=1.46). And greater-than-monthly indoor pesticide use was associated with diffuse large B-cell lymphoma in both populations (OR=2.01).
There was an inverse association between alcohol use and B-NHL for both populations (OR=0.46).
Among Palestinian Arabs only, risk factors for B-NHL included gardening (OR=1.93) and a history of herpes (OR=3.73), mononucleosis (OR=6.34), rubella (OR=2.86), and blood transfusion (OR=2.53).
Risk factors that applied to Israeli Jews only included growing fruits and vegetables (OR=1.87) and self-reported autoimmune diseases (OR=1.99).
The researchers said differences in risk factors by ethnicity could reflect differences in lifestyle, medical systems, and reporting patterns, while variations by B-NHL subtypes suggest specific causal factors for different types of disease. However, these findings require further investigation to reveal their mechanisms.
“Apart from the scientific contribution that this research provides in terms of understanding risk factors for NHL, the study entails an important research cooperation among many institutions,” said study author Ora Paltiel, of Hadassah-Hebrew University Medical Organization in Jerusalem, Israel.
“The study provided opportunities for training Palestinian and Israeli researchers and will provide for intellectual interaction for years to come. The data collected will also provide a research platform for the future study of lymphoma. Epidemiologic research has the potential to improve and preserve human health, and it can also serve as a bridge to dialogue among nations.” ![]()
New research has revealed factors that may increase the risk of B-cell non-Hodgkin lymphoma (B-NHL) in Israelis and Palestinians.
This large-scale, epidemiological study indicated that each group had its own unique risk factors.
However, in both groups, recreational sun exposure, black hair-dye use, a history of hospitalization for infection, and having a first-degree relative with a hematopoietic malignancy were all associated with B-NHL.
A team of Palestinian and Israeli researchers reported these findings in PLOS ONE.
The researchers noted that Israelis and Palestinians share the same ecosystem but differ in terms of lifestyle, health behaviors, and medical systems. Yet both populations report high incidences of NHL.
To gain some insight into this phenomenon, the team conducted a study examining risk factors for B-NHL and its subtypes in these two populations.
The researchers looked at medical history, environmental factors, and lifestyle factors in 823 B-NHL patients and 808 healthy controls.
There were 516 Israeli Jews with B-NHL and 307 Palestinian Arabs with B-NHL. The mean age at diagnosis was 60 and 51, respectively.
The proportion of patients with diffuse large B-cell lymphoma was 71% of Palestinian Arabs and 41% of Israeli Jews. The proportion of patients with follicular lymphoma was 14% and 28%, respectively. And the proportion of patients with marginal zone lymphoma was 2% and 14%, respectively.
Using data from questionnaires, pathology review, serology, and genotyping, the researchers uncovered potential risk factors for B-NHL common to both populations and other factors unique to each population.
Results
The data showed that, in both Palestinian Arabs and Israeli Jews, B-NHL was associated with:
- Recreational sun exposure (odds ratio [OR]=1.4)
- Black hair-dye use (OR=1.70)
- A history of hospitalization for infection (OR=1.68)
- Having a first-degree relative with a hematopoietic malignancy (OR=1.69).
Smoking was associated with follicular lymphoma in both populations (OR=1.46). And greater-than-monthly indoor pesticide use was associated with diffuse large B-cell lymphoma in both populations (OR=2.01).
There was an inverse association between alcohol use and B-NHL for both populations (OR=0.46).
Among Palestinian Arabs only, risk factors for B-NHL included gardening (OR=1.93) and a history of herpes (OR=3.73), mononucleosis (OR=6.34), rubella (OR=2.86), and blood transfusion (OR=2.53).
Risk factors that applied to Israeli Jews only included growing fruits and vegetables (OR=1.87) and self-reported autoimmune diseases (OR=1.99).
The researchers said differences in risk factors by ethnicity could reflect differences in lifestyle, medical systems, and reporting patterns, while variations by B-NHL subtypes suggest specific causal factors for different types of disease. However, these findings require further investigation to reveal their mechanisms.
“Apart from the scientific contribution that this research provides in terms of understanding risk factors for NHL, the study entails an important research cooperation among many institutions,” said study author Ora Paltiel, of Hadassah-Hebrew University Medical Organization in Jerusalem, Israel.
“The study provided opportunities for training Palestinian and Israeli researchers and will provide for intellectual interaction for years to come. The data collected will also provide a research platform for the future study of lymphoma. Epidemiologic research has the potential to improve and preserve human health, and it can also serve as a bridge to dialogue among nations.” ![]()
New research has revealed factors that may increase the risk of B-cell non-Hodgkin lymphoma (B-NHL) in Israelis and Palestinians.
This large-scale, epidemiological study indicated that each group had its own unique risk factors.
However, in both groups, recreational sun exposure, black hair-dye use, a history of hospitalization for infection, and having a first-degree relative with a hematopoietic malignancy were all associated with B-NHL.
A team of Palestinian and Israeli researchers reported these findings in PLOS ONE.
The researchers noted that Israelis and Palestinians share the same ecosystem but differ in terms of lifestyle, health behaviors, and medical systems. Yet both populations report high incidences of NHL.
To gain some insight into this phenomenon, the team conducted a study examining risk factors for B-NHL and its subtypes in these two populations.
The researchers looked at medical history, environmental factors, and lifestyle factors in 823 B-NHL patients and 808 healthy controls.
There were 516 Israeli Jews with B-NHL and 307 Palestinian Arabs with B-NHL. The mean age at diagnosis was 60 and 51, respectively.
The proportion of patients with diffuse large B-cell lymphoma was 71% of Palestinian Arabs and 41% of Israeli Jews. The proportion of patients with follicular lymphoma was 14% and 28%, respectively. And the proportion of patients with marginal zone lymphoma was 2% and 14%, respectively.
Using data from questionnaires, pathology review, serology, and genotyping, the researchers uncovered potential risk factors for B-NHL common to both populations and other factors unique to each population.
Results
The data showed that, in both Palestinian Arabs and Israeli Jews, B-NHL was associated with:
- Recreational sun exposure (odds ratio [OR]=1.4)
- Black hair-dye use (OR=1.70)
- A history of hospitalization for infection (OR=1.68)
- Having a first-degree relative with a hematopoietic malignancy (OR=1.69).
Smoking was associated with follicular lymphoma in both populations (OR=1.46). And greater-than-monthly indoor pesticide use was associated with diffuse large B-cell lymphoma in both populations (OR=2.01).
There was an inverse association between alcohol use and B-NHL for both populations (OR=0.46).
Among Palestinian Arabs only, risk factors for B-NHL included gardening (OR=1.93) and a history of herpes (OR=3.73), mononucleosis (OR=6.34), rubella (OR=2.86), and blood transfusion (OR=2.53).
Risk factors that applied to Israeli Jews only included growing fruits and vegetables (OR=1.87) and self-reported autoimmune diseases (OR=1.99).
The researchers said differences in risk factors by ethnicity could reflect differences in lifestyle, medical systems, and reporting patterns, while variations by B-NHL subtypes suggest specific causal factors for different types of disease. However, these findings require further investigation to reveal their mechanisms.
“Apart from the scientific contribution that this research provides in terms of understanding risk factors for NHL, the study entails an important research cooperation among many institutions,” said study author Ora Paltiel, of Hadassah-Hebrew University Medical Organization in Jerusalem, Israel.
“The study provided opportunities for training Palestinian and Israeli researchers and will provide for intellectual interaction for years to come. The data collected will also provide a research platform for the future study of lymphoma. Epidemiologic research has the potential to improve and preserve human health, and it can also serve as a bridge to dialogue among nations.” ![]()
European Commission approves rituximab biosimilar
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
The European Commission has approved a biosimilar rituximab product, Truxima™, for all the same indications as the reference product, MabThera.
This means Truxima (formerly called CT-P10) is approved for use in the European Union to treat patients with non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis (RA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).
Truxima, a product of Celltrion Healthcare Hungary Kft, is the first biosimilar monoclonal antibody approved in an oncology indication worldwide.
The approval is based on data submitted to the European Medicines Agency.
The agency’s Committee for Medicinal Products for Human Use (CHMP) said the evidence suggests Truxima and MabThera are similar in terms of efficacy, safety, immunogenicity, pharmacodynamics, and pharmacokinetics in patients with RA and advanced follicular lymphoma (FL).
Therefore, the European Commission approved Truxima for the following indications.
Non-Hodgkin lymphoma
Truxima is indicated for use in combination with chemotherapy to treat previously untreated patients with stage III-IV FL.
Truxima maintenance therapy is indicated for the treatment of FL patients responding to induction therapy.
Truxima monotherapy is indicated for the treatment of patients with stage III-IV FL who are chemo-resistant or are in their second or subsequent relapse after chemotherapy.
Truxima is indicated for use in combination with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) for the treatment of patients with CD20-positive diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia
Truxima in combination with chemotherapy is indicated for the treatment of patients with previously untreated and relapsed/refractory chronic lymphocytic leukemia.
The CHMP noted that limited efficacy and safety data are available for patients previously treated with monoclonal antibodies, including rituximab, or patients who are refractory to previous rituximab plus chemotherapy.
RA, GPA, and MPA
Truxima in combination with methotrexate is indicated for the treatment of adults with severe, active RA who have had an inadequate response to or cannot tolerate other disease-modifying anti-rheumatic drugs, including one or more tumor necrosis factor inhibitor therapies.
Truxima in combination with glucocorticoids is indicated for the induction of remission in adults with severe, active GPA or MPA.
Truxima studies
There are 3 ongoing, phase 3 trials of Truxima in patients with RA (NCT02149121), advanced FL (NCT02162771), and low-tumor-burden FL (NCT02260804).
Results from the phase 1/3 trial in patients with newly diagnosed, advanced FL suggest that Truxima and the reference rituximab are similar with regard to pharmacokinetics, immunogenicity, and safety (B Coiffier et al. ASH 2016, abstract 1807).
Results from the phase 3 study of RA patients indicate that Truxima is similar to reference products (EU and US-sourced rituximab) with regard to pharmacodynamics, safety, and efficacy for up to 24 weeks (DH Yoo et al. 2016 ACR/ARHP Annual Meeting, abstract 1635). ![]()
Drug produces high response rates in AITL

Photo by Larry Young
SAN FRANCISCO—Treatment with 5-azacitidine (5-AZA) can produce a high response rate in patients with relapsed/refractory angioimmunoblastic T-cell lymphoma (AITL), according to a small study.
The overall response rate (ORR) among AITL patients was 75%, and the complete response (CR) rate was 42%.
However, this study also included patients with other types of peripheral T-cell lymphoma (PTCL), and most of these patients did not respond to 5-AZA.
Richard Delarue, MD, of Necker University Hospital in Paris, France, presented these results at the 9th Annual T-cell Lymphoma Forum.
Results were also presented at the 2016 ASH Annual Meeting (abstract 4164). Dr Delarue reported receiving honoraria from Celgene.
Patients
The study included 19 patients with relapsed/refractory PTCL. Twelve patients had AITL, 3 had adult T-cell leukemia/lymphoma (ATLL), 2 had PTCL not otherwise specified, 1 had enteropathy-associated T-cell lymphoma, and 1 had transformed mycosis fungoides.
At diagnosis, the median age was 71 (range, 39-85) for AITL patients and 59 (range, 32-83) for the other PTCL patients. Seventy-five percent of AITL patients had an IPI score of 3 to 5 and a PIT score of 3 to 4. Eighty-six percent of the other PTCL patients had an IPI score of 3 to 5, and 57% had a PIT score of 3 to 4.
At the time of 5-AZA treatment, all patients had stage III/IV disease. The AITL patients had received a median of 2 (range, 0-6) prior lines of therapy, and the other PTCL patients had received a median of 3 (range, 0-7).
Two patients did not receive chemotherapy before 5-AZA because of the presence of associated chronic myelomonocytic leukemia (CMML) that required treatment first.
Ninety-two percent of AITL patients had TET2 mutations (n=11), 33% had DNMT3A mutations (n=4), and 0% had IDH2 mutations. One of the non-AITL patients had a TET2 mutation.
Treatment
Patients received a subcutaneous injection of 5-AZA at 75 mg/m² for 7 consecutive days every 28 days until progression or unacceptable toxicity. Six patients also received 4 to 8 infusions of rituximab because of EBV-DNA positivity.
The patients received a median of 3 cycles of 5-AZA. At the time of analysis, 4 patients were still receiving therapy.
The median follow-up was 84 days (range, 19 to 1236).
Toxicity
“Hematological toxicity was as expected with 5-azacitidine,” Dr Delarue said.
However, 2 patients had “unusual” adverse reactions. One patient had grade 2 polyneuropathy, which was considered related to a paraneoplastic syndrome.
The other patient had grade 3 diarrhea related to colitis of unknown origin, and this led to treatment interruption.
There were no treatment-related deaths.
Efficacy
Dr Delarue noted that the ORR was significantly higher in AITL patients than in patients with the other PTCL subtypes (P=0.0198).
The ORR was 53% in the entire cohort (10/19), 75% (9/12) among AITL patients, and 14% among patients with other PTCLs (1/7).
“The only patient with a response in the ‘other PTCL’ group was a patient with HTLV1-associated ATLL . . . , but he relapsed a couple of weeks after the second cycle,” Dr Delarue explained.
Among the AITL patients, the CR rate was 42% (5/12), the partial response rate was 33% (4/12), and the rate of stable disease was 25% (3/12).
Six AITL patients eventually progressed—after 2, 2, 3, 4, 4, and 20 cycles of therapy, respectively.
Two AITL patients are off therapy but remain in CR after 9 and 10 months (5 and 6 cycles of treatment), respectively.
The median progression-free survival for AITL patients was 16 months, and the median overall survival was 17 months.
Dr DeLarue noted that 4 of the AITL patients had CMML, 1 had non-CMML myelodysplastic syndrome, 3 had monocytosis without CMML, and 4 had normal monocyte counts.
He also said that, at present, it’s not possible to correlate the results observed in the AITL patients with their mutational status.
However, he and his colleagues are planning a prospective study of 5-AZA in patients with relapsed/refractory AITL and T follicular helper cell PTCL not otherwise specified. 5-AZA will be compared to investigator’s choice in this study.
Dr DeLarue said this trial will provide an opportunity to use the new oral formulation of 5-AZA (CC-486). And he and his colleagues welcome collaborators. ![]()

Photo by Larry Young
SAN FRANCISCO—Treatment with 5-azacitidine (5-AZA) can produce a high response rate in patients with relapsed/refractory angioimmunoblastic T-cell lymphoma (AITL), according to a small study.
The overall response rate (ORR) among AITL patients was 75%, and the complete response (CR) rate was 42%.
However, this study also included patients with other types of peripheral T-cell lymphoma (PTCL), and most of these patients did not respond to 5-AZA.
Richard Delarue, MD, of Necker University Hospital in Paris, France, presented these results at the 9th Annual T-cell Lymphoma Forum.
Results were also presented at the 2016 ASH Annual Meeting (abstract 4164). Dr Delarue reported receiving honoraria from Celgene.
Patients
The study included 19 patients with relapsed/refractory PTCL. Twelve patients had AITL, 3 had adult T-cell leukemia/lymphoma (ATLL), 2 had PTCL not otherwise specified, 1 had enteropathy-associated T-cell lymphoma, and 1 had transformed mycosis fungoides.
At diagnosis, the median age was 71 (range, 39-85) for AITL patients and 59 (range, 32-83) for the other PTCL patients. Seventy-five percent of AITL patients had an IPI score of 3 to 5 and a PIT score of 3 to 4. Eighty-six percent of the other PTCL patients had an IPI score of 3 to 5, and 57% had a PIT score of 3 to 4.
At the time of 5-AZA treatment, all patients had stage III/IV disease. The AITL patients had received a median of 2 (range, 0-6) prior lines of therapy, and the other PTCL patients had received a median of 3 (range, 0-7).
Two patients did not receive chemotherapy before 5-AZA because of the presence of associated chronic myelomonocytic leukemia (CMML) that required treatment first.
Ninety-two percent of AITL patients had TET2 mutations (n=11), 33% had DNMT3A mutations (n=4), and 0% had IDH2 mutations. One of the non-AITL patients had a TET2 mutation.
Treatment
Patients received a subcutaneous injection of 5-AZA at 75 mg/m² for 7 consecutive days every 28 days until progression or unacceptable toxicity. Six patients also received 4 to 8 infusions of rituximab because of EBV-DNA positivity.
The patients received a median of 3 cycles of 5-AZA. At the time of analysis, 4 patients were still receiving therapy.
The median follow-up was 84 days (range, 19 to 1236).
Toxicity
“Hematological toxicity was as expected with 5-azacitidine,” Dr Delarue said.
However, 2 patients had “unusual” adverse reactions. One patient had grade 2 polyneuropathy, which was considered related to a paraneoplastic syndrome.
The other patient had grade 3 diarrhea related to colitis of unknown origin, and this led to treatment interruption.
There were no treatment-related deaths.
Efficacy
Dr Delarue noted that the ORR was significantly higher in AITL patients than in patients with the other PTCL subtypes (P=0.0198).
The ORR was 53% in the entire cohort (10/19), 75% (9/12) among AITL patients, and 14% among patients with other PTCLs (1/7).
“The only patient with a response in the ‘other PTCL’ group was a patient with HTLV1-associated ATLL . . . , but he relapsed a couple of weeks after the second cycle,” Dr Delarue explained.
Among the AITL patients, the CR rate was 42% (5/12), the partial response rate was 33% (4/12), and the rate of stable disease was 25% (3/12).
Six AITL patients eventually progressed—after 2, 2, 3, 4, 4, and 20 cycles of therapy, respectively.
Two AITL patients are off therapy but remain in CR after 9 and 10 months (5 and 6 cycles of treatment), respectively.
The median progression-free survival for AITL patients was 16 months, and the median overall survival was 17 months.
Dr DeLarue noted that 4 of the AITL patients had CMML, 1 had non-CMML myelodysplastic syndrome, 3 had monocytosis without CMML, and 4 had normal monocyte counts.
He also said that, at present, it’s not possible to correlate the results observed in the AITL patients with their mutational status.
However, he and his colleagues are planning a prospective study of 5-AZA in patients with relapsed/refractory AITL and T follicular helper cell PTCL not otherwise specified. 5-AZA will be compared to investigator’s choice in this study.
Dr DeLarue said this trial will provide an opportunity to use the new oral formulation of 5-AZA (CC-486). And he and his colleagues welcome collaborators. ![]()

Photo by Larry Young
SAN FRANCISCO—Treatment with 5-azacitidine (5-AZA) can produce a high response rate in patients with relapsed/refractory angioimmunoblastic T-cell lymphoma (AITL), according to a small study.
The overall response rate (ORR) among AITL patients was 75%, and the complete response (CR) rate was 42%.
However, this study also included patients with other types of peripheral T-cell lymphoma (PTCL), and most of these patients did not respond to 5-AZA.
Richard Delarue, MD, of Necker University Hospital in Paris, France, presented these results at the 9th Annual T-cell Lymphoma Forum.
Results were also presented at the 2016 ASH Annual Meeting (abstract 4164). Dr Delarue reported receiving honoraria from Celgene.
Patients
The study included 19 patients with relapsed/refractory PTCL. Twelve patients had AITL, 3 had adult T-cell leukemia/lymphoma (ATLL), 2 had PTCL not otherwise specified, 1 had enteropathy-associated T-cell lymphoma, and 1 had transformed mycosis fungoides.
At diagnosis, the median age was 71 (range, 39-85) for AITL patients and 59 (range, 32-83) for the other PTCL patients. Seventy-five percent of AITL patients had an IPI score of 3 to 5 and a PIT score of 3 to 4. Eighty-six percent of the other PTCL patients had an IPI score of 3 to 5, and 57% had a PIT score of 3 to 4.
At the time of 5-AZA treatment, all patients had stage III/IV disease. The AITL patients had received a median of 2 (range, 0-6) prior lines of therapy, and the other PTCL patients had received a median of 3 (range, 0-7).
Two patients did not receive chemotherapy before 5-AZA because of the presence of associated chronic myelomonocytic leukemia (CMML) that required treatment first.
Ninety-two percent of AITL patients had TET2 mutations (n=11), 33% had DNMT3A mutations (n=4), and 0% had IDH2 mutations. One of the non-AITL patients had a TET2 mutation.
Treatment
Patients received a subcutaneous injection of 5-AZA at 75 mg/m² for 7 consecutive days every 28 days until progression or unacceptable toxicity. Six patients also received 4 to 8 infusions of rituximab because of EBV-DNA positivity.
The patients received a median of 3 cycles of 5-AZA. At the time of analysis, 4 patients were still receiving therapy.
The median follow-up was 84 days (range, 19 to 1236).
Toxicity
“Hematological toxicity was as expected with 5-azacitidine,” Dr Delarue said.
However, 2 patients had “unusual” adverse reactions. One patient had grade 2 polyneuropathy, which was considered related to a paraneoplastic syndrome.
The other patient had grade 3 diarrhea related to colitis of unknown origin, and this led to treatment interruption.
There were no treatment-related deaths.
Efficacy
Dr Delarue noted that the ORR was significantly higher in AITL patients than in patients with the other PTCL subtypes (P=0.0198).
The ORR was 53% in the entire cohort (10/19), 75% (9/12) among AITL patients, and 14% among patients with other PTCLs (1/7).
“The only patient with a response in the ‘other PTCL’ group was a patient with HTLV1-associated ATLL . . . , but he relapsed a couple of weeks after the second cycle,” Dr Delarue explained.
Among the AITL patients, the CR rate was 42% (5/12), the partial response rate was 33% (4/12), and the rate of stable disease was 25% (3/12).
Six AITL patients eventually progressed—after 2, 2, 3, 4, 4, and 20 cycles of therapy, respectively.
Two AITL patients are off therapy but remain in CR after 9 and 10 months (5 and 6 cycles of treatment), respectively.
The median progression-free survival for AITL patients was 16 months, and the median overall survival was 17 months.
Dr DeLarue noted that 4 of the AITL patients had CMML, 1 had non-CMML myelodysplastic syndrome, 3 had monocytosis without CMML, and 4 had normal monocyte counts.
He also said that, at present, it’s not possible to correlate the results observed in the AITL patients with their mutational status.
However, he and his colleagues are planning a prospective study of 5-AZA in patients with relapsed/refractory AITL and T follicular helper cell PTCL not otherwise specified. 5-AZA will be compared to investigator’s choice in this study.
Dr DeLarue said this trial will provide an opportunity to use the new oral formulation of 5-AZA (CC-486). And he and his colleagues welcome collaborators. ![]()
Obinutuzumab approved to treat FL in Canada

Health Canada has approved the use of obinutuzumab (Gazyva®), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who relapsed after, or are refractory to, a rituximab-containing regimen.
Obinutuzumab is also approved in Canada for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is a product of Roche.
Health Canada’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial.
The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
At last follow-up, the median overall survival had not been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%). ![]()

Health Canada has approved the use of obinutuzumab (Gazyva®), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who relapsed after, or are refractory to, a rituximab-containing regimen.
Obinutuzumab is also approved in Canada for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is a product of Roche.
Health Canada’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial.
The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
At last follow-up, the median overall survival had not been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%). ![]()

Health Canada has approved the use of obinutuzumab (Gazyva®), an anti-CD20 monoclonal antibody, in patients with follicular lymphoma (FL).
The approval means obinutuzumab can be given, first in combination with bendamustine and then alone as maintenance therapy, to FL patients who relapsed after, or are refractory to, a rituximab-containing regimen.
Obinutuzumab is also approved in Canada for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is a product of Roche.
Health Canada’s approval of obinutuzumab in FL is based on results from the phase 3 GADOLIN trial.
The study included 413 patients with rituximab-refractory non-Hodgkin lymphoma, including 321 patients with FL, 46 with marginal zone lymphoma, and 28 with small lymphocytic lymphoma.
The patients were randomized to receive bendamustine alone (control arm) or a combination of bendamustine and obinutuzumab followed by obinutuzumab maintenance (every 2 months for 2 years or until progression).
The primary endpoint of the study was progression-free survival (PFS), as assessed by an independent review committee (IRC). The secondary endpoints were PFS assessed by investigator review, best overall response, complete response (CR), partial response (PR), duration of response, overall survival, and safety profile.
Among patients with FL, the obinutuzumab regimen improved PFS compared to bendamustine alone, as assessed by the IRC (hazard ratio [HR]=0.48, P<0.0001). The median PFS was not reached in patients receiving the obinutuzumab regimen but was 13.8 months in those receiving bendamustine alone.
Investigator-assessed PFS was consistent with IRC-assessed PFS. Investigators said the median PFS with the obinutuzumab regimen was more than double that with bendamustine alone—29.2 months vs 13.7 months (HR=0.48, P<0.0001).
The best overall response for patients receiving the obinutuzumab regimen was 78.7% (15.5% CR, 63.2% PR), compared to 74.7% (18.7% CR, 56% PR) for those receiving bendamustine alone, as assessed by the IRC.
The median duration of response was not reached for patients receiving the obinutuzumab regimen and was 11.6 months for those receiving bendamustine alone.
At last follow-up, the median overall survival had not been reached in either study arm.
The most common grade 3/4 adverse events observed in patients receiving the obinutuzumab regimen were neutropenia (33%), infusion reactions (11%), and thrombocytopenia (10%).
The most common adverse events of any grade were infusion reactions (69%), neutropenia (35%), nausea (54%), fatigue (39%), cough (26%), diarrhea (27%), constipation (19%), fever (18%), thrombocytopenia (15%), vomiting (22%), upper respiratory tract infection (13%), decreased appetite (18%), joint or muscle pain (12%), sinusitis (12%), anemia (12%), general weakness (11%), and urinary tract infection (10%). ![]()
Circulating DNA catches lymphoma relapse early
A newer technique aimed at detect circulating tumor DNA in the blood – cancer personalized profiling by deep sequencing (CAPP-Seq) – detected recurrence of diffuse large B cell lymphoma more than 6 months earlier than radiographic findings in a study at Stanford (Calif.) University, where the technique was invented.
The findings signal another win for “liquid biopsy,” the measurement of tumor DNA circulating in the blood, which is rapidly emerging as a quick and powerful tool for the diagnosis of a range of cancers and tumor subtypes, and prediction of tumor behavior and treatment response. Investigators at Stanford and elsewhere are studying liquid biopsy not only for lymphoma, but also for colorectal, thyroid, breast, prostate, and most other cancers. The Stanford team recently reported that its circulating DNA-detecting CAPP-Seq technique also helps in lung cancer.
In the new study, Stanford used CAPP-Seq (Cancer Personalized Profiling by deep Sequencing), which it called “an ultrasensitive capture-based targeted sequencing method” to analyze 166 plasma and 118 tissue samples from 92 patients with diffuse large B cell lymphoma (DLBCL) at diagnosis and various point afterward. The team compared the results to radiologic, and other standard diagnostic and monitoring techniques (Sci Transl Med. 2016 Nov 9;8[364]:364ra155).
At diagnosis, the amount of circulating DNA (ctDNA) correlated strongly with clinical indices and was independently predictive of patient outcomes; “whereas 100% of pretreatment samples had detectable ctDNA, only 37% of samples had abnormally high serum” lactate dehydrogenase, currently the most commonly used biomarker for DLBCL, said investigators, led by research fellow Florian Scherer, MD.
The group detected ctDNA in 73% of patients (8/11) who eventually relapsed a mean of 188 days before relapse was detected by standard-of-care radiologic techniques.
CAPP-Seq identified nine patients with a particular type of activated B cell-like tumor, for whom ibrutinib (Imbruvica) is particularly effective; ctDNA also predicted the transformation of indolent follicular lymphoma to DLBCL “with high sensitivity and specificity,” the group reported.
Stanford anticipates “ctDNA will have broad utility for dissecting tumor heterogeneity within and between patients with lymphomas and other cancer types, with applications for the identification of adverse risk groups, the discovery of resistance mechanisms to diverse therapies, and the development of risk-adapted therapeutics.”
The team said its approach “outperformed immunoglobulin sequencing and radiographic imaging for the detection of minimal residual disease and facilitated noninvasive identification of emergent resistance mutations to targeted therapies.” Meanwhile, while biomarkers hold “great promise for risk stratification and therapeutic targeting,” they are “currently difficult to measure in clinical settings,” the investigators said.
Roche bought the rights to CAPP-Seq from Stanford in 2015. Several authors are coinventors on patent applications for CAPP-Seq and also Roche consultants. Two are employees. Dr. Scherer had no disclosures. The work was funded by Stanford, the American Society of Hematology, the National Cancer Institute, and others.
A newer technique aimed at detect circulating tumor DNA in the blood – cancer personalized profiling by deep sequencing (CAPP-Seq) – detected recurrence of diffuse large B cell lymphoma more than 6 months earlier than radiographic findings in a study at Stanford (Calif.) University, where the technique was invented.
The findings signal another win for “liquid biopsy,” the measurement of tumor DNA circulating in the blood, which is rapidly emerging as a quick and powerful tool for the diagnosis of a range of cancers and tumor subtypes, and prediction of tumor behavior and treatment response. Investigators at Stanford and elsewhere are studying liquid biopsy not only for lymphoma, but also for colorectal, thyroid, breast, prostate, and most other cancers. The Stanford team recently reported that its circulating DNA-detecting CAPP-Seq technique also helps in lung cancer.
In the new study, Stanford used CAPP-Seq (Cancer Personalized Profiling by deep Sequencing), which it called “an ultrasensitive capture-based targeted sequencing method” to analyze 166 plasma and 118 tissue samples from 92 patients with diffuse large B cell lymphoma (DLBCL) at diagnosis and various point afterward. The team compared the results to radiologic, and other standard diagnostic and monitoring techniques (Sci Transl Med. 2016 Nov 9;8[364]:364ra155).
At diagnosis, the amount of circulating DNA (ctDNA) correlated strongly with clinical indices and was independently predictive of patient outcomes; “whereas 100% of pretreatment samples had detectable ctDNA, only 37% of samples had abnormally high serum” lactate dehydrogenase, currently the most commonly used biomarker for DLBCL, said investigators, led by research fellow Florian Scherer, MD.
The group detected ctDNA in 73% of patients (8/11) who eventually relapsed a mean of 188 days before relapse was detected by standard-of-care radiologic techniques.
CAPP-Seq identified nine patients with a particular type of activated B cell-like tumor, for whom ibrutinib (Imbruvica) is particularly effective; ctDNA also predicted the transformation of indolent follicular lymphoma to DLBCL “with high sensitivity and specificity,” the group reported.
Stanford anticipates “ctDNA will have broad utility for dissecting tumor heterogeneity within and between patients with lymphomas and other cancer types, with applications for the identification of adverse risk groups, the discovery of resistance mechanisms to diverse therapies, and the development of risk-adapted therapeutics.”
The team said its approach “outperformed immunoglobulin sequencing and radiographic imaging for the detection of minimal residual disease and facilitated noninvasive identification of emergent resistance mutations to targeted therapies.” Meanwhile, while biomarkers hold “great promise for risk stratification and therapeutic targeting,” they are “currently difficult to measure in clinical settings,” the investigators said.
Roche bought the rights to CAPP-Seq from Stanford in 2015. Several authors are coinventors on patent applications for CAPP-Seq and also Roche consultants. Two are employees. Dr. Scherer had no disclosures. The work was funded by Stanford, the American Society of Hematology, the National Cancer Institute, and others.
A newer technique aimed at detect circulating tumor DNA in the blood – cancer personalized profiling by deep sequencing (CAPP-Seq) – detected recurrence of diffuse large B cell lymphoma more than 6 months earlier than radiographic findings in a study at Stanford (Calif.) University, where the technique was invented.
The findings signal another win for “liquid biopsy,” the measurement of tumor DNA circulating in the blood, which is rapidly emerging as a quick and powerful tool for the diagnosis of a range of cancers and tumor subtypes, and prediction of tumor behavior and treatment response. Investigators at Stanford and elsewhere are studying liquid biopsy not only for lymphoma, but also for colorectal, thyroid, breast, prostate, and most other cancers. The Stanford team recently reported that its circulating DNA-detecting CAPP-Seq technique also helps in lung cancer.
In the new study, Stanford used CAPP-Seq (Cancer Personalized Profiling by deep Sequencing), which it called “an ultrasensitive capture-based targeted sequencing method” to analyze 166 plasma and 118 tissue samples from 92 patients with diffuse large B cell lymphoma (DLBCL) at diagnosis and various point afterward. The team compared the results to radiologic, and other standard diagnostic and monitoring techniques (Sci Transl Med. 2016 Nov 9;8[364]:364ra155).
At diagnosis, the amount of circulating DNA (ctDNA) correlated strongly with clinical indices and was independently predictive of patient outcomes; “whereas 100% of pretreatment samples had detectable ctDNA, only 37% of samples had abnormally high serum” lactate dehydrogenase, currently the most commonly used biomarker for DLBCL, said investigators, led by research fellow Florian Scherer, MD.
The group detected ctDNA in 73% of patients (8/11) who eventually relapsed a mean of 188 days before relapse was detected by standard-of-care radiologic techniques.
CAPP-Seq identified nine patients with a particular type of activated B cell-like tumor, for whom ibrutinib (Imbruvica) is particularly effective; ctDNA also predicted the transformation of indolent follicular lymphoma to DLBCL “with high sensitivity and specificity,” the group reported.
Stanford anticipates “ctDNA will have broad utility for dissecting tumor heterogeneity within and between patients with lymphomas and other cancer types, with applications for the identification of adverse risk groups, the discovery of resistance mechanisms to diverse therapies, and the development of risk-adapted therapeutics.”
The team said its approach “outperformed immunoglobulin sequencing and radiographic imaging for the detection of minimal residual disease and facilitated noninvasive identification of emergent resistance mutations to targeted therapies.” Meanwhile, while biomarkers hold “great promise for risk stratification and therapeutic targeting,” they are “currently difficult to measure in clinical settings,” the investigators said.
Roche bought the rights to CAPP-Seq from Stanford in 2015. Several authors are coinventors on patent applications for CAPP-Seq and also Roche consultants. Two are employees. Dr. Scherer had no disclosures. The work was funded by Stanford, the American Society of Hematology, the National Cancer Institute, and others.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: Major finding: Circulating tumor DNA was found in 73% of relapse patients a mean of 188 days before relapse was detected by standard-of-care radiologic techniques. Circulating tumor DNA was found in the plasma of 100% of patients at diagnosis, but only 37% had abnormally high serum lactate dehydrogenase, currently the most commonly used biomarker.
Data source: Analysis of 166 plasma and 118 tissue samples from 92 patients with diffuse large B cell lymphoma.
Disclosures: Roche bought the rights to CAPP-Seq from Stanford (Calif.) University in 2015. Several authors are coinventors on patent applications for CAPP-Seq and also Roche consults. Two are employees. The work was funded by Stanford, the American Society of Hematology, the National Cancer Institute, and others.
Study provides new insight into B-cell metabolism
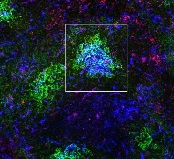
the spleen of a mouse, showing
inactivated GSK3 (magenta)
in B cells (blue) near follicular
dendritic cells (green).
Image from the lab of
Robert Rickert, PhD
Research published in Nature Immunology helps explain how B-cell metabolism adapts to different environments.
The study suggests the protein GSK3 acts as a metabolic checkpoint regulator in B cells, promoting the survival of circulating B cells while limiting the growth and proliferation of B cells in germinal centers.
“Our research shows that the protein GSK3 plays a crucial role in helping B cells meet the energy needs of their distinct states,” said study author Robert Rickert, PhD, of Sanford Burnham Prebys Medical Discovery Institute in La Jolla, California.
“The findings are particularly relevant for certain B-cell pathologies, including lymphoma subtypes, where there is an increased demand for energy to support the hyperproliferation of cells in a microenvironment that may be limited in nutrients.”
Dr Rickert and his colleagues noted that B cells predominate in a quiescent state until they encounter an antigen, which prompts the cells to grow, proliferate, and differentiate.
The team’s new study showed that GSK3 adjusts B-cell metabolism to match the needs of these different cell states.
In circulating B cells, GSK3 limits overall metabolic activity. In proliferating B cells in germinal centers, GSK3 slows glycolysis and the production of mitochondria.
In fact, GSK3 function is essential for B-cell survival in germinal centers. To understand why, the researchers looked at how B cells in these regions generate energy.
The team found that because these B cells are so metabolically active, they consume nearly all available glucose. That switches on glycolysis.
High glycolytic activity leads to an accumulation of toxic reactive oxygen species, as does rapid manufacture of mitochondria, which tend to leak the same chemicals.
Thus, by restraining the metabolism in specific ways, GSK3 prevents cell death induced by reactive oxygen species.
“Our results were really surprising,” Dr Rickert said. “Until now, we would have thought that slowing metabolism would only be important for preventing B cells from becoming cancerous, which it indeed may be. These studies provide insight into the dynamic nature of B-cell metabolism that literally ‘fuels’ differentiation in the germinal center to produce an effective antibody response.”
“It’s not yet clear whether or how GSK3 might be a target for future therapies for B cell-related diseases, but this research opens a lot of doors for further studies. To start with, we plan to investigate how GSK3 is regulated in lymphoma and how that relates to changes in metabolism. That research could lead to new approaches to treating lymphoma.”
This research was performed in collaboration with scientists at Eli Lilly and the Lunenfeld-Tanenbaum Research Institute at the University of Toronto. Funding was provided by the National Institutes of Health, the Lilly Research Award Program, the Arthritis National Research Foundation, and the Canadian Institutes of Health Research. ![]()
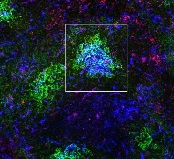
the spleen of a mouse, showing
inactivated GSK3 (magenta)
in B cells (blue) near follicular
dendritic cells (green).
Image from the lab of
Robert Rickert, PhD
Research published in Nature Immunology helps explain how B-cell metabolism adapts to different environments.
The study suggests the protein GSK3 acts as a metabolic checkpoint regulator in B cells, promoting the survival of circulating B cells while limiting the growth and proliferation of B cells in germinal centers.
“Our research shows that the protein GSK3 plays a crucial role in helping B cells meet the energy needs of their distinct states,” said study author Robert Rickert, PhD, of Sanford Burnham Prebys Medical Discovery Institute in La Jolla, California.
“The findings are particularly relevant for certain B-cell pathologies, including lymphoma subtypes, where there is an increased demand for energy to support the hyperproliferation of cells in a microenvironment that may be limited in nutrients.”
Dr Rickert and his colleagues noted that B cells predominate in a quiescent state until they encounter an antigen, which prompts the cells to grow, proliferate, and differentiate.
The team’s new study showed that GSK3 adjusts B-cell metabolism to match the needs of these different cell states.
In circulating B cells, GSK3 limits overall metabolic activity. In proliferating B cells in germinal centers, GSK3 slows glycolysis and the production of mitochondria.
In fact, GSK3 function is essential for B-cell survival in germinal centers. To understand why, the researchers looked at how B cells in these regions generate energy.
The team found that because these B cells are so metabolically active, they consume nearly all available glucose. That switches on glycolysis.
High glycolytic activity leads to an accumulation of toxic reactive oxygen species, as does rapid manufacture of mitochondria, which tend to leak the same chemicals.
Thus, by restraining the metabolism in specific ways, GSK3 prevents cell death induced by reactive oxygen species.
“Our results were really surprising,” Dr Rickert said. “Until now, we would have thought that slowing metabolism would only be important for preventing B cells from becoming cancerous, which it indeed may be. These studies provide insight into the dynamic nature of B-cell metabolism that literally ‘fuels’ differentiation in the germinal center to produce an effective antibody response.”
“It’s not yet clear whether or how GSK3 might be a target for future therapies for B cell-related diseases, but this research opens a lot of doors for further studies. To start with, we plan to investigate how GSK3 is regulated in lymphoma and how that relates to changes in metabolism. That research could lead to new approaches to treating lymphoma.”
This research was performed in collaboration with scientists at Eli Lilly and the Lunenfeld-Tanenbaum Research Institute at the University of Toronto. Funding was provided by the National Institutes of Health, the Lilly Research Award Program, the Arthritis National Research Foundation, and the Canadian Institutes of Health Research. ![]()
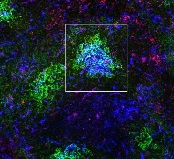
the spleen of a mouse, showing
inactivated GSK3 (magenta)
in B cells (blue) near follicular
dendritic cells (green).
Image from the lab of
Robert Rickert, PhD
Research published in Nature Immunology helps explain how B-cell metabolism adapts to different environments.
The study suggests the protein GSK3 acts as a metabolic checkpoint regulator in B cells, promoting the survival of circulating B cells while limiting the growth and proliferation of B cells in germinal centers.
“Our research shows that the protein GSK3 plays a crucial role in helping B cells meet the energy needs of their distinct states,” said study author Robert Rickert, PhD, of Sanford Burnham Prebys Medical Discovery Institute in La Jolla, California.
“The findings are particularly relevant for certain B-cell pathologies, including lymphoma subtypes, where there is an increased demand for energy to support the hyperproliferation of cells in a microenvironment that may be limited in nutrients.”
Dr Rickert and his colleagues noted that B cells predominate in a quiescent state until they encounter an antigen, which prompts the cells to grow, proliferate, and differentiate.
The team’s new study showed that GSK3 adjusts B-cell metabolism to match the needs of these different cell states.
In circulating B cells, GSK3 limits overall metabolic activity. In proliferating B cells in germinal centers, GSK3 slows glycolysis and the production of mitochondria.
In fact, GSK3 function is essential for B-cell survival in germinal centers. To understand why, the researchers looked at how B cells in these regions generate energy.
The team found that because these B cells are so metabolically active, they consume nearly all available glucose. That switches on glycolysis.
High glycolytic activity leads to an accumulation of toxic reactive oxygen species, as does rapid manufacture of mitochondria, which tend to leak the same chemicals.
Thus, by restraining the metabolism in specific ways, GSK3 prevents cell death induced by reactive oxygen species.
“Our results were really surprising,” Dr Rickert said. “Until now, we would have thought that slowing metabolism would only be important for preventing B cells from becoming cancerous, which it indeed may be. These studies provide insight into the dynamic nature of B-cell metabolism that literally ‘fuels’ differentiation in the germinal center to produce an effective antibody response.”
“It’s not yet clear whether or how GSK3 might be a target for future therapies for B cell-related diseases, but this research opens a lot of doors for further studies. To start with, we plan to investigate how GSK3 is regulated in lymphoma and how that relates to changes in metabolism. That research could lead to new approaches to treating lymphoma.”
This research was performed in collaboration with scientists at Eli Lilly and the Lunenfeld-Tanenbaum Research Institute at the University of Toronto. Funding was provided by the National Institutes of Health, the Lilly Research Award Program, the Arthritis National Research Foundation, and the Canadian Institutes of Health Research. ![]()
Combined checkpoint blockade promising in HL

© Todd Buchanan 2016
SAN DIEGO—Immune checkpoint blockade with nivolumab plus ipilimumab has shown promise in treating hematologic malignancies, particularly classical Hodgkin lymphoma (HL), based on results of the combination cohort of the phase 1 CheckMate 039 study.
Thirty-one heavily pre-treated HL patients achieved an overall response rate (ORR) of 74%, including 6 complete responses.
And in transplant-naïve HL patients, the combination produced an ORR of 67%.
“Most in the room would be familiar with the excellent results that we have seen with monotherapy with nivolumab,” Stephen Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, said at the 2016 ASH Annual Meeting.
“In classical Hodgkin lymphoma, we’ve seen meaningful and clinically quite stellar results and durable responses.”
“Our plan was, as part of this trial [CheckMate 039], to then move to see whether adding a further checkpoint, ipilimumab, could enhance the results seen with nivolumab.”
Dr Ansell presented the findings for the checkpoint combination as abstract 183. He disclosed research funding from Bristol-Myers Squibb, the company that funded the study.
Checkpoint inhibitors
Nivolumab and ipilimumab are both fully human monoclonal antibodies, but ipilimumab “works in a slightly different fashion from nivolumab,” Dr Ansell said.
Nivolumab targets the programmed death receptor-1 (PD-1) and disrupts PD-1 pathway signaling and restores anti-tumor T-cell function.
Ipilimumab targets cytotoxic T-lymphocyte antigen 4 (CTLA-4) and induces anti-tumor immunity.
The combination has shown superior efficacy, compared to either agent alone, in preclinical studies and a phase 1 trial of patients with advanced melanoma.
So the investigators added a combination cohort to CheckMate 039.
Combination cohort study design
Patients were eligible to enroll if they had relapsed or refractory HL, B-cell non-Hodgkin lymphoma (NHL, including follicular or diffuse large B-cell lymphoma), T-cell NHL (including cutaneous or peripheral T-cell lymphoma), or multiple myeloma (MM).
Patients could not have had prior organ or allogeneic stem cell transplant and no prior immune checkpoint blockade therapy.
Treatment consisted of nivolumab at 3 mg/kg IV plus ipilimumab at 1 mg/kg IV every 3 weeks for 4 doses. The combination phase was followed by nivolumab monotherapy at the same dose every 2 weeks for 2 years.
The primary endpoint was safety and tolerability. Secondary endpoints included investigator-assessed best overall response, duration of response, progression-free survival (PFS), and biomarker analyses.
Patient characteristics
The investigators enrolled 31 HL, 15 B-cell NHL, 11 T-cell NHL, and 7 MM patients. Most patients, Dr Ansell noted, were heavily pretreated.
HL patients were 42% male, 52% had an ECOG status of 1, and they had a median of 4 (range, 2 to 10) prior systemic therapies. Forty-two percent had prior autologous stem cell transplant (ASCT).
“Interestingly, in the Hodgkin cohort, a number of patients had not proceeded to an autologous transplant, but predominantly because these were chemo-refractory or chemo-resistant patients not eligible for a transplant,” Dr Ansell pointed out.
Of the HL patients, 18 were transplant-naïve, 13 were chemo-resistant, 3 were ineligible for ASCT, and 2 declined the procedure.
B-cell NHL patients were 73% male, and 80% had an ECOG status of 1. They had a median of 3 (range, 1 to 16) prior systemic therapies. Seven percent had a prior ASCT.
T-cell NHL patients were 55% male, 73% had an ECOG status of 1, and they had a median of 4 (range, 1 to 11) prior systemic therapies. None had a prior ASCT.
MM patients were 86% male, 71% had an ECOG status of 1, and they had a median of 5 (range, 2 to 20) prior systemic therapies. More than half had a prior ASCT.
Patient disposition
With follow-up approaching a year, more patients with HL are still on treatment (39%) compared with B-cell NHL (13%), T-cell NHL (18%), and MM (0%) patients.
“Of note, however, is that the reasons for going off treatment were predominantly disease progression,” Dr Ansell said.
“The vast majority of patients who came off treatment came off treatment because their disease progressed, and the numbers that came off because of toxicity were relatively low.”
Seven HL patients went off treatment due to disease progression and 2 due to study drug toxicity.
Eleven B-cell NHL patients went off treatment due to disease progression and 2 withdrew due to unrelated adverse events (AEs).
Five T-cell NHL patients went off treatment due to disease progression and 2 due to study drug toxicity.
And 4 MM patients withdrew due to disease progression, 1 due to study drug toxicity, and 1 due to AEs unrelated to the study drug.
About two-thirds of HL patients, over 90% of B-cell NHL patients, about 80% of T-cell NHL patients, and about 70% of MM patients received 90% or more of the intended dose of each drug.
Safety
One patient with primary mediastinal B-cell lymphoma was included in the safety analysis, for a total of 65 patients treated.
“The majority of patients had some degree of adverse event,” Dr Ansell explained. “But if one looks at the grade 3 and 4 adverse events, those were seen in a more modest number of patients, in a minority of patients. And most importantly, if one looks at the adverse events that led to discontinuation, one can see that this was in a significant minority of patients.”
Five patients discontinued due to treatment-related AEs, which were pneumonitis (n=3), pneumonia and pneumonitis (n=1), and diabetic ketoacidosis (n=1).
Overall, 51 patients (78%) experienced an AE; 19 (29%) had a grade 3–4 AE, 14 (22%) had a serious AE, and 5 (8%) discontinued due to an AE.
Of 31 HL patients, 28 (90%) had an AE, 8 (26%) had a grade 3–4 AE, 6 (19%) had a serious AE, and 2 (6%) discontinued due to an AE.
All 11 T-cell NHL patients experienced an AE, 5 patients (45%) a grade 3-4 AE, 4 patients (36%) had a serious AE, and 2 patients (18%) discontinued because of an AE.
About half of B-cell NHL and MM patients experienced an AE, with 1 MM patient discontinuing as a result of it and no B-cell NHL patient discontinuing due to an AE.
“I would highlight that most of the adverse events were, as expected, immunological in nature . . . . ,” Dr Ansell said. “A very modest number of patients had grade 3 and 4 toxicities.”
The most common drug-related AEs of any grade were fatigue (n=17; 26%), pyrexia (n=15; 23%), rash (n=7; 11%), diarrhea (n=12; 18%), and nausea, pneumonitis, cough, and infusion-related reactions, with 9 patients each (14%).
Efficacy
Twenty-three HL patients (74%) achieved an overall response, including 6 patients (19%) with a complete response and 17 (55%) with a partial response. Three patients (10%) had stable disease, and 3 (10%) had relapsed or progressive disease. Response was not reported for 2 patients (6%).
“Most of these responses are durable, and, very encouraging, you can see patients out approaching a year continuing on therapy,” Dr Ansell said.
The ORR in the 18 transplant-naive patients was 67% (n=67).
The median duration of response for HL patients was not reached and ranged from 0.0 to 13.4 months.
B-cell NHL patients had an ORR of 20% (n=3). There were no complete responses and 3 (20%) partial responses. One patient (7%) had stable disease, and 8 (53%) had relapsed or progressive disase. The median duration of partial response was not reached and ranged from 11.0 to 12.7 months.
T-cell NHL patients had an ORR of 9% (n=1). There were no complete responses and 1 (9%) partial response. Four patients (36%) had stable disease, and 3 (27%) had relapsed or progressive disease. The median duration of partial response was not reached and was 3.9 months.
Except for 1 patient with stable disease, MM patients did not respond to therapy.
Biomarker analysis
All 19 HL patients with a known PD-L1 status at baseline saw their tumor burden decrease to below baseline levels. This may be because HL is characterized by high PD-L1 expression and high responsiveness to checkpoint blockade.
Patients with NHL, on the other hand, have a diverse group of tumors characterized by variable PD-L1 expression. Eight of 13 patients with known expression saw their tumor burden decrease with treatment to below baseline.
Encouraged by the results, the investigators believe further investigation of the combination is in order, as the combination, with limited follow-up, achieved a high and durable ORR in HL patients, including those who were transplant-naïve. ![]()

© Todd Buchanan 2016
SAN DIEGO—Immune checkpoint blockade with nivolumab plus ipilimumab has shown promise in treating hematologic malignancies, particularly classical Hodgkin lymphoma (HL), based on results of the combination cohort of the phase 1 CheckMate 039 study.
Thirty-one heavily pre-treated HL patients achieved an overall response rate (ORR) of 74%, including 6 complete responses.
And in transplant-naïve HL patients, the combination produced an ORR of 67%.
“Most in the room would be familiar with the excellent results that we have seen with monotherapy with nivolumab,” Stephen Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, said at the 2016 ASH Annual Meeting.
“In classical Hodgkin lymphoma, we’ve seen meaningful and clinically quite stellar results and durable responses.”
“Our plan was, as part of this trial [CheckMate 039], to then move to see whether adding a further checkpoint, ipilimumab, could enhance the results seen with nivolumab.”
Dr Ansell presented the findings for the checkpoint combination as abstract 183. He disclosed research funding from Bristol-Myers Squibb, the company that funded the study.
Checkpoint inhibitors
Nivolumab and ipilimumab are both fully human monoclonal antibodies, but ipilimumab “works in a slightly different fashion from nivolumab,” Dr Ansell said.
Nivolumab targets the programmed death receptor-1 (PD-1) and disrupts PD-1 pathway signaling and restores anti-tumor T-cell function.
Ipilimumab targets cytotoxic T-lymphocyte antigen 4 (CTLA-4) and induces anti-tumor immunity.
The combination has shown superior efficacy, compared to either agent alone, in preclinical studies and a phase 1 trial of patients with advanced melanoma.
So the investigators added a combination cohort to CheckMate 039.
Combination cohort study design
Patients were eligible to enroll if they had relapsed or refractory HL, B-cell non-Hodgkin lymphoma (NHL, including follicular or diffuse large B-cell lymphoma), T-cell NHL (including cutaneous or peripheral T-cell lymphoma), or multiple myeloma (MM).
Patients could not have had prior organ or allogeneic stem cell transplant and no prior immune checkpoint blockade therapy.
Treatment consisted of nivolumab at 3 mg/kg IV plus ipilimumab at 1 mg/kg IV every 3 weeks for 4 doses. The combination phase was followed by nivolumab monotherapy at the same dose every 2 weeks for 2 years.
The primary endpoint was safety and tolerability. Secondary endpoints included investigator-assessed best overall response, duration of response, progression-free survival (PFS), and biomarker analyses.
Patient characteristics
The investigators enrolled 31 HL, 15 B-cell NHL, 11 T-cell NHL, and 7 MM patients. Most patients, Dr Ansell noted, were heavily pretreated.
HL patients were 42% male, 52% had an ECOG status of 1, and they had a median of 4 (range, 2 to 10) prior systemic therapies. Forty-two percent had prior autologous stem cell transplant (ASCT).
“Interestingly, in the Hodgkin cohort, a number of patients had not proceeded to an autologous transplant, but predominantly because these were chemo-refractory or chemo-resistant patients not eligible for a transplant,” Dr Ansell pointed out.
Of the HL patients, 18 were transplant-naïve, 13 were chemo-resistant, 3 were ineligible for ASCT, and 2 declined the procedure.
B-cell NHL patients were 73% male, and 80% had an ECOG status of 1. They had a median of 3 (range, 1 to 16) prior systemic therapies. Seven percent had a prior ASCT.
T-cell NHL patients were 55% male, 73% had an ECOG status of 1, and they had a median of 4 (range, 1 to 11) prior systemic therapies. None had a prior ASCT.
MM patients were 86% male, 71% had an ECOG status of 1, and they had a median of 5 (range, 2 to 20) prior systemic therapies. More than half had a prior ASCT.
Patient disposition
With follow-up approaching a year, more patients with HL are still on treatment (39%) compared with B-cell NHL (13%), T-cell NHL (18%), and MM (0%) patients.
“Of note, however, is that the reasons for going off treatment were predominantly disease progression,” Dr Ansell said.
“The vast majority of patients who came off treatment came off treatment because their disease progressed, and the numbers that came off because of toxicity were relatively low.”
Seven HL patients went off treatment due to disease progression and 2 due to study drug toxicity.
Eleven B-cell NHL patients went off treatment due to disease progression and 2 withdrew due to unrelated adverse events (AEs).
Five T-cell NHL patients went off treatment due to disease progression and 2 due to study drug toxicity.
And 4 MM patients withdrew due to disease progression, 1 due to study drug toxicity, and 1 due to AEs unrelated to the study drug.
About two-thirds of HL patients, over 90% of B-cell NHL patients, about 80% of T-cell NHL patients, and about 70% of MM patients received 90% or more of the intended dose of each drug.
Safety
One patient with primary mediastinal B-cell lymphoma was included in the safety analysis, for a total of 65 patients treated.
“The majority of patients had some degree of adverse event,” Dr Ansell explained. “But if one looks at the grade 3 and 4 adverse events, those were seen in a more modest number of patients, in a minority of patients. And most importantly, if one looks at the adverse events that led to discontinuation, one can see that this was in a significant minority of patients.”
Five patients discontinued due to treatment-related AEs, which were pneumonitis (n=3), pneumonia and pneumonitis (n=1), and diabetic ketoacidosis (n=1).
Overall, 51 patients (78%) experienced an AE; 19 (29%) had a grade 3–4 AE, 14 (22%) had a serious AE, and 5 (8%) discontinued due to an AE.
Of 31 HL patients, 28 (90%) had an AE, 8 (26%) had a grade 3–4 AE, 6 (19%) had a serious AE, and 2 (6%) discontinued due to an AE.
All 11 T-cell NHL patients experienced an AE, 5 patients (45%) a grade 3-4 AE, 4 patients (36%) had a serious AE, and 2 patients (18%) discontinued because of an AE.
About half of B-cell NHL and MM patients experienced an AE, with 1 MM patient discontinuing as a result of it and no B-cell NHL patient discontinuing due to an AE.
“I would highlight that most of the adverse events were, as expected, immunological in nature . . . . ,” Dr Ansell said. “A very modest number of patients had grade 3 and 4 toxicities.”
The most common drug-related AEs of any grade were fatigue (n=17; 26%), pyrexia (n=15; 23%), rash (n=7; 11%), diarrhea (n=12; 18%), and nausea, pneumonitis, cough, and infusion-related reactions, with 9 patients each (14%).
Efficacy
Twenty-three HL patients (74%) achieved an overall response, including 6 patients (19%) with a complete response and 17 (55%) with a partial response. Three patients (10%) had stable disease, and 3 (10%) had relapsed or progressive disease. Response was not reported for 2 patients (6%).
“Most of these responses are durable, and, very encouraging, you can see patients out approaching a year continuing on therapy,” Dr Ansell said.
The ORR in the 18 transplant-naive patients was 67% (n=67).
The median duration of response for HL patients was not reached and ranged from 0.0 to 13.4 months.
B-cell NHL patients had an ORR of 20% (n=3). There were no complete responses and 3 (20%) partial responses. One patient (7%) had stable disease, and 8 (53%) had relapsed or progressive disase. The median duration of partial response was not reached and ranged from 11.0 to 12.7 months.
T-cell NHL patients had an ORR of 9% (n=1). There were no complete responses and 1 (9%) partial response. Four patients (36%) had stable disease, and 3 (27%) had relapsed or progressive disease. The median duration of partial response was not reached and was 3.9 months.
Except for 1 patient with stable disease, MM patients did not respond to therapy.
Biomarker analysis
All 19 HL patients with a known PD-L1 status at baseline saw their tumor burden decrease to below baseline levels. This may be because HL is characterized by high PD-L1 expression and high responsiveness to checkpoint blockade.
Patients with NHL, on the other hand, have a diverse group of tumors characterized by variable PD-L1 expression. Eight of 13 patients with known expression saw their tumor burden decrease with treatment to below baseline.
Encouraged by the results, the investigators believe further investigation of the combination is in order, as the combination, with limited follow-up, achieved a high and durable ORR in HL patients, including those who were transplant-naïve. ![]()

© Todd Buchanan 2016
SAN DIEGO—Immune checkpoint blockade with nivolumab plus ipilimumab has shown promise in treating hematologic malignancies, particularly classical Hodgkin lymphoma (HL), based on results of the combination cohort of the phase 1 CheckMate 039 study.
Thirty-one heavily pre-treated HL patients achieved an overall response rate (ORR) of 74%, including 6 complete responses.
And in transplant-naïve HL patients, the combination produced an ORR of 67%.
“Most in the room would be familiar with the excellent results that we have seen with monotherapy with nivolumab,” Stephen Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, said at the 2016 ASH Annual Meeting.
“In classical Hodgkin lymphoma, we’ve seen meaningful and clinically quite stellar results and durable responses.”
“Our plan was, as part of this trial [CheckMate 039], to then move to see whether adding a further checkpoint, ipilimumab, could enhance the results seen with nivolumab.”
Dr Ansell presented the findings for the checkpoint combination as abstract 183. He disclosed research funding from Bristol-Myers Squibb, the company that funded the study.
Checkpoint inhibitors
Nivolumab and ipilimumab are both fully human monoclonal antibodies, but ipilimumab “works in a slightly different fashion from nivolumab,” Dr Ansell said.
Nivolumab targets the programmed death receptor-1 (PD-1) and disrupts PD-1 pathway signaling and restores anti-tumor T-cell function.
Ipilimumab targets cytotoxic T-lymphocyte antigen 4 (CTLA-4) and induces anti-tumor immunity.
The combination has shown superior efficacy, compared to either agent alone, in preclinical studies and a phase 1 trial of patients with advanced melanoma.
So the investigators added a combination cohort to CheckMate 039.
Combination cohort study design
Patients were eligible to enroll if they had relapsed or refractory HL, B-cell non-Hodgkin lymphoma (NHL, including follicular or diffuse large B-cell lymphoma), T-cell NHL (including cutaneous or peripheral T-cell lymphoma), or multiple myeloma (MM).
Patients could not have had prior organ or allogeneic stem cell transplant and no prior immune checkpoint blockade therapy.
Treatment consisted of nivolumab at 3 mg/kg IV plus ipilimumab at 1 mg/kg IV every 3 weeks for 4 doses. The combination phase was followed by nivolumab monotherapy at the same dose every 2 weeks for 2 years.
The primary endpoint was safety and tolerability. Secondary endpoints included investigator-assessed best overall response, duration of response, progression-free survival (PFS), and biomarker analyses.
Patient characteristics
The investigators enrolled 31 HL, 15 B-cell NHL, 11 T-cell NHL, and 7 MM patients. Most patients, Dr Ansell noted, were heavily pretreated.
HL patients were 42% male, 52% had an ECOG status of 1, and they had a median of 4 (range, 2 to 10) prior systemic therapies. Forty-two percent had prior autologous stem cell transplant (ASCT).
“Interestingly, in the Hodgkin cohort, a number of patients had not proceeded to an autologous transplant, but predominantly because these were chemo-refractory or chemo-resistant patients not eligible for a transplant,” Dr Ansell pointed out.
Of the HL patients, 18 were transplant-naïve, 13 were chemo-resistant, 3 were ineligible for ASCT, and 2 declined the procedure.
B-cell NHL patients were 73% male, and 80% had an ECOG status of 1. They had a median of 3 (range, 1 to 16) prior systemic therapies. Seven percent had a prior ASCT.
T-cell NHL patients were 55% male, 73% had an ECOG status of 1, and they had a median of 4 (range, 1 to 11) prior systemic therapies. None had a prior ASCT.
MM patients were 86% male, 71% had an ECOG status of 1, and they had a median of 5 (range, 2 to 20) prior systemic therapies. More than half had a prior ASCT.
Patient disposition
With follow-up approaching a year, more patients with HL are still on treatment (39%) compared with B-cell NHL (13%), T-cell NHL (18%), and MM (0%) patients.
“Of note, however, is that the reasons for going off treatment were predominantly disease progression,” Dr Ansell said.
“The vast majority of patients who came off treatment came off treatment because their disease progressed, and the numbers that came off because of toxicity were relatively low.”
Seven HL patients went off treatment due to disease progression and 2 due to study drug toxicity.
Eleven B-cell NHL patients went off treatment due to disease progression and 2 withdrew due to unrelated adverse events (AEs).
Five T-cell NHL patients went off treatment due to disease progression and 2 due to study drug toxicity.
And 4 MM patients withdrew due to disease progression, 1 due to study drug toxicity, and 1 due to AEs unrelated to the study drug.
About two-thirds of HL patients, over 90% of B-cell NHL patients, about 80% of T-cell NHL patients, and about 70% of MM patients received 90% or more of the intended dose of each drug.
Safety
One patient with primary mediastinal B-cell lymphoma was included in the safety analysis, for a total of 65 patients treated.
“The majority of patients had some degree of adverse event,” Dr Ansell explained. “But if one looks at the grade 3 and 4 adverse events, those were seen in a more modest number of patients, in a minority of patients. And most importantly, if one looks at the adverse events that led to discontinuation, one can see that this was in a significant minority of patients.”
Five patients discontinued due to treatment-related AEs, which were pneumonitis (n=3), pneumonia and pneumonitis (n=1), and diabetic ketoacidosis (n=1).
Overall, 51 patients (78%) experienced an AE; 19 (29%) had a grade 3–4 AE, 14 (22%) had a serious AE, and 5 (8%) discontinued due to an AE.
Of 31 HL patients, 28 (90%) had an AE, 8 (26%) had a grade 3–4 AE, 6 (19%) had a serious AE, and 2 (6%) discontinued due to an AE.
All 11 T-cell NHL patients experienced an AE, 5 patients (45%) a grade 3-4 AE, 4 patients (36%) had a serious AE, and 2 patients (18%) discontinued because of an AE.
About half of B-cell NHL and MM patients experienced an AE, with 1 MM patient discontinuing as a result of it and no B-cell NHL patient discontinuing due to an AE.
“I would highlight that most of the adverse events were, as expected, immunological in nature . . . . ,” Dr Ansell said. “A very modest number of patients had grade 3 and 4 toxicities.”
The most common drug-related AEs of any grade were fatigue (n=17; 26%), pyrexia (n=15; 23%), rash (n=7; 11%), diarrhea (n=12; 18%), and nausea, pneumonitis, cough, and infusion-related reactions, with 9 patients each (14%).
Efficacy
Twenty-three HL patients (74%) achieved an overall response, including 6 patients (19%) with a complete response and 17 (55%) with a partial response. Three patients (10%) had stable disease, and 3 (10%) had relapsed or progressive disease. Response was not reported for 2 patients (6%).
“Most of these responses are durable, and, very encouraging, you can see patients out approaching a year continuing on therapy,” Dr Ansell said.
The ORR in the 18 transplant-naive patients was 67% (n=67).
The median duration of response for HL patients was not reached and ranged from 0.0 to 13.4 months.
B-cell NHL patients had an ORR of 20% (n=3). There were no complete responses and 3 (20%) partial responses. One patient (7%) had stable disease, and 8 (53%) had relapsed or progressive disase. The median duration of partial response was not reached and ranged from 11.0 to 12.7 months.
T-cell NHL patients had an ORR of 9% (n=1). There were no complete responses and 1 (9%) partial response. Four patients (36%) had stable disease, and 3 (27%) had relapsed or progressive disease. The median duration of partial response was not reached and was 3.9 months.
Except for 1 patient with stable disease, MM patients did not respond to therapy.
Biomarker analysis
All 19 HL patients with a known PD-L1 status at baseline saw their tumor burden decrease to below baseline levels. This may be because HL is characterized by high PD-L1 expression and high responsiveness to checkpoint blockade.
Patients with NHL, on the other hand, have a diverse group of tumors characterized by variable PD-L1 expression. Eight of 13 patients with known expression saw their tumor burden decrease with treatment to below baseline.
Encouraged by the results, the investigators believe further investigation of the combination is in order, as the combination, with limited follow-up, achieved a high and durable ORR in HL patients, including those who were transplant-naïve.