User login
Brentuximab vedotin approved in Japan

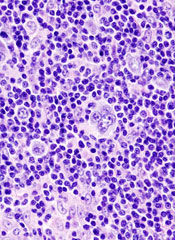
Credit: Linda Bartlett
The Japanese Ministry of Health, Labour and Welfare has approved brentuximab vedotin (Adcetris) for the treatment of patients with relapsed or refractory, CD30+ Hodgkin lymphoma (HL) or anaplastic large-cell lymphoma (ALCL).
The approval was based on a phase 1/2 trial in Japanese patients with relapsed or refractory, CD30+ HL or systemic ALCL, as well as data from two phase 2 trials—one of 102 HL patients and one of 58 patients with ALCL.
Brentuximab vedotin is an antibody-drug conjugate consisting of an anti-CD30 monoclonal antibody attached by a protease-cleavable linker to a microtubule disrupting agent, monomethyl auristatin E.
The conjugate employs a linker system designed to be stable in the bloodstream but release monomethyl auristatin E upon internalization into CD30-expressing tumor cells.
Brentuximab vedotin was approved by the US Food and Drug Administration (FDA) in August 2011 and gained conditional approval from Health Canada in February 2013 for the following indications:
- To treat HL patients who had failed autologous stem cell transplant (auto-SCT) or were not eligible for auto-SCT and had failed at least 2 prior multi-agent chemotherapy regimens
- To treat patients with systemic ALCL after they failed at least 1 multi-agent chemotherapy regimen.
The drug received conditional marketing authorization by the European Commission in October 2012 to treat:
- Adult patients with relapsed or refractory, systemic ALCL
- Adults with relapsed or refractory, CD30-positive HL who had undergone auto-SCT or received 2 prior therapies when auto-SCT or multi-agent chemotherapy were not appropriate.
The FDA has granted brentuximab vedotin orphan designation to treat mycosis fungoides. And trials have suggested the drug is active in diffuse large B-cell lymphoma, as well as leukemias and multiple myeloma.
However, brentuximab vedotin also made the FDA watch list due to adverse events associated with the drug’s use. The FDA added a boxed warning to the drug’s label in January 2012, after 3 cases of progressive multifocal leukoencephalopathy were reported in patients receiving brentuximab vedotin. ![]()

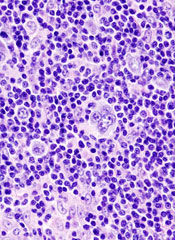
Credit: Linda Bartlett
The Japanese Ministry of Health, Labour and Welfare has approved brentuximab vedotin (Adcetris) for the treatment of patients with relapsed or refractory, CD30+ Hodgkin lymphoma (HL) or anaplastic large-cell lymphoma (ALCL).
The approval was based on a phase 1/2 trial in Japanese patients with relapsed or refractory, CD30+ HL or systemic ALCL, as well as data from two phase 2 trials—one of 102 HL patients and one of 58 patients with ALCL.
Brentuximab vedotin is an antibody-drug conjugate consisting of an anti-CD30 monoclonal antibody attached by a protease-cleavable linker to a microtubule disrupting agent, monomethyl auristatin E.
The conjugate employs a linker system designed to be stable in the bloodstream but release monomethyl auristatin E upon internalization into CD30-expressing tumor cells.
Brentuximab vedotin was approved by the US Food and Drug Administration (FDA) in August 2011 and gained conditional approval from Health Canada in February 2013 for the following indications:
- To treat HL patients who had failed autologous stem cell transplant (auto-SCT) or were not eligible for auto-SCT and had failed at least 2 prior multi-agent chemotherapy regimens
- To treat patients with systemic ALCL after they failed at least 1 multi-agent chemotherapy regimen.
The drug received conditional marketing authorization by the European Commission in October 2012 to treat:
- Adult patients with relapsed or refractory, systemic ALCL
- Adults with relapsed or refractory, CD30-positive HL who had undergone auto-SCT or received 2 prior therapies when auto-SCT or multi-agent chemotherapy were not appropriate.
The FDA has granted brentuximab vedotin orphan designation to treat mycosis fungoides. And trials have suggested the drug is active in diffuse large B-cell lymphoma, as well as leukemias and multiple myeloma.
However, brentuximab vedotin also made the FDA watch list due to adverse events associated with the drug’s use. The FDA added a boxed warning to the drug’s label in January 2012, after 3 cases of progressive multifocal leukoencephalopathy were reported in patients receiving brentuximab vedotin. ![]()

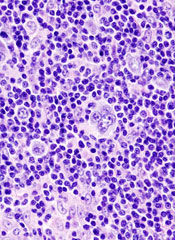
Credit: Linda Bartlett
The Japanese Ministry of Health, Labour and Welfare has approved brentuximab vedotin (Adcetris) for the treatment of patients with relapsed or refractory, CD30+ Hodgkin lymphoma (HL) or anaplastic large-cell lymphoma (ALCL).
The approval was based on a phase 1/2 trial in Japanese patients with relapsed or refractory, CD30+ HL or systemic ALCL, as well as data from two phase 2 trials—one of 102 HL patients and one of 58 patients with ALCL.
Brentuximab vedotin is an antibody-drug conjugate consisting of an anti-CD30 monoclonal antibody attached by a protease-cleavable linker to a microtubule disrupting agent, monomethyl auristatin E.
The conjugate employs a linker system designed to be stable in the bloodstream but release monomethyl auristatin E upon internalization into CD30-expressing tumor cells.
Brentuximab vedotin was approved by the US Food and Drug Administration (FDA) in August 2011 and gained conditional approval from Health Canada in February 2013 for the following indications:
- To treat HL patients who had failed autologous stem cell transplant (auto-SCT) or were not eligible for auto-SCT and had failed at least 2 prior multi-agent chemotherapy regimens
- To treat patients with systemic ALCL after they failed at least 1 multi-agent chemotherapy regimen.
The drug received conditional marketing authorization by the European Commission in October 2012 to treat:
- Adult patients with relapsed or refractory, systemic ALCL
- Adults with relapsed or refractory, CD30-positive HL who had undergone auto-SCT or received 2 prior therapies when auto-SCT or multi-agent chemotherapy were not appropriate.
The FDA has granted brentuximab vedotin orphan designation to treat mycosis fungoides. And trials have suggested the drug is active in diffuse large B-cell lymphoma, as well as leukemias and multiple myeloma.
However, brentuximab vedotin also made the FDA watch list due to adverse events associated with the drug’s use. The FDA added a boxed warning to the drug’s label in January 2012, after 3 cases of progressive multifocal leukoencephalopathy were reported in patients receiving brentuximab vedotin. ![]()
VIDEO: Idelalisib shows promise in refractory non-Hodgkin lymphoma
NEW ORLEANS – When indolent B-cell non-Hodgkin lymphoma becomes refractory to rituximab and alkylating agents, few therapeutic options remain. But the PI3kd inhibitor idelalisib may someday offer a new treatment choice. Dr. Ajay Gopal discusses the promising findings from a phase II trial of idelalisib, including a 57% response rate.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – When indolent B-cell non-Hodgkin lymphoma becomes refractory to rituximab and alkylating agents, few therapeutic options remain. But the PI3kd inhibitor idelalisib may someday offer a new treatment choice. Dr. Ajay Gopal discusses the promising findings from a phase II trial of idelalisib, including a 57% response rate.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – When indolent B-cell non-Hodgkin lymphoma becomes refractory to rituximab and alkylating agents, few therapeutic options remain. But the PI3kd inhibitor idelalisib may someday offer a new treatment choice. Dr. Ajay Gopal discusses the promising findings from a phase II trial of idelalisib, including a 57% response rate.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
No survival benefit for routine surveillance scans in classical Hodgkin disease
CHICAGO – Routine surveillance imaging does not improve clinical outcomes in patients with classic Hodgkin disease who are in first complete remission and it sharply increases costs, researchers reported at the annual meeting of the American Society of Clinical Oncology.
The team, led by Dr. Sai Ravi Pingali, retrospectively reviewed the charts of 241 adult patients who achieved a complete remission after first-line therapy.
In 68%, the treating physicians’ planned approach was routine surveillance imaging, which consisted of radiologic imaging with scans every few months, plus clinical exams and laboratory testing. In the other 32%, the planned approach was clinical surveillance, meaning that radiologic imaging was performed only if concerning signs or symptoms occurred.
The two groups had statistically indistinguishable overall survival, and in both groups, all patients experiencing relapse successfully achieved a second complete remission with salvage therapy.
In the routinely imaged group, scanning increased costs by nearly $20,000 per patient and by almost $600,000 per each relapse detected. In addition, patients were exposed to the associated radiation.
"We were unable to detect an overall survival benefit associated with routine surveillance imaging, although I have to acknowledge that our study was limited in power given the small number of deaths and relapses," commented Dr. Pingali, an oncologist with the Medical College of Wisconsin Affiliated Hospitals in Milwaukee.
"Relapses in both ... groups were effectively salvaged with autologous stem cell transplantation, arguing against a critical advantage of detection of asymptomatic relapse. Also, we need to keep in mind that the costs associated with routine surveillance imaging are significant, and it is also associated with potential risks, both in terms of radiation exposure and unnecessary work-up," he added.
"We do not feel that potential risks and costs without overall survival benefit or any other clinical benefit justify the practice of routine surveillance imaging in classical Hodgkin lymphoma patients who have achieved a complete remission after first-line therapy. We recommend that such patients be followed clinically," Dr. Pingali concluded.
Invited discussant Dr. Leo Gordon of Northwestern University in Chicago, agreed that accumulating data argue against routine imaging for surveillance in this context and noted that insurers will likely not continue to cover scans having no proven benefit. The data should prompt a revision of guidelines and reeducation of clinicians and patients, he said.
"For translational researchers and investigators and academics, I think we need to convince journal reviewers that a manuscript is acceptable if scans are not so frequent. And for industry trials, I think we need to discuss with the Food and Drug Administration the endpoint of progression-free survival and that those endpoints may not only be driven by scans but by more mundane parameters," he said—namely, the history and physical examination.
But session comoderator Dr. Gilles A. Salles of Hospices Civils de Lyon, Université Claude Bernard, France, expressed reservations, noting that the study did not provide information on how patients were allocated to groups and the time frame of relapse.
"It may be different whether relapses occur early, in the first year, or they occur later, and that may have some implications for the surveillance," he said. "I understand that you and many others jumped over the idea that we should immediately stop. A few people may think that we need more solid data, despite the provocative and quality data that were presented, to really make this jump in clinical practice. That’s my personal opinion."
Dr. Pingali and his team retrospectively reviewed the charts of adult patients who received a new diagnosis of classical Hodgkin lymphoma between 2000 and 2010 at three institutions, achieved complete remission after first-line therapy and had at least 2 years of follow-up.
The routine surveillance imaging and clinical surveillance groups had similar demographic and disease characteristics, Dr. Pingali reported. The former were significantly more likely to have received ABVD (doxorubicin [Adriamycin], bleomycin, vinblastine, and dacarbazine) and less likely to have received the Stanford V regimen as first-line therapy, and they were significantly less likely to have received radiation therapy.
With a median duration of follow-up of about 4 years, the groups did not differ significantly with respect to overall survival. "When we look at the 5-year time point, when typically the surveillance CT scans are discontinued, the curves are pretty much superimposable," he pointed out.
There were five deaths in the routine surveillance imaging group, one of which was from relapsed disease; the other deaths were from cancer, heart failure, hip fracture, and myelodysplastic syndrome. There were four deaths in the clinical surveillance group: two were from non-Hodgkin lymphoma and two from unknown causes while the patient was in confirmed remission.
All of the six patients in the routinely imaged group and all of the five patients in the clinically followed group experiencing a relapse achieved another complete remission with second-line therapy.
The mean number of scans received was 1.14 in the clinical surveillance group – usually the scan performed after first-line treatment to confirm remission, according to Dr. Pingali – and 4.25 in the routine surveillance imaging group. The ratio of scans to detected relapses was 18 vs. 124.
The extra charges incurred from scans using the routine surveillance imaging approach were $18,896/patient and $593,698/relapse.
"It is important to note that this does not include additional costs from the work-up of the false-positive scans and also the wages lost," he noted.
Dr. Pingali disclosed no relevant conflicts of interest. Dr. Gordon disclosed that he receives honoraria from Genentech and research funding from Millennium and Pharmacyclics. Dr. Salles disclosed serving as an advisor or consultant for Calistoga Pharmaceuticals, Celgene; Genentech, Janssen Pharmaceutica, and Roche. He has served as a speaker or a member of a speakers bureau and has received grants for clinical research from Celgene and Roche.
CHICAGO – Routine surveillance imaging does not improve clinical outcomes in patients with classic Hodgkin disease who are in first complete remission and it sharply increases costs, researchers reported at the annual meeting of the American Society of Clinical Oncology.
The team, led by Dr. Sai Ravi Pingali, retrospectively reviewed the charts of 241 adult patients who achieved a complete remission after first-line therapy.
In 68%, the treating physicians’ planned approach was routine surveillance imaging, which consisted of radiologic imaging with scans every few months, plus clinical exams and laboratory testing. In the other 32%, the planned approach was clinical surveillance, meaning that radiologic imaging was performed only if concerning signs or symptoms occurred.
The two groups had statistically indistinguishable overall survival, and in both groups, all patients experiencing relapse successfully achieved a second complete remission with salvage therapy.
In the routinely imaged group, scanning increased costs by nearly $20,000 per patient and by almost $600,000 per each relapse detected. In addition, patients were exposed to the associated radiation.
"We were unable to detect an overall survival benefit associated with routine surveillance imaging, although I have to acknowledge that our study was limited in power given the small number of deaths and relapses," commented Dr. Pingali, an oncologist with the Medical College of Wisconsin Affiliated Hospitals in Milwaukee.
"Relapses in both ... groups were effectively salvaged with autologous stem cell transplantation, arguing against a critical advantage of detection of asymptomatic relapse. Also, we need to keep in mind that the costs associated with routine surveillance imaging are significant, and it is also associated with potential risks, both in terms of radiation exposure and unnecessary work-up," he added.
"We do not feel that potential risks and costs without overall survival benefit or any other clinical benefit justify the practice of routine surveillance imaging in classical Hodgkin lymphoma patients who have achieved a complete remission after first-line therapy. We recommend that such patients be followed clinically," Dr. Pingali concluded.
Invited discussant Dr. Leo Gordon of Northwestern University in Chicago, agreed that accumulating data argue against routine imaging for surveillance in this context and noted that insurers will likely not continue to cover scans having no proven benefit. The data should prompt a revision of guidelines and reeducation of clinicians and patients, he said.
"For translational researchers and investigators and academics, I think we need to convince journal reviewers that a manuscript is acceptable if scans are not so frequent. And for industry trials, I think we need to discuss with the Food and Drug Administration the endpoint of progression-free survival and that those endpoints may not only be driven by scans but by more mundane parameters," he said—namely, the history and physical examination.
But session comoderator Dr. Gilles A. Salles of Hospices Civils de Lyon, Université Claude Bernard, France, expressed reservations, noting that the study did not provide information on how patients were allocated to groups and the time frame of relapse.
"It may be different whether relapses occur early, in the first year, or they occur later, and that may have some implications for the surveillance," he said. "I understand that you and many others jumped over the idea that we should immediately stop. A few people may think that we need more solid data, despite the provocative and quality data that were presented, to really make this jump in clinical practice. That’s my personal opinion."
Dr. Pingali and his team retrospectively reviewed the charts of adult patients who received a new diagnosis of classical Hodgkin lymphoma between 2000 and 2010 at three institutions, achieved complete remission after first-line therapy and had at least 2 years of follow-up.
The routine surveillance imaging and clinical surveillance groups had similar demographic and disease characteristics, Dr. Pingali reported. The former were significantly more likely to have received ABVD (doxorubicin [Adriamycin], bleomycin, vinblastine, and dacarbazine) and less likely to have received the Stanford V regimen as first-line therapy, and they were significantly less likely to have received radiation therapy.
With a median duration of follow-up of about 4 years, the groups did not differ significantly with respect to overall survival. "When we look at the 5-year time point, when typically the surveillance CT scans are discontinued, the curves are pretty much superimposable," he pointed out.
There were five deaths in the routine surveillance imaging group, one of which was from relapsed disease; the other deaths were from cancer, heart failure, hip fracture, and myelodysplastic syndrome. There were four deaths in the clinical surveillance group: two were from non-Hodgkin lymphoma and two from unknown causes while the patient was in confirmed remission.
All of the six patients in the routinely imaged group and all of the five patients in the clinically followed group experiencing a relapse achieved another complete remission with second-line therapy.
The mean number of scans received was 1.14 in the clinical surveillance group – usually the scan performed after first-line treatment to confirm remission, according to Dr. Pingali – and 4.25 in the routine surveillance imaging group. The ratio of scans to detected relapses was 18 vs. 124.
The extra charges incurred from scans using the routine surveillance imaging approach were $18,896/patient and $593,698/relapse.
"It is important to note that this does not include additional costs from the work-up of the false-positive scans and also the wages lost," he noted.
Dr. Pingali disclosed no relevant conflicts of interest. Dr. Gordon disclosed that he receives honoraria from Genentech and research funding from Millennium and Pharmacyclics. Dr. Salles disclosed serving as an advisor or consultant for Calistoga Pharmaceuticals, Celgene; Genentech, Janssen Pharmaceutica, and Roche. He has served as a speaker or a member of a speakers bureau and has received grants for clinical research from Celgene and Roche.
CHICAGO – Routine surveillance imaging does not improve clinical outcomes in patients with classic Hodgkin disease who are in first complete remission and it sharply increases costs, researchers reported at the annual meeting of the American Society of Clinical Oncology.
The team, led by Dr. Sai Ravi Pingali, retrospectively reviewed the charts of 241 adult patients who achieved a complete remission after first-line therapy.
In 68%, the treating physicians’ planned approach was routine surveillance imaging, which consisted of radiologic imaging with scans every few months, plus clinical exams and laboratory testing. In the other 32%, the planned approach was clinical surveillance, meaning that radiologic imaging was performed only if concerning signs or symptoms occurred.
The two groups had statistically indistinguishable overall survival, and in both groups, all patients experiencing relapse successfully achieved a second complete remission with salvage therapy.
In the routinely imaged group, scanning increased costs by nearly $20,000 per patient and by almost $600,000 per each relapse detected. In addition, patients were exposed to the associated radiation.
"We were unable to detect an overall survival benefit associated with routine surveillance imaging, although I have to acknowledge that our study was limited in power given the small number of deaths and relapses," commented Dr. Pingali, an oncologist with the Medical College of Wisconsin Affiliated Hospitals in Milwaukee.
"Relapses in both ... groups were effectively salvaged with autologous stem cell transplantation, arguing against a critical advantage of detection of asymptomatic relapse. Also, we need to keep in mind that the costs associated with routine surveillance imaging are significant, and it is also associated with potential risks, both in terms of radiation exposure and unnecessary work-up," he added.
"We do not feel that potential risks and costs without overall survival benefit or any other clinical benefit justify the practice of routine surveillance imaging in classical Hodgkin lymphoma patients who have achieved a complete remission after first-line therapy. We recommend that such patients be followed clinically," Dr. Pingali concluded.
Invited discussant Dr. Leo Gordon of Northwestern University in Chicago, agreed that accumulating data argue against routine imaging for surveillance in this context and noted that insurers will likely not continue to cover scans having no proven benefit. The data should prompt a revision of guidelines and reeducation of clinicians and patients, he said.
"For translational researchers and investigators and academics, I think we need to convince journal reviewers that a manuscript is acceptable if scans are not so frequent. And for industry trials, I think we need to discuss with the Food and Drug Administration the endpoint of progression-free survival and that those endpoints may not only be driven by scans but by more mundane parameters," he said—namely, the history and physical examination.
But session comoderator Dr. Gilles A. Salles of Hospices Civils de Lyon, Université Claude Bernard, France, expressed reservations, noting that the study did not provide information on how patients were allocated to groups and the time frame of relapse.
"It may be different whether relapses occur early, in the first year, or they occur later, and that may have some implications for the surveillance," he said. "I understand that you and many others jumped over the idea that we should immediately stop. A few people may think that we need more solid data, despite the provocative and quality data that were presented, to really make this jump in clinical practice. That’s my personal opinion."
Dr. Pingali and his team retrospectively reviewed the charts of adult patients who received a new diagnosis of classical Hodgkin lymphoma between 2000 and 2010 at three institutions, achieved complete remission after first-line therapy and had at least 2 years of follow-up.
The routine surveillance imaging and clinical surveillance groups had similar demographic and disease characteristics, Dr. Pingali reported. The former were significantly more likely to have received ABVD (doxorubicin [Adriamycin], bleomycin, vinblastine, and dacarbazine) and less likely to have received the Stanford V regimen as first-line therapy, and they were significantly less likely to have received radiation therapy.
With a median duration of follow-up of about 4 years, the groups did not differ significantly with respect to overall survival. "When we look at the 5-year time point, when typically the surveillance CT scans are discontinued, the curves are pretty much superimposable," he pointed out.
There were five deaths in the routine surveillance imaging group, one of which was from relapsed disease; the other deaths were from cancer, heart failure, hip fracture, and myelodysplastic syndrome. There were four deaths in the clinical surveillance group: two were from non-Hodgkin lymphoma and two from unknown causes while the patient was in confirmed remission.
All of the six patients in the routinely imaged group and all of the five patients in the clinically followed group experiencing a relapse achieved another complete remission with second-line therapy.
The mean number of scans received was 1.14 in the clinical surveillance group – usually the scan performed after first-line treatment to confirm remission, according to Dr. Pingali – and 4.25 in the routine surveillance imaging group. The ratio of scans to detected relapses was 18 vs. 124.
The extra charges incurred from scans using the routine surveillance imaging approach were $18,896/patient and $593,698/relapse.
"It is important to note that this does not include additional costs from the work-up of the false-positive scans and also the wages lost," he noted.
Dr. Pingali disclosed no relevant conflicts of interest. Dr. Gordon disclosed that he receives honoraria from Genentech and research funding from Millennium and Pharmacyclics. Dr. Salles disclosed serving as an advisor or consultant for Calistoga Pharmaceuticals, Celgene; Genentech, Janssen Pharmaceutica, and Roche. He has served as a speaker or a member of a speakers bureau and has received grants for clinical research from Celgene and Roche.
AT THE ASCO ANNUAL MEETING 2013
Major finding: The ratio of scans to detected relapses was 18 for the clinical surveillance group and 124 for the routine scan group. The extra charges incurred from scans using the routine surveillance imaging approach were $18,896/patient and $593,698/relapse.
Data source: A retrospective analysis of 241 patients with classical Hodgkin lymphoma in first complete remission
Disclosures: Dr. Pingali disclosed no relevant conflicts of interest. Dr. Gordon disclosed that he receives honoraria from Genentech and research funding from Millennium and Pharmacyclics. Dr. Salles disclosed serving as an advisor or consultant for Calistoga Pharmaceuticals, Celgene; Genentech, Janssen Pharmaceutica, and Roche. He has served as a speaker or a member of a speakers bureau and has received grants for clinical research from Celgene and Roche.
Panobinostat shows promise in refractory Hodgkin lymphoma
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
