User login
AI will change the practice of medicine
Remembering the importance of caring
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
Remembering the importance of caring
Remembering the importance of caring
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
As artificial intelligence (AI) takes on more and more tasks in medical care that mimic human cognition, hospitalists and other physicians will need to adapt to a changing role.
Today AI can identify tuberculosis infections in chest radiographs with almost complete accuracy, diagnose melanoma from images of skin lesions more accurately than dermatologists can, and identify metastatic cells in images of lymph node tissue more accurately than pathologists can. The next 20 years are likely to see further acceleration in the capabilities, according to a recent article by S. Claiborne Johnston, MD, PhD.
“AI will change the practice of medicine. The art of medicine, including all the humanistic components, will only become more important over time. As dean of a medical school, I’m training students who will be practicing in 2065,” Dr. Johnston said. “If I’m not thinking about the future, I’m failing my students and the society they will serve.”
The contributions of AI will shift the emphasis for human caregivers to the caring. Studies have shown that the skills of caring are associated with improved patient outcomes, but most medical schools allocate substantial time in the curriculum to memorization and analysis – tasks that will become less demanding as artificial intelligence improves. The art of caring – communication, empathy, shared decision making, leadership, and team building – is usually a minor part of the medical school curriculum.
Effective leadership and creativity are distant aspirations for artificial intelligence but are growing needs in a system of care that is ever more complex.
At Dr. Johnston’s school, the Dell Medical School at the University of Texas at Austin, they have reduced the duration of basic science instruction to 12 months and emphasized group problem solving, while deemphasizing memorization. This has freed up additional time for instruction in the art of caring, leadership, and creativity.
“Hospitalists should acknowledge the value of caring,” Dr. Johnston said. “They do it every day with every patient. It is important today, and will be more important tomorrow.”
Reference
Johnston SC. Anticipating and training the physician of the future: The importance of caring in an age of artificial intelligence. Acad Med. 2018;93(8):1105-6. doi: 10.1097/ACM.0000000000002175.
The past and future of hospital medicine
Challenges faced, and overcome
While I hope I’ll still be doing much the same work for many more years, I’m clearly at a stage of life that most of my career is behind me. So I guess it’s natural that I think about the past a little more than I used to. And one of the things that makes me smile is how I’m like George Costanza in The Comeback episode of “Seinfeld.”
In 1997 I had just delivered a presentation about what the future might hold for hospitalists to the roughly 110 attendees at the first in-person meeting of SHM (then known as the National Association of Inpatient Physicians). During the Q&A that followed, someone asked me what clinical content I would include in the hospitalist-specific test or board exam that I had speculated might be in our future. I took his tone and body language to suggest his main intent was to convey that I was crazy to think that such a test might ever be worthwhile.
A pregnant silence followed his question, after which I gave a tentative response that I worried made me sound dumb. So like George in “Seinfeld,” I continued to think about this, and days later came up with what I’m sure would have been a terrific comeback that would have gotten a robust laugh from the audience without being demeaning to the questioner. For the last 22 years I’ve been waiting for someone to ask me the same question so I can finally deliver my winner of a response.
There have been other missed opportunities, but when I think about the past and future of our field and our Society, I’m reminded of many past accomplishments and a promising future.
When Dr. Win Whitcomb and I founded SHM, I had the idea that, among its most important roles, would be serving as a forum for exchange of ideas among hospitalists and providing robust practice management resources for hospitalist groups. Through the efforts of so many people, including Angela Musial, the first SHM staff person, and so many other staff and members, we now have dozens of active special interest groups, informative publications, an active online discussion forum, and blogs. And our annual conference has grown a lot from that first meeting of 110 people; HM19 will bring together nearly 5,000 of us to educate, inspire, and support one another. Collectively, there are a lot of ideas being exchanged through SHM.
When SHM was brand new I had hope that it would grow. But I never guessed that hospital medicine would become the fastest-growing field in the history of U.S. health care.
I also never guessed that the term “nocturnist” would become a standard part of our field’s lexicon. I used it solely as a reliable way to get a laugh and find it really funny and delightful that it caught on.
And OB hospitalists? Neurohospitalists? I never saw these and the many other variations coming at all. But I see it as validating an idea first adopted by medicine and pediatrics. But dermatology hospitalists? Yep, that’s a thing too. The hospitalist model has been adopted, in at least a few places, by nearly every specialty in medicine.
And it is terrific that March 7, 2019, is the first National Hospitalist Day. SHM made this happen too.
I also think about the future of our field and see some pretty big challenges, though our past success as a field makes me confident we’ll navigate them effectively.
The burden of administrative, regulatory, and EHR-related tasks just keeps growing for hospitalists. This often means it is difficult or impossible see as many patients in a day as might have been reasonable in the past. In the near term, the only solution might be to reduce patient loads, but that isn’t a sustainable solution in the long term. I’m convinced we need to offload much of the work we do today that isn’t purely clinical, so that a typical hospitalist in the future can see more patients each day without working harder or longer.
I imagine a future in which the typical hospitalist goes home after seeing 20 or more patients in a day and isn’t completely exhausted and stressed, but sees it as a good day at work. I’m not sure exactly how we’ll get there, but it will probably include things like no longer having to devote any time or attention to whether the patient is inpatient or observation status, or whether they have had a qualifying 3-midnight stay so Medicare will cover a skilled nursing facility. I’m excited to see how this will evolve.
Dr. Nelson is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
Challenges faced, and overcome
Challenges faced, and overcome
While I hope I’ll still be doing much the same work for many more years, I’m clearly at a stage of life that most of my career is behind me. So I guess it’s natural that I think about the past a little more than I used to. And one of the things that makes me smile is how I’m like George Costanza in The Comeback episode of “Seinfeld.”
In 1997 I had just delivered a presentation about what the future might hold for hospitalists to the roughly 110 attendees at the first in-person meeting of SHM (then known as the National Association of Inpatient Physicians). During the Q&A that followed, someone asked me what clinical content I would include in the hospitalist-specific test or board exam that I had speculated might be in our future. I took his tone and body language to suggest his main intent was to convey that I was crazy to think that such a test might ever be worthwhile.
A pregnant silence followed his question, after which I gave a tentative response that I worried made me sound dumb. So like George in “Seinfeld,” I continued to think about this, and days later came up with what I’m sure would have been a terrific comeback that would have gotten a robust laugh from the audience without being demeaning to the questioner. For the last 22 years I’ve been waiting for someone to ask me the same question so I can finally deliver my winner of a response.
There have been other missed opportunities, but when I think about the past and future of our field and our Society, I’m reminded of many past accomplishments and a promising future.
When Dr. Win Whitcomb and I founded SHM, I had the idea that, among its most important roles, would be serving as a forum for exchange of ideas among hospitalists and providing robust practice management resources for hospitalist groups. Through the efforts of so many people, including Angela Musial, the first SHM staff person, and so many other staff and members, we now have dozens of active special interest groups, informative publications, an active online discussion forum, and blogs. And our annual conference has grown a lot from that first meeting of 110 people; HM19 will bring together nearly 5,000 of us to educate, inspire, and support one another. Collectively, there are a lot of ideas being exchanged through SHM.
When SHM was brand new I had hope that it would grow. But I never guessed that hospital medicine would become the fastest-growing field in the history of U.S. health care.
I also never guessed that the term “nocturnist” would become a standard part of our field’s lexicon. I used it solely as a reliable way to get a laugh and find it really funny and delightful that it caught on.
And OB hospitalists? Neurohospitalists? I never saw these and the many other variations coming at all. But I see it as validating an idea first adopted by medicine and pediatrics. But dermatology hospitalists? Yep, that’s a thing too. The hospitalist model has been adopted, in at least a few places, by nearly every specialty in medicine.
And it is terrific that March 7, 2019, is the first National Hospitalist Day. SHM made this happen too.
I also think about the future of our field and see some pretty big challenges, though our past success as a field makes me confident we’ll navigate them effectively.
The burden of administrative, regulatory, and EHR-related tasks just keeps growing for hospitalists. This often means it is difficult or impossible see as many patients in a day as might have been reasonable in the past. In the near term, the only solution might be to reduce patient loads, but that isn’t a sustainable solution in the long term. I’m convinced we need to offload much of the work we do today that isn’t purely clinical, so that a typical hospitalist in the future can see more patients each day without working harder or longer.
I imagine a future in which the typical hospitalist goes home after seeing 20 or more patients in a day and isn’t completely exhausted and stressed, but sees it as a good day at work. I’m not sure exactly how we’ll get there, but it will probably include things like no longer having to devote any time or attention to whether the patient is inpatient or observation status, or whether they have had a qualifying 3-midnight stay so Medicare will cover a skilled nursing facility. I’m excited to see how this will evolve.
Dr. Nelson is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
While I hope I’ll still be doing much the same work for many more years, I’m clearly at a stage of life that most of my career is behind me. So I guess it’s natural that I think about the past a little more than I used to. And one of the things that makes me smile is how I’m like George Costanza in The Comeback episode of “Seinfeld.”
In 1997 I had just delivered a presentation about what the future might hold for hospitalists to the roughly 110 attendees at the first in-person meeting of SHM (then known as the National Association of Inpatient Physicians). During the Q&A that followed, someone asked me what clinical content I would include in the hospitalist-specific test or board exam that I had speculated might be in our future. I took his tone and body language to suggest his main intent was to convey that I was crazy to think that such a test might ever be worthwhile.
A pregnant silence followed his question, after which I gave a tentative response that I worried made me sound dumb. So like George in “Seinfeld,” I continued to think about this, and days later came up with what I’m sure would have been a terrific comeback that would have gotten a robust laugh from the audience without being demeaning to the questioner. For the last 22 years I’ve been waiting for someone to ask me the same question so I can finally deliver my winner of a response.
There have been other missed opportunities, but when I think about the past and future of our field and our Society, I’m reminded of many past accomplishments and a promising future.
When Dr. Win Whitcomb and I founded SHM, I had the idea that, among its most important roles, would be serving as a forum for exchange of ideas among hospitalists and providing robust practice management resources for hospitalist groups. Through the efforts of so many people, including Angela Musial, the first SHM staff person, and so many other staff and members, we now have dozens of active special interest groups, informative publications, an active online discussion forum, and blogs. And our annual conference has grown a lot from that first meeting of 110 people; HM19 will bring together nearly 5,000 of us to educate, inspire, and support one another. Collectively, there are a lot of ideas being exchanged through SHM.
When SHM was brand new I had hope that it would grow. But I never guessed that hospital medicine would become the fastest-growing field in the history of U.S. health care.
I also never guessed that the term “nocturnist” would become a standard part of our field’s lexicon. I used it solely as a reliable way to get a laugh and find it really funny and delightful that it caught on.
And OB hospitalists? Neurohospitalists? I never saw these and the many other variations coming at all. But I see it as validating an idea first adopted by medicine and pediatrics. But dermatology hospitalists? Yep, that’s a thing too. The hospitalist model has been adopted, in at least a few places, by nearly every specialty in medicine.
And it is terrific that March 7, 2019, is the first National Hospitalist Day. SHM made this happen too.
I also think about the future of our field and see some pretty big challenges, though our past success as a field makes me confident we’ll navigate them effectively.
The burden of administrative, regulatory, and EHR-related tasks just keeps growing for hospitalists. This often means it is difficult or impossible see as many patients in a day as might have been reasonable in the past. In the near term, the only solution might be to reduce patient loads, but that isn’t a sustainable solution in the long term. I’m convinced we need to offload much of the work we do today that isn’t purely clinical, so that a typical hospitalist in the future can see more patients each day without working harder or longer.
I imagine a future in which the typical hospitalist goes home after seeing 20 or more patients in a day and isn’t completely exhausted and stressed, but sees it as a good day at work. I’m not sure exactly how we’ll get there, but it will probably include things like no longer having to devote any time or attention to whether the patient is inpatient or observation status, or whether they have had a qualifying 3-midnight stay so Medicare will cover a skilled nursing facility. I’m excited to see how this will evolve.
Dr. Nelson is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
The power of policy at HM19
Mini-track features CMS insights
Due to the steadily growing interest of SHM members in health care policy and advocacy issues, the 2019 Annual Conference will include a mini-track dedicated to policy issues.
To be held on Monday, March 25th at HM19 in Orlando, the health care policy mini-track will update conference attendees on some of the Washington developments that affect hospitalists, said Josh Boswell, director of government relations at SHM.
“Many of the policy developments in D.C. are directly impacting our members’ practices,” he said. “A couple of years ago, it was decided to add a specific track at the annual conference to cover some of these policy issues, and we’ve generally had positive feedback on the sessions.”
This year, the mini-track will consist of two separate sessions, held back to back. “Both sessions are designed to give attendees an entrée into health policy and explain developments that are happening right now in Washington that impact their practice,” said Joshua Lapps, government relations manager at SHM.
The first session – “CMS Policy Update: An Overview of Meaningful Measures and the Quality Payment Program” – will take place from 2:00 to 3:30 p.m., and will feature Reena Duseja, MD, MS, the acting director for Quality Measurement and Value-Based Incentives Group in the Centers for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services. Dr. Duseja oversees the development of measures and analyses for a variety of CMS quality reporting and value-based purchasing programs. She is also an emergency medicine physician and was an associate professor at the University of California, San Francisco, in the department of emergency medicine, where she led quality improvement activities.
“The session with Dr. Duseja will be an inside look into the approach that CMS is taking for quality measurement and pay-for-performance programs, specifically looking at the quality payment program which came out of the Medicare Access and Chip Reauthorization Act,” Mr. Lapps said. “It will be a high-level discussion about how the programs affect hospitalists, and how hospitalists participate in the programs. It’s also a chance for attendees to hear some of the thinking inside CMS.”
Dr. Duseja is also hoping to get feedback from HM19 attendees. “She wants the session to be educational for our members, as well as an opportunity for her to learn from hospitalists,” Mr. Lapps said.
According to Dr. Duseja, her presentation will provide attendees with an overview of the Quality Payment Program under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), specifically highlighting policy changes from 2018 to 2019 to the Merit-based Incentive Payment System (MIPS) and Meaningful Measures Initiative. Attendees will learn more about CMS’s approach to quality and quality measurement, as well as the future of quality reporting programs.
Following Dr. Duseja’s presentation, the second mini-track session will take place from 3:40 to 4:25 p.m. It will focus more intently on the processes around health care policy making.
“We heard from our members who attended this mini-track at the past two annual conferences that they would like us to explain how policy making works: the play-by-play in D.C. on how we get to where we are,” Mr. Boswell said.
The second session will feature a presentation by Jennifer Bell, founding partner at Chamber Hill Strategies, who represents SHM in Washington. “Jennifer will be discussing how Washington works, the policy process and the pressure points at which SHM and its members can exert influence,” Mr. Lapps said.
Attendees can expect to learn a lot from either session, Mr. Lapps said. “Attendees will learn about the basic contours of the Quality Payment Program that Medicare oversees, and some of the specific new elements of that program this year that were designed with hospitalists in mind. For example, Dr. Duseja will be talking about a facility-based reporting option under the Merit-Based Incentive Payment System. I think our members should gain a concrete understanding of some of the new directions that CMS is heading this year. Overall, they’ll have a better sense of the vision behind quality measures and quality measurement. This is a really exciting opportunity to hear from someone who is both a clinician and works on policy at CMS.”
The policy mini-track offers hospitalists a chance to get a look “behind the curtain” at policy making from someone who is helping to write the rules.
“Attendees will gain insight on where they fit in these programs – and also have the opportunity to tell Dr. Duseja if they don’t feel these programs are a good fit for them,” Mr. Boswell said. “Oftentimes these programs are not structured ideally for hospitalists. So, hearing directly from hospitalists who are experiencing problems would be extraordinarily helpful to a CMS official. I think attendees should view the policy track not only as an opportunity to learn from CMS, but as an opportunity to educate CMS about our issues.”
Mini-track features CMS insights
Mini-track features CMS insights
Due to the steadily growing interest of SHM members in health care policy and advocacy issues, the 2019 Annual Conference will include a mini-track dedicated to policy issues.
To be held on Monday, March 25th at HM19 in Orlando, the health care policy mini-track will update conference attendees on some of the Washington developments that affect hospitalists, said Josh Boswell, director of government relations at SHM.
“Many of the policy developments in D.C. are directly impacting our members’ practices,” he said. “A couple of years ago, it was decided to add a specific track at the annual conference to cover some of these policy issues, and we’ve generally had positive feedback on the sessions.”
This year, the mini-track will consist of two separate sessions, held back to back. “Both sessions are designed to give attendees an entrée into health policy and explain developments that are happening right now in Washington that impact their practice,” said Joshua Lapps, government relations manager at SHM.
The first session – “CMS Policy Update: An Overview of Meaningful Measures and the Quality Payment Program” – will take place from 2:00 to 3:30 p.m., and will feature Reena Duseja, MD, MS, the acting director for Quality Measurement and Value-Based Incentives Group in the Centers for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services. Dr. Duseja oversees the development of measures and analyses for a variety of CMS quality reporting and value-based purchasing programs. She is also an emergency medicine physician and was an associate professor at the University of California, San Francisco, in the department of emergency medicine, where she led quality improvement activities.
“The session with Dr. Duseja will be an inside look into the approach that CMS is taking for quality measurement and pay-for-performance programs, specifically looking at the quality payment program which came out of the Medicare Access and Chip Reauthorization Act,” Mr. Lapps said. “It will be a high-level discussion about how the programs affect hospitalists, and how hospitalists participate in the programs. It’s also a chance for attendees to hear some of the thinking inside CMS.”
Dr. Duseja is also hoping to get feedback from HM19 attendees. “She wants the session to be educational for our members, as well as an opportunity for her to learn from hospitalists,” Mr. Lapps said.
According to Dr. Duseja, her presentation will provide attendees with an overview of the Quality Payment Program under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), specifically highlighting policy changes from 2018 to 2019 to the Merit-based Incentive Payment System (MIPS) and Meaningful Measures Initiative. Attendees will learn more about CMS’s approach to quality and quality measurement, as well as the future of quality reporting programs.
Following Dr. Duseja’s presentation, the second mini-track session will take place from 3:40 to 4:25 p.m. It will focus more intently on the processes around health care policy making.
“We heard from our members who attended this mini-track at the past two annual conferences that they would like us to explain how policy making works: the play-by-play in D.C. on how we get to where we are,” Mr. Boswell said.
The second session will feature a presentation by Jennifer Bell, founding partner at Chamber Hill Strategies, who represents SHM in Washington. “Jennifer will be discussing how Washington works, the policy process and the pressure points at which SHM and its members can exert influence,” Mr. Lapps said.
Attendees can expect to learn a lot from either session, Mr. Lapps said. “Attendees will learn about the basic contours of the Quality Payment Program that Medicare oversees, and some of the specific new elements of that program this year that were designed with hospitalists in mind. For example, Dr. Duseja will be talking about a facility-based reporting option under the Merit-Based Incentive Payment System. I think our members should gain a concrete understanding of some of the new directions that CMS is heading this year. Overall, they’ll have a better sense of the vision behind quality measures and quality measurement. This is a really exciting opportunity to hear from someone who is both a clinician and works on policy at CMS.”
The policy mini-track offers hospitalists a chance to get a look “behind the curtain” at policy making from someone who is helping to write the rules.
“Attendees will gain insight on where they fit in these programs – and also have the opportunity to tell Dr. Duseja if they don’t feel these programs are a good fit for them,” Mr. Boswell said. “Oftentimes these programs are not structured ideally for hospitalists. So, hearing directly from hospitalists who are experiencing problems would be extraordinarily helpful to a CMS official. I think attendees should view the policy track not only as an opportunity to learn from CMS, but as an opportunity to educate CMS about our issues.”
Due to the steadily growing interest of SHM members in health care policy and advocacy issues, the 2019 Annual Conference will include a mini-track dedicated to policy issues.
To be held on Monday, March 25th at HM19 in Orlando, the health care policy mini-track will update conference attendees on some of the Washington developments that affect hospitalists, said Josh Boswell, director of government relations at SHM.
“Many of the policy developments in D.C. are directly impacting our members’ practices,” he said. “A couple of years ago, it was decided to add a specific track at the annual conference to cover some of these policy issues, and we’ve generally had positive feedback on the sessions.”
This year, the mini-track will consist of two separate sessions, held back to back. “Both sessions are designed to give attendees an entrée into health policy and explain developments that are happening right now in Washington that impact their practice,” said Joshua Lapps, government relations manager at SHM.
The first session – “CMS Policy Update: An Overview of Meaningful Measures and the Quality Payment Program” – will take place from 2:00 to 3:30 p.m., and will feature Reena Duseja, MD, MS, the acting director for Quality Measurement and Value-Based Incentives Group in the Centers for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services. Dr. Duseja oversees the development of measures and analyses for a variety of CMS quality reporting and value-based purchasing programs. She is also an emergency medicine physician and was an associate professor at the University of California, San Francisco, in the department of emergency medicine, where she led quality improvement activities.
“The session with Dr. Duseja will be an inside look into the approach that CMS is taking for quality measurement and pay-for-performance programs, specifically looking at the quality payment program which came out of the Medicare Access and Chip Reauthorization Act,” Mr. Lapps said. “It will be a high-level discussion about how the programs affect hospitalists, and how hospitalists participate in the programs. It’s also a chance for attendees to hear some of the thinking inside CMS.”
Dr. Duseja is also hoping to get feedback from HM19 attendees. “She wants the session to be educational for our members, as well as an opportunity for her to learn from hospitalists,” Mr. Lapps said.
According to Dr. Duseja, her presentation will provide attendees with an overview of the Quality Payment Program under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), specifically highlighting policy changes from 2018 to 2019 to the Merit-based Incentive Payment System (MIPS) and Meaningful Measures Initiative. Attendees will learn more about CMS’s approach to quality and quality measurement, as well as the future of quality reporting programs.
Following Dr. Duseja’s presentation, the second mini-track session will take place from 3:40 to 4:25 p.m. It will focus more intently on the processes around health care policy making.
“We heard from our members who attended this mini-track at the past two annual conferences that they would like us to explain how policy making works: the play-by-play in D.C. on how we get to where we are,” Mr. Boswell said.
The second session will feature a presentation by Jennifer Bell, founding partner at Chamber Hill Strategies, who represents SHM in Washington. “Jennifer will be discussing how Washington works, the policy process and the pressure points at which SHM and its members can exert influence,” Mr. Lapps said.
Attendees can expect to learn a lot from either session, Mr. Lapps said. “Attendees will learn about the basic contours of the Quality Payment Program that Medicare oversees, and some of the specific new elements of that program this year that were designed with hospitalists in mind. For example, Dr. Duseja will be talking about a facility-based reporting option under the Merit-Based Incentive Payment System. I think our members should gain a concrete understanding of some of the new directions that CMS is heading this year. Overall, they’ll have a better sense of the vision behind quality measures and quality measurement. This is a really exciting opportunity to hear from someone who is both a clinician and works on policy at CMS.”
The policy mini-track offers hospitalists a chance to get a look “behind the curtain” at policy making from someone who is helping to write the rules.
“Attendees will gain insight on where they fit in these programs – and also have the opportunity to tell Dr. Duseja if they don’t feel these programs are a good fit for them,” Mr. Boswell said. “Oftentimes these programs are not structured ideally for hospitalists. So, hearing directly from hospitalists who are experiencing problems would be extraordinarily helpful to a CMS official. I think attendees should view the policy track not only as an opportunity to learn from CMS, but as an opportunity to educate CMS about our issues.”
Crafting a “well-rounded” program
New tracks, interactive programs highlight HM19
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”
New tracks, interactive programs highlight HM19
New tracks, interactive programs highlight HM19
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”
Hospitalist movers and shakers – March 2019
Flora Kisuule, MD, SFHM, has been awarded the 2018 Excellence in Service and Professionalism Award by Johns Hopkins Bayview Medical Center, Baltimore. Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview, assistant professor at Johns Hopkins University School of Medicine, and assistant professor in the Johns Hopkins Bloomberg School of Public Health.
Dr. Kisuule codeveloped a hospitalist fellowship program for Johns Hopkins University, which she now directs. She has served on several Society of Hospital Medicine committees and consulted on hospitalist programs around the world. Dr. Kisuule is joining the SHM Board of Directors in March 2019.
Paul Hain, DO, was promoted recently to chief medical officer and senior vice president of market delivery for Blue Cross/Blue Shield of Texas. Dr. Hain has a wealth of experience in leadership, including helping create the pediatric hospitalist program at Vanderbilt Children’s Hospital in Nashville, Tenn.
With BC/BS, Dr. Hain will oversee the region’s public relations, community investments, government relations, and lobbying. He will help sponsor Medicare and Medicaid in the state, while also supporting enterprise and marketing efforts. Dr. Hain joins BC/BS after serving as vice president and medical director of population health and network development at the Children’s Medical Center of Dallas.
Laura M. Rosch, DO, recently was selected by Kansas City University as the new campus dean in the Joplin (Mo.) College of Osteopathic Medicine. Dr. Rosch is a practicing hospitalist in Illinois, where she was chair of internal medicine at the Chicago College of Osteopathic Medicine prior to taking her current position.
Dr. Rosch will manage daily operations for the Joplin medical school, streamlining the school with the main campus. She is a former president of the Illinois Osteopathic Medicine Society and holds a master’s degree in nutrition science.
Suzan Lowry, MD, has been named health officer for Charles County, Md., by the county Department of Health and Charles County Commissioners. A longtime pediatrician with 20 years’ experience, Dr. Lowry has served as a pediatric hospitalist educator at Children’s National Medical Center in Washington, D.C.
Dr. Lowry has spent a majority of her career working on behalf of public health. Most recently, she has worked at the United States Marine Corps Quantico Health Clinic in Virginia.
Robyn Chase, DO, a staff hospitalist at Yavapai Regional Medical Center (Prescott, Ariz.), recently was selected as the hospital’s Physician of the Year for 2018.
Dr. Chase has practiced at YRMC since 2010 and is a board-certified internist. She also serves as an associate professor at the University of Arizona, Phoenix.
Kevin Dishman, MD, has been elevated to senior vice president and chief medical officer at Stormont Vail Health (Topeka, Kan.). Dr. Dishman also will be president of Stormont medical services division’s medical staff.
Dr. Dishman came to Stormont in 2000 to work as a hospitalist. Most recently, he has served as the center’s vice president of acute care services. In his new role, Dr. Dishman will be charged with, among other duties, seeking out physicians to bring to Stormont’s Topeka location.
BUSINESS MOVES
The Hazel Hawkins Memorial Hospital Women’s Center (Hollister, Calif.) recently established a relationship with Pediatrix Medical Group (Sunrise, Fla.) to provide pediatric hospitalists to help with high-risk delivery of newborns. The hospitalists also will advise Hazel Hawkins staff with regards to critical care transport and assist with the care of newborns and the treatment of child and teen patients.
Hazel Hawkins has been in operation for the past 5 years. Pediatrix hospitalists will be used as consultants for attending staff and emergency physicians and will help treat patients in emergency situations.
American Physician Partners (Brentwood, Tenn.), a national hospital medicine management services company, has acquired private physician group Progressive Medical Associates (Mesa, Ariz.). Progressive’s 37 physicians and 21 private clinicians – working at Banner Health’s 28 nonprofit hospitals covering six states – join the APP team.
Flora Kisuule, MD, SFHM, has been awarded the 2018 Excellence in Service and Professionalism Award by Johns Hopkins Bayview Medical Center, Baltimore. Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview, assistant professor at Johns Hopkins University School of Medicine, and assistant professor in the Johns Hopkins Bloomberg School of Public Health.
Dr. Kisuule codeveloped a hospitalist fellowship program for Johns Hopkins University, which she now directs. She has served on several Society of Hospital Medicine committees and consulted on hospitalist programs around the world. Dr. Kisuule is joining the SHM Board of Directors in March 2019.
Paul Hain, DO, was promoted recently to chief medical officer and senior vice president of market delivery for Blue Cross/Blue Shield of Texas. Dr. Hain has a wealth of experience in leadership, including helping create the pediatric hospitalist program at Vanderbilt Children’s Hospital in Nashville, Tenn.
With BC/BS, Dr. Hain will oversee the region’s public relations, community investments, government relations, and lobbying. He will help sponsor Medicare and Medicaid in the state, while also supporting enterprise and marketing efforts. Dr. Hain joins BC/BS after serving as vice president and medical director of population health and network development at the Children’s Medical Center of Dallas.
Laura M. Rosch, DO, recently was selected by Kansas City University as the new campus dean in the Joplin (Mo.) College of Osteopathic Medicine. Dr. Rosch is a practicing hospitalist in Illinois, where she was chair of internal medicine at the Chicago College of Osteopathic Medicine prior to taking her current position.
Dr. Rosch will manage daily operations for the Joplin medical school, streamlining the school with the main campus. She is a former president of the Illinois Osteopathic Medicine Society and holds a master’s degree in nutrition science.
Suzan Lowry, MD, has been named health officer for Charles County, Md., by the county Department of Health and Charles County Commissioners. A longtime pediatrician with 20 years’ experience, Dr. Lowry has served as a pediatric hospitalist educator at Children’s National Medical Center in Washington, D.C.
Dr. Lowry has spent a majority of her career working on behalf of public health. Most recently, she has worked at the United States Marine Corps Quantico Health Clinic in Virginia.
Robyn Chase, DO, a staff hospitalist at Yavapai Regional Medical Center (Prescott, Ariz.), recently was selected as the hospital’s Physician of the Year for 2018.
Dr. Chase has practiced at YRMC since 2010 and is a board-certified internist. She also serves as an associate professor at the University of Arizona, Phoenix.
Kevin Dishman, MD, has been elevated to senior vice president and chief medical officer at Stormont Vail Health (Topeka, Kan.). Dr. Dishman also will be president of Stormont medical services division’s medical staff.
Dr. Dishman came to Stormont in 2000 to work as a hospitalist. Most recently, he has served as the center’s vice president of acute care services. In his new role, Dr. Dishman will be charged with, among other duties, seeking out physicians to bring to Stormont’s Topeka location.
BUSINESS MOVES
The Hazel Hawkins Memorial Hospital Women’s Center (Hollister, Calif.) recently established a relationship with Pediatrix Medical Group (Sunrise, Fla.) to provide pediatric hospitalists to help with high-risk delivery of newborns. The hospitalists also will advise Hazel Hawkins staff with regards to critical care transport and assist with the care of newborns and the treatment of child and teen patients.
Hazel Hawkins has been in operation for the past 5 years. Pediatrix hospitalists will be used as consultants for attending staff and emergency physicians and will help treat patients in emergency situations.
American Physician Partners (Brentwood, Tenn.), a national hospital medicine management services company, has acquired private physician group Progressive Medical Associates (Mesa, Ariz.). Progressive’s 37 physicians and 21 private clinicians – working at Banner Health’s 28 nonprofit hospitals covering six states – join the APP team.
Flora Kisuule, MD, SFHM, has been awarded the 2018 Excellence in Service and Professionalism Award by Johns Hopkins Bayview Medical Center, Baltimore. Dr. Kisuule is associate director of the division of hospital medicine at Johns Hopkins Bayview, assistant professor at Johns Hopkins University School of Medicine, and assistant professor in the Johns Hopkins Bloomberg School of Public Health.
Dr. Kisuule codeveloped a hospitalist fellowship program for Johns Hopkins University, which she now directs. She has served on several Society of Hospital Medicine committees and consulted on hospitalist programs around the world. Dr. Kisuule is joining the SHM Board of Directors in March 2019.
Paul Hain, DO, was promoted recently to chief medical officer and senior vice president of market delivery for Blue Cross/Blue Shield of Texas. Dr. Hain has a wealth of experience in leadership, including helping create the pediatric hospitalist program at Vanderbilt Children’s Hospital in Nashville, Tenn.
With BC/BS, Dr. Hain will oversee the region’s public relations, community investments, government relations, and lobbying. He will help sponsor Medicare and Medicaid in the state, while also supporting enterprise and marketing efforts. Dr. Hain joins BC/BS after serving as vice president and medical director of population health and network development at the Children’s Medical Center of Dallas.
Laura M. Rosch, DO, recently was selected by Kansas City University as the new campus dean in the Joplin (Mo.) College of Osteopathic Medicine. Dr. Rosch is a practicing hospitalist in Illinois, where she was chair of internal medicine at the Chicago College of Osteopathic Medicine prior to taking her current position.
Dr. Rosch will manage daily operations for the Joplin medical school, streamlining the school with the main campus. She is a former president of the Illinois Osteopathic Medicine Society and holds a master’s degree in nutrition science.
Suzan Lowry, MD, has been named health officer for Charles County, Md., by the county Department of Health and Charles County Commissioners. A longtime pediatrician with 20 years’ experience, Dr. Lowry has served as a pediatric hospitalist educator at Children’s National Medical Center in Washington, D.C.
Dr. Lowry has spent a majority of her career working on behalf of public health. Most recently, she has worked at the United States Marine Corps Quantico Health Clinic in Virginia.
Robyn Chase, DO, a staff hospitalist at Yavapai Regional Medical Center (Prescott, Ariz.), recently was selected as the hospital’s Physician of the Year for 2018.
Dr. Chase has practiced at YRMC since 2010 and is a board-certified internist. She also serves as an associate professor at the University of Arizona, Phoenix.
Kevin Dishman, MD, has been elevated to senior vice president and chief medical officer at Stormont Vail Health (Topeka, Kan.). Dr. Dishman also will be president of Stormont medical services division’s medical staff.
Dr. Dishman came to Stormont in 2000 to work as a hospitalist. Most recently, he has served as the center’s vice president of acute care services. In his new role, Dr. Dishman will be charged with, among other duties, seeking out physicians to bring to Stormont’s Topeka location.
BUSINESS MOVES
The Hazel Hawkins Memorial Hospital Women’s Center (Hollister, Calif.) recently established a relationship with Pediatrix Medical Group (Sunrise, Fla.) to provide pediatric hospitalists to help with high-risk delivery of newborns. The hospitalists also will advise Hazel Hawkins staff with regards to critical care transport and assist with the care of newborns and the treatment of child and teen patients.
Hazel Hawkins has been in operation for the past 5 years. Pediatrix hospitalists will be used as consultants for attending staff and emergency physicians and will help treat patients in emergency situations.
American Physician Partners (Brentwood, Tenn.), a national hospital medicine management services company, has acquired private physician group Progressive Medical Associates (Mesa, Ariz.). Progressive’s 37 physicians and 21 private clinicians – working at Banner Health’s 28 nonprofit hospitals covering six states – join the APP team.
Hospitalist scheduling: A search for balance
Survey says ...
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
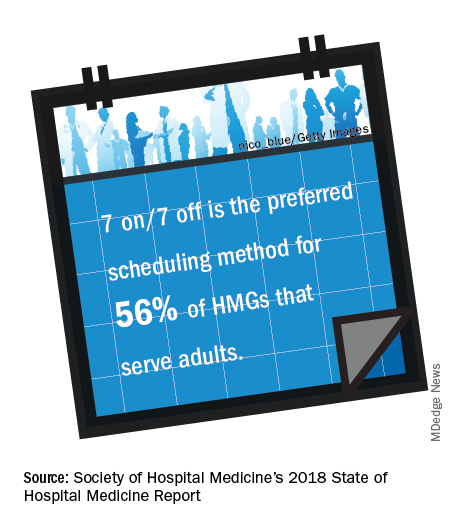
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.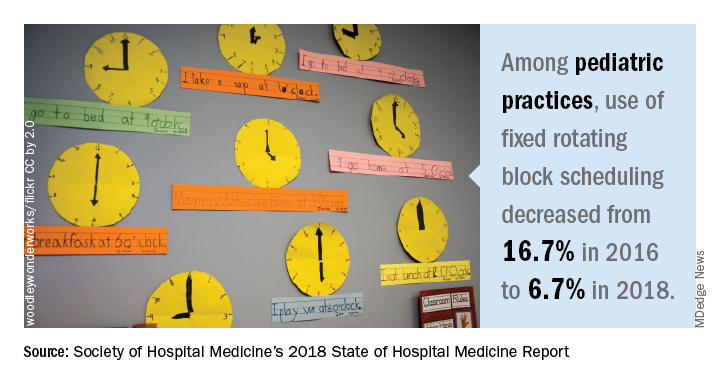
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Survey says ...
Survey says ...
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Hospitalists on the Hill
Advocating for HM in DC
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
Advocating for HM in DC
Advocating for HM in DC
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
Advancing coherence: Your “meta-leadership” objective
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Learn to balance organizational priorities
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Helping quality improvement teams succeed
QI coaches may be the answer
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
QI coaches may be the answer
QI coaches may be the answer
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
Hospitalists understand the need for quality improvement (QI) as an important part of health care, and they take active roles in – or personally drive – many of the QI efforts at their own facilities. But too often the results are inconsistent and the adoption of new practices slow.
Help can come from a QI Coach, according to a recent paper describing a model of successful coaching. “We wanted to be able to help novice QI teams to be successful,” said the paper’s lead author Danielle Olds, PhD. “Unfortunately, most QI projects are not successful for a variety of reasons including inadequate project planning, a lack of QI skills, a lack of leadership and stakeholder buy-in, and inappropriate measures and methods.”
The coaching model outlined comes from the VAQS program, launched in 1998 to provide structured training around QI and the care of veterans. The seven-step process outlined in the paper provides a road map to overcoming typical QI stumbling blocks and create more successful projects.
“Improvement should be a part of everyone’s practice, however most clinicians have not been trained in how to successfully lead a formal QI project,” said Dr. Olds, who is based at the University of Kansas Medical Center in Kansas City. “Hospitals can bridge this gap by providing QI coaches as a resource to guide teams through the process.”
The model offers a new way for hospitalists to take the lead on QI. “Hospitalists who may have extensive experience in conducting QI could use a model, such as ours, to guide their coaching of teams within their facility,” she said. “Because of the nature of hospitalist practice, they are in an ideal position to understand improvement needs at a systems level within their facility. I would strongly encourage hospitalists to engage in QI because of the wealth of knowledge and experience that they could bring.”
Reference
Olds DM et al. “VA Quality Scholars Quality Improvement Coach Model to Facilitate Learning and Success.” Qual Manag Healthcare. 2018;27(2):87-92. doi: 10.1097/QMH.0000000000000164. Accessed 2018 Jun 11.
Shaping the future of hospital medicine
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.