User login
Neutropenia and the White Blood Cells
FDA warns of possible link between breast implants and ALCL
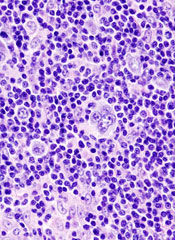
The Food and Drug Administration (FDA), after a review of reported cases of anaplastic large-cell lymphoma (ALCL), warns that there may be a link between silicone and saline breast implants and the rare cancer.
People with breast implants “may have a very small but significant risk of ALCL in the scar capsule adjacent to the implant,” according to the agency.
The FDA based its announcement on a review of literature published between January 1997 and May 2010 that identified 34 unique cases of ALCL in women with either type of breast implant.
William Maisel, MD, chief scientist and deputy director for science in the FDA’s Center for Devices and Radiological Health, said, “We need more data and are asking that healthcare professionals tell us about any confirmed cases they identify.”
Of the 34 unique ALCL cases reviewed, 24 had silicone and 7 had saline implants; 3 implants did not have the type specified. The women ranged in age from 28 to 87 years, with a median age of 51 years.
ALCL occurred in 19 women who received implants for aesthetic augmentation, 11 for reconstruction, and 4 had no reason recorded for the implant.
The women developed ALCL in a median of 8 years from time of implant, ranging from 1 year to 23 years. Most of the patients were diagnosed because they had implant-related symptoms, such as seromas, capsular contractures, or peri-implant masses that needed implant revision surgery.
Physicians found lymphoma cells in the seroma surrounding the implant, in the fibrous capsule, or within a peri-implant mass in all of the ALCL cases.
According to the FDA report, CD30 status was positive in all 29 of the cases that included this information, which is consistent with an ALCL diagnosis. ALCL cases in the rest of the body can be either ALK-positive or ALK-negative. The 26 reports of ALCL in women with breast implants that included ALK status were all ALK-negative.
The FDA recommends that physicians consider an ALCL diagnosis if patients present with capsular contracture or masses adjacent to the breast implant. Physicians should report all confirmed cases of ALCL in people with breast implants to Medwatch.
The FDA does not recommend removing breast implants in patients without symptoms, which include pain, lumps, swelllng, or asymmetry that develop after the surgical site is fully healed. The agency plans to update its review of silicone breast implants in spring 2011.
ALCL occurs in about 1 in 500,000 women each year in the United States, according to the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute. In the breast, ALCL occurs in approximately 3 in 100,000,000 women annually in the US. ![]()
The Food and Drug Administration (FDA), after a review of reported cases of anaplastic large-cell lymphoma (ALCL), warns that there may be a link between silicone and saline breast implants and the rare cancer.
People with breast implants “may have a very small but significant risk of ALCL in the scar capsule adjacent to the implant,” according to the agency.
The FDA based its announcement on a review of literature published between January 1997 and May 2010 that identified 34 unique cases of ALCL in women with either type of breast implant.
William Maisel, MD, chief scientist and deputy director for science in the FDA’s Center for Devices and Radiological Health, said, “We need more data and are asking that healthcare professionals tell us about any confirmed cases they identify.”
Of the 34 unique ALCL cases reviewed, 24 had silicone and 7 had saline implants; 3 implants did not have the type specified. The women ranged in age from 28 to 87 years, with a median age of 51 years.
ALCL occurred in 19 women who received implants for aesthetic augmentation, 11 for reconstruction, and 4 had no reason recorded for the implant.
The women developed ALCL in a median of 8 years from time of implant, ranging from 1 year to 23 years. Most of the patients were diagnosed because they had implant-related symptoms, such as seromas, capsular contractures, or peri-implant masses that needed implant revision surgery.
Physicians found lymphoma cells in the seroma surrounding the implant, in the fibrous capsule, or within a peri-implant mass in all of the ALCL cases.
According to the FDA report, CD30 status was positive in all 29 of the cases that included this information, which is consistent with an ALCL diagnosis. ALCL cases in the rest of the body can be either ALK-positive or ALK-negative. The 26 reports of ALCL in women with breast implants that included ALK status were all ALK-negative.
The FDA recommends that physicians consider an ALCL diagnosis if patients present with capsular contracture or masses adjacent to the breast implant. Physicians should report all confirmed cases of ALCL in people with breast implants to Medwatch.
The FDA does not recommend removing breast implants in patients without symptoms, which include pain, lumps, swelllng, or asymmetry that develop after the surgical site is fully healed. The agency plans to update its review of silicone breast implants in spring 2011.
ALCL occurs in about 1 in 500,000 women each year in the United States, according to the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute. In the breast, ALCL occurs in approximately 3 in 100,000,000 women annually in the US. ![]()
The Food and Drug Administration (FDA), after a review of reported cases of anaplastic large-cell lymphoma (ALCL), warns that there may be a link between silicone and saline breast implants and the rare cancer.
People with breast implants “may have a very small but significant risk of ALCL in the scar capsule adjacent to the implant,” according to the agency.
The FDA based its announcement on a review of literature published between January 1997 and May 2010 that identified 34 unique cases of ALCL in women with either type of breast implant.
William Maisel, MD, chief scientist and deputy director for science in the FDA’s Center for Devices and Radiological Health, said, “We need more data and are asking that healthcare professionals tell us about any confirmed cases they identify.”
Of the 34 unique ALCL cases reviewed, 24 had silicone and 7 had saline implants; 3 implants did not have the type specified. The women ranged in age from 28 to 87 years, with a median age of 51 years.
ALCL occurred in 19 women who received implants for aesthetic augmentation, 11 for reconstruction, and 4 had no reason recorded for the implant.
The women developed ALCL in a median of 8 years from time of implant, ranging from 1 year to 23 years. Most of the patients were diagnosed because they had implant-related symptoms, such as seromas, capsular contractures, or peri-implant masses that needed implant revision surgery.
Physicians found lymphoma cells in the seroma surrounding the implant, in the fibrous capsule, or within a peri-implant mass in all of the ALCL cases.
According to the FDA report, CD30 status was positive in all 29 of the cases that included this information, which is consistent with an ALCL diagnosis. ALCL cases in the rest of the body can be either ALK-positive or ALK-negative. The 26 reports of ALCL in women with breast implants that included ALK status were all ALK-negative.
The FDA recommends that physicians consider an ALCL diagnosis if patients present with capsular contracture or masses adjacent to the breast implant. Physicians should report all confirmed cases of ALCL in people with breast implants to Medwatch.
The FDA does not recommend removing breast implants in patients without symptoms, which include pain, lumps, swelllng, or asymmetry that develop after the surgical site is fully healed. The agency plans to update its review of silicone breast implants in spring 2011.
ALCL occurs in about 1 in 500,000 women each year in the United States, according to the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute. In the breast, ALCL occurs in approximately 3 in 100,000,000 women annually in the US. ![]()
Brentuximab and Refractory Hodgkin's Lymphoma
Brentuximab vedotin, an investigational agent, was associated with complete remission in 34% of patients whose Hodgkin's lymphoma recurred after autologous stem cell transplants, based on data from a phase II trial of 102 patients. For the full story, see http://tinyurl.com/2937bbx
Brentuximab vedotin, an investigational agent, was associated with complete remission in 34% of patients whose Hodgkin's lymphoma recurred after autologous stem cell transplants, based on data from a phase II trial of 102 patients. For the full story, see http://tinyurl.com/2937bbx
Brentuximab vedotin, an investigational agent, was associated with complete remission in 34% of patients whose Hodgkin's lymphoma recurred after autologous stem cell transplants, based on data from a phase II trial of 102 patients. For the full story, see http://tinyurl.com/2937bbx
Denileukin diftitox has significant, durable responses in CTCL
The recombinant fusion protein denileukin diftitox (DD) produced a significant and durable overall response rate at 2 dose levels as compared to placebo in patients with cutaneous T-cell lymphoma (CTCL).
These phase 3 results confirm the efficacy, safety, and clinical benefit of DD in CD25-positive, stage IA to III CTCL. An earlier trial included more heavily pretreated late-stage patients.
Andres Negro-Vilar, MD, PhD, and colleagues reported the current results March 8 ahead of print in the Journal of Clinical Oncology.
The investigators randomized 144 patients—44 to placebo, 45 to 9 mg/kg/day DD, and 55 to 18 m/kg/day DD. Patients received the treatment on days 1 through 5 of each 21-day course for up to 8 courses.
Patients were a median age of 59 years, two thirds had disease stage IIA or earlier, and 94% had received 3 or fewer prior therapies. Prior therapies included phototherapy (48%), interferon alfa (20%), electron beam readiotherapy (48%), system cytotoxic chemotherapy (26%), topical chemotherapy (25%), and other therapies (30%).
Most patients (85%) had mycosis fungoides, 6.3% had Sézary syndrome, and 8.3% had other cutaneous lymphomas.
After a median of 6 treatment courses, patients receiving either dose of DD had a statistically significant overall response rate (ORR) compared to placebo.
Patients in the 18 µg DD group had a 49% ORR, including 9% complete response (CR) or clinical complete response (CCR). This compared to an ORR of 16% for placebo patients (P=0.0015).
Patients in the 9 µg group had a 37.8% ORR, including 11% CR/CCR. This ORR was also significantly better compared to placebo (P=0.0297).
About half of the placebo patients experienced progressive disease compared with 21% of the DD-treated patients.
Progression-free survival (PFS) was significantly longer in the DD-treated patients. The 18 µg-arm had a median PFS of 971 days, the 9 µg-arm had a median PFS of 794 days, and the placebo patients had a median PFS of 124 days.
DD-treated patients in both dose groups experienced significantly superior duration of response, time to response, and time to treatment failure compared to the placebo patients.
DD-treated patients reported more adverse events and serious adverse events than the placebo patients. The investigators observed that the AEs occurred most frequently during the first 2 or 3 treatment courses and then declined to placebo levels.
DD combines the diphtheria toxin with human interleukin-2 (IL-2). DD binds to and is internalized by the IL-2 receptor. Therefore, it is most efficient at killing cells that express the intermediate- or high-affinity IL-2 receptor.
The investigators suggest that the 18 µg/kg/day dose may improve the response rate without increasing toxicity. The higher dose “provides more benefit, such as a higher ORR and statistically significant improvements in several supportive end points . . . DD may represent an important treatment option for many patients with these challenging diseases,” they said. ![]()
The recombinant fusion protein denileukin diftitox (DD) produced a significant and durable overall response rate at 2 dose levels as compared to placebo in patients with cutaneous T-cell lymphoma (CTCL).
These phase 3 results confirm the efficacy, safety, and clinical benefit of DD in CD25-positive, stage IA to III CTCL. An earlier trial included more heavily pretreated late-stage patients.
Andres Negro-Vilar, MD, PhD, and colleagues reported the current results March 8 ahead of print in the Journal of Clinical Oncology.
The investigators randomized 144 patients—44 to placebo, 45 to 9 mg/kg/day DD, and 55 to 18 m/kg/day DD. Patients received the treatment on days 1 through 5 of each 21-day course for up to 8 courses.
Patients were a median age of 59 years, two thirds had disease stage IIA or earlier, and 94% had received 3 or fewer prior therapies. Prior therapies included phototherapy (48%), interferon alfa (20%), electron beam readiotherapy (48%), system cytotoxic chemotherapy (26%), topical chemotherapy (25%), and other therapies (30%).
Most patients (85%) had mycosis fungoides, 6.3% had Sézary syndrome, and 8.3% had other cutaneous lymphomas.
After a median of 6 treatment courses, patients receiving either dose of DD had a statistically significant overall response rate (ORR) compared to placebo.
Patients in the 18 µg DD group had a 49% ORR, including 9% complete response (CR) or clinical complete response (CCR). This compared to an ORR of 16% for placebo patients (P=0.0015).
Patients in the 9 µg group had a 37.8% ORR, including 11% CR/CCR. This ORR was also significantly better compared to placebo (P=0.0297).
About half of the placebo patients experienced progressive disease compared with 21% of the DD-treated patients.
Progression-free survival (PFS) was significantly longer in the DD-treated patients. The 18 µg-arm had a median PFS of 971 days, the 9 µg-arm had a median PFS of 794 days, and the placebo patients had a median PFS of 124 days.
DD-treated patients in both dose groups experienced significantly superior duration of response, time to response, and time to treatment failure compared to the placebo patients.
DD-treated patients reported more adverse events and serious adverse events than the placebo patients. The investigators observed that the AEs occurred most frequently during the first 2 or 3 treatment courses and then declined to placebo levels.
DD combines the diphtheria toxin with human interleukin-2 (IL-2). DD binds to and is internalized by the IL-2 receptor. Therefore, it is most efficient at killing cells that express the intermediate- or high-affinity IL-2 receptor.
The investigators suggest that the 18 µg/kg/day dose may improve the response rate without increasing toxicity. The higher dose “provides more benefit, such as a higher ORR and statistically significant improvements in several supportive end points . . . DD may represent an important treatment option for many patients with these challenging diseases,” they said. ![]()
The recombinant fusion protein denileukin diftitox (DD) produced a significant and durable overall response rate at 2 dose levels as compared to placebo in patients with cutaneous T-cell lymphoma (CTCL).
These phase 3 results confirm the efficacy, safety, and clinical benefit of DD in CD25-positive, stage IA to III CTCL. An earlier trial included more heavily pretreated late-stage patients.
Andres Negro-Vilar, MD, PhD, and colleagues reported the current results March 8 ahead of print in the Journal of Clinical Oncology.
The investigators randomized 144 patients—44 to placebo, 45 to 9 mg/kg/day DD, and 55 to 18 m/kg/day DD. Patients received the treatment on days 1 through 5 of each 21-day course for up to 8 courses.
Patients were a median age of 59 years, two thirds had disease stage IIA or earlier, and 94% had received 3 or fewer prior therapies. Prior therapies included phototherapy (48%), interferon alfa (20%), electron beam readiotherapy (48%), system cytotoxic chemotherapy (26%), topical chemotherapy (25%), and other therapies (30%).
Most patients (85%) had mycosis fungoides, 6.3% had Sézary syndrome, and 8.3% had other cutaneous lymphomas.
After a median of 6 treatment courses, patients receiving either dose of DD had a statistically significant overall response rate (ORR) compared to placebo.
Patients in the 18 µg DD group had a 49% ORR, including 9% complete response (CR) or clinical complete response (CCR). This compared to an ORR of 16% for placebo patients (P=0.0015).
Patients in the 9 µg group had a 37.8% ORR, including 11% CR/CCR. This ORR was also significantly better compared to placebo (P=0.0297).
About half of the placebo patients experienced progressive disease compared with 21% of the DD-treated patients.
Progression-free survival (PFS) was significantly longer in the DD-treated patients. The 18 µg-arm had a median PFS of 971 days, the 9 µg-arm had a median PFS of 794 days, and the placebo patients had a median PFS of 124 days.
DD-treated patients in both dose groups experienced significantly superior duration of response, time to response, and time to treatment failure compared to the placebo patients.
DD-treated patients reported more adverse events and serious adverse events than the placebo patients. The investigators observed that the AEs occurred most frequently during the first 2 or 3 treatment courses and then declined to placebo levels.
DD combines the diphtheria toxin with human interleukin-2 (IL-2). DD binds to and is internalized by the IL-2 receptor. Therefore, it is most efficient at killing cells that express the intermediate- or high-affinity IL-2 receptor.
The investigators suggest that the 18 µg/kg/day dose may improve the response rate without increasing toxicity. The higher dose “provides more benefit, such as a higher ORR and statistically significant improvements in several supportive end points . . . DD may represent an important treatment option for many patients with these challenging diseases,” they said. ![]()
ODAC votes against one leukemia, one NHL drug
The Oncologic Drugs Advisory Committee (ODAC) recommended yesterday against approval of pixantrone for the treatment of recurrent or refractory aggressive non-Hodgkin’s lymphoma (NHL).
ODAC voted unanimously against the approval of pixantrone, saying that the drug did not demonstrate a statistically significant improvement over the control arm. The complete response rate was 20.0% with pixantrone and 5.7% with the comparator therapies.
ODAC also expressed concern that the phase 3 trial was stopped early at 44% of planned enrollment due to poor accrual. And only 8 of the 70 patients enrolled were US patients, raising concern about whether the results held true for the US population.
Pixantrone dimaleate, an aza-anthracenedione, is developed by the Seattle-based Cell Therapeutics, Inc.
ODAC also considered the application of Australian drug maker ChemGenex Pharmaceuticals for omacetaxine mepesuccinate. In a 7-1 decision, ODAC recommended a single genetic test be developed and approved prior to consideration of omacetaxine for the treatment of adults with chronic myeloid leukemia with the Bcr-Abl T3151 mutation.
The drug maker used 2 different tests to identify patients with the mutation. In addition, 23 of 66 patients did not have central laboratory confirmation of the mutation. ODAC was concerned that the comparability of the tests was unknown.
The applicant had submitted data on efficacy and safety prior to completing the planned enrollment of 100 patients, which meant that data from approximately a third of the planned population were missing at the time of consideration.
The US Food and Drug Administration usually follows the recommendations of ODAC. ![]()
The Oncologic Drugs Advisory Committee (ODAC) recommended yesterday against approval of pixantrone for the treatment of recurrent or refractory aggressive non-Hodgkin’s lymphoma (NHL).
ODAC voted unanimously against the approval of pixantrone, saying that the drug did not demonstrate a statistically significant improvement over the control arm. The complete response rate was 20.0% with pixantrone and 5.7% with the comparator therapies.
ODAC also expressed concern that the phase 3 trial was stopped early at 44% of planned enrollment due to poor accrual. And only 8 of the 70 patients enrolled were US patients, raising concern about whether the results held true for the US population.
Pixantrone dimaleate, an aza-anthracenedione, is developed by the Seattle-based Cell Therapeutics, Inc.
ODAC also considered the application of Australian drug maker ChemGenex Pharmaceuticals for omacetaxine mepesuccinate. In a 7-1 decision, ODAC recommended a single genetic test be developed and approved prior to consideration of omacetaxine for the treatment of adults with chronic myeloid leukemia with the Bcr-Abl T3151 mutation.
The drug maker used 2 different tests to identify patients with the mutation. In addition, 23 of 66 patients did not have central laboratory confirmation of the mutation. ODAC was concerned that the comparability of the tests was unknown.
The applicant had submitted data on efficacy and safety prior to completing the planned enrollment of 100 patients, which meant that data from approximately a third of the planned population were missing at the time of consideration.
The US Food and Drug Administration usually follows the recommendations of ODAC. ![]()
The Oncologic Drugs Advisory Committee (ODAC) recommended yesterday against approval of pixantrone for the treatment of recurrent or refractory aggressive non-Hodgkin’s lymphoma (NHL).
ODAC voted unanimously against the approval of pixantrone, saying that the drug did not demonstrate a statistically significant improvement over the control arm. The complete response rate was 20.0% with pixantrone and 5.7% with the comparator therapies.
ODAC also expressed concern that the phase 3 trial was stopped early at 44% of planned enrollment due to poor accrual. And only 8 of the 70 patients enrolled were US patients, raising concern about whether the results held true for the US population.
Pixantrone dimaleate, an aza-anthracenedione, is developed by the Seattle-based Cell Therapeutics, Inc.
ODAC also considered the application of Australian drug maker ChemGenex Pharmaceuticals for omacetaxine mepesuccinate. In a 7-1 decision, ODAC recommended a single genetic test be developed and approved prior to consideration of omacetaxine for the treatment of adults with chronic myeloid leukemia with the Bcr-Abl T3151 mutation.
The drug maker used 2 different tests to identify patients with the mutation. In addition, 23 of 66 patients did not have central laboratory confirmation of the mutation. ODAC was concerned that the comparability of the tests was unknown.
The applicant had submitted data on efficacy and safety prior to completing the planned enrollment of 100 patients, which meant that data from approximately a third of the planned population were missing at the time of consideration.
The US Food and Drug Administration usually follows the recommendations of ODAC. ![]()
Phase 3 trial of pixantrone leaves FDA uneasy
The phase 3 EXTEND PIX301 trial, which will be reviewed by the US Food and Drug Administration’s (FDA) Oncologic Drugs Advisory Committee (ODAC) in the near future, is raising serious questions among members regarding the efficacy and safety of pixantrone.
The drug is intended to treat non-Hodgkin’s lymphoma (NHL) that has resisted at least 2 other treatments.
Among multiple concerns, the trial only included 40% of the original 320 participants that were to be enrolled.
A possible explanation is that third-line patients wanted to use multi-agent chemotherapy or supportive care. Regardless of the reason, ODAC members are unsure if 140 participants can provide enough evidence for reliable conclusions.
Twenty percent of patients receiving pixantrone achieved complete responses (CR) or unconfirmed complete responses (CRu), compared to less than 6% in the comparator group (P=0.021).
However, it has been noted that if only 2 fewer patients achieved CR or CRu, the data would not be statistically significant (P=0.06).
The comparator arm was the doctors’ choice of other single-agent chemotherapy.
Grade 3-4 serious adverse events, including neutropenia, anemia, leukopenia, and thrombocytopenia, were higher in the pixantrone arm (77% versus 52%).
There were 12 deaths from adverse events in the pixantrone arm of the study from cardiac failure, infection, respiratory failure, and other causes.
There were only 5 deaths from adverse events in the comparator arm, suggesting that pixantrone is cardiotoxic, although the FDA did not claim to be able to draw conclusions relative to other NHL drugs.
The committee moved 2 patients from the pixantrone arm of the study to a different response category and 1 from the comparator arm after reviewing radiology scans. No bias was detected during the review.
ODAC was scheduled to meet Wednesday, February 10, but the meeting was postponed due to heavy snow.
The EXTEND PIX301 trial is sponsored by Cell Therapeutics, the company developing pixantrone. ![]()
The phase 3 EXTEND PIX301 trial, which will be reviewed by the US Food and Drug Administration’s (FDA) Oncologic Drugs Advisory Committee (ODAC) in the near future, is raising serious questions among members regarding the efficacy and safety of pixantrone.
The drug is intended to treat non-Hodgkin’s lymphoma (NHL) that has resisted at least 2 other treatments.
Among multiple concerns, the trial only included 40% of the original 320 participants that were to be enrolled.
A possible explanation is that third-line patients wanted to use multi-agent chemotherapy or supportive care. Regardless of the reason, ODAC members are unsure if 140 participants can provide enough evidence for reliable conclusions.
Twenty percent of patients receiving pixantrone achieved complete responses (CR) or unconfirmed complete responses (CRu), compared to less than 6% in the comparator group (P=0.021).
However, it has been noted that if only 2 fewer patients achieved CR or CRu, the data would not be statistically significant (P=0.06).
The comparator arm was the doctors’ choice of other single-agent chemotherapy.
Grade 3-4 serious adverse events, including neutropenia, anemia, leukopenia, and thrombocytopenia, were higher in the pixantrone arm (77% versus 52%).
There were 12 deaths from adverse events in the pixantrone arm of the study from cardiac failure, infection, respiratory failure, and other causes.
There were only 5 deaths from adverse events in the comparator arm, suggesting that pixantrone is cardiotoxic, although the FDA did not claim to be able to draw conclusions relative to other NHL drugs.
The committee moved 2 patients from the pixantrone arm of the study to a different response category and 1 from the comparator arm after reviewing radiology scans. No bias was detected during the review.
ODAC was scheduled to meet Wednesday, February 10, but the meeting was postponed due to heavy snow.
The EXTEND PIX301 trial is sponsored by Cell Therapeutics, the company developing pixantrone. ![]()
The phase 3 EXTEND PIX301 trial, which will be reviewed by the US Food and Drug Administration’s (FDA) Oncologic Drugs Advisory Committee (ODAC) in the near future, is raising serious questions among members regarding the efficacy and safety of pixantrone.
The drug is intended to treat non-Hodgkin’s lymphoma (NHL) that has resisted at least 2 other treatments.
Among multiple concerns, the trial only included 40% of the original 320 participants that were to be enrolled.
A possible explanation is that third-line patients wanted to use multi-agent chemotherapy or supportive care. Regardless of the reason, ODAC members are unsure if 140 participants can provide enough evidence for reliable conclusions.
Twenty percent of patients receiving pixantrone achieved complete responses (CR) or unconfirmed complete responses (CRu), compared to less than 6% in the comparator group (P=0.021).
However, it has been noted that if only 2 fewer patients achieved CR or CRu, the data would not be statistically significant (P=0.06).
The comparator arm was the doctors’ choice of other single-agent chemotherapy.
Grade 3-4 serious adverse events, including neutropenia, anemia, leukopenia, and thrombocytopenia, were higher in the pixantrone arm (77% versus 52%).
There were 12 deaths from adverse events in the pixantrone arm of the study from cardiac failure, infection, respiratory failure, and other causes.
There were only 5 deaths from adverse events in the comparator arm, suggesting that pixantrone is cardiotoxic, although the FDA did not claim to be able to draw conclusions relative to other NHL drugs.
The committee moved 2 patients from the pixantrone arm of the study to a different response category and 1 from the comparator arm after reviewing radiology scans. No bias was detected during the review.
ODAC was scheduled to meet Wednesday, February 10, but the meeting was postponed due to heavy snow.
The EXTEND PIX301 trial is sponsored by Cell Therapeutics, the company developing pixantrone. ![]()
Multiple Myeloma in the Elderly
In the VISTA trial, the Spanish Myeloma Group created an induction regimen of bortezomib, melphalan, and prednisone that elderly patients could tolerate. This year the group took that regimen a step further.
In the VISTA trial, the Spanish Myeloma Group created an induction regimen of bortezomib, melphalan, and prednisone that elderly patients could tolerate. This year the group took that regimen a step further.
In the VISTA trial, the Spanish Myeloma Group created an induction regimen of bortezomib, melphalan, and prednisone that elderly patients could tolerate. This year the group took that regimen a step further.
First-Line Lymphoma Treatments
Bendamustine plus rituximab has the potential to replace standard CHOP chemotherapy plus rituximab in the first-line treatment of advanced lymphomas. Dr. Mathias J. Rummel discusses data presented at the annual meeting of the American Society of Hematology.
Bendamustine plus rituximab has the potential to replace standard CHOP chemotherapy plus rituximab in the first-line treatment of advanced lymphomas. Dr. Mathias J. Rummel discusses data presented at the annual meeting of the American Society of Hematology.
Bendamustine plus rituximab has the potential to replace standard CHOP chemotherapy plus rituximab in the first-line treatment of advanced lymphomas. Dr. Mathias J. Rummel discusses data presented at the annual meeting of the American Society of Hematology.
Fostamatinib successfully targets the B-cell receptor
NEW YORK—Fostamatinib, a potent, specific inhibitor of spleen tyrosine kinase (Syk), shows promise as a targeted therapy for non-Hodgkin’s lymphoma (NHL) and leukemia.
The B-cell receptor is present on both normal B cells and malignant B cells. Signaling through this receptor is necessary for B-cell maturation and survival. A subset of aggressive lymphomas, as well as follicular lymphomas, appear to rely on signaling from this receptor for survival, said Jonathan Friedberg, MD, of the University of Rochester in New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Syk mediates and amplifies the B-cell receptor signal and initiates downstream events. Inhibition of Syk results in lymphoma cell death in vitro, he said.
“Syk is expressed in aggressive B-cell lines. Altered B-cell receptor signaling distinguishes follicular lymphoma cells from non-malignant B cells,” said Dr Friedberg. “Syk activity is increased in follicular lymphoma cells compared to normal cells.”
Fostamatinib is an orally available drug that has been shown to be safe in healthy human volunteers and is active in the treatment of rheumatoid arthritis and idiopathic thrombocytopenic purpura (ITP). A study of 19 ITP patients found the drug was well tolerated and yielded a 75% response rate.
Dr Friedberg presented the results of the first phase 1/2 trial of fostamatinib in heavily pretreated patients with relapsed/refractory NHL. The phase 1 study evaluated 200 mg and 250 mg twice-daily doses of fostamatinib in 13 patients, median age 74 years. The dose-limiting toxicities were neutropenia, thrombocytopenia, and diarrhea. The 200 mg twice-daily dose was chosen for phase 2 testing.
The phase 2 study enrolled 68 patients with relapsed/refractory disease, including diffuse large B-cell lymphoma (DLBCL) (23 patients), follicular lymphoma (21 patients), and other NHLs (24 patients). The other NHLs mainly included patients with chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL).
The drug was well tolerated, he said. Adverse events were mainly grade 1 or 2. The most common toxicities included diarrhea, fatigue, cytopenias, nausea, and hypertension. He noted that 20% of patients developed hypertension, which was easily controlled. Five patients developed febrile neutropenia and 1 patient had pancytopenia.
Response rates were 21% for DLBCL patients, 10% for follicular lymphoma patients, 55% for CLL/SLL. Stable disease was observed in an additional 22 patients. Median progression-free survival was 4.2 months and response duration exceeded 4 months.
“Some patients had bulky lymphadenopathy that resolved completely with this agent,” said Dr Friedberg. “As the lymphocyte count increased, the lymph nodes melted away.” White blood cell counts normalized in almost all CLL patients, he noted.
The future development of the drug is likely to include rational combinations with other agents. Ongoing laboratory studies are evaluating fostamatinib with mTOR inhibitors, rituximab, proteasome inhibitors, and chemotherapeutic agents.
“Additional clinical trials are planned to identify lymphomas dependent upon the BCR pathway, and to confirm the exciting effects of this truly targeted therapy for B-cell lymphomas and leukemia,” he said. ![]()
NEW YORK—Fostamatinib, a potent, specific inhibitor of spleen tyrosine kinase (Syk), shows promise as a targeted therapy for non-Hodgkin’s lymphoma (NHL) and leukemia.
The B-cell receptor is present on both normal B cells and malignant B cells. Signaling through this receptor is necessary for B-cell maturation and survival. A subset of aggressive lymphomas, as well as follicular lymphomas, appear to rely on signaling from this receptor for survival, said Jonathan Friedberg, MD, of the University of Rochester in New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Syk mediates and amplifies the B-cell receptor signal and initiates downstream events. Inhibition of Syk results in lymphoma cell death in vitro, he said.
“Syk is expressed in aggressive B-cell lines. Altered B-cell receptor signaling distinguishes follicular lymphoma cells from non-malignant B cells,” said Dr Friedberg. “Syk activity is increased in follicular lymphoma cells compared to normal cells.”
Fostamatinib is an orally available drug that has been shown to be safe in healthy human volunteers and is active in the treatment of rheumatoid arthritis and idiopathic thrombocytopenic purpura (ITP). A study of 19 ITP patients found the drug was well tolerated and yielded a 75% response rate.
Dr Friedberg presented the results of the first phase 1/2 trial of fostamatinib in heavily pretreated patients with relapsed/refractory NHL. The phase 1 study evaluated 200 mg and 250 mg twice-daily doses of fostamatinib in 13 patients, median age 74 years. The dose-limiting toxicities were neutropenia, thrombocytopenia, and diarrhea. The 200 mg twice-daily dose was chosen for phase 2 testing.
The phase 2 study enrolled 68 patients with relapsed/refractory disease, including diffuse large B-cell lymphoma (DLBCL) (23 patients), follicular lymphoma (21 patients), and other NHLs (24 patients). The other NHLs mainly included patients with chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL).
The drug was well tolerated, he said. Adverse events were mainly grade 1 or 2. The most common toxicities included diarrhea, fatigue, cytopenias, nausea, and hypertension. He noted that 20% of patients developed hypertension, which was easily controlled. Five patients developed febrile neutropenia and 1 patient had pancytopenia.
Response rates were 21% for DLBCL patients, 10% for follicular lymphoma patients, 55% for CLL/SLL. Stable disease was observed in an additional 22 patients. Median progression-free survival was 4.2 months and response duration exceeded 4 months.
“Some patients had bulky lymphadenopathy that resolved completely with this agent,” said Dr Friedberg. “As the lymphocyte count increased, the lymph nodes melted away.” White blood cell counts normalized in almost all CLL patients, he noted.
The future development of the drug is likely to include rational combinations with other agents. Ongoing laboratory studies are evaluating fostamatinib with mTOR inhibitors, rituximab, proteasome inhibitors, and chemotherapeutic agents.
“Additional clinical trials are planned to identify lymphomas dependent upon the BCR pathway, and to confirm the exciting effects of this truly targeted therapy for B-cell lymphomas and leukemia,” he said. ![]()
NEW YORK—Fostamatinib, a potent, specific inhibitor of spleen tyrosine kinase (Syk), shows promise as a targeted therapy for non-Hodgkin’s lymphoma (NHL) and leukemia.
The B-cell receptor is present on both normal B cells and malignant B cells. Signaling through this receptor is necessary for B-cell maturation and survival. A subset of aggressive lymphomas, as well as follicular lymphomas, appear to rely on signaling from this receptor for survival, said Jonathan Friedberg, MD, of the University of Rochester in New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Syk mediates and amplifies the B-cell receptor signal and initiates downstream events. Inhibition of Syk results in lymphoma cell death in vitro, he said.
“Syk is expressed in aggressive B-cell lines. Altered B-cell receptor signaling distinguishes follicular lymphoma cells from non-malignant B cells,” said Dr Friedberg. “Syk activity is increased in follicular lymphoma cells compared to normal cells.”
Fostamatinib is an orally available drug that has been shown to be safe in healthy human volunteers and is active in the treatment of rheumatoid arthritis and idiopathic thrombocytopenic purpura (ITP). A study of 19 ITP patients found the drug was well tolerated and yielded a 75% response rate.
Dr Friedberg presented the results of the first phase 1/2 trial of fostamatinib in heavily pretreated patients with relapsed/refractory NHL. The phase 1 study evaluated 200 mg and 250 mg twice-daily doses of fostamatinib in 13 patients, median age 74 years. The dose-limiting toxicities were neutropenia, thrombocytopenia, and diarrhea. The 200 mg twice-daily dose was chosen for phase 2 testing.
The phase 2 study enrolled 68 patients with relapsed/refractory disease, including diffuse large B-cell lymphoma (DLBCL) (23 patients), follicular lymphoma (21 patients), and other NHLs (24 patients). The other NHLs mainly included patients with chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL).
The drug was well tolerated, he said. Adverse events were mainly grade 1 or 2. The most common toxicities included diarrhea, fatigue, cytopenias, nausea, and hypertension. He noted that 20% of patients developed hypertension, which was easily controlled. Five patients developed febrile neutropenia and 1 patient had pancytopenia.
Response rates were 21% for DLBCL patients, 10% for follicular lymphoma patients, 55% for CLL/SLL. Stable disease was observed in an additional 22 patients. Median progression-free survival was 4.2 months and response duration exceeded 4 months.
“Some patients had bulky lymphadenopathy that resolved completely with this agent,” said Dr Friedberg. “As the lymphocyte count increased, the lymph nodes melted away.” White blood cell counts normalized in almost all CLL patients, he noted.
The future development of the drug is likely to include rational combinations with other agents. Ongoing laboratory studies are evaluating fostamatinib with mTOR inhibitors, rituximab, proteasome inhibitors, and chemotherapeutic agents.
“Additional clinical trials are planned to identify lymphomas dependent upon the BCR pathway, and to confirm the exciting effects of this truly targeted therapy for B-cell lymphomas and leukemia,” he said. ![]()
Panobinostat shows promise in refractory Hodgkin lymphoma
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
New York, NY —Growing evidence suggests that the potent pan-deacetylase inhibitor panobinostat (LBH589) shows promising clinical activity in heavily pretreated patients with relapsed/refractory Hodgkin’s lymphoma.
Panobinostat targets both epigenetic and non-epigenetic oncogenic pathways and is among a group of novel antineoplastic agents that inhibit the activity of histone deacetylases, said Myron Czuczman, MD, of Roswell Park Cancer Institute in Buffalo, New York, at the Chemotherapy Foundation Symposium held November 10-13, 2009.
Panobinostat is currently under clinical investigation in a variety of solid tumors and hematologic malignancies. Promising results in relapsed/refractory Hodgkin’s lymphoma were presented earlier in the year at the European Hematology Association annual meeting in Berlin, Germany.
Dr Czuczman updated those results from the phase 1/2 trial of Hodgkin’s lymphoma patients with a variety of advanced hematologic malignancies who were refractory to treatments. One group of patients had leukemias or high-risk myelodysplastic syndromes and another group had lymphoma or myeloma.
The patients received 2 schedules of oral panobinostat: once-a-day on Monday, Wednesday, and Friday (MWF) every week or MWF every other week. PET and CT data were evaluated for best response.
So far, 61 patients in the lymphoma and myeloma group have been treated, and 53 patients have been evaluated. The investigators have recorded 1 complete response, 10 partial responses, and 31 patients with stable disease. Of the 31 patients with stable disease, 25 patients had a decrease in tumor burden, and additional responses are likely in this group, said Dr Czuczman.
For patients in the lymphoma or myeloma group, “about three-quarters of the patients had some evidence of antitumor activity,” said Dr Czuczman.
He noted that this group has had a range of prior therapies, including surgery, radiotherapy, stem cell transplantation, and cytotoxic chemotherapy. The median number of prior chemotherapeutic regimens was 5. “These patients had limited treatment options,” he said.
Safety analysis reveals that the most common grade 3/4 adverse events with panobinostat therapy have been thrombocytopenia, neutropenia, fatigue, and anemia. The maximum tolerated dose for patients in this group is 40 mg MWF every week or 60 mg MWF every other week. “More than 60% of the patients have had dose reductions, mostly due to cytopenia, which is not surprising given their limited bone marrow reserve,” he said.
Dr Czuczman said that panobinostat was well tolerated and induced antitumor activity in heavily pretreated patients. “The drug has a role in the treatment of patients with treatment-refractory Hodgkin’s lymphoma and possibly in earlier stages of the disease as well,” he said.
Further updates of this ongoing study will follow, and a global phase 2 study is currently underway using panobinostat at 40 mg/day on MWF every week in patients with Hodgkin’s lymphoma.
In addition, Dr Czuczman has started a phase 1 study in relapsed/refractory Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients using panobinostat in an intrapatient dose modification program that allows patients to escalate or deescalate doses depending on their tolerance of the drug.![]()
