User login
Reducing outpatient medication costs
For many patients, paying for medication presents a serious challenge. Studies show that up to 45% of Americans do not fill prescriptions secondary to cost, and medication nonadherence leads to morbidity and mortality, with costs from $100 billion to $300 billion annually.
One way to address the problem is by empowering clinicians to reduce patient outpatient medication costs – the goal described in a recent abstract.
Initial testing was promising. One patient, admitted for the fourth time in 14 months for hypertriglyceridemia-induced pancreatitis secondary to medication nonadherence, was able to reduce 90-day outpatient medication cost by 95%, from $1,287.00 to $61.79. By reducing his readmissions, the institution saved more than $20,000 a year.
The researchers secured internal grant funding to develop an automated version of the tool. “We currently have technology that can dramatically reduce the cost of many medications with early promising results for patient outcomes, readmissions rates and overall systemic cost,” Dr. Kubey said. “We are working rapidly to further develop and study our tool and, if prospective results confirm our initial findings, we will seek to provide this tool to clinicians broadly.”
Such tools are a true win-win. Hospitalists using them help ensure that discharged patients are able to afford the often life-saving medications that will keep them healthy and out of the hospital, improve readmission rates, patient satisfaction metrics, total system cost, and, most important, do right by our patients in need for whom we are charged to care, Dr. Kubey said.
“Hospitalists first must be aware that savings of 90% or more are possible for many medications and that medication nonadherence because of cost is a serious issue affecting nearly half the patients we see,” he said. “The first step is simply asking patients if medication cost is proving troublesome – we cannot address what we do not see. The second step is to use current discount tools such as GoodRx, NeedyMeds, and the like – and, we hope, in the not too distant future, our tool, which we plan to integrate into EHR prescribing to make it easy and nearly instantaneous for hospitalists to prescribe the most high-value, low-cost medication regimen for each individual patient at discharge.”
Reference
Kubey A et al. Expensive free hospitalizations – A novel approach to reducing outpatient medication cost [abstract]. J Hosp Med. 2017; 12 (suppl 2). Accessed Aug. 7, 2017.
For many patients, paying for medication presents a serious challenge. Studies show that up to 45% of Americans do not fill prescriptions secondary to cost, and medication nonadherence leads to morbidity and mortality, with costs from $100 billion to $300 billion annually.
One way to address the problem is by empowering clinicians to reduce patient outpatient medication costs – the goal described in a recent abstract.
Initial testing was promising. One patient, admitted for the fourth time in 14 months for hypertriglyceridemia-induced pancreatitis secondary to medication nonadherence, was able to reduce 90-day outpatient medication cost by 95%, from $1,287.00 to $61.79. By reducing his readmissions, the institution saved more than $20,000 a year.
The researchers secured internal grant funding to develop an automated version of the tool. “We currently have technology that can dramatically reduce the cost of many medications with early promising results for patient outcomes, readmissions rates and overall systemic cost,” Dr. Kubey said. “We are working rapidly to further develop and study our tool and, if prospective results confirm our initial findings, we will seek to provide this tool to clinicians broadly.”
Such tools are a true win-win. Hospitalists using them help ensure that discharged patients are able to afford the often life-saving medications that will keep them healthy and out of the hospital, improve readmission rates, patient satisfaction metrics, total system cost, and, most important, do right by our patients in need for whom we are charged to care, Dr. Kubey said.
“Hospitalists first must be aware that savings of 90% or more are possible for many medications and that medication nonadherence because of cost is a serious issue affecting nearly half the patients we see,” he said. “The first step is simply asking patients if medication cost is proving troublesome – we cannot address what we do not see. The second step is to use current discount tools such as GoodRx, NeedyMeds, and the like – and, we hope, in the not too distant future, our tool, which we plan to integrate into EHR prescribing to make it easy and nearly instantaneous for hospitalists to prescribe the most high-value, low-cost medication regimen for each individual patient at discharge.”
Reference
Kubey A et al. Expensive free hospitalizations – A novel approach to reducing outpatient medication cost [abstract]. J Hosp Med. 2017; 12 (suppl 2). Accessed Aug. 7, 2017.
For many patients, paying for medication presents a serious challenge. Studies show that up to 45% of Americans do not fill prescriptions secondary to cost, and medication nonadherence leads to morbidity and mortality, with costs from $100 billion to $300 billion annually.
One way to address the problem is by empowering clinicians to reduce patient outpatient medication costs – the goal described in a recent abstract.
Initial testing was promising. One patient, admitted for the fourth time in 14 months for hypertriglyceridemia-induced pancreatitis secondary to medication nonadherence, was able to reduce 90-day outpatient medication cost by 95%, from $1,287.00 to $61.79. By reducing his readmissions, the institution saved more than $20,000 a year.
The researchers secured internal grant funding to develop an automated version of the tool. “We currently have technology that can dramatically reduce the cost of many medications with early promising results for patient outcomes, readmissions rates and overall systemic cost,” Dr. Kubey said. “We are working rapidly to further develop and study our tool and, if prospective results confirm our initial findings, we will seek to provide this tool to clinicians broadly.”
Such tools are a true win-win. Hospitalists using them help ensure that discharged patients are able to afford the often life-saving medications that will keep them healthy and out of the hospital, improve readmission rates, patient satisfaction metrics, total system cost, and, most important, do right by our patients in need for whom we are charged to care, Dr. Kubey said.
“Hospitalists first must be aware that savings of 90% or more are possible for many medications and that medication nonadherence because of cost is a serious issue affecting nearly half the patients we see,” he said. “The first step is simply asking patients if medication cost is proving troublesome – we cannot address what we do not see. The second step is to use current discount tools such as GoodRx, NeedyMeds, and the like – and, we hope, in the not too distant future, our tool, which we plan to integrate into EHR prescribing to make it easy and nearly instantaneous for hospitalists to prescribe the most high-value, low-cost medication regimen for each individual patient at discharge.”
Reference
Kubey A et al. Expensive free hospitalizations – A novel approach to reducing outpatient medication cost [abstract]. J Hosp Med. 2017; 12 (suppl 2). Accessed Aug. 7, 2017.
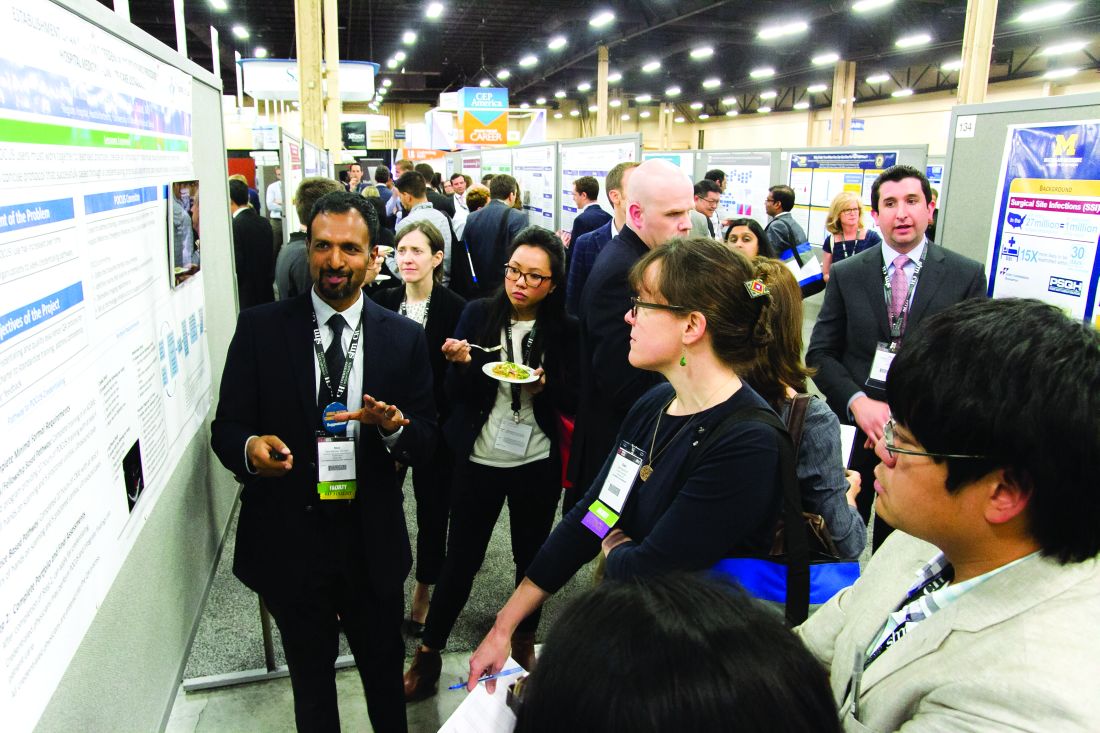
RIV spotlights HM-focused research in real-time
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
12 things pharmacists want hospitalists to know
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
It’s hard to rank anything in hospital medicine much higher than making sure patients receive the medications they need. When mistakes happen, the care is less than optimal, and, in the worst cases, there can be disastrous consequences. Yet, the pharmacy process – involving interplay between hospitalists and pharmacists – can sometimes be clunky and inefficient, even in the age of electronic health records (EHRs).
The Hospitalist surveyed a half-dozen experts, who touched on the need for extra vigilance, areas at high risk for miscues, ways to refine communications and, ultimately, how to improve the care of patients. The following are tips and helpful hints for front-line hospitalists caring for hospitalized patients.
1. Avoid assumptions and shortcuts when reviewing a patient’s home medication list.
“As the saying goes, ‘garbage in, garbage out.’ This applies to completing a comprehensive medication review for a patient at the time of admission to the hospital, to ensure the patient is started on the right medications,” said Lisa Kroon, PharmD, chair of the department of clinical pharmacy at the University of California, San Francisco.
The EHR “is often more of a record of which medications have been ordered by a provider at some point,” she notes.
Doug Humber, PharmD, clinical professor of pharmacy at the University of California, San Diego, said hospitalists should be sure to ask patients about over-the-counter drugs, herbals, and nutraceuticals.
Dr. Kroon encourages hospitalists to conduct a complete medication review, which helps determine what should be continued at discharge.
“Sometimes, not all medications a patient was taking at home need to be restarted, such as vitamins or supplements, so avoid just entering, ‘Restart all home meds,’ ” she said.
2. Pay close attention to adjustments based on liver and kidney function.
“A hospitalist may take a more hands-off approach and just make the assumption that their medications are dose-adjusted appropriately, and I think that might be a bad assumption. [Don’t assume] that things are just automatically going to be adjusted,” Dr. Humber said.
That said, hospitalists also need to be cognizant of adjustments for reasons that aren’t kidney or liver related.
“It is well known that patients with renal and hepatic disease often require dosage adjustments for optimal therapeutic response, but patients with other characteristics and conditions also may require dosage adjustments due to variations in pharmacokinetics and pharmacodynamics,” said Erika Thomas, MBA, RPh,, a pharmacist and director of the Inpatient Care Practitioners section of the American Society of Health-System Pharmacists. “Patients who are obese, elderly, neonatal, pediatric, and those with other comorbidities also may require dosage adjustment.”
Drug-drug interactions might call for unique dosage adjustments, too, she adds.
3. Carefully choose drug-information sources.
“Hospitalists can contact drug-information centers that answer complex clinical questions about drugs if they do not have the time to explore themselves,” he said.
Creighton University, Omaha, Neb., for example, has such a center that has been nationally recognized.
4. Carefully review patients’ medications when they transfer from different levels of care.
Certain medications are started in the ICU that may not need to be continued on the non-ICU floor or at discharge, said MacKenzie Clark, PharmD, program pharmacist at the University of California, San Francisco. One example is quetiapine, which is used in the ICU for delirium.
“Unfortunately, we are seeing patients erroneously continued on this [medication] on the floor. Some are even discharged on this [med],” Clark said, adding that a specific order set can be developed that has a 72-hour automatic stop date for all orders for quetiapine when used specifically for delirium.
“[The order set] can help reduce the chance that it be continued unnecessarily when a patient transfers out of the ICU,” she explains.
Another class of medication that is often initiated in the ICU is proton pump inhibitors for stress ulcer prophylaxis. Continuing these on the floor or at discharge, Clark said, should be carefully considered to avoid unnecessary use and potential adverse effects.
5. Seek opportunities to change from intravenous to oral medications – it could mean big savings.
Intravenous medications usually are more expensive than oral formulations. They also increase the risk of infection. Those are two good reasons to switch patients from IV to oral (PO) as early as possible.
“We find that physicians often don’t know how much drugs cost,” said Marilyn Stebbins, PharmD, vice chair of clinical innovation at University of California, San Francisco.
A common example, she said, is IV acetaminophen, the cost of which skyrocketed in 2014. Institutions can save significant dollars by limiting use of IV acetaminophen outside the perioperative area to patients unable to tolerate oral medications. For patients who are candidates for IV acetaminophen, consider setting an automatic expiration of the order at 24 hours.
Hospitalists can help reduce the drug budget by supporting IV-to-PO programs, in which pharmacists can automatically change an IV medication to PO formulation after verifying a patient is able to tolerate orals.
6. Consider a patient’s health insurance coverage when prescribing a drug at discharge.
“Don’t start the fancy drug that the patient can’t continue at home,” said Ian Jenkins, MD, SFHM, a hospitalist and health sciences clinical professor at the University of California, San Diego, and member of the UCSD pharmacy and therapeutics committee. “New anticoagulants are a great example. We run outpatient claims against their insurance before starting anything, as a policy to avoid this.”
7. Tell the pharmacist what you’re thinking.
Dr. Jenkins uses a case of sepsis as an example:
“If you make it clear that’s what’s happening, you can get a stat loading-dose infused and meet [The Joint Commission] goals for management and improve care, rather than just routine antibiotic starts,” he said.
“Why are you starting the anticoagulant? Recommendations could differ if it’s for acute PE (pulmonary embolism) versus just bridging, which pharmacists these days might catch as overtreatment,” he said. “Keep [the pharmacy] posted about upcoming changes, so they can do discharge planning and anticipate things like glucose management changes with steroid-dose fluctuations.”
8. Beware chronic medications that are not on the hospital formulary.
Your hospital likely has a formulary for chronic medications, such as ACE inhibitors, angiotensin receptor blockers, and statins, which might be different than what the patient was taking at home. So, changes might need to be made, Dr. Clark.
“Pharmacists can assist in this,” she said. “Often, a ‘therapeutic interchange program’ can be established whereby a pharmacist can automatically change the medication to a therapeutically equivalent one and ensure the appropriate dose conversion.”
At discharge, the reverse process is required.
“Be sure you are not discharging the patient on the hospital formulary drug [e.g., ramipril] ... when they already have lisinopril in their medicine cabinet at home,” Clark said. “This can lead to confusion by the patient about which medication to take and result in unintended duplicate drug therapy or worse. A patient may not take either medication because they aren’t sure just what to take.”
9. Don’t hesitate to rely on pharmacists’ expertise.
“To ensure that patients enter and leave the hospital on the right medications and [that they are] taken at the right dose and time, do not forget to enlist your pharmacists to provide support during care transitions,” Dr. Stebbins said.
Dr. Humber said pharmacists are “uniquely qualified” to be medication experts in a facility, and that “kind of experience and that type of expertise to the care of the hospitalized patient is paramount.”
Dr. Thomas said that pharmacists can save hospitalists time.
“Check with your pharmacist on available decision-support tools, available infusion devices, institutional medication-related protocols, and medications within a drug class.”Additionally, encourage pharmacists to join you for rounds, if they’re not already doing so. Dr. Humber also said hospitalists should consider more one-on-one communications, noting that it’s always better to chat “face to face than it is over the phone or with a text message. Things can certainly get misinterpreted.”
10. Consider asking a pharmacist for advice on how to administer complicated regimens.
“Drugs can be administered in a variety of ways, including nasogastric, sublingual, oral, rectal, IV infusion, epidural, intra-arterial, topical, extracorporeal, and intrathecal,” Dr. Thomas said. “Not all drug formulations can be administered by all routes for a variety of reasons. Pharmacists can assist in determining the safest and most effective route of administration for drug formulations.”
11. Not all patients need broad-spectrum antibiotics for a prolonged period of time.
According to the Centers for Disease Control and Prevention, 20%-50% of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, Dr. Kroon said.
“Specifying the dose, duration, and indication for all courses of antibiotics helps promote the appropriate use of antibiotics,” she noted.
Pharmacists play a large role in antibiotic dosing based on therapeutic levels, such as with vancomycin or on organ function, as with renal dose-adjustments; and in identifying drug-drug interactions that occur frequently with antibiotics, such as with the separation of quinolones from many supplements.
12. When ordering medications, a complete and legible signature is required.
With new computerized physician order entry ordering, it seems intuitive that what a physician orders is what they want, Dr. Kroon said. But, if medication orders are not completely clear, errors can arise at steps in the medication management process, such as when a pharmacist verifies and approves the medication order or at medication administration by a nurse. To avoid errors, she suggests that every medication order have the drug name, dose, route, and frequency. She also suggested that all “PRN” – as needed – orders need an indication and additional specificity if there are multiple medications.
For pain medications, an example might be: “Tylenol 1,000 mg PO q8h prn mild pain; Norco 5-325mg, 1 tab PO q4h prn moderate pain; oxycodone 5mg PO q4h prn severe pain.” This, Dr. Kroon explains, allows nurses to know when a specific medication should be administered to a patient. “Writing complete orders alleviates unnecessary paging to the ordering providers and ensures the timely administration of medications to patients,” she said.
VIDEO: Attaining the tools to start your own quality improvement project
Quality improvement at the program level is a major concern for most hospitalists. That’s exactly why Venkata Dontaraju, MD, MRCP, FHM, attended a Tuesday afternoon HM17 workshop entitled “Adding to Your Toolbox: QI Methodologies.”
Dr. Dontaraju, a hospitalist for 7 years with Rockford Health Physicians in Loves Park, Ill., wants to begin QI projects of his own. He planned to attend a number of QI-focused sessions at the annual meeting, with the toolbox session laying the foundation for such work.
“There is a lot of emphasis on cutting down the waste in health care, and also improving the processes,” he said. “That is where the role of QI comes into place. I want to do QI projects at my own hospital, but I first want to get the tools necessary for a successful project.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Quality improvement at the program level is a major concern for most hospitalists. That’s exactly why Venkata Dontaraju, MD, MRCP, FHM, attended a Tuesday afternoon HM17 workshop entitled “Adding to Your Toolbox: QI Methodologies.”
Dr. Dontaraju, a hospitalist for 7 years with Rockford Health Physicians in Loves Park, Ill., wants to begin QI projects of his own. He planned to attend a number of QI-focused sessions at the annual meeting, with the toolbox session laying the foundation for such work.
“There is a lot of emphasis on cutting down the waste in health care, and also improving the processes,” he said. “That is where the role of QI comes into place. I want to do QI projects at my own hospital, but I first want to get the tools necessary for a successful project.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Quality improvement at the program level is a major concern for most hospitalists. That’s exactly why Venkata Dontaraju, MD, MRCP, FHM, attended a Tuesday afternoon HM17 workshop entitled “Adding to Your Toolbox: QI Methodologies.”
Dr. Dontaraju, a hospitalist for 7 years with Rockford Health Physicians in Loves Park, Ill., wants to begin QI projects of his own. He planned to attend a number of QI-focused sessions at the annual meeting, with the toolbox session laying the foundation for such work.
“There is a lot of emphasis on cutting down the waste in health care, and also improving the processes,” he said. “That is where the role of QI comes into place. I want to do QI projects at my own hospital, but I first want to get the tools necessary for a successful project.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
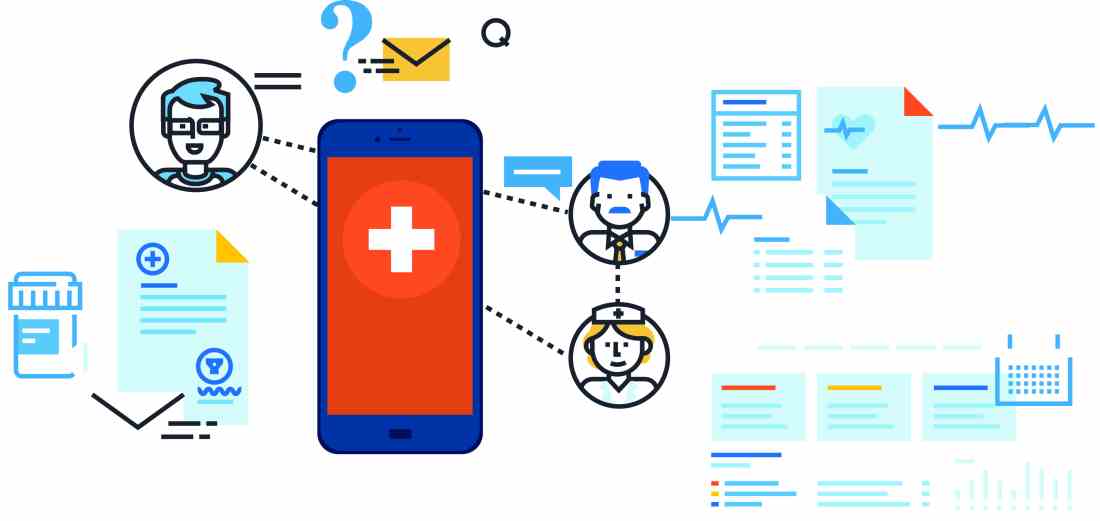
Consider apps for better patient health
Hospitalists should not overlook apps as tools for better health: Smartphone ownership is rising among all demographic groups, and more than 165,000 health apps exist in app stores. Many apps are aimed at helping caregivers and patients with complex medical conditions.
“Patient-facing mobile health applications (mHealth apps) – those intended for use by patients to manage their health – have the potential to help high-need, high-cost populations manage their health, but a variety of questions related to their utility and function have not previously been explored,” Karandeep Singh, MD, MMSc, said in “Many Mobile Health Apps Target High-Need, High-Cost Populations, But Gaps Remain.”1
- How well do apps serve the needs of patients with varying levels of engagement with their health?
- Can we infer an app’s clinical utility or usability based on its app store rating?
- Do apps appropriately respond to information entered by the user indicating that he or she might be in danger?
- How well do apps protect the privacy and security of user-entered health data?
- Are app costs a barrier to patients’ purchasing and using them?
- The study team found a variety of apps for patients with chronic conditions.
“While many apps allow users to track health information, most apps did not respond appropriately when a user entered potentially dangerous health information,” Dr. Singh says. “Consumers’ ratings of apps on the iOS and Android app stores were poor indications of the apps’ clinical utility or usability. Finally, we found that many apps enable sharing of information with others but primarily through insecure means. This is especially problematic because just under two-thirds of apps we evaluated had a privacy policy.”
He cautions hospitalists that app ratings may have little bearing on its clinical utility as judged by a physician.
“Additionally, for patients tracking health findings using apps during an inpatient stay, the most secure way of sharing this information is the old-fashioned way, in person or in print,” he explains. “Unlike hospital-based health information systems, health data stored in apps is generally not regulated by HIPAA. Hospitalists should not assume that a ‘secure messaging’ system provided by a patient-facing app is actually secure.”
The American Medical Association, American Heart Association, Healthcare Information and Management Systems Society, and digital health nonprofit DHX Group are the founders of the new guideline-writing organization called Xcertia. Xcertia will provide guidance for developing, evaluating, or recommending mHealth apps.
“I hope that hospitalists keenly interested in apps will take an active role in Xcertia, to ensure that their voices are heard in what looks to be an unprecedented large-scale effort in the United States,” Dr. Singh says. “While a medication list printed on a discharge summary cannot remind patients to take their meds, apps can do this quite well.”
Reference
1. Singh, K, Drouin, K, Newmark, L, et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Affairs. 2016;35(12):2310-8.
Hospitalists should not overlook apps as tools for better health: Smartphone ownership is rising among all demographic groups, and more than 165,000 health apps exist in app stores. Many apps are aimed at helping caregivers and patients with complex medical conditions.
“Patient-facing mobile health applications (mHealth apps) – those intended for use by patients to manage their health – have the potential to help high-need, high-cost populations manage their health, but a variety of questions related to their utility and function have not previously been explored,” Karandeep Singh, MD, MMSc, said in “Many Mobile Health Apps Target High-Need, High-Cost Populations, But Gaps Remain.”1
- How well do apps serve the needs of patients with varying levels of engagement with their health?
- Can we infer an app’s clinical utility or usability based on its app store rating?
- Do apps appropriately respond to information entered by the user indicating that he or she might be in danger?
- How well do apps protect the privacy and security of user-entered health data?
- Are app costs a barrier to patients’ purchasing and using them?
- The study team found a variety of apps for patients with chronic conditions.
“While many apps allow users to track health information, most apps did not respond appropriately when a user entered potentially dangerous health information,” Dr. Singh says. “Consumers’ ratings of apps on the iOS and Android app stores were poor indications of the apps’ clinical utility or usability. Finally, we found that many apps enable sharing of information with others but primarily through insecure means. This is especially problematic because just under two-thirds of apps we evaluated had a privacy policy.”
He cautions hospitalists that app ratings may have little bearing on its clinical utility as judged by a physician.
“Additionally, for patients tracking health findings using apps during an inpatient stay, the most secure way of sharing this information is the old-fashioned way, in person or in print,” he explains. “Unlike hospital-based health information systems, health data stored in apps is generally not regulated by HIPAA. Hospitalists should not assume that a ‘secure messaging’ system provided by a patient-facing app is actually secure.”
The American Medical Association, American Heart Association, Healthcare Information and Management Systems Society, and digital health nonprofit DHX Group are the founders of the new guideline-writing organization called Xcertia. Xcertia will provide guidance for developing, evaluating, or recommending mHealth apps.
“I hope that hospitalists keenly interested in apps will take an active role in Xcertia, to ensure that their voices are heard in what looks to be an unprecedented large-scale effort in the United States,” Dr. Singh says. “While a medication list printed on a discharge summary cannot remind patients to take their meds, apps can do this quite well.”
Reference
1. Singh, K, Drouin, K, Newmark, L, et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Affairs. 2016;35(12):2310-8.
Hospitalists should not overlook apps as tools for better health: Smartphone ownership is rising among all demographic groups, and more than 165,000 health apps exist in app stores. Many apps are aimed at helping caregivers and patients with complex medical conditions.
“Patient-facing mobile health applications (mHealth apps) – those intended for use by patients to manage their health – have the potential to help high-need, high-cost populations manage their health, but a variety of questions related to their utility and function have not previously been explored,” Karandeep Singh, MD, MMSc, said in “Many Mobile Health Apps Target High-Need, High-Cost Populations, But Gaps Remain.”1
- How well do apps serve the needs of patients with varying levels of engagement with their health?
- Can we infer an app’s clinical utility or usability based on its app store rating?
- Do apps appropriately respond to information entered by the user indicating that he or she might be in danger?
- How well do apps protect the privacy and security of user-entered health data?
- Are app costs a barrier to patients’ purchasing and using them?
- The study team found a variety of apps for patients with chronic conditions.
“While many apps allow users to track health information, most apps did not respond appropriately when a user entered potentially dangerous health information,” Dr. Singh says. “Consumers’ ratings of apps on the iOS and Android app stores were poor indications of the apps’ clinical utility or usability. Finally, we found that many apps enable sharing of information with others but primarily through insecure means. This is especially problematic because just under two-thirds of apps we evaluated had a privacy policy.”
He cautions hospitalists that app ratings may have little bearing on its clinical utility as judged by a physician.
“Additionally, for patients tracking health findings using apps during an inpatient stay, the most secure way of sharing this information is the old-fashioned way, in person or in print,” he explains. “Unlike hospital-based health information systems, health data stored in apps is generally not regulated by HIPAA. Hospitalists should not assume that a ‘secure messaging’ system provided by a patient-facing app is actually secure.”
The American Medical Association, American Heart Association, Healthcare Information and Management Systems Society, and digital health nonprofit DHX Group are the founders of the new guideline-writing organization called Xcertia. Xcertia will provide guidance for developing, evaluating, or recommending mHealth apps.
“I hope that hospitalists keenly interested in apps will take an active role in Xcertia, to ensure that their voices are heard in what looks to be an unprecedented large-scale effort in the United States,” Dr. Singh says. “While a medication list printed on a discharge summary cannot remind patients to take their meds, apps can do this quite well.”
Reference
1. Singh, K, Drouin, K, Newmark, L, et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Affairs. 2016;35(12):2310-8.
Startup Pharmacy Takes Mail-Order to Next Level, Could Solve Medication Management Issue for Millions
It only takes one idea to help change the face of medicine and, recently, Forbes posted an article outlining a small startup pharmacy that could change the way we get our medication. Manchester, N.H.-based Pill Pack takes the whole mail-order pharmacy to a new level.
Medication management can be a major issue for seniors and their caregivers. Seniors are at risk for such problems as overmedication and drug interactions, if medications are not properly managed.
An UpToDate article says that a survey for adults aged 57-85 shows:
- At least one prescription medication was used by 81%;
- Five or more prescription medications were used by 29% of the overall survey population and by 36% of people aged 75 to 85 years; and
- 46% of prescription users also took at least one over-the-counter medication.
Hospitalists see it every day; the readmit because prescribed medication isn’t taken correctly. Possibly, Pill Pack might be one step in the right direction. TH
Lisa Courtney is director of operations at Baptist Health Systems in Birmingham, Ala., and a member of Team Hospitalist.
It only takes one idea to help change the face of medicine and, recently, Forbes posted an article outlining a small startup pharmacy that could change the way we get our medication. Manchester, N.H.-based Pill Pack takes the whole mail-order pharmacy to a new level.
Medication management can be a major issue for seniors and their caregivers. Seniors are at risk for such problems as overmedication and drug interactions, if medications are not properly managed.
An UpToDate article says that a survey for adults aged 57-85 shows:
- At least one prescription medication was used by 81%;
- Five or more prescription medications were used by 29% of the overall survey population and by 36% of people aged 75 to 85 years; and
- 46% of prescription users also took at least one over-the-counter medication.
Hospitalists see it every day; the readmit because prescribed medication isn’t taken correctly. Possibly, Pill Pack might be one step in the right direction. TH
Lisa Courtney is director of operations at Baptist Health Systems in Birmingham, Ala., and a member of Team Hospitalist.
It only takes one idea to help change the face of medicine and, recently, Forbes posted an article outlining a small startup pharmacy that could change the way we get our medication. Manchester, N.H.-based Pill Pack takes the whole mail-order pharmacy to a new level.
Medication management can be a major issue for seniors and their caregivers. Seniors are at risk for such problems as overmedication and drug interactions, if medications are not properly managed.
An UpToDate article says that a survey for adults aged 57-85 shows:
- At least one prescription medication was used by 81%;
- Five or more prescription medications were used by 29% of the overall survey population and by 36% of people aged 75 to 85 years; and
- 46% of prescription users also took at least one over-the-counter medication.
Hospitalists see it every day; the readmit because prescribed medication isn’t taken correctly. Possibly, Pill Pack might be one step in the right direction. TH
Lisa Courtney is director of operations at Baptist Health Systems in Birmingham, Ala., and a member of Team Hospitalist.
Implementing Physician Value-Based Purchasing in Your Practice: HM15 Session Analysis
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
Insulin Rules in the Hospital
Although new medications to manage and treat hyperglycemia and diabetes continuously appear on the market, national guidelines and position statements consistently refer to insulin as the treatment of choice in the inpatient hospital setting.
“When patients are admitted to the hospital, our standard is to switch from the outpatient regimen [wide variety of medications] to the inpatient regimen—insulin,” says Paul M. Szumita, PharmD, BCPS, clinical pharmacy practice manager director at Brigham and Women’s Hospital in Boston.
For critically ill patients in ICUs or during the peri-operative period, intravenous infusion of insulin is preferred. Most general medicine and surgery patients are managed with subcutaneous insulin.
“Using a basal bolus regimen starting at a total daily dose of 0.3-0.5 unit/kg is sufficient for most patients,” says Guillermo Umpierrez, MD, CDE, FCAE, FACP, professor of medicine at Emory University in Atlanta, Ga., and a member of the board of directors for the American Diabetes Association; however, for most general medicine and surgical patients who have low oral intake or are NPO, a recent trial reported that the administration of basal insulin alone plus correction doses with rapid-acting insulin analogs before meals is as good as a basal bolus regimen. A regimen should be tweaked throughout the inpatient’s stay with an aim to reach the goal of minimal or no hypoglycemia.1
Planning for a discharge regimen should start early in the hospital stay, Dr. Szumita says, and should be based on several factors:
- The patient’s Hb1c;
- The prior regimen and how it was performing;
- The patient’s wishes; and
- Collaboration with outpatient providers.
At discharge, it is critical that patients be clear about what medications they should be on post-discharge and that they follow-up with outpatient providers in a timely manner. TH
Karen Appold is a freelance writer in Pennsylvania.
Reference
- Umpierrez GE, Smiley D, Hermayer K, et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169-2174.
Although new medications to manage and treat hyperglycemia and diabetes continuously appear on the market, national guidelines and position statements consistently refer to insulin as the treatment of choice in the inpatient hospital setting.
“When patients are admitted to the hospital, our standard is to switch from the outpatient regimen [wide variety of medications] to the inpatient regimen—insulin,” says Paul M. Szumita, PharmD, BCPS, clinical pharmacy practice manager director at Brigham and Women’s Hospital in Boston.
For critically ill patients in ICUs or during the peri-operative period, intravenous infusion of insulin is preferred. Most general medicine and surgery patients are managed with subcutaneous insulin.
“Using a basal bolus regimen starting at a total daily dose of 0.3-0.5 unit/kg is sufficient for most patients,” says Guillermo Umpierrez, MD, CDE, FCAE, FACP, professor of medicine at Emory University in Atlanta, Ga., and a member of the board of directors for the American Diabetes Association; however, for most general medicine and surgical patients who have low oral intake or are NPO, a recent trial reported that the administration of basal insulin alone plus correction doses with rapid-acting insulin analogs before meals is as good as a basal bolus regimen. A regimen should be tweaked throughout the inpatient’s stay with an aim to reach the goal of minimal or no hypoglycemia.1
Planning for a discharge regimen should start early in the hospital stay, Dr. Szumita says, and should be based on several factors:
- The patient’s Hb1c;
- The prior regimen and how it was performing;
- The patient’s wishes; and
- Collaboration with outpatient providers.
At discharge, it is critical that patients be clear about what medications they should be on post-discharge and that they follow-up with outpatient providers in a timely manner. TH
Karen Appold is a freelance writer in Pennsylvania.
Reference
- Umpierrez GE, Smiley D, Hermayer K, et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169-2174.
Although new medications to manage and treat hyperglycemia and diabetes continuously appear on the market, national guidelines and position statements consistently refer to insulin as the treatment of choice in the inpatient hospital setting.
“When patients are admitted to the hospital, our standard is to switch from the outpatient regimen [wide variety of medications] to the inpatient regimen—insulin,” says Paul M. Szumita, PharmD, BCPS, clinical pharmacy practice manager director at Brigham and Women’s Hospital in Boston.
For critically ill patients in ICUs or during the peri-operative period, intravenous infusion of insulin is preferred. Most general medicine and surgery patients are managed with subcutaneous insulin.
“Using a basal bolus regimen starting at a total daily dose of 0.3-0.5 unit/kg is sufficient for most patients,” says Guillermo Umpierrez, MD, CDE, FCAE, FACP, professor of medicine at Emory University in Atlanta, Ga., and a member of the board of directors for the American Diabetes Association; however, for most general medicine and surgical patients who have low oral intake or are NPO, a recent trial reported that the administration of basal insulin alone plus correction doses with rapid-acting insulin analogs before meals is as good as a basal bolus regimen. A regimen should be tweaked throughout the inpatient’s stay with an aim to reach the goal of minimal or no hypoglycemia.1
Planning for a discharge regimen should start early in the hospital stay, Dr. Szumita says, and should be based on several factors:
- The patient’s Hb1c;
- The prior regimen and how it was performing;
- The patient’s wishes; and
- Collaboration with outpatient providers.
At discharge, it is critical that patients be clear about what medications they should be on post-discharge and that they follow-up with outpatient providers in a timely manner. TH
Karen Appold is a freelance writer in Pennsylvania.
Reference
- Umpierrez GE, Smiley D, Hermayer K, et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169-2174.
Medication Reconciliation Toolkit Updated, Available to Hospitalists
Adverse drug events and medication errors are unfortunately all too common within hospitals, but hospitalists can now take the lead in preventing them using SHM’s MARQUIS [Multi-Center Medication Reconciliation Quality Improvement Study] toolkit.
The authors of the new toolkit outline the hospitalist’s role in reducing medication errors as:
- Take responsibility for the accuracy of the medication reconciliation process for each patient under your care;
- Lead, coordinate, or participate in medication reconciliation quality improvement (QI) efforts with other key team members on the “front lines” to inform the hospital QI team on key interventions that would lead to improved patient outcomes;
- Become trained in taking the “best possible medication history” and in using effective discharge medication counseling; and
- Identify patients who are at high risk for a medication reconciliation error and would benefit from a more intensive medication reconciliation process.
“The MARQUIS study is important because it shows the potential of a mentored implementation effort, working with local hospitalist leaders and a QI toolkit, to improve medication safety related to the medication reconciliation process,” says MARQUIS principal investigator Jeff Schnipper, MD, MPH, FHM.
“It also shows the importance of institutional commitment to the success of these efforts. Lastly, hospitalists need to realize that medication reconciliation is not just some external regulatory requirement—it’s about the safety of the medications they order—and, therefore, that they need to ensure the quality of the process for the patients they care for and to lead efforts to improve the process across their hospitals.”
For more information, visit www.hospitalmedicine.org/marquis.
Adverse drug events and medication errors are unfortunately all too common within hospitals, but hospitalists can now take the lead in preventing them using SHM’s MARQUIS [Multi-Center Medication Reconciliation Quality Improvement Study] toolkit.
The authors of the new toolkit outline the hospitalist’s role in reducing medication errors as:
- Take responsibility for the accuracy of the medication reconciliation process for each patient under your care;
- Lead, coordinate, or participate in medication reconciliation quality improvement (QI) efforts with other key team members on the “front lines” to inform the hospital QI team on key interventions that would lead to improved patient outcomes;
- Become trained in taking the “best possible medication history” and in using effective discharge medication counseling; and
- Identify patients who are at high risk for a medication reconciliation error and would benefit from a more intensive medication reconciliation process.
“The MARQUIS study is important because it shows the potential of a mentored implementation effort, working with local hospitalist leaders and a QI toolkit, to improve medication safety related to the medication reconciliation process,” says MARQUIS principal investigator Jeff Schnipper, MD, MPH, FHM.
“It also shows the importance of institutional commitment to the success of these efforts. Lastly, hospitalists need to realize that medication reconciliation is not just some external regulatory requirement—it’s about the safety of the medications they order—and, therefore, that they need to ensure the quality of the process for the patients they care for and to lead efforts to improve the process across their hospitals.”
For more information, visit www.hospitalmedicine.org/marquis.
Adverse drug events and medication errors are unfortunately all too common within hospitals, but hospitalists can now take the lead in preventing them using SHM’s MARQUIS [Multi-Center Medication Reconciliation Quality Improvement Study] toolkit.
The authors of the new toolkit outline the hospitalist’s role in reducing medication errors as:
- Take responsibility for the accuracy of the medication reconciliation process for each patient under your care;
- Lead, coordinate, or participate in medication reconciliation quality improvement (QI) efforts with other key team members on the “front lines” to inform the hospital QI team on key interventions that would lead to improved patient outcomes;
- Become trained in taking the “best possible medication history” and in using effective discharge medication counseling; and
- Identify patients who are at high risk for a medication reconciliation error and would benefit from a more intensive medication reconciliation process.
“The MARQUIS study is important because it shows the potential of a mentored implementation effort, working with local hospitalist leaders and a QI toolkit, to improve medication safety related to the medication reconciliation process,” says MARQUIS principal investigator Jeff Schnipper, MD, MPH, FHM.
“It also shows the importance of institutional commitment to the success of these efforts. Lastly, hospitalists need to realize that medication reconciliation is not just some external regulatory requirement—it’s about the safety of the medications they order—and, therefore, that they need to ensure the quality of the process for the patients they care for and to lead efforts to improve the process across their hospitals.”
For more information, visit www.hospitalmedicine.org/marquis.
Registration for ASHP’s Medication Safety Collaborative Still Open
Maybe you just returned from HM14 in Las Vegas and are ready to head back. Or maybe you missed out on SHM’s annual meeting but would like to meet up with an important part of the hospitalist team: hospital and health system pharmacists.
Regardless of your motivation, the American Society of Health-System Pharmacist’s (ASHP’s) combination of three meetings in one brings a wealth of information to hospitalists—physicians and pharmacists alike—and now SHM members can register for the Medication Safety Collaborative at the applicable ASHP member rates.
SHM members receive the ASHP member rate at ASHP’s meeting within a meeting for hospital and health system pharmacists, to be held May 31-June 4 in Las Vegas.
Many hospitalists will be especially interested in the Medication Safety Collaborative, which brings the entire hospital team together to share best practices in medication and patient safety.
The Medication Safety Collaborative consists of three meetings:
- ASHP Informatics Institute: An event for informaticists to innovate, interact, and improve the use of information technology in healthcare;
- The Medication Safety Collaborative: For inter-professional teams of health system-based clinicians, coordinators, managers, and administrators who focus on patient safety and quality; and
- Pharmacy Practice Policy: The most relevant issues affecting health system pharmacy practice today at ASHP’s first Pharmacy Practice and Policy Meeting.
Maybe you just returned from HM14 in Las Vegas and are ready to head back. Or maybe you missed out on SHM’s annual meeting but would like to meet up with an important part of the hospitalist team: hospital and health system pharmacists.
Regardless of your motivation, the American Society of Health-System Pharmacist’s (ASHP’s) combination of three meetings in one brings a wealth of information to hospitalists—physicians and pharmacists alike—and now SHM members can register for the Medication Safety Collaborative at the applicable ASHP member rates.
SHM members receive the ASHP member rate at ASHP’s meeting within a meeting for hospital and health system pharmacists, to be held May 31-June 4 in Las Vegas.
Many hospitalists will be especially interested in the Medication Safety Collaborative, which brings the entire hospital team together to share best practices in medication and patient safety.
The Medication Safety Collaborative consists of three meetings:
- ASHP Informatics Institute: An event for informaticists to innovate, interact, and improve the use of information technology in healthcare;
- The Medication Safety Collaborative: For inter-professional teams of health system-based clinicians, coordinators, managers, and administrators who focus on patient safety and quality; and
- Pharmacy Practice Policy: The most relevant issues affecting health system pharmacy practice today at ASHP’s first Pharmacy Practice and Policy Meeting.
Maybe you just returned from HM14 in Las Vegas and are ready to head back. Or maybe you missed out on SHM’s annual meeting but would like to meet up with an important part of the hospitalist team: hospital and health system pharmacists.
Regardless of your motivation, the American Society of Health-System Pharmacist’s (ASHP’s) combination of three meetings in one brings a wealth of information to hospitalists—physicians and pharmacists alike—and now SHM members can register for the Medication Safety Collaborative at the applicable ASHP member rates.
SHM members receive the ASHP member rate at ASHP’s meeting within a meeting for hospital and health system pharmacists, to be held May 31-June 4 in Las Vegas.
Many hospitalists will be especially interested in the Medication Safety Collaborative, which brings the entire hospital team together to share best practices in medication and patient safety.
The Medication Safety Collaborative consists of three meetings:
- ASHP Informatics Institute: An event for informaticists to innovate, interact, and improve the use of information technology in healthcare;
- The Medication Safety Collaborative: For inter-professional teams of health system-based clinicians, coordinators, managers, and administrators who focus on patient safety and quality; and
- Pharmacy Practice Policy: The most relevant issues affecting health system pharmacy practice today at ASHP’s first Pharmacy Practice and Policy Meeting.