User login
Risks of watchful waiting in follicular lymphoma
A subset of follicular lymphoma (FL) patients managed with watchful waiting are vulnerable to organ dysfunction and transformation, according to research published in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study, about 24% of FL patients managed with watchful waiting developed significant organ dysfunction or transformation at first progression over 8.2 years of follow-up.
Organ dysfunction and transformation were associated with significantly worse overall survival (OS) that could not be predicted based on baseline characteristics.
Gwynivere A. Davies, MD, of the University of Calgary in Alberta, Canada, and her colleagues conducted this study using data from the Alberta Lymphoma Database. The team gathered data on patients with grade 1-3a FL who were diagnosed between 1994 and 2011.
The investigators identified 238 patients who were initially managed with watchful waiting. The patients had a median age of 54.1 years (range, 24.7-69.9) at diagnosis, and 83.2% were advanced stage.
The 10-year OS rate for these patients was 81.2%. At a median follow-up of 98.5 months, 71% (n=169) of patients had progressed and required therapy.
At the time of progression, 24.4% of patients (n=58) had organ dysfunction and/or transformation. The median time to organ dysfunction/transformation was 29.9 months.
These adverse outcomes were significantly associated with inferior OS. The 10-year OS rate was 65.4% for patients with transformation at progression and 83.2% for those without transformation (P=0.0017).
The 10-year OS rate was 71.5% for those with organ dysfunction at progression and 82.7% for those without organ dysfunction (P=0.028).
Comparison to treated patients
The investigators also looked at a comparison group of 236 FL patients managed with immediate rituximab-based chemotherapy (R-chemo), most of whom were scheduled to receive (72.9%) rituximab maintenance. Their median age was 52.1 (range, 27.3-65.4), and most (82.6%) had advanced stage disease.
At a median follow-up of 100.2 months, the median progression-free survival (PFS) was not reached. The 10-year OS rate was 84%.
The 10-year PFS rate after first R-chemo was 57.1% for patients who received immediate R-chemo (n=236) and 50.5% for patients who were initially managed with watchful waiting and proceeded to R-chemo (n=133; P=0.506). This was not affected by rituximab maintenance.
The investigators noted that OS measured from diagnosis was not affected by initial watchful waiting.
However, in a landmark analysis, OS was inferior when measured from R-chemo at first progression for watchful waiting recipients compared to patients who received immediate R-chemo. The 10-year OS rates were 74.4% and 84.0%, respectively (P=0.02).
The risk of transformation at first progression was significantly different between the groups. At 10 years, the rate of transformation was 25.5% in the watchful waiting group and 6.3% in the immediate R-chemo group (P<0.0001).
The investigators said these findings, taken together, suggest changes may be warranted for FL patients managed with watchful waiting.
“Consideration should be given to implementing standardized follow-up imaging, with early initiation of rituximab-based therapy if there is evidence of progression in an attempt to prevent these potentially clinically impactful events [i.e., organ dysfunction and transformation],” Dr. Davies and her coauthors wrote.
Dr. Davies reported no financial disclosures. Her coauthors reported disclosures related to Janssen, Gilead Sciences, Lundbeck, Roche, AbbVie, Amgen, Seattle Genetics, Bristol-Myers Squibb, Servier Laboratories, and Merck.
A subset of follicular lymphoma (FL) patients managed with watchful waiting are vulnerable to organ dysfunction and transformation, according to research published in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study, about 24% of FL patients managed with watchful waiting developed significant organ dysfunction or transformation at first progression over 8.2 years of follow-up.
Organ dysfunction and transformation were associated with significantly worse overall survival (OS) that could not be predicted based on baseline characteristics.
Gwynivere A. Davies, MD, of the University of Calgary in Alberta, Canada, and her colleagues conducted this study using data from the Alberta Lymphoma Database. The team gathered data on patients with grade 1-3a FL who were diagnosed between 1994 and 2011.
The investigators identified 238 patients who were initially managed with watchful waiting. The patients had a median age of 54.1 years (range, 24.7-69.9) at diagnosis, and 83.2% were advanced stage.
The 10-year OS rate for these patients was 81.2%. At a median follow-up of 98.5 months, 71% (n=169) of patients had progressed and required therapy.
At the time of progression, 24.4% of patients (n=58) had organ dysfunction and/or transformation. The median time to organ dysfunction/transformation was 29.9 months.
These adverse outcomes were significantly associated with inferior OS. The 10-year OS rate was 65.4% for patients with transformation at progression and 83.2% for those without transformation (P=0.0017).
The 10-year OS rate was 71.5% for those with organ dysfunction at progression and 82.7% for those without organ dysfunction (P=0.028).
Comparison to treated patients
The investigators also looked at a comparison group of 236 FL patients managed with immediate rituximab-based chemotherapy (R-chemo), most of whom were scheduled to receive (72.9%) rituximab maintenance. Their median age was 52.1 (range, 27.3-65.4), and most (82.6%) had advanced stage disease.
At a median follow-up of 100.2 months, the median progression-free survival (PFS) was not reached. The 10-year OS rate was 84%.
The 10-year PFS rate after first R-chemo was 57.1% for patients who received immediate R-chemo (n=236) and 50.5% for patients who were initially managed with watchful waiting and proceeded to R-chemo (n=133; P=0.506). This was not affected by rituximab maintenance.
The investigators noted that OS measured from diagnosis was not affected by initial watchful waiting.
However, in a landmark analysis, OS was inferior when measured from R-chemo at first progression for watchful waiting recipients compared to patients who received immediate R-chemo. The 10-year OS rates were 74.4% and 84.0%, respectively (P=0.02).
The risk of transformation at first progression was significantly different between the groups. At 10 years, the rate of transformation was 25.5% in the watchful waiting group and 6.3% in the immediate R-chemo group (P<0.0001).
The investigators said these findings, taken together, suggest changes may be warranted for FL patients managed with watchful waiting.
“Consideration should be given to implementing standardized follow-up imaging, with early initiation of rituximab-based therapy if there is evidence of progression in an attempt to prevent these potentially clinically impactful events [i.e., organ dysfunction and transformation],” Dr. Davies and her coauthors wrote.
Dr. Davies reported no financial disclosures. Her coauthors reported disclosures related to Janssen, Gilead Sciences, Lundbeck, Roche, AbbVie, Amgen, Seattle Genetics, Bristol-Myers Squibb, Servier Laboratories, and Merck.
A subset of follicular lymphoma (FL) patients managed with watchful waiting are vulnerable to organ dysfunction and transformation, according to research published in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study, about 24% of FL patients managed with watchful waiting developed significant organ dysfunction or transformation at first progression over 8.2 years of follow-up.
Organ dysfunction and transformation were associated with significantly worse overall survival (OS) that could not be predicted based on baseline characteristics.
Gwynivere A. Davies, MD, of the University of Calgary in Alberta, Canada, and her colleagues conducted this study using data from the Alberta Lymphoma Database. The team gathered data on patients with grade 1-3a FL who were diagnosed between 1994 and 2011.
The investigators identified 238 patients who were initially managed with watchful waiting. The patients had a median age of 54.1 years (range, 24.7-69.9) at diagnosis, and 83.2% were advanced stage.
The 10-year OS rate for these patients was 81.2%. At a median follow-up of 98.5 months, 71% (n=169) of patients had progressed and required therapy.
At the time of progression, 24.4% of patients (n=58) had organ dysfunction and/or transformation. The median time to organ dysfunction/transformation was 29.9 months.
These adverse outcomes were significantly associated with inferior OS. The 10-year OS rate was 65.4% for patients with transformation at progression and 83.2% for those without transformation (P=0.0017).
The 10-year OS rate was 71.5% for those with organ dysfunction at progression and 82.7% for those without organ dysfunction (P=0.028).
Comparison to treated patients
The investigators also looked at a comparison group of 236 FL patients managed with immediate rituximab-based chemotherapy (R-chemo), most of whom were scheduled to receive (72.9%) rituximab maintenance. Their median age was 52.1 (range, 27.3-65.4), and most (82.6%) had advanced stage disease.
At a median follow-up of 100.2 months, the median progression-free survival (PFS) was not reached. The 10-year OS rate was 84%.
The 10-year PFS rate after first R-chemo was 57.1% for patients who received immediate R-chemo (n=236) and 50.5% for patients who were initially managed with watchful waiting and proceeded to R-chemo (n=133; P=0.506). This was not affected by rituximab maintenance.
The investigators noted that OS measured from diagnosis was not affected by initial watchful waiting.
However, in a landmark analysis, OS was inferior when measured from R-chemo at first progression for watchful waiting recipients compared to patients who received immediate R-chemo. The 10-year OS rates were 74.4% and 84.0%, respectively (P=0.02).
The risk of transformation at first progression was significantly different between the groups. At 10 years, the rate of transformation was 25.5% in the watchful waiting group and 6.3% in the immediate R-chemo group (P<0.0001).
The investigators said these findings, taken together, suggest changes may be warranted for FL patients managed with watchful waiting.
“Consideration should be given to implementing standardized follow-up imaging, with early initiation of rituximab-based therapy if there is evidence of progression in an attempt to prevent these potentially clinically impactful events [i.e., organ dysfunction and transformation],” Dr. Davies and her coauthors wrote.
Dr. Davies reported no financial disclosures. Her coauthors reported disclosures related to Janssen, Gilead Sciences, Lundbeck, Roche, AbbVie, Amgen, Seattle Genetics, Bristol-Myers Squibb, Servier Laboratories, and Merck.
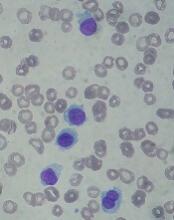
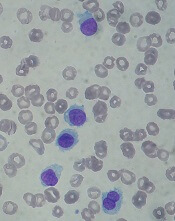
FDA approves drug for hairy cell leukemia
The U.S. Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a Boxed Warning noting that the drug poses risks of capillary leak syndrome (CLS) and hemolytic uremic syndrome (HUS). Treatment with moxetumomab pasudotox should be delayed or discontinued in patients who develop CLS and discontinued in patients with HUS.
The FDA granted the application for moxetumomab pasudotox fast track and priority review designations, and the drug received orphan drug designation from the FDA.
The agency granted the approval of moxetumomab pasudotox to AstraZeneca Pharmaceuticals based on results from a phase 3 trial (NCT01829711).
Data from this study were presented at the 2018 ASCO Annual Meeting (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75% (60/80), the complete response (CR) rate was 41% (33/80), and the durable CR rate was 30% (24/80). Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most frequent treatment-related adverse events (AEs) were nausea (28%), peripheral edema (26%), headache (21%), and pyrexia (20%). Other treatment-related AEs included infections (8%) and neutropenia (3%).
Treatment-related AEs that led to discontinuation included HUS (5%), CLS (3%), and increased blood creatinine (3%).
In all, seven patients (9%) had CLS, and seven (9%) had HUS. This includes four (5%) patients who had both. CLS and HUS proved manageable and reversible.
There were three deaths in this trial, but none of them were considered treatment-related.
The U.S. Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a Boxed Warning noting that the drug poses risks of capillary leak syndrome (CLS) and hemolytic uremic syndrome (HUS). Treatment with moxetumomab pasudotox should be delayed or discontinued in patients who develop CLS and discontinued in patients with HUS.
The FDA granted the application for moxetumomab pasudotox fast track and priority review designations, and the drug received orphan drug designation from the FDA.
The agency granted the approval of moxetumomab pasudotox to AstraZeneca Pharmaceuticals based on results from a phase 3 trial (NCT01829711).
Data from this study were presented at the 2018 ASCO Annual Meeting (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75% (60/80), the complete response (CR) rate was 41% (33/80), and the durable CR rate was 30% (24/80). Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most frequent treatment-related adverse events (AEs) were nausea (28%), peripheral edema (26%), headache (21%), and pyrexia (20%). Other treatment-related AEs included infections (8%) and neutropenia (3%).
Treatment-related AEs that led to discontinuation included HUS (5%), CLS (3%), and increased blood creatinine (3%).
In all, seven patients (9%) had CLS, and seven (9%) had HUS. This includes four (5%) patients who had both. CLS and HUS proved manageable and reversible.
There were three deaths in this trial, but none of them were considered treatment-related.
The U.S. Food and Drug Administration (FDA) has approved moxetumomab pasudotox-tdfk (Lumoxiti), a CD22-directed cytotoxin, to treat hairy cell leukemia (HCL).
Moxetumomab pasudotox is approved to treat adults with relapsed or refractory HCL who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
The prescribing information for moxetumomab pasudotox includes a Boxed Warning noting that the drug poses risks of capillary leak syndrome (CLS) and hemolytic uremic syndrome (HUS). Treatment with moxetumomab pasudotox should be delayed or discontinued in patients who develop CLS and discontinued in patients with HUS.
The FDA granted the application for moxetumomab pasudotox fast track and priority review designations, and the drug received orphan drug designation from the FDA.
The agency granted the approval of moxetumomab pasudotox to AstraZeneca Pharmaceuticals based on results from a phase 3 trial (NCT01829711).
Data from this study were presented at the 2018 ASCO Annual Meeting (abstract 7004).
The trial included 80 patients with relapsed or refractory HCL who had received at least two prior lines of therapy.
At a median of 16.7 months of follow-up, the objective response rate was 75% (60/80), the complete response (CR) rate was 41% (33/80), and the durable CR rate was 30% (24/80). Durable CR was defined as CR with hematologic remission for more than 180 days.
Most patients with a CR achieved minimal residual disease negativity (82%; 27/33).
The median duration of response was not reached, nor was the median progression-free survival.
The most frequent treatment-related adverse events (AEs) were nausea (28%), peripheral edema (26%), headache (21%), and pyrexia (20%). Other treatment-related AEs included infections (8%) and neutropenia (3%).
Treatment-related AEs that led to discontinuation included HUS (5%), CLS (3%), and increased blood creatinine (3%).
In all, seven patients (9%) had CLS, and seven (9%) had HUS. This includes four (5%) patients who had both. CLS and HUS proved manageable and reversible.
There were three deaths in this trial, but none of them were considered treatment-related.
MRD data added to venetoclax label
The U.S. Food and Drug Administration (FDA) has expanded the label for venetoclax tablets (Venclexta®) to include data on minimal residual disease (MRD).
The drug’s prescribing information now includes details on MRD negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was FDA approved in June for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL.
The patients were randomized to receive:
- Venetoclax at 400 mg daily for 24 months (after a 5-week ramp-up period) plus rituximab at 375 mg/m2 on day 1 for the first cycle and at 500 mg/m2 on day 1 for cycles 2 to 6 (n=194)
- Bendamustine at 70 mg/m2 on days 1 and 2 for 6 cycles plus rituximab at the same schedule as the venetoclax arm (n=195).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction, and the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood 3 months after the last dose of rituximab. At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response (CR) or CR with incomplete marrow recovery (CRi). MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Three percent (3/106) of patients in the venetoclax arm who achieved CR/CRi were MRD negative in both the peripheral blood and the bone marrow.
“The rates of MRD negativity seen with Venclexta plus rituximab are very encouraging,” said MURANO investigator John Seymour, MBBS, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Additional results from the MURANO trial were published in The New England Journal of Medicine in March and are included in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the U.S. and by AbbVie outside the U.S.
The U.S. Food and Drug Administration (FDA) has expanded the label for venetoclax tablets (Venclexta®) to include data on minimal residual disease (MRD).
The drug’s prescribing information now includes details on MRD negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was FDA approved in June for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL.
The patients were randomized to receive:
- Venetoclax at 400 mg daily for 24 months (after a 5-week ramp-up period) plus rituximab at 375 mg/m2 on day 1 for the first cycle and at 500 mg/m2 on day 1 for cycles 2 to 6 (n=194)
- Bendamustine at 70 mg/m2 on days 1 and 2 for 6 cycles plus rituximab at the same schedule as the venetoclax arm (n=195).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction, and the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood 3 months after the last dose of rituximab. At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response (CR) or CR with incomplete marrow recovery (CRi). MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Three percent (3/106) of patients in the venetoclax arm who achieved CR/CRi were MRD negative in both the peripheral blood and the bone marrow.
“The rates of MRD negativity seen with Venclexta plus rituximab are very encouraging,” said MURANO investigator John Seymour, MBBS, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Additional results from the MURANO trial were published in The New England Journal of Medicine in March and are included in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the U.S. and by AbbVie outside the U.S.
The U.S. Food and Drug Administration (FDA) has expanded the label for venetoclax tablets (Venclexta®) to include data on minimal residual disease (MRD).
The drug’s prescribing information now includes details on MRD negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was FDA approved in June for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL.
The patients were randomized to receive:
- Venetoclax at 400 mg daily for 24 months (after a 5-week ramp-up period) plus rituximab at 375 mg/m2 on day 1 for the first cycle and at 500 mg/m2 on day 1 for cycles 2 to 6 (n=194)
- Bendamustine at 70 mg/m2 on days 1 and 2 for 6 cycles plus rituximab at the same schedule as the venetoclax arm (n=195).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction, and the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood 3 months after the last dose of rituximab. At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response (CR) or CR with incomplete marrow recovery (CRi). MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Three percent (3/106) of patients in the venetoclax arm who achieved CR/CRi were MRD negative in both the peripheral blood and the bone marrow.
“The rates of MRD negativity seen with Venclexta plus rituximab are very encouraging,” said MURANO investigator John Seymour, MBBS, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Additional results from the MURANO trial were published in The New England Journal of Medicine in March and are included in the prescribing information for venetoclax.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the U.S. and by AbbVie outside the U.S.
Regimens produce similar results in FL
Rituximab plus lenalidomide had efficacy similar to that of rituximab plus chemotherapy in the treatment of follicular lymphoma (FL) in a phase 3 trial.
Patients with previously untreated FL had similar complete response (CR) rates and progression-free survival (PFS) rates whether they received rituximab-based chemotherapy or rituximab plus lenalidomide.
These results were published in The New England Journal of Medicine.
The trial, RELEVANCE, included 1,030 patients with previously untreated FL. They were randomized to receive rituximab plus chemotherapy (n=517) or rituximab plus lenalidomide (n=513) for 18 cycles.
Patients in the chemotherapy arm received one of three regimens—R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone), rituximab and bendamustine, or R-CVP (rituximab, cyclophosphamide, vincristine, and prednisone).
Patients in both treatment arms went on to receive rituximab maintenance every 8 weeks for 12 cycles. The total duration of treatment was 120 weeks. The median age of the combined groups was 59 years.
The coprimary endpoints were CR (confirmed or unconfirmed) and PFS. After a median follow-up of 37.9 months, the rates of coprimary endpoints were similar between the treatment arms.
CR was observed in 48% of the rituximab-lenalidomide arm and 53% of the rituximab-chemotherapy arm (P=0.13).
The interim 3-year PFS rate was 77% in the rituximab-lenalidomide arm and 78% in the rituximab-chemotherapy arm. The hazard ratio for progression or death from any cause was 1.10 (P=0.48).
The efficacy of rituximab plus chemotherapy was greater in low-risk patients (based on Follicular Lymphoma International Prognostic Index scores) and in patients whose disease was Ann Arbor stage I or II, whereas the efficacy of rituximab-lenalidomide was independent of prognostic factors.
Safety was the biggest area of difference, with some adverse events (AEs) being more common in one arm than the other.
AEs that were more common with rituximab-lenalidomide include cutaneous reactions (43% vs 24%), diarrhea (37% vs 19%), rash (29% vs 8%), abdominal pain (15% vs 9%), peripheral edema (14% vs 9%), muscle spasms (13% vs 4%), myalgia (14% vs 6%), and tumor flare reaction (6% vs <1%).
AEs that were more common with rituximab-chemotherapy were anemia (89% vs 66%), fatigue (29% vs 23%), nausea (42% vs 20%), vomiting (19% vs 7%), febrile neutropenia (7% vs 2%), leukopenia (10% vs 4%), and peripheral neuropathy (16% vs 7%).
Grade 3/4 cutaneous reactions were more common with rituximab-lenalidomide (7% vs 1%), and grade 3/4 neutropenia was more common with rituximab-chemotherapy (50% vs 32%).
The RELEVANCE trial was sponsored by Celgene and the Lymphoma Academic Research Organisation. The study authors reported various disclosures, including financial ties to Celgene.
Rituximab plus lenalidomide had efficacy similar to that of rituximab plus chemotherapy in the treatment of follicular lymphoma (FL) in a phase 3 trial.
Patients with previously untreated FL had similar complete response (CR) rates and progression-free survival (PFS) rates whether they received rituximab-based chemotherapy or rituximab plus lenalidomide.
These results were published in The New England Journal of Medicine.
The trial, RELEVANCE, included 1,030 patients with previously untreated FL. They were randomized to receive rituximab plus chemotherapy (n=517) or rituximab plus lenalidomide (n=513) for 18 cycles.
Patients in the chemotherapy arm received one of three regimens—R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone), rituximab and bendamustine, or R-CVP (rituximab, cyclophosphamide, vincristine, and prednisone).
Patients in both treatment arms went on to receive rituximab maintenance every 8 weeks for 12 cycles. The total duration of treatment was 120 weeks. The median age of the combined groups was 59 years.
The coprimary endpoints were CR (confirmed or unconfirmed) and PFS. After a median follow-up of 37.9 months, the rates of coprimary endpoints were similar between the treatment arms.
CR was observed in 48% of the rituximab-lenalidomide arm and 53% of the rituximab-chemotherapy arm (P=0.13).
The interim 3-year PFS rate was 77% in the rituximab-lenalidomide arm and 78% in the rituximab-chemotherapy arm. The hazard ratio for progression or death from any cause was 1.10 (P=0.48).
The efficacy of rituximab plus chemotherapy was greater in low-risk patients (based on Follicular Lymphoma International Prognostic Index scores) and in patients whose disease was Ann Arbor stage I or II, whereas the efficacy of rituximab-lenalidomide was independent of prognostic factors.
Safety was the biggest area of difference, with some adverse events (AEs) being more common in one arm than the other.
AEs that were more common with rituximab-lenalidomide include cutaneous reactions (43% vs 24%), diarrhea (37% vs 19%), rash (29% vs 8%), abdominal pain (15% vs 9%), peripheral edema (14% vs 9%), muscle spasms (13% vs 4%), myalgia (14% vs 6%), and tumor flare reaction (6% vs <1%).
AEs that were more common with rituximab-chemotherapy were anemia (89% vs 66%), fatigue (29% vs 23%), nausea (42% vs 20%), vomiting (19% vs 7%), febrile neutropenia (7% vs 2%), leukopenia (10% vs 4%), and peripheral neuropathy (16% vs 7%).
Grade 3/4 cutaneous reactions were more common with rituximab-lenalidomide (7% vs 1%), and grade 3/4 neutropenia was more common with rituximab-chemotherapy (50% vs 32%).
The RELEVANCE trial was sponsored by Celgene and the Lymphoma Academic Research Organisation. The study authors reported various disclosures, including financial ties to Celgene.
Rituximab plus lenalidomide had efficacy similar to that of rituximab plus chemotherapy in the treatment of follicular lymphoma (FL) in a phase 3 trial.
Patients with previously untreated FL had similar complete response (CR) rates and progression-free survival (PFS) rates whether they received rituximab-based chemotherapy or rituximab plus lenalidomide.
These results were published in The New England Journal of Medicine.
The trial, RELEVANCE, included 1,030 patients with previously untreated FL. They were randomized to receive rituximab plus chemotherapy (n=517) or rituximab plus lenalidomide (n=513) for 18 cycles.
Patients in the chemotherapy arm received one of three regimens—R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone), rituximab and bendamustine, or R-CVP (rituximab, cyclophosphamide, vincristine, and prednisone).
Patients in both treatment arms went on to receive rituximab maintenance every 8 weeks for 12 cycles. The total duration of treatment was 120 weeks. The median age of the combined groups was 59 years.
The coprimary endpoints were CR (confirmed or unconfirmed) and PFS. After a median follow-up of 37.9 months, the rates of coprimary endpoints were similar between the treatment arms.
CR was observed in 48% of the rituximab-lenalidomide arm and 53% of the rituximab-chemotherapy arm (P=0.13).
The interim 3-year PFS rate was 77% in the rituximab-lenalidomide arm and 78% in the rituximab-chemotherapy arm. The hazard ratio for progression or death from any cause was 1.10 (P=0.48).
The efficacy of rituximab plus chemotherapy was greater in low-risk patients (based on Follicular Lymphoma International Prognostic Index scores) and in patients whose disease was Ann Arbor stage I or II, whereas the efficacy of rituximab-lenalidomide was independent of prognostic factors.
Safety was the biggest area of difference, with some adverse events (AEs) being more common in one arm than the other.
AEs that were more common with rituximab-lenalidomide include cutaneous reactions (43% vs 24%), diarrhea (37% vs 19%), rash (29% vs 8%), abdominal pain (15% vs 9%), peripheral edema (14% vs 9%), muscle spasms (13% vs 4%), myalgia (14% vs 6%), and tumor flare reaction (6% vs <1%).
AEs that were more common with rituximab-chemotherapy were anemia (89% vs 66%), fatigue (29% vs 23%), nausea (42% vs 20%), vomiting (19% vs 7%), febrile neutropenia (7% vs 2%), leukopenia (10% vs 4%), and peripheral neuropathy (16% vs 7%).
Grade 3/4 cutaneous reactions were more common with rituximab-lenalidomide (7% vs 1%), and grade 3/4 neutropenia was more common with rituximab-chemotherapy (50% vs 32%).
The RELEVANCE trial was sponsored by Celgene and the Lymphoma Academic Research Organisation. The study authors reported various disclosures, including financial ties to Celgene.
Ibrutinib maintains efficacy over time
Extended follow-up of the RESONATE-2 trial showed that first-line ibrutinib sustained efficacy in elderly patients with chronic lymphocytic leukemia (CLL).
Patients who received ibrutinib had a long-term progression-free survival benefit over those who received chlorambucil.
The depth of response to ibrutinib improved over time, which meant there was a substantial increase in the proportion of patients achieving complete response.
Additionally, rates of some serious adverse events associated with ibrutinib decreased over time.
Paul M. Barr, MD, of the University of Rochester in New York, and his colleagues reported these findings in Haematologica.
Previously reported results of the RESONATE-2 trial, which showed an 84% reduction in the risk of death for ibrutinib versus chlorambucil, led to the approval of ibrutinib for first-line CLL treatment, the authors said.
The study included 269 patients with untreated CLL or small lymphocytic lymphoma who had active disease and were at least 65 years of age. They were randomized to receive ibrutinib (n=136) or chlorambucil (n=133).
At a median follow-up of 29 months, 79% (107/136) of patients remained on ibrutinib.
There was an 88% reduction in the risk of progression or death for patients randomized to ibrutinib (P<0.0001).
The rate of complete response improved over time in ibrutinib-treated patients, from 7% at 12 months to 15% at 24 months and 18% at 36 months (maximum follow-up).
The overall response rate (ORR) with ibrutinib was 92%, with comparable findings in high-risk subgroups. The ORR was 100% in patients with del(11q) and 95% in those with unmutated IGHV.
Lymphadenopathy improved in most ibrutinib-treated patients, with complete resolution in 42%, compared to 7% of patients who received chlorambucil.
Splenomegaly improved by at least 50% in 95% of ibrutinib-treated patients and 52% in chlorambucil recipients, with complete resolution in 56% and 22%, respectively.
Adverse events of grade 3 or greater were generally seen more often in the first year of ibrutinib therapy and decreased over time.
The rate of grade 3 or higher neutropenia decreased from 8.1% in the first 12 months of treatment to 0% in the third year. The rate of grade 3 or higher anemia decreased from 5.9% to 1%. And the rate of grade 3 or higher thrombocytopenia decreased from 2.2% to 0%.
The rate of atrial fibrillation increased from 6% in the primary analysis to 10% in extended follow-up. However, investigators said ibrutinib dose reductions and discontinuations because of this adverse event were uncommon and less frequent with extended treatment.
“Atrial fibrillation therefore appears manageable and does not frequently necessitate ibrutinib discontinuation,” they concluded.
This study was supported by Pharmacyclics, an AbbVie company, and by grants from the National Institutes of Health and the MD Anderson Moon Shot Program in CLL. Pharmacyclics designed the study and performed analysis of the data. Several study authors reported funding from various companies, including Pharmacyclics.
Extended follow-up of the RESONATE-2 trial showed that first-line ibrutinib sustained efficacy in elderly patients with chronic lymphocytic leukemia (CLL).
Patients who received ibrutinib had a long-term progression-free survival benefit over those who received chlorambucil.
The depth of response to ibrutinib improved over time, which meant there was a substantial increase in the proportion of patients achieving complete response.
Additionally, rates of some serious adverse events associated with ibrutinib decreased over time.
Paul M. Barr, MD, of the University of Rochester in New York, and his colleagues reported these findings in Haematologica.
Previously reported results of the RESONATE-2 trial, which showed an 84% reduction in the risk of death for ibrutinib versus chlorambucil, led to the approval of ibrutinib for first-line CLL treatment, the authors said.
The study included 269 patients with untreated CLL or small lymphocytic lymphoma who had active disease and were at least 65 years of age. They were randomized to receive ibrutinib (n=136) or chlorambucil (n=133).
At a median follow-up of 29 months, 79% (107/136) of patients remained on ibrutinib.
There was an 88% reduction in the risk of progression or death for patients randomized to ibrutinib (P<0.0001).
The rate of complete response improved over time in ibrutinib-treated patients, from 7% at 12 months to 15% at 24 months and 18% at 36 months (maximum follow-up).
The overall response rate (ORR) with ibrutinib was 92%, with comparable findings in high-risk subgroups. The ORR was 100% in patients with del(11q) and 95% in those with unmutated IGHV.
Lymphadenopathy improved in most ibrutinib-treated patients, with complete resolution in 42%, compared to 7% of patients who received chlorambucil.
Splenomegaly improved by at least 50% in 95% of ibrutinib-treated patients and 52% in chlorambucil recipients, with complete resolution in 56% and 22%, respectively.
Adverse events of grade 3 or greater were generally seen more often in the first year of ibrutinib therapy and decreased over time.
The rate of grade 3 or higher neutropenia decreased from 8.1% in the first 12 months of treatment to 0% in the third year. The rate of grade 3 or higher anemia decreased from 5.9% to 1%. And the rate of grade 3 or higher thrombocytopenia decreased from 2.2% to 0%.
The rate of atrial fibrillation increased from 6% in the primary analysis to 10% in extended follow-up. However, investigators said ibrutinib dose reductions and discontinuations because of this adverse event were uncommon and less frequent with extended treatment.
“Atrial fibrillation therefore appears manageable and does not frequently necessitate ibrutinib discontinuation,” they concluded.
This study was supported by Pharmacyclics, an AbbVie company, and by grants from the National Institutes of Health and the MD Anderson Moon Shot Program in CLL. Pharmacyclics designed the study and performed analysis of the data. Several study authors reported funding from various companies, including Pharmacyclics.
Extended follow-up of the RESONATE-2 trial showed that first-line ibrutinib sustained efficacy in elderly patients with chronic lymphocytic leukemia (CLL).
Patients who received ibrutinib had a long-term progression-free survival benefit over those who received chlorambucil.
The depth of response to ibrutinib improved over time, which meant there was a substantial increase in the proportion of patients achieving complete response.
Additionally, rates of some serious adverse events associated with ibrutinib decreased over time.
Paul M. Barr, MD, of the University of Rochester in New York, and his colleagues reported these findings in Haematologica.
Previously reported results of the RESONATE-2 trial, which showed an 84% reduction in the risk of death for ibrutinib versus chlorambucil, led to the approval of ibrutinib for first-line CLL treatment, the authors said.
The study included 269 patients with untreated CLL or small lymphocytic lymphoma who had active disease and were at least 65 years of age. They were randomized to receive ibrutinib (n=136) or chlorambucil (n=133).
At a median follow-up of 29 months, 79% (107/136) of patients remained on ibrutinib.
There was an 88% reduction in the risk of progression or death for patients randomized to ibrutinib (P<0.0001).
The rate of complete response improved over time in ibrutinib-treated patients, from 7% at 12 months to 15% at 24 months and 18% at 36 months (maximum follow-up).
The overall response rate (ORR) with ibrutinib was 92%, with comparable findings in high-risk subgroups. The ORR was 100% in patients with del(11q) and 95% in those with unmutated IGHV.
Lymphadenopathy improved in most ibrutinib-treated patients, with complete resolution in 42%, compared to 7% of patients who received chlorambucil.
Splenomegaly improved by at least 50% in 95% of ibrutinib-treated patients and 52% in chlorambucil recipients, with complete resolution in 56% and 22%, respectively.
Adverse events of grade 3 or greater were generally seen more often in the first year of ibrutinib therapy and decreased over time.
The rate of grade 3 or higher neutropenia decreased from 8.1% in the first 12 months of treatment to 0% in the third year. The rate of grade 3 or higher anemia decreased from 5.9% to 1%. And the rate of grade 3 or higher thrombocytopenia decreased from 2.2% to 0%.
The rate of atrial fibrillation increased from 6% in the primary analysis to 10% in extended follow-up. However, investigators said ibrutinib dose reductions and discontinuations because of this adverse event were uncommon and less frequent with extended treatment.
“Atrial fibrillation therefore appears manageable and does not frequently necessitate ibrutinib discontinuation,” they concluded.
This study was supported by Pharmacyclics, an AbbVie company, and by grants from the National Institutes of Health and the MD Anderson Moon Shot Program in CLL. Pharmacyclics designed the study and performed analysis of the data. Several study authors reported funding from various companies, including Pharmacyclics.
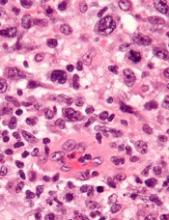
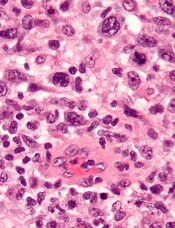
TYK2 inhibitors could treat ALCL, team says
Preclinical research indicates that TYK2 inhibitors could be effective in treating anaplastic large-cell lymphoma (ALCL).
Researchers found evidence to suggest that TYK2 “is highly expressed in all cases of human ALCL.”
The team also discovered that TYK2 inhibition induces apoptosis in ALCL cells, and it delays tumor onset and prolongs survival in a mouse model of ALCL.
Olaf Merkel, PhD, of the Medical University of Vienna in Austria, and his colleagues detailed these findings in Leukemia.
The researchers said their analyses suggest TYK2 is expressed in all types of ALCL, regardless of ALK status, and TYK2 mediates the same anti-apoptotic response across ALCLs.
“Therefore, we could consider TYK2 signaling as the Achilles’ heel of ALCL, as, in all patients we have analyzed, the tumor cells relied on this activity to support the essential survival signal,” Dr. Merkel said.
He and his colleagues found that disrupting TYK2—either via gene knockdown or with small-molecule TYK2 inhibitors—induced apoptosis in human ALCL cells in vitro.
In a mouse model of NPM-ALK-induced lymphoma, Tyk2 deletion slowed the rate of tumor growth and significantly prolonged survival. The median survival was 53.3 weeks in mice with Tyk2 deletion and 16.0 weeks in control mice (P<0.0001).
Additional experiments in human ALCL cell lines showed that “TYK2 is activated by autocrine production of IL-10 and IL-22 and by interaction with specific receptors expressed by the cells,” the researchers said.
They also found that “activated TYK2 leads to STAT1 and STAT3 phosphorylation, activated expression of MCL1, and aberrant ALCL cell survival.”
Taking these findings together, the researchers concluded that TYK2 inhibitors could be effective for treating ALCL.
“We are looking forward to TYK2 inhibitors becoming available . . . ,” said study author Lukas Kenner, MD, of the Medical University of Vienna.
“[I]n the more rare lymphomas, we urgently need better therapies.”
Preclinical research indicates that TYK2 inhibitors could be effective in treating anaplastic large-cell lymphoma (ALCL).
Researchers found evidence to suggest that TYK2 “is highly expressed in all cases of human ALCL.”
The team also discovered that TYK2 inhibition induces apoptosis in ALCL cells, and it delays tumor onset and prolongs survival in a mouse model of ALCL.
Olaf Merkel, PhD, of the Medical University of Vienna in Austria, and his colleagues detailed these findings in Leukemia.
The researchers said their analyses suggest TYK2 is expressed in all types of ALCL, regardless of ALK status, and TYK2 mediates the same anti-apoptotic response across ALCLs.
“Therefore, we could consider TYK2 signaling as the Achilles’ heel of ALCL, as, in all patients we have analyzed, the tumor cells relied on this activity to support the essential survival signal,” Dr. Merkel said.
He and his colleagues found that disrupting TYK2—either via gene knockdown or with small-molecule TYK2 inhibitors—induced apoptosis in human ALCL cells in vitro.
In a mouse model of NPM-ALK-induced lymphoma, Tyk2 deletion slowed the rate of tumor growth and significantly prolonged survival. The median survival was 53.3 weeks in mice with Tyk2 deletion and 16.0 weeks in control mice (P<0.0001).
Additional experiments in human ALCL cell lines showed that “TYK2 is activated by autocrine production of IL-10 and IL-22 and by interaction with specific receptors expressed by the cells,” the researchers said.
They also found that “activated TYK2 leads to STAT1 and STAT3 phosphorylation, activated expression of MCL1, and aberrant ALCL cell survival.”
Taking these findings together, the researchers concluded that TYK2 inhibitors could be effective for treating ALCL.
“We are looking forward to TYK2 inhibitors becoming available . . . ,” said study author Lukas Kenner, MD, of the Medical University of Vienna.
“[I]n the more rare lymphomas, we urgently need better therapies.”
Preclinical research indicates that TYK2 inhibitors could be effective in treating anaplastic large-cell lymphoma (ALCL).
Researchers found evidence to suggest that TYK2 “is highly expressed in all cases of human ALCL.”
The team also discovered that TYK2 inhibition induces apoptosis in ALCL cells, and it delays tumor onset and prolongs survival in a mouse model of ALCL.
Olaf Merkel, PhD, of the Medical University of Vienna in Austria, and his colleagues detailed these findings in Leukemia.
The researchers said their analyses suggest TYK2 is expressed in all types of ALCL, regardless of ALK status, and TYK2 mediates the same anti-apoptotic response across ALCLs.
“Therefore, we could consider TYK2 signaling as the Achilles’ heel of ALCL, as, in all patients we have analyzed, the tumor cells relied on this activity to support the essential survival signal,” Dr. Merkel said.
He and his colleagues found that disrupting TYK2—either via gene knockdown or with small-molecule TYK2 inhibitors—induced apoptosis in human ALCL cells in vitro.
In a mouse model of NPM-ALK-induced lymphoma, Tyk2 deletion slowed the rate of tumor growth and significantly prolonged survival. The median survival was 53.3 weeks in mice with Tyk2 deletion and 16.0 weeks in control mice (P<0.0001).
Additional experiments in human ALCL cell lines showed that “TYK2 is activated by autocrine production of IL-10 and IL-22 and by interaction with specific receptors expressed by the cells,” the researchers said.
They also found that “activated TYK2 leads to STAT1 and STAT3 phosphorylation, activated expression of MCL1, and aberrant ALCL cell survival.”
Taking these findings together, the researchers concluded that TYK2 inhibitors could be effective for treating ALCL.
“We are looking forward to TYK2 inhibitors becoming available . . . ,” said study author Lukas Kenner, MD, of the Medical University of Vienna.
“[I]n the more rare lymphomas, we urgently need better therapies.”
Predicting early outcomes in DLBCL
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to researchers.
Pretreatment ctDNA levels predicted 24-month event-free survival as well as overall survival in a prospective study.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy.
Ash A. Alizadeh, MD, PhD, of Stanford University in California, and his colleagues reported these findings in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, the researchers wrote.
In an evaluation of pretreatment ctDNA levels, the researchers found a 2.5 log haploid genome equivalents per milliliter threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P=0.007) for frontline treatment and 2.9 (P=0.01) for salvage therapy.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy.
An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P=0.0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P<0.001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index and interim PET/CT studies, results of multivariable analyses showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, according to researchers. Conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to researchers.
Pretreatment ctDNA levels predicted 24-month event-free survival as well as overall survival in a prospective study.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy.
Ash A. Alizadeh, MD, PhD, of Stanford University in California, and his colleagues reported these findings in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, the researchers wrote.
In an evaluation of pretreatment ctDNA levels, the researchers found a 2.5 log haploid genome equivalents per milliliter threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P=0.007) for frontline treatment and 2.9 (P=0.01) for salvage therapy.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy.
An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P=0.0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P<0.001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index and interim PET/CT studies, results of multivariable analyses showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, according to researchers. Conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
Measurement of circulating tumor DNA (ctDNA) could be a new and useful tool for predicting survival outcomes and response to therapy in patients with diffuse large B-cell lymphoma (DLBCL), according to researchers.
Pretreatment ctDNA levels predicted 24-month event-free survival as well as overall survival in a prospective study.
Changes in ctDNA during treatment were prognostic for outcomes as early as 21 days into therapy.
Ash A. Alizadeh, MD, PhD, of Stanford University in California, and his colleagues reported these findings in the Journal of Clinical Oncology.
ctDNA was detected in 98% of the 217 patients evaluated, which demonstrated the “potentially universal applicability” of this approach, the researchers wrote.
In an evaluation of pretreatment ctDNA levels, the researchers found a 2.5 log haploid genome equivalents per milliliter threshold stratified patient outcomes. Event-free survival was significantly inferior at 24 months in patients with ctDNA above that threshold, with hazard ratios of 2.6 (P=0.007) for frontline treatment and 2.9 (P=0.01) for salvage therapy.
On-treatment ctDNA levels were favorably prognostic for outcomes in patients receiving frontline therapy.
An early molecular response (EMR), defined as a 2-log decrease in ctDNA levels after one cycle of treatment, was associated with a 24-month event-free survival of 83% versus 50% for no EMR (P=0.0015).
Major molecular response (MMR), defined as a 2.5-log drop in ctDNA after two cycles of treatment, was associated with a 24-month event-free survival of 82% versus 46% for no MMR in patients on frontline therapy (P<0.001).
In one cohort of patients receiving salvage therapy, EMR also predicted superior 24-month event-free survival.
The EMR measure was also favorably prognostic for overall survival in both the frontline and salvage settings.
The prognostic value of measuring ctDNA was independent of International Prognostic Index and interim PET/CT studies, results of multivariable analyses showed.
Patients had “excellent outcomes” if they had both molecular response and favorable interim PET results, according to researchers. Conversely, patients were at “extremely high risk” for treatment failure if they had no molecular response and a positive PET scan.
“The identification of patients at exceptionally high risk (i.e., interim PET/CT positive and not achieving EMR/MMR) could provide an opportunity for early intervention with alternative treatments, including autologous bone marrow transplantation or chimeric antigen receptor T cells,” the researchers wrote.
Patients in the study were all treated with combination immunochemotherapy according to local standards.
Dr. Alizadeh reported disclosures related to CiberMed, Forty Seven, Janssen Oncology, Celgene, Roche/Genentech, and Gilead, as well as patent filings on ctDNA detection assigned to Stanford University.
NICE says CAR T-cell therapy isn’t cost-effective
The National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending against the use of axicabtagene ciloleucel (Yescarta) in England.
Axicabtagene ciloleucel is a chimeric antigen receptor (CAR) T-cell therapy that was just approved by the European Commission to treat patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) or primary mediastinal B-cell lymphoma (PMBCL) who have received two or more lines of systemic therapy.
However, NICE has said it isn’t clear how much of a benefit axicabtagene ciloleucel may provide over salvage chemotherapy.
Additionally, the cost of axicabtagene ciloleucel is too high for the therapy to be considered a cost-effective use of National Health Service (NHS) resources.
NICE’s draft guidance points out that there is no standard treatment for patients with relapsed or refractory DLBCL or PMBCL who have received two or more systemic therapies. These patients receive best supportive care, which usually includes salvage chemotherapy.
Results from the ZUMA-1 trial suggest the majority of DLBCL/PMBCL patients given axicabtagene ciloleucel do respond to treatment.
However, there is no direct data comparing axicabtagene ciloleucel with salvage chemotherapy, so the benefit of the CAR T-cell therapy over chemotherapy is unknown.
The draft guidance also notes that axicabtagene ciloleucel meets NICE’s criteria to be considered a life-extending treatment at the end of life.
However, the CAR T-cell therapy cannot be considered a cost-effective use of NHS resources. The cost-effectiveness estimates for axicabtagene ciloleucel, compared with salvage chemotherapy, were above £50,000 per year of quality adjusted life gained, the upper limit of the specially extended range of cost-effectiveness for cancer treatments.
Furthermore, axicabtagene ciloleucel does not meet the criteria for inclusion in the Cancer Drugs Fund. NICE said axicabtagene ciloleucel does not have the plausible potential to be cost effective, which would be necessary for inclusion in the fund while further evidence of the treatment’s longer-term benefits is collected.
“Although promising, there is still much more we need to know about CAR-T, and, unfortunately, in this case, we are not able to recommend axicabtagene ciloleucel for use in the NHS in England at the cost per patient set by Kite Pharma,” said Meindert Boysen, director of the centre for health technology evaluation at NICE.
The consultation period for the draft guidance runs until September 18, 2018.
The National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending against the use of axicabtagene ciloleucel (Yescarta) in England.
Axicabtagene ciloleucel is a chimeric antigen receptor (CAR) T-cell therapy that was just approved by the European Commission to treat patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) or primary mediastinal B-cell lymphoma (PMBCL) who have received two or more lines of systemic therapy.
However, NICE has said it isn’t clear how much of a benefit axicabtagene ciloleucel may provide over salvage chemotherapy.
Additionally, the cost of axicabtagene ciloleucel is too high for the therapy to be considered a cost-effective use of National Health Service (NHS) resources.
NICE’s draft guidance points out that there is no standard treatment for patients with relapsed or refractory DLBCL or PMBCL who have received two or more systemic therapies. These patients receive best supportive care, which usually includes salvage chemotherapy.
Results from the ZUMA-1 trial suggest the majority of DLBCL/PMBCL patients given axicabtagene ciloleucel do respond to treatment.
However, there is no direct data comparing axicabtagene ciloleucel with salvage chemotherapy, so the benefit of the CAR T-cell therapy over chemotherapy is unknown.
The draft guidance also notes that axicabtagene ciloleucel meets NICE’s criteria to be considered a life-extending treatment at the end of life.
However, the CAR T-cell therapy cannot be considered a cost-effective use of NHS resources. The cost-effectiveness estimates for axicabtagene ciloleucel, compared with salvage chemotherapy, were above £50,000 per year of quality adjusted life gained, the upper limit of the specially extended range of cost-effectiveness for cancer treatments.
Furthermore, axicabtagene ciloleucel does not meet the criteria for inclusion in the Cancer Drugs Fund. NICE said axicabtagene ciloleucel does not have the plausible potential to be cost effective, which would be necessary for inclusion in the fund while further evidence of the treatment’s longer-term benefits is collected.
“Although promising, there is still much more we need to know about CAR-T, and, unfortunately, in this case, we are not able to recommend axicabtagene ciloleucel for use in the NHS in England at the cost per patient set by Kite Pharma,” said Meindert Boysen, director of the centre for health technology evaluation at NICE.
The consultation period for the draft guidance runs until September 18, 2018.
The National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending against the use of axicabtagene ciloleucel (Yescarta) in England.
Axicabtagene ciloleucel is a chimeric antigen receptor (CAR) T-cell therapy that was just approved by the European Commission to treat patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) or primary mediastinal B-cell lymphoma (PMBCL) who have received two or more lines of systemic therapy.
However, NICE has said it isn’t clear how much of a benefit axicabtagene ciloleucel may provide over salvage chemotherapy.
Additionally, the cost of axicabtagene ciloleucel is too high for the therapy to be considered a cost-effective use of National Health Service (NHS) resources.
NICE’s draft guidance points out that there is no standard treatment for patients with relapsed or refractory DLBCL or PMBCL who have received two or more systemic therapies. These patients receive best supportive care, which usually includes salvage chemotherapy.
Results from the ZUMA-1 trial suggest the majority of DLBCL/PMBCL patients given axicabtagene ciloleucel do respond to treatment.
However, there is no direct data comparing axicabtagene ciloleucel with salvage chemotherapy, so the benefit of the CAR T-cell therapy over chemotherapy is unknown.
The draft guidance also notes that axicabtagene ciloleucel meets NICE’s criteria to be considered a life-extending treatment at the end of life.
However, the CAR T-cell therapy cannot be considered a cost-effective use of NHS resources. The cost-effectiveness estimates for axicabtagene ciloleucel, compared with salvage chemotherapy, were above £50,000 per year of quality adjusted life gained, the upper limit of the specially extended range of cost-effectiveness for cancer treatments.
Furthermore, axicabtagene ciloleucel does not meet the criteria for inclusion in the Cancer Drugs Fund. NICE said axicabtagene ciloleucel does not have the plausible potential to be cost effective, which would be necessary for inclusion in the fund while further evidence of the treatment’s longer-term benefits is collected.
“Although promising, there is still much more we need to know about CAR-T, and, unfortunately, in this case, we are not able to recommend axicabtagene ciloleucel for use in the NHS in England at the cost per patient set by Kite Pharma,” said Meindert Boysen, director of the centre for health technology evaluation at NICE.
The consultation period for the draft guidance runs until September 18, 2018.
EC approves CAR T-cell therapy for DLBCL, PMBCL
The European Commission (EC) has approved the chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (Yescarta®) to treat two types of lymphoma.
Axicabtagene ciloleucel is now approved to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and primary mediastinal large B-cell lymphoma (PMBCL) after two or more lines of systemic therapy.
The approval extends to all member countries of the European Union, as well as Norway, Iceland, and Liechtenstein.
The EC’s approval of axicabtagene ciloleucel is supported by data from the ZUMA-1 trial.
Results from this phase 2 trial were presented at the 2017 ASH Annual Meeting and published simultaneously in NEJM.
The trial enrolled 111 patients with relapsed/refractory B-cell lymphomas. There were 101 patients who received axicabtagene ciloleucel—77 with DLBCL, 8 with PMBCL, and 16 with transformed follicular lymphoma (TFL).
Patients received conditioning with low-dose cyclophosphamide and fludarabine, followed by axicabtagene ciloleucel.
The objective response rate (ORR) was 82% (n=83), and the complete response (CR) rate was 54% (n=55).
Among the DLBCL patients, the ORR was 82% (63/77), and the CR rate was 49% (38/77). In the patients with PMBCL or TFL, the ORR was 83% (20/24), and the CR rate was 71% (17/24).
With a median follow-up of 15.4 months, 42% of patients retained their response, and 40% retained a CR.
At 18 months, the overall survival rate was 52%. Most deaths were due to disease progression.
However, 2 patients died of adverse events related to axicabtagene ciloleucel, both cytokine release syndrome.
The most common grade 3 or higher adverse events were neutropenia (78%), anemia (43%), thrombocytopenia (38%), and febrile neutropenia (31%).
Grade 3 or higher cytokine release syndrome occurred in 13% of patients, and grade 3 or higher neurologic events occurred in 28%.
The European Commission (EC) has approved the chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (Yescarta®) to treat two types of lymphoma.
Axicabtagene ciloleucel is now approved to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and primary mediastinal large B-cell lymphoma (PMBCL) after two or more lines of systemic therapy.
The approval extends to all member countries of the European Union, as well as Norway, Iceland, and Liechtenstein.
The EC’s approval of axicabtagene ciloleucel is supported by data from the ZUMA-1 trial.
Results from this phase 2 trial were presented at the 2017 ASH Annual Meeting and published simultaneously in NEJM.
The trial enrolled 111 patients with relapsed/refractory B-cell lymphomas. There were 101 patients who received axicabtagene ciloleucel—77 with DLBCL, 8 with PMBCL, and 16 with transformed follicular lymphoma (TFL).
Patients received conditioning with low-dose cyclophosphamide and fludarabine, followed by axicabtagene ciloleucel.
The objective response rate (ORR) was 82% (n=83), and the complete response (CR) rate was 54% (n=55).
Among the DLBCL patients, the ORR was 82% (63/77), and the CR rate was 49% (38/77). In the patients with PMBCL or TFL, the ORR was 83% (20/24), and the CR rate was 71% (17/24).
With a median follow-up of 15.4 months, 42% of patients retained their response, and 40% retained a CR.
At 18 months, the overall survival rate was 52%. Most deaths were due to disease progression.
However, 2 patients died of adverse events related to axicabtagene ciloleucel, both cytokine release syndrome.
The most common grade 3 or higher adverse events were neutropenia (78%), anemia (43%), thrombocytopenia (38%), and febrile neutropenia (31%).
Grade 3 or higher cytokine release syndrome occurred in 13% of patients, and grade 3 or higher neurologic events occurred in 28%.
The European Commission (EC) has approved the chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (Yescarta®) to treat two types of lymphoma.
Axicabtagene ciloleucel is now approved to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and primary mediastinal large B-cell lymphoma (PMBCL) after two or more lines of systemic therapy.
The approval extends to all member countries of the European Union, as well as Norway, Iceland, and Liechtenstein.
The EC’s approval of axicabtagene ciloleucel is supported by data from the ZUMA-1 trial.
Results from this phase 2 trial were presented at the 2017 ASH Annual Meeting and published simultaneously in NEJM.
The trial enrolled 111 patients with relapsed/refractory B-cell lymphomas. There were 101 patients who received axicabtagene ciloleucel—77 with DLBCL, 8 with PMBCL, and 16 with transformed follicular lymphoma (TFL).
Patients received conditioning with low-dose cyclophosphamide and fludarabine, followed by axicabtagene ciloleucel.
The objective response rate (ORR) was 82% (n=83), and the complete response (CR) rate was 54% (n=55).
Among the DLBCL patients, the ORR was 82% (63/77), and the CR rate was 49% (38/77). In the patients with PMBCL or TFL, the ORR was 83% (20/24), and the CR rate was 71% (17/24).
With a median follow-up of 15.4 months, 42% of patients retained their response, and 40% retained a CR.
At 18 months, the overall survival rate was 52%. Most deaths were due to disease progression.
However, 2 patients died of adverse events related to axicabtagene ciloleucel, both cytokine release syndrome.
The most common grade 3 or higher adverse events were neutropenia (78%), anemia (43%), thrombocytopenia (38%), and febrile neutropenia (31%).
Grade 3 or higher cytokine release syndrome occurred in 13% of patients, and grade 3 or higher neurologic events occurred in 28%.
EC approves CAR T-cell therapy for ALL, DLBCL
The European Commission (EC) has granted approval for tisagenlecleucel (Kymriah®), a chimeric antigen receptor (CAR) T-cell therapy targeting CD19.
Tisagenlecleucel (formerly CTL019) is now approved for use in pediatric and young adult patients up to 25 years of age with B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse post-transplant, or in second or later relapse.
Tisagenlecleucel is also approved to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who have received two or more lines of systemic therapy.
The EC’s approval extends to all member countries of the European Union, as well as Norway, Iceland, and Liechtenstein.
Novartis expects to launch tisagenlecleucel initially for pediatric ALL. The company said timing for tisagenlecleucel availability in each country will depend on multiple factors, including the onboarding of qualified treatment centers for the appropriate indications, as well as the completion of national reimbursement procedures.
The EC’s approval of tisagenlecleucel is based on results from the phase 2 JULIET and ELIANA trials.
JULIET trial
Updated results from JULIET were presented at the 23rd Annual Congress of the European Hematology Association in June (abstract S799).
The trial enrolled 165 adults with relapsed/refractory DLBCL, and 111 of them received a single infusion of tisagenlecleucel. Most of the patients who discontinued before dosing did so due to disease progression or clinical deterioration. The patients’ median age at baseline was 56 (range, 22-76).
Ninety-two percent of patients received bridging therapy, and 93% received lymphodepleting chemotherapy prior to tisagenlecleucel.
The median time from infusion to data cutoff was 13.9 months.
The overall response rate was 52%, and the complete response (CR) rate was 40%. The median duration of response was not reached.
At the time of data cutoff, none of the responders had gone on to receive a stem cell transplant.
For all infused patients (n=111), the 12-month overall survival (OS) rate was 49%, and the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome (CRS). Fifteen percent of patients received tocilizumab for CRS, including 3% of patients with grade 2 CRS and 50% of patients with grade 3 CRS.
Other adverse events (AEs) of interest included grade 3/4 neurologic events (12%), grade 3/4 cytopenias lasting more than 28 days (32%), grade 3/4 infections (20%), and grade 3/4 febrile neutropenia (15%).
ELIANA trial
Updated results from ELIANA were published in NEJM in February.
The trial included 75 children and young adults with relapsed/refractory ALL. The patients’ median age was 11 (range, 3 to 23).
All 75 patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CR with incomplete hematologic recovery (CRi) within 3 months.
The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to transplant while in remission. At last follow-up, 4 were still in remission, and 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least one AE, and 95% had AEs thought to be related to tisagenlecleucel. The rate of grade 3/4 AEs was 88%, and the rate of related grade 3/4 AEs was 73%.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).
The European Commission (EC) has granted approval for tisagenlecleucel (Kymriah®), a chimeric antigen receptor (CAR) T-cell therapy targeting CD19.
Tisagenlecleucel (formerly CTL019) is now approved for use in pediatric and young adult patients up to 25 years of age with B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse post-transplant, or in second or later relapse.
Tisagenlecleucel is also approved to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who have received two or more lines of systemic therapy.
The EC’s approval extends to all member countries of the European Union, as well as Norway, Iceland, and Liechtenstein.
Novartis expects to launch tisagenlecleucel initially for pediatric ALL. The company said timing for tisagenlecleucel availability in each country will depend on multiple factors, including the onboarding of qualified treatment centers for the appropriate indications, as well as the completion of national reimbursement procedures.
The EC’s approval of tisagenlecleucel is based on results from the phase 2 JULIET and ELIANA trials.
JULIET trial
Updated results from JULIET were presented at the 23rd Annual Congress of the European Hematology Association in June (abstract S799).
The trial enrolled 165 adults with relapsed/refractory DLBCL, and 111 of them received a single infusion of tisagenlecleucel. Most of the patients who discontinued before dosing did so due to disease progression or clinical deterioration. The patients’ median age at baseline was 56 (range, 22-76).
Ninety-two percent of patients received bridging therapy, and 93% received lymphodepleting chemotherapy prior to tisagenlecleucel.
The median time from infusion to data cutoff was 13.9 months.
The overall response rate was 52%, and the complete response (CR) rate was 40%. The median duration of response was not reached.
At the time of data cutoff, none of the responders had gone on to receive a stem cell transplant.
For all infused patients (n=111), the 12-month overall survival (OS) rate was 49%, and the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome (CRS). Fifteen percent of patients received tocilizumab for CRS, including 3% of patients with grade 2 CRS and 50% of patients with grade 3 CRS.
Other adverse events (AEs) of interest included grade 3/4 neurologic events (12%), grade 3/4 cytopenias lasting more than 28 days (32%), grade 3/4 infections (20%), and grade 3/4 febrile neutropenia (15%).
ELIANA trial
Updated results from ELIANA were published in NEJM in February.
The trial included 75 children and young adults with relapsed/refractory ALL. The patients’ median age was 11 (range, 3 to 23).
All 75 patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CR with incomplete hematologic recovery (CRi) within 3 months.
The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to transplant while in remission. At last follow-up, 4 were still in remission, and 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least one AE, and 95% had AEs thought to be related to tisagenlecleucel. The rate of grade 3/4 AEs was 88%, and the rate of related grade 3/4 AEs was 73%.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).
The European Commission (EC) has granted approval for tisagenlecleucel (Kymriah®), a chimeric antigen receptor (CAR) T-cell therapy targeting CD19.
Tisagenlecleucel (formerly CTL019) is now approved for use in pediatric and young adult patients up to 25 years of age with B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse post-transplant, or in second or later relapse.
Tisagenlecleucel is also approved to treat adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who have received two or more lines of systemic therapy.
The EC’s approval extends to all member countries of the European Union, as well as Norway, Iceland, and Liechtenstein.
Novartis expects to launch tisagenlecleucel initially for pediatric ALL. The company said timing for tisagenlecleucel availability in each country will depend on multiple factors, including the onboarding of qualified treatment centers for the appropriate indications, as well as the completion of national reimbursement procedures.
The EC’s approval of tisagenlecleucel is based on results from the phase 2 JULIET and ELIANA trials.
JULIET trial
Updated results from JULIET were presented at the 23rd Annual Congress of the European Hematology Association in June (abstract S799).
The trial enrolled 165 adults with relapsed/refractory DLBCL, and 111 of them received a single infusion of tisagenlecleucel. Most of the patients who discontinued before dosing did so due to disease progression or clinical deterioration. The patients’ median age at baseline was 56 (range, 22-76).
Ninety-two percent of patients received bridging therapy, and 93% received lymphodepleting chemotherapy prior to tisagenlecleucel.
The median time from infusion to data cutoff was 13.9 months.
The overall response rate was 52%, and the complete response (CR) rate was 40%. The median duration of response was not reached.
At the time of data cutoff, none of the responders had gone on to receive a stem cell transplant.
For all infused patients (n=111), the 12-month overall survival (OS) rate was 49%, and the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome (CRS). Fifteen percent of patients received tocilizumab for CRS, including 3% of patients with grade 2 CRS and 50% of patients with grade 3 CRS.
Other adverse events (AEs) of interest included grade 3/4 neurologic events (12%), grade 3/4 cytopenias lasting more than 28 days (32%), grade 3/4 infections (20%), and grade 3/4 febrile neutropenia (15%).
ELIANA trial
Updated results from ELIANA were published in NEJM in February.
The trial included 75 children and young adults with relapsed/refractory ALL. The patients’ median age was 11 (range, 3 to 23).
All 75 patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CR with incomplete hematologic recovery (CRi) within 3 months.
The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to transplant while in remission. At last follow-up, 4 were still in remission, and 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least one AE, and 95% had AEs thought to be related to tisagenlecleucel. The rate of grade 3/4 AEs was 88%, and the rate of related grade 3/4 AEs was 73%.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).