User login
Duvelisib NDA granted priority review
The US Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for duvelisib, a dual PI3K delta/gamma inhibitor.
With this NDA, Verastem, Inc., is seeking full approval of duvelisib for the treatment of relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval of the drug for the treatment of relapsed or refractory follicular lymphoma (FL).
The FDA expects to make a decision on the NDA by October 5, 2018.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The application for duvelisib is supported by data from DUO™, a randomized, phase 3 study of patients with relapsed or refractory CLL/SLL, and DYNAMO™, a phase 2 study of patients with refractory indolent non-Hodgkin lymphoma.
Phase 3 DUO trial
Results from DUO were presented at the 2017 ASH Annual Meeting in December.
This study included 319 CLL/SLL patients who were randomized 1:1 to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The study’s primary endpoint was met, as duvelisib conferred a significant improvement in median progression-free survival (PFS) over ofatumumab.
Per an independent review committee, the median PFS was 13.3 months with duvelisib and 9.9 months with ofatumumab (hazard ratio=0.52; P<0.0001). Duvelisib maintained a PFS advantage in all patient subgroups analyzed.
The overall response rate was 73.8% with duvelisib and 45.3% with ofatumumab (P<0.0001). The complete response rate was 0.6% in both arms.
Overall survival (OS) was similar in the duvelisib and ofatumumab arms (hazard ratio=0.99; P=0.4807). The median OS was not reached in either arm.
The most common grade 3 or higher adverse events (AEs)—in the duvelisib and ofatumumab arms, respectively—were neutropenia (30% vs 17%), anemia (13% vs 5%), diarrhea (15% vs 1%), pneumonia (14% vs 1%), and colitis (12% vs 1%).
Thirty-five percent of patients discontinued duvelisib due to an AE.
Severe opportunistic infections occurred in 6% of duvelisib recipients—bronchopulmonary aspergillosis (n=4), fungal infection (n=2), Pneumocystis jirovecii pneumonia (n=2), and cytomegalovirus colitis (n=1).
There were 4 deaths related to duvelisib—staphylococcal pneumonia (n=2), general physical health deterioration (n=1), and sepsis (n=1).
Phase 2 DYNAMO trial
Results from DYNAMO were presented at the 22nd EHA Congress (abstract S777) in June 2017.
This trial enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate, per an independent review committee, was 43%. One patient achieved a complete response, and 35 had a partial response. The median duration of response was 7.9 months.
The median PFS was 8.3 months, and the median OS was 27.8 months.
The most common grade 3 or higher AEs were neutropenia (22%), anemia (13%), diarrhea (16%), lipase increase (10%), and thrombocytopenia (9%).
There were 2 serious opportunistic infections—Pneumocystis pneumonia and fungal pneumonia.
There were 3 deaths attributed to duvelisib—toxic epidermal necrolysis/sepsis syndrome (n=1), drug reaction/eosinophilia/systemic symptoms (n=1), and pneumonitis/pneumonia (n=1).
The US Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for duvelisib, a dual PI3K delta/gamma inhibitor.
With this NDA, Verastem, Inc., is seeking full approval of duvelisib for the treatment of relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval of the drug for the treatment of relapsed or refractory follicular lymphoma (FL).
The FDA expects to make a decision on the NDA by October 5, 2018.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The application for duvelisib is supported by data from DUO™, a randomized, phase 3 study of patients with relapsed or refractory CLL/SLL, and DYNAMO™, a phase 2 study of patients with refractory indolent non-Hodgkin lymphoma.
Phase 3 DUO trial
Results from DUO were presented at the 2017 ASH Annual Meeting in December.
This study included 319 CLL/SLL patients who were randomized 1:1 to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The study’s primary endpoint was met, as duvelisib conferred a significant improvement in median progression-free survival (PFS) over ofatumumab.
Per an independent review committee, the median PFS was 13.3 months with duvelisib and 9.9 months with ofatumumab (hazard ratio=0.52; P<0.0001). Duvelisib maintained a PFS advantage in all patient subgroups analyzed.
The overall response rate was 73.8% with duvelisib and 45.3% with ofatumumab (P<0.0001). The complete response rate was 0.6% in both arms.
Overall survival (OS) was similar in the duvelisib and ofatumumab arms (hazard ratio=0.99; P=0.4807). The median OS was not reached in either arm.
The most common grade 3 or higher adverse events (AEs)—in the duvelisib and ofatumumab arms, respectively—were neutropenia (30% vs 17%), anemia (13% vs 5%), diarrhea (15% vs 1%), pneumonia (14% vs 1%), and colitis (12% vs 1%).
Thirty-five percent of patients discontinued duvelisib due to an AE.
Severe opportunistic infections occurred in 6% of duvelisib recipients—bronchopulmonary aspergillosis (n=4), fungal infection (n=2), Pneumocystis jirovecii pneumonia (n=2), and cytomegalovirus colitis (n=1).
There were 4 deaths related to duvelisib—staphylococcal pneumonia (n=2), general physical health deterioration (n=1), and sepsis (n=1).
Phase 2 DYNAMO trial
Results from DYNAMO were presented at the 22nd EHA Congress (abstract S777) in June 2017.
This trial enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate, per an independent review committee, was 43%. One patient achieved a complete response, and 35 had a partial response. The median duration of response was 7.9 months.
The median PFS was 8.3 months, and the median OS was 27.8 months.
The most common grade 3 or higher AEs were neutropenia (22%), anemia (13%), diarrhea (16%), lipase increase (10%), and thrombocytopenia (9%).
There were 2 serious opportunistic infections—Pneumocystis pneumonia and fungal pneumonia.
There were 3 deaths attributed to duvelisib—toxic epidermal necrolysis/sepsis syndrome (n=1), drug reaction/eosinophilia/systemic symptoms (n=1), and pneumonitis/pneumonia (n=1).
The US Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for duvelisib, a dual PI3K delta/gamma inhibitor.
With this NDA, Verastem, Inc., is seeking full approval of duvelisib for the treatment of relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval of the drug for the treatment of relapsed or refractory follicular lymphoma (FL).
The FDA expects to make a decision on the NDA by October 5, 2018.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The application for duvelisib is supported by data from DUO™, a randomized, phase 3 study of patients with relapsed or refractory CLL/SLL, and DYNAMO™, a phase 2 study of patients with refractory indolent non-Hodgkin lymphoma.
Phase 3 DUO trial
Results from DUO were presented at the 2017 ASH Annual Meeting in December.
This study included 319 CLL/SLL patients who were randomized 1:1 to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The study’s primary endpoint was met, as duvelisib conferred a significant improvement in median progression-free survival (PFS) over ofatumumab.
Per an independent review committee, the median PFS was 13.3 months with duvelisib and 9.9 months with ofatumumab (hazard ratio=0.52; P<0.0001). Duvelisib maintained a PFS advantage in all patient subgroups analyzed.
The overall response rate was 73.8% with duvelisib and 45.3% with ofatumumab (P<0.0001). The complete response rate was 0.6% in both arms.
Overall survival (OS) was similar in the duvelisib and ofatumumab arms (hazard ratio=0.99; P=0.4807). The median OS was not reached in either arm.
The most common grade 3 or higher adverse events (AEs)—in the duvelisib and ofatumumab arms, respectively—were neutropenia (30% vs 17%), anemia (13% vs 5%), diarrhea (15% vs 1%), pneumonia (14% vs 1%), and colitis (12% vs 1%).
Thirty-five percent of patients discontinued duvelisib due to an AE.
Severe opportunistic infections occurred in 6% of duvelisib recipients—bronchopulmonary aspergillosis (n=4), fungal infection (n=2), Pneumocystis jirovecii pneumonia (n=2), and cytomegalovirus colitis (n=1).
There were 4 deaths related to duvelisib—staphylococcal pneumonia (n=2), general physical health deterioration (n=1), and sepsis (n=1).
Phase 2 DYNAMO trial
Results from DYNAMO were presented at the 22nd EHA Congress (abstract S777) in June 2017.
This trial enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate, per an independent review committee, was 43%. One patient achieved a complete response, and 35 had a partial response. The median duration of response was 7.9 months.
The median PFS was 8.3 months, and the median OS was 27.8 months.
The most common grade 3 or higher AEs were neutropenia (22%), anemia (13%), diarrhea (16%), lipase increase (10%), and thrombocytopenia (9%).
There were 2 serious opportunistic infections—Pneumocystis pneumonia and fungal pneumonia.
There were 3 deaths attributed to duvelisib—toxic epidermal necrolysis/sepsis syndrome (n=1), drug reaction/eosinophilia/systemic symptoms (n=1), and pneumonitis/pneumonia (n=1).
Project provides ‘unprecedented understanding’ of cancers
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
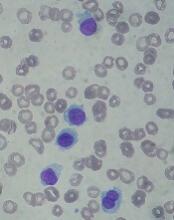
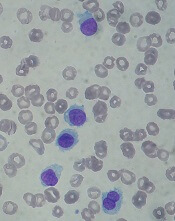
Drug receives priority review for HCL
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
ICER assesses value of CAR T-cell therapies
The Institute for Clinical and Economic Review (ICER) has made policy recommendations intended to ensure affordability and access to chimeric antigen receptor (CAR) T-cell therapies.
ICER released a Final Evidence Report on tisagenlecleucel (Kymriah, Novartis) and axicabtagene ciloleucel (Yescarta, Kite Pharma/Gilead), 2 CAR T-cell therapies approved in the US to treat B-cell acute lymphoblastic leukemia (B-ALL) and non-Hodgkin lymphoma (NHL), respectively.
The report says the pricing of these therapies aligns with patient benefit, but changes will be needed in future pricing, payment, and delivery mechanisms to ensure patient access without threatening health system affordability.
“Given the currently available evidence, these therapies appear to be effective options for those with B-ALL or NHL, though uncertainty in the evidence raised questions around the long-term value for money,” said Dan Ollendorf, PhD, ICER’s chief scientific officer.
Net health benefit
ICER’s report says tisagenlecleucel provides a net health benefit for children with B-ALL, and both tisagenlecleucel and axicabtagene ciloleucel provide a net health benefit for adults with certain types of NHL. (Novartis is seeking approval for tisagenlecleucel in NHL).
The evidence suggests there is at least a small net health benefit of the CAR T-cell therapies compared to other therapies. The benefit may be substantial, but uncertainties remain.
The data show complete remission (CR), disease-free survival (DFS), and overall survival (OS) rates are superior for NHL patients who receive axicabtagene ciloleucel, compared to patients who receive standard chemoimmunotherapy regimens.
Similarly, B-ALL patients treated with tisagenlecleucel have superior CR, DFS, and OS rates to patients treated with standard therapies. CR and OS rates are also superior in NHL patients treated with tisagenlecleucel, but DFS has not been reported in this population.
The report says there is insufficient evidence to distinguish between the 2 CAR T-cell therapies for the treatment of NHL.
Toxicity and uncertainty
The report highlights the fact that cytokine release syndrome, neurological symptoms, and B-cell aplasia have been observed in patients who receive CAR T-cell therapies. However, these sometimes severe adverse events are generally “manageable.”
In addition to toxicity, the report highlights sources of uncertainty. These include the fact that studies of tisagenlecleucel and axicabtagene ciloleucel are small, single-arm trials with short follow-up; comparisons with historical controls may be misleading; and improvements in the CAR T-cell manufacturing process may change outcomes.
Cost-effectiveness
The report states that the cost-effectiveness of each therapy fell below or within commonly cited thresholds of $50,000 to $150,000 per quality-adjusted life-year (QALY) over a lifetime.
For its analyses, ICER used the wholesale acquisition cost (WAC) plus an assumed hospital mark-up. The analyses were also based on the assumption that survival benefits observed in clinical trials would continue after the trials ended.
For tisagenlecleucel in pediatric B-ALL, the WAC is $475,000. The long-term cost-effectiveness compared to clofarabine is $45,871 per QALY gained.
For axicabtagene ciloleucel in adults with NHL, the WAC is $373,000. The long-term cost-effectiveness compared to salvage chemotherapy is $136,078 per QALY gained. The effectiveness assumptions for chemotherapy were based on an average of salvage chemotherapy regimens from the SCHOLAR-1 trial, and the cost assumptions were based on the cost of the R-DHAP (rituximab, dexamethasone, cytarabine, and cisplatin) regimen.
The report says tisagenlecleucel’s price would remain in alignment with value even if price premiums of 102% to 194% were applied.
Meanwhile, axicabtagene ciloleucel’s price could be increased by up to 11% and remain in alignment with the upper threshold ($150,000 per QALY gained) but would need to be discounted by 28% to align with the lower threshold ($100,000 per QALY gained).
Tisagenlecleucel, as a treatment for B-ALL, is not expected to cross the $915 million threshold for annual budget impact.
However, the short-term costs of axicabtagene ciloleucel for relapsed/refractory NHL could exceed the threshold. Only 38% of the estimated 5900 eligible patients could receive axicabtagene ciloleucel in a year before crossing the threshold.
Because of these findings, ICER issued an “Affordability and Access Alert” for axicabtagene ciloleucel.
This alert is intended to signal when the added costs associated with a new treatment may be difficult for the healthcare system to absorb over the short-term without displacing other needed services or contributing to unsustainable growth in healthcare insurance costs.
“Based on current evidence, both therapies appear to be priced in alignment with their clinical value, but there are potential short-term affordability concerns—for axicabtagene ciloleucel under its current indication and for both treatments should they receive future approvals for broader patient populations,” Dr Ollendorf said.
Panel voting results
ICER’s report was reviewed at a public meeting of the California Technology Assessment Forum on March 2.
Most of the panel said tisagenlecleucel provides intermediate long-term value for money when treating B-ALL. However, the significant uncertainty surrounding the long-term risks and benefits of the therapy precluded a high-value vote.
After deliberating on the value of axicabtagene ciloleucel to treat NHL, the panel’s votes were split between low-value and intermediate-value, driven by similar concerns about long-term uncertainty.
Policy recommendations
Following the voting session, ICER convened a policy roundtable of experts, including physicians, patient advocates, manufacturer representatives, and payer representatives.
Based on the roundtable discussion, ICER developed recommendations for enhanced stakeholder communication, innovative payment models, generation of additional evidence, settings of care, and patient education.
“With many other potentially transformative therapies in the pipeline, stakeholders must collaborate now to develop payment and delivery systems that can ensure timely patient access, manage short-term affordability for expensive one-time treatments, and continue to reward the innovation that brings these new treatments to market,” Dr Ollendorf said.
Some of ICER’s recommendations include:
- When launching novel therapies approved with limited clinical evidence, such as CAR T-cell therapies, manufacturers and payers should consider using a lower launch price that could be increased if substantial clinical benefits are confirmed or using a higher initial price tied to a requirement for refunds or rebates if real-world evidence fails to confirm high expectations.
- Outcomes-based pricing arrangements must be linked to “meaningful clinical outcomes assessed with sufficient follow up.”
- Hospital mark-up for CAR T-cell therapies “should reflect the expected additional cost for care delivered in the hospital, rather than a percentage of the drug cost to avoid perverse incentives in choosing the treatment location.”
- Initially, CAR T-cell therapies should be delivered in “manufacturer-accredited centers to ensure the quality and appropriateness of care.” Later, “centers of excellence accredited by specialty societies” can administer these therapies, as long as providers have “sufficient expertise” to manage serious side effects.
- Centers should ensure that patients understand what to expect from CAR T-cell therapy, including long-term consequences.
- Because additional evidence on CAR T-cell therapies is needed, all patients who receive these therapies should enter into a registry with planned long-term follow-up.
- Studies should determine the optimal timing of CAR T-cell therapy in the sequence of treatments for B-ALL and NHL.
Additional recommendations and more details are available in ICER’s report.
About ICER
ICER is an independent, non-profit research institute that produces reports analyzing evidence on the effectiveness and value of drugs and other medical services.
ICER’s reports include evidence-based calculations of prices for new drugs that reflect the degree of improvement expected in long-term patient outcomes, while also highlighting price levels that might contribute to unaffordable short-term cost growth for the overall healthcare system.
ICER’s reports incorporate input from stakeholders and are the subject of public hearings through 3 core programs: the California Technology Assessment Forum, the Midwest Comparative Effectiveness Public Advisory Council, and the New England Comparative Effectiveness Public Advisory Council.
These independent panels review ICER’s reports at public meetings to deliberate on the evidence and develop recommendations for how patients, clinicians, insurers, and policymakers can improve the quality and value of healthcare.
The Institute for Clinical and Economic Review (ICER) has made policy recommendations intended to ensure affordability and access to chimeric antigen receptor (CAR) T-cell therapies.
ICER released a Final Evidence Report on tisagenlecleucel (Kymriah, Novartis) and axicabtagene ciloleucel (Yescarta, Kite Pharma/Gilead), 2 CAR T-cell therapies approved in the US to treat B-cell acute lymphoblastic leukemia (B-ALL) and non-Hodgkin lymphoma (NHL), respectively.
The report says the pricing of these therapies aligns with patient benefit, but changes will be needed in future pricing, payment, and delivery mechanisms to ensure patient access without threatening health system affordability.
“Given the currently available evidence, these therapies appear to be effective options for those with B-ALL or NHL, though uncertainty in the evidence raised questions around the long-term value for money,” said Dan Ollendorf, PhD, ICER’s chief scientific officer.
Net health benefit
ICER’s report says tisagenlecleucel provides a net health benefit for children with B-ALL, and both tisagenlecleucel and axicabtagene ciloleucel provide a net health benefit for adults with certain types of NHL. (Novartis is seeking approval for tisagenlecleucel in NHL).
The evidence suggests there is at least a small net health benefit of the CAR T-cell therapies compared to other therapies. The benefit may be substantial, but uncertainties remain.
The data show complete remission (CR), disease-free survival (DFS), and overall survival (OS) rates are superior for NHL patients who receive axicabtagene ciloleucel, compared to patients who receive standard chemoimmunotherapy regimens.
Similarly, B-ALL patients treated with tisagenlecleucel have superior CR, DFS, and OS rates to patients treated with standard therapies. CR and OS rates are also superior in NHL patients treated with tisagenlecleucel, but DFS has not been reported in this population.
The report says there is insufficient evidence to distinguish between the 2 CAR T-cell therapies for the treatment of NHL.
Toxicity and uncertainty
The report highlights the fact that cytokine release syndrome, neurological symptoms, and B-cell aplasia have been observed in patients who receive CAR T-cell therapies. However, these sometimes severe adverse events are generally “manageable.”
In addition to toxicity, the report highlights sources of uncertainty. These include the fact that studies of tisagenlecleucel and axicabtagene ciloleucel are small, single-arm trials with short follow-up; comparisons with historical controls may be misleading; and improvements in the CAR T-cell manufacturing process may change outcomes.
Cost-effectiveness
The report states that the cost-effectiveness of each therapy fell below or within commonly cited thresholds of $50,000 to $150,000 per quality-adjusted life-year (QALY) over a lifetime.
For its analyses, ICER used the wholesale acquisition cost (WAC) plus an assumed hospital mark-up. The analyses were also based on the assumption that survival benefits observed in clinical trials would continue after the trials ended.
For tisagenlecleucel in pediatric B-ALL, the WAC is $475,000. The long-term cost-effectiveness compared to clofarabine is $45,871 per QALY gained.
For axicabtagene ciloleucel in adults with NHL, the WAC is $373,000. The long-term cost-effectiveness compared to salvage chemotherapy is $136,078 per QALY gained. The effectiveness assumptions for chemotherapy were based on an average of salvage chemotherapy regimens from the SCHOLAR-1 trial, and the cost assumptions were based on the cost of the R-DHAP (rituximab, dexamethasone, cytarabine, and cisplatin) regimen.
The report says tisagenlecleucel’s price would remain in alignment with value even if price premiums of 102% to 194% were applied.
Meanwhile, axicabtagene ciloleucel’s price could be increased by up to 11% and remain in alignment with the upper threshold ($150,000 per QALY gained) but would need to be discounted by 28% to align with the lower threshold ($100,000 per QALY gained).
Tisagenlecleucel, as a treatment for B-ALL, is not expected to cross the $915 million threshold for annual budget impact.
However, the short-term costs of axicabtagene ciloleucel for relapsed/refractory NHL could exceed the threshold. Only 38% of the estimated 5900 eligible patients could receive axicabtagene ciloleucel in a year before crossing the threshold.
Because of these findings, ICER issued an “Affordability and Access Alert” for axicabtagene ciloleucel.
This alert is intended to signal when the added costs associated with a new treatment may be difficult for the healthcare system to absorb over the short-term without displacing other needed services or contributing to unsustainable growth in healthcare insurance costs.
“Based on current evidence, both therapies appear to be priced in alignment with their clinical value, but there are potential short-term affordability concerns—for axicabtagene ciloleucel under its current indication and for both treatments should they receive future approvals for broader patient populations,” Dr Ollendorf said.
Panel voting results
ICER’s report was reviewed at a public meeting of the California Technology Assessment Forum on March 2.
Most of the panel said tisagenlecleucel provides intermediate long-term value for money when treating B-ALL. However, the significant uncertainty surrounding the long-term risks and benefits of the therapy precluded a high-value vote.
After deliberating on the value of axicabtagene ciloleucel to treat NHL, the panel’s votes were split between low-value and intermediate-value, driven by similar concerns about long-term uncertainty.
Policy recommendations
Following the voting session, ICER convened a policy roundtable of experts, including physicians, patient advocates, manufacturer representatives, and payer representatives.
Based on the roundtable discussion, ICER developed recommendations for enhanced stakeholder communication, innovative payment models, generation of additional evidence, settings of care, and patient education.
“With many other potentially transformative therapies in the pipeline, stakeholders must collaborate now to develop payment and delivery systems that can ensure timely patient access, manage short-term affordability for expensive one-time treatments, and continue to reward the innovation that brings these new treatments to market,” Dr Ollendorf said.
Some of ICER’s recommendations include:
- When launching novel therapies approved with limited clinical evidence, such as CAR T-cell therapies, manufacturers and payers should consider using a lower launch price that could be increased if substantial clinical benefits are confirmed or using a higher initial price tied to a requirement for refunds or rebates if real-world evidence fails to confirm high expectations.
- Outcomes-based pricing arrangements must be linked to “meaningful clinical outcomes assessed with sufficient follow up.”
- Hospital mark-up for CAR T-cell therapies “should reflect the expected additional cost for care delivered in the hospital, rather than a percentage of the drug cost to avoid perverse incentives in choosing the treatment location.”
- Initially, CAR T-cell therapies should be delivered in “manufacturer-accredited centers to ensure the quality and appropriateness of care.” Later, “centers of excellence accredited by specialty societies” can administer these therapies, as long as providers have “sufficient expertise” to manage serious side effects.
- Centers should ensure that patients understand what to expect from CAR T-cell therapy, including long-term consequences.
- Because additional evidence on CAR T-cell therapies is needed, all patients who receive these therapies should enter into a registry with planned long-term follow-up.
- Studies should determine the optimal timing of CAR T-cell therapy in the sequence of treatments for B-ALL and NHL.
Additional recommendations and more details are available in ICER’s report.
About ICER
ICER is an independent, non-profit research institute that produces reports analyzing evidence on the effectiveness and value of drugs and other medical services.
ICER’s reports include evidence-based calculations of prices for new drugs that reflect the degree of improvement expected in long-term patient outcomes, while also highlighting price levels that might contribute to unaffordable short-term cost growth for the overall healthcare system.
ICER’s reports incorporate input from stakeholders and are the subject of public hearings through 3 core programs: the California Technology Assessment Forum, the Midwest Comparative Effectiveness Public Advisory Council, and the New England Comparative Effectiveness Public Advisory Council.
These independent panels review ICER’s reports at public meetings to deliberate on the evidence and develop recommendations for how patients, clinicians, insurers, and policymakers can improve the quality and value of healthcare.
The Institute for Clinical and Economic Review (ICER) has made policy recommendations intended to ensure affordability and access to chimeric antigen receptor (CAR) T-cell therapies.
ICER released a Final Evidence Report on tisagenlecleucel (Kymriah, Novartis) and axicabtagene ciloleucel (Yescarta, Kite Pharma/Gilead), 2 CAR T-cell therapies approved in the US to treat B-cell acute lymphoblastic leukemia (B-ALL) and non-Hodgkin lymphoma (NHL), respectively.
The report says the pricing of these therapies aligns with patient benefit, but changes will be needed in future pricing, payment, and delivery mechanisms to ensure patient access without threatening health system affordability.
“Given the currently available evidence, these therapies appear to be effective options for those with B-ALL or NHL, though uncertainty in the evidence raised questions around the long-term value for money,” said Dan Ollendorf, PhD, ICER’s chief scientific officer.
Net health benefit
ICER’s report says tisagenlecleucel provides a net health benefit for children with B-ALL, and both tisagenlecleucel and axicabtagene ciloleucel provide a net health benefit for adults with certain types of NHL. (Novartis is seeking approval for tisagenlecleucel in NHL).
The evidence suggests there is at least a small net health benefit of the CAR T-cell therapies compared to other therapies. The benefit may be substantial, but uncertainties remain.
The data show complete remission (CR), disease-free survival (DFS), and overall survival (OS) rates are superior for NHL patients who receive axicabtagene ciloleucel, compared to patients who receive standard chemoimmunotherapy regimens.
Similarly, B-ALL patients treated with tisagenlecleucel have superior CR, DFS, and OS rates to patients treated with standard therapies. CR and OS rates are also superior in NHL patients treated with tisagenlecleucel, but DFS has not been reported in this population.
The report says there is insufficient evidence to distinguish between the 2 CAR T-cell therapies for the treatment of NHL.
Toxicity and uncertainty
The report highlights the fact that cytokine release syndrome, neurological symptoms, and B-cell aplasia have been observed in patients who receive CAR T-cell therapies. However, these sometimes severe adverse events are generally “manageable.”
In addition to toxicity, the report highlights sources of uncertainty. These include the fact that studies of tisagenlecleucel and axicabtagene ciloleucel are small, single-arm trials with short follow-up; comparisons with historical controls may be misleading; and improvements in the CAR T-cell manufacturing process may change outcomes.
Cost-effectiveness
The report states that the cost-effectiveness of each therapy fell below or within commonly cited thresholds of $50,000 to $150,000 per quality-adjusted life-year (QALY) over a lifetime.
For its analyses, ICER used the wholesale acquisition cost (WAC) plus an assumed hospital mark-up. The analyses were also based on the assumption that survival benefits observed in clinical trials would continue after the trials ended.
For tisagenlecleucel in pediatric B-ALL, the WAC is $475,000. The long-term cost-effectiveness compared to clofarabine is $45,871 per QALY gained.
For axicabtagene ciloleucel in adults with NHL, the WAC is $373,000. The long-term cost-effectiveness compared to salvage chemotherapy is $136,078 per QALY gained. The effectiveness assumptions for chemotherapy were based on an average of salvage chemotherapy regimens from the SCHOLAR-1 trial, and the cost assumptions were based on the cost of the R-DHAP (rituximab, dexamethasone, cytarabine, and cisplatin) regimen.
The report says tisagenlecleucel’s price would remain in alignment with value even if price premiums of 102% to 194% were applied.
Meanwhile, axicabtagene ciloleucel’s price could be increased by up to 11% and remain in alignment with the upper threshold ($150,000 per QALY gained) but would need to be discounted by 28% to align with the lower threshold ($100,000 per QALY gained).
Tisagenlecleucel, as a treatment for B-ALL, is not expected to cross the $915 million threshold for annual budget impact.
However, the short-term costs of axicabtagene ciloleucel for relapsed/refractory NHL could exceed the threshold. Only 38% of the estimated 5900 eligible patients could receive axicabtagene ciloleucel in a year before crossing the threshold.
Because of these findings, ICER issued an “Affordability and Access Alert” for axicabtagene ciloleucel.
This alert is intended to signal when the added costs associated with a new treatment may be difficult for the healthcare system to absorb over the short-term without displacing other needed services or contributing to unsustainable growth in healthcare insurance costs.
“Based on current evidence, both therapies appear to be priced in alignment with their clinical value, but there are potential short-term affordability concerns—for axicabtagene ciloleucel under its current indication and for both treatments should they receive future approvals for broader patient populations,” Dr Ollendorf said.
Panel voting results
ICER’s report was reviewed at a public meeting of the California Technology Assessment Forum on March 2.
Most of the panel said tisagenlecleucel provides intermediate long-term value for money when treating B-ALL. However, the significant uncertainty surrounding the long-term risks and benefits of the therapy precluded a high-value vote.
After deliberating on the value of axicabtagene ciloleucel to treat NHL, the panel’s votes were split between low-value and intermediate-value, driven by similar concerns about long-term uncertainty.
Policy recommendations
Following the voting session, ICER convened a policy roundtable of experts, including physicians, patient advocates, manufacturer representatives, and payer representatives.
Based on the roundtable discussion, ICER developed recommendations for enhanced stakeholder communication, innovative payment models, generation of additional evidence, settings of care, and patient education.
“With many other potentially transformative therapies in the pipeline, stakeholders must collaborate now to develop payment and delivery systems that can ensure timely patient access, manage short-term affordability for expensive one-time treatments, and continue to reward the innovation that brings these new treatments to market,” Dr Ollendorf said.
Some of ICER’s recommendations include:
- When launching novel therapies approved with limited clinical evidence, such as CAR T-cell therapies, manufacturers and payers should consider using a lower launch price that could be increased if substantial clinical benefits are confirmed or using a higher initial price tied to a requirement for refunds or rebates if real-world evidence fails to confirm high expectations.
- Outcomes-based pricing arrangements must be linked to “meaningful clinical outcomes assessed with sufficient follow up.”
- Hospital mark-up for CAR T-cell therapies “should reflect the expected additional cost for care delivered in the hospital, rather than a percentage of the drug cost to avoid perverse incentives in choosing the treatment location.”
- Initially, CAR T-cell therapies should be delivered in “manufacturer-accredited centers to ensure the quality and appropriateness of care.” Later, “centers of excellence accredited by specialty societies” can administer these therapies, as long as providers have “sufficient expertise” to manage serious side effects.
- Centers should ensure that patients understand what to expect from CAR T-cell therapy, including long-term consequences.
- Because additional evidence on CAR T-cell therapies is needed, all patients who receive these therapies should enter into a registry with planned long-term follow-up.
- Studies should determine the optimal timing of CAR T-cell therapy in the sequence of treatments for B-ALL and NHL.
Additional recommendations and more details are available in ICER’s report.
About ICER
ICER is an independent, non-profit research institute that produces reports analyzing evidence on the effectiveness and value of drugs and other medical services.
ICER’s reports include evidence-based calculations of prices for new drugs that reflect the degree of improvement expected in long-term patient outcomes, while also highlighting price levels that might contribute to unaffordable short-term cost growth for the overall healthcare system.
ICER’s reports incorporate input from stakeholders and are the subject of public hearings through 3 core programs: the California Technology Assessment Forum, the Midwest Comparative Effectiveness Public Advisory Council, and the New England Comparative Effectiveness Public Advisory Council.
These independent panels review ICER’s reports at public meetings to deliberate on the evidence and develop recommendations for how patients, clinicians, insurers, and policymakers can improve the quality and value of healthcare.
FDA releases updates on BIA-ALCL
The US Food and Drug Administration (FDA) has released new information on breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The agency said it is now aware of 414 cases of BIA-ALCL, which includes 9 patients who died.
In addition, the medical literature suggests that patients with textured breast implants have a lifetime risk of developing BIA-ALCL that ranges from 1 in 3817 to 1 in 30,000.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health.
“We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants. As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
Reports to FDA
Most of the BIA-ALCL cases reported to the FDA occurred in patients with textured implants (n=242), but 30 occurred in patients with smooth implants. In the remaining 173 cases, the implant surface was not specified.
There were more silicone implants (n=234) than saline implants (n=179), and there was 1 case in which the implant filling was not specified.
The patients’ median age was 53 (range, 24-90), and the median time from last implant to BIA-ALCL diagnosis was 8 years (range, 0-44).
Cases of BIA-ALCL were ALK-negative (n=124) or did not have ALK status specified (n=290). And they were CD30-positive (n=126) or did not have CD30 status specified (n=288).
The most common clinical presentation was seroma (n=203), followed by breast swelling/pain (n=101), peri-implant mass/lump (n=45), and capsular contracture (n=42). In some cases, more than one clinical presentation was listed, and there were 141 cases where clinical presentation was unspecified/uncertain.
Medical literature
The FDA said a “significant body of medical literature” on BIA-ALCL has been published since the agency’s 2011 report on this malignancy.
For the aforementioned lifetime risk estimates—1 case of BIA-ALCL in 3817 to 30,000 individuals with textured implants—the FDA cited 3 sources:
- BIA-ALCL Resources : By the numbers, and what they mean
- Breast Implant–Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk
- Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast.
Recommendations, more updates
The FDA said this updated information does not change its recommendations regarding breast implants. The agency said the decision to obtain breast implants should be made based on individual needs and with the most complete information about risks and benefits.
“We hope that this information prompts providers and patients to have important, informed conversations about breast implants and the risk of BIA-ALCL,” Dr Ashar said. “At the same time, we remain committed to working in partnership with all stakeholders to continue to study, understand, and provide updates about this important public health issue.”
The FDA is also updating the content and format of the webpage for the agency’s breast implant post-approval studies to make current information about these studies easier for patients to read and understand.
The US Food and Drug Administration (FDA) has released new information on breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The agency said it is now aware of 414 cases of BIA-ALCL, which includes 9 patients who died.
In addition, the medical literature suggests that patients with textured breast implants have a lifetime risk of developing BIA-ALCL that ranges from 1 in 3817 to 1 in 30,000.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health.
“We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants. As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
Reports to FDA
Most of the BIA-ALCL cases reported to the FDA occurred in patients with textured implants (n=242), but 30 occurred in patients with smooth implants. In the remaining 173 cases, the implant surface was not specified.
There were more silicone implants (n=234) than saline implants (n=179), and there was 1 case in which the implant filling was not specified.
The patients’ median age was 53 (range, 24-90), and the median time from last implant to BIA-ALCL diagnosis was 8 years (range, 0-44).
Cases of BIA-ALCL were ALK-negative (n=124) or did not have ALK status specified (n=290). And they were CD30-positive (n=126) or did not have CD30 status specified (n=288).
The most common clinical presentation was seroma (n=203), followed by breast swelling/pain (n=101), peri-implant mass/lump (n=45), and capsular contracture (n=42). In some cases, more than one clinical presentation was listed, and there were 141 cases where clinical presentation was unspecified/uncertain.
Medical literature
The FDA said a “significant body of medical literature” on BIA-ALCL has been published since the agency’s 2011 report on this malignancy.
For the aforementioned lifetime risk estimates—1 case of BIA-ALCL in 3817 to 30,000 individuals with textured implants—the FDA cited 3 sources:
- BIA-ALCL Resources : By the numbers, and what they mean
- Breast Implant–Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk
- Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast.
Recommendations, more updates
The FDA said this updated information does not change its recommendations regarding breast implants. The agency said the decision to obtain breast implants should be made based on individual needs and with the most complete information about risks and benefits.
“We hope that this information prompts providers and patients to have important, informed conversations about breast implants and the risk of BIA-ALCL,” Dr Ashar said. “At the same time, we remain committed to working in partnership with all stakeholders to continue to study, understand, and provide updates about this important public health issue.”
The FDA is also updating the content and format of the webpage for the agency’s breast implant post-approval studies to make current information about these studies easier for patients to read and understand.
The US Food and Drug Administration (FDA) has released new information on breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The agency said it is now aware of 414 cases of BIA-ALCL, which includes 9 patients who died.
In addition, the medical literature suggests that patients with textured breast implants have a lifetime risk of developing BIA-ALCL that ranges from 1 in 3817 to 1 in 30,000.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health.
“We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants. As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
Reports to FDA
Most of the BIA-ALCL cases reported to the FDA occurred in patients with textured implants (n=242), but 30 occurred in patients with smooth implants. In the remaining 173 cases, the implant surface was not specified.
There were more silicone implants (n=234) than saline implants (n=179), and there was 1 case in which the implant filling was not specified.
The patients’ median age was 53 (range, 24-90), and the median time from last implant to BIA-ALCL diagnosis was 8 years (range, 0-44).
Cases of BIA-ALCL were ALK-negative (n=124) or did not have ALK status specified (n=290). And they were CD30-positive (n=126) or did not have CD30 status specified (n=288).
The most common clinical presentation was seroma (n=203), followed by breast swelling/pain (n=101), peri-implant mass/lump (n=45), and capsular contracture (n=42). In some cases, more than one clinical presentation was listed, and there were 141 cases where clinical presentation was unspecified/uncertain.
Medical literature
The FDA said a “significant body of medical literature” on BIA-ALCL has been published since the agency’s 2011 report on this malignancy.
For the aforementioned lifetime risk estimates—1 case of BIA-ALCL in 3817 to 30,000 individuals with textured implants—the FDA cited 3 sources:
- BIA-ALCL Resources : By the numbers, and what they mean
- Breast Implant–Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk
- Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast.
Recommendations, more updates
The FDA said this updated information does not change its recommendations regarding breast implants. The agency said the decision to obtain breast implants should be made based on individual needs and with the most complete information about risks and benefits.
“We hope that this information prompts providers and patients to have important, informed conversations about breast implants and the risk of BIA-ALCL,” Dr Ashar said. “At the same time, we remain committed to working in partnership with all stakeholders to continue to study, understand, and provide updates about this important public health issue.”
The FDA is also updating the content and format of the webpage for the agency’s breast implant post-approval studies to make current information about these studies easier for patients to read and understand.
Drug receives orphan designation for CTCL
The US Food and Drug Administration (FDA) has granted orphan drug designation to TTI-621 for the treatment of cutaneous T-cell lymphoma (CTCL).
TTI-621 is designed to activate the innate immune system by blocking the activity of CD47, a protein commonly found on the surface of cancer cells.
TTI-621 is a SIRPaFc fusion protein that consists of the CD47-binding domain of human SIRPa linked to the Fc region of a human immunoglobulin.
The drug is intended to act as a soluble decoy receptor, preventing CD47 from delivering its inhibitory signal, thereby enabling the activation of macrophage anti-tumor effects by pro-phagocytic signals.
TTI-621 is under investigation in a phase 1 trial of patients with relapsed/refractory solid tumors and CTCL (NCT02890368). Results from the dose-escalation portion of this study were presented at the 2017 ASH Annual Meeting (abstract 4076*).
The dose-escalation portion had a 3+3 design. TTI-621 was first given as a single intratumoral injection at 1 mg, 3 mg, or 10 mg. Then, it was given at 10 mg on Monday, Wednesday, and Friday for 1 week. Next, it was given on the same 3-day schedule for 2 weeks.
Results were reported for 18 patients, 56% of whom were male. They had a median age of 69 (range, 32-85) and a median number of 3 prior therapies (range, 1-16), including radiation (39%).
Eleven patients had CTCL, and 10 were evaluable. Researchers said they observed “rapid decreases in circulating Sézary cells and/or the size of mycosis fungoides tumors” after treatment with TTI-621.
Nine of the 10 patients had a reduction in CAILS score from baseline, and 3 had a reduction in circulating Sézary cells.
There were no dose-limiting toxicities, so the 10 mg dose given 3 times a week for 2 weeks was considered the optimal dose schedule.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted orphan drug designation to TTI-621 for the treatment of cutaneous T-cell lymphoma (CTCL).
TTI-621 is designed to activate the innate immune system by blocking the activity of CD47, a protein commonly found on the surface of cancer cells.
TTI-621 is a SIRPaFc fusion protein that consists of the CD47-binding domain of human SIRPa linked to the Fc region of a human immunoglobulin.
The drug is intended to act as a soluble decoy receptor, preventing CD47 from delivering its inhibitory signal, thereby enabling the activation of macrophage anti-tumor effects by pro-phagocytic signals.
TTI-621 is under investigation in a phase 1 trial of patients with relapsed/refractory solid tumors and CTCL (NCT02890368). Results from the dose-escalation portion of this study were presented at the 2017 ASH Annual Meeting (abstract 4076*).
The dose-escalation portion had a 3+3 design. TTI-621 was first given as a single intratumoral injection at 1 mg, 3 mg, or 10 mg. Then, it was given at 10 mg on Monday, Wednesday, and Friday for 1 week. Next, it was given on the same 3-day schedule for 2 weeks.
Results were reported for 18 patients, 56% of whom were male. They had a median age of 69 (range, 32-85) and a median number of 3 prior therapies (range, 1-16), including radiation (39%).
Eleven patients had CTCL, and 10 were evaluable. Researchers said they observed “rapid decreases in circulating Sézary cells and/or the size of mycosis fungoides tumors” after treatment with TTI-621.
Nine of the 10 patients had a reduction in CAILS score from baseline, and 3 had a reduction in circulating Sézary cells.
There were no dose-limiting toxicities, so the 10 mg dose given 3 times a week for 2 weeks was considered the optimal dose schedule.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted orphan drug designation to TTI-621 for the treatment of cutaneous T-cell lymphoma (CTCL).
TTI-621 is designed to activate the innate immune system by blocking the activity of CD47, a protein commonly found on the surface of cancer cells.
TTI-621 is a SIRPaFc fusion protein that consists of the CD47-binding domain of human SIRPa linked to the Fc region of a human immunoglobulin.
The drug is intended to act as a soluble decoy receptor, preventing CD47 from delivering its inhibitory signal, thereby enabling the activation of macrophage anti-tumor effects by pro-phagocytic signals.
TTI-621 is under investigation in a phase 1 trial of patients with relapsed/refractory solid tumors and CTCL (NCT02890368). Results from the dose-escalation portion of this study were presented at the 2017 ASH Annual Meeting (abstract 4076*).
The dose-escalation portion had a 3+3 design. TTI-621 was first given as a single intratumoral injection at 1 mg, 3 mg, or 10 mg. Then, it was given at 10 mg on Monday, Wednesday, and Friday for 1 week. Next, it was given on the same 3-day schedule for 2 weeks.
Results were reported for 18 patients, 56% of whom were male. They had a median age of 69 (range, 32-85) and a median number of 3 prior therapies (range, 1-16), including radiation (39%).
Eleven patients had CTCL, and 10 were evaluable. Researchers said they observed “rapid decreases in circulating Sézary cells and/or the size of mycosis fungoides tumors” after treatment with TTI-621.
Nine of the 10 patients had a reduction in CAILS score from baseline, and 3 had a reduction in circulating Sézary cells.
There were no dose-limiting toxicities, so the 10 mg dose given 3 times a week for 2 weeks was considered the optimal dose schedule.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
*Data in the abstract differ from the presentation.
Lymphoma, breast cancer survivors have greater risk of CHF
ORLANDO—Results of a retrospective study showed that survivors of lymphoma or breast cancer had a significantly greater risk of congestive heart failure (CHF) than patients who did not have cancer.
This increased risk was observed as early as a year after cancer diagnosis but was still present 20 years after diagnosis.
Overall, 1 in 10 cancer patients had CHF at the 20-year mark.
“The majority of patients do not develop heart failure, but our research helps us recognize the factors associated with it and the importance of appropriate heart care following cancer treatment,” said Carolyn Larsen, MD, of the Mayo Clinic in Rochester, Minnesota.
“Our research suggests that periodic cardiac imaging to monitor for heart damage may be needed for some cancer patients, even if they have no signs of heart damage initially after chemotherapy. Additionally, it emphasizes that working to live a heart-healthy lifestyle is important for cancer patients and survivors to reduce the overall risk of heart disease.”
Dr Larsen and her colleagues presented this research as a poster (abstract 1105-066) at the American College of Cardiology’s 67th Annual Scientific Session & Expo (ACC.18).
Patients
Using data from the Rochester Epidemiology Project, the researchers retrospectively tracked CHF cases in 900 cancer patients and 1550 non-cancer patients. Patients were treated in Olmsted County in Minnesota from 1985 to 2010.
For both patient groups, the median age at baseline was about 53, a little more than 90% of each group was white, and nearly 80% of each group was female.
Six to 7% of patients had diabetes, and about 30% of each group had hypertension. Thirty-eight percent of each group had hyperlipidemia, and 31% were obese.
Five percent of cancer patients and 2% of controls had coronary artery disease (P<0.001). This was the only significant difference in baseline characteristics.
Cancer patients had been diagnosed with non-Hodgkin lymphoma (28%), Hodgkin lymphoma (9%), or breast cancer (64%). Forty-seven percent had received radiation, including right chest (21%), left chest (23%), and mediastinal (4%).
Eighty-four percent of patients had received anthracycline therapy. The median doxorubicin isotoxic dose was 240 mg/m2.
At baseline, 12% of cancer patients were on beta-blockers, 8% were on angiotensin converting enzyme inhibitors, 4% were on angiotensin receptor blockers, and 11% were on statins.
Results
Cancer patients were more than 3 times as likely as controls to develop CHF. The hazard ratio (HR) was 3.6 (P<0.01) in an analysis adjusted for age, gender, diabetes, hypertension, coronary artery disease, dyslipidemia, and obesity at baseline.
The increased CHF risk among cancer patients was evident after the first year from cancer diagnosis and persisted at 20 years of follow-up.
“The risk of heart failure doesn’t go away after a couple of years,” Dr Larsen said. “It’s a long-term issue that patients need to discuss with their doctors and use as motivation to stay heart healthy.”
The incidence of CHF—in cancer patients and controls, respectively—was as follows:
- 1 year—1.5% vs 0.1%
- 5 years—3.1% vs 0.9%
- 10 years—5.0% vs 2%
- 20 years—10.1% vs 5.8%.
A multivariable analysis in the cancer patients revealed a few independent risk factors for CHF, including:
- Doxorubicin isotoxic dose ≥ 300 mg/m2 (HR=2.34, P=0.003)
- Age at diagnosis (HR=3.06 for age ≥ 80 vs 60-69, P=0.01)
- Coronary artery disease at diagnosis (HR=2.27, P=0.04)
- Diabetes mellitus at diagnosis (HR=2.39, P<0.01).
Dr Larsen said additional research is needed to determine why diabetes carries a greater risk than other traditional risk factors, such as high blood pressure, in this group.
Mitigating risk
These findings raise important questions about what the appropriate surveillance should be for heart problems post-cancer treatment, Dr Larsen said. She believes more frequent cardiac imaging may be warranted in some patients to detect signs of CHF earlier.
“It’s an area that needs to be better defined,” Dr Larsen said. “An echocardiogram is usually done 6 to 12 months after cancer treatment with an anthracycline, but how often should it be done after that? We need to be more vigilant in making sure we try to prevent or control heart issues post-cancer care, especially in light of the growing appreciation of the connection between some cancer treatments and heart disease.”
Dr Larsen also noted that patients themselves can play a role in decreasing their risk of CHF, even if they are starting at a disadvantage.
A heart-healthy lifestyle—maintaining a normal body weight, regular exercise, and controlling other risk factors such as high blood pressure, diabetes, and high cholesterol—can help lower the risk of heart disease and CHF.
“If patients know they have received a drug treatment that might increase their risk of heart failure, it’s even more important to take care of the aspects of their life that they can control to reduce their risk as much as possible and to work with their medical care team to detect issues as early as possible,” Dr Larsen said.
ORLANDO—Results of a retrospective study showed that survivors of lymphoma or breast cancer had a significantly greater risk of congestive heart failure (CHF) than patients who did not have cancer.
This increased risk was observed as early as a year after cancer diagnosis but was still present 20 years after diagnosis.
Overall, 1 in 10 cancer patients had CHF at the 20-year mark.
“The majority of patients do not develop heart failure, but our research helps us recognize the factors associated with it and the importance of appropriate heart care following cancer treatment,” said Carolyn Larsen, MD, of the Mayo Clinic in Rochester, Minnesota.
“Our research suggests that periodic cardiac imaging to monitor for heart damage may be needed for some cancer patients, even if they have no signs of heart damage initially after chemotherapy. Additionally, it emphasizes that working to live a heart-healthy lifestyle is important for cancer patients and survivors to reduce the overall risk of heart disease.”
Dr Larsen and her colleagues presented this research as a poster (abstract 1105-066) at the American College of Cardiology’s 67th Annual Scientific Session & Expo (ACC.18).
Patients
Using data from the Rochester Epidemiology Project, the researchers retrospectively tracked CHF cases in 900 cancer patients and 1550 non-cancer patients. Patients were treated in Olmsted County in Minnesota from 1985 to 2010.
For both patient groups, the median age at baseline was about 53, a little more than 90% of each group was white, and nearly 80% of each group was female.
Six to 7% of patients had diabetes, and about 30% of each group had hypertension. Thirty-eight percent of each group had hyperlipidemia, and 31% were obese.
Five percent of cancer patients and 2% of controls had coronary artery disease (P<0.001). This was the only significant difference in baseline characteristics.
Cancer patients had been diagnosed with non-Hodgkin lymphoma (28%), Hodgkin lymphoma (9%), or breast cancer (64%). Forty-seven percent had received radiation, including right chest (21%), left chest (23%), and mediastinal (4%).
Eighty-four percent of patients had received anthracycline therapy. The median doxorubicin isotoxic dose was 240 mg/m2.
At baseline, 12% of cancer patients were on beta-blockers, 8% were on angiotensin converting enzyme inhibitors, 4% were on angiotensin receptor blockers, and 11% were on statins.
Results
Cancer patients were more than 3 times as likely as controls to develop CHF. The hazard ratio (HR) was 3.6 (P<0.01) in an analysis adjusted for age, gender, diabetes, hypertension, coronary artery disease, dyslipidemia, and obesity at baseline.
The increased CHF risk among cancer patients was evident after the first year from cancer diagnosis and persisted at 20 years of follow-up.
“The risk of heart failure doesn’t go away after a couple of years,” Dr Larsen said. “It’s a long-term issue that patients need to discuss with their doctors and use as motivation to stay heart healthy.”
The incidence of CHF—in cancer patients and controls, respectively—was as follows:
- 1 year—1.5% vs 0.1%
- 5 years—3.1% vs 0.9%
- 10 years—5.0% vs 2%
- 20 years—10.1% vs 5.8%.
A multivariable analysis in the cancer patients revealed a few independent risk factors for CHF, including:
- Doxorubicin isotoxic dose ≥ 300 mg/m2 (HR=2.34, P=0.003)
- Age at diagnosis (HR=3.06 for age ≥ 80 vs 60-69, P=0.01)
- Coronary artery disease at diagnosis (HR=2.27, P=0.04)
- Diabetes mellitus at diagnosis (HR=2.39, P<0.01).
Dr Larsen said additional research is needed to determine why diabetes carries a greater risk than other traditional risk factors, such as high blood pressure, in this group.
Mitigating risk
These findings raise important questions about what the appropriate surveillance should be for heart problems post-cancer treatment, Dr Larsen said. She believes more frequent cardiac imaging may be warranted in some patients to detect signs of CHF earlier.
“It’s an area that needs to be better defined,” Dr Larsen said. “An echocardiogram is usually done 6 to 12 months after cancer treatment with an anthracycline, but how often should it be done after that? We need to be more vigilant in making sure we try to prevent or control heart issues post-cancer care, especially in light of the growing appreciation of the connection between some cancer treatments and heart disease.”
Dr Larsen also noted that patients themselves can play a role in decreasing their risk of CHF, even if they are starting at a disadvantage.
A heart-healthy lifestyle—maintaining a normal body weight, regular exercise, and controlling other risk factors such as high blood pressure, diabetes, and high cholesterol—can help lower the risk of heart disease and CHF.
“If patients know they have received a drug treatment that might increase their risk of heart failure, it’s even more important to take care of the aspects of their life that they can control to reduce their risk as much as possible and to work with their medical care team to detect issues as early as possible,” Dr Larsen said.
ORLANDO—Results of a retrospective study showed that survivors of lymphoma or breast cancer had a significantly greater risk of congestive heart failure (CHF) than patients who did not have cancer.
This increased risk was observed as early as a year after cancer diagnosis but was still present 20 years after diagnosis.
Overall, 1 in 10 cancer patients had CHF at the 20-year mark.
“The majority of patients do not develop heart failure, but our research helps us recognize the factors associated with it and the importance of appropriate heart care following cancer treatment,” said Carolyn Larsen, MD, of the Mayo Clinic in Rochester, Minnesota.
“Our research suggests that periodic cardiac imaging to monitor for heart damage may be needed for some cancer patients, even if they have no signs of heart damage initially after chemotherapy. Additionally, it emphasizes that working to live a heart-healthy lifestyle is important for cancer patients and survivors to reduce the overall risk of heart disease.”
Dr Larsen and her colleagues presented this research as a poster (abstract 1105-066) at the American College of Cardiology’s 67th Annual Scientific Session & Expo (ACC.18).
Patients
Using data from the Rochester Epidemiology Project, the researchers retrospectively tracked CHF cases in 900 cancer patients and 1550 non-cancer patients. Patients were treated in Olmsted County in Minnesota from 1985 to 2010.
For both patient groups, the median age at baseline was about 53, a little more than 90% of each group was white, and nearly 80% of each group was female.
Six to 7% of patients had diabetes, and about 30% of each group had hypertension. Thirty-eight percent of each group had hyperlipidemia, and 31% were obese.
Five percent of cancer patients and 2% of controls had coronary artery disease (P<0.001). This was the only significant difference in baseline characteristics.
Cancer patients had been diagnosed with non-Hodgkin lymphoma (28%), Hodgkin lymphoma (9%), or breast cancer (64%). Forty-seven percent had received radiation, including right chest (21%), left chest (23%), and mediastinal (4%).
Eighty-four percent of patients had received anthracycline therapy. The median doxorubicin isotoxic dose was 240 mg/m2.
At baseline, 12% of cancer patients were on beta-blockers, 8% were on angiotensin converting enzyme inhibitors, 4% were on angiotensin receptor blockers, and 11% were on statins.
Results
Cancer patients were more than 3 times as likely as controls to develop CHF. The hazard ratio (HR) was 3.6 (P<0.01) in an analysis adjusted for age, gender, diabetes, hypertension, coronary artery disease, dyslipidemia, and obesity at baseline.
The increased CHF risk among cancer patients was evident after the first year from cancer diagnosis and persisted at 20 years of follow-up.
“The risk of heart failure doesn’t go away after a couple of years,” Dr Larsen said. “It’s a long-term issue that patients need to discuss with their doctors and use as motivation to stay heart healthy.”
The incidence of CHF—in cancer patients and controls, respectively—was as follows:
- 1 year—1.5% vs 0.1%
- 5 years—3.1% vs 0.9%
- 10 years—5.0% vs 2%
- 20 years—10.1% vs 5.8%.
A multivariable analysis in the cancer patients revealed a few independent risk factors for CHF, including:
- Doxorubicin isotoxic dose ≥ 300 mg/m2 (HR=2.34, P=0.003)
- Age at diagnosis (HR=3.06 for age ≥ 80 vs 60-69, P=0.01)
- Coronary artery disease at diagnosis (HR=2.27, P=0.04)
- Diabetes mellitus at diagnosis (HR=2.39, P<0.01).
Dr Larsen said additional research is needed to determine why diabetes carries a greater risk than other traditional risk factors, such as high blood pressure, in this group.
Mitigating risk
These findings raise important questions about what the appropriate surveillance should be for heart problems post-cancer treatment, Dr Larsen said. She believes more frequent cardiac imaging may be warranted in some patients to detect signs of CHF earlier.
“It’s an area that needs to be better defined,” Dr Larsen said. “An echocardiogram is usually done 6 to 12 months after cancer treatment with an anthracycline, but how often should it be done after that? We need to be more vigilant in making sure we try to prevent or control heart issues post-cancer care, especially in light of the growing appreciation of the connection between some cancer treatments and heart disease.”
Dr Larsen also noted that patients themselves can play a role in decreasing their risk of CHF, even if they are starting at a disadvantage.
A heart-healthy lifestyle—maintaining a normal body weight, regular exercise, and controlling other risk factors such as high blood pressure, diabetes, and high cholesterol—can help lower the risk of heart disease and CHF.
“If patients know they have received a drug treatment that might increase their risk of heart failure, it’s even more important to take care of the aspects of their life that they can control to reduce their risk as much as possible and to work with their medical care team to detect issues as early as possible,” Dr Larsen said.
Study confirms higher risk of infection with CB transplant
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
Company withdraws application for idelalisib
Gilead Sciences International Ltd. recently withdrew its application for European approval of idelalisib (Zydelig) in combination with rituximab and bendamustine for the treatment of relapsed/refractory chronic lymphocytic leukemia (CLL).
Idelalisib is currently approved in the European Union for use in combination with an anti-CD20 monoclonal antibody (rituximab or ofatumumab) to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment of CLL in the presence of 17p deletion or TP53 mutation in patients who are not eligible for any other therapies.
Idelalisib is also approved as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment.
In seeking expanded approval for idelalisib, Gilead submitted data from a study (NCT01569295) comparing idelalisib plus bendamustine and rituximab to placebo plus bendamustine and rituximab.
Interim results from this study were published in The Lancet Oncology in March 2017.
Gilead withdrew the application for idelalisib after the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) had evaluated documentation provided by the company and formulated lists of questions.
Gilead had not responded to the last round of questions at the time of the withdrawal.
At that point, the CHMP was of the provisional opinion that idelalisib should not be approved for use in combination with rituximab and bendamustine in patients with relapsed/refractory CLL.
The CHMP said additional, longer-term data are needed to show the benefits of idelalisib plus rituximab and bendamustine outweigh the risks.
Gilead said its withdrawal of the application was based on the CHMP’s opinion that there was insufficient evidence of a favorable benefit-risk profile.
The company also said the withdrawal does not impact ongoing trials of idelalisib.
Gilead Sciences International Ltd. recently withdrew its application for European approval of idelalisib (Zydelig) in combination with rituximab and bendamustine for the treatment of relapsed/refractory chronic lymphocytic leukemia (CLL).
Idelalisib is currently approved in the European Union for use in combination with an anti-CD20 monoclonal antibody (rituximab or ofatumumab) to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment of CLL in the presence of 17p deletion or TP53 mutation in patients who are not eligible for any other therapies.
Idelalisib is also approved as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment.
In seeking expanded approval for idelalisib, Gilead submitted data from a study (NCT01569295) comparing idelalisib plus bendamustine and rituximab to placebo plus bendamustine and rituximab.
Interim results from this study were published in The Lancet Oncology in March 2017.
Gilead withdrew the application for idelalisib after the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) had evaluated documentation provided by the company and formulated lists of questions.
Gilead had not responded to the last round of questions at the time of the withdrawal.
At that point, the CHMP was of the provisional opinion that idelalisib should not be approved for use in combination with rituximab and bendamustine in patients with relapsed/refractory CLL.
The CHMP said additional, longer-term data are needed to show the benefits of idelalisib plus rituximab and bendamustine outweigh the risks.
Gilead said its withdrawal of the application was based on the CHMP’s opinion that there was insufficient evidence of a favorable benefit-risk profile.
The company also said the withdrawal does not impact ongoing trials of idelalisib.
Gilead Sciences International Ltd. recently withdrew its application for European approval of idelalisib (Zydelig) in combination with rituximab and bendamustine for the treatment of relapsed/refractory chronic lymphocytic leukemia (CLL).
Idelalisib is currently approved in the European Union for use in combination with an anti-CD20 monoclonal antibody (rituximab or ofatumumab) to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment of CLL in the presence of 17p deletion or TP53 mutation in patients who are not eligible for any other therapies.
Idelalisib is also approved as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment.
In seeking expanded approval for idelalisib, Gilead submitted data from a study (NCT01569295) comparing idelalisib plus bendamustine and rituximab to placebo plus bendamustine and rituximab.
Interim results from this study were published in The Lancet Oncology in March 2017.
Gilead withdrew the application for idelalisib after the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) had evaluated documentation provided by the company and formulated lists of questions.
Gilead had not responded to the last round of questions at the time of the withdrawal.
At that point, the CHMP was of the provisional opinion that idelalisib should not be approved for use in combination with rituximab and bendamustine in patients with relapsed/refractory CLL.
The CHMP said additional, longer-term data are needed to show the benefits of idelalisib plus rituximab and bendamustine outweigh the risks.
Gilead said its withdrawal of the application was based on the CHMP’s opinion that there was insufficient evidence of a favorable benefit-risk profile.
The company also said the withdrawal does not impact ongoing trials of idelalisib.
Antibody has ‘very promising activity’ in rel/ref CTCL
LA JOLLA, CA—An antibody targeting KIR3DL2 has “very promising activity” in relapsed/refractory cutaneous T-cell lymphoma (CTCL), according to a speaker at the 10th Annual T-cell Lymphoma Forum.
The antibody, IPH4102, produced an overall response rate (ORR) of 44% in a phase 1 trial of CTCL patients, with an ORR of 50% in patients with Sézary syndrome (SS).
There were 2 serious adverse events (AEs) that were considered possibly related to IPH4102, and 1 of these was fatal.
Youn H. Kim, MD, of Stanford Cancer Institute in Palo Alto, California, presented these results at this year’s T-cell Lymphoma Forum. The research was sponsored by Innate Pharma, the company developing IPH4102.
“KIR3DL2 is a target that’s a member of the killer immunoglobulin-like receptor [KIR] family, and it’s also very specifically expressed in CTCL,” Dr Kim explained. “The antibody [IPH4102] is Fc-modified to enhance the antibody-dependent cell cytotoxicity and also works by antibody-dependent cell phagocytosis. It binds and, with the immunologic effect, kills the cancer cells.”
“[IPH4102] is specific for cancer cells because [KIR3DL2] is only minimally expressed in normal T cells as well as natural killer [NK] cells. About a third of NK cells that do express [KIR3DL2] don’t get affected [by IPH4102]. So it looks like the killer cells don’t kill each other, and they specifically target the neoplastic cells.”
Patients
Dr Kim and her colleagues have tested IPH4102 in 25 patients with relapsed/refractory CTCL—20 with SS, 4 with mycosis fungoides (MF), and 1 with CD4+ CTCL not otherwise specified. At baseline, patients had a median age of 71 (range, 42-90).
The patients had received a median of 4 prior systemic regimens (range, 2-10). Among the MF and SS patients, 1 patient had stage IB disease, 3 had stage IIB, and 20 had stage IVA disease.
Treatment
This study has a dose-escalation portion (accelerated 3+3 design) and an expansion portion. Dr Kim presented results for the 25 patients in the dose-escalation portion, which was completed in May 2017.
Patients received IPH4102 at 10 dose levels, ranging from 0.0001 mg/kg to 10 mg/kg. They received the drug once weekly for 4 doses, every 2 weeks for 10 doses, and every 4 weeks thereafter. They were treated until progression or unacceptable toxicity.
The expansion cohorts (which include SS and transformed MF patients) started enrolling in July 2017, with patients receiving IPH4102 at the recommended phase 2 dose—750 mg.
Safety
There were no dose-limiting toxicities with IPH4102. So the equivalent of 10 mg/kg—a 750 mg flat dose—was deemed the recommended phase 2 (and expansion) dose.
The incidence of AEs was 92% (n=23), and the incidence of treatment-related AEs was 52% (n=13).
Treatment-related AEs included lymphopenia (16%, n=4), asthenia (12%, n=3), nausea (8%, n=2), chills (8%, n=2), pyrexia (8%, n=2), arthralgia (8%, n=2), and muscle spasms (8%, n=2).
Eight patients had serious AEs, and 2 had serious AEs that were considered possibly related to treatment.
One patient had grade 2 atrial flutter diagnosed 1 hour after the first dose of IPH4102. The patient had a history of cardiac arrhythmia. She was hospitalized after the atrial flutter, received amiodarone, and the arrhythmia resolved. She went on to receive 15 more doses of IPH4102 without recurrence.
The other patient with a serious AE considered possibly related to treatment had hepatitis that occurred 6 weeks after the last dose of IPH4102. The patient had discontinued treatment due to progression after receiving IPH4102 for a year and achieving a partial response (PR).
This patient ultimately died of the hepatitis. Another fatal AE, considered unrelated to treatment, was Staphylococcus aureus sepsis.
“The safety looks very solid,” Dr Kim said, “[with] very low numbers of any significant severe adverse effects.”
Efficacy
The best global ORR was 44%, with 10 PRs and 1 complete response (CR). Twelve patients had stable disease, and 2 progressed.
In patients with SS, the best global ORR was 50%. One patient had a CR, 9 had PRs, and 8 had stable disease. The ORR was 60% in the skin and a 65% in the blood compartment for patients with SS.
Four responses were ongoing at last follow-up. The median follow-up was 15 months.
The median duration of response for the entire cohort was 8.2 months (range, 64 days to 519+ days). For SS patients, the median duration of response was 9.9 months (range, 64 days to 519+ days).
The median progression-free survival was 9.8 months overall (range, 28 days to 610+ days). For SS patients, the median progression-free survival was 10.8 months (range, 28 days to 610+ days).
“So with the efficacy and the safety profile, we are really hoping to get this drug to the phase 2 level and are excited to move forward,” Dr Kim concluded.
LA JOLLA, CA—An antibody targeting KIR3DL2 has “very promising activity” in relapsed/refractory cutaneous T-cell lymphoma (CTCL), according to a speaker at the 10th Annual T-cell Lymphoma Forum.
The antibody, IPH4102, produced an overall response rate (ORR) of 44% in a phase 1 trial of CTCL patients, with an ORR of 50% in patients with Sézary syndrome (SS).
There were 2 serious adverse events (AEs) that were considered possibly related to IPH4102, and 1 of these was fatal.
Youn H. Kim, MD, of Stanford Cancer Institute in Palo Alto, California, presented these results at this year’s T-cell Lymphoma Forum. The research was sponsored by Innate Pharma, the company developing IPH4102.
“KIR3DL2 is a target that’s a member of the killer immunoglobulin-like receptor [KIR] family, and it’s also very specifically expressed in CTCL,” Dr Kim explained. “The antibody [IPH4102] is Fc-modified to enhance the antibody-dependent cell cytotoxicity and also works by antibody-dependent cell phagocytosis. It binds and, with the immunologic effect, kills the cancer cells.”
“[IPH4102] is specific for cancer cells because [KIR3DL2] is only minimally expressed in normal T cells as well as natural killer [NK] cells. About a third of NK cells that do express [KIR3DL2] don’t get affected [by IPH4102]. So it looks like the killer cells don’t kill each other, and they specifically target the neoplastic cells.”
Patients
Dr Kim and her colleagues have tested IPH4102 in 25 patients with relapsed/refractory CTCL—20 with SS, 4 with mycosis fungoides (MF), and 1 with CD4+ CTCL not otherwise specified. At baseline, patients had a median age of 71 (range, 42-90).
The patients had received a median of 4 prior systemic regimens (range, 2-10). Among the MF and SS patients, 1 patient had stage IB disease, 3 had stage IIB, and 20 had stage IVA disease.
Treatment
This study has a dose-escalation portion (accelerated 3+3 design) and an expansion portion. Dr Kim presented results for the 25 patients in the dose-escalation portion, which was completed in May 2017.
Patients received IPH4102 at 10 dose levels, ranging from 0.0001 mg/kg to 10 mg/kg. They received the drug once weekly for 4 doses, every 2 weeks for 10 doses, and every 4 weeks thereafter. They were treated until progression or unacceptable toxicity.
The expansion cohorts (which include SS and transformed MF patients) started enrolling in July 2017, with patients receiving IPH4102 at the recommended phase 2 dose—750 mg.
Safety
There were no dose-limiting toxicities with IPH4102. So the equivalent of 10 mg/kg—a 750 mg flat dose—was deemed the recommended phase 2 (and expansion) dose.
The incidence of AEs was 92% (n=23), and the incidence of treatment-related AEs was 52% (n=13).
Treatment-related AEs included lymphopenia (16%, n=4), asthenia (12%, n=3), nausea (8%, n=2), chills (8%, n=2), pyrexia (8%, n=2), arthralgia (8%, n=2), and muscle spasms (8%, n=2).
Eight patients had serious AEs, and 2 had serious AEs that were considered possibly related to treatment.
One patient had grade 2 atrial flutter diagnosed 1 hour after the first dose of IPH4102. The patient had a history of cardiac arrhythmia. She was hospitalized after the atrial flutter, received amiodarone, and the arrhythmia resolved. She went on to receive 15 more doses of IPH4102 without recurrence.
The other patient with a serious AE considered possibly related to treatment had hepatitis that occurred 6 weeks after the last dose of IPH4102. The patient had discontinued treatment due to progression after receiving IPH4102 for a year and achieving a partial response (PR).
This patient ultimately died of the hepatitis. Another fatal AE, considered unrelated to treatment, was Staphylococcus aureus sepsis.
“The safety looks very solid,” Dr Kim said, “[with] very low numbers of any significant severe adverse effects.”
Efficacy
The best global ORR was 44%, with 10 PRs and 1 complete response (CR). Twelve patients had stable disease, and 2 progressed.
In patients with SS, the best global ORR was 50%. One patient had a CR, 9 had PRs, and 8 had stable disease. The ORR was 60% in the skin and a 65% in the blood compartment for patients with SS.
Four responses were ongoing at last follow-up. The median follow-up was 15 months.
The median duration of response for the entire cohort was 8.2 months (range, 64 days to 519+ days). For SS patients, the median duration of response was 9.9 months (range, 64 days to 519+ days).
The median progression-free survival was 9.8 months overall (range, 28 days to 610+ days). For SS patients, the median progression-free survival was 10.8 months (range, 28 days to 610+ days).
“So with the efficacy and the safety profile, we are really hoping to get this drug to the phase 2 level and are excited to move forward,” Dr Kim concluded.
LA JOLLA, CA—An antibody targeting KIR3DL2 has “very promising activity” in relapsed/refractory cutaneous T-cell lymphoma (CTCL), according to a speaker at the 10th Annual T-cell Lymphoma Forum.
The antibody, IPH4102, produced an overall response rate (ORR) of 44% in a phase 1 trial of CTCL patients, with an ORR of 50% in patients with Sézary syndrome (SS).
There were 2 serious adverse events (AEs) that were considered possibly related to IPH4102, and 1 of these was fatal.
Youn H. Kim, MD, of Stanford Cancer Institute in Palo Alto, California, presented these results at this year’s T-cell Lymphoma Forum. The research was sponsored by Innate Pharma, the company developing IPH4102.
“KIR3DL2 is a target that’s a member of the killer immunoglobulin-like receptor [KIR] family, and it’s also very specifically expressed in CTCL,” Dr Kim explained. “The antibody [IPH4102] is Fc-modified to enhance the antibody-dependent cell cytotoxicity and also works by antibody-dependent cell phagocytosis. It binds and, with the immunologic effect, kills the cancer cells.”
“[IPH4102] is specific for cancer cells because [KIR3DL2] is only minimally expressed in normal T cells as well as natural killer [NK] cells. About a third of NK cells that do express [KIR3DL2] don’t get affected [by IPH4102]. So it looks like the killer cells don’t kill each other, and they specifically target the neoplastic cells.”
Patients
Dr Kim and her colleagues have tested IPH4102 in 25 patients with relapsed/refractory CTCL—20 with SS, 4 with mycosis fungoides (MF), and 1 with CD4+ CTCL not otherwise specified. At baseline, patients had a median age of 71 (range, 42-90).
The patients had received a median of 4 prior systemic regimens (range, 2-10). Among the MF and SS patients, 1 patient had stage IB disease, 3 had stage IIB, and 20 had stage IVA disease.
Treatment
This study has a dose-escalation portion (accelerated 3+3 design) and an expansion portion. Dr Kim presented results for the 25 patients in the dose-escalation portion, which was completed in May 2017.
Patients received IPH4102 at 10 dose levels, ranging from 0.0001 mg/kg to 10 mg/kg. They received the drug once weekly for 4 doses, every 2 weeks for 10 doses, and every 4 weeks thereafter. They were treated until progression or unacceptable toxicity.
The expansion cohorts (which include SS and transformed MF patients) started enrolling in July 2017, with patients receiving IPH4102 at the recommended phase 2 dose—750 mg.
Safety
There were no dose-limiting toxicities with IPH4102. So the equivalent of 10 mg/kg—a 750 mg flat dose—was deemed the recommended phase 2 (and expansion) dose.
The incidence of AEs was 92% (n=23), and the incidence of treatment-related AEs was 52% (n=13).
Treatment-related AEs included lymphopenia (16%, n=4), asthenia (12%, n=3), nausea (8%, n=2), chills (8%, n=2), pyrexia (8%, n=2), arthralgia (8%, n=2), and muscle spasms (8%, n=2).
Eight patients had serious AEs, and 2 had serious AEs that were considered possibly related to treatment.
One patient had grade 2 atrial flutter diagnosed 1 hour after the first dose of IPH4102. The patient had a history of cardiac arrhythmia. She was hospitalized after the atrial flutter, received amiodarone, and the arrhythmia resolved. She went on to receive 15 more doses of IPH4102 without recurrence.
The other patient with a serious AE considered possibly related to treatment had hepatitis that occurred 6 weeks after the last dose of IPH4102. The patient had discontinued treatment due to progression after receiving IPH4102 for a year and achieving a partial response (PR).
This patient ultimately died of the hepatitis. Another fatal AE, considered unrelated to treatment, was Staphylococcus aureus sepsis.
“The safety looks very solid,” Dr Kim said, “[with] very low numbers of any significant severe adverse effects.”
Efficacy
The best global ORR was 44%, with 10 PRs and 1 complete response (CR). Twelve patients had stable disease, and 2 progressed.
In patients with SS, the best global ORR was 50%. One patient had a CR, 9 had PRs, and 8 had stable disease. The ORR was 60% in the skin and a 65% in the blood compartment for patients with SS.
Four responses were ongoing at last follow-up. The median follow-up was 15 months.
The median duration of response for the entire cohort was 8.2 months (range, 64 days to 519+ days). For SS patients, the median duration of response was 9.9 months (range, 64 days to 519+ days).
The median progression-free survival was 9.8 months overall (range, 28 days to 610+ days). For SS patients, the median progression-free survival was 10.8 months (range, 28 days to 610+ days).
“So with the efficacy and the safety profile, we are really hoping to get this drug to the phase 2 level and are excited to move forward,” Dr Kim concluded.