User login
Radioimmunoconjugate shows activity in NHL
CHICAGO—The radioimmunoconjugate 177Lu-NNV003 has demonstrated activity against non-Hodgkin lymphomas (NHLs).
Experiments showed that 177Lu-NNV003 can inhibit proliferation in mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and chronic lymphocytic leukemia (CLL) cell lines.
177Lu-NNV003 also exhibited an antitumor effect and prolonged survival in mouse models of MCL, DLBCL, and CLL.
These results were presented at the AACR Annual Meeting 2018 (abstract 848).
This research was conducted by employees of Nordic Nanovector and other researchers. Nordic Nanovector is the company developing 177Lu-NNV003.
177Lu-NNV003 consists of a chimeric antibody targeting CD37 (NNV003) conjugated with p-SCN-Bn-DOTA, which chelates the β-emitting radionuclide lutetium-177.
The researchers found that 177Lu-NNV003 inhibited proliferation in all 3 NHL cell lines tested—MEC-2 (CLL), DOHH2 (DLBCL), and REC-1 (MCL). DOHH2 was the most radiosensitive cell line.
The unlabeled NNV003 antibody, on the other hand, did not exhibit an antiproliferative effect in these cell lines. However, NNV003 did induce antibody-dependent cellular cytotoxicity in MEC-2 and DOHH2 cells and antibody-dependent cellular phagocytosis in MEC-2 cells.
The researchers found that 177Lu-NNV003 targeted CD37-positive cells and demonstrated antitumor effects in mouse models of MCL, CLL, and DLBCL.
REC-1 model
177Lu-NNV003 prolonged survival in CB17 SCID mice injected with REC-1 cells and cured 50% to 60% of the mice.
Median survival times were 55 days in mice that received sodium chloride (NaCl), 85 days in mice that received NNV003 (0.167 mg/kg), and 61 days in mice that received 177Lu-IgG1 (100 MBq/kg).
On the other hand, mice treated with 177Lu-NNV003 had a median survival of 152 days (100 MBq/kg), or the median survival was not reached (50 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of NaCl (P<0.001) or 177Lu-IgG1 (P<0.002).
MEC-2 model
177Lu-NNV003 also prolonged survival in NRG mice injected with MEC-2 cells.
The median survival was 21 days in mice that received NaCl, NNV003 (2 x 0.33 mg/kg), or 177Lu-IgG1 (200 MBq/kg).
However, mice treated with 177Lu-NNV003 had a median survival of 32 days (200 MBq/kg) or 29 days (2 x 200 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of 177Lu-IgG1 (P<0.025) or 2 x NNV003 (P<0.02).
DOHH2 model
RAG-2 mice injected with DOHH2 cells had survival times surpassing 200 days after treatment with NNV003 or 177Lu-NNV003.
The median survival was not reached in mice that received NNV003 (at 2 or 30 mg/kg) or 177Lu-NNV003 (at 200, 300, or 400 MBq/kg). But the median survival was 46 days in mice that received NaCl and 47 days in mice that received 177Lu-IgG1 (300 MBq/kg).
The difference in survival was significant for recipients of NNV003 or 177Lu-NNV003 compared to recipients of 177Lu-IgG1 or NaCl (P<0.001 for all).
Toxicity and biodistribution
The researchers noted that the 177Lu-labeled antibodies caused transient hematologic toxicity in the mice.
In the MEC-2 and DOHH2 models, there was no redistribution of 177Lu-NNV003 in organs after initial uptake. (The researchers did not report on biodistribution in the REC-1 model.)
177Lu-NNV003 had low uptake in the liver, spleen, kidneys, and femur. The researchers said this suggests 177Lu-NNV003 is stable in vivo, as free lutetium-177 tends to accumulate in bones.
CHICAGO—The radioimmunoconjugate 177Lu-NNV003 has demonstrated activity against non-Hodgkin lymphomas (NHLs).
Experiments showed that 177Lu-NNV003 can inhibit proliferation in mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and chronic lymphocytic leukemia (CLL) cell lines.
177Lu-NNV003 also exhibited an antitumor effect and prolonged survival in mouse models of MCL, DLBCL, and CLL.
These results were presented at the AACR Annual Meeting 2018 (abstract 848).
This research was conducted by employees of Nordic Nanovector and other researchers. Nordic Nanovector is the company developing 177Lu-NNV003.
177Lu-NNV003 consists of a chimeric antibody targeting CD37 (NNV003) conjugated with p-SCN-Bn-DOTA, which chelates the β-emitting radionuclide lutetium-177.
The researchers found that 177Lu-NNV003 inhibited proliferation in all 3 NHL cell lines tested—MEC-2 (CLL), DOHH2 (DLBCL), and REC-1 (MCL). DOHH2 was the most radiosensitive cell line.
The unlabeled NNV003 antibody, on the other hand, did not exhibit an antiproliferative effect in these cell lines. However, NNV003 did induce antibody-dependent cellular cytotoxicity in MEC-2 and DOHH2 cells and antibody-dependent cellular phagocytosis in MEC-2 cells.
The researchers found that 177Lu-NNV003 targeted CD37-positive cells and demonstrated antitumor effects in mouse models of MCL, CLL, and DLBCL.
REC-1 model
177Lu-NNV003 prolonged survival in CB17 SCID mice injected with REC-1 cells and cured 50% to 60% of the mice.
Median survival times were 55 days in mice that received sodium chloride (NaCl), 85 days in mice that received NNV003 (0.167 mg/kg), and 61 days in mice that received 177Lu-IgG1 (100 MBq/kg).
On the other hand, mice treated with 177Lu-NNV003 had a median survival of 152 days (100 MBq/kg), or the median survival was not reached (50 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of NaCl (P<0.001) or 177Lu-IgG1 (P<0.002).
MEC-2 model
177Lu-NNV003 also prolonged survival in NRG mice injected with MEC-2 cells.
The median survival was 21 days in mice that received NaCl, NNV003 (2 x 0.33 mg/kg), or 177Lu-IgG1 (200 MBq/kg).
However, mice treated with 177Lu-NNV003 had a median survival of 32 days (200 MBq/kg) or 29 days (2 x 200 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of 177Lu-IgG1 (P<0.025) or 2 x NNV003 (P<0.02).
DOHH2 model
RAG-2 mice injected with DOHH2 cells had survival times surpassing 200 days after treatment with NNV003 or 177Lu-NNV003.
The median survival was not reached in mice that received NNV003 (at 2 or 30 mg/kg) or 177Lu-NNV003 (at 200, 300, or 400 MBq/kg). But the median survival was 46 days in mice that received NaCl and 47 days in mice that received 177Lu-IgG1 (300 MBq/kg).
The difference in survival was significant for recipients of NNV003 or 177Lu-NNV003 compared to recipients of 177Lu-IgG1 or NaCl (P<0.001 for all).
Toxicity and biodistribution
The researchers noted that the 177Lu-labeled antibodies caused transient hematologic toxicity in the mice.
In the MEC-2 and DOHH2 models, there was no redistribution of 177Lu-NNV003 in organs after initial uptake. (The researchers did not report on biodistribution in the REC-1 model.)
177Lu-NNV003 had low uptake in the liver, spleen, kidneys, and femur. The researchers said this suggests 177Lu-NNV003 is stable in vivo, as free lutetium-177 tends to accumulate in bones.
CHICAGO—The radioimmunoconjugate 177Lu-NNV003 has demonstrated activity against non-Hodgkin lymphomas (NHLs).
Experiments showed that 177Lu-NNV003 can inhibit proliferation in mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and chronic lymphocytic leukemia (CLL) cell lines.
177Lu-NNV003 also exhibited an antitumor effect and prolonged survival in mouse models of MCL, DLBCL, and CLL.
These results were presented at the AACR Annual Meeting 2018 (abstract 848).
This research was conducted by employees of Nordic Nanovector and other researchers. Nordic Nanovector is the company developing 177Lu-NNV003.
177Lu-NNV003 consists of a chimeric antibody targeting CD37 (NNV003) conjugated with p-SCN-Bn-DOTA, which chelates the β-emitting radionuclide lutetium-177.
The researchers found that 177Lu-NNV003 inhibited proliferation in all 3 NHL cell lines tested—MEC-2 (CLL), DOHH2 (DLBCL), and REC-1 (MCL). DOHH2 was the most radiosensitive cell line.
The unlabeled NNV003 antibody, on the other hand, did not exhibit an antiproliferative effect in these cell lines. However, NNV003 did induce antibody-dependent cellular cytotoxicity in MEC-2 and DOHH2 cells and antibody-dependent cellular phagocytosis in MEC-2 cells.
The researchers found that 177Lu-NNV003 targeted CD37-positive cells and demonstrated antitumor effects in mouse models of MCL, CLL, and DLBCL.
REC-1 model
177Lu-NNV003 prolonged survival in CB17 SCID mice injected with REC-1 cells and cured 50% to 60% of the mice.
Median survival times were 55 days in mice that received sodium chloride (NaCl), 85 days in mice that received NNV003 (0.167 mg/kg), and 61 days in mice that received 177Lu-IgG1 (100 MBq/kg).
On the other hand, mice treated with 177Lu-NNV003 had a median survival of 152 days (100 MBq/kg), or the median survival was not reached (50 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of NaCl (P<0.001) or 177Lu-IgG1 (P<0.002).
MEC-2 model
177Lu-NNV003 also prolonged survival in NRG mice injected with MEC-2 cells.
The median survival was 21 days in mice that received NaCl, NNV003 (2 x 0.33 mg/kg), or 177Lu-IgG1 (200 MBq/kg).
However, mice treated with 177Lu-NNV003 had a median survival of 32 days (200 MBq/kg) or 29 days (2 x 200 MBq/kg).
The difference in survival was significant for 177Lu-NNV003 recipients compared to recipients of 177Lu-IgG1 (P<0.025) or 2 x NNV003 (P<0.02).
DOHH2 model
RAG-2 mice injected with DOHH2 cells had survival times surpassing 200 days after treatment with NNV003 or 177Lu-NNV003.
The median survival was not reached in mice that received NNV003 (at 2 or 30 mg/kg) or 177Lu-NNV003 (at 200, 300, or 400 MBq/kg). But the median survival was 46 days in mice that received NaCl and 47 days in mice that received 177Lu-IgG1 (300 MBq/kg).
The difference in survival was significant for recipients of NNV003 or 177Lu-NNV003 compared to recipients of 177Lu-IgG1 or NaCl (P<0.001 for all).
Toxicity and biodistribution
The researchers noted that the 177Lu-labeled antibodies caused transient hematologic toxicity in the mice.
In the MEC-2 and DOHH2 models, there was no redistribution of 177Lu-NNV003 in organs after initial uptake. (The researchers did not report on biodistribution in the REC-1 model.)
177Lu-NNV003 had low uptake in the liver, spleen, kidneys, and femur. The researchers said this suggests 177Lu-NNV003 is stable in vivo, as free lutetium-177 tends to accumulate in bones.
CDK inhibitor synergizes with venetoclax in CLL
CHICAGO—Researchers have reported “strong synergy” between the CDK2/9 inhibitor CYC065 and the Bcl-2 inhibitor venetoclax in chronic lymphocytic leukemia (CLL).
Experiments indicated that CYC065 and venetoclax target parallel mechanisms that promote survival in CLL cells, working together to induce apoptosis.
The drugs demonstrated synergy even in CLL samples that are inherently resistant to each drug alone.
William Plunkett, PhD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, and his colleagues reported these findings at the AACR Annual Meeting 2018 (abstract 3905).
This research was supported by Cyclacel Pharmaceuticals, Inc., the company developing CYC065.
The researchers explained that CYC065 depletes Mcl-1 to induce apoptosis in CLL cells, while venetoclax induces apoptosis via inhibition of Bcl-2. However, upregulation of Mcl-1 is associated with resistance to venetoclax.
Therefore, the researchers theorized that combining CYC065 and venetoclax would serve to target 2 mechanisms that promote survival in CLL cells.
Experiments showed that CYC065 and venetoclax combined synergistically in CLL samples with or without 17p deletion. However, the researchers observed heterogeneity in response across samples.
The team said both drugs appeared to be less potent in some del(17p) samples. However, they also observed “great synergy” in del(17p) samples that were resistant to CYC065 or venetoclax alone.
The researchers noted differences in the kinetics of cell death in response to each drug and said this is consistent with the drugs’ different mechanisms of action.
Maximal cell death was reached at 6 to 8 hours with venetoclax but took at least 24 hours with CYC065.
The researchers also assessed the reversibility of CYC065 and venetoclax. They incubated CLL cells with each drug alone and in combination, then washed and incubated cells in drug-free media.
The team observed no additional cell death after the removal of CYC065, venetoclax, or the combination. They said this suggests an “adequate exposure time” is needed to maximize the induction of apoptosis with these drugs.
“[T]he combination of CYC065 and venetoclax is strongly synergistic in primary CLL cells from patients, including those with 17p deletions,” said Spiro Rombotis, president and chief executive officer of Cyclacel.
“In addition, the combination was active in 2 CLL samples which were resistant to either agent alone. These findings support the hypothesis that dual targeting of the Mcl-1- and Bcl-2-dependent mechanisms could induce synergistic cell death by apoptosis.”
Based on these results, Cyclacel is planning a trial of CYC065 and venetoclax in patients with relapsed/refractory CLL.
CHICAGO—Researchers have reported “strong synergy” between the CDK2/9 inhibitor CYC065 and the Bcl-2 inhibitor venetoclax in chronic lymphocytic leukemia (CLL).
Experiments indicated that CYC065 and venetoclax target parallel mechanisms that promote survival in CLL cells, working together to induce apoptosis.
The drugs demonstrated synergy even in CLL samples that are inherently resistant to each drug alone.
William Plunkett, PhD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, and his colleagues reported these findings at the AACR Annual Meeting 2018 (abstract 3905).
This research was supported by Cyclacel Pharmaceuticals, Inc., the company developing CYC065.
The researchers explained that CYC065 depletes Mcl-1 to induce apoptosis in CLL cells, while venetoclax induces apoptosis via inhibition of Bcl-2. However, upregulation of Mcl-1 is associated with resistance to venetoclax.
Therefore, the researchers theorized that combining CYC065 and venetoclax would serve to target 2 mechanisms that promote survival in CLL cells.
Experiments showed that CYC065 and venetoclax combined synergistically in CLL samples with or without 17p deletion. However, the researchers observed heterogeneity in response across samples.
The team said both drugs appeared to be less potent in some del(17p) samples. However, they also observed “great synergy” in del(17p) samples that were resistant to CYC065 or venetoclax alone.
The researchers noted differences in the kinetics of cell death in response to each drug and said this is consistent with the drugs’ different mechanisms of action.
Maximal cell death was reached at 6 to 8 hours with venetoclax but took at least 24 hours with CYC065.
The researchers also assessed the reversibility of CYC065 and venetoclax. They incubated CLL cells with each drug alone and in combination, then washed and incubated cells in drug-free media.
The team observed no additional cell death after the removal of CYC065, venetoclax, or the combination. They said this suggests an “adequate exposure time” is needed to maximize the induction of apoptosis with these drugs.
“[T]he combination of CYC065 and venetoclax is strongly synergistic in primary CLL cells from patients, including those with 17p deletions,” said Spiro Rombotis, president and chief executive officer of Cyclacel.
“In addition, the combination was active in 2 CLL samples which were resistant to either agent alone. These findings support the hypothesis that dual targeting of the Mcl-1- and Bcl-2-dependent mechanisms could induce synergistic cell death by apoptosis.”
Based on these results, Cyclacel is planning a trial of CYC065 and venetoclax in patients with relapsed/refractory CLL.
CHICAGO—Researchers have reported “strong synergy” between the CDK2/9 inhibitor CYC065 and the Bcl-2 inhibitor venetoclax in chronic lymphocytic leukemia (CLL).
Experiments indicated that CYC065 and venetoclax target parallel mechanisms that promote survival in CLL cells, working together to induce apoptosis.
The drugs demonstrated synergy even in CLL samples that are inherently resistant to each drug alone.
William Plunkett, PhD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, and his colleagues reported these findings at the AACR Annual Meeting 2018 (abstract 3905).
This research was supported by Cyclacel Pharmaceuticals, Inc., the company developing CYC065.
The researchers explained that CYC065 depletes Mcl-1 to induce apoptosis in CLL cells, while venetoclax induces apoptosis via inhibition of Bcl-2. However, upregulation of Mcl-1 is associated with resistance to venetoclax.
Therefore, the researchers theorized that combining CYC065 and venetoclax would serve to target 2 mechanisms that promote survival in CLL cells.
Experiments showed that CYC065 and venetoclax combined synergistically in CLL samples with or without 17p deletion. However, the researchers observed heterogeneity in response across samples.
The team said both drugs appeared to be less potent in some del(17p) samples. However, they also observed “great synergy” in del(17p) samples that were resistant to CYC065 or venetoclax alone.
The researchers noted differences in the kinetics of cell death in response to each drug and said this is consistent with the drugs’ different mechanisms of action.
Maximal cell death was reached at 6 to 8 hours with venetoclax but took at least 24 hours with CYC065.
The researchers also assessed the reversibility of CYC065 and venetoclax. They incubated CLL cells with each drug alone and in combination, then washed and incubated cells in drug-free media.
The team observed no additional cell death after the removal of CYC065, venetoclax, or the combination. They said this suggests an “adequate exposure time” is needed to maximize the induction of apoptosis with these drugs.
“[T]he combination of CYC065 and venetoclax is strongly synergistic in primary CLL cells from patients, including those with 17p deletions,” said Spiro Rombotis, president and chief executive officer of Cyclacel.
“In addition, the combination was active in 2 CLL samples which were resistant to either agent alone. These findings support the hypothesis that dual targeting of the Mcl-1- and Bcl-2-dependent mechanisms could induce synergistic cell death by apoptosis.”
Based on these results, Cyclacel is planning a trial of CYC065 and venetoclax in patients with relapsed/refractory CLL.
FDA places tazemetostat trials on partial hold
The US Food and Drug Administration (FDA) has placed a partial hold on clinical trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The hold has halted enrollment in US-based trials of tazemetostat, but study subjects who have not experienced disease progression may continue to receive the drug.
The hold is due to an adverse event observed in a pediatric patient on a phase 1 study of tazemetostat.
The patient, who had advanced poorly differentiated chordoma, developed a secondary T-cell lymphoma while taking tazemetostat.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. Now, the patient has discontinued tazemetostat and is being treated for T-cell lymphoma.
More than 750 patients have been treated with tazemetostat to date, and this is the only case of secondary lymphoma that has been observed, according to Epizyme, Inc., the company developing tazemetostat.
The company also noted that doses of tazemetostat explored in its phase 1 pediatric study are higher than those used in the phase 2 adult studies.
Epizyme has begun taking steps to address the hold on tazemetostat trials—updating the informed consent, investigator’s brochure, and study protocols.
The company will need to confirm alignment with the FDA in order to resume US enrollment.
“We are working expeditiously with clinical trial investigators and regulatory authorities to initiate the appropriate steps to resume enrollment,” said Robert Bazemore, president and chief executive officer of Epizyme.
“Epizyme, along with our global investigator community, has been very encouraged by the clinical responses and tolerability of tazemetostat observed in pediatric and adult patients with hematological malignancies and solid tumors enrolled in our trials. We remain encouraged by the potential of tazemetostat to address the unmet needs of many patients living with cancer.”
The US Food and Drug Administration (FDA) has placed a partial hold on clinical trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The hold has halted enrollment in US-based trials of tazemetostat, but study subjects who have not experienced disease progression may continue to receive the drug.
The hold is due to an adverse event observed in a pediatric patient on a phase 1 study of tazemetostat.
The patient, who had advanced poorly differentiated chordoma, developed a secondary T-cell lymphoma while taking tazemetostat.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. Now, the patient has discontinued tazemetostat and is being treated for T-cell lymphoma.
More than 750 patients have been treated with tazemetostat to date, and this is the only case of secondary lymphoma that has been observed, according to Epizyme, Inc., the company developing tazemetostat.
The company also noted that doses of tazemetostat explored in its phase 1 pediatric study are higher than those used in the phase 2 adult studies.
Epizyme has begun taking steps to address the hold on tazemetostat trials—updating the informed consent, investigator’s brochure, and study protocols.
The company will need to confirm alignment with the FDA in order to resume US enrollment.
“We are working expeditiously with clinical trial investigators and regulatory authorities to initiate the appropriate steps to resume enrollment,” said Robert Bazemore, president and chief executive officer of Epizyme.
“Epizyme, along with our global investigator community, has been very encouraged by the clinical responses and tolerability of tazemetostat observed in pediatric and adult patients with hematological malignancies and solid tumors enrolled in our trials. We remain encouraged by the potential of tazemetostat to address the unmet needs of many patients living with cancer.”
The US Food and Drug Administration (FDA) has placed a partial hold on clinical trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The hold has halted enrollment in US-based trials of tazemetostat, but study subjects who have not experienced disease progression may continue to receive the drug.
The hold is due to an adverse event observed in a pediatric patient on a phase 1 study of tazemetostat.
The patient, who had advanced poorly differentiated chordoma, developed a secondary T-cell lymphoma while taking tazemetostat.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. Now, the patient has discontinued tazemetostat and is being treated for T-cell lymphoma.
More than 750 patients have been treated with tazemetostat to date, and this is the only case of secondary lymphoma that has been observed, according to Epizyme, Inc., the company developing tazemetostat.
The company also noted that doses of tazemetostat explored in its phase 1 pediatric study are higher than those used in the phase 2 adult studies.
Epizyme has begun taking steps to address the hold on tazemetostat trials—updating the informed consent, investigator’s brochure, and study protocols.
The company will need to confirm alignment with the FDA in order to resume US enrollment.
“We are working expeditiously with clinical trial investigators and regulatory authorities to initiate the appropriate steps to resume enrollment,” said Robert Bazemore, president and chief executive officer of Epizyme.
“Epizyme, along with our global investigator community, has been very encouraged by the clinical responses and tolerability of tazemetostat observed in pediatric and adult patients with hematological malignancies and solid tumors enrolled in our trials. We remain encouraged by the potential of tazemetostat to address the unmet needs of many patients living with cancer.”
Art education benefits blood cancer patients
New research suggests a bedside visual art intervention (BVAI) can reduce pain and anxiety in inpatients with hematologic malignancies, including those undergoing transplant.
The BVAI involved an educator teaching patients art technique one-on-one for approximately 30 minutes.
After a single session, patients had significant improvements in positive mood and pain scores, as well as decreases in negative mood and anxiety.
Alexandra P. Wolanskyj, MD, of Mayo Clinic in Rochester, Minnesota, and her colleagues reported these results in the European Journal of Cancer Care.
The study included 21 patients, 19 of them female. Their median age was 53.5 (range, 19-75). Six patients were undergoing hematopoietic stem cell transplant.
The patients had multiple myeloma (n=5), acute myeloid leukemia (n=5), non-Hodgkin lymphoma (n=3), Hodgkin lymphoma (n=2), acute lymphoblastic leukemia (n=1), chronic lymphocytic leukemia (n=1), amyloidosis (n=1), Gardner-Diamond syndrome (n=1), myelodysplastic syndrome (n=1), and Waldenstrom’s macroglobulinemia (n=1).
Nearly half of patients had relapsed disease (47.6%), 23.8% had active and new disease, 19.0% had active disease with primary resistance on chemotherapy, and 9.5% of patients were in remission.
Intervention
The researchers recruited an educator from a community art center to teach art at the patients’ bedsides. Sessions were intended to be about 30 minutes. However, patients could stop at any time or continue beyond 30 minutes.
Patients and their families could make art or just observe. Materials used included watercolors, oil pastels, colored pencils, and clay (all non-toxic and odorless). The materials were left with patients so they could continue to use them after the sessions.
Results
The researchers assessed patients’ pain, anxiety, and mood at baseline and after the patients had a session with the art educator.
After the BVAI, patients had a significant decrease in pain, according to the Visual Analog Scale (VAS). The 14 patients who reported any pain at baseline had a mean reduction in VAS score of 1.5, or a 35.1% reduction in pain (P=0.017).
Patients had a 21.6% reduction in anxiety after the BVAI. Among the 20 patients who completed this assessment, there was a mean 9.2-point decrease in State-Trait Anxiety Inventory (STAI) score (P=0.001).
In addition, patients had a significant increase in positive mood and a significant decrease in negative mood after the BVAI. Mood was assessed in 20 patients using the Positive and Negative Affect Schedule (PANAS) scale.
Positive mood increased 14.6% (P=0.003), and negative mood decreased 18.0% (P=0.015) after the BVAI. Patients’ mean PANAS scores increased 4.6 points for positive mood and decreased 3.3 points for negative mood.
All 21 patients completed a questionnaire on the BVAI. All but 1 patient (95%) said the intervention was positive overall, and 85% of patients (n=18) said they would be interested in participating in future art-based interventions.
The researchers said these results suggest experiences provided by artists in the community may be an adjunct to conventional treatments in patients with cancer-related mood symptoms and pain.
New research suggests a bedside visual art intervention (BVAI) can reduce pain and anxiety in inpatients with hematologic malignancies, including those undergoing transplant.
The BVAI involved an educator teaching patients art technique one-on-one for approximately 30 minutes.
After a single session, patients had significant improvements in positive mood and pain scores, as well as decreases in negative mood and anxiety.
Alexandra P. Wolanskyj, MD, of Mayo Clinic in Rochester, Minnesota, and her colleagues reported these results in the European Journal of Cancer Care.
The study included 21 patients, 19 of them female. Their median age was 53.5 (range, 19-75). Six patients were undergoing hematopoietic stem cell transplant.
The patients had multiple myeloma (n=5), acute myeloid leukemia (n=5), non-Hodgkin lymphoma (n=3), Hodgkin lymphoma (n=2), acute lymphoblastic leukemia (n=1), chronic lymphocytic leukemia (n=1), amyloidosis (n=1), Gardner-Diamond syndrome (n=1), myelodysplastic syndrome (n=1), and Waldenstrom’s macroglobulinemia (n=1).
Nearly half of patients had relapsed disease (47.6%), 23.8% had active and new disease, 19.0% had active disease with primary resistance on chemotherapy, and 9.5% of patients were in remission.
Intervention
The researchers recruited an educator from a community art center to teach art at the patients’ bedsides. Sessions were intended to be about 30 minutes. However, patients could stop at any time or continue beyond 30 minutes.
Patients and their families could make art or just observe. Materials used included watercolors, oil pastels, colored pencils, and clay (all non-toxic and odorless). The materials were left with patients so they could continue to use them after the sessions.
Results
The researchers assessed patients’ pain, anxiety, and mood at baseline and after the patients had a session with the art educator.
After the BVAI, patients had a significant decrease in pain, according to the Visual Analog Scale (VAS). The 14 patients who reported any pain at baseline had a mean reduction in VAS score of 1.5, or a 35.1% reduction in pain (P=0.017).
Patients had a 21.6% reduction in anxiety after the BVAI. Among the 20 patients who completed this assessment, there was a mean 9.2-point decrease in State-Trait Anxiety Inventory (STAI) score (P=0.001).
In addition, patients had a significant increase in positive mood and a significant decrease in negative mood after the BVAI. Mood was assessed in 20 patients using the Positive and Negative Affect Schedule (PANAS) scale.
Positive mood increased 14.6% (P=0.003), and negative mood decreased 18.0% (P=0.015) after the BVAI. Patients’ mean PANAS scores increased 4.6 points for positive mood and decreased 3.3 points for negative mood.
All 21 patients completed a questionnaire on the BVAI. All but 1 patient (95%) said the intervention was positive overall, and 85% of patients (n=18) said they would be interested in participating in future art-based interventions.
The researchers said these results suggest experiences provided by artists in the community may be an adjunct to conventional treatments in patients with cancer-related mood symptoms and pain.
New research suggests a bedside visual art intervention (BVAI) can reduce pain and anxiety in inpatients with hematologic malignancies, including those undergoing transplant.
The BVAI involved an educator teaching patients art technique one-on-one for approximately 30 minutes.
After a single session, patients had significant improvements in positive mood and pain scores, as well as decreases in negative mood and anxiety.
Alexandra P. Wolanskyj, MD, of Mayo Clinic in Rochester, Minnesota, and her colleagues reported these results in the European Journal of Cancer Care.
The study included 21 patients, 19 of them female. Their median age was 53.5 (range, 19-75). Six patients were undergoing hematopoietic stem cell transplant.
The patients had multiple myeloma (n=5), acute myeloid leukemia (n=5), non-Hodgkin lymphoma (n=3), Hodgkin lymphoma (n=2), acute lymphoblastic leukemia (n=1), chronic lymphocytic leukemia (n=1), amyloidosis (n=1), Gardner-Diamond syndrome (n=1), myelodysplastic syndrome (n=1), and Waldenstrom’s macroglobulinemia (n=1).
Nearly half of patients had relapsed disease (47.6%), 23.8% had active and new disease, 19.0% had active disease with primary resistance on chemotherapy, and 9.5% of patients were in remission.
Intervention
The researchers recruited an educator from a community art center to teach art at the patients’ bedsides. Sessions were intended to be about 30 minutes. However, patients could stop at any time or continue beyond 30 minutes.
Patients and their families could make art or just observe. Materials used included watercolors, oil pastels, colored pencils, and clay (all non-toxic and odorless). The materials were left with patients so they could continue to use them after the sessions.
Results
The researchers assessed patients’ pain, anxiety, and mood at baseline and after the patients had a session with the art educator.
After the BVAI, patients had a significant decrease in pain, according to the Visual Analog Scale (VAS). The 14 patients who reported any pain at baseline had a mean reduction in VAS score of 1.5, or a 35.1% reduction in pain (P=0.017).
Patients had a 21.6% reduction in anxiety after the BVAI. Among the 20 patients who completed this assessment, there was a mean 9.2-point decrease in State-Trait Anxiety Inventory (STAI) score (P=0.001).
In addition, patients had a significant increase in positive mood and a significant decrease in negative mood after the BVAI. Mood was assessed in 20 patients using the Positive and Negative Affect Schedule (PANAS) scale.
Positive mood increased 14.6% (P=0.003), and negative mood decreased 18.0% (P=0.015) after the BVAI. Patients’ mean PANAS scores increased 4.6 points for positive mood and decreased 3.3 points for negative mood.
All 21 patients completed a questionnaire on the BVAI. All but 1 patient (95%) said the intervention was positive overall, and 85% of patients (n=18) said they would be interested in participating in future art-based interventions.
The researchers said these results suggest experiences provided by artists in the community may be an adjunct to conventional treatments in patients with cancer-related mood symptoms and pain.
Inhibitor outperforms rivals in leukemia, lymphoma
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
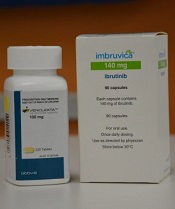
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
Team uses iPSCs to create ‘universal’ CAR T cells
CHICAGO—Researchers have used induced pluripotent stem cells (iPSCs) to create a “universal” chimeric antigen receptor (CAR) T-cell therapy known as FT819.
The team says FT819 has the potential to be mass-produced, stored, and made readily available for cancer patients.
In in vitro experiments, FT819 demonstrated activity against leukemia and lymphoma.
These results were presented at the AACR Annual Meeting 2018 (abstract LB-108).
The research was conducted by employees of Fate Therapeutics, Inc., the company developing FT819, as well as Memorial Sloan-Kettering Cancer Center.
About FT819
FT819 is produced from a master iPSC line generated using T cells from healthy donors.
“A master iPSC line has unlimited capacity to self-renew and can be banked and renewably used,” said Bob Valamehr, PhD, vice-president of cancer immunotherapy at Fate Therapeutics, Inc.
“We started with cells from a healthy donor rather than the patient, created a master cell line, and used the master cell line to produce large quantities of ‘universal’ CAR19 T cells that are not patient-restricted. These first-of-kind CAR19 T cells, called FT819, can be packaged, stored, and made readily available for treatment of a large number of patients.”
FT819 has 2 targeting receptors—a CAR targeting CD19-positive tumor cells and a CD16 Fc receptor that can engage other therapies (such as tumor antigen-targeting monoclonal antibodies) to overcome antigen escape.
The master iPSC line used for the production of FT819 is engineered in a one-time event to insert a CD19 CAR into the T-cell receptor α constant (TRAC) locus. This is done to eliminate T-cell receptor expression and reduce the likelihood of graft-versus-host disease.
Previous research showed that targeting a CAR to the TRAC locus results in uniform CAR expression and enhances T-cell potency. In fact, TRAC-CAR T cells outperformed conventionally generated CAR T cells by preventing T-cell exhaustion in a mouse model of acute lymphoblastic leukemia.
In vitro experiments
With the current work, the researchers found that FT819 displayed an efficient cytotoxic T-cell response when challenged with CD19-positive tumor cells. FT819 produced cytokines (IFN-gamma, TNF-alpha, and IL-2) and mediators of cell death (CD107a/b, perforin, and granzyme B).
FT819 was also target-specific, attacking only CD19-positive tumor cells and sparing CD19-negative tumor cells in experiments with Raji (Burkitt lymphoma) and Nalm-6 (B-cell acute lymphoblastic leukemia) cell lines.
The researchers said they observed consistent antigen-specific cytotoxicity against Nalm-6 cells with FT819 but variability in antigen-specific cytotoxicity with conventional CAR T cells.
In addition, when combined with rituximab, FT819 elicited antibody-dependent cell-mediated cytotoxicity against CD19-negative, CD20-positive tumor cells.
“Through the development of FT819, we believe there is significant opportunity to lower the cost of CAR T-cell manufacture, enhance the quality of the product, and create a readily available supply of a more efficacious product to reach more patients in need,” Dr Valamehr said.
CHICAGO—Researchers have used induced pluripotent stem cells (iPSCs) to create a “universal” chimeric antigen receptor (CAR) T-cell therapy known as FT819.
The team says FT819 has the potential to be mass-produced, stored, and made readily available for cancer patients.
In in vitro experiments, FT819 demonstrated activity against leukemia and lymphoma.
These results were presented at the AACR Annual Meeting 2018 (abstract LB-108).
The research was conducted by employees of Fate Therapeutics, Inc., the company developing FT819, as well as Memorial Sloan-Kettering Cancer Center.
About FT819
FT819 is produced from a master iPSC line generated using T cells from healthy donors.
“A master iPSC line has unlimited capacity to self-renew and can be banked and renewably used,” said Bob Valamehr, PhD, vice-president of cancer immunotherapy at Fate Therapeutics, Inc.
“We started with cells from a healthy donor rather than the patient, created a master cell line, and used the master cell line to produce large quantities of ‘universal’ CAR19 T cells that are not patient-restricted. These first-of-kind CAR19 T cells, called FT819, can be packaged, stored, and made readily available for treatment of a large number of patients.”
FT819 has 2 targeting receptors—a CAR targeting CD19-positive tumor cells and a CD16 Fc receptor that can engage other therapies (such as tumor antigen-targeting monoclonal antibodies) to overcome antigen escape.
The master iPSC line used for the production of FT819 is engineered in a one-time event to insert a CD19 CAR into the T-cell receptor α constant (TRAC) locus. This is done to eliminate T-cell receptor expression and reduce the likelihood of graft-versus-host disease.
Previous research showed that targeting a CAR to the TRAC locus results in uniform CAR expression and enhances T-cell potency. In fact, TRAC-CAR T cells outperformed conventionally generated CAR T cells by preventing T-cell exhaustion in a mouse model of acute lymphoblastic leukemia.
In vitro experiments
With the current work, the researchers found that FT819 displayed an efficient cytotoxic T-cell response when challenged with CD19-positive tumor cells. FT819 produced cytokines (IFN-gamma, TNF-alpha, and IL-2) and mediators of cell death (CD107a/b, perforin, and granzyme B).
FT819 was also target-specific, attacking only CD19-positive tumor cells and sparing CD19-negative tumor cells in experiments with Raji (Burkitt lymphoma) and Nalm-6 (B-cell acute lymphoblastic leukemia) cell lines.
The researchers said they observed consistent antigen-specific cytotoxicity against Nalm-6 cells with FT819 but variability in antigen-specific cytotoxicity with conventional CAR T cells.
In addition, when combined with rituximab, FT819 elicited antibody-dependent cell-mediated cytotoxicity against CD19-negative, CD20-positive tumor cells.
“Through the development of FT819, we believe there is significant opportunity to lower the cost of CAR T-cell manufacture, enhance the quality of the product, and create a readily available supply of a more efficacious product to reach more patients in need,” Dr Valamehr said.
CHICAGO—Researchers have used induced pluripotent stem cells (iPSCs) to create a “universal” chimeric antigen receptor (CAR) T-cell therapy known as FT819.
The team says FT819 has the potential to be mass-produced, stored, and made readily available for cancer patients.
In in vitro experiments, FT819 demonstrated activity against leukemia and lymphoma.
These results were presented at the AACR Annual Meeting 2018 (abstract LB-108).
The research was conducted by employees of Fate Therapeutics, Inc., the company developing FT819, as well as Memorial Sloan-Kettering Cancer Center.
About FT819
FT819 is produced from a master iPSC line generated using T cells from healthy donors.
“A master iPSC line has unlimited capacity to self-renew and can be banked and renewably used,” said Bob Valamehr, PhD, vice-president of cancer immunotherapy at Fate Therapeutics, Inc.
“We started with cells from a healthy donor rather than the patient, created a master cell line, and used the master cell line to produce large quantities of ‘universal’ CAR19 T cells that are not patient-restricted. These first-of-kind CAR19 T cells, called FT819, can be packaged, stored, and made readily available for treatment of a large number of patients.”
FT819 has 2 targeting receptors—a CAR targeting CD19-positive tumor cells and a CD16 Fc receptor that can engage other therapies (such as tumor antigen-targeting monoclonal antibodies) to overcome antigen escape.
The master iPSC line used for the production of FT819 is engineered in a one-time event to insert a CD19 CAR into the T-cell receptor α constant (TRAC) locus. This is done to eliminate T-cell receptor expression and reduce the likelihood of graft-versus-host disease.
Previous research showed that targeting a CAR to the TRAC locus results in uniform CAR expression and enhances T-cell potency. In fact, TRAC-CAR T cells outperformed conventionally generated CAR T cells by preventing T-cell exhaustion in a mouse model of acute lymphoblastic leukemia.
In vitro experiments
With the current work, the researchers found that FT819 displayed an efficient cytotoxic T-cell response when challenged with CD19-positive tumor cells. FT819 produced cytokines (IFN-gamma, TNF-alpha, and IL-2) and mediators of cell death (CD107a/b, perforin, and granzyme B).
FT819 was also target-specific, attacking only CD19-positive tumor cells and sparing CD19-negative tumor cells in experiments with Raji (Burkitt lymphoma) and Nalm-6 (B-cell acute lymphoblastic leukemia) cell lines.
The researchers said they observed consistent antigen-specific cytotoxicity against Nalm-6 cells with FT819 but variability in antigen-specific cytotoxicity with conventional CAR T cells.
In addition, when combined with rituximab, FT819 elicited antibody-dependent cell-mediated cytotoxicity against CD19-negative, CD20-positive tumor cells.
“Through the development of FT819, we believe there is significant opportunity to lower the cost of CAR T-cell manufacture, enhance the quality of the product, and create a readily available supply of a more efficacious product to reach more patients in need,” Dr Valamehr said.
Research reveals new subtypes of DLBCL
New research helps explain why some patients with diffuse large B-cell lymphoma (DLBCL) respond well to immunochemotherapy and others do not.
Researchers analyzed samples from nearly 600 DLBCL patients and identified 4 new genetic subtypes of the disease.
Patients with 2 of these subtypes had overall survival (OS) rates that were roughly twice as high as OS rates in patients with the other 2 subtypes.
Louis M. Staudt, MD, PhD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues described these findings in NEJM.
The researchers noted that the current subtypes of DLBCL—germinal center B-cell-like (GCB) and activated B-cell-like (ABC) DLBCL—are associated with OS after treatment with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
Patients with ABC DLBCL have a much lower OS rate, on average, than patients with GCB DLBCL. However, even in the GCB subgroup, many patients relapse after treatment.
“The first question we wanted to tackle was whether there were other molecular features of the tumors that could help us explain why some people were well-served by chemotherapy,” Dr Staudt said.
“And the second, related question was, if we could understand who was not responding well to treatment, could we understand the genetics of these tumors to suggest new potential therapies beyond chemotherapy? The answer to both questions was ‘yes.’”
Dr Staudt and his colleagues analyzed tumor samples from 574 patients with DLBCL, performing exome and transcriptome sequencing, array-based DNA copy-number analysis, and targeted amplicon resequencing of 372 genes to find recurrent aberrations.
The team also developed an algorithm to discover genetic subtypes based on the co-occurrence of genetic alterations.
In this way, they identified 4 genetic subtypes:
- MCD, which was named based on the co-occurrence of MYD88L265P and CD79B mutations
- BN2, whose name was based on the presence of BCL6 fusions and NOTCH2 mutations
- N1, named for NOTCH1 mutations
- EZB, named for EZH2 mutations and BCL2 translocations.
The researchers said aberrations in multiple genes distinguished each of these subtypes from other DLBCLs, and the subtypes differed phenotypically.
Patients with BN2 or EZB subtypes had much higher OS rates after receiving R-CHOP than patients with MCD or N1 subtypes. The predicted 5-year OS rates were 26% for MCD patients, 36% for N1 patients, 65% for BN2 patients, and 68% for EZB patients.
The researchers said they found evidence to suggest that MCD and BN2 DLBCLs rely on chronic active B-cell receptor signaling that is amenable to therapeutic inhibition.
The team also noted that some of the subtypes they identified can be found in both ABC and GCB DLBCLs. For example, a patient could have ABC DLBCL, which is associated with a lower OS rate after R-CHOP, but also have the BN2 genetic subtype that responds well to R-CHOP.
“This shows we’ve gone beyond where we were,” Dr Staudt said. “Before, even with our most advanced molecular diagnosis, we would have said all ABC tumors are the ‘bad’ type, and they need to be treated aggressively.”
“Now, we can implement this kind of classification and say that, even if a patient has the ‘bad’ ABC type, they have the ‘good’ genetic type, BN2. So there’s a much better chance of chemotherapy curing the disease.”
Data from this study will be shared through the National Cancer Institute’s Genomic Data Commons to make it available for future research.
Dr Staudt said he and his colleagues hope their new molecular classification will be used in clinical trials so that DLBCL treatment can move toward more targeted therapies.
“The goal is to find the right drug for the right person at the right time,” Dr Staudt said. “And we feel this genetic understanding of diffuse lymphoma is a step forward in precision therapy.”
New research helps explain why some patients with diffuse large B-cell lymphoma (DLBCL) respond well to immunochemotherapy and others do not.
Researchers analyzed samples from nearly 600 DLBCL patients and identified 4 new genetic subtypes of the disease.
Patients with 2 of these subtypes had overall survival (OS) rates that were roughly twice as high as OS rates in patients with the other 2 subtypes.
Louis M. Staudt, MD, PhD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues described these findings in NEJM.
The researchers noted that the current subtypes of DLBCL—germinal center B-cell-like (GCB) and activated B-cell-like (ABC) DLBCL—are associated with OS after treatment with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
Patients with ABC DLBCL have a much lower OS rate, on average, than patients with GCB DLBCL. However, even in the GCB subgroup, many patients relapse after treatment.
“The first question we wanted to tackle was whether there were other molecular features of the tumors that could help us explain why some people were well-served by chemotherapy,” Dr Staudt said.
“And the second, related question was, if we could understand who was not responding well to treatment, could we understand the genetics of these tumors to suggest new potential therapies beyond chemotherapy? The answer to both questions was ‘yes.’”
Dr Staudt and his colleagues analyzed tumor samples from 574 patients with DLBCL, performing exome and transcriptome sequencing, array-based DNA copy-number analysis, and targeted amplicon resequencing of 372 genes to find recurrent aberrations.
The team also developed an algorithm to discover genetic subtypes based on the co-occurrence of genetic alterations.
In this way, they identified 4 genetic subtypes:
- MCD, which was named based on the co-occurrence of MYD88L265P and CD79B mutations
- BN2, whose name was based on the presence of BCL6 fusions and NOTCH2 mutations
- N1, named for NOTCH1 mutations
- EZB, named for EZH2 mutations and BCL2 translocations.
The researchers said aberrations in multiple genes distinguished each of these subtypes from other DLBCLs, and the subtypes differed phenotypically.
Patients with BN2 or EZB subtypes had much higher OS rates after receiving R-CHOP than patients with MCD or N1 subtypes. The predicted 5-year OS rates were 26% for MCD patients, 36% for N1 patients, 65% for BN2 patients, and 68% for EZB patients.
The researchers said they found evidence to suggest that MCD and BN2 DLBCLs rely on chronic active B-cell receptor signaling that is amenable to therapeutic inhibition.
The team also noted that some of the subtypes they identified can be found in both ABC and GCB DLBCLs. For example, a patient could have ABC DLBCL, which is associated with a lower OS rate after R-CHOP, but also have the BN2 genetic subtype that responds well to R-CHOP.
“This shows we’ve gone beyond where we were,” Dr Staudt said. “Before, even with our most advanced molecular diagnosis, we would have said all ABC tumors are the ‘bad’ type, and they need to be treated aggressively.”
“Now, we can implement this kind of classification and say that, even if a patient has the ‘bad’ ABC type, they have the ‘good’ genetic type, BN2. So there’s a much better chance of chemotherapy curing the disease.”
Data from this study will be shared through the National Cancer Institute’s Genomic Data Commons to make it available for future research.
Dr Staudt said he and his colleagues hope their new molecular classification will be used in clinical trials so that DLBCL treatment can move toward more targeted therapies.
“The goal is to find the right drug for the right person at the right time,” Dr Staudt said. “And we feel this genetic understanding of diffuse lymphoma is a step forward in precision therapy.”
New research helps explain why some patients with diffuse large B-cell lymphoma (DLBCL) respond well to immunochemotherapy and others do not.
Researchers analyzed samples from nearly 600 DLBCL patients and identified 4 new genetic subtypes of the disease.
Patients with 2 of these subtypes had overall survival (OS) rates that were roughly twice as high as OS rates in patients with the other 2 subtypes.
Louis M. Staudt, MD, PhD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues described these findings in NEJM.
The researchers noted that the current subtypes of DLBCL—germinal center B-cell-like (GCB) and activated B-cell-like (ABC) DLBCL—are associated with OS after treatment with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
Patients with ABC DLBCL have a much lower OS rate, on average, than patients with GCB DLBCL. However, even in the GCB subgroup, many patients relapse after treatment.
“The first question we wanted to tackle was whether there were other molecular features of the tumors that could help us explain why some people were well-served by chemotherapy,” Dr Staudt said.
“And the second, related question was, if we could understand who was not responding well to treatment, could we understand the genetics of these tumors to suggest new potential therapies beyond chemotherapy? The answer to both questions was ‘yes.’”
Dr Staudt and his colleagues analyzed tumor samples from 574 patients with DLBCL, performing exome and transcriptome sequencing, array-based DNA copy-number analysis, and targeted amplicon resequencing of 372 genes to find recurrent aberrations.
The team also developed an algorithm to discover genetic subtypes based on the co-occurrence of genetic alterations.
In this way, they identified 4 genetic subtypes:
- MCD, which was named based on the co-occurrence of MYD88L265P and CD79B mutations
- BN2, whose name was based on the presence of BCL6 fusions and NOTCH2 mutations
- N1, named for NOTCH1 mutations
- EZB, named for EZH2 mutations and BCL2 translocations.
The researchers said aberrations in multiple genes distinguished each of these subtypes from other DLBCLs, and the subtypes differed phenotypically.
Patients with BN2 or EZB subtypes had much higher OS rates after receiving R-CHOP than patients with MCD or N1 subtypes. The predicted 5-year OS rates were 26% for MCD patients, 36% for N1 patients, 65% for BN2 patients, and 68% for EZB patients.
The researchers said they found evidence to suggest that MCD and BN2 DLBCLs rely on chronic active B-cell receptor signaling that is amenable to therapeutic inhibition.
The team also noted that some of the subtypes they identified can be found in both ABC and GCB DLBCLs. For example, a patient could have ABC DLBCL, which is associated with a lower OS rate after R-CHOP, but also have the BN2 genetic subtype that responds well to R-CHOP.
“This shows we’ve gone beyond where we were,” Dr Staudt said. “Before, even with our most advanced molecular diagnosis, we would have said all ABC tumors are the ‘bad’ type, and they need to be treated aggressively.”
“Now, we can implement this kind of classification and say that, even if a patient has the ‘bad’ ABC type, they have the ‘good’ genetic type, BN2. So there’s a much better chance of chemotherapy curing the disease.”
Data from this study will be shared through the National Cancer Institute’s Genomic Data Commons to make it available for future research.
Dr Staudt said he and his colleagues hope their new molecular classification will be used in clinical trials so that DLBCL treatment can move toward more targeted therapies.
“The goal is to find the right drug for the right person at the right time,” Dr Staudt said. “And we feel this genetic understanding of diffuse lymphoma is a step forward in precision therapy.”
Tazemetostat exhibits antitumor activity in phase 1 trial
The EZH2 inhibitor tazemetostat demonstrated a “favorable safety profile and antitumor activity” in a phase 1 study, according to researchers.
The drug produced responses in 8 of 21 patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), including 3 complete responses (CRs).
The maximum tolerated dose of tazemetostat was not reached, and there were no fatal adverse events (AEs) related to treatment.
Grade 3/4 treatment-related AEs included thrombocytopenia, neutropenia, hepatocellular injury, and hypertension.
Antoine Italiano, MD, PhD, of Institut Bergonié in Bordeaux, France, and his colleagues reported these results in The Lancet Oncology. The trial was sponsored by Epizyme and Eisai.
The study enrolled 64 patients—43 with solid tumors and 21 with B-cell NHL. The following characteristics and dosing information pertain only to the patients with NHL.
Thirteen patients had diffuse large B-cell lymphoma (DLBCL), 7 had follicular lymphoma (FL), and 1 had marginal zone lymphoma (MZL).
The patients’ median age was 62 (range, 53-70), and 71% were male. They had an ECOG performance status of 0 (62%) or 1 (38%).
Most patients had received at least 3 prior therapies—38% had 3, 14% had 4, and 33% had 5 or more prior therapies. Forty-eight percent had prior hematopoietic stem cell transplant.
The patients received escalating doses of tazemetostat twice daily—100 mg (n=1), 200 mg (n=2), 400 mg (n=1), 800 mg (n=8), and 1600 mg (n=4).
The remaining 5 patients were enrolled in a substudy to evaluate food effect. These patients received a single 200 mg dose on day -8 and day -1, with or without food, followed by 400 mg twice daily starting on day 1. Specific results on the food effects were not included in the paper.
Safety
In the entire study cohort, there was 1 dose-limiting toxicity—grade 4 thrombocytopenia—at the 1600 mg dose. The maximum tolerated dose of tazemetostat was not reached, but the researchers decided upon 800 mg twice daily as the recommended phase 2 dose.
Overall, 77% (n=49) of patients had treatment-related AEs. Grade 3/4 treatment-related AEs included thrombocytopenia (4%, n=2), neutropenia (4%, n=2), hepatocellular injury (2%, n=1), and hypertension (2%, n=1).
Serious treatment-related AEs were neutropenia in 1 patient (800 mg group) and anemia and thrombocytopenia in another patient (1600 mg group).
Seven patients (11%) had fatal AEs, but none were considered treatment-related. They included general physical health deterioration (1 at 200 mg, 1 at 1600 mg, and 2 at 400 mg), respiratory distress (2 at 400 mg), and septic shock (1 at 1600 mg).
Efficacy
Eight of the 21 NHL patients responded to treatment. Three patients had a CR—1 with DLBCL and 2 with FL. Of the 5 partial responders, 3 had DLBCL, 1 had FL, and 1 had MZL.
The median time to first response was 3.5 months, and the median duration of response was 12.4 months.
The 3 complete responders remained on tazemetostat beyond 27.6 months (FL patient), 28.8 months (FL patient), and 33.6 months (DLBCL patient).
Two of the 43 patients with solid tumors responded to tazemetostat—1 with a CR and 1 with a partial response.
The complete responder had an INI1-negative malignant rhabdoid tumor, and the partial responder had a SMARCA4-negative malignant rhabdoid tumor of the ovary.
“Today’s publication in The Lancet Oncology reports the safety and tolerability endpoints for tazemetostat in this study, which enabled further evaluation of EZH2 inhibition in INI1- and SMARCA4-negative solid tumors and NHL,” Dr Italiano said. “I’m also encouraged by the preliminary antitumor activity observed in this study.”
The EZH2 inhibitor tazemetostat demonstrated a “favorable safety profile and antitumor activity” in a phase 1 study, according to researchers.
The drug produced responses in 8 of 21 patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), including 3 complete responses (CRs).
The maximum tolerated dose of tazemetostat was not reached, and there were no fatal adverse events (AEs) related to treatment.
Grade 3/4 treatment-related AEs included thrombocytopenia, neutropenia, hepatocellular injury, and hypertension.
Antoine Italiano, MD, PhD, of Institut Bergonié in Bordeaux, France, and his colleagues reported these results in The Lancet Oncology. The trial was sponsored by Epizyme and Eisai.
The study enrolled 64 patients—43 with solid tumors and 21 with B-cell NHL. The following characteristics and dosing information pertain only to the patients with NHL.
Thirteen patients had diffuse large B-cell lymphoma (DLBCL), 7 had follicular lymphoma (FL), and 1 had marginal zone lymphoma (MZL).
The patients’ median age was 62 (range, 53-70), and 71% were male. They had an ECOG performance status of 0 (62%) or 1 (38%).
Most patients had received at least 3 prior therapies—38% had 3, 14% had 4, and 33% had 5 or more prior therapies. Forty-eight percent had prior hematopoietic stem cell transplant.
The patients received escalating doses of tazemetostat twice daily—100 mg (n=1), 200 mg (n=2), 400 mg (n=1), 800 mg (n=8), and 1600 mg (n=4).
The remaining 5 patients were enrolled in a substudy to evaluate food effect. These patients received a single 200 mg dose on day -8 and day -1, with or without food, followed by 400 mg twice daily starting on day 1. Specific results on the food effects were not included in the paper.
Safety
In the entire study cohort, there was 1 dose-limiting toxicity—grade 4 thrombocytopenia—at the 1600 mg dose. The maximum tolerated dose of tazemetostat was not reached, but the researchers decided upon 800 mg twice daily as the recommended phase 2 dose.
Overall, 77% (n=49) of patients had treatment-related AEs. Grade 3/4 treatment-related AEs included thrombocytopenia (4%, n=2), neutropenia (4%, n=2), hepatocellular injury (2%, n=1), and hypertension (2%, n=1).
Serious treatment-related AEs were neutropenia in 1 patient (800 mg group) and anemia and thrombocytopenia in another patient (1600 mg group).
Seven patients (11%) had fatal AEs, but none were considered treatment-related. They included general physical health deterioration (1 at 200 mg, 1 at 1600 mg, and 2 at 400 mg), respiratory distress (2 at 400 mg), and septic shock (1 at 1600 mg).
Efficacy
Eight of the 21 NHL patients responded to treatment. Three patients had a CR—1 with DLBCL and 2 with FL. Of the 5 partial responders, 3 had DLBCL, 1 had FL, and 1 had MZL.
The median time to first response was 3.5 months, and the median duration of response was 12.4 months.
The 3 complete responders remained on tazemetostat beyond 27.6 months (FL patient), 28.8 months (FL patient), and 33.6 months (DLBCL patient).
Two of the 43 patients with solid tumors responded to tazemetostat—1 with a CR and 1 with a partial response.
The complete responder had an INI1-negative malignant rhabdoid tumor, and the partial responder had a SMARCA4-negative malignant rhabdoid tumor of the ovary.
“Today’s publication in The Lancet Oncology reports the safety and tolerability endpoints for tazemetostat in this study, which enabled further evaluation of EZH2 inhibition in INI1- and SMARCA4-negative solid tumors and NHL,” Dr Italiano said. “I’m also encouraged by the preliminary antitumor activity observed in this study.”
The EZH2 inhibitor tazemetostat demonstrated a “favorable safety profile and antitumor activity” in a phase 1 study, according to researchers.
The drug produced responses in 8 of 21 patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), including 3 complete responses (CRs).
The maximum tolerated dose of tazemetostat was not reached, and there were no fatal adverse events (AEs) related to treatment.
Grade 3/4 treatment-related AEs included thrombocytopenia, neutropenia, hepatocellular injury, and hypertension.
Antoine Italiano, MD, PhD, of Institut Bergonié in Bordeaux, France, and his colleagues reported these results in The Lancet Oncology. The trial was sponsored by Epizyme and Eisai.
The study enrolled 64 patients—43 with solid tumors and 21 with B-cell NHL. The following characteristics and dosing information pertain only to the patients with NHL.
Thirteen patients had diffuse large B-cell lymphoma (DLBCL), 7 had follicular lymphoma (FL), and 1 had marginal zone lymphoma (MZL).
The patients’ median age was 62 (range, 53-70), and 71% were male. They had an ECOG performance status of 0 (62%) or 1 (38%).
Most patients had received at least 3 prior therapies—38% had 3, 14% had 4, and 33% had 5 or more prior therapies. Forty-eight percent had prior hematopoietic stem cell transplant.
The patients received escalating doses of tazemetostat twice daily—100 mg (n=1), 200 mg (n=2), 400 mg (n=1), 800 mg (n=8), and 1600 mg (n=4).
The remaining 5 patients were enrolled in a substudy to evaluate food effect. These patients received a single 200 mg dose on day -8 and day -1, with or without food, followed by 400 mg twice daily starting on day 1. Specific results on the food effects were not included in the paper.
Safety
In the entire study cohort, there was 1 dose-limiting toxicity—grade 4 thrombocytopenia—at the 1600 mg dose. The maximum tolerated dose of tazemetostat was not reached, but the researchers decided upon 800 mg twice daily as the recommended phase 2 dose.
Overall, 77% (n=49) of patients had treatment-related AEs. Grade 3/4 treatment-related AEs included thrombocytopenia (4%, n=2), neutropenia (4%, n=2), hepatocellular injury (2%, n=1), and hypertension (2%, n=1).
Serious treatment-related AEs were neutropenia in 1 patient (800 mg group) and anemia and thrombocytopenia in another patient (1600 mg group).
Seven patients (11%) had fatal AEs, but none were considered treatment-related. They included general physical health deterioration (1 at 200 mg, 1 at 1600 mg, and 2 at 400 mg), respiratory distress (2 at 400 mg), and septic shock (1 at 1600 mg).
Efficacy
Eight of the 21 NHL patients responded to treatment. Three patients had a CR—1 with DLBCL and 2 with FL. Of the 5 partial responders, 3 had DLBCL, 1 had FL, and 1 had MZL.
The median time to first response was 3.5 months, and the median duration of response was 12.4 months.
The 3 complete responders remained on tazemetostat beyond 27.6 months (FL patient), 28.8 months (FL patient), and 33.6 months (DLBCL patient).
Two of the 43 patients with solid tumors responded to tazemetostat—1 with a CR and 1 with a partial response.
The complete responder had an INI1-negative malignant rhabdoid tumor, and the partial responder had a SMARCA4-negative malignant rhabdoid tumor of the ovary.
“Today’s publication in The Lancet Oncology reports the safety and tolerability endpoints for tazemetostat in this study, which enabled further evaluation of EZH2 inhibition in INI1- and SMARCA4-negative solid tumors and NHL,” Dr Italiano said. “I’m also encouraged by the preliminary antitumor activity observed in this study.”
Combo improves outcomes in MCL
A 2-drug combination can improve outcomes in patients with mantle cell lymphoma (MCL), according to researchers.
In a phase 2 trial of MCL patients, the BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax produced an overall response rate of 71% and a complete response (CR) rate of 62%.
“This was in patients who we expected to have a poor outcome on conventional therapy, and in which treatment with either ibrutinib or venetoclax alone was expected to see only 21% of patients show a complete response,” said Constantine Tam, MBBS, MD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
The most common adverse events (AEs) in patients receiving venetoclax and ibrutinib were diarrhea (83%), fatigue (75%), and nausea/vomiting (71%). Fourteen patients (58%) had serious AEs, including 2 with tumor lysis syndrome.
Dr Tam and his colleagues reported these results in NEJM.
The study included 24 patients—23 with relapsed/refractory MCL and 1 with previously untreated MCL. They had a median age of 68 (range, 47-81).
Most patients had high-risk (75%) or intermediate-risk (21%) disease, according to the MCL International Prognostic Index. Half of patients (including the previously untreated patient) had a TP53 aberration, and 25% had an NF-κB pathway mutation.
The relapsed/refractory patients had a median of 2 prior therapies (range, 1-6), and 48% were refractory to their most recent therapy.
Patients received ibrutinib monotherapy at 560 mg daily for 4 weeks. Then, patients began receiving venetoclax as well, in increasing doses, up to 400 mg per day. Patients received treatment until progression or unacceptable toxicity.
Efficacy
The study’s primary endpoint was CR at week 16, as assessed without PET. This was to allow the researchers to compare CR results in this trial to CR results in the PCYC-1104-CA study, a phase 2 trial of ibrutinib monotherapy in MCL.
According to CT, the CR rate was 42% in patients who received venetoclax and ibrutinib. This is significantly higher than the 9% CR rate observed in the patients treated with ibrutinib alone (P<0.001).
However, according to PET/CT, the 16-week CR rate was 62% in patients who received venetoclax and ibrutinib, and the overall response rate was 71%.
Overall, the rate of minimal residual disease (MRD) negativity was 67% (n=16) in the bone marrow according to flow cytometry and 38% (n=9) in the blood according to allele-specific oligonucleotide-polymerase chain reaction (ASO-PCR). However, not all patients were evaluable for MRD.
Among evaluable patients with a CR, 93% (14/15) were MRD negative according to flow cytometry, and 82% (9/11) were negative according to ASO-PCR.
The median progression-free survival was not reached at a median follow-up of 15.9 months. The estimated progression-free survival was 75% at 12 months and 57% at 18 months.
The rate of overall survival was 79% at 12 months and 74% at 18 months.
“These very promising results have triggered additional and larger studies to better understand the synergistic benefits of the venetoclax-ibrutinib treatment combination in MCL patients,” Dr Tam said.
Safety
The most common AEs were diarrhea (83%); fatigue (75%); nausea/vomiting (71%); bleeding, bruising, or postoperative hemorrhage (54%); musculoskeletal or connective-tissue pain (50%); cough or dyspnea (46%); soft-tissue infection (42%); upper respiratory tract infection (42%); neutropenia (33%); and lower respiratory tract infection (33%).
Grade 3/4 AEs included neutropenia (33%), thrombocytopenia (17%), anemia (12%), diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), lower respiratory tract infection (8%), soft-tissue infection (8%), cough or dyspnea (4%), musculoskeletal or connective-tissue pain (4%), and bleeding, bruising, or postoperative hemorrhage (4%).
Serious AEs included diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), pyrexia (8%), pleural effusion (8%), cardiac failure (4%), and soft-tissue infection (4%).
The patients who developed tumor lysis syndrome were among the first 15 patients who started venetoclax at a dose of 50 mg per day. Because of these cases, the study protocol was amended to lower the starting dose of venetoclax to 20 mg daily. After that, there were no additional cases of tumor lysis syndrome.
There were 6 deaths during the study. Four were attributed to disease progression, 1 to malignant otitis externa, and 1 to cardiac failure in a patient in CR.
A 2-drug combination can improve outcomes in patients with mantle cell lymphoma (MCL), according to researchers.
In a phase 2 trial of MCL patients, the BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax produced an overall response rate of 71% and a complete response (CR) rate of 62%.
“This was in patients who we expected to have a poor outcome on conventional therapy, and in which treatment with either ibrutinib or venetoclax alone was expected to see only 21% of patients show a complete response,” said Constantine Tam, MBBS, MD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
The most common adverse events (AEs) in patients receiving venetoclax and ibrutinib were diarrhea (83%), fatigue (75%), and nausea/vomiting (71%). Fourteen patients (58%) had serious AEs, including 2 with tumor lysis syndrome.
Dr Tam and his colleagues reported these results in NEJM.
The study included 24 patients—23 with relapsed/refractory MCL and 1 with previously untreated MCL. They had a median age of 68 (range, 47-81).
Most patients had high-risk (75%) or intermediate-risk (21%) disease, according to the MCL International Prognostic Index. Half of patients (including the previously untreated patient) had a TP53 aberration, and 25% had an NF-κB pathway mutation.
The relapsed/refractory patients had a median of 2 prior therapies (range, 1-6), and 48% were refractory to their most recent therapy.
Patients received ibrutinib monotherapy at 560 mg daily for 4 weeks. Then, patients began receiving venetoclax as well, in increasing doses, up to 400 mg per day. Patients received treatment until progression or unacceptable toxicity.
Efficacy
The study’s primary endpoint was CR at week 16, as assessed without PET. This was to allow the researchers to compare CR results in this trial to CR results in the PCYC-1104-CA study, a phase 2 trial of ibrutinib monotherapy in MCL.
According to CT, the CR rate was 42% in patients who received venetoclax and ibrutinib. This is significantly higher than the 9% CR rate observed in the patients treated with ibrutinib alone (P<0.001).
However, according to PET/CT, the 16-week CR rate was 62% in patients who received venetoclax and ibrutinib, and the overall response rate was 71%.
Overall, the rate of minimal residual disease (MRD) negativity was 67% (n=16) in the bone marrow according to flow cytometry and 38% (n=9) in the blood according to allele-specific oligonucleotide-polymerase chain reaction (ASO-PCR). However, not all patients were evaluable for MRD.
Among evaluable patients with a CR, 93% (14/15) were MRD negative according to flow cytometry, and 82% (9/11) were negative according to ASO-PCR.
The median progression-free survival was not reached at a median follow-up of 15.9 months. The estimated progression-free survival was 75% at 12 months and 57% at 18 months.
The rate of overall survival was 79% at 12 months and 74% at 18 months.
“These very promising results have triggered additional and larger studies to better understand the synergistic benefits of the venetoclax-ibrutinib treatment combination in MCL patients,” Dr Tam said.
Safety
The most common AEs were diarrhea (83%); fatigue (75%); nausea/vomiting (71%); bleeding, bruising, or postoperative hemorrhage (54%); musculoskeletal or connective-tissue pain (50%); cough or dyspnea (46%); soft-tissue infection (42%); upper respiratory tract infection (42%); neutropenia (33%); and lower respiratory tract infection (33%).
Grade 3/4 AEs included neutropenia (33%), thrombocytopenia (17%), anemia (12%), diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), lower respiratory tract infection (8%), soft-tissue infection (8%), cough or dyspnea (4%), musculoskeletal or connective-tissue pain (4%), and bleeding, bruising, or postoperative hemorrhage (4%).
Serious AEs included diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), pyrexia (8%), pleural effusion (8%), cardiac failure (4%), and soft-tissue infection (4%).
The patients who developed tumor lysis syndrome were among the first 15 patients who started venetoclax at a dose of 50 mg per day. Because of these cases, the study protocol was amended to lower the starting dose of venetoclax to 20 mg daily. After that, there were no additional cases of tumor lysis syndrome.
There were 6 deaths during the study. Four were attributed to disease progression, 1 to malignant otitis externa, and 1 to cardiac failure in a patient in CR.
A 2-drug combination can improve outcomes in patients with mantle cell lymphoma (MCL), according to researchers.
In a phase 2 trial of MCL patients, the BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax produced an overall response rate of 71% and a complete response (CR) rate of 62%.
“This was in patients who we expected to have a poor outcome on conventional therapy, and in which treatment with either ibrutinib or venetoclax alone was expected to see only 21% of patients show a complete response,” said Constantine Tam, MBBS, MD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
The most common adverse events (AEs) in patients receiving venetoclax and ibrutinib were diarrhea (83%), fatigue (75%), and nausea/vomiting (71%). Fourteen patients (58%) had serious AEs, including 2 with tumor lysis syndrome.
Dr Tam and his colleagues reported these results in NEJM.
The study included 24 patients—23 with relapsed/refractory MCL and 1 with previously untreated MCL. They had a median age of 68 (range, 47-81).
Most patients had high-risk (75%) or intermediate-risk (21%) disease, according to the MCL International Prognostic Index. Half of patients (including the previously untreated patient) had a TP53 aberration, and 25% had an NF-κB pathway mutation.
The relapsed/refractory patients had a median of 2 prior therapies (range, 1-6), and 48% were refractory to their most recent therapy.
Patients received ibrutinib monotherapy at 560 mg daily for 4 weeks. Then, patients began receiving venetoclax as well, in increasing doses, up to 400 mg per day. Patients received treatment until progression or unacceptable toxicity.
Efficacy
The study’s primary endpoint was CR at week 16, as assessed without PET. This was to allow the researchers to compare CR results in this trial to CR results in the PCYC-1104-CA study, a phase 2 trial of ibrutinib monotherapy in MCL.
According to CT, the CR rate was 42% in patients who received venetoclax and ibrutinib. This is significantly higher than the 9% CR rate observed in the patients treated with ibrutinib alone (P<0.001).
However, according to PET/CT, the 16-week CR rate was 62% in patients who received venetoclax and ibrutinib, and the overall response rate was 71%.
Overall, the rate of minimal residual disease (MRD) negativity was 67% (n=16) in the bone marrow according to flow cytometry and 38% (n=9) in the blood according to allele-specific oligonucleotide-polymerase chain reaction (ASO-PCR). However, not all patients were evaluable for MRD.
Among evaluable patients with a CR, 93% (14/15) were MRD negative according to flow cytometry, and 82% (9/11) were negative according to ASO-PCR.
The median progression-free survival was not reached at a median follow-up of 15.9 months. The estimated progression-free survival was 75% at 12 months and 57% at 18 months.
The rate of overall survival was 79% at 12 months and 74% at 18 months.
“These very promising results have triggered additional and larger studies to better understand the synergistic benefits of the venetoclax-ibrutinib treatment combination in MCL patients,” Dr Tam said.
Safety
The most common AEs were diarrhea (83%); fatigue (75%); nausea/vomiting (71%); bleeding, bruising, or postoperative hemorrhage (54%); musculoskeletal or connective-tissue pain (50%); cough or dyspnea (46%); soft-tissue infection (42%); upper respiratory tract infection (42%); neutropenia (33%); and lower respiratory tract infection (33%).
Grade 3/4 AEs included neutropenia (33%), thrombocytopenia (17%), anemia (12%), diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), lower respiratory tract infection (8%), soft-tissue infection (8%), cough or dyspnea (4%), musculoskeletal or connective-tissue pain (4%), and bleeding, bruising, or postoperative hemorrhage (4%).
Serious AEs included diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), pyrexia (8%), pleural effusion (8%), cardiac failure (4%), and soft-tissue infection (4%).
The patients who developed tumor lysis syndrome were among the first 15 patients who started venetoclax at a dose of 50 mg per day. Because of these cases, the study protocol was amended to lower the starting dose of venetoclax to 20 mg daily. After that, there were no additional cases of tumor lysis syndrome.
There were 6 deaths during the study. Four were attributed to disease progression, 1 to malignant otitis externa, and 1 to cardiac failure in a patient in CR.
Tenalisib receives orphan designation for CTCL
The US Food and Drug Administration (FDA) has granted orphan drug designation to tenalisib for treatment of cutaneous T-cell lymphoma (CTCL).
Tenalisib (formerly RP6530) is a dual PI3K delta/gamma inhibitor under development by Rhizen Pharmaceuticals SA.
The FDA previously granted tenalisib fast track and orphan drug designations for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib has been investigated in a phase 1 trial of patients with relapsed/refractory PTCL and CTCL. Results from this trial were presented at the 10th Annual T-cell Lymphoma Forum in February.
The data included 55 patients—28 with CTCL and 27 with PTCL—who received varying doses of tenalisib. The maximum tolerated dose was an 800 mg daily fasting dose.
Fourteen PTCL patients were evaluable for efficacy, and 7 responded (50%) to treatment. Three patients had a complete response, and 4 had a partial response.
Eighteen CTCL patients were evaluable for efficacy. Eight patients responded (44%), all with partial responses.
In the entire cohort, treatment-related adverse events (AEs) of grade 3 or higher included transaminitis (20%), rash (5%), neutropenia (2%), hypophosphatemia (2%), international normalized ratio increase (2%), sepsis (2%), pyrexia (2%), and diplopia secondary to neuropathy (2%).
Four CTCL patients stopped tenalisib due to a treatment-related AE—transaminitis, sepsis, diarrhea, and diplopia secondary to neuropathy. One PTCL patient stopped treatment due to a related AE, which was transaminitis.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.
The US Food and Drug Administration (FDA) has granted orphan drug designation to tenalisib for treatment of cutaneous T-cell lymphoma (CTCL).
Tenalisib (formerly RP6530) is a dual PI3K delta/gamma inhibitor under development by Rhizen Pharmaceuticals SA.
The FDA previously granted tenalisib fast track and orphan drug designations for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib has been investigated in a phase 1 trial of patients with relapsed/refractory PTCL and CTCL. Results from this trial were presented at the 10th Annual T-cell Lymphoma Forum in February.
The data included 55 patients—28 with CTCL and 27 with PTCL—who received varying doses of tenalisib. The maximum tolerated dose was an 800 mg daily fasting dose.
Fourteen PTCL patients were evaluable for efficacy, and 7 responded (50%) to treatment. Three patients had a complete response, and 4 had a partial response.
Eighteen CTCL patients were evaluable for efficacy. Eight patients responded (44%), all with partial responses.
In the entire cohort, treatment-related adverse events (AEs) of grade 3 or higher included transaminitis (20%), rash (5%), neutropenia (2%), hypophosphatemia (2%), international normalized ratio increase (2%), sepsis (2%), pyrexia (2%), and diplopia secondary to neuropathy (2%).
Four CTCL patients stopped tenalisib due to a treatment-related AE—transaminitis, sepsis, diarrhea, and diplopia secondary to neuropathy. One PTCL patient stopped treatment due to a related AE, which was transaminitis.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.
The US Food and Drug Administration (FDA) has granted orphan drug designation to tenalisib for treatment of cutaneous T-cell lymphoma (CTCL).
Tenalisib (formerly RP6530) is a dual PI3K delta/gamma inhibitor under development by Rhizen Pharmaceuticals SA.
The FDA previously granted tenalisib fast track and orphan drug designations for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib has been investigated in a phase 1 trial of patients with relapsed/refractory PTCL and CTCL. Results from this trial were presented at the 10th Annual T-cell Lymphoma Forum in February.
The data included 55 patients—28 with CTCL and 27 with PTCL—who received varying doses of tenalisib. The maximum tolerated dose was an 800 mg daily fasting dose.
Fourteen PTCL patients were evaluable for efficacy, and 7 responded (50%) to treatment. Three patients had a complete response, and 4 had a partial response.
Eighteen CTCL patients were evaluable for efficacy. Eight patients responded (44%), all with partial responses.
In the entire cohort, treatment-related adverse events (AEs) of grade 3 or higher included transaminitis (20%), rash (5%), neutropenia (2%), hypophosphatemia (2%), international normalized ratio increase (2%), sepsis (2%), pyrexia (2%), and diplopia secondary to neuropathy (2%).
Four CTCL patients stopped tenalisib due to a treatment-related AE—transaminitis, sepsis, diarrhea, and diplopia secondary to neuropathy. One PTCL patient stopped treatment due to a related AE, which was transaminitis.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.