User login
Overcoming resistance to ibrutinib in CLL
New research appears to explain why ibrutinib may be less effective in certain patients with chronic lymphocytic leukemia (CLL).
It seems the Bruton’s tyrosine kinase (BTK) inhibitor has a diminished capacity to delocalize and kill tumor cells expressing an adhesive protein called CD49d.
But combining ibrutinib with drugs that block CD49d activation could prevent CLL cells from sheltering in lymphoid organs.
Valter Gattei, MD, of CRO Aviano National Cancer Institute in Aviano, Italy, and his colleagues reported these findings in the Journal of Experimental Medicine.
The team noted that CD49d, the α chain of the CD49d/CD29 integrin heterodimer very late antigen 4 (VLA-4), is expressed in about 40% of CLL cases.
These patients tend to have poorer outcomes than patients who do not express CD49d, but the role of VLA-4 in CLL was unclear.
With this study, researchers found that B-cell receptor (BCR) signaling can activate VLA-4 in CD49d-expressing CLL cells, thereby enhancing the cells’ adhesiveness.
Even though ibrutinib treatment impaired BCR signaling in these cells, it was unable to fully prevent the pathway from activating VLA-4 and enhancing cell adhesion.
The researchers analyzed 3 cohorts of CLL patients and found that patients expressing higher levels of CD49d had reduced responses to ibrutinib.
The BTK inhibitor appeared less able to displace tumor cells from lymph nodes into the blood, resulting in decreased lymph node shrinkage and shorter progression-free survival times.
“Our results suggest that VLA-4-expressing CLL cells residing in the secondary lymphoid organs can receive BCR-mediated stimuli that can activate VLA-4 even in the presence of ibrutinib,” said study author Antonella Zucchetto, ScD, also of CRO Aviano National Cancer Institute.
“This activation leads to enhanced retention of VLA-4-positive CLL cells in tissue sites, thereby affecting patient outcome.”
Fortunately, the researchers found a way around this obstacle. Inhibiting BTK and phosphatidylinositide 3-kinase (PI3K) simultaneously completely blocked VLA-4 activation in CLL cells.
The researchers treated CLL cells with ibrutinib, the PI3K inhibitor idelalisib, or a combination of both.
Neither drug alone was able to fully block anti-IgM-induced VLA-4 activation. However, the team found that simultaneous inhibition of BTK and PI3K “completely abolished the integrin response to BCR triggering.”
The researchers also added idelalisib to ibrutinib-treated CLL cells (collected from patients at day 30 on ibrutinib) and observed a complete upset of anti-IgM–induced VLA-4 activation.
“Our data suggest that evaluation of CD49d expression in patients initiating ibrutinib therapy may identify those cases that would benefit from combination therapy approaches designed to completely block VLA-4 activation and VLA-4-mediated retention of leukemic cells in protective tissue compartments,” Dr Gattei said. ![]()
New research appears to explain why ibrutinib may be less effective in certain patients with chronic lymphocytic leukemia (CLL).
It seems the Bruton’s tyrosine kinase (BTK) inhibitor has a diminished capacity to delocalize and kill tumor cells expressing an adhesive protein called CD49d.
But combining ibrutinib with drugs that block CD49d activation could prevent CLL cells from sheltering in lymphoid organs.
Valter Gattei, MD, of CRO Aviano National Cancer Institute in Aviano, Italy, and his colleagues reported these findings in the Journal of Experimental Medicine.
The team noted that CD49d, the α chain of the CD49d/CD29 integrin heterodimer very late antigen 4 (VLA-4), is expressed in about 40% of CLL cases.
These patients tend to have poorer outcomes than patients who do not express CD49d, but the role of VLA-4 in CLL was unclear.
With this study, researchers found that B-cell receptor (BCR) signaling can activate VLA-4 in CD49d-expressing CLL cells, thereby enhancing the cells’ adhesiveness.
Even though ibrutinib treatment impaired BCR signaling in these cells, it was unable to fully prevent the pathway from activating VLA-4 and enhancing cell adhesion.
The researchers analyzed 3 cohorts of CLL patients and found that patients expressing higher levels of CD49d had reduced responses to ibrutinib.
The BTK inhibitor appeared less able to displace tumor cells from lymph nodes into the blood, resulting in decreased lymph node shrinkage and shorter progression-free survival times.
“Our results suggest that VLA-4-expressing CLL cells residing in the secondary lymphoid organs can receive BCR-mediated stimuli that can activate VLA-4 even in the presence of ibrutinib,” said study author Antonella Zucchetto, ScD, also of CRO Aviano National Cancer Institute.
“This activation leads to enhanced retention of VLA-4-positive CLL cells in tissue sites, thereby affecting patient outcome.”
Fortunately, the researchers found a way around this obstacle. Inhibiting BTK and phosphatidylinositide 3-kinase (PI3K) simultaneously completely blocked VLA-4 activation in CLL cells.
The researchers treated CLL cells with ibrutinib, the PI3K inhibitor idelalisib, or a combination of both.
Neither drug alone was able to fully block anti-IgM-induced VLA-4 activation. However, the team found that simultaneous inhibition of BTK and PI3K “completely abolished the integrin response to BCR triggering.”
The researchers also added idelalisib to ibrutinib-treated CLL cells (collected from patients at day 30 on ibrutinib) and observed a complete upset of anti-IgM–induced VLA-4 activation.
“Our data suggest that evaluation of CD49d expression in patients initiating ibrutinib therapy may identify those cases that would benefit from combination therapy approaches designed to completely block VLA-4 activation and VLA-4-mediated retention of leukemic cells in protective tissue compartments,” Dr Gattei said. ![]()
New research appears to explain why ibrutinib may be less effective in certain patients with chronic lymphocytic leukemia (CLL).
It seems the Bruton’s tyrosine kinase (BTK) inhibitor has a diminished capacity to delocalize and kill tumor cells expressing an adhesive protein called CD49d.
But combining ibrutinib with drugs that block CD49d activation could prevent CLL cells from sheltering in lymphoid organs.
Valter Gattei, MD, of CRO Aviano National Cancer Institute in Aviano, Italy, and his colleagues reported these findings in the Journal of Experimental Medicine.
The team noted that CD49d, the α chain of the CD49d/CD29 integrin heterodimer very late antigen 4 (VLA-4), is expressed in about 40% of CLL cases.
These patients tend to have poorer outcomes than patients who do not express CD49d, but the role of VLA-4 in CLL was unclear.
With this study, researchers found that B-cell receptor (BCR) signaling can activate VLA-4 in CD49d-expressing CLL cells, thereby enhancing the cells’ adhesiveness.
Even though ibrutinib treatment impaired BCR signaling in these cells, it was unable to fully prevent the pathway from activating VLA-4 and enhancing cell adhesion.
The researchers analyzed 3 cohorts of CLL patients and found that patients expressing higher levels of CD49d had reduced responses to ibrutinib.
The BTK inhibitor appeared less able to displace tumor cells from lymph nodes into the blood, resulting in decreased lymph node shrinkage and shorter progression-free survival times.
“Our results suggest that VLA-4-expressing CLL cells residing in the secondary lymphoid organs can receive BCR-mediated stimuli that can activate VLA-4 even in the presence of ibrutinib,” said study author Antonella Zucchetto, ScD, also of CRO Aviano National Cancer Institute.
“This activation leads to enhanced retention of VLA-4-positive CLL cells in tissue sites, thereby affecting patient outcome.”
Fortunately, the researchers found a way around this obstacle. Inhibiting BTK and phosphatidylinositide 3-kinase (PI3K) simultaneously completely blocked VLA-4 activation in CLL cells.
The researchers treated CLL cells with ibrutinib, the PI3K inhibitor idelalisib, or a combination of both.
Neither drug alone was able to fully block anti-IgM-induced VLA-4 activation. However, the team found that simultaneous inhibition of BTK and PI3K “completely abolished the integrin response to BCR triggering.”
The researchers also added idelalisib to ibrutinib-treated CLL cells (collected from patients at day 30 on ibrutinib) and observed a complete upset of anti-IgM–induced VLA-4 activation.
“Our data suggest that evaluation of CD49d expression in patients initiating ibrutinib therapy may identify those cases that would benefit from combination therapy approaches designed to completely block VLA-4 activation and VLA-4-mediated retention of leukemic cells in protective tissue compartments,” Dr Gattei said. ![]()
DLBCL survivors at greater risk of autoimmune, infectious diseases
ATLANTA—A population-based study indicates that, compared to other cancer survivors, patients who survive diffuse large B-cell lymphoma (DLBCL) have an increased risk of autoimmune and infectious diseases.
For example, investigators found the risk of being diagnosed with impaired humoral immunity was 16.2 times higher in female DLBCL survivors than in breast cancer survivors, 14.8 times higher in male DLBCL survivors than in prostate cancer survivors, and 12.5 times higher in all DLBCL survivors than in survivors of head and neck cancer.
“Most of the treatments that we give for lymphoma have profound effects on the immune system, either directly or indirectly, including many of the T-cell-directed therapies,” said Tanaya Shree, MD, PhD, of Stanford University Medical Center in California.
“There have been studies on many of the effects suffered by lymphoma survivors, but very little is known about their immune health.”
Dr Shree and her colleagues undertook this study to determine how the immune system fares in lymphoma survivors. The investigators limited their analysis to survivors of DLBCL.
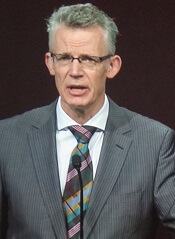
Dr Shree presented the findings at the 2017 ASH Annual Meeting (abstract 198*).
Study design
Investigators pulled data from the California Cancer Registry for patients with DLBCL as their first primary cancer diagnosed between 1991 and 2012. Patients had to be 18 or older at diagnosis and have survived more than a year after diagnosis.
“Importantly, we counted only diagnoses [of autoimmune and infectious diseases] that first appeared between 1 and 10 years after cancer diagnosis,” Dr Shree explained. “So any diagnosis we saw that had also been seen prior to cancer diagnosis or even up to 1 year post-cancer diagnosis, we considered to be pre-existing and were excluded from the analysis in order to really focus on new incident cases during survivorship.”
Investigators used the same criteria for the comparator cohorts.
The survivor data was linked to statewide discharge databases, and investigators performed the incidence analysis based on ICD-9 codes.
Investigators used Poisson regression analysis to obtain incident ratios and adjusted the models for age, race, and year of diagnosis.
They graphed the incident rate ratios for all the diagnoses that were significantly different between the DLBCL cohort and the comparator cohorts.
“[W]e considered a P value of less than 0.0005 to be significant,” Dr Shree clarified.
Survivor characteristics
The cohorts comprised 802,255 survivors of DLBCL (n=21,690), breast cancer (n=337,591), prostate cancer (n=325,533), melanoma (n=73,196), and head and neck cancer (n=44,245).
“At least 75% of patients in each cohort were aged 40 to 79,” Dr Shree noted, “with a good representation of elderly patients.”
The median follow-up time was 6.1 years for DLBCL patients and ranged from 5.7 years for head and neck cancer survivors to 8.3 years for prostate cancer survivors.
About three-quarters of patients in each cohort had hospitalization data within 1 to 10 years from cancer diagnosis.
DLBCL vs breast cancer
“Interestingly, we found some familiar names amongst the top-scoring diagnoses,” Dr Shree said.
Deficiency of humoral immunity (16.2-fold), autoimmune hemolytic anemia (9.9-fold), Sicca syndrome (6.9-fold), and immune thrombocytopenia (3.1-fold) were higher in female DLBCL survivors than breast cancer survivors.
“All of these have known associations with lymphoma,” Dr Shree said. “But we also found, surprisingly, increased rates of fungal [6.0-fold] and viral pneumonia [3.3-fold], and many other codes associated with respiratory infections. We also found a 3-fold increased rate of meningitis.”
“The only diagnosis statistically more common amongst breast cancer patients was cervicitis and endocervicitis, and this likely relates to the fact that many of these patients are undergoing hormone therapy.”
DLBCL vs prostate cancer
“We saw some of the same diagnoses come up as top-scoring hits, including viral [4.5-fold] and fungal pneumonia [8.2-fold], and meningitis [3.9-fold], and, in this case, Staphylococcal meningitis [8.6-fold],” Dr Shree said.
Deficiency of humoral immunity (14.8-fold), autoimmune hemolytic anemia (8.9-fold), Sicca syndrome (8.6-fold), and immune thrombocytopenia (4.8-fold) were also higher in the male DLBCL survivors than in prostate cancer survivors.
“No diagnoses were statistically more common in the prostate cancer survivors [than in male DLBCL survivors],” Dr Shree noted.
DLBCL vs head and neck cancer
“Again, the top 4 hits were the same 4 diagnoses we have been seeing repeatedly,” Dr Shree said.
Deficiency of humoral immunity (12.5-fold), autoimmune hemolytic anemia (9.3-fold), Sicca syndrome (5.5-fold), and immune thrombocytopenia (4.5-fold) were increased for DLBCL survivors compared to survivors of head and neck cancer.
DLBCL survivors also had an increased risk of respiratory infections, especially viral (4.4-fold) and fungal pneumonias (4.0-fold), meningitis (3.0-fold), and chronic lymphocytic thyroiditis (2.8-fold), also known as Hashimoto’s thyroiditis.
On the other hand, bacterial pneumonias and skin infections were more common in the head and neck cancer survivors than in DLBCL survivors.
DLBCL vs melanoma
“Interestingly, we did not see an increased risk for immune thrombocytopenias [in DLBCL survivors] compared to melanoma survivors in this comparison, which we had in all the other comparisons,” Dr Shree noted.
“But we did see [an increased risk for] the other diagnoses that we had been tracking, including, again, fungal pneumonia [6.9-fold], viral pneumonia [4.7-fold], and miscellaneous viral infections [2.6-fold].”
The only diagnosis that was statistically more common among melanoma survivors than DLBCL survivors was vitiligo.
Risks persist over time
The investigators assessed whether the elevated risks were static over the 1- to 10-year analysis period.
They took the top diagnoses—humoral deficiency, autoimmune hemolytic anemia, Sicca syndrome, and immune thrombocytopenia—and reviewed them for all cohorts to determine the rate of new cases.
“[F]or 3 out of these 4 diagnoses [humoral deficiency, autoimmune hemolytic anemia, and Sicca syndrome], increased incident rates are highest in the first 1 to 3 years after diagnosis in the lymphoma patients,” Dr Shree said.
“But even at 5 to 10 years out, these patients continue to have increased incidence of these diagnoses compared to the other cohorts, suggesting that these risks really do remain elevated over some time.”
The investigators repeated the analysis using broader categories of diagnoses with each category encompassing many ICD-9 codes.
“[I]n 12 out of 18 broad categories that we looked at, we can still find statistically significant differences in the incident rates for these diagnoses, and they were all increased in the lymphoma patients compared to the other cohorts,” Dr Shree explained.
“[T]hese increases were seen across multiple comparisons, suggesting that this phenomenon seems to be really lymphoma-specific and not specific to any of the individual comparisons we had chosen to perform.”
The findings, she said, have a lot of implications.
“We are particularly interested in which features of patients’ treatment contribute most to these elevated risks,” Dr Shree said. “And, of course, we want to know what to be able to tell our patients and how to follow them during survivorship.”
The investigators are currently validating their findings with further analysis of the Stanford lymphoma survivors cohort of approximately 3500 patients. ![]()
*Data in the abstract differ from the presentation.
ATLANTA—A population-based study indicates that, compared to other cancer survivors, patients who survive diffuse large B-cell lymphoma (DLBCL) have an increased risk of autoimmune and infectious diseases.
For example, investigators found the risk of being diagnosed with impaired humoral immunity was 16.2 times higher in female DLBCL survivors than in breast cancer survivors, 14.8 times higher in male DLBCL survivors than in prostate cancer survivors, and 12.5 times higher in all DLBCL survivors than in survivors of head and neck cancer.
“Most of the treatments that we give for lymphoma have profound effects on the immune system, either directly or indirectly, including many of the T-cell-directed therapies,” said Tanaya Shree, MD, PhD, of Stanford University Medical Center in California.
“There have been studies on many of the effects suffered by lymphoma survivors, but very little is known about their immune health.”
Dr Shree and her colleagues undertook this study to determine how the immune system fares in lymphoma survivors. The investigators limited their analysis to survivors of DLBCL.
Dr Shree presented the findings at the 2017 ASH Annual Meeting (abstract 198*).
Study design
Investigators pulled data from the California Cancer Registry for patients with DLBCL as their first primary cancer diagnosed between 1991 and 2012. Patients had to be 18 or older at diagnosis and have survived more than a year after diagnosis.
“Importantly, we counted only diagnoses [of autoimmune and infectious diseases] that first appeared between 1 and 10 years after cancer diagnosis,” Dr Shree explained. “So any diagnosis we saw that had also been seen prior to cancer diagnosis or even up to 1 year post-cancer diagnosis, we considered to be pre-existing and were excluded from the analysis in order to really focus on new incident cases during survivorship.”
Investigators used the same criteria for the comparator cohorts.
The survivor data was linked to statewide discharge databases, and investigators performed the incidence analysis based on ICD-9 codes.
Investigators used Poisson regression analysis to obtain incident ratios and adjusted the models for age, race, and year of diagnosis.
They graphed the incident rate ratios for all the diagnoses that were significantly different between the DLBCL cohort and the comparator cohorts.
“[W]e considered a P value of less than 0.0005 to be significant,” Dr Shree clarified.
Survivor characteristics
The cohorts comprised 802,255 survivors of DLBCL (n=21,690), breast cancer (n=337,591), prostate cancer (n=325,533), melanoma (n=73,196), and head and neck cancer (n=44,245).
“At least 75% of patients in each cohort were aged 40 to 79,” Dr Shree noted, “with a good representation of elderly patients.”
The median follow-up time was 6.1 years for DLBCL patients and ranged from 5.7 years for head and neck cancer survivors to 8.3 years for prostate cancer survivors.
About three-quarters of patients in each cohort had hospitalization data within 1 to 10 years from cancer diagnosis.
DLBCL vs breast cancer
“Interestingly, we found some familiar names amongst the top-scoring diagnoses,” Dr Shree said.
Deficiency of humoral immunity (16.2-fold), autoimmune hemolytic anemia (9.9-fold), Sicca syndrome (6.9-fold), and immune thrombocytopenia (3.1-fold) were higher in female DLBCL survivors than breast cancer survivors.
“All of these have known associations with lymphoma,” Dr Shree said. “But we also found, surprisingly, increased rates of fungal [6.0-fold] and viral pneumonia [3.3-fold], and many other codes associated with respiratory infections. We also found a 3-fold increased rate of meningitis.”
“The only diagnosis statistically more common amongst breast cancer patients was cervicitis and endocervicitis, and this likely relates to the fact that many of these patients are undergoing hormone therapy.”
DLBCL vs prostate cancer
“We saw some of the same diagnoses come up as top-scoring hits, including viral [4.5-fold] and fungal pneumonia [8.2-fold], and meningitis [3.9-fold], and, in this case, Staphylococcal meningitis [8.6-fold],” Dr Shree said.
Deficiency of humoral immunity (14.8-fold), autoimmune hemolytic anemia (8.9-fold), Sicca syndrome (8.6-fold), and immune thrombocytopenia (4.8-fold) were also higher in the male DLBCL survivors than in prostate cancer survivors.
“No diagnoses were statistically more common in the prostate cancer survivors [than in male DLBCL survivors],” Dr Shree noted.
DLBCL vs head and neck cancer
“Again, the top 4 hits were the same 4 diagnoses we have been seeing repeatedly,” Dr Shree said.
Deficiency of humoral immunity (12.5-fold), autoimmune hemolytic anemia (9.3-fold), Sicca syndrome (5.5-fold), and immune thrombocytopenia (4.5-fold) were increased for DLBCL survivors compared to survivors of head and neck cancer.
DLBCL survivors also had an increased risk of respiratory infections, especially viral (4.4-fold) and fungal pneumonias (4.0-fold), meningitis (3.0-fold), and chronic lymphocytic thyroiditis (2.8-fold), also known as Hashimoto’s thyroiditis.
On the other hand, bacterial pneumonias and skin infections were more common in the head and neck cancer survivors than in DLBCL survivors.
DLBCL vs melanoma
“Interestingly, we did not see an increased risk for immune thrombocytopenias [in DLBCL survivors] compared to melanoma survivors in this comparison, which we had in all the other comparisons,” Dr Shree noted.
“But we did see [an increased risk for] the other diagnoses that we had been tracking, including, again, fungal pneumonia [6.9-fold], viral pneumonia [4.7-fold], and miscellaneous viral infections [2.6-fold].”
The only diagnosis that was statistically more common among melanoma survivors than DLBCL survivors was vitiligo.
Risks persist over time
The investigators assessed whether the elevated risks were static over the 1- to 10-year analysis period.
They took the top diagnoses—humoral deficiency, autoimmune hemolytic anemia, Sicca syndrome, and immune thrombocytopenia—and reviewed them for all cohorts to determine the rate of new cases.
“[F]or 3 out of these 4 diagnoses [humoral deficiency, autoimmune hemolytic anemia, and Sicca syndrome], increased incident rates are highest in the first 1 to 3 years after diagnosis in the lymphoma patients,” Dr Shree said.
“But even at 5 to 10 years out, these patients continue to have increased incidence of these diagnoses compared to the other cohorts, suggesting that these risks really do remain elevated over some time.”
The investigators repeated the analysis using broader categories of diagnoses with each category encompassing many ICD-9 codes.
“[I]n 12 out of 18 broad categories that we looked at, we can still find statistically significant differences in the incident rates for these diagnoses, and they were all increased in the lymphoma patients compared to the other cohorts,” Dr Shree explained.
“[T]hese increases were seen across multiple comparisons, suggesting that this phenomenon seems to be really lymphoma-specific and not specific to any of the individual comparisons we had chosen to perform.”
The findings, she said, have a lot of implications.
“We are particularly interested in which features of patients’ treatment contribute most to these elevated risks,” Dr Shree said. “And, of course, we want to know what to be able to tell our patients and how to follow them during survivorship.”
The investigators are currently validating their findings with further analysis of the Stanford lymphoma survivors cohort of approximately 3500 patients. ![]()
*Data in the abstract differ from the presentation.
ATLANTA—A population-based study indicates that, compared to other cancer survivors, patients who survive diffuse large B-cell lymphoma (DLBCL) have an increased risk of autoimmune and infectious diseases.
For example, investigators found the risk of being diagnosed with impaired humoral immunity was 16.2 times higher in female DLBCL survivors than in breast cancer survivors, 14.8 times higher in male DLBCL survivors than in prostate cancer survivors, and 12.5 times higher in all DLBCL survivors than in survivors of head and neck cancer.
“Most of the treatments that we give for lymphoma have profound effects on the immune system, either directly or indirectly, including many of the T-cell-directed therapies,” said Tanaya Shree, MD, PhD, of Stanford University Medical Center in California.
“There have been studies on many of the effects suffered by lymphoma survivors, but very little is known about their immune health.”
Dr Shree and her colleagues undertook this study to determine how the immune system fares in lymphoma survivors. The investigators limited their analysis to survivors of DLBCL.
Dr Shree presented the findings at the 2017 ASH Annual Meeting (abstract 198*).
Study design
Investigators pulled data from the California Cancer Registry for patients with DLBCL as their first primary cancer diagnosed between 1991 and 2012. Patients had to be 18 or older at diagnosis and have survived more than a year after diagnosis.
“Importantly, we counted only diagnoses [of autoimmune and infectious diseases] that first appeared between 1 and 10 years after cancer diagnosis,” Dr Shree explained. “So any diagnosis we saw that had also been seen prior to cancer diagnosis or even up to 1 year post-cancer diagnosis, we considered to be pre-existing and were excluded from the analysis in order to really focus on new incident cases during survivorship.”
Investigators used the same criteria for the comparator cohorts.
The survivor data was linked to statewide discharge databases, and investigators performed the incidence analysis based on ICD-9 codes.
Investigators used Poisson regression analysis to obtain incident ratios and adjusted the models for age, race, and year of diagnosis.
They graphed the incident rate ratios for all the diagnoses that were significantly different between the DLBCL cohort and the comparator cohorts.
“[W]e considered a P value of less than 0.0005 to be significant,” Dr Shree clarified.
Survivor characteristics
The cohorts comprised 802,255 survivors of DLBCL (n=21,690), breast cancer (n=337,591), prostate cancer (n=325,533), melanoma (n=73,196), and head and neck cancer (n=44,245).
“At least 75% of patients in each cohort were aged 40 to 79,” Dr Shree noted, “with a good representation of elderly patients.”
The median follow-up time was 6.1 years for DLBCL patients and ranged from 5.7 years for head and neck cancer survivors to 8.3 years for prostate cancer survivors.
About three-quarters of patients in each cohort had hospitalization data within 1 to 10 years from cancer diagnosis.
DLBCL vs breast cancer
“Interestingly, we found some familiar names amongst the top-scoring diagnoses,” Dr Shree said.
Deficiency of humoral immunity (16.2-fold), autoimmune hemolytic anemia (9.9-fold), Sicca syndrome (6.9-fold), and immune thrombocytopenia (3.1-fold) were higher in female DLBCL survivors than breast cancer survivors.
“All of these have known associations with lymphoma,” Dr Shree said. “But we also found, surprisingly, increased rates of fungal [6.0-fold] and viral pneumonia [3.3-fold], and many other codes associated with respiratory infections. We also found a 3-fold increased rate of meningitis.”
“The only diagnosis statistically more common amongst breast cancer patients was cervicitis and endocervicitis, and this likely relates to the fact that many of these patients are undergoing hormone therapy.”
DLBCL vs prostate cancer
“We saw some of the same diagnoses come up as top-scoring hits, including viral [4.5-fold] and fungal pneumonia [8.2-fold], and meningitis [3.9-fold], and, in this case, Staphylococcal meningitis [8.6-fold],” Dr Shree said.
Deficiency of humoral immunity (14.8-fold), autoimmune hemolytic anemia (8.9-fold), Sicca syndrome (8.6-fold), and immune thrombocytopenia (4.8-fold) were also higher in the male DLBCL survivors than in prostate cancer survivors.
“No diagnoses were statistically more common in the prostate cancer survivors [than in male DLBCL survivors],” Dr Shree noted.
DLBCL vs head and neck cancer
“Again, the top 4 hits were the same 4 diagnoses we have been seeing repeatedly,” Dr Shree said.
Deficiency of humoral immunity (12.5-fold), autoimmune hemolytic anemia (9.3-fold), Sicca syndrome (5.5-fold), and immune thrombocytopenia (4.5-fold) were increased for DLBCL survivors compared to survivors of head and neck cancer.
DLBCL survivors also had an increased risk of respiratory infections, especially viral (4.4-fold) and fungal pneumonias (4.0-fold), meningitis (3.0-fold), and chronic lymphocytic thyroiditis (2.8-fold), also known as Hashimoto’s thyroiditis.
On the other hand, bacterial pneumonias and skin infections were more common in the head and neck cancer survivors than in DLBCL survivors.
DLBCL vs melanoma
“Interestingly, we did not see an increased risk for immune thrombocytopenias [in DLBCL survivors] compared to melanoma survivors in this comparison, which we had in all the other comparisons,” Dr Shree noted.
“But we did see [an increased risk for] the other diagnoses that we had been tracking, including, again, fungal pneumonia [6.9-fold], viral pneumonia [4.7-fold], and miscellaneous viral infections [2.6-fold].”
The only diagnosis that was statistically more common among melanoma survivors than DLBCL survivors was vitiligo.
Risks persist over time
The investigators assessed whether the elevated risks were static over the 1- to 10-year analysis period.
They took the top diagnoses—humoral deficiency, autoimmune hemolytic anemia, Sicca syndrome, and immune thrombocytopenia—and reviewed them for all cohorts to determine the rate of new cases.
“[F]or 3 out of these 4 diagnoses [humoral deficiency, autoimmune hemolytic anemia, and Sicca syndrome], increased incident rates are highest in the first 1 to 3 years after diagnosis in the lymphoma patients,” Dr Shree said.
“But even at 5 to 10 years out, these patients continue to have increased incidence of these diagnoses compared to the other cohorts, suggesting that these risks really do remain elevated over some time.”
The investigators repeated the analysis using broader categories of diagnoses with each category encompassing many ICD-9 codes.
“[I]n 12 out of 18 broad categories that we looked at, we can still find statistically significant differences in the incident rates for these diagnoses, and they were all increased in the lymphoma patients compared to the other cohorts,” Dr Shree explained.
“[T]hese increases were seen across multiple comparisons, suggesting that this phenomenon seems to be really lymphoma-specific and not specific to any of the individual comparisons we had chosen to perform.”
The findings, she said, have a lot of implications.
“We are particularly interested in which features of patients’ treatment contribute most to these elevated risks,” Dr Shree said. “And, of course, we want to know what to be able to tell our patients and how to follow them during survivorship.”
The investigators are currently validating their findings with further analysis of the Stanford lymphoma survivors cohort of approximately 3500 patients. ![]()
*Data in the abstract differ from the presentation.
Update reveals ongoing responses in ZUMA-1
ATLANTA—The chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (axi-cel; KTE-C19) is showing consistent, ongoing responses more than a year after infusion.
An updated analysis of the phase 1/2 ZUMA-1 trial showed that 42% of patients who received axi-cel maintained an objective response at a median follow-up of 15.4 months.
Forty percent of patients have maintained a complete response (CR).
This compares with a 44% objective response rate and a 39% CR rate in the primary analysis of phase 2 ZUMA-1 data, when the median follow-up was 8.7 months.
Sattva S. Neelapu, MD, of MD Anderson Cancer Center in Houston, Texas, reported the long-term results from ZUMA-1 at the 2017 ASH Annual Meeting (abstract 578). The findings were published simultaneously in NEJM.
The primary phase 2 analysis was previously presented at the AACR Annual Meeting 2017.
At ASH 2017, Dr Neelapu disclosed that he has received research funding and served as a consultant for Kite Pharma, the developer of axi-cel. Kite Pharma and the Leukemia & Lymphoma Society Therapy Acceleration Program supported ZUMA-1.
Study schema and patient characteristics
Phase 1 of ZUMA-1 enrolled 7 patients with diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), or transformed follicular lymphoma (TFL).
In phase 2, 101 patients were grouped into 2 cohorts—77 with refractory DLBCL and 24 with refractory PMBCL/TFL.
A total of 108 patients were treated in phases 1 and 2 and were included in the long-term pooled analysis.
Patients received a conditioning regimen of cyclophosphamide and fludarabine and, 2 days later, a fixed dose of axi-cel at 2 x 106 CAR T cells/kg.
“Importantly, the product could be manufactured for 99% of enrolled patients,” Dr Neelapu said. “Moreover, 91% of the enrolled patients were dosed with axi-cel, and there were no patients lost to follow-up.”
Patients in the pooled analysis were a median age of 58 (range, 23–76), and 27 (25%) were 65 or older.
Seventy-three patients (68%) were male, 62 (57%) had an ECOG status of 1, 90 (83%) had stage III or IV disease, and 48 (44%) had an IPI score of 3 to 4.
Seventy-six patients (70%) had received 3 or more prior therapies.
Eighty patients (74%) were refractory to their second or later line of therapy, and 70 (65%) had progressive disease as their best response to their last prior therapy. Twenty-five patients (23%) had relapsed after autologous stem cell transplant.
Response
The data cutoff for the long-term analysis was August 11, 2017.
In addition to the ongoing responses mentioned above, the best objective response was 82% in both the phase 2 primary analysis and the long-term analysis for phases 1 and 2.
CR as the best objective response increased from 54% in the primary analysis to 58% at the longer follow-up.
“We did observe deepening of the responses over time,” Dr Neelapu said. “At the time of the first tumor assessment, 60 patients had either partial remission or stable disease. But 23 of those 60 eventually achieved a complete remission up to 15 months post-infusion without any additional therapy.”
The median time to conversion from partial response to CR was 64 days (range, 49–242).
“The durability of these responses was observed consistently across key covariates,” Dr Neelapu added, “including the refractory subgroups, the disease stage groups, IPI risk groups. The CD19 status at baseline did not matter, nor did the cell of origin, or the CD4/CD8 ratio of the product.”
Furthermore, the investigators observed no differences in patients who received tocilizumab or corticosteroids.
The median duration of response for all patients was 11.1 months. For those who achieved CR, the median duration of response has not yet been reached.
Three of the 7 patients (43%) in the phase 1 part of the trial had an ongoing CR at 24 months.
At the median follow-up of 15.4 months, 42% of patients were progression-free, and 56% were alive.
The median overall survival has not been reached. Investigators estimated the 18-month overall survival to be 52%.
Safety
Adverse events (AEs) of grade 3 or higher occurred in 97% of patients, and serious AEs of grade 3 or higher occurred in 46% of patients in the updated analysis.
No new axi-cel-related AEs of cytokine release syndrome, neurologic events, or grade 5 AEs have arisen since the primary analysis.
There were four grade 5 events, 2 of which were related to axi-cel.
“All these four grade 5 events were previously reported—three in the phase 2 and one in the phase 1 trial,” Dr Neelapu said.
Most patients experienced hypogammaglobulinemia and B-cell aplasia. Eight percent of patients had IVIG support during the study.
Infections, such as pneumonia, influenza, and viral infection, were the most common new-onset treatment-emergent serious AEs occurring after 6 months in 10 patients. All were manageable and resolved prior to the data cut-off.
Persistence and resistance
“We observed long-term persistence of the CAR T cells,” Dr Neelapu said.
CAR T cells persisted in 71% of patients still responding at 1 year. And durable responses were observed in patients with and without detectable CAR T cells.
A central review committee analyzed biopsies of 21 evaluable patients at progression to try to determine the mechanism of resistance.
Fourteen of 21 (67%) biopsies were CD19-positive. Of these, 9 were PD-L1-positive, 4 were PD-L1-negative, and 1 was not evaluable.
Seven patients (33%) were CD19-negative compared to baseline. Of these, 4 were PD-L1-positive, 2 were PD-L1-negative, and 1 was not evaluable.
“This PD-L1 expression was observed in both CD19-positive relapses and CD19-negative relapses,” Dr Neelapu emphasized.
Of the 21 patients, 62% were PD-L1-positive.
Investigators hypothesize that 2 potential mechanisms could contribute to relapse: loss of CD19 and expression of PD-L1.
Axi-cel (Yescarta™) was approved by the US Food and Drug Administration in October for the treatment of adults with relapsed or refractory large B-cell lymphoma. ![]()
ATLANTA—The chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (axi-cel; KTE-C19) is showing consistent, ongoing responses more than a year after infusion.
An updated analysis of the phase 1/2 ZUMA-1 trial showed that 42% of patients who received axi-cel maintained an objective response at a median follow-up of 15.4 months.
Forty percent of patients have maintained a complete response (CR).
This compares with a 44% objective response rate and a 39% CR rate in the primary analysis of phase 2 ZUMA-1 data, when the median follow-up was 8.7 months.
Sattva S. Neelapu, MD, of MD Anderson Cancer Center in Houston, Texas, reported the long-term results from ZUMA-1 at the 2017 ASH Annual Meeting (abstract 578). The findings were published simultaneously in NEJM.
The primary phase 2 analysis was previously presented at the AACR Annual Meeting 2017.
At ASH 2017, Dr Neelapu disclosed that he has received research funding and served as a consultant for Kite Pharma, the developer of axi-cel. Kite Pharma and the Leukemia & Lymphoma Society Therapy Acceleration Program supported ZUMA-1.
Study schema and patient characteristics
Phase 1 of ZUMA-1 enrolled 7 patients with diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), or transformed follicular lymphoma (TFL).
In phase 2, 101 patients were grouped into 2 cohorts—77 with refractory DLBCL and 24 with refractory PMBCL/TFL.
A total of 108 patients were treated in phases 1 and 2 and were included in the long-term pooled analysis.
Patients received a conditioning regimen of cyclophosphamide and fludarabine and, 2 days later, a fixed dose of axi-cel at 2 x 106 CAR T cells/kg.
“Importantly, the product could be manufactured for 99% of enrolled patients,” Dr Neelapu said. “Moreover, 91% of the enrolled patients were dosed with axi-cel, and there were no patients lost to follow-up.”
Patients in the pooled analysis were a median age of 58 (range, 23–76), and 27 (25%) were 65 or older.
Seventy-three patients (68%) were male, 62 (57%) had an ECOG status of 1, 90 (83%) had stage III or IV disease, and 48 (44%) had an IPI score of 3 to 4.
Seventy-six patients (70%) had received 3 or more prior therapies.
Eighty patients (74%) were refractory to their second or later line of therapy, and 70 (65%) had progressive disease as their best response to their last prior therapy. Twenty-five patients (23%) had relapsed after autologous stem cell transplant.
Response
The data cutoff for the long-term analysis was August 11, 2017.
In addition to the ongoing responses mentioned above, the best objective response was 82% in both the phase 2 primary analysis and the long-term analysis for phases 1 and 2.
CR as the best objective response increased from 54% in the primary analysis to 58% at the longer follow-up.
“We did observe deepening of the responses over time,” Dr Neelapu said. “At the time of the first tumor assessment, 60 patients had either partial remission or stable disease. But 23 of those 60 eventually achieved a complete remission up to 15 months post-infusion without any additional therapy.”
The median time to conversion from partial response to CR was 64 days (range, 49–242).
“The durability of these responses was observed consistently across key covariates,” Dr Neelapu added, “including the refractory subgroups, the disease stage groups, IPI risk groups. The CD19 status at baseline did not matter, nor did the cell of origin, or the CD4/CD8 ratio of the product.”
Furthermore, the investigators observed no differences in patients who received tocilizumab or corticosteroids.
The median duration of response for all patients was 11.1 months. For those who achieved CR, the median duration of response has not yet been reached.
Three of the 7 patients (43%) in the phase 1 part of the trial had an ongoing CR at 24 months.
At the median follow-up of 15.4 months, 42% of patients were progression-free, and 56% were alive.
The median overall survival has not been reached. Investigators estimated the 18-month overall survival to be 52%.
Safety
Adverse events (AEs) of grade 3 or higher occurred in 97% of patients, and serious AEs of grade 3 or higher occurred in 46% of patients in the updated analysis.
No new axi-cel-related AEs of cytokine release syndrome, neurologic events, or grade 5 AEs have arisen since the primary analysis.
There were four grade 5 events, 2 of which were related to axi-cel.
“All these four grade 5 events were previously reported—three in the phase 2 and one in the phase 1 trial,” Dr Neelapu said.
Most patients experienced hypogammaglobulinemia and B-cell aplasia. Eight percent of patients had IVIG support during the study.
Infections, such as pneumonia, influenza, and viral infection, were the most common new-onset treatment-emergent serious AEs occurring after 6 months in 10 patients. All were manageable and resolved prior to the data cut-off.
Persistence and resistance
“We observed long-term persistence of the CAR T cells,” Dr Neelapu said.
CAR T cells persisted in 71% of patients still responding at 1 year. And durable responses were observed in patients with and without detectable CAR T cells.
A central review committee analyzed biopsies of 21 evaluable patients at progression to try to determine the mechanism of resistance.
Fourteen of 21 (67%) biopsies were CD19-positive. Of these, 9 were PD-L1-positive, 4 were PD-L1-negative, and 1 was not evaluable.
Seven patients (33%) were CD19-negative compared to baseline. Of these, 4 were PD-L1-positive, 2 were PD-L1-negative, and 1 was not evaluable.
“This PD-L1 expression was observed in both CD19-positive relapses and CD19-negative relapses,” Dr Neelapu emphasized.
Of the 21 patients, 62% were PD-L1-positive.
Investigators hypothesize that 2 potential mechanisms could contribute to relapse: loss of CD19 and expression of PD-L1.
Axi-cel (Yescarta™) was approved by the US Food and Drug Administration in October for the treatment of adults with relapsed or refractory large B-cell lymphoma. ![]()
ATLANTA—The chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (axi-cel; KTE-C19) is showing consistent, ongoing responses more than a year after infusion.
An updated analysis of the phase 1/2 ZUMA-1 trial showed that 42% of patients who received axi-cel maintained an objective response at a median follow-up of 15.4 months.
Forty percent of patients have maintained a complete response (CR).
This compares with a 44% objective response rate and a 39% CR rate in the primary analysis of phase 2 ZUMA-1 data, when the median follow-up was 8.7 months.
Sattva S. Neelapu, MD, of MD Anderson Cancer Center in Houston, Texas, reported the long-term results from ZUMA-1 at the 2017 ASH Annual Meeting (abstract 578). The findings were published simultaneously in NEJM.
The primary phase 2 analysis was previously presented at the AACR Annual Meeting 2017.
At ASH 2017, Dr Neelapu disclosed that he has received research funding and served as a consultant for Kite Pharma, the developer of axi-cel. Kite Pharma and the Leukemia & Lymphoma Society Therapy Acceleration Program supported ZUMA-1.
Study schema and patient characteristics
Phase 1 of ZUMA-1 enrolled 7 patients with diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), or transformed follicular lymphoma (TFL).
In phase 2, 101 patients were grouped into 2 cohorts—77 with refractory DLBCL and 24 with refractory PMBCL/TFL.
A total of 108 patients were treated in phases 1 and 2 and were included in the long-term pooled analysis.
Patients received a conditioning regimen of cyclophosphamide and fludarabine and, 2 days later, a fixed dose of axi-cel at 2 x 106 CAR T cells/kg.
“Importantly, the product could be manufactured for 99% of enrolled patients,” Dr Neelapu said. “Moreover, 91% of the enrolled patients were dosed with axi-cel, and there were no patients lost to follow-up.”
Patients in the pooled analysis were a median age of 58 (range, 23–76), and 27 (25%) were 65 or older.
Seventy-three patients (68%) were male, 62 (57%) had an ECOG status of 1, 90 (83%) had stage III or IV disease, and 48 (44%) had an IPI score of 3 to 4.
Seventy-six patients (70%) had received 3 or more prior therapies.
Eighty patients (74%) were refractory to their second or later line of therapy, and 70 (65%) had progressive disease as their best response to their last prior therapy. Twenty-five patients (23%) had relapsed after autologous stem cell transplant.
Response
The data cutoff for the long-term analysis was August 11, 2017.
In addition to the ongoing responses mentioned above, the best objective response was 82% in both the phase 2 primary analysis and the long-term analysis for phases 1 and 2.
CR as the best objective response increased from 54% in the primary analysis to 58% at the longer follow-up.
“We did observe deepening of the responses over time,” Dr Neelapu said. “At the time of the first tumor assessment, 60 patients had either partial remission or stable disease. But 23 of those 60 eventually achieved a complete remission up to 15 months post-infusion without any additional therapy.”
The median time to conversion from partial response to CR was 64 days (range, 49–242).
“The durability of these responses was observed consistently across key covariates,” Dr Neelapu added, “including the refractory subgroups, the disease stage groups, IPI risk groups. The CD19 status at baseline did not matter, nor did the cell of origin, or the CD4/CD8 ratio of the product.”
Furthermore, the investigators observed no differences in patients who received tocilizumab or corticosteroids.
The median duration of response for all patients was 11.1 months. For those who achieved CR, the median duration of response has not yet been reached.
Three of the 7 patients (43%) in the phase 1 part of the trial had an ongoing CR at 24 months.
At the median follow-up of 15.4 months, 42% of patients were progression-free, and 56% were alive.
The median overall survival has not been reached. Investigators estimated the 18-month overall survival to be 52%.
Safety
Adverse events (AEs) of grade 3 or higher occurred in 97% of patients, and serious AEs of grade 3 or higher occurred in 46% of patients in the updated analysis.
No new axi-cel-related AEs of cytokine release syndrome, neurologic events, or grade 5 AEs have arisen since the primary analysis.
There were four grade 5 events, 2 of which were related to axi-cel.
“All these four grade 5 events were previously reported—three in the phase 2 and one in the phase 1 trial,” Dr Neelapu said.
Most patients experienced hypogammaglobulinemia and B-cell aplasia. Eight percent of patients had IVIG support during the study.
Infections, such as pneumonia, influenza, and viral infection, were the most common new-onset treatment-emergent serious AEs occurring after 6 months in 10 patients. All were manageable and resolved prior to the data cut-off.
Persistence and resistance
“We observed long-term persistence of the CAR T cells,” Dr Neelapu said.
CAR T cells persisted in 71% of patients still responding at 1 year. And durable responses were observed in patients with and without detectable CAR T cells.
A central review committee analyzed biopsies of 21 evaluable patients at progression to try to determine the mechanism of resistance.
Fourteen of 21 (67%) biopsies were CD19-positive. Of these, 9 were PD-L1-positive, 4 were PD-L1-negative, and 1 was not evaluable.
Seven patients (33%) were CD19-negative compared to baseline. Of these, 4 were PD-L1-positive, 2 were PD-L1-negative, and 1 was not evaluable.
“This PD-L1 expression was observed in both CD19-positive relapses and CD19-negative relapses,” Dr Neelapu emphasized.
Of the 21 patients, 62% were PD-L1-positive.
Investigators hypothesize that 2 potential mechanisms could contribute to relapse: loss of CD19 and expression of PD-L1.
Axi-cel (Yescarta™) was approved by the US Food and Drug Administration in October for the treatment of adults with relapsed or refractory large B-cell lymphoma. ![]()
Research explains why cisplatin causes hearing loss
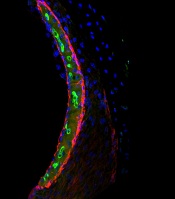
Researchers have gained new insight into hearing loss caused by cisplatin.
By measuring and mapping cisplatin retention in mouse and human inner ear tissues, the researchers found that cisplatin builds up in the inner ear and can remain there for years.
The team also found that a region in the inner ear called the stria vascularis could be targeted to prevent hearing loss resulting from cisplatin.
Lisa L. Cunningham, PhD, of the National Institute on Deafness and other Communications Disorders (NIDCD) in Bethesda, Maryland, and her colleagues reported these findings in Nature Communications.
The researchers noted that cisplatin can cause permanent hearing loss in 40% to 80% of treated patients. The team’s new findings help explain why.
The researchers found that, in most areas of the body, cisplatin is eliminated within days or weeks of treatment, but, in the inner ear, the drug remains much longer.
The team developed a mouse model that represents cisplatin-induced hearing loss seen in human patients.
By looking at inner ear tissue of mice after the first, second, and third cisplatin treatment, the researchers saw that cisplatin remained in the mouse inner ear much longer than in most other body tissues, and the drug builds up with each successive treatment.
The team also studied inner ear tissue donated by deceased adults who had been treated with cisplatin and found the drug is retained in the inner ear months or years after treatment.
When the researchers examined inner ear tissue from a child, they found cisplatin buildup that was even higher than that seen in adults.
Taken together, these results suggest the inner ear readily takes up cisplatin but has limited ability to remove the drug.
In mice and human tissues, the researchers saw the highest buildup of cisplatin in a part of the inner ear called the stria vascularis, which helps maintain the positive electrical charge in inner ear fluid that certain cells need to detect sound.
The team found the accumulation of cisplatin in the stria vascularis contributed to cisplatin-related hearing loss.
“Our findings suggest that if we can prevent cisplatin from entering the stria vascularis in the inner ear during treatment, we may be able to protect cancer patients from developing cisplatin-induced hearing loss,” Dr Cunningham said. ![]()
Researchers have gained new insight into hearing loss caused by cisplatin.
By measuring and mapping cisplatin retention in mouse and human inner ear tissues, the researchers found that cisplatin builds up in the inner ear and can remain there for years.
The team also found that a region in the inner ear called the stria vascularis could be targeted to prevent hearing loss resulting from cisplatin.
Lisa L. Cunningham, PhD, of the National Institute on Deafness and other Communications Disorders (NIDCD) in Bethesda, Maryland, and her colleagues reported these findings in Nature Communications.
The researchers noted that cisplatin can cause permanent hearing loss in 40% to 80% of treated patients. The team’s new findings help explain why.
The researchers found that, in most areas of the body, cisplatin is eliminated within days or weeks of treatment, but, in the inner ear, the drug remains much longer.
The team developed a mouse model that represents cisplatin-induced hearing loss seen in human patients.
By looking at inner ear tissue of mice after the first, second, and third cisplatin treatment, the researchers saw that cisplatin remained in the mouse inner ear much longer than in most other body tissues, and the drug builds up with each successive treatment.
The team also studied inner ear tissue donated by deceased adults who had been treated with cisplatin and found the drug is retained in the inner ear months or years after treatment.
When the researchers examined inner ear tissue from a child, they found cisplatin buildup that was even higher than that seen in adults.
Taken together, these results suggest the inner ear readily takes up cisplatin but has limited ability to remove the drug.
In mice and human tissues, the researchers saw the highest buildup of cisplatin in a part of the inner ear called the stria vascularis, which helps maintain the positive electrical charge in inner ear fluid that certain cells need to detect sound.
The team found the accumulation of cisplatin in the stria vascularis contributed to cisplatin-related hearing loss.
“Our findings suggest that if we can prevent cisplatin from entering the stria vascularis in the inner ear during treatment, we may be able to protect cancer patients from developing cisplatin-induced hearing loss,” Dr Cunningham said. ![]()
Researchers have gained new insight into hearing loss caused by cisplatin.
By measuring and mapping cisplatin retention in mouse and human inner ear tissues, the researchers found that cisplatin builds up in the inner ear and can remain there for years.
The team also found that a region in the inner ear called the stria vascularis could be targeted to prevent hearing loss resulting from cisplatin.
Lisa L. Cunningham, PhD, of the National Institute on Deafness and other Communications Disorders (NIDCD) in Bethesda, Maryland, and her colleagues reported these findings in Nature Communications.
The researchers noted that cisplatin can cause permanent hearing loss in 40% to 80% of treated patients. The team’s new findings help explain why.
The researchers found that, in most areas of the body, cisplatin is eliminated within days or weeks of treatment, but, in the inner ear, the drug remains much longer.
The team developed a mouse model that represents cisplatin-induced hearing loss seen in human patients.
By looking at inner ear tissue of mice after the first, second, and third cisplatin treatment, the researchers saw that cisplatin remained in the mouse inner ear much longer than in most other body tissues, and the drug builds up with each successive treatment.
The team also studied inner ear tissue donated by deceased adults who had been treated with cisplatin and found the drug is retained in the inner ear months or years after treatment.
When the researchers examined inner ear tissue from a child, they found cisplatin buildup that was even higher than that seen in adults.
Taken together, these results suggest the inner ear readily takes up cisplatin but has limited ability to remove the drug.
In mice and human tissues, the researchers saw the highest buildup of cisplatin in a part of the inner ear called the stria vascularis, which helps maintain the positive electrical charge in inner ear fluid that certain cells need to detect sound.
The team found the accumulation of cisplatin in the stria vascularis contributed to cisplatin-related hearing loss.
“Our findings suggest that if we can prevent cisplatin from entering the stria vascularis in the inner ear during treatment, we may be able to protect cancer patients from developing cisplatin-induced hearing loss,” Dr Cunningham said. ![]()
Drug receives fast track, orphan designations for PTCL
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available. ![]()
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available. ![]()
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available. ![]()
*Data in the abstract differ from the presentation.
Chemo-free combo should be option for rel/ref CLL, doc says
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
ATLANTA—The combination of venetoclax and rituximab (VR) should be a standard treatment option for adults with relapsed/refractory chronic lymphocytic leukemia (CLL), according to a speaker at the 2017 ASH Annual Meeting.
Data from the phase 3 MURANO study showed that patients with relapsed/refractory CLL who received VR had significantly longer progression-free survival (PFS) than those who received bendamustine and rituximab (BR).
In addition, “secondary endpoints were consistently in favor of venetoclax-rituximab,” said study investigator John F. Seymour, MBBS, PhD, of Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
Adverse events (AEs) were largely consistent with the known safety profiles of the drugs studied, but tumor lysis syndrome (TLS) was infrequent and occurred at a similar frequency in both treatment arms.
“Thus, overall, I believe venetoclax and rituximab should be considered as a suitable standard therapeutic option in patients with relapsed/refractory CLL,” Dr Seymour said.
It is important to note, however, that patients in the VR arm of this study could receive venetoclax for up to 2 years, whereas patients in the BR arm received study treatment for a maximum of six 28-day cycles.
Dr Seymour presented results from MURANO as a late-breaking abstract at ASH (LBA-2). The study was sponsored by Hoffman-La Roche and AbbVie.
MURANO enrolled 389 CLL patients who had received 1 to 3 prior therapies. Patients were randomized to receive VR (n=194) or BR (n=195). Baseline characteristics were similar between the treatment arms.
In both arms, patients received a single monthly dose of rituximab for 6 cycles. The first dose was 375 mg/m2, and all subsequent doses were 500 mg/m2.
In the VR arm, patients received a 4-week or 5-week dose ramp-up of venetoclax from 20 mg to 400 mg daily. This was intended to mitigate the risk of TLS, which has been observed in previous studies of venetoclax.
Patients in the VR arm continued with daily venetoclax at 400 mg for a maximum of 2 years or until disease progression or cessation due to toxicity. They started receiving rituximab after the ramp-up period (at week 6).
In the BR arm, patients received bendamustine at 70 mg/m2 on days 1 and 2 of each 28-day cycle for 6 cycles. Patients could proceed to subsequent therapy if they progressed.
The median follow-up was 23.8 months (range, 0-37.4 months).
Twenty-five percent of patients in the VR arm and 17% in the BR arm discontinued treatment ahead of schedule. Reasons for discontinuation (in the VR and BR arms, respectively) were disease progression (5% and 3%), AEs (12% and 6%), death (1% and 2%), and “other” (6% and 7%).
Survival
The study’s primary endpoint was investigator-assessed PFS. PFS according to an independent review committee (IRC) was a secondary endpoint.
According to investigators, the median PFS was not reached in the VR arm and was 17.0 months in the BR arm (hazard ratio [HR]=0.17, P<0.0001). According to the IRC, the median PFS was not reached in the VR arm and was 18.1 months in the BR arm (HR=0.17, P<0.0001).
According to investigators, the estimated PFS at 24 months was 84.9% in the VR arm and 36.3% in the BR arm. According to the IRC, the 24-month PFS was 82.8% and 37.4%, respectively.
The benefit with VR was consistent across subgroups. Patients had a PFS benefit regardless of their number of prior therapies, deletion 17p status, TP53 mutational status, baseline IGHV mutational status, and whether they had relapsed or refractory disease.
Dr Seymour acknowledged that the differences in treatment duration between the BR and VR arms may have affected the interpretation of these results.
“[T]he treatment duration differed, although, of course, the capacity to deliver more than 6 cycles of bendamustine-rituximab would have been problematic,” he said. “There is some data that antibody treatment may prolong progression-free survival. However, when this study was designed, in 2013, that data was certainly not available. And I believe, currently, maintenance antibody is not an accepted standard of treatment.”
The median overall survival (OS) was not reached in either treatment arm. The 1-year OS rate was 95.9% in the VR arm and 91.1% in the BR arm. The 2-year OS rate was 91.9% and 86.6%, respectively (HR=0.48, P=0.0186).
“[W]ith median follow-up of just on 2 years, there is already a clinically meaningful difference [in OS between the treatment arms],” Dr Seymour said.
“This is not attributable to any difference in availability of novel therapies. Of the 54 patients who received subsequent therapy after progression on the bendamustine-rituximab arm, 40 of those received novel targeted agents.”
Response and MRD
According to investigators, the overall response rate was 93.3% (181/194) in the VR arm and 67.7% (312/195) in the BR arm (P<0.0001). According to the IRC, the overall response rate was 92.3% (179/194) and 72.3% (141/195), respectively (P<0.0001).
According to investigators, the rate of complete response (CR) or CR with incomplete marrow recovery (CRi) was 26.8% (n=52) in the VR arm and 8.2% (n=16) in the BR arm. According to the IRC, the CR/CRi rate was 8.2% (n=16) and 3.6% (n=7), respectively.
Dr Seymour acknowledged the differences in CR/CRi between investigator and IRC assessments. He said 28 of the 42 discrepancies in the VR arm “were attributable to residual CT scan nodal abnormalities in the 16- to 30-mm size.” However, he also noted that 88% of these patients were negative for minimal residual disease (MRD) in the peripheral blood at that time point.
MRD was assessed every 3 months. Patients were counted as MRD-positive if they were positive by either allele-specific oligonucleotide polymerase chain reaction or multicolor flow cytometry. Patients were also counted as MRD-positive if there was a failure to collect a sample.
The proportion of patients who were MRD-negative in the VR and BR arms, respectively, was:
- 45% and 6% at 4 months
- 62% and 13% at 9 months
- 60% and 10% at 12 months
- 57% and 9% at 15 months
- 60% and 5% at 18 months.
Dr Seymour pointed out that 65 patients in the VR arm surpassed the maximum treatment duration for venetoclax (2 years) and therefore stopped receiving the drug, but only 12 of these patients have follow-up beyond 3 months.
“So information about the durability of response after cessation remains immature at the moment,” he said.
Safety
All patients in the VR arm and 98% in the BR arm had at least 1 AE. The rate of serious AEs was 46% and 43%, respectively. The rate of grade 3/4 AEs was 82% and 70%, respectively.
Grade 3/4 AEs with at least a 2% difference in incidence between the treatment arms (in the VR and BR arms, respectively) were neutropenia (58% and 39%), anemia (11% and 14%), thrombocytopenia (6% and 10%), febrile neutropenia (4% and 10%), pneumonia (5% and 8%), infusion-related reactions (2% and 5%), TLS (3% and 1%), hypotension (0% and 3%), hyperglycemia (2% and 0%), and hypogammaglobulinemia (2% and 0%).
The rate of grade 5 AEs was 5% in the VR arm and 6% in the BR arm.
Grade 5 AEs in the VR arm were pneumonia (n=3), sepsis (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1).
Grade 5 AEs in the BR arm included sepsis (n=2), lung cancer (n=2), Listeria sepsis (n=1), Scedosporium infection (n=1), lymphoma (n=1), hemorrhagic stroke (n=1), pulmonary embolism (n=1), acute myeloid leukemia (n=1), and sudden death (n=1). ![]()
Risk stratification may be possible with JCAR017
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017. ![]()
*Data in the presentation differ from the abstract.
ATLANTA—Data suggest a therapeutic window may exist for chimeric antigen receptor (CAR) T-cell expansion with JCAR017, according to a preliminary model.
In a core set of 67 patients with diffuse large B-cell lymphoma (DLBCL) who had received JCAR017 in the TRANSCEND NHL 001 trial, investigators observed that baseline high tumor burden and inflammatory biomarkers were associated with high CAR T-cell expansion and increased rates of cytokine release syndrome (CRS) and neurotoxicity.
If the model holds up, researchers say they could potentially identify patients at risk for low or high T-cell expansion levels and develop a strategy to enhance or limit the expansion.
TRANSCEND NHL 001 (NCT02631044) is a multicenter, phase 1 trial in relapsed or refractory non-Hodgkin lymphoma evaluating 2 dose levels of JCAR017, also known as lisocabtagene maraleucel, or liso-cel for short.
Liso-cel is a CD19-directed 4-1BB CAR T cell administered at precise doses of CD4+ and CD8+ CAR T cells. It had previously demonstrated high complete remission (CR) rates and low incidences of CRS and neurotoxicity.
Tanya Saddiqi, MD, of City of Hope National Medical Center in Duarte, California, presented data from the dose-finding and expansion cohorts at the 2017 ASH Annual Meeting (abstract 193*).
Study design
Patients with DLBCL after 2 lines of prior therapy or mantle cell lymphoma after 1 prior line of therapy were eligible to enroll in TRANSCEND NHL 001.
Patients with de novo DLBCL, those who transformed from follicular lymphoma, or those with high-grade B-cell lymphoma made up the pivotal or core population. All DLBCL patients enrolled on the trial comprised the full population.
Patients were screened, enrolled, and underwent apheresis. Bridging therapy was permitted while their CAR T cells were being manufactured.
Patients then had a PET scan and lab tests prior to lymphodepletion.
“This is the time point of our interest,” Dr Saddiqi said, “to see if there are any patient characteristics or biomarkers that we can identify . . . that could help us figure out which patients are at higher risk of toxicity, potentially.”
Lymphodepletion consisted of fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2 for 3 days).
Patients received the JCAR017 infusion, and, at specific time points thereafter, cytokine, pharmacokinetic (PK), and clinical lab evaluations were conducted. PK evaluation and scans were performed every 3 months for the first year after JCAR017 infusion, and safety and viral vector follow-up for 15 years.
Dose levels were 5 x 107 cells as a single or double dose (DL1S) and 1 x 108 cells as a single dose (DL2S). Dose level 2 was chosen for further study, and double dosing was discontinued.
“Double dosing was actually not pursued further,” Dr Saddiqi explained, “because it did not seem to add any benefit over single dosing.”
At the time of the presentation, 91 total patients were treated, 67 of whom were the core population.
Results
Dr Saddiqi reported that patients treated with JCAR017 achieved a relatively high best overall response rate (ORR) and high durable CR rates.
“And this seems to be especially true for the core set of patients and particularly for patients at dose level 2,” she added.
At all dose levels, the core patients had a best ORR of 84% (41/49) and a CR rate of 61% (30/49).
At follow-up of 3 months or longer, the core group had an ORR of 65% (26/40) for all dose levels, 52% (11/21) for dose level 1, and 80% (12/15) for dose level 2.
The 3-month CR rate was 53% (21/40) for all dose levels in the core group, 33% (7/21) in dose level 1, and 73% (11/15) in dose level 2.
Dr Saddiqi noted that CRS and neurotoxicity did not differ by dose level or schedule, and there were no grade 5 events of CRS or neurotoxicity.
“Among the core group, dose level change did not add to their toxicity,” she said. “And so the question is: Is it patient factors, is it tumor factors? What is it that is actually causing the toxicities in these patients?”
Dr Saddiqi focused the presentation on patient factors.
Patient factors
The data showed that tumor burden and lactose dehydrogenase (LDH) levels were higher in patients with CRS and neurotoxicity.
Univariate analysis revealed that CRS and neurotoxicity were associated with a shorter time since diagnosis.
However, prior number of therapies, patient weight, and disease stage were not associated with CRS or neurotoxicity.
Investigators were able to identify preliminary risk boundaries. Core patients with high LDH levels (≥ 500 U/L) and sum of the products of diameters (SPD) ≥ 50 cm2 at baseline had an 8-fold increase in risk of CRS and neurotoxicity.
“Inversely, if these patients did not meet the cutoff for LDH or SPD,” Dr Saddiqi pointed out, “if they were lower than that, they have significantly lower CRS and neurotoxicity events.”
Investigators also observed that baseline markers of inflammation and inflammatory cytokines trended higher in patients with CRS and neurotoxicity. For CRS, this includes ferritin, C-reactive protein (CRP), IL-10, IL-15, IL-16, TNFα, and MIP-1β. For neurotoxicity, this includes ferritin, CRP, d-Dimer, IL-6, IL-15, TNFα, and MIP-1α.
The team also observed that tumor burden, baseline markers of inflammation, and inflammatory cytokines trended lower in core patients with durable responses.
“Interestingly, it’s inversely true that patients who did have these higher levels [of inflammation markers], and higher tumor burden, and higher LDH, actually were the ones that were either showing no response at 3 months or had lost their response by the 3-month assessment point,” Dr Saddiqi explained.
And in patients with higher baseline tumor burden and inflammatory cytokine levels, JCAR017 T-cell expansion trended higher.
“Some were deemed to be super expanders because their CAR T-cell levels were very high in their blood,” she added.
The investigators created a preliminary logistic model based on the data that suggests a therapeutic window might be able to limit toxicity and optimize efficacy.
The model indicates that patients with higher tumor burden, higher LDH, and higher inflammatory state at baseline seem to be the ones who are having more CRS and more neurotoxicity after CAR T-cell infusion.
“They are expanding their cells much more, yet their responses at 3 months seem to be affected adversely by this entire situation,” Dr Saddiqi said.
"One explanation, potentially, could be that these CAR T cells are seeing a lot of antigen when they go into the body. They have the perfect cytokine milieu to grow, expand, and go crazy in the body, if you will, and very quickly peter out as well because there’s T-cell exhaustion that happens rather rapidly and clinical responses are then then lost.”
The investigators believe that if they can identify those patients ahead of time who may be at risk of too high expansion or too low expansion of their CAR T cells, they may be able to find strategies to push expansion into the “sweet spot of CAR T-cell expansion and ultimately get the holy grail of having durable responses for all with minimal toxicity,” Dr Saddiqi concluded.
TRANSCEND NHL 001 is sponsored by Juno Therapeutics, Inc. Dr Saddiqi has served on a steering committee for JCAR017.
*Data in the presentation differ from the abstract.
Pembrolizumab sBLA receives priority review
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths.
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths.
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths.
*Data in the abstract differ from the presentation.
Technique may be effective for diagnosing NHL
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.”
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.”
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.”
Combo prolongs survival in lymphoma models
Combination treatment with 2 monoclonal antibodies (mAbs) has demonstrated preclinical efficacy against B-cell lymphomas, according to researchers.
The investigators tested different combinations of mAbs to see how they interact with each other and what effect this has on how the immune system fights cancer.
One combination—an anti-CD27 mAb and anti-CD20 mAb—greatly increased survival in mouse models of B-cell lymphoma.
The researchers reported these results in Cancer Cell.
“By combining 2 specific antibodies—anti-CD27 and anti-CD20—we’ve increased the ability of the immune system to destroy cancer cells,” said study author Sean Lim, MBChB, PhD, of the University of Southampton in the UK.
“It’s very exciting to see that this drug combination has an impact on survival of mice with lymphoma, as improvements in treatment are urgently needed. The next stage will be to see if what we’ve discovered can be replicated in patients.”
For this study, Dr Lim and her colleagues tested combinations of tumor-targeting mAbs and immunomodulatory mAbs. The group found that an anti-CD27 mAb enhanced anti-CD20 therapy in various preclinical models.
The investigators first tested anti-CD20 and anti-CD27 (both alone and in combination) in the murine B-cell lymphoma model BCL1.
All control BCL1 mice had died by 30 days from baseline, all mice that received anti-CD20 alone died by day 40, and 30% of mice that received anti-CD27 alone were still alive past 100 days.
In contrast, 100% of mice that received anti-CD20 and anti-CD27 in combination were still alive and lymphoma-free past the 100-day mark.
The researchers also tested the mAbs in the A31 B-cell lymphoma model and the Eµ-TCL1 B-chronic lymphocytic leukemia model.
Results were similar to those observed with the BCL1 model. The combination of anti-CD20 and anti-CD27 significantly improved survival in A31 and Eµ-TCL1 mice, with all mice that received this combination surviving past 100 days.
As far as mechanisms of action, the investigators noted that anti-CD20 binds to B cells and mediates antibody-dependent cellular phagocytosis of the mAb-opsonized cells.
The researchers said the addition of anti-CD27 stimulates CD8+ T cells and natural killer cells, which induces the release of CCL3, CCL4, and CCL5, and this potentially attracts myeloid cells.
In addition, anti-CD27 (via the stimulation of CD8+ T and natural killer cells) induces the release of interferon gamma, which activates macrophages to express more Fc gamma receptor IV and promotes their inflammatory capacity. This increases the number of macrophages available for antibody-dependent cellular phagocytosis as well as the cells’ phagocytic ability.
Based on these findings, researchers are now conducting a phase 2 trial to test the anti-CD20 mAb rituximab and the anti-CD27 mAb varililumab in patients with relapsed and/or refractory B-cell non-Hodgkin lymphoma.
Combination treatment with 2 monoclonal antibodies (mAbs) has demonstrated preclinical efficacy against B-cell lymphomas, according to researchers.
The investigators tested different combinations of mAbs to see how they interact with each other and what effect this has on how the immune system fights cancer.
One combination—an anti-CD27 mAb and anti-CD20 mAb—greatly increased survival in mouse models of B-cell lymphoma.
The researchers reported these results in Cancer Cell.
“By combining 2 specific antibodies—anti-CD27 and anti-CD20—we’ve increased the ability of the immune system to destroy cancer cells,” said study author Sean Lim, MBChB, PhD, of the University of Southampton in the UK.
“It’s very exciting to see that this drug combination has an impact on survival of mice with lymphoma, as improvements in treatment are urgently needed. The next stage will be to see if what we’ve discovered can be replicated in patients.”
For this study, Dr Lim and her colleagues tested combinations of tumor-targeting mAbs and immunomodulatory mAbs. The group found that an anti-CD27 mAb enhanced anti-CD20 therapy in various preclinical models.
The investigators first tested anti-CD20 and anti-CD27 (both alone and in combination) in the murine B-cell lymphoma model BCL1.
All control BCL1 mice had died by 30 days from baseline, all mice that received anti-CD20 alone died by day 40, and 30% of mice that received anti-CD27 alone were still alive past 100 days.
In contrast, 100% of mice that received anti-CD20 and anti-CD27 in combination were still alive and lymphoma-free past the 100-day mark.
The researchers also tested the mAbs in the A31 B-cell lymphoma model and the Eµ-TCL1 B-chronic lymphocytic leukemia model.
Results were similar to those observed with the BCL1 model. The combination of anti-CD20 and anti-CD27 significantly improved survival in A31 and Eµ-TCL1 mice, with all mice that received this combination surviving past 100 days.
As far as mechanisms of action, the investigators noted that anti-CD20 binds to B cells and mediates antibody-dependent cellular phagocytosis of the mAb-opsonized cells.
The researchers said the addition of anti-CD27 stimulates CD8+ T cells and natural killer cells, which induces the release of CCL3, CCL4, and CCL5, and this potentially attracts myeloid cells.
In addition, anti-CD27 (via the stimulation of CD8+ T and natural killer cells) induces the release of interferon gamma, which activates macrophages to express more Fc gamma receptor IV and promotes their inflammatory capacity. This increases the number of macrophages available for antibody-dependent cellular phagocytosis as well as the cells’ phagocytic ability.
Based on these findings, researchers are now conducting a phase 2 trial to test the anti-CD20 mAb rituximab and the anti-CD27 mAb varililumab in patients with relapsed and/or refractory B-cell non-Hodgkin lymphoma.
Combination treatment with 2 monoclonal antibodies (mAbs) has demonstrated preclinical efficacy against B-cell lymphomas, according to researchers.
The investigators tested different combinations of mAbs to see how they interact with each other and what effect this has on how the immune system fights cancer.
One combination—an anti-CD27 mAb and anti-CD20 mAb—greatly increased survival in mouse models of B-cell lymphoma.
The researchers reported these results in Cancer Cell.
“By combining 2 specific antibodies—anti-CD27 and anti-CD20—we’ve increased the ability of the immune system to destroy cancer cells,” said study author Sean Lim, MBChB, PhD, of the University of Southampton in the UK.
“It’s very exciting to see that this drug combination has an impact on survival of mice with lymphoma, as improvements in treatment are urgently needed. The next stage will be to see if what we’ve discovered can be replicated in patients.”
For this study, Dr Lim and her colleagues tested combinations of tumor-targeting mAbs and immunomodulatory mAbs. The group found that an anti-CD27 mAb enhanced anti-CD20 therapy in various preclinical models.
The investigators first tested anti-CD20 and anti-CD27 (both alone and in combination) in the murine B-cell lymphoma model BCL1.
All control BCL1 mice had died by 30 days from baseline, all mice that received anti-CD20 alone died by day 40, and 30% of mice that received anti-CD27 alone were still alive past 100 days.
In contrast, 100% of mice that received anti-CD20 and anti-CD27 in combination were still alive and lymphoma-free past the 100-day mark.
The researchers also tested the mAbs in the A31 B-cell lymphoma model and the Eµ-TCL1 B-chronic lymphocytic leukemia model.
Results were similar to those observed with the BCL1 model. The combination of anti-CD20 and anti-CD27 significantly improved survival in A31 and Eµ-TCL1 mice, with all mice that received this combination surviving past 100 days.
As far as mechanisms of action, the investigators noted that anti-CD20 binds to B cells and mediates antibody-dependent cellular phagocytosis of the mAb-opsonized cells.
The researchers said the addition of anti-CD27 stimulates CD8+ T cells and natural killer cells, which induces the release of CCL3, CCL4, and CCL5, and this potentially attracts myeloid cells.
In addition, anti-CD27 (via the stimulation of CD8+ T and natural killer cells) induces the release of interferon gamma, which activates macrophages to express more Fc gamma receptor IV and promotes their inflammatory capacity. This increases the number of macrophages available for antibody-dependent cellular phagocytosis as well as the cells’ phagocytic ability.
Based on these findings, researchers are now conducting a phase 2 trial to test the anti-CD20 mAb rituximab and the anti-CD27 mAb varililumab in patients with relapsed and/or refractory B-cell non-Hodgkin lymphoma.