User login
Triplet disappoints in follicular lymphoma trial

Photo courtesy of ASH
ORLANDO, FL—A 3-drug regimen is likely not worth pursuing as a first-line treatment option for follicular lymphoma (FL), according to a presentation at the 2015 ASH Annual Meeting.
In a phase 1 study, combination ibrutinib, rituximab, and lenalidomide did not provide any response benefit over that previously observed with rituximab and lenalidomide.
But the triplet increased toxicity—particularly the incidence of rash—and necessitated dose modifications.
Chaitra S. Ujjani, MD, of Georgetown University Hospital in Washington, DC, presented these results at the meeting as abstract 471.*
“The combination of rituximab and lenalidomide has demonstrated remarkable activity in follicular lymphoma,” Dr Ujjani began.
She noted that, in the CALGB 50401 trial of relapsed FL (Leonard et al. JCO 2015), the combination elicited an overall response rate (ORR) of 76% and a complete response (CR) rate of 39%, and the 2-year time to progression was 52%.
In the CALGB 50803 trial of previously untreated FL (Martin et al. ASCO 2014, 8521), the regimen produced an ORR of 96%, a CR rate of 71%, and a 2-year progression-free survival (PFS) of 89%. In another trial of previously untreated FL (Fowler et al. Lanc Onc 2014), the ORR was 90%, the CR rate was 80%, and the 3-year PFS was 79%.
Ibrutinib has also demonstrated activity in FL, Dr Ujjani pointed out. In a phase 1 study of relapsed FL (Fowler et al. ASH 2012), the drug produced an ORR of 55%, 3 of 11 patients achieved a CR, and the median PFS was 13.4 months.
In a phase 2 study of ibrutinib in relapsed FL (Bartlett et al. ASH 2014, 800), the ORR was 30%, 1 of 40 patients achieved a CR, and the median PFS was 9.9 months.
With this in mind, Dr Ujjani and her colleagues conducted the A051103 trial to determine the activity and tolerability of rituximab, lenalidomide, and ibrutinib in previously untreated patients with FL.
Study design
The study enrolled patients with grade 1-3a FL; stage III, IV, or bulky stage II disease; an ECOG performance status less than 2; and adequate organ function.
They received 4 doses of rituximab at 375 mg/m2 on days 1, 8, 15, and 22 of cycle 1 (28 days). They received 4 additional doses (375 mg/m2) on day 1 of cycles 4, 6, 8, and 10.
The patients received lenalidomide according to their assigned dosing cohort on days 1 to 21 for 18 cycles. They received daily ibrutinib according to their assigned dosing cohort until progression or unacceptable toxicity.
The study had a 3+3 dose-escalation design. Dose level (DL) 0 was lenalidomide at 15 mg and ibrutinib at 420 mg, DL1 was lenalidomide at 15 mg and ibrutinib at 560 mg, and DL2 was lenalidomide at 20 mg and ibrutinib at 560 mg.
Patients also received allopurinol at 300 mg daily for tumor lysis prophylaxis and aspirin as thromboprophylaxis while on lenalidomide.
The researchers assessed dose-limiting toxicities (DLTs) weekly during cycle 1. Given the known incidence of rash with lenalidomide, grade 3 rash that resolved to less than grade 2 within 10 days was not included as a DLT.
Once the maximum-tolerated dose was determined, there was a 10-patient expansion cohort.
Patients and treatment
Twenty-two patients were enrolled between June 2013 and May 2015. Their median age was 53.5 years (range, 36-81), and 68% were male.
Seventy-three percent of patients had grade 1/2 disease, and 77% had stage IV disease. By FLIPI, 18% of patients were low-risk, 55% were intermediate-risk, and 27% were high-risk.
Three patients were treated at DL0, 3 at DL1, and 16 at DL2. There were no DLTs reported at any dose level.
However, 11 patients required dose reductions due to toxicity (7 due to rash), and 12 patients ultimately discontinued treatment.
Reasons for discontinuation included progression (n=2), new diagnosis of carcinoma requiring systemic therapy (n=2), patient decision (n=3), and adverse events (n=6), including grade 3 rash (n=2), grade 3 atrial flutter (n=1), grade 3 diarrhea (n=1), hypertension (n=1), and depression (n=1). (One patient discontinued due to rash and progression.)
Adverse events
Dr Ujjani said the hematologic toxicity profile was similar to that observed with rituximab and lenalidomide in the front-line setting. Grade 3/4 hematologic toxicities included neutropenia (18.2%), thrombocytopenia (4.5%), anemia (4.5%), and lymphopenia (4.5%).
The most common non-hematologic toxicities (occurring in more than 20% of patients) were rash, diarrhea, fatigue, infusion-related reactions, nausea, infection, and neoplasms. There were no grade 4 non-hematologic toxicities.
Compared to rituximab and lenalidomide, the triplet was associated with an increase in rash, diarrhea, arthralgia, and neoplasm. There were 2 cutaneous neoplasms and 3 carcinomas.
Rash
“While no protocol-defined DLTs were observed, the regimen was associated with clinically significant rash,” Dr Ujjani noted. “Rash may have been related to individual study drugs or drug-drug interactions.”
Rash occurred in 82% of patients overall, 100% of patients treated at DL0, 67% at DL1, and 81% at DL2. The incidence of grade 1/2 rash was 46% overall, 67% at DL0, 33% at DL1, and 44% at DL2. The incidence of grade 3 rash was 36% overall, 33% at DL0 and DL1, and 38% at DL2.
The incidence of rash was similar whether or not patients received allopurinol. Ten of 11 patients on allopurinol had a rash, and 8 of 11 patients not on allopurinol had a rash.
“The time of [rash] onset was typically during cycle 1 but was seen as late as cycle 5,” Dr Ujjani said. “Grade 1 and 2 rashes resolved spontaneously without dose modification. The incidence of these milder rashes were comparable to our prior reports of rituximab and lenalidomide.”
“Grade 3 rash, however, occurred in 36% of patients, which is significantly higher than [with] rituximab and lenalidomide, [which is] typically 7% to 8%, or single-agent ibrutinib, which is about 3% to 4%.”
Patients with grade 3 rash were managed with supportive care, including acetaminophen, diphenhydramine, and oral corticosteroids.
All but 1 patient (7/8) had dose delays and reductions due to rash. One patient withdrew from the study because of rash, and 1 patient withdrew because of disease progression that occurred during a dose delay for rash.
Response and survival
The ORR was 95% for the entire cohort, 100% at DL0 and DL1 and 94% at DL2. The CR/unconfirmed CR rate was 63% overall, 67% at DL0, 33% at DL1, and 69% at DL2.
The partial response rate was 32% overall, 33% at DL0, 67% at DL1, and 25% at DL2. Five percent of patients had stable disease, all at DL2 (6% of this group).
The median time to first response was 2.3 months (range, 1.9 to 11.1). And the median time to best response was 5.5 months (range, 1.9 to 20.2).
At a median follow-up of 12.3 months, all patients are still alive. The 12-month PFS is 84%.
“Preliminary response data were similar to the prior CALGB/Alliance study of rituximab and lenalidomide,” Dr Ujjani noted. “However, given the increased toxicity and required dose modifications, the additional benefit of a third agent is not apparent, and further investigation of the triplet in this setting seems unwarranted.” ![]()
*Data in the abstract differ from data presented at the meeting.

Photo courtesy of ASH
ORLANDO, FL—A 3-drug regimen is likely not worth pursuing as a first-line treatment option for follicular lymphoma (FL), according to a presentation at the 2015 ASH Annual Meeting.
In a phase 1 study, combination ibrutinib, rituximab, and lenalidomide did not provide any response benefit over that previously observed with rituximab and lenalidomide.
But the triplet increased toxicity—particularly the incidence of rash—and necessitated dose modifications.
Chaitra S. Ujjani, MD, of Georgetown University Hospital in Washington, DC, presented these results at the meeting as abstract 471.*
“The combination of rituximab and lenalidomide has demonstrated remarkable activity in follicular lymphoma,” Dr Ujjani began.
She noted that, in the CALGB 50401 trial of relapsed FL (Leonard et al. JCO 2015), the combination elicited an overall response rate (ORR) of 76% and a complete response (CR) rate of 39%, and the 2-year time to progression was 52%.
In the CALGB 50803 trial of previously untreated FL (Martin et al. ASCO 2014, 8521), the regimen produced an ORR of 96%, a CR rate of 71%, and a 2-year progression-free survival (PFS) of 89%. In another trial of previously untreated FL (Fowler et al. Lanc Onc 2014), the ORR was 90%, the CR rate was 80%, and the 3-year PFS was 79%.
Ibrutinib has also demonstrated activity in FL, Dr Ujjani pointed out. In a phase 1 study of relapsed FL (Fowler et al. ASH 2012), the drug produced an ORR of 55%, 3 of 11 patients achieved a CR, and the median PFS was 13.4 months.
In a phase 2 study of ibrutinib in relapsed FL (Bartlett et al. ASH 2014, 800), the ORR was 30%, 1 of 40 patients achieved a CR, and the median PFS was 9.9 months.
With this in mind, Dr Ujjani and her colleagues conducted the A051103 trial to determine the activity and tolerability of rituximab, lenalidomide, and ibrutinib in previously untreated patients with FL.
Study design
The study enrolled patients with grade 1-3a FL; stage III, IV, or bulky stage II disease; an ECOG performance status less than 2; and adequate organ function.
They received 4 doses of rituximab at 375 mg/m2 on days 1, 8, 15, and 22 of cycle 1 (28 days). They received 4 additional doses (375 mg/m2) on day 1 of cycles 4, 6, 8, and 10.
The patients received lenalidomide according to their assigned dosing cohort on days 1 to 21 for 18 cycles. They received daily ibrutinib according to their assigned dosing cohort until progression or unacceptable toxicity.
The study had a 3+3 dose-escalation design. Dose level (DL) 0 was lenalidomide at 15 mg and ibrutinib at 420 mg, DL1 was lenalidomide at 15 mg and ibrutinib at 560 mg, and DL2 was lenalidomide at 20 mg and ibrutinib at 560 mg.
Patients also received allopurinol at 300 mg daily for tumor lysis prophylaxis and aspirin as thromboprophylaxis while on lenalidomide.
The researchers assessed dose-limiting toxicities (DLTs) weekly during cycle 1. Given the known incidence of rash with lenalidomide, grade 3 rash that resolved to less than grade 2 within 10 days was not included as a DLT.
Once the maximum-tolerated dose was determined, there was a 10-patient expansion cohort.
Patients and treatment
Twenty-two patients were enrolled between June 2013 and May 2015. Their median age was 53.5 years (range, 36-81), and 68% were male.
Seventy-three percent of patients had grade 1/2 disease, and 77% had stage IV disease. By FLIPI, 18% of patients were low-risk, 55% were intermediate-risk, and 27% were high-risk.
Three patients were treated at DL0, 3 at DL1, and 16 at DL2. There were no DLTs reported at any dose level.
However, 11 patients required dose reductions due to toxicity (7 due to rash), and 12 patients ultimately discontinued treatment.
Reasons for discontinuation included progression (n=2), new diagnosis of carcinoma requiring systemic therapy (n=2), patient decision (n=3), and adverse events (n=6), including grade 3 rash (n=2), grade 3 atrial flutter (n=1), grade 3 diarrhea (n=1), hypertension (n=1), and depression (n=1). (One patient discontinued due to rash and progression.)
Adverse events
Dr Ujjani said the hematologic toxicity profile was similar to that observed with rituximab and lenalidomide in the front-line setting. Grade 3/4 hematologic toxicities included neutropenia (18.2%), thrombocytopenia (4.5%), anemia (4.5%), and lymphopenia (4.5%).
The most common non-hematologic toxicities (occurring in more than 20% of patients) were rash, diarrhea, fatigue, infusion-related reactions, nausea, infection, and neoplasms. There were no grade 4 non-hematologic toxicities.
Compared to rituximab and lenalidomide, the triplet was associated with an increase in rash, diarrhea, arthralgia, and neoplasm. There were 2 cutaneous neoplasms and 3 carcinomas.
Rash
“While no protocol-defined DLTs were observed, the regimen was associated with clinically significant rash,” Dr Ujjani noted. “Rash may have been related to individual study drugs or drug-drug interactions.”
Rash occurred in 82% of patients overall, 100% of patients treated at DL0, 67% at DL1, and 81% at DL2. The incidence of grade 1/2 rash was 46% overall, 67% at DL0, 33% at DL1, and 44% at DL2. The incidence of grade 3 rash was 36% overall, 33% at DL0 and DL1, and 38% at DL2.
The incidence of rash was similar whether or not patients received allopurinol. Ten of 11 patients on allopurinol had a rash, and 8 of 11 patients not on allopurinol had a rash.
“The time of [rash] onset was typically during cycle 1 but was seen as late as cycle 5,” Dr Ujjani said. “Grade 1 and 2 rashes resolved spontaneously without dose modification. The incidence of these milder rashes were comparable to our prior reports of rituximab and lenalidomide.”
“Grade 3 rash, however, occurred in 36% of patients, which is significantly higher than [with] rituximab and lenalidomide, [which is] typically 7% to 8%, or single-agent ibrutinib, which is about 3% to 4%.”
Patients with grade 3 rash were managed with supportive care, including acetaminophen, diphenhydramine, and oral corticosteroids.
All but 1 patient (7/8) had dose delays and reductions due to rash. One patient withdrew from the study because of rash, and 1 patient withdrew because of disease progression that occurred during a dose delay for rash.
Response and survival
The ORR was 95% for the entire cohort, 100% at DL0 and DL1 and 94% at DL2. The CR/unconfirmed CR rate was 63% overall, 67% at DL0, 33% at DL1, and 69% at DL2.
The partial response rate was 32% overall, 33% at DL0, 67% at DL1, and 25% at DL2. Five percent of patients had stable disease, all at DL2 (6% of this group).
The median time to first response was 2.3 months (range, 1.9 to 11.1). And the median time to best response was 5.5 months (range, 1.9 to 20.2).
At a median follow-up of 12.3 months, all patients are still alive. The 12-month PFS is 84%.
“Preliminary response data were similar to the prior CALGB/Alliance study of rituximab and lenalidomide,” Dr Ujjani noted. “However, given the increased toxicity and required dose modifications, the additional benefit of a third agent is not apparent, and further investigation of the triplet in this setting seems unwarranted.” ![]()
*Data in the abstract differ from data presented at the meeting.

Photo courtesy of ASH
ORLANDO, FL—A 3-drug regimen is likely not worth pursuing as a first-line treatment option for follicular lymphoma (FL), according to a presentation at the 2015 ASH Annual Meeting.
In a phase 1 study, combination ibrutinib, rituximab, and lenalidomide did not provide any response benefit over that previously observed with rituximab and lenalidomide.
But the triplet increased toxicity—particularly the incidence of rash—and necessitated dose modifications.
Chaitra S. Ujjani, MD, of Georgetown University Hospital in Washington, DC, presented these results at the meeting as abstract 471.*
“The combination of rituximab and lenalidomide has demonstrated remarkable activity in follicular lymphoma,” Dr Ujjani began.
She noted that, in the CALGB 50401 trial of relapsed FL (Leonard et al. JCO 2015), the combination elicited an overall response rate (ORR) of 76% and a complete response (CR) rate of 39%, and the 2-year time to progression was 52%.
In the CALGB 50803 trial of previously untreated FL (Martin et al. ASCO 2014, 8521), the regimen produced an ORR of 96%, a CR rate of 71%, and a 2-year progression-free survival (PFS) of 89%. In another trial of previously untreated FL (Fowler et al. Lanc Onc 2014), the ORR was 90%, the CR rate was 80%, and the 3-year PFS was 79%.
Ibrutinib has also demonstrated activity in FL, Dr Ujjani pointed out. In a phase 1 study of relapsed FL (Fowler et al. ASH 2012), the drug produced an ORR of 55%, 3 of 11 patients achieved a CR, and the median PFS was 13.4 months.
In a phase 2 study of ibrutinib in relapsed FL (Bartlett et al. ASH 2014, 800), the ORR was 30%, 1 of 40 patients achieved a CR, and the median PFS was 9.9 months.
With this in mind, Dr Ujjani and her colleagues conducted the A051103 trial to determine the activity and tolerability of rituximab, lenalidomide, and ibrutinib in previously untreated patients with FL.
Study design
The study enrolled patients with grade 1-3a FL; stage III, IV, or bulky stage II disease; an ECOG performance status less than 2; and adequate organ function.
They received 4 doses of rituximab at 375 mg/m2 on days 1, 8, 15, and 22 of cycle 1 (28 days). They received 4 additional doses (375 mg/m2) on day 1 of cycles 4, 6, 8, and 10.
The patients received lenalidomide according to their assigned dosing cohort on days 1 to 21 for 18 cycles. They received daily ibrutinib according to their assigned dosing cohort until progression or unacceptable toxicity.
The study had a 3+3 dose-escalation design. Dose level (DL) 0 was lenalidomide at 15 mg and ibrutinib at 420 mg, DL1 was lenalidomide at 15 mg and ibrutinib at 560 mg, and DL2 was lenalidomide at 20 mg and ibrutinib at 560 mg.
Patients also received allopurinol at 300 mg daily for tumor lysis prophylaxis and aspirin as thromboprophylaxis while on lenalidomide.
The researchers assessed dose-limiting toxicities (DLTs) weekly during cycle 1. Given the known incidence of rash with lenalidomide, grade 3 rash that resolved to less than grade 2 within 10 days was not included as a DLT.
Once the maximum-tolerated dose was determined, there was a 10-patient expansion cohort.
Patients and treatment
Twenty-two patients were enrolled between June 2013 and May 2015. Their median age was 53.5 years (range, 36-81), and 68% were male.
Seventy-three percent of patients had grade 1/2 disease, and 77% had stage IV disease. By FLIPI, 18% of patients were low-risk, 55% were intermediate-risk, and 27% were high-risk.
Three patients were treated at DL0, 3 at DL1, and 16 at DL2. There were no DLTs reported at any dose level.
However, 11 patients required dose reductions due to toxicity (7 due to rash), and 12 patients ultimately discontinued treatment.
Reasons for discontinuation included progression (n=2), new diagnosis of carcinoma requiring systemic therapy (n=2), patient decision (n=3), and adverse events (n=6), including grade 3 rash (n=2), grade 3 atrial flutter (n=1), grade 3 diarrhea (n=1), hypertension (n=1), and depression (n=1). (One patient discontinued due to rash and progression.)
Adverse events
Dr Ujjani said the hematologic toxicity profile was similar to that observed with rituximab and lenalidomide in the front-line setting. Grade 3/4 hematologic toxicities included neutropenia (18.2%), thrombocytopenia (4.5%), anemia (4.5%), and lymphopenia (4.5%).
The most common non-hematologic toxicities (occurring in more than 20% of patients) were rash, diarrhea, fatigue, infusion-related reactions, nausea, infection, and neoplasms. There were no grade 4 non-hematologic toxicities.
Compared to rituximab and lenalidomide, the triplet was associated with an increase in rash, diarrhea, arthralgia, and neoplasm. There were 2 cutaneous neoplasms and 3 carcinomas.
Rash
“While no protocol-defined DLTs were observed, the regimen was associated with clinically significant rash,” Dr Ujjani noted. “Rash may have been related to individual study drugs or drug-drug interactions.”
Rash occurred in 82% of patients overall, 100% of patients treated at DL0, 67% at DL1, and 81% at DL2. The incidence of grade 1/2 rash was 46% overall, 67% at DL0, 33% at DL1, and 44% at DL2. The incidence of grade 3 rash was 36% overall, 33% at DL0 and DL1, and 38% at DL2.
The incidence of rash was similar whether or not patients received allopurinol. Ten of 11 patients on allopurinol had a rash, and 8 of 11 patients not on allopurinol had a rash.
“The time of [rash] onset was typically during cycle 1 but was seen as late as cycle 5,” Dr Ujjani said. “Grade 1 and 2 rashes resolved spontaneously without dose modification. The incidence of these milder rashes were comparable to our prior reports of rituximab and lenalidomide.”
“Grade 3 rash, however, occurred in 36% of patients, which is significantly higher than [with] rituximab and lenalidomide, [which is] typically 7% to 8%, or single-agent ibrutinib, which is about 3% to 4%.”
Patients with grade 3 rash were managed with supportive care, including acetaminophen, diphenhydramine, and oral corticosteroids.
All but 1 patient (7/8) had dose delays and reductions due to rash. One patient withdrew from the study because of rash, and 1 patient withdrew because of disease progression that occurred during a dose delay for rash.
Response and survival
The ORR was 95% for the entire cohort, 100% at DL0 and DL1 and 94% at DL2. The CR/unconfirmed CR rate was 63% overall, 67% at DL0, 33% at DL1, and 69% at DL2.
The partial response rate was 32% overall, 33% at DL0, 67% at DL1, and 25% at DL2. Five percent of patients had stable disease, all at DL2 (6% of this group).
The median time to first response was 2.3 months (range, 1.9 to 11.1). And the median time to best response was 5.5 months (range, 1.9 to 20.2).
At a median follow-up of 12.3 months, all patients are still alive. The 12-month PFS is 84%.
“Preliminary response data were similar to the prior CALGB/Alliance study of rituximab and lenalidomide,” Dr Ujjani noted. “However, given the increased toxicity and required dose modifications, the additional benefit of a third agent is not apparent, and further investigation of the triplet in this setting seems unwarranted.” ![]()
*Data in the abstract differ from data presented at the meeting.
FDA approves rapid-infusion bendamustine

Photo by Bill Branson
The US Food and Drug Administration (FDA) has approved the use of Bendeka, a liquid, low-volume (50 mL), 10-minute infusion formulation of bendamustine hydrochloride.
Bendeka is now approved to treat patients with chronic lymphocytic leukemia (CLL) and patients with indolent B-cell non-Hodgkin lymphoma (NHL) that has progressed during or within 6 months of treatment with rituximab or a rituximab-containing regimen.
The FDA previously granted Bendeka orphan drug designation for CLL and indolent B-cell NHL.
Under a license agreement with Eagle Pharmaceuticals, Inc., Teva Pharmaceutical Industries Ltd. is responsible for all US commercial activities for Bendeka.
Teva said it expects to make Bendeka commercially available to prescribers during the first quarter of 2016. For details on the drug, see the full prescribing information.
Teva also markets bendamustine hydrochloride under the trade name Treanda, which is FDA-approved to treat CLL and NHL and is available in 2 formulations:
- A solution of 45 mg/0.5 mL or 180 mg/2 mL in a single-dose vial
- A 25 mg or 100 mg lyophilized powder in a single-dose vial for reconstitution.


Photo by Bill Branson
The US Food and Drug Administration (FDA) has approved the use of Bendeka, a liquid, low-volume (50 mL), 10-minute infusion formulation of bendamustine hydrochloride.
Bendeka is now approved to treat patients with chronic lymphocytic leukemia (CLL) and patients with indolent B-cell non-Hodgkin lymphoma (NHL) that has progressed during or within 6 months of treatment with rituximab or a rituximab-containing regimen.
The FDA previously granted Bendeka orphan drug designation for CLL and indolent B-cell NHL.
Under a license agreement with Eagle Pharmaceuticals, Inc., Teva Pharmaceutical Industries Ltd. is responsible for all US commercial activities for Bendeka.
Teva said it expects to make Bendeka commercially available to prescribers during the first quarter of 2016. For details on the drug, see the full prescribing information.
Teva also markets bendamustine hydrochloride under the trade name Treanda, which is FDA-approved to treat CLL and NHL and is available in 2 formulations:
- A solution of 45 mg/0.5 mL or 180 mg/2 mL in a single-dose vial
- A 25 mg or 100 mg lyophilized powder in a single-dose vial for reconstitution.


Photo by Bill Branson
The US Food and Drug Administration (FDA) has approved the use of Bendeka, a liquid, low-volume (50 mL), 10-minute infusion formulation of bendamustine hydrochloride.
Bendeka is now approved to treat patients with chronic lymphocytic leukemia (CLL) and patients with indolent B-cell non-Hodgkin lymphoma (NHL) that has progressed during or within 6 months of treatment with rituximab or a rituximab-containing regimen.
The FDA previously granted Bendeka orphan drug designation for CLL and indolent B-cell NHL.
Under a license agreement with Eagle Pharmaceuticals, Inc., Teva Pharmaceutical Industries Ltd. is responsible for all US commercial activities for Bendeka.
Teva said it expects to make Bendeka commercially available to prescribers during the first quarter of 2016. For details on the drug, see the full prescribing information.
Teva also markets bendamustine hydrochloride under the trade name Treanda, which is FDA-approved to treat CLL and NHL and is available in 2 formulations:
- A solution of 45 mg/0.5 mL or 180 mg/2 mL in a single-dose vial
- A 25 mg or 100 mg lyophilized powder in a single-dose vial for reconstitution.

FDA grants KTE-C19 breakthrough designation

The US Food and Drug Administration (FDA) has granted breakthrough designation for the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 as a treatment for refractory diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), and transformed follicular lymphoma (TFL).
To create KTE-C19, T cells are modified to express a CAR designed to target CD19, a cell-surface protein expressed in B-cell lymphomas and leukemias.
Breakthrough therapy designation is designed to accelerate the development and review of medicines that demonstrate early clinical evidence of a substantial improvement over current treatment options for serious diseases.
The designation conveys all the features of the FDA’s fast track program, as well as more intensive FDA guidance on an efficient drug development program and eligibility for rolling review and priority review.
KTE-C19 research
In a study published in the Journal of Clinical Oncology last year, researchers evaluated KTE-C19 in 15 patients with advanced B-cell malignancies.
The patients received a conditioning regimen of cyclophosphamide and fludarabine, followed 1 day later by a single infusion of KTE-C19. The researchers noted that the conditioning regimen is known to be active against B-cell malignancies and could have made a direct contribution to patient responses.
Thirteen patients were evaluable for response. One patient was lost to follow-up because of noncompliance, and 1 died soon after treatment. The researchers said the cause of death was likely cardiac arrhythmia.
The overall response rate was 92%. Eight patients achieved a complete response (CR), and 4 had a partial response (PR).
Of the 7 patients with DLBCL, 4 achieved a CR, 2 achieved a PR, and 1 had stable disease. Three of the CRs were ongoing at the time of publication, with the duration ranging from 9 months to 22 months.
Of the 4 patients with chronic lymphocytic leukemia, 3 had a CR, and 1 had a PR. All 3 CRs were ongoing at the time of publication, with the duration ranging from 14 months to 23 months.
Among the 2 patients with indolent lymphomas, 1 achieved a CR, and 1 had a PR. The duration of the CR was 11 months at the time of publication.
KTE-C19 elicited a number of adverse events, including fever, hypotension, delirium, and other neurologic toxicities. All but 2 patients experienced grade 3/4 adverse events.
Three patients developed unexpected neurologic abnormalities. One patient experienced aphasia and right-sided facial paresis. One patient developed aphasia, confusion, and severe, generalized myoclonus. And 1 patient had aphasia, confusion, hemifacial spasms, apraxia, and gait disturbances.
KTE-C19 is currently under investigation in a phase 2 trial of refractory DLBCL, PMBCL, and TFL (ZUMA-1), a phase 2 trial of relapsed/refractory mantle cell lymphoma (ZUMA-2), a phase 1/2 trial of relapsed/refractory adult acute lymphoblastic leukemia (ZUMA-3), and a phase 1/2 trial of relapsed/refractory pediatric acute lymphoblastic leukemia (ZUMA-4).
Data from ZUMA-1 were presented at the 2015 ASH Annual Meeting (abstracts 2730 and 3991).
KTE-C19 is under development by Kite Pharma. ![]()

The US Food and Drug Administration (FDA) has granted breakthrough designation for the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 as a treatment for refractory diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), and transformed follicular lymphoma (TFL).
To create KTE-C19, T cells are modified to express a CAR designed to target CD19, a cell-surface protein expressed in B-cell lymphomas and leukemias.
Breakthrough therapy designation is designed to accelerate the development and review of medicines that demonstrate early clinical evidence of a substantial improvement over current treatment options for serious diseases.
The designation conveys all the features of the FDA’s fast track program, as well as more intensive FDA guidance on an efficient drug development program and eligibility for rolling review and priority review.
KTE-C19 research
In a study published in the Journal of Clinical Oncology last year, researchers evaluated KTE-C19 in 15 patients with advanced B-cell malignancies.
The patients received a conditioning regimen of cyclophosphamide and fludarabine, followed 1 day later by a single infusion of KTE-C19. The researchers noted that the conditioning regimen is known to be active against B-cell malignancies and could have made a direct contribution to patient responses.
Thirteen patients were evaluable for response. One patient was lost to follow-up because of noncompliance, and 1 died soon after treatment. The researchers said the cause of death was likely cardiac arrhythmia.
The overall response rate was 92%. Eight patients achieved a complete response (CR), and 4 had a partial response (PR).
Of the 7 patients with DLBCL, 4 achieved a CR, 2 achieved a PR, and 1 had stable disease. Three of the CRs were ongoing at the time of publication, with the duration ranging from 9 months to 22 months.
Of the 4 patients with chronic lymphocytic leukemia, 3 had a CR, and 1 had a PR. All 3 CRs were ongoing at the time of publication, with the duration ranging from 14 months to 23 months.
Among the 2 patients with indolent lymphomas, 1 achieved a CR, and 1 had a PR. The duration of the CR was 11 months at the time of publication.
KTE-C19 elicited a number of adverse events, including fever, hypotension, delirium, and other neurologic toxicities. All but 2 patients experienced grade 3/4 adverse events.
Three patients developed unexpected neurologic abnormalities. One patient experienced aphasia and right-sided facial paresis. One patient developed aphasia, confusion, and severe, generalized myoclonus. And 1 patient had aphasia, confusion, hemifacial spasms, apraxia, and gait disturbances.
KTE-C19 is currently under investigation in a phase 2 trial of refractory DLBCL, PMBCL, and TFL (ZUMA-1), a phase 2 trial of relapsed/refractory mantle cell lymphoma (ZUMA-2), a phase 1/2 trial of relapsed/refractory adult acute lymphoblastic leukemia (ZUMA-3), and a phase 1/2 trial of relapsed/refractory pediatric acute lymphoblastic leukemia (ZUMA-4).
Data from ZUMA-1 were presented at the 2015 ASH Annual Meeting (abstracts 2730 and 3991).
KTE-C19 is under development by Kite Pharma. ![]()

The US Food and Drug Administration (FDA) has granted breakthrough designation for the chimeric antigen receptor (CAR) T-cell therapy KTE-C19 as a treatment for refractory diffuse large B-cell lymphoma (DLBCL), primary mediastinal B-cell lymphoma (PMBCL), and transformed follicular lymphoma (TFL).
To create KTE-C19, T cells are modified to express a CAR designed to target CD19, a cell-surface protein expressed in B-cell lymphomas and leukemias.
Breakthrough therapy designation is designed to accelerate the development and review of medicines that demonstrate early clinical evidence of a substantial improvement over current treatment options for serious diseases.
The designation conveys all the features of the FDA’s fast track program, as well as more intensive FDA guidance on an efficient drug development program and eligibility for rolling review and priority review.
KTE-C19 research
In a study published in the Journal of Clinical Oncology last year, researchers evaluated KTE-C19 in 15 patients with advanced B-cell malignancies.
The patients received a conditioning regimen of cyclophosphamide and fludarabine, followed 1 day later by a single infusion of KTE-C19. The researchers noted that the conditioning regimen is known to be active against B-cell malignancies and could have made a direct contribution to patient responses.
Thirteen patients were evaluable for response. One patient was lost to follow-up because of noncompliance, and 1 died soon after treatment. The researchers said the cause of death was likely cardiac arrhythmia.
The overall response rate was 92%. Eight patients achieved a complete response (CR), and 4 had a partial response (PR).
Of the 7 patients with DLBCL, 4 achieved a CR, 2 achieved a PR, and 1 had stable disease. Three of the CRs were ongoing at the time of publication, with the duration ranging from 9 months to 22 months.
Of the 4 patients with chronic lymphocytic leukemia, 3 had a CR, and 1 had a PR. All 3 CRs were ongoing at the time of publication, with the duration ranging from 14 months to 23 months.
Among the 2 patients with indolent lymphomas, 1 achieved a CR, and 1 had a PR. The duration of the CR was 11 months at the time of publication.
KTE-C19 elicited a number of adverse events, including fever, hypotension, delirium, and other neurologic toxicities. All but 2 patients experienced grade 3/4 adverse events.
Three patients developed unexpected neurologic abnormalities. One patient experienced aphasia and right-sided facial paresis. One patient developed aphasia, confusion, and severe, generalized myoclonus. And 1 patient had aphasia, confusion, hemifacial spasms, apraxia, and gait disturbances.
KTE-C19 is currently under investigation in a phase 2 trial of refractory DLBCL, PMBCL, and TFL (ZUMA-1), a phase 2 trial of relapsed/refractory mantle cell lymphoma (ZUMA-2), a phase 1/2 trial of relapsed/refractory adult acute lymphoblastic leukemia (ZUMA-3), and a phase 1/2 trial of relapsed/refractory pediatric acute lymphoblastic leukemia (ZUMA-4).
Data from ZUMA-1 were presented at the 2015 ASH Annual Meeting (abstracts 2730 and 3991).
KTE-C19 is under development by Kite Pharma. ![]()
2nd-gen BTK inhibitor may be safer, team says

ORLANDO, FL—The second-generation BTK inhibitor acalabrutinib (ACP-196) can elicit durable partial responses in patients with chronic lymphocytic leukemia (CLL) while producing minimal side effects, according to researchers.
They said data suggest that, compared to the first-generation BTK inhibitor ibrutinib, acalabrutinib more selectively blocks the BTK pathway.
And it does so without disrupting other molecular pathways that are important for preserving platelet and immune function, thereby avoiding or minimizing certain side effects.
John C. Byrd, MD, of The Ohio State University Comprehensive Cancer Center in Columbus, and his colleagues reported data from an ongoing phase 1/2 trial of acalabrutinib in NEJM and at the 2015 ASH Annual Meeting (abstract 831). The study was sponsored by Acerta Pharma.
The researchers reported on 61 patients with relapsed CLL. They had a median age of 62 (range, 44-84) and a median of 3 prior therapies (range, 1-13).
Most patients had an ECOG performance status of 1 (59%) or 0 (36%). Most had high-risk (67%) or intermediate-risk disease (31%) according to Rai classification. Forty-six percent of patients had lymph nodes ≥ 5 cm in diameter, and 5% had lymph nodes ≥ 10 cm.
Seventy-five percent of patients had unmutated immunoglobulin variable-region heavy-chain gene, 31% had 17p deletion, 29% had 17q deletion, and 81% had β2-microglobulin > 3.5 mg/liter.
Patients enrolled in the phase 1 portion of the study received escalating doses of acalabrutinib, with a maximum dose of 400 mg once daily. Patients involved in the phase 2 portion of the study were treated with a 100 mg dose twice daily.
Adverse events and discontinuation
At a median follow-up of 14.3 months (range, 0.5 to 20), 53 patients are still receiving treatment.
The primary reasons for treatment discontinuation were investigator or patient decision (n=2), active autoimmune hemolytic anemia that required additional therapy (n=1), fatal pneumonia (n=1), CLL progression, and adverse events of diarrhea (n=1), gastritis (n=1), and dyspnea (n=1).
The most common adverse events of all grades (occurring in at least 20% of patients) were headache (43%), diarrhea (39%), increased weight (26%), pyrexia (23%), upper respiratory tract infection (23%), fatigue (21%), peripheral edema (21%), hypertension (20%), and nausea (20%).
Grade 3/4 adverse events included diarrhea (2%), increased weight (2%), pyrexia (3%), fatigue (3%), hypertension (7%), and arthralgia (2%).
Response
The overall response rate among the 60 evaluable patients was 95%. This included partial responses in 85% of patients and partial responses with lymphocytosis in 10%. The rate of stable disease was 5%.
The researchers noted that responses occurred in all dosing cohorts, and the response rate increased over time.
All 18 patients with 17p deletion experienced a partial response (89%) or partial response with lymphocytosis (11%). But 1 of these patients later progressed.
All 4 patients who previously received idelalisib responded to acalabrutinib, with partial responses in 75% and partial responses with lymphocytosis in 25%.
There were no cases of Richter’s transformation.
In all, 1 patient experienced progression at 16 months, and 1 patient died of pneumonia at 13 months.
“This data is very exciting because it illustrates that acalabrutinib is a highly potent and selective oral BTK inhibitor that can be given safely in patients with relapsed CLL,” Dr Byrd said. “What is particularly remarkable is how well patients are tolerating this therapy.”
Clinical trials of acalabrutinib in CLL are ongoing, including a phase 3 head-to-head comparison of ibrutinib and acalabrutinib. ![]()

ORLANDO, FL—The second-generation BTK inhibitor acalabrutinib (ACP-196) can elicit durable partial responses in patients with chronic lymphocytic leukemia (CLL) while producing minimal side effects, according to researchers.
They said data suggest that, compared to the first-generation BTK inhibitor ibrutinib, acalabrutinib more selectively blocks the BTK pathway.
And it does so without disrupting other molecular pathways that are important for preserving platelet and immune function, thereby avoiding or minimizing certain side effects.
John C. Byrd, MD, of The Ohio State University Comprehensive Cancer Center in Columbus, and his colleagues reported data from an ongoing phase 1/2 trial of acalabrutinib in NEJM and at the 2015 ASH Annual Meeting (abstract 831). The study was sponsored by Acerta Pharma.
The researchers reported on 61 patients with relapsed CLL. They had a median age of 62 (range, 44-84) and a median of 3 prior therapies (range, 1-13).
Most patients had an ECOG performance status of 1 (59%) or 0 (36%). Most had high-risk (67%) or intermediate-risk disease (31%) according to Rai classification. Forty-six percent of patients had lymph nodes ≥ 5 cm in diameter, and 5% had lymph nodes ≥ 10 cm.
Seventy-five percent of patients had unmutated immunoglobulin variable-region heavy-chain gene, 31% had 17p deletion, 29% had 17q deletion, and 81% had β2-microglobulin > 3.5 mg/liter.
Patients enrolled in the phase 1 portion of the study received escalating doses of acalabrutinib, with a maximum dose of 400 mg once daily. Patients involved in the phase 2 portion of the study were treated with a 100 mg dose twice daily.
Adverse events and discontinuation
At a median follow-up of 14.3 months (range, 0.5 to 20), 53 patients are still receiving treatment.
The primary reasons for treatment discontinuation were investigator or patient decision (n=2), active autoimmune hemolytic anemia that required additional therapy (n=1), fatal pneumonia (n=1), CLL progression, and adverse events of diarrhea (n=1), gastritis (n=1), and dyspnea (n=1).
The most common adverse events of all grades (occurring in at least 20% of patients) were headache (43%), diarrhea (39%), increased weight (26%), pyrexia (23%), upper respiratory tract infection (23%), fatigue (21%), peripheral edema (21%), hypertension (20%), and nausea (20%).
Grade 3/4 adverse events included diarrhea (2%), increased weight (2%), pyrexia (3%), fatigue (3%), hypertension (7%), and arthralgia (2%).
Response
The overall response rate among the 60 evaluable patients was 95%. This included partial responses in 85% of patients and partial responses with lymphocytosis in 10%. The rate of stable disease was 5%.
The researchers noted that responses occurred in all dosing cohorts, and the response rate increased over time.
All 18 patients with 17p deletion experienced a partial response (89%) or partial response with lymphocytosis (11%). But 1 of these patients later progressed.
All 4 patients who previously received idelalisib responded to acalabrutinib, with partial responses in 75% and partial responses with lymphocytosis in 25%.
There were no cases of Richter’s transformation.
In all, 1 patient experienced progression at 16 months, and 1 patient died of pneumonia at 13 months.
“This data is very exciting because it illustrates that acalabrutinib is a highly potent and selective oral BTK inhibitor that can be given safely in patients with relapsed CLL,” Dr Byrd said. “What is particularly remarkable is how well patients are tolerating this therapy.”
Clinical trials of acalabrutinib in CLL are ongoing, including a phase 3 head-to-head comparison of ibrutinib and acalabrutinib. ![]()

ORLANDO, FL—The second-generation BTK inhibitor acalabrutinib (ACP-196) can elicit durable partial responses in patients with chronic lymphocytic leukemia (CLL) while producing minimal side effects, according to researchers.
They said data suggest that, compared to the first-generation BTK inhibitor ibrutinib, acalabrutinib more selectively blocks the BTK pathway.
And it does so without disrupting other molecular pathways that are important for preserving platelet and immune function, thereby avoiding or minimizing certain side effects.
John C. Byrd, MD, of The Ohio State University Comprehensive Cancer Center in Columbus, and his colleagues reported data from an ongoing phase 1/2 trial of acalabrutinib in NEJM and at the 2015 ASH Annual Meeting (abstract 831). The study was sponsored by Acerta Pharma.
The researchers reported on 61 patients with relapsed CLL. They had a median age of 62 (range, 44-84) and a median of 3 prior therapies (range, 1-13).
Most patients had an ECOG performance status of 1 (59%) or 0 (36%). Most had high-risk (67%) or intermediate-risk disease (31%) according to Rai classification. Forty-six percent of patients had lymph nodes ≥ 5 cm in diameter, and 5% had lymph nodes ≥ 10 cm.
Seventy-five percent of patients had unmutated immunoglobulin variable-region heavy-chain gene, 31% had 17p deletion, 29% had 17q deletion, and 81% had β2-microglobulin > 3.5 mg/liter.
Patients enrolled in the phase 1 portion of the study received escalating doses of acalabrutinib, with a maximum dose of 400 mg once daily. Patients involved in the phase 2 portion of the study were treated with a 100 mg dose twice daily.
Adverse events and discontinuation
At a median follow-up of 14.3 months (range, 0.5 to 20), 53 patients are still receiving treatment.
The primary reasons for treatment discontinuation were investigator or patient decision (n=2), active autoimmune hemolytic anemia that required additional therapy (n=1), fatal pneumonia (n=1), CLL progression, and adverse events of diarrhea (n=1), gastritis (n=1), and dyspnea (n=1).
The most common adverse events of all grades (occurring in at least 20% of patients) were headache (43%), diarrhea (39%), increased weight (26%), pyrexia (23%), upper respiratory tract infection (23%), fatigue (21%), peripheral edema (21%), hypertension (20%), and nausea (20%).
Grade 3/4 adverse events included diarrhea (2%), increased weight (2%), pyrexia (3%), fatigue (3%), hypertension (7%), and arthralgia (2%).
Response
The overall response rate among the 60 evaluable patients was 95%. This included partial responses in 85% of patients and partial responses with lymphocytosis in 10%. The rate of stable disease was 5%.
The researchers noted that responses occurred in all dosing cohorts, and the response rate increased over time.
All 18 patients with 17p deletion experienced a partial response (89%) or partial response with lymphocytosis (11%). But 1 of these patients later progressed.
All 4 patients who previously received idelalisib responded to acalabrutinib, with partial responses in 75% and partial responses with lymphocytosis in 25%.
There were no cases of Richter’s transformation.
In all, 1 patient experienced progression at 16 months, and 1 patient died of pneumonia at 13 months.
“This data is very exciting because it illustrates that acalabrutinib is a highly potent and selective oral BTK inhibitor that can be given safely in patients with relapsed CLL,” Dr Byrd said. “What is particularly remarkable is how well patients are tolerating this therapy.”
Clinical trials of acalabrutinib in CLL are ongoing, including a phase 3 head-to-head comparison of ibrutinib and acalabrutinib. ![]()
CAR exhibits activity in resistant B-cell malignancies

Photo courtesy of ASH
ORLANDO, FL—Allogeneic chimeric antigen receptor (CAR) T cells directed against CD19 can have “significant” activity against resistant B-cell malignancies, even when given without prior chemotherapy, according to a presentation at the 2015 ASH Annual Meeting.
Nine of 20 patients responded to treatment with the CAR T cells, despite having failed prior allogeneic transplant. The best responses were observed in patients with acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL).
“Malignancies that were resistant to allogeneic transplants and standard donor lymphocyte infusions regressed after infusions of allogeneic anti-CD19 CAR T cells,” said James N. Kochenderfer, MD, of the National Cancer Institute in Bethesda, Maryland.
“Allogeneic anti-CD19 CAR T cells seem to be particularly effective against ALL and CLL, suggesting a possible antigenic stimulation that may be more pronounced in these malignancies.”
Adverse events associated with these CAR T cells included severe but reversible cytokine release syndrome, mild aphasia, and muscle damage. There were no cases of acute graft-vs-host disease (GVHD).
Dr Kochenderfer presented these results at ASH as abstract 99.
For this phase 1 study, researchers tested a CAR T-cell therapy that was originally developed by Dr Kochenderfer and his colleagues. The therapy is now known as KTE-C19 and is under development by Kite Pharmaceuticals. However, the company did not sponsor this trial.
The study was open to patients with any CD19+ B-cell malignancy that persisted after allogeneic transplant.
All patients except those with ALL were required to have received at least one standard donor lymphocyte infusion. In addition, patients were only eligible if they had minimal or no GVHD and were not receiving any systemic immunosuppressive drugs.
The trial included 20 patients—5 each with ALL, CLL, mantle cell lymphoma (MCL), and diffuse large B-cell lymphoma (DLBCL).
All patients received a single infusion of CAR T cells derived from their original transplant donor. Production of these cells took 8 days. The highest dose of CAR T cells given was 107 cells/kg.
Four of the ALL patients obtained a minimal-residual disease-negative complete response (CR), but 2 of these patients subsequently relapsed. Of the other 2 patients, 1 remains in CR at 18 months of follow-up, and the other went on to receive a second allogeneic transplant. That patient remains in CR today.
Among the CLL patients, 1 achieved a CR, and 1 achieved a partial response (PR). One patient had stable disease (SD), and the other 2 progressed. Both the CR and the PR are ongoing at 36 and 18 months of follow-up, respectively.
One MCL patient achieved a CR, 1 had a PR, and 3 had SD. The CR is ongoing at 31 months. One DLBCL patient achieved a CR, 3 had SD, and 1 progressed.
Dr Kochenderfer noted that response was associated with higher blood CAR T-cell levels. There was a significant difference in CAR T-cell levels between responders and nonresponders (P=0.001).
In addition, the presence of blood B-cell levels before CAR T-cell infusion was associated with higher blood CAR T-cell levels. Patients with normal or high B lymphocytes had higher levels of CAR T cells in their blood (P=0.04).
Patients with high tumor burdens developed severe cytokine-release syndrome with fever, tachycardia, and hypotension. The ALL patients were particularly susceptible to cytokine-release syndrome.
Dr Kochenderfer said neurologic toxicity was rare and mild. There was 1 case of mild aphasia.
There were 2 patients with elevations in CPK, indicating muscle damage. Those patients also reported muscle pain, and 1 patient reported weakness.
“This is one of the first reports, I think, of muscle damage in CAR T-cell patients,” Dr Kochenderfer said.
None of the patients developed acute GVHD after CAR T-cell therapy. One patient had continued worsening of pre-existing chronic GVHD after treatment, and 1 patient developed mild chronic eye GVHD more than a year after CAR T-cell infusion.
Dr Kochenderfer said additional details from this trial will be published in an upcoming issue of the Journal of Clinical Oncology. ![]()

Photo courtesy of ASH
ORLANDO, FL—Allogeneic chimeric antigen receptor (CAR) T cells directed against CD19 can have “significant” activity against resistant B-cell malignancies, even when given without prior chemotherapy, according to a presentation at the 2015 ASH Annual Meeting.
Nine of 20 patients responded to treatment with the CAR T cells, despite having failed prior allogeneic transplant. The best responses were observed in patients with acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL).
“Malignancies that were resistant to allogeneic transplants and standard donor lymphocyte infusions regressed after infusions of allogeneic anti-CD19 CAR T cells,” said James N. Kochenderfer, MD, of the National Cancer Institute in Bethesda, Maryland.
“Allogeneic anti-CD19 CAR T cells seem to be particularly effective against ALL and CLL, suggesting a possible antigenic stimulation that may be more pronounced in these malignancies.”
Adverse events associated with these CAR T cells included severe but reversible cytokine release syndrome, mild aphasia, and muscle damage. There were no cases of acute graft-vs-host disease (GVHD).
Dr Kochenderfer presented these results at ASH as abstract 99.
For this phase 1 study, researchers tested a CAR T-cell therapy that was originally developed by Dr Kochenderfer and his colleagues. The therapy is now known as KTE-C19 and is under development by Kite Pharmaceuticals. However, the company did not sponsor this trial.
The study was open to patients with any CD19+ B-cell malignancy that persisted after allogeneic transplant.
All patients except those with ALL were required to have received at least one standard donor lymphocyte infusion. In addition, patients were only eligible if they had minimal or no GVHD and were not receiving any systemic immunosuppressive drugs.
The trial included 20 patients—5 each with ALL, CLL, mantle cell lymphoma (MCL), and diffuse large B-cell lymphoma (DLBCL).
All patients received a single infusion of CAR T cells derived from their original transplant donor. Production of these cells took 8 days. The highest dose of CAR T cells given was 107 cells/kg.
Four of the ALL patients obtained a minimal-residual disease-negative complete response (CR), but 2 of these patients subsequently relapsed. Of the other 2 patients, 1 remains in CR at 18 months of follow-up, and the other went on to receive a second allogeneic transplant. That patient remains in CR today.
Among the CLL patients, 1 achieved a CR, and 1 achieved a partial response (PR). One patient had stable disease (SD), and the other 2 progressed. Both the CR and the PR are ongoing at 36 and 18 months of follow-up, respectively.
One MCL patient achieved a CR, 1 had a PR, and 3 had SD. The CR is ongoing at 31 months. One DLBCL patient achieved a CR, 3 had SD, and 1 progressed.
Dr Kochenderfer noted that response was associated with higher blood CAR T-cell levels. There was a significant difference in CAR T-cell levels between responders and nonresponders (P=0.001).
In addition, the presence of blood B-cell levels before CAR T-cell infusion was associated with higher blood CAR T-cell levels. Patients with normal or high B lymphocytes had higher levels of CAR T cells in their blood (P=0.04).
Patients with high tumor burdens developed severe cytokine-release syndrome with fever, tachycardia, and hypotension. The ALL patients were particularly susceptible to cytokine-release syndrome.
Dr Kochenderfer said neurologic toxicity was rare and mild. There was 1 case of mild aphasia.
There were 2 patients with elevations in CPK, indicating muscle damage. Those patients also reported muscle pain, and 1 patient reported weakness.
“This is one of the first reports, I think, of muscle damage in CAR T-cell patients,” Dr Kochenderfer said.
None of the patients developed acute GVHD after CAR T-cell therapy. One patient had continued worsening of pre-existing chronic GVHD after treatment, and 1 patient developed mild chronic eye GVHD more than a year after CAR T-cell infusion.
Dr Kochenderfer said additional details from this trial will be published in an upcoming issue of the Journal of Clinical Oncology. ![]()

Photo courtesy of ASH
ORLANDO, FL—Allogeneic chimeric antigen receptor (CAR) T cells directed against CD19 can have “significant” activity against resistant B-cell malignancies, even when given without prior chemotherapy, according to a presentation at the 2015 ASH Annual Meeting.
Nine of 20 patients responded to treatment with the CAR T cells, despite having failed prior allogeneic transplant. The best responses were observed in patients with acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL).
“Malignancies that were resistant to allogeneic transplants and standard donor lymphocyte infusions regressed after infusions of allogeneic anti-CD19 CAR T cells,” said James N. Kochenderfer, MD, of the National Cancer Institute in Bethesda, Maryland.
“Allogeneic anti-CD19 CAR T cells seem to be particularly effective against ALL and CLL, suggesting a possible antigenic stimulation that may be more pronounced in these malignancies.”
Adverse events associated with these CAR T cells included severe but reversible cytokine release syndrome, mild aphasia, and muscle damage. There were no cases of acute graft-vs-host disease (GVHD).
Dr Kochenderfer presented these results at ASH as abstract 99.
For this phase 1 study, researchers tested a CAR T-cell therapy that was originally developed by Dr Kochenderfer and his colleagues. The therapy is now known as KTE-C19 and is under development by Kite Pharmaceuticals. However, the company did not sponsor this trial.
The study was open to patients with any CD19+ B-cell malignancy that persisted after allogeneic transplant.
All patients except those with ALL were required to have received at least one standard donor lymphocyte infusion. In addition, patients were only eligible if they had minimal or no GVHD and were not receiving any systemic immunosuppressive drugs.
The trial included 20 patients—5 each with ALL, CLL, mantle cell lymphoma (MCL), and diffuse large B-cell lymphoma (DLBCL).
All patients received a single infusion of CAR T cells derived from their original transplant donor. Production of these cells took 8 days. The highest dose of CAR T cells given was 107 cells/kg.
Four of the ALL patients obtained a minimal-residual disease-negative complete response (CR), but 2 of these patients subsequently relapsed. Of the other 2 patients, 1 remains in CR at 18 months of follow-up, and the other went on to receive a second allogeneic transplant. That patient remains in CR today.
Among the CLL patients, 1 achieved a CR, and 1 achieved a partial response (PR). One patient had stable disease (SD), and the other 2 progressed. Both the CR and the PR are ongoing at 36 and 18 months of follow-up, respectively.
One MCL patient achieved a CR, 1 had a PR, and 3 had SD. The CR is ongoing at 31 months. One DLBCL patient achieved a CR, 3 had SD, and 1 progressed.
Dr Kochenderfer noted that response was associated with higher blood CAR T-cell levels. There was a significant difference in CAR T-cell levels between responders and nonresponders (P=0.001).
In addition, the presence of blood B-cell levels before CAR T-cell infusion was associated with higher blood CAR T-cell levels. Patients with normal or high B lymphocytes had higher levels of CAR T cells in their blood (P=0.04).
Patients with high tumor burdens developed severe cytokine-release syndrome with fever, tachycardia, and hypotension. The ALL patients were particularly susceptible to cytokine-release syndrome.
Dr Kochenderfer said neurologic toxicity was rare and mild. There was 1 case of mild aphasia.
There were 2 patients with elevations in CPK, indicating muscle damage. Those patients also reported muscle pain, and 1 patient reported weakness.
“This is one of the first reports, I think, of muscle damage in CAR T-cell patients,” Dr Kochenderfer said.
None of the patients developed acute GVHD after CAR T-cell therapy. One patient had continued worsening of pre-existing chronic GVHD after treatment, and 1 patient developed mild chronic eye GVHD more than a year after CAR T-cell infusion.
Dr Kochenderfer said additional details from this trial will be published in an upcoming issue of the Journal of Clinical Oncology. ![]()
Ibrutinib ‘treatment of choice’ in rel/ref MCL
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—The BTK inhibitor ibrutinib should be considered the treatment of choice for patients with relapsed or refractory mantle cell lymphoma (MCL), according to a speaker at the 2015 ASH Annual Meeting.
Results of the phase 3 RAY trial showed that ibrutinib can prolong progression-free survival (PFS) when compared to the mTOR inhibitor temsirolimus.
There was no significant difference in overall survival (OS) between the treatment arms, but this outcome was influenced by the fact that patients were allowed to cross over from the temsirolimus arm to the ibrutinib arm after they progressed.
A majority of patients in both arms experienced adverse events (AEs), and the incidence of grade 3 or higher AEs was high—about 70% with ibrutinib and 90% with temsirolimus.
Simon Rule, MD, of Derriford Hospital in Plymouth, UK, presented these results at the meeting as abstract 469. The study has been published in The Lancet as well.
The research was sponsored by Janssen Biotech, Inc., which is jointly developing and commercializing ibrutinib with Pharmacyclics LLC, an AbbVie company.
Study design
The trial included 280 patients with relapsed or refractory MCL. They were enrolled from December 2012 to November 2013.
The patients were randomized to receive oral ibrutinib (n=139) at 560 mg or intravenous temsirolimus (n=141) at 175 mg on days 1, 8, and 15 of cycle 1 and 75 mg on days 1, 8, and 15 of all subsequent 21-day cycles until disease progression or unacceptable toxicity.
Starting July 2014, patients were allowed to cross over from the ibrutinib arm to the temsirolimus arm if they had progressive disease, as confirmed by an independent review committee. Thirty-two patients ultimately crossed over.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The median age was 67 (range, 39-84) in the ibrutinib arm and 68 (range, 34-88) in the temsirolimus arm. Most patients had an ECOG performance status of 0 (48.2% and 47.5%, respectively) or 1 (51.1% in both arms).
The median number of prior therapies was 2 in both arms (range, 1-9). A majority of patients had 1 to 2 prior lines of therapy—68.3% in the ibrutinib arm and 66% in the temsirolimus arm.
The median time from the end of last therapy was 8.25 months for the ibrutinib arm and 7.03 months for the temsirolimus arm. And about 30% of patients in each arm were refractory to their last therapy—25.9% and 33.3%, respectively.
About half of patients in each arm had intermediate-risk disease (46.8% in the ibrutinib arm and 48.9% in the temsirolimus arm), followed by low-risk (31.7% and 29.8%, respectively) and high-risk disease (21.6% and 21.3%, respectively).
Most patients had stage IV disease—80.6% in the ibrutinib arm and 85.1% in the temsirolimus arm.
PFS
The study’s primary endpoint was PFS, as assessed by an independent review committee.
At a median follow-up of 20 months, the median PFS was 14.6 months for patients in the ibrutinib arm and 6.2 months for patients in the temsirolimus arm (hazard ratio=0.43, P<0.0001). At 2 years, the PFS was 41% in the ibrutinib arm and 7% in the temsirolimus arm.
Dr Rule noted that, looking at these data, people might question the validity of temsirolimus as a comparator to ibrutinib for this patient population.
“If you look at the median PFS for temsirolimus here, it’s 6.2 months,” he said. “In the registration study for Velcade—bortezomib—in the US, PFS was 6.5 months. If you look at the median PFS in the lenalidomide study that got registration, it was 4 months. So [the PFS for temsirolimus] is very representative of an oral novel agent in the context of mantle cell lymphoma.”
Dr Rule also pointed out that the improvement in PFS with ibrutinib was consistent across subgroups (ie, older age, risk score, tumor bulk, refractory disease). The only exception was patients with blastoid histology, but this was a very small group.
Secondary endpoints
The median OS was not reached in the ibrutinib arm but was 21.3 months in the temsirolimus arm.
This difference was not statistically significant, but Dr Rule noted that the trial was not powered for OS, and the analysis is confounded by the crossover. Twenty-three percent of patients in the temsirolimus arm ultimately received ibrutinib.
The overall response rate (ORR) was 71.9% in the ibrutinib arm and 40.4% in the temsirolimus arm (P<0.0001), according to the independent review committee. The complete response rates were 18.7% (n=26) and 1.4% (n=2), respectively.
The median duration of response was not reached with ibrutinib but was 7 months for temsirolimus. The median time to next treatment was not reached with ibrutinib, but it was 11.6 months in the temsirolimus arm (P<0.0001).
And the median duration of study treatment was 14.4 months in the ibrutinib arm and 3 months in the temsirolimus arm.
Timing counts
Dr Rule also presented response and PFS data according to the number of prior therapies patients received.
He noted that patients were more likely to respond to temsirolimus if they had received fewer prior therapies, but this was not the case with ibrutinib. Ibrutinib produced consistent ORRs regardless of when it was given.
In the ibrutinib arm, the ORR was 71.9% for patients who had received 1 prior line of therapy, 68.4% for those who received 2 prior therapies, and 75% for those who received 3 prior therapies. In the temsirolimus arm, the ORRs were 48%, 39.5%, and 33.3%, respectively.
Conversely, patients had a greater PFS benefit if they received ibrutinib earlier in their treatment course, but this was not true for temsirolimus.
At the median follow-up of 20 months, PFS was more than 60% for ibrutinib-treated patients who had received 1 prior line of therapy and less than 30% for ibrutinib-treated patients who received 2 or more prior lines of therapy. PFS was less than 15% for patients in the temsirolimus arm, regardless of their number of prior therapies.
“So that’s perhaps the first hint that, if we’re going to be using [ibrutinib], we should be using it earlier on,” Dr Rule said. “And I also suspect that, with further follow-up with this study, if this holds up, there will be, indeed, a survival benefit observed.”
Safety
“Despite patients on the ibrutinib arm being exposed to drug more than 4 times longer than those with temsirolimus, the frequency of most cumulative adverse events was lower in the ibrutinib arm,” Dr Rule said.
Still, he noted that most patients had some adverse events. And grade 3 or higher adverse events were reported in 67.6% of patients on ibrutinib and 87.1% of patients on temsirolimus.
Grade 3 or higher AEs included atrial fibrillation (AFib) and major bleeding. AFib occurred in 4.3% of patients in the ibrutinib arm and 1.4% in the temsirolimus arm. Major bleeding occurred in 10.1% and 6.5%, respectively.
Five of the 6 patients with AFib in the ibrutinib arm and all 3 patients who developed AFib in the temsirolimus arm had risk factors for AFib prior to treatment. None of these patients discontinued treatment due to AFib.
Dr Rule said there was no evidence to suggest that either drug increases the risk of second primary malignancies, although 3.6% of patients in the ibrutinib arm and 2.9% in the temsirolimus arm were diagnosed with second primary malignancies (mostly non-melanoma skin cancers).
The most common treatment-emergent AEs (≥20%) of any grade for the ibrutinib arm were diarrhea (28.8%), cough (22.3%), and fatigue (22.3%).
The most common treatment-emergent AEs (>20%) of any grade for the temsirolimus arm were thrombocytopenia (56.1%), anemia (43.2%), diarrhea (30.9%), fatigue (28.8%), neutropenia (25.9%), epistaxis (23.7%), cough (22.3%), peripheral edema (22.3%), nausea (21.6%), pyrexia (20.9%), and stomatitis (20.9%).
The most common hematologic AEs (≥10%) in the ibrutinib and temsirolimus arms, respectively, were thrombocytopenia (18% vs 56.1%), anemia (18% vs 43.2%), and neutropenia (15.8% vs 25.9%).
Six percent of patients in the ibrutinib arm and 26% in the temsirolimus arm discontinued treatment due to AEs.
At a median follow-up of 20 months, 42% of patients in the ibrutinib arm and 45% in the temsirolimus arm had died. The most common cause of death associated with ibrutinib was disease progression, and deaths in the temsirolimus arm were primarily attributed to AEs. ![]()
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—The BTK inhibitor ibrutinib should be considered the treatment of choice for patients with relapsed or refractory mantle cell lymphoma (MCL), according to a speaker at the 2015 ASH Annual Meeting.
Results of the phase 3 RAY trial showed that ibrutinib can prolong progression-free survival (PFS) when compared to the mTOR inhibitor temsirolimus.
There was no significant difference in overall survival (OS) between the treatment arms, but this outcome was influenced by the fact that patients were allowed to cross over from the temsirolimus arm to the ibrutinib arm after they progressed.
A majority of patients in both arms experienced adverse events (AEs), and the incidence of grade 3 or higher AEs was high—about 70% with ibrutinib and 90% with temsirolimus.
Simon Rule, MD, of Derriford Hospital in Plymouth, UK, presented these results at the meeting as abstract 469. The study has been published in The Lancet as well.
The research was sponsored by Janssen Biotech, Inc., which is jointly developing and commercializing ibrutinib with Pharmacyclics LLC, an AbbVie company.
Study design
The trial included 280 patients with relapsed or refractory MCL. They were enrolled from December 2012 to November 2013.
The patients were randomized to receive oral ibrutinib (n=139) at 560 mg or intravenous temsirolimus (n=141) at 175 mg on days 1, 8, and 15 of cycle 1 and 75 mg on days 1, 8, and 15 of all subsequent 21-day cycles until disease progression or unacceptable toxicity.
Starting July 2014, patients were allowed to cross over from the ibrutinib arm to the temsirolimus arm if they had progressive disease, as confirmed by an independent review committee. Thirty-two patients ultimately crossed over.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The median age was 67 (range, 39-84) in the ibrutinib arm and 68 (range, 34-88) in the temsirolimus arm. Most patients had an ECOG performance status of 0 (48.2% and 47.5%, respectively) or 1 (51.1% in both arms).
The median number of prior therapies was 2 in both arms (range, 1-9). A majority of patients had 1 to 2 prior lines of therapy—68.3% in the ibrutinib arm and 66% in the temsirolimus arm.
The median time from the end of last therapy was 8.25 months for the ibrutinib arm and 7.03 months for the temsirolimus arm. And about 30% of patients in each arm were refractory to their last therapy—25.9% and 33.3%, respectively.
About half of patients in each arm had intermediate-risk disease (46.8% in the ibrutinib arm and 48.9% in the temsirolimus arm), followed by low-risk (31.7% and 29.8%, respectively) and high-risk disease (21.6% and 21.3%, respectively).
Most patients had stage IV disease—80.6% in the ibrutinib arm and 85.1% in the temsirolimus arm.
PFS
The study’s primary endpoint was PFS, as assessed by an independent review committee.
At a median follow-up of 20 months, the median PFS was 14.6 months for patients in the ibrutinib arm and 6.2 months for patients in the temsirolimus arm (hazard ratio=0.43, P<0.0001). At 2 years, the PFS was 41% in the ibrutinib arm and 7% in the temsirolimus arm.
Dr Rule noted that, looking at these data, people might question the validity of temsirolimus as a comparator to ibrutinib for this patient population.
“If you look at the median PFS for temsirolimus here, it’s 6.2 months,” he said. “In the registration study for Velcade—bortezomib—in the US, PFS was 6.5 months. If you look at the median PFS in the lenalidomide study that got registration, it was 4 months. So [the PFS for temsirolimus] is very representative of an oral novel agent in the context of mantle cell lymphoma.”
Dr Rule also pointed out that the improvement in PFS with ibrutinib was consistent across subgroups (ie, older age, risk score, tumor bulk, refractory disease). The only exception was patients with blastoid histology, but this was a very small group.
Secondary endpoints
The median OS was not reached in the ibrutinib arm but was 21.3 months in the temsirolimus arm.
This difference was not statistically significant, but Dr Rule noted that the trial was not powered for OS, and the analysis is confounded by the crossover. Twenty-three percent of patients in the temsirolimus arm ultimately received ibrutinib.
The overall response rate (ORR) was 71.9% in the ibrutinib arm and 40.4% in the temsirolimus arm (P<0.0001), according to the independent review committee. The complete response rates were 18.7% (n=26) and 1.4% (n=2), respectively.
The median duration of response was not reached with ibrutinib but was 7 months for temsirolimus. The median time to next treatment was not reached with ibrutinib, but it was 11.6 months in the temsirolimus arm (P<0.0001).
And the median duration of study treatment was 14.4 months in the ibrutinib arm and 3 months in the temsirolimus arm.
Timing counts
Dr Rule also presented response and PFS data according to the number of prior therapies patients received.
He noted that patients were more likely to respond to temsirolimus if they had received fewer prior therapies, but this was not the case with ibrutinib. Ibrutinib produced consistent ORRs regardless of when it was given.
In the ibrutinib arm, the ORR was 71.9% for patients who had received 1 prior line of therapy, 68.4% for those who received 2 prior therapies, and 75% for those who received 3 prior therapies. In the temsirolimus arm, the ORRs were 48%, 39.5%, and 33.3%, respectively.
Conversely, patients had a greater PFS benefit if they received ibrutinib earlier in their treatment course, but this was not true for temsirolimus.
At the median follow-up of 20 months, PFS was more than 60% for ibrutinib-treated patients who had received 1 prior line of therapy and less than 30% for ibrutinib-treated patients who received 2 or more prior lines of therapy. PFS was less than 15% for patients in the temsirolimus arm, regardless of their number of prior therapies.
“So that’s perhaps the first hint that, if we’re going to be using [ibrutinib], we should be using it earlier on,” Dr Rule said. “And I also suspect that, with further follow-up with this study, if this holds up, there will be, indeed, a survival benefit observed.”
Safety
“Despite patients on the ibrutinib arm being exposed to drug more than 4 times longer than those with temsirolimus, the frequency of most cumulative adverse events was lower in the ibrutinib arm,” Dr Rule said.
Still, he noted that most patients had some adverse events. And grade 3 or higher adverse events were reported in 67.6% of patients on ibrutinib and 87.1% of patients on temsirolimus.
Grade 3 or higher AEs included atrial fibrillation (AFib) and major bleeding. AFib occurred in 4.3% of patients in the ibrutinib arm and 1.4% in the temsirolimus arm. Major bleeding occurred in 10.1% and 6.5%, respectively.
Five of the 6 patients with AFib in the ibrutinib arm and all 3 patients who developed AFib in the temsirolimus arm had risk factors for AFib prior to treatment. None of these patients discontinued treatment due to AFib.
Dr Rule said there was no evidence to suggest that either drug increases the risk of second primary malignancies, although 3.6% of patients in the ibrutinib arm and 2.9% in the temsirolimus arm were diagnosed with second primary malignancies (mostly non-melanoma skin cancers).
The most common treatment-emergent AEs (≥20%) of any grade for the ibrutinib arm were diarrhea (28.8%), cough (22.3%), and fatigue (22.3%).
The most common treatment-emergent AEs (>20%) of any grade for the temsirolimus arm were thrombocytopenia (56.1%), anemia (43.2%), diarrhea (30.9%), fatigue (28.8%), neutropenia (25.9%), epistaxis (23.7%), cough (22.3%), peripheral edema (22.3%), nausea (21.6%), pyrexia (20.9%), and stomatitis (20.9%).
The most common hematologic AEs (≥10%) in the ibrutinib and temsirolimus arms, respectively, were thrombocytopenia (18% vs 56.1%), anemia (18% vs 43.2%), and neutropenia (15.8% vs 25.9%).
Six percent of patients in the ibrutinib arm and 26% in the temsirolimus arm discontinued treatment due to AEs.
At a median follow-up of 20 months, 42% of patients in the ibrutinib arm and 45% in the temsirolimus arm had died. The most common cause of death associated with ibrutinib was disease progression, and deaths in the temsirolimus arm were primarily attributed to AEs. ![]()
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—The BTK inhibitor ibrutinib should be considered the treatment of choice for patients with relapsed or refractory mantle cell lymphoma (MCL), according to a speaker at the 2015 ASH Annual Meeting.
Results of the phase 3 RAY trial showed that ibrutinib can prolong progression-free survival (PFS) when compared to the mTOR inhibitor temsirolimus.
There was no significant difference in overall survival (OS) between the treatment arms, but this outcome was influenced by the fact that patients were allowed to cross over from the temsirolimus arm to the ibrutinib arm after they progressed.
A majority of patients in both arms experienced adverse events (AEs), and the incidence of grade 3 or higher AEs was high—about 70% with ibrutinib and 90% with temsirolimus.
Simon Rule, MD, of Derriford Hospital in Plymouth, UK, presented these results at the meeting as abstract 469. The study has been published in The Lancet as well.
The research was sponsored by Janssen Biotech, Inc., which is jointly developing and commercializing ibrutinib with Pharmacyclics LLC, an AbbVie company.
Study design
The trial included 280 patients with relapsed or refractory MCL. They were enrolled from December 2012 to November 2013.
The patients were randomized to receive oral ibrutinib (n=139) at 560 mg or intravenous temsirolimus (n=141) at 175 mg on days 1, 8, and 15 of cycle 1 and 75 mg on days 1, 8, and 15 of all subsequent 21-day cycles until disease progression or unacceptable toxicity.
Starting July 2014, patients were allowed to cross over from the ibrutinib arm to the temsirolimus arm if they had progressive disease, as confirmed by an independent review committee. Thirty-two patients ultimately crossed over.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The median age was 67 (range, 39-84) in the ibrutinib arm and 68 (range, 34-88) in the temsirolimus arm. Most patients had an ECOG performance status of 0 (48.2% and 47.5%, respectively) or 1 (51.1% in both arms).
The median number of prior therapies was 2 in both arms (range, 1-9). A majority of patients had 1 to 2 prior lines of therapy—68.3% in the ibrutinib arm and 66% in the temsirolimus arm.
The median time from the end of last therapy was 8.25 months for the ibrutinib arm and 7.03 months for the temsirolimus arm. And about 30% of patients in each arm were refractory to their last therapy—25.9% and 33.3%, respectively.
About half of patients in each arm had intermediate-risk disease (46.8% in the ibrutinib arm and 48.9% in the temsirolimus arm), followed by low-risk (31.7% and 29.8%, respectively) and high-risk disease (21.6% and 21.3%, respectively).
Most patients had stage IV disease—80.6% in the ibrutinib arm and 85.1% in the temsirolimus arm.
PFS
The study’s primary endpoint was PFS, as assessed by an independent review committee.
At a median follow-up of 20 months, the median PFS was 14.6 months for patients in the ibrutinib arm and 6.2 months for patients in the temsirolimus arm (hazard ratio=0.43, P<0.0001). At 2 years, the PFS was 41% in the ibrutinib arm and 7% in the temsirolimus arm.
Dr Rule noted that, looking at these data, people might question the validity of temsirolimus as a comparator to ibrutinib for this patient population.
“If you look at the median PFS for temsirolimus here, it’s 6.2 months,” he said. “In the registration study for Velcade—bortezomib—in the US, PFS was 6.5 months. If you look at the median PFS in the lenalidomide study that got registration, it was 4 months. So [the PFS for temsirolimus] is very representative of an oral novel agent in the context of mantle cell lymphoma.”
Dr Rule also pointed out that the improvement in PFS with ibrutinib was consistent across subgroups (ie, older age, risk score, tumor bulk, refractory disease). The only exception was patients with blastoid histology, but this was a very small group.
Secondary endpoints
The median OS was not reached in the ibrutinib arm but was 21.3 months in the temsirolimus arm.
This difference was not statistically significant, but Dr Rule noted that the trial was not powered for OS, and the analysis is confounded by the crossover. Twenty-three percent of patients in the temsirolimus arm ultimately received ibrutinib.
The overall response rate (ORR) was 71.9% in the ibrutinib arm and 40.4% in the temsirolimus arm (P<0.0001), according to the independent review committee. The complete response rates were 18.7% (n=26) and 1.4% (n=2), respectively.
The median duration of response was not reached with ibrutinib but was 7 months for temsirolimus. The median time to next treatment was not reached with ibrutinib, but it was 11.6 months in the temsirolimus arm (P<0.0001).
And the median duration of study treatment was 14.4 months in the ibrutinib arm and 3 months in the temsirolimus arm.
Timing counts
Dr Rule also presented response and PFS data according to the number of prior therapies patients received.
He noted that patients were more likely to respond to temsirolimus if they had received fewer prior therapies, but this was not the case with ibrutinib. Ibrutinib produced consistent ORRs regardless of when it was given.
In the ibrutinib arm, the ORR was 71.9% for patients who had received 1 prior line of therapy, 68.4% for those who received 2 prior therapies, and 75% for those who received 3 prior therapies. In the temsirolimus arm, the ORRs were 48%, 39.5%, and 33.3%, respectively.
Conversely, patients had a greater PFS benefit if they received ibrutinib earlier in their treatment course, but this was not true for temsirolimus.
At the median follow-up of 20 months, PFS was more than 60% for ibrutinib-treated patients who had received 1 prior line of therapy and less than 30% for ibrutinib-treated patients who received 2 or more prior lines of therapy. PFS was less than 15% for patients in the temsirolimus arm, regardless of their number of prior therapies.
“So that’s perhaps the first hint that, if we’re going to be using [ibrutinib], we should be using it earlier on,” Dr Rule said. “And I also suspect that, with further follow-up with this study, if this holds up, there will be, indeed, a survival benefit observed.”
Safety
“Despite patients on the ibrutinib arm being exposed to drug more than 4 times longer than those with temsirolimus, the frequency of most cumulative adverse events was lower in the ibrutinib arm,” Dr Rule said.
Still, he noted that most patients had some adverse events. And grade 3 or higher adverse events were reported in 67.6% of patients on ibrutinib and 87.1% of patients on temsirolimus.
Grade 3 or higher AEs included atrial fibrillation (AFib) and major bleeding. AFib occurred in 4.3% of patients in the ibrutinib arm and 1.4% in the temsirolimus arm. Major bleeding occurred in 10.1% and 6.5%, respectively.
Five of the 6 patients with AFib in the ibrutinib arm and all 3 patients who developed AFib in the temsirolimus arm had risk factors for AFib prior to treatment. None of these patients discontinued treatment due to AFib.
Dr Rule said there was no evidence to suggest that either drug increases the risk of second primary malignancies, although 3.6% of patients in the ibrutinib arm and 2.9% in the temsirolimus arm were diagnosed with second primary malignancies (mostly non-melanoma skin cancers).
The most common treatment-emergent AEs (≥20%) of any grade for the ibrutinib arm were diarrhea (28.8%), cough (22.3%), and fatigue (22.3%).
The most common treatment-emergent AEs (>20%) of any grade for the temsirolimus arm were thrombocytopenia (56.1%), anemia (43.2%), diarrhea (30.9%), fatigue (28.8%), neutropenia (25.9%), epistaxis (23.7%), cough (22.3%), peripheral edema (22.3%), nausea (21.6%), pyrexia (20.9%), and stomatitis (20.9%).
The most common hematologic AEs (≥10%) in the ibrutinib and temsirolimus arms, respectively, were thrombocytopenia (18% vs 56.1%), anemia (18% vs 43.2%), and neutropenia (15.8% vs 25.9%).
Six percent of patients in the ibrutinib arm and 26% in the temsirolimus arm discontinued treatment due to AEs.
At a median follow-up of 20 months, 42% of patients in the ibrutinib arm and 45% in the temsirolimus arm had died. The most common cause of death associated with ibrutinib was disease progression, and deaths in the temsirolimus arm were primarily attributed to AEs. ![]()
Trial of ofatumumab in FL stopped early

Photo courtesy of GSK
Genmab A/S said it is stopping a phase 3 trial of ofatumumab in follicular lymphoma (FL) after a planned interim analysis suggested the drug was unlikely to demonstrate superiority over rituximab.
The trial was designed to compare these 2 drugs as single-agent treatment in FL patients who had relapsed at least 6 months after completing treatment with a rituximab-containing regimen.
An interim analysis performed by an independent data monitoring committee indicated that, if the trial was to be completed as planned, it was unlikely that ofatumumab would improve progression-free survival (PFS) when compared to rituximab.
Genmab noted that this analysis did not reveal any new safety signals associated with ofatumumab, and no other ongoing trials of ofatumumab will be affected by the results of this analysis.
“The outcome of the interim analysis in this study is disappointing, as we had hoped to see superiority of ofatumumab,” said Jan van de Winkel, PhD, chief executive officer of Genmab. “The data from the study will now be prepared so that it can be presented at a future scientific conference.”
The goal of the study was to randomize up to 516 patients to receive ofatumumab (at 1000 mg) or rituximab (at 375 mg/m2) by intravenous infusion for 4 weekly doses.
Patients who had stable or responsive disease would then receive single infusions of ofatumumab or rituximab every 2 months for 4 additional doses—a total of 8 doses over 9 months. The primary endpoint of the study was PFS.
Past disappointments
This is not the first time ofatumumab has fallen short of expectations. Last year, the drug failed to meet the primary endpoint in two phase 3 trials.
In the OMB114242 trial, ofatumumab failed to improve PFS when compared to physicians’ choice in patients with bulky, fludarabine-refractory chronic lymphocytic leukemia (CLL).
In the ORCHARRD trial, ofatumumab plus chemotherapy failed to improve PFS when compared to rituximab plus chemotherapy in patients with relapsed or refractory diffuse large B-cell lymphoma.
About ofatumumab
Ofatumumab is a human monoclonal antibody designed to target the CD20 molecule found on the surface of CLL cells and normal B lymphocytes.
In the US, ofatumumab is approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
In the European Union (EU), ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat patients with CLL who have not received prior therapy and who are not eligible for fludarabine-based therapy.
In more than 50 countries worldwide, including the US and EU member countries, ofatumumab is approved as monotherapy for the treatment of patients with CLL who are refractory after prior treatment with fludarabine and alemtuzumab.
Ofatumumab is marketed as Arzerra under a collaboration agreement between Genmab and Novartis (formerly GSK). ![]()

Photo courtesy of GSK
Genmab A/S said it is stopping a phase 3 trial of ofatumumab in follicular lymphoma (FL) after a planned interim analysis suggested the drug was unlikely to demonstrate superiority over rituximab.
The trial was designed to compare these 2 drugs as single-agent treatment in FL patients who had relapsed at least 6 months after completing treatment with a rituximab-containing regimen.
An interim analysis performed by an independent data monitoring committee indicated that, if the trial was to be completed as planned, it was unlikely that ofatumumab would improve progression-free survival (PFS) when compared to rituximab.
Genmab noted that this analysis did not reveal any new safety signals associated with ofatumumab, and no other ongoing trials of ofatumumab will be affected by the results of this analysis.
“The outcome of the interim analysis in this study is disappointing, as we had hoped to see superiority of ofatumumab,” said Jan van de Winkel, PhD, chief executive officer of Genmab. “The data from the study will now be prepared so that it can be presented at a future scientific conference.”
The goal of the study was to randomize up to 516 patients to receive ofatumumab (at 1000 mg) or rituximab (at 375 mg/m2) by intravenous infusion for 4 weekly doses.
Patients who had stable or responsive disease would then receive single infusions of ofatumumab or rituximab every 2 months for 4 additional doses—a total of 8 doses over 9 months. The primary endpoint of the study was PFS.
Past disappointments
This is not the first time ofatumumab has fallen short of expectations. Last year, the drug failed to meet the primary endpoint in two phase 3 trials.
In the OMB114242 trial, ofatumumab failed to improve PFS when compared to physicians’ choice in patients with bulky, fludarabine-refractory chronic lymphocytic leukemia (CLL).
In the ORCHARRD trial, ofatumumab plus chemotherapy failed to improve PFS when compared to rituximab plus chemotherapy in patients with relapsed or refractory diffuse large B-cell lymphoma.
About ofatumumab
Ofatumumab is a human monoclonal antibody designed to target the CD20 molecule found on the surface of CLL cells and normal B lymphocytes.
In the US, ofatumumab is approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
In the European Union (EU), ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat patients with CLL who have not received prior therapy and who are not eligible for fludarabine-based therapy.
In more than 50 countries worldwide, including the US and EU member countries, ofatumumab is approved as monotherapy for the treatment of patients with CLL who are refractory after prior treatment with fludarabine and alemtuzumab.
Ofatumumab is marketed as Arzerra under a collaboration agreement between Genmab and Novartis (formerly GSK). ![]()

Photo courtesy of GSK
Genmab A/S said it is stopping a phase 3 trial of ofatumumab in follicular lymphoma (FL) after a planned interim analysis suggested the drug was unlikely to demonstrate superiority over rituximab.
The trial was designed to compare these 2 drugs as single-agent treatment in FL patients who had relapsed at least 6 months after completing treatment with a rituximab-containing regimen.
An interim analysis performed by an independent data monitoring committee indicated that, if the trial was to be completed as planned, it was unlikely that ofatumumab would improve progression-free survival (PFS) when compared to rituximab.
Genmab noted that this analysis did not reveal any new safety signals associated with ofatumumab, and no other ongoing trials of ofatumumab will be affected by the results of this analysis.
“The outcome of the interim analysis in this study is disappointing, as we had hoped to see superiority of ofatumumab,” said Jan van de Winkel, PhD, chief executive officer of Genmab. “The data from the study will now be prepared so that it can be presented at a future scientific conference.”
The goal of the study was to randomize up to 516 patients to receive ofatumumab (at 1000 mg) or rituximab (at 375 mg/m2) by intravenous infusion for 4 weekly doses.
Patients who had stable or responsive disease would then receive single infusions of ofatumumab or rituximab every 2 months for 4 additional doses—a total of 8 doses over 9 months. The primary endpoint of the study was PFS.
Past disappointments
This is not the first time ofatumumab has fallen short of expectations. Last year, the drug failed to meet the primary endpoint in two phase 3 trials.
In the OMB114242 trial, ofatumumab failed to improve PFS when compared to physicians’ choice in patients with bulky, fludarabine-refractory chronic lymphocytic leukemia (CLL).
In the ORCHARRD trial, ofatumumab plus chemotherapy failed to improve PFS when compared to rituximab plus chemotherapy in patients with relapsed or refractory diffuse large B-cell lymphoma.
About ofatumumab
Ofatumumab is a human monoclonal antibody designed to target the CD20 molecule found on the surface of CLL cells and normal B lymphocytes.
In the US, ofatumumab is approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
In the European Union (EU), ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat patients with CLL who have not received prior therapy and who are not eligible for fludarabine-based therapy.
In more than 50 countries worldwide, including the US and EU member countries, ofatumumab is approved as monotherapy for the treatment of patients with CLL who are refractory after prior treatment with fludarabine and alemtuzumab.
Ofatumumab is marketed as Arzerra under a collaboration agreement between Genmab and Novartis (formerly GSK).
ESRD treatments linked to different cancers

Photo by Anna Frodesiak
Patients with end-stage renal disease (ESRD) may have different cancer risks according to the treatment they are receiving, a new study suggests.
Researchers found that patients had a higher risk of developing infection-related and immune-related cancers—including Hodgkin and non-Hodgkin lymphoma (NHL)—after receiving a kidney transplant.
But patients had a higher risk of ESRD-related cancers when they were on dialysis.
Elizabeth Yanik, PhD, of the National Cancer Institute in Bethesda, Maryland, and her colleagues reported these results in the Journal of the American Society of Nephrology.
The researchers theorized that assessing patterns in ESRD patients across periods of dialysis and kidney transplant might inform cancer etiology.
So the team studied registry data on 202,195 kidney transplant candidates and recipients, comparing the incidence of cancers during kidney function intervals (time with a transplant) to the incidence during nonfunction intervals (waitlist or time after transplant failure [dialysis]). The analysis was adjusted for demographic characteristics.
Results showed the incidence of infection-related and immune-related cancers was higher during kidney function intervals than nonfunction intervals.
Cancers with a significantly higher incidence included Kaposi’s sarcoma (hazard ratio [HR]=9.1, P<0.001), NHL (HR=3.2, P<0.001), Hodgkin lymphoma (HR=3.0, P<0.001), lip cancer (HR=3.4, P<0.001), nonepithelial skin cancers (HR=3.8, P<0.001), melanoma (HR=1.9, P<0.001), prostate cancer (HR=1.2, P=0.003), anal cancer (HR=1.8, P=0.01), other genital cancers (HR=1.5, P=0.03), lung cancer (HR=1.3 P<0.001), and pancreatic cancer (HR=1.5, P=0.004).
Dr Yanik and her colleagues noted that, of these cancers, NHL, anal cancer, lung cancer, melanoma, nonepithelial skin cancers, and pancreatic cancer consistently increased in incidence with each transition to a kidney function interval and decreased with each transition to a nonfunction interval.
And the 2 types of transitions were significant for NHL, lung cancer, melanoma, nonepithelial skin cancers, and pancreatic cancer.
The researchers also identified cancers with a significantly lower incidence during kidney function intervals. This included kidney cancer (HR=0.77, P<0.001), thyroid cancer (HR=0.67, P<0.001), breast cancer (HR=0.81, P=0.002), and liver cancer (HR=0.59, P=0.001).
The team noted that, among cancers with a lower incidence during kidney function intervals, kidney cancer, thyroid cancer, and myeloma consistently decreased in incidence with each transition to a kidney function interval and increased in incidence with each transition to a nonfunction interval. But both transitions were only significant for kidney and thyroid cancers.
“Our study indicates that the needs of individuals with end-stage renal disease, in terms of cancer prevention and cancer screening, will likely differ over time,” Dr Yanik said.
“Vigilance for kidney cancer and thyroid cancer may be of particular importance while these individuals are on dialysis. Extra consideration for screening for melanoma or lung cancer may be called for while taking immunosuppressant medications following a kidney transplant.”

Photo by Anna Frodesiak
Patients with end-stage renal disease (ESRD) may have different cancer risks according to the treatment they are receiving, a new study suggests.
Researchers found that patients had a higher risk of developing infection-related and immune-related cancers—including Hodgkin and non-Hodgkin lymphoma (NHL)—after receiving a kidney transplant.
But patients had a higher risk of ESRD-related cancers when they were on dialysis.
Elizabeth Yanik, PhD, of the National Cancer Institute in Bethesda, Maryland, and her colleagues reported these results in the Journal of the American Society of Nephrology.
The researchers theorized that assessing patterns in ESRD patients across periods of dialysis and kidney transplant might inform cancer etiology.
So the team studied registry data on 202,195 kidney transplant candidates and recipients, comparing the incidence of cancers during kidney function intervals (time with a transplant) to the incidence during nonfunction intervals (waitlist or time after transplant failure [dialysis]). The analysis was adjusted for demographic characteristics.
Results showed the incidence of infection-related and immune-related cancers was higher during kidney function intervals than nonfunction intervals.
Cancers with a significantly higher incidence included Kaposi’s sarcoma (hazard ratio [HR]=9.1, P<0.001), NHL (HR=3.2, P<0.001), Hodgkin lymphoma (HR=3.0, P<0.001), lip cancer (HR=3.4, P<0.001), nonepithelial skin cancers (HR=3.8, P<0.001), melanoma (HR=1.9, P<0.001), prostate cancer (HR=1.2, P=0.003), anal cancer (HR=1.8, P=0.01), other genital cancers (HR=1.5, P=0.03), lung cancer (HR=1.3 P<0.001), and pancreatic cancer (HR=1.5, P=0.004).
Dr Yanik and her colleagues noted that, of these cancers, NHL, anal cancer, lung cancer, melanoma, nonepithelial skin cancers, and pancreatic cancer consistently increased in incidence with each transition to a kidney function interval and decreased with each transition to a nonfunction interval.
And the 2 types of transitions were significant for NHL, lung cancer, melanoma, nonepithelial skin cancers, and pancreatic cancer.
The researchers also identified cancers with a significantly lower incidence during kidney function intervals. This included kidney cancer (HR=0.77, P<0.001), thyroid cancer (HR=0.67, P<0.001), breast cancer (HR=0.81, P=0.002), and liver cancer (HR=0.59, P=0.001).
The team noted that, among cancers with a lower incidence during kidney function intervals, kidney cancer, thyroid cancer, and myeloma consistently decreased in incidence with each transition to a kidney function interval and increased in incidence with each transition to a nonfunction interval. But both transitions were only significant for kidney and thyroid cancers.
“Our study indicates that the needs of individuals with end-stage renal disease, in terms of cancer prevention and cancer screening, will likely differ over time,” Dr Yanik said.
“Vigilance for kidney cancer and thyroid cancer may be of particular importance while these individuals are on dialysis. Extra consideration for screening for melanoma or lung cancer may be called for while taking immunosuppressant medications following a kidney transplant.”

Photo by Anna Frodesiak
Patients with end-stage renal disease (ESRD) may have different cancer risks according to the treatment they are receiving, a new study suggests.
Researchers found that patients had a higher risk of developing infection-related and immune-related cancers—including Hodgkin and non-Hodgkin lymphoma (NHL)—after receiving a kidney transplant.
But patients had a higher risk of ESRD-related cancers when they were on dialysis.
Elizabeth Yanik, PhD, of the National Cancer Institute in Bethesda, Maryland, and her colleagues reported these results in the Journal of the American Society of Nephrology.
The researchers theorized that assessing patterns in ESRD patients across periods of dialysis and kidney transplant might inform cancer etiology.
So the team studied registry data on 202,195 kidney transplant candidates and recipients, comparing the incidence of cancers during kidney function intervals (time with a transplant) to the incidence during nonfunction intervals (waitlist or time after transplant failure [dialysis]). The analysis was adjusted for demographic characteristics.
Results showed the incidence of infection-related and immune-related cancers was higher during kidney function intervals than nonfunction intervals.
Cancers with a significantly higher incidence included Kaposi’s sarcoma (hazard ratio [HR]=9.1, P<0.001), NHL (HR=3.2, P<0.001), Hodgkin lymphoma (HR=3.0, P<0.001), lip cancer (HR=3.4, P<0.001), nonepithelial skin cancers (HR=3.8, P<0.001), melanoma (HR=1.9, P<0.001), prostate cancer (HR=1.2, P=0.003), anal cancer (HR=1.8, P=0.01), other genital cancers (HR=1.5, P=0.03), lung cancer (HR=1.3 P<0.001), and pancreatic cancer (HR=1.5, P=0.004).
Dr Yanik and her colleagues noted that, of these cancers, NHL, anal cancer, lung cancer, melanoma, nonepithelial skin cancers, and pancreatic cancer consistently increased in incidence with each transition to a kidney function interval and decreased with each transition to a nonfunction interval.
And the 2 types of transitions were significant for NHL, lung cancer, melanoma, nonepithelial skin cancers, and pancreatic cancer.
The researchers also identified cancers with a significantly lower incidence during kidney function intervals. This included kidney cancer (HR=0.77, P<0.001), thyroid cancer (HR=0.67, P<0.001), breast cancer (HR=0.81, P=0.002), and liver cancer (HR=0.59, P=0.001).
The team noted that, among cancers with a lower incidence during kidney function intervals, kidney cancer, thyroid cancer, and myeloma consistently decreased in incidence with each transition to a kidney function interval and increased in incidence with each transition to a nonfunction interval. But both transitions were only significant for kidney and thyroid cancers.
“Our study indicates that the needs of individuals with end-stage renal disease, in terms of cancer prevention and cancer screening, will likely differ over time,” Dr Yanik said.
“Vigilance for kidney cancer and thyroid cancer may be of particular importance while these individuals are on dialysis. Extra consideration for screening for melanoma or lung cancer may be called for while taking immunosuppressant medications following a kidney transplant.”
Inhibitor exhibits ‘modest’ activity in lymphoma
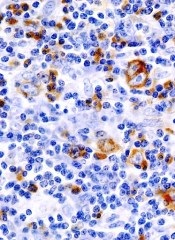
A small-molecule inhibitor has shown modest anticancer activity in a phase 1 trial of patients with relapsed/refractory lymphoma or multiple myeloma (MM), according to an investigator involved in the study.
A majority of patients who recieved the drug, pevonedistat, achieved stable disease, and a few patients with lymphoma experienced partial responses.
Investigators said pevonedistat could be given safely, although 100% of patients experienced adverse events (AEs), and a majority experienced grade 3 or higher AEs.
“The most important findings from our study are that pevonedistat hits its target in cancer cells in patients, can be given safely, and has modest activity in heavily pretreated patients with relapsed/refractory lymphoma, suggesting that we are on the right path,” said Jatin J. Shah, MD, of The University of Texas MD Anderson Cancer Center in Houston.
Dr Shah and his colleagues reported these findings in Clinical Cancer Research. The trial was sponsored by Millennium Pharmaceuticals, Inc., the company developing pevonedistat.
Pevonedistat is a first-in-class, investigational, small-molecule inhibitor of the NEDD8-activating enzyme.
“This enzyme is part of the ubiquitin-proteasome system, which is the target of a number of FDA-approved anticancer therapeutics, including bortezomib . . . ,” Dr Shah explained. “Pevonedistat also alters the ability of cancer cells to repair damaged DNA.”
Patient and treatment characteristics
Dr Shah and his colleagues enrolled 44 patients on this trial. Seventeen patients had relapsed/refractory MM, and 27 had relapsed/refractory lymphoma.
The types of lymphoma were diffuse large B-cell lymphoma (n=10), follicular lymphoma (n=5), Hodgkin lymphoma (n=5), small lymphocytic lymphoma/chronic lymphocytic leukemia (n=2), mantle cell lymphoma (n=1), lymphoplasmacytic lymphoma (n=1), peripheral T-cell lymphoma (n=1), splenic marginal zone B-cell lymphoma (n=1), and “other” (n=1).
Twenty-seven patients received escalating doses of pevonedistat on schedule A, which was days 1, 2, 8, and 9 of a 21-day cycle, and 17 patients received escalating doses of the drug on schedule B, which was days 1, 4, 8, and 11 of a 21-day cycle.
Safety
The maximum tolerated doses were 110 mg/m2 and 196 mg/m2 on schedule A and B, respectively. The dose-limiting toxicities were febrile neutropenia, transaminase elevations, and muscle cramps on schedule A, and thrombocytopenia on schedule B.
On schedule A, 100% of patients experienced AEs, and 59% had AEs of grade 3 or higher. The grade 3 or higher AEs were anemia (19%), thrombocytopenia (4%), neutropenia (7%), fatigue (7%), ALT increase (4%), AST increase (7%), diarrhea (4%), pain (4%), dyspnea (4%), hypercalcemia (7%), hypophosphatemia (11%), hyperkalemia (4%), muscle spasms (4%), abdominal discomfort (4%), and pneumonia (4%).
On schedule B, 100% of patients experienced AEs, and 71% had grade 3 or higher AEs. The grade 3 or higher AEs were anemia (6%), thrombocytopenia (6%), neutropenia (12%), fatigue (6%), ALT increase (6%), pyrexia (6%), pain (6%), dyspnea (6%), hypophosphatemia (6%), muscle spasms (6%), upper respiratory tract infection (6%), dehydration (6%), hyperbilirubinemia (6%), and pneumonia (12%).
Efficacy
Three patients had a partial response to treatment, including 1 patient with relapsed nodular sclerosis Hodgkin lymphoma, 1 with relapsed diffuse large B-cell lymphoma, and 1 with relapsed peripheral T-cell lymphoma.
Another 30 patients, 17 with lymphoma and 13 with MM, had stable disease.
“Although pevonedistat had modest activity as a single-agent treatment, we expect greater activity when it is given in combination with standard therapy,” Dr Shah said.
“The pharmacodynamics data showed that pevonedistat hit its target in cancer cells in patients at low doses. This is important because it may mean that we do not need to escalate the dose in future trials to increase anticancer activity. This has the potential to increase the risk-benefit ratio of pevonedistat.”
Dr Shah said a limitation of this study is that it included a small number of patients, all of whom were very heavily pretreated, which may limit assessment of how active pevonedistat could be.
A small-molecule inhibitor has shown modest anticancer activity in a phase 1 trial of patients with relapsed/refractory lymphoma or multiple myeloma (MM), according to an investigator involved in the study.
A majority of patients who recieved the drug, pevonedistat, achieved stable disease, and a few patients with lymphoma experienced partial responses.
Investigators said pevonedistat could be given safely, although 100% of patients experienced adverse events (AEs), and a majority experienced grade 3 or higher AEs.
“The most important findings from our study are that pevonedistat hits its target in cancer cells in patients, can be given safely, and has modest activity in heavily pretreated patients with relapsed/refractory lymphoma, suggesting that we are on the right path,” said Jatin J. Shah, MD, of The University of Texas MD Anderson Cancer Center in Houston.
Dr Shah and his colleagues reported these findings in Clinical Cancer Research. The trial was sponsored by Millennium Pharmaceuticals, Inc., the company developing pevonedistat.
Pevonedistat is a first-in-class, investigational, small-molecule inhibitor of the NEDD8-activating enzyme.
“This enzyme is part of the ubiquitin-proteasome system, which is the target of a number of FDA-approved anticancer therapeutics, including bortezomib . . . ,” Dr Shah explained. “Pevonedistat also alters the ability of cancer cells to repair damaged DNA.”
Patient and treatment characteristics
Dr Shah and his colleagues enrolled 44 patients on this trial. Seventeen patients had relapsed/refractory MM, and 27 had relapsed/refractory lymphoma.
The types of lymphoma were diffuse large B-cell lymphoma (n=10), follicular lymphoma (n=5), Hodgkin lymphoma (n=5), small lymphocytic lymphoma/chronic lymphocytic leukemia (n=2), mantle cell lymphoma (n=1), lymphoplasmacytic lymphoma (n=1), peripheral T-cell lymphoma (n=1), splenic marginal zone B-cell lymphoma (n=1), and “other” (n=1).
Twenty-seven patients received escalating doses of pevonedistat on schedule A, which was days 1, 2, 8, and 9 of a 21-day cycle, and 17 patients received escalating doses of the drug on schedule B, which was days 1, 4, 8, and 11 of a 21-day cycle.
Safety
The maximum tolerated doses were 110 mg/m2 and 196 mg/m2 on schedule A and B, respectively. The dose-limiting toxicities were febrile neutropenia, transaminase elevations, and muscle cramps on schedule A, and thrombocytopenia on schedule B.
On schedule A, 100% of patients experienced AEs, and 59% had AEs of grade 3 or higher. The grade 3 or higher AEs were anemia (19%), thrombocytopenia (4%), neutropenia (7%), fatigue (7%), ALT increase (4%), AST increase (7%), diarrhea (4%), pain (4%), dyspnea (4%), hypercalcemia (7%), hypophosphatemia (11%), hyperkalemia (4%), muscle spasms (4%), abdominal discomfort (4%), and pneumonia (4%).
On schedule B, 100% of patients experienced AEs, and 71% had grade 3 or higher AEs. The grade 3 or higher AEs were anemia (6%), thrombocytopenia (6%), neutropenia (12%), fatigue (6%), ALT increase (6%), pyrexia (6%), pain (6%), dyspnea (6%), hypophosphatemia (6%), muscle spasms (6%), upper respiratory tract infection (6%), dehydration (6%), hyperbilirubinemia (6%), and pneumonia (12%).
Efficacy
Three patients had a partial response to treatment, including 1 patient with relapsed nodular sclerosis Hodgkin lymphoma, 1 with relapsed diffuse large B-cell lymphoma, and 1 with relapsed peripheral T-cell lymphoma.
Another 30 patients, 17 with lymphoma and 13 with MM, had stable disease.
“Although pevonedistat had modest activity as a single-agent treatment, we expect greater activity when it is given in combination with standard therapy,” Dr Shah said.
“The pharmacodynamics data showed that pevonedistat hit its target in cancer cells in patients at low doses. This is important because it may mean that we do not need to escalate the dose in future trials to increase anticancer activity. This has the potential to increase the risk-benefit ratio of pevonedistat.”
Dr Shah said a limitation of this study is that it included a small number of patients, all of whom were very heavily pretreated, which may limit assessment of how active pevonedistat could be.
A small-molecule inhibitor has shown modest anticancer activity in a phase 1 trial of patients with relapsed/refractory lymphoma or multiple myeloma (MM), according to an investigator involved in the study.
A majority of patients who recieved the drug, pevonedistat, achieved stable disease, and a few patients with lymphoma experienced partial responses.
Investigators said pevonedistat could be given safely, although 100% of patients experienced adverse events (AEs), and a majority experienced grade 3 or higher AEs.
“The most important findings from our study are that pevonedistat hits its target in cancer cells in patients, can be given safely, and has modest activity in heavily pretreated patients with relapsed/refractory lymphoma, suggesting that we are on the right path,” said Jatin J. Shah, MD, of The University of Texas MD Anderson Cancer Center in Houston.
Dr Shah and his colleagues reported these findings in Clinical Cancer Research. The trial was sponsored by Millennium Pharmaceuticals, Inc., the company developing pevonedistat.
Pevonedistat is a first-in-class, investigational, small-molecule inhibitor of the NEDD8-activating enzyme.
“This enzyme is part of the ubiquitin-proteasome system, which is the target of a number of FDA-approved anticancer therapeutics, including bortezomib . . . ,” Dr Shah explained. “Pevonedistat also alters the ability of cancer cells to repair damaged DNA.”
Patient and treatment characteristics
Dr Shah and his colleagues enrolled 44 patients on this trial. Seventeen patients had relapsed/refractory MM, and 27 had relapsed/refractory lymphoma.
The types of lymphoma were diffuse large B-cell lymphoma (n=10), follicular lymphoma (n=5), Hodgkin lymphoma (n=5), small lymphocytic lymphoma/chronic lymphocytic leukemia (n=2), mantle cell lymphoma (n=1), lymphoplasmacytic lymphoma (n=1), peripheral T-cell lymphoma (n=1), splenic marginal zone B-cell lymphoma (n=1), and “other” (n=1).
Twenty-seven patients received escalating doses of pevonedistat on schedule A, which was days 1, 2, 8, and 9 of a 21-day cycle, and 17 patients received escalating doses of the drug on schedule B, which was days 1, 4, 8, and 11 of a 21-day cycle.
Safety
The maximum tolerated doses were 110 mg/m2 and 196 mg/m2 on schedule A and B, respectively. The dose-limiting toxicities were febrile neutropenia, transaminase elevations, and muscle cramps on schedule A, and thrombocytopenia on schedule B.
On schedule A, 100% of patients experienced AEs, and 59% had AEs of grade 3 or higher. The grade 3 or higher AEs were anemia (19%), thrombocytopenia (4%), neutropenia (7%), fatigue (7%), ALT increase (4%), AST increase (7%), diarrhea (4%), pain (4%), dyspnea (4%), hypercalcemia (7%), hypophosphatemia (11%), hyperkalemia (4%), muscle spasms (4%), abdominal discomfort (4%), and pneumonia (4%).
On schedule B, 100% of patients experienced AEs, and 71% had grade 3 or higher AEs. The grade 3 or higher AEs were anemia (6%), thrombocytopenia (6%), neutropenia (12%), fatigue (6%), ALT increase (6%), pyrexia (6%), pain (6%), dyspnea (6%), hypophosphatemia (6%), muscle spasms (6%), upper respiratory tract infection (6%), dehydration (6%), hyperbilirubinemia (6%), and pneumonia (12%).
Efficacy
Three patients had a partial response to treatment, including 1 patient with relapsed nodular sclerosis Hodgkin lymphoma, 1 with relapsed diffuse large B-cell lymphoma, and 1 with relapsed peripheral T-cell lymphoma.
Another 30 patients, 17 with lymphoma and 13 with MM, had stable disease.
“Although pevonedistat had modest activity as a single-agent treatment, we expect greater activity when it is given in combination with standard therapy,” Dr Shah said.
“The pharmacodynamics data showed that pevonedistat hit its target in cancer cells in patients at low doses. This is important because it may mean that we do not need to escalate the dose in future trials to increase anticancer activity. This has the potential to increase the risk-benefit ratio of pevonedistat.”
Dr Shah said a limitation of this study is that it included a small number of patients, all of whom were very heavily pretreated, which may limit assessment of how active pevonedistat could be.
Drug ‘life-changing’ for CLL patients in phase 1 trial

Photo courtesy of NIH
A novel Bruton’s tyrosine kinase inhibitor has proven life-changing for patients with chronic lymphocytic leukemia (CLL) who received the drug as part of a phase 1 trial, according to the study’s lead author.
The inhibitor, ONO/GS-4059, produced a response in 96% of evaluable CLL patients.
Most CLL patients are still on the study after 3 years, although a handful withdrew due to adverse events (AEs) or disease progression.
“These patients were confronted with a cruel reality: they had failed multiple chemotherapy lines, and there were no other treatment options available for them,” said lead study author Harriet Walter, MBChB, of the University of Leicester in the UK.
“This drug has changed their lives. From desperate and tired, they are now leading a normal and really active life. This is hugely rewarding and encouraging.”
Dr Walter and her colleagues reported these results in Blood. The trial was funded by ONO Pharmaceuticals, the company developing ONO/GS-4059.
This study opened in January 2012, and 90 patients were enrolled at centers in the UK and France. There were 28 patients with CLL and 62 with non-Hodgkin lymphoma (NHL), including 16 with mantle cell lymphoma (MCL) and 35 with diffuse large B-cell lymphoma (DLBCL).
The study also included patients with follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, and Waldenstrom’s macroglobulinemia, but patient numbers were small for these groups, so the results were not discussed in detail.
There were 9 dose-escalation cohorts in this study. ONO/GS-4059 was given once-daily at doses ranging from 20 mg to 600 mg. Or the drug was given twice daily at doses of 240 mg or 300 mg.
Results
The maximum tolerated dose was not reached in the CLL cohort, but it was 480 mg once-daily in the NHL cohort. Four NHL patients had a dose-limiting toxicity.
In the CLL cohort, 2 patients went off study due to progression and 5 due to AEs.
In the NHL cohort, 49 patients discontinued treatment, 32 due to progression and 5 due to dose-limiting toxicities or AEs. The other 12 NHL patients discontinued due to patient or investigator decision, proceeding to transplant (n=1), or death due to progressive disease.
The median duration of follow-up was 560 days for CLL patients, 309 days for MCL patients, and 60 days for DLBCL patients.
The overall estimated mean progression-free survival was 874 days for CLL patients, 341 days for MCL patients, and 54 days for DLBCL patients.
CLL patients
Of all 28 CLL patients, 16 had relapsed CLL, 11 had refractory disease, and 1 had unknown status. The median number of prior therapies was 3.5 (range, 2-7).
Twenty-five patients were evaluable. Of the 3 who were not evaluable, 1 had not reached cycle 3 disease assessment at the time of data analysis, 1 progressed during cycle 1, and 1 was withdrawn due to an AE (idiopathic thrombocytopenia).
Of the 25 evaluable patients, 24 (96%) responded to ONO/GS-4059. The researchers said they observed rapid resolution of bulky lymphadenopathy within the first 3 months of treatment, but improvement in lymphadenopathy continued for up to 18 months in most patients.
The median treatment duration for these patients is 80 weeks, and 21 patients are still on treatment. Two of the evaluable patients progressed during therapy, one at cycle 3 and one at cycle 12.
MCL patients
Of the 16 MCL patients enrolled, 7 were refractory to their last course of immuno-chemotherapy. The median number of prior therapies was 3 (range, 2-7).
Eleven of 12 (92%) evaluable patients with MCL responded to ONO/GS-4059. Six patients had a partial response, and 5 had a complete response (CR) or unconfirmed CR.
Three patients progressed after an initial response. Four patients were not evaluable because they progressed.
The median treatment duration for MCL patients is 40 weeks, and 8 patients remain on study.
DLBCL patients
All 35 DLBCL patients had relapsed or refractory disease. The median number of prior treatments was 3
(range, 2-10), and 30 patients were refractory to their last line of chemotherapy.
Eleven of 31 (35%) patients with non-germinal center B-cell (non-GCB) DLBCL responded to ONO/GS-4059. Two non-GCB DLBCL patients had a confirmed CR, 1 had an unconfirmed CR, and the rest had partial responses.
The median duration of response was 54 days. And, among responders, the median treatment duration was 12 weeks.
The majority of non-GCB DLBCL patients progressed. There were no responses among the 2 patients with GCB DLBCL, and there were no responses among patients with primary mediastinal B-cell lymphoma or plasmablastic DLBCL.
Toxicity
AEs in this study were mostly grade 1/2—75% in the CLL cohort and 50% in the NHL cohort. However, treatment-related grade 3/4 AEs occurred in 14.3% of CLL patients and 16.1% of NHL patients.
Grade 3/4 events were mainly hematologic in nature and included neutropenia (10%), anemia (13.3%), and thrombocytopenia (13.3%).
There was a grade 3 episode of drug-related hemorrhage in a CLL patient, which resulted in a psoas hematoma (with concomitant CLL progression) in the presence of a normal platelet count. This patient was among those taken off the study.
“The next step is now to see how best we can improve on these outstanding results,” said study author Martin Dyer, DPhil, of the University of Leicester.
“A further study using this drug in combination with additional targeted agents is shortly to open in Leicester with the aim of achieving cure. In parallel with the clinical development of the drug, our team of scientists at the Haematological Research Institute are studying how this drug is working and how to overcome potential resistance.”

Photo courtesy of NIH
A novel Bruton’s tyrosine kinase inhibitor has proven life-changing for patients with chronic lymphocytic leukemia (CLL) who received the drug as part of a phase 1 trial, according to the study’s lead author.
The inhibitor, ONO/GS-4059, produced a response in 96% of evaluable CLL patients.
Most CLL patients are still on the study after 3 years, although a handful withdrew due to adverse events (AEs) or disease progression.
“These patients were confronted with a cruel reality: they had failed multiple chemotherapy lines, and there were no other treatment options available for them,” said lead study author Harriet Walter, MBChB, of the University of Leicester in the UK.
“This drug has changed their lives. From desperate and tired, they are now leading a normal and really active life. This is hugely rewarding and encouraging.”
Dr Walter and her colleagues reported these results in Blood. The trial was funded by ONO Pharmaceuticals, the company developing ONO/GS-4059.
This study opened in January 2012, and 90 patients were enrolled at centers in the UK and France. There were 28 patients with CLL and 62 with non-Hodgkin lymphoma (NHL), including 16 with mantle cell lymphoma (MCL) and 35 with diffuse large B-cell lymphoma (DLBCL).
The study also included patients with follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, and Waldenstrom’s macroglobulinemia, but patient numbers were small for these groups, so the results were not discussed in detail.
There were 9 dose-escalation cohorts in this study. ONO/GS-4059 was given once-daily at doses ranging from 20 mg to 600 mg. Or the drug was given twice daily at doses of 240 mg or 300 mg.
Results
The maximum tolerated dose was not reached in the CLL cohort, but it was 480 mg once-daily in the NHL cohort. Four NHL patients had a dose-limiting toxicity.
In the CLL cohort, 2 patients went off study due to progression and 5 due to AEs.
In the NHL cohort, 49 patients discontinued treatment, 32 due to progression and 5 due to dose-limiting toxicities or AEs. The other 12 NHL patients discontinued due to patient or investigator decision, proceeding to transplant (n=1), or death due to progressive disease.
The median duration of follow-up was 560 days for CLL patients, 309 days for MCL patients, and 60 days for DLBCL patients.
The overall estimated mean progression-free survival was 874 days for CLL patients, 341 days for MCL patients, and 54 days for DLBCL patients.
CLL patients
Of all 28 CLL patients, 16 had relapsed CLL, 11 had refractory disease, and 1 had unknown status. The median number of prior therapies was 3.5 (range, 2-7).
Twenty-five patients were evaluable. Of the 3 who were not evaluable, 1 had not reached cycle 3 disease assessment at the time of data analysis, 1 progressed during cycle 1, and 1 was withdrawn due to an AE (idiopathic thrombocytopenia).
Of the 25 evaluable patients, 24 (96%) responded to ONO/GS-4059. The researchers said they observed rapid resolution of bulky lymphadenopathy within the first 3 months of treatment, but improvement in lymphadenopathy continued for up to 18 months in most patients.
The median treatment duration for these patients is 80 weeks, and 21 patients are still on treatment. Two of the evaluable patients progressed during therapy, one at cycle 3 and one at cycle 12.
MCL patients
Of the 16 MCL patients enrolled, 7 were refractory to their last course of immuno-chemotherapy. The median number of prior therapies was 3 (range, 2-7).
Eleven of 12 (92%) evaluable patients with MCL responded to ONO/GS-4059. Six patients had a partial response, and 5 had a complete response (CR) or unconfirmed CR.
Three patients progressed after an initial response. Four patients were not evaluable because they progressed.
The median treatment duration for MCL patients is 40 weeks, and 8 patients remain on study.
DLBCL patients
All 35 DLBCL patients had relapsed or refractory disease. The median number of prior treatments was 3
(range, 2-10), and 30 patients were refractory to their last line of chemotherapy.
Eleven of 31 (35%) patients with non-germinal center B-cell (non-GCB) DLBCL responded to ONO/GS-4059. Two non-GCB DLBCL patients had a confirmed CR, 1 had an unconfirmed CR, and the rest had partial responses.
The median duration of response was 54 days. And, among responders, the median treatment duration was 12 weeks.
The majority of non-GCB DLBCL patients progressed. There were no responses among the 2 patients with GCB DLBCL, and there were no responses among patients with primary mediastinal B-cell lymphoma or plasmablastic DLBCL.
Toxicity
AEs in this study were mostly grade 1/2—75% in the CLL cohort and 50% in the NHL cohort. However, treatment-related grade 3/4 AEs occurred in 14.3% of CLL patients and 16.1% of NHL patients.
Grade 3/4 events were mainly hematologic in nature and included neutropenia (10%), anemia (13.3%), and thrombocytopenia (13.3%).
There was a grade 3 episode of drug-related hemorrhage in a CLL patient, which resulted in a psoas hematoma (with concomitant CLL progression) in the presence of a normal platelet count. This patient was among those taken off the study.
“The next step is now to see how best we can improve on these outstanding results,” said study author Martin Dyer, DPhil, of the University of Leicester.
“A further study using this drug in combination with additional targeted agents is shortly to open in Leicester with the aim of achieving cure. In parallel with the clinical development of the drug, our team of scientists at the Haematological Research Institute are studying how this drug is working and how to overcome potential resistance.”

Photo courtesy of NIH
A novel Bruton’s tyrosine kinase inhibitor has proven life-changing for patients with chronic lymphocytic leukemia (CLL) who received the drug as part of a phase 1 trial, according to the study’s lead author.
The inhibitor, ONO/GS-4059, produced a response in 96% of evaluable CLL patients.
Most CLL patients are still on the study after 3 years, although a handful withdrew due to adverse events (AEs) or disease progression.
“These patients were confronted with a cruel reality: they had failed multiple chemotherapy lines, and there were no other treatment options available for them,” said lead study author Harriet Walter, MBChB, of the University of Leicester in the UK.
“This drug has changed their lives. From desperate and tired, they are now leading a normal and really active life. This is hugely rewarding and encouraging.”
Dr Walter and her colleagues reported these results in Blood. The trial was funded by ONO Pharmaceuticals, the company developing ONO/GS-4059.
This study opened in January 2012, and 90 patients were enrolled at centers in the UK and France. There were 28 patients with CLL and 62 with non-Hodgkin lymphoma (NHL), including 16 with mantle cell lymphoma (MCL) and 35 with diffuse large B-cell lymphoma (DLBCL).
The study also included patients with follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, and Waldenstrom’s macroglobulinemia, but patient numbers were small for these groups, so the results were not discussed in detail.
There were 9 dose-escalation cohorts in this study. ONO/GS-4059 was given once-daily at doses ranging from 20 mg to 600 mg. Or the drug was given twice daily at doses of 240 mg or 300 mg.
Results
The maximum tolerated dose was not reached in the CLL cohort, but it was 480 mg once-daily in the NHL cohort. Four NHL patients had a dose-limiting toxicity.
In the CLL cohort, 2 patients went off study due to progression and 5 due to AEs.
In the NHL cohort, 49 patients discontinued treatment, 32 due to progression and 5 due to dose-limiting toxicities or AEs. The other 12 NHL patients discontinued due to patient or investigator decision, proceeding to transplant (n=1), or death due to progressive disease.
The median duration of follow-up was 560 days for CLL patients, 309 days for MCL patients, and 60 days for DLBCL patients.
The overall estimated mean progression-free survival was 874 days for CLL patients, 341 days for MCL patients, and 54 days for DLBCL patients.
CLL patients
Of all 28 CLL patients, 16 had relapsed CLL, 11 had refractory disease, and 1 had unknown status. The median number of prior therapies was 3.5 (range, 2-7).
Twenty-five patients were evaluable. Of the 3 who were not evaluable, 1 had not reached cycle 3 disease assessment at the time of data analysis, 1 progressed during cycle 1, and 1 was withdrawn due to an AE (idiopathic thrombocytopenia).
Of the 25 evaluable patients, 24 (96%) responded to ONO/GS-4059. The researchers said they observed rapid resolution of bulky lymphadenopathy within the first 3 months of treatment, but improvement in lymphadenopathy continued for up to 18 months in most patients.
The median treatment duration for these patients is 80 weeks, and 21 patients are still on treatment. Two of the evaluable patients progressed during therapy, one at cycle 3 and one at cycle 12.
MCL patients
Of the 16 MCL patients enrolled, 7 were refractory to their last course of immuno-chemotherapy. The median number of prior therapies was 3 (range, 2-7).
Eleven of 12 (92%) evaluable patients with MCL responded to ONO/GS-4059. Six patients had a partial response, and 5 had a complete response (CR) or unconfirmed CR.
Three patients progressed after an initial response. Four patients were not evaluable because they progressed.
The median treatment duration for MCL patients is 40 weeks, and 8 patients remain on study.
DLBCL patients
All 35 DLBCL patients had relapsed or refractory disease. The median number of prior treatments was 3
(range, 2-10), and 30 patients were refractory to their last line of chemotherapy.
Eleven of 31 (35%) patients with non-germinal center B-cell (non-GCB) DLBCL responded to ONO/GS-4059. Two non-GCB DLBCL patients had a confirmed CR, 1 had an unconfirmed CR, and the rest had partial responses.
The median duration of response was 54 days. And, among responders, the median treatment duration was 12 weeks.
The majority of non-GCB DLBCL patients progressed. There were no responses among the 2 patients with GCB DLBCL, and there were no responses among patients with primary mediastinal B-cell lymphoma or plasmablastic DLBCL.
Toxicity
AEs in this study were mostly grade 1/2—75% in the CLL cohort and 50% in the NHL cohort. However, treatment-related grade 3/4 AEs occurred in 14.3% of CLL patients and 16.1% of NHL patients.
Grade 3/4 events were mainly hematologic in nature and included neutropenia (10%), anemia (13.3%), and thrombocytopenia (13.3%).
There was a grade 3 episode of drug-related hemorrhage in a CLL patient, which resulted in a psoas hematoma (with concomitant CLL progression) in the presence of a normal platelet count. This patient was among those taken off the study.
“The next step is now to see how best we can improve on these outstanding results,” said study author Martin Dyer, DPhil, of the University of Leicester.
“A further study using this drug in combination with additional targeted agents is shortly to open in Leicester with the aim of achieving cure. In parallel with the clinical development of the drug, our team of scientists at the Haematological Research Institute are studying how this drug is working and how to overcome potential resistance.”