User login
Cochrane Data: Food, Water in Labor OK in Low-Risk Women
Major Finding: In women at low risk of needing general anesthesia during childbirth, there was no significant association with eating and drinking during labor and the rate of cesarean section, operative vaginal birth, or Apgar scores of less than 7 at 5 minutes.
Data Source: A Cochrane database review of five randomized controlled trials comprising 3,130 women.
Disclosures: The review was sponsored by the University of the Witwatersrand and the University of Liverpool, as well as the National Institute for Health Research, and by a World Health Organization grant. One of the authors was the primary investigator on a study included in the review.
Women at low risk of complications during childbirth should be allowed to take food and water as they desire during active labor, a Cochrane database review has concluded.
“The review identified no benefits or harms of restricting foods and fluids during labor in women at low risk of needing anesthesia,” wrote lead author Mandisa Singata, R.N., and her associates. “Given these findings, women should be free to eat and drink in labor or not, as they wish” (Cochrane Database Syst. Rev. 2010;CD003930 [doi:10.1002/14651858.CD003930.pub2]).
The review of five studies comprising 3,130 women suggests that the prohibition on oral intake during labor may be based on outdated concerns, wrote Ms. Singata of the University of Witwatersrand, East London, South Africa, and her associates.
“Restricting oral food and fluid intake … is a strongly held obstetric and anesthetic tradition,” related to research performed in the 1940s on regurgitation under general anesthetic and resulting inhalation pneumonia. “Most [eating prohibitions] are based on historical, but important, concerns related to these risks. … The incidence is very rare with modern anesthetic techniques and the use of regional rather than general anesthesia.”
Ms. Singata and her colleagues identified five randomized controlled trials that examined this issue. The studies were conducted from 1999 to 2009.
All included women at low risk of requiring general anesthesia during childbirth. One study looked at restricting intake to ice chips and sips of water vs. full access to food and drink. Two compared water only to encouraging the consumption of some food and fluid, and two compared water only to carbohydrate drinks during labor.
The analysis was dominated by the largest and most recent study, which contained 2,443 women. The other four studies together comprised 687 women. The largest study was conducted in a “highly medicalized environment,” in which 30% of women had a cesarean section, over 50% had oxytocin, just under 70% received intravenous fluids and epidural anesthesia, and 27% underwent operative vaginal birth.
“In addition, 20% of the women in the water-only arm ate during labor and 295 in the food and fluid arm chose not to eat in labor. This clearly reflects the wide variation in women's wishes for food and fluids during labor,” the authors wrote.
When considering any restriction of food and fluid versus allowing them, the authors found no significant associations with the rate of cesarean section, operative vaginal birth, or Apgar scores of less than 7 at 5 minutes. Neither were there significant relationships with duration of labor, maternal nausea or vomiting, narcotic pain relief, or infant admission to intensive care.
None of the outcomes were significantly related in any of the other analyses: complete restriction of food and fluid vs. freedom to eat and drink, water only vs. freedom to eat and drink, or complete food and fluid restriction vs. carbohydrate-based fluid only.
Major Finding: In women at low risk of needing general anesthesia during childbirth, there was no significant association with eating and drinking during labor and the rate of cesarean section, operative vaginal birth, or Apgar scores of less than 7 at 5 minutes.
Data Source: A Cochrane database review of five randomized controlled trials comprising 3,130 women.
Disclosures: The review was sponsored by the University of the Witwatersrand and the University of Liverpool, as well as the National Institute for Health Research, and by a World Health Organization grant. One of the authors was the primary investigator on a study included in the review.
Women at low risk of complications during childbirth should be allowed to take food and water as they desire during active labor, a Cochrane database review has concluded.
“The review identified no benefits or harms of restricting foods and fluids during labor in women at low risk of needing anesthesia,” wrote lead author Mandisa Singata, R.N., and her associates. “Given these findings, women should be free to eat and drink in labor or not, as they wish” (Cochrane Database Syst. Rev. 2010;CD003930 [doi:10.1002/14651858.CD003930.pub2]).
The review of five studies comprising 3,130 women suggests that the prohibition on oral intake during labor may be based on outdated concerns, wrote Ms. Singata of the University of Witwatersrand, East London, South Africa, and her associates.
“Restricting oral food and fluid intake … is a strongly held obstetric and anesthetic tradition,” related to research performed in the 1940s on regurgitation under general anesthetic and resulting inhalation pneumonia. “Most [eating prohibitions] are based on historical, but important, concerns related to these risks. … The incidence is very rare with modern anesthetic techniques and the use of regional rather than general anesthesia.”
Ms. Singata and her colleagues identified five randomized controlled trials that examined this issue. The studies were conducted from 1999 to 2009.
All included women at low risk of requiring general anesthesia during childbirth. One study looked at restricting intake to ice chips and sips of water vs. full access to food and drink. Two compared water only to encouraging the consumption of some food and fluid, and two compared water only to carbohydrate drinks during labor.
The analysis was dominated by the largest and most recent study, which contained 2,443 women. The other four studies together comprised 687 women. The largest study was conducted in a “highly medicalized environment,” in which 30% of women had a cesarean section, over 50% had oxytocin, just under 70% received intravenous fluids and epidural anesthesia, and 27% underwent operative vaginal birth.
“In addition, 20% of the women in the water-only arm ate during labor and 295 in the food and fluid arm chose not to eat in labor. This clearly reflects the wide variation in women's wishes for food and fluids during labor,” the authors wrote.
When considering any restriction of food and fluid versus allowing them, the authors found no significant associations with the rate of cesarean section, operative vaginal birth, or Apgar scores of less than 7 at 5 minutes. Neither were there significant relationships with duration of labor, maternal nausea or vomiting, narcotic pain relief, or infant admission to intensive care.
None of the outcomes were significantly related in any of the other analyses: complete restriction of food and fluid vs. freedom to eat and drink, water only vs. freedom to eat and drink, or complete food and fluid restriction vs. carbohydrate-based fluid only.
Major Finding: In women at low risk of needing general anesthesia during childbirth, there was no significant association with eating and drinking during labor and the rate of cesarean section, operative vaginal birth, or Apgar scores of less than 7 at 5 minutes.
Data Source: A Cochrane database review of five randomized controlled trials comprising 3,130 women.
Disclosures: The review was sponsored by the University of the Witwatersrand and the University of Liverpool, as well as the National Institute for Health Research, and by a World Health Organization grant. One of the authors was the primary investigator on a study included in the review.
Women at low risk of complications during childbirth should be allowed to take food and water as they desire during active labor, a Cochrane database review has concluded.
“The review identified no benefits or harms of restricting foods and fluids during labor in women at low risk of needing anesthesia,” wrote lead author Mandisa Singata, R.N., and her associates. “Given these findings, women should be free to eat and drink in labor or not, as they wish” (Cochrane Database Syst. Rev. 2010;CD003930 [doi:10.1002/14651858.CD003930.pub2]).
The review of five studies comprising 3,130 women suggests that the prohibition on oral intake during labor may be based on outdated concerns, wrote Ms. Singata of the University of Witwatersrand, East London, South Africa, and her associates.
“Restricting oral food and fluid intake … is a strongly held obstetric and anesthetic tradition,” related to research performed in the 1940s on regurgitation under general anesthetic and resulting inhalation pneumonia. “Most [eating prohibitions] are based on historical, but important, concerns related to these risks. … The incidence is very rare with modern anesthetic techniques and the use of regional rather than general anesthesia.”
Ms. Singata and her colleagues identified five randomized controlled trials that examined this issue. The studies were conducted from 1999 to 2009.
All included women at low risk of requiring general anesthesia during childbirth. One study looked at restricting intake to ice chips and sips of water vs. full access to food and drink. Two compared water only to encouraging the consumption of some food and fluid, and two compared water only to carbohydrate drinks during labor.
The analysis was dominated by the largest and most recent study, which contained 2,443 women. The other four studies together comprised 687 women. The largest study was conducted in a “highly medicalized environment,” in which 30% of women had a cesarean section, over 50% had oxytocin, just under 70% received intravenous fluids and epidural anesthesia, and 27% underwent operative vaginal birth.
“In addition, 20% of the women in the water-only arm ate during labor and 295 in the food and fluid arm chose not to eat in labor. This clearly reflects the wide variation in women's wishes for food and fluids during labor,” the authors wrote.
When considering any restriction of food and fluid versus allowing them, the authors found no significant associations with the rate of cesarean section, operative vaginal birth, or Apgar scores of less than 7 at 5 minutes. Neither were there significant relationships with duration of labor, maternal nausea or vomiting, narcotic pain relief, or infant admission to intensive care.
None of the outcomes were significantly related in any of the other analyses: complete restriction of food and fluid vs. freedom to eat and drink, water only vs. freedom to eat and drink, or complete food and fluid restriction vs. carbohydrate-based fluid only.
Slight Uptick Seen in Teen Pregnancy Rates : Increase unlikely to be due solely to increase in abstinence-only sex education, experts say.
Major Finding: The rates of teen pregnancy, birth, and abortion increased in 2006 after declining every year since 1990.
Data Source: Data compiled from national-level and state-level sources.
Disclosures: Preparation of the report was funded by the Brush Foundation, the California Wellness Foundation, and the Annie E. Casey Foundation.
Teen pregnancy rates increased 3% in the United States in 2006 after declining every year since 1990, according to a report from the Guttmacher Institute.
In addition, teen births rose 4% and teen abortions rose 1% between 2005 and 2006, according to the report, which the institute compiled from a variety of national and state-level sources.
The teen pregnancy rate hit its peak in 1990, with 117 pregnancies per 1,000 women aged 15–19 years. By 2005 it had declined 40%, to 70/1,000. But in 2006, the rate increased to 72/1,000.
“After more than a decade of progress, this reversal is deeply troubling,” Heather Boonstra, a senior public policy associate at the Guttmacher Institute, said in a prepared statement. “It coincides with an increase in rigid abstinence-only-until-marriage programs, which received major funding boosts under the Bush administration. A strong body of research shows that these programs do not work. Fortunately, the heyday of this failed experiment has come to an end with the enactment of a new teen pregnancy prevention initiative that ensures that programs will be age appropriate, medically accurate, and, most importantly, based on research demonstrating their effectiveness.”
Two experts interviewed by this news organization weren't so sure that the increase in pregnancy rates could be attributed to abstinence-only sex education. “The temporal association between the increase in abstinence-only programs and the increase in the pregnancy rate definitely deserves closer attention,” said Dr. Lee Savio Beers, a pediatrician who is director of the healthy generations clinic at Children's National Medical Center, Washington, D.C. “I don't know that anyone knows for sure whether it's directly related, but the two kind of came together. It's such a multifactorial issue that we may never have an answer on that.”
Dr. Melissa Kottke, who is with the department of ob.gyn. at Emory University and is director of the Jane Fonda Center for Adolescent Reproductive Health, both in Atlanta, said, “I think there's going to be a lot of things contributing to [increases in teen pregnancy rates], and I don't think we're going to know what all of those are.”
Dr. Kottke listed some of the other possibilities: teenage sexual activity, poverty, the media, parenting, funding for care, and funding for family planning services. “All of those things are going to contribute,” she said, “and I don't think we're going to be able to point our finger at one thing or the other.”
About the Guttmacher Institute, Dr. Beers said, “They're a well-respected organization. Their policy views tend to be on the liberal side. But I think everyone pretty much agrees that their facts are good, and their numbers are good, and for pregnancy numbers, they're better than pretty much anyone.”
Although the long decline and recent uptick in teen pregnancy rates were seen in blacks, Hispanics, and non-Hispanic whites, there were some substantial racial and ethic differences (see box). Among black teens, the pregnancy rate declined by 45%, from 224/1,000 in 1990 to 123/1,000 in 2005, and then increased 2.4%, to 126/1,000 in 2006.
Among Hispanic teens, the pregnancy rate declined by 26%, from 170/1,000 in 1992 to 125/1,000 in 2005, and then increased 1% to 127/1,000 in 2006.
And among non-Hispanic whites, the rate declined by 51%, from 87/1,000 in 1990 to 43/1,000 in 2005, and then increased 2% to 44/1,000 in 2006.
State-level data were not available for 2006, but in 2005 the highest teen pregnancy rates were in New Mexico (93/1,000), Nevada (90/1,000), and Arizona (89/1,000). The lowest rates were in New Hampshire (33/1,000), Vermont (49/1,000), and Maine (48/1,000).
Although there has been a long decline in the teen pregnancy rate in the United States, even at their low point in 2005, the U.S teen pregnancy, birth, and abortion rates were still way above those for all other developed nations, Dr. Beers said.
And Dr. Kottke said that there's already evidence that the 1-year uptick is not a statistical fluke. She's seen preliminary data for 2007 indicating that the increase in teen pregnancy, birth, and abortion rates increased for a second year.
Physicians have a unique opportunity to help turn these numbers around, she said. “What we know is that young people still trust their physicians, and they look to their physicians for important education. Physicians who are serving young teens need to make sure they are an avenue for education, for care, and for confidentiality.”
The full report is available at www.guttmacher.org/pubs/USTPtrends.pdf
Vitals
Source Elsevier Global Medical News
Major Finding: The rates of teen pregnancy, birth, and abortion increased in 2006 after declining every year since 1990.
Data Source: Data compiled from national-level and state-level sources.
Disclosures: Preparation of the report was funded by the Brush Foundation, the California Wellness Foundation, and the Annie E. Casey Foundation.
Teen pregnancy rates increased 3% in the United States in 2006 after declining every year since 1990, according to a report from the Guttmacher Institute.
In addition, teen births rose 4% and teen abortions rose 1% between 2005 and 2006, according to the report, which the institute compiled from a variety of national and state-level sources.
The teen pregnancy rate hit its peak in 1990, with 117 pregnancies per 1,000 women aged 15–19 years. By 2005 it had declined 40%, to 70/1,000. But in 2006, the rate increased to 72/1,000.
“After more than a decade of progress, this reversal is deeply troubling,” Heather Boonstra, a senior public policy associate at the Guttmacher Institute, said in a prepared statement. “It coincides with an increase in rigid abstinence-only-until-marriage programs, which received major funding boosts under the Bush administration. A strong body of research shows that these programs do not work. Fortunately, the heyday of this failed experiment has come to an end with the enactment of a new teen pregnancy prevention initiative that ensures that programs will be age appropriate, medically accurate, and, most importantly, based on research demonstrating their effectiveness.”
Two experts interviewed by this news organization weren't so sure that the increase in pregnancy rates could be attributed to abstinence-only sex education. “The temporal association between the increase in abstinence-only programs and the increase in the pregnancy rate definitely deserves closer attention,” said Dr. Lee Savio Beers, a pediatrician who is director of the healthy generations clinic at Children's National Medical Center, Washington, D.C. “I don't know that anyone knows for sure whether it's directly related, but the two kind of came together. It's such a multifactorial issue that we may never have an answer on that.”
Dr. Melissa Kottke, who is with the department of ob.gyn. at Emory University and is director of the Jane Fonda Center for Adolescent Reproductive Health, both in Atlanta, said, “I think there's going to be a lot of things contributing to [increases in teen pregnancy rates], and I don't think we're going to know what all of those are.”
Dr. Kottke listed some of the other possibilities: teenage sexual activity, poverty, the media, parenting, funding for care, and funding for family planning services. “All of those things are going to contribute,” she said, “and I don't think we're going to be able to point our finger at one thing or the other.”
About the Guttmacher Institute, Dr. Beers said, “They're a well-respected organization. Their policy views tend to be on the liberal side. But I think everyone pretty much agrees that their facts are good, and their numbers are good, and for pregnancy numbers, they're better than pretty much anyone.”
Although the long decline and recent uptick in teen pregnancy rates were seen in blacks, Hispanics, and non-Hispanic whites, there were some substantial racial and ethic differences (see box). Among black teens, the pregnancy rate declined by 45%, from 224/1,000 in 1990 to 123/1,000 in 2005, and then increased 2.4%, to 126/1,000 in 2006.
Among Hispanic teens, the pregnancy rate declined by 26%, from 170/1,000 in 1992 to 125/1,000 in 2005, and then increased 1% to 127/1,000 in 2006.
And among non-Hispanic whites, the rate declined by 51%, from 87/1,000 in 1990 to 43/1,000 in 2005, and then increased 2% to 44/1,000 in 2006.
State-level data were not available for 2006, but in 2005 the highest teen pregnancy rates were in New Mexico (93/1,000), Nevada (90/1,000), and Arizona (89/1,000). The lowest rates were in New Hampshire (33/1,000), Vermont (49/1,000), and Maine (48/1,000).
Although there has been a long decline in the teen pregnancy rate in the United States, even at their low point in 2005, the U.S teen pregnancy, birth, and abortion rates were still way above those for all other developed nations, Dr. Beers said.
And Dr. Kottke said that there's already evidence that the 1-year uptick is not a statistical fluke. She's seen preliminary data for 2007 indicating that the increase in teen pregnancy, birth, and abortion rates increased for a second year.
Physicians have a unique opportunity to help turn these numbers around, she said. “What we know is that young people still trust their physicians, and they look to their physicians for important education. Physicians who are serving young teens need to make sure they are an avenue for education, for care, and for confidentiality.”
The full report is available at www.guttmacher.org/pubs/USTPtrends.pdf
Vitals
Source Elsevier Global Medical News
Major Finding: The rates of teen pregnancy, birth, and abortion increased in 2006 after declining every year since 1990.
Data Source: Data compiled from national-level and state-level sources.
Disclosures: Preparation of the report was funded by the Brush Foundation, the California Wellness Foundation, and the Annie E. Casey Foundation.
Teen pregnancy rates increased 3% in the United States in 2006 after declining every year since 1990, according to a report from the Guttmacher Institute.
In addition, teen births rose 4% and teen abortions rose 1% between 2005 and 2006, according to the report, which the institute compiled from a variety of national and state-level sources.
The teen pregnancy rate hit its peak in 1990, with 117 pregnancies per 1,000 women aged 15–19 years. By 2005 it had declined 40%, to 70/1,000. But in 2006, the rate increased to 72/1,000.
“After more than a decade of progress, this reversal is deeply troubling,” Heather Boonstra, a senior public policy associate at the Guttmacher Institute, said in a prepared statement. “It coincides with an increase in rigid abstinence-only-until-marriage programs, which received major funding boosts under the Bush administration. A strong body of research shows that these programs do not work. Fortunately, the heyday of this failed experiment has come to an end with the enactment of a new teen pregnancy prevention initiative that ensures that programs will be age appropriate, medically accurate, and, most importantly, based on research demonstrating their effectiveness.”
Two experts interviewed by this news organization weren't so sure that the increase in pregnancy rates could be attributed to abstinence-only sex education. “The temporal association between the increase in abstinence-only programs and the increase in the pregnancy rate definitely deserves closer attention,” said Dr. Lee Savio Beers, a pediatrician who is director of the healthy generations clinic at Children's National Medical Center, Washington, D.C. “I don't know that anyone knows for sure whether it's directly related, but the two kind of came together. It's such a multifactorial issue that we may never have an answer on that.”
Dr. Melissa Kottke, who is with the department of ob.gyn. at Emory University and is director of the Jane Fonda Center for Adolescent Reproductive Health, both in Atlanta, said, “I think there's going to be a lot of things contributing to [increases in teen pregnancy rates], and I don't think we're going to know what all of those are.”
Dr. Kottke listed some of the other possibilities: teenage sexual activity, poverty, the media, parenting, funding for care, and funding for family planning services. “All of those things are going to contribute,” she said, “and I don't think we're going to be able to point our finger at one thing or the other.”
About the Guttmacher Institute, Dr. Beers said, “They're a well-respected organization. Their policy views tend to be on the liberal side. But I think everyone pretty much agrees that their facts are good, and their numbers are good, and for pregnancy numbers, they're better than pretty much anyone.”
Although the long decline and recent uptick in teen pregnancy rates were seen in blacks, Hispanics, and non-Hispanic whites, there were some substantial racial and ethic differences (see box). Among black teens, the pregnancy rate declined by 45%, from 224/1,000 in 1990 to 123/1,000 in 2005, and then increased 2.4%, to 126/1,000 in 2006.
Among Hispanic teens, the pregnancy rate declined by 26%, from 170/1,000 in 1992 to 125/1,000 in 2005, and then increased 1% to 127/1,000 in 2006.
And among non-Hispanic whites, the rate declined by 51%, from 87/1,000 in 1990 to 43/1,000 in 2005, and then increased 2% to 44/1,000 in 2006.
State-level data were not available for 2006, but in 2005 the highest teen pregnancy rates were in New Mexico (93/1,000), Nevada (90/1,000), and Arizona (89/1,000). The lowest rates were in New Hampshire (33/1,000), Vermont (49/1,000), and Maine (48/1,000).
Although there has been a long decline in the teen pregnancy rate in the United States, even at their low point in 2005, the U.S teen pregnancy, birth, and abortion rates were still way above those for all other developed nations, Dr. Beers said.
And Dr. Kottke said that there's already evidence that the 1-year uptick is not a statistical fluke. She's seen preliminary data for 2007 indicating that the increase in teen pregnancy, birth, and abortion rates increased for a second year.
Physicians have a unique opportunity to help turn these numbers around, she said. “What we know is that young people still trust their physicians, and they look to their physicians for important education. Physicians who are serving young teens need to make sure they are an avenue for education, for care, and for confidentiality.”
The full report is available at www.guttmacher.org/pubs/USTPtrends.pdf
Vitals
Source Elsevier Global Medical News
Stillbirth: Preventable tragedy or a lethal “act of nature”?
Stillbirth late in pregnancy is a major obstetric tragedy. It traumatizes the mother, reverberates through the family for weeks, months, and, sometimes, painful years, and creates recurring waves of sadness, loneliness, anger, and wonder about a child who might have been.
Stillbirth is often defined as fetal loss after 20 weeks of pregnancy (if gestational age is known). By that definition, there are about 6 stillbirths for every 1,000 total births in the United States. Over the past 20 years, the rate of early fetal loss (at 20 to 27 weeks’ gestation) has remained relatively stable, whereas the rate of late fetal loss (28 weeks and later) has decreased by about 30%—likely because of better obstetric care.
Yet much more can be—should be—done to prevent stillbirth because, in part, a substantial number of stillbirths occur after 37 weeks of pregnancy. Here is one standardized, inexpensive way that we can reduce late fetal loss.
Assessing fetal movement
The Cochrane Systematic Review on the assessment of fetal movement as an indicator of fetal well-being, which was updated in 2006, concluded that 1) available data were insufficient to influence practice and 2) robust research was needed in this area.1
In a recent study of more than 65,000 pregnancies, however, Tveit and coworkers reported that taking a standardized approach to a woman’s report of decreased fetal movement reduced the rate of late fetal loss by approximately 33%.2 The study was designed as a multicenter intervention comprising:
- 7 months of preintervention (baseline) data collection, followed by
- standardized changes in practice, and then
- 17 more months of data collection.
Those “changes in practice” included 1) a standardized approach to patient education on how a mother should assess, and respond to, what she perceives to be a decrease in fetal movement and 2) a guideline for clinicians on how to respond when a patient offers a chief complaint of decreased fetal movement.
The centerpiece of the study’s patient education intervention is a brochure that includes a kick chart and detailed advice to the mother about how to count kicks and respond to what she perceives to be a decrease in fetal movement. She is advised to never wait until the next day to contact a health-care provider when she thinks that fetal movement has decreased.
The clinical guideline used in the study recommends that clinicians obtain, from all women who report decreased fetal movement, a nonstress test (NST) and an obstetric sonogram to assess fetal movement, amniotic fluid volume, and fetal growth and anatomy.
Impact of the intervention
Here is what investigators found:
- Before the intervention, baseline late fetal loss rate for the entire pregnant population at the study sites was 3 for every 1,000 births; afterward, that rate fell to 2 for every 1,000.
- The intervention did not significantly increase the number of women who self-reported decreased fetal movement.
- Before the intervention, 6.3% of pregnant women reported decreased fetal movement; afterward, that rate was 6.6%.
- Among women who reported decreased fetal movement, the late fetal loss rate fell—from 4.2% at baseline to 2.4% after the intervention (P < .004).
- Among women who reported decreased fetal movement, the late fetal loss of a normally formed fetus decreased—from 3.9% to 2.2% (P < .005).
- Because of ultrasonography, antenatal detection of growth-restricted fetuses increased significantly after the intervention.
You can do a world of good by providing support for a woman who has just experienced stillbirth; in fact, such support, done well, is as important as the interventions you put in place to prevent fetal loss. Although few high-quality studies have yielded evidence that can guide your response, after the tragedy of a stillbirth, to a grieving mother and her family, two small-scale observational and qualitative studies1,2 recommend that you:
- reduce the woman’s perception of chaos and loss of control
- support an individualized approach to her interaction with, and separation from, the fetus
- support her grieving and be sensitive to its critical steps, including denial, isolation, anger, and depression
- provide her with a comprehensible explanation for the stillbirth
- develop a well-organized care pathway from diagnosis of the loss through to delivery or surgical termination and recovery
- provide opportunity for follow-up with her and her family as a way to offer closure.
What lesson can we take home?
In many birthing centers in the United States, the approach to decreased fetal movement isn’t standardized. Taking a standardized approach to patient education about fetal movement and having a standardized clinical response that includes NST and sonography—the cornerstones of the Tviet study—is likely to reduce the rate of late fetal loss.
This approach to testing has a serendipitous advantage: It isn’t associated with a massive increase in cost for additional testing.
Many hurdles ahead
The risk of late fetal loss is influenced by many variables, including:
- gestational length
- maternal age
- race and ethnicity (see the FIGURE )
- parity
- level of education
- history of fetal loss
- numerous maternal and fetal diseases (e.g., maternal diabetes, hyperthyroidism, and hypertension; fetal growth restriction and congenital anomalies).
Key word: “Optimize.” The question of how to develop clinical algorithms that optimize pregnancy outcome by identifying an optimal upper limit of an optimal time for delivery hasn’t been answered because the matter hasn’t been exhaustively studied in randomized trials. It will be a challenge to validate such algorithms, because any strategy runs the risk of utilizing substantial health-care resources for modest clinical gain.3–5
Until sophisticated, multifactorial algorithms for identifying an optimal due date are developed, clinicians are left to select a few prominent variables to guide their recommendations—such as gestational length and maternal age. For a healthy woman, expectant management of pregnancy beyond 41 weeks is associated with an increase in the rates of stillbirth; meconium staining and meconium aspiration syndrome; and cesarean delivery. Based on these observations, many obstetricians routinely offer elective delivery to women who have reached 41 weeks’ gestation but have not begun spontaneous labor.6
As I noted, in addition to gestational age, such variables as the mother’s age and race influence optimal timing of delivery. Examples: For a woman 40 to 44 years old, delivery between 38 and 39 weeks’ gestation may be optimal to prevent stillbirth. For a woman 25 to 29 years old, it is likely safe to allow the pregnancy to progress to 41, possibly 42 weeks’ gestation before delivery.7
In addition, given the increased risk of stillbirth among black women ( FIGURE ), it might be reasonable to consider using race to 1) guide the decision to initiate fetal testing and 2) determine the optimal time for delivery.8,9
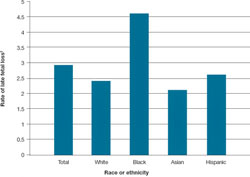
FIGURE Looking by race and ethnicity, blacks have the highest rate of late* fetal loss
*28 weeks or later.
† For every 1,000 (total) births beyond 20 weeks’ gestation.
Adapted from: Centers for Disease Control and Prevention. MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. Natl Vit Stat Rep. 2009;57:1–20.
4,000 fewer tragedies would be a blessing
With 4 million births annually in the United States, a late fetal loss rate of 3 for every 1,000 total births means 12,000 near-term stillbirths. Monitoring fetal movement, and responding promptly and in a standardized manner when it decreases, would reduce late fetal loss by 33%. That is 4,000 more live births, every year.
Look how a small shift in practice can bring a significant change in outcome—each one of those babies a precious gift to a mother and family!
1. Mangesi L, Hofmeyr GJ. Fetal movement counting for assessment of fetal wellbeing. Cochrane Database Syst Rev. 2007;(1):CD004909.-
2. Tveit JVH, Saastad E, Stray-Pedersen B, et al. Reduction of late stillbirth with the introduction of fetal movement information and guidelines—a clinical quality improvement. BMC Pregnancy Childbirth. 2009;9:32.-
3. Nicholson JM, Parry S, Caughey AB, Rosen S, Keen A, Macones GA. The impact of the active management of risk in pregnancy at term on birth outcomes: a randomized clinical trial. Am J Obstet Gynecol. 2008;198:511.e1-511.e15.
4. Klein MC. Preventive Labor Induction-AMORIPAT: much promise, not yet realized. Birth. 2009;36:83-85.
5. Fretts RC, Elkin EB, Myers ER, Heffner LJ. Should older women have antepartum testing to prevent unexplained stillbirth? Obstet Gynecol. 2004;104:56-64.
6. Bahtiyar MO, Funai EF, Rosenberg V, et al. Stillbirth at term in women of advanced maternal age in the United States: when could the antenatal testing be initiated? Am J Perinatol. 2008;25:301-304.
7. Caughey AB, Sundaram V, Kaimal AJ, et al. Systematic review: elective induction of labor versus expectant management of pregnancy. Ann Intern Med. 2009;151:252-263.
8. Willinger M, Ko CW, Reddy UM. Racial disparities in stillbirth risk across gestation in the United States. Am J Obstet Gynecol. 2009;201:469.e1-469.e8.
9. MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. Natl Vital Stat Rep. 2009;57:1-19.
Stillbirth late in pregnancy is a major obstetric tragedy. It traumatizes the mother, reverberates through the family for weeks, months, and, sometimes, painful years, and creates recurring waves of sadness, loneliness, anger, and wonder about a child who might have been.
Stillbirth is often defined as fetal loss after 20 weeks of pregnancy (if gestational age is known). By that definition, there are about 6 stillbirths for every 1,000 total births in the United States. Over the past 20 years, the rate of early fetal loss (at 20 to 27 weeks’ gestation) has remained relatively stable, whereas the rate of late fetal loss (28 weeks and later) has decreased by about 30%—likely because of better obstetric care.
Yet much more can be—should be—done to prevent stillbirth because, in part, a substantial number of stillbirths occur after 37 weeks of pregnancy. Here is one standardized, inexpensive way that we can reduce late fetal loss.
Assessing fetal movement
The Cochrane Systematic Review on the assessment of fetal movement as an indicator of fetal well-being, which was updated in 2006, concluded that 1) available data were insufficient to influence practice and 2) robust research was needed in this area.1
In a recent study of more than 65,000 pregnancies, however, Tveit and coworkers reported that taking a standardized approach to a woman’s report of decreased fetal movement reduced the rate of late fetal loss by approximately 33%.2 The study was designed as a multicenter intervention comprising:
- 7 months of preintervention (baseline) data collection, followed by
- standardized changes in practice, and then
- 17 more months of data collection.
Those “changes in practice” included 1) a standardized approach to patient education on how a mother should assess, and respond to, what she perceives to be a decrease in fetal movement and 2) a guideline for clinicians on how to respond when a patient offers a chief complaint of decreased fetal movement.
The centerpiece of the study’s patient education intervention is a brochure that includes a kick chart and detailed advice to the mother about how to count kicks and respond to what she perceives to be a decrease in fetal movement. She is advised to never wait until the next day to contact a health-care provider when she thinks that fetal movement has decreased.
The clinical guideline used in the study recommends that clinicians obtain, from all women who report decreased fetal movement, a nonstress test (NST) and an obstetric sonogram to assess fetal movement, amniotic fluid volume, and fetal growth and anatomy.
Impact of the intervention
Here is what investigators found:
- Before the intervention, baseline late fetal loss rate for the entire pregnant population at the study sites was 3 for every 1,000 births; afterward, that rate fell to 2 for every 1,000.
- The intervention did not significantly increase the number of women who self-reported decreased fetal movement.
- Before the intervention, 6.3% of pregnant women reported decreased fetal movement; afterward, that rate was 6.6%.
- Among women who reported decreased fetal movement, the late fetal loss rate fell—from 4.2% at baseline to 2.4% after the intervention (P < .004).
- Among women who reported decreased fetal movement, the late fetal loss of a normally formed fetus decreased—from 3.9% to 2.2% (P < .005).
- Because of ultrasonography, antenatal detection of growth-restricted fetuses increased significantly after the intervention.
You can do a world of good by providing support for a woman who has just experienced stillbirth; in fact, such support, done well, is as important as the interventions you put in place to prevent fetal loss. Although few high-quality studies have yielded evidence that can guide your response, after the tragedy of a stillbirth, to a grieving mother and her family, two small-scale observational and qualitative studies1,2 recommend that you:
- reduce the woman’s perception of chaos and loss of control
- support an individualized approach to her interaction with, and separation from, the fetus
- support her grieving and be sensitive to its critical steps, including denial, isolation, anger, and depression
- provide her with a comprehensible explanation for the stillbirth
- develop a well-organized care pathway from diagnosis of the loss through to delivery or surgical termination and recovery
- provide opportunity for follow-up with her and her family as a way to offer closure.
What lesson can we take home?
In many birthing centers in the United States, the approach to decreased fetal movement isn’t standardized. Taking a standardized approach to patient education about fetal movement and having a standardized clinical response that includes NST and sonography—the cornerstones of the Tviet study—is likely to reduce the rate of late fetal loss.
This approach to testing has a serendipitous advantage: It isn’t associated with a massive increase in cost for additional testing.
Many hurdles ahead
The risk of late fetal loss is influenced by many variables, including:
- gestational length
- maternal age
- race and ethnicity (see the FIGURE )
- parity
- level of education
- history of fetal loss
- numerous maternal and fetal diseases (e.g., maternal diabetes, hyperthyroidism, and hypertension; fetal growth restriction and congenital anomalies).
Key word: “Optimize.” The question of how to develop clinical algorithms that optimize pregnancy outcome by identifying an optimal upper limit of an optimal time for delivery hasn’t been answered because the matter hasn’t been exhaustively studied in randomized trials. It will be a challenge to validate such algorithms, because any strategy runs the risk of utilizing substantial health-care resources for modest clinical gain.3–5
Until sophisticated, multifactorial algorithms for identifying an optimal due date are developed, clinicians are left to select a few prominent variables to guide their recommendations—such as gestational length and maternal age. For a healthy woman, expectant management of pregnancy beyond 41 weeks is associated with an increase in the rates of stillbirth; meconium staining and meconium aspiration syndrome; and cesarean delivery. Based on these observations, many obstetricians routinely offer elective delivery to women who have reached 41 weeks’ gestation but have not begun spontaneous labor.6
As I noted, in addition to gestational age, such variables as the mother’s age and race influence optimal timing of delivery. Examples: For a woman 40 to 44 years old, delivery between 38 and 39 weeks’ gestation may be optimal to prevent stillbirth. For a woman 25 to 29 years old, it is likely safe to allow the pregnancy to progress to 41, possibly 42 weeks’ gestation before delivery.7
In addition, given the increased risk of stillbirth among black women ( FIGURE ), it might be reasonable to consider using race to 1) guide the decision to initiate fetal testing and 2) determine the optimal time for delivery.8,9
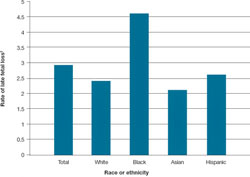
FIGURE Looking by race and ethnicity, blacks have the highest rate of late* fetal loss
*28 weeks or later.
† For every 1,000 (total) births beyond 20 weeks’ gestation.
Adapted from: Centers for Disease Control and Prevention. MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. Natl Vit Stat Rep. 2009;57:1–20.
4,000 fewer tragedies would be a blessing
With 4 million births annually in the United States, a late fetal loss rate of 3 for every 1,000 total births means 12,000 near-term stillbirths. Monitoring fetal movement, and responding promptly and in a standardized manner when it decreases, would reduce late fetal loss by 33%. That is 4,000 more live births, every year.
Look how a small shift in practice can bring a significant change in outcome—each one of those babies a precious gift to a mother and family!
Stillbirth late in pregnancy is a major obstetric tragedy. It traumatizes the mother, reverberates through the family for weeks, months, and, sometimes, painful years, and creates recurring waves of sadness, loneliness, anger, and wonder about a child who might have been.
Stillbirth is often defined as fetal loss after 20 weeks of pregnancy (if gestational age is known). By that definition, there are about 6 stillbirths for every 1,000 total births in the United States. Over the past 20 years, the rate of early fetal loss (at 20 to 27 weeks’ gestation) has remained relatively stable, whereas the rate of late fetal loss (28 weeks and later) has decreased by about 30%—likely because of better obstetric care.
Yet much more can be—should be—done to prevent stillbirth because, in part, a substantial number of stillbirths occur after 37 weeks of pregnancy. Here is one standardized, inexpensive way that we can reduce late fetal loss.
Assessing fetal movement
The Cochrane Systematic Review on the assessment of fetal movement as an indicator of fetal well-being, which was updated in 2006, concluded that 1) available data were insufficient to influence practice and 2) robust research was needed in this area.1
In a recent study of more than 65,000 pregnancies, however, Tveit and coworkers reported that taking a standardized approach to a woman’s report of decreased fetal movement reduced the rate of late fetal loss by approximately 33%.2 The study was designed as a multicenter intervention comprising:
- 7 months of preintervention (baseline) data collection, followed by
- standardized changes in practice, and then
- 17 more months of data collection.
Those “changes in practice” included 1) a standardized approach to patient education on how a mother should assess, and respond to, what she perceives to be a decrease in fetal movement and 2) a guideline for clinicians on how to respond when a patient offers a chief complaint of decreased fetal movement.
The centerpiece of the study’s patient education intervention is a brochure that includes a kick chart and detailed advice to the mother about how to count kicks and respond to what she perceives to be a decrease in fetal movement. She is advised to never wait until the next day to contact a health-care provider when she thinks that fetal movement has decreased.
The clinical guideline used in the study recommends that clinicians obtain, from all women who report decreased fetal movement, a nonstress test (NST) and an obstetric sonogram to assess fetal movement, amniotic fluid volume, and fetal growth and anatomy.
Impact of the intervention
Here is what investigators found:
- Before the intervention, baseline late fetal loss rate for the entire pregnant population at the study sites was 3 for every 1,000 births; afterward, that rate fell to 2 for every 1,000.
- The intervention did not significantly increase the number of women who self-reported decreased fetal movement.
- Before the intervention, 6.3% of pregnant women reported decreased fetal movement; afterward, that rate was 6.6%.
- Among women who reported decreased fetal movement, the late fetal loss rate fell—from 4.2% at baseline to 2.4% after the intervention (P < .004).
- Among women who reported decreased fetal movement, the late fetal loss of a normally formed fetus decreased—from 3.9% to 2.2% (P < .005).
- Because of ultrasonography, antenatal detection of growth-restricted fetuses increased significantly after the intervention.
You can do a world of good by providing support for a woman who has just experienced stillbirth; in fact, such support, done well, is as important as the interventions you put in place to prevent fetal loss. Although few high-quality studies have yielded evidence that can guide your response, after the tragedy of a stillbirth, to a grieving mother and her family, two small-scale observational and qualitative studies1,2 recommend that you:
- reduce the woman’s perception of chaos and loss of control
- support an individualized approach to her interaction with, and separation from, the fetus
- support her grieving and be sensitive to its critical steps, including denial, isolation, anger, and depression
- provide her with a comprehensible explanation for the stillbirth
- develop a well-organized care pathway from diagnosis of the loss through to delivery or surgical termination and recovery
- provide opportunity for follow-up with her and her family as a way to offer closure.
What lesson can we take home?
In many birthing centers in the United States, the approach to decreased fetal movement isn’t standardized. Taking a standardized approach to patient education about fetal movement and having a standardized clinical response that includes NST and sonography—the cornerstones of the Tviet study—is likely to reduce the rate of late fetal loss.
This approach to testing has a serendipitous advantage: It isn’t associated with a massive increase in cost for additional testing.
Many hurdles ahead
The risk of late fetal loss is influenced by many variables, including:
- gestational length
- maternal age
- race and ethnicity (see the FIGURE )
- parity
- level of education
- history of fetal loss
- numerous maternal and fetal diseases (e.g., maternal diabetes, hyperthyroidism, and hypertension; fetal growth restriction and congenital anomalies).
Key word: “Optimize.” The question of how to develop clinical algorithms that optimize pregnancy outcome by identifying an optimal upper limit of an optimal time for delivery hasn’t been answered because the matter hasn’t been exhaustively studied in randomized trials. It will be a challenge to validate such algorithms, because any strategy runs the risk of utilizing substantial health-care resources for modest clinical gain.3–5
Until sophisticated, multifactorial algorithms for identifying an optimal due date are developed, clinicians are left to select a few prominent variables to guide their recommendations—such as gestational length and maternal age. For a healthy woman, expectant management of pregnancy beyond 41 weeks is associated with an increase in the rates of stillbirth; meconium staining and meconium aspiration syndrome; and cesarean delivery. Based on these observations, many obstetricians routinely offer elective delivery to women who have reached 41 weeks’ gestation but have not begun spontaneous labor.6
As I noted, in addition to gestational age, such variables as the mother’s age and race influence optimal timing of delivery. Examples: For a woman 40 to 44 years old, delivery between 38 and 39 weeks’ gestation may be optimal to prevent stillbirth. For a woman 25 to 29 years old, it is likely safe to allow the pregnancy to progress to 41, possibly 42 weeks’ gestation before delivery.7
In addition, given the increased risk of stillbirth among black women ( FIGURE ), it might be reasonable to consider using race to 1) guide the decision to initiate fetal testing and 2) determine the optimal time for delivery.8,9
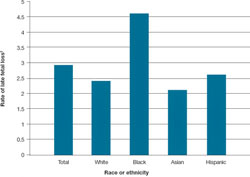
FIGURE Looking by race and ethnicity, blacks have the highest rate of late* fetal loss
*28 weeks or later.
† For every 1,000 (total) births beyond 20 weeks’ gestation.
Adapted from: Centers for Disease Control and Prevention. MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. Natl Vit Stat Rep. 2009;57:1–20.
4,000 fewer tragedies would be a blessing
With 4 million births annually in the United States, a late fetal loss rate of 3 for every 1,000 total births means 12,000 near-term stillbirths. Monitoring fetal movement, and responding promptly and in a standardized manner when it decreases, would reduce late fetal loss by 33%. That is 4,000 more live births, every year.
Look how a small shift in practice can bring a significant change in outcome—each one of those babies a precious gift to a mother and family!
1. Mangesi L, Hofmeyr GJ. Fetal movement counting for assessment of fetal wellbeing. Cochrane Database Syst Rev. 2007;(1):CD004909.-
2. Tveit JVH, Saastad E, Stray-Pedersen B, et al. Reduction of late stillbirth with the introduction of fetal movement information and guidelines—a clinical quality improvement. BMC Pregnancy Childbirth. 2009;9:32.-
3. Nicholson JM, Parry S, Caughey AB, Rosen S, Keen A, Macones GA. The impact of the active management of risk in pregnancy at term on birth outcomes: a randomized clinical trial. Am J Obstet Gynecol. 2008;198:511.e1-511.e15.
4. Klein MC. Preventive Labor Induction-AMORIPAT: much promise, not yet realized. Birth. 2009;36:83-85.
5. Fretts RC, Elkin EB, Myers ER, Heffner LJ. Should older women have antepartum testing to prevent unexplained stillbirth? Obstet Gynecol. 2004;104:56-64.
6. Bahtiyar MO, Funai EF, Rosenberg V, et al. Stillbirth at term in women of advanced maternal age in the United States: when could the antenatal testing be initiated? Am J Perinatol. 2008;25:301-304.
7. Caughey AB, Sundaram V, Kaimal AJ, et al. Systematic review: elective induction of labor versus expectant management of pregnancy. Ann Intern Med. 2009;151:252-263.
8. Willinger M, Ko CW, Reddy UM. Racial disparities in stillbirth risk across gestation in the United States. Am J Obstet Gynecol. 2009;201:469.e1-469.e8.
9. MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. Natl Vital Stat Rep. 2009;57:1-19.
1. Mangesi L, Hofmeyr GJ. Fetal movement counting for assessment of fetal wellbeing. Cochrane Database Syst Rev. 2007;(1):CD004909.-
2. Tveit JVH, Saastad E, Stray-Pedersen B, et al. Reduction of late stillbirth with the introduction of fetal movement information and guidelines—a clinical quality improvement. BMC Pregnancy Childbirth. 2009;9:32.-
3. Nicholson JM, Parry S, Caughey AB, Rosen S, Keen A, Macones GA. The impact of the active management of risk in pregnancy at term on birth outcomes: a randomized clinical trial. Am J Obstet Gynecol. 2008;198:511.e1-511.e15.
4. Klein MC. Preventive Labor Induction-AMORIPAT: much promise, not yet realized. Birth. 2009;36:83-85.
5. Fretts RC, Elkin EB, Myers ER, Heffner LJ. Should older women have antepartum testing to prevent unexplained stillbirth? Obstet Gynecol. 2004;104:56-64.
6. Bahtiyar MO, Funai EF, Rosenberg V, et al. Stillbirth at term in women of advanced maternal age in the United States: when could the antenatal testing be initiated? Am J Perinatol. 2008;25:301-304.
7. Caughey AB, Sundaram V, Kaimal AJ, et al. Systematic review: elective induction of labor versus expectant management of pregnancy. Ann Intern Med. 2009;151:252-263.
8. Willinger M, Ko CW, Reddy UM. Racial disparities in stillbirth risk across gestation in the United States. Am J Obstet Gynecol. 2009;201:469.e1-469.e8.
9. MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. Natl Vital Stat Rep. 2009;57:1-19.
IUGR Infants May Be at Risk for Atherosclerosis
Major Finding: Abdominal aortic intima media thickness was significantly greater in infants with IUGR than in controls, as was blood pressure, in one small study. In a second study of 59 IUGR fetuses, fetal ultrasonographic cardiovascular indices were significantly worse in the fetuses that died compared with survivors.
Data Source: The first study involved 25 infants with IUGR and 25 controls, while the second included 59 IUGR fetuses, in which the 8 fetuses that died were compared with survivors.
Disclosures: None reported.
HAMBURG, GERMANY — The environment experienced in utero was found in two small studies to influence the development of later cardiovascular disease and even perinatal death.
“We found that in fetuses and neonates with intrauterine growth restriction, aortic intima media wall thickness is increased with respect to controls, suggesting that it may represent an in utero marker of potential atherosclerosis development,” lead author Dr. Erich Cosmi said at the World Congress on Ultrasound in Obstetrics and Gynecology.
Doppler ultrasound revealed that maximum abdominal aortic intima media thickness (aIMT) was significantly increased in 25 infants with intrauterine growth restriction (IUGR), compared with 25 controls, at a mean gestational age of 32 weeks (2.05 mm vs. 1.05 mm) and at a mean of 18 months after birth (2.3 mm vs. 1.06 mm).
Blood pressure values were also significantly correlated with prenatal and postnatal aIMT values, reported Dr. Cosmi of the department of obstetrics and gynecology, University of Padua (Italy). Systolic blood pressure was 123 mm Hg in IUGR infants and 104 mm Hg in controls, which was significantly different at a P value of .0004.
When asked by the audience if any of the infants were on hypertension medication at the time of evaluation, Dr. Cosmi responded, “No, but they are now. We didn't know they would have hypertension. It was surprising for us.”
The researchers also assessed renal function after birth, as previous research in animal models suggests a renal contribution to developmentally programmed hypertension.
Compared with controls, IUGR infants had significantly higher urinary microalbumin (4.4 mg/L vs. 10.7 mg/L) and sodium (56 mmol/L vs. 122 mmol/L) levels and albumin/creatinine ratios (14.7 mg/g vs. 26.9 mg/g). All are markers of glomerular function.
Kidney length and volume were similar, as were levels of lysozyme, a marker of tubular function.
“The clinical implications of this study are that fetuses that were IUGR necessitate follow-up after birth, as they are at risk for cardiovascular disease,” Dr. Cosmi said in an interview.
Fetuses were classified as IUGR if their estimated fetal weight was below the 10th percentile with Doppler velocimetry greater than 2 standard deviations.
In a separate study presented during the same session, Dr. Elisenda Eixarchof the University of Barcelona reported that perinatal death in preterm IUGR fetuses is associated with the presence of markedly abnormal myocardial function before delivery and biomarkers of myocardial cell damage in cord blood.
Among 59 IUGR fetuses, the 8 fetuses who died as compared with survivors had significantly worse myocardial performance index z scores (2.5 vs. 1.7), left E/A (ratio of peak velocity during early diastolic filling to peak velocity during atrial contraction) z scores (2.4 vs. 0.8), and right E/A z scores (2.3 vs. 1). Only cardiac output was not significantly different at 816 mL/min per kilogram in those who died and 750 mL/min per kilogram in survivors.
Significant increases were also observed in fetuses who died versus survivors in B-type natriuretic peptide (350 pg/mL vs. 64 pg/mL), heart-type fatty acid–binding protein (23 mcg/L vs. 11 mcg/L), and troponin I levels (0.07 ng/mL vs. 0.02 ng/mL).
Major Finding: Abdominal aortic intima media thickness was significantly greater in infants with IUGR than in controls, as was blood pressure, in one small study. In a second study of 59 IUGR fetuses, fetal ultrasonographic cardiovascular indices were significantly worse in the fetuses that died compared with survivors.
Data Source: The first study involved 25 infants with IUGR and 25 controls, while the second included 59 IUGR fetuses, in which the 8 fetuses that died were compared with survivors.
Disclosures: None reported.
HAMBURG, GERMANY — The environment experienced in utero was found in two small studies to influence the development of later cardiovascular disease and even perinatal death.
“We found that in fetuses and neonates with intrauterine growth restriction, aortic intima media wall thickness is increased with respect to controls, suggesting that it may represent an in utero marker of potential atherosclerosis development,” lead author Dr. Erich Cosmi said at the World Congress on Ultrasound in Obstetrics and Gynecology.
Doppler ultrasound revealed that maximum abdominal aortic intima media thickness (aIMT) was significantly increased in 25 infants with intrauterine growth restriction (IUGR), compared with 25 controls, at a mean gestational age of 32 weeks (2.05 mm vs. 1.05 mm) and at a mean of 18 months after birth (2.3 mm vs. 1.06 mm).
Blood pressure values were also significantly correlated with prenatal and postnatal aIMT values, reported Dr. Cosmi of the department of obstetrics and gynecology, University of Padua (Italy). Systolic blood pressure was 123 mm Hg in IUGR infants and 104 mm Hg in controls, which was significantly different at a P value of .0004.
When asked by the audience if any of the infants were on hypertension medication at the time of evaluation, Dr. Cosmi responded, “No, but they are now. We didn't know they would have hypertension. It was surprising for us.”
The researchers also assessed renal function after birth, as previous research in animal models suggests a renal contribution to developmentally programmed hypertension.
Compared with controls, IUGR infants had significantly higher urinary microalbumin (4.4 mg/L vs. 10.7 mg/L) and sodium (56 mmol/L vs. 122 mmol/L) levels and albumin/creatinine ratios (14.7 mg/g vs. 26.9 mg/g). All are markers of glomerular function.
Kidney length and volume were similar, as were levels of lysozyme, a marker of tubular function.
“The clinical implications of this study are that fetuses that were IUGR necessitate follow-up after birth, as they are at risk for cardiovascular disease,” Dr. Cosmi said in an interview.
Fetuses were classified as IUGR if their estimated fetal weight was below the 10th percentile with Doppler velocimetry greater than 2 standard deviations.
In a separate study presented during the same session, Dr. Elisenda Eixarchof the University of Barcelona reported that perinatal death in preterm IUGR fetuses is associated with the presence of markedly abnormal myocardial function before delivery and biomarkers of myocardial cell damage in cord blood.
Among 59 IUGR fetuses, the 8 fetuses who died as compared with survivors had significantly worse myocardial performance index z scores (2.5 vs. 1.7), left E/A (ratio of peak velocity during early diastolic filling to peak velocity during atrial contraction) z scores (2.4 vs. 0.8), and right E/A z scores (2.3 vs. 1). Only cardiac output was not significantly different at 816 mL/min per kilogram in those who died and 750 mL/min per kilogram in survivors.
Significant increases were also observed in fetuses who died versus survivors in B-type natriuretic peptide (350 pg/mL vs. 64 pg/mL), heart-type fatty acid–binding protein (23 mcg/L vs. 11 mcg/L), and troponin I levels (0.07 ng/mL vs. 0.02 ng/mL).
Major Finding: Abdominal aortic intima media thickness was significantly greater in infants with IUGR than in controls, as was blood pressure, in one small study. In a second study of 59 IUGR fetuses, fetal ultrasonographic cardiovascular indices were significantly worse in the fetuses that died compared with survivors.
Data Source: The first study involved 25 infants with IUGR and 25 controls, while the second included 59 IUGR fetuses, in which the 8 fetuses that died were compared with survivors.
Disclosures: None reported.
HAMBURG, GERMANY — The environment experienced in utero was found in two small studies to influence the development of later cardiovascular disease and even perinatal death.
“We found that in fetuses and neonates with intrauterine growth restriction, aortic intima media wall thickness is increased with respect to controls, suggesting that it may represent an in utero marker of potential atherosclerosis development,” lead author Dr. Erich Cosmi said at the World Congress on Ultrasound in Obstetrics and Gynecology.
Doppler ultrasound revealed that maximum abdominal aortic intima media thickness (aIMT) was significantly increased in 25 infants with intrauterine growth restriction (IUGR), compared with 25 controls, at a mean gestational age of 32 weeks (2.05 mm vs. 1.05 mm) and at a mean of 18 months after birth (2.3 mm vs. 1.06 mm).
Blood pressure values were also significantly correlated with prenatal and postnatal aIMT values, reported Dr. Cosmi of the department of obstetrics and gynecology, University of Padua (Italy). Systolic blood pressure was 123 mm Hg in IUGR infants and 104 mm Hg in controls, which was significantly different at a P value of .0004.
When asked by the audience if any of the infants were on hypertension medication at the time of evaluation, Dr. Cosmi responded, “No, but they are now. We didn't know they would have hypertension. It was surprising for us.”
The researchers also assessed renal function after birth, as previous research in animal models suggests a renal contribution to developmentally programmed hypertension.
Compared with controls, IUGR infants had significantly higher urinary microalbumin (4.4 mg/L vs. 10.7 mg/L) and sodium (56 mmol/L vs. 122 mmol/L) levels and albumin/creatinine ratios (14.7 mg/g vs. 26.9 mg/g). All are markers of glomerular function.
Kidney length and volume were similar, as were levels of lysozyme, a marker of tubular function.
“The clinical implications of this study are that fetuses that were IUGR necessitate follow-up after birth, as they are at risk for cardiovascular disease,” Dr. Cosmi said in an interview.
Fetuses were classified as IUGR if their estimated fetal weight was below the 10th percentile with Doppler velocimetry greater than 2 standard deviations.
In a separate study presented during the same session, Dr. Elisenda Eixarchof the University of Barcelona reported that perinatal death in preterm IUGR fetuses is associated with the presence of markedly abnormal myocardial function before delivery and biomarkers of myocardial cell damage in cord blood.
Among 59 IUGR fetuses, the 8 fetuses who died as compared with survivors had significantly worse myocardial performance index z scores (2.5 vs. 1.7), left E/A (ratio of peak velocity during early diastolic filling to peak velocity during atrial contraction) z scores (2.4 vs. 0.8), and right E/A z scores (2.3 vs. 1). Only cardiac output was not significantly different at 816 mL/min per kilogram in those who died and 750 mL/min per kilogram in survivors.
Significant increases were also observed in fetuses who died versus survivors in B-type natriuretic peptide (350 pg/mL vs. 64 pg/mL), heart-type fatty acid–binding protein (23 mcg/L vs. 11 mcg/L), and troponin I levels (0.07 ng/mL vs. 0.02 ng/mL).
2009 H1N1 Maternal Deaths May Up Overall Rate
Major Finding: Of the six pregnant and two postpartum patients who died, six had underlying medical conditions. None had received antiviral medication within 48 hours after symptom onset.
Data Source: Data from 94 pregnant women, 8 postpartum women, and 137 nonpregnant women of reproductive age who were hospitalized with or died of 2009 H1N1 influenza.
Disclosures: None reported.
Maternal mortality from 2009 influenza H1N1 was estimated at 4.3/100,000 live births in California, based on the results of statewide surveillance.
The maternal mortality ratio—the number of maternal deaths per 100,000 live births—from any cause was 19.3 in California in 2005 and 13.3 in the United States in 2006. More than two-thirds of maternal deaths in the United States are directly related to obstetrical factors, and deaths from influenza had been rare prior to the 2009 influenza H1N1 outbreak, Dr. Janice K. Louieof the California Department of Public Health, Richmond, and her associates wrote (N. Engl. J. Med. 2010;362:27-35).
Now, the high maternal death rate attributed to this flu has the potential to notably increase the overall maternal mortality rate in the United States for 2009, Dr. Louie and her associates said.
From April 23 through Aug. 11, 2009, data were reported for 94 pregnant women, 8 postpartum women, and 137 nonpregnant women of reproductive age who were hospitalized with or died of 2009 H1N1 influenza.
Of the 78 pregnant women whose race/ethnicity was known, 43 were Hispanic, 15 were white, 9 were Asian or Pacific Islander, 6 were non-Hispanic black, and 5 were “other.”
About one-third (32) of the 93 pregnant women for whom the data were available had underlying medical conditions that placed them at increased risk for influenza complications, as did a fourth (2) of the 8 postpartum women and two-thirds (82) of the 137 nonpregnant women. The most common condition was asthma, affecting 16% of the pregnant and 28% of the nonpregnant women.
The most commonly reported symptoms among pregnant patients were cough (93%), fever (91%), sore throat (41%), shortness of breath (41%), muscle aches (41%), and nausea or vomiting (33%).
Eighteen (19%) of the pregnant patients were admitted to intensive care, as were 4 of the 8 (50%) postpartum patients and 41 (30%) of the nonpregnant patients.
In some of the cases, reliance on rapid influenza tests appears to have contributed to treatment delays. Rapid influenza tests were falsely negative in 38% of the total 153 who were tested. Of those 58 patients, 28 (48%) were pregnant. Only 7 of the 25 (28%) pregnant women with falsely negative results for whom information was available received antiviral treatment within the recommended 48 hours after symptom onset. Five of the eight patients (63%) who died had false-negative rapid test results, Dr. Louie and her associates noted.
In all, while 81% of both pregnant and nonpregnant women received antiviral treatment, only half of the pregnant women and a third of the nonpregnant women received it within the recommended 48-hour time frame, the investigators reported.
Of the six pregnant and two postpartum patients who died, six had underlying medical conditions, including hypothyroidism in two, gestational diabetes in one, and a history of Hodgkin's disease in one. All eight required intensive care, and none had received antiviral medication within 48 hours after symptom onset.
The maternal mortality ratio was based on an estimated 188,383 births in the state of California from April 3 through Aug. 5. The eight deaths caused by 2009 H1N1 during that time resulted in a cause-specific maternal mortality ratio of 4.3, they said.
Major Finding: Of the six pregnant and two postpartum patients who died, six had underlying medical conditions. None had received antiviral medication within 48 hours after symptom onset.
Data Source: Data from 94 pregnant women, 8 postpartum women, and 137 nonpregnant women of reproductive age who were hospitalized with or died of 2009 H1N1 influenza.
Disclosures: None reported.
Maternal mortality from 2009 influenza H1N1 was estimated at 4.3/100,000 live births in California, based on the results of statewide surveillance.
The maternal mortality ratio—the number of maternal deaths per 100,000 live births—from any cause was 19.3 in California in 2005 and 13.3 in the United States in 2006. More than two-thirds of maternal deaths in the United States are directly related to obstetrical factors, and deaths from influenza had been rare prior to the 2009 influenza H1N1 outbreak, Dr. Janice K. Louieof the California Department of Public Health, Richmond, and her associates wrote (N. Engl. J. Med. 2010;362:27-35).
Now, the high maternal death rate attributed to this flu has the potential to notably increase the overall maternal mortality rate in the United States for 2009, Dr. Louie and her associates said.
From April 23 through Aug. 11, 2009, data were reported for 94 pregnant women, 8 postpartum women, and 137 nonpregnant women of reproductive age who were hospitalized with or died of 2009 H1N1 influenza.
Of the 78 pregnant women whose race/ethnicity was known, 43 were Hispanic, 15 were white, 9 were Asian or Pacific Islander, 6 were non-Hispanic black, and 5 were “other.”
About one-third (32) of the 93 pregnant women for whom the data were available had underlying medical conditions that placed them at increased risk for influenza complications, as did a fourth (2) of the 8 postpartum women and two-thirds (82) of the 137 nonpregnant women. The most common condition was asthma, affecting 16% of the pregnant and 28% of the nonpregnant women.
The most commonly reported symptoms among pregnant patients were cough (93%), fever (91%), sore throat (41%), shortness of breath (41%), muscle aches (41%), and nausea or vomiting (33%).
Eighteen (19%) of the pregnant patients were admitted to intensive care, as were 4 of the 8 (50%) postpartum patients and 41 (30%) of the nonpregnant patients.
In some of the cases, reliance on rapid influenza tests appears to have contributed to treatment delays. Rapid influenza tests were falsely negative in 38% of the total 153 who were tested. Of those 58 patients, 28 (48%) were pregnant. Only 7 of the 25 (28%) pregnant women with falsely negative results for whom information was available received antiviral treatment within the recommended 48 hours after symptom onset. Five of the eight patients (63%) who died had false-negative rapid test results, Dr. Louie and her associates noted.
In all, while 81% of both pregnant and nonpregnant women received antiviral treatment, only half of the pregnant women and a third of the nonpregnant women received it within the recommended 48-hour time frame, the investigators reported.
Of the six pregnant and two postpartum patients who died, six had underlying medical conditions, including hypothyroidism in two, gestational diabetes in one, and a history of Hodgkin's disease in one. All eight required intensive care, and none had received antiviral medication within 48 hours after symptom onset.
The maternal mortality ratio was based on an estimated 188,383 births in the state of California from April 3 through Aug. 5. The eight deaths caused by 2009 H1N1 during that time resulted in a cause-specific maternal mortality ratio of 4.3, they said.
Major Finding: Of the six pregnant and two postpartum patients who died, six had underlying medical conditions. None had received antiviral medication within 48 hours after symptom onset.
Data Source: Data from 94 pregnant women, 8 postpartum women, and 137 nonpregnant women of reproductive age who were hospitalized with or died of 2009 H1N1 influenza.
Disclosures: None reported.
Maternal mortality from 2009 influenza H1N1 was estimated at 4.3/100,000 live births in California, based on the results of statewide surveillance.
The maternal mortality ratio—the number of maternal deaths per 100,000 live births—from any cause was 19.3 in California in 2005 and 13.3 in the United States in 2006. More than two-thirds of maternal deaths in the United States are directly related to obstetrical factors, and deaths from influenza had been rare prior to the 2009 influenza H1N1 outbreak, Dr. Janice K. Louieof the California Department of Public Health, Richmond, and her associates wrote (N. Engl. J. Med. 2010;362:27-35).
Now, the high maternal death rate attributed to this flu has the potential to notably increase the overall maternal mortality rate in the United States for 2009, Dr. Louie and her associates said.
From April 23 through Aug. 11, 2009, data were reported for 94 pregnant women, 8 postpartum women, and 137 nonpregnant women of reproductive age who were hospitalized with or died of 2009 H1N1 influenza.
Of the 78 pregnant women whose race/ethnicity was known, 43 were Hispanic, 15 were white, 9 were Asian or Pacific Islander, 6 were non-Hispanic black, and 5 were “other.”
About one-third (32) of the 93 pregnant women for whom the data were available had underlying medical conditions that placed them at increased risk for influenza complications, as did a fourth (2) of the 8 postpartum women and two-thirds (82) of the 137 nonpregnant women. The most common condition was asthma, affecting 16% of the pregnant and 28% of the nonpregnant women.
The most commonly reported symptoms among pregnant patients were cough (93%), fever (91%), sore throat (41%), shortness of breath (41%), muscle aches (41%), and nausea or vomiting (33%).
Eighteen (19%) of the pregnant patients were admitted to intensive care, as were 4 of the 8 (50%) postpartum patients and 41 (30%) of the nonpregnant patients.
In some of the cases, reliance on rapid influenza tests appears to have contributed to treatment delays. Rapid influenza tests were falsely negative in 38% of the total 153 who were tested. Of those 58 patients, 28 (48%) were pregnant. Only 7 of the 25 (28%) pregnant women with falsely negative results for whom information was available received antiviral treatment within the recommended 48 hours after symptom onset. Five of the eight patients (63%) who died had false-negative rapid test results, Dr. Louie and her associates noted.
In all, while 81% of both pregnant and nonpregnant women received antiviral treatment, only half of the pregnant women and a third of the nonpregnant women received it within the recommended 48-hour time frame, the investigators reported.
Of the six pregnant and two postpartum patients who died, six had underlying medical conditions, including hypothyroidism in two, gestational diabetes in one, and a history of Hodgkin's disease in one. All eight required intensive care, and none had received antiviral medication within 48 hours after symptom onset.
The maternal mortality ratio was based on an estimated 188,383 births in the state of California from April 3 through Aug. 5. The eight deaths caused by 2009 H1N1 during that time resulted in a cause-specific maternal mortality ratio of 4.3, they said.
Misoprostol vs. Oxytocin For Postpartum Bleeding
Major Finding: Oral misoprostol may be an alternative to intravenous oxytocin for controlling postpartum hemorrhage.
Data Source: Efficacy of oral misoprostol as an alternative to intravenous oxytocin was studied in 978 women in four hospitals in one trial, and in another 809 women who had received prophylactic oxytocin during the third stage of labor in five hospitals in a second trial.
Disclosures: Both studies were funded by the Bill and Melinda Gates Foundation. Dr. Winikoff and Ms. Blum said they had no financial conflicts to disclose.
Oral misoprostol may be as effective as intravenous oxytocin for controlling postpartum hemorrhage, based on data from two studies. Both studies involved an off-label use of misoprostol, and each study included more than 800 women.
Oxytocin is the drug of choice for postpartum bleeding, but misoprostol may be more feasible in areas with limited resources, said Dr. Beverly Winikoff of Gynuity Health Projects in New York City and her colleagues.
The first study, conducted by Dr. Winikoff and her colleagues, assessed the effectiveness of oral misoprostol as an alternative to oxytocin at four hospitals: one in Ecuador, one in Egypt, and two in Vietnam. The researchers randomized 488 women to receive four 200-mcg tablets of misoprostol and an intravenous saline placebo, while 490 women received 40 IU of intravenous oxytocin and placebo tablets. The average age of the patients was 25 years, and the median blood loss at the time of treatment was 700 mL (Lancet 2010 Jan. 7 [doi:10.1016/S0140-6736(09)61924-3]).
Within 20 minutes of administration, active bleeding was controlled in 440 (90%) of the women in the misoprostol group and 468 (96%) of the women in the oxytocin group. This difference was statistically significant. In addition, significantly more women in the misoprostol group bled at least 300 mL after treatment, compared with the oxytocin group (30% vs. 17%).
Oxytocin stopped active bleeding 2 minutes faster, on average, than did misoprostol, and women in the oxytocin group lost approximately 50 mL less blood than did women in the misoprostol group, the researchers noted. Women in the misoprostol group were significantly more likely than those in the oxytocin group to report shivering (47% vs. 17%) and fever (44% vs. 6%). No women in this study had hysterectomies and no deaths were reported.
Although the difference in treatments was statistically significant, misoprostol could substitute for oxytocin in certain settings, Dr. Winikoff and her colleagues said. “Since many women in developing countries deliver at home or at low-level facilities, misoprostol provides a potential for immediate treatment of postpartum hemorrhage.”
In a second study conducted by Gynuity Health Projects, lead author Jennifer Blum and her colleagues compared 800 mcg of oral misoprostol to 40 IU of intravenous oxytocin for primary postpartum hemorrhage in women who had received prophylactic oxytocin during the third stage of labor. This study included 407 women in the misoprostol group and 402 women in the oxytocin group. As in the first study, the average age of the patients was 25 years, and the median blood loss at the time of treatment was 700 mL. The study was conducted at five hospitals: one in Egypt, one in Turkey, one in Burkina Faso, and two in Vietnam (Lancet 2010 Jan. 7 [doi:10.1016/S0140-6736(09)61923-1]).
Within 20 minutes of administration, active bleeding was controlled in 363 (89%) of the misoprostol group and 360 (90%) of the oxytocin group. Additional blood loss of at least 300 mL occurred in 139 women (34%) in the misoprostol group and 123 women (31%) in the oxytocin group. The differences in bleeding between the two groups were not significant. But women in the misoprostol group were significantly more likely than those in the oxytocin group to report shivering (37% vs. 15%) and fever (22% vs. 15%). In this study, six women had hysterectomies (four with misoprostol and two with oxytonin), and two of these women died because of uncontrolled postpartum bleeding (both with misoprostol).
Major Finding: Oral misoprostol may be an alternative to intravenous oxytocin for controlling postpartum hemorrhage.
Data Source: Efficacy of oral misoprostol as an alternative to intravenous oxytocin was studied in 978 women in four hospitals in one trial, and in another 809 women who had received prophylactic oxytocin during the third stage of labor in five hospitals in a second trial.
Disclosures: Both studies were funded by the Bill and Melinda Gates Foundation. Dr. Winikoff and Ms. Blum said they had no financial conflicts to disclose.
Oral misoprostol may be as effective as intravenous oxytocin for controlling postpartum hemorrhage, based on data from two studies. Both studies involved an off-label use of misoprostol, and each study included more than 800 women.
Oxytocin is the drug of choice for postpartum bleeding, but misoprostol may be more feasible in areas with limited resources, said Dr. Beverly Winikoff of Gynuity Health Projects in New York City and her colleagues.
The first study, conducted by Dr. Winikoff and her colleagues, assessed the effectiveness of oral misoprostol as an alternative to oxytocin at four hospitals: one in Ecuador, one in Egypt, and two in Vietnam. The researchers randomized 488 women to receive four 200-mcg tablets of misoprostol and an intravenous saline placebo, while 490 women received 40 IU of intravenous oxytocin and placebo tablets. The average age of the patients was 25 years, and the median blood loss at the time of treatment was 700 mL (Lancet 2010 Jan. 7 [doi:10.1016/S0140-6736(09)61924-3]).
Within 20 minutes of administration, active bleeding was controlled in 440 (90%) of the women in the misoprostol group and 468 (96%) of the women in the oxytocin group. This difference was statistically significant. In addition, significantly more women in the misoprostol group bled at least 300 mL after treatment, compared with the oxytocin group (30% vs. 17%).
Oxytocin stopped active bleeding 2 minutes faster, on average, than did misoprostol, and women in the oxytocin group lost approximately 50 mL less blood than did women in the misoprostol group, the researchers noted. Women in the misoprostol group were significantly more likely than those in the oxytocin group to report shivering (47% vs. 17%) and fever (44% vs. 6%). No women in this study had hysterectomies and no deaths were reported.
Although the difference in treatments was statistically significant, misoprostol could substitute for oxytocin in certain settings, Dr. Winikoff and her colleagues said. “Since many women in developing countries deliver at home or at low-level facilities, misoprostol provides a potential for immediate treatment of postpartum hemorrhage.”
In a second study conducted by Gynuity Health Projects, lead author Jennifer Blum and her colleagues compared 800 mcg of oral misoprostol to 40 IU of intravenous oxytocin for primary postpartum hemorrhage in women who had received prophylactic oxytocin during the third stage of labor. This study included 407 women in the misoprostol group and 402 women in the oxytocin group. As in the first study, the average age of the patients was 25 years, and the median blood loss at the time of treatment was 700 mL. The study was conducted at five hospitals: one in Egypt, one in Turkey, one in Burkina Faso, and two in Vietnam (Lancet 2010 Jan. 7 [doi:10.1016/S0140-6736(09)61923-1]).
Within 20 minutes of administration, active bleeding was controlled in 363 (89%) of the misoprostol group and 360 (90%) of the oxytocin group. Additional blood loss of at least 300 mL occurred in 139 women (34%) in the misoprostol group and 123 women (31%) in the oxytocin group. The differences in bleeding between the two groups were not significant. But women in the misoprostol group were significantly more likely than those in the oxytocin group to report shivering (37% vs. 15%) and fever (22% vs. 15%). In this study, six women had hysterectomies (four with misoprostol and two with oxytonin), and two of these women died because of uncontrolled postpartum bleeding (both with misoprostol).
Major Finding: Oral misoprostol may be an alternative to intravenous oxytocin for controlling postpartum hemorrhage.
Data Source: Efficacy of oral misoprostol as an alternative to intravenous oxytocin was studied in 978 women in four hospitals in one trial, and in another 809 women who had received prophylactic oxytocin during the third stage of labor in five hospitals in a second trial.
Disclosures: Both studies were funded by the Bill and Melinda Gates Foundation. Dr. Winikoff and Ms. Blum said they had no financial conflicts to disclose.
Oral misoprostol may be as effective as intravenous oxytocin for controlling postpartum hemorrhage, based on data from two studies. Both studies involved an off-label use of misoprostol, and each study included more than 800 women.
Oxytocin is the drug of choice for postpartum bleeding, but misoprostol may be more feasible in areas with limited resources, said Dr. Beverly Winikoff of Gynuity Health Projects in New York City and her colleagues.
The first study, conducted by Dr. Winikoff and her colleagues, assessed the effectiveness of oral misoprostol as an alternative to oxytocin at four hospitals: one in Ecuador, one in Egypt, and two in Vietnam. The researchers randomized 488 women to receive four 200-mcg tablets of misoprostol and an intravenous saline placebo, while 490 women received 40 IU of intravenous oxytocin and placebo tablets. The average age of the patients was 25 years, and the median blood loss at the time of treatment was 700 mL (Lancet 2010 Jan. 7 [doi:10.1016/S0140-6736(09)61924-3]).
Within 20 minutes of administration, active bleeding was controlled in 440 (90%) of the women in the misoprostol group and 468 (96%) of the women in the oxytocin group. This difference was statistically significant. In addition, significantly more women in the misoprostol group bled at least 300 mL after treatment, compared with the oxytocin group (30% vs. 17%).
Oxytocin stopped active bleeding 2 minutes faster, on average, than did misoprostol, and women in the oxytocin group lost approximately 50 mL less blood than did women in the misoprostol group, the researchers noted. Women in the misoprostol group were significantly more likely than those in the oxytocin group to report shivering (47% vs. 17%) and fever (44% vs. 6%). No women in this study had hysterectomies and no deaths were reported.
Although the difference in treatments was statistically significant, misoprostol could substitute for oxytocin in certain settings, Dr. Winikoff and her colleagues said. “Since many women in developing countries deliver at home or at low-level facilities, misoprostol provides a potential for immediate treatment of postpartum hemorrhage.”
In a second study conducted by Gynuity Health Projects, lead author Jennifer Blum and her colleagues compared 800 mcg of oral misoprostol to 40 IU of intravenous oxytocin for primary postpartum hemorrhage in women who had received prophylactic oxytocin during the third stage of labor. This study included 407 women in the misoprostol group and 402 women in the oxytocin group. As in the first study, the average age of the patients was 25 years, and the median blood loss at the time of treatment was 700 mL. The study was conducted at five hospitals: one in Egypt, one in Turkey, one in Burkina Faso, and two in Vietnam (Lancet 2010 Jan. 7 [doi:10.1016/S0140-6736(09)61923-1]).
Within 20 minutes of administration, active bleeding was controlled in 363 (89%) of the misoprostol group and 360 (90%) of the oxytocin group. Additional blood loss of at least 300 mL occurred in 139 women (34%) in the misoprostol group and 123 women (31%) in the oxytocin group. The differences in bleeding between the two groups were not significant. But women in the misoprostol group were significantly more likely than those in the oxytocin group to report shivering (37% vs. 15%) and fever (22% vs. 15%). In this study, six women had hysterectomies (four with misoprostol and two with oxytonin), and two of these women died because of uncontrolled postpartum bleeding (both with misoprostol).
Aspirin Fails to Prevent Recurrent Miscarriages
Major Findings: Neither aspirin nor a combination of aspirin and low-molecular-weight heparin improved live birth rates in a study of 364 women with unexplained recurrent miscarriages.
Data Source: The randomized placebo-controlled ALIFE study.
Disclosures: The ALIFE trial received funding from ZonMW, the Dutch Organization for Health Research and Development (945-27-003); an unrestricted grant from GlaxoSmithKline BV;and study medications (calcium carbasalate and placebo) from Vemedia BV. None of the funding sources were involved in the study protocol preparation, trial management, or data analysis, according to the abstract. Dr. Kaandorp had no financial disclosures. Dr. Middeldorp and another coinvestigator disclosed consultancy, honoraria, and research funding from GSK.
NEW ORLEANS — Neither aspirin nor a combination of aspirin and low-molecular-weight heparin improved live birth rates in a randomized, placebo-controlled trial conducted in 364 women with unexplained recurrent miscarriages.
An intent-to-treat analysis of the ALIFE (Anticoagulants for Living Fetuses) study showed live birth rates in women seeking to carry a pregnancy to term were not affected by prophylaxis. The rates were 54.5% in 123 women given low-dose aspirin and nadroparin (a low-molecular-weight heparin [LMWH]sold in Europe), 50.8% in 120 women given low-dose aspirin alone, and 57% in 121 women given placebo.
When the investigators looked only at women who became pregnant during the trial, the live birth rates were hardly better and not significantly different: 69.1% in 97 women treated with the aspirin-LMWH combination, 61.1% in 99 women given aspirin alone, and 67% in 103 women given placebo.
“We couldn't find the beneficial effects in our study of three treatment arms—[there was] no difference at all,” Dr. Stef P. Kaandorp said during a press briefing at the annual meeting of the American Society of Hematology.
Despite a dearth of evidence in support of anticoagulant prophylaxis, a large albeit unknown number of physicians give these agents to desperate women in the United States and Europe, according to Dr. Kaandorp and his co-investigators at eight centers in The Netherlands.
The desire to help these women carry a child to term is so strong that colleagues in the United States, France, and Israel had argued that giving a placebo would be unethical in this population, senior author Dr. Saskia Middeldorp said in an interview. Obstetricians warned they would not participate if the investigators ignored their advice and went ahead with the trial.
In addition, many pregnant women buy aspirin over-the-counter to prevent miscarriage based on advice from other women in on-line chat rooms, according to Dr. Middeldorp, an internist specializing in vascular medicine at Leiden University Medical Center.
It is not clear whether the trial's findings will put an end to these practices. Dr. Bradford Schwartz, who moderated the press briefing, said the decision in the United States is up to the individual physician.
“I would say this is high-quality data that is likely to influence the way people make their therapeutics decisions. It certainly should influence those decisions,” said Dr. Schwartz, a professor of medicine and biochemistry and dean of the University of Illinois College of Medicine at Urbana-Champaign.
Dr. Kaandorp, a research fellow in the department of obstetrics and gynecology at the Academic Medical Center in Amsterdam, sympathized with physicians who want to help these women, but he was emphatic that anticoagulant prophylaxis is not justified in women with unexplained recurrent miscarriages. “To give medication that is potentially harmful is not the way to do it,” he said.
None of the participants in the study had excess bleeding events, but the study was too small to detect these, Dr. Kaandorp added in response to a question. About 40% of the women who had been injected with LMWH had skin reactions. Half of this group also had bruising, compared with 19% in the aspirin-only group and 12% of women on placebo (P less than .001).
The rationale for using aspirin and heparin to prevent miscarriage is based on the possibility that hypercoagulability might contribute to miscarriage. Evidence supports the use of these agents for this purpose in women with antiphospholipid syndrome (Obstet. Gynecol. 2002;99:135-44), and suggests that recurrent miscarriage might be related to thrombosis risk (Hum. Reprod. 2005;20:1729-32).
A literature review by four of the current authors found, however, “a paucity in studies on the efficacy and safety of aspirin and heparin in women with a history of at least two miscarriages without apparent causes other than inherited thrombophilia” (Cochrane Database Syst. Rev. 2009 Jan. 21;CD004734).
The ALIFE trial excluded women with antiphospholipid syndrome as well as those with a history of thrombosis, uterus anomaly, abnormal karyotype, or indication for anticoagulants. To be eligible, women aged 18-42 years had to have two or more unexplained miscarriages and be either trying to conceive or less than 6 weeks pregnant.
Women in the two aspirin arms took calcium carbasalate (Ascal) equivalent to acetylsalicylic acid 80 mg daily from the day of randomization until 36 weeks of gestational age. Nadroparin 2,850 IU was injected after a pregnancy was confirmed by ultrasound from 6 weeks of gestational age until the end of pregnancy.
The average age was about 33 years, and the median number of unexplained miscarriages was three. Among the women who were randomized, 103 completed treatment in each of the aspirin-plus-nadroparin and placebo arms; 104 took all treatments in the aspirin-only group.
The author could find no significant differences in subgroup analyses of women with inherited thrombophilia, preceding live birth, age less than 36 years, or three or more previous miscarriages. The investigators did see a trend toward improved live birth rate in 47 women with inherited thrombophilia, however (relative risk ratio 1.56, P = .18).
The study was underpowered to draw a conclusion on whether women with inherited thrombophilia might benefit from anticoagulant prophylaxis, Dr. Kaandorp said, promising to explore this question. “At this moment I think we should not treat those women, but should do another trial in that population,” he said.
'We couldn't find the beneficial effects in our study of three treatment arms—[there was] no difference at all.'
Source DR. KAANDORP
My Take
Study Confirms Common Sense
In women in whom no specific cause is found for miscarriage, no specific treatment should be used. Thus a treatment that is specific for pregnant women with inherited thrombophilia or antiphospholipid syndrome should not be given to pregnant women without such diagnoses. If you use aspirin in midpregnancy, you increase the risk of pregnancy loss and placental abruption. So if there is no proven benefit to this treatment, this seems like a bad deal. On the other hand, if a woman comes into an ob.gyn.'s office having had two miscarriages and says, “Do something,” some physicians may say, “Give them what they want.”
But this study has shown that aspirin does not prevent recurrent idiopathic miscarriages and does cause bruising. Low-molecular-weight heparin is probably even worse in terms of potential risks and complications.
If you do not find the problem you are looking for—that is, inherited thrombophilia or antiphospholipid syndrome—treatment is dangerous and not helpful.
Are these data new? Prior studies of aspirin use in pregnancy have demonstrated an increased risk of placental abruption in aspirin-treated women. The current study confirmed what logic told you was the right thing to do: Don't use them.
In practice I occasionally see physicians prescribe a treatment for a pregnant patient, saying, “What harm can it do?” It was that kind of thinking that led to the DES debacle some 40 years ago. When dealing with pregnancy, you can't say, “What harm can it do?” because the results can be disastrous. It is good that these researchers performed this study because it confirmed what most rational physicians know: We should use only treatments definitely shown to work, especially during pregnancy.
GERSON WEISS, M.D., is the chairman of the department of obstetrics and gynecology at New Jersey Medical School, Newark. He said he had no relevant disclosures.
Major Findings: Neither aspirin nor a combination of aspirin and low-molecular-weight heparin improved live birth rates in a study of 364 women with unexplained recurrent miscarriages.
Data Source: The randomized placebo-controlled ALIFE study.
Disclosures: The ALIFE trial received funding from ZonMW, the Dutch Organization for Health Research and Development (945-27-003); an unrestricted grant from GlaxoSmithKline BV;and study medications (calcium carbasalate and placebo) from Vemedia BV. None of the funding sources were involved in the study protocol preparation, trial management, or data analysis, according to the abstract. Dr. Kaandorp had no financial disclosures. Dr. Middeldorp and another coinvestigator disclosed consultancy, honoraria, and research funding from GSK.
NEW ORLEANS — Neither aspirin nor a combination of aspirin and low-molecular-weight heparin improved live birth rates in a randomized, placebo-controlled trial conducted in 364 women with unexplained recurrent miscarriages.
An intent-to-treat analysis of the ALIFE (Anticoagulants for Living Fetuses) study showed live birth rates in women seeking to carry a pregnancy to term were not affected by prophylaxis. The rates were 54.5% in 123 women given low-dose aspirin and nadroparin (a low-molecular-weight heparin [LMWH]sold in Europe), 50.8% in 120 women given low-dose aspirin alone, and 57% in 121 women given placebo.
When the investigators looked only at women who became pregnant during the trial, the live birth rates were hardly better and not significantly different: 69.1% in 97 women treated with the aspirin-LMWH combination, 61.1% in 99 women given aspirin alone, and 67% in 103 women given placebo.
“We couldn't find the beneficial effects in our study of three treatment arms—[there was] no difference at all,” Dr. Stef P. Kaandorp said during a press briefing at the annual meeting of the American Society of Hematology.
Despite a dearth of evidence in support of anticoagulant prophylaxis, a large albeit unknown number of physicians give these agents to desperate women in the United States and Europe, according to Dr. Kaandorp and his co-investigators at eight centers in The Netherlands.
The desire to help these women carry a child to term is so strong that colleagues in the United States, France, and Israel had argued that giving a placebo would be unethical in this population, senior author Dr. Saskia Middeldorp said in an interview. Obstetricians warned they would not participate if the investigators ignored their advice and went ahead with the trial.
In addition, many pregnant women buy aspirin over-the-counter to prevent miscarriage based on advice from other women in on-line chat rooms, according to Dr. Middeldorp, an internist specializing in vascular medicine at Leiden University Medical Center.
It is not clear whether the trial's findings will put an end to these practices. Dr. Bradford Schwartz, who moderated the press briefing, said the decision in the United States is up to the individual physician.
“I would say this is high-quality data that is likely to influence the way people make their therapeutics decisions. It certainly should influence those decisions,” said Dr. Schwartz, a professor of medicine and biochemistry and dean of the University of Illinois College of Medicine at Urbana-Champaign.
Dr. Kaandorp, a research fellow in the department of obstetrics and gynecology at the Academic Medical Center in Amsterdam, sympathized with physicians who want to help these women, but he was emphatic that anticoagulant prophylaxis is not justified in women with unexplained recurrent miscarriages. “To give medication that is potentially harmful is not the way to do it,” he said.
None of the participants in the study had excess bleeding events, but the study was too small to detect these, Dr. Kaandorp added in response to a question. About 40% of the women who had been injected with LMWH had skin reactions. Half of this group also had bruising, compared with 19% in the aspirin-only group and 12% of women on placebo (P less than .001).
The rationale for using aspirin and heparin to prevent miscarriage is based on the possibility that hypercoagulability might contribute to miscarriage. Evidence supports the use of these agents for this purpose in women with antiphospholipid syndrome (Obstet. Gynecol. 2002;99:135-44), and suggests that recurrent miscarriage might be related to thrombosis risk (Hum. Reprod. 2005;20:1729-32).
A literature review by four of the current authors found, however, “a paucity in studies on the efficacy and safety of aspirin and heparin in women with a history of at least two miscarriages without apparent causes other than inherited thrombophilia” (Cochrane Database Syst. Rev. 2009 Jan. 21;CD004734).
The ALIFE trial excluded women with antiphospholipid syndrome as well as those with a history of thrombosis, uterus anomaly, abnormal karyotype, or indication for anticoagulants. To be eligible, women aged 18-42 years had to have two or more unexplained miscarriages and be either trying to conceive or less than 6 weeks pregnant.
Women in the two aspirin arms took calcium carbasalate (Ascal) equivalent to acetylsalicylic acid 80 mg daily from the day of randomization until 36 weeks of gestational age. Nadroparin 2,850 IU was injected after a pregnancy was confirmed by ultrasound from 6 weeks of gestational age until the end of pregnancy.
The average age was about 33 years, and the median number of unexplained miscarriages was three. Among the women who were randomized, 103 completed treatment in each of the aspirin-plus-nadroparin and placebo arms; 104 took all treatments in the aspirin-only group.
The author could find no significant differences in subgroup analyses of women with inherited thrombophilia, preceding live birth, age less than 36 years, or three or more previous miscarriages. The investigators did see a trend toward improved live birth rate in 47 women with inherited thrombophilia, however (relative risk ratio 1.56, P = .18).
The study was underpowered to draw a conclusion on whether women with inherited thrombophilia might benefit from anticoagulant prophylaxis, Dr. Kaandorp said, promising to explore this question. “At this moment I think we should not treat those women, but should do another trial in that population,” he said.
'We couldn't find the beneficial effects in our study of three treatment arms—[there was] no difference at all.'
Source DR. KAANDORP
My Take
Study Confirms Common Sense
In women in whom no specific cause is found for miscarriage, no specific treatment should be used. Thus a treatment that is specific for pregnant women with inherited thrombophilia or antiphospholipid syndrome should not be given to pregnant women without such diagnoses. If you use aspirin in midpregnancy, you increase the risk of pregnancy loss and placental abruption. So if there is no proven benefit to this treatment, this seems like a bad deal. On the other hand, if a woman comes into an ob.gyn.'s office having had two miscarriages and says, “Do something,” some physicians may say, “Give them what they want.”
But this study has shown that aspirin does not prevent recurrent idiopathic miscarriages and does cause bruising. Low-molecular-weight heparin is probably even worse in terms of potential risks and complications.
If you do not find the problem you are looking for—that is, inherited thrombophilia or antiphospholipid syndrome—treatment is dangerous and not helpful.
Are these data new? Prior studies of aspirin use in pregnancy have demonstrated an increased risk of placental abruption in aspirin-treated women. The current study confirmed what logic told you was the right thing to do: Don't use them.
In practice I occasionally see physicians prescribe a treatment for a pregnant patient, saying, “What harm can it do?” It was that kind of thinking that led to the DES debacle some 40 years ago. When dealing with pregnancy, you can't say, “What harm can it do?” because the results can be disastrous. It is good that these researchers performed this study because it confirmed what most rational physicians know: We should use only treatments definitely shown to work, especially during pregnancy.
GERSON WEISS, M.D., is the chairman of the department of obstetrics and gynecology at New Jersey Medical School, Newark. He said he had no relevant disclosures.
Major Findings: Neither aspirin nor a combination of aspirin and low-molecular-weight heparin improved live birth rates in a study of 364 women with unexplained recurrent miscarriages.
Data Source: The randomized placebo-controlled ALIFE study.
Disclosures: The ALIFE trial received funding from ZonMW, the Dutch Organization for Health Research and Development (945-27-003); an unrestricted grant from GlaxoSmithKline BV;and study medications (calcium carbasalate and placebo) from Vemedia BV. None of the funding sources were involved in the study protocol preparation, trial management, or data analysis, according to the abstract. Dr. Kaandorp had no financial disclosures. Dr. Middeldorp and another coinvestigator disclosed consultancy, honoraria, and research funding from GSK.
NEW ORLEANS — Neither aspirin nor a combination of aspirin and low-molecular-weight heparin improved live birth rates in a randomized, placebo-controlled trial conducted in 364 women with unexplained recurrent miscarriages.
An intent-to-treat analysis of the ALIFE (Anticoagulants for Living Fetuses) study showed live birth rates in women seeking to carry a pregnancy to term were not affected by prophylaxis. The rates were 54.5% in 123 women given low-dose aspirin and nadroparin (a low-molecular-weight heparin [LMWH]sold in Europe), 50.8% in 120 women given low-dose aspirin alone, and 57% in 121 women given placebo.
When the investigators looked only at women who became pregnant during the trial, the live birth rates were hardly better and not significantly different: 69.1% in 97 women treated with the aspirin-LMWH combination, 61.1% in 99 women given aspirin alone, and 67% in 103 women given placebo.
“We couldn't find the beneficial effects in our study of three treatment arms—[there was] no difference at all,” Dr. Stef P. Kaandorp said during a press briefing at the annual meeting of the American Society of Hematology.
Despite a dearth of evidence in support of anticoagulant prophylaxis, a large albeit unknown number of physicians give these agents to desperate women in the United States and Europe, according to Dr. Kaandorp and his co-investigators at eight centers in The Netherlands.
The desire to help these women carry a child to term is so strong that colleagues in the United States, France, and Israel had argued that giving a placebo would be unethical in this population, senior author Dr. Saskia Middeldorp said in an interview. Obstetricians warned they would not participate if the investigators ignored their advice and went ahead with the trial.
In addition, many pregnant women buy aspirin over-the-counter to prevent miscarriage based on advice from other women in on-line chat rooms, according to Dr. Middeldorp, an internist specializing in vascular medicine at Leiden University Medical Center.
It is not clear whether the trial's findings will put an end to these practices. Dr. Bradford Schwartz, who moderated the press briefing, said the decision in the United States is up to the individual physician.
“I would say this is high-quality data that is likely to influence the way people make their therapeutics decisions. It certainly should influence those decisions,” said Dr. Schwartz, a professor of medicine and biochemistry and dean of the University of Illinois College of Medicine at Urbana-Champaign.
Dr. Kaandorp, a research fellow in the department of obstetrics and gynecology at the Academic Medical Center in Amsterdam, sympathized with physicians who want to help these women, but he was emphatic that anticoagulant prophylaxis is not justified in women with unexplained recurrent miscarriages. “To give medication that is potentially harmful is not the way to do it,” he said.
None of the participants in the study had excess bleeding events, but the study was too small to detect these, Dr. Kaandorp added in response to a question. About 40% of the women who had been injected with LMWH had skin reactions. Half of this group also had bruising, compared with 19% in the aspirin-only group and 12% of women on placebo (P less than .001).
The rationale for using aspirin and heparin to prevent miscarriage is based on the possibility that hypercoagulability might contribute to miscarriage. Evidence supports the use of these agents for this purpose in women with antiphospholipid syndrome (Obstet. Gynecol. 2002;99:135-44), and suggests that recurrent miscarriage might be related to thrombosis risk (Hum. Reprod. 2005;20:1729-32).
A literature review by four of the current authors found, however, “a paucity in studies on the efficacy and safety of aspirin and heparin in women with a history of at least two miscarriages without apparent causes other than inherited thrombophilia” (Cochrane Database Syst. Rev. 2009 Jan. 21;CD004734).
The ALIFE trial excluded women with antiphospholipid syndrome as well as those with a history of thrombosis, uterus anomaly, abnormal karyotype, or indication for anticoagulants. To be eligible, women aged 18-42 years had to have two or more unexplained miscarriages and be either trying to conceive or less than 6 weeks pregnant.
Women in the two aspirin arms took calcium carbasalate (Ascal) equivalent to acetylsalicylic acid 80 mg daily from the day of randomization until 36 weeks of gestational age. Nadroparin 2,850 IU was injected after a pregnancy was confirmed by ultrasound from 6 weeks of gestational age until the end of pregnancy.
The average age was about 33 years, and the median number of unexplained miscarriages was three. Among the women who were randomized, 103 completed treatment in each of the aspirin-plus-nadroparin and placebo arms; 104 took all treatments in the aspirin-only group.
The author could find no significant differences in subgroup analyses of women with inherited thrombophilia, preceding live birth, age less than 36 years, or three or more previous miscarriages. The investigators did see a trend toward improved live birth rate in 47 women with inherited thrombophilia, however (relative risk ratio 1.56, P = .18).
The study was underpowered to draw a conclusion on whether women with inherited thrombophilia might benefit from anticoagulant prophylaxis, Dr. Kaandorp said, promising to explore this question. “At this moment I think we should not treat those women, but should do another trial in that population,” he said.
'We couldn't find the beneficial effects in our study of three treatment arms—[there was] no difference at all.'
Source DR. KAANDORP
My Take
Study Confirms Common Sense
In women in whom no specific cause is found for miscarriage, no specific treatment should be used. Thus a treatment that is specific for pregnant women with inherited thrombophilia or antiphospholipid syndrome should not be given to pregnant women without such diagnoses. If you use aspirin in midpregnancy, you increase the risk of pregnancy loss and placental abruption. So if there is no proven benefit to this treatment, this seems like a bad deal. On the other hand, if a woman comes into an ob.gyn.'s office having had two miscarriages and says, “Do something,” some physicians may say, “Give them what they want.”
But this study has shown that aspirin does not prevent recurrent idiopathic miscarriages and does cause bruising. Low-molecular-weight heparin is probably even worse in terms of potential risks and complications.
If you do not find the problem you are looking for—that is, inherited thrombophilia or antiphospholipid syndrome—treatment is dangerous and not helpful.
Are these data new? Prior studies of aspirin use in pregnancy have demonstrated an increased risk of placental abruption in aspirin-treated women. The current study confirmed what logic told you was the right thing to do: Don't use them.
In practice I occasionally see physicians prescribe a treatment for a pregnant patient, saying, “What harm can it do?” It was that kind of thinking that led to the DES debacle some 40 years ago. When dealing with pregnancy, you can't say, “What harm can it do?” because the results can be disastrous. It is good that these researchers performed this study because it confirmed what most rational physicians know: We should use only treatments definitely shown to work, especially during pregnancy.
GERSON WEISS, M.D., is the chairman of the department of obstetrics and gynecology at New Jersey Medical School, Newark. He said he had no relevant disclosures.
Live 3-D Imaging Captures Fetal Heart Defects
Major Finding: Live 3-D volume imaging provided the “face-on” view of the fetal interventricular septum in all but 1 of 153 singleton pregnancies.
Data Source: Exams were performed on an iU-22 ultrasound scanner, with images taken between 20 and 30 weeks' gestation.
Disclosures: None reported.
HAMBURG, GERMANY — A novel technique that incorporates motion into 3-D ultrasonography allows clinicians to rapidly capture a view of the fetal heart that is difficult to obtain by standard sonography, according to Dr. Yi Xiong.
In a study of 153 singleton pregnancies, the en face, or “face-on,” view of the fetal interventricular septum was visualized using live 3-D imaging in all but 1 case, Dr. Xiong reported at the World Congress on Ultrasound in Obstetrics and Gynecology.
There were seven abnormal cases including one isolated ventricular septal defect, one atrioventricular septal defect, three truncus arteriosus with ventricular septal defects, and one case of tetralogy of Fallot.
Only one case—a transposition of the great arteries without a ventricular septal defect—could not be displayed with live 3-D imaging. It was subsequently diagnosed by 2-D ultrasound and confirmed by postnatal echocardiography and surgery.
Although further studies are required to evaluate the sensitivity and reproducibility of this technique in a large population, live 3-D imaging may be a useful tool for the rapid assessment and diagnosis of fetal ventricular septal defects, said Dr. Xiong of the Prince of Wales Hospital at the Chinese University of Hong Kong.
Defects in the crest of the interventricular septum, the atrioventricular valves, and outflow tracts make up the majority of congenital heart defects observed in infants.
Ultrasound is the modality of choice to assess the fetal heart, but even with 3-D ultrasound, the rapid beating of the fetal heart can result in motion artifact. Several methods have been used in an attempt to reduce this limitation.
“The 3-D images can be acquired in real time; therefore, the motion artifacts are no longer a problem,” coauthor Dr. Tze Kin Lau, also with the university, said in an interview.
In the current study, the exams were performed on an iU-22 ultrasound scanner (Philips Medical System) with a 7-2 MHz matrix-array transducer. All images were taken between 20 and 30 weeks' gestation, Dr. Xiong said.
With an apical four-chamber view as the starting point, the live 3-D imaging function is activated; the acquisition angle is adjusted to 72 degrees, and the volume is cropped along the z-axis to display the 3-D image of the four-chamber view.
When the fetus remains quiescent for 1-2 seconds, the “freeze” button is pressed, creating a cine sequence of real-time 3-D volumes, Dr. Xiong explained.
The best volume is chosen and then cropped along the x-axis by moving the red “render box” to the right side of the interventricular septum (IVS). The resultant volume is then turned 90 degrees along the y-axis to make the right side of the IVS face the operator. Finally, the green render box is scrolled back along the original z-axis for complete display of the en face view of the IVS.
Although live 3-D imaging was used in the study, Dr. Lau acknowledged that conventional 2-D ultrasound is usually used at their hospital to identify congenital heart defects.
Major Finding: Live 3-D volume imaging provided the “face-on” view of the fetal interventricular septum in all but 1 of 153 singleton pregnancies.
Data Source: Exams were performed on an iU-22 ultrasound scanner, with images taken between 20 and 30 weeks' gestation.
Disclosures: None reported.
HAMBURG, GERMANY — A novel technique that incorporates motion into 3-D ultrasonography allows clinicians to rapidly capture a view of the fetal heart that is difficult to obtain by standard sonography, according to Dr. Yi Xiong.
In a study of 153 singleton pregnancies, the en face, or “face-on,” view of the fetal interventricular septum was visualized using live 3-D imaging in all but 1 case, Dr. Xiong reported at the World Congress on Ultrasound in Obstetrics and Gynecology.
There were seven abnormal cases including one isolated ventricular septal defect, one atrioventricular septal defect, three truncus arteriosus with ventricular septal defects, and one case of tetralogy of Fallot.
Only one case—a transposition of the great arteries without a ventricular septal defect—could not be displayed with live 3-D imaging. It was subsequently diagnosed by 2-D ultrasound and confirmed by postnatal echocardiography and surgery.
Although further studies are required to evaluate the sensitivity and reproducibility of this technique in a large population, live 3-D imaging may be a useful tool for the rapid assessment and diagnosis of fetal ventricular septal defects, said Dr. Xiong of the Prince of Wales Hospital at the Chinese University of Hong Kong.
Defects in the crest of the interventricular septum, the atrioventricular valves, and outflow tracts make up the majority of congenital heart defects observed in infants.
Ultrasound is the modality of choice to assess the fetal heart, but even with 3-D ultrasound, the rapid beating of the fetal heart can result in motion artifact. Several methods have been used in an attempt to reduce this limitation.
“The 3-D images can be acquired in real time; therefore, the motion artifacts are no longer a problem,” coauthor Dr. Tze Kin Lau, also with the university, said in an interview.
In the current study, the exams were performed on an iU-22 ultrasound scanner (Philips Medical System) with a 7-2 MHz matrix-array transducer. All images were taken between 20 and 30 weeks' gestation, Dr. Xiong said.
With an apical four-chamber view as the starting point, the live 3-D imaging function is activated; the acquisition angle is adjusted to 72 degrees, and the volume is cropped along the z-axis to display the 3-D image of the four-chamber view.
When the fetus remains quiescent for 1-2 seconds, the “freeze” button is pressed, creating a cine sequence of real-time 3-D volumes, Dr. Xiong explained.
The best volume is chosen and then cropped along the x-axis by moving the red “render box” to the right side of the interventricular septum (IVS). The resultant volume is then turned 90 degrees along the y-axis to make the right side of the IVS face the operator. Finally, the green render box is scrolled back along the original z-axis for complete display of the en face view of the IVS.
Although live 3-D imaging was used in the study, Dr. Lau acknowledged that conventional 2-D ultrasound is usually used at their hospital to identify congenital heart defects.
Major Finding: Live 3-D volume imaging provided the “face-on” view of the fetal interventricular septum in all but 1 of 153 singleton pregnancies.
Data Source: Exams were performed on an iU-22 ultrasound scanner, with images taken between 20 and 30 weeks' gestation.
Disclosures: None reported.
HAMBURG, GERMANY — A novel technique that incorporates motion into 3-D ultrasonography allows clinicians to rapidly capture a view of the fetal heart that is difficult to obtain by standard sonography, according to Dr. Yi Xiong.
In a study of 153 singleton pregnancies, the en face, or “face-on,” view of the fetal interventricular septum was visualized using live 3-D imaging in all but 1 case, Dr. Xiong reported at the World Congress on Ultrasound in Obstetrics and Gynecology.
There were seven abnormal cases including one isolated ventricular septal defect, one atrioventricular septal defect, three truncus arteriosus with ventricular septal defects, and one case of tetralogy of Fallot.
Only one case—a transposition of the great arteries without a ventricular septal defect—could not be displayed with live 3-D imaging. It was subsequently diagnosed by 2-D ultrasound and confirmed by postnatal echocardiography and surgery.
Although further studies are required to evaluate the sensitivity and reproducibility of this technique in a large population, live 3-D imaging may be a useful tool for the rapid assessment and diagnosis of fetal ventricular septal defects, said Dr. Xiong of the Prince of Wales Hospital at the Chinese University of Hong Kong.
Defects in the crest of the interventricular septum, the atrioventricular valves, and outflow tracts make up the majority of congenital heart defects observed in infants.
Ultrasound is the modality of choice to assess the fetal heart, but even with 3-D ultrasound, the rapid beating of the fetal heart can result in motion artifact. Several methods have been used in an attempt to reduce this limitation.
“The 3-D images can be acquired in real time; therefore, the motion artifacts are no longer a problem,” coauthor Dr. Tze Kin Lau, also with the university, said in an interview.
In the current study, the exams were performed on an iU-22 ultrasound scanner (Philips Medical System) with a 7-2 MHz matrix-array transducer. All images were taken between 20 and 30 weeks' gestation, Dr. Xiong said.
With an apical four-chamber view as the starting point, the live 3-D imaging function is activated; the acquisition angle is adjusted to 72 degrees, and the volume is cropped along the z-axis to display the 3-D image of the four-chamber view.
When the fetus remains quiescent for 1-2 seconds, the “freeze” button is pressed, creating a cine sequence of real-time 3-D volumes, Dr. Xiong explained.
The best volume is chosen and then cropped along the x-axis by moving the red “render box” to the right side of the interventricular septum (IVS). The resultant volume is then turned 90 degrees along the y-axis to make the right side of the IVS face the operator. Finally, the green render box is scrolled back along the original z-axis for complete display of the en face view of the IVS.
Although live 3-D imaging was used in the study, Dr. Lau acknowledged that conventional 2-D ultrasound is usually used at their hospital to identify congenital heart defects.
Does treatment of mild gestational diabetes improve pregnancy outcome?
Whether testing for GDM is justified has been a source of contention for more than 20 years. The identification of people who are afflicted with any disease is most useful when treatment is known to produce a benefit. Until recently, evidence that treatment of GDM provides maternal, fetal, or neonatal benefit has been observational. This lack of definitive data has been particularly striking in cases involving glucose intolerance not severe enough to require initial treatment with anything more than diet.
Two blinded, randomized, controlled trials published within the past 5 years—one from Australia (the Australian Carbohydrate Intolerance Study in Pregnant Women [ACHOIS study]1 ) and the other from the Maternal–Fetal Medicine Units (MFMU) Network (cited above)—provide evidence that treatment of less severe GDM does reduce the incidence of adverse maternal and perinatal outcomes.
Details of the trials
Both studies randomized women who had mild GDM to a treatment group and a group that received only routine prenatal care. Treatment consisted of changes in diet, with the addition of insulin if certain maternal glycemic thresholds were met during the course of pregnancy.
Although sample size and results of the 50-g 1-hour glucose screening test and fasting glucose tolerance test were similar in both studies, comparison between the trials is difficult because of differences in:
- maternal prepregnancy body mass indices
- selection of candidates for glucose tolerance testing
- glucose loads during the glucose tolerance test (75 and 100 g in the ACHOIS and MFMU studies, respectively)
- glycemic thresholds and number of exceeded thresholds needed to define GDM
- percentage of patients requiring insulin in addition to diet treatment (20% and 8% in the ACHOIS and MFMU studies, respectively).
Absent from both studies is reporting of daily blood glucose values, which would have facilitated analysis of the nature of the relationship between maternal glucose concentrations and clinical outcomes.
Nonetheless, after adjusting for confounders, both studies found a reduction in the rate of macrosomia, preeclampsia, and maternal weight gain among women in the study group, compared with the control group.
In these studies, positive outcomes were achieved for most subjects using a simple and inexpensive intervention: diet change. Because the majority of large babies are born to women who are overweight and obese and who do not have GDM, it seems reasonable to speculate that the application of diet change and weight monitoring to this growing subset of the obstetric population may achieve positive short- and long-term outcomes for both mother and baby. Confirmation of this speculation awaits the execution of well-designed, adequately powered randomized trials. Until then, it seems reasonable for you to advocate weight loss and balanced nutrition for your patients who are planning to conceive or who are already pregnant, with an eye toward reduced rates of macrosomia, shoulder dystocia, cesarean delivery, and hypertensive disorders.—DAVID A. SACKS, MD
Reference
1. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477-2486.
Whether testing for GDM is justified has been a source of contention for more than 20 years. The identification of people who are afflicted with any disease is most useful when treatment is known to produce a benefit. Until recently, evidence that treatment of GDM provides maternal, fetal, or neonatal benefit has been observational. This lack of definitive data has been particularly striking in cases involving glucose intolerance not severe enough to require initial treatment with anything more than diet.
Two blinded, randomized, controlled trials published within the past 5 years—one from Australia (the Australian Carbohydrate Intolerance Study in Pregnant Women [ACHOIS study]1 ) and the other from the Maternal–Fetal Medicine Units (MFMU) Network (cited above)—provide evidence that treatment of less severe GDM does reduce the incidence of adverse maternal and perinatal outcomes.
Details of the trials
Both studies randomized women who had mild GDM to a treatment group and a group that received only routine prenatal care. Treatment consisted of changes in diet, with the addition of insulin if certain maternal glycemic thresholds were met during the course of pregnancy.
Although sample size and results of the 50-g 1-hour glucose screening test and fasting glucose tolerance test were similar in both studies, comparison between the trials is difficult because of differences in:
- maternal prepregnancy body mass indices
- selection of candidates for glucose tolerance testing
- glucose loads during the glucose tolerance test (75 and 100 g in the ACHOIS and MFMU studies, respectively)
- glycemic thresholds and number of exceeded thresholds needed to define GDM
- percentage of patients requiring insulin in addition to diet treatment (20% and 8% in the ACHOIS and MFMU studies, respectively).
Absent from both studies is reporting of daily blood glucose values, which would have facilitated analysis of the nature of the relationship between maternal glucose concentrations and clinical outcomes.
Nonetheless, after adjusting for confounders, both studies found a reduction in the rate of macrosomia, preeclampsia, and maternal weight gain among women in the study group, compared with the control group.
In these studies, positive outcomes were achieved for most subjects using a simple and inexpensive intervention: diet change. Because the majority of large babies are born to women who are overweight and obese and who do not have GDM, it seems reasonable to speculate that the application of diet change and weight monitoring to this growing subset of the obstetric population may achieve positive short- and long-term outcomes for both mother and baby. Confirmation of this speculation awaits the execution of well-designed, adequately powered randomized trials. Until then, it seems reasonable for you to advocate weight loss and balanced nutrition for your patients who are planning to conceive or who are already pregnant, with an eye toward reduced rates of macrosomia, shoulder dystocia, cesarean delivery, and hypertensive disorders.—DAVID A. SACKS, MD
Whether testing for GDM is justified has been a source of contention for more than 20 years. The identification of people who are afflicted with any disease is most useful when treatment is known to produce a benefit. Until recently, evidence that treatment of GDM provides maternal, fetal, or neonatal benefit has been observational. This lack of definitive data has been particularly striking in cases involving glucose intolerance not severe enough to require initial treatment with anything more than diet.
Two blinded, randomized, controlled trials published within the past 5 years—one from Australia (the Australian Carbohydrate Intolerance Study in Pregnant Women [ACHOIS study]1 ) and the other from the Maternal–Fetal Medicine Units (MFMU) Network (cited above)—provide evidence that treatment of less severe GDM does reduce the incidence of adverse maternal and perinatal outcomes.
Details of the trials
Both studies randomized women who had mild GDM to a treatment group and a group that received only routine prenatal care. Treatment consisted of changes in diet, with the addition of insulin if certain maternal glycemic thresholds were met during the course of pregnancy.
Although sample size and results of the 50-g 1-hour glucose screening test and fasting glucose tolerance test were similar in both studies, comparison between the trials is difficult because of differences in:
- maternal prepregnancy body mass indices
- selection of candidates for glucose tolerance testing
- glucose loads during the glucose tolerance test (75 and 100 g in the ACHOIS and MFMU studies, respectively)
- glycemic thresholds and number of exceeded thresholds needed to define GDM
- percentage of patients requiring insulin in addition to diet treatment (20% and 8% in the ACHOIS and MFMU studies, respectively).
Absent from both studies is reporting of daily blood glucose values, which would have facilitated analysis of the nature of the relationship between maternal glucose concentrations and clinical outcomes.
Nonetheless, after adjusting for confounders, both studies found a reduction in the rate of macrosomia, preeclampsia, and maternal weight gain among women in the study group, compared with the control group.
In these studies, positive outcomes were achieved for most subjects using a simple and inexpensive intervention: diet change. Because the majority of large babies are born to women who are overweight and obese and who do not have GDM, it seems reasonable to speculate that the application of diet change and weight monitoring to this growing subset of the obstetric population may achieve positive short- and long-term outcomes for both mother and baby. Confirmation of this speculation awaits the execution of well-designed, adequately powered randomized trials. Until then, it seems reasonable for you to advocate weight loss and balanced nutrition for your patients who are planning to conceive or who are already pregnant, with an eye toward reduced rates of macrosomia, shoulder dystocia, cesarean delivery, and hypertensive disorders.—DAVID A. SACKS, MD
Reference
1. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477-2486.
Reference
1. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477-2486.
PRENATAL COUNSELING
Three important areas of research into stillbirth have evolved over the past year, furthering our understanding of the phenomenon and our ability to provide comprehensive, evidence-based care:
- Genetic studies. Karyotype analysis is useful in determining the cause of stillbirth, especially when analysis is based on a sample of amniotic fluid that was obtained before delivery. And array-based comparative genomic hybridization, which yields information on the chromosome count as well as micro-duplications and deletions, can be performed on nondividing cells.
- Risk factors. Further investigation implicates advanced maternal age, obesity, and African-American race.
- Classification. Paring down the more than three dozen systems that exist for classification of stillbirth was the main challenge addressed by an international consensus group in 2009 and the focus of a separate analysis.
The individual studies that contribute to our knowledge base in these areas are discussed in more detail in the articles that follow.
Stillbirth is broadly defined as fetal demise after 20 weeks’ gestation and with a fetal weight exceeding 350 g. In the United States, stillbirth occurs in 1 of every 160 live births (6 stillbirths for every 1,000 live births). Although the rate of neonatal demise has decreased over the past decade, the rate of stillbirth has declined less strikingly.
For an analysis of karyotype, amniotic fluid is best
Korteweg FJ, Bouman K, Erwich JJ, et al. Cytogenetic analysis after evaluation of 750 fetal deaths: proposal for diagnosis workup. Obstet Gynecol. 2008;111:865–874.
ACOG Practice Bulletin #102: Management of stillbirth. Obstet Gynecol. 2009;113:748–760.
When stillbirth occurs, determination of the cause of death fulfills several goals:
- It informs counseling of the parents, who must come to terms with the loss
- It aids in determining the risk of recurrence, which informs family planning
- It furthers research into stillbirth and facilitates the comparison of national and international data.
Chromosomal anomaly is one potential cause of stillbirth. Its frequency depends on the presence of structural malformation. For example, Korteweg and colleagues found a rate of chromosomal anomaly of 4.6% among stillbirths involving fetuses without structural abnormality, but the rate rose to 38% when anatomic malformation was present. The distribution of chromosomes among stillbirths mirrored the pattern seen in live births, including 45, X and trisomies of chromosome 21, 13, and 18.
The utility of karyotype assessment when ultrasonography (US) has not identified structural malformation has been debated. Given the 5% incidence of chromosomal anomaly in the absence of structural abnormality, and the limitations of US in detecting subtle dysmorphology, a karyotype seems advisable to assess all stillbirths.
Comparison of methods points to superiority of amniocentesis
Because fewer than 20% of skin biopsies result in a useful culture, postmortem skin biopsy for karyotype assessment is unreliable. Korteweg and colleagues evaluated other methods of obtaining cells for examination and found that a successful karyotype is most likely with predelivery amniocentesis (85%), followed by umbilical cord culture (32.1%). A karyotype of cells from fascia lata and skin biopsy yielded poor results, especially in the setting of maceration. Placental biopsy is likely to provide an adequate karyotype (71% probability) but findings may be confounded by confined placental mosaicism.1
ACOG also advocates predelivery amniocentesis
In its 2009 practice bulletin, ACOG supported inclusion of amniocentesis in the assessment of stillbirth and preparation for delivery. Once an epidural is placed, amniocentesis provides cells for karyotype assessment, polymerase chain reaction (PCR) for viral studies, and any other metabolic or specific genetic studies that may be indicated by fetopsy.
If amniocentesis is not performed, ACOG recommends umbilical cord culture as an alternative. Because nondividing cells can be utilized in fluorescence in situ hybridization (FISH) for chromosome 13, 18, 21, X, and Y, this method should be considered in any case involving culture failure (TABLE).2
TABLE
Genetic components of stillbirth assessment
| Type of assessment | Steps |
|---|---|
| Inspection of fetus and placenta | Measure head circumference and length of fetus |
| Weigh fetus and placenta | |
| Photograph fetus and placenta, including frontal and profile shots of whole body, face, extremities, palms, and any abnormality | |
| Document findings | |
| Cytologic analysis | Obtain consent from parents |
| Obtain acceptable specimens using one of the following sterile techniques: | |
| • Amniocentesis at the time of prenatal diagnosis of demise • Placental block (1 x 1 cm) taken from below the cord-insertion site on the unfixed placenta • Umbilical cord segment (1.5 cm) • Internal fetal tissue specimen, e.g., costochondral junction or patella (not skin) | |
| Preserve specimens in a sterile culture medium of lactated Ringer’s solution at room temperature during transfer to laboratory | |
| Fetopsy | Obtain parental consent; if no consent is given, send placenta for pathologic analysis |
| Perform autopsy and pathologic assessment of the placenta | |
| Consider whole-body fetal radiographs | |
| Source: ACOG Practice Bulletin #102 | |
Perform predelivery amniocentesis whenever possible at the time of diagnosis of demise to obtain a cell sample for karyotype analysis to determine the cause of death.
Array-based comparative genomic hybridization makes assessment of nondividing cells possible
Raca G, Artzer A, Thorson L, et al. Array-based comparative hybridization (aCGH) in the genetic evaluation of stillbirth. Am J Med Genet A. 2009;149A:2437–2443.
Array-based comparative genomic hybridization (aCGH) makes it possible to assess the chromosome count and perform a high-resolution search for microduplications and deletions. With known segments of the genome printed on slides, the clinical scientist can analyze DNA from nondividing cells from a stillbirth. The ability to use nondividing cells is important because no cell culture is required. (Cell culture is often difficult to obtain after stillbirth.) Depending on the array selected, the resolution can be as fine as a single nucleotide polymorphism.
aCGH can inform preconception counseling
Raca and colleagues used a range of arrays to assess 15 stillbirths that involved two or more malformations. Chromosomal abnormalities, including trisomy 21 and an unbalanced translocation, were detected by aCGH in two infants. Identification of these abnormalities helped inform counseling of the parents:
- In the case of trisomy 21, parental karyotypes revealed a nontranslocation event, making it possible to assure the parents that the risk of recurrence is low
- The unbalanced translocation resulted from a balanced chromosome translocation in the mother and was associated with a significant risk of recurrence (in this case, FISH would not have helped because chromosomes 13, 18, 21, X, and Y were not involved).
Limitations of aCGH
One limitation is an inability to detect polyploidy such as triploidy or tetraploidy. This problem can be circumvented through the use of a FISH preparation prior to aCGH.
In most centers, parental blood samples are drawn at the time of aCGH studies. Because aCGH offers greater resolution of chromosome regions, an increasing number of benign variations (i.e., present in one parent) are being identified. As aCGH technology advances, we are accumulating data on copy-number variations.
A large clinical trial is needed to assess the full potential of aCGH in this setting.
Use of array-basic comparative genomic hybridization to assess cells from a stillborn fetus can help determine the cause of death and inform counseling of the parents about the risk of recurrence.
Risk factors for stillbirth include
advanced maternal age, obesity, and black race
ACOG Practice Bulletin #102: Management of stillbirth. Obstet Gynecol. 2009;113:748–760.
Willinger M, Ko CW, Reddy UM. Racial disparities in stillbirth risk across gestation in the United States. Am J Obstet Gynecol. 2009;201:469.e1–469.e8.
Fretts RC. The study of stillbirth. Am J Obstet Gynecol. 2009;201:429–430.
Women who have diseases such as insulin-dependent diabetes and systemic lupus erythematosus have long been recognized as having a six- to 20-fold increase in the risk of stillbirth, compared with the general population. However, each of these disorders accounts for 2% and less than 1% of the pregnant population, respectively, so their overall contribution to stillbirth is small. Larger portions of the population have a lower—but still significant—risk of stillbirth:
- women older than 35 years
- women who have a body mass index (BMI) above 30
- non-Hispanic black women.
Each of these categories represents 15% or more of the typical obstetric population, and each group faces a risk of stillbirth approaching 1%. The ACOG practice bulletin and the study by Willinger and colleagues address these risks in detail.
Advanced maternal age is particularly risky among nulliparous women
Advanced maternal age (>35 years) is associated with increased rates of chromosomal abnormality and maternal morbidity, such as hypertension, that are known to raise the risk of stillbirth. Even when these and other variables associated with advanced maternal age, such as placenta previa, diabetes, and multiple gestation, are controlled, however, the increased risk of stillbirth remains.
Advanced maternal age in a first pregnancy carries a particularly elevated risk. For example, the risk of stillbirth in a 40-year-old nulliparous woman is more than twice the risk in a 40-year-old multiparous woman (1 in every 116 pregnancies vs 1 in every 304).3
The increased risk of stillbirth associated with advanced maternal age is present at all gestational ages, though it becomes most profound at 37 to 42 weeks’ gestation, notably for:
- women 35 to 39 years old (1 in every 382 pregnancies; relative risk [RR] of 1.32, compared with women <35 years old; 95% confidence interval [CI], 1.22, 1.43)
- women >40 years old (1 in every 267 pregnancies; RR, 1.88; 95% CI, 1.64, 2.16).
These numbers remain significant even after controlling for medical conditions.3
The utility of antepartum surveillance and induction of labor for delivery is unclear, given the risk of iatrogenic prematurity.
Risk of stillbirth is doubled among obese and markedly obese women
Although the number of adults who are overweight (BMI 25–30) has remained fairly constant over the past 20 years (30% to 35% of the population), the percentage of women of reproductive age who are obese (BMI >30) has risen markedly. Obesity is now present in 35% of the population, and marked obesity (BMI >40) affects an additional 6%. Both obese and markedly obese women face a twofold relative risk of stillbirth, compared with women of normal weight. The rate of stillbirth in this population is 12 to 18 for every 1,000 births—a 1.2% to 1.8% risk.
Although obesity-related stillbirth likely has multiple causes, the risk remains elevated even after exclusion of confounding factors such as smoking, gestational diabetes, and preeclampsia.
Race is an independent contributor
Racial differences in the rate of stillbirth remain despite a decrease in the overall stillbirth rate over the past 20 years ( FIGURE ). In 2003, the rate of stillbirth was 5 for every 1,000 births among non-Hispanic whites, 5.5 among Hispanics, and 12 among non-Hispanic blacks. In other words, the risk of stillbirth was 1 in 202, 1 in 183, and 1 in 87 births for white, Hispanic, and black women, respectively.
Willinger and colleagues utilized data from the National Center for Health Statistics and assessed 2001–2002 birth and infant death datasets for 36 states, examining the stillbirth hazard risk for more than 5 million singleton pregnancies. Stillbirth peaked at 20 to 23 weeks and 39 to 41 weeks’ gestation, as expected. However, at 20 to 23 weeks, the risk of stillbirth among non-Hispanic black women was more than twice the rate for non-Hispanic white women (RR, 2.8). Although it then declined as term approached, it remained greater than that of non-Hispanic white women (RR, 1.6).
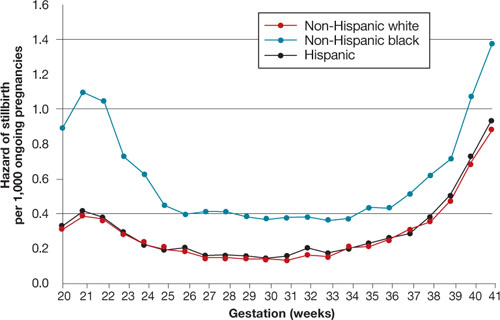
FIGURE Racial disparities in the risk of stillbirth
Hazard of stillbirth for singleton pregnancies by gestational age and race and ethnicity, 2001–2002. SOURCE: Willinger et al. Greater acceptance and use of induction of labor at term among whites merits attention
In an editorial accompanying the study by Willinger and colleagues, Fretts pointed out the higher rate of induction of labor at term among white women that has been observed in at least three studies of vital statistics. (Willinger and colleagues also pointed out this difference.) The acceptance and use of labor induction at term—and the lower stillbirth rate—among white women warrants further investigation.
Education appears to reduce the risk of stillbirth to a greater degree among whites than it does among blacks. Again, nulliparity and advanced maternal age were important contributors to the risk of stillbirth across all three races.
Counsel African-American gravidas and women older than 35 years that their risk of stillbirth is elevated.
Obese women should be advised to lose weight before conception if at all possible to reduce the risk of stillbirth.
Needed: Standardized analysis
and documentation of stillbirth
Reddy UM, Goldberg R, Silver R, et al. Stillbirth classification—developing an international consensus for research: executive summary of a National Institute of Child Health and Human Development workshop. Obstet Gynecol. 2009;114:901–914.
Flenady V, Frøen JF, Pinar H, et al. An evaluation of classification systems for stillbirth. BMC Pregnancy Childbirth. 2009;9:24.
Further guidance for the clinical management of stillbirth will come from investigations of the underlying pathologies and associated risk factors. Key to development of this guidance is the involvement of obstetricians in documenting the antenatal record and delivery information. Also needed is a standardized system for recording this information. More than three dozen systems have been developed to classify stillbirth, at the expense of uniformity of content.
An international consensus group published guidelines on how to describe the cause of death in research endeavors, recognizing the need to maintain the ability to attach a level of uncertainty. In addition, Flenady and colleagues compared the most widely used systems in clinical practice, assigning the highest score for components such as ease of use, inter observer variability, and proportion of unexplained stillbirths to CODAC [cause of death and two associated causes]. This system assigns a primary cause of death from a specified list of choices and allows inclusion of two possible contributing causes.
Both the international consensus classification and the CODAC scoring system are accessible through links embedded within the articles. Both systems require the establishment of standardized evaluation and review of stillbirth that should include obstetricians, pathologists, and geneticists.
Because assessment and classification of stillbirth are fundamental to its prevention, as well as a critical part of clinical practice, ObGyns should become familiar with the international consensus classification and CODAC scoring systems and adopt a standardized approach to assessment and documentation.
1. Rodgers CS, Creasy MR, Fitchett M, Maliszewska CT, Pratt NR, Waters JJ. Solid tissue culture for cytogenetic analysis: a collaborative survey for the Association of Clinical Cytogeneticists. J Clin Pathol. 1996;49:638-641.
2. Rivasi F, Schirosi L, Bettelli S, et al. FISH analysis in cell touch preparations and cytological specimens from formalin-fixed fetal autopsies. Diagn Cytopathol. 2008;36:633-636.
3. Reddy UM, Ko CW, Willinger M. Maternal age and the risk of stillbirth throughout pregnancy in the United States. Am J Obstet Gynecol. 2006;195:764-770.
4. MacDorman MF, Mathews TJ. NCHS Data Brief #9: Recent trends in infant mortality in the United States. Atlanta, Ga: National Center for Health Statistics; October 2008. Available at: http://www.cdc.gov/nchs/data/databriefs/db09.htm. Accessed Dec. 15, 2009.
Three important areas of research into stillbirth have evolved over the past year, furthering our understanding of the phenomenon and our ability to provide comprehensive, evidence-based care:
- Genetic studies. Karyotype analysis is useful in determining the cause of stillbirth, especially when analysis is based on a sample of amniotic fluid that was obtained before delivery. And array-based comparative genomic hybridization, which yields information on the chromosome count as well as micro-duplications and deletions, can be performed on nondividing cells.
- Risk factors. Further investigation implicates advanced maternal age, obesity, and African-American race.
- Classification. Paring down the more than three dozen systems that exist for classification of stillbirth was the main challenge addressed by an international consensus group in 2009 and the focus of a separate analysis.
The individual studies that contribute to our knowledge base in these areas are discussed in more detail in the articles that follow.
Stillbirth is broadly defined as fetal demise after 20 weeks’ gestation and with a fetal weight exceeding 350 g. In the United States, stillbirth occurs in 1 of every 160 live births (6 stillbirths for every 1,000 live births). Although the rate of neonatal demise has decreased over the past decade, the rate of stillbirth has declined less strikingly.
For an analysis of karyotype, amniotic fluid is best
Korteweg FJ, Bouman K, Erwich JJ, et al. Cytogenetic analysis after evaluation of 750 fetal deaths: proposal for diagnosis workup. Obstet Gynecol. 2008;111:865–874.
ACOG Practice Bulletin #102: Management of stillbirth. Obstet Gynecol. 2009;113:748–760.
When stillbirth occurs, determination of the cause of death fulfills several goals:
- It informs counseling of the parents, who must come to terms with the loss
- It aids in determining the risk of recurrence, which informs family planning
- It furthers research into stillbirth and facilitates the comparison of national and international data.
Chromosomal anomaly is one potential cause of stillbirth. Its frequency depends on the presence of structural malformation. For example, Korteweg and colleagues found a rate of chromosomal anomaly of 4.6% among stillbirths involving fetuses without structural abnormality, but the rate rose to 38% when anatomic malformation was present. The distribution of chromosomes among stillbirths mirrored the pattern seen in live births, including 45, X and trisomies of chromosome 21, 13, and 18.
The utility of karyotype assessment when ultrasonography (US) has not identified structural malformation has been debated. Given the 5% incidence of chromosomal anomaly in the absence of structural abnormality, and the limitations of US in detecting subtle dysmorphology, a karyotype seems advisable to assess all stillbirths.
Comparison of methods points to superiority of amniocentesis
Because fewer than 20% of skin biopsies result in a useful culture, postmortem skin biopsy for karyotype assessment is unreliable. Korteweg and colleagues evaluated other methods of obtaining cells for examination and found that a successful karyotype is most likely with predelivery amniocentesis (85%), followed by umbilical cord culture (32.1%). A karyotype of cells from fascia lata and skin biopsy yielded poor results, especially in the setting of maceration. Placental biopsy is likely to provide an adequate karyotype (71% probability) but findings may be confounded by confined placental mosaicism.1
ACOG also advocates predelivery amniocentesis
In its 2009 practice bulletin, ACOG supported inclusion of amniocentesis in the assessment of stillbirth and preparation for delivery. Once an epidural is placed, amniocentesis provides cells for karyotype assessment, polymerase chain reaction (PCR) for viral studies, and any other metabolic or specific genetic studies that may be indicated by fetopsy.
If amniocentesis is not performed, ACOG recommends umbilical cord culture as an alternative. Because nondividing cells can be utilized in fluorescence in situ hybridization (FISH) for chromosome 13, 18, 21, X, and Y, this method should be considered in any case involving culture failure (TABLE).2
TABLE
Genetic components of stillbirth assessment
| Type of assessment | Steps |
|---|---|
| Inspection of fetus and placenta | Measure head circumference and length of fetus |
| Weigh fetus and placenta | |
| Photograph fetus and placenta, including frontal and profile shots of whole body, face, extremities, palms, and any abnormality | |
| Document findings | |
| Cytologic analysis | Obtain consent from parents |
| Obtain acceptable specimens using one of the following sterile techniques: | |
| • Amniocentesis at the time of prenatal diagnosis of demise • Placental block (1 x 1 cm) taken from below the cord-insertion site on the unfixed placenta • Umbilical cord segment (1.5 cm) • Internal fetal tissue specimen, e.g., costochondral junction or patella (not skin) | |
| Preserve specimens in a sterile culture medium of lactated Ringer’s solution at room temperature during transfer to laboratory | |
| Fetopsy | Obtain parental consent; if no consent is given, send placenta for pathologic analysis |
| Perform autopsy and pathologic assessment of the placenta | |
| Consider whole-body fetal radiographs | |
| Source: ACOG Practice Bulletin #102 | |
Perform predelivery amniocentesis whenever possible at the time of diagnosis of demise to obtain a cell sample for karyotype analysis to determine the cause of death.
Array-based comparative genomic hybridization makes assessment of nondividing cells possible
Raca G, Artzer A, Thorson L, et al. Array-based comparative hybridization (aCGH) in the genetic evaluation of stillbirth. Am J Med Genet A. 2009;149A:2437–2443.
Array-based comparative genomic hybridization (aCGH) makes it possible to assess the chromosome count and perform a high-resolution search for microduplications and deletions. With known segments of the genome printed on slides, the clinical scientist can analyze DNA from nondividing cells from a stillbirth. The ability to use nondividing cells is important because no cell culture is required. (Cell culture is often difficult to obtain after stillbirth.) Depending on the array selected, the resolution can be as fine as a single nucleotide polymorphism.
aCGH can inform preconception counseling
Raca and colleagues used a range of arrays to assess 15 stillbirths that involved two or more malformations. Chromosomal abnormalities, including trisomy 21 and an unbalanced translocation, were detected by aCGH in two infants. Identification of these abnormalities helped inform counseling of the parents:
- In the case of trisomy 21, parental karyotypes revealed a nontranslocation event, making it possible to assure the parents that the risk of recurrence is low
- The unbalanced translocation resulted from a balanced chromosome translocation in the mother and was associated with a significant risk of recurrence (in this case, FISH would not have helped because chromosomes 13, 18, 21, X, and Y were not involved).
Limitations of aCGH
One limitation is an inability to detect polyploidy such as triploidy or tetraploidy. This problem can be circumvented through the use of a FISH preparation prior to aCGH.
In most centers, parental blood samples are drawn at the time of aCGH studies. Because aCGH offers greater resolution of chromosome regions, an increasing number of benign variations (i.e., present in one parent) are being identified. As aCGH technology advances, we are accumulating data on copy-number variations.
A large clinical trial is needed to assess the full potential of aCGH in this setting.
Use of array-basic comparative genomic hybridization to assess cells from a stillborn fetus can help determine the cause of death and inform counseling of the parents about the risk of recurrence.
Risk factors for stillbirth include
advanced maternal age, obesity, and black race
ACOG Practice Bulletin #102: Management of stillbirth. Obstet Gynecol. 2009;113:748–760.
Willinger M, Ko CW, Reddy UM. Racial disparities in stillbirth risk across gestation in the United States. Am J Obstet Gynecol. 2009;201:469.e1–469.e8.
Fretts RC. The study of stillbirth. Am J Obstet Gynecol. 2009;201:429–430.
Women who have diseases such as insulin-dependent diabetes and systemic lupus erythematosus have long been recognized as having a six- to 20-fold increase in the risk of stillbirth, compared with the general population. However, each of these disorders accounts for 2% and less than 1% of the pregnant population, respectively, so their overall contribution to stillbirth is small. Larger portions of the population have a lower—but still significant—risk of stillbirth:
- women older than 35 years
- women who have a body mass index (BMI) above 30
- non-Hispanic black women.
Each of these categories represents 15% or more of the typical obstetric population, and each group faces a risk of stillbirth approaching 1%. The ACOG practice bulletin and the study by Willinger and colleagues address these risks in detail.
Advanced maternal age is particularly risky among nulliparous women
Advanced maternal age (>35 years) is associated with increased rates of chromosomal abnormality and maternal morbidity, such as hypertension, that are known to raise the risk of stillbirth. Even when these and other variables associated with advanced maternal age, such as placenta previa, diabetes, and multiple gestation, are controlled, however, the increased risk of stillbirth remains.
Advanced maternal age in a first pregnancy carries a particularly elevated risk. For example, the risk of stillbirth in a 40-year-old nulliparous woman is more than twice the risk in a 40-year-old multiparous woman (1 in every 116 pregnancies vs 1 in every 304).3
The increased risk of stillbirth associated with advanced maternal age is present at all gestational ages, though it becomes most profound at 37 to 42 weeks’ gestation, notably for:
- women 35 to 39 years old (1 in every 382 pregnancies; relative risk [RR] of 1.32, compared with women <35 years old; 95% confidence interval [CI], 1.22, 1.43)
- women >40 years old (1 in every 267 pregnancies; RR, 1.88; 95% CI, 1.64, 2.16).
These numbers remain significant even after controlling for medical conditions.3
The utility of antepartum surveillance and induction of labor for delivery is unclear, given the risk of iatrogenic prematurity.
Risk of stillbirth is doubled among obese and markedly obese women
Although the number of adults who are overweight (BMI 25–30) has remained fairly constant over the past 20 years (30% to 35% of the population), the percentage of women of reproductive age who are obese (BMI >30) has risen markedly. Obesity is now present in 35% of the population, and marked obesity (BMI >40) affects an additional 6%. Both obese and markedly obese women face a twofold relative risk of stillbirth, compared with women of normal weight. The rate of stillbirth in this population is 12 to 18 for every 1,000 births—a 1.2% to 1.8% risk.
Although obesity-related stillbirth likely has multiple causes, the risk remains elevated even after exclusion of confounding factors such as smoking, gestational diabetes, and preeclampsia.
Race is an independent contributor
Racial differences in the rate of stillbirth remain despite a decrease in the overall stillbirth rate over the past 20 years ( FIGURE ). In 2003, the rate of stillbirth was 5 for every 1,000 births among non-Hispanic whites, 5.5 among Hispanics, and 12 among non-Hispanic blacks. In other words, the risk of stillbirth was 1 in 202, 1 in 183, and 1 in 87 births for white, Hispanic, and black women, respectively.
Willinger and colleagues utilized data from the National Center for Health Statistics and assessed 2001–2002 birth and infant death datasets for 36 states, examining the stillbirth hazard risk for more than 5 million singleton pregnancies. Stillbirth peaked at 20 to 23 weeks and 39 to 41 weeks’ gestation, as expected. However, at 20 to 23 weeks, the risk of stillbirth among non-Hispanic black women was more than twice the rate for non-Hispanic white women (RR, 2.8). Although it then declined as term approached, it remained greater than that of non-Hispanic white women (RR, 1.6).
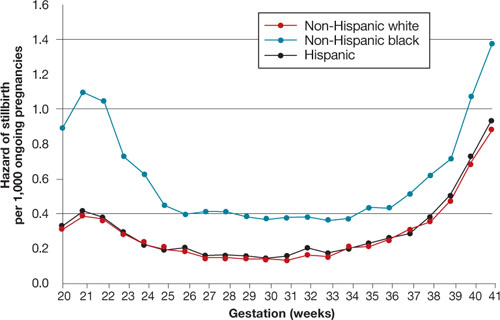
FIGURE Racial disparities in the risk of stillbirth
Hazard of stillbirth for singleton pregnancies by gestational age and race and ethnicity, 2001–2002. SOURCE: Willinger et al. Greater acceptance and use of induction of labor at term among whites merits attention
In an editorial accompanying the study by Willinger and colleagues, Fretts pointed out the higher rate of induction of labor at term among white women that has been observed in at least three studies of vital statistics. (Willinger and colleagues also pointed out this difference.) The acceptance and use of labor induction at term—and the lower stillbirth rate—among white women warrants further investigation.
Education appears to reduce the risk of stillbirth to a greater degree among whites than it does among blacks. Again, nulliparity and advanced maternal age were important contributors to the risk of stillbirth across all three races.
Counsel African-American gravidas and women older than 35 years that their risk of stillbirth is elevated.
Obese women should be advised to lose weight before conception if at all possible to reduce the risk of stillbirth.
Needed: Standardized analysis
and documentation of stillbirth
Reddy UM, Goldberg R, Silver R, et al. Stillbirth classification—developing an international consensus for research: executive summary of a National Institute of Child Health and Human Development workshop. Obstet Gynecol. 2009;114:901–914.
Flenady V, Frøen JF, Pinar H, et al. An evaluation of classification systems for stillbirth. BMC Pregnancy Childbirth. 2009;9:24.
Further guidance for the clinical management of stillbirth will come from investigations of the underlying pathologies and associated risk factors. Key to development of this guidance is the involvement of obstetricians in documenting the antenatal record and delivery information. Also needed is a standardized system for recording this information. More than three dozen systems have been developed to classify stillbirth, at the expense of uniformity of content.
An international consensus group published guidelines on how to describe the cause of death in research endeavors, recognizing the need to maintain the ability to attach a level of uncertainty. In addition, Flenady and colleagues compared the most widely used systems in clinical practice, assigning the highest score for components such as ease of use, inter observer variability, and proportion of unexplained stillbirths to CODAC [cause of death and two associated causes]. This system assigns a primary cause of death from a specified list of choices and allows inclusion of two possible contributing causes.
Both the international consensus classification and the CODAC scoring system are accessible through links embedded within the articles. Both systems require the establishment of standardized evaluation and review of stillbirth that should include obstetricians, pathologists, and geneticists.
Because assessment and classification of stillbirth are fundamental to its prevention, as well as a critical part of clinical practice, ObGyns should become familiar with the international consensus classification and CODAC scoring systems and adopt a standardized approach to assessment and documentation.
Three important areas of research into stillbirth have evolved over the past year, furthering our understanding of the phenomenon and our ability to provide comprehensive, evidence-based care:
- Genetic studies. Karyotype analysis is useful in determining the cause of stillbirth, especially when analysis is based on a sample of amniotic fluid that was obtained before delivery. And array-based comparative genomic hybridization, which yields information on the chromosome count as well as micro-duplications and deletions, can be performed on nondividing cells.
- Risk factors. Further investigation implicates advanced maternal age, obesity, and African-American race.
- Classification. Paring down the more than three dozen systems that exist for classification of stillbirth was the main challenge addressed by an international consensus group in 2009 and the focus of a separate analysis.
The individual studies that contribute to our knowledge base in these areas are discussed in more detail in the articles that follow.
Stillbirth is broadly defined as fetal demise after 20 weeks’ gestation and with a fetal weight exceeding 350 g. In the United States, stillbirth occurs in 1 of every 160 live births (6 stillbirths for every 1,000 live births). Although the rate of neonatal demise has decreased over the past decade, the rate of stillbirth has declined less strikingly.
For an analysis of karyotype, amniotic fluid is best
Korteweg FJ, Bouman K, Erwich JJ, et al. Cytogenetic analysis after evaluation of 750 fetal deaths: proposal for diagnosis workup. Obstet Gynecol. 2008;111:865–874.
ACOG Practice Bulletin #102: Management of stillbirth. Obstet Gynecol. 2009;113:748–760.
When stillbirth occurs, determination of the cause of death fulfills several goals:
- It informs counseling of the parents, who must come to terms with the loss
- It aids in determining the risk of recurrence, which informs family planning
- It furthers research into stillbirth and facilitates the comparison of national and international data.
Chromosomal anomaly is one potential cause of stillbirth. Its frequency depends on the presence of structural malformation. For example, Korteweg and colleagues found a rate of chromosomal anomaly of 4.6% among stillbirths involving fetuses without structural abnormality, but the rate rose to 38% when anatomic malformation was present. The distribution of chromosomes among stillbirths mirrored the pattern seen in live births, including 45, X and trisomies of chromosome 21, 13, and 18.
The utility of karyotype assessment when ultrasonography (US) has not identified structural malformation has been debated. Given the 5% incidence of chromosomal anomaly in the absence of structural abnormality, and the limitations of US in detecting subtle dysmorphology, a karyotype seems advisable to assess all stillbirths.
Comparison of methods points to superiority of amniocentesis
Because fewer than 20% of skin biopsies result in a useful culture, postmortem skin biopsy for karyotype assessment is unreliable. Korteweg and colleagues evaluated other methods of obtaining cells for examination and found that a successful karyotype is most likely with predelivery amniocentesis (85%), followed by umbilical cord culture (32.1%). A karyotype of cells from fascia lata and skin biopsy yielded poor results, especially in the setting of maceration. Placental biopsy is likely to provide an adequate karyotype (71% probability) but findings may be confounded by confined placental mosaicism.1
ACOG also advocates predelivery amniocentesis
In its 2009 practice bulletin, ACOG supported inclusion of amniocentesis in the assessment of stillbirth and preparation for delivery. Once an epidural is placed, amniocentesis provides cells for karyotype assessment, polymerase chain reaction (PCR) for viral studies, and any other metabolic or specific genetic studies that may be indicated by fetopsy.
If amniocentesis is not performed, ACOG recommends umbilical cord culture as an alternative. Because nondividing cells can be utilized in fluorescence in situ hybridization (FISH) for chromosome 13, 18, 21, X, and Y, this method should be considered in any case involving culture failure (TABLE).2
TABLE
Genetic components of stillbirth assessment
| Type of assessment | Steps |
|---|---|
| Inspection of fetus and placenta | Measure head circumference and length of fetus |
| Weigh fetus and placenta | |
| Photograph fetus and placenta, including frontal and profile shots of whole body, face, extremities, palms, and any abnormality | |
| Document findings | |
| Cytologic analysis | Obtain consent from parents |
| Obtain acceptable specimens using one of the following sterile techniques: | |
| • Amniocentesis at the time of prenatal diagnosis of demise • Placental block (1 x 1 cm) taken from below the cord-insertion site on the unfixed placenta • Umbilical cord segment (1.5 cm) • Internal fetal tissue specimen, e.g., costochondral junction or patella (not skin) | |
| Preserve specimens in a sterile culture medium of lactated Ringer’s solution at room temperature during transfer to laboratory | |
| Fetopsy | Obtain parental consent; if no consent is given, send placenta for pathologic analysis |
| Perform autopsy and pathologic assessment of the placenta | |
| Consider whole-body fetal radiographs | |
| Source: ACOG Practice Bulletin #102 | |
Perform predelivery amniocentesis whenever possible at the time of diagnosis of demise to obtain a cell sample for karyotype analysis to determine the cause of death.
Array-based comparative genomic hybridization makes assessment of nondividing cells possible
Raca G, Artzer A, Thorson L, et al. Array-based comparative hybridization (aCGH) in the genetic evaluation of stillbirth. Am J Med Genet A. 2009;149A:2437–2443.
Array-based comparative genomic hybridization (aCGH) makes it possible to assess the chromosome count and perform a high-resolution search for microduplications and deletions. With known segments of the genome printed on slides, the clinical scientist can analyze DNA from nondividing cells from a stillbirth. The ability to use nondividing cells is important because no cell culture is required. (Cell culture is often difficult to obtain after stillbirth.) Depending on the array selected, the resolution can be as fine as a single nucleotide polymorphism.
aCGH can inform preconception counseling
Raca and colleagues used a range of arrays to assess 15 stillbirths that involved two or more malformations. Chromosomal abnormalities, including trisomy 21 and an unbalanced translocation, were detected by aCGH in two infants. Identification of these abnormalities helped inform counseling of the parents:
- In the case of trisomy 21, parental karyotypes revealed a nontranslocation event, making it possible to assure the parents that the risk of recurrence is low
- The unbalanced translocation resulted from a balanced chromosome translocation in the mother and was associated with a significant risk of recurrence (in this case, FISH would not have helped because chromosomes 13, 18, 21, X, and Y were not involved).
Limitations of aCGH
One limitation is an inability to detect polyploidy such as triploidy or tetraploidy. This problem can be circumvented through the use of a FISH preparation prior to aCGH.
In most centers, parental blood samples are drawn at the time of aCGH studies. Because aCGH offers greater resolution of chromosome regions, an increasing number of benign variations (i.e., present in one parent) are being identified. As aCGH technology advances, we are accumulating data on copy-number variations.
A large clinical trial is needed to assess the full potential of aCGH in this setting.
Use of array-basic comparative genomic hybridization to assess cells from a stillborn fetus can help determine the cause of death and inform counseling of the parents about the risk of recurrence.
Risk factors for stillbirth include
advanced maternal age, obesity, and black race
ACOG Practice Bulletin #102: Management of stillbirth. Obstet Gynecol. 2009;113:748–760.
Willinger M, Ko CW, Reddy UM. Racial disparities in stillbirth risk across gestation in the United States. Am J Obstet Gynecol. 2009;201:469.e1–469.e8.
Fretts RC. The study of stillbirth. Am J Obstet Gynecol. 2009;201:429–430.
Women who have diseases such as insulin-dependent diabetes and systemic lupus erythematosus have long been recognized as having a six- to 20-fold increase in the risk of stillbirth, compared with the general population. However, each of these disorders accounts for 2% and less than 1% of the pregnant population, respectively, so their overall contribution to stillbirth is small. Larger portions of the population have a lower—but still significant—risk of stillbirth:
- women older than 35 years
- women who have a body mass index (BMI) above 30
- non-Hispanic black women.
Each of these categories represents 15% or more of the typical obstetric population, and each group faces a risk of stillbirth approaching 1%. The ACOG practice bulletin and the study by Willinger and colleagues address these risks in detail.
Advanced maternal age is particularly risky among nulliparous women
Advanced maternal age (>35 years) is associated with increased rates of chromosomal abnormality and maternal morbidity, such as hypertension, that are known to raise the risk of stillbirth. Even when these and other variables associated with advanced maternal age, such as placenta previa, diabetes, and multiple gestation, are controlled, however, the increased risk of stillbirth remains.
Advanced maternal age in a first pregnancy carries a particularly elevated risk. For example, the risk of stillbirth in a 40-year-old nulliparous woman is more than twice the risk in a 40-year-old multiparous woman (1 in every 116 pregnancies vs 1 in every 304).3
The increased risk of stillbirth associated with advanced maternal age is present at all gestational ages, though it becomes most profound at 37 to 42 weeks’ gestation, notably for:
- women 35 to 39 years old (1 in every 382 pregnancies; relative risk [RR] of 1.32, compared with women <35 years old; 95% confidence interval [CI], 1.22, 1.43)
- women >40 years old (1 in every 267 pregnancies; RR, 1.88; 95% CI, 1.64, 2.16).
These numbers remain significant even after controlling for medical conditions.3
The utility of antepartum surveillance and induction of labor for delivery is unclear, given the risk of iatrogenic prematurity.
Risk of stillbirth is doubled among obese and markedly obese women
Although the number of adults who are overweight (BMI 25–30) has remained fairly constant over the past 20 years (30% to 35% of the population), the percentage of women of reproductive age who are obese (BMI >30) has risen markedly. Obesity is now present in 35% of the population, and marked obesity (BMI >40) affects an additional 6%. Both obese and markedly obese women face a twofold relative risk of stillbirth, compared with women of normal weight. The rate of stillbirth in this population is 12 to 18 for every 1,000 births—a 1.2% to 1.8% risk.
Although obesity-related stillbirth likely has multiple causes, the risk remains elevated even after exclusion of confounding factors such as smoking, gestational diabetes, and preeclampsia.
Race is an independent contributor
Racial differences in the rate of stillbirth remain despite a decrease in the overall stillbirth rate over the past 20 years ( FIGURE ). In 2003, the rate of stillbirth was 5 for every 1,000 births among non-Hispanic whites, 5.5 among Hispanics, and 12 among non-Hispanic blacks. In other words, the risk of stillbirth was 1 in 202, 1 in 183, and 1 in 87 births for white, Hispanic, and black women, respectively.
Willinger and colleagues utilized data from the National Center for Health Statistics and assessed 2001–2002 birth and infant death datasets for 36 states, examining the stillbirth hazard risk for more than 5 million singleton pregnancies. Stillbirth peaked at 20 to 23 weeks and 39 to 41 weeks’ gestation, as expected. However, at 20 to 23 weeks, the risk of stillbirth among non-Hispanic black women was more than twice the rate for non-Hispanic white women (RR, 2.8). Although it then declined as term approached, it remained greater than that of non-Hispanic white women (RR, 1.6).
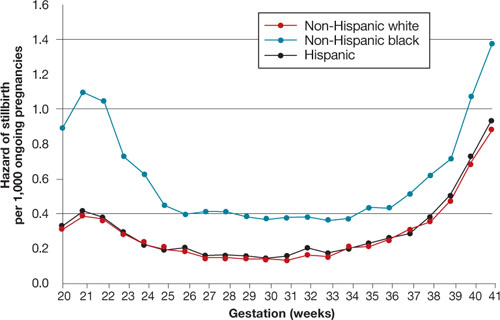
FIGURE Racial disparities in the risk of stillbirth
Hazard of stillbirth for singleton pregnancies by gestational age and race and ethnicity, 2001–2002. SOURCE: Willinger et al. Greater acceptance and use of induction of labor at term among whites merits attention
In an editorial accompanying the study by Willinger and colleagues, Fretts pointed out the higher rate of induction of labor at term among white women that has been observed in at least three studies of vital statistics. (Willinger and colleagues also pointed out this difference.) The acceptance and use of labor induction at term—and the lower stillbirth rate—among white women warrants further investigation.
Education appears to reduce the risk of stillbirth to a greater degree among whites than it does among blacks. Again, nulliparity and advanced maternal age were important contributors to the risk of stillbirth across all three races.
Counsel African-American gravidas and women older than 35 years that their risk of stillbirth is elevated.
Obese women should be advised to lose weight before conception if at all possible to reduce the risk of stillbirth.
Needed: Standardized analysis
and documentation of stillbirth
Reddy UM, Goldberg R, Silver R, et al. Stillbirth classification—developing an international consensus for research: executive summary of a National Institute of Child Health and Human Development workshop. Obstet Gynecol. 2009;114:901–914.
Flenady V, Frøen JF, Pinar H, et al. An evaluation of classification systems for stillbirth. BMC Pregnancy Childbirth. 2009;9:24.
Further guidance for the clinical management of stillbirth will come from investigations of the underlying pathologies and associated risk factors. Key to development of this guidance is the involvement of obstetricians in documenting the antenatal record and delivery information. Also needed is a standardized system for recording this information. More than three dozen systems have been developed to classify stillbirth, at the expense of uniformity of content.
An international consensus group published guidelines on how to describe the cause of death in research endeavors, recognizing the need to maintain the ability to attach a level of uncertainty. In addition, Flenady and colleagues compared the most widely used systems in clinical practice, assigning the highest score for components such as ease of use, inter observer variability, and proportion of unexplained stillbirths to CODAC [cause of death and two associated causes]. This system assigns a primary cause of death from a specified list of choices and allows inclusion of two possible contributing causes.
Both the international consensus classification and the CODAC scoring system are accessible through links embedded within the articles. Both systems require the establishment of standardized evaluation and review of stillbirth that should include obstetricians, pathologists, and geneticists.
Because assessment and classification of stillbirth are fundamental to its prevention, as well as a critical part of clinical practice, ObGyns should become familiar with the international consensus classification and CODAC scoring systems and adopt a standardized approach to assessment and documentation.
1. Rodgers CS, Creasy MR, Fitchett M, Maliszewska CT, Pratt NR, Waters JJ. Solid tissue culture for cytogenetic analysis: a collaborative survey for the Association of Clinical Cytogeneticists. J Clin Pathol. 1996;49:638-641.
2. Rivasi F, Schirosi L, Bettelli S, et al. FISH analysis in cell touch preparations and cytological specimens from formalin-fixed fetal autopsies. Diagn Cytopathol. 2008;36:633-636.
3. Reddy UM, Ko CW, Willinger M. Maternal age and the risk of stillbirth throughout pregnancy in the United States. Am J Obstet Gynecol. 2006;195:764-770.
4. MacDorman MF, Mathews TJ. NCHS Data Brief #9: Recent trends in infant mortality in the United States. Atlanta, Ga: National Center for Health Statistics; October 2008. Available at: http://www.cdc.gov/nchs/data/databriefs/db09.htm. Accessed Dec. 15, 2009.
1. Rodgers CS, Creasy MR, Fitchett M, Maliszewska CT, Pratt NR, Waters JJ. Solid tissue culture for cytogenetic analysis: a collaborative survey for the Association of Clinical Cytogeneticists. J Clin Pathol. 1996;49:638-641.
2. Rivasi F, Schirosi L, Bettelli S, et al. FISH analysis in cell touch preparations and cytological specimens from formalin-fixed fetal autopsies. Diagn Cytopathol. 2008;36:633-636.
3. Reddy UM, Ko CW, Willinger M. Maternal age and the risk of stillbirth throughout pregnancy in the United States. Am J Obstet Gynecol. 2006;195:764-770.
4. MacDorman MF, Mathews TJ. NCHS Data Brief #9: Recent trends in infant mortality in the United States. Atlanta, Ga: National Center for Health Statistics; October 2008. Available at: http://www.cdc.gov/nchs/data/databriefs/db09.htm. Accessed Dec. 15, 2009.
