User login
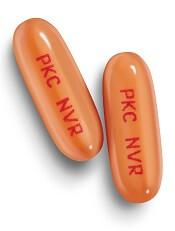
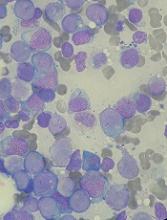
FDA expands approved use of bosutinib in CML
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
CHMP recommends generic drug for ET
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation. ![]()
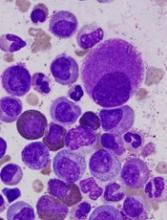
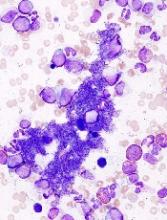
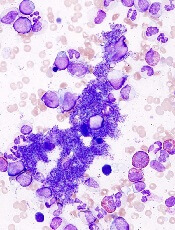
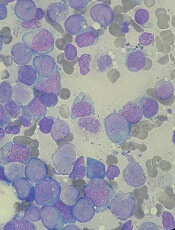
Health Canada approves midostaurin for AML
Health Canada has approved use of the multi-targeted kinase inhibitor midostaurin (Rydapt™).
This makes midostaurin the first targeted therapy approved to treat FLT3-mutated acute myeloid leukemia (AML) in Canada.
Midostaurin is approved for use with standard cytarabine and daunorubicin induction and cytarabine consolidation for the treatment of adults with newly diagnosed FLT3-mutated AML.
Health Canada’s approval of midostaurin is based on results from the phase 3 RATIFY trial, which were published in NEJM in August.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infection.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis.
Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm. ![]()
Health Canada has approved use of the multi-targeted kinase inhibitor midostaurin (Rydapt™).
This makes midostaurin the first targeted therapy approved to treat FLT3-mutated acute myeloid leukemia (AML) in Canada.
Midostaurin is approved for use with standard cytarabine and daunorubicin induction and cytarabine consolidation for the treatment of adults with newly diagnosed FLT3-mutated AML.
Health Canada’s approval of midostaurin is based on results from the phase 3 RATIFY trial, which were published in NEJM in August.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infection.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis.
Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm. ![]()
Health Canada has approved use of the multi-targeted kinase inhibitor midostaurin (Rydapt™).
This makes midostaurin the first targeted therapy approved to treat FLT3-mutated acute myeloid leukemia (AML) in Canada.
Midostaurin is approved for use with standard cytarabine and daunorubicin induction and cytarabine consolidation for the treatment of adults with newly diagnosed FLT3-mutated AML.
Health Canada’s approval of midostaurin is based on results from the phase 3 RATIFY trial, which were published in NEJM in August.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infection.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis.
Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm. ![]()
Companies launch generic busulfan in US
Two companies have announced the US launch of a generic busulfan product, Myleran Injection.
Mylan NV and Aspen have partnered to develop Myleran (busulfan) Injection, 60 mg/10 mL (6 mg/mL) Single-dose Vial, a generic version of Otsuka Pharmaceutical’s Busulfex® Injection.
The US Food and Drug Administration approved Myleran Injection for use in combination with cyclophosphamide as a conditioning regimen prior to allogeneic hematopoietic stem cell transplant in patients with chronic myeloid leukemia. ![]()
Two companies have announced the US launch of a generic busulfan product, Myleran Injection.
Mylan NV and Aspen have partnered to develop Myleran (busulfan) Injection, 60 mg/10 mL (6 mg/mL) Single-dose Vial, a generic version of Otsuka Pharmaceutical’s Busulfex® Injection.
The US Food and Drug Administration approved Myleran Injection for use in combination with cyclophosphamide as a conditioning regimen prior to allogeneic hematopoietic stem cell transplant in patients with chronic myeloid leukemia. ![]()
Two companies have announced the US launch of a generic busulfan product, Myleran Injection.
Mylan NV and Aspen have partnered to develop Myleran (busulfan) Injection, 60 mg/10 mL (6 mg/mL) Single-dose Vial, a generic version of Otsuka Pharmaceutical’s Busulfex® Injection.
The US Food and Drug Administration approved Myleran Injection for use in combination with cyclophosphamide as a conditioning regimen prior to allogeneic hematopoietic stem cell transplant in patients with chronic myeloid leukemia. ![]()
FDA approves use of heparin products
The US Food and Drug Administration (FDA) has approved use of Mylan NV’s heparin products.
This includes Heparin Sodium Injection at 1000 USP/mL, 5000 USP/mL, 10,000 USP/mL, and 20,000 USP/mL, all of which are packaged in multi-dose vials.
These products should be available in the coming weeks, according to Rajiv Malik, the president of Mylan.
Mylan’s heparin products are approved for the same uses as other heparin products approved in the US.
This includes as prophylaxis and treatment for venous thrombosis and its extension, pulmonary embolism, and peripheral arterial embolism.
The heparin products can also be used to treat atrial fibrillation with embolization, prevent clotting in arterial and cardiac surgery, and diagnose/treat acute and chronic consumptive coagulopathies (disseminated intravascular coagulation).
Low-dose heparin can be used to prevent post-operative deep vein thrombosis and pulmonary embolism in patients undergoing major abdominothoracic surgery or who, for other reasons, are at risk of developing thromboembolic disease.
Heparin can also be used as an anticoagulant in blood transfusions, extracorporeal circulation, and dialysis procedures, as well as in blood samples for laboratory purposes.
“We are very proud of today’s FDA approval of Heparin Sodium Injection, as this approval adds yet another highly complex and difficult-to-manufacture product to our portfolio,” Malik said.
“We expect to make our heparin products available to US hospitals in the coming weeks, further supporting our institutional customers in meeting the needs of their patients who depend on high-quality anticoagulants.” ![]()
The US Food and Drug Administration (FDA) has approved use of Mylan NV’s heparin products.
This includes Heparin Sodium Injection at 1000 USP/mL, 5000 USP/mL, 10,000 USP/mL, and 20,000 USP/mL, all of which are packaged in multi-dose vials.
These products should be available in the coming weeks, according to Rajiv Malik, the president of Mylan.
Mylan’s heparin products are approved for the same uses as other heparin products approved in the US.
This includes as prophylaxis and treatment for venous thrombosis and its extension, pulmonary embolism, and peripheral arterial embolism.
The heparin products can also be used to treat atrial fibrillation with embolization, prevent clotting in arterial and cardiac surgery, and diagnose/treat acute and chronic consumptive coagulopathies (disseminated intravascular coagulation).
Low-dose heparin can be used to prevent post-operative deep vein thrombosis and pulmonary embolism in patients undergoing major abdominothoracic surgery or who, for other reasons, are at risk of developing thromboembolic disease.
Heparin can also be used as an anticoagulant in blood transfusions, extracorporeal circulation, and dialysis procedures, as well as in blood samples for laboratory purposes.
“We are very proud of today’s FDA approval of Heparin Sodium Injection, as this approval adds yet another highly complex and difficult-to-manufacture product to our portfolio,” Malik said.
“We expect to make our heparin products available to US hospitals in the coming weeks, further supporting our institutional customers in meeting the needs of their patients who depend on high-quality anticoagulants.” ![]()
The US Food and Drug Administration (FDA) has approved use of Mylan NV’s heparin products.
This includes Heparin Sodium Injection at 1000 USP/mL, 5000 USP/mL, 10,000 USP/mL, and 20,000 USP/mL, all of which are packaged in multi-dose vials.
These products should be available in the coming weeks, according to Rajiv Malik, the president of Mylan.
Mylan’s heparin products are approved for the same uses as other heparin products approved in the US.
This includes as prophylaxis and treatment for venous thrombosis and its extension, pulmonary embolism, and peripheral arterial embolism.
The heparin products can also be used to treat atrial fibrillation with embolization, prevent clotting in arterial and cardiac surgery, and diagnose/treat acute and chronic consumptive coagulopathies (disseminated intravascular coagulation).
Low-dose heparin can be used to prevent post-operative deep vein thrombosis and pulmonary embolism in patients undergoing major abdominothoracic surgery or who, for other reasons, are at risk of developing thromboembolic disease.
Heparin can also be used as an anticoagulant in blood transfusions, extracorporeal circulation, and dialysis procedures, as well as in blood samples for laboratory purposes.
“We are very proud of today’s FDA approval of Heparin Sodium Injection, as this approval adds yet another highly complex and difficult-to-manufacture product to our portfolio,” Malik said.
“We expect to make our heparin products available to US hospitals in the coming weeks, further supporting our institutional customers in meeting the needs of their patients who depend on high-quality anticoagulants.” ![]()
Drug receives fast track designation for FLT3+ rel/ref AML
The US Food and Drug Administration (FDA) has granted fast track designation to crenolanib for the treatment of patients with FLT3 mutation-positive relapsed or refractory acute myeloid leukemia (AML).
Crenolanib is a benzimidazole type I tyrosine kinase inhibitor (TKI) that selectively inhibits signaling of wild-type and mutant isoforms of FLT3 and PDGFRα/β.
Crenolanib is being developed by Arog Pharmaceuticals, Inc.
The company is preparing for a phase 3, randomized, double-blind trial of crenolanib versus placebo in combination with best supportive care in patients with FLT3+ relapsed or refractory AML.
Results from a phase 2 trial of crenolanib in relapsed/refractory FLT3+ AML were presented at the 2016 ASCO Annual Meeting (abstract 7008).
The trial enrolled 69 patients who had a median age of 60 (range, 21-87). Twenty-nine patients had FLT3 ITD, 29 had ITD and D835, and 11 had D835.
Nineteen patients were TKI-naïve, 39 had received a prior TKI, and 11 had secondary AML.
Patients received crenolanib at 100 mg three times a day (n=43) or 66 mg/m2 three times a day (n=26).
In the TKI-naïve patients, the overall response rate (ORR) was 47% (n=9), and 37% of patients had a complete response (CR) or CR with incomplete count recovery (CRi). The median overall survival (OS) was 238 days (range, 25-547).
In patients who previously received a TKI, the ORR was 28% (n=11), and the CR/CRi rate was 15% (n=6). The median OS was 94 days (range, 8-338).
In patients with secondary AML, the ORR was 9% (n=1, partial response). The median OS in this group was 64 days (range, 27-221).
Treatment-emergent adverse events (all grades and grade 3/4, respectively) included nausea (70%, 9%), vomiting (58%, 9%), diarrhea (56%, 2%), fatigue (36%, 11%), febrile neutropenia (35%, 35%), pneumonia (32%, 23%), peripheral edema (30%, 2%), pleural effusion (21%, 8%), dyspnea (20%, 5%), and epistaxis (20%, 8%).
Two patients discontinued crenolanib due to adverse events. One patient discontinued due to grade 3 fatigue, abdominal pain, and headache. The other discontinued due to grade 3 pneumonia.
There were 2 neutropenic septic deaths, which occurred 2 days and 21 days after the discontinuation of crenolanib.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the new drug application or biologics license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to crenolanib for the treatment of patients with FLT3 mutation-positive relapsed or refractory acute myeloid leukemia (AML).
Crenolanib is a benzimidazole type I tyrosine kinase inhibitor (TKI) that selectively inhibits signaling of wild-type and mutant isoforms of FLT3 and PDGFRα/β.
Crenolanib is being developed by Arog Pharmaceuticals, Inc.
The company is preparing for a phase 3, randomized, double-blind trial of crenolanib versus placebo in combination with best supportive care in patients with FLT3+ relapsed or refractory AML.
Results from a phase 2 trial of crenolanib in relapsed/refractory FLT3+ AML were presented at the 2016 ASCO Annual Meeting (abstract 7008).
The trial enrolled 69 patients who had a median age of 60 (range, 21-87). Twenty-nine patients had FLT3 ITD, 29 had ITD and D835, and 11 had D835.
Nineteen patients were TKI-naïve, 39 had received a prior TKI, and 11 had secondary AML.
Patients received crenolanib at 100 mg three times a day (n=43) or 66 mg/m2 three times a day (n=26).
In the TKI-naïve patients, the overall response rate (ORR) was 47% (n=9), and 37% of patients had a complete response (CR) or CR with incomplete count recovery (CRi). The median overall survival (OS) was 238 days (range, 25-547).
In patients who previously received a TKI, the ORR was 28% (n=11), and the CR/CRi rate was 15% (n=6). The median OS was 94 days (range, 8-338).
In patients with secondary AML, the ORR was 9% (n=1, partial response). The median OS in this group was 64 days (range, 27-221).
Treatment-emergent adverse events (all grades and grade 3/4, respectively) included nausea (70%, 9%), vomiting (58%, 9%), diarrhea (56%, 2%), fatigue (36%, 11%), febrile neutropenia (35%, 35%), pneumonia (32%, 23%), peripheral edema (30%, 2%), pleural effusion (21%, 8%), dyspnea (20%, 5%), and epistaxis (20%, 8%).
Two patients discontinued crenolanib due to adverse events. One patient discontinued due to grade 3 fatigue, abdominal pain, and headache. The other discontinued due to grade 3 pneumonia.
There were 2 neutropenic septic deaths, which occurred 2 days and 21 days after the discontinuation of crenolanib.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the new drug application or biologics license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to crenolanib for the treatment of patients with FLT3 mutation-positive relapsed or refractory acute myeloid leukemia (AML).
Crenolanib is a benzimidazole type I tyrosine kinase inhibitor (TKI) that selectively inhibits signaling of wild-type and mutant isoforms of FLT3 and PDGFRα/β.
Crenolanib is being developed by Arog Pharmaceuticals, Inc.
The company is preparing for a phase 3, randomized, double-blind trial of crenolanib versus placebo in combination with best supportive care in patients with FLT3+ relapsed or refractory AML.
Results from a phase 2 trial of crenolanib in relapsed/refractory FLT3+ AML were presented at the 2016 ASCO Annual Meeting (abstract 7008).
The trial enrolled 69 patients who had a median age of 60 (range, 21-87). Twenty-nine patients had FLT3 ITD, 29 had ITD and D835, and 11 had D835.
Nineteen patients were TKI-naïve, 39 had received a prior TKI, and 11 had secondary AML.
Patients received crenolanib at 100 mg three times a day (n=43) or 66 mg/m2 three times a day (n=26).
In the TKI-naïve patients, the overall response rate (ORR) was 47% (n=9), and 37% of patients had a complete response (CR) or CR with incomplete count recovery (CRi). The median overall survival (OS) was 238 days (range, 25-547).
In patients who previously received a TKI, the ORR was 28% (n=11), and the CR/CRi rate was 15% (n=6). The median OS was 94 days (range, 8-338).
In patients with secondary AML, the ORR was 9% (n=1, partial response). The median OS in this group was 64 days (range, 27-221).
Treatment-emergent adverse events (all grades and grade 3/4, respectively) included nausea (70%, 9%), vomiting (58%, 9%), diarrhea (56%, 2%), fatigue (36%, 11%), febrile neutropenia (35%, 35%), pneumonia (32%, 23%), peripheral edema (30%, 2%), pleural effusion (21%, 8%), dyspnea (20%, 5%), and epistaxis (20%, 8%).
Two patients discontinued crenolanib due to adverse events. One patient discontinued due to grade 3 fatigue, abdominal pain, and headache. The other discontinued due to grade 3 pneumonia.
There were 2 neutropenic septic deaths, which occurred 2 days and 21 days after the discontinuation of crenolanib.
About fast track designation
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review. In addition, the company developing the product may be allowed to submit sections of the new drug application or biologics license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA. ![]()
FDA grants priority review to NDA for avatrombopag
The US Food and Drug Administration (FDA) has granted priority review to the new drug application (NDA) for avatrombopag.
Avatrombopag is a second-generation thrombopoietin receptor agonist that is intended to address the limitations of existing treatments for thrombocytopenia.
With this NDA, Dova Pharmaceuticals, Inc., is seeking approval of avatrombopag for the treatment of thrombocytopenia in patients with chronic liver disease who are scheduled to undergo a procedure.
The FDA expects to make a decision on the NDA by May 21, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Phase 3 trials
The NDA submission for avatrombopag is supported by 2 identically designed phase 3 trials, ADAPT 1 and ADAPT 2. Results from these trials were presented at the 2017 American Association for the Study of Liver Disease (AASLD) Meeting last month (abstract 217).
The studies randomized 435 patients with thrombocytopenia and chronic liver disease who were scheduled to undergo a procedure.
Patients with low baseline platelet counts (<40x 109/L) were randomized to receive 60 mg of avatrombopag or placebo daily for 5 days.
Patients with higher baseline platelet counts (40 to <50 x 109/L) were randomized to receive 40 mg of avatrombopag or placebo daily for 5 days.
Patients underwent their procedures 5 to 8 days after their last dose of avatrombopag.
In ADAPT-1, 85 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 78 controls completed the study.
In ADAPT-2, 68 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 68 controls completed the study.
Efficacy
The primary efficacy endpoint of these trials was the proportion of patients who did not require any bleeding rescue up to 7 days post-procedure. Bleeding rescue included platelet transfusion, fresh frozen plasma, cryoprecipitate, vitamin K (phytonadione), desmopressin, recombinant activated factor VII, aminocaproicacid, tranexamic acid, whole blood transfusion, packed red cell transfusion, surgical intervention, or interventional radiology.
In ADAPT-1, the primary endpoint was achieved by 66% of patients who received avatrombopag at 60 mg and 23% of those who received placebo in the low-platelet-count cohort (P<0.0001). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 38% of controls in the higher-platelet-count cohort (P<0.0001).
In ADAPT-2, the primary endpoint was achieved by 69% of patients who received avatrombopag at 60 mg and 35% of those who received placebo in the low-platelet-count cohort (P<0.0006). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 33% of controls in the higher- platelet-count cohort (P<0.0001).
A secondary efficacy endpoint was the proportion of patients achieving the target platelet count (≥50 x 109/L).
In ADAPT-1, this endpoint was met by 69% of patients who received avatrombopag at 60 mg and 4% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 88% of patients who received avatrombopag at 40 mg and 21% of controls in the higher-platelet-count cohort (P<0.0001)
In ADAPT-2, this endpoint was met by 67% of patients who received avatrombopag at 60 mg and 7% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 93% of patients who received avatrombopag at 40 mg and 39% of controls in the higher-platelet-count cohort (P<0.0001).
Safety
The researchers pooled safety data from the 2 trials.
Treatment-emergent adverse events (AEs) occurred in 58.2% of controls and 56% of avatrombopag-treated patients in the low-platelet-count cohort (60 mg). Treatment-emergent AEs also occurred in 50.8% of controls and 51.3% of avatrombopag-treated patients in the higher-platelet-count cohort (40 mg).
The most frequently reported treatment-emergent AEs were pyrexia, abdominal pain, nausea, headache, diarrhea, and fatigue.
One patient experienced partial portal vein thrombosis that was considered non-serious and potentially related to avatrombopag.
Treatment-related AEs occurred in 17.6% of controls and 11.3% of avatrombopag-treated patients in the low-platelet-count cohort. Treatment-related AEs also occurred in 6.2% of controls and 7% of avatrombopag-treated patients in the higher-platelet-count cohort.
Serious AEs occurred in 13.2%, 6.9%, 3.1%, and 7.8%, respectively.
There were 3 deaths—2 in the 40 mg avatrombopag arm in ADAPT-1 and 1 in the control group in ADAPT-2. None of the deaths was considered treatment-related.
Future directions
Dova Pharmaceuticals, Inc., is planning to explore the potential use of avatrombopag in a broader population of patients with thrombocytopenia. This includes patients undergoing surgical procedures associated with a high risk of bleeding and patients who develop thrombocytopenia after receiving chemotherapy.
In addition, the company is exploring a potential regulatory approval pathway for avatrombopag for the treatment of adults with chronic immune thrombocytopenic purpura based on results from a completed phase 3 trial in this patient population. ![]()
The US Food and Drug Administration (FDA) has granted priority review to the new drug application (NDA) for avatrombopag.
Avatrombopag is a second-generation thrombopoietin receptor agonist that is intended to address the limitations of existing treatments for thrombocytopenia.
With this NDA, Dova Pharmaceuticals, Inc., is seeking approval of avatrombopag for the treatment of thrombocytopenia in patients with chronic liver disease who are scheduled to undergo a procedure.
The FDA expects to make a decision on the NDA by May 21, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Phase 3 trials
The NDA submission for avatrombopag is supported by 2 identically designed phase 3 trials, ADAPT 1 and ADAPT 2. Results from these trials were presented at the 2017 American Association for the Study of Liver Disease (AASLD) Meeting last month (abstract 217).
The studies randomized 435 patients with thrombocytopenia and chronic liver disease who were scheduled to undergo a procedure.
Patients with low baseline platelet counts (<40x 109/L) were randomized to receive 60 mg of avatrombopag or placebo daily for 5 days.
Patients with higher baseline platelet counts (40 to <50 x 109/L) were randomized to receive 40 mg of avatrombopag or placebo daily for 5 days.
Patients underwent their procedures 5 to 8 days after their last dose of avatrombopag.
In ADAPT-1, 85 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 78 controls completed the study.
In ADAPT-2, 68 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 68 controls completed the study.
Efficacy
The primary efficacy endpoint of these trials was the proportion of patients who did not require any bleeding rescue up to 7 days post-procedure. Bleeding rescue included platelet transfusion, fresh frozen plasma, cryoprecipitate, vitamin K (phytonadione), desmopressin, recombinant activated factor VII, aminocaproicacid, tranexamic acid, whole blood transfusion, packed red cell transfusion, surgical intervention, or interventional radiology.
In ADAPT-1, the primary endpoint was achieved by 66% of patients who received avatrombopag at 60 mg and 23% of those who received placebo in the low-platelet-count cohort (P<0.0001). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 38% of controls in the higher-platelet-count cohort (P<0.0001).
In ADAPT-2, the primary endpoint was achieved by 69% of patients who received avatrombopag at 60 mg and 35% of those who received placebo in the low-platelet-count cohort (P<0.0006). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 33% of controls in the higher- platelet-count cohort (P<0.0001).
A secondary efficacy endpoint was the proportion of patients achieving the target platelet count (≥50 x 109/L).
In ADAPT-1, this endpoint was met by 69% of patients who received avatrombopag at 60 mg and 4% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 88% of patients who received avatrombopag at 40 mg and 21% of controls in the higher-platelet-count cohort (P<0.0001)
In ADAPT-2, this endpoint was met by 67% of patients who received avatrombopag at 60 mg and 7% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 93% of patients who received avatrombopag at 40 mg and 39% of controls in the higher-platelet-count cohort (P<0.0001).
Safety
The researchers pooled safety data from the 2 trials.
Treatment-emergent adverse events (AEs) occurred in 58.2% of controls and 56% of avatrombopag-treated patients in the low-platelet-count cohort (60 mg). Treatment-emergent AEs also occurred in 50.8% of controls and 51.3% of avatrombopag-treated patients in the higher-platelet-count cohort (40 mg).
The most frequently reported treatment-emergent AEs were pyrexia, abdominal pain, nausea, headache, diarrhea, and fatigue.
One patient experienced partial portal vein thrombosis that was considered non-serious and potentially related to avatrombopag.
Treatment-related AEs occurred in 17.6% of controls and 11.3% of avatrombopag-treated patients in the low-platelet-count cohort. Treatment-related AEs also occurred in 6.2% of controls and 7% of avatrombopag-treated patients in the higher-platelet-count cohort.
Serious AEs occurred in 13.2%, 6.9%, 3.1%, and 7.8%, respectively.
There were 3 deaths—2 in the 40 mg avatrombopag arm in ADAPT-1 and 1 in the control group in ADAPT-2. None of the deaths was considered treatment-related.
Future directions
Dova Pharmaceuticals, Inc., is planning to explore the potential use of avatrombopag in a broader population of patients with thrombocytopenia. This includes patients undergoing surgical procedures associated with a high risk of bleeding and patients who develop thrombocytopenia after receiving chemotherapy.
In addition, the company is exploring a potential regulatory approval pathway for avatrombopag for the treatment of adults with chronic immune thrombocytopenic purpura based on results from a completed phase 3 trial in this patient population. ![]()
The US Food and Drug Administration (FDA) has granted priority review to the new drug application (NDA) for avatrombopag.
Avatrombopag is a second-generation thrombopoietin receptor agonist that is intended to address the limitations of existing treatments for thrombocytopenia.
With this NDA, Dova Pharmaceuticals, Inc., is seeking approval of avatrombopag for the treatment of thrombocytopenia in patients with chronic liver disease who are scheduled to undergo a procedure.
The FDA expects to make a decision on the NDA by May 21, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Phase 3 trials
The NDA submission for avatrombopag is supported by 2 identically designed phase 3 trials, ADAPT 1 and ADAPT 2. Results from these trials were presented at the 2017 American Association for the Study of Liver Disease (AASLD) Meeting last month (abstract 217).
The studies randomized 435 patients with thrombocytopenia and chronic liver disease who were scheduled to undergo a procedure.
Patients with low baseline platelet counts (<40x 109/L) were randomized to receive 60 mg of avatrombopag or placebo daily for 5 days.
Patients with higher baseline platelet counts (40 to <50 x 109/L) were randomized to receive 40 mg of avatrombopag or placebo daily for 5 days.
Patients underwent their procedures 5 to 8 days after their last dose of avatrombopag.
In ADAPT-1, 85 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 78 controls completed the study.
In ADAPT-2, 68 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 68 controls completed the study.
Efficacy
The primary efficacy endpoint of these trials was the proportion of patients who did not require any bleeding rescue up to 7 days post-procedure. Bleeding rescue included platelet transfusion, fresh frozen plasma, cryoprecipitate, vitamin K (phytonadione), desmopressin, recombinant activated factor VII, aminocaproicacid, tranexamic acid, whole blood transfusion, packed red cell transfusion, surgical intervention, or interventional radiology.
In ADAPT-1, the primary endpoint was achieved by 66% of patients who received avatrombopag at 60 mg and 23% of those who received placebo in the low-platelet-count cohort (P<0.0001). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 38% of controls in the higher-platelet-count cohort (P<0.0001).
In ADAPT-2, the primary endpoint was achieved by 69% of patients who received avatrombopag at 60 mg and 35% of those who received placebo in the low-platelet-count cohort (P<0.0006). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 33% of controls in the higher- platelet-count cohort (P<0.0001).
A secondary efficacy endpoint was the proportion of patients achieving the target platelet count (≥50 x 109/L).
In ADAPT-1, this endpoint was met by 69% of patients who received avatrombopag at 60 mg and 4% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 88% of patients who received avatrombopag at 40 mg and 21% of controls in the higher-platelet-count cohort (P<0.0001)
In ADAPT-2, this endpoint was met by 67% of patients who received avatrombopag at 60 mg and 7% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 93% of patients who received avatrombopag at 40 mg and 39% of controls in the higher-platelet-count cohort (P<0.0001).
Safety
The researchers pooled safety data from the 2 trials.
Treatment-emergent adverse events (AEs) occurred in 58.2% of controls and 56% of avatrombopag-treated patients in the low-platelet-count cohort (60 mg). Treatment-emergent AEs also occurred in 50.8% of controls and 51.3% of avatrombopag-treated patients in the higher-platelet-count cohort (40 mg).
The most frequently reported treatment-emergent AEs were pyrexia, abdominal pain, nausea, headache, diarrhea, and fatigue.
One patient experienced partial portal vein thrombosis that was considered non-serious and potentially related to avatrombopag.
Treatment-related AEs occurred in 17.6% of controls and 11.3% of avatrombopag-treated patients in the low-platelet-count cohort. Treatment-related AEs also occurred in 6.2% of controls and 7% of avatrombopag-treated patients in the higher-platelet-count cohort.
Serious AEs occurred in 13.2%, 6.9%, 3.1%, and 7.8%, respectively.
There were 3 deaths—2 in the 40 mg avatrombopag arm in ADAPT-1 and 1 in the control group in ADAPT-2. None of the deaths was considered treatment-related.
Future directions
Dova Pharmaceuticals, Inc., is planning to explore the potential use of avatrombopag in a broader population of patients with thrombocytopenia. This includes patients undergoing surgical procedures associated with a high risk of bleeding and patients who develop thrombocytopenia after receiving chemotherapy.
In addition, the company is exploring a potential regulatory approval pathway for avatrombopag for the treatment of adults with chronic immune thrombocytopenic purpura based on results from a completed phase 3 trial in this patient population.
Withdrawn drug receives orphan designation for HA
The US Food and Drug Administration (FDA) has granted orphan drug designation to rofecoxib (TRM-201) as a potential treatment for degenerative joint disease in hemophilia, also known as hemophilic arthropathy (HA).
Rofecoxib is a COX-2 selective non-steroidal anti-inflammatory drug (NSAID) that was previously sold in the US under the name Vioxx.
Vioxx was FDA-approved to relieve the signs and symptoms of osteoarthritis, manage acute pain in adults, and treat primary dysmenorrhea.
Merck & Co. pulled Vioxx from the US market in 2004 due to safety concerns. The drug was shown to increase a person’s risk of cardiovascular events, including heart attack and stroke.
Now, Tremeau Pharmaceuticals, Inc., is working to bring rofecoxib back to market to treat patients with HA.
HA patients should not receive traditional NSAIDs due to their effects on platelet aggregation and the risk of gastrointestinal ulcers associated with these drugs. Therefore, high potency opioids are the current standard of care in HA.
“Being granted an orphan drug designation for rofecoxib by FDA is an important regulatory milestone for Tremeau and affirms our strategy of providing non-opioid pain treatments for rare diseases like hemophilic arthropathy,” said Bradford C. Sippy, chief executive officer of Tremeau.
Sippy is a former Merck employee who helped with the recall of Vioxx and knew the final patent protecting the drug’s monopoly was expiring this fall.
When it stopped making Vioxx, Merck was facing thousands of lawsuits from people claiming the drug caused their heart attacks or strokes.
Merck’s own research showed the drug doubled those risks, but lawyers for patients claimed the company downplayed or concealed that. Merck initially fought the lawsuits but, in 2007, agreed to a $4.85 billion settlement.
If approved to treat HA, rofecoxib would carry a warning about the increased risk of heart attack and stroke associated with the drug.
Although the orphan designation for rofecoxib is a step toward FDA approval, Sippy said Tremeau must still raise $25 million or more to fund trials of the drug in hemophilia patients.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to rofecoxib (TRM-201) as a potential treatment for degenerative joint disease in hemophilia, also known as hemophilic arthropathy (HA).
Rofecoxib is a COX-2 selective non-steroidal anti-inflammatory drug (NSAID) that was previously sold in the US under the name Vioxx.
Vioxx was FDA-approved to relieve the signs and symptoms of osteoarthritis, manage acute pain in adults, and treat primary dysmenorrhea.
Merck & Co. pulled Vioxx from the US market in 2004 due to safety concerns. The drug was shown to increase a person’s risk of cardiovascular events, including heart attack and stroke.
Now, Tremeau Pharmaceuticals, Inc., is working to bring rofecoxib back to market to treat patients with HA.
HA patients should not receive traditional NSAIDs due to their effects on platelet aggregation and the risk of gastrointestinal ulcers associated with these drugs. Therefore, high potency opioids are the current standard of care in HA.
“Being granted an orphan drug designation for rofecoxib by FDA is an important regulatory milestone for Tremeau and affirms our strategy of providing non-opioid pain treatments for rare diseases like hemophilic arthropathy,” said Bradford C. Sippy, chief executive officer of Tremeau.
Sippy is a former Merck employee who helped with the recall of Vioxx and knew the final patent protecting the drug’s monopoly was expiring this fall.
When it stopped making Vioxx, Merck was facing thousands of lawsuits from people claiming the drug caused their heart attacks or strokes.
Merck’s own research showed the drug doubled those risks, but lawyers for patients claimed the company downplayed or concealed that. Merck initially fought the lawsuits but, in 2007, agreed to a $4.85 billion settlement.
If approved to treat HA, rofecoxib would carry a warning about the increased risk of heart attack and stroke associated with the drug.
Although the orphan designation for rofecoxib is a step toward FDA approval, Sippy said Tremeau must still raise $25 million or more to fund trials of the drug in hemophilia patients.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to rofecoxib (TRM-201) as a potential treatment for degenerative joint disease in hemophilia, also known as hemophilic arthropathy (HA).
Rofecoxib is a COX-2 selective non-steroidal anti-inflammatory drug (NSAID) that was previously sold in the US under the name Vioxx.
Vioxx was FDA-approved to relieve the signs and symptoms of osteoarthritis, manage acute pain in adults, and treat primary dysmenorrhea.
Merck & Co. pulled Vioxx from the US market in 2004 due to safety concerns. The drug was shown to increase a person’s risk of cardiovascular events, including heart attack and stroke.
Now, Tremeau Pharmaceuticals, Inc., is working to bring rofecoxib back to market to treat patients with HA.
HA patients should not receive traditional NSAIDs due to their effects on platelet aggregation and the risk of gastrointestinal ulcers associated with these drugs. Therefore, high potency opioids are the current standard of care in HA.
“Being granted an orphan drug designation for rofecoxib by FDA is an important regulatory milestone for Tremeau and affirms our strategy of providing non-opioid pain treatments for rare diseases like hemophilic arthropathy,” said Bradford C. Sippy, chief executive officer of Tremeau.
Sippy is a former Merck employee who helped with the recall of Vioxx and knew the final patent protecting the drug’s monopoly was expiring this fall.
When it stopped making Vioxx, Merck was facing thousands of lawsuits from people claiming the drug caused their heart attacks or strokes.
Merck’s own research showed the drug doubled those risks, but lawyers for patients claimed the company downplayed or concealed that. Merck initially fought the lawsuits but, in 2007, agreed to a $4.85 billion settlement.
If approved to treat HA, rofecoxib would carry a warning about the increased risk of heart attack and stroke associated with the drug.
Although the orphan designation for rofecoxib is a step toward FDA approval, Sippy said Tremeau must still raise $25 million or more to fund trials of the drug in hemophilia patients.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
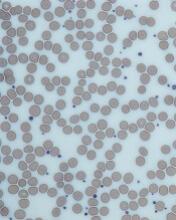
Nilotinib approved to treat kids with CML in EU
The European Commission has approved nilotinib (Tasigna®) for the treatment of pediatric patients.
The drug is now approved to treat children age 2 and older with newly diagnosed, Philadelphia chromosome-positive (Ph+), chronic phase (CP) chronic myeloid leukemia (CML) or Ph+ CP-CML with resistance or intolerance to prior therapy, including imatinib.
Nilotinib is the only second-generation tyrosine kinase inhibitor currently approved in the European Union (EU) for the treatment of Ph+ CP-CML in children. The approval applies to all EU member states.
According to Novartis, the expanded indication for nilotinib is based on 2 prospective studies of the drug in children with Ph+ CP-CML, which were part of a formal “pediatric investigation plan” agreed upon with the European Medicines Agency.
The company said 69 patients received nilotinib in these studies. The patients ranged in age from 2 to 18. They had either newly diagnosed Ph+ CP-CML or Ph+ CP-CML with resistance or intolerance to prior therapy, including imatinib.
In the newly diagnosed patients, the major molecular response (MMR) rate was 60.0% (95% CI: 38.7, 78.9) at 12 cycles, with 15 patients achieving MMR.
In patients with resistance or intolerance to prior therapy, the MMR rate was 40.9% (95% CI: 26.3, 56.8) at 12 cycles, with 18 patients being in MMR.
In newly diagnosed patients, the cumulative MMR rate was 64.0% by cycle 12. In patients with resistance or intolerance to prior therapy, the cumulative MMR rate was 47.7% by cycle 12.
Adverse events were generally consistent with those observed in adults, with the exception of hyperbilirubinemia and transaminase elevation, which were reported at a higher frequency than in adults.
The rate of grade 3/4 hyperbilirubinemia was 13.0%, the rate of grade 3/4 AST elevation was 1.4%, and the rate of grade 3/4 ALT elevation was 8.7%.
There were no deaths on treatment or after treatment discontinuation.
The European Commission has approved nilotinib (Tasigna®) for the treatment of pediatric patients.
The drug is now approved to treat children age 2 and older with newly diagnosed, Philadelphia chromosome-positive (Ph+), chronic phase (CP) chronic myeloid leukemia (CML) or Ph+ CP-CML with resistance or intolerance to prior therapy, including imatinib.
Nilotinib is the only second-generation tyrosine kinase inhibitor currently approved in the European Union (EU) for the treatment of Ph+ CP-CML in children. The approval applies to all EU member states.
According to Novartis, the expanded indication for nilotinib is based on 2 prospective studies of the drug in children with Ph+ CP-CML, which were part of a formal “pediatric investigation plan” agreed upon with the European Medicines Agency.
The company said 69 patients received nilotinib in these studies. The patients ranged in age from 2 to 18. They had either newly diagnosed Ph+ CP-CML or Ph+ CP-CML with resistance or intolerance to prior therapy, including imatinib.
In the newly diagnosed patients, the major molecular response (MMR) rate was 60.0% (95% CI: 38.7, 78.9) at 12 cycles, with 15 patients achieving MMR.
In patients with resistance or intolerance to prior therapy, the MMR rate was 40.9% (95% CI: 26.3, 56.8) at 12 cycles, with 18 patients being in MMR.
In newly diagnosed patients, the cumulative MMR rate was 64.0% by cycle 12. In patients with resistance or intolerance to prior therapy, the cumulative MMR rate was 47.7% by cycle 12.
Adverse events were generally consistent with those observed in adults, with the exception of hyperbilirubinemia and transaminase elevation, which were reported at a higher frequency than in adults.
The rate of grade 3/4 hyperbilirubinemia was 13.0%, the rate of grade 3/4 AST elevation was 1.4%, and the rate of grade 3/4 ALT elevation was 8.7%.
There were no deaths on treatment or after treatment discontinuation.
The European Commission has approved nilotinib (Tasigna®) for the treatment of pediatric patients.
The drug is now approved to treat children age 2 and older with newly diagnosed, Philadelphia chromosome-positive (Ph+), chronic phase (CP) chronic myeloid leukemia (CML) or Ph+ CP-CML with resistance or intolerance to prior therapy, including imatinib.
Nilotinib is the only second-generation tyrosine kinase inhibitor currently approved in the European Union (EU) for the treatment of Ph+ CP-CML in children. The approval applies to all EU member states.
According to Novartis, the expanded indication for nilotinib is based on 2 prospective studies of the drug in children with Ph+ CP-CML, which were part of a formal “pediatric investigation plan” agreed upon with the European Medicines Agency.
The company said 69 patients received nilotinib in these studies. The patients ranged in age from 2 to 18. They had either newly diagnosed Ph+ CP-CML or Ph+ CP-CML with resistance or intolerance to prior therapy, including imatinib.
In the newly diagnosed patients, the major molecular response (MMR) rate was 60.0% (95% CI: 38.7, 78.9) at 12 cycles, with 15 patients achieving MMR.
In patients with resistance or intolerance to prior therapy, the MMR rate was 40.9% (95% CI: 26.3, 56.8) at 12 cycles, with 18 patients being in MMR.
In newly diagnosed patients, the cumulative MMR rate was 64.0% by cycle 12. In patients with resistance or intolerance to prior therapy, the cumulative MMR rate was 47.7% by cycle 12.
Adverse events were generally consistent with those observed in adults, with the exception of hyperbilirubinemia and transaminase elevation, which were reported at a higher frequency than in adults.
The rate of grade 3/4 hyperbilirubinemia was 13.0%, the rate of grade 3/4 AST elevation was 1.4%, and the rate of grade 3/4 ALT elevation was 8.7%.
There were no deaths on treatment or after treatment discontinuation.
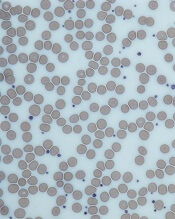
Product approved to treat patients with hemophilia A and inhibitors
The US Food and Drug Administration (FDA) has approved use of emicizumab-kxwh (Hemlibra®), a bispecific factor IXa- and factor X-directed antibody.
Emicizumab is approved as routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults and children who have hemophilia A and factor VIII (FVIII) inhibitors.
Emicizumab can be self-administered once-weekly via subcutaneous injection.
The labeling for emicizumab contains a boxed warning noting that patients who received emicizumab in conjunction with activated prothrombin complex concentrate developed thrombotic microangiopathy (TMA) and thromboembolic events (TEs).
Therefore, patients should discontinue prophylactic use of bypassing agents (BPAs) the day before starting prophylaxis with emicizumab.
The FDA granted the approval of emicizumab to Genentech, Inc. The agency granted the application for emicizumab priority review, and the product received breakthrough therapy and orphan drug designations.
Access to emicizumab
According to Genentech, emicizumab will be available shortly.
The company said it will be offering comprehensive services to help minimize barriers to access and reimbursement. Patients can call 866-436-5427 (866-HEMLIBRA) for more information.
For people who qualify, Genentech plans to offer patient assistance programs through Genentech Access Solutions. More information is available at 866-422-2377 (866-4ACCESS) or http://www.Genentech-Access.com.
Emicizumab trials
The biologics license application for emicizumab was supported by results from a pair of phase 3 studies—HAVEN 1 and HAVEN 2.
Results from HAVEN 1 were published in NEJM and presented at the 26th ISTH Congress in July. Interim results from HAVEN 2 were presented at ISTH as well.
HAVEN 1
The study enrolled 109 patients (age 12 and older) with hemophilia A and FVIII inhibitors who were previously treated with BPAs on-demand or as prophylaxis.
The patients were randomized to receive emicizumab prophylaxis or no prophylaxis. On-demand treatment of breakthrough bleeds with BPAs was allowed.
There was a significant reduction in treated bleeds of 87% with emicizumab prophylaxis compared to no prophylaxis (95% CI: 72.3; 94.3, P<0.0001). And there was an 80% reduction in all bleeds with emicizumab (95% CI: 62.5; 89.8, P<0.0001).
Adverse events occurring in at least 5% of patients treated with emicizumab were local injection site reactions, headache, fatigue, upper respiratory tract infection, and arthralgia.
Two patients experienced TEs, and 3 had TMA while receiving emicizumab prophylaxis and more than 100 u/kg/day of activated prothrombin complex concentrate, on average, for 24 hours or more before the event. Two of these patients had also received recombinant factor VIIa.
Neither TE required anticoagulation therapy, and 1 patient restarted emicizumab. The cases of TMA observed were transient, and 1 patient restarted emicizumab.
HAVEN 2
In this single-arm trial, researchers evaluated emicizumab prophylaxis in children younger than 12 years of age who had hemophilia A with FVIII inhibitors.
The interim efficacy analysis, after at least 12 weeks of treatment, included 23 children.
After a median observation time of 38.1 weeks, 87% (95% CI: 66.4; 97.2) of children who received emicizumab experienced 0 treated bleeds. The percentage with 0 treated or non-treated bleeds was lower, at 34.8% (95% CI: 16.4; 57.3).
The most common adverse events (observed in at least 10% of patients) were mild injection site reactions and nasopharyngitis. No TEs or TMAs were observed.
HAVEN 3 and 4
Emicizumab is now being studied in 2 additional phase 3 trials.
In HAVEN 3, researchers are evaluating emicizumab prophylaxis dosed once weekly or once every other week in patients age 12 and older with hemophilia A without FVIII inhibitors.
In HAVEN 4, researchers are evaluating emicizumab prophylaxis dosed every 4 weeks in patients age 12 and older with hemophilia A, with or without inhibitors.
The US Food and Drug Administration (FDA) has approved use of emicizumab-kxwh (Hemlibra®), a bispecific factor IXa- and factor X-directed antibody.
Emicizumab is approved as routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults and children who have hemophilia A and factor VIII (FVIII) inhibitors.
Emicizumab can be self-administered once-weekly via subcutaneous injection.
The labeling for emicizumab contains a boxed warning noting that patients who received emicizumab in conjunction with activated prothrombin complex concentrate developed thrombotic microangiopathy (TMA) and thromboembolic events (TEs).
Therefore, patients should discontinue prophylactic use of bypassing agents (BPAs) the day before starting prophylaxis with emicizumab.
The FDA granted the approval of emicizumab to Genentech, Inc. The agency granted the application for emicizumab priority review, and the product received breakthrough therapy and orphan drug designations.
Access to emicizumab
According to Genentech, emicizumab will be available shortly.
The company said it will be offering comprehensive services to help minimize barriers to access and reimbursement. Patients can call 866-436-5427 (866-HEMLIBRA) for more information.
For people who qualify, Genentech plans to offer patient assistance programs through Genentech Access Solutions. More information is available at 866-422-2377 (866-4ACCESS) or http://www.Genentech-Access.com.
Emicizumab trials
The biologics license application for emicizumab was supported by results from a pair of phase 3 studies—HAVEN 1 and HAVEN 2.
Results from HAVEN 1 were published in NEJM and presented at the 26th ISTH Congress in July. Interim results from HAVEN 2 were presented at ISTH as well.
HAVEN 1
The study enrolled 109 patients (age 12 and older) with hemophilia A and FVIII inhibitors who were previously treated with BPAs on-demand or as prophylaxis.
The patients were randomized to receive emicizumab prophylaxis or no prophylaxis. On-demand treatment of breakthrough bleeds with BPAs was allowed.
There was a significant reduction in treated bleeds of 87% with emicizumab prophylaxis compared to no prophylaxis (95% CI: 72.3; 94.3, P<0.0001). And there was an 80% reduction in all bleeds with emicizumab (95% CI: 62.5; 89.8, P<0.0001).
Adverse events occurring in at least 5% of patients treated with emicizumab were local injection site reactions, headache, fatigue, upper respiratory tract infection, and arthralgia.
Two patients experienced TEs, and 3 had TMA while receiving emicizumab prophylaxis and more than 100 u/kg/day of activated prothrombin complex concentrate, on average, for 24 hours or more before the event. Two of these patients had also received recombinant factor VIIa.
Neither TE required anticoagulation therapy, and 1 patient restarted emicizumab. The cases of TMA observed were transient, and 1 patient restarted emicizumab.
HAVEN 2
In this single-arm trial, researchers evaluated emicizumab prophylaxis in children younger than 12 years of age who had hemophilia A with FVIII inhibitors.
The interim efficacy analysis, after at least 12 weeks of treatment, included 23 children.
After a median observation time of 38.1 weeks, 87% (95% CI: 66.4; 97.2) of children who received emicizumab experienced 0 treated bleeds. The percentage with 0 treated or non-treated bleeds was lower, at 34.8% (95% CI: 16.4; 57.3).
The most common adverse events (observed in at least 10% of patients) were mild injection site reactions and nasopharyngitis. No TEs or TMAs were observed.
HAVEN 3 and 4
Emicizumab is now being studied in 2 additional phase 3 trials.
In HAVEN 3, researchers are evaluating emicizumab prophylaxis dosed once weekly or once every other week in patients age 12 and older with hemophilia A without FVIII inhibitors.
In HAVEN 4, researchers are evaluating emicizumab prophylaxis dosed every 4 weeks in patients age 12 and older with hemophilia A, with or without inhibitors.
The US Food and Drug Administration (FDA) has approved use of emicizumab-kxwh (Hemlibra®), a bispecific factor IXa- and factor X-directed antibody.
Emicizumab is approved as routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults and children who have hemophilia A and factor VIII (FVIII) inhibitors.
Emicizumab can be self-administered once-weekly via subcutaneous injection.
The labeling for emicizumab contains a boxed warning noting that patients who received emicizumab in conjunction with activated prothrombin complex concentrate developed thrombotic microangiopathy (TMA) and thromboembolic events (TEs).
Therefore, patients should discontinue prophylactic use of bypassing agents (BPAs) the day before starting prophylaxis with emicizumab.
The FDA granted the approval of emicizumab to Genentech, Inc. The agency granted the application for emicizumab priority review, and the product received breakthrough therapy and orphan drug designations.
Access to emicizumab
According to Genentech, emicizumab will be available shortly.
The company said it will be offering comprehensive services to help minimize barriers to access and reimbursement. Patients can call 866-436-5427 (866-HEMLIBRA) for more information.
For people who qualify, Genentech plans to offer patient assistance programs through Genentech Access Solutions. More information is available at 866-422-2377 (866-4ACCESS) or http://www.Genentech-Access.com.
Emicizumab trials
The biologics license application for emicizumab was supported by results from a pair of phase 3 studies—HAVEN 1 and HAVEN 2.
Results from HAVEN 1 were published in NEJM and presented at the 26th ISTH Congress in July. Interim results from HAVEN 2 were presented at ISTH as well.
HAVEN 1
The study enrolled 109 patients (age 12 and older) with hemophilia A and FVIII inhibitors who were previously treated with BPAs on-demand or as prophylaxis.
The patients were randomized to receive emicizumab prophylaxis or no prophylaxis. On-demand treatment of breakthrough bleeds with BPAs was allowed.
There was a significant reduction in treated bleeds of 87% with emicizumab prophylaxis compared to no prophylaxis (95% CI: 72.3; 94.3, P<0.0001). And there was an 80% reduction in all bleeds with emicizumab (95% CI: 62.5; 89.8, P<0.0001).
Adverse events occurring in at least 5% of patients treated with emicizumab were local injection site reactions, headache, fatigue, upper respiratory tract infection, and arthralgia.
Two patients experienced TEs, and 3 had TMA while receiving emicizumab prophylaxis and more than 100 u/kg/day of activated prothrombin complex concentrate, on average, for 24 hours or more before the event. Two of these patients had also received recombinant factor VIIa.
Neither TE required anticoagulation therapy, and 1 patient restarted emicizumab. The cases of TMA observed were transient, and 1 patient restarted emicizumab.
HAVEN 2
In this single-arm trial, researchers evaluated emicizumab prophylaxis in children younger than 12 years of age who had hemophilia A with FVIII inhibitors.
The interim efficacy analysis, after at least 12 weeks of treatment, included 23 children.
After a median observation time of 38.1 weeks, 87% (95% CI: 66.4; 97.2) of children who received emicizumab experienced 0 treated bleeds. The percentage with 0 treated or non-treated bleeds was lower, at 34.8% (95% CI: 16.4; 57.3).
The most common adverse events (observed in at least 10% of patients) were mild injection site reactions and nasopharyngitis. No TEs or TMAs were observed.
HAVEN 3 and 4
Emicizumab is now being studied in 2 additional phase 3 trials.
In HAVEN 3, researchers are evaluating emicizumab prophylaxis dosed once weekly or once every other week in patients age 12 and older with hemophilia A without FVIII inhibitors.
In HAVEN 4, researchers are evaluating emicizumab prophylaxis dosed every 4 weeks in patients age 12 and older with hemophilia A, with or without inhibitors.