User login
Healthcare spending doesn’t impact cancer outcomes

receiving treatment
Photo by Rhoda Baer
A new study suggests that higher healthcare spending is not associated with better cancer outcomes in the US, but state-level wealth is.
Researchers found that higher gross domestic product (GDP) per capita was associated with lower mortality for all cancers, colorectal cancer, and breast cancer.
However, higher healthcare spending was only associated with lower mortality for breast cancer—not colorectal cancer or all cancers combined.
Jad Chahoud, MD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues reported these findings in JNCCN.
To investigate the implications of socioeconomic status and health expenditures on cancer outcomes, the researchers conducted an ecological study at the state level for 3 distinct patient populations: breast cancer, colorectal cancer, and all-cancer patients.
The team extracted data on GDP and healthcare spending per capita from the 2009 Bureau of Economic Analysis and the Centers for Medicare & Medicaid Services, respectively.
Using data from the National Cancer Institute, the researchers retrieved breast, colorectal, and all-cancer age-adjusted rates and computed mortality/incidence (M/I) ratios for each population.
The team found that higher GDP per capita was significantly associated with lower M/I ratios for all cancers (rho=–0.4406; P=0.0017), breast cancer (rho=–0.3605; P=0.0118), and colorectal cancer (rho=–0.3612; P=0.0117).
But higher healthcare spending was only associated with a lower M/I ratio for breast cancer (rho=–0.4237; P=0.0027).
In a related editorial, Melissa A. Simon, MD, of Northwestern University Feinberg School of Medicine in Chicago, Illinois, and her colleagues pointed out that the data in this study predate the Affordable Care Act. So the results may not reflect the current state of affairs in the US.
The authors also said these data should not be used to guide—or misguide—policy makers to cap or decrease spending for certain health issues.
“Increased spending does not necessarily improve quality of care, but capping or cutting spending on healthcare does not necessarily solve problems either,” the authors wrote.
In a counterpoint editorial, Dr Chahoud and his colleagues said the goal of their study was not to misguide policy makers.
The team doesn’t recommend capping healthcare spending. Rather, they want to see “smart” spending that will have an impact on patient outcomes. ![]()

receiving treatment
Photo by Rhoda Baer
A new study suggests that higher healthcare spending is not associated with better cancer outcomes in the US, but state-level wealth is.
Researchers found that higher gross domestic product (GDP) per capita was associated with lower mortality for all cancers, colorectal cancer, and breast cancer.
However, higher healthcare spending was only associated with lower mortality for breast cancer—not colorectal cancer or all cancers combined.
Jad Chahoud, MD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues reported these findings in JNCCN.
To investigate the implications of socioeconomic status and health expenditures on cancer outcomes, the researchers conducted an ecological study at the state level for 3 distinct patient populations: breast cancer, colorectal cancer, and all-cancer patients.
The team extracted data on GDP and healthcare spending per capita from the 2009 Bureau of Economic Analysis and the Centers for Medicare & Medicaid Services, respectively.
Using data from the National Cancer Institute, the researchers retrieved breast, colorectal, and all-cancer age-adjusted rates and computed mortality/incidence (M/I) ratios for each population.
The team found that higher GDP per capita was significantly associated with lower M/I ratios for all cancers (rho=–0.4406; P=0.0017), breast cancer (rho=–0.3605; P=0.0118), and colorectal cancer (rho=–0.3612; P=0.0117).
But higher healthcare spending was only associated with a lower M/I ratio for breast cancer (rho=–0.4237; P=0.0027).
In a related editorial, Melissa A. Simon, MD, of Northwestern University Feinberg School of Medicine in Chicago, Illinois, and her colleagues pointed out that the data in this study predate the Affordable Care Act. So the results may not reflect the current state of affairs in the US.
The authors also said these data should not be used to guide—or misguide—policy makers to cap or decrease spending for certain health issues.
“Increased spending does not necessarily improve quality of care, but capping or cutting spending on healthcare does not necessarily solve problems either,” the authors wrote.
In a counterpoint editorial, Dr Chahoud and his colleagues said the goal of their study was not to misguide policy makers.
The team doesn’t recommend capping healthcare spending. Rather, they want to see “smart” spending that will have an impact on patient outcomes. ![]()

receiving treatment
Photo by Rhoda Baer
A new study suggests that higher healthcare spending is not associated with better cancer outcomes in the US, but state-level wealth is.
Researchers found that higher gross domestic product (GDP) per capita was associated with lower mortality for all cancers, colorectal cancer, and breast cancer.
However, higher healthcare spending was only associated with lower mortality for breast cancer—not colorectal cancer or all cancers combined.
Jad Chahoud, MD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues reported these findings in JNCCN.
To investigate the implications of socioeconomic status and health expenditures on cancer outcomes, the researchers conducted an ecological study at the state level for 3 distinct patient populations: breast cancer, colorectal cancer, and all-cancer patients.
The team extracted data on GDP and healthcare spending per capita from the 2009 Bureau of Economic Analysis and the Centers for Medicare & Medicaid Services, respectively.
Using data from the National Cancer Institute, the researchers retrieved breast, colorectal, and all-cancer age-adjusted rates and computed mortality/incidence (M/I) ratios for each population.
The team found that higher GDP per capita was significantly associated with lower M/I ratios for all cancers (rho=–0.4406; P=0.0017), breast cancer (rho=–0.3605; P=0.0118), and colorectal cancer (rho=–0.3612; P=0.0117).
But higher healthcare spending was only associated with a lower M/I ratio for breast cancer (rho=–0.4237; P=0.0027).
In a related editorial, Melissa A. Simon, MD, of Northwestern University Feinberg School of Medicine in Chicago, Illinois, and her colleagues pointed out that the data in this study predate the Affordable Care Act. So the results may not reflect the current state of affairs in the US.
The authors also said these data should not be used to guide—or misguide—policy makers to cap or decrease spending for certain health issues.
“Increased spending does not necessarily improve quality of care, but capping or cutting spending on healthcare does not necessarily solve problems either,” the authors wrote.
In a counterpoint editorial, Dr Chahoud and his colleagues said the goal of their study was not to misguide policy makers.
The team doesn’t recommend capping healthcare spending. Rather, they want to see “smart” spending that will have an impact on patient outcomes. ![]()
Chemo during pregnancy may impact baby’s fertility

Photo by Nina Matthews
Preclinical research suggests the chemotherapy drug etoposide may have adverse effects on the developing ovaries of female fetuses.
Researchers found that etoposide can damage the development of mouse ovary tissue in vitro.
However, if the drug is given after ovarian follicles have developed, the damage is not significant.
The researchers said further study is needed to assess whether etoposide has similar effects on human tissue.
“In a study involving mouse tissue, we have shown that etoposide can damage the development of the ovaries while a fetus is in the womb,” said study author Norah Spears, DPhil, of the University of Edinburgh in the UK.
“The drug affects the germ cells in the ovaries, which are the cells that give rise to eggs. This is important because it could mean that the fertility of the offspring could be affected in later life.”
Dr Spears and her colleagues reported these findings in BMC Cancer.
The researchers noted that etoposide is considered safe for use in the second and third trimester of pregnancy because it has a low risk of miscarriage and birth defects. However, little is known about the effects of the drug on the unborn baby in later life.
A woman’s reproductive lifespan is determined before birth, while the ovaries are developing in the womb. The second and third trimesters are particularly important, as that’s when female germ cells form ovarian follicles, which determine how many eggs a woman will be able to release in her lifetime.
Ovarian follicles each contain an oocyte. The process by which oocytes become enclosed in follicles starts about 17 weeks into fetal development and is only completed in late pregnancy.
Dr Spears and her colleagues found that exposing mouse ovaries to etoposide before follicles had formed caused the death of most germ cells. The few remaining germ cells went on to form unhealthy follicles. Once oocytes were enclosed in follicles, however, etoposide had no significant adverse effects.
The researchers collected fetal and neonatal ovaries from mice and cultured them in the lab. The team then exposed groups of 6 ovaries each to different doses of etoposide.
When fetal ovaries were treated with etoposide prior to follicle formation, this resulted in dose-dependent damage. Total follicle numbers declined by 72% to 90% in response to medium and high doses of etoposide, respectively.
In neonatal ovaries after follicle formation, etoposide only had minor effects, even at doses higher than those used to treat fetal ovaries.
“Our work indicates that female mouse germ cells are particularly susceptible to damage by etoposide at a specific early developmental stage, immediately prior to follicle formation, and that there could be possible consequences to the fertility of females born to women who were treated with etoposide during the second trimester of their pregnancy,” Dr Spears said.
She and her colleagues noted that additional research is needed to determine if these effects might occur in humans. And research is needed to determine whether the adverse effects of etoposide in germ cells are caused by damage to the DNA or because etoposide affects other processes such as transcription. ![]()

Photo by Nina Matthews
Preclinical research suggests the chemotherapy drug etoposide may have adverse effects on the developing ovaries of female fetuses.
Researchers found that etoposide can damage the development of mouse ovary tissue in vitro.
However, if the drug is given after ovarian follicles have developed, the damage is not significant.
The researchers said further study is needed to assess whether etoposide has similar effects on human tissue.
“In a study involving mouse tissue, we have shown that etoposide can damage the development of the ovaries while a fetus is in the womb,” said study author Norah Spears, DPhil, of the University of Edinburgh in the UK.
“The drug affects the germ cells in the ovaries, which are the cells that give rise to eggs. This is important because it could mean that the fertility of the offspring could be affected in later life.”
Dr Spears and her colleagues reported these findings in BMC Cancer.
The researchers noted that etoposide is considered safe for use in the second and third trimester of pregnancy because it has a low risk of miscarriage and birth defects. However, little is known about the effects of the drug on the unborn baby in later life.
A woman’s reproductive lifespan is determined before birth, while the ovaries are developing in the womb. The second and third trimesters are particularly important, as that’s when female germ cells form ovarian follicles, which determine how many eggs a woman will be able to release in her lifetime.
Ovarian follicles each contain an oocyte. The process by which oocytes become enclosed in follicles starts about 17 weeks into fetal development and is only completed in late pregnancy.
Dr Spears and her colleagues found that exposing mouse ovaries to etoposide before follicles had formed caused the death of most germ cells. The few remaining germ cells went on to form unhealthy follicles. Once oocytes were enclosed in follicles, however, etoposide had no significant adverse effects.
The researchers collected fetal and neonatal ovaries from mice and cultured them in the lab. The team then exposed groups of 6 ovaries each to different doses of etoposide.
When fetal ovaries were treated with etoposide prior to follicle formation, this resulted in dose-dependent damage. Total follicle numbers declined by 72% to 90% in response to medium and high doses of etoposide, respectively.
In neonatal ovaries after follicle formation, etoposide only had minor effects, even at doses higher than those used to treat fetal ovaries.
“Our work indicates that female mouse germ cells are particularly susceptible to damage by etoposide at a specific early developmental stage, immediately prior to follicle formation, and that there could be possible consequences to the fertility of females born to women who were treated with etoposide during the second trimester of their pregnancy,” Dr Spears said.
She and her colleagues noted that additional research is needed to determine if these effects might occur in humans. And research is needed to determine whether the adverse effects of etoposide in germ cells are caused by damage to the DNA or because etoposide affects other processes such as transcription. ![]()

Photo by Nina Matthews
Preclinical research suggests the chemotherapy drug etoposide may have adverse effects on the developing ovaries of female fetuses.
Researchers found that etoposide can damage the development of mouse ovary tissue in vitro.
However, if the drug is given after ovarian follicles have developed, the damage is not significant.
The researchers said further study is needed to assess whether etoposide has similar effects on human tissue.
“In a study involving mouse tissue, we have shown that etoposide can damage the development of the ovaries while a fetus is in the womb,” said study author Norah Spears, DPhil, of the University of Edinburgh in the UK.
“The drug affects the germ cells in the ovaries, which are the cells that give rise to eggs. This is important because it could mean that the fertility of the offspring could be affected in later life.”
Dr Spears and her colleagues reported these findings in BMC Cancer.
The researchers noted that etoposide is considered safe for use in the second and third trimester of pregnancy because it has a low risk of miscarriage and birth defects. However, little is known about the effects of the drug on the unborn baby in later life.
A woman’s reproductive lifespan is determined before birth, while the ovaries are developing in the womb. The second and third trimesters are particularly important, as that’s when female germ cells form ovarian follicles, which determine how many eggs a woman will be able to release in her lifetime.
Ovarian follicles each contain an oocyte. The process by which oocytes become enclosed in follicles starts about 17 weeks into fetal development and is only completed in late pregnancy.
Dr Spears and her colleagues found that exposing mouse ovaries to etoposide before follicles had formed caused the death of most germ cells. The few remaining germ cells went on to form unhealthy follicles. Once oocytes were enclosed in follicles, however, etoposide had no significant adverse effects.
The researchers collected fetal and neonatal ovaries from mice and cultured them in the lab. The team then exposed groups of 6 ovaries each to different doses of etoposide.
When fetal ovaries were treated with etoposide prior to follicle formation, this resulted in dose-dependent damage. Total follicle numbers declined by 72% to 90% in response to medium and high doses of etoposide, respectively.
In neonatal ovaries after follicle formation, etoposide only had minor effects, even at doses higher than those used to treat fetal ovaries.
“Our work indicates that female mouse germ cells are particularly susceptible to damage by etoposide at a specific early developmental stage, immediately prior to follicle formation, and that there could be possible consequences to the fertility of females born to women who were treated with etoposide during the second trimester of their pregnancy,” Dr Spears said.
She and her colleagues noted that additional research is needed to determine if these effects might occur in humans. And research is needed to determine whether the adverse effects of etoposide in germ cells are caused by damage to the DNA or because etoposide affects other processes such as transcription. ![]()
FDA authorizes use of Zika assay

Photo by Juan D. Alfonso
The US Food and Drug Administration (FDA) has granted emergency use authorization (EUA) for the xMAP® MultiFLEX™ Zika RNA Assay.
This multiplex nucleic acid test is designed to detect Zika virus RNA in blood serum, plasma, or urine (collected alongside a patient-matched serum or plasma specimen).
The xMAP® MultiFLEX™ Zika RNA Assay is available for purchase by laboratories that are certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA) to perform high complexity tests.
The assay uses the Luminex® 100/200™ analyzer, MAGPIX® system, or other authorized instruments to simultaneously test for 6 genetic targets of the Zika virus.
The xMAP® MultiFLEX™ Zika RNA Assay was designed by GenArraytion, Inc. and is marketed by Luminex Corporation.
For more information on the test, see the fact sheet for healthcare providers on the Luminex website.
About the EUA
The EUA does not mean the xMAP® MultiFLEX™ Zika RNA Assay is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency.
The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
This means the xMAP® MultiFLEX™ Zika RNA Assay is only authorized as long as circumstances exist to justify the authorization of the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner. ![]()

Photo by Juan D. Alfonso
The US Food and Drug Administration (FDA) has granted emergency use authorization (EUA) for the xMAP® MultiFLEX™ Zika RNA Assay.
This multiplex nucleic acid test is designed to detect Zika virus RNA in blood serum, plasma, or urine (collected alongside a patient-matched serum or plasma specimen).
The xMAP® MultiFLEX™ Zika RNA Assay is available for purchase by laboratories that are certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA) to perform high complexity tests.
The assay uses the Luminex® 100/200™ analyzer, MAGPIX® system, or other authorized instruments to simultaneously test for 6 genetic targets of the Zika virus.
The xMAP® MultiFLEX™ Zika RNA Assay was designed by GenArraytion, Inc. and is marketed by Luminex Corporation.
For more information on the test, see the fact sheet for healthcare providers on the Luminex website.
About the EUA
The EUA does not mean the xMAP® MultiFLEX™ Zika RNA Assay is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency.
The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
This means the xMAP® MultiFLEX™ Zika RNA Assay is only authorized as long as circumstances exist to justify the authorization of the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner. ![]()

Photo by Juan D. Alfonso
The US Food and Drug Administration (FDA) has granted emergency use authorization (EUA) for the xMAP® MultiFLEX™ Zika RNA Assay.
This multiplex nucleic acid test is designed to detect Zika virus RNA in blood serum, plasma, or urine (collected alongside a patient-matched serum or plasma specimen).
The xMAP® MultiFLEX™ Zika RNA Assay is available for purchase by laboratories that are certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA) to perform high complexity tests.
The assay uses the Luminex® 100/200™ analyzer, MAGPIX® system, or other authorized instruments to simultaneously test for 6 genetic targets of the Zika virus.
The xMAP® MultiFLEX™ Zika RNA Assay was designed by GenArraytion, Inc. and is marketed by Luminex Corporation.
For more information on the test, see the fact sheet for healthcare providers on the Luminex website.
About the EUA
The EUA does not mean the xMAP® MultiFLEX™ Zika RNA Assay is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency.
The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
This means the xMAP® MultiFLEX™ Zika RNA Assay is only authorized as long as circumstances exist to justify the authorization of the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner. ![]()
Odor-baited mosquito traps can fight malaria

Photo courtesy of the CDC
Solar-powered mosquito traps incorporating human odor can reduce the incidence of malaria, according to research published in The Lancet.
Researchers introduced these traps to homes on the Kenyan island of Rusinga.
The population of malaria-carrying mosquitoes declined by 42% in homes that had the traps.
And the prevalence of malaria was 30% lower among people living in houses with a trap than among those in houses without a trap.
“The objective of the trial on Rusinga Island in Lake Victoria was to investigate whether malaria mosquitoes can be captured and destroyed using traps with a lure so that the risk of new malaria infections is minimized,” explained study author Willem Takken, PhD, of Wageningen University and Research Centre in Wageningen, Netherlands.
The trial enrolled 34,041 participants. Each individual was assigned to a cluster, which consisted of 50 or 51 geographically contiguous households. There were 81 clusters in all.
The researchers installed their solar-powered, odor-baited mosquito trapping systems (SMoTS) in the various households, cluster by cluster, until all of the clusters had the traps.
During the roll-out period—between June 3, 2013, and May 16, 2015—SMoTS were installed in 4358 households.
The density of Anopheles mosquitoes was lower in the clusters with SMoTS than those without. The adjusted estimated effectiveness of the traps was 42.2%.
The densities of Anopheles funestus and Anopheles gambiae mosquitoes were lower in clusters with SMoTS than those without. The adjusted estimated effectiveness was 69.2% (P=0.005) and 10.8% (P=0.6), respectively.
The prevalence of malaria was 29.8% lower in clusters with SMoTS than those without (P<0.0001).
About 24% of people in clusters with SMoTS were positive for Plasmodium parasites (23.7%, 1552/6550), compared to about 35% of people in clusters without SMoTS (34.5%, 2002/5795).
“Ultimately, we want to eradicate malaria completely, in an environmentally friendly and sustainable manner,” Dr Takken said.
“As we use a natural lure—namely, human odor—in our approach, there is no negative impact on the environment, and it is very improbable that the mosquitoes will become ‘resistant’ to being captured. After all, the mosquitoes need their attraction to the lure in order to be able to survive.”
Dr Takken and his colleagues believe their SMoTS may also be able to combat dengue fever and the Zika virus. Aedes aegypti is a vector for these viruses, and this mosquito is attracted to the same humanized scent that attracts malaria-carrying mosquitoes. ![]()

Photo courtesy of the CDC
Solar-powered mosquito traps incorporating human odor can reduce the incidence of malaria, according to research published in The Lancet.
Researchers introduced these traps to homes on the Kenyan island of Rusinga.
The population of malaria-carrying mosquitoes declined by 42% in homes that had the traps.
And the prevalence of malaria was 30% lower among people living in houses with a trap than among those in houses without a trap.
“The objective of the trial on Rusinga Island in Lake Victoria was to investigate whether malaria mosquitoes can be captured and destroyed using traps with a lure so that the risk of new malaria infections is minimized,” explained study author Willem Takken, PhD, of Wageningen University and Research Centre in Wageningen, Netherlands.
The trial enrolled 34,041 participants. Each individual was assigned to a cluster, which consisted of 50 or 51 geographically contiguous households. There were 81 clusters in all.
The researchers installed their solar-powered, odor-baited mosquito trapping systems (SMoTS) in the various households, cluster by cluster, until all of the clusters had the traps.
During the roll-out period—between June 3, 2013, and May 16, 2015—SMoTS were installed in 4358 households.
The density of Anopheles mosquitoes was lower in the clusters with SMoTS than those without. The adjusted estimated effectiveness of the traps was 42.2%.
The densities of Anopheles funestus and Anopheles gambiae mosquitoes were lower in clusters with SMoTS than those without. The adjusted estimated effectiveness was 69.2% (P=0.005) and 10.8% (P=0.6), respectively.
The prevalence of malaria was 29.8% lower in clusters with SMoTS than those without (P<0.0001).
About 24% of people in clusters with SMoTS were positive for Plasmodium parasites (23.7%, 1552/6550), compared to about 35% of people in clusters without SMoTS (34.5%, 2002/5795).
“Ultimately, we want to eradicate malaria completely, in an environmentally friendly and sustainable manner,” Dr Takken said.
“As we use a natural lure—namely, human odor—in our approach, there is no negative impact on the environment, and it is very improbable that the mosquitoes will become ‘resistant’ to being captured. After all, the mosquitoes need their attraction to the lure in order to be able to survive.”
Dr Takken and his colleagues believe their SMoTS may also be able to combat dengue fever and the Zika virus. Aedes aegypti is a vector for these viruses, and this mosquito is attracted to the same humanized scent that attracts malaria-carrying mosquitoes. ![]()

Photo courtesy of the CDC
Solar-powered mosquito traps incorporating human odor can reduce the incidence of malaria, according to research published in The Lancet.
Researchers introduced these traps to homes on the Kenyan island of Rusinga.
The population of malaria-carrying mosquitoes declined by 42% in homes that had the traps.
And the prevalence of malaria was 30% lower among people living in houses with a trap than among those in houses without a trap.
“The objective of the trial on Rusinga Island in Lake Victoria was to investigate whether malaria mosquitoes can be captured and destroyed using traps with a lure so that the risk of new malaria infections is minimized,” explained study author Willem Takken, PhD, of Wageningen University and Research Centre in Wageningen, Netherlands.
The trial enrolled 34,041 participants. Each individual was assigned to a cluster, which consisted of 50 or 51 geographically contiguous households. There were 81 clusters in all.
The researchers installed their solar-powered, odor-baited mosquito trapping systems (SMoTS) in the various households, cluster by cluster, until all of the clusters had the traps.
During the roll-out period—between June 3, 2013, and May 16, 2015—SMoTS were installed in 4358 households.
The density of Anopheles mosquitoes was lower in the clusters with SMoTS than those without. The adjusted estimated effectiveness of the traps was 42.2%.
The densities of Anopheles funestus and Anopheles gambiae mosquitoes were lower in clusters with SMoTS than those without. The adjusted estimated effectiveness was 69.2% (P=0.005) and 10.8% (P=0.6), respectively.
The prevalence of malaria was 29.8% lower in clusters with SMoTS than those without (P<0.0001).
About 24% of people in clusters with SMoTS were positive for Plasmodium parasites (23.7%, 1552/6550), compared to about 35% of people in clusters without SMoTS (34.5%, 2002/5795).
“Ultimately, we want to eradicate malaria completely, in an environmentally friendly and sustainable manner,” Dr Takken said.
“As we use a natural lure—namely, human odor—in our approach, there is no negative impact on the environment, and it is very improbable that the mosquitoes will become ‘resistant’ to being captured. After all, the mosquitoes need their attraction to the lure in order to be able to survive.”
Dr Takken and his colleagues believe their SMoTS may also be able to combat dengue fever and the Zika virus. Aedes aegypti is a vector for these viruses, and this mosquito is attracted to the same humanized scent that attracts malaria-carrying mosquitoes. ![]()
FDA approves field trial of GE mosquitoes

Photo courtesy of
Muhammad Mahdi Karim
The US Food and Drug Administration (FDA) is allowing a company to proceed with a field trial of genetically engineered (GE) Aedes aegypti mosquitoes in the Florida Keys.
The FDA said the trial, designed to determine if the GE mosquitoes will suppress the local Aedes aegypti population, will not have a significant impact on the environment.
The FDA’s decision does not mean the GE mosquitoes are approved for commercial use or even that the trial will go ahead.
The company developing the mosquitoes, Oxitec, must ensure that all other local, state, and federal requirements are met before conducting the field trial.
Oxitec and its local partner, the Florida Keys Mosquito Control District, will then determine whether and when to begin the trial in Key Haven, Florida.
The goal of the field trial is to reduce the population of Aedes aegypti mosquitoes in the Florida Keys. These non-native mosquitoes spread the Zika virus, dengue fever, and chikungunya.
If it proceeds, the trial will involve male Aedes aegypti mosquitoes that have been genetically engineered so their offspring die before reaching adulthood.
The GE mosquitoes, which do not bite or spread disease, will be released to mate with wild female Aedes aegypti. The resulting offspring are expected to die before they can begin mating themselves, thereby reducing the overall population.
Efficacy trials in Brazil, Panama, and the Cayman Islands have tested this approach, and, in each of these trials, the population of Aedes aegypti was reduced by more than 90%.
“We’ve been developing this approach for many years, and, from these results, we are convinced that our solution is both highly effective and has sound environmental credentials,” said Oxitec’s Chief Executive Officer Hadyn Parry.
“We’re delighted with the announcement today that the FDA, after their extensive review of our dossier and thousands of public comments for a trial in the Florida Keys, have published their final view that this will not have a significant impact on the environment. We are now looking forward to working with the community in the Florida Keys moving forward.”
The FDA published a final finding of no significant impact (FONSI) and a final environmental assessment (EA) regarding the trial on August 5. Both documents are available on the FDA’s website.
More information on Oxitec’s technology and the trial can be found on the company’s website. ![]()

Photo courtesy of
Muhammad Mahdi Karim
The US Food and Drug Administration (FDA) is allowing a company to proceed with a field trial of genetically engineered (GE) Aedes aegypti mosquitoes in the Florida Keys.
The FDA said the trial, designed to determine if the GE mosquitoes will suppress the local Aedes aegypti population, will not have a significant impact on the environment.
The FDA’s decision does not mean the GE mosquitoes are approved for commercial use or even that the trial will go ahead.
The company developing the mosquitoes, Oxitec, must ensure that all other local, state, and federal requirements are met before conducting the field trial.
Oxitec and its local partner, the Florida Keys Mosquito Control District, will then determine whether and when to begin the trial in Key Haven, Florida.
The goal of the field trial is to reduce the population of Aedes aegypti mosquitoes in the Florida Keys. These non-native mosquitoes spread the Zika virus, dengue fever, and chikungunya.
If it proceeds, the trial will involve male Aedes aegypti mosquitoes that have been genetically engineered so their offspring die before reaching adulthood.
The GE mosquitoes, which do not bite or spread disease, will be released to mate with wild female Aedes aegypti. The resulting offspring are expected to die before they can begin mating themselves, thereby reducing the overall population.
Efficacy trials in Brazil, Panama, and the Cayman Islands have tested this approach, and, in each of these trials, the population of Aedes aegypti was reduced by more than 90%.
“We’ve been developing this approach for many years, and, from these results, we are convinced that our solution is both highly effective and has sound environmental credentials,” said Oxitec’s Chief Executive Officer Hadyn Parry.
“We’re delighted with the announcement today that the FDA, after their extensive review of our dossier and thousands of public comments for a trial in the Florida Keys, have published their final view that this will not have a significant impact on the environment. We are now looking forward to working with the community in the Florida Keys moving forward.”
The FDA published a final finding of no significant impact (FONSI) and a final environmental assessment (EA) regarding the trial on August 5. Both documents are available on the FDA’s website.
More information on Oxitec’s technology and the trial can be found on the company’s website. ![]()

Photo courtesy of
Muhammad Mahdi Karim
The US Food and Drug Administration (FDA) is allowing a company to proceed with a field trial of genetically engineered (GE) Aedes aegypti mosquitoes in the Florida Keys.
The FDA said the trial, designed to determine if the GE mosquitoes will suppress the local Aedes aegypti population, will not have a significant impact on the environment.
The FDA’s decision does not mean the GE mosquitoes are approved for commercial use or even that the trial will go ahead.
The company developing the mosquitoes, Oxitec, must ensure that all other local, state, and federal requirements are met before conducting the field trial.
Oxitec and its local partner, the Florida Keys Mosquito Control District, will then determine whether and when to begin the trial in Key Haven, Florida.
The goal of the field trial is to reduce the population of Aedes aegypti mosquitoes in the Florida Keys. These non-native mosquitoes spread the Zika virus, dengue fever, and chikungunya.
If it proceeds, the trial will involve male Aedes aegypti mosquitoes that have been genetically engineered so their offspring die before reaching adulthood.
The GE mosquitoes, which do not bite or spread disease, will be released to mate with wild female Aedes aegypti. The resulting offspring are expected to die before they can begin mating themselves, thereby reducing the overall population.
Efficacy trials in Brazil, Panama, and the Cayman Islands have tested this approach, and, in each of these trials, the population of Aedes aegypti was reduced by more than 90%.
“We’ve been developing this approach for many years, and, from these results, we are convinced that our solution is both highly effective and has sound environmental credentials,” said Oxitec’s Chief Executive Officer Hadyn Parry.
“We’re delighted with the announcement today that the FDA, after their extensive review of our dossier and thousands of public comments for a trial in the Florida Keys, have published their final view that this will not have a significant impact on the environment. We are now looking forward to working with the community in the Florida Keys moving forward.”
The FDA published a final finding of no significant impact (FONSI) and a final environmental assessment (EA) regarding the trial on August 5. Both documents are available on the FDA’s website.
More information on Oxitec’s technology and the trial can be found on the company’s website. ![]()
Vaccines protect monkeys from Zika infection

Photo by Einar Fredriksen
Three types of investigational vaccines can protect monkeys from Zika virus infection, according to research published in Science.
Investigators found that an inactivated virus vaccine, a DNA-based vaccine, and an adenovirus vector-based vaccine induced immune responses and protected against infection in rhesus macaques challenged with the Zika virus.
In addition, there were no adverse events observed with any of the vaccines.
The investigators first tested the inactivated Zika virus vaccine in 16 rhesus macaques. Eight animals received the experimental vaccine, and 8 received a placebo injection.
Within 2 weeks of the initial injection, all vaccinated animals developed neutralizing antibodies as well as antibodies specific to the viral envelope protein, a key vaccine target on the Zika virus. A second dose was given 4 weeks later, which substantially boosted antibody levels.
The monkeys were then challenged with Zika virus. Following exposure, the vaccinated animals had no detectable virus and showed no other evidence of infection, while the group that received the placebo injection developed high levels of virus replication in the blood and other tissues for 6 to 7 days.
In another experiment, the investigators administered 2 doses of a DNA vaccine, 1 dose of an adenovirus vector vaccine, or a placebo injection to 3 groups of 4 monkeys each. The group that received the DNA vaccine received a booster shot 4 weeks after the initial vaccination.
Minimal levels of antibodies were detected after the first injection of the DNA vaccine. However, after the second injection, investigators detected Zika-specific neutralizing antibodies in the animals.
The adenovirus vector-based vaccine induced Zika-specific neutralizing antibodies 2 weeks after the single injection.
The animals were exposed to Zika virus 4 weeks after the final vaccination. Both the DNA vaccine and the adenovirus vector vaccine provided complete protection against infection.
The investigators said these encouraging findings suggest a path forward for clinical development of Zika vaccines in humans. ![]()

Photo by Einar Fredriksen
Three types of investigational vaccines can protect monkeys from Zika virus infection, according to research published in Science.
Investigators found that an inactivated virus vaccine, a DNA-based vaccine, and an adenovirus vector-based vaccine induced immune responses and protected against infection in rhesus macaques challenged with the Zika virus.
In addition, there were no adverse events observed with any of the vaccines.
The investigators first tested the inactivated Zika virus vaccine in 16 rhesus macaques. Eight animals received the experimental vaccine, and 8 received a placebo injection.
Within 2 weeks of the initial injection, all vaccinated animals developed neutralizing antibodies as well as antibodies specific to the viral envelope protein, a key vaccine target on the Zika virus. A second dose was given 4 weeks later, which substantially boosted antibody levels.
The monkeys were then challenged with Zika virus. Following exposure, the vaccinated animals had no detectable virus and showed no other evidence of infection, while the group that received the placebo injection developed high levels of virus replication in the blood and other tissues for 6 to 7 days.
In another experiment, the investigators administered 2 doses of a DNA vaccine, 1 dose of an adenovirus vector vaccine, or a placebo injection to 3 groups of 4 monkeys each. The group that received the DNA vaccine received a booster shot 4 weeks after the initial vaccination.
Minimal levels of antibodies were detected after the first injection of the DNA vaccine. However, after the second injection, investigators detected Zika-specific neutralizing antibodies in the animals.
The adenovirus vector-based vaccine induced Zika-specific neutralizing antibodies 2 weeks after the single injection.
The animals were exposed to Zika virus 4 weeks after the final vaccination. Both the DNA vaccine and the adenovirus vector vaccine provided complete protection against infection.
The investigators said these encouraging findings suggest a path forward for clinical development of Zika vaccines in humans. ![]()

Photo by Einar Fredriksen
Three types of investigational vaccines can protect monkeys from Zika virus infection, according to research published in Science.
Investigators found that an inactivated virus vaccine, a DNA-based vaccine, and an adenovirus vector-based vaccine induced immune responses and protected against infection in rhesus macaques challenged with the Zika virus.
In addition, there were no adverse events observed with any of the vaccines.
The investigators first tested the inactivated Zika virus vaccine in 16 rhesus macaques. Eight animals received the experimental vaccine, and 8 received a placebo injection.
Within 2 weeks of the initial injection, all vaccinated animals developed neutralizing antibodies as well as antibodies specific to the viral envelope protein, a key vaccine target on the Zika virus. A second dose was given 4 weeks later, which substantially boosted antibody levels.
The monkeys were then challenged with Zika virus. Following exposure, the vaccinated animals had no detectable virus and showed no other evidence of infection, while the group that received the placebo injection developed high levels of virus replication in the blood and other tissues for 6 to 7 days.
In another experiment, the investigators administered 2 doses of a DNA vaccine, 1 dose of an adenovirus vector vaccine, or a placebo injection to 3 groups of 4 monkeys each. The group that received the DNA vaccine received a booster shot 4 weeks after the initial vaccination.
Minimal levels of antibodies were detected after the first injection of the DNA vaccine. However, after the second injection, investigators detected Zika-specific neutralizing antibodies in the animals.
The adenovirus vector-based vaccine induced Zika-specific neutralizing antibodies 2 weeks after the single injection.
The animals were exposed to Zika virus 4 weeks after the final vaccination. Both the DNA vaccine and the adenovirus vector vaccine provided complete protection against infection.
The investigators said these encouraging findings suggest a path forward for clinical development of Zika vaccines in humans. ![]()
Plant sugars influence malaria transmission

feeding on Barleria lupilina.
Photo from Domonbabele
F. d. S. Hien et al.
A study published in PLOS Pathogens suggests the plant-based part of Anopheles mosquitoes’ diet affects malaria transmission by influencing the interaction between the mosquitoes and Plasmodium parasites.
Recent studies have shown that Anopheles female mosquitoes, which can transmit the malaria parasite P falciparum, locate and display preferences for natural sources of plant sugar.
These studies also suggested that environmental sugars influence the lifespan and blood-feeding rate of mosquitoes and, therefore, their malaria transmission potential.
Whether the type of plant sugar could also affect the malaria host-pathogen interactions was unclear.
To find out, Thierry Lefevre, PhD, of the Institut de Recherche en Sciences de la Santé in Bobo Dioulasso, Burkina Faso, and his colleagues examined the impact of plant diversity on mosquito susceptibility to malaria parasites.
The team studied the natural interactions between the P falciparum parasite, the Anopheles coluzzii mosquito (a major vector of P falciparum in Africa), and several natural plant-derived sugar sources growing in the vicinity of human dwellings in Burkina Faso.
The latter included 2 ornamental flowering plants (Barleria lupilina and Thevetia neriifolia) as well as mangoes and the grape-like fruit from the Lannea microcarpa tree.
The researchers raised groups of Anopheles mosquitos in cages and provided each of them with a different plant sugar source or with a 5% glucose solution.
Sugar-fed mosquitoes were then starved for 24 hours before being offered a parasite-containing blood meal. The blood was drawn from healthy Plasmodium-infected local human volunteers and diluted to a consistent concentration of parasites.
Blood-fed female mosquitoes were housed in a biosafety room and continued to be fed their assigned plant sugar source.
Seven or 14 days after the blood-meal, roughly 30 mosquitoes from each group were examined under the microscope for traits that influence malaria transmission.
The researchers found that different sugar sources had different effects on all traits examined, including the infection and survival rates of the mosquitoes and the survival rate of the parasites 7 days after the blood meal.
The plant sugar source also influenced the proportion of mosquitoes harboring sporozoites and the timing of sporozoite release.
To predict the relative contribution of the different plants to overall malaria transmission, the researchers used the various experimental results in an epidemiological model.
This suggested that plant sugar source can be a significant driver of malaria transmission dynamics.
Compared to the baseline scenario with the 5% glucose solution, both L microcarpa and B lupilina increased malaria transmission by an estimated 30% and 40%, respectively, mainly because of increased infection rates among mosquitoes exposed to parasites through their blood-meal.
In contrast, T neriifolia, with its negative effect on infection rate and decreased longevity, was predicted to decrease malaria transmission by 30% compared with sugar water.
The researchers said these findings suggest that planting anti-Plasmodium plant sugar sources could be a promising alternative strategy for controlling malaria. ![]()

feeding on Barleria lupilina.
Photo from Domonbabele
F. d. S. Hien et al.
A study published in PLOS Pathogens suggests the plant-based part of Anopheles mosquitoes’ diet affects malaria transmission by influencing the interaction between the mosquitoes and Plasmodium parasites.
Recent studies have shown that Anopheles female mosquitoes, which can transmit the malaria parasite P falciparum, locate and display preferences for natural sources of plant sugar.
These studies also suggested that environmental sugars influence the lifespan and blood-feeding rate of mosquitoes and, therefore, their malaria transmission potential.
Whether the type of plant sugar could also affect the malaria host-pathogen interactions was unclear.
To find out, Thierry Lefevre, PhD, of the Institut de Recherche en Sciences de la Santé in Bobo Dioulasso, Burkina Faso, and his colleagues examined the impact of plant diversity on mosquito susceptibility to malaria parasites.
The team studied the natural interactions between the P falciparum parasite, the Anopheles coluzzii mosquito (a major vector of P falciparum in Africa), and several natural plant-derived sugar sources growing in the vicinity of human dwellings in Burkina Faso.
The latter included 2 ornamental flowering plants (Barleria lupilina and Thevetia neriifolia) as well as mangoes and the grape-like fruit from the Lannea microcarpa tree.
The researchers raised groups of Anopheles mosquitos in cages and provided each of them with a different plant sugar source or with a 5% glucose solution.
Sugar-fed mosquitoes were then starved for 24 hours before being offered a parasite-containing blood meal. The blood was drawn from healthy Plasmodium-infected local human volunteers and diluted to a consistent concentration of parasites.
Blood-fed female mosquitoes were housed in a biosafety room and continued to be fed their assigned plant sugar source.
Seven or 14 days after the blood-meal, roughly 30 mosquitoes from each group were examined under the microscope for traits that influence malaria transmission.
The researchers found that different sugar sources had different effects on all traits examined, including the infection and survival rates of the mosquitoes and the survival rate of the parasites 7 days after the blood meal.
The plant sugar source also influenced the proportion of mosquitoes harboring sporozoites and the timing of sporozoite release.
To predict the relative contribution of the different plants to overall malaria transmission, the researchers used the various experimental results in an epidemiological model.
This suggested that plant sugar source can be a significant driver of malaria transmission dynamics.
Compared to the baseline scenario with the 5% glucose solution, both L microcarpa and B lupilina increased malaria transmission by an estimated 30% and 40%, respectively, mainly because of increased infection rates among mosquitoes exposed to parasites through their blood-meal.
In contrast, T neriifolia, with its negative effect on infection rate and decreased longevity, was predicted to decrease malaria transmission by 30% compared with sugar water.
The researchers said these findings suggest that planting anti-Plasmodium plant sugar sources could be a promising alternative strategy for controlling malaria. ![]()

feeding on Barleria lupilina.
Photo from Domonbabele
F. d. S. Hien et al.
A study published in PLOS Pathogens suggests the plant-based part of Anopheles mosquitoes’ diet affects malaria transmission by influencing the interaction between the mosquitoes and Plasmodium parasites.
Recent studies have shown that Anopheles female mosquitoes, which can transmit the malaria parasite P falciparum, locate and display preferences for natural sources of plant sugar.
These studies also suggested that environmental sugars influence the lifespan and blood-feeding rate of mosquitoes and, therefore, their malaria transmission potential.
Whether the type of plant sugar could also affect the malaria host-pathogen interactions was unclear.
To find out, Thierry Lefevre, PhD, of the Institut de Recherche en Sciences de la Santé in Bobo Dioulasso, Burkina Faso, and his colleagues examined the impact of plant diversity on mosquito susceptibility to malaria parasites.
The team studied the natural interactions between the P falciparum parasite, the Anopheles coluzzii mosquito (a major vector of P falciparum in Africa), and several natural plant-derived sugar sources growing in the vicinity of human dwellings in Burkina Faso.
The latter included 2 ornamental flowering plants (Barleria lupilina and Thevetia neriifolia) as well as mangoes and the grape-like fruit from the Lannea microcarpa tree.
The researchers raised groups of Anopheles mosquitos in cages and provided each of them with a different plant sugar source or with a 5% glucose solution.
Sugar-fed mosquitoes were then starved for 24 hours before being offered a parasite-containing blood meal. The blood was drawn from healthy Plasmodium-infected local human volunteers and diluted to a consistent concentration of parasites.
Blood-fed female mosquitoes were housed in a biosafety room and continued to be fed their assigned plant sugar source.
Seven or 14 days after the blood-meal, roughly 30 mosquitoes from each group were examined under the microscope for traits that influence malaria transmission.
The researchers found that different sugar sources had different effects on all traits examined, including the infection and survival rates of the mosquitoes and the survival rate of the parasites 7 days after the blood meal.
The plant sugar source also influenced the proportion of mosquitoes harboring sporozoites and the timing of sporozoite release.
To predict the relative contribution of the different plants to overall malaria transmission, the researchers used the various experimental results in an epidemiological model.
This suggested that plant sugar source can be a significant driver of malaria transmission dynamics.
Compared to the baseline scenario with the 5% glucose solution, both L microcarpa and B lupilina increased malaria transmission by an estimated 30% and 40%, respectively, mainly because of increased infection rates among mosquitoes exposed to parasites through their blood-meal.
In contrast, T neriifolia, with its negative effect on infection rate and decreased longevity, was predicted to decrease malaria transmission by 30% compared with sugar water.
The researchers said these findings suggest that planting anti-Plasmodium plant sugar sources could be a promising alternative strategy for controlling malaria.
Team creates database of autophagy-related proteins

Image by Sarah Pfau
Scientists have identified previously undiscovered proteins related to autophagy and created a database containing them.
The team believes this database will enable the scientific community to find ways to activate autophagy inside human cells.
And it could aid the development of drugs to treat age-related conditions such as cancer.
The team described the creation of the database in the journal Autophagy.
The database is available here: https://ilir.warwick.ac.uk/.
“Our novel database resource will open a lot of new avenues in basic and translational science,” said Ioannis Nezis, PhD, of the University of Warwick in Coventry, UK.
“Identifying novel selective autophagy-related proteins will help for the development of novel pharmaceutical drug targets for a large variety of diseases like cancer, neurodegeneration, and other aging-related diseases, infections, diabetes, obesity, and Crohn’s disease.”
“Importantly, understanding the molecular mechanisms of selective autophagy will help researchers to find interventions to activate the autophagic pathway to prevent aging and promote healthy well-being during the life course.”

Image by Sarah Pfau
Scientists have identified previously undiscovered proteins related to autophagy and created a database containing them.
The team believes this database will enable the scientific community to find ways to activate autophagy inside human cells.
And it could aid the development of drugs to treat age-related conditions such as cancer.
The team described the creation of the database in the journal Autophagy.
The database is available here: https://ilir.warwick.ac.uk/.
“Our novel database resource will open a lot of new avenues in basic and translational science,” said Ioannis Nezis, PhD, of the University of Warwick in Coventry, UK.
“Identifying novel selective autophagy-related proteins will help for the development of novel pharmaceutical drug targets for a large variety of diseases like cancer, neurodegeneration, and other aging-related diseases, infections, diabetes, obesity, and Crohn’s disease.”
“Importantly, understanding the molecular mechanisms of selective autophagy will help researchers to find interventions to activate the autophagic pathway to prevent aging and promote healthy well-being during the life course.”

Image by Sarah Pfau
Scientists have identified previously undiscovered proteins related to autophagy and created a database containing them.
The team believes this database will enable the scientific community to find ways to activate autophagy inside human cells.
And it could aid the development of drugs to treat age-related conditions such as cancer.
The team described the creation of the database in the journal Autophagy.
The database is available here: https://ilir.warwick.ac.uk/.
“Our novel database resource will open a lot of new avenues in basic and translational science,” said Ioannis Nezis, PhD, of the University of Warwick in Coventry, UK.
“Identifying novel selective autophagy-related proteins will help for the development of novel pharmaceutical drug targets for a large variety of diseases like cancer, neurodegeneration, and other aging-related diseases, infections, diabetes, obesity, and Crohn’s disease.”
“Importantly, understanding the molecular mechanisms of selective autophagy will help researchers to find interventions to activate the autophagic pathway to prevent aging and promote healthy well-being during the life course.”
Overcoming drug resistance in malaria

infecting a red blood cell
Photo courtesy of St. Jude
Children’s Research Hospital
New research helps explain how one of Plasmodium falciparum’s best weapons against antimalarial drugs can actually be exploited to treat malaria.
Investigators believe the findings, published in PLOS Pathogens, might be used to stop the emergence and spread of drug-resistant malaria.
The team noted that mutations in the P falciparum chloroquine resistance transporter (PfCRT) confer resistance to
chloroquine and related antimalarial drugs by enabling the protein to transport the drugs away from their targets within the parasite’s digestive vacuole.
However, chloroquine resistance-conferring isoforms of PfCRT (PfCRTCQR) also render the parasite hypersensitive to a subset of structurally diverse drugs. And mutations in PfCRTCQR that suppress this hypersensitivity simultaneously reinstate sensitivity to chloroquine and related drugs.
With this study, the investigators uncovered 2 mechanisms by which PfCRT causes P falciparum to become hypersensitive to antimalarial drugs.
First, they found that quinine, which normally exerts its killing effect within the parasite’s digestive vacuole, can bind tightly to certain forms of PfCRT. This blocks the function of the protein, which is essential to the parasite’s survival.
Second, the team found that amantadine, which normally sequesters within the digestive vacuole as well, is leaked back into the cytosol via PfCRT.
The investigators noted that, in both of these cases, mutations that suppress hypersensitivity also revoke PfCRT’s ability to transport chloroquine, which explains why rescue from hypersensitivity restores the parasite’s sensitivity to chloroquine.
“[C]hanges that allow the protein to move chloroquine away from its antimalarial target simultaneously enable the protein to deliver other drugs to their antimalarial targets,” explained study author Rowena Martin, PhD, of Australian National University in Canberra.
“[W]hen the protein adapts itself to fend off one of these drugs, it is no longer able to deal with chloroquine and, hence, the parasite is re-sensitized to chloroquine. Essentially, the parasite can’t have its cake and eat it too. So if chloroquine or a related drug is paired with a drug that is super-active against the modified protein, no matter what the parasite tries to do, it’s ‘checkmate’ for malaria.”
Dr Martin and her colleagues believe their findings provide a foundation for understanding and exploiting the hypersensitivity of chloroquine-resistant parasites to several antimalarial drugs that are currently available.
“Health authorities could use our research to find ways to prolong the lifespan of antimalarial drugs,” said Sashika Richards, a PhD student at Australian National University.
“The current frontline antimalarial drug, artemisinin, is already failing in Asia, and we don’t have anything to replace it. It will be at least 5 years before the next new drug makes it to market. The low-hanging fruit is gone, and it’s now very costly and time-consuming to develop new treatments for malaria.”

infecting a red blood cell
Photo courtesy of St. Jude
Children’s Research Hospital
New research helps explain how one of Plasmodium falciparum’s best weapons against antimalarial drugs can actually be exploited to treat malaria.
Investigators believe the findings, published in PLOS Pathogens, might be used to stop the emergence and spread of drug-resistant malaria.
The team noted that mutations in the P falciparum chloroquine resistance transporter (PfCRT) confer resistance to
chloroquine and related antimalarial drugs by enabling the protein to transport the drugs away from their targets within the parasite’s digestive vacuole.
However, chloroquine resistance-conferring isoforms of PfCRT (PfCRTCQR) also render the parasite hypersensitive to a subset of structurally diverse drugs. And mutations in PfCRTCQR that suppress this hypersensitivity simultaneously reinstate sensitivity to chloroquine and related drugs.
With this study, the investigators uncovered 2 mechanisms by which PfCRT causes P falciparum to become hypersensitive to antimalarial drugs.
First, they found that quinine, which normally exerts its killing effect within the parasite’s digestive vacuole, can bind tightly to certain forms of PfCRT. This blocks the function of the protein, which is essential to the parasite’s survival.
Second, the team found that amantadine, which normally sequesters within the digestive vacuole as well, is leaked back into the cytosol via PfCRT.
The investigators noted that, in both of these cases, mutations that suppress hypersensitivity also revoke PfCRT’s ability to transport chloroquine, which explains why rescue from hypersensitivity restores the parasite’s sensitivity to chloroquine.
“[C]hanges that allow the protein to move chloroquine away from its antimalarial target simultaneously enable the protein to deliver other drugs to their antimalarial targets,” explained study author Rowena Martin, PhD, of Australian National University in Canberra.
“[W]hen the protein adapts itself to fend off one of these drugs, it is no longer able to deal with chloroquine and, hence, the parasite is re-sensitized to chloroquine. Essentially, the parasite can’t have its cake and eat it too. So if chloroquine or a related drug is paired with a drug that is super-active against the modified protein, no matter what the parasite tries to do, it’s ‘checkmate’ for malaria.”
Dr Martin and her colleagues believe their findings provide a foundation for understanding and exploiting the hypersensitivity of chloroquine-resistant parasites to several antimalarial drugs that are currently available.
“Health authorities could use our research to find ways to prolong the lifespan of antimalarial drugs,” said Sashika Richards, a PhD student at Australian National University.
“The current frontline antimalarial drug, artemisinin, is already failing in Asia, and we don’t have anything to replace it. It will be at least 5 years before the next new drug makes it to market. The low-hanging fruit is gone, and it’s now very costly and time-consuming to develop new treatments for malaria.”

infecting a red blood cell
Photo courtesy of St. Jude
Children’s Research Hospital
New research helps explain how one of Plasmodium falciparum’s best weapons against antimalarial drugs can actually be exploited to treat malaria.
Investigators believe the findings, published in PLOS Pathogens, might be used to stop the emergence and spread of drug-resistant malaria.
The team noted that mutations in the P falciparum chloroquine resistance transporter (PfCRT) confer resistance to
chloroquine and related antimalarial drugs by enabling the protein to transport the drugs away from their targets within the parasite’s digestive vacuole.
However, chloroquine resistance-conferring isoforms of PfCRT (PfCRTCQR) also render the parasite hypersensitive to a subset of structurally diverse drugs. And mutations in PfCRTCQR that suppress this hypersensitivity simultaneously reinstate sensitivity to chloroquine and related drugs.
With this study, the investigators uncovered 2 mechanisms by which PfCRT causes P falciparum to become hypersensitive to antimalarial drugs.
First, they found that quinine, which normally exerts its killing effect within the parasite’s digestive vacuole, can bind tightly to certain forms of PfCRT. This blocks the function of the protein, which is essential to the parasite’s survival.
Second, the team found that amantadine, which normally sequesters within the digestive vacuole as well, is leaked back into the cytosol via PfCRT.
The investigators noted that, in both of these cases, mutations that suppress hypersensitivity also revoke PfCRT’s ability to transport chloroquine, which explains why rescue from hypersensitivity restores the parasite’s sensitivity to chloroquine.
“[C]hanges that allow the protein to move chloroquine away from its antimalarial target simultaneously enable the protein to deliver other drugs to their antimalarial targets,” explained study author Rowena Martin, PhD, of Australian National University in Canberra.
“[W]hen the protein adapts itself to fend off one of these drugs, it is no longer able to deal with chloroquine and, hence, the parasite is re-sensitized to chloroquine. Essentially, the parasite can’t have its cake and eat it too. So if chloroquine or a related drug is paired with a drug that is super-active against the modified protein, no matter what the parasite tries to do, it’s ‘checkmate’ for malaria.”
Dr Martin and her colleagues believe their findings provide a foundation for understanding and exploiting the hypersensitivity of chloroquine-resistant parasites to several antimalarial drugs that are currently available.
“Health authorities could use our research to find ways to prolong the lifespan of antimalarial drugs,” said Sashika Richards, a PhD student at Australian National University.
“The current frontline antimalarial drug, artemisinin, is already failing in Asia, and we don’t have anything to replace it. It will be at least 5 years before the next new drug makes it to market. The low-hanging fruit is gone, and it’s now very costly and time-consuming to develop new treatments for malaria.”
Microneedle system could replace blood draws, team says
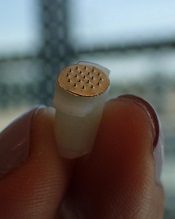
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc.
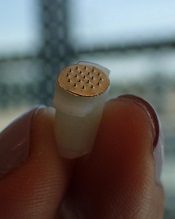
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc.
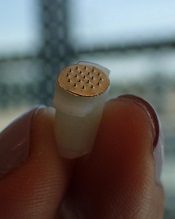
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc.