User login
Cell-free DNA kit receives CE-IVD mark
Vela Diagnostics’ Sentosa® SX Cell-free DNA (cfDNA) Kit has received the CE-IVD mark, which means this kit is approved for in vitro diagnostics use in the European Union.
The Sentosa® SX cfDNA Kit is intended to extract free-circulating DNA from human plasma.
The kit was developed for use in next-generation sequencing and real-time polymerase chain reaction workflows.
The kit is designed to run on the Sentosa® SX101 instrument and works with whole blood samples collected in Cell-free DNA BCT from Streck, K2, or K3 EDTA tubes.
Automated sample extraction with the Sentosa® SX cfDNA Kit takes approximately 3.5 hours. It requires 20 minutes of operator hands-on time and 4 mL of plasma from the clinical sample.
The Sentosa® SX cfDNA Kit is able to recover low-frequency DNA variants in blood, according to Vela Diagnostics.
Results from a pilot study testing the kit were presented in a poster at the AMP 2016 Annual Meeting. ![]()
Vela Diagnostics’ Sentosa® SX Cell-free DNA (cfDNA) Kit has received the CE-IVD mark, which means this kit is approved for in vitro diagnostics use in the European Union.
The Sentosa® SX cfDNA Kit is intended to extract free-circulating DNA from human plasma.
The kit was developed for use in next-generation sequencing and real-time polymerase chain reaction workflows.
The kit is designed to run on the Sentosa® SX101 instrument and works with whole blood samples collected in Cell-free DNA BCT from Streck, K2, or K3 EDTA tubes.
Automated sample extraction with the Sentosa® SX cfDNA Kit takes approximately 3.5 hours. It requires 20 minutes of operator hands-on time and 4 mL of plasma from the clinical sample.
The Sentosa® SX cfDNA Kit is able to recover low-frequency DNA variants in blood, according to Vela Diagnostics.
Results from a pilot study testing the kit were presented in a poster at the AMP 2016 Annual Meeting. ![]()
Vela Diagnostics’ Sentosa® SX Cell-free DNA (cfDNA) Kit has received the CE-IVD mark, which means this kit is approved for in vitro diagnostics use in the European Union.
The Sentosa® SX cfDNA Kit is intended to extract free-circulating DNA from human plasma.
The kit was developed for use in next-generation sequencing and real-time polymerase chain reaction workflows.
The kit is designed to run on the Sentosa® SX101 instrument and works with whole blood samples collected in Cell-free DNA BCT from Streck, K2, or K3 EDTA tubes.
Automated sample extraction with the Sentosa® SX cfDNA Kit takes approximately 3.5 hours. It requires 20 minutes of operator hands-on time and 4 mL of plasma from the clinical sample.
The Sentosa® SX cfDNA Kit is able to recover low-frequency DNA variants in blood, according to Vela Diagnostics.
Results from a pilot study testing the kit were presented in a poster at the AMP 2016 Annual Meeting. ![]()
Team finds no evidence that gadolinium causes neurologic harm
CHICAGO—There is no evidence to suggest that accumulation of gadolinium in the brain speeds cognitive decline, according to research presented at RSNA 2017, the annual meeting of the Radiological Society of North America.*
Recent studies have revealed that traces of the contrast agent gadolinium can be retained in the brain for years after magnetic resonance imaging (MRI).
Earlier this year, the US Food and Drug Administration recommended cautious use of gadolinium-based contrast agents due to the risk of gadolinium retention in various organs, including the brain.
The European Medicines Agency went a step further, recommending restricting the use of some linear gadolinium agents and suspending the authorization of other agents.
Still, very little is known about the health effects of gadolinium that is retained in the brain.
Robert J. McDonald, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues conducted a study to gain some insight.
The team used the Mayo Clinic Study of Aging (MCSA), the world’s largest prospective population-based cohort on aging, to study the effects of gadolinium exposure on neurologic and neurocognitive function.
All MCSA participants underwent extensive neurologic evaluation and neuropsychological testing at baseline and 15-month follow-up intervals.
The researchers compared neurologic and neurocognitive scores of patients with no history of prior gadolinium exposure and patients who underwent prior MRI with gadolinium-based contrast agents.
The team adjusted their analysis for age, sex, education level, baseline neurocognitive performance, and other factors.
The study included 4261 cognitively normal men and women with a mean age of 72 (range, 50-90). The mean duration of study participation was 3.7 years.
Roughly a quarter of the patients (25.6%, n=1092) had received gadolinium-based contrast agents. These patients received a median of 2 doses (range, 1-28), and the median time since first gadolinium exposure was 5.6 years.
The researchers found that gadolinium exposure was not a significant predictor of cognitive decline, as assessed by changes in clinical dementia rating (P=0.48), Blessed dementia scale (P=0.68), and mental status exam score (P=0.55).
Likewise, gadolinium exposure was not a significant predictor of diminished neuropsychological performance (P=0.13) or diminished motor performance (P=0.43), as assessed by the Unified Parkinson’s Disease Rating Scale.
Finally, gadolinium exposure was not an independent risk factor in the rate of cognitive decline from normal cognitive status to dementia (P=0.91).
“Right now, there is concern over the safety of gadolinium-based contrast agents, particularly relating to gadolinium retention in the brain and other tissues,” Dr McDonald said.
“This study provides useful data that, at the reasonable doses 95% of the population is likely to receive in their lifetime, there is no evidence, at this point, that gadolinium retention in the brain is associated with adverse clinical outcomes.” ![]()
*Abstract SSM16-01: Assessment of the Neurologic Effects of Intracranial Gadolinium Deposition Using a Large Population Based Cohort.
CHICAGO—There is no evidence to suggest that accumulation of gadolinium in the brain speeds cognitive decline, according to research presented at RSNA 2017, the annual meeting of the Radiological Society of North America.*
Recent studies have revealed that traces of the contrast agent gadolinium can be retained in the brain for years after magnetic resonance imaging (MRI).
Earlier this year, the US Food and Drug Administration recommended cautious use of gadolinium-based contrast agents due to the risk of gadolinium retention in various organs, including the brain.
The European Medicines Agency went a step further, recommending restricting the use of some linear gadolinium agents and suspending the authorization of other agents.
Still, very little is known about the health effects of gadolinium that is retained in the brain.
Robert J. McDonald, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues conducted a study to gain some insight.
The team used the Mayo Clinic Study of Aging (MCSA), the world’s largest prospective population-based cohort on aging, to study the effects of gadolinium exposure on neurologic and neurocognitive function.
All MCSA participants underwent extensive neurologic evaluation and neuropsychological testing at baseline and 15-month follow-up intervals.
The researchers compared neurologic and neurocognitive scores of patients with no history of prior gadolinium exposure and patients who underwent prior MRI with gadolinium-based contrast agents.
The team adjusted their analysis for age, sex, education level, baseline neurocognitive performance, and other factors.
The study included 4261 cognitively normal men and women with a mean age of 72 (range, 50-90). The mean duration of study participation was 3.7 years.
Roughly a quarter of the patients (25.6%, n=1092) had received gadolinium-based contrast agents. These patients received a median of 2 doses (range, 1-28), and the median time since first gadolinium exposure was 5.6 years.
The researchers found that gadolinium exposure was not a significant predictor of cognitive decline, as assessed by changes in clinical dementia rating (P=0.48), Blessed dementia scale (P=0.68), and mental status exam score (P=0.55).
Likewise, gadolinium exposure was not a significant predictor of diminished neuropsychological performance (P=0.13) or diminished motor performance (P=0.43), as assessed by the Unified Parkinson’s Disease Rating Scale.
Finally, gadolinium exposure was not an independent risk factor in the rate of cognitive decline from normal cognitive status to dementia (P=0.91).
“Right now, there is concern over the safety of gadolinium-based contrast agents, particularly relating to gadolinium retention in the brain and other tissues,” Dr McDonald said.
“This study provides useful data that, at the reasonable doses 95% of the population is likely to receive in their lifetime, there is no evidence, at this point, that gadolinium retention in the brain is associated with adverse clinical outcomes.” ![]()
*Abstract SSM16-01: Assessment of the Neurologic Effects of Intracranial Gadolinium Deposition Using a Large Population Based Cohort.
CHICAGO—There is no evidence to suggest that accumulation of gadolinium in the brain speeds cognitive decline, according to research presented at RSNA 2017, the annual meeting of the Radiological Society of North America.*
Recent studies have revealed that traces of the contrast agent gadolinium can be retained in the brain for years after magnetic resonance imaging (MRI).
Earlier this year, the US Food and Drug Administration recommended cautious use of gadolinium-based contrast agents due to the risk of gadolinium retention in various organs, including the brain.
The European Medicines Agency went a step further, recommending restricting the use of some linear gadolinium agents and suspending the authorization of other agents.
Still, very little is known about the health effects of gadolinium that is retained in the brain.
Robert J. McDonald, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues conducted a study to gain some insight.
The team used the Mayo Clinic Study of Aging (MCSA), the world’s largest prospective population-based cohort on aging, to study the effects of gadolinium exposure on neurologic and neurocognitive function.
All MCSA participants underwent extensive neurologic evaluation and neuropsychological testing at baseline and 15-month follow-up intervals.
The researchers compared neurologic and neurocognitive scores of patients with no history of prior gadolinium exposure and patients who underwent prior MRI with gadolinium-based contrast agents.
The team adjusted their analysis for age, sex, education level, baseline neurocognitive performance, and other factors.
The study included 4261 cognitively normal men and women with a mean age of 72 (range, 50-90). The mean duration of study participation was 3.7 years.
Roughly a quarter of the patients (25.6%, n=1092) had received gadolinium-based contrast agents. These patients received a median of 2 doses (range, 1-28), and the median time since first gadolinium exposure was 5.6 years.
The researchers found that gadolinium exposure was not a significant predictor of cognitive decline, as assessed by changes in clinical dementia rating (P=0.48), Blessed dementia scale (P=0.68), and mental status exam score (P=0.55).
Likewise, gadolinium exposure was not a significant predictor of diminished neuropsychological performance (P=0.13) or diminished motor performance (P=0.43), as assessed by the Unified Parkinson’s Disease Rating Scale.
Finally, gadolinium exposure was not an independent risk factor in the rate of cognitive decline from normal cognitive status to dementia (P=0.91).
“Right now, there is concern over the safety of gadolinium-based contrast agents, particularly relating to gadolinium retention in the brain and other tissues,” Dr McDonald said.
“This study provides useful data that, at the reasonable doses 95% of the population is likely to receive in their lifetime, there is no evidence, at this point, that gadolinium retention in the brain is associated with adverse clinical outcomes.” ![]()
*Abstract SSM16-01: Assessment of the Neurologic Effects of Intracranial Gadolinium Deposition Using a Large Population Based Cohort.
Authors’ contributions to studies often unclear
Although many scientific journals try to provide details about authors’ contributions to a publication by requiring explicit statements, contribution statements get much less attention than authorship order, according to research published in Science Advances.
Researchers surveyed more than 6000 corresponding authors of studies published in recent years and found they consider contribution statements helpful for understanding the specific skills individual authors bring to a study.
However, the respondents said they still use author order for deciphering which authors did how much of the work and deserve most of the credit.
“The lack of uniformity and detail in contribution statements leaves open the door for varied interpretations, which could be why only a minority of respondents found them more useful than author order,” said Henry Sauermann, PhD, of ESMT Berlin in Germany.
Dr Sauermann and his colleagues also examined the relationship between author order and contribution statements on more than 12,000 published articles.
The contribution statements studied did include information about the types of work contributed by each author. However, multiple authors could be listed under the same contributions, and the statements had little information about the level of effort for each author.
The statements also said little about how important a particular contribution was for project success.
Still, Dr Sauermann and his colleagues noted that author order has its own problems.
“When we talked to scientists, many think that there are certain norms, and they know how to interpret author order,” Dr Sauermann said. “But when you really push, it’s not clear at all, at least not at the level of detail we need.”
That’s further complicated by the fact that conventions of author order vary depending on the research field.
This work also revealed a difference of opinion between junior and senior researchers, with the former caring more strongly about contribution statements and how they are discussed and crafted.
“When we read open-ended responses to our survey questions, we got the impression of a really divided community,” Dr Sauermann said. “Some believe that forcing more detail in contribution statements is great, and some are concerned that it could really hurt teamwork and collaboration. It’s not that everyone is lukewarm; many really care.”
That level of interest could pave the way for more discussion, which is something Dr Sauermann said is ultimately needed for the scientific and research community to move forward and add more clarity to the process.
“This is not going to get any easier,” Dr Sauermann said. “It’s going to get harder as how we perform research changes and as teams get bigger and more diverse.” ![]()
Although many scientific journals try to provide details about authors’ contributions to a publication by requiring explicit statements, contribution statements get much less attention than authorship order, according to research published in Science Advances.
Researchers surveyed more than 6000 corresponding authors of studies published in recent years and found they consider contribution statements helpful for understanding the specific skills individual authors bring to a study.
However, the respondents said they still use author order for deciphering which authors did how much of the work and deserve most of the credit.
“The lack of uniformity and detail in contribution statements leaves open the door for varied interpretations, which could be why only a minority of respondents found them more useful than author order,” said Henry Sauermann, PhD, of ESMT Berlin in Germany.
Dr Sauermann and his colleagues also examined the relationship between author order and contribution statements on more than 12,000 published articles.
The contribution statements studied did include information about the types of work contributed by each author. However, multiple authors could be listed under the same contributions, and the statements had little information about the level of effort for each author.
The statements also said little about how important a particular contribution was for project success.
Still, Dr Sauermann and his colleagues noted that author order has its own problems.
“When we talked to scientists, many think that there are certain norms, and they know how to interpret author order,” Dr Sauermann said. “But when you really push, it’s not clear at all, at least not at the level of detail we need.”
That’s further complicated by the fact that conventions of author order vary depending on the research field.
This work also revealed a difference of opinion between junior and senior researchers, with the former caring more strongly about contribution statements and how they are discussed and crafted.
“When we read open-ended responses to our survey questions, we got the impression of a really divided community,” Dr Sauermann said. “Some believe that forcing more detail in contribution statements is great, and some are concerned that it could really hurt teamwork and collaboration. It’s not that everyone is lukewarm; many really care.”
That level of interest could pave the way for more discussion, which is something Dr Sauermann said is ultimately needed for the scientific and research community to move forward and add more clarity to the process.
“This is not going to get any easier,” Dr Sauermann said. “It’s going to get harder as how we perform research changes and as teams get bigger and more diverse.” ![]()
Although many scientific journals try to provide details about authors’ contributions to a publication by requiring explicit statements, contribution statements get much less attention than authorship order, according to research published in Science Advances.
Researchers surveyed more than 6000 corresponding authors of studies published in recent years and found they consider contribution statements helpful for understanding the specific skills individual authors bring to a study.
However, the respondents said they still use author order for deciphering which authors did how much of the work and deserve most of the credit.
“The lack of uniformity and detail in contribution statements leaves open the door for varied interpretations, which could be why only a minority of respondents found them more useful than author order,” said Henry Sauermann, PhD, of ESMT Berlin in Germany.
Dr Sauermann and his colleagues also examined the relationship between author order and contribution statements on more than 12,000 published articles.
The contribution statements studied did include information about the types of work contributed by each author. However, multiple authors could be listed under the same contributions, and the statements had little information about the level of effort for each author.
The statements also said little about how important a particular contribution was for project success.
Still, Dr Sauermann and his colleagues noted that author order has its own problems.
“When we talked to scientists, many think that there are certain norms, and they know how to interpret author order,” Dr Sauermann said. “But when you really push, it’s not clear at all, at least not at the level of detail we need.”
That’s further complicated by the fact that conventions of author order vary depending on the research field.
This work also revealed a difference of opinion between junior and senior researchers, with the former caring more strongly about contribution statements and how they are discussed and crafted.
“When we read open-ended responses to our survey questions, we got the impression of a really divided community,” Dr Sauermann said. “Some believe that forcing more detail in contribution statements is great, and some are concerned that it could really hurt teamwork and collaboration. It’s not that everyone is lukewarm; many really care.”
That level of interest could pave the way for more discussion, which is something Dr Sauermann said is ultimately needed for the scientific and research community to move forward and add more clarity to the process.
“This is not going to get any easier,” Dr Sauermann said. “It’s going to get harder as how we perform research changes and as teams get bigger and more diverse.” ![]()
PTSD can persist in cancer survivors
Cancer patients may experience lasting post-traumatic stress disorder (PTSD), according to a study published in the journal Cancer.
Approximately one-fifth of patients involved in the study experienced PTSD several months after their cancer diagnosis, and roughly a third of these patients continued to live with PTSD 4 years later.
Researchers say these findings highlight the need for early identification, careful monitoring, and treatment of PTSD in cancer survivors.
Caryn Mei Hsien Chan, PhD, of the National University of Malaysia in Kuala Lumpur, and her colleagues conducted this research.
The study included 469 adults with various cancers who were within 1 month of cancer diagnosis at enrollment.
Patients who had significant psychological distress (defined as a Hospital Anxiety and Depression Scale total cutoff score of 16 or higher) underwent
testing for PTSD at 6 months of follow-up. All patients were tested for PTSD at 4 years of follow-up (regardless of their Hospital Anxiety and Depression Scale score).
The incidence of PTSD was 21.7% at 6 months and 6.1% at 4 years. Although overall rates of PTSD decreased with time, roughly one-third of patients initially diagnosed with PTSD were found to have persistent or worsening symptoms 4 years later.
“Many cancer patients believe they need to adopt a ‘warrior mentality’ and remain positive and optimistic from diagnosis through treatment to stand a better chance of beating their cancer,” Dr Chan said.
“To these patients, seeking help for the emotional issues they face is akin to admitting weakness. There needs to be greater awareness that there is nothing wrong with getting help to manage the emotional upheaval—particularly depression, anxiety, and PTSD—post-cancer.”
Dr Chan also stressed that many patients live in fear that their cancer may come back, and they may think the cancer has returned with every lump or bump, pain or ache, fatigue or fever.
In addition, cancer survivors might skip visits to their oncologists or other physicians to avoid triggering memories of their past cancer experience. This can lead to delays in seeking help for new symptoms or even refusal of treatment for unrelated conditions.
“We need psychological evaluation and support services for patients with cancer at an initial stage and at continued follows-up because psychological well-being and mental health—and by extension, quality of life—are just as important as physical health,” Dr Chan noted. ![]()
Cancer patients may experience lasting post-traumatic stress disorder (PTSD), according to a study published in the journal Cancer.
Approximately one-fifth of patients involved in the study experienced PTSD several months after their cancer diagnosis, and roughly a third of these patients continued to live with PTSD 4 years later.
Researchers say these findings highlight the need for early identification, careful monitoring, and treatment of PTSD in cancer survivors.
Caryn Mei Hsien Chan, PhD, of the National University of Malaysia in Kuala Lumpur, and her colleagues conducted this research.
The study included 469 adults with various cancers who were within 1 month of cancer diagnosis at enrollment.
Patients who had significant psychological distress (defined as a Hospital Anxiety and Depression Scale total cutoff score of 16 or higher) underwent
testing for PTSD at 6 months of follow-up. All patients were tested for PTSD at 4 years of follow-up (regardless of their Hospital Anxiety and Depression Scale score).
The incidence of PTSD was 21.7% at 6 months and 6.1% at 4 years. Although overall rates of PTSD decreased with time, roughly one-third of patients initially diagnosed with PTSD were found to have persistent or worsening symptoms 4 years later.
“Many cancer patients believe they need to adopt a ‘warrior mentality’ and remain positive and optimistic from diagnosis through treatment to stand a better chance of beating their cancer,” Dr Chan said.
“To these patients, seeking help for the emotional issues they face is akin to admitting weakness. There needs to be greater awareness that there is nothing wrong with getting help to manage the emotional upheaval—particularly depression, anxiety, and PTSD—post-cancer.”
Dr Chan also stressed that many patients live in fear that their cancer may come back, and they may think the cancer has returned with every lump or bump, pain or ache, fatigue or fever.
In addition, cancer survivors might skip visits to their oncologists or other physicians to avoid triggering memories of their past cancer experience. This can lead to delays in seeking help for new symptoms or even refusal of treatment for unrelated conditions.
“We need psychological evaluation and support services for patients with cancer at an initial stage and at continued follows-up because psychological well-being and mental health—and by extension, quality of life—are just as important as physical health,” Dr Chan noted. ![]()
Cancer patients may experience lasting post-traumatic stress disorder (PTSD), according to a study published in the journal Cancer.
Approximately one-fifth of patients involved in the study experienced PTSD several months after their cancer diagnosis, and roughly a third of these patients continued to live with PTSD 4 years later.
Researchers say these findings highlight the need for early identification, careful monitoring, and treatment of PTSD in cancer survivors.
Caryn Mei Hsien Chan, PhD, of the National University of Malaysia in Kuala Lumpur, and her colleagues conducted this research.
The study included 469 adults with various cancers who were within 1 month of cancer diagnosis at enrollment.
Patients who had significant psychological distress (defined as a Hospital Anxiety and Depression Scale total cutoff score of 16 or higher) underwent
testing for PTSD at 6 months of follow-up. All patients were tested for PTSD at 4 years of follow-up (regardless of their Hospital Anxiety and Depression Scale score).
The incidence of PTSD was 21.7% at 6 months and 6.1% at 4 years. Although overall rates of PTSD decreased with time, roughly one-third of patients initially diagnosed with PTSD were found to have persistent or worsening symptoms 4 years later.
“Many cancer patients believe they need to adopt a ‘warrior mentality’ and remain positive and optimistic from diagnosis through treatment to stand a better chance of beating their cancer,” Dr Chan said.
“To these patients, seeking help for the emotional issues they face is akin to admitting weakness. There needs to be greater awareness that there is nothing wrong with getting help to manage the emotional upheaval—particularly depression, anxiety, and PTSD—post-cancer.”
Dr Chan also stressed that many patients live in fear that their cancer may come back, and they may think the cancer has returned with every lump or bump, pain or ache, fatigue or fever.
In addition, cancer survivors might skip visits to their oncologists or other physicians to avoid triggering memories of their past cancer experience. This can lead to delays in seeking help for new symptoms or even refusal of treatment for unrelated conditions.
“We need psychological evaluation and support services for patients with cancer at an initial stage and at continued follows-up because psychological well-being and mental health—and by extension, quality of life—are just as important as physical health,” Dr Chan noted. ![]()
Antimalarial might fight Zika virus
Preclinical research suggests a drug used to prevent and treat malaria may also be effective against Zika virus.
Investigators found that chloroquine can protect human neural progenitors from infection with Zika virus.
The drug also decreased Zika-induced mortality in one mouse model and hindered transmission of Zika virus from mother to fetus in another mouse model.
Alexey Terskikh, PhD, of Sanford Burnham Prebys Medical Discovery Institute in La Jolla, California, and his colleagues conducted this research and disclosed the results in Scientific Reports.
“There is still an urgent need to bolster our preparedness and capacity to respond to the next Zika outbreak,” Dr Terskikh said. “Our latest research suggests the antimalaria drug chloroquine may be an effective drug to treat and prevent Zika infections.”
The investigators first found that chloroquine reduced Zika infection in primary human fetal neural precursor cells.
The team also discovered that chloroquine reduced the percentage of Zika-positive cells and the level of apoptosis in neurospheres derived from human induced pluripotent stem cells.
The investigators then tested chloroquine in AG129 mice, which lack receptors for type I and II interferons and have been used to model Zika virus infection.
Some of these mice received chloroquine (50 mg/kg/day) in their drinking water for 2 days and were then infected with Zika virus. The mice continued to receive chloroquine at the same dose for 5 days and then received 5 mg/kg/day until the end of the experiment.
Control AG129 mice were infected with Zika virus and received regular drinking water.
Compared to controls, chloroquine-treated mice had significantly prolonged survival and a significant reduction in Zika-induced weight loss (P<0.01 for both).
Next, the investigators used SJL mice to study horizontal and vertical transmission of Zika. They observed successful transmission of the virus from males to females and from mothers to pups.
The team then analyzed the effects of chloroquine on fetal transmission of Zika. Pregnant SJL mice were infected with Zika and given drinking water containing chloroquine (30 mg/kg/day) starting on day E13.5. The mice were euthanized on E18.5, and maternal blood and fetal brain samples were collected.
Chloroquine treatment resulted in a roughly 20-fold reduction in Zika virus titers in the maternal blood and fetal brain.
“Although chloroquine didn’t completely clear Zika from infected mice, it did reduce the viral load, suggesting it could limit the neurological damage found in newborns infected by the virus,” Dr Terskikh said.
“Chloroquine has a long history of successfully treating malaria, and there are no reports of it causing birth defects. Additional studies are certainly needed to determine the precise details of how it works. But given its low cost, availability, and safety history, further study in a clinical trial to test its effectiveness against Zika virus in humans is merited.” ![]()
Preclinical research suggests a drug used to prevent and treat malaria may also be effective against Zika virus.
Investigators found that chloroquine can protect human neural progenitors from infection with Zika virus.
The drug also decreased Zika-induced mortality in one mouse model and hindered transmission of Zika virus from mother to fetus in another mouse model.
Alexey Terskikh, PhD, of Sanford Burnham Prebys Medical Discovery Institute in La Jolla, California, and his colleagues conducted this research and disclosed the results in Scientific Reports.
“There is still an urgent need to bolster our preparedness and capacity to respond to the next Zika outbreak,” Dr Terskikh said. “Our latest research suggests the antimalaria drug chloroquine may be an effective drug to treat and prevent Zika infections.”
The investigators first found that chloroquine reduced Zika infection in primary human fetal neural precursor cells.
The team also discovered that chloroquine reduced the percentage of Zika-positive cells and the level of apoptosis in neurospheres derived from human induced pluripotent stem cells.
The investigators then tested chloroquine in AG129 mice, which lack receptors for type I and II interferons and have been used to model Zika virus infection.
Some of these mice received chloroquine (50 mg/kg/day) in their drinking water for 2 days and were then infected with Zika virus. The mice continued to receive chloroquine at the same dose for 5 days and then received 5 mg/kg/day until the end of the experiment.
Control AG129 mice were infected with Zika virus and received regular drinking water.
Compared to controls, chloroquine-treated mice had significantly prolonged survival and a significant reduction in Zika-induced weight loss (P<0.01 for both).
Next, the investigators used SJL mice to study horizontal and vertical transmission of Zika. They observed successful transmission of the virus from males to females and from mothers to pups.
The team then analyzed the effects of chloroquine on fetal transmission of Zika. Pregnant SJL mice were infected with Zika and given drinking water containing chloroquine (30 mg/kg/day) starting on day E13.5. The mice were euthanized on E18.5, and maternal blood and fetal brain samples were collected.
Chloroquine treatment resulted in a roughly 20-fold reduction in Zika virus titers in the maternal blood and fetal brain.
“Although chloroquine didn’t completely clear Zika from infected mice, it did reduce the viral load, suggesting it could limit the neurological damage found in newborns infected by the virus,” Dr Terskikh said.
“Chloroquine has a long history of successfully treating malaria, and there are no reports of it causing birth defects. Additional studies are certainly needed to determine the precise details of how it works. But given its low cost, availability, and safety history, further study in a clinical trial to test its effectiveness against Zika virus in humans is merited.” ![]()
Preclinical research suggests a drug used to prevent and treat malaria may also be effective against Zika virus.
Investigators found that chloroquine can protect human neural progenitors from infection with Zika virus.
The drug also decreased Zika-induced mortality in one mouse model and hindered transmission of Zika virus from mother to fetus in another mouse model.
Alexey Terskikh, PhD, of Sanford Burnham Prebys Medical Discovery Institute in La Jolla, California, and his colleagues conducted this research and disclosed the results in Scientific Reports.
“There is still an urgent need to bolster our preparedness and capacity to respond to the next Zika outbreak,” Dr Terskikh said. “Our latest research suggests the antimalaria drug chloroquine may be an effective drug to treat and prevent Zika infections.”
The investigators first found that chloroquine reduced Zika infection in primary human fetal neural precursor cells.
The team also discovered that chloroquine reduced the percentage of Zika-positive cells and the level of apoptosis in neurospheres derived from human induced pluripotent stem cells.
The investigators then tested chloroquine in AG129 mice, which lack receptors for type I and II interferons and have been used to model Zika virus infection.
Some of these mice received chloroquine (50 mg/kg/day) in their drinking water for 2 days and were then infected with Zika virus. The mice continued to receive chloroquine at the same dose for 5 days and then received 5 mg/kg/day until the end of the experiment.
Control AG129 mice were infected with Zika virus and received regular drinking water.
Compared to controls, chloroquine-treated mice had significantly prolonged survival and a significant reduction in Zika-induced weight loss (P<0.01 for both).
Next, the investigators used SJL mice to study horizontal and vertical transmission of Zika. They observed successful transmission of the virus from males to females and from mothers to pups.
The team then analyzed the effects of chloroquine on fetal transmission of Zika. Pregnant SJL mice were infected with Zika and given drinking water containing chloroquine (30 mg/kg/day) starting on day E13.5. The mice were euthanized on E18.5, and maternal blood and fetal brain samples were collected.
Chloroquine treatment resulted in a roughly 20-fold reduction in Zika virus titers in the maternal blood and fetal brain.
“Although chloroquine didn’t completely clear Zika from infected mice, it did reduce the viral load, suggesting it could limit the neurological damage found in newborns infected by the virus,” Dr Terskikh said.
“Chloroquine has a long history of successfully treating malaria, and there are no reports of it causing birth defects. Additional studies are certainly needed to determine the precise details of how it works. But given its low cost, availability, and safety history, further study in a clinical trial to test its effectiveness against Zika virus in humans is merited.” ![]()
Parity laws don’t lower oral cancer drug costs for everyone
US state laws intended to ensure fair prices for oral cancer drugs have had a mixed impact on patients’ pocketbooks, according to a study published in JAMA Oncology.
A total of 43 states and Washington, DC, have enacted parity laws, which require that patients pay no more for an oral cancer treatment than they would for an infusion of the same treatment.
Researchers analyzed the impact of these laws and observed modest improvements in costs for some patients.
However, patients who were already paying the most for their medications saw their monthly costs go up.
“Although parity laws appear to help reduce out-of-pocket spending for some patients, they may not fully address affordability for patients needing cancer drugs,” said study author Stacie B. Dusetzina, PhD, of the University of North Carolina at Chapel Hill.
“We need to consider ways to address drug pricing directly and to improve benefit design to make sure that all patients can access prescribed drugs.”
To gauge the impact of parity laws on treatment costs, Dr Dusetzina and her colleagues analyzed health claims data for 63,780 adults from 3 large, nationwide insurance companies before and after the laws were enacted, from 2008 to 2012.
The team compared the cost of filling an oral cancer drug prescription for patients with health insurance plans that were covered by the state laws (fully insured) and patients whose plans were not (self-funded). All patients lived in 1 of 16 states that had passed parity laws at the time of the study.
About half of patients (51.4%) had fully insured plans, and the other half (48.6%) had self-funded plans.
For the entire cohort, the use of oral cancer drugs increased from 18% in the months before parity laws were passed to 22% in the months after (adjusted difference-in-differences risk ratio [aDDRR], 1.04; 95% confidence interval [CI], 0.96-1.13; P=0.34).
The proportion of prescription fills for oral drugs without copayment increased from 15.0% to 53.0% for patients with fully insured plans and from 12.3% to 18.0% in patients with self-funded plans (aDDRR, 2.36; 95% CI, 2.00-2.79; P<0.001).
“From our results, it looks like many plans decided they would just set the co-pay for oral drugs to $0,” Dr Dusetzina said. “Instead of $30 per month, those fills were now $0.”
The proportion of prescription fills with out-of-pocket cost of more than $100 per month increased from 8.4% to 11.1% for patients with fully insured plans but decreased from 12.0% to 11.7% for those with self-funded plans (aDDRR, 1.36; 95% CI, 1.11-1.68; P=0.004).
Patients paying the most for their oral cancer drug prescriptions experienced increases in their monthly out-of-pocket costs after parity laws were passed.
For patients whose costs were more expensive than 95% of other patients, their out-of-pocket costs increased an estimated $143.25 per month. Those paying more than 90% of what other patients paid saw their costs increase by $37.19 per month.
“One of the biggest problems with parity laws as they are written is that they don’t address the prices of these medications, which can be very high,” Dr Dusetzina noted.
“Parity can be reached as long as the coverage is the same for both oral and infused cancer therapies. Because we’re now seeing more people insured by plans with high deductibles or plans that require them to pay a percentage of their drug costs, parity may not reduce spending for some patients.”
However, Dr Dusetzina and her colleagues did find that patients who paid the least for their oral cancer treatments saw their estimated monthly out-of-pocket spending decrease.
Patients in the 25th percentile saw an estimated decrease of $19.44 per month, those in the 50th percentile saw a $32.13 decrease, and patients in the 75th percentile saw a decrease of $10.83.
On the other hand, the researchers also found that average 6-month healthcare costs—including what was paid by insurance companies and patients—did not change significantly as a result of parity laws.
The aDDRR was 0.96 (95% CI, 0.90-1.02; P=0.09) for all cancer treatments and 1.06 (95% CI, 0.93-1.20; P=0.40) for oral cancer drugs.
“One of the key arguments against passing parity, both for states that haven’t passed it and for legislation at the federal level, has been that it may increase costs to health plans,” Dr Dusetzina said. “But we didn’t find evidence of that.” ![]()
US state laws intended to ensure fair prices for oral cancer drugs have had a mixed impact on patients’ pocketbooks, according to a study published in JAMA Oncology.
A total of 43 states and Washington, DC, have enacted parity laws, which require that patients pay no more for an oral cancer treatment than they would for an infusion of the same treatment.
Researchers analyzed the impact of these laws and observed modest improvements in costs for some patients.
However, patients who were already paying the most for their medications saw their monthly costs go up.
“Although parity laws appear to help reduce out-of-pocket spending for some patients, they may not fully address affordability for patients needing cancer drugs,” said study author Stacie B. Dusetzina, PhD, of the University of North Carolina at Chapel Hill.
“We need to consider ways to address drug pricing directly and to improve benefit design to make sure that all patients can access prescribed drugs.”
To gauge the impact of parity laws on treatment costs, Dr Dusetzina and her colleagues analyzed health claims data for 63,780 adults from 3 large, nationwide insurance companies before and after the laws were enacted, from 2008 to 2012.
The team compared the cost of filling an oral cancer drug prescription for patients with health insurance plans that were covered by the state laws (fully insured) and patients whose plans were not (self-funded). All patients lived in 1 of 16 states that had passed parity laws at the time of the study.
About half of patients (51.4%) had fully insured plans, and the other half (48.6%) had self-funded plans.
For the entire cohort, the use of oral cancer drugs increased from 18% in the months before parity laws were passed to 22% in the months after (adjusted difference-in-differences risk ratio [aDDRR], 1.04; 95% confidence interval [CI], 0.96-1.13; P=0.34).
The proportion of prescription fills for oral drugs without copayment increased from 15.0% to 53.0% for patients with fully insured plans and from 12.3% to 18.0% in patients with self-funded plans (aDDRR, 2.36; 95% CI, 2.00-2.79; P<0.001).
“From our results, it looks like many plans decided they would just set the co-pay for oral drugs to $0,” Dr Dusetzina said. “Instead of $30 per month, those fills were now $0.”
The proportion of prescription fills with out-of-pocket cost of more than $100 per month increased from 8.4% to 11.1% for patients with fully insured plans but decreased from 12.0% to 11.7% for those with self-funded plans (aDDRR, 1.36; 95% CI, 1.11-1.68; P=0.004).
Patients paying the most for their oral cancer drug prescriptions experienced increases in their monthly out-of-pocket costs after parity laws were passed.
For patients whose costs were more expensive than 95% of other patients, their out-of-pocket costs increased an estimated $143.25 per month. Those paying more than 90% of what other patients paid saw their costs increase by $37.19 per month.
“One of the biggest problems with parity laws as they are written is that they don’t address the prices of these medications, which can be very high,” Dr Dusetzina noted.
“Parity can be reached as long as the coverage is the same for both oral and infused cancer therapies. Because we’re now seeing more people insured by plans with high deductibles or plans that require them to pay a percentage of their drug costs, parity may not reduce spending for some patients.”
However, Dr Dusetzina and her colleagues did find that patients who paid the least for their oral cancer treatments saw their estimated monthly out-of-pocket spending decrease.
Patients in the 25th percentile saw an estimated decrease of $19.44 per month, those in the 50th percentile saw a $32.13 decrease, and patients in the 75th percentile saw a decrease of $10.83.
On the other hand, the researchers also found that average 6-month healthcare costs—including what was paid by insurance companies and patients—did not change significantly as a result of parity laws.
The aDDRR was 0.96 (95% CI, 0.90-1.02; P=0.09) for all cancer treatments and 1.06 (95% CI, 0.93-1.20; P=0.40) for oral cancer drugs.
“One of the key arguments against passing parity, both for states that haven’t passed it and for legislation at the federal level, has been that it may increase costs to health plans,” Dr Dusetzina said. “But we didn’t find evidence of that.” ![]()
US state laws intended to ensure fair prices for oral cancer drugs have had a mixed impact on patients’ pocketbooks, according to a study published in JAMA Oncology.
A total of 43 states and Washington, DC, have enacted parity laws, which require that patients pay no more for an oral cancer treatment than they would for an infusion of the same treatment.
Researchers analyzed the impact of these laws and observed modest improvements in costs for some patients.
However, patients who were already paying the most for their medications saw their monthly costs go up.
“Although parity laws appear to help reduce out-of-pocket spending for some patients, they may not fully address affordability for patients needing cancer drugs,” said study author Stacie B. Dusetzina, PhD, of the University of North Carolina at Chapel Hill.
“We need to consider ways to address drug pricing directly and to improve benefit design to make sure that all patients can access prescribed drugs.”
To gauge the impact of parity laws on treatment costs, Dr Dusetzina and her colleagues analyzed health claims data for 63,780 adults from 3 large, nationwide insurance companies before and after the laws were enacted, from 2008 to 2012.
The team compared the cost of filling an oral cancer drug prescription for patients with health insurance plans that were covered by the state laws (fully insured) and patients whose plans were not (self-funded). All patients lived in 1 of 16 states that had passed parity laws at the time of the study.
About half of patients (51.4%) had fully insured plans, and the other half (48.6%) had self-funded plans.
For the entire cohort, the use of oral cancer drugs increased from 18% in the months before parity laws were passed to 22% in the months after (adjusted difference-in-differences risk ratio [aDDRR], 1.04; 95% confidence interval [CI], 0.96-1.13; P=0.34).
The proportion of prescription fills for oral drugs without copayment increased from 15.0% to 53.0% for patients with fully insured plans and from 12.3% to 18.0% in patients with self-funded plans (aDDRR, 2.36; 95% CI, 2.00-2.79; P<0.001).
“From our results, it looks like many plans decided they would just set the co-pay for oral drugs to $0,” Dr Dusetzina said. “Instead of $30 per month, those fills were now $0.”
The proportion of prescription fills with out-of-pocket cost of more than $100 per month increased from 8.4% to 11.1% for patients with fully insured plans but decreased from 12.0% to 11.7% for those with self-funded plans (aDDRR, 1.36; 95% CI, 1.11-1.68; P=0.004).
Patients paying the most for their oral cancer drug prescriptions experienced increases in their monthly out-of-pocket costs after parity laws were passed.
For patients whose costs were more expensive than 95% of other patients, their out-of-pocket costs increased an estimated $143.25 per month. Those paying more than 90% of what other patients paid saw their costs increase by $37.19 per month.
“One of the biggest problems with parity laws as they are written is that they don’t address the prices of these medications, which can be very high,” Dr Dusetzina noted.
“Parity can be reached as long as the coverage is the same for both oral and infused cancer therapies. Because we’re now seeing more people insured by plans with high deductibles or plans that require them to pay a percentage of their drug costs, parity may not reduce spending for some patients.”
However, Dr Dusetzina and her colleagues did find that patients who paid the least for their oral cancer treatments saw their estimated monthly out-of-pocket spending decrease.
Patients in the 25th percentile saw an estimated decrease of $19.44 per month, those in the 50th percentile saw a $32.13 decrease, and patients in the 75th percentile saw a decrease of $10.83.
On the other hand, the researchers also found that average 6-month healthcare costs—including what was paid by insurance companies and patients—did not change significantly as a result of parity laws.
The aDDRR was 0.96 (95% CI, 0.90-1.02; P=0.09) for all cancer treatments and 1.06 (95% CI, 0.93-1.20; P=0.40) for oral cancer drugs.
“One of the key arguments against passing parity, both for states that haven’t passed it and for legislation at the federal level, has been that it may increase costs to health plans,” Dr Dusetzina said. “But we didn’t find evidence of that.” ![]()
FDA approves IV formulation of aprepitant for CINV
The US Food and Drug Administration (FDA) has approved use of an intravenous (IV) formulation of aprepitant (CINVANTI™) to prevent chemotherapy-induced nausea and vomiting (CINV).
CINVANTI is intended to be used in combination with other antiemetic agents to prevent acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC).
CINVANTI is to be used in combination with a 5-HT3 receptor antagonist and dexamethasone.
The full prescribing information is available at www.cinvanti.com.
The US commercial launch of CINVANTI is planned for January 2018.
CINVANTI is the first IV formulation to directly deliver aprepitant, a substance P/neurokinin-1 (NK1) receptor antagonist.
Aprepitant is also the active ingredient in EMEND® capsules, which were approved by the FDA in 2003. EMEND IV®, which was approved in 2008, contains aprepitant’s prodrug, fosaprepitant.
Heron Therapeutics, Inc., developed CINVANTI in an attempt to provide an IV formulation of aprepitant that has the same efficacy as IV fosaprepitant but does not pose the risk of adverse events (AEs) related to polysorbate 80.
“Aprepitant has long been the standard in the NK1 class, and it remains the only single-agent NK1 with proven efficacy in preventing CINV in both the acute and delayed phases in HEC and MEC,” said Rudolph M. Navari, MD, PhD, of the University of Alabama Birmingham School of Medicine.
“Because CINVANTI is a novel, polysorbate 80-free, IV formulation of aprepitant, it enables physicians to provide patients with standard-of-care efficacy without the potential risk of polysorbate 80-related adverse events, such as infusion-site reactions.”
The FDA approved CINVANTI based on data demonstrating the bioequivalence of CINVANTI to EMEND IV.
A phase 1, randomized, 2-way cross-over study comparing the drugs enrolled 100 healthy subjects. The subjects received CINVANTI at 130 mg or EMEND IV at 150 mg, given over 30 minutes on day 1 of periods 1 and 2.
The researchers said 90% confidence intervals for CINVANTI AUC0-t (area under the time-concentration curve from time 0 to the last measurable concentration), AUC0-inf (area under the time-concentration curve from time 0 extrapolated to infinity), and C12h (plasma concentration at 12 hours) “were well within bioequivalence bounds,” which was 80% to 125%.
The team also found the incidence of treatment-emergent AEs was lower with CINVANTI than EMEND IV—21% and 28%, respectively. The same was true for related treatment-emergent AEs—15% and 28%, respectively.
These data were presented at the Hematology/Oncology Pharmacy Association Annual Conference in March/April and the Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) Annual Meeting in June. ![]()
The US Food and Drug Administration (FDA) has approved use of an intravenous (IV) formulation of aprepitant (CINVANTI™) to prevent chemotherapy-induced nausea and vomiting (CINV).
CINVANTI is intended to be used in combination with other antiemetic agents to prevent acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC).
CINVANTI is to be used in combination with a 5-HT3 receptor antagonist and dexamethasone.
The full prescribing information is available at www.cinvanti.com.
The US commercial launch of CINVANTI is planned for January 2018.
CINVANTI is the first IV formulation to directly deliver aprepitant, a substance P/neurokinin-1 (NK1) receptor antagonist.
Aprepitant is also the active ingredient in EMEND® capsules, which were approved by the FDA in 2003. EMEND IV®, which was approved in 2008, contains aprepitant’s prodrug, fosaprepitant.
Heron Therapeutics, Inc., developed CINVANTI in an attempt to provide an IV formulation of aprepitant that has the same efficacy as IV fosaprepitant but does not pose the risk of adverse events (AEs) related to polysorbate 80.
“Aprepitant has long been the standard in the NK1 class, and it remains the only single-agent NK1 with proven efficacy in preventing CINV in both the acute and delayed phases in HEC and MEC,” said Rudolph M. Navari, MD, PhD, of the University of Alabama Birmingham School of Medicine.
“Because CINVANTI is a novel, polysorbate 80-free, IV formulation of aprepitant, it enables physicians to provide patients with standard-of-care efficacy without the potential risk of polysorbate 80-related adverse events, such as infusion-site reactions.”
The FDA approved CINVANTI based on data demonstrating the bioequivalence of CINVANTI to EMEND IV.
A phase 1, randomized, 2-way cross-over study comparing the drugs enrolled 100 healthy subjects. The subjects received CINVANTI at 130 mg or EMEND IV at 150 mg, given over 30 minutes on day 1 of periods 1 and 2.
The researchers said 90% confidence intervals for CINVANTI AUC0-t (area under the time-concentration curve from time 0 to the last measurable concentration), AUC0-inf (area under the time-concentration curve from time 0 extrapolated to infinity), and C12h (plasma concentration at 12 hours) “were well within bioequivalence bounds,” which was 80% to 125%.
The team also found the incidence of treatment-emergent AEs was lower with CINVANTI than EMEND IV—21% and 28%, respectively. The same was true for related treatment-emergent AEs—15% and 28%, respectively.
These data were presented at the Hematology/Oncology Pharmacy Association Annual Conference in March/April and the Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) Annual Meeting in June. ![]()
The US Food and Drug Administration (FDA) has approved use of an intravenous (IV) formulation of aprepitant (CINVANTI™) to prevent chemotherapy-induced nausea and vomiting (CINV).
CINVANTI is intended to be used in combination with other antiemetic agents to prevent acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic chemotherapy (HEC) and moderately emetogenic chemotherapy (MEC).
CINVANTI is to be used in combination with a 5-HT3 receptor antagonist and dexamethasone.
The full prescribing information is available at www.cinvanti.com.
The US commercial launch of CINVANTI is planned for January 2018.
CINVANTI is the first IV formulation to directly deliver aprepitant, a substance P/neurokinin-1 (NK1) receptor antagonist.
Aprepitant is also the active ingredient in EMEND® capsules, which were approved by the FDA in 2003. EMEND IV®, which was approved in 2008, contains aprepitant’s prodrug, fosaprepitant.
Heron Therapeutics, Inc., developed CINVANTI in an attempt to provide an IV formulation of aprepitant that has the same efficacy as IV fosaprepitant but does not pose the risk of adverse events (AEs) related to polysorbate 80.
“Aprepitant has long been the standard in the NK1 class, and it remains the only single-agent NK1 with proven efficacy in preventing CINV in both the acute and delayed phases in HEC and MEC,” said Rudolph M. Navari, MD, PhD, of the University of Alabama Birmingham School of Medicine.
“Because CINVANTI is a novel, polysorbate 80-free, IV formulation of aprepitant, it enables physicians to provide patients with standard-of-care efficacy without the potential risk of polysorbate 80-related adverse events, such as infusion-site reactions.”
The FDA approved CINVANTI based on data demonstrating the bioequivalence of CINVANTI to EMEND IV.
A phase 1, randomized, 2-way cross-over study comparing the drugs enrolled 100 healthy subjects. The subjects received CINVANTI at 130 mg or EMEND IV at 150 mg, given over 30 minutes on day 1 of periods 1 and 2.
The researchers said 90% confidence intervals for CINVANTI AUC0-t (area under the time-concentration curve from time 0 to the last measurable concentration), AUC0-inf (area under the time-concentration curve from time 0 extrapolated to infinity), and C12h (plasma concentration at 12 hours) “were well within bioequivalence bounds,” which was 80% to 125%.
The team also found the incidence of treatment-emergent AEs was lower with CINVANTI than EMEND IV—21% and 28%, respectively. The same was true for related treatment-emergent AEs—15% and 28%, respectively.
These data were presented at the Hematology/Oncology Pharmacy Association Annual Conference in March/April and the Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) Annual Meeting in June.
FDA grants drug orphan designation for treatment of malaria
The US Food and Drug Administration (FDA) has granted orphan drug designation to artemisone, a product candidate for the treatment of malaria.
Artemisone is a synthetic derivative of the antimalarial drug artemisinin, which “has been optimized for potency, stability, and safety,” according to Artemis Therapeutics, Inc., the company developing artemisone.
The company said phase 2 trial data suggest artemisone is effective against Plasmodium falciparum malaria.
Ninety-five patients were enrolled in the trial, and they received a 2-day or 3-day course of artemisone. Patients also received a second antimalarial drug on the final day of artemisone treatment (in compliance with recommendations from the World Health Organization).
At 28 days, the cure rates were 100% in both the 2-day and 3-day course groups. However, parasite clearance time was 25% faster with the 2-day course.
Artemis Therapeutics, Inc. has not yet released safety data from this trial.
Phase 1 data suggested artemisone was well tolerated by healthy subjects. There were no serious adverse events in the trial and no clinically relevant changes in laboratory and vital parameters, according to researchers.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to artemisone, a product candidate for the treatment of malaria.
Artemisone is a synthetic derivative of the antimalarial drug artemisinin, which “has been optimized for potency, stability, and safety,” according to Artemis Therapeutics, Inc., the company developing artemisone.
The company said phase 2 trial data suggest artemisone is effective against Plasmodium falciparum malaria.
Ninety-five patients were enrolled in the trial, and they received a 2-day or 3-day course of artemisone. Patients also received a second antimalarial drug on the final day of artemisone treatment (in compliance with recommendations from the World Health Organization).
At 28 days, the cure rates were 100% in both the 2-day and 3-day course groups. However, parasite clearance time was 25% faster with the 2-day course.
Artemis Therapeutics, Inc. has not yet released safety data from this trial.
Phase 1 data suggested artemisone was well tolerated by healthy subjects. There were no serious adverse events in the trial and no clinically relevant changes in laboratory and vital parameters, according to researchers.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to artemisone, a product candidate for the treatment of malaria.
Artemisone is a synthetic derivative of the antimalarial drug artemisinin, which “has been optimized for potency, stability, and safety,” according to Artemis Therapeutics, Inc., the company developing artemisone.
The company said phase 2 trial data suggest artemisone is effective against Plasmodium falciparum malaria.
Ninety-five patients were enrolled in the trial, and they received a 2-day or 3-day course of artemisone. Patients also received a second antimalarial drug on the final day of artemisone treatment (in compliance with recommendations from the World Health Organization).
At 28 days, the cure rates were 100% in both the 2-day and 3-day course groups. However, parasite clearance time was 25% faster with the 2-day course.
Artemis Therapeutics, Inc. has not yet released safety data from this trial.
Phase 1 data suggested artemisone was well tolerated by healthy subjects. There were no serious adverse events in the trial and no clinically relevant changes in laboratory and vital parameters, according to researchers.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
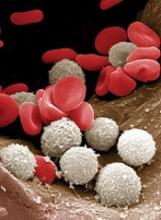
FDA approves wider use of hematology analyzer
The US Food and Drug Administration (FDA) has expanded the approved use of the XW-100 Automated Hematology Analyzer.
The analyzer can now be used at non-traditional laboratory sites by non-medical personnel.
The XW-100 Automated Hematology Analyzer is intended for use in patients age 2 and older who require a whole blood cell count and white blood cell differential.
Test results can be used with other clinical and laboratory findings to provide early alerts of patients with serious conditions, such as severe anemia and agranulocytosis, who require additional testing.
The XW-100 Automated Hematology Analyzer is not intended to diagnose or monitor patients with primary and/or secondary hematologic diseases.
The device works by using a blood sample to classify and quantify 12 hematology parameters, which provides patients with a blood component profile as part of their overall health assessment.
Expanded clearance
The FDA granted the XW-100 Automated Hematology Analyzer a waiver under the Clinical Laboratory Improvement Amendments of 1988 (CLIA). The waiver allows the device to be used by a variety of non-traditional laboratory sites, including physicians’ offices, clinics, or other types of healthcare facilities with a CLIA Certificate of Waiver.
The XW-100 Automated Hematology Analyzer was reviewed through the dual submission pathway, a streamlined regulatory pathway for 510(k) marketing clearance and CLIA Waiver by Application.
A 510(k) notification is a premarket submission made by device manufacturers to the FDA to demonstrate that the new device is substantially equivalent to a legally marketed predicate device.
The XW-100 Automated Hematology Analyzer was originally cleared through the 510(k) pathway in 2015 for use at the patient’s point-of-care.
To support the use of this device in CLIA-waived settings with non-medical personnel, the analyzer is now accompanied by simple instructions for operator actions when results are flagged or outside of a specified range.
To further ensure accurate testing in this setting and to eliminate results that are most susceptible to inaccuracy or require additional testing, the number of hematology parameters has been reduced to 12.
The FDA found this modified version of the XW-100 Automated Hematology Analyzer to be substantially equivalent to the 2015 model.
In addition, data submitted by Sysmex America, Inc. (the company marketing the analyzer) demonstrated ease of use and a low risk of false results when the modified XW-100 Automated Hematology Analyzer was used by untrained operators.
The FDA reviewed data from a study conducted on 582 samples collected from patients ages 2 to 92.
In this study, researchers compared XW-100 Automated Hematology Analyzer results collected by non-medical personnel in CLIA-waived settings to results from a hematology analyzer in an accredited clinical laboratory.
Results showed that, by following the manufacturer’s instructions for use, accurate testing can be effectively conducted by untrained personnel.
The US Food and Drug Administration (FDA) has expanded the approved use of the XW-100 Automated Hematology Analyzer.
The analyzer can now be used at non-traditional laboratory sites by non-medical personnel.
The XW-100 Automated Hematology Analyzer is intended for use in patients age 2 and older who require a whole blood cell count and white blood cell differential.
Test results can be used with other clinical and laboratory findings to provide early alerts of patients with serious conditions, such as severe anemia and agranulocytosis, who require additional testing.
The XW-100 Automated Hematology Analyzer is not intended to diagnose or monitor patients with primary and/or secondary hematologic diseases.
The device works by using a blood sample to classify and quantify 12 hematology parameters, which provides patients with a blood component profile as part of their overall health assessment.
Expanded clearance
The FDA granted the XW-100 Automated Hematology Analyzer a waiver under the Clinical Laboratory Improvement Amendments of 1988 (CLIA). The waiver allows the device to be used by a variety of non-traditional laboratory sites, including physicians’ offices, clinics, or other types of healthcare facilities with a CLIA Certificate of Waiver.
The XW-100 Automated Hematology Analyzer was reviewed through the dual submission pathway, a streamlined regulatory pathway for 510(k) marketing clearance and CLIA Waiver by Application.
A 510(k) notification is a premarket submission made by device manufacturers to the FDA to demonstrate that the new device is substantially equivalent to a legally marketed predicate device.
The XW-100 Automated Hematology Analyzer was originally cleared through the 510(k) pathway in 2015 for use at the patient’s point-of-care.
To support the use of this device in CLIA-waived settings with non-medical personnel, the analyzer is now accompanied by simple instructions for operator actions when results are flagged or outside of a specified range.
To further ensure accurate testing in this setting and to eliminate results that are most susceptible to inaccuracy or require additional testing, the number of hematology parameters has been reduced to 12.
The FDA found this modified version of the XW-100 Automated Hematology Analyzer to be substantially equivalent to the 2015 model.
In addition, data submitted by Sysmex America, Inc. (the company marketing the analyzer) demonstrated ease of use and a low risk of false results when the modified XW-100 Automated Hematology Analyzer was used by untrained operators.
The FDA reviewed data from a study conducted on 582 samples collected from patients ages 2 to 92.
In this study, researchers compared XW-100 Automated Hematology Analyzer results collected by non-medical personnel in CLIA-waived settings to results from a hematology analyzer in an accredited clinical laboratory.
Results showed that, by following the manufacturer’s instructions for use, accurate testing can be effectively conducted by untrained personnel.
The US Food and Drug Administration (FDA) has expanded the approved use of the XW-100 Automated Hematology Analyzer.
The analyzer can now be used at non-traditional laboratory sites by non-medical personnel.
The XW-100 Automated Hematology Analyzer is intended for use in patients age 2 and older who require a whole blood cell count and white blood cell differential.
Test results can be used with other clinical and laboratory findings to provide early alerts of patients with serious conditions, such as severe anemia and agranulocytosis, who require additional testing.
The XW-100 Automated Hematology Analyzer is not intended to diagnose or monitor patients with primary and/or secondary hematologic diseases.
The device works by using a blood sample to classify and quantify 12 hematology parameters, which provides patients with a blood component profile as part of their overall health assessment.
Expanded clearance
The FDA granted the XW-100 Automated Hematology Analyzer a waiver under the Clinical Laboratory Improvement Amendments of 1988 (CLIA). The waiver allows the device to be used by a variety of non-traditional laboratory sites, including physicians’ offices, clinics, or other types of healthcare facilities with a CLIA Certificate of Waiver.
The XW-100 Automated Hematology Analyzer was reviewed through the dual submission pathway, a streamlined regulatory pathway for 510(k) marketing clearance and CLIA Waiver by Application.
A 510(k) notification is a premarket submission made by device manufacturers to the FDA to demonstrate that the new device is substantially equivalent to a legally marketed predicate device.
The XW-100 Automated Hematology Analyzer was originally cleared through the 510(k) pathway in 2015 for use at the patient’s point-of-care.
To support the use of this device in CLIA-waived settings with non-medical personnel, the analyzer is now accompanied by simple instructions for operator actions when results are flagged or outside of a specified range.
To further ensure accurate testing in this setting and to eliminate results that are most susceptible to inaccuracy or require additional testing, the number of hematology parameters has been reduced to 12.
The FDA found this modified version of the XW-100 Automated Hematology Analyzer to be substantially equivalent to the 2015 model.
In addition, data submitted by Sysmex America, Inc. (the company marketing the analyzer) demonstrated ease of use and a low risk of false results when the modified XW-100 Automated Hematology Analyzer was used by untrained operators.
The FDA reviewed data from a study conducted on 582 samples collected from patients ages 2 to 92.
In this study, researchers compared XW-100 Automated Hematology Analyzer results collected by non-medical personnel in CLIA-waived settings to results from a hematology analyzer in an accredited clinical laboratory.
Results showed that, by following the manufacturer’s instructions for use, accurate testing can be effectively conducted by untrained personnel.
Intervention improves well-being in AYAs with cancer
SAN DIEGO—New research suggests an intervention can improve psychosocial health in adolescents and young adults (AYAs) living with cancer.
The intervention, Promoting Resilience in Stress Management (PRISM), is designed to help patients manage stress, set goals, and change their perspective.
Overall, PRISM improved resilience, enhanced quality of life, increased hope, and lowered distress and depression in the patients studied.
Abby R. Rosenberg, MD, of Seattle Children’s Research Institute in Seattle, Washington, presented these results at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 176*).
“The experience of cancer is stressful in all realms, but we tend to focus more on physical symptoms than the equally important social and emotional challenges,” Dr Rosenberg said.
“This is particularly true for adolescents and young adults who already struggle with normal developmental changes. When you throw cancer into the mix, it can become much harder.”
With this in mind, Dr Rosenberg and her colleagues tested PRISM in AYAs with cancer. The trial included 99 English-speaking patients, ages 12 to 25, who were diagnosed with new or newly recurrent cancer.
The patients were randomized to receive PRISM (n=49) plus standard psychosocial supportive care or standard care alone (n=50). Standard care at Seattle Children’s Research Institute includes a dedicated social worker and access to psychologists, child-life specialists, and other experts in AYA oncology care, as needed.
PRISM targets 4 topics:
- Managing stress with skills based on mindfulness and relaxation
- Setting goals that are specific and realistic, as well as planning for roadblocks
- Positive reframing, or recognizing and replacing negative self-talk
- Making meaning, or identifying benefits, gratitude, purpose, and legacy.
Each of the 4 topics were discussed with patients in separate, one-on-one sessions with a trained research associate. The sessions lasted 30 minutes to an hour. Patients also received boosters and worksheets for practicing the skills discussed in the meetings.
After all 4 sessions had been completed, patients could participate in an optional family meeting. During this meeting, patients could discuss with their family members which aspects of PRISM worked.
Results
Patients completed surveys at study enrollment, 2 months, 4 months, and 6 months. There were 74 participants who were still alive and well enough to complete the 6-month survey—36 in the PRISM group and 38 in the control group.
At the 6-month mark, PRISM was associated with (sometimes significant) improvements in resilience (P=0.02), generic quality of life (P=0.08), cancer-specific quality of life (P=0.01), hope (P=0.34), and distress (P=0.03). (P values are for absolute difference from baseline to 6 months.)
In addition, the incidence of depression at 6 months was lower in the PRISM group than the control group—6% and 21%, respectively (odds ratio=0.09, 95% CI 0.01, 1.09).
All but 4 of the PRISM recipients chose to participate in the family meeting following their one-on-one sessions.
“We included the family meeting because teens told us they wanted to share with their parents, and parents told us they wanted to know what their children had learned,” Dr Rosenberg said. “While the specific impact of this meeting is yet to be determined, we hope it will guide families so that there is continued support of teen or young adult patients.”
Now, Dr Rosenberg and her colleagues would like to test PRISM in other patient populations.
“We need to include a much larger cultural demographic in future studies,” Dr Rosenberg noted. “Beyond that, we also need to determine if this type of intervention could translate to other centers where usual care may not be as comprehensive as what we have here.”
*Some data in the abstract differ from the presentation.
SAN DIEGO—New research suggests an intervention can improve psychosocial health in adolescents and young adults (AYAs) living with cancer.
The intervention, Promoting Resilience in Stress Management (PRISM), is designed to help patients manage stress, set goals, and change their perspective.
Overall, PRISM improved resilience, enhanced quality of life, increased hope, and lowered distress and depression in the patients studied.
Abby R. Rosenberg, MD, of Seattle Children’s Research Institute in Seattle, Washington, presented these results at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 176*).
“The experience of cancer is stressful in all realms, but we tend to focus more on physical symptoms than the equally important social and emotional challenges,” Dr Rosenberg said.
“This is particularly true for adolescents and young adults who already struggle with normal developmental changes. When you throw cancer into the mix, it can become much harder.”
With this in mind, Dr Rosenberg and her colleagues tested PRISM in AYAs with cancer. The trial included 99 English-speaking patients, ages 12 to 25, who were diagnosed with new or newly recurrent cancer.
The patients were randomized to receive PRISM (n=49) plus standard psychosocial supportive care or standard care alone (n=50). Standard care at Seattle Children’s Research Institute includes a dedicated social worker and access to psychologists, child-life specialists, and other experts in AYA oncology care, as needed.
PRISM targets 4 topics:
- Managing stress with skills based on mindfulness and relaxation
- Setting goals that are specific and realistic, as well as planning for roadblocks
- Positive reframing, or recognizing and replacing negative self-talk
- Making meaning, or identifying benefits, gratitude, purpose, and legacy.
Each of the 4 topics were discussed with patients in separate, one-on-one sessions with a trained research associate. The sessions lasted 30 minutes to an hour. Patients also received boosters and worksheets for practicing the skills discussed in the meetings.
After all 4 sessions had been completed, patients could participate in an optional family meeting. During this meeting, patients could discuss with their family members which aspects of PRISM worked.
Results
Patients completed surveys at study enrollment, 2 months, 4 months, and 6 months. There were 74 participants who were still alive and well enough to complete the 6-month survey—36 in the PRISM group and 38 in the control group.
At the 6-month mark, PRISM was associated with (sometimes significant) improvements in resilience (P=0.02), generic quality of life (P=0.08), cancer-specific quality of life (P=0.01), hope (P=0.34), and distress (P=0.03). (P values are for absolute difference from baseline to 6 months.)
In addition, the incidence of depression at 6 months was lower in the PRISM group than the control group—6% and 21%, respectively (odds ratio=0.09, 95% CI 0.01, 1.09).
All but 4 of the PRISM recipients chose to participate in the family meeting following their one-on-one sessions.
“We included the family meeting because teens told us they wanted to share with their parents, and parents told us they wanted to know what their children had learned,” Dr Rosenberg said. “While the specific impact of this meeting is yet to be determined, we hope it will guide families so that there is continued support of teen or young adult patients.”
Now, Dr Rosenberg and her colleagues would like to test PRISM in other patient populations.
“We need to include a much larger cultural demographic in future studies,” Dr Rosenberg noted. “Beyond that, we also need to determine if this type of intervention could translate to other centers where usual care may not be as comprehensive as what we have here.”
*Some data in the abstract differ from the presentation.
SAN DIEGO—New research suggests an intervention can improve psychosocial health in adolescents and young adults (AYAs) living with cancer.
The intervention, Promoting Resilience in Stress Management (PRISM), is designed to help patients manage stress, set goals, and change their perspective.
Overall, PRISM improved resilience, enhanced quality of life, increased hope, and lowered distress and depression in the patients studied.
Abby R. Rosenberg, MD, of Seattle Children’s Research Institute in Seattle, Washington, presented these results at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 176*).
“The experience of cancer is stressful in all realms, but we tend to focus more on physical symptoms than the equally important social and emotional challenges,” Dr Rosenberg said.
“This is particularly true for adolescents and young adults who already struggle with normal developmental changes. When you throw cancer into the mix, it can become much harder.”
With this in mind, Dr Rosenberg and her colleagues tested PRISM in AYAs with cancer. The trial included 99 English-speaking patients, ages 12 to 25, who were diagnosed with new or newly recurrent cancer.
The patients were randomized to receive PRISM (n=49) plus standard psychosocial supportive care or standard care alone (n=50). Standard care at Seattle Children’s Research Institute includes a dedicated social worker and access to psychologists, child-life specialists, and other experts in AYA oncology care, as needed.
PRISM targets 4 topics:
- Managing stress with skills based on mindfulness and relaxation
- Setting goals that are specific and realistic, as well as planning for roadblocks
- Positive reframing, or recognizing and replacing negative self-talk
- Making meaning, or identifying benefits, gratitude, purpose, and legacy.
Each of the 4 topics were discussed with patients in separate, one-on-one sessions with a trained research associate. The sessions lasted 30 minutes to an hour. Patients also received boosters and worksheets for practicing the skills discussed in the meetings.
After all 4 sessions had been completed, patients could participate in an optional family meeting. During this meeting, patients could discuss with their family members which aspects of PRISM worked.
Results
Patients completed surveys at study enrollment, 2 months, 4 months, and 6 months. There were 74 participants who were still alive and well enough to complete the 6-month survey—36 in the PRISM group and 38 in the control group.
At the 6-month mark, PRISM was associated with (sometimes significant) improvements in resilience (P=0.02), generic quality of life (P=0.08), cancer-specific quality of life (P=0.01), hope (P=0.34), and distress (P=0.03). (P values are for absolute difference from baseline to 6 months.)
In addition, the incidence of depression at 6 months was lower in the PRISM group than the control group—6% and 21%, respectively (odds ratio=0.09, 95% CI 0.01, 1.09).
All but 4 of the PRISM recipients chose to participate in the family meeting following their one-on-one sessions.
“We included the family meeting because teens told us they wanted to share with their parents, and parents told us they wanted to know what their children had learned,” Dr Rosenberg said. “While the specific impact of this meeting is yet to be determined, we hope it will guide families so that there is continued support of teen or young adult patients.”
Now, Dr Rosenberg and her colleagues would like to test PRISM in other patient populations.
“We need to include a much larger cultural demographic in future studies,” Dr Rosenberg noted. “Beyond that, we also need to determine if this type of intervention could translate to other centers where usual care may not be as comprehensive as what we have here.”
*Some data in the abstract differ from the presentation.