User login
Bright light therapy improves sleep in cancer survivors
Results of a pilot study suggest that systematic bright light exposure can improve sleep in fatigued cancer survivors.
Subjects who were exposed to bright light every morning for 4 weeks had a significantly greater improvement in sleep efficiency than those who were exposed to dim light over the same period.
In fact, subjects in the bright light group were able to achieve clinically normal levels of sleep efficiency, and subjects in the dim light group were not.
Sleep efficiency is the percentage of time in bed that subjects spent sleeping.
Lisa M. Wu, PhD, of Northwestern University in Chicago, Illinois, and her colleagues reported these results in the Journal of Clinical Sleep Medicine.
The team noted that cancer patients report sleep disturbances at a significantly higher rate than the general population. Between 23% and 44% of cancer patients experience insomnia symptoms even years after treatment.
With this in mind, the researchers studied 44 individuals who had completed cancer treatment and met criteria for clinically significant fatigue at screening.
The subjects had an average age of 53.6, and 75% percent were female. Roughly 55% (n=24) had been diagnosed with a hematologic malignancy.
The subjects were randomized to a bright white light intervention or a dim red light intervention. Subjects in both treatment arms were provided with a light box and instructed to use it every morning for 30 minutes for 4 weeks. Sleep was evaluated using wrist actigraphy and the Pittsburgh Sleep Quality Index.
At baseline, 52.6% of subjects in the dim light group and 60% in the bright light group exceeded the clinical cutoff for poor sleep efficiency (≤ 85%). The mean sleep efficiency was 81.8% and 82.8%, respectively.
During the study period, sleep efficiency improved significantly more among subjects exposed to the bright light than those exposed to the dim light (P=0.003).
The mean sleep efficiency was in the clinically normal range for subjects in the bright light group at the end of the intervention (86.06%) and 3 weeks after (85.77%).
However, the cutoff for poor sleep efficiency was not reached in the dim light group, either at the end of the intervention (mean=79.35%) or 3 weeks after (mean=80.88%).
Total sleep time tended to increase over the study period for subjects in the bright light group, but there was no significant difference in total sleep time between the bright light and dim light groups.
Likewise, there was no significant between-group difference in waking after sleep onset, although this outcome tended to decrease over the study period for subjects in the bright light group.
“Systematic light exposure using bright white light is a low-cost and easily disseminated intervention that offers a feasible and potentially effective alternative to improve sleep in cancer survivors,” Dr Wu said.
However, she and her colleagues noted that larger-scale studies are needed. ![]()
Results of a pilot study suggest that systematic bright light exposure can improve sleep in fatigued cancer survivors.
Subjects who were exposed to bright light every morning for 4 weeks had a significantly greater improvement in sleep efficiency than those who were exposed to dim light over the same period.
In fact, subjects in the bright light group were able to achieve clinically normal levels of sleep efficiency, and subjects in the dim light group were not.
Sleep efficiency is the percentage of time in bed that subjects spent sleeping.
Lisa M. Wu, PhD, of Northwestern University in Chicago, Illinois, and her colleagues reported these results in the Journal of Clinical Sleep Medicine.
The team noted that cancer patients report sleep disturbances at a significantly higher rate than the general population. Between 23% and 44% of cancer patients experience insomnia symptoms even years after treatment.
With this in mind, the researchers studied 44 individuals who had completed cancer treatment and met criteria for clinically significant fatigue at screening.
The subjects had an average age of 53.6, and 75% percent were female. Roughly 55% (n=24) had been diagnosed with a hematologic malignancy.
The subjects were randomized to a bright white light intervention or a dim red light intervention. Subjects in both treatment arms were provided with a light box and instructed to use it every morning for 30 minutes for 4 weeks. Sleep was evaluated using wrist actigraphy and the Pittsburgh Sleep Quality Index.
At baseline, 52.6% of subjects in the dim light group and 60% in the bright light group exceeded the clinical cutoff for poor sleep efficiency (≤ 85%). The mean sleep efficiency was 81.8% and 82.8%, respectively.
During the study period, sleep efficiency improved significantly more among subjects exposed to the bright light than those exposed to the dim light (P=0.003).
The mean sleep efficiency was in the clinically normal range for subjects in the bright light group at the end of the intervention (86.06%) and 3 weeks after (85.77%).
However, the cutoff for poor sleep efficiency was not reached in the dim light group, either at the end of the intervention (mean=79.35%) or 3 weeks after (mean=80.88%).
Total sleep time tended to increase over the study period for subjects in the bright light group, but there was no significant difference in total sleep time between the bright light and dim light groups.
Likewise, there was no significant between-group difference in waking after sleep onset, although this outcome tended to decrease over the study period for subjects in the bright light group.
“Systematic light exposure using bright white light is a low-cost and easily disseminated intervention that offers a feasible and potentially effective alternative to improve sleep in cancer survivors,” Dr Wu said.
However, she and her colleagues noted that larger-scale studies are needed. ![]()
Results of a pilot study suggest that systematic bright light exposure can improve sleep in fatigued cancer survivors.
Subjects who were exposed to bright light every morning for 4 weeks had a significantly greater improvement in sleep efficiency than those who were exposed to dim light over the same period.
In fact, subjects in the bright light group were able to achieve clinically normal levels of sleep efficiency, and subjects in the dim light group were not.
Sleep efficiency is the percentage of time in bed that subjects spent sleeping.
Lisa M. Wu, PhD, of Northwestern University in Chicago, Illinois, and her colleagues reported these results in the Journal of Clinical Sleep Medicine.
The team noted that cancer patients report sleep disturbances at a significantly higher rate than the general population. Between 23% and 44% of cancer patients experience insomnia symptoms even years after treatment.
With this in mind, the researchers studied 44 individuals who had completed cancer treatment and met criteria for clinically significant fatigue at screening.
The subjects had an average age of 53.6, and 75% percent were female. Roughly 55% (n=24) had been diagnosed with a hematologic malignancy.
The subjects were randomized to a bright white light intervention or a dim red light intervention. Subjects in both treatment arms were provided with a light box and instructed to use it every morning for 30 minutes for 4 weeks. Sleep was evaluated using wrist actigraphy and the Pittsburgh Sleep Quality Index.
At baseline, 52.6% of subjects in the dim light group and 60% in the bright light group exceeded the clinical cutoff for poor sleep efficiency (≤ 85%). The mean sleep efficiency was 81.8% and 82.8%, respectively.
During the study period, sleep efficiency improved significantly more among subjects exposed to the bright light than those exposed to the dim light (P=0.003).
The mean sleep efficiency was in the clinically normal range for subjects in the bright light group at the end of the intervention (86.06%) and 3 weeks after (85.77%).
However, the cutoff for poor sleep efficiency was not reached in the dim light group, either at the end of the intervention (mean=79.35%) or 3 weeks after (mean=80.88%).
Total sleep time tended to increase over the study period for subjects in the bright light group, but there was no significant difference in total sleep time between the bright light and dim light groups.
Likewise, there was no significant between-group difference in waking after sleep onset, although this outcome tended to decrease over the study period for subjects in the bright light group.
“Systematic light exposure using bright white light is a low-cost and easily disseminated intervention that offers a feasible and potentially effective alternative to improve sleep in cancer survivors,” Dr Wu said.
However, she and her colleagues noted that larger-scale studies are needed. ![]()
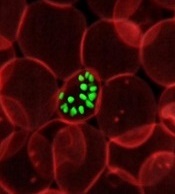
Compound may treat drug-resistant malaria
The antimicrobial agent triclosan may be able to fight drug-resistant malaria, according to research published in Scientific Reports.
For this work, researchers used an artificially intelligent “robot scientist” named Eve to perform a high-throughput screen of potential antimalarial compounds.
The screen revealed that triclosan is effective against Plasmodium parasites that have grown resistant to the antimalarial drug pyrimethamine.
Researchers have known for some time that triclosan inhibits in vitro growth of Plasmodium parasites. They assumed this was because triclosan inhibits the enzyme enoyl reductase (ENR).
However, subsequent work showed that improving triclosan’s ability to target ENR had no effect on parasite growth in the blood.
With the current study, researchers discovered that triclosan also affects parasite growth by inhibiting an enzyme called dihydrofolate reductase (DHFR), which is the target of the antimalarial drug pyrimethamine.
The researchers conducted growth competition experiments with 3 yeast strains dependent on a DHFR enzyme from Plasmodium falciparum, a DHFR enzyme from Plasmodium vivax, and human DHFR.
The team used Eve to screen compounds and identify drugs that inhibit the parasite targets but not the human counterpart.
The researchers found that triclosan was able to target and act on DHFR in both wild-type and pyrimethamine-resistant P falciparum and P vivax parasites.
Because triclosan inhibits both ENR and DHFR, the researchers think it may be possible to target Plasmodium parasites at both the liver and blood stages.
“The discovery by our robot ‘colleague’ Eve that triclosan is effective against malaria targets offers hope that we may be able to use it to develop a new drug,” said study author Elizabeth Bilsland, PhD, of the University of Campinas in Brazil.
“We know it is a safe compound, and its ability to target 2 points in the malaria parasite’s life-cycle means the parasite will find it difficult to evolve resistance.”
Eve was developed to speed up the drug discovery process by automatically developing and testing hypotheses to explain observations, run experiments using laboratory robotics, interpret the results to amend hypotheses, and then repeat the cycle.
“Artificial intelligence and machine-learning enables us to create automated scientists that do not just take a ‘brute force’ approach but, rather, take an intelligent approach to science,” said Ross King, PhD, a professor at the University of Manchester in the UK who led the development of Eve.
“This could greatly speed up the drug discovery process and potentially reap huge rewards.” ![]()
The antimicrobial agent triclosan may be able to fight drug-resistant malaria, according to research published in Scientific Reports.
For this work, researchers used an artificially intelligent “robot scientist” named Eve to perform a high-throughput screen of potential antimalarial compounds.
The screen revealed that triclosan is effective against Plasmodium parasites that have grown resistant to the antimalarial drug pyrimethamine.
Researchers have known for some time that triclosan inhibits in vitro growth of Plasmodium parasites. They assumed this was because triclosan inhibits the enzyme enoyl reductase (ENR).
However, subsequent work showed that improving triclosan’s ability to target ENR had no effect on parasite growth in the blood.
With the current study, researchers discovered that triclosan also affects parasite growth by inhibiting an enzyme called dihydrofolate reductase (DHFR), which is the target of the antimalarial drug pyrimethamine.
The researchers conducted growth competition experiments with 3 yeast strains dependent on a DHFR enzyme from Plasmodium falciparum, a DHFR enzyme from Plasmodium vivax, and human DHFR.
The team used Eve to screen compounds and identify drugs that inhibit the parasite targets but not the human counterpart.
The researchers found that triclosan was able to target and act on DHFR in both wild-type and pyrimethamine-resistant P falciparum and P vivax parasites.
Because triclosan inhibits both ENR and DHFR, the researchers think it may be possible to target Plasmodium parasites at both the liver and blood stages.
“The discovery by our robot ‘colleague’ Eve that triclosan is effective against malaria targets offers hope that we may be able to use it to develop a new drug,” said study author Elizabeth Bilsland, PhD, of the University of Campinas in Brazil.
“We know it is a safe compound, and its ability to target 2 points in the malaria parasite’s life-cycle means the parasite will find it difficult to evolve resistance.”
Eve was developed to speed up the drug discovery process by automatically developing and testing hypotheses to explain observations, run experiments using laboratory robotics, interpret the results to amend hypotheses, and then repeat the cycle.
“Artificial intelligence and machine-learning enables us to create automated scientists that do not just take a ‘brute force’ approach but, rather, take an intelligent approach to science,” said Ross King, PhD, a professor at the University of Manchester in the UK who led the development of Eve.
“This could greatly speed up the drug discovery process and potentially reap huge rewards.” ![]()
The antimicrobial agent triclosan may be able to fight drug-resistant malaria, according to research published in Scientific Reports.
For this work, researchers used an artificially intelligent “robot scientist” named Eve to perform a high-throughput screen of potential antimalarial compounds.
The screen revealed that triclosan is effective against Plasmodium parasites that have grown resistant to the antimalarial drug pyrimethamine.
Researchers have known for some time that triclosan inhibits in vitro growth of Plasmodium parasites. They assumed this was because triclosan inhibits the enzyme enoyl reductase (ENR).
However, subsequent work showed that improving triclosan’s ability to target ENR had no effect on parasite growth in the blood.
With the current study, researchers discovered that triclosan also affects parasite growth by inhibiting an enzyme called dihydrofolate reductase (DHFR), which is the target of the antimalarial drug pyrimethamine.
The researchers conducted growth competition experiments with 3 yeast strains dependent on a DHFR enzyme from Plasmodium falciparum, a DHFR enzyme from Plasmodium vivax, and human DHFR.
The team used Eve to screen compounds and identify drugs that inhibit the parasite targets but not the human counterpart.
The researchers found that triclosan was able to target and act on DHFR in both wild-type and pyrimethamine-resistant P falciparum and P vivax parasites.
Because triclosan inhibits both ENR and DHFR, the researchers think it may be possible to target Plasmodium parasites at both the liver and blood stages.
“The discovery by our robot ‘colleague’ Eve that triclosan is effective against malaria targets offers hope that we may be able to use it to develop a new drug,” said study author Elizabeth Bilsland, PhD, of the University of Campinas in Brazil.
“We know it is a safe compound, and its ability to target 2 points in the malaria parasite’s life-cycle means the parasite will find it difficult to evolve resistance.”
Eve was developed to speed up the drug discovery process by automatically developing and testing hypotheses to explain observations, run experiments using laboratory robotics, interpret the results to amend hypotheses, and then repeat the cycle.
“Artificial intelligence and machine-learning enables us to create automated scientists that do not just take a ‘brute force’ approach but, rather, take an intelligent approach to science,” said Ross King, PhD, a professor at the University of Manchester in the UK who led the development of Eve.
“This could greatly speed up the drug discovery process and potentially reap huge rewards.” ![]()
FDA aims to improve access to clinical trial info
The US Food and Drug Administration (FDA) says it is taking new steps to improve public access to clinical trial information.
The agency is launching a pilot program to evaluate whether releasing portions of clinical study reports (CSRs) will improve public access to drug approval information.
The FDA is also planning to add NCT numbers to FDA materials to make it easier to match listings on ClinicalTrials.gov to FDA communications.
FDA Commissioner Scott Gottlieb, MD, noted that, when a drug is approved, the FDA releases certain information the agency used when reviewing the new drug application (NDA).
This includes summaries written by medical reviewers that capture their assessment of the data, the proposed labeling or other requirements, and other data supporting safe and effective use. This information is included in the drug approvals database, Drugs@FDA.
Dr Gottlieb said these summaries are packaged in a format that can sometimes make it difficult for external audiences to extract all of the detailed clinical evidence that supported the FDA’s approval decisions.
Therefore, the agency is launching a pilot program to evaluate whether disclosing certain information included in CSRs will provide stakeholders with more details on the clinical evidence supporting a drug application and more transparency into the FDA’s decision-making process.
The FDA plans to select up to 9 recently approved NDAs whose sponsors will provide portions of CSRs from trials that were submitted to the FDA.
The CSRs will be posted on a new web page on the FDA’s website that describes the pilot program, in addition to appearing on Drugs@FDA along with the drug’s approval information.
The pilot will begin this month. The FDA will soon begin contacting sponsors to see if they are interested in participating in the pilot.
The agency will provide participating sponsors with additional information to ensure their understanding of the process. The FDA also promises to protect patient privacy, trade secret, and confidential commercial information in the CSRs it releases.
Once the pilot program is complete, the FDA will seek public feedback through a Federal Register notice and docket for public comments.
To augment the CSR pilot, the FDA is adding NCT numbers to materials for future drug approvals.
The agency believes this will make it easier to associate listings on ClinicalTrials.gov with FDA communications about specific drugs, including product labeling and advisory committee meeting materials. ![]()
The US Food and Drug Administration (FDA) says it is taking new steps to improve public access to clinical trial information.
The agency is launching a pilot program to evaluate whether releasing portions of clinical study reports (CSRs) will improve public access to drug approval information.
The FDA is also planning to add NCT numbers to FDA materials to make it easier to match listings on ClinicalTrials.gov to FDA communications.
FDA Commissioner Scott Gottlieb, MD, noted that, when a drug is approved, the FDA releases certain information the agency used when reviewing the new drug application (NDA).
This includes summaries written by medical reviewers that capture their assessment of the data, the proposed labeling or other requirements, and other data supporting safe and effective use. This information is included in the drug approvals database, Drugs@FDA.
Dr Gottlieb said these summaries are packaged in a format that can sometimes make it difficult for external audiences to extract all of the detailed clinical evidence that supported the FDA’s approval decisions.
Therefore, the agency is launching a pilot program to evaluate whether disclosing certain information included in CSRs will provide stakeholders with more details on the clinical evidence supporting a drug application and more transparency into the FDA’s decision-making process.
The FDA plans to select up to 9 recently approved NDAs whose sponsors will provide portions of CSRs from trials that were submitted to the FDA.
The CSRs will be posted on a new web page on the FDA’s website that describes the pilot program, in addition to appearing on Drugs@FDA along with the drug’s approval information.
The pilot will begin this month. The FDA will soon begin contacting sponsors to see if they are interested in participating in the pilot.
The agency will provide participating sponsors with additional information to ensure their understanding of the process. The FDA also promises to protect patient privacy, trade secret, and confidential commercial information in the CSRs it releases.
Once the pilot program is complete, the FDA will seek public feedback through a Federal Register notice and docket for public comments.
To augment the CSR pilot, the FDA is adding NCT numbers to materials for future drug approvals.
The agency believes this will make it easier to associate listings on ClinicalTrials.gov with FDA communications about specific drugs, including product labeling and advisory committee meeting materials. ![]()
The US Food and Drug Administration (FDA) says it is taking new steps to improve public access to clinical trial information.
The agency is launching a pilot program to evaluate whether releasing portions of clinical study reports (CSRs) will improve public access to drug approval information.
The FDA is also planning to add NCT numbers to FDA materials to make it easier to match listings on ClinicalTrials.gov to FDA communications.
FDA Commissioner Scott Gottlieb, MD, noted that, when a drug is approved, the FDA releases certain information the agency used when reviewing the new drug application (NDA).
This includes summaries written by medical reviewers that capture their assessment of the data, the proposed labeling or other requirements, and other data supporting safe and effective use. This information is included in the drug approvals database, Drugs@FDA.
Dr Gottlieb said these summaries are packaged in a format that can sometimes make it difficult for external audiences to extract all of the detailed clinical evidence that supported the FDA’s approval decisions.
Therefore, the agency is launching a pilot program to evaluate whether disclosing certain information included in CSRs will provide stakeholders with more details on the clinical evidence supporting a drug application and more transparency into the FDA’s decision-making process.
The FDA plans to select up to 9 recently approved NDAs whose sponsors will provide portions of CSRs from trials that were submitted to the FDA.
The CSRs will be posted on a new web page on the FDA’s website that describes the pilot program, in addition to appearing on Drugs@FDA along with the drug’s approval information.
The pilot will begin this month. The FDA will soon begin contacting sponsors to see if they are interested in participating in the pilot.
The agency will provide participating sponsors with additional information to ensure their understanding of the process. The FDA also promises to protect patient privacy, trade secret, and confidential commercial information in the CSRs it releases.
Once the pilot program is complete, the FDA will seek public feedback through a Federal Register notice and docket for public comments.
To augment the CSR pilot, the FDA is adding NCT numbers to materials for future drug approvals.
The agency believes this will make it easier to associate listings on ClinicalTrials.gov with FDA communications about specific drugs, including product labeling and advisory committee meeting materials. ![]()
Drug’s label updated to include risk of allergic reactions
The US Food and Drug Administration (FDA) and Tesaro, Inc., have updated the prescribing information for Varubi® (rolapitant) injectable emulsion to include a new warning about the risk of allergic reactions.
Varubi injectable emulsion is a substance P/neurokinin receptor antagonist approved to prevent delayed nausea and vomiting associated with chemotherapy in adults.
Since Varubi injectable emulsion gained FDA approval, there have been reports of anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions to the drug, some of which required hospitalization.
Now, the labeling for Varubi injectable emulsion has been changed to include information about these events. The changes include modifications to the CONTRAINDICATIONS, WARNINGS and PRECAUTIONS, and ADVERSE REACTIONS sections of the label.
Since Varubi injectable emulsion was introduced to the US market in late November 2017, at least 7000 doses of the drug have been administered to patients receiving emetogenic chemotherapy in the US, according to Tesaro.
Anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions have occurred during or soon after the infusion of Varubi. Most reactions have occurred within the first few minutes of administration.
The FDA has advised that patients who are hypersensitive to any component of Varubi injectable emulsion (including soybean oil) do not receive the drug. And patients with known allergies to legumes or other related allergens should be monitored closely.
The FDA said healthcare professionals should be vigilant for signs of hypersensitivity or anaphylaxis in all patients receiving Varubi injectable emulsion, both during administration and afterward.
Symptoms of anaphylaxis can include wheezing, difficulty breathing, swelling of the face or throat, hives, flushing, itching, abdominal cramping, abdominal pain, vomiting, back pain, chest pain, hypotension, and shock.
If anaphylaxis or any other serious hypersensitivity/infusion reaction occurs, Varubi injectable emulsion should be stopped immediately and permanently. The patient should receive appropriate medical management, including epinephrine and/or antihistamines.
To ensure patients and healthcare professionals are aware of the label update to Varubi injectable emulsion, Tesaro has issued a Dear Healthcare Professional letter. In addition, the updated prescribing information has been posted on the Varubi website.
For any questions about the use of Varubi injectable emulsion or to report adverse events related to the drug, contact Tesaro’s medical information department at 1-844-4-TESARO (1-844-483-7276).
Adverse events related to Varubi should also be reported to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
The US Food and Drug Administration (FDA) and Tesaro, Inc., have updated the prescribing information for Varubi® (rolapitant) injectable emulsion to include a new warning about the risk of allergic reactions.
Varubi injectable emulsion is a substance P/neurokinin receptor antagonist approved to prevent delayed nausea and vomiting associated with chemotherapy in adults.
Since Varubi injectable emulsion gained FDA approval, there have been reports of anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions to the drug, some of which required hospitalization.
Now, the labeling for Varubi injectable emulsion has been changed to include information about these events. The changes include modifications to the CONTRAINDICATIONS, WARNINGS and PRECAUTIONS, and ADVERSE REACTIONS sections of the label.
Since Varubi injectable emulsion was introduced to the US market in late November 2017, at least 7000 doses of the drug have been administered to patients receiving emetogenic chemotherapy in the US, according to Tesaro.
Anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions have occurred during or soon after the infusion of Varubi. Most reactions have occurred within the first few minutes of administration.
The FDA has advised that patients who are hypersensitive to any component of Varubi injectable emulsion (including soybean oil) do not receive the drug. And patients with known allergies to legumes or other related allergens should be monitored closely.
The FDA said healthcare professionals should be vigilant for signs of hypersensitivity or anaphylaxis in all patients receiving Varubi injectable emulsion, both during administration and afterward.
Symptoms of anaphylaxis can include wheezing, difficulty breathing, swelling of the face or throat, hives, flushing, itching, abdominal cramping, abdominal pain, vomiting, back pain, chest pain, hypotension, and shock.
If anaphylaxis or any other serious hypersensitivity/infusion reaction occurs, Varubi injectable emulsion should be stopped immediately and permanently. The patient should receive appropriate medical management, including epinephrine and/or antihistamines.
To ensure patients and healthcare professionals are aware of the label update to Varubi injectable emulsion, Tesaro has issued a Dear Healthcare Professional letter. In addition, the updated prescribing information has been posted on the Varubi website.
For any questions about the use of Varubi injectable emulsion or to report adverse events related to the drug, contact Tesaro’s medical information department at 1-844-4-TESARO (1-844-483-7276).
Adverse events related to Varubi should also be reported to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
The US Food and Drug Administration (FDA) and Tesaro, Inc., have updated the prescribing information for Varubi® (rolapitant) injectable emulsion to include a new warning about the risk of allergic reactions.
Varubi injectable emulsion is a substance P/neurokinin receptor antagonist approved to prevent delayed nausea and vomiting associated with chemotherapy in adults.
Since Varubi injectable emulsion gained FDA approval, there have been reports of anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions to the drug, some of which required hospitalization.
Now, the labeling for Varubi injectable emulsion has been changed to include information about these events. The changes include modifications to the CONTRAINDICATIONS, WARNINGS and PRECAUTIONS, and ADVERSE REACTIONS sections of the label.
Since Varubi injectable emulsion was introduced to the US market in late November 2017, at least 7000 doses of the drug have been administered to patients receiving emetogenic chemotherapy in the US, according to Tesaro.
Anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions have occurred during or soon after the infusion of Varubi. Most reactions have occurred within the first few minutes of administration.
The FDA has advised that patients who are hypersensitive to any component of Varubi injectable emulsion (including soybean oil) do not receive the drug. And patients with known allergies to legumes or other related allergens should be monitored closely.
The FDA said healthcare professionals should be vigilant for signs of hypersensitivity or anaphylaxis in all patients receiving Varubi injectable emulsion, both during administration and afterward.
Symptoms of anaphylaxis can include wheezing, difficulty breathing, swelling of the face or throat, hives, flushing, itching, abdominal cramping, abdominal pain, vomiting, back pain, chest pain, hypotension, and shock.
If anaphylaxis or any other serious hypersensitivity/infusion reaction occurs, Varubi injectable emulsion should be stopped immediately and permanently. The patient should receive appropriate medical management, including epinephrine and/or antihistamines.
To ensure patients and healthcare professionals are aware of the label update to Varubi injectable emulsion, Tesaro has issued a Dear Healthcare Professional letter. In addition, the updated prescribing information has been posted on the Varubi website.
For any questions about the use of Varubi injectable emulsion or to report adverse events related to the drug, contact Tesaro’s medical information department at 1-844-4-TESARO (1-844-483-7276).
Adverse events related to Varubi should also be reported to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
How a malaria parasite is evading treatment
New research has revealed mutations that help the malaria parasite Plasmodium falciparum evade treatment.
Researchers used whole-genome analyses and chemogenetics to identify drug targets and resistance genes in cell lines of P falciparum that are resistant to antimalarial compounds.
The group’s work confirmed previously known mutations that contribute to the parasite’s resistance but also revealed new targets that may deepen our understanding of the parasite’s underlying biology.
“This exploration of the P falciparum resistome—the collection of antibiotic resistance genes—and its druggable genome will help guide new drug discovery efforts and advance our understanding of how the malaria parasite evolves to fight back,” said Elizabeth Winzeler, PhD, of the University of California San Diego School of Medicine.
She and her colleagues conducted this research and reported the results in Science.
“A single human [malaria] infection can result in a person containing upwards of a trillion asexual blood-stage parasites,” Dr Winzeler said. “Even with a relatively slow random mutation rate, these numbers confer extraordinary adaptability.”
“In just a few cycles of replication, the P falciparum genome can acquire a random genetic change that may render at least one parasite resistant to the activity of a drug or human-encoded antibody.”
Such rapid evolution can be exploited in vitro to document how the parasite evolves in the presence of antimalarials, and it can be used to reveal new drug targets.
With this in mind, Dr Winzeler and her colleagues performed a genome analysis of 262 P falciparum parasites resistant to 37 groups of compounds.
In 83 genes associated with drug resistance, the researchers identified hundreds of changes that could be mediating the resistance, including 159 gene amplifications and 148 nonsynonymous mutations.
The team then used clones of well-studied P falciparum parasites and exposed them to the compounds over time to induce resistance, monitoring the genetic changes that occurred as resistance developed.
The researchers were able to identify a likely target or resistance gene for every compound.
In addition, the team identified mutations that repeatedly occurred upon individual exposure to a variety of drugs, meaning these mutations are likely mediating resistance to numerous existing treatments.
“Our findings showed and underscored the challenging complexity of evolved drug resistance in P falciparum, but they also identified new drug targets or resistance genes for every compound for which resistant parasites were generated,” Dr Winzeler said.
“It revealed the complicated chemogenetic landscape of P falciparum but also provided a potential guide for designing new small-molecule inhibitors to fight this pathogen.” ![]()
New research has revealed mutations that help the malaria parasite Plasmodium falciparum evade treatment.
Researchers used whole-genome analyses and chemogenetics to identify drug targets and resistance genes in cell lines of P falciparum that are resistant to antimalarial compounds.
The group’s work confirmed previously known mutations that contribute to the parasite’s resistance but also revealed new targets that may deepen our understanding of the parasite’s underlying biology.
“This exploration of the P falciparum resistome—the collection of antibiotic resistance genes—and its druggable genome will help guide new drug discovery efforts and advance our understanding of how the malaria parasite evolves to fight back,” said Elizabeth Winzeler, PhD, of the University of California San Diego School of Medicine.
She and her colleagues conducted this research and reported the results in Science.
“A single human [malaria] infection can result in a person containing upwards of a trillion asexual blood-stage parasites,” Dr Winzeler said. “Even with a relatively slow random mutation rate, these numbers confer extraordinary adaptability.”
“In just a few cycles of replication, the P falciparum genome can acquire a random genetic change that may render at least one parasite resistant to the activity of a drug or human-encoded antibody.”
Such rapid evolution can be exploited in vitro to document how the parasite evolves in the presence of antimalarials, and it can be used to reveal new drug targets.
With this in mind, Dr Winzeler and her colleagues performed a genome analysis of 262 P falciparum parasites resistant to 37 groups of compounds.
In 83 genes associated with drug resistance, the researchers identified hundreds of changes that could be mediating the resistance, including 159 gene amplifications and 148 nonsynonymous mutations.
The team then used clones of well-studied P falciparum parasites and exposed them to the compounds over time to induce resistance, monitoring the genetic changes that occurred as resistance developed.
The researchers were able to identify a likely target or resistance gene for every compound.
In addition, the team identified mutations that repeatedly occurred upon individual exposure to a variety of drugs, meaning these mutations are likely mediating resistance to numerous existing treatments.
“Our findings showed and underscored the challenging complexity of evolved drug resistance in P falciparum, but they also identified new drug targets or resistance genes for every compound for which resistant parasites were generated,” Dr Winzeler said.
“It revealed the complicated chemogenetic landscape of P falciparum but also provided a potential guide for designing new small-molecule inhibitors to fight this pathogen.” ![]()
New research has revealed mutations that help the malaria parasite Plasmodium falciparum evade treatment.
Researchers used whole-genome analyses and chemogenetics to identify drug targets and resistance genes in cell lines of P falciparum that are resistant to antimalarial compounds.
The group’s work confirmed previously known mutations that contribute to the parasite’s resistance but also revealed new targets that may deepen our understanding of the parasite’s underlying biology.
“This exploration of the P falciparum resistome—the collection of antibiotic resistance genes—and its druggable genome will help guide new drug discovery efforts and advance our understanding of how the malaria parasite evolves to fight back,” said Elizabeth Winzeler, PhD, of the University of California San Diego School of Medicine.
She and her colleagues conducted this research and reported the results in Science.
“A single human [malaria] infection can result in a person containing upwards of a trillion asexual blood-stage parasites,” Dr Winzeler said. “Even with a relatively slow random mutation rate, these numbers confer extraordinary adaptability.”
“In just a few cycles of replication, the P falciparum genome can acquire a random genetic change that may render at least one parasite resistant to the activity of a drug or human-encoded antibody.”
Such rapid evolution can be exploited in vitro to document how the parasite evolves in the presence of antimalarials, and it can be used to reveal new drug targets.
With this in mind, Dr Winzeler and her colleagues performed a genome analysis of 262 P falciparum parasites resistant to 37 groups of compounds.
In 83 genes associated with drug resistance, the researchers identified hundreds of changes that could be mediating the resistance, including 159 gene amplifications and 148 nonsynonymous mutations.
The team then used clones of well-studied P falciparum parasites and exposed them to the compounds over time to induce resistance, monitoring the genetic changes that occurred as resistance developed.
The researchers were able to identify a likely target or resistance gene for every compound.
In addition, the team identified mutations that repeatedly occurred upon individual exposure to a variety of drugs, meaning these mutations are likely mediating resistance to numerous existing treatments.
“Our findings showed and underscored the challenging complexity of evolved drug resistance in P falciparum, but they also identified new drug targets or resistance genes for every compound for which resistant parasites were generated,” Dr Winzeler said.
“It revealed the complicated chemogenetic landscape of P falciparum but also provided a potential guide for designing new small-molecule inhibitors to fight this pathogen.” ![]()
Method prolongs lifespan of blood samples
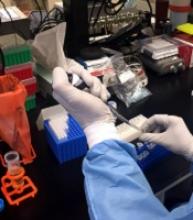
A new blood stabilization method significantly prolongs the lifespan of blood samples for microfluidic sorting and transcriptome profiling of rare circulating tumor cells (CTCs), according to researchers.
The method involves reducing the storage temperature to 4° C to reversibly slow down cellular processes while also counteracting the platelet activation that can occur because of the low temperature.
The researchers said this work overcomes a significant barrier to the translation of liquid biopsy technologies for precision oncology and other applications.
Keith Wong, PhD, of the Massachusetts General Hospital Center for Engineering in Medicine (MGH-CEM), and his colleagues described this work in Nature Communications.
When isolating CTCs from fresh, unprocessed blood, timing is everything. Even minor changes in the quality of a blood sample—such as the breakdown of red cells, leukocyte activation, or clot formation— can greatly affect cell-sorting mechanisms and the quality of the biomolecules isolated for cancer detection.
According to published studies, factors such as the total number of CTCs in a sample and the number with high-quality RNA decrease by around 50% within the first 4 to 5 hours after the sample is collected.
“At Mass. General, we have the luxury of being so integrated with the clinical team that we can process blood specimens in the lab typically within an hour or 2 after they are drawn,” Dr Wong said.
“But to make these liquid biopsy technologies routine lab tests for the rest of the world, we need ways to keep blood alive for much longer than several hours, since these assays are best performed in central laboratories for reasons of cost-effectiveness and reproducibility.”
With this in mind, Dr Wong and his colleagues set out to preserve blood in its native state with minimal alterations.
“We wanted to slow down the biological clock as much as possible by using hypothermia, but that is not as simple as it sounds,” said study author Shannon Tessier, PhD, also of MGH-CEM.
“Low temperature is a powerful means to decrease metabolism, but a host of unwanted side effects occur at the same time. In some ways, these challenges are similar to those we face in organ preservation, where we have to optimize strategies for a very complex mix of cells.”
To achieve these goals, the researchers first analyzed the effects of hypothermic storage conditions.
The team found that hypothermic storage (4° C) of blood anticoagulated with acid citrate dextrose maintained “cellular morphology, integrity, and surface epitope stability of diverse hematologic cell types” over 72 hours.
However, the researchers also observed platelet activation.
“We are preserving the blood very well, including the coagulation function of platelets,” Dr Wong said. “But, unfortunately, cooling causes profound activation of platelets. Now, we need a targeted approach for platelets so they don’t form nasty clots in the microfluidic blood-sorting device.”
Fortunately, the researchers found that glycoprotein IIb/IIIa inhibitors were able to counter cooling-induced platelet aggregation. And ion chelation treatment with ethylenediaminetetraacetic acid removed activated platelets from leukocytes.
The team said these steps—hypothermic storage, treatment with glycoprotein IIb/IIIa inhibitors, and ion chelation—allowed whole blood preserved for 3 days to be processed as if it were freshly drawn, with very high purity and virtually no loss in CTC numbers.
“The critical achievement here is that the isolated tumor cells contain high-quality RNA that is suitable for demanding molecular assays, such as single-cell qPCR, droplet digital PCR, and RNA sequencing,” Dr Tessier said.
To test their blood preservation method, Dr Tessier and her colleagues used blood specimens from a group of 10 patients with metastatic prostate cancer.
The researchers compared CTC analysis in preserved blood samples and paired fresh samples from the same patients.
There was 92% agreement in the detection of 12 cancer-specific gene transcripts between the fresh and preserved blood samples.
In addition, there was 100% agreement in the detection of a transcript called AR-V7. Recently published studies showed that the presence of AR-V7 mRNA in prostate cancer CTCs predicts resistance to androgen receptor inhibitors, indicating that chemotherapy may be a better option for such patients.
“The ability to preserve the blood for several days and still be able to pick up this clinically relevant biomarker is remarkable,” said study author David Miyamoto, MD, PhD, of MGH Cancer Center.
“This is very exciting for clinicians because AR-V7 mRNA can only be detected using CTCs and not with circulating tumor DNA or other cell-free assays.”
The researchers highlighted the universal nature of their blood preservation approach by pointing to its compatibility with the microfluidic CTC-iChip device, which isolates tumor cells by rapid removal of blood cells. The team said this suggests the potential impact of this work extends beyond cancer detection.
“With exciting breakthroughs in immunotherapy, stem cell transplantation, and regenerative medicine—in which peripheral blood is often the source of cells for functional assays or ex vivo expansion—the ability to preserve live cells will greatly ease logistical timelines and reduce the cost of complex cell-based assays,” Dr Wong said. ![]()
A new blood stabilization method significantly prolongs the lifespan of blood samples for microfluidic sorting and transcriptome profiling of rare circulating tumor cells (CTCs), according to researchers.
The method involves reducing the storage temperature to 4° C to reversibly slow down cellular processes while also counteracting the platelet activation that can occur because of the low temperature.
The researchers said this work overcomes a significant barrier to the translation of liquid biopsy technologies for precision oncology and other applications.
Keith Wong, PhD, of the Massachusetts General Hospital Center for Engineering in Medicine (MGH-CEM), and his colleagues described this work in Nature Communications.
When isolating CTCs from fresh, unprocessed blood, timing is everything. Even minor changes in the quality of a blood sample—such as the breakdown of red cells, leukocyte activation, or clot formation— can greatly affect cell-sorting mechanisms and the quality of the biomolecules isolated for cancer detection.
According to published studies, factors such as the total number of CTCs in a sample and the number with high-quality RNA decrease by around 50% within the first 4 to 5 hours after the sample is collected.
“At Mass. General, we have the luxury of being so integrated with the clinical team that we can process blood specimens in the lab typically within an hour or 2 after they are drawn,” Dr Wong said.
“But to make these liquid biopsy technologies routine lab tests for the rest of the world, we need ways to keep blood alive for much longer than several hours, since these assays are best performed in central laboratories for reasons of cost-effectiveness and reproducibility.”
With this in mind, Dr Wong and his colleagues set out to preserve blood in its native state with minimal alterations.
“We wanted to slow down the biological clock as much as possible by using hypothermia, but that is not as simple as it sounds,” said study author Shannon Tessier, PhD, also of MGH-CEM.
“Low temperature is a powerful means to decrease metabolism, but a host of unwanted side effects occur at the same time. In some ways, these challenges are similar to those we face in organ preservation, where we have to optimize strategies for a very complex mix of cells.”
To achieve these goals, the researchers first analyzed the effects of hypothermic storage conditions.
The team found that hypothermic storage (4° C) of blood anticoagulated with acid citrate dextrose maintained “cellular morphology, integrity, and surface epitope stability of diverse hematologic cell types” over 72 hours.
However, the researchers also observed platelet activation.
“We are preserving the blood very well, including the coagulation function of platelets,” Dr Wong said. “But, unfortunately, cooling causes profound activation of platelets. Now, we need a targeted approach for platelets so they don’t form nasty clots in the microfluidic blood-sorting device.”
Fortunately, the researchers found that glycoprotein IIb/IIIa inhibitors were able to counter cooling-induced platelet aggregation. And ion chelation treatment with ethylenediaminetetraacetic acid removed activated platelets from leukocytes.
The team said these steps—hypothermic storage, treatment with glycoprotein IIb/IIIa inhibitors, and ion chelation—allowed whole blood preserved for 3 days to be processed as if it were freshly drawn, with very high purity and virtually no loss in CTC numbers.
“The critical achievement here is that the isolated tumor cells contain high-quality RNA that is suitable for demanding molecular assays, such as single-cell qPCR, droplet digital PCR, and RNA sequencing,” Dr Tessier said.
To test their blood preservation method, Dr Tessier and her colleagues used blood specimens from a group of 10 patients with metastatic prostate cancer.
The researchers compared CTC analysis in preserved blood samples and paired fresh samples from the same patients.
There was 92% agreement in the detection of 12 cancer-specific gene transcripts between the fresh and preserved blood samples.
In addition, there was 100% agreement in the detection of a transcript called AR-V7. Recently published studies showed that the presence of AR-V7 mRNA in prostate cancer CTCs predicts resistance to androgen receptor inhibitors, indicating that chemotherapy may be a better option for such patients.
“The ability to preserve the blood for several days and still be able to pick up this clinically relevant biomarker is remarkable,” said study author David Miyamoto, MD, PhD, of MGH Cancer Center.
“This is very exciting for clinicians because AR-V7 mRNA can only be detected using CTCs and not with circulating tumor DNA or other cell-free assays.”
The researchers highlighted the universal nature of their blood preservation approach by pointing to its compatibility with the microfluidic CTC-iChip device, which isolates tumor cells by rapid removal of blood cells. The team said this suggests the potential impact of this work extends beyond cancer detection.
“With exciting breakthroughs in immunotherapy, stem cell transplantation, and regenerative medicine—in which peripheral blood is often the source of cells for functional assays or ex vivo expansion—the ability to preserve live cells will greatly ease logistical timelines and reduce the cost of complex cell-based assays,” Dr Wong said. ![]()
A new blood stabilization method significantly prolongs the lifespan of blood samples for microfluidic sorting and transcriptome profiling of rare circulating tumor cells (CTCs), according to researchers.
The method involves reducing the storage temperature to 4° C to reversibly slow down cellular processes while also counteracting the platelet activation that can occur because of the low temperature.
The researchers said this work overcomes a significant barrier to the translation of liquid biopsy technologies for precision oncology and other applications.
Keith Wong, PhD, of the Massachusetts General Hospital Center for Engineering in Medicine (MGH-CEM), and his colleagues described this work in Nature Communications.
When isolating CTCs from fresh, unprocessed blood, timing is everything. Even minor changes in the quality of a blood sample—such as the breakdown of red cells, leukocyte activation, or clot formation— can greatly affect cell-sorting mechanisms and the quality of the biomolecules isolated for cancer detection.
According to published studies, factors such as the total number of CTCs in a sample and the number with high-quality RNA decrease by around 50% within the first 4 to 5 hours after the sample is collected.
“At Mass. General, we have the luxury of being so integrated with the clinical team that we can process blood specimens in the lab typically within an hour or 2 after they are drawn,” Dr Wong said.
“But to make these liquid biopsy technologies routine lab tests for the rest of the world, we need ways to keep blood alive for much longer than several hours, since these assays are best performed in central laboratories for reasons of cost-effectiveness and reproducibility.”
With this in mind, Dr Wong and his colleagues set out to preserve blood in its native state with minimal alterations.
“We wanted to slow down the biological clock as much as possible by using hypothermia, but that is not as simple as it sounds,” said study author Shannon Tessier, PhD, also of MGH-CEM.
“Low temperature is a powerful means to decrease metabolism, but a host of unwanted side effects occur at the same time. In some ways, these challenges are similar to those we face in organ preservation, where we have to optimize strategies for a very complex mix of cells.”
To achieve these goals, the researchers first analyzed the effects of hypothermic storage conditions.
The team found that hypothermic storage (4° C) of blood anticoagulated with acid citrate dextrose maintained “cellular morphology, integrity, and surface epitope stability of diverse hematologic cell types” over 72 hours.
However, the researchers also observed platelet activation.
“We are preserving the blood very well, including the coagulation function of platelets,” Dr Wong said. “But, unfortunately, cooling causes profound activation of platelets. Now, we need a targeted approach for platelets so they don’t form nasty clots in the microfluidic blood-sorting device.”
Fortunately, the researchers found that glycoprotein IIb/IIIa inhibitors were able to counter cooling-induced platelet aggregation. And ion chelation treatment with ethylenediaminetetraacetic acid removed activated platelets from leukocytes.
The team said these steps—hypothermic storage, treatment with glycoprotein IIb/IIIa inhibitors, and ion chelation—allowed whole blood preserved for 3 days to be processed as if it were freshly drawn, with very high purity and virtually no loss in CTC numbers.
“The critical achievement here is that the isolated tumor cells contain high-quality RNA that is suitable for demanding molecular assays, such as single-cell qPCR, droplet digital PCR, and RNA sequencing,” Dr Tessier said.
To test their blood preservation method, Dr Tessier and her colleagues used blood specimens from a group of 10 patients with metastatic prostate cancer.
The researchers compared CTC analysis in preserved blood samples and paired fresh samples from the same patients.
There was 92% agreement in the detection of 12 cancer-specific gene transcripts between the fresh and preserved blood samples.
In addition, there was 100% agreement in the detection of a transcript called AR-V7. Recently published studies showed that the presence of AR-V7 mRNA in prostate cancer CTCs predicts resistance to androgen receptor inhibitors, indicating that chemotherapy may be a better option for such patients.
“The ability to preserve the blood for several days and still be able to pick up this clinically relevant biomarker is remarkable,” said study author David Miyamoto, MD, PhD, of MGH Cancer Center.
“This is very exciting for clinicians because AR-V7 mRNA can only be detected using CTCs and not with circulating tumor DNA or other cell-free assays.”
The researchers highlighted the universal nature of their blood preservation approach by pointing to its compatibility with the microfluidic CTC-iChip device, which isolates tumor cells by rapid removal of blood cells. The team said this suggests the potential impact of this work extends beyond cancer detection.
“With exciting breakthroughs in immunotherapy, stem cell transplantation, and regenerative medicine—in which peripheral blood is often the source of cells for functional assays or ex vivo expansion—the ability to preserve live cells will greatly ease logistical timelines and reduce the cost of complex cell-based assays,” Dr Wong said. ![]()
FDA aims to improve review of generic drugs
The US Food and Drug Administration (FDA) has announced that it is taking new steps to facilitate efficient review of generic drugs.
The agency has released 2 documents intended to help streamline and improve the submission and review of generic drug applications, or Abbreviated New Drug Applications (ANDAs).
The first document is a draft guidance for industry, “Good ANDA Submission Practices,” which highlights common, recurring deficiencies the FDA sees in generic drug applications that may lead to a delay in their approval.
The FDA’s goal in releasing this document is to reduce the number of review cycles for ANDAs by helping applicants avoid these deficiencies.
The second document is a Manual of Policies and Procedures (MAPP), “Good ANDA Assessment Practices,” which outlines ANDA assessment practices for FDA staff.
This document formalizes a more streamlined generic review process, including the introduction of new templates designed to make each cycle of the review process more efficient and complete.
Releasing these new documents is part of the FDA’s Drug Competition Action Plan, which has 3 main goals:
- To reduce actions by branded pharmaceutical companies that can delay generic drug entry into the marketplace
- To resolve scientific and regulatory obstacles that can make it difficult to win approval of generic versions of certain complex drugs
- To improve the efficiency and predictability of the FDA’s generic review process to reduce the time it takes to get a generic drug approved and lessen the number of review cycles needed for generic applications.
The new MAPP and draft guidance documents for ANDAs are intended to help the FDA meet the third goal of the Drug Competition Action Plan.
The FDA is hoping to address the second goal of the plan later this year, building upon its initiatives to accelerate review and approval of complex generics.
The agency is also planning to develop guidance documents during the first quarter of 2018 that will address 3 issues related to the first goal of the plan—potential abuses of the citizen petition process, companies that restrict access to testing samples of branded drugs, and abuses of the single, shared system REMS (risk evaluation and mitigation strategy) negotiation process. ![]()
The US Food and Drug Administration (FDA) has announced that it is taking new steps to facilitate efficient review of generic drugs.
The agency has released 2 documents intended to help streamline and improve the submission and review of generic drug applications, or Abbreviated New Drug Applications (ANDAs).
The first document is a draft guidance for industry, “Good ANDA Submission Practices,” which highlights common, recurring deficiencies the FDA sees in generic drug applications that may lead to a delay in their approval.
The FDA’s goal in releasing this document is to reduce the number of review cycles for ANDAs by helping applicants avoid these deficiencies.
The second document is a Manual of Policies and Procedures (MAPP), “Good ANDA Assessment Practices,” which outlines ANDA assessment practices for FDA staff.
This document formalizes a more streamlined generic review process, including the introduction of new templates designed to make each cycle of the review process more efficient and complete.
Releasing these new documents is part of the FDA’s Drug Competition Action Plan, which has 3 main goals:
- To reduce actions by branded pharmaceutical companies that can delay generic drug entry into the marketplace
- To resolve scientific and regulatory obstacles that can make it difficult to win approval of generic versions of certain complex drugs
- To improve the efficiency and predictability of the FDA’s generic review process to reduce the time it takes to get a generic drug approved and lessen the number of review cycles needed for generic applications.
The new MAPP and draft guidance documents for ANDAs are intended to help the FDA meet the third goal of the Drug Competition Action Plan.
The FDA is hoping to address the second goal of the plan later this year, building upon its initiatives to accelerate review and approval of complex generics.
The agency is also planning to develop guidance documents during the first quarter of 2018 that will address 3 issues related to the first goal of the plan—potential abuses of the citizen petition process, companies that restrict access to testing samples of branded drugs, and abuses of the single, shared system REMS (risk evaluation and mitigation strategy) negotiation process. ![]()
The US Food and Drug Administration (FDA) has announced that it is taking new steps to facilitate efficient review of generic drugs.
The agency has released 2 documents intended to help streamline and improve the submission and review of generic drug applications, or Abbreviated New Drug Applications (ANDAs).
The first document is a draft guidance for industry, “Good ANDA Submission Practices,” which highlights common, recurring deficiencies the FDA sees in generic drug applications that may lead to a delay in their approval.
The FDA’s goal in releasing this document is to reduce the number of review cycles for ANDAs by helping applicants avoid these deficiencies.
The second document is a Manual of Policies and Procedures (MAPP), “Good ANDA Assessment Practices,” which outlines ANDA assessment practices for FDA staff.
This document formalizes a more streamlined generic review process, including the introduction of new templates designed to make each cycle of the review process more efficient and complete.
Releasing these new documents is part of the FDA’s Drug Competition Action Plan, which has 3 main goals:
- To reduce actions by branded pharmaceutical companies that can delay generic drug entry into the marketplace
- To resolve scientific and regulatory obstacles that can make it difficult to win approval of generic versions of certain complex drugs
- To improve the efficiency and predictability of the FDA’s generic review process to reduce the time it takes to get a generic drug approved and lessen the number of review cycles needed for generic applications.
The new MAPP and draft guidance documents for ANDAs are intended to help the FDA meet the third goal of the Drug Competition Action Plan.
The FDA is hoping to address the second goal of the plan later this year, building upon its initiatives to accelerate review and approval of complex generics.
The agency is also planning to develop guidance documents during the first quarter of 2018 that will address 3 issues related to the first goal of the plan—potential abuses of the citizen petition process, companies that restrict access to testing samples of branded drugs, and abuses of the single, shared system REMS (risk evaluation and mitigation strategy) negotiation process.
Obesity has negative impact on HSC compartment
Obesity can affect the long-term health of hematopoietic stem cells (HSCs), according to research published in the Journal of Experimental Medicine.
Conducted largely in models of obese mice, the research showed that obesity causes durable and harmful changes to the HSC compartment.
“Keeping this compartment healthy is essential to human health,” said study author Damien Reynaud, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This includes maintaining the diverse pool of [HSCs] needed to produce blood cells the body needs to function properly.”
Although still poorly understood, research is showing that age and environmental stresses can lessen the healthy diversity of cells in the hematopoietic system.
This can include skewing blood cell formation toward myeloid cells and possibly promoting pre-leukemic fates, according to Dr Reynaud and his colleagues.
With the current study, the team found that obesity-related stresses alter the cellular architecture of the HSC compartment and reduce its long-term functional fitness.
Tests in obese mice showed these effects were progressive. And some of the harmful manifestations persisted even after the researchers normalized the animals’ weight through dietary controls.
These alterations of the hematopoietic system appear to be linked to overexpression of the transcription factor Gfi1.
The researchers found that oxidative stresses in the body caused by obesity drive overexpression of Gfi1. When this happens, it produces a lasting alteration of the HSC compartment.
The researchers said their study provides groundwork to investigate how lifestyle choices, such as diet, can durably impact blood formation and may contribute to the development of blood cancers.
The study also raises questions about the use of HSCs isolated from obese transplant donors.
“Little is known about how obesity in marrow donors could affect the quality of the hematopoietic stem cell compartment,” Dr Reynaud explained.
“We want to better understand the molecular alterations in obesity to predict potential risks associated with the therapeutic use of stem cells isolated from obese donors.”
Obesity can affect the long-term health of hematopoietic stem cells (HSCs), according to research published in the Journal of Experimental Medicine.
Conducted largely in models of obese mice, the research showed that obesity causes durable and harmful changes to the HSC compartment.
“Keeping this compartment healthy is essential to human health,” said study author Damien Reynaud, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This includes maintaining the diverse pool of [HSCs] needed to produce blood cells the body needs to function properly.”
Although still poorly understood, research is showing that age and environmental stresses can lessen the healthy diversity of cells in the hematopoietic system.
This can include skewing blood cell formation toward myeloid cells and possibly promoting pre-leukemic fates, according to Dr Reynaud and his colleagues.
With the current study, the team found that obesity-related stresses alter the cellular architecture of the HSC compartment and reduce its long-term functional fitness.
Tests in obese mice showed these effects were progressive. And some of the harmful manifestations persisted even after the researchers normalized the animals’ weight through dietary controls.
These alterations of the hematopoietic system appear to be linked to overexpression of the transcription factor Gfi1.
The researchers found that oxidative stresses in the body caused by obesity drive overexpression of Gfi1. When this happens, it produces a lasting alteration of the HSC compartment.
The researchers said their study provides groundwork to investigate how lifestyle choices, such as diet, can durably impact blood formation and may contribute to the development of blood cancers.
The study also raises questions about the use of HSCs isolated from obese transplant donors.
“Little is known about how obesity in marrow donors could affect the quality of the hematopoietic stem cell compartment,” Dr Reynaud explained.
“We want to better understand the molecular alterations in obesity to predict potential risks associated with the therapeutic use of stem cells isolated from obese donors.”
Obesity can affect the long-term health of hematopoietic stem cells (HSCs), according to research published in the Journal of Experimental Medicine.
Conducted largely in models of obese mice, the research showed that obesity causes durable and harmful changes to the HSC compartment.
“Keeping this compartment healthy is essential to human health,” said study author Damien Reynaud, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This includes maintaining the diverse pool of [HSCs] needed to produce blood cells the body needs to function properly.”
Although still poorly understood, research is showing that age and environmental stresses can lessen the healthy diversity of cells in the hematopoietic system.
This can include skewing blood cell formation toward myeloid cells and possibly promoting pre-leukemic fates, according to Dr Reynaud and his colleagues.
With the current study, the team found that obesity-related stresses alter the cellular architecture of the HSC compartment and reduce its long-term functional fitness.
Tests in obese mice showed these effects were progressive. And some of the harmful manifestations persisted even after the researchers normalized the animals’ weight through dietary controls.
These alterations of the hematopoietic system appear to be linked to overexpression of the transcription factor Gfi1.
The researchers found that oxidative stresses in the body caused by obesity drive overexpression of Gfi1. When this happens, it produces a lasting alteration of the HSC compartment.
The researchers said their study provides groundwork to investigate how lifestyle choices, such as diet, can durably impact blood formation and may contribute to the development of blood cancers.
The study also raises questions about the use of HSCs isolated from obese transplant donors.
“Little is known about how obesity in marrow donors could affect the quality of the hematopoietic stem cell compartment,” Dr Reynaud explained.
“We want to better understand the molecular alterations in obesity to predict potential risks associated with the therapeutic use of stem cells isolated from obese donors.”
FDA issues requirements, recommendations for GBCA use
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program.
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program.
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program.
Gene-based Zika vaccine proves immunogenic in healthy adults
An experimental Zika vaccine is safe and induces an immune response in healthy adults, according to research published in The Lancet.
Investigators tested 2 potential Zika vaccines, VRC5288 and VRC5283, in a pair of phase 1 trials.
Both vaccines were considered well-tolerated, but one of them, VRC5283, induced a greater immune response than the other.
Both vaccines were developed by investigators at the National Institute of Allergy and Infectious Diseases (NIAID).
Now, NIAID is leading an international effort to evaluate VRC5283 in a phase 2/2b trial.
“Following early reports that Zika infection during pregnancy can lead to birth defects, NIAID scientists rapidly created one of the first investigational Zika vaccines using a DNA-based platform and began initial studies in healthy adults less than 1 year later,” said NIAID Director Anthony S. Fauci, MD.
To create their vaccines, the investigators inserted into plasmids genes that encode proteins found on the surface of the Zika virus.
The team developed 2 different plasmids for clinical testing: VRC5288 (Zika virus and Japanese encephalitis virus chimera) and VRC5283 (wild-type Zika virus).
In August 2016, NIAID initiated a phase 1 trial of the VRC5288 plasmid in 80 healthy volunteers ages 18 to 35. Subjects received a 4 mg dose via a needle and syringe injection in the arm muscle.
They received doses of VRC5288 at 0 and 8 weeks; 0 and 12 weeks; 0, 4, and 8 weeks; or 0, 4, and 20 weeks.
In December 2016, NIAID initiated a separate trial testing the VRC5283 plasmid. This study enrolled 45 healthy volunteers ages 18 to 50.
Subjects in this trial received 4 mg doses of VRC5283 at 0, 4, and 8 weeks. They were vaccinated in 3 different ways—via single-dose needle and syringe injection in 1 arm, via split-dose needle and syringe injection in each arm, or via needle-free injection in each arm.
Safety
The vaccinations were considered safe and well-tolerated in both trials, although some participants experienced mild to moderate reactions.
Local reactions (with VRC5288 and VRC5283, respectively) included pain/tenderness (mild—46% and 73%, moderate—0% and 7%), mild swelling (1% and 7%), and mild redness (6% and 2%).
Systemic reactions (with VRC5288 and VRC5283, respectively) included malaise (mild—25% and 33%, moderate—3% and 4%), myalgia (mild—18% and 13%, moderate—4% and 7%), headache (mild—19% and 29%, moderate—4% and 4%), chills (mild—6% and 2%, moderate—1% and 2%), nausea (mild—8% and 4%, moderate—1% and 0%), and joint pain (mild—5% and 16%, moderate—0% and 2%).
Immunogenicity
The investigators analyzed blood samples from all subjects 4 weeks after their final vaccinations.
The team found that 60% to 89% of subjects generated a neutralizing antibody response to VRC5288, and 77% to 100% of subjects generated a neutralizing antibody response to VRC5283.
Subjects who received VRC5283 via the needle-free injector all generated a neutralizing antibody response and had the highest levels of neutralizing antibodies.
Subjects who received VRC5283 in a split-dose administered to both arms had more robust immune responses than those receiving the full dose in 1 arm.
“NIAID has begun phase 2 testing of this candidate to determine if it can prevent Zika virus infection, and the promising phase 1 data . . . support its continued development,” Dr Fauci said.
An experimental Zika vaccine is safe and induces an immune response in healthy adults, according to research published in The Lancet.
Investigators tested 2 potential Zika vaccines, VRC5288 and VRC5283, in a pair of phase 1 trials.
Both vaccines were considered well-tolerated, but one of them, VRC5283, induced a greater immune response than the other.
Both vaccines were developed by investigators at the National Institute of Allergy and Infectious Diseases (NIAID).
Now, NIAID is leading an international effort to evaluate VRC5283 in a phase 2/2b trial.
“Following early reports that Zika infection during pregnancy can lead to birth defects, NIAID scientists rapidly created one of the first investigational Zika vaccines using a DNA-based platform and began initial studies in healthy adults less than 1 year later,” said NIAID Director Anthony S. Fauci, MD.
To create their vaccines, the investigators inserted into plasmids genes that encode proteins found on the surface of the Zika virus.
The team developed 2 different plasmids for clinical testing: VRC5288 (Zika virus and Japanese encephalitis virus chimera) and VRC5283 (wild-type Zika virus).
In August 2016, NIAID initiated a phase 1 trial of the VRC5288 plasmid in 80 healthy volunteers ages 18 to 35. Subjects received a 4 mg dose via a needle and syringe injection in the arm muscle.
They received doses of VRC5288 at 0 and 8 weeks; 0 and 12 weeks; 0, 4, and 8 weeks; or 0, 4, and 20 weeks.
In December 2016, NIAID initiated a separate trial testing the VRC5283 plasmid. This study enrolled 45 healthy volunteers ages 18 to 50.
Subjects in this trial received 4 mg doses of VRC5283 at 0, 4, and 8 weeks. They were vaccinated in 3 different ways—via single-dose needle and syringe injection in 1 arm, via split-dose needle and syringe injection in each arm, or via needle-free injection in each arm.
Safety
The vaccinations were considered safe and well-tolerated in both trials, although some participants experienced mild to moderate reactions.
Local reactions (with VRC5288 and VRC5283, respectively) included pain/tenderness (mild—46% and 73%, moderate—0% and 7%), mild swelling (1% and 7%), and mild redness (6% and 2%).
Systemic reactions (with VRC5288 and VRC5283, respectively) included malaise (mild—25% and 33%, moderate—3% and 4%), myalgia (mild—18% and 13%, moderate—4% and 7%), headache (mild—19% and 29%, moderate—4% and 4%), chills (mild—6% and 2%, moderate—1% and 2%), nausea (mild—8% and 4%, moderate—1% and 0%), and joint pain (mild—5% and 16%, moderate—0% and 2%).
Immunogenicity
The investigators analyzed blood samples from all subjects 4 weeks after their final vaccinations.
The team found that 60% to 89% of subjects generated a neutralizing antibody response to VRC5288, and 77% to 100% of subjects generated a neutralizing antibody response to VRC5283.
Subjects who received VRC5283 via the needle-free injector all generated a neutralizing antibody response and had the highest levels of neutralizing antibodies.
Subjects who received VRC5283 in a split-dose administered to both arms had more robust immune responses than those receiving the full dose in 1 arm.
“NIAID has begun phase 2 testing of this candidate to determine if it can prevent Zika virus infection, and the promising phase 1 data . . . support its continued development,” Dr Fauci said.
An experimental Zika vaccine is safe and induces an immune response in healthy adults, according to research published in The Lancet.
Investigators tested 2 potential Zika vaccines, VRC5288 and VRC5283, in a pair of phase 1 trials.
Both vaccines were considered well-tolerated, but one of them, VRC5283, induced a greater immune response than the other.
Both vaccines were developed by investigators at the National Institute of Allergy and Infectious Diseases (NIAID).
Now, NIAID is leading an international effort to evaluate VRC5283 in a phase 2/2b trial.
“Following early reports that Zika infection during pregnancy can lead to birth defects, NIAID scientists rapidly created one of the first investigational Zika vaccines using a DNA-based platform and began initial studies in healthy adults less than 1 year later,” said NIAID Director Anthony S. Fauci, MD.
To create their vaccines, the investigators inserted into plasmids genes that encode proteins found on the surface of the Zika virus.
The team developed 2 different plasmids for clinical testing: VRC5288 (Zika virus and Japanese encephalitis virus chimera) and VRC5283 (wild-type Zika virus).
In August 2016, NIAID initiated a phase 1 trial of the VRC5288 plasmid in 80 healthy volunteers ages 18 to 35. Subjects received a 4 mg dose via a needle and syringe injection in the arm muscle.
They received doses of VRC5288 at 0 and 8 weeks; 0 and 12 weeks; 0, 4, and 8 weeks; or 0, 4, and 20 weeks.
In December 2016, NIAID initiated a separate trial testing the VRC5283 plasmid. This study enrolled 45 healthy volunteers ages 18 to 50.
Subjects in this trial received 4 mg doses of VRC5283 at 0, 4, and 8 weeks. They were vaccinated in 3 different ways—via single-dose needle and syringe injection in 1 arm, via split-dose needle and syringe injection in each arm, or via needle-free injection in each arm.
Safety
The vaccinations were considered safe and well-tolerated in both trials, although some participants experienced mild to moderate reactions.
Local reactions (with VRC5288 and VRC5283, respectively) included pain/tenderness (mild—46% and 73%, moderate—0% and 7%), mild swelling (1% and 7%), and mild redness (6% and 2%).
Systemic reactions (with VRC5288 and VRC5283, respectively) included malaise (mild—25% and 33%, moderate—3% and 4%), myalgia (mild—18% and 13%, moderate—4% and 7%), headache (mild—19% and 29%, moderate—4% and 4%), chills (mild—6% and 2%, moderate—1% and 2%), nausea (mild—8% and 4%, moderate—1% and 0%), and joint pain (mild—5% and 16%, moderate—0% and 2%).
Immunogenicity
The investigators analyzed blood samples from all subjects 4 weeks after their final vaccinations.
The team found that 60% to 89% of subjects generated a neutralizing antibody response to VRC5288, and 77% to 100% of subjects generated a neutralizing antibody response to VRC5283.
Subjects who received VRC5283 via the needle-free injector all generated a neutralizing antibody response and had the highest levels of neutralizing antibodies.
Subjects who received VRC5283 in a split-dose administered to both arms had more robust immune responses than those receiving the full dose in 1 arm.
“NIAID has begun phase 2 testing of this candidate to determine if it can prevent Zika virus infection, and the promising phase 1 data . . . support its continued development,” Dr Fauci said.