User login
Partnering for pulmonary fibrosis
The CHEST Foundation raises awareness for the most common interstitial lung disease.
On August 27, the CHEST Foundation and the Feldman Family Foundation will be hosting the 9th annual Irv Feldman Texas Hold ‘Em Tournament & Casino Night fundraiser supporting patient access and the provision of better quality of life for patients battling the interstitial lung disease – pulmonary fibrosis.
“My dad, Irv, had pulmonary fibrosis and deeply loved to play poker. It was always a family activity, and it continued through when he got sick. We played at his kitchen table when he couldn’t leave the house, and we even brought cards and chips to his hospital and rehab rooms,” said Mitch Feldman, President of the Feldman Family Foundation and member of the CHEST Foundation Board of Trustees. “During these few hours of poker play, he all but forgot about his illness and showed virtually no symptoms of the disease. In his honor, we created an event where people would come together to have fun playing poker while raising money for the disease [that] so deeply impacted our family.”
Through years of hosting the event, the Feldman family and the CHEST Foundation secured funding to develop a pulmonary fibrosis patient education resource hub that serves as a resource for those newly diagnosed and living with this disease. The Feldman Family and the CHEST Foundation continue to raise funds to support both early diagnosis and closing the gap between diagnosis and beginning treatment.
Partnering to address gaps
Affecting around 400,000 people in the United States, ILDs are frequently misdiagnosed as more common lung diseases. Some studies show that reaching an appropriate diagnosis for rarer lung diseases can take upwards of several years.
To begin addressing the issue of delays in diagnosis, the American College of Chest Physicians (CHEST) and Three Lakes Foundation are collaborating on a multiphase educational initiative aiming to reduce the time it takes to identify interstitial lung diseases like pulmonary fibrosis.
The initiative is called “Bridging SpecialtiesTM: Timely Diagnosis for ILD Patients” to highlight the collaboration of pulmonary and primary care medicine. A steering committee of medical experts – including pulmonologists, primary care physicians, and a nursing professional – will work to create materials that will aid in identifying and diagnosing complex lung diseases quicker.
“By having experts from both pulmonary and primary care medicine as members of the steering committee, we are bringing together the pieces of the puzzle that is a complex diagnosis,” said Bridging Specialties steering committee member and family medicine physician, Dr. William Lago. “Patients first see their family medicine or primary care clinicians and, all too often, the most complex lung diseases present in ways that are indistinguishable from more common conditions like asthma and COPD. Bringing together experts in both fields will yield the best results in creating a path to diagnosis.”
To learn more about the Bridging SpecialtiesTM: Timely Diagnosis for ILD Patients initiative and to sign up for updates, visit https://tinyurl.com/2p92ha6r.
For ticket and donation information to the Irv Feldman Texas Hold ‘Em Tournament & Casino Night, visit the CHEST Foundation website at foundation.chestnet.org.
The CHEST Foundation raises awareness for the most common interstitial lung disease.
On August 27, the CHEST Foundation and the Feldman Family Foundation will be hosting the 9th annual Irv Feldman Texas Hold ‘Em Tournament & Casino Night fundraiser supporting patient access and the provision of better quality of life for patients battling the interstitial lung disease – pulmonary fibrosis.
“My dad, Irv, had pulmonary fibrosis and deeply loved to play poker. It was always a family activity, and it continued through when he got sick. We played at his kitchen table when he couldn’t leave the house, and we even brought cards and chips to his hospital and rehab rooms,” said Mitch Feldman, President of the Feldman Family Foundation and member of the CHEST Foundation Board of Trustees. “During these few hours of poker play, he all but forgot about his illness and showed virtually no symptoms of the disease. In his honor, we created an event where people would come together to have fun playing poker while raising money for the disease [that] so deeply impacted our family.”
Through years of hosting the event, the Feldman family and the CHEST Foundation secured funding to develop a pulmonary fibrosis patient education resource hub that serves as a resource for those newly diagnosed and living with this disease. The Feldman Family and the CHEST Foundation continue to raise funds to support both early diagnosis and closing the gap between diagnosis and beginning treatment.
Partnering to address gaps
Affecting around 400,000 people in the United States, ILDs are frequently misdiagnosed as more common lung diseases. Some studies show that reaching an appropriate diagnosis for rarer lung diseases can take upwards of several years.
To begin addressing the issue of delays in diagnosis, the American College of Chest Physicians (CHEST) and Three Lakes Foundation are collaborating on a multiphase educational initiative aiming to reduce the time it takes to identify interstitial lung diseases like pulmonary fibrosis.
The initiative is called “Bridging SpecialtiesTM: Timely Diagnosis for ILD Patients” to highlight the collaboration of pulmonary and primary care medicine. A steering committee of medical experts – including pulmonologists, primary care physicians, and a nursing professional – will work to create materials that will aid in identifying and diagnosing complex lung diseases quicker.
“By having experts from both pulmonary and primary care medicine as members of the steering committee, we are bringing together the pieces of the puzzle that is a complex diagnosis,” said Bridging Specialties steering committee member and family medicine physician, Dr. William Lago. “Patients first see their family medicine or primary care clinicians and, all too often, the most complex lung diseases present in ways that are indistinguishable from more common conditions like asthma and COPD. Bringing together experts in both fields will yield the best results in creating a path to diagnosis.”
To learn more about the Bridging SpecialtiesTM: Timely Diagnosis for ILD Patients initiative and to sign up for updates, visit https://tinyurl.com/2p92ha6r.
For ticket and donation information to the Irv Feldman Texas Hold ‘Em Tournament & Casino Night, visit the CHEST Foundation website at foundation.chestnet.org.
The CHEST Foundation raises awareness for the most common interstitial lung disease.
On August 27, the CHEST Foundation and the Feldman Family Foundation will be hosting the 9th annual Irv Feldman Texas Hold ‘Em Tournament & Casino Night fundraiser supporting patient access and the provision of better quality of life for patients battling the interstitial lung disease – pulmonary fibrosis.
“My dad, Irv, had pulmonary fibrosis and deeply loved to play poker. It was always a family activity, and it continued through when he got sick. We played at his kitchen table when he couldn’t leave the house, and we even brought cards and chips to his hospital and rehab rooms,” said Mitch Feldman, President of the Feldman Family Foundation and member of the CHEST Foundation Board of Trustees. “During these few hours of poker play, he all but forgot about his illness and showed virtually no symptoms of the disease. In his honor, we created an event where people would come together to have fun playing poker while raising money for the disease [that] so deeply impacted our family.”
Through years of hosting the event, the Feldman family and the CHEST Foundation secured funding to develop a pulmonary fibrosis patient education resource hub that serves as a resource for those newly diagnosed and living with this disease. The Feldman Family and the CHEST Foundation continue to raise funds to support both early diagnosis and closing the gap between diagnosis and beginning treatment.
Partnering to address gaps
Affecting around 400,000 people in the United States, ILDs are frequently misdiagnosed as more common lung diseases. Some studies show that reaching an appropriate diagnosis for rarer lung diseases can take upwards of several years.
To begin addressing the issue of delays in diagnosis, the American College of Chest Physicians (CHEST) and Three Lakes Foundation are collaborating on a multiphase educational initiative aiming to reduce the time it takes to identify interstitial lung diseases like pulmonary fibrosis.
The initiative is called “Bridging SpecialtiesTM: Timely Diagnosis for ILD Patients” to highlight the collaboration of pulmonary and primary care medicine. A steering committee of medical experts – including pulmonologists, primary care physicians, and a nursing professional – will work to create materials that will aid in identifying and diagnosing complex lung diseases quicker.
“By having experts from both pulmonary and primary care medicine as members of the steering committee, we are bringing together the pieces of the puzzle that is a complex diagnosis,” said Bridging Specialties steering committee member and family medicine physician, Dr. William Lago. “Patients first see their family medicine or primary care clinicians and, all too often, the most complex lung diseases present in ways that are indistinguishable from more common conditions like asthma and COPD. Bringing together experts in both fields will yield the best results in creating a path to diagnosis.”
To learn more about the Bridging SpecialtiesTM: Timely Diagnosis for ILD Patients initiative and to sign up for updates, visit https://tinyurl.com/2p92ha6r.
For ticket and donation information to the Irv Feldman Texas Hold ‘Em Tournament & Casino Night, visit the CHEST Foundation website at foundation.chestnet.org.
Diffuse Lung Disease & Transplant Network
Interstitial Lung Disease Section
Diagnosis of idiopathic pulmonary fibrosis: Is tissue still an issue?
Per ATS/ERS/JRS/ALAT guidelines, diagnosis of IPF requires exclusion of known causes of interstitial lung disease (ILD) and either the presence of a usual interstitial pneumonia (UIP) or probable UIP pattern on HRCT scan or specific combinations of HRCT scan and histopathologic patterns. Surgical lung biopsy (SLB) is the gold standard for histopathologic diagnosis.
The recent update (Raghu, et al. Am J Respir Crit Care Med. 2022;205[9]:1084-92) made a conditional recommendation for transbronchial lung cryobiopsy (TBLC) as an acceptable alternative to SLB in patients with undetermined ILD. Systematic analysis revealed a diagnostic yield of 79% (85% when ≥ 3 sites were sampled) by TBLC compared with 90% on SLB. With consideration of this diagnostic yield vs the risk of pneumothorax, severe bleeding, and procedural mortality, TBLC is an attractive tool compared with SLB. Overall, the utility of TBLC remains limited to experienced centers due to dependence on proceduralist and pathologist skills for optimal success and more data are awaited.
No recommendation was made for or against the use of genomic classifiers (GC) for the diagnosis of UIP in patients with undetermined ILD undergoing transbronchial biopsy. Although, meta-analysis revealed a specificity of 92%, this may be driven by patient enrichment with a high probability for UIP population. GC has the potential to reduce SLB-associated risks and provide diagnostic information for multidisciplinary discussion in certain scenarios. However, limitations arise from the inability to distinguish specific ILD subtype associated with the UIP pattern; further improvement in sensitivity and understanding of downstream consequences of false-negative results is necessary.
Kevin Dsouza, MD
Fellow-in-Training
Interstitial Lung Disease Section
Diagnosis of idiopathic pulmonary fibrosis: Is tissue still an issue?
Per ATS/ERS/JRS/ALAT guidelines, diagnosis of IPF requires exclusion of known causes of interstitial lung disease (ILD) and either the presence of a usual interstitial pneumonia (UIP) or probable UIP pattern on HRCT scan or specific combinations of HRCT scan and histopathologic patterns. Surgical lung biopsy (SLB) is the gold standard for histopathologic diagnosis.
The recent update (Raghu, et al. Am J Respir Crit Care Med. 2022;205[9]:1084-92) made a conditional recommendation for transbronchial lung cryobiopsy (TBLC) as an acceptable alternative to SLB in patients with undetermined ILD. Systematic analysis revealed a diagnostic yield of 79% (85% when ≥ 3 sites were sampled) by TBLC compared with 90% on SLB. With consideration of this diagnostic yield vs the risk of pneumothorax, severe bleeding, and procedural mortality, TBLC is an attractive tool compared with SLB. Overall, the utility of TBLC remains limited to experienced centers due to dependence on proceduralist and pathologist skills for optimal success and more data are awaited.
No recommendation was made for or against the use of genomic classifiers (GC) for the diagnosis of UIP in patients with undetermined ILD undergoing transbronchial biopsy. Although, meta-analysis revealed a specificity of 92%, this may be driven by patient enrichment with a high probability for UIP population. GC has the potential to reduce SLB-associated risks and provide diagnostic information for multidisciplinary discussion in certain scenarios. However, limitations arise from the inability to distinguish specific ILD subtype associated with the UIP pattern; further improvement in sensitivity and understanding of downstream consequences of false-negative results is necessary.
Kevin Dsouza, MD
Fellow-in-Training
Interstitial Lung Disease Section
Diagnosis of idiopathic pulmonary fibrosis: Is tissue still an issue?
Per ATS/ERS/JRS/ALAT guidelines, diagnosis of IPF requires exclusion of known causes of interstitial lung disease (ILD) and either the presence of a usual interstitial pneumonia (UIP) or probable UIP pattern on HRCT scan or specific combinations of HRCT scan and histopathologic patterns. Surgical lung biopsy (SLB) is the gold standard for histopathologic diagnosis.
The recent update (Raghu, et al. Am J Respir Crit Care Med. 2022;205[9]:1084-92) made a conditional recommendation for transbronchial lung cryobiopsy (TBLC) as an acceptable alternative to SLB in patients with undetermined ILD. Systematic analysis revealed a diagnostic yield of 79% (85% when ≥ 3 sites were sampled) by TBLC compared with 90% on SLB. With consideration of this diagnostic yield vs the risk of pneumothorax, severe bleeding, and procedural mortality, TBLC is an attractive tool compared with SLB. Overall, the utility of TBLC remains limited to experienced centers due to dependence on proceduralist and pathologist skills for optimal success and more data are awaited.
No recommendation was made for or against the use of genomic classifiers (GC) for the diagnosis of UIP in patients with undetermined ILD undergoing transbronchial biopsy. Although, meta-analysis revealed a specificity of 92%, this may be driven by patient enrichment with a high probability for UIP population. GC has the potential to reduce SLB-associated risks and provide diagnostic information for multidisciplinary discussion in certain scenarios. However, limitations arise from the inability to distinguish specific ILD subtype associated with the UIP pattern; further improvement in sensitivity and understanding of downstream consequences of false-negative results is necessary.
Kevin Dsouza, MD
Fellow-in-Training
Thoracic Oncology & Chest Procedures Network
Ultrasound and Chest Imaging Section
Advanced critical care echocardiography: A noninvasive tool for hemodynamic assessment in critically ill patients
Hemodynamic assessments in critically ill patients are important to guide accurate management; however, traditional invasive methods of measuring cardiac output have significant limitations, including risks of infection and bleeding. ACCE can provide a multitude of hemodynamic measurements from cardiac output (CO) to right ventricular systolic pressure (RVSP) and left atrial pressure (LAP). Combinations of left ventricular function parameters, along with estimation of filling pressures, can help distinguish between types of shock. Schmidt and colleagues (Sci Rep. 2022;12[1]:7187) demonstrated that measurement of these indices in the majority of patients helped elucidate the cause for hemodynamic compromise. They found presence of a cardiac index (CI) < 2.5/min.m2 was associated with a doubling of ICU mortality as compared with predictions based on severity of illness scores in otherwise hemodynamically stable patients. Hollenberg and colleagues (Am J Cardiol. 2021;153:135-39) demonstrated the feasibility of a simpler stratification using the left ventricular ejection fraction (LVEF) and CI in coronavirus disease 2019 patients with shock, where low CI despite having a preserved LVEF was associated with worse outcomes.
Quick, reliable data are an intensivist’s friend. Utilizing ACCE at the bedside adds another tool in our arsenal to provide real-time hemodynamic data that can be used to manage patients in the ICU. ACCE also allows repeated measurements to determine changes based on therapeutic interventions initiated.
In recognition of the importance of ACCE as a tool for intensivists, the National Board of Echocardiography (NBE) now offers a pathway toward board certification with the Examination of Special Competence in Critical Care Echocardiography (CCEeXAM). CHEST continues to offer cutting-edge courses in ACCE, as well as a board review course for learners interested in sitting for the CCEeXAM.
Amik Sodhi, MD, FCCP
Gul Zaidi, MD, FCCP
Members-at-Large
Ultrasound and Chest Imaging Section
Advanced critical care echocardiography: A noninvasive tool for hemodynamic assessment in critically ill patients
Hemodynamic assessments in critically ill patients are important to guide accurate management; however, traditional invasive methods of measuring cardiac output have significant limitations, including risks of infection and bleeding. ACCE can provide a multitude of hemodynamic measurements from cardiac output (CO) to right ventricular systolic pressure (RVSP) and left atrial pressure (LAP). Combinations of left ventricular function parameters, along with estimation of filling pressures, can help distinguish between types of shock. Schmidt and colleagues (Sci Rep. 2022;12[1]:7187) demonstrated that measurement of these indices in the majority of patients helped elucidate the cause for hemodynamic compromise. They found presence of a cardiac index (CI) < 2.5/min.m2 was associated with a doubling of ICU mortality as compared with predictions based on severity of illness scores in otherwise hemodynamically stable patients. Hollenberg and colleagues (Am J Cardiol. 2021;153:135-39) demonstrated the feasibility of a simpler stratification using the left ventricular ejection fraction (LVEF) and CI in coronavirus disease 2019 patients with shock, where low CI despite having a preserved LVEF was associated with worse outcomes.
Quick, reliable data are an intensivist’s friend. Utilizing ACCE at the bedside adds another tool in our arsenal to provide real-time hemodynamic data that can be used to manage patients in the ICU. ACCE also allows repeated measurements to determine changes based on therapeutic interventions initiated.
In recognition of the importance of ACCE as a tool for intensivists, the National Board of Echocardiography (NBE) now offers a pathway toward board certification with the Examination of Special Competence in Critical Care Echocardiography (CCEeXAM). CHEST continues to offer cutting-edge courses in ACCE, as well as a board review course for learners interested in sitting for the CCEeXAM.
Amik Sodhi, MD, FCCP
Gul Zaidi, MD, FCCP
Members-at-Large
Ultrasound and Chest Imaging Section
Advanced critical care echocardiography: A noninvasive tool for hemodynamic assessment in critically ill patients
Hemodynamic assessments in critically ill patients are important to guide accurate management; however, traditional invasive methods of measuring cardiac output have significant limitations, including risks of infection and bleeding. ACCE can provide a multitude of hemodynamic measurements from cardiac output (CO) to right ventricular systolic pressure (RVSP) and left atrial pressure (LAP). Combinations of left ventricular function parameters, along with estimation of filling pressures, can help distinguish between types of shock. Schmidt and colleagues (Sci Rep. 2022;12[1]:7187) demonstrated that measurement of these indices in the majority of patients helped elucidate the cause for hemodynamic compromise. They found presence of a cardiac index (CI) < 2.5/min.m2 was associated with a doubling of ICU mortality as compared with predictions based on severity of illness scores in otherwise hemodynamically stable patients. Hollenberg and colleagues (Am J Cardiol. 2021;153:135-39) demonstrated the feasibility of a simpler stratification using the left ventricular ejection fraction (LVEF) and CI in coronavirus disease 2019 patients with shock, where low CI despite having a preserved LVEF was associated with worse outcomes.
Quick, reliable data are an intensivist’s friend. Utilizing ACCE at the bedside adds another tool in our arsenal to provide real-time hemodynamic data that can be used to manage patients in the ICU. ACCE also allows repeated measurements to determine changes based on therapeutic interventions initiated.
In recognition of the importance of ACCE as a tool for intensivists, the National Board of Echocardiography (NBE) now offers a pathway toward board certification with the Examination of Special Competence in Critical Care Echocardiography (CCEeXAM). CHEST continues to offer cutting-edge courses in ACCE, as well as a board review course for learners interested in sitting for the CCEeXAM.
Amik Sodhi, MD, FCCP
Gul Zaidi, MD, FCCP
Members-at-Large
Thoracic Oncology & Chest Procedures Network
Interventional Procedures Section
Mind the gap: Improving adherence to lung cancer screening follow-up
The gap in adherence rates between a disciplined clinical trial and the heterogenous patchwork of U.S. health care is hardly unusual, but as lung cancer remains the number one cancer killer both worldwide and in the United States, one such disparity bears closer scrutiny.
In 2011, the National Lung Screening Trial (NLST) demonstrated a 20% reduction in lung cancer mortality with the implementation of low dose CT scan screening with 95% adherence to CT scan follow-up within 15 months of initial screening imaging (Aberle, et al. N Engl J Med. 2011;365[5]:395-409). Unfortunately, estimates of real-world adherence to lung cancer screening (LCS) follow-up fall to 51% even within an extended 18-month window (Hirsch, et al. Ann Am Thorac Soc. 2019;16[10]:1329-32).
Recent studies compared adherence to LCS follow-up between centralized and decentralized screening programs. Centralized programs used dedicated program coordinators and a tracking system, while decentralized programs relied on primary care providers.(Sakoda, et al. JAMA Network Open. 2021;4[4]:e218559). A subsequent study demonstrated adherence of 70% vs 41% among patients in centralized vs decentralized programs, respectively (Smith, et al. Chest. 2022;161[3]:818-25).
This gap is even more pronounced in majority-Black populations. Kunitomo and colleagues showed 33% lower odds of adherence to LCS follow-up compared with White patients (Kunitomo, et al. Chest. 2022;161[1]:266-75). Another study in a diverse, majority-Black patient population showed only 31% adherence to LCS follow-up at 1 year (Erkmen, et al. Cancer Causes Control. 2021;32[3]:291-8).
How could we close this gap? Centralized LCS programs show promise of increasing adherence to LCS follow-up. Heightened awareness of and targeted investment to mitigate racial inequities in LCS is imperative.
Jose De Cardenas MD
John Howe, MD
Members-at-Large
Interventional Procedures Section
Mind the gap: Improving adherence to lung cancer screening follow-up
The gap in adherence rates between a disciplined clinical trial and the heterogenous patchwork of U.S. health care is hardly unusual, but as lung cancer remains the number one cancer killer both worldwide and in the United States, one such disparity bears closer scrutiny.
In 2011, the National Lung Screening Trial (NLST) demonstrated a 20% reduction in lung cancer mortality with the implementation of low dose CT scan screening with 95% adherence to CT scan follow-up within 15 months of initial screening imaging (Aberle, et al. N Engl J Med. 2011;365[5]:395-409). Unfortunately, estimates of real-world adherence to lung cancer screening (LCS) follow-up fall to 51% even within an extended 18-month window (Hirsch, et al. Ann Am Thorac Soc. 2019;16[10]:1329-32).
Recent studies compared adherence to LCS follow-up between centralized and decentralized screening programs. Centralized programs used dedicated program coordinators and a tracking system, while decentralized programs relied on primary care providers.(Sakoda, et al. JAMA Network Open. 2021;4[4]:e218559). A subsequent study demonstrated adherence of 70% vs 41% among patients in centralized vs decentralized programs, respectively (Smith, et al. Chest. 2022;161[3]:818-25).
This gap is even more pronounced in majority-Black populations. Kunitomo and colleagues showed 33% lower odds of adherence to LCS follow-up compared with White patients (Kunitomo, et al. Chest. 2022;161[1]:266-75). Another study in a diverse, majority-Black patient population showed only 31% adherence to LCS follow-up at 1 year (Erkmen, et al. Cancer Causes Control. 2021;32[3]:291-8).
How could we close this gap? Centralized LCS programs show promise of increasing adherence to LCS follow-up. Heightened awareness of and targeted investment to mitigate racial inequities in LCS is imperative.
Jose De Cardenas MD
John Howe, MD
Members-at-Large
Interventional Procedures Section
Mind the gap: Improving adherence to lung cancer screening follow-up
The gap in adherence rates between a disciplined clinical trial and the heterogenous patchwork of U.S. health care is hardly unusual, but as lung cancer remains the number one cancer killer both worldwide and in the United States, one such disparity bears closer scrutiny.
In 2011, the National Lung Screening Trial (NLST) demonstrated a 20% reduction in lung cancer mortality with the implementation of low dose CT scan screening with 95% adherence to CT scan follow-up within 15 months of initial screening imaging (Aberle, et al. N Engl J Med. 2011;365[5]:395-409). Unfortunately, estimates of real-world adherence to lung cancer screening (LCS) follow-up fall to 51% even within an extended 18-month window (Hirsch, et al. Ann Am Thorac Soc. 2019;16[10]:1329-32).
Recent studies compared adherence to LCS follow-up between centralized and decentralized screening programs. Centralized programs used dedicated program coordinators and a tracking system, while decentralized programs relied on primary care providers.(Sakoda, et al. JAMA Network Open. 2021;4[4]:e218559). A subsequent study demonstrated adherence of 70% vs 41% among patients in centralized vs decentralized programs, respectively (Smith, et al. Chest. 2022;161[3]:818-25).
This gap is even more pronounced in majority-Black populations. Kunitomo and colleagues showed 33% lower odds of adherence to LCS follow-up compared with White patients (Kunitomo, et al. Chest. 2022;161[1]:266-75). Another study in a diverse, majority-Black patient population showed only 31% adherence to LCS follow-up at 1 year (Erkmen, et al. Cancer Causes Control. 2021;32[3]:291-8).
How could we close this gap? Centralized LCS programs show promise of increasing adherence to LCS follow-up. Heightened awareness of and targeted investment to mitigate racial inequities in LCS is imperative.
Jose De Cardenas MD
John Howe, MD
Members-at-Large
Sleep Medicine Network
Home-based Mechanical Ventilation and Neuromuscular Disease Section
Navigating the latest device supply chain challenge: Mechanical airway clearance
(distal airways). Cough augmentation techniques provide lung volume recruitment on the insufflation phase, in addition to mobilization of secretions with augmentation of the peak expiratory flow rate to >160 L/min on the exhalation phase.
A mechanical insufflation-exsufflation (MI-E) device (T70 Cough Assist - Phillips) is now on indefinite backorder. This creates a dangerous situation for our patients requiring cough augmentation for survival. Alternative options that provide both MI-E and high frequency oscillation include two systems (Synclara Cough System – Hill-rom and the Biwaze Cough System-ABM Respiratory Care).
The Synclara can only be obtained in a direct-to-patient model, contracting with individual respiratory therapists, outside of the standard durable medical equipment model. The final MI-E model option is the VOCSYN multifunctional ventilator (ventilator, cough assist, nebulizer, oxygen concentrator, suction). This multifunction ventilator has had variable acceptance with HCPCS code E0467. If the VOCSYN is chosen, the patient cannot have been issued any component devices or have reached the 36-month cap for oxygen equipment (CR 10854 special payment rule, 42 CFR414.222).
As the supply of devices is exhausted, we will need to shift to evidence-based manual options. Manual cough augmentation can be done effectively with a bag-valve mask, using breath stacking to achieve maximal lung insufflation, optimizing the length tension relationship of elastic recoil on exhalation to increase peak cough flow (PCF).
This can be done alone but is more effective when combined with manually assisted cough (Bach JR. Chest. 1993;104[5]:1553-62). These interventions require training of the caregivers, using resources such as those found at www.canventottawa.ca.
With continued supply chain instability, manual airway clearance techniques should be considered in patients with less advanced cough impairment (PCF 160-270 L/min), to save the remaining devices for those with PCF of <160 L/min.
Jeanette Brown, MD, PhD
Karin Provost, DO, PhD
Members-at-Large
Home-based Mechanical Ventilation and Neuromuscular Disease Section
Navigating the latest device supply chain challenge: Mechanical airway clearance
(distal airways). Cough augmentation techniques provide lung volume recruitment on the insufflation phase, in addition to mobilization of secretions with augmentation of the peak expiratory flow rate to >160 L/min on the exhalation phase.
A mechanical insufflation-exsufflation (MI-E) device (T70 Cough Assist - Phillips) is now on indefinite backorder. This creates a dangerous situation for our patients requiring cough augmentation for survival. Alternative options that provide both MI-E and high frequency oscillation include two systems (Synclara Cough System – Hill-rom and the Biwaze Cough System-ABM Respiratory Care).
The Synclara can only be obtained in a direct-to-patient model, contracting with individual respiratory therapists, outside of the standard durable medical equipment model. The final MI-E model option is the VOCSYN multifunctional ventilator (ventilator, cough assist, nebulizer, oxygen concentrator, suction). This multifunction ventilator has had variable acceptance with HCPCS code E0467. If the VOCSYN is chosen, the patient cannot have been issued any component devices or have reached the 36-month cap for oxygen equipment (CR 10854 special payment rule, 42 CFR414.222).
As the supply of devices is exhausted, we will need to shift to evidence-based manual options. Manual cough augmentation can be done effectively with a bag-valve mask, using breath stacking to achieve maximal lung insufflation, optimizing the length tension relationship of elastic recoil on exhalation to increase peak cough flow (PCF).
This can be done alone but is more effective when combined with manually assisted cough (Bach JR. Chest. 1993;104[5]:1553-62). These interventions require training of the caregivers, using resources such as those found at www.canventottawa.ca.
With continued supply chain instability, manual airway clearance techniques should be considered in patients with less advanced cough impairment (PCF 160-270 L/min), to save the remaining devices for those with PCF of <160 L/min.
Jeanette Brown, MD, PhD
Karin Provost, DO, PhD
Members-at-Large
Home-based Mechanical Ventilation and Neuromuscular Disease Section
Navigating the latest device supply chain challenge: Mechanical airway clearance
(distal airways). Cough augmentation techniques provide lung volume recruitment on the insufflation phase, in addition to mobilization of secretions with augmentation of the peak expiratory flow rate to >160 L/min on the exhalation phase.
A mechanical insufflation-exsufflation (MI-E) device (T70 Cough Assist - Phillips) is now on indefinite backorder. This creates a dangerous situation for our patients requiring cough augmentation for survival. Alternative options that provide both MI-E and high frequency oscillation include two systems (Synclara Cough System – Hill-rom and the Biwaze Cough System-ABM Respiratory Care).
The Synclara can only be obtained in a direct-to-patient model, contracting with individual respiratory therapists, outside of the standard durable medical equipment model. The final MI-E model option is the VOCSYN multifunctional ventilator (ventilator, cough assist, nebulizer, oxygen concentrator, suction). This multifunction ventilator has had variable acceptance with HCPCS code E0467. If the VOCSYN is chosen, the patient cannot have been issued any component devices or have reached the 36-month cap for oxygen equipment (CR 10854 special payment rule, 42 CFR414.222).
As the supply of devices is exhausted, we will need to shift to evidence-based manual options. Manual cough augmentation can be done effectively with a bag-valve mask, using breath stacking to achieve maximal lung insufflation, optimizing the length tension relationship of elastic recoil on exhalation to increase peak cough flow (PCF).
This can be done alone but is more effective when combined with manually assisted cough (Bach JR. Chest. 1993;104[5]:1553-62). These interventions require training of the caregivers, using resources such as those found at www.canventottawa.ca.
With continued supply chain instability, manual airway clearance techniques should be considered in patients with less advanced cough impairment (PCF 160-270 L/min), to save the remaining devices for those with PCF of <160 L/min.
Jeanette Brown, MD, PhD
Karin Provost, DO, PhD
Members-at-Large
Airways Disorders Network
Asthma and COPD Section
Go TEAM! Shared decision-making tool for patient-clinician collaboration in severe asthma
Shared decision-making is associated with improved medication adherence in adults (Wilson, et al. Am J Respir Crit Care Med. 2010;181[6]:566-77) and quality of life and asthma control in children (Taylor, et al. J Asthma. 2018;55[6]:675-83). The Global Initiative for Asthma committee recommends a patient-clinician partnership. Activated and engaged patients play a major role in their asthma management (https://ginasthma.org/gina-reports). Shared decision-making discussions should include potential benefits and harms of the therapeutic options, patient’s values and lifestyle preferences, and addressing concerns.
The CHEST Foundation, the Allergy and Asthma Network, and the American College of Allergy, Asthma, and Immunology developed an online shared decision- making tool for severe asthma (https://asthma.chestnet.org/sdm-tool).
This tool utilizes patient’s values, specifics about triggers, asthma control, medication side effects, and lifestyle preferences to identify personalized management options. The tool provides information about recommended therapeutic options in simple terms, including potential benefits, possible side effects, expected treatment frequency and duration, and financial aid information. The treatment options currently explained in this tool include anti-immunoglobulin E, anti-interleukin-5, anti-interleukin-4/13, bronchial thermoplasty, long-acting muscarinic antagonist, macrolides, oral corticosteroids, and standard of care.
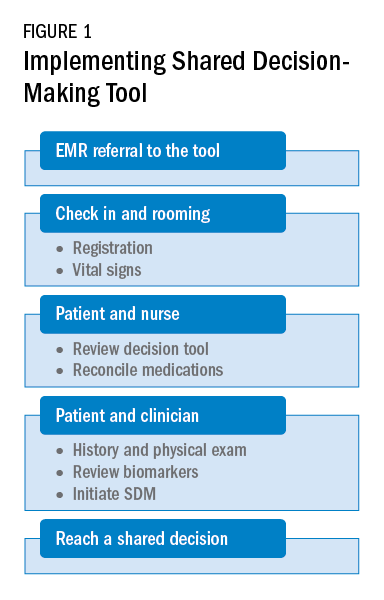
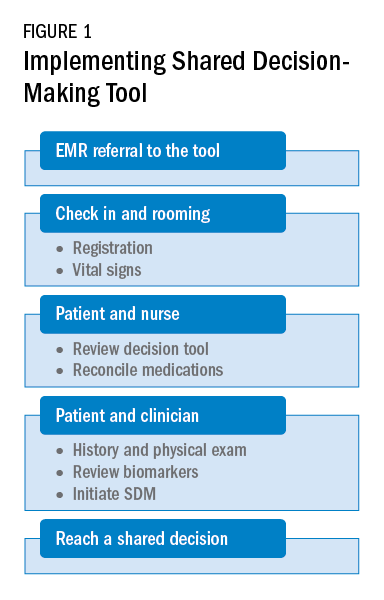
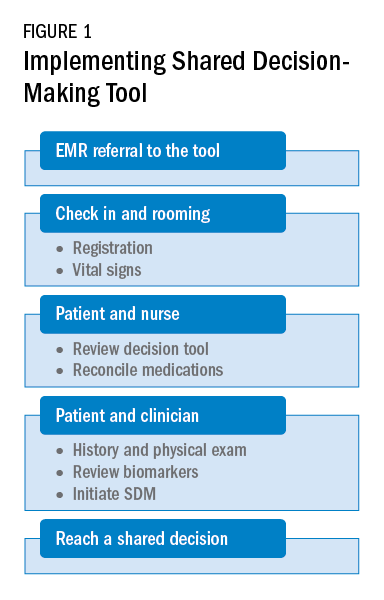
As a team, the patient and the health care professional can use this tool during office visits to help guide management. Figure 1 shows a suggested workflow to utilize the tool in clinical practice.
Potential barriers include excess time and increased human resources. Barrier mitigation may include reviewing the tool and reconciling the medications before the clinician enters the room. With these interventions, many clinician encounters may be completed in 10 to 15 minutes.
Farrukh Abbas, MBBS
Fellow-in-Training
Asthma and COPD Section
Go TEAM! Shared decision-making tool for patient-clinician collaboration in severe asthma
Shared decision-making is associated with improved medication adherence in adults (Wilson, et al. Am J Respir Crit Care Med. 2010;181[6]:566-77) and quality of life and asthma control in children (Taylor, et al. J Asthma. 2018;55[6]:675-83). The Global Initiative for Asthma committee recommends a patient-clinician partnership. Activated and engaged patients play a major role in their asthma management (https://ginasthma.org/gina-reports). Shared decision-making discussions should include potential benefits and harms of the therapeutic options, patient’s values and lifestyle preferences, and addressing concerns.
The CHEST Foundation, the Allergy and Asthma Network, and the American College of Allergy, Asthma, and Immunology developed an online shared decision- making tool for severe asthma (https://asthma.chestnet.org/sdm-tool).
This tool utilizes patient’s values, specifics about triggers, asthma control, medication side effects, and lifestyle preferences to identify personalized management options. The tool provides information about recommended therapeutic options in simple terms, including potential benefits, possible side effects, expected treatment frequency and duration, and financial aid information. The treatment options currently explained in this tool include anti-immunoglobulin E, anti-interleukin-5, anti-interleukin-4/13, bronchial thermoplasty, long-acting muscarinic antagonist, macrolides, oral corticosteroids, and standard of care.
As a team, the patient and the health care professional can use this tool during office visits to help guide management. Figure 1 shows a suggested workflow to utilize the tool in clinical practice.
Potential barriers include excess time and increased human resources. Barrier mitigation may include reviewing the tool and reconciling the medications before the clinician enters the room. With these interventions, many clinician encounters may be completed in 10 to 15 minutes.
Farrukh Abbas, MBBS
Fellow-in-Training
Asthma and COPD Section
Go TEAM! Shared decision-making tool for patient-clinician collaboration in severe asthma
Shared decision-making is associated with improved medication adherence in adults (Wilson, et al. Am J Respir Crit Care Med. 2010;181[6]:566-77) and quality of life and asthma control in children (Taylor, et al. J Asthma. 2018;55[6]:675-83). The Global Initiative for Asthma committee recommends a patient-clinician partnership. Activated and engaged patients play a major role in their asthma management (https://ginasthma.org/gina-reports). Shared decision-making discussions should include potential benefits and harms of the therapeutic options, patient’s values and lifestyle preferences, and addressing concerns.
The CHEST Foundation, the Allergy and Asthma Network, and the American College of Allergy, Asthma, and Immunology developed an online shared decision- making tool for severe asthma (https://asthma.chestnet.org/sdm-tool).
This tool utilizes patient’s values, specifics about triggers, asthma control, medication side effects, and lifestyle preferences to identify personalized management options. The tool provides information about recommended therapeutic options in simple terms, including potential benefits, possible side effects, expected treatment frequency and duration, and financial aid information. The treatment options currently explained in this tool include anti-immunoglobulin E, anti-interleukin-5, anti-interleukin-4/13, bronchial thermoplasty, long-acting muscarinic antagonist, macrolides, oral corticosteroids, and standard of care.
As a team, the patient and the health care professional can use this tool during office visits to help guide management. Figure 1 shows a suggested workflow to utilize the tool in clinical practice.
Potential barriers include excess time and increased human resources. Barrier mitigation may include reviewing the tool and reconciling the medications before the clinician enters the room. With these interventions, many clinician encounters may be completed in 10 to 15 minutes.
Farrukh Abbas, MBBS
Fellow-in-Training
This month in the journal CHEST®
Dupilumab Reduces Oral Corticosteroid Use in Patients With Corticosteroid-Dependent Severe Asthma. By Lawrence D. Sher, MD, et al.
Carriage and Transmission of Macrolide Resistance Genes in Patients With Chronic Respiratory Conditions and Their Close Contacts. By Yiming Wang, MSc, et al.
An Evaluation of Factors That Influence Referral to Pulmonary Rehabilitation Programs Among People With COPD. By Sarah Hug, BSc, et al.
Prevalence and Outcomes of Previously Healthy Adults Among Patients Hospitalized With Community-Onset Sepsis. By Mohammad Alrawashdeh, PhD, MSN, et al.
Screening Strategies for Pulmonary Hypertension in Patients With Interstitial Lung Disease: A Multidisciplinary Delphi Study. By Franck F. Rahaghi, MD, et al.
Race- and Ethnicity-Based Spirometry Reference Equations: Are They Accurate for Genetically Admixed Children? By Jonathan Witonsky, MD, et al.
No VTE Recurrence After 1-Year Follow Up of Hospitalized Patients With COVID-19 and a VTE Event: A Prospective Study. By Maxime Delrue, MD, PhD, et al.
Patient Perspectives on Longitudinal Adherence to Lung Cancer Screening. By Anna Holman, BS, et al.
Dupilumab Reduces Oral Corticosteroid Use in Patients With Corticosteroid-Dependent Severe Asthma. By Lawrence D. Sher, MD, et al.
Carriage and Transmission of Macrolide Resistance Genes in Patients With Chronic Respiratory Conditions and Their Close Contacts. By Yiming Wang, MSc, et al.
An Evaluation of Factors That Influence Referral to Pulmonary Rehabilitation Programs Among People With COPD. By Sarah Hug, BSc, et al.
Prevalence and Outcomes of Previously Healthy Adults Among Patients Hospitalized With Community-Onset Sepsis. By Mohammad Alrawashdeh, PhD, MSN, et al.
Screening Strategies for Pulmonary Hypertension in Patients With Interstitial Lung Disease: A Multidisciplinary Delphi Study. By Franck F. Rahaghi, MD, et al.
Race- and Ethnicity-Based Spirometry Reference Equations: Are They Accurate for Genetically Admixed Children? By Jonathan Witonsky, MD, et al.
No VTE Recurrence After 1-Year Follow Up of Hospitalized Patients With COVID-19 and a VTE Event: A Prospective Study. By Maxime Delrue, MD, PhD, et al.
Patient Perspectives on Longitudinal Adherence to Lung Cancer Screening. By Anna Holman, BS, et al.
Dupilumab Reduces Oral Corticosteroid Use in Patients With Corticosteroid-Dependent Severe Asthma. By Lawrence D. Sher, MD, et al.
Carriage and Transmission of Macrolide Resistance Genes in Patients With Chronic Respiratory Conditions and Their Close Contacts. By Yiming Wang, MSc, et al.
An Evaluation of Factors That Influence Referral to Pulmonary Rehabilitation Programs Among People With COPD. By Sarah Hug, BSc, et al.
Prevalence and Outcomes of Previously Healthy Adults Among Patients Hospitalized With Community-Onset Sepsis. By Mohammad Alrawashdeh, PhD, MSN, et al.
Screening Strategies for Pulmonary Hypertension in Patients With Interstitial Lung Disease: A Multidisciplinary Delphi Study. By Franck F. Rahaghi, MD, et al.
Race- and Ethnicity-Based Spirometry Reference Equations: Are They Accurate for Genetically Admixed Children? By Jonathan Witonsky, MD, et al.
No VTE Recurrence After 1-Year Follow Up of Hospitalized Patients With COVID-19 and a VTE Event: A Prospective Study. By Maxime Delrue, MD, PhD, et al.
Patient Perspectives on Longitudinal Adherence to Lung Cancer Screening. By Anna Holman, BS, et al.
Starting CHEST 2022 off with a step kick
, with a bang—or, more accurately, with a step kick, swivel, and stomp—at the Wildhorse Saloon.
The Wildhorse is famous for hosting daily line dancing lessons on the largest dance floor in the downtown area and for having a menu full of Nashville favorites, including Nashville hot chicken and a hearty selection of entrees (as well as a decadent bananas foster) with a “Jack Daniels” single barrel whiskey glaze.
The opening reception offers attendees the opportunity to relax and reconnect with their peers from across the fields of pulmonary, critical care, and sleep medicine before the jam-packed schedule of more than 300 educational sessions starts the following day.
But the fun doesn’t stop there. Attendees interested in exploring the city after hours have a host of options, from world-class music venues to iconic distilleries and restaurants. The Music City Center, where CHEST 2022 will be held, is located in the SoBro neighborhood of Nashville, not far from the Arts District, Downtown, and Music Row.
According to Nashville local and CHEST member Meredith Pugh, MD, MSCI, “it goes without saying that we have the best music scene in the country, but it’s a great place for outdoor activities and food.”
For those who don’t get their fill at the Wildhorse, Dr. Pugh recommends attendees check out the Assembly Food Hall (.3 miles from the convention center) to try the city’s famous Nashville Hot Chicken and a variety of other local options. And, don’t miss the many excellent options for BBQ. Fellow Nashville transplant and CHEST member Todd Rice, MD, FCCP, suggests Martin’s Bar-B-Que Joint and Jack’s Bar-B-Que—both within walking distance of the Music City Center—as well as other local options.
To learn more about everything Nashville has to offer, and get more recommendations from Drs. Rice and Pugh, check out the latest CHEST 2022 blog on chestnet.org
, with a bang—or, more accurately, with a step kick, swivel, and stomp—at the Wildhorse Saloon.
The Wildhorse is famous for hosting daily line dancing lessons on the largest dance floor in the downtown area and for having a menu full of Nashville favorites, including Nashville hot chicken and a hearty selection of entrees (as well as a decadent bananas foster) with a “Jack Daniels” single barrel whiskey glaze.
The opening reception offers attendees the opportunity to relax and reconnect with their peers from across the fields of pulmonary, critical care, and sleep medicine before the jam-packed schedule of more than 300 educational sessions starts the following day.
But the fun doesn’t stop there. Attendees interested in exploring the city after hours have a host of options, from world-class music venues to iconic distilleries and restaurants. The Music City Center, where CHEST 2022 will be held, is located in the SoBro neighborhood of Nashville, not far from the Arts District, Downtown, and Music Row.
According to Nashville local and CHEST member Meredith Pugh, MD, MSCI, “it goes without saying that we have the best music scene in the country, but it’s a great place for outdoor activities and food.”
For those who don’t get their fill at the Wildhorse, Dr. Pugh recommends attendees check out the Assembly Food Hall (.3 miles from the convention center) to try the city’s famous Nashville Hot Chicken and a variety of other local options. And, don’t miss the many excellent options for BBQ. Fellow Nashville transplant and CHEST member Todd Rice, MD, FCCP, suggests Martin’s Bar-B-Que Joint and Jack’s Bar-B-Que—both within walking distance of the Music City Center—as well as other local options.
To learn more about everything Nashville has to offer, and get more recommendations from Drs. Rice and Pugh, check out the latest CHEST 2022 blog on chestnet.org
, with a bang—or, more accurately, with a step kick, swivel, and stomp—at the Wildhorse Saloon.
The Wildhorse is famous for hosting daily line dancing lessons on the largest dance floor in the downtown area and for having a menu full of Nashville favorites, including Nashville hot chicken and a hearty selection of entrees (as well as a decadent bananas foster) with a “Jack Daniels” single barrel whiskey glaze.
The opening reception offers attendees the opportunity to relax and reconnect with their peers from across the fields of pulmonary, critical care, and sleep medicine before the jam-packed schedule of more than 300 educational sessions starts the following day.
But the fun doesn’t stop there. Attendees interested in exploring the city after hours have a host of options, from world-class music venues to iconic distilleries and restaurants. The Music City Center, where CHEST 2022 will be held, is located in the SoBro neighborhood of Nashville, not far from the Arts District, Downtown, and Music Row.
According to Nashville local and CHEST member Meredith Pugh, MD, MSCI, “it goes without saying that we have the best music scene in the country, but it’s a great place for outdoor activities and food.”
For those who don’t get their fill at the Wildhorse, Dr. Pugh recommends attendees check out the Assembly Food Hall (.3 miles from the convention center) to try the city’s famous Nashville Hot Chicken and a variety of other local options. And, don’t miss the many excellent options for BBQ. Fellow Nashville transplant and CHEST member Todd Rice, MD, FCCP, suggests Martin’s Bar-B-Que Joint and Jack’s Bar-B-Que—both within walking distance of the Music City Center—as well as other local options.
To learn more about everything Nashville has to offer, and get more recommendations from Drs. Rice and Pugh, check out the latest CHEST 2022 blog on chestnet.org
Beyond CPAP: Looking to alternative treatments for obstructive sleep apnea
Overview of the problem
Obstructive sleep apnea (OSA) is an extraordinarily common condition impacting nearly 1 billion individuals globally (Benjafield AV, et al. Lancet Respir Med. 2019;7[8]:687). For the past 40 years, the mainstay of treatment has been continuous positive airway pressure (CPAP). However, CPAP usage is highly variable, and not all sleep apnea is created the same with respect to underlying mechanism or patient symptoms. Currently, there is a global CPAP shortage, which has expedited the need for alternative therapies in OSA (Owens RL, et al. Am J Respir Crit Care Med. 2021;204[8]:887).
Characterizing OSA
First, it is important to understand that sleep apnea emerges for multiple reasons. Some examples include: an excessively collapsible airway, insufficient upper airway reflexes, low arousal threshold (awakening easily to ventilatory disturbance), as well as an unstable chemoreflex system. This list is not comprehensive. However, we believe that the future of OSA management will be targeted therapy for individual OSA traits.
Notably, the patient experience of OSA is also highly variable. Some individuals are excessively sleepy. Some individuals experience OSA as insomnia. Other patients are asymptomatic, but present to the sleep clinic at the behest of a disgruntled bed partner. These individual factors should all be kept in mind when deciding when and how to treat sleep apnea.
OSA scoring – past, present, and future
The traditional method for scoring sleep apnea severity is the apnea-hypopnea index (AHI), with mild, moderate, and severe OSA being stratified by the number of events per hour. This metric has shaped many of the modern sleep practices and consensus recommendations but is simply not sophisticated enough to capture the nuance of how or why an individual’s sleep is disrupted from flow-limited breathing. As such, there has been a push in recent times to tailor treatment for OSA to an individual’s physiology. Examples of alternative metrics which quantify sleep apnea traits include the apnea-hypopnea event duration, the sleep apnea-specific hypoxic burden (area under the SpO2 curve for flow-limited events), as well as the arousal intensity from sleep in the setting of flow-limited breathing. There are numerous other metrics that have been proposed but are beyond the scope of this review (Malhotra A, et al. Sleep. 2021;44[7]:zsab030).
What therapies are available and how can we individualize them to our patients?
As noted, CPAP has been the gold-standard for OSA treatment for 40 years but is not always accepted or tolerated (Malhotra A, et al. Chest. 2018;153[4]:843). Broad categories of OSA management are presented as follows.
Surgery for OSA
Upper airway surgery is effective for pediatric OSA treatment, where enlarged tonsils are often the culprit for flow-limited breathing in sleep. For adults, however, there is no one best surgery or surgical candidate. For instance, surgery can be used to improve CPAP tolerance or as a primary OSA treatment. Many individuals with sinus disease may require sinus surgery or septoplasty to improve CPAP tolerability by creating more space for airflow through the nasopharynx. Retrognathic individuals, on the other hand, may benefit from maxillomandibular advancement. Others may benefit from genioglossus advancement or hyoid suspension. The characteristics of the soft palate can be predictive of surgical success with respect to uvulopalatopharyngoplasty (UPPP), with longer uvulas and redundant soft palate tissue being attractive surgical targets. Obviously, this list is far from comprehensive, but Friedman tongue position, tonsil size, and body mass index also appear to be important in predicting surgical success (MacKay S, et al. JAMA. 2020;324[12]:1168).
Hypoglossal nerve stimulation is one surgical treatment option for patients with moderate-severe OSA who are unable or unwilling to use CPAP therapy, have a BMI <32-35 kg/m2 (center-dependent), no concentric velopharyngeal collapse on drug-induced sleep endoscopy, and fewer than 25% central/mixed apneas on their sleep study. Areas for further study are whether unilateral or bilateral stimulation are most effective, as well as which of the sleep apnea traits are most predictive of a treatment response (Strohl MM, et al. Curr Sleep Med Rep. 2017;3[3]:133).
Notably, surgical techniques are highly variable, and there are individual patient characteristics, such as lower loop gain (more stable ventilatory control), which may have a greater likelihood of successful upper airway surgery. This is likely because making the upper airway more patent allows for ventilatory overshoots and thereby airway collapse and cyclic, unstable breathing in those with an unstable ventilatory control system. Trials with prespecified surgical techniques based on individual traits are welcome. Additionally, the metrics of a successful surgical treatment for OSA, much like the AHI, are in need of evolution. The Sher criteria, for instance (50% AHI reduction to an AHI < 20/h), are arbitrary, and their clinical utility is unclear.
Oral appliances
Oral appliances fall into two broad categories – tongue-retaining devices and mandibular advancement splints (MAS). Of the two, MAS are much more commonly prescribed. Of the MAS devices, custom made devices by an American Academy of Dental Sleep Medicine (AADSM)–trained dentist are recommended over noncustom MAS in the treatment of primary snoring or OSA for those unwilling or unable to wear CPAP. Notably, the 2015 American Academy of Sleep Medicine (AASM) and AADSM shared guidelines were unable to make OSA treatment recommendations based on severity of disease as stratified by the AHI due to the limited quality of evidence. These devices are broadly thought to work by protruding the mandible/tongue and, in-turn, advancing multiple soft tissue components of the velopharynx. Relatively recent work suggests that the following OSA traits are associated with MAS efficacy: lower loop gain, higher arousal threshold, lower ventilatory response to arousal, moderate pharyngeal collapsibility, and weaker upper airway dilator muscle compensation. However, in order for these devices to be successful, close follow-up for titration with a AADSM-certified dentist, as well as a follow-up efficacy sleep study, are recommended. Adherence for custom device use appears to be about 70% use greater than 4 hours per night, with 35% to 40% of those prescribed a device achieving an AHI less than 5/h. Over the counter devices are not routinely recommended, though some practices do use these devices as a trial to see if patients may tolerate custom made devices (Ramar K, et al. J Clin Sleep Med. 2015;11[7]:773).
Upper airway training
Upper airway training has been shown possibly to be effective in treating OSA, though the ideal endotype is still being established. Upper airway training has taken many forms, from woodwind instrument playing, to nocturnal electrical stimulation of the tongue, and, more recently, daytime awake transoral neuromuscular stimulation. These interventions appear to be effective for mild sleep apnea and snoring, but the best training regimen has yet to be established. Equally, as with other routine exercise, there appears to be a “use it or lose it” component, and the ideal maintenance regimen for each of these therapies is yet to be determined.
Weight loss and bariatric surgery
Obesity is a common, reversible risk factor for OSA. However, not all obese individuals develop OSA (typically those with robust upper airway reflexes). Improvements in weight appear to correlate with reductions in tongue fat, which correlate to AHI reduction. Weight loss also creates lower CPAP requirements for many individuals, conceivably improving tolerability. Ongoing work is seeking to understand whether there are changes in upper airway muscle recruitability as well as other change in endotype traits following weight loss surgery.
Pharmacotherapy for OSA
There is a great deal of promise in tailoring pharmacotherapy to individual sleep traits. Acetazolamide, for instance, results in improvements an AHI for both obstructive and central sleep apnea through changes in chemosensitivity and is generally well-tolerated (Schmickl CN, et al. Physiol Rep. 2021;9[20]:e15071). Eszopiclone has been used to raise the arousal threshold for those who awaken from breathing events too easily. With added time, individuals with a low arousal threshold can more effectively recruit upper airway dilator muscles without waking up. Pharmacotherapy to improve upper airway recruitability with combination noradrenergic stimulation and antimuscarinic activity has limited data thus far but may be a useful part of the sleep armamentarium moving forward.
Summary
OSA is a public health priority, and the current global CPAP shortage emphasizes the need for alternative OSA therapies. The ideal therapy for a given patient requires a careful consideration of their individual traits and will be much more refined when endotyping is available in a routine clinical setting. Individualized sleep apnea treatment is the future of sleep medicine and a one-size fits all approach no longer meets the needs of our patients given the current state of sleep medicine knowledge.
Dr. Nokes, Dr. Schmickl, and Dr. Malhotra are with the University of California, San Diego, Division of Pulmonary, Critical Care, and Sleep Medicine, La, Jolla, CA. Dr. Nokes also is with the Veterans Affairs San Diego Healthcare System, sleep section, San Diego, CA. Dr. Vahabzadeh-Hagh is with the University of California, San Diego, Department of Otolaryngology, San Diego, CA.
Overview of the problem
Obstructive sleep apnea (OSA) is an extraordinarily common condition impacting nearly 1 billion individuals globally (Benjafield AV, et al. Lancet Respir Med. 2019;7[8]:687). For the past 40 years, the mainstay of treatment has been continuous positive airway pressure (CPAP). However, CPAP usage is highly variable, and not all sleep apnea is created the same with respect to underlying mechanism or patient symptoms. Currently, there is a global CPAP shortage, which has expedited the need for alternative therapies in OSA (Owens RL, et al. Am J Respir Crit Care Med. 2021;204[8]:887).
Characterizing OSA
First, it is important to understand that sleep apnea emerges for multiple reasons. Some examples include: an excessively collapsible airway, insufficient upper airway reflexes, low arousal threshold (awakening easily to ventilatory disturbance), as well as an unstable chemoreflex system. This list is not comprehensive. However, we believe that the future of OSA management will be targeted therapy for individual OSA traits.
Notably, the patient experience of OSA is also highly variable. Some individuals are excessively sleepy. Some individuals experience OSA as insomnia. Other patients are asymptomatic, but present to the sleep clinic at the behest of a disgruntled bed partner. These individual factors should all be kept in mind when deciding when and how to treat sleep apnea.
OSA scoring – past, present, and future
The traditional method for scoring sleep apnea severity is the apnea-hypopnea index (AHI), with mild, moderate, and severe OSA being stratified by the number of events per hour. This metric has shaped many of the modern sleep practices and consensus recommendations but is simply not sophisticated enough to capture the nuance of how or why an individual’s sleep is disrupted from flow-limited breathing. As such, there has been a push in recent times to tailor treatment for OSA to an individual’s physiology. Examples of alternative metrics which quantify sleep apnea traits include the apnea-hypopnea event duration, the sleep apnea-specific hypoxic burden (area under the SpO2 curve for flow-limited events), as well as the arousal intensity from sleep in the setting of flow-limited breathing. There are numerous other metrics that have been proposed but are beyond the scope of this review (Malhotra A, et al. Sleep. 2021;44[7]:zsab030).
What therapies are available and how can we individualize them to our patients?
As noted, CPAP has been the gold-standard for OSA treatment for 40 years but is not always accepted or tolerated (Malhotra A, et al. Chest. 2018;153[4]:843). Broad categories of OSA management are presented as follows.
Surgery for OSA
Upper airway surgery is effective for pediatric OSA treatment, where enlarged tonsils are often the culprit for flow-limited breathing in sleep. For adults, however, there is no one best surgery or surgical candidate. For instance, surgery can be used to improve CPAP tolerance or as a primary OSA treatment. Many individuals with sinus disease may require sinus surgery or septoplasty to improve CPAP tolerability by creating more space for airflow through the nasopharynx. Retrognathic individuals, on the other hand, may benefit from maxillomandibular advancement. Others may benefit from genioglossus advancement or hyoid suspension. The characteristics of the soft palate can be predictive of surgical success with respect to uvulopalatopharyngoplasty (UPPP), with longer uvulas and redundant soft palate tissue being attractive surgical targets. Obviously, this list is far from comprehensive, but Friedman tongue position, tonsil size, and body mass index also appear to be important in predicting surgical success (MacKay S, et al. JAMA. 2020;324[12]:1168).
Hypoglossal nerve stimulation is one surgical treatment option for patients with moderate-severe OSA who are unable or unwilling to use CPAP therapy, have a BMI <32-35 kg/m2 (center-dependent), no concentric velopharyngeal collapse on drug-induced sleep endoscopy, and fewer than 25% central/mixed apneas on their sleep study. Areas for further study are whether unilateral or bilateral stimulation are most effective, as well as which of the sleep apnea traits are most predictive of a treatment response (Strohl MM, et al. Curr Sleep Med Rep. 2017;3[3]:133).
Notably, surgical techniques are highly variable, and there are individual patient characteristics, such as lower loop gain (more stable ventilatory control), which may have a greater likelihood of successful upper airway surgery. This is likely because making the upper airway more patent allows for ventilatory overshoots and thereby airway collapse and cyclic, unstable breathing in those with an unstable ventilatory control system. Trials with prespecified surgical techniques based on individual traits are welcome. Additionally, the metrics of a successful surgical treatment for OSA, much like the AHI, are in need of evolution. The Sher criteria, for instance (50% AHI reduction to an AHI < 20/h), are arbitrary, and their clinical utility is unclear.
Oral appliances
Oral appliances fall into two broad categories – tongue-retaining devices and mandibular advancement splints (MAS). Of the two, MAS are much more commonly prescribed. Of the MAS devices, custom made devices by an American Academy of Dental Sleep Medicine (AADSM)–trained dentist are recommended over noncustom MAS in the treatment of primary snoring or OSA for those unwilling or unable to wear CPAP. Notably, the 2015 American Academy of Sleep Medicine (AASM) and AADSM shared guidelines were unable to make OSA treatment recommendations based on severity of disease as stratified by the AHI due to the limited quality of evidence. These devices are broadly thought to work by protruding the mandible/tongue and, in-turn, advancing multiple soft tissue components of the velopharynx. Relatively recent work suggests that the following OSA traits are associated with MAS efficacy: lower loop gain, higher arousal threshold, lower ventilatory response to arousal, moderate pharyngeal collapsibility, and weaker upper airway dilator muscle compensation. However, in order for these devices to be successful, close follow-up for titration with a AADSM-certified dentist, as well as a follow-up efficacy sleep study, are recommended. Adherence for custom device use appears to be about 70% use greater than 4 hours per night, with 35% to 40% of those prescribed a device achieving an AHI less than 5/h. Over the counter devices are not routinely recommended, though some practices do use these devices as a trial to see if patients may tolerate custom made devices (Ramar K, et al. J Clin Sleep Med. 2015;11[7]:773).
Upper airway training
Upper airway training has been shown possibly to be effective in treating OSA, though the ideal endotype is still being established. Upper airway training has taken many forms, from woodwind instrument playing, to nocturnal electrical stimulation of the tongue, and, more recently, daytime awake transoral neuromuscular stimulation. These interventions appear to be effective for mild sleep apnea and snoring, but the best training regimen has yet to be established. Equally, as with other routine exercise, there appears to be a “use it or lose it” component, and the ideal maintenance regimen for each of these therapies is yet to be determined.
Weight loss and bariatric surgery
Obesity is a common, reversible risk factor for OSA. However, not all obese individuals develop OSA (typically those with robust upper airway reflexes). Improvements in weight appear to correlate with reductions in tongue fat, which correlate to AHI reduction. Weight loss also creates lower CPAP requirements for many individuals, conceivably improving tolerability. Ongoing work is seeking to understand whether there are changes in upper airway muscle recruitability as well as other change in endotype traits following weight loss surgery.
Pharmacotherapy for OSA
There is a great deal of promise in tailoring pharmacotherapy to individual sleep traits. Acetazolamide, for instance, results in improvements an AHI for both obstructive and central sleep apnea through changes in chemosensitivity and is generally well-tolerated (Schmickl CN, et al. Physiol Rep. 2021;9[20]:e15071). Eszopiclone has been used to raise the arousal threshold for those who awaken from breathing events too easily. With added time, individuals with a low arousal threshold can more effectively recruit upper airway dilator muscles without waking up. Pharmacotherapy to improve upper airway recruitability with combination noradrenergic stimulation and antimuscarinic activity has limited data thus far but may be a useful part of the sleep armamentarium moving forward.
Summary
OSA is a public health priority, and the current global CPAP shortage emphasizes the need for alternative OSA therapies. The ideal therapy for a given patient requires a careful consideration of their individual traits and will be much more refined when endotyping is available in a routine clinical setting. Individualized sleep apnea treatment is the future of sleep medicine and a one-size fits all approach no longer meets the needs of our patients given the current state of sleep medicine knowledge.
Dr. Nokes, Dr. Schmickl, and Dr. Malhotra are with the University of California, San Diego, Division of Pulmonary, Critical Care, and Sleep Medicine, La, Jolla, CA. Dr. Nokes also is with the Veterans Affairs San Diego Healthcare System, sleep section, San Diego, CA. Dr. Vahabzadeh-Hagh is with the University of California, San Diego, Department of Otolaryngology, San Diego, CA.
Overview of the problem
Obstructive sleep apnea (OSA) is an extraordinarily common condition impacting nearly 1 billion individuals globally (Benjafield AV, et al. Lancet Respir Med. 2019;7[8]:687). For the past 40 years, the mainstay of treatment has been continuous positive airway pressure (CPAP). However, CPAP usage is highly variable, and not all sleep apnea is created the same with respect to underlying mechanism or patient symptoms. Currently, there is a global CPAP shortage, which has expedited the need for alternative therapies in OSA (Owens RL, et al. Am J Respir Crit Care Med. 2021;204[8]:887).
Characterizing OSA
First, it is important to understand that sleep apnea emerges for multiple reasons. Some examples include: an excessively collapsible airway, insufficient upper airway reflexes, low arousal threshold (awakening easily to ventilatory disturbance), as well as an unstable chemoreflex system. This list is not comprehensive. However, we believe that the future of OSA management will be targeted therapy for individual OSA traits.
Notably, the patient experience of OSA is also highly variable. Some individuals are excessively sleepy. Some individuals experience OSA as insomnia. Other patients are asymptomatic, but present to the sleep clinic at the behest of a disgruntled bed partner. These individual factors should all be kept in mind when deciding when and how to treat sleep apnea.
OSA scoring – past, present, and future
The traditional method for scoring sleep apnea severity is the apnea-hypopnea index (AHI), with mild, moderate, and severe OSA being stratified by the number of events per hour. This metric has shaped many of the modern sleep practices and consensus recommendations but is simply not sophisticated enough to capture the nuance of how or why an individual’s sleep is disrupted from flow-limited breathing. As such, there has been a push in recent times to tailor treatment for OSA to an individual’s physiology. Examples of alternative metrics which quantify sleep apnea traits include the apnea-hypopnea event duration, the sleep apnea-specific hypoxic burden (area under the SpO2 curve for flow-limited events), as well as the arousal intensity from sleep in the setting of flow-limited breathing. There are numerous other metrics that have been proposed but are beyond the scope of this review (Malhotra A, et al. Sleep. 2021;44[7]:zsab030).
What therapies are available and how can we individualize them to our patients?
As noted, CPAP has been the gold-standard for OSA treatment for 40 years but is not always accepted or tolerated (Malhotra A, et al. Chest. 2018;153[4]:843). Broad categories of OSA management are presented as follows.
Surgery for OSA
Upper airway surgery is effective for pediatric OSA treatment, where enlarged tonsils are often the culprit for flow-limited breathing in sleep. For adults, however, there is no one best surgery or surgical candidate. For instance, surgery can be used to improve CPAP tolerance or as a primary OSA treatment. Many individuals with sinus disease may require sinus surgery or septoplasty to improve CPAP tolerability by creating more space for airflow through the nasopharynx. Retrognathic individuals, on the other hand, may benefit from maxillomandibular advancement. Others may benefit from genioglossus advancement or hyoid suspension. The characteristics of the soft palate can be predictive of surgical success with respect to uvulopalatopharyngoplasty (UPPP), with longer uvulas and redundant soft palate tissue being attractive surgical targets. Obviously, this list is far from comprehensive, but Friedman tongue position, tonsil size, and body mass index also appear to be important in predicting surgical success (MacKay S, et al. JAMA. 2020;324[12]:1168).
Hypoglossal nerve stimulation is one surgical treatment option for patients with moderate-severe OSA who are unable or unwilling to use CPAP therapy, have a BMI <32-35 kg/m2 (center-dependent), no concentric velopharyngeal collapse on drug-induced sleep endoscopy, and fewer than 25% central/mixed apneas on their sleep study. Areas for further study are whether unilateral or bilateral stimulation are most effective, as well as which of the sleep apnea traits are most predictive of a treatment response (Strohl MM, et al. Curr Sleep Med Rep. 2017;3[3]:133).
Notably, surgical techniques are highly variable, and there are individual patient characteristics, such as lower loop gain (more stable ventilatory control), which may have a greater likelihood of successful upper airway surgery. This is likely because making the upper airway more patent allows for ventilatory overshoots and thereby airway collapse and cyclic, unstable breathing in those with an unstable ventilatory control system. Trials with prespecified surgical techniques based on individual traits are welcome. Additionally, the metrics of a successful surgical treatment for OSA, much like the AHI, are in need of evolution. The Sher criteria, for instance (50% AHI reduction to an AHI < 20/h), are arbitrary, and their clinical utility is unclear.
Oral appliances
Oral appliances fall into two broad categories – tongue-retaining devices and mandibular advancement splints (MAS). Of the two, MAS are much more commonly prescribed. Of the MAS devices, custom made devices by an American Academy of Dental Sleep Medicine (AADSM)–trained dentist are recommended over noncustom MAS in the treatment of primary snoring or OSA for those unwilling or unable to wear CPAP. Notably, the 2015 American Academy of Sleep Medicine (AASM) and AADSM shared guidelines were unable to make OSA treatment recommendations based on severity of disease as stratified by the AHI due to the limited quality of evidence. These devices are broadly thought to work by protruding the mandible/tongue and, in-turn, advancing multiple soft tissue components of the velopharynx. Relatively recent work suggests that the following OSA traits are associated with MAS efficacy: lower loop gain, higher arousal threshold, lower ventilatory response to arousal, moderate pharyngeal collapsibility, and weaker upper airway dilator muscle compensation. However, in order for these devices to be successful, close follow-up for titration with a AADSM-certified dentist, as well as a follow-up efficacy sleep study, are recommended. Adherence for custom device use appears to be about 70% use greater than 4 hours per night, with 35% to 40% of those prescribed a device achieving an AHI less than 5/h. Over the counter devices are not routinely recommended, though some practices do use these devices as a trial to see if patients may tolerate custom made devices (Ramar K, et al. J Clin Sleep Med. 2015;11[7]:773).
Upper airway training
Upper airway training has been shown possibly to be effective in treating OSA, though the ideal endotype is still being established. Upper airway training has taken many forms, from woodwind instrument playing, to nocturnal electrical stimulation of the tongue, and, more recently, daytime awake transoral neuromuscular stimulation. These interventions appear to be effective for mild sleep apnea and snoring, but the best training regimen has yet to be established. Equally, as with other routine exercise, there appears to be a “use it or lose it” component, and the ideal maintenance regimen for each of these therapies is yet to be determined.
Weight loss and bariatric surgery
Obesity is a common, reversible risk factor for OSA. However, not all obese individuals develop OSA (typically those with robust upper airway reflexes). Improvements in weight appear to correlate with reductions in tongue fat, which correlate to AHI reduction. Weight loss also creates lower CPAP requirements for many individuals, conceivably improving tolerability. Ongoing work is seeking to understand whether there are changes in upper airway muscle recruitability as well as other change in endotype traits following weight loss surgery.
Pharmacotherapy for OSA
There is a great deal of promise in tailoring pharmacotherapy to individual sleep traits. Acetazolamide, for instance, results in improvements an AHI for both obstructive and central sleep apnea through changes in chemosensitivity and is generally well-tolerated (Schmickl CN, et al. Physiol Rep. 2021;9[20]:e15071). Eszopiclone has been used to raise the arousal threshold for those who awaken from breathing events too easily. With added time, individuals with a low arousal threshold can more effectively recruit upper airway dilator muscles without waking up. Pharmacotherapy to improve upper airway recruitability with combination noradrenergic stimulation and antimuscarinic activity has limited data thus far but may be a useful part of the sleep armamentarium moving forward.
Summary
OSA is a public health priority, and the current global CPAP shortage emphasizes the need for alternative OSA therapies. The ideal therapy for a given patient requires a careful consideration of their individual traits and will be much more refined when endotyping is available in a routine clinical setting. Individualized sleep apnea treatment is the future of sleep medicine and a one-size fits all approach no longer meets the needs of our patients given the current state of sleep medicine knowledge.
Dr. Nokes, Dr. Schmickl, and Dr. Malhotra are with the University of California, San Diego, Division of Pulmonary, Critical Care, and Sleep Medicine, La, Jolla, CA. Dr. Nokes also is with the Veterans Affairs San Diego Healthcare System, sleep section, San Diego, CA. Dr. Vahabzadeh-Hagh is with the University of California, San Diego, Department of Otolaryngology, San Diego, CA.
From the President: A day in the life
For those of you in the Northern Hemisphere, like me, spring has transitioned into summer, allowing us all to spend more time outdoors, gathering again with family, friends, and colleagues. And, while people are always happy to hear about what’s going on with the family, or how things are going at Emory, the most common question I get is “So what’s it like to be President of CHEST?” Now that I’ve been on the job for 6 months, I thought it was well enough time to pull back the curtain on the role for all of you out in CHEST-land who might be interested, as well. For the purposes of this column, I’ll be incorporating things that occurred over the past week.
As I’ve previously reported, the most important decisions that relate to CHEST strategy are made by the Board of Regents. While I do have the privilege of organizing and running Board meetings, most presidential duties between these meetings focus on communication: with our members, our leaders, and other organizations. One of the best parts of the job is the opportunity to interact with our members; between the [email protected] account and my own, I receive a couple of emails each day with questions about navigating CHEST, or ideas about ways that things might be better accomplished. With our recent Network and section reorganization, many of those questions have focused on leadership opportunities, inquiring about whether the writer should apply, or asking for information about the qualities that might increase the odds of earning a position. My answer is almost always the same: go ahead and throw your name in the hat; for most members, the sections are the first place to start the journey in CHEST leadership. And I’m pleased to say that I’ve had the chance to see some of the members who’ve reached out to me in the past selected for the positions to which they’d applied (in full disclosure, I have little role in selecting leadership positions; Network and section positions are chosen by current members of those Networks and sections). I look forward to watching their progress in our organizational leadership.
While CHEST CEO Robert Musacchio and I communicate almost every day, Wednesday is our weekly meeting during which we review progress on our organizational goals, the status of ongoing projects, and concerns from our membership and leadership. I also have the pleasure of meeting with my co-Presidents every other week; though Jack, Doreen, and Steve have always been happy to offer their counsel on very short notice, this semimonthly meeting helps to provide continuity in leadership, as well as a more formal opportunity for me to meet with trusted advisors to get a sounding board on active issues that affect CHEST. And, this gets to the other main job of CHEST President, which is to facilitate the making of important decisions on behalf of the College. I receive sporadic emails from CHEST staff as we are approached by other organizations or international partners for input on or approval for statements that they wish to make. In the case where the topic is clearly in the CHEST wheelhouse and the statement is consistent with our organizational goals, I can unilaterally sign off; a common example of something that fits in this category is content related to tobacco cessation. In the more frequent situation where the statement for approval is a bit more complex, I will usually refer the request to one of our committee, Network, or section chairs for consideration. Since the turnaround time on these requests is usually pretty short, I may ask them to advise me on their own, although they sometimes opt to run things by their own membership for further input or to achieve consensus.
The CHEST President also serves as ambassador to other organizations; this week, I had the pleasure of participating in a meeting with the American Board of Internal Medicine and a number of medical specialty leaders focused on how professional societies can help to mitigate the spread of medical misinformation. I also interfaced with several of our international partners in the pulmonary space, as they plan their own international meetings, to see how CHEST can contribute to the success of those endeavors by contributing content, speakers, or both. At the time of this writing, the CHEST Congress in Bologna, Italy, is right around the corner, and so I also spent time working with our Italian partners and program co-chair William Kelly, MD, FCCP, to finalize the meeting’s opening session. Though our own international meeting is still months away, work continues with the annual meeting innovations group, and I’ve been working with my own small team on some special surprises that you’ll hear more about in the coming months! The other CHEST meeting-related item on the front burner is the selection of the keynote speaker. The way this works is that I outline in broad strokes a sense of the flavor I’m targeting, and the CHEST staff work with a consulting group to propose some options. They provide me with a brief biography in clips, and we narrow the list down. As I write, we are finalizing our invitation, and I look forward to formally announcing the CHEST 2022 keynote speaker shortly!
After I explain the breadth of duties involved in my role, the most common follow-up question asked of me is whether I am enjoying the position. I’ll concede that it’s not for everyone. There’s a lot less independent decision-making than people assume. But, if you like getting to meet and interact with people from around the globe, helping them to see how CHEST can help them in their pursuits or career goals (and how they can help CHEST in our mission), it’s a super fun job. And I’ll most definitely miss it when I’m done.
So that, in brief, is an overview of what the CHEST President does. But each week is different. And, I get better at the job each day, as I learn something new about the position, the organization, and our outstanding members, leaders, and staff. I look forward to continuing to represent each of you in making decisions and communicating on behalf of CHEST. As always, I remain interested in your input as to how things are going; please consider reaching out to me at [email protected] at your convenience. ... I expect to have a few minutes to write back sometime next Thursday.
Until next time,
David
For those of you in the Northern Hemisphere, like me, spring has transitioned into summer, allowing us all to spend more time outdoors, gathering again with family, friends, and colleagues. And, while people are always happy to hear about what’s going on with the family, or how things are going at Emory, the most common question I get is “So what’s it like to be President of CHEST?” Now that I’ve been on the job for 6 months, I thought it was well enough time to pull back the curtain on the role for all of you out in CHEST-land who might be interested, as well. For the purposes of this column, I’ll be incorporating things that occurred over the past week.
As I’ve previously reported, the most important decisions that relate to CHEST strategy are made by the Board of Regents. While I do have the privilege of organizing and running Board meetings, most presidential duties between these meetings focus on communication: with our members, our leaders, and other organizations. One of the best parts of the job is the opportunity to interact with our members; between the [email protected] account and my own, I receive a couple of emails each day with questions about navigating CHEST, or ideas about ways that things might be better accomplished. With our recent Network and section reorganization, many of those questions have focused on leadership opportunities, inquiring about whether the writer should apply, or asking for information about the qualities that might increase the odds of earning a position. My answer is almost always the same: go ahead and throw your name in the hat; for most members, the sections are the first place to start the journey in CHEST leadership. And I’m pleased to say that I’ve had the chance to see some of the members who’ve reached out to me in the past selected for the positions to which they’d applied (in full disclosure, I have little role in selecting leadership positions; Network and section positions are chosen by current members of those Networks and sections). I look forward to watching their progress in our organizational leadership.
While CHEST CEO Robert Musacchio and I communicate almost every day, Wednesday is our weekly meeting during which we review progress on our organizational goals, the status of ongoing projects, and concerns from our membership and leadership. I also have the pleasure of meeting with my co-Presidents every other week; though Jack, Doreen, and Steve have always been happy to offer their counsel on very short notice, this semimonthly meeting helps to provide continuity in leadership, as well as a more formal opportunity for me to meet with trusted advisors to get a sounding board on active issues that affect CHEST. And, this gets to the other main job of CHEST President, which is to facilitate the making of important decisions on behalf of the College. I receive sporadic emails from CHEST staff as we are approached by other organizations or international partners for input on or approval for statements that they wish to make. In the case where the topic is clearly in the CHEST wheelhouse and the statement is consistent with our organizational goals, I can unilaterally sign off; a common example of something that fits in this category is content related to tobacco cessation. In the more frequent situation where the statement for approval is a bit more complex, I will usually refer the request to one of our committee, Network, or section chairs for consideration. Since the turnaround time on these requests is usually pretty short, I may ask them to advise me on their own, although they sometimes opt to run things by their own membership for further input or to achieve consensus.
The CHEST President also serves as ambassador to other organizations; this week, I had the pleasure of participating in a meeting with the American Board of Internal Medicine and a number of medical specialty leaders focused on how professional societies can help to mitigate the spread of medical misinformation. I also interfaced with several of our international partners in the pulmonary space, as they plan their own international meetings, to see how CHEST can contribute to the success of those endeavors by contributing content, speakers, or both. At the time of this writing, the CHEST Congress in Bologna, Italy, is right around the corner, and so I also spent time working with our Italian partners and program co-chair William Kelly, MD, FCCP, to finalize the meeting’s opening session. Though our own international meeting is still months away, work continues with the annual meeting innovations group, and I’ve been working with my own small team on some special surprises that you’ll hear more about in the coming months! The other CHEST meeting-related item on the front burner is the selection of the keynote speaker. The way this works is that I outline in broad strokes a sense of the flavor I’m targeting, and the CHEST staff work with a consulting group to propose some options. They provide me with a brief biography in clips, and we narrow the list down. As I write, we are finalizing our invitation, and I look forward to formally announcing the CHEST 2022 keynote speaker shortly!
After I explain the breadth of duties involved in my role, the most common follow-up question asked of me is whether I am enjoying the position. I’ll concede that it’s not for everyone. There’s a lot less independent decision-making than people assume. But, if you like getting to meet and interact with people from around the globe, helping them to see how CHEST can help them in their pursuits or career goals (and how they can help CHEST in our mission), it’s a super fun job. And I’ll most definitely miss it when I’m done.
So that, in brief, is an overview of what the CHEST President does. But each week is different. And, I get better at the job each day, as I learn something new about the position, the organization, and our outstanding members, leaders, and staff. I look forward to continuing to represent each of you in making decisions and communicating on behalf of CHEST. As always, I remain interested in your input as to how things are going; please consider reaching out to me at [email protected] at your convenience. ... I expect to have a few minutes to write back sometime next Thursday.
Until next time,
David
For those of you in the Northern Hemisphere, like me, spring has transitioned into summer, allowing us all to spend more time outdoors, gathering again with family, friends, and colleagues. And, while people are always happy to hear about what’s going on with the family, or how things are going at Emory, the most common question I get is “So what’s it like to be President of CHEST?” Now that I’ve been on the job for 6 months, I thought it was well enough time to pull back the curtain on the role for all of you out in CHEST-land who might be interested, as well. For the purposes of this column, I’ll be incorporating things that occurred over the past week.
As I’ve previously reported, the most important decisions that relate to CHEST strategy are made by the Board of Regents. While I do have the privilege of organizing and running Board meetings, most presidential duties between these meetings focus on communication: with our members, our leaders, and other organizations. One of the best parts of the job is the opportunity to interact with our members; between the [email protected] account and my own, I receive a couple of emails each day with questions about navigating CHEST, or ideas about ways that things might be better accomplished. With our recent Network and section reorganization, many of those questions have focused on leadership opportunities, inquiring about whether the writer should apply, or asking for information about the qualities that might increase the odds of earning a position. My answer is almost always the same: go ahead and throw your name in the hat; for most members, the sections are the first place to start the journey in CHEST leadership. And I’m pleased to say that I’ve had the chance to see some of the members who’ve reached out to me in the past selected for the positions to which they’d applied (in full disclosure, I have little role in selecting leadership positions; Network and section positions are chosen by current members of those Networks and sections). I look forward to watching their progress in our organizational leadership.
While CHEST CEO Robert Musacchio and I communicate almost every day, Wednesday is our weekly meeting during which we review progress on our organizational goals, the status of ongoing projects, and concerns from our membership and leadership. I also have the pleasure of meeting with my co-Presidents every other week; though Jack, Doreen, and Steve have always been happy to offer their counsel on very short notice, this semimonthly meeting helps to provide continuity in leadership, as well as a more formal opportunity for me to meet with trusted advisors to get a sounding board on active issues that affect CHEST. And, this gets to the other main job of CHEST President, which is to facilitate the making of important decisions on behalf of the College. I receive sporadic emails from CHEST staff as we are approached by other organizations or international partners for input on or approval for statements that they wish to make. In the case where the topic is clearly in the CHEST wheelhouse and the statement is consistent with our organizational goals, I can unilaterally sign off; a common example of something that fits in this category is content related to tobacco cessation. In the more frequent situation where the statement for approval is a bit more complex, I will usually refer the request to one of our committee, Network, or section chairs for consideration. Since the turnaround time on these requests is usually pretty short, I may ask them to advise me on their own, although they sometimes opt to run things by their own membership for further input or to achieve consensus.
The CHEST President also serves as ambassador to other organizations; this week, I had the pleasure of participating in a meeting with the American Board of Internal Medicine and a number of medical specialty leaders focused on how professional societies can help to mitigate the spread of medical misinformation. I also interfaced with several of our international partners in the pulmonary space, as they plan their own international meetings, to see how CHEST can contribute to the success of those endeavors by contributing content, speakers, or both. At the time of this writing, the CHEST Congress in Bologna, Italy, is right around the corner, and so I also spent time working with our Italian partners and program co-chair William Kelly, MD, FCCP, to finalize the meeting’s opening session. Though our own international meeting is still months away, work continues with the annual meeting innovations group, and I’ve been working with my own small team on some special surprises that you’ll hear more about in the coming months! The other CHEST meeting-related item on the front burner is the selection of the keynote speaker. The way this works is that I outline in broad strokes a sense of the flavor I’m targeting, and the CHEST staff work with a consulting group to propose some options. They provide me with a brief biography in clips, and we narrow the list down. As I write, we are finalizing our invitation, and I look forward to formally announcing the CHEST 2022 keynote speaker shortly!
After I explain the breadth of duties involved in my role, the most common follow-up question asked of me is whether I am enjoying the position. I’ll concede that it’s not for everyone. There’s a lot less independent decision-making than people assume. But, if you like getting to meet and interact with people from around the globe, helping them to see how CHEST can help them in their pursuits or career goals (and how they can help CHEST in our mission), it’s a super fun job. And I’ll most definitely miss it when I’m done.
So that, in brief, is an overview of what the CHEST President does. But each week is different. And, I get better at the job each day, as I learn something new about the position, the organization, and our outstanding members, leaders, and staff. I look forward to continuing to represent each of you in making decisions and communicating on behalf of CHEST. As always, I remain interested in your input as to how things are going; please consider reaching out to me at [email protected] at your convenience. ... I expect to have a few minutes to write back sometime next Thursday.
Until next time,
David












