User login
Five reasons to update your will
You have a will, so you can rest easy, right? Not necessarily. Even though it can provide for some contingencies, an old will can’t cover every change that may have occurred since it was first drawn. Professionals advise that you review your will every few years and more often if situations such as the following five have occurred since you last updated your will.
#1. Family changes
If you’ve had any changes in your family situation, you will probably need to update your will. Events such as marriage, divorce, death, birth, adoption, or a falling out with a loved one may affect how your estate will be distributed, who should act as guardian for your dependents, and who should be named as executor of your estate.
#2. Relocating to a new state
The laws among the states vary. Moving to a new state or purchasing property in another state can affect your estate plan and how property in that state will be taxed and distributed.
#3. Tax law changes
Federal and state legislatures are continually tinkering with federal estate and state inheritance tax laws. An old will may fail to take advantage of strategies that will minimize estate taxes.
#4. You want to support a favorite cause
If you have developed a connection to a cause, you may want to benefit a particular charity with a gift in your estate. Contact us for sample language you can share with your attorney to include a gift to us in your will.
#5. Changes in your estate’s value
When you made your will, your assets may have been relatively modest. Now the value may be larger and your will no longer reflects how you would like your estate divided.
Consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI. Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
You have a will, so you can rest easy, right? Not necessarily. Even though it can provide for some contingencies, an old will can’t cover every change that may have occurred since it was first drawn. Professionals advise that you review your will every few years and more often if situations such as the following five have occurred since you last updated your will.
#1. Family changes
If you’ve had any changes in your family situation, you will probably need to update your will. Events such as marriage, divorce, death, birth, adoption, or a falling out with a loved one may affect how your estate will be distributed, who should act as guardian for your dependents, and who should be named as executor of your estate.
#2. Relocating to a new state
The laws among the states vary. Moving to a new state or purchasing property in another state can affect your estate plan and how property in that state will be taxed and distributed.
#3. Tax law changes
Federal and state legislatures are continually tinkering with federal estate and state inheritance tax laws. An old will may fail to take advantage of strategies that will minimize estate taxes.
#4. You want to support a favorite cause
If you have developed a connection to a cause, you may want to benefit a particular charity with a gift in your estate. Contact us for sample language you can share with your attorney to include a gift to us in your will.
#5. Changes in your estate’s value
When you made your will, your assets may have been relatively modest. Now the value may be larger and your will no longer reflects how you would like your estate divided.
Consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI. Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
You have a will, so you can rest easy, right? Not necessarily. Even though it can provide for some contingencies, an old will can’t cover every change that may have occurred since it was first drawn. Professionals advise that you review your will every few years and more often if situations such as the following five have occurred since you last updated your will.
#1. Family changes
If you’ve had any changes in your family situation, you will probably need to update your will. Events such as marriage, divorce, death, birth, adoption, or a falling out with a loved one may affect how your estate will be distributed, who should act as guardian for your dependents, and who should be named as executor of your estate.
#2. Relocating to a new state
The laws among the states vary. Moving to a new state or purchasing property in another state can affect your estate plan and how property in that state will be taxed and distributed.
#3. Tax law changes
Federal and state legislatures are continually tinkering with federal estate and state inheritance tax laws. An old will may fail to take advantage of strategies that will minimize estate taxes.
#4. You want to support a favorite cause
If you have developed a connection to a cause, you may want to benefit a particular charity with a gift in your estate. Contact us for sample language you can share with your attorney to include a gift to us in your will.
#5. Changes in your estate’s value
When you made your will, your assets may have been relatively modest. Now the value may be larger and your will no longer reflects how you would like your estate divided.
Consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI. Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
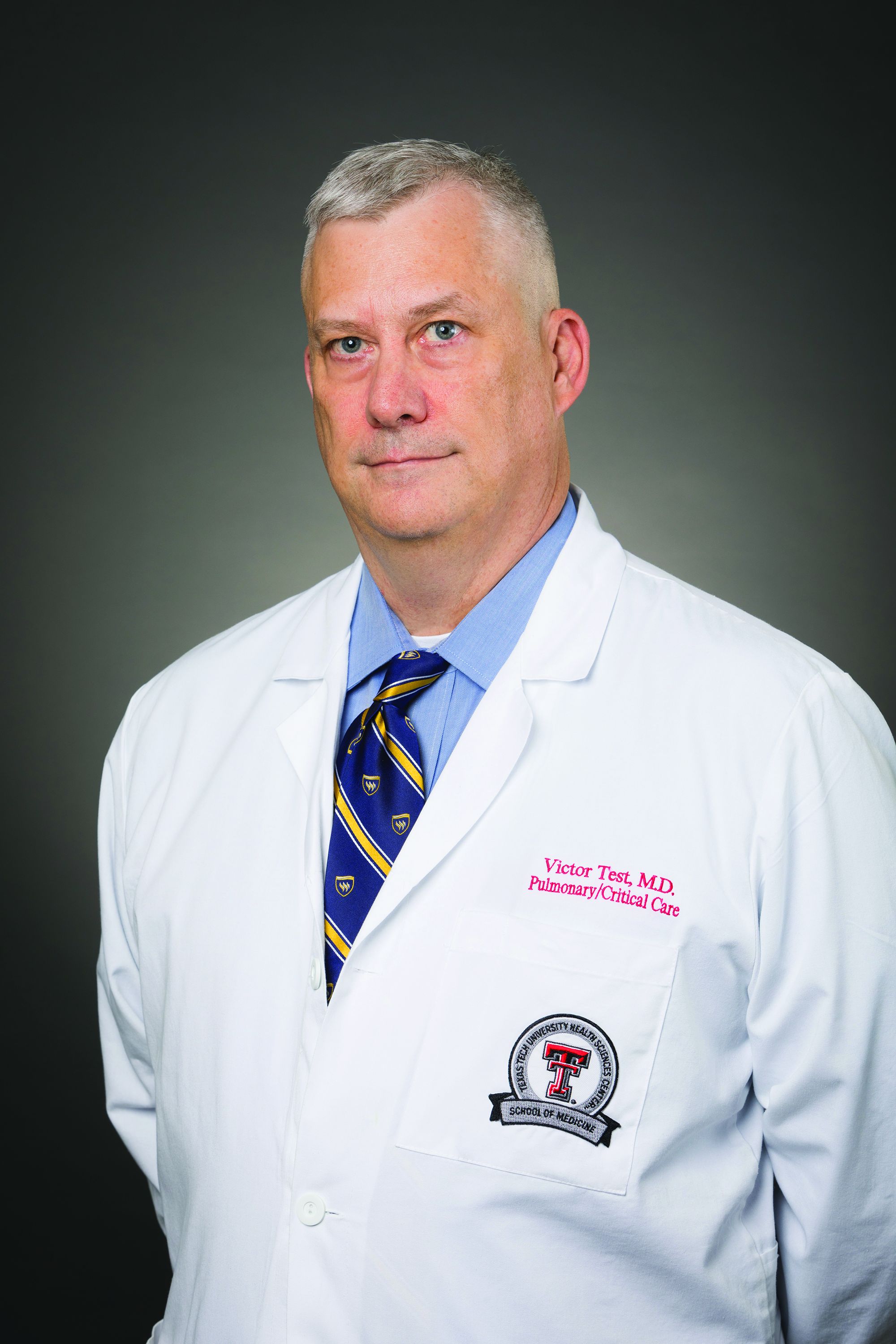
Victor Test, MD, FCCP, receives Medal of Valor from AMA
The American Medical Association (AMA) honored CHEST Board Member Victor J. Test, MD, FCCP, with the AMA Medal of Valor for his work on behalf of patients and his community during the COVID-19 pandemic.
The award, which recognizes physicians who demonstrate courage under extraordinary circumstances, was presented to Dr. Test because of his quick decisive actions during the onset of the pandemic, including personally securing personal protective equipment to supply the critical care faculty and fellows at the Texas Tech University hospital in Lubbock and building plexiglass and PVC chambers for the physicians and nursing staff caring for patients with COVID-19.
Read more here.
The American Medical Association (AMA) honored CHEST Board Member Victor J. Test, MD, FCCP, with the AMA Medal of Valor for his work on behalf of patients and his community during the COVID-19 pandemic.
The award, which recognizes physicians who demonstrate courage under extraordinary circumstances, was presented to Dr. Test because of his quick decisive actions during the onset of the pandemic, including personally securing personal protective equipment to supply the critical care faculty and fellows at the Texas Tech University hospital in Lubbock and building plexiglass and PVC chambers for the physicians and nursing staff caring for patients with COVID-19.
Read more here.
The American Medical Association (AMA) honored CHEST Board Member Victor J. Test, MD, FCCP, with the AMA Medal of Valor for his work on behalf of patients and his community during the COVID-19 pandemic.
The award, which recognizes physicians who demonstrate courage under extraordinary circumstances, was presented to Dr. Test because of his quick decisive actions during the onset of the pandemic, including personally securing personal protective equipment to supply the critical care faculty and fellows at the Texas Tech University hospital in Lubbock and building plexiglass and PVC chambers for the physicians and nursing staff caring for patients with COVID-19.
Read more here.
Off to the races with The CHEST Foundation
The CHEST Foundation cordially invites CHEST members and colleagues, health care professionals, and others to champion lung health and attend the annual Belmont Stakes Dinner and Auction, Saturday, June 11, in New York at the beautiful Water Club overlooking the East River.
Hosted by CHEST President-Elect Doreen Addrizzo-Harris, MD, FCCP, this year’s celebration will include a lively cocktail reception, a silent and live auction, dinner, and a rooftop after-party for young professionals to network with colleagues and CHEST leadership and take the challenge for a chance to win great prizes, including a Peloton, ultrasound machine, and access to CHEST courses and events. Fully immerse yourself in the event, and wear your race-day best!
This year, we are honoring two outstanding patients and advocates, Betsy Glaeser and Fred Schick, for their remarkable achievements in patient empowerment and access. Glaeser, who was diagnosed with nontuberculous mycobacteria (disease NTM) more than 20 years ago, pioneered opportunities for NTM-specific research funding and runs a hundreds-strong support group for people with NTM and bronchiectasis. Schick, who has pulmonary fibrosis, is an active ambassador in the patient community in Chicago and also leads local support groups for others with the disease.
All proceeds from the evening’s events will benefit the CHEST Foundation’s continued work toward bringing impactful, informative resources to patients.
As the patient-focused philanthropic arm of the American College of Chest Physicians, the CHEST Foundation is on a mission to champion lung health and strives to give health care professionals, patients, and caregivers opportunities to come together, give back, and advocate for change.
Since its inception, the Foundation has provided more than $8 million in research grants and $3 million in community grants, created free patient education resources for more than 80 disease states, and provided thousands of units of personal protective equipment and $1 million for pandemic relief efforts through COVID-19 Reaction Microgrants.
Support the continued work of the Foundation – and watch some of the most exciting few minutes in sports among colleagues and friends – at this year’s Belmont Stakes Dinner and Auction. To purchase a ticket, or to learn more about sponsorship benefits or underwriting opportunities, contact Angela Perillo at [email protected] or +1 (224) 521-9520.
The CHEST Foundation cordially invites CHEST members and colleagues, health care professionals, and others to champion lung health and attend the annual Belmont Stakes Dinner and Auction, Saturday, June 11, in New York at the beautiful Water Club overlooking the East River.
Hosted by CHEST President-Elect Doreen Addrizzo-Harris, MD, FCCP, this year’s celebration will include a lively cocktail reception, a silent and live auction, dinner, and a rooftop after-party for young professionals to network with colleagues and CHEST leadership and take the challenge for a chance to win great prizes, including a Peloton, ultrasound machine, and access to CHEST courses and events. Fully immerse yourself in the event, and wear your race-day best!
This year, we are honoring two outstanding patients and advocates, Betsy Glaeser and Fred Schick, for their remarkable achievements in patient empowerment and access. Glaeser, who was diagnosed with nontuberculous mycobacteria (disease NTM) more than 20 years ago, pioneered opportunities for NTM-specific research funding and runs a hundreds-strong support group for people with NTM and bronchiectasis. Schick, who has pulmonary fibrosis, is an active ambassador in the patient community in Chicago and also leads local support groups for others with the disease.
All proceeds from the evening’s events will benefit the CHEST Foundation’s continued work toward bringing impactful, informative resources to patients.
As the patient-focused philanthropic arm of the American College of Chest Physicians, the CHEST Foundation is on a mission to champion lung health and strives to give health care professionals, patients, and caregivers opportunities to come together, give back, and advocate for change.
Since its inception, the Foundation has provided more than $8 million in research grants and $3 million in community grants, created free patient education resources for more than 80 disease states, and provided thousands of units of personal protective equipment and $1 million for pandemic relief efforts through COVID-19 Reaction Microgrants.
Support the continued work of the Foundation – and watch some of the most exciting few minutes in sports among colleagues and friends – at this year’s Belmont Stakes Dinner and Auction. To purchase a ticket, or to learn more about sponsorship benefits or underwriting opportunities, contact Angela Perillo at [email protected] or +1 (224) 521-9520.
The CHEST Foundation cordially invites CHEST members and colleagues, health care professionals, and others to champion lung health and attend the annual Belmont Stakes Dinner and Auction, Saturday, June 11, in New York at the beautiful Water Club overlooking the East River.
Hosted by CHEST President-Elect Doreen Addrizzo-Harris, MD, FCCP, this year’s celebration will include a lively cocktail reception, a silent and live auction, dinner, and a rooftop after-party for young professionals to network with colleagues and CHEST leadership and take the challenge for a chance to win great prizes, including a Peloton, ultrasound machine, and access to CHEST courses and events. Fully immerse yourself in the event, and wear your race-day best!
This year, we are honoring two outstanding patients and advocates, Betsy Glaeser and Fred Schick, for their remarkable achievements in patient empowerment and access. Glaeser, who was diagnosed with nontuberculous mycobacteria (disease NTM) more than 20 years ago, pioneered opportunities for NTM-specific research funding and runs a hundreds-strong support group for people with NTM and bronchiectasis. Schick, who has pulmonary fibrosis, is an active ambassador in the patient community in Chicago and also leads local support groups for others with the disease.
All proceeds from the evening’s events will benefit the CHEST Foundation’s continued work toward bringing impactful, informative resources to patients.
As the patient-focused philanthropic arm of the American College of Chest Physicians, the CHEST Foundation is on a mission to champion lung health and strives to give health care professionals, patients, and caregivers opportunities to come together, give back, and advocate for change.
Since its inception, the Foundation has provided more than $8 million in research grants and $3 million in community grants, created free patient education resources for more than 80 disease states, and provided thousands of units of personal protective equipment and $1 million for pandemic relief efforts through COVID-19 Reaction Microgrants.
Support the continued work of the Foundation – and watch some of the most exciting few minutes in sports among colleagues and friends – at this year’s Belmont Stakes Dinner and Auction. To purchase a ticket, or to learn more about sponsorship benefits or underwriting opportunities, contact Angela Perillo at [email protected] or +1 (224) 521-9520.
Chest Infections and Disaster Response
Addressing disparities of socioeconomic status, race, and education in vaccine hesitancy and uptake
Vaccine hesitancy is described by the World Health Organization (WHO) as a “delay in acceptance or refusal of vaccination, despite availability of vaccine services.”1 Disparities in COVID-19 vaccine uptake, in addition to preexisting views of vaccine hesitancy, are consistently in the mainstream news.
The United States has a high rate of vaccine hesitancy, with a third of the country surveyed in 2021 stating they were unlikely to become vaccinated against COVID-19.2 This is in contrast to over 90% of people in Australia, China, and Norway saying they were highly likely to become vaccinated. Prepandemic, however, vaccination rates for preventable respiratory illness were already suboptimal. In fact, in 2019, the WHO declared vaccine hesitancy a top 10 priority due to the threat low vaccination causes on a global level.1
U.S. health care systems’ cost to patients may serve as a disincentive for health care utilization, decreasing health care contacts. Further, changes in insurance can lead to provider discontinuity, which may erode the trusted patient-physician relationship. These realities may contribute to vaccine hesitancy that has been inversely correlated to both number of health care visits and trust in health care providers. Vaccine hesitancy exacerbates health disparities.1 Health literacy (understanding of health), education level, and general vaccine knowledge contribute to vaccine hesitancy also. Additionally, high social vulnerability (a score calculated from factors related to socioeconomic status, race, household makeup, housing type, and transportation) is strongly inversely correlated with vaccination rates. In places with both high social vulnerability and vaccine hesitancy, the vaccine-hesitant individuals have far fewer vaccinations.3
Providers can impact vaccine uptake. Broadly, efforts to understand and address issues of trust in health care are needed. Educational materials should be disseminated to high-risk and medically underserved communities. At medical appointments, assessment of vaccination status, followed by providing individualized information regarding vaccine benefits and specific concerns may help increase uptake. In a survey of high-risk adults, only 14.8 and 18.5% of patients stated that the pneumococcal vaccine was offered to them in the last year and 5 years, respectively.1 Providers can have a strong impact on people obtaining vaccines; over half of patients receive vaccines when their provider recommends it.1,4 As a medical community focused on respiratory health, we need to prioritize offering vaccinations during inpatient and outpatient encounters.
By Jamie R. Felzer, MD, MPH
Network Member
Cassie C. Kennedy, MD, FCCP
Vice Chair, Council of Networks
Dr. Felzer is a Fellow and Dr. Kennedy is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MN.
References
1. Gatwood J et al. Am J Health Promot. 2021;35:908.
2. Wong LP et al. Infect Dis Poverty. 2021;10:122.
3. Crane MA et al. Health Aff (Millwood). 2021;40:1792.
4. Strully KW et al. Front Public Health. 2021;9:645268.
Addressing disparities of socioeconomic status, race, and education in vaccine hesitancy and uptake
Vaccine hesitancy is described by the World Health Organization (WHO) as a “delay in acceptance or refusal of vaccination, despite availability of vaccine services.”1 Disparities in COVID-19 vaccine uptake, in addition to preexisting views of vaccine hesitancy, are consistently in the mainstream news.
The United States has a high rate of vaccine hesitancy, with a third of the country surveyed in 2021 stating they were unlikely to become vaccinated against COVID-19.2 This is in contrast to over 90% of people in Australia, China, and Norway saying they were highly likely to become vaccinated. Prepandemic, however, vaccination rates for preventable respiratory illness were already suboptimal. In fact, in 2019, the WHO declared vaccine hesitancy a top 10 priority due to the threat low vaccination causes on a global level.1
U.S. health care systems’ cost to patients may serve as a disincentive for health care utilization, decreasing health care contacts. Further, changes in insurance can lead to provider discontinuity, which may erode the trusted patient-physician relationship. These realities may contribute to vaccine hesitancy that has been inversely correlated to both number of health care visits and trust in health care providers. Vaccine hesitancy exacerbates health disparities.1 Health literacy (understanding of health), education level, and general vaccine knowledge contribute to vaccine hesitancy also. Additionally, high social vulnerability (a score calculated from factors related to socioeconomic status, race, household makeup, housing type, and transportation) is strongly inversely correlated with vaccination rates. In places with both high social vulnerability and vaccine hesitancy, the vaccine-hesitant individuals have far fewer vaccinations.3
Providers can impact vaccine uptake. Broadly, efforts to understand and address issues of trust in health care are needed. Educational materials should be disseminated to high-risk and medically underserved communities. At medical appointments, assessment of vaccination status, followed by providing individualized information regarding vaccine benefits and specific concerns may help increase uptake. In a survey of high-risk adults, only 14.8 and 18.5% of patients stated that the pneumococcal vaccine was offered to them in the last year and 5 years, respectively.1 Providers can have a strong impact on people obtaining vaccines; over half of patients receive vaccines when their provider recommends it.1,4 As a medical community focused on respiratory health, we need to prioritize offering vaccinations during inpatient and outpatient encounters.
By Jamie R. Felzer, MD, MPH
Network Member
Cassie C. Kennedy, MD, FCCP
Vice Chair, Council of Networks
Dr. Felzer is a Fellow and Dr. Kennedy is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MN.
References
1. Gatwood J et al. Am J Health Promot. 2021;35:908.
2. Wong LP et al. Infect Dis Poverty. 2021;10:122.
3. Crane MA et al. Health Aff (Millwood). 2021;40:1792.
4. Strully KW et al. Front Public Health. 2021;9:645268.
Addressing disparities of socioeconomic status, race, and education in vaccine hesitancy and uptake
Vaccine hesitancy is described by the World Health Organization (WHO) as a “delay in acceptance or refusal of vaccination, despite availability of vaccine services.”1 Disparities in COVID-19 vaccine uptake, in addition to preexisting views of vaccine hesitancy, are consistently in the mainstream news.
The United States has a high rate of vaccine hesitancy, with a third of the country surveyed in 2021 stating they were unlikely to become vaccinated against COVID-19.2 This is in contrast to over 90% of people in Australia, China, and Norway saying they were highly likely to become vaccinated. Prepandemic, however, vaccination rates for preventable respiratory illness were already suboptimal. In fact, in 2019, the WHO declared vaccine hesitancy a top 10 priority due to the threat low vaccination causes on a global level.1
U.S. health care systems’ cost to patients may serve as a disincentive for health care utilization, decreasing health care contacts. Further, changes in insurance can lead to provider discontinuity, which may erode the trusted patient-physician relationship. These realities may contribute to vaccine hesitancy that has been inversely correlated to both number of health care visits and trust in health care providers. Vaccine hesitancy exacerbates health disparities.1 Health literacy (understanding of health), education level, and general vaccine knowledge contribute to vaccine hesitancy also. Additionally, high social vulnerability (a score calculated from factors related to socioeconomic status, race, household makeup, housing type, and transportation) is strongly inversely correlated with vaccination rates. In places with both high social vulnerability and vaccine hesitancy, the vaccine-hesitant individuals have far fewer vaccinations.3
Providers can impact vaccine uptake. Broadly, efforts to understand and address issues of trust in health care are needed. Educational materials should be disseminated to high-risk and medically underserved communities. At medical appointments, assessment of vaccination status, followed by providing individualized information regarding vaccine benefits and specific concerns may help increase uptake. In a survey of high-risk adults, only 14.8 and 18.5% of patients stated that the pneumococcal vaccine was offered to them in the last year and 5 years, respectively.1 Providers can have a strong impact on people obtaining vaccines; over half of patients receive vaccines when their provider recommends it.1,4 As a medical community focused on respiratory health, we need to prioritize offering vaccinations during inpatient and outpatient encounters.
By Jamie R. Felzer, MD, MPH
Network Member
Cassie C. Kennedy, MD, FCCP
Vice Chair, Council of Networks
Dr. Felzer is a Fellow and Dr. Kennedy is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MN.
References
1. Gatwood J et al. Am J Health Promot. 2021;35:908.
2. Wong LP et al. Infect Dis Poverty. 2021;10:122.
3. Crane MA et al. Health Aff (Millwood). 2021;40:1792.
4. Strully KW et al. Front Public Health. 2021;9:645268.
FeNO guidelines. Marijuana use in pregnancy.
Airway disorders
FeNO guidelines and the art of clinical medicine
The American Thoracic Society (ATS) recently published new guidelines on the use of fractional exhaled nitric oxide (FeNO) in the management of asthma (Khatri S. Am J Respir Crit Care Med. 2021;204[10]:e97-e109). The previous iteration dealt with questions about the interpretation of FeNO levels. However, the updated guidelines address a single question: Should patients with asthma in whom treatment is being contemplated undergo FeNO testing?
Several roles of nitric oxide (NO) have been discovered, including as a marker of eosinophilic airway inflammation or T2-inflammation. The fraction of NO during steady-state exhalation, easily measured by a handheld device, is a standardized quantitative noninvasive method to assess severity of airway eosinophilic inflammation. However, factors like concomitant sinusitis, bronchoconstriction, obesity, and smoking can also affect FeNO levels, and interpretation is context-dependent. Moreover, some biologic agents have variable effects on FeNO while still being effective in controlling T2 inflammation. Therefore, FeNO is neither the broadest nor the most sensitive signal of T2 inflammation, and there is much unknown about using FeNO to guide asthma treatment. Heterogeneity is one of the many challenges, as different endotypes and clinical subsets vary in the inflammatory pathways leading to airway hyperresponsiveness and remodeling.
The panel assessed the value of FeNO testing in improving asthma control questionnaire scores (ACT, ACQ-7), oral corticosteroid use, asthma exacerbations, lung function, health care utilization, and cost-effectiveness. FeNO-guided therapy compared with therapy without FeNO reduced exacerbations and oral corticosteroid use, though effect size was modest. Among other outcomes, while the trend favored FeNO, it did not reach statistical significance. Adverse effects of FeNO testing were trivial, and the cost is moderate though dependent on the institution size and testing frequency. Thus, for clinicians who manage adults and children 4 years of age and older, in whom treatment for asthma is being considered, it is suggested that FeNO testing be done in addition to usual care. The guidelines do not recommend specific steps to modify treatment based on FeNO results but suggest a decision framework, reminding us that clinical context is key and FeNO is merely one signal. In recognizing its own fallibility, this document suggests that in the continually evolving world of asthma, the art of clinical medicine still reigns supreme.
Uddalak Majumdar, MDDr. Majumdar is a Fellow, Pulmonary & Critical Care Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
Sleep medicine
Marijuana use in pregnancy
Marijuana is the most commonly used illegal drug in the United States. According to the CDC, about 1 in 20 women report using marijuana while pregnant (https://www.cdc.gov/marijuana/health-effects/pregnancy.html). As states legalize marijuana for medicinal or recreational purposes, its use by pregnant women could increase even further. While some use it to ease morning sickness and anxiety, they may not be aware that it can pose risks.
Research has been raising concerns about the effects of marijuana use during pregnancy for years. A study from 1978 linked maternal cannabis use with children’s behavioral problems and deficits in language comprehension, visual perception, attention, and memory (Life Sci. 1995;56[23-24]:2159-68). ). More recent research has linked use to low birth weight, reduced IQ, autism, delusional thoughts, and attention problems, although some other studies have not identified such associations.
A new study shows that children of women who use marijuana during or soon after pregnancy were twice as likely to become anxious, aggressive, or hyperactive. This corresponded with widespread reductions in immune-related gene expression in the placenta, which correlated with anxiety and hyperactivity (Proc National Acad Sci. 2021;118[47]e2106115118).
Chemicals from marijuana can be passed to the baby through breast milk. THC is stored in body fat and slowly released over time. Exposure could still occur even after stopping use (Marijuana use during pregnancy and lactation. ACOG Committee Opinion, Number 722, October 2017).
Studies have shown that THC can pass through the mother’s bloodstream to the placenta and the fetus. This occurs independent of how cannabis is consumed (smoking, vaping, eating, or oils/creams). Patients should be educated that no amount has been proven safe to use during pregnancy or breastfeeding.
Anita Rajagopal, MD, FCCP, Respiratory-Related Sleep Disorders Section, Member-at-Large
Dr. Rajagopal is Network Medical Director, Community Physician Network, Sleep Medicine/Medical Director, Community Health Network Sleep-Wake Disorders Center, Community Health Network, Indianapolis, Indiana.
Airway disorders
FeNO guidelines and the art of clinical medicine
The American Thoracic Society (ATS) recently published new guidelines on the use of fractional exhaled nitric oxide (FeNO) in the management of asthma (Khatri S. Am J Respir Crit Care Med. 2021;204[10]:e97-e109). The previous iteration dealt with questions about the interpretation of FeNO levels. However, the updated guidelines address a single question: Should patients with asthma in whom treatment is being contemplated undergo FeNO testing?
Several roles of nitric oxide (NO) have been discovered, including as a marker of eosinophilic airway inflammation or T2-inflammation. The fraction of NO during steady-state exhalation, easily measured by a handheld device, is a standardized quantitative noninvasive method to assess severity of airway eosinophilic inflammation. However, factors like concomitant sinusitis, bronchoconstriction, obesity, and smoking can also affect FeNO levels, and interpretation is context-dependent. Moreover, some biologic agents have variable effects on FeNO while still being effective in controlling T2 inflammation. Therefore, FeNO is neither the broadest nor the most sensitive signal of T2 inflammation, and there is much unknown about using FeNO to guide asthma treatment. Heterogeneity is one of the many challenges, as different endotypes and clinical subsets vary in the inflammatory pathways leading to airway hyperresponsiveness and remodeling.
The panel assessed the value of FeNO testing in improving asthma control questionnaire scores (ACT, ACQ-7), oral corticosteroid use, asthma exacerbations, lung function, health care utilization, and cost-effectiveness. FeNO-guided therapy compared with therapy without FeNO reduced exacerbations and oral corticosteroid use, though effect size was modest. Among other outcomes, while the trend favored FeNO, it did not reach statistical significance. Adverse effects of FeNO testing were trivial, and the cost is moderate though dependent on the institution size and testing frequency. Thus, for clinicians who manage adults and children 4 years of age and older, in whom treatment for asthma is being considered, it is suggested that FeNO testing be done in addition to usual care. The guidelines do not recommend specific steps to modify treatment based on FeNO results but suggest a decision framework, reminding us that clinical context is key and FeNO is merely one signal. In recognizing its own fallibility, this document suggests that in the continually evolving world of asthma, the art of clinical medicine still reigns supreme.
Uddalak Majumdar, MDDr. Majumdar is a Fellow, Pulmonary & Critical Care Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
Sleep medicine
Marijuana use in pregnancy
Marijuana is the most commonly used illegal drug in the United States. According to the CDC, about 1 in 20 women report using marijuana while pregnant (https://www.cdc.gov/marijuana/health-effects/pregnancy.html). As states legalize marijuana for medicinal or recreational purposes, its use by pregnant women could increase even further. While some use it to ease morning sickness and anxiety, they may not be aware that it can pose risks.
Research has been raising concerns about the effects of marijuana use during pregnancy for years. A study from 1978 linked maternal cannabis use with children’s behavioral problems and deficits in language comprehension, visual perception, attention, and memory (Life Sci. 1995;56[23-24]:2159-68). ). More recent research has linked use to low birth weight, reduced IQ, autism, delusional thoughts, and attention problems, although some other studies have not identified such associations.
A new study shows that children of women who use marijuana during or soon after pregnancy were twice as likely to become anxious, aggressive, or hyperactive. This corresponded with widespread reductions in immune-related gene expression in the placenta, which correlated with anxiety and hyperactivity (Proc National Acad Sci. 2021;118[47]e2106115118).
Chemicals from marijuana can be passed to the baby through breast milk. THC is stored in body fat and slowly released over time. Exposure could still occur even after stopping use (Marijuana use during pregnancy and lactation. ACOG Committee Opinion, Number 722, October 2017).
Studies have shown that THC can pass through the mother’s bloodstream to the placenta and the fetus. This occurs independent of how cannabis is consumed (smoking, vaping, eating, or oils/creams). Patients should be educated that no amount has been proven safe to use during pregnancy or breastfeeding.
Anita Rajagopal, MD, FCCP, Respiratory-Related Sleep Disorders Section, Member-at-Large
Dr. Rajagopal is Network Medical Director, Community Physician Network, Sleep Medicine/Medical Director, Community Health Network Sleep-Wake Disorders Center, Community Health Network, Indianapolis, Indiana.
Airway disorders
FeNO guidelines and the art of clinical medicine
The American Thoracic Society (ATS) recently published new guidelines on the use of fractional exhaled nitric oxide (FeNO) in the management of asthma (Khatri S. Am J Respir Crit Care Med. 2021;204[10]:e97-e109). The previous iteration dealt with questions about the interpretation of FeNO levels. However, the updated guidelines address a single question: Should patients with asthma in whom treatment is being contemplated undergo FeNO testing?
Several roles of nitric oxide (NO) have been discovered, including as a marker of eosinophilic airway inflammation or T2-inflammation. The fraction of NO during steady-state exhalation, easily measured by a handheld device, is a standardized quantitative noninvasive method to assess severity of airway eosinophilic inflammation. However, factors like concomitant sinusitis, bronchoconstriction, obesity, and smoking can also affect FeNO levels, and interpretation is context-dependent. Moreover, some biologic agents have variable effects on FeNO while still being effective in controlling T2 inflammation. Therefore, FeNO is neither the broadest nor the most sensitive signal of T2 inflammation, and there is much unknown about using FeNO to guide asthma treatment. Heterogeneity is one of the many challenges, as different endotypes and clinical subsets vary in the inflammatory pathways leading to airway hyperresponsiveness and remodeling.
The panel assessed the value of FeNO testing in improving asthma control questionnaire scores (ACT, ACQ-7), oral corticosteroid use, asthma exacerbations, lung function, health care utilization, and cost-effectiveness. FeNO-guided therapy compared with therapy without FeNO reduced exacerbations and oral corticosteroid use, though effect size was modest. Among other outcomes, while the trend favored FeNO, it did not reach statistical significance. Adverse effects of FeNO testing were trivial, and the cost is moderate though dependent on the institution size and testing frequency. Thus, for clinicians who manage adults and children 4 years of age and older, in whom treatment for asthma is being considered, it is suggested that FeNO testing be done in addition to usual care. The guidelines do not recommend specific steps to modify treatment based on FeNO results but suggest a decision framework, reminding us that clinical context is key and FeNO is merely one signal. In recognizing its own fallibility, this document suggests that in the continually evolving world of asthma, the art of clinical medicine still reigns supreme.
Uddalak Majumdar, MDDr. Majumdar is a Fellow, Pulmonary & Critical Care Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, Ohio.
Sleep medicine
Marijuana use in pregnancy
Marijuana is the most commonly used illegal drug in the United States. According to the CDC, about 1 in 20 women report using marijuana while pregnant (https://www.cdc.gov/marijuana/health-effects/pregnancy.html). As states legalize marijuana for medicinal or recreational purposes, its use by pregnant women could increase even further. While some use it to ease morning sickness and anxiety, they may not be aware that it can pose risks.
Research has been raising concerns about the effects of marijuana use during pregnancy for years. A study from 1978 linked maternal cannabis use with children’s behavioral problems and deficits in language comprehension, visual perception, attention, and memory (Life Sci. 1995;56[23-24]:2159-68). ). More recent research has linked use to low birth weight, reduced IQ, autism, delusional thoughts, and attention problems, although some other studies have not identified such associations.
A new study shows that children of women who use marijuana during or soon after pregnancy were twice as likely to become anxious, aggressive, or hyperactive. This corresponded with widespread reductions in immune-related gene expression in the placenta, which correlated with anxiety and hyperactivity (Proc National Acad Sci. 2021;118[47]e2106115118).
Chemicals from marijuana can be passed to the baby through breast milk. THC is stored in body fat and slowly released over time. Exposure could still occur even after stopping use (Marijuana use during pregnancy and lactation. ACOG Committee Opinion, Number 722, October 2017).
Studies have shown that THC can pass through the mother’s bloodstream to the placenta and the fetus. This occurs independent of how cannabis is consumed (smoking, vaping, eating, or oils/creams). Patients should be educated that no amount has been proven safe to use during pregnancy or breastfeeding.
Anita Rajagopal, MD, FCCP, Respiratory-Related Sleep Disorders Section, Member-at-Large
Dr. Rajagopal is Network Medical Director, Community Physician Network, Sleep Medicine/Medical Director, Community Health Network Sleep-Wake Disorders Center, Community Health Network, Indianapolis, Indiana.
President’s report
New year, new CHEST President. Same as it has always been, except it has never been this way before. In past years, the transition of the CHEST Presidency occurred at our annual meeting, with a formal handover of leadership and a large reception. While there’s no Presidential football to hand over or secret codes to change for the incoming administration, there are usually several pending issues related to ongoing endeavors that need to be discussed between the outgoing and incoming leadership, in addition to some pearls of wisdom and the figurative “keys to the car.”
Now that CHEST has changed its President’s year to transition alongside the calendar year, there are few associated formalities. I awakened on New Year’s Day with my new title and the associated responsibility. Past President Steve Simpson, the mensch that he is, sent along with my colluding spouse a lovely and inspirational message for me to peruse, full of thoughtful advice and reflections on his year as President. I don’t know if this has ever been done before, but it is a tradition that I fully intend on continuing at the end of my term.
What has CHEST been up to during the first few months of my tenure? January saw us hold our first Board of Regents meeting for 2022, as well as the meeting of the CHEST Critical Care SEEK editorial board, where they worked to put together Volume 32, which will be out later this year. Watching some of the best and brightest medical minds from around the country discuss hot topics in critical care was a great experience (even if I didn’t have much to offer this august group), but the educational content was secondary to the interactions. Not only are these really smart folks teaching and learning from each other, but many of them are also clearly long-term colleagues, and watching this medical meeting was a lot like watching a reunion of friends who hadn’t seen each other in years. And, it struck me that what I’ve really been missing the most in the context of the social isolation that has accompanied the medical challenges of the pandemic is the pleasure of meeting in person with other folks to share stories, tell jokes, commiserate a bit, and catch up on the time that COVID-19 has stolen from us.
As we move further into 2022, I’m hoping that CHEST and our sister societies can help make up for this lost time by giving us the chance to meet in person once again. And to help build these experiences, we held an experiential design team along with our annual CHEST Program Committee meeting in February. Not only will the 2022 annual meeting in Nashville have the opportunity to hear from and network the best and brightest in pulmonary, critical care, and sleep medicine, but to celebrate our getting back together for the first time in years, we are also putting together some special surprises that CHEST has never done before. Keep an eye out for sneak peaks of these plans later in the spring and summer.
Another of our foci in 2022 is our ongoing push to help historically disenfranchised groups feel more engaged with CHEST. Many of you contributed to last year’s initiative to gather data on the kinds of things that we can do better, and I’ve just put together a presidential task force to develop final recommendations to further our goals of improving diversity, equity, and inclusion and to present to the Board of Regents for our April meeting.
Hopefully, many of you have seen some of the “Pardon the Introduction” series that CHEST has been featuring on its social media channels. We’ve put these together to showcase some of our leadership, their experiences, and opportunities for our members to get more involved with the College. Selfishly, I admit that they have also served as an excuse for me to catch up with some old friends and share our CHEST stories. We will be continuing to produce this series throughout the year; please let us know if there are specific folks you’d like us to feature!
Lastly, I wanted to thank the many of you who have reached out to me with questions, comments, and feedback. One of my main initiatives for the year is to make sure we are meeting the needs of as many of our members as possible, and this is something we can only do well if the lines of communication are wide open. Please continue to reach out to me, either by emailing me at [email protected] or messaging me on Twitter @ChestPrez.
New year, new CHEST President. Same as it has always been, except it has never been this way before. In past years, the transition of the CHEST Presidency occurred at our annual meeting, with a formal handover of leadership and a large reception. While there’s no Presidential football to hand over or secret codes to change for the incoming administration, there are usually several pending issues related to ongoing endeavors that need to be discussed between the outgoing and incoming leadership, in addition to some pearls of wisdom and the figurative “keys to the car.”
Now that CHEST has changed its President’s year to transition alongside the calendar year, there are few associated formalities. I awakened on New Year’s Day with my new title and the associated responsibility. Past President Steve Simpson, the mensch that he is, sent along with my colluding spouse a lovely and inspirational message for me to peruse, full of thoughtful advice and reflections on his year as President. I don’t know if this has ever been done before, but it is a tradition that I fully intend on continuing at the end of my term.
What has CHEST been up to during the first few months of my tenure? January saw us hold our first Board of Regents meeting for 2022, as well as the meeting of the CHEST Critical Care SEEK editorial board, where they worked to put together Volume 32, which will be out later this year. Watching some of the best and brightest medical minds from around the country discuss hot topics in critical care was a great experience (even if I didn’t have much to offer this august group), but the educational content was secondary to the interactions. Not only are these really smart folks teaching and learning from each other, but many of them are also clearly long-term colleagues, and watching this medical meeting was a lot like watching a reunion of friends who hadn’t seen each other in years. And, it struck me that what I’ve really been missing the most in the context of the social isolation that has accompanied the medical challenges of the pandemic is the pleasure of meeting in person with other folks to share stories, tell jokes, commiserate a bit, and catch up on the time that COVID-19 has stolen from us.
As we move further into 2022, I’m hoping that CHEST and our sister societies can help make up for this lost time by giving us the chance to meet in person once again. And to help build these experiences, we held an experiential design team along with our annual CHEST Program Committee meeting in February. Not only will the 2022 annual meeting in Nashville have the opportunity to hear from and network the best and brightest in pulmonary, critical care, and sleep medicine, but to celebrate our getting back together for the first time in years, we are also putting together some special surprises that CHEST has never done before. Keep an eye out for sneak peaks of these plans later in the spring and summer.
Another of our foci in 2022 is our ongoing push to help historically disenfranchised groups feel more engaged with CHEST. Many of you contributed to last year’s initiative to gather data on the kinds of things that we can do better, and I’ve just put together a presidential task force to develop final recommendations to further our goals of improving diversity, equity, and inclusion and to present to the Board of Regents for our April meeting.
Hopefully, many of you have seen some of the “Pardon the Introduction” series that CHEST has been featuring on its social media channels. We’ve put these together to showcase some of our leadership, their experiences, and opportunities for our members to get more involved with the College. Selfishly, I admit that they have also served as an excuse for me to catch up with some old friends and share our CHEST stories. We will be continuing to produce this series throughout the year; please let us know if there are specific folks you’d like us to feature!
Lastly, I wanted to thank the many of you who have reached out to me with questions, comments, and feedback. One of my main initiatives for the year is to make sure we are meeting the needs of as many of our members as possible, and this is something we can only do well if the lines of communication are wide open. Please continue to reach out to me, either by emailing me at [email protected] or messaging me on Twitter @ChestPrez.
New year, new CHEST President. Same as it has always been, except it has never been this way before. In past years, the transition of the CHEST Presidency occurred at our annual meeting, with a formal handover of leadership and a large reception. While there’s no Presidential football to hand over or secret codes to change for the incoming administration, there are usually several pending issues related to ongoing endeavors that need to be discussed between the outgoing and incoming leadership, in addition to some pearls of wisdom and the figurative “keys to the car.”
Now that CHEST has changed its President’s year to transition alongside the calendar year, there are few associated formalities. I awakened on New Year’s Day with my new title and the associated responsibility. Past President Steve Simpson, the mensch that he is, sent along with my colluding spouse a lovely and inspirational message for me to peruse, full of thoughtful advice and reflections on his year as President. I don’t know if this has ever been done before, but it is a tradition that I fully intend on continuing at the end of my term.
What has CHEST been up to during the first few months of my tenure? January saw us hold our first Board of Regents meeting for 2022, as well as the meeting of the CHEST Critical Care SEEK editorial board, where they worked to put together Volume 32, which will be out later this year. Watching some of the best and brightest medical minds from around the country discuss hot topics in critical care was a great experience (even if I didn’t have much to offer this august group), but the educational content was secondary to the interactions. Not only are these really smart folks teaching and learning from each other, but many of them are also clearly long-term colleagues, and watching this medical meeting was a lot like watching a reunion of friends who hadn’t seen each other in years. And, it struck me that what I’ve really been missing the most in the context of the social isolation that has accompanied the medical challenges of the pandemic is the pleasure of meeting in person with other folks to share stories, tell jokes, commiserate a bit, and catch up on the time that COVID-19 has stolen from us.
As we move further into 2022, I’m hoping that CHEST and our sister societies can help make up for this lost time by giving us the chance to meet in person once again. And to help build these experiences, we held an experiential design team along with our annual CHEST Program Committee meeting in February. Not only will the 2022 annual meeting in Nashville have the opportunity to hear from and network the best and brightest in pulmonary, critical care, and sleep medicine, but to celebrate our getting back together for the first time in years, we are also putting together some special surprises that CHEST has never done before. Keep an eye out for sneak peaks of these plans later in the spring and summer.
Another of our foci in 2022 is our ongoing push to help historically disenfranchised groups feel more engaged with CHEST. Many of you contributed to last year’s initiative to gather data on the kinds of things that we can do better, and I’ve just put together a presidential task force to develop final recommendations to further our goals of improving diversity, equity, and inclusion and to present to the Board of Regents for our April meeting.
Hopefully, many of you have seen some of the “Pardon the Introduction” series that CHEST has been featuring on its social media channels. We’ve put these together to showcase some of our leadership, their experiences, and opportunities for our members to get more involved with the College. Selfishly, I admit that they have also served as an excuse for me to catch up with some old friends and share our CHEST stories. We will be continuing to produce this series throughout the year; please let us know if there are specific folks you’d like us to feature!
Lastly, I wanted to thank the many of you who have reached out to me with questions, comments, and feedback. One of my main initiatives for the year is to make sure we are meeting the needs of as many of our members as possible, and this is something we can only do well if the lines of communication are wide open. Please continue to reach out to me, either by emailing me at [email protected] or messaging me on Twitter @ChestPrez.
Meet our new CHEST President-Designate
We are happy to introduce John (Jack) D. Buckley, MD, MPH, FCCP, who will serve his term as CHEST President in 2024. A pulmonologist and critical care physician with an extensive background in education, he currently serves as the division leader of Pulmonary and Critical Care Medicine for the Henry Ford Medical Group and Health System.
Dr. Buckley received his undergraduate degree from Kalamazoo College and medical degree from Wayne State University. His residency in internal medicine and fellowships in pulmonary and critical care and health services research were completed at Indiana University. He additionally earned a Master of Public Health degree, also from Indiana University.
His impressive academic record includes authoring or co-authoring more than 40 publications and book chapters, as well as presenting over 100 lectures at international conferences. As a former fellowship program training director at two institutions, Dr. Buckley has long been committed to championing and furthering pulmonary and critical care medical education. In a collaboration between the Chinese Thoracic Society and CHEST, he served 6 years on a steering committee to help establish pulmonary and critical care medicine as a subspecialty in China. He and the group assisted with the development of fellowship training programs and presented at several Chinese Thoracic Society annual meetings and board review events.
For Dr. Buckley’s dedication to advancing PCCM education and faculty development, he received the CHEST Master Clinician Educator Award in 2016 and has been an annual Distinguished CHEST Educator (DCE) recipient since the award’s inception in 2017.
Dr. Buckley has been an active and engaged member of CHEST since 1997. He has served in leadership roles across many domains of the organization, including CHEST 2022 Congress Italy, Chair of the CHEST 2013 Scientific Program Committee, Board of Regents, Compensation Committee, Governance Committee, Training and Transitions Committee (Chair, 2011-2012) and Bylaws Committee (Chair, 2010-2012), Honor Lecture and Awards Committee, and the Affiliate NetWork. He currently serves on the CHEST SEEKTM Pulmonary Medicine Editorial Board and is the Chair of the Pulmonary Medicine Board Review.
We look forward to welcoming Dr. Buckley as CHEST President in 2024.
We are happy to introduce John (Jack) D. Buckley, MD, MPH, FCCP, who will serve his term as CHEST President in 2024. A pulmonologist and critical care physician with an extensive background in education, he currently serves as the division leader of Pulmonary and Critical Care Medicine for the Henry Ford Medical Group and Health System.
Dr. Buckley received his undergraduate degree from Kalamazoo College and medical degree from Wayne State University. His residency in internal medicine and fellowships in pulmonary and critical care and health services research were completed at Indiana University. He additionally earned a Master of Public Health degree, also from Indiana University.
His impressive academic record includes authoring or co-authoring more than 40 publications and book chapters, as well as presenting over 100 lectures at international conferences. As a former fellowship program training director at two institutions, Dr. Buckley has long been committed to championing and furthering pulmonary and critical care medical education. In a collaboration between the Chinese Thoracic Society and CHEST, he served 6 years on a steering committee to help establish pulmonary and critical care medicine as a subspecialty in China. He and the group assisted with the development of fellowship training programs and presented at several Chinese Thoracic Society annual meetings and board review events.
For Dr. Buckley’s dedication to advancing PCCM education and faculty development, he received the CHEST Master Clinician Educator Award in 2016 and has been an annual Distinguished CHEST Educator (DCE) recipient since the award’s inception in 2017.
Dr. Buckley has been an active and engaged member of CHEST since 1997. He has served in leadership roles across many domains of the organization, including CHEST 2022 Congress Italy, Chair of the CHEST 2013 Scientific Program Committee, Board of Regents, Compensation Committee, Governance Committee, Training and Transitions Committee (Chair, 2011-2012) and Bylaws Committee (Chair, 2010-2012), Honor Lecture and Awards Committee, and the Affiliate NetWork. He currently serves on the CHEST SEEKTM Pulmonary Medicine Editorial Board and is the Chair of the Pulmonary Medicine Board Review.
We look forward to welcoming Dr. Buckley as CHEST President in 2024.
We are happy to introduce John (Jack) D. Buckley, MD, MPH, FCCP, who will serve his term as CHEST President in 2024. A pulmonologist and critical care physician with an extensive background in education, he currently serves as the division leader of Pulmonary and Critical Care Medicine for the Henry Ford Medical Group and Health System.
Dr. Buckley received his undergraduate degree from Kalamazoo College and medical degree from Wayne State University. His residency in internal medicine and fellowships in pulmonary and critical care and health services research were completed at Indiana University. He additionally earned a Master of Public Health degree, also from Indiana University.
His impressive academic record includes authoring or co-authoring more than 40 publications and book chapters, as well as presenting over 100 lectures at international conferences. As a former fellowship program training director at two institutions, Dr. Buckley has long been committed to championing and furthering pulmonary and critical care medical education. In a collaboration between the Chinese Thoracic Society and CHEST, he served 6 years on a steering committee to help establish pulmonary and critical care medicine as a subspecialty in China. He and the group assisted with the development of fellowship training programs and presented at several Chinese Thoracic Society annual meetings and board review events.
For Dr. Buckley’s dedication to advancing PCCM education and faculty development, he received the CHEST Master Clinician Educator Award in 2016 and has been an annual Distinguished CHEST Educator (DCE) recipient since the award’s inception in 2017.
Dr. Buckley has been an active and engaged member of CHEST since 1997. He has served in leadership roles across many domains of the organization, including CHEST 2022 Congress Italy, Chair of the CHEST 2013 Scientific Program Committee, Board of Regents, Compensation Committee, Governance Committee, Training and Transitions Committee (Chair, 2011-2012) and Bylaws Committee (Chair, 2010-2012), Honor Lecture and Awards Committee, and the Affiliate NetWork. He currently serves on the CHEST SEEKTM Pulmonary Medicine Editorial Board and is the Chair of the Pulmonary Medicine Board Review.
We look forward to welcoming Dr. Buckley as CHEST President in 2024.
A mentor in medicine ... a mentor in life
Edward Carl Rosenow III, MD, Master FCCP
November 2, 1934 - December 21, 2021
We remember our close friend and colleague
On Monday, January 3, 1972, in Rochester, Minnesota, the weather was as expected - a high of 20 F and a low of -50 F. At 7:30 that morning, a group of three young physicians, residents in internal medicine on a month-long rotation in the inpatient pulmonary ward in one of the Mayo Clinic hospitals, was awaiting the arrival of the staff consultant to begin the rounds. It was the very first day of his first-year residency at Mayo for one of the residents. He had applied for residency training to begin in July but, instead, accepted Mayo’s offer to join the residency program 6 months earlier, in January – in Minnesota. That new resident was me. The pulmonary consultant had a friendly and disarming demeanor and gentle visage. He introduced himself to me with a smile, saying, “Welcome to Mayo. I am Ed Rosenow. Let me know if I can be of help in your training.”
Thus began my almost half-century’ relationship with Ed. During my residency in internal medicine and fellowship in pulmonary and critical care medicine, he was a constant and dependable fount of wisdom and knowledge. His daily lectures with chest x-rays after the morning rounds were legendary. By one estimate, he had collected over 4,500 chest x-rays to teach. These were hard copies and heavy to carry around. Ed lugged them under his arms daily for the lectures (there were no digital radiology or CT or MRI scanners then).
Ed was voted the “teacher of the year” every year for countless years. He was my first teacher in bronchoscopy and esophagoscopy. At that time, the division of pulmonary diseases was known as the division of thoracic diseases, and consultants in thoracic diseases performed bronchoscopy and rigid esophagoscopy.
Ed exemplified the best in compassion, amicability, collegiality, thoughtfulness, and a caring personality. In addition to possessing superb clinical acumen, he volunteered in local medical clinics for the less fortunate. In my mind, it is not too farfetched to describe Ed as “A man for all seasons.”*
Among Ed’s many professional accomplishments, his dedication and loyalty to the American College of Chest Physicians (CHEST) and the CHEST Foundation remain unsurpassed. In the years before and after he became the President of CHEST, Ed spent countless hours rewriting the ‘constitution’ of the organization, its bylaws. Many of the current committee structures, rules, and regulations are based on Ed’s work. During a meeting of the regents, one regent exclaimed, ”ACCP is Rosenow and Rosenow is ACCP!”
Ed was a founding member of the CHEST Foundation, the philanthropic arm of the College. Ed’s constant encouragement of young pulmonologists to participate in CHEST surely resulted in a significant increase in their membership. He was the ceaseless force behind my work and deep involvement with CHEST and the CHEST Foundation.
Describing my long association with Ed transcends this note. Suffice it to say that my being named the first Edward W. and Betty Knight Scripps Professor of Medicine in Honor of Edward C. Rosenow III, MD at Mayo Medical School is the greatest honor that I fondly cherish. I like to think that Ed strived for nearly a half-century to help me be a good person and a good doctor. I often question myself if I have met his goal. This question will linger in my mind for the rest of my life.
Udaya B. S. Prakash, MD, Master FCCP, Rochester, MN
Past President, American College of Chest Physicians (2002-2003)
*A man for all seasons: A man who is ready to cope with any contingency and whose behavior is always appropriate to every occasion. The English grammarian Robert Whittington (1480-1553) applied this description to the English statesman and scholar Sir Thomas More (1478-1535), and Robert Bolt used it as the title of his 1960 play about More.
My association with Dr. Rosenow dates back to 2002. I was attending the CHEST annual meeting, and I saw Dr. Rosenow walking toward me. He came up and said, “Hi. My name is Ed Rosenow. What is yours?” “Suhail Raoof,” I answered. Taking me aside, we spent almost a half-hour discussing my family, where I work, my career goals, and how the College could help me achieve some of those goals. His unassuming nature, humility, and sincere desire to help rang out loud and clear.
That day proved to be a turning point in my life. For the next almost 17 years, Ed and I set up monthly calls to connect. Each time, he was eager to listen and know what was happening in my life—the good, the bad, the important, and the mundane. My problems would become his problems; solutions to my problems would become joint solutions. He guided me on my path to leadership with CHEST, culminating in my presidency.
Ed taught thousands of his colleagues the true meaning and power of mentorship. Early in his career, he realized that true happiness comes from helping and guiding others. Dr. Rosenow experienced a sense of genuine happiness and pride in witnessing the accomplishments of his friends and trainees. His gentle ways, unparalleled kindness, and modesty made him the quintessential role model, who one and all tried to emulate.
Aptly stated by Dr. John Studdard, FCCP, one of his students at Mayo Clinic, “Ed Rosenow was the finest doctor I have ever known, but an even better person. He balanced a great intellect and curiosity with great humility, was an incredible teacher, educator, and mentor, and all of this with a special sense of humor.”
Among his many positive traits, Ed possessed two qualities that played very important roles in his life— inquisitiveness and perseverance. In the early 1960s, there was a paucity of information on drug-induced lung disease. He embraced this gap in medical knowledge, resolved to fill it, and, for the next almost 50 years, Dr. Rosenow extensively researched, published, and lectured on drug-related lung injury.
Ed felt strongly that a good pulmonologist had to be a skilled chest radiologist. He was instrumental in introducing “Chest Imaging for the Pulmonologist” sessions at the annual CHEST meetings. With his enduring cataloging of consultation cases and collection of teaching file chest x-rays, it is no wonder that he amassed one of the best teaching resources, including some of the most rare lung conditions.
Ed was a visionary. He envisioned CHEST to be a closely knit “family of professionals,” united in the desire to provide compassionate care of the highest order to patients and help each colleague accomplish their goals and aspirations. During his CHEST presidency, he and Dr. Bart Chernow realized the importance of having a philanthropic arm of the College that would support worthy projects through fundraising. Soon after the establishment of the CHEST Foundation, he became its President and then Chair.
Dr. Rosenow’s hard work, dedication, and unwavering commitment to professional and social organizations he served earned him the highest of accolades and honors. He had the rare distinction of being recognized as a Master by two professional organizations—CHEST and the American College of Physicians. Awards of the highest order were showered upon him by the Mayo Clinic, including establishing the Mayo Fellows Hall of Fame of Outstanding Teachers. Several endowed professorships and honors are named after him. The award he cherished most was the Karis Award (karis meaning “to care” in Greek). When I asked him how he felt to be the recipient of so many awards, he blushed and said, “Gee, there were plenty others who deserved them more than me. I was just doing my job.”
To everyone he met, Ed emphasized the importance of the “culture of caring and giving.” He taught his students that medicine is not a profession; it is a way of life. It is as much an art as it is a science. He reiterated his platinum rule to “Take care of every patient like you would want a member of your family cared for.”
Today, thousands of his students, including me, are deeply indebted to Dr. Rosenow for the impactful and profound role he played in our lives and for teaching us the core values that really matter. He left an indelible mark on our profession and our outlook. He redefined our responsibilities to our patients and colleagues. In his own quiet and effective way, Ed nurtured and inspired us to dream, think, persevere, and accomplish. His legacy will live on as we try to emulate his teachings, exceptional qualities, and humanistic approach. He will be missed greatly.
“His life was gentle, and the elements mixed so well in him that Nature might stand up and say to all the world,” ‘This was a man’.” Shakespeare
Suhail Raoof, MD, Master FCCP, New York, NY
Past President, American College of Chest Physicians (2011-2012)
Edward Carl Rosenow III, MD, Master FCCP
November 2, 1934 - December 21, 2021
We remember our close friend and colleague
On Monday, January 3, 1972, in Rochester, Minnesota, the weather was as expected - a high of 20 F and a low of -50 F. At 7:30 that morning, a group of three young physicians, residents in internal medicine on a month-long rotation in the inpatient pulmonary ward in one of the Mayo Clinic hospitals, was awaiting the arrival of the staff consultant to begin the rounds. It was the very first day of his first-year residency at Mayo for one of the residents. He had applied for residency training to begin in July but, instead, accepted Mayo’s offer to join the residency program 6 months earlier, in January – in Minnesota. That new resident was me. The pulmonary consultant had a friendly and disarming demeanor and gentle visage. He introduced himself to me with a smile, saying, “Welcome to Mayo. I am Ed Rosenow. Let me know if I can be of help in your training.”
Thus began my almost half-century’ relationship with Ed. During my residency in internal medicine and fellowship in pulmonary and critical care medicine, he was a constant and dependable fount of wisdom and knowledge. His daily lectures with chest x-rays after the morning rounds were legendary. By one estimate, he had collected over 4,500 chest x-rays to teach. These were hard copies and heavy to carry around. Ed lugged them under his arms daily for the lectures (there were no digital radiology or CT or MRI scanners then).
Ed was voted the “teacher of the year” every year for countless years. He was my first teacher in bronchoscopy and esophagoscopy. At that time, the division of pulmonary diseases was known as the division of thoracic diseases, and consultants in thoracic diseases performed bronchoscopy and rigid esophagoscopy.
Ed exemplified the best in compassion, amicability, collegiality, thoughtfulness, and a caring personality. In addition to possessing superb clinical acumen, he volunteered in local medical clinics for the less fortunate. In my mind, it is not too farfetched to describe Ed as “A man for all seasons.”*
Among Ed’s many professional accomplishments, his dedication and loyalty to the American College of Chest Physicians (CHEST) and the CHEST Foundation remain unsurpassed. In the years before and after he became the President of CHEST, Ed spent countless hours rewriting the ‘constitution’ of the organization, its bylaws. Many of the current committee structures, rules, and regulations are based on Ed’s work. During a meeting of the regents, one regent exclaimed, ”ACCP is Rosenow and Rosenow is ACCP!”
Ed was a founding member of the CHEST Foundation, the philanthropic arm of the College. Ed’s constant encouragement of young pulmonologists to participate in CHEST surely resulted in a significant increase in their membership. He was the ceaseless force behind my work and deep involvement with CHEST and the CHEST Foundation.
Describing my long association with Ed transcends this note. Suffice it to say that my being named the first Edward W. and Betty Knight Scripps Professor of Medicine in Honor of Edward C. Rosenow III, MD at Mayo Medical School is the greatest honor that I fondly cherish. I like to think that Ed strived for nearly a half-century to help me be a good person and a good doctor. I often question myself if I have met his goal. This question will linger in my mind for the rest of my life.
Udaya B. S. Prakash, MD, Master FCCP, Rochester, MN
Past President, American College of Chest Physicians (2002-2003)
*A man for all seasons: A man who is ready to cope with any contingency and whose behavior is always appropriate to every occasion. The English grammarian Robert Whittington (1480-1553) applied this description to the English statesman and scholar Sir Thomas More (1478-1535), and Robert Bolt used it as the title of his 1960 play about More.
My association with Dr. Rosenow dates back to 2002. I was attending the CHEST annual meeting, and I saw Dr. Rosenow walking toward me. He came up and said, “Hi. My name is Ed Rosenow. What is yours?” “Suhail Raoof,” I answered. Taking me aside, we spent almost a half-hour discussing my family, where I work, my career goals, and how the College could help me achieve some of those goals. His unassuming nature, humility, and sincere desire to help rang out loud and clear.
That day proved to be a turning point in my life. For the next almost 17 years, Ed and I set up monthly calls to connect. Each time, he was eager to listen and know what was happening in my life—the good, the bad, the important, and the mundane. My problems would become his problems; solutions to my problems would become joint solutions. He guided me on my path to leadership with CHEST, culminating in my presidency.
Ed taught thousands of his colleagues the true meaning and power of mentorship. Early in his career, he realized that true happiness comes from helping and guiding others. Dr. Rosenow experienced a sense of genuine happiness and pride in witnessing the accomplishments of his friends and trainees. His gentle ways, unparalleled kindness, and modesty made him the quintessential role model, who one and all tried to emulate.
Aptly stated by Dr. John Studdard, FCCP, one of his students at Mayo Clinic, “Ed Rosenow was the finest doctor I have ever known, but an even better person. He balanced a great intellect and curiosity with great humility, was an incredible teacher, educator, and mentor, and all of this with a special sense of humor.”
Among his many positive traits, Ed possessed two qualities that played very important roles in his life— inquisitiveness and perseverance. In the early 1960s, there was a paucity of information on drug-induced lung disease. He embraced this gap in medical knowledge, resolved to fill it, and, for the next almost 50 years, Dr. Rosenow extensively researched, published, and lectured on drug-related lung injury.
Ed felt strongly that a good pulmonologist had to be a skilled chest radiologist. He was instrumental in introducing “Chest Imaging for the Pulmonologist” sessions at the annual CHEST meetings. With his enduring cataloging of consultation cases and collection of teaching file chest x-rays, it is no wonder that he amassed one of the best teaching resources, including some of the most rare lung conditions.
Ed was a visionary. He envisioned CHEST to be a closely knit “family of professionals,” united in the desire to provide compassionate care of the highest order to patients and help each colleague accomplish their goals and aspirations. During his CHEST presidency, he and Dr. Bart Chernow realized the importance of having a philanthropic arm of the College that would support worthy projects through fundraising. Soon after the establishment of the CHEST Foundation, he became its President and then Chair.
Dr. Rosenow’s hard work, dedication, and unwavering commitment to professional and social organizations he served earned him the highest of accolades and honors. He had the rare distinction of being recognized as a Master by two professional organizations—CHEST and the American College of Physicians. Awards of the highest order were showered upon him by the Mayo Clinic, including establishing the Mayo Fellows Hall of Fame of Outstanding Teachers. Several endowed professorships and honors are named after him. The award he cherished most was the Karis Award (karis meaning “to care” in Greek). When I asked him how he felt to be the recipient of so many awards, he blushed and said, “Gee, there were plenty others who deserved them more than me. I was just doing my job.”
To everyone he met, Ed emphasized the importance of the “culture of caring and giving.” He taught his students that medicine is not a profession; it is a way of life. It is as much an art as it is a science. He reiterated his platinum rule to “Take care of every patient like you would want a member of your family cared for.”
Today, thousands of his students, including me, are deeply indebted to Dr. Rosenow for the impactful and profound role he played in our lives and for teaching us the core values that really matter. He left an indelible mark on our profession and our outlook. He redefined our responsibilities to our patients and colleagues. In his own quiet and effective way, Ed nurtured and inspired us to dream, think, persevere, and accomplish. His legacy will live on as we try to emulate his teachings, exceptional qualities, and humanistic approach. He will be missed greatly.
“His life was gentle, and the elements mixed so well in him that Nature might stand up and say to all the world,” ‘This was a man’.” Shakespeare
Suhail Raoof, MD, Master FCCP, New York, NY
Past President, American College of Chest Physicians (2011-2012)
Edward Carl Rosenow III, MD, Master FCCP
November 2, 1934 - December 21, 2021
We remember our close friend and colleague
On Monday, January 3, 1972, in Rochester, Minnesota, the weather was as expected - a high of 20 F and a low of -50 F. At 7:30 that morning, a group of three young physicians, residents in internal medicine on a month-long rotation in the inpatient pulmonary ward in one of the Mayo Clinic hospitals, was awaiting the arrival of the staff consultant to begin the rounds. It was the very first day of his first-year residency at Mayo for one of the residents. He had applied for residency training to begin in July but, instead, accepted Mayo’s offer to join the residency program 6 months earlier, in January – in Minnesota. That new resident was me. The pulmonary consultant had a friendly and disarming demeanor and gentle visage. He introduced himself to me with a smile, saying, “Welcome to Mayo. I am Ed Rosenow. Let me know if I can be of help in your training.”
Thus began my almost half-century’ relationship with Ed. During my residency in internal medicine and fellowship in pulmonary and critical care medicine, he was a constant and dependable fount of wisdom and knowledge. His daily lectures with chest x-rays after the morning rounds were legendary. By one estimate, he had collected over 4,500 chest x-rays to teach. These were hard copies and heavy to carry around. Ed lugged them under his arms daily for the lectures (there were no digital radiology or CT or MRI scanners then).
Ed was voted the “teacher of the year” every year for countless years. He was my first teacher in bronchoscopy and esophagoscopy. At that time, the division of pulmonary diseases was known as the division of thoracic diseases, and consultants in thoracic diseases performed bronchoscopy and rigid esophagoscopy.
Ed exemplified the best in compassion, amicability, collegiality, thoughtfulness, and a caring personality. In addition to possessing superb clinical acumen, he volunteered in local medical clinics for the less fortunate. In my mind, it is not too farfetched to describe Ed as “A man for all seasons.”*
Among Ed’s many professional accomplishments, his dedication and loyalty to the American College of Chest Physicians (CHEST) and the CHEST Foundation remain unsurpassed. In the years before and after he became the President of CHEST, Ed spent countless hours rewriting the ‘constitution’ of the organization, its bylaws. Many of the current committee structures, rules, and regulations are based on Ed’s work. During a meeting of the regents, one regent exclaimed, ”ACCP is Rosenow and Rosenow is ACCP!”
Ed was a founding member of the CHEST Foundation, the philanthropic arm of the College. Ed’s constant encouragement of young pulmonologists to participate in CHEST surely resulted in a significant increase in their membership. He was the ceaseless force behind my work and deep involvement with CHEST and the CHEST Foundation.
Describing my long association with Ed transcends this note. Suffice it to say that my being named the first Edward W. and Betty Knight Scripps Professor of Medicine in Honor of Edward C. Rosenow III, MD at Mayo Medical School is the greatest honor that I fondly cherish. I like to think that Ed strived for nearly a half-century to help me be a good person and a good doctor. I often question myself if I have met his goal. This question will linger in my mind for the rest of my life.
Udaya B. S. Prakash, MD, Master FCCP, Rochester, MN
Past President, American College of Chest Physicians (2002-2003)
*A man for all seasons: A man who is ready to cope with any contingency and whose behavior is always appropriate to every occasion. The English grammarian Robert Whittington (1480-1553) applied this description to the English statesman and scholar Sir Thomas More (1478-1535), and Robert Bolt used it as the title of his 1960 play about More.
My association with Dr. Rosenow dates back to 2002. I was attending the CHEST annual meeting, and I saw Dr. Rosenow walking toward me. He came up and said, “Hi. My name is Ed Rosenow. What is yours?” “Suhail Raoof,” I answered. Taking me aside, we spent almost a half-hour discussing my family, where I work, my career goals, and how the College could help me achieve some of those goals. His unassuming nature, humility, and sincere desire to help rang out loud and clear.
That day proved to be a turning point in my life. For the next almost 17 years, Ed and I set up monthly calls to connect. Each time, he was eager to listen and know what was happening in my life—the good, the bad, the important, and the mundane. My problems would become his problems; solutions to my problems would become joint solutions. He guided me on my path to leadership with CHEST, culminating in my presidency.
Ed taught thousands of his colleagues the true meaning and power of mentorship. Early in his career, he realized that true happiness comes from helping and guiding others. Dr. Rosenow experienced a sense of genuine happiness and pride in witnessing the accomplishments of his friends and trainees. His gentle ways, unparalleled kindness, and modesty made him the quintessential role model, who one and all tried to emulate.
Aptly stated by Dr. John Studdard, FCCP, one of his students at Mayo Clinic, “Ed Rosenow was the finest doctor I have ever known, but an even better person. He balanced a great intellect and curiosity with great humility, was an incredible teacher, educator, and mentor, and all of this with a special sense of humor.”
Among his many positive traits, Ed possessed two qualities that played very important roles in his life— inquisitiveness and perseverance. In the early 1960s, there was a paucity of information on drug-induced lung disease. He embraced this gap in medical knowledge, resolved to fill it, and, for the next almost 50 years, Dr. Rosenow extensively researched, published, and lectured on drug-related lung injury.
Ed felt strongly that a good pulmonologist had to be a skilled chest radiologist. He was instrumental in introducing “Chest Imaging for the Pulmonologist” sessions at the annual CHEST meetings. With his enduring cataloging of consultation cases and collection of teaching file chest x-rays, it is no wonder that he amassed one of the best teaching resources, including some of the most rare lung conditions.
Ed was a visionary. He envisioned CHEST to be a closely knit “family of professionals,” united in the desire to provide compassionate care of the highest order to patients and help each colleague accomplish their goals and aspirations. During his CHEST presidency, he and Dr. Bart Chernow realized the importance of having a philanthropic arm of the College that would support worthy projects through fundraising. Soon after the establishment of the CHEST Foundation, he became its President and then Chair.
Dr. Rosenow’s hard work, dedication, and unwavering commitment to professional and social organizations he served earned him the highest of accolades and honors. He had the rare distinction of being recognized as a Master by two professional organizations—CHEST and the American College of Physicians. Awards of the highest order were showered upon him by the Mayo Clinic, including establishing the Mayo Fellows Hall of Fame of Outstanding Teachers. Several endowed professorships and honors are named after him. The award he cherished most was the Karis Award (karis meaning “to care” in Greek). When I asked him how he felt to be the recipient of so many awards, he blushed and said, “Gee, there were plenty others who deserved them more than me. I was just doing my job.”
To everyone he met, Ed emphasized the importance of the “culture of caring and giving.” He taught his students that medicine is not a profession; it is a way of life. It is as much an art as it is a science. He reiterated his platinum rule to “Take care of every patient like you would want a member of your family cared for.”
Today, thousands of his students, including me, are deeply indebted to Dr. Rosenow for the impactful and profound role he played in our lives and for teaching us the core values that really matter. He left an indelible mark on our profession and our outlook. He redefined our responsibilities to our patients and colleagues. In his own quiet and effective way, Ed nurtured and inspired us to dream, think, persevere, and accomplish. His legacy will live on as we try to emulate his teachings, exceptional qualities, and humanistic approach. He will be missed greatly.
“His life was gentle, and the elements mixed so well in him that Nature might stand up and say to all the world,” ‘This was a man’.” Shakespeare
Suhail Raoof, MD, Master FCCP, New York, NY
Past President, American College of Chest Physicians (2011-2012)
Edward C. Rosenow III, MD, Master FCCP/Master Endowment - Master Teacher Endowment Lecture
The legacy and impact of Ed Rosenow, MD, Master FCCP, will never be forgotten. CHEST nominates and recognizes those physicians who embody that passion and commitment of Dr. Rosenow with an awarded lecture fully funded by the Ed Rosenow, MD, Master FCCP Endowment through the CHEST Foundation. Be a part of Dr. Rosenow’s legacy and make a donation in his memory to the Rosenow Endowment today at chestfoundation.org.
The legacy and impact of Ed Rosenow, MD, Master FCCP, will never be forgotten. CHEST nominates and recognizes those physicians who embody that passion and commitment of Dr. Rosenow with an awarded lecture fully funded by the Ed Rosenow, MD, Master FCCP Endowment through the CHEST Foundation. Be a part of Dr. Rosenow’s legacy and make a donation in his memory to the Rosenow Endowment today at chestfoundation.org.
The legacy and impact of Ed Rosenow, MD, Master FCCP, will never be forgotten. CHEST nominates and recognizes those physicians who embody that passion and commitment of Dr. Rosenow with an awarded lecture fully funded by the Ed Rosenow, MD, Master FCCP Endowment through the CHEST Foundation. Be a part of Dr. Rosenow’s legacy and make a donation in his memory to the Rosenow Endowment today at chestfoundation.org.
Partnership news from the CHEST Foundation: New grant concentrated on diversity, equity, and inclusion
American College of Chest Physicians, American Thoracic Society, and American Lung Association partner to support historically marginalized physician-scientists targeting lung disease
The American College of Chest Physicians (CHEST), the American Thoracic Society, and the American Lung Association are pleased to announce that they are partnering to sponsor a scholar in pulmonary and critical care medicine in the prestigious Harold Amos Medical Faculty Development Program (AMFDP), a Robert Wood Johnson Foundation initiative.
Developed to increase the pool of applicants from historically marginalized backgrounds pursuing careers in medicine, dentistry, or nursing, the AMFDP invites applicants to apply each year to help shape medicine into a more equitable, more accessible practice.
Together, CHEST, ATS, and American Lung Association will provide funding for awards of $420,000 over 4 years to support pulmonary/critical care medicine scholars.
“I am immensely proud to be leading an initiative that has continued to help shape the careers of so many physician-scientists in such a meaningful way,” said David Wilkes, MD, National Director of the Harold Amos Medical Faculty Development Program for the Robert Wood Johnson Foundation, and a member of ATS and CHEST. “That these three highly respected respiratory societies are joining efforts to help fulfill the AMFDP’s mission speaks volumes about their commitment as allies and influencers in the quest to eliminate lung health disparities. This is a model for other specialty societies to collaborate on addressing disparities.”
“In the context of an increasingly diverse population, it is more important than ever that our patients have confidence and trust in those who care for them, something that will be easier to develop as we diversify our workforce,” said CHEST President David Schulman, MD, MPH, FCCP. “CHEST is incredibly excited to be working with the American Lung Association, the American Thoracic Society, and the Harold Amos Medical Faculty Development Program to fund training for individuals who have been traditionally underrepresented in medicine as they pursue careers in pulmonary and critical care medicine.”
“Health equity is woven into the fabric of the ATS,” said ATS President Lynn Schnapp, MD, ATSF. “And, partnering with our peers in the pulmonary and critical care space is a wonderful opportunity to advance our shared goal of cultivating the next generation of leaders in health access and equity.”
“The American Lung Association has historically funded researchers at the beginning of their careers, helping to build the foundation for the next great group of leaders,” said Albert Rizzo, MD, Chief Medical Officer for the Lung Association. “It is critical to the advancement of lung health and the care of patients to have physicians and scientists from diverse backgrounds, so we are honored to provide support for these individuals and increase diversity in pulmonary medicine.”
The call for application is now open. To learn more and to apply go to rwjf.org.
American College of Chest Physicians, American Thoracic Society, and American Lung Association partner to support historically marginalized physician-scientists targeting lung disease
American College of Chest Physicians, American Thoracic Society, and American Lung Association partner to support historically marginalized physician-scientists targeting lung disease
The American College of Chest Physicians (CHEST), the American Thoracic Society, and the American Lung Association are pleased to announce that they are partnering to sponsor a scholar in pulmonary and critical care medicine in the prestigious Harold Amos Medical Faculty Development Program (AMFDP), a Robert Wood Johnson Foundation initiative.
Developed to increase the pool of applicants from historically marginalized backgrounds pursuing careers in medicine, dentistry, or nursing, the AMFDP invites applicants to apply each year to help shape medicine into a more equitable, more accessible practice.
Together, CHEST, ATS, and American Lung Association will provide funding for awards of $420,000 over 4 years to support pulmonary/critical care medicine scholars.
“I am immensely proud to be leading an initiative that has continued to help shape the careers of so many physician-scientists in such a meaningful way,” said David Wilkes, MD, National Director of the Harold Amos Medical Faculty Development Program for the Robert Wood Johnson Foundation, and a member of ATS and CHEST. “That these three highly respected respiratory societies are joining efforts to help fulfill the AMFDP’s mission speaks volumes about their commitment as allies and influencers in the quest to eliminate lung health disparities. This is a model for other specialty societies to collaborate on addressing disparities.”
“In the context of an increasingly diverse population, it is more important than ever that our patients have confidence and trust in those who care for them, something that will be easier to develop as we diversify our workforce,” said CHEST President David Schulman, MD, MPH, FCCP. “CHEST is incredibly excited to be working with the American Lung Association, the American Thoracic Society, and the Harold Amos Medical Faculty Development Program to fund training for individuals who have been traditionally underrepresented in medicine as they pursue careers in pulmonary and critical care medicine.”
“Health equity is woven into the fabric of the ATS,” said ATS President Lynn Schnapp, MD, ATSF. “And, partnering with our peers in the pulmonary and critical care space is a wonderful opportunity to advance our shared goal of cultivating the next generation of leaders in health access and equity.”
“The American Lung Association has historically funded researchers at the beginning of their careers, helping to build the foundation for the next great group of leaders,” said Albert Rizzo, MD, Chief Medical Officer for the Lung Association. “It is critical to the advancement of lung health and the care of patients to have physicians and scientists from diverse backgrounds, so we are honored to provide support for these individuals and increase diversity in pulmonary medicine.”
The call for application is now open. To learn more and to apply go to rwjf.org.
The American College of Chest Physicians (CHEST), the American Thoracic Society, and the American Lung Association are pleased to announce that they are partnering to sponsor a scholar in pulmonary and critical care medicine in the prestigious Harold Amos Medical Faculty Development Program (AMFDP), a Robert Wood Johnson Foundation initiative.
Developed to increase the pool of applicants from historically marginalized backgrounds pursuing careers in medicine, dentistry, or nursing, the AMFDP invites applicants to apply each year to help shape medicine into a more equitable, more accessible practice.
Together, CHEST, ATS, and American Lung Association will provide funding for awards of $420,000 over 4 years to support pulmonary/critical care medicine scholars.
“I am immensely proud to be leading an initiative that has continued to help shape the careers of so many physician-scientists in such a meaningful way,” said David Wilkes, MD, National Director of the Harold Amos Medical Faculty Development Program for the Robert Wood Johnson Foundation, and a member of ATS and CHEST. “That these three highly respected respiratory societies are joining efforts to help fulfill the AMFDP’s mission speaks volumes about their commitment as allies and influencers in the quest to eliminate lung health disparities. This is a model for other specialty societies to collaborate on addressing disparities.”
“In the context of an increasingly diverse population, it is more important than ever that our patients have confidence and trust in those who care for them, something that will be easier to develop as we diversify our workforce,” said CHEST President David Schulman, MD, MPH, FCCP. “CHEST is incredibly excited to be working with the American Lung Association, the American Thoracic Society, and the Harold Amos Medical Faculty Development Program to fund training for individuals who have been traditionally underrepresented in medicine as they pursue careers in pulmonary and critical care medicine.”
“Health equity is woven into the fabric of the ATS,” said ATS President Lynn Schnapp, MD, ATSF. “And, partnering with our peers in the pulmonary and critical care space is a wonderful opportunity to advance our shared goal of cultivating the next generation of leaders in health access and equity.”
“The American Lung Association has historically funded researchers at the beginning of their careers, helping to build the foundation for the next great group of leaders,” said Albert Rizzo, MD, Chief Medical Officer for the Lung Association. “It is critical to the advancement of lung health and the care of patients to have physicians and scientists from diverse backgrounds, so we are honored to provide support for these individuals and increase diversity in pulmonary medicine.”
The call for application is now open. To learn more and to apply go to rwjf.org.