User login
Busting three myths about planned giving
Gifts to charitable organizations, such as the AGA Research Foundation, in your future plans can ensure that your support for our mission to fund young investigators will continue even after your lifetime. See these three fast facts about planned giving.
- Planned gifts are complicated and confusing. They don’t have to be. There are many types of planned gifts: Most are simple and affordable, like a gift in your will or living trust. You just need to find the one that best meets your needs.
- Wills are only for older adults. Having a plan for the future is important – no matter your age. A will makes your wishes known and provides your loved ones with peace of mind.
- Planned gifts are only for the wealthy. Anyone can make a planned gift. Gifts of all sizes make a difference at the AGA Research Foundation. In fact, you may even be able to make a bigger impact than you thought possible when you make a planned gift.
For 2022, consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI.
Want to learn more about including a gift to the AGA Research Foundation in your plans? Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
Gifts to charitable organizations, such as the AGA Research Foundation, in your future plans can ensure that your support for our mission to fund young investigators will continue even after your lifetime. See these three fast facts about planned giving.
- Planned gifts are complicated and confusing. They don’t have to be. There are many types of planned gifts: Most are simple and affordable, like a gift in your will or living trust. You just need to find the one that best meets your needs.
- Wills are only for older adults. Having a plan for the future is important – no matter your age. A will makes your wishes known and provides your loved ones with peace of mind.
- Planned gifts are only for the wealthy. Anyone can make a planned gift. Gifts of all sizes make a difference at the AGA Research Foundation. In fact, you may even be able to make a bigger impact than you thought possible when you make a planned gift.
For 2022, consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI.
Want to learn more about including a gift to the AGA Research Foundation in your plans? Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
Gifts to charitable organizations, such as the AGA Research Foundation, in your future plans can ensure that your support for our mission to fund young investigators will continue even after your lifetime. See these three fast facts about planned giving.
- Planned gifts are complicated and confusing. They don’t have to be. There are many types of planned gifts: Most are simple and affordable, like a gift in your will or living trust. You just need to find the one that best meets your needs.
- Wills are only for older adults. Having a plan for the future is important – no matter your age. A will makes your wishes known and provides your loved ones with peace of mind.
- Planned gifts are only for the wealthy. Anyone can make a planned gift. Gifts of all sizes make a difference at the AGA Research Foundation. In fact, you may even be able to make a bigger impact than you thought possible when you make a planned gift.
For 2022, consider including a gift to the AGA Research Foundation in your will. You will help spark future discoveries in GI.
Want to learn more about including a gift to the AGA Research Foundation in your plans? Visit our website at https://gastro.planmylegacy.org or contact us at [email protected].
Meet the new CHEST Physician Editor in Chief
Angel O. Coz Yataco, MD, FCCP, is a Pulmonary and Critical Care specialist at the Respiratory Institute at the Cleveland Clinic. He previously served as the Medical Director of the Intensive Care Unit at the Lexington Veterans Affairs Medical Center and was an Associate Professor of Medicine at the University of Kentucky. Dr. Coz received his medical degree from Universidad Peruana Cayetano Heredia in Lima, Peru. He completed residency training in internal medicine and did his fellowship training in pulmonary and critical care medicine at Henry Ford Hospital.
Dr. Coz was a member of the 2021 Surviving Sepsis Campaign Guidelines panel and serves on the American Board of Internal Medicine Governance – Critical Care Medicine examination board. He holds multiple leadership positions at CHEST—Chair of the Council of NetWorks; a member of the Guidelines Oversight Committee; and served as the Critical Care Section Editor for CHEST Physician since 2018. He has been awarded the Distinguished CHEST Educator (DCE) designation every year since its inception in 2018 and received the CHEST Presidential Citation Award in 2021.
Dr. Coz has given multiple talks on critical care, sepsis, and pulmonary topics at the national and international level. He has published several peer-reviewed articles and serves as ad hoc reviewer for CHEST, Journal of Critical Care, Critical Care Medicine, Critical Connections, Intensive Care Medicine, and Annals of Pharmacotherapy, among others.
Angel O. Coz Yataco, MD, FCCP, is a Pulmonary and Critical Care specialist at the Respiratory Institute at the Cleveland Clinic. He previously served as the Medical Director of the Intensive Care Unit at the Lexington Veterans Affairs Medical Center and was an Associate Professor of Medicine at the University of Kentucky. Dr. Coz received his medical degree from Universidad Peruana Cayetano Heredia in Lima, Peru. He completed residency training in internal medicine and did his fellowship training in pulmonary and critical care medicine at Henry Ford Hospital.
Dr. Coz was a member of the 2021 Surviving Sepsis Campaign Guidelines panel and serves on the American Board of Internal Medicine Governance – Critical Care Medicine examination board. He holds multiple leadership positions at CHEST—Chair of the Council of NetWorks; a member of the Guidelines Oversight Committee; and served as the Critical Care Section Editor for CHEST Physician since 2018. He has been awarded the Distinguished CHEST Educator (DCE) designation every year since its inception in 2018 and received the CHEST Presidential Citation Award in 2021.
Dr. Coz has given multiple talks on critical care, sepsis, and pulmonary topics at the national and international level. He has published several peer-reviewed articles and serves as ad hoc reviewer for CHEST, Journal of Critical Care, Critical Care Medicine, Critical Connections, Intensive Care Medicine, and Annals of Pharmacotherapy, among others.
Angel O. Coz Yataco, MD, FCCP, is a Pulmonary and Critical Care specialist at the Respiratory Institute at the Cleveland Clinic. He previously served as the Medical Director of the Intensive Care Unit at the Lexington Veterans Affairs Medical Center and was an Associate Professor of Medicine at the University of Kentucky. Dr. Coz received his medical degree from Universidad Peruana Cayetano Heredia in Lima, Peru. He completed residency training in internal medicine and did his fellowship training in pulmonary and critical care medicine at Henry Ford Hospital.
Dr. Coz was a member of the 2021 Surviving Sepsis Campaign Guidelines panel and serves on the American Board of Internal Medicine Governance – Critical Care Medicine examination board. He holds multiple leadership positions at CHEST—Chair of the Council of NetWorks; a member of the Guidelines Oversight Committee; and served as the Critical Care Section Editor for CHEST Physician since 2018. He has been awarded the Distinguished CHEST Educator (DCE) designation every year since its inception in 2018 and received the CHEST Presidential Citation Award in 2021.
Dr. Coz has given multiple talks on critical care, sepsis, and pulmonary topics at the national and international level. He has published several peer-reviewed articles and serves as ad hoc reviewer for CHEST, Journal of Critical Care, Critical Care Medicine, Critical Connections, Intensive Care Medicine, and Annals of Pharmacotherapy, among others.
Welcome our new board members
Humayun Anjum, MD
Dr. Anjum is currently working as a pulmonary and critical care physician at Baylor Scott & White Medical Center- Grapevine in Dallas, Texas.
He is an Adjunct Clinical Assistant Professor at University of Houston and University of North Texas. He recently moved to Dallas from Corpus Christi, Texas where, he served as the core faculty for the Internal Medicine residency program and the Pulmonary Disease fellowship program. He is passionate about learning and teaching and has been very intricately involved with CHEST and the CHEST Foundation for the last few years. Currently, he serves as the chair of the Practice Operations Network steering committee. Dr. Anjum is particularly interested in medical practice management and administration and hopes to continue sharing his knowledge through various platforms to help his fellow physicians.
Loren J. Harris, MD FACS FCCP
Dr. Harris is the Chairman of the Department of Surgery and Chief of Thoracic Surgery at Richmond University Medical Center in Staten Island, NY.
He has been in clinical surgical practice for over 20 years and also has over 20 years of experience teaching both medical students and surgical residents and fellows. In addition, he served as Program Director of the general surgery residency program at Maimonides Medical Center from 2014 to 2017. Dr. Harris has published and presented throughout his career both nationally and internationally. His main research and clinical interests are in the appropriate staging and treatment of non-small cell lung cancer. He served as the Chair of the CHEST Marketing Committee; was the editor Pulmonary Perspectives; and is a co-author on two chapters in the most recent edition of the Diagnosis and Management Guidelines for Lung Cancer published by CHEST in 2013. Dr. Harris has also received several prestigious awards including the CHEST Soffer Award for Editorial Excellence.
Diego Maselli, MD
Dr. Maselli is an Associate Professor of Medicine in the Division of Pulmonary Diseases & Critical Care Medicine at UT Health in San Antonio.
He is the director of the Severe Asthma Program at UT Health and his research focuses on severe asthma, COPD, and bronchiectasis. Dr. Maselli has been designated a Distinguished CHEST Educator since 2017 when the program was initiated. He serves on the steering committee of the Airways Network.
Daniel R. Ouellette, MD
Dr. Ouellette has been a clinician, teacher, and researcher in pulmonary and critical care medicine for 35 years.
He is currently a Senior Staff Physician at Henry Ford Hospital in Detroit where he is the Medical Director for the Pulmonary Ward. He is also an Associate Clinical Professor of Medicine at the Wayne State University School of Medicine, and the Medical Director of the Respiratory Therapy program at Oakland Community College. Dr. Ouellette has over 20 years of military service and was the Consultant to the US Army Surgeon General for Pulmonary Medicine during the last several years of his military career. An active CHEST leader, he has chaired the Guideline Oversight Committee, the Clinical Pulmonary Network, and the Council of Governors, has been a member of the Board of Regents, and held many leadership roles with CHEST and other societies in the development of evidence-based clinical practice guidelines. Dr. Ouellette’s clinical areas of interest include general pulmonary and critical care medicine and evidence-based practice.
Saiprakash Venkateshiah, MD, FCCP
Dr. Venkateshiah is an Associate Professor of Medicine in the Division of Pulmonary, Allergy, Critical Care and Sleep Medicine at Emory University, Atlanta, GA.
He is a clinician educator and a “general pulmonologist” practicing the entire gamut of pulmonary, critical care, and sleep medicine. Dr. Venkateshiah has been a CHEST member for close to 2 decades. He has been involved with CHEST NetWork leadership since 2012, starting as steering committee member of Clinical Pulmonary Medicine Network transitioning to Vice-Chair and Chair. He was previously a member of the Executive Committee of the Council of Networks and the Scientific Program Committee for CHEST 2019 and CHEST 2020. He is currently a steering committee member of the education committees of CHEST and American Academy of Sleep Medicine. He is also a steering committee member of the CHEST Sleep NetWork.
Humayun Anjum, MD
Dr. Anjum is currently working as a pulmonary and critical care physician at Baylor Scott & White Medical Center- Grapevine in Dallas, Texas.
He is an Adjunct Clinical Assistant Professor at University of Houston and University of North Texas. He recently moved to Dallas from Corpus Christi, Texas where, he served as the core faculty for the Internal Medicine residency program and the Pulmonary Disease fellowship program. He is passionate about learning and teaching and has been very intricately involved with CHEST and the CHEST Foundation for the last few years. Currently, he serves as the chair of the Practice Operations Network steering committee. Dr. Anjum is particularly interested in medical practice management and administration and hopes to continue sharing his knowledge through various platforms to help his fellow physicians.
Loren J. Harris, MD FACS FCCP
Dr. Harris is the Chairman of the Department of Surgery and Chief of Thoracic Surgery at Richmond University Medical Center in Staten Island, NY.
He has been in clinical surgical practice for over 20 years and also has over 20 years of experience teaching both medical students and surgical residents and fellows. In addition, he served as Program Director of the general surgery residency program at Maimonides Medical Center from 2014 to 2017. Dr. Harris has published and presented throughout his career both nationally and internationally. His main research and clinical interests are in the appropriate staging and treatment of non-small cell lung cancer. He served as the Chair of the CHEST Marketing Committee; was the editor Pulmonary Perspectives; and is a co-author on two chapters in the most recent edition of the Diagnosis and Management Guidelines for Lung Cancer published by CHEST in 2013. Dr. Harris has also received several prestigious awards including the CHEST Soffer Award for Editorial Excellence.
Diego Maselli, MD
Dr. Maselli is an Associate Professor of Medicine in the Division of Pulmonary Diseases & Critical Care Medicine at UT Health in San Antonio.
He is the director of the Severe Asthma Program at UT Health and his research focuses on severe asthma, COPD, and bronchiectasis. Dr. Maselli has been designated a Distinguished CHEST Educator since 2017 when the program was initiated. He serves on the steering committee of the Airways Network.
Daniel R. Ouellette, MD
Dr. Ouellette has been a clinician, teacher, and researcher in pulmonary and critical care medicine for 35 years.
He is currently a Senior Staff Physician at Henry Ford Hospital in Detroit where he is the Medical Director for the Pulmonary Ward. He is also an Associate Clinical Professor of Medicine at the Wayne State University School of Medicine, and the Medical Director of the Respiratory Therapy program at Oakland Community College. Dr. Ouellette has over 20 years of military service and was the Consultant to the US Army Surgeon General for Pulmonary Medicine during the last several years of his military career. An active CHEST leader, he has chaired the Guideline Oversight Committee, the Clinical Pulmonary Network, and the Council of Governors, has been a member of the Board of Regents, and held many leadership roles with CHEST and other societies in the development of evidence-based clinical practice guidelines. Dr. Ouellette’s clinical areas of interest include general pulmonary and critical care medicine and evidence-based practice.
Saiprakash Venkateshiah, MD, FCCP
Dr. Venkateshiah is an Associate Professor of Medicine in the Division of Pulmonary, Allergy, Critical Care and Sleep Medicine at Emory University, Atlanta, GA.
He is a clinician educator and a “general pulmonologist” practicing the entire gamut of pulmonary, critical care, and sleep medicine. Dr. Venkateshiah has been a CHEST member for close to 2 decades. He has been involved with CHEST NetWork leadership since 2012, starting as steering committee member of Clinical Pulmonary Medicine Network transitioning to Vice-Chair and Chair. He was previously a member of the Executive Committee of the Council of Networks and the Scientific Program Committee for CHEST 2019 and CHEST 2020. He is currently a steering committee member of the education committees of CHEST and American Academy of Sleep Medicine. He is also a steering committee member of the CHEST Sleep NetWork.
Humayun Anjum, MD
Dr. Anjum is currently working as a pulmonary and critical care physician at Baylor Scott & White Medical Center- Grapevine in Dallas, Texas.
He is an Adjunct Clinical Assistant Professor at University of Houston and University of North Texas. He recently moved to Dallas from Corpus Christi, Texas where, he served as the core faculty for the Internal Medicine residency program and the Pulmonary Disease fellowship program. He is passionate about learning and teaching and has been very intricately involved with CHEST and the CHEST Foundation for the last few years. Currently, he serves as the chair of the Practice Operations Network steering committee. Dr. Anjum is particularly interested in medical practice management and administration and hopes to continue sharing his knowledge through various platforms to help his fellow physicians.
Loren J. Harris, MD FACS FCCP
Dr. Harris is the Chairman of the Department of Surgery and Chief of Thoracic Surgery at Richmond University Medical Center in Staten Island, NY.
He has been in clinical surgical practice for over 20 years and also has over 20 years of experience teaching both medical students and surgical residents and fellows. In addition, he served as Program Director of the general surgery residency program at Maimonides Medical Center from 2014 to 2017. Dr. Harris has published and presented throughout his career both nationally and internationally. His main research and clinical interests are in the appropriate staging and treatment of non-small cell lung cancer. He served as the Chair of the CHEST Marketing Committee; was the editor Pulmonary Perspectives; and is a co-author on two chapters in the most recent edition of the Diagnosis and Management Guidelines for Lung Cancer published by CHEST in 2013. Dr. Harris has also received several prestigious awards including the CHEST Soffer Award for Editorial Excellence.
Diego Maselli, MD
Dr. Maselli is an Associate Professor of Medicine in the Division of Pulmonary Diseases & Critical Care Medicine at UT Health in San Antonio.
He is the director of the Severe Asthma Program at UT Health and his research focuses on severe asthma, COPD, and bronchiectasis. Dr. Maselli has been designated a Distinguished CHEST Educator since 2017 when the program was initiated. He serves on the steering committee of the Airways Network.
Daniel R. Ouellette, MD
Dr. Ouellette has been a clinician, teacher, and researcher in pulmonary and critical care medicine for 35 years.
He is currently a Senior Staff Physician at Henry Ford Hospital in Detroit where he is the Medical Director for the Pulmonary Ward. He is also an Associate Clinical Professor of Medicine at the Wayne State University School of Medicine, and the Medical Director of the Respiratory Therapy program at Oakland Community College. Dr. Ouellette has over 20 years of military service and was the Consultant to the US Army Surgeon General for Pulmonary Medicine during the last several years of his military career. An active CHEST leader, he has chaired the Guideline Oversight Committee, the Clinical Pulmonary Network, and the Council of Governors, has been a member of the Board of Regents, and held many leadership roles with CHEST and other societies in the development of evidence-based clinical practice guidelines. Dr. Ouellette’s clinical areas of interest include general pulmonary and critical care medicine and evidence-based practice.
Saiprakash Venkateshiah, MD, FCCP
Dr. Venkateshiah is an Associate Professor of Medicine in the Division of Pulmonary, Allergy, Critical Care and Sleep Medicine at Emory University, Atlanta, GA.
He is a clinician educator and a “general pulmonologist” practicing the entire gamut of pulmonary, critical care, and sleep medicine. Dr. Venkateshiah has been a CHEST member for close to 2 decades. He has been involved with CHEST NetWork leadership since 2012, starting as steering committee member of Clinical Pulmonary Medicine Network transitioning to Vice-Chair and Chair. He was previously a member of the Executive Committee of the Council of Networks and the Scientific Program Committee for CHEST 2019 and CHEST 2020. He is currently a steering committee member of the education committees of CHEST and American Academy of Sleep Medicine. He is also a steering committee member of the CHEST Sleep NetWork.
Staying home, staying connected
Fundraising in a virtual environment
When the United States went into a 2-week quarantine to slow the spread of the COVID-19 coronavirus in March 2020, everything changed. In the months following, social distancing, working from home, and wearing masks became the norm, and life needed to find a way to go on.
The world adapted to a virtual environment, but some of the hardest hit by this change were non-profit organizations that relied on in-person contact to encourage donations that support their worthwhile missions.
This was even more challenging for the CHEST Foundation as our donors work on the front lines of the pandemic.
“It was important for us to not only stay engaged with our donors but also to recognize what those on the front lines are dealing with,” says Angela Perillo, Director, Development & Foundation Operations at the American College of Chest Physicians. “Through these events, we wanted to provide some respite from the stresses of their long days.”
The CHEST Foundation is about championing lung health, and there was no greater awareness of the need than now. It was time to get creative.
Viva la vino
A well-known “secret” is CHEST CEO Bob Mussachio’s love of wine, and he’s not alone in his passion for the grape. Perillo put this knowledge to good use creating a wine tasting series that took people around the world one bottle at a time.
The online Viva La Vino evening gatherings serve to bring donors together for a night of good wines and good conversation. A benefit to the virtual wine nights is that no one has to travel but that it keeps the group together and keeps the Foundation at the forefront of everyone’s minds.
“I love attending the wine nights. They are so interesting, and I get to see people who don’t live in New York – it’s just great,” says regular participant Ilene (Lenie) Rosen.
The wines are shipped directly to the participants’ homes and during the online Zoom session, Mussachio guides the tasting by scrolling through a presentation on the wine’s background and what to expect from the taste. As the wines are tasted, the participants have a chance to share their review.
“It’s always enthralling to me how much our members know about wine. It makes for a really fun evening listening to their critiques and even learning a bit myself. These events have provided a great platform to stay engaged with our donors and enjoy an evening at home with company,” says Perillo.
Doubling down on a good cause
After hosting its in-person event in the first week of March 2020, the Irv Feldman Texas Hold ’Em poker tournament also shifted to a virtual environment to stay engaged with its players.
Supported by the CHEST Foundation, the Feldman Family Foundation created a series of poker tournaments through an online platform that worked with Zoom to retain the engagement offered by in-person events. Through the Zoom call, players are able to talk to each other either in the main room or in breakout rooms created for each table.
Poker player and recent winner of one of the tournaments, Kim Coles started playing professionally during the pandemic and enjoys playing in an online environment.
“I had participated in charity poker tournaments before, but it wasn’t until I joined Poker Power—a group focused on teaching women how to play poker—that I really came to the table ready to compete,” says Coles. “Playing in an online setting is a lot more accessible for a lot of people, especially for women. A traditional poker tournament can be intimidating to a new player, but online has a way of evening the playing field.”
In an online setting, Feldman and Coles both note that buying in is a lot easier and lends itself well to fundraising.
“There is no fumbling around for your wallet or having to swipe your credit card,” says Coles. “It’s just the press of a button, and your credit card is already linked. It’s all going to a good cause, so it makes sense to keep buying in to keep playing.”
Looking into the future, while Feldman says that the virtual events have been successful, there’s nothing like in-person.
“Through our virtual events, we were able to expand our network of players beyond the Chicagoland area, and these individuals have expressed their interest in attending our live events,” says Feldman. “With this extended network, I am very much looking forward to being able to get together in-person again for what I expect be one of our best tournaments to date.”
The 8th Annual Irv Feldman Texas Hold ‘Em Annual Tournament & Casino Night will be held in early April 2022 in the Chicago suburbs, and all are welcome to attend. Visit the CHEST Foundation’s website to learn more about the tournament and upcoming events at chestfoundation.org.
Fundraising in a virtual environment
Fundraising in a virtual environment
When the United States went into a 2-week quarantine to slow the spread of the COVID-19 coronavirus in March 2020, everything changed. In the months following, social distancing, working from home, and wearing masks became the norm, and life needed to find a way to go on.
The world adapted to a virtual environment, but some of the hardest hit by this change were non-profit organizations that relied on in-person contact to encourage donations that support their worthwhile missions.
This was even more challenging for the CHEST Foundation as our donors work on the front lines of the pandemic.
“It was important for us to not only stay engaged with our donors but also to recognize what those on the front lines are dealing with,” says Angela Perillo, Director, Development & Foundation Operations at the American College of Chest Physicians. “Through these events, we wanted to provide some respite from the stresses of their long days.”
The CHEST Foundation is about championing lung health, and there was no greater awareness of the need than now. It was time to get creative.
Viva la vino
A well-known “secret” is CHEST CEO Bob Mussachio’s love of wine, and he’s not alone in his passion for the grape. Perillo put this knowledge to good use creating a wine tasting series that took people around the world one bottle at a time.
The online Viva La Vino evening gatherings serve to bring donors together for a night of good wines and good conversation. A benefit to the virtual wine nights is that no one has to travel but that it keeps the group together and keeps the Foundation at the forefront of everyone’s minds.
“I love attending the wine nights. They are so interesting, and I get to see people who don’t live in New York – it’s just great,” says regular participant Ilene (Lenie) Rosen.
The wines are shipped directly to the participants’ homes and during the online Zoom session, Mussachio guides the tasting by scrolling through a presentation on the wine’s background and what to expect from the taste. As the wines are tasted, the participants have a chance to share their review.
“It’s always enthralling to me how much our members know about wine. It makes for a really fun evening listening to their critiques and even learning a bit myself. These events have provided a great platform to stay engaged with our donors and enjoy an evening at home with company,” says Perillo.
Doubling down on a good cause
After hosting its in-person event in the first week of March 2020, the Irv Feldman Texas Hold ’Em poker tournament also shifted to a virtual environment to stay engaged with its players.
Supported by the CHEST Foundation, the Feldman Family Foundation created a series of poker tournaments through an online platform that worked with Zoom to retain the engagement offered by in-person events. Through the Zoom call, players are able to talk to each other either in the main room or in breakout rooms created for each table.
Poker player and recent winner of one of the tournaments, Kim Coles started playing professionally during the pandemic and enjoys playing in an online environment.
“I had participated in charity poker tournaments before, but it wasn’t until I joined Poker Power—a group focused on teaching women how to play poker—that I really came to the table ready to compete,” says Coles. “Playing in an online setting is a lot more accessible for a lot of people, especially for women. A traditional poker tournament can be intimidating to a new player, but online has a way of evening the playing field.”
In an online setting, Feldman and Coles both note that buying in is a lot easier and lends itself well to fundraising.
“There is no fumbling around for your wallet or having to swipe your credit card,” says Coles. “It’s just the press of a button, and your credit card is already linked. It’s all going to a good cause, so it makes sense to keep buying in to keep playing.”
Looking into the future, while Feldman says that the virtual events have been successful, there’s nothing like in-person.
“Through our virtual events, we were able to expand our network of players beyond the Chicagoland area, and these individuals have expressed their interest in attending our live events,” says Feldman. “With this extended network, I am very much looking forward to being able to get together in-person again for what I expect be one of our best tournaments to date.”
The 8th Annual Irv Feldman Texas Hold ‘Em Annual Tournament & Casino Night will be held in early April 2022 in the Chicago suburbs, and all are welcome to attend. Visit the CHEST Foundation’s website to learn more about the tournament and upcoming events at chestfoundation.org.
When the United States went into a 2-week quarantine to slow the spread of the COVID-19 coronavirus in March 2020, everything changed. In the months following, social distancing, working from home, and wearing masks became the norm, and life needed to find a way to go on.
The world adapted to a virtual environment, but some of the hardest hit by this change were non-profit organizations that relied on in-person contact to encourage donations that support their worthwhile missions.
This was even more challenging for the CHEST Foundation as our donors work on the front lines of the pandemic.
“It was important for us to not only stay engaged with our donors but also to recognize what those on the front lines are dealing with,” says Angela Perillo, Director, Development & Foundation Operations at the American College of Chest Physicians. “Through these events, we wanted to provide some respite from the stresses of their long days.”
The CHEST Foundation is about championing lung health, and there was no greater awareness of the need than now. It was time to get creative.
Viva la vino
A well-known “secret” is CHEST CEO Bob Mussachio’s love of wine, and he’s not alone in his passion for the grape. Perillo put this knowledge to good use creating a wine tasting series that took people around the world one bottle at a time.
The online Viva La Vino evening gatherings serve to bring donors together for a night of good wines and good conversation. A benefit to the virtual wine nights is that no one has to travel but that it keeps the group together and keeps the Foundation at the forefront of everyone’s minds.
“I love attending the wine nights. They are so interesting, and I get to see people who don’t live in New York – it’s just great,” says regular participant Ilene (Lenie) Rosen.
The wines are shipped directly to the participants’ homes and during the online Zoom session, Mussachio guides the tasting by scrolling through a presentation on the wine’s background and what to expect from the taste. As the wines are tasted, the participants have a chance to share their review.
“It’s always enthralling to me how much our members know about wine. It makes for a really fun evening listening to their critiques and even learning a bit myself. These events have provided a great platform to stay engaged with our donors and enjoy an evening at home with company,” says Perillo.
Doubling down on a good cause
After hosting its in-person event in the first week of March 2020, the Irv Feldman Texas Hold ’Em poker tournament also shifted to a virtual environment to stay engaged with its players.
Supported by the CHEST Foundation, the Feldman Family Foundation created a series of poker tournaments through an online platform that worked with Zoom to retain the engagement offered by in-person events. Through the Zoom call, players are able to talk to each other either in the main room or in breakout rooms created for each table.
Poker player and recent winner of one of the tournaments, Kim Coles started playing professionally during the pandemic and enjoys playing in an online environment.
“I had participated in charity poker tournaments before, but it wasn’t until I joined Poker Power—a group focused on teaching women how to play poker—that I really came to the table ready to compete,” says Coles. “Playing in an online setting is a lot more accessible for a lot of people, especially for women. A traditional poker tournament can be intimidating to a new player, but online has a way of evening the playing field.”
In an online setting, Feldman and Coles both note that buying in is a lot easier and lends itself well to fundraising.
“There is no fumbling around for your wallet or having to swipe your credit card,” says Coles. “It’s just the press of a button, and your credit card is already linked. It’s all going to a good cause, so it makes sense to keep buying in to keep playing.”
Looking into the future, while Feldman says that the virtual events have been successful, there’s nothing like in-person.
“Through our virtual events, we were able to expand our network of players beyond the Chicagoland area, and these individuals have expressed their interest in attending our live events,” says Feldman. “With this extended network, I am very much looking forward to being able to get together in-person again for what I expect be one of our best tournaments to date.”
The 8th Annual Irv Feldman Texas Hold ‘Em Annual Tournament & Casino Night will be held in early April 2022 in the Chicago suburbs, and all are welcome to attend. Visit the CHEST Foundation’s website to learn more about the tournament and upcoming events at chestfoundation.org.
Our CHEST 2021 Award Recipients
ANNUAL AWARDS
Master FCCP
Curtis N. Sessler, MD, Master FCCP
College Medalist Award
Margaret Pisani, MD, MPH, FCCP
Distinguished Service Award
Christopher Carroll, MD, FCCP
Master Clinician Educator
Doreen Addrizzo-Harris, MD, FCCP
Early Career Clinician Educator
Matthew C. Miles, MD, FCCP
Alfred Soffer Award for Editorial Excellence
Scott Manaker, MD, PhD, FCCP
Presidential Citation
COVID-19 Task Force
Ryan Maves, MD, FCCP
Christopher Carroll, MD, FCCP
Neha Dangayach, MD
Jeffrey Dichter, MD, FCCP
Alice Gallo De Moraes, MD
James Geiling, MD, MPH, FCCP
Holly Keyt, MD, FCCP
Stephanie M. Levine, MD, FCCP
Septimu Murgu, MD, FCCP
Marcos Restrepo, MD, PhD, FCCP
Steven Q. Simpson, MD, FCCP
Angel Coz Yataco, MD, FCCP
Staff: Katlyn Froslan, Heather Watkins, Robb Rabito, CHCP, Lilly Rodriguez, Karla Velilla
HONOR LECTURE AND MEMORIAL AWARDS
Distinguished Scientist Honor Lecture in Cardiopulmonary Physiology
KENNETH I. BERGER, MD, FCCP
Probing the Small Airways in the Assessment of Dyspnea
The lecture is generously funded by the CHEST Foundation.
Presidential Honor Lecture
CURTIS N. SESSLER, MD, Master FCCP
Navigating the Road to Well-Being in the ICU
Margaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical Ventilation
DEBRA WEESE-MAYER, MD
Artificial Ventilation, a True Life-Saver for Children with CCHS & ROHHAD
The Margaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical Ventilation is generously supported by International Ventilator Users Network of Post-Polio Health International and the CHEST Foundation.
RICHARD S. IRWIN, MD, MASTER FCCP HONOR LECTURE
PETER J. MAZZONE, MD, MPH, FCCP
Shared Decision Making in the Evaluation and Management of Early Stage Lung Cancer
The lecture is generously funded by the CHEST Foundation.
Edward C. Rosenow III, MD, Master FCCP/Master Teacher Honor Lecture
DIANE E. STOVER, MD, FCCP
The Many Faces of Organizing Pneumonia—What’s the O(O)P With That?
The lecture is generously funded by the CHEST Foundation.
Pasquale Ciaglia Memorial Lecture in Interventional Medicine
MICHAEL J. SIMOFF, MD, FCCP
Robotic Bronchoscopy: Platform to the Future?
The lecture is generously funded by the CHEST Foundation.
Roger C. Bone Memorial Lecture in Critical Care
OGNJEN GAJIC, MD, FCCP
Patient Comes First: Prioritizing Relevant From Irrelevant in Critical Care Medicine
The lecture is generously funded by the CHEST Foundation.
Thomas L. Petty, MD, Master FCCP Memorial Lecture
JEAN BOURBEAU, MD, FCCP
Pulmonary Rehabilitation and Self-Management in COPD: Understanding the Past to Build the Future
The lecture is generously funded by the CHEST Foundation.
CHEST FOUNDATION GRANT AWARDS
CHEST Foundation Research Grant in Lung Cancer
This grant is supported by the CHEST Foundation.
Daniel Ryan, MD, Royal College of Surgeons Ireland, Dublin, Ireland
Microbial Signatures Associated With Malignant Pleural Effusions in Lung Cancer
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
This grant is jointly supported by the CHEST Foundation and RHA.
Miguel Divo, MD, Brigham and Women’s Hospital, Boston, MA
Biomarker Profiles in Smokers Who Are at Risk of Developing Chronic Obstructive Pulmonary Disease (COPD)
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
This grant is supported by AstraZeneca LP.
Stephen Milne, MBBS, Woolcock Institute of Medical Research, Vancouver, BC, Canada
The Oral Metagenome in COPD: Towards a Biomarker of Exacerbation Risk
CHEST Foundation Research Grant in Critical Care
This grant is supported by the CHEST Foundation.
Jacqueline Stocking, PhD, University of California, Davis, Davis, CA
University of California Critical Care Research Collaborative: Predictive Model and Risk Calculator for Early and Late Postoperative Respiratory Failure
CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency
This grant is jointly supported by the CHEST Foundation and the Alpha-1 Foundation.
John Charles Rotondo, PhD, University of Ferrara, Ferrara, Italy
Alpha-1 Antitrypsin Protein as a Possible Marker of Disease Progression in COVID-19 Patients
CHEST Foundation Research Grant in Nontuberculous Mycobacteria Diseases
This grant is supported by Insmed Incorporated.
Edward Chan, MD, Rocky Mountain Regional Veterans Affairs Medical Center, Denver, CO
Visualization and Quantitation of Azithromycin, Clofazimine, and Amikacin Distribution in Surgically Removed Lung Tissues From Patients With Nontuberculous Mycobacterial Lung Disease
CHEST Foundation Research Grant in Cystic Fibrosis
This grant is supported by Vertex Pharmaceuticals Incorporated.
Shahid Sheikh, MD, FCCP, Nationwide Children’s Hospital, Columbus, OH
Impact of CFTR Modulator Therapy Elexacaftor-Tezacaftor-Ivacaftor on CF- Related Chronic Sinus Disease
John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis
This grant is in honor of John R. Addrizzo, MD, FCCP and is jointly supported by the Addrizzo family and the CHEST Foundation.
Maneesh Bhargava, MD, PhD, FCCP, Minneapolis VA Health Care System, Minneapolis, MN
Inflammatory Protein Panel for Sarcoidosis Diagnosis and Prognosis
CHEST Foundation Research Grant in Severe Asthma
This grant is supported by the CHEST Foundation.
Felix Reyes, MD, Montefiore Medical Center, Bronx, NY
Design and Implementation of an Asthma Action Plan Generator: A Pilot Study Assessing User Satisfaction and Clinical Impact
CHEST Foundation Research Grant in Pulmonary Fibrosis
These grants are supported by an independent grant from Boehringer Ingelheim Pharmaceuticals, Inc. and Genentech, Inc.
Marco Mura, MD, PhD, Western University, London, Ontario, Canada
Validation of the Risk Stratification Score in Idiopathic Pulmonary Fibrosis
Janelle Pugashetti, MD, University of California, Davis, Davis, CA
Determining Biomarkers of Immunosuppressant Responsiveness in Patients With CTD-ILD
CHEST Foundation Research Grant in Pulmonary Hypertension
These grants are supported by the CHEST Foundation.
Michael Lee, MD, University of California San Francisco, San Francisco, CA
Transpulmonary Metabolomic Gradients During Exercise in Systemic Sclerosis-Associated Pulmonary Hypertension
Navneet Singh, MD, Warren Alpert School of Medicine at Brown University, Providence, RI
Mitochondrial Dysfunction and Oxidative Stress in Pulmonary Hypertension
CHEST Foundation Research Grant in Sleep Medicine
These grants are funded by Jazz Pharmaceuticals, Inc.
Shahid Karim, MBChB, Mayo Clinic, Rochester, MN
Effects of OSA on Atrial and Ventricular Arrhythmia in HCM: An Incidence Study
Thomas Tolbert, MD, Mount Sinai Hospital, New York, NY
Performance Characteristics of Obstructive Sleep Apnea Physiologic Traits Measured by Phenotyping Using Polysomnography
CHEST Foundation and American Academy of Sleep Medicine Foundation Research Grant in Sleep Medicine
This grant is jointly supported by the CHEST Foundation and AASM Foundation.
Marta Kaminska, MD, McGill University Health Centre, Montreal, QC, Canada
Long-term Noninvasive Ventilation in COPD: Impact on Health Care Utilization
CHEST Foundation and APCCMPD Research Grant in Medical Education
This grant is jointly supported by the CHEST Foundation and APCCMPD.
Mark Adelman, MD, NYU School of Medicine, New York, NY
Virtual Reality Simulation Training for the Management of Tracheostomy Emergencies
CHEST Foundation Research Grant in COVID-19
These grants are supported by the CHEST Foundation.
Marlene Cano, MD, PhD, Washington University, St. Louis, MO
Circulating Mitochondrial DNA Is a Potential Biomarker for Severe Illness in COVID-19
Brandon Walsh, MD, New York University, New York, NY
How Would Existing Ventilator Allocation Guidelines Perform During the COVID-19 Pandemic: A Retrospective Observational Simulated Cohort Study
CHEST Foundation and ATS Research Grant in COVID-19 and Diversity
These grants are jointly supported by the CHEST Foundation and ATS.
Navitha Ramesh, MD, FCCP, UPMC Harrisburg, Harrisburg, PA
Improving Lung Health in the Nepali- Bhutanese Refugee Community in Harrisburg, PA
Inderjit Singh, MBBCh, Yale University, New Haven, CT
Dynamic Invasive Hemodynamic, Echocardiographic, and Plasma Biomarker Phenotyping in Post-COVID-19 Long Hauler Syndrome
CHEST Foundation Community Service Grants Honoring D. Robert McCaffree, MD, Master FCCP
Valerie Andrews, BS, The JUDAHH Project, Sacramento, CA
Asthma Mitigation Project
Chanda Holsey, DrPh, National Medical Association, Silver Spring, MD
Providing Lung Health Education to At Risk Communities
Arzu Ari, PhD, FCCP, Texas State University, San Marcos, TX
Training Future Respiratory Care Practitioners in Turkey: A Path to Successful Disease Management in Pulmonary Medicine
Panagis Galiatsatos, MD, MPH, John Hopkins University, Baltimore, MD
The Lung Health Ambassador Program: A Health Equity Initiative for Cystic Fibrosis
Patricia George, MD, National Jewish Health, Denver, CO
Development of Breathe Strong PH: An Informational Website About Pulmonary Hypertension and Related Diseases
Nishant Gupta, MD, MS, University of Cincinnati, Cincinnati, OH
Global Dissemination of the Lymphangioleiomyomatosis (LAM) Clinical Practice Guidelines
Syed Naqvi, MD, MBBS, Hoag Hospital Newport Beach, Newport Beach, CA
Asthma Managment in Rural Pakistan
These grants are supported by the CHEST Foundation.
Alfred Soffer Research Award Winners
Mathieu Saint-Pierre, MD: Methacholine Challenge Testing: A Clinical Prediction Model Utilizing Demographic Data And Spirometry Results
Tie: Milind K Bhagat, MD: High Flow Nasal Cannula Fio2 Cutoffs Identified Early In The Hospital Course Are Associated With Increased Mortality Risk In Hospitalized Patients With COVID-19
Amber J Meservey, MD: Outcomes Of Patients Across The Spectrum Of Pulmonary Hypertension Groups Prescribed Inhaled Treprostinil
Young Investigator Award Winners
William B. Feldman, MD: COPD Exacerbations And Pneumonia Hospitalizations In New Users Of Combination Maintenance Inhalers: A Comparative Effectiveness And Safety Study
Christopher Streiler, MD: Community Pulmonologist Access To Multidisciplinary Discussion At An Academic Referral Center Leads To Changes In Management Of Interstitial Lung Disease
Top 5 Abstract Posters
Winner: Riley Kermanian: Management Of Coronary Artery Calcification In Patients Enrolled In A Low-Dose Computerized Tomography Lung Cancer Screening Program
Winner: Rohit Reddy: Outcomes Of Extracorporeal Membrane Oxygenation In ARDS Due To Covid-19: Comparison Of The First And The Second Wave
Winner: Taylor A. Intihar, BA: Light Patterns Of The Medical ICU: Are We Disrupting Circadian Rhythms?
Runner up: Jason Wong, MD: Completion Of Pulmonary Rehabilitation Is Associated With Improvement In Depression Scores And Other Quality Of Life Measures In Patients With Interstitial Lung Disease
Runner up: Harshil Shah, MD: Impact Of Sepsis On Outcomes Of Hospitalizations Due To COPD
Case Report Session Winners
Remarkable Pulmonary Cases: Mena Botros, MD: Clinical Outcomes In Lung Transplant Recipients With SARS-COV2
Bacterial Infections: Benjamin Carmel, DO: Cotton Swab Today, Brain Abscess Tomorrow
Challenging Critical Care Cases: Rajaninder Sharma, MD: Pulmonary Tumor Thrombotic Microangiopathy: The Rare And Fatal Association Of Adenocarcinoma And Right Ventricular Failure
Diffuse Lung Diseases: Rizwana RR Rana, MBBS: A Rare Cause Of Pulmonary Nodules
Viruses, Fungi, and Parasites Infections: Michelle Forson, MD: Strongyloidiasis-Related Eosinophilic Pleural Effusion: An Unexpected Differential For Post-Cardiac Injury Syndrome
Critical Care Cases: Act Quickly: Christina Jee Ah Rhee, MD: Airway Implications Of Cricoarytenoid Arthritis: A Report And Review Of The Literature
Airway Issues: Benadin Varajic, MD: An Unusual And Life-Threatening Complication Of Endotracheal Intubation
Miscellaneous Cases 1: Shrey Shah, MD: A Case Of Pulmonary Arterial Hypertension From Vitamin C Deficiency
Miscellaneous Cases 2: Glenn W. Pottmeyer, DO, MPH: Biliary Stent Migration: A Rare Cause Of Right-Sided Pulmonary Abscess
Case Report Poster Winners
Advanced Cancer Case Report Posters: Sangita Goel, MD: Let’s Meet in the Middle: Simultaneous Endoscopic and Bronchoscopic Suture Repair to Close a Left Main-Stem Malignant Broncho-Esophageal Fistula
Cardiovascular Case Report Posters: Marianna Weaver, DO: Swan-Ganz And Intra-Pericardial Pressure Guided Pericardiocentesis in Scleroderma-Associated PAH
Remarkable Cases Posters 1: Katie Capp, MD: Humidifier-Associated Hypersensitivity Pneumonitis
Remarkable Cases Posters 2: Sahar Samani, MD: Artifactual Hypoxemia in Patients With Hydroxyurea-Induced Blue Lunula Fingernails
CHEST 2021 CHEST Challenge
1st Place
The Ohio State University
Sarah Cohen, MD
Gregory Eisinger, MD
Kyle Stinehart, MD
Program Director: Jennifer McCallister, MD, FCCP
2nd Place
SUNY Buffalo
Arjun Saradna, MBBS
Rajesh Kunadharaju, MD
Ahmed Munir, MBBS
Program Director: Jeffrey Mador, MD
3rd Place
Interfaith Medical Center
Tahmina Jahir, MD
Ruby Risal, MD
Binav Shrestha, MBBS
Program Director: Marie Frances Schmidt, MD, FCCP
ANNUAL AWARDS
Master FCCP
Curtis N. Sessler, MD, Master FCCP
College Medalist Award
Margaret Pisani, MD, MPH, FCCP
Distinguished Service Award
Christopher Carroll, MD, FCCP
Master Clinician Educator
Doreen Addrizzo-Harris, MD, FCCP
Early Career Clinician Educator
Matthew C. Miles, MD, FCCP
Alfred Soffer Award for Editorial Excellence
Scott Manaker, MD, PhD, FCCP
Presidential Citation
COVID-19 Task Force
Ryan Maves, MD, FCCP
Christopher Carroll, MD, FCCP
Neha Dangayach, MD
Jeffrey Dichter, MD, FCCP
Alice Gallo De Moraes, MD
James Geiling, MD, MPH, FCCP
Holly Keyt, MD, FCCP
Stephanie M. Levine, MD, FCCP
Septimu Murgu, MD, FCCP
Marcos Restrepo, MD, PhD, FCCP
Steven Q. Simpson, MD, FCCP
Angel Coz Yataco, MD, FCCP
Staff: Katlyn Froslan, Heather Watkins, Robb Rabito, CHCP, Lilly Rodriguez, Karla Velilla
HONOR LECTURE AND MEMORIAL AWARDS
Distinguished Scientist Honor Lecture in Cardiopulmonary Physiology
KENNETH I. BERGER, MD, FCCP
Probing the Small Airways in the Assessment of Dyspnea
The lecture is generously funded by the CHEST Foundation.
Presidential Honor Lecture
CURTIS N. SESSLER, MD, Master FCCP
Navigating the Road to Well-Being in the ICU
Margaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical Ventilation
DEBRA WEESE-MAYER, MD
Artificial Ventilation, a True Life-Saver for Children with CCHS & ROHHAD
The Margaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical Ventilation is generously supported by International Ventilator Users Network of Post-Polio Health International and the CHEST Foundation.
RICHARD S. IRWIN, MD, MASTER FCCP HONOR LECTURE
PETER J. MAZZONE, MD, MPH, FCCP
Shared Decision Making in the Evaluation and Management of Early Stage Lung Cancer
The lecture is generously funded by the CHEST Foundation.
Edward C. Rosenow III, MD, Master FCCP/Master Teacher Honor Lecture
DIANE E. STOVER, MD, FCCP
The Many Faces of Organizing Pneumonia—What’s the O(O)P With That?
The lecture is generously funded by the CHEST Foundation.
Pasquale Ciaglia Memorial Lecture in Interventional Medicine
MICHAEL J. SIMOFF, MD, FCCP
Robotic Bronchoscopy: Platform to the Future?
The lecture is generously funded by the CHEST Foundation.
Roger C. Bone Memorial Lecture in Critical Care
OGNJEN GAJIC, MD, FCCP
Patient Comes First: Prioritizing Relevant From Irrelevant in Critical Care Medicine
The lecture is generously funded by the CHEST Foundation.
Thomas L. Petty, MD, Master FCCP Memorial Lecture
JEAN BOURBEAU, MD, FCCP
Pulmonary Rehabilitation and Self-Management in COPD: Understanding the Past to Build the Future
The lecture is generously funded by the CHEST Foundation.
CHEST FOUNDATION GRANT AWARDS
CHEST Foundation Research Grant in Lung Cancer
This grant is supported by the CHEST Foundation.
Daniel Ryan, MD, Royal College of Surgeons Ireland, Dublin, Ireland
Microbial Signatures Associated With Malignant Pleural Effusions in Lung Cancer
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
This grant is jointly supported by the CHEST Foundation and RHA.
Miguel Divo, MD, Brigham and Women’s Hospital, Boston, MA
Biomarker Profiles in Smokers Who Are at Risk of Developing Chronic Obstructive Pulmonary Disease (COPD)
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
This grant is supported by AstraZeneca LP.
Stephen Milne, MBBS, Woolcock Institute of Medical Research, Vancouver, BC, Canada
The Oral Metagenome in COPD: Towards a Biomarker of Exacerbation Risk
CHEST Foundation Research Grant in Critical Care
This grant is supported by the CHEST Foundation.
Jacqueline Stocking, PhD, University of California, Davis, Davis, CA
University of California Critical Care Research Collaborative: Predictive Model and Risk Calculator for Early and Late Postoperative Respiratory Failure
CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency
This grant is jointly supported by the CHEST Foundation and the Alpha-1 Foundation.
John Charles Rotondo, PhD, University of Ferrara, Ferrara, Italy
Alpha-1 Antitrypsin Protein as a Possible Marker of Disease Progression in COVID-19 Patients
CHEST Foundation Research Grant in Nontuberculous Mycobacteria Diseases
This grant is supported by Insmed Incorporated.
Edward Chan, MD, Rocky Mountain Regional Veterans Affairs Medical Center, Denver, CO
Visualization and Quantitation of Azithromycin, Clofazimine, and Amikacin Distribution in Surgically Removed Lung Tissues From Patients With Nontuberculous Mycobacterial Lung Disease
CHEST Foundation Research Grant in Cystic Fibrosis
This grant is supported by Vertex Pharmaceuticals Incorporated.
Shahid Sheikh, MD, FCCP, Nationwide Children’s Hospital, Columbus, OH
Impact of CFTR Modulator Therapy Elexacaftor-Tezacaftor-Ivacaftor on CF- Related Chronic Sinus Disease
John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis
This grant is in honor of John R. Addrizzo, MD, FCCP and is jointly supported by the Addrizzo family and the CHEST Foundation.
Maneesh Bhargava, MD, PhD, FCCP, Minneapolis VA Health Care System, Minneapolis, MN
Inflammatory Protein Panel for Sarcoidosis Diagnosis and Prognosis
CHEST Foundation Research Grant in Severe Asthma
This grant is supported by the CHEST Foundation.
Felix Reyes, MD, Montefiore Medical Center, Bronx, NY
Design and Implementation of an Asthma Action Plan Generator: A Pilot Study Assessing User Satisfaction and Clinical Impact
CHEST Foundation Research Grant in Pulmonary Fibrosis
These grants are supported by an independent grant from Boehringer Ingelheim Pharmaceuticals, Inc. and Genentech, Inc.
Marco Mura, MD, PhD, Western University, London, Ontario, Canada
Validation of the Risk Stratification Score in Idiopathic Pulmonary Fibrosis
Janelle Pugashetti, MD, University of California, Davis, Davis, CA
Determining Biomarkers of Immunosuppressant Responsiveness in Patients With CTD-ILD
CHEST Foundation Research Grant in Pulmonary Hypertension
These grants are supported by the CHEST Foundation.
Michael Lee, MD, University of California San Francisco, San Francisco, CA
Transpulmonary Metabolomic Gradients During Exercise in Systemic Sclerosis-Associated Pulmonary Hypertension
Navneet Singh, MD, Warren Alpert School of Medicine at Brown University, Providence, RI
Mitochondrial Dysfunction and Oxidative Stress in Pulmonary Hypertension
CHEST Foundation Research Grant in Sleep Medicine
These grants are funded by Jazz Pharmaceuticals, Inc.
Shahid Karim, MBChB, Mayo Clinic, Rochester, MN
Effects of OSA on Atrial and Ventricular Arrhythmia in HCM: An Incidence Study
Thomas Tolbert, MD, Mount Sinai Hospital, New York, NY
Performance Characteristics of Obstructive Sleep Apnea Physiologic Traits Measured by Phenotyping Using Polysomnography
CHEST Foundation and American Academy of Sleep Medicine Foundation Research Grant in Sleep Medicine
This grant is jointly supported by the CHEST Foundation and AASM Foundation.
Marta Kaminska, MD, McGill University Health Centre, Montreal, QC, Canada
Long-term Noninvasive Ventilation in COPD: Impact on Health Care Utilization
CHEST Foundation and APCCMPD Research Grant in Medical Education
This grant is jointly supported by the CHEST Foundation and APCCMPD.
Mark Adelman, MD, NYU School of Medicine, New York, NY
Virtual Reality Simulation Training for the Management of Tracheostomy Emergencies
CHEST Foundation Research Grant in COVID-19
These grants are supported by the CHEST Foundation.
Marlene Cano, MD, PhD, Washington University, St. Louis, MO
Circulating Mitochondrial DNA Is a Potential Biomarker for Severe Illness in COVID-19
Brandon Walsh, MD, New York University, New York, NY
How Would Existing Ventilator Allocation Guidelines Perform During the COVID-19 Pandemic: A Retrospective Observational Simulated Cohort Study
CHEST Foundation and ATS Research Grant in COVID-19 and Diversity
These grants are jointly supported by the CHEST Foundation and ATS.
Navitha Ramesh, MD, FCCP, UPMC Harrisburg, Harrisburg, PA
Improving Lung Health in the Nepali- Bhutanese Refugee Community in Harrisburg, PA
Inderjit Singh, MBBCh, Yale University, New Haven, CT
Dynamic Invasive Hemodynamic, Echocardiographic, and Plasma Biomarker Phenotyping in Post-COVID-19 Long Hauler Syndrome
CHEST Foundation Community Service Grants Honoring D. Robert McCaffree, MD, Master FCCP
Valerie Andrews, BS, The JUDAHH Project, Sacramento, CA
Asthma Mitigation Project
Chanda Holsey, DrPh, National Medical Association, Silver Spring, MD
Providing Lung Health Education to At Risk Communities
Arzu Ari, PhD, FCCP, Texas State University, San Marcos, TX
Training Future Respiratory Care Practitioners in Turkey: A Path to Successful Disease Management in Pulmonary Medicine
Panagis Galiatsatos, MD, MPH, John Hopkins University, Baltimore, MD
The Lung Health Ambassador Program: A Health Equity Initiative for Cystic Fibrosis
Patricia George, MD, National Jewish Health, Denver, CO
Development of Breathe Strong PH: An Informational Website About Pulmonary Hypertension and Related Diseases
Nishant Gupta, MD, MS, University of Cincinnati, Cincinnati, OH
Global Dissemination of the Lymphangioleiomyomatosis (LAM) Clinical Practice Guidelines
Syed Naqvi, MD, MBBS, Hoag Hospital Newport Beach, Newport Beach, CA
Asthma Managment in Rural Pakistan
These grants are supported by the CHEST Foundation.
Alfred Soffer Research Award Winners
Mathieu Saint-Pierre, MD: Methacholine Challenge Testing: A Clinical Prediction Model Utilizing Demographic Data And Spirometry Results
Tie: Milind K Bhagat, MD: High Flow Nasal Cannula Fio2 Cutoffs Identified Early In The Hospital Course Are Associated With Increased Mortality Risk In Hospitalized Patients With COVID-19
Amber J Meservey, MD: Outcomes Of Patients Across The Spectrum Of Pulmonary Hypertension Groups Prescribed Inhaled Treprostinil
Young Investigator Award Winners
William B. Feldman, MD: COPD Exacerbations And Pneumonia Hospitalizations In New Users Of Combination Maintenance Inhalers: A Comparative Effectiveness And Safety Study
Christopher Streiler, MD: Community Pulmonologist Access To Multidisciplinary Discussion At An Academic Referral Center Leads To Changes In Management Of Interstitial Lung Disease
Top 5 Abstract Posters
Winner: Riley Kermanian: Management Of Coronary Artery Calcification In Patients Enrolled In A Low-Dose Computerized Tomography Lung Cancer Screening Program
Winner: Rohit Reddy: Outcomes Of Extracorporeal Membrane Oxygenation In ARDS Due To Covid-19: Comparison Of The First And The Second Wave
Winner: Taylor A. Intihar, BA: Light Patterns Of The Medical ICU: Are We Disrupting Circadian Rhythms?
Runner up: Jason Wong, MD: Completion Of Pulmonary Rehabilitation Is Associated With Improvement In Depression Scores And Other Quality Of Life Measures In Patients With Interstitial Lung Disease
Runner up: Harshil Shah, MD: Impact Of Sepsis On Outcomes Of Hospitalizations Due To COPD
Case Report Session Winners
Remarkable Pulmonary Cases: Mena Botros, MD: Clinical Outcomes In Lung Transplant Recipients With SARS-COV2
Bacterial Infections: Benjamin Carmel, DO: Cotton Swab Today, Brain Abscess Tomorrow
Challenging Critical Care Cases: Rajaninder Sharma, MD: Pulmonary Tumor Thrombotic Microangiopathy: The Rare And Fatal Association Of Adenocarcinoma And Right Ventricular Failure
Diffuse Lung Diseases: Rizwana RR Rana, MBBS: A Rare Cause Of Pulmonary Nodules
Viruses, Fungi, and Parasites Infections: Michelle Forson, MD: Strongyloidiasis-Related Eosinophilic Pleural Effusion: An Unexpected Differential For Post-Cardiac Injury Syndrome
Critical Care Cases: Act Quickly: Christina Jee Ah Rhee, MD: Airway Implications Of Cricoarytenoid Arthritis: A Report And Review Of The Literature
Airway Issues: Benadin Varajic, MD: An Unusual And Life-Threatening Complication Of Endotracheal Intubation
Miscellaneous Cases 1: Shrey Shah, MD: A Case Of Pulmonary Arterial Hypertension From Vitamin C Deficiency
Miscellaneous Cases 2: Glenn W. Pottmeyer, DO, MPH: Biliary Stent Migration: A Rare Cause Of Right-Sided Pulmonary Abscess
Case Report Poster Winners
Advanced Cancer Case Report Posters: Sangita Goel, MD: Let’s Meet in the Middle: Simultaneous Endoscopic and Bronchoscopic Suture Repair to Close a Left Main-Stem Malignant Broncho-Esophageal Fistula
Cardiovascular Case Report Posters: Marianna Weaver, DO: Swan-Ganz And Intra-Pericardial Pressure Guided Pericardiocentesis in Scleroderma-Associated PAH
Remarkable Cases Posters 1: Katie Capp, MD: Humidifier-Associated Hypersensitivity Pneumonitis
Remarkable Cases Posters 2: Sahar Samani, MD: Artifactual Hypoxemia in Patients With Hydroxyurea-Induced Blue Lunula Fingernails
CHEST 2021 CHEST Challenge
1st Place
The Ohio State University
Sarah Cohen, MD
Gregory Eisinger, MD
Kyle Stinehart, MD
Program Director: Jennifer McCallister, MD, FCCP
2nd Place
SUNY Buffalo
Arjun Saradna, MBBS
Rajesh Kunadharaju, MD
Ahmed Munir, MBBS
Program Director: Jeffrey Mador, MD
3rd Place
Interfaith Medical Center
Tahmina Jahir, MD
Ruby Risal, MD
Binav Shrestha, MBBS
Program Director: Marie Frances Schmidt, MD, FCCP
ANNUAL AWARDS
Master FCCP
Curtis N. Sessler, MD, Master FCCP
College Medalist Award
Margaret Pisani, MD, MPH, FCCP
Distinguished Service Award
Christopher Carroll, MD, FCCP
Master Clinician Educator
Doreen Addrizzo-Harris, MD, FCCP
Early Career Clinician Educator
Matthew C. Miles, MD, FCCP
Alfred Soffer Award for Editorial Excellence
Scott Manaker, MD, PhD, FCCP
Presidential Citation
COVID-19 Task Force
Ryan Maves, MD, FCCP
Christopher Carroll, MD, FCCP
Neha Dangayach, MD
Jeffrey Dichter, MD, FCCP
Alice Gallo De Moraes, MD
James Geiling, MD, MPH, FCCP
Holly Keyt, MD, FCCP
Stephanie M. Levine, MD, FCCP
Septimu Murgu, MD, FCCP
Marcos Restrepo, MD, PhD, FCCP
Steven Q. Simpson, MD, FCCP
Angel Coz Yataco, MD, FCCP
Staff: Katlyn Froslan, Heather Watkins, Robb Rabito, CHCP, Lilly Rodriguez, Karla Velilla
HONOR LECTURE AND MEMORIAL AWARDS
Distinguished Scientist Honor Lecture in Cardiopulmonary Physiology
KENNETH I. BERGER, MD, FCCP
Probing the Small Airways in the Assessment of Dyspnea
The lecture is generously funded by the CHEST Foundation.
Presidential Honor Lecture
CURTIS N. SESSLER, MD, Master FCCP
Navigating the Road to Well-Being in the ICU
Margaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical Ventilation
DEBRA WEESE-MAYER, MD
Artificial Ventilation, a True Life-Saver for Children with CCHS & ROHHAD
The Margaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical Ventilation is generously supported by International Ventilator Users Network of Post-Polio Health International and the CHEST Foundation.
RICHARD S. IRWIN, MD, MASTER FCCP HONOR LECTURE
PETER J. MAZZONE, MD, MPH, FCCP
Shared Decision Making in the Evaluation and Management of Early Stage Lung Cancer
The lecture is generously funded by the CHEST Foundation.
Edward C. Rosenow III, MD, Master FCCP/Master Teacher Honor Lecture
DIANE E. STOVER, MD, FCCP
The Many Faces of Organizing Pneumonia—What’s the O(O)P With That?
The lecture is generously funded by the CHEST Foundation.
Pasquale Ciaglia Memorial Lecture in Interventional Medicine
MICHAEL J. SIMOFF, MD, FCCP
Robotic Bronchoscopy: Platform to the Future?
The lecture is generously funded by the CHEST Foundation.
Roger C. Bone Memorial Lecture in Critical Care
OGNJEN GAJIC, MD, FCCP
Patient Comes First: Prioritizing Relevant From Irrelevant in Critical Care Medicine
The lecture is generously funded by the CHEST Foundation.
Thomas L. Petty, MD, Master FCCP Memorial Lecture
JEAN BOURBEAU, MD, FCCP
Pulmonary Rehabilitation and Self-Management in COPD: Understanding the Past to Build the Future
The lecture is generously funded by the CHEST Foundation.
CHEST FOUNDATION GRANT AWARDS
CHEST Foundation Research Grant in Lung Cancer
This grant is supported by the CHEST Foundation.
Daniel Ryan, MD, Royal College of Surgeons Ireland, Dublin, Ireland
Microbial Signatures Associated With Malignant Pleural Effusions in Lung Cancer
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
This grant is jointly supported by the CHEST Foundation and RHA.
Miguel Divo, MD, Brigham and Women’s Hospital, Boston, MA
Biomarker Profiles in Smokers Who Are at Risk of Developing Chronic Obstructive Pulmonary Disease (COPD)
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
This grant is supported by AstraZeneca LP.
Stephen Milne, MBBS, Woolcock Institute of Medical Research, Vancouver, BC, Canada
The Oral Metagenome in COPD: Towards a Biomarker of Exacerbation Risk
CHEST Foundation Research Grant in Critical Care
This grant is supported by the CHEST Foundation.
Jacqueline Stocking, PhD, University of California, Davis, Davis, CA
University of California Critical Care Research Collaborative: Predictive Model and Risk Calculator for Early and Late Postoperative Respiratory Failure
CHEST Foundation and the Alpha-1 Foundation Research Grant in Alpha-1 Antitrypsin Deficiency
This grant is jointly supported by the CHEST Foundation and the Alpha-1 Foundation.
John Charles Rotondo, PhD, University of Ferrara, Ferrara, Italy
Alpha-1 Antitrypsin Protein as a Possible Marker of Disease Progression in COVID-19 Patients
CHEST Foundation Research Grant in Nontuberculous Mycobacteria Diseases
This grant is supported by Insmed Incorporated.
Edward Chan, MD, Rocky Mountain Regional Veterans Affairs Medical Center, Denver, CO
Visualization and Quantitation of Azithromycin, Clofazimine, and Amikacin Distribution in Surgically Removed Lung Tissues From Patients With Nontuberculous Mycobacterial Lung Disease
CHEST Foundation Research Grant in Cystic Fibrosis
This grant is supported by Vertex Pharmaceuticals Incorporated.
Shahid Sheikh, MD, FCCP, Nationwide Children’s Hospital, Columbus, OH
Impact of CFTR Modulator Therapy Elexacaftor-Tezacaftor-Ivacaftor on CF- Related Chronic Sinus Disease
John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis
This grant is in honor of John R. Addrizzo, MD, FCCP and is jointly supported by the Addrizzo family and the CHEST Foundation.
Maneesh Bhargava, MD, PhD, FCCP, Minneapolis VA Health Care System, Minneapolis, MN
Inflammatory Protein Panel for Sarcoidosis Diagnosis and Prognosis
CHEST Foundation Research Grant in Severe Asthma
This grant is supported by the CHEST Foundation.
Felix Reyes, MD, Montefiore Medical Center, Bronx, NY
Design and Implementation of an Asthma Action Plan Generator: A Pilot Study Assessing User Satisfaction and Clinical Impact
CHEST Foundation Research Grant in Pulmonary Fibrosis
These grants are supported by an independent grant from Boehringer Ingelheim Pharmaceuticals, Inc. and Genentech, Inc.
Marco Mura, MD, PhD, Western University, London, Ontario, Canada
Validation of the Risk Stratification Score in Idiopathic Pulmonary Fibrosis
Janelle Pugashetti, MD, University of California, Davis, Davis, CA
Determining Biomarkers of Immunosuppressant Responsiveness in Patients With CTD-ILD
CHEST Foundation Research Grant in Pulmonary Hypertension
These grants are supported by the CHEST Foundation.
Michael Lee, MD, University of California San Francisco, San Francisco, CA
Transpulmonary Metabolomic Gradients During Exercise in Systemic Sclerosis-Associated Pulmonary Hypertension
Navneet Singh, MD, Warren Alpert School of Medicine at Brown University, Providence, RI
Mitochondrial Dysfunction and Oxidative Stress in Pulmonary Hypertension
CHEST Foundation Research Grant in Sleep Medicine
These grants are funded by Jazz Pharmaceuticals, Inc.
Shahid Karim, MBChB, Mayo Clinic, Rochester, MN
Effects of OSA on Atrial and Ventricular Arrhythmia in HCM: An Incidence Study
Thomas Tolbert, MD, Mount Sinai Hospital, New York, NY
Performance Characteristics of Obstructive Sleep Apnea Physiologic Traits Measured by Phenotyping Using Polysomnography
CHEST Foundation and American Academy of Sleep Medicine Foundation Research Grant in Sleep Medicine
This grant is jointly supported by the CHEST Foundation and AASM Foundation.
Marta Kaminska, MD, McGill University Health Centre, Montreal, QC, Canada
Long-term Noninvasive Ventilation in COPD: Impact on Health Care Utilization
CHEST Foundation and APCCMPD Research Grant in Medical Education
This grant is jointly supported by the CHEST Foundation and APCCMPD.
Mark Adelman, MD, NYU School of Medicine, New York, NY
Virtual Reality Simulation Training for the Management of Tracheostomy Emergencies
CHEST Foundation Research Grant in COVID-19
These grants are supported by the CHEST Foundation.
Marlene Cano, MD, PhD, Washington University, St. Louis, MO
Circulating Mitochondrial DNA Is a Potential Biomarker for Severe Illness in COVID-19
Brandon Walsh, MD, New York University, New York, NY
How Would Existing Ventilator Allocation Guidelines Perform During the COVID-19 Pandemic: A Retrospective Observational Simulated Cohort Study
CHEST Foundation and ATS Research Grant in COVID-19 and Diversity
These grants are jointly supported by the CHEST Foundation and ATS.
Navitha Ramesh, MD, FCCP, UPMC Harrisburg, Harrisburg, PA
Improving Lung Health in the Nepali- Bhutanese Refugee Community in Harrisburg, PA
Inderjit Singh, MBBCh, Yale University, New Haven, CT
Dynamic Invasive Hemodynamic, Echocardiographic, and Plasma Biomarker Phenotyping in Post-COVID-19 Long Hauler Syndrome
CHEST Foundation Community Service Grants Honoring D. Robert McCaffree, MD, Master FCCP
Valerie Andrews, BS, The JUDAHH Project, Sacramento, CA
Asthma Mitigation Project
Chanda Holsey, DrPh, National Medical Association, Silver Spring, MD
Providing Lung Health Education to At Risk Communities
Arzu Ari, PhD, FCCP, Texas State University, San Marcos, TX
Training Future Respiratory Care Practitioners in Turkey: A Path to Successful Disease Management in Pulmonary Medicine
Panagis Galiatsatos, MD, MPH, John Hopkins University, Baltimore, MD
The Lung Health Ambassador Program: A Health Equity Initiative for Cystic Fibrosis
Patricia George, MD, National Jewish Health, Denver, CO
Development of Breathe Strong PH: An Informational Website About Pulmonary Hypertension and Related Diseases
Nishant Gupta, MD, MS, University of Cincinnati, Cincinnati, OH
Global Dissemination of the Lymphangioleiomyomatosis (LAM) Clinical Practice Guidelines
Syed Naqvi, MD, MBBS, Hoag Hospital Newport Beach, Newport Beach, CA
Asthma Managment in Rural Pakistan
These grants are supported by the CHEST Foundation.
Alfred Soffer Research Award Winners
Mathieu Saint-Pierre, MD: Methacholine Challenge Testing: A Clinical Prediction Model Utilizing Demographic Data And Spirometry Results
Tie: Milind K Bhagat, MD: High Flow Nasal Cannula Fio2 Cutoffs Identified Early In The Hospital Course Are Associated With Increased Mortality Risk In Hospitalized Patients With COVID-19
Amber J Meservey, MD: Outcomes Of Patients Across The Spectrum Of Pulmonary Hypertension Groups Prescribed Inhaled Treprostinil
Young Investigator Award Winners
William B. Feldman, MD: COPD Exacerbations And Pneumonia Hospitalizations In New Users Of Combination Maintenance Inhalers: A Comparative Effectiveness And Safety Study
Christopher Streiler, MD: Community Pulmonologist Access To Multidisciplinary Discussion At An Academic Referral Center Leads To Changes In Management Of Interstitial Lung Disease
Top 5 Abstract Posters
Winner: Riley Kermanian: Management Of Coronary Artery Calcification In Patients Enrolled In A Low-Dose Computerized Tomography Lung Cancer Screening Program
Winner: Rohit Reddy: Outcomes Of Extracorporeal Membrane Oxygenation In ARDS Due To Covid-19: Comparison Of The First And The Second Wave
Winner: Taylor A. Intihar, BA: Light Patterns Of The Medical ICU: Are We Disrupting Circadian Rhythms?
Runner up: Jason Wong, MD: Completion Of Pulmonary Rehabilitation Is Associated With Improvement In Depression Scores And Other Quality Of Life Measures In Patients With Interstitial Lung Disease
Runner up: Harshil Shah, MD: Impact Of Sepsis On Outcomes Of Hospitalizations Due To COPD
Case Report Session Winners
Remarkable Pulmonary Cases: Mena Botros, MD: Clinical Outcomes In Lung Transplant Recipients With SARS-COV2
Bacterial Infections: Benjamin Carmel, DO: Cotton Swab Today, Brain Abscess Tomorrow
Challenging Critical Care Cases: Rajaninder Sharma, MD: Pulmonary Tumor Thrombotic Microangiopathy: The Rare And Fatal Association Of Adenocarcinoma And Right Ventricular Failure
Diffuse Lung Diseases: Rizwana RR Rana, MBBS: A Rare Cause Of Pulmonary Nodules
Viruses, Fungi, and Parasites Infections: Michelle Forson, MD: Strongyloidiasis-Related Eosinophilic Pleural Effusion: An Unexpected Differential For Post-Cardiac Injury Syndrome
Critical Care Cases: Act Quickly: Christina Jee Ah Rhee, MD: Airway Implications Of Cricoarytenoid Arthritis: A Report And Review Of The Literature
Airway Issues: Benadin Varajic, MD: An Unusual And Life-Threatening Complication Of Endotracheal Intubation
Miscellaneous Cases 1: Shrey Shah, MD: A Case Of Pulmonary Arterial Hypertension From Vitamin C Deficiency
Miscellaneous Cases 2: Glenn W. Pottmeyer, DO, MPH: Biliary Stent Migration: A Rare Cause Of Right-Sided Pulmonary Abscess
Case Report Poster Winners
Advanced Cancer Case Report Posters: Sangita Goel, MD: Let’s Meet in the Middle: Simultaneous Endoscopic and Bronchoscopic Suture Repair to Close a Left Main-Stem Malignant Broncho-Esophageal Fistula
Cardiovascular Case Report Posters: Marianna Weaver, DO: Swan-Ganz And Intra-Pericardial Pressure Guided Pericardiocentesis in Scleroderma-Associated PAH
Remarkable Cases Posters 1: Katie Capp, MD: Humidifier-Associated Hypersensitivity Pneumonitis
Remarkable Cases Posters 2: Sahar Samani, MD: Artifactual Hypoxemia in Patients With Hydroxyurea-Induced Blue Lunula Fingernails
CHEST 2021 CHEST Challenge
1st Place
The Ohio State University
Sarah Cohen, MD
Gregory Eisinger, MD
Kyle Stinehart, MD
Program Director: Jennifer McCallister, MD, FCCP
2nd Place
SUNY Buffalo
Arjun Saradna, MBBS
Rajesh Kunadharaju, MD
Ahmed Munir, MBBS
Program Director: Jeffrey Mador, MD
3rd Place
Interfaith Medical Center
Tahmina Jahir, MD
Ruby Risal, MD
Binav Shrestha, MBBS
Program Director: Marie Frances Schmidt, MD, FCCP
Repositioning CHEST Networks for the future
Angel Coz, MD, FCCP, Chair, Council of Networks
Cassie Kennedy, MD, FCCP, Vice-Chair, Council of Networks
Aneesa Das, MD, FCCP, Co-Chair, Networks Task Force
David Zielinski, MD, FCCP, Co-Chair, Networks Task Force
Welcome to the new year and your new Networks structure. We are excited to introduce the updated approach that will address the evolving needs of the Networks.
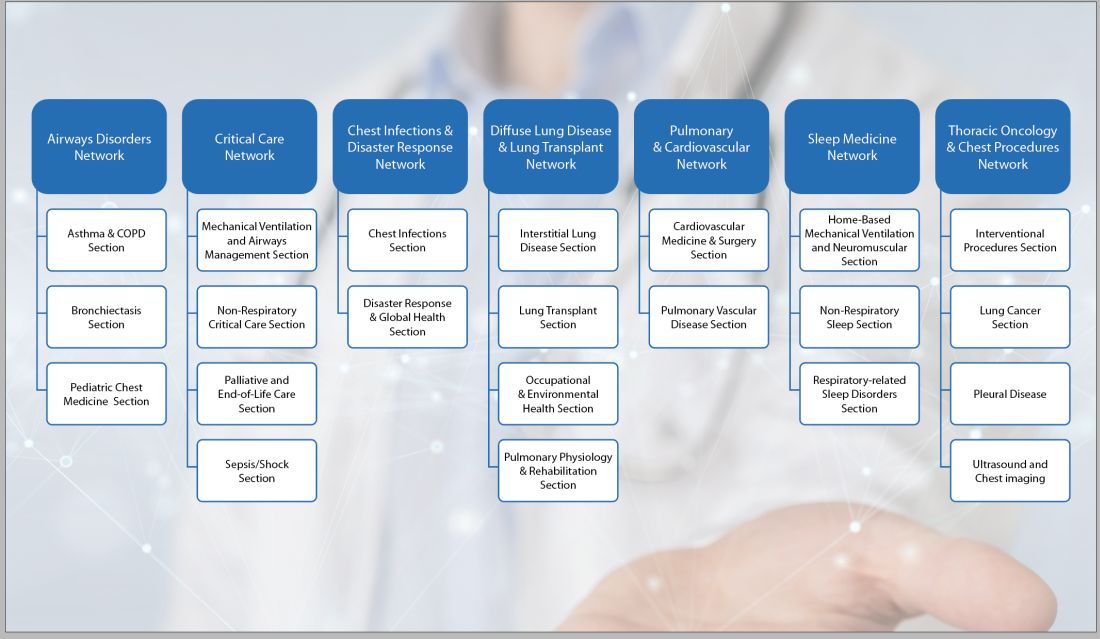
This transition has been more than 2 years in the making. In 2019, under the directive of former CHEST President, Dr. Stephanie Levine, the Networks Task Force was charged with guiding a redevelopment plan with the goal of better serving CHEST membership and aligning closer with curriculum categories and other CHEST priorities.
The Networks Task Force was led by Co-Chairs, Aneesa Das, MD, FCCP, and David Zielinski, MD, FCCP, along with Council of Networks Chair, Angel Coz, MD, FCCP; Jack Buckley, MD, MPH, FCCP; Christopher Carroll, MD, FCCP; De De Gardner, DrPH, RRT, FCCP; Sandhya Khurana, MD, FCCP; and David Schulman, MD, FCCP. They focused on learning what Networks aspects worked, what could be improved, and how to increase the Networks’ overall influence and visibility.
The task force attentively listened to member comments and considered the insight and feedback from Network steering committee leaders. The group learned that Network priorities should include:
- Creating sustainable resources for Network members.
- Increasing digital presence.
- Generating additional leadership pathways and opportunities.
After 2 years of investigation and thoughtful strategic planning, the task force presented a plan to the Council of Networks for a new structure to achieve these objectives. The Governance Committee and College Board of Regents accepted the proposal in summer 2021.
Under the new structure, previously defined steering committees are now known as Sections. There are 22 Sections grouped under the leadership umbrella of 7 Networks. The Networks are composed of the Section chairs, vice chairs and members-at-large. The Council of Networks still provides oversight. This layered approach is intended to help reduce silos and support improved collaboration between groups.
You might notice that many of the new Sections promote different areas of interest These changes allow the groups to align closer to CHEST’s curriculum areas. The Networks are better positioned to act as content experts in more CHEST initiatives. The new Sections each focus on a specific curriculum area of pulmonary, critical care, and sleep medicine.
You will also notice that not all of the original individual Networks mapped over into the new structure. The Task Force determined that these special interests have broad appeal across all domains and would benefit from collective curriculum integration rather than being relegated to individual Sections. The decision to dissolve these individual steering committees was neither taken lightly, nor was it easy. The intent is that these interest areas will have increased access to resources and support under the expanded structure.
We are optimistic this new structure will enhance your Network experience. As with any meaningful change, we may face some growing pains along the way. Your Network leadership is open to feedback and making adjustments to better serve the CHEST membership.
Here are your ways to stay (or get) involved with the Networks and be informed.
- Subscribe to receive the latest information on topics most important to you by joining a Network. Network membership gives you access to Network News, a bi-yearly communication from your Network chair with relevant education course offerings, key events in the CHEST community, and up-to-date information on happenings in your Network.
- Join multiple Networks, or change your affiliation any time, by logging in to your CHEST Account, and indicate your preferences on the Networks page.
- Apply for a position when the call for nominations opens. Keep an eye out soon for an announcement
- Join a Network call. Contact the Networks staff liaison for access to the call information. Call information will be available soon on the individual Network webpages.
In the meantime, please take a few minutes to become acquainted with our new structure. Visit the new Network webpages at chestnet.org/networks.
We hope you are as excited as we are with what’s in store for CHEST members.
Angel Coz, MD, FCCP, Chair, Council of Networks
Cassie Kennedy, MD, FCCP, Vice-Chair, Council of Networks
Aneesa Das, MD, FCCP, Co-Chair, Networks Task Force
David Zielinski, MD, FCCP, Co-Chair, Networks Task Force
Welcome to the new year and your new Networks structure. We are excited to introduce the updated approach that will address the evolving needs of the Networks.
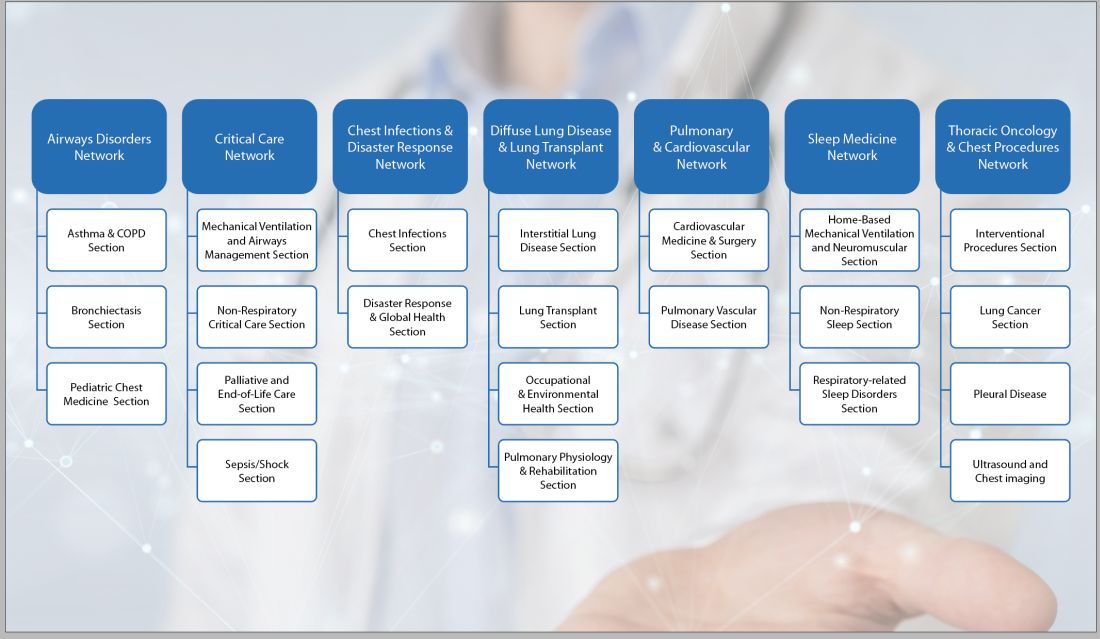
This transition has been more than 2 years in the making. In 2019, under the directive of former CHEST President, Dr. Stephanie Levine, the Networks Task Force was charged with guiding a redevelopment plan with the goal of better serving CHEST membership and aligning closer with curriculum categories and other CHEST priorities.
The Networks Task Force was led by Co-Chairs, Aneesa Das, MD, FCCP, and David Zielinski, MD, FCCP, along with Council of Networks Chair, Angel Coz, MD, FCCP; Jack Buckley, MD, MPH, FCCP; Christopher Carroll, MD, FCCP; De De Gardner, DrPH, RRT, FCCP; Sandhya Khurana, MD, FCCP; and David Schulman, MD, FCCP. They focused on learning what Networks aspects worked, what could be improved, and how to increase the Networks’ overall influence and visibility.
The task force attentively listened to member comments and considered the insight and feedback from Network steering committee leaders. The group learned that Network priorities should include:
- Creating sustainable resources for Network members.
- Increasing digital presence.
- Generating additional leadership pathways and opportunities.
After 2 years of investigation and thoughtful strategic planning, the task force presented a plan to the Council of Networks for a new structure to achieve these objectives. The Governance Committee and College Board of Regents accepted the proposal in summer 2021.
Under the new structure, previously defined steering committees are now known as Sections. There are 22 Sections grouped under the leadership umbrella of 7 Networks. The Networks are composed of the Section chairs, vice chairs and members-at-large. The Council of Networks still provides oversight. This layered approach is intended to help reduce silos and support improved collaboration between groups.
You might notice that many of the new Sections promote different areas of interest These changes allow the groups to align closer to CHEST’s curriculum areas. The Networks are better positioned to act as content experts in more CHEST initiatives. The new Sections each focus on a specific curriculum area of pulmonary, critical care, and sleep medicine.
You will also notice that not all of the original individual Networks mapped over into the new structure. The Task Force determined that these special interests have broad appeal across all domains and would benefit from collective curriculum integration rather than being relegated to individual Sections. The decision to dissolve these individual steering committees was neither taken lightly, nor was it easy. The intent is that these interest areas will have increased access to resources and support under the expanded structure.
We are optimistic this new structure will enhance your Network experience. As with any meaningful change, we may face some growing pains along the way. Your Network leadership is open to feedback and making adjustments to better serve the CHEST membership.
Here are your ways to stay (or get) involved with the Networks and be informed.
- Subscribe to receive the latest information on topics most important to you by joining a Network. Network membership gives you access to Network News, a bi-yearly communication from your Network chair with relevant education course offerings, key events in the CHEST community, and up-to-date information on happenings in your Network.
- Join multiple Networks, or change your affiliation any time, by logging in to your CHEST Account, and indicate your preferences on the Networks page.
- Apply for a position when the call for nominations opens. Keep an eye out soon for an announcement
- Join a Network call. Contact the Networks staff liaison for access to the call information. Call information will be available soon on the individual Network webpages.
In the meantime, please take a few minutes to become acquainted with our new structure. Visit the new Network webpages at chestnet.org/networks.
We hope you are as excited as we are with what’s in store for CHEST members.
Angel Coz, MD, FCCP, Chair, Council of Networks
Cassie Kennedy, MD, FCCP, Vice-Chair, Council of Networks
Aneesa Das, MD, FCCP, Co-Chair, Networks Task Force
David Zielinski, MD, FCCP, Co-Chair, Networks Task Force
Welcome to the new year and your new Networks structure. We are excited to introduce the updated approach that will address the evolving needs of the Networks.
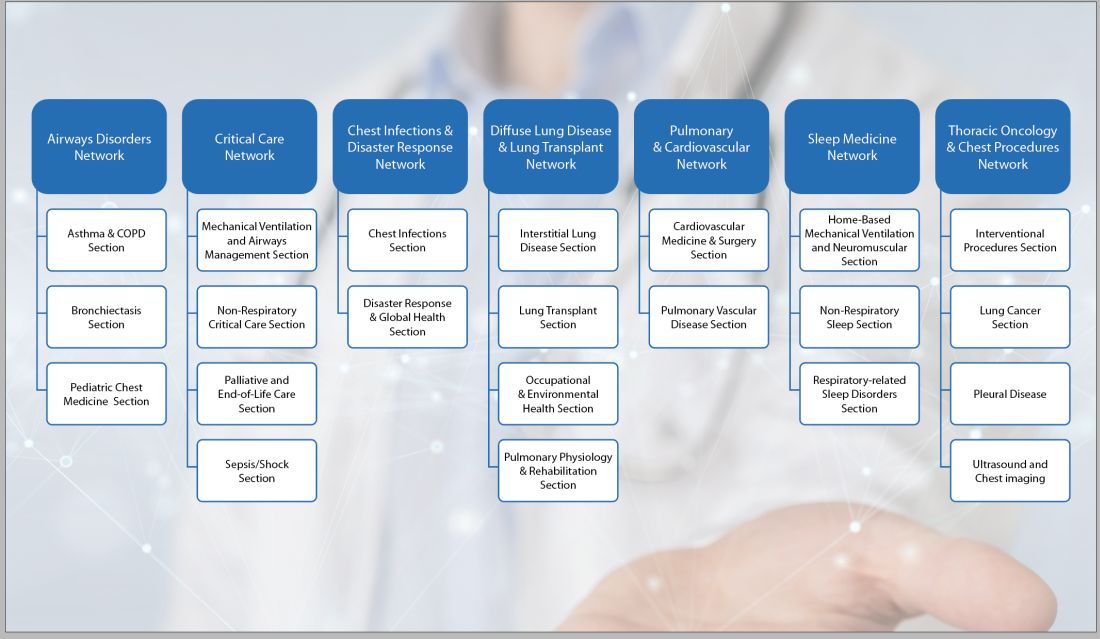
This transition has been more than 2 years in the making. In 2019, under the directive of former CHEST President, Dr. Stephanie Levine, the Networks Task Force was charged with guiding a redevelopment plan with the goal of better serving CHEST membership and aligning closer with curriculum categories and other CHEST priorities.
The Networks Task Force was led by Co-Chairs, Aneesa Das, MD, FCCP, and David Zielinski, MD, FCCP, along with Council of Networks Chair, Angel Coz, MD, FCCP; Jack Buckley, MD, MPH, FCCP; Christopher Carroll, MD, FCCP; De De Gardner, DrPH, RRT, FCCP; Sandhya Khurana, MD, FCCP; and David Schulman, MD, FCCP. They focused on learning what Networks aspects worked, what could be improved, and how to increase the Networks’ overall influence and visibility.
The task force attentively listened to member comments and considered the insight and feedback from Network steering committee leaders. The group learned that Network priorities should include:
- Creating sustainable resources for Network members.
- Increasing digital presence.
- Generating additional leadership pathways and opportunities.
After 2 years of investigation and thoughtful strategic planning, the task force presented a plan to the Council of Networks for a new structure to achieve these objectives. The Governance Committee and College Board of Regents accepted the proposal in summer 2021.
Under the new structure, previously defined steering committees are now known as Sections. There are 22 Sections grouped under the leadership umbrella of 7 Networks. The Networks are composed of the Section chairs, vice chairs and members-at-large. The Council of Networks still provides oversight. This layered approach is intended to help reduce silos and support improved collaboration between groups.
You might notice that many of the new Sections promote different areas of interest These changes allow the groups to align closer to CHEST’s curriculum areas. The Networks are better positioned to act as content experts in more CHEST initiatives. The new Sections each focus on a specific curriculum area of pulmonary, critical care, and sleep medicine.
You will also notice that not all of the original individual Networks mapped over into the new structure. The Task Force determined that these special interests have broad appeal across all domains and would benefit from collective curriculum integration rather than being relegated to individual Sections. The decision to dissolve these individual steering committees was neither taken lightly, nor was it easy. The intent is that these interest areas will have increased access to resources and support under the expanded structure.
We are optimistic this new structure will enhance your Network experience. As with any meaningful change, we may face some growing pains along the way. Your Network leadership is open to feedback and making adjustments to better serve the CHEST membership.
Here are your ways to stay (or get) involved with the Networks and be informed.
- Subscribe to receive the latest information on topics most important to you by joining a Network. Network membership gives you access to Network News, a bi-yearly communication from your Network chair with relevant education course offerings, key events in the CHEST community, and up-to-date information on happenings in your Network.
- Join multiple Networks, or change your affiliation any time, by logging in to your CHEST Account, and indicate your preferences on the Networks page.
- Apply for a position when the call for nominations opens. Keep an eye out soon for an announcement
- Join a Network call. Contact the Networks staff liaison for access to the call information. Call information will be available soon on the individual Network webpages.
In the meantime, please take a few minutes to become acquainted with our new structure. Visit the new Network webpages at chestnet.org/networks.
We hope you are as excited as we are with what’s in store for CHEST members.
This month in the journal CHEST®
Editor’s picks
Revisiting mild asthma: current knowledge and future needs. By Dr. A. Mohan, et al.
Treatment of Mycobacterium abscessus pulmonary disease. By Dr. D. Griffith, et al.
The utility of the rapid shallow breathing index in predicting successful extubation: A systematic review and meta-analysis. By Dr. K. Burns, et al.
National temporal trends in hospitalization and inpatient mortality in patients with pulmonary sarcoidosis in the United States between 2007 – 2018. By Dr. N. Obi Ogugua, et al.
How I Do It: Considering lung transplantation for patients with COVID-19. By Dr. S. Nathan.
Addressing race in pulmonary function testing by aligning intent and evidence with practice and perception. By Dr. N. Bhakta, et al.
Editor’s picks
Editor’s picks
Revisiting mild asthma: current knowledge and future needs. By Dr. A. Mohan, et al.
Treatment of Mycobacterium abscessus pulmonary disease. By Dr. D. Griffith, et al.
The utility of the rapid shallow breathing index in predicting successful extubation: A systematic review and meta-analysis. By Dr. K. Burns, et al.
National temporal trends in hospitalization and inpatient mortality in patients with pulmonary sarcoidosis in the United States between 2007 – 2018. By Dr. N. Obi Ogugua, et al.
How I Do It: Considering lung transplantation for patients with COVID-19. By Dr. S. Nathan.
Addressing race in pulmonary function testing by aligning intent and evidence with practice and perception. By Dr. N. Bhakta, et al.
Revisiting mild asthma: current knowledge and future needs. By Dr. A. Mohan, et al.
Treatment of Mycobacterium abscessus pulmonary disease. By Dr. D. Griffith, et al.
The utility of the rapid shallow breathing index in predicting successful extubation: A systematic review and meta-analysis. By Dr. K. Burns, et al.
National temporal trends in hospitalization and inpatient mortality in patients with pulmonary sarcoidosis in the United States between 2007 – 2018. By Dr. N. Obi Ogugua, et al.
How I Do It: Considering lung transplantation for patients with COVID-19. By Dr. S. Nathan.
Addressing race in pulmonary function testing by aligning intent and evidence with practice and perception. By Dr. N. Bhakta, et al.
The people’s paper
With this issue, we usher in a new era for CHEST Physician, as I hand over the reins of Editor-in-Chief to Angel Coz, MD, FCCP. I have had the pleasure of serving in this role over the last 4 years, and though I will still have the privilege of appearing within these pages with some frequency as I move into my new role as CHEST President, I would like to mark this milestone by passing along a few thoughts on how CHEST Physician has developed over the last few years, and reflecting on the goals I set for us way back in the January 2018 issue (on page 46 of that issue, for those of you holding on to our back issues).
I’ve always viewed CHEST Physician as “the People’s Paper” of CHEST. While we don’t feature first-run scientific manuscripts and authors aren’t likely to reference our articles in other publications, your editorial board and our partners at Frontline aim to give our readers a broad overview of recent publications and presentations in pulmonary, critical care, and sleep medicine, along with expert commentary about how those developments might affect the care we provide to our patients. I can’t thank our editorial board members enough for the hours they spend selecting a small number of items to feature among all of the new medical developments each month.
One of the main goals we had established over the last few years was to create more opportunities for CHEST Physician to serve as the voice of the members and leaders of the American College of Chest Physicians. We achieved the latter part of this goal, with leadership penning quarterly columns on actions of the Board of Regents, developments within the annual meeting, as well as ongoing columns from our NetWorks. And, we have also provided a more reliable voice for our members, with authors of our Sleep Strategies, Critical Care Commentary, and Pulmonary Perspectives columns providing a broader and more representative sample of our membership than ever before.
One of the areas where I would love to see more progress is with reader engagement. It has been a delight to receive feedback from CHEST members, even when the author is taking issue with something we have published. CHEST Physician will be a better publication than it already is with your ongoing input. Please, if you see something that we write that you particularly like (or don’t!) or if there’s something you’d like to see that we haven’t written, please reach out to us! You can always reach us at [email protected].
In closing, I want to thank all of the steadfast CHEST Physician readers for making my 4 years as Editor-in-Chief enjoyable and meaningful. While I am so pleased with the current state of this publication, I cannot wait to see its ongoing evolution under the leadership of Dr. Coz and his editorial board.
With this issue, we usher in a new era for CHEST Physician, as I hand over the reins of Editor-in-Chief to Angel Coz, MD, FCCP. I have had the pleasure of serving in this role over the last 4 years, and though I will still have the privilege of appearing within these pages with some frequency as I move into my new role as CHEST President, I would like to mark this milestone by passing along a few thoughts on how CHEST Physician has developed over the last few years, and reflecting on the goals I set for us way back in the January 2018 issue (on page 46 of that issue, for those of you holding on to our back issues).
I’ve always viewed CHEST Physician as “the People’s Paper” of CHEST. While we don’t feature first-run scientific manuscripts and authors aren’t likely to reference our articles in other publications, your editorial board and our partners at Frontline aim to give our readers a broad overview of recent publications and presentations in pulmonary, critical care, and sleep medicine, along with expert commentary about how those developments might affect the care we provide to our patients. I can’t thank our editorial board members enough for the hours they spend selecting a small number of items to feature among all of the new medical developments each month.
One of the main goals we had established over the last few years was to create more opportunities for CHEST Physician to serve as the voice of the members and leaders of the American College of Chest Physicians. We achieved the latter part of this goal, with leadership penning quarterly columns on actions of the Board of Regents, developments within the annual meeting, as well as ongoing columns from our NetWorks. And, we have also provided a more reliable voice for our members, with authors of our Sleep Strategies, Critical Care Commentary, and Pulmonary Perspectives columns providing a broader and more representative sample of our membership than ever before.
One of the areas where I would love to see more progress is with reader engagement. It has been a delight to receive feedback from CHEST members, even when the author is taking issue with something we have published. CHEST Physician will be a better publication than it already is with your ongoing input. Please, if you see something that we write that you particularly like (or don’t!) or if there’s something you’d like to see that we haven’t written, please reach out to us! You can always reach us at [email protected].
In closing, I want to thank all of the steadfast CHEST Physician readers for making my 4 years as Editor-in-Chief enjoyable and meaningful. While I am so pleased with the current state of this publication, I cannot wait to see its ongoing evolution under the leadership of Dr. Coz and his editorial board.
With this issue, we usher in a new era for CHEST Physician, as I hand over the reins of Editor-in-Chief to Angel Coz, MD, FCCP. I have had the pleasure of serving in this role over the last 4 years, and though I will still have the privilege of appearing within these pages with some frequency as I move into my new role as CHEST President, I would like to mark this milestone by passing along a few thoughts on how CHEST Physician has developed over the last few years, and reflecting on the goals I set for us way back in the January 2018 issue (on page 46 of that issue, for those of you holding on to our back issues).
I’ve always viewed CHEST Physician as “the People’s Paper” of CHEST. While we don’t feature first-run scientific manuscripts and authors aren’t likely to reference our articles in other publications, your editorial board and our partners at Frontline aim to give our readers a broad overview of recent publications and presentations in pulmonary, critical care, and sleep medicine, along with expert commentary about how those developments might affect the care we provide to our patients. I can’t thank our editorial board members enough for the hours they spend selecting a small number of items to feature among all of the new medical developments each month.
One of the main goals we had established over the last few years was to create more opportunities for CHEST Physician to serve as the voice of the members and leaders of the American College of Chest Physicians. We achieved the latter part of this goal, with leadership penning quarterly columns on actions of the Board of Regents, developments within the annual meeting, as well as ongoing columns from our NetWorks. And, we have also provided a more reliable voice for our members, with authors of our Sleep Strategies, Critical Care Commentary, and Pulmonary Perspectives columns providing a broader and more representative sample of our membership than ever before.
One of the areas where I would love to see more progress is with reader engagement. It has been a delight to receive feedback from CHEST members, even when the author is taking issue with something we have published. CHEST Physician will be a better publication than it already is with your ongoing input. Please, if you see something that we write that you particularly like (or don’t!) or if there’s something you’d like to see that we haven’t written, please reach out to us! You can always reach us at [email protected].
In closing, I want to thank all of the steadfast CHEST Physician readers for making my 4 years as Editor-in-Chief enjoyable and meaningful. While I am so pleased with the current state of this publication, I cannot wait to see its ongoing evolution under the leadership of Dr. Coz and his editorial board.
Top case
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Vivy Tran, MD, wrote in “Definitive diverticular hemorrhage: Diagnosis and management”:
Diverticular hemorrhage is the most common cause of colonic bleeding, accounting for 20%-65% of cases of severe lower intestinal bleeding in adults. Urgent colonoscopy after purging the colon of blood, clots, and stool is the most accurate method of diagnosing and guiding treatment of definitive diverticular hemorrhage. The diagnosis of definitive diverticular hemorrhage depends upon identification of some stigmata of recent hemorrhage in a single diverticulum, which can include active arterial bleeding, oozing, non-bleeding visible vessel, adherent clot, or flat spot. Although other approaches, such as nuclear medicine scans and angiography of various types (CT, MRI, or standard angiography), for the early diagnosis of patients with severe hematochezia are utilized in many medical centers, only active bleeding can be detected by these techniques.
Would love to hear how diverticular bleeds are managed at your institution.
See how AGA members responded and join the discussion.
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Vivy Tran, MD, wrote in “Definitive diverticular hemorrhage: Diagnosis and management”:
Diverticular hemorrhage is the most common cause of colonic bleeding, accounting for 20%-65% of cases of severe lower intestinal bleeding in adults. Urgent colonoscopy after purging the colon of blood, clots, and stool is the most accurate method of diagnosing and guiding treatment of definitive diverticular hemorrhage. The diagnosis of definitive diverticular hemorrhage depends upon identification of some stigmata of recent hemorrhage in a single diverticulum, which can include active arterial bleeding, oozing, non-bleeding visible vessel, adherent clot, or flat spot. Although other approaches, such as nuclear medicine scans and angiography of various types (CT, MRI, or standard angiography), for the early diagnosis of patients with severe hematochezia are utilized in many medical centers, only active bleeding can be detected by these techniques.
Would love to hear how diverticular bleeds are managed at your institution.
See how AGA members responded and join the discussion.
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Vivy Tran, MD, wrote in “Definitive diverticular hemorrhage: Diagnosis and management”:
Diverticular hemorrhage is the most common cause of colonic bleeding, accounting for 20%-65% of cases of severe lower intestinal bleeding in adults. Urgent colonoscopy after purging the colon of blood, clots, and stool is the most accurate method of diagnosing and guiding treatment of definitive diverticular hemorrhage. The diagnosis of definitive diverticular hemorrhage depends upon identification of some stigmata of recent hemorrhage in a single diverticulum, which can include active arterial bleeding, oozing, non-bleeding visible vessel, adherent clot, or flat spot. Although other approaches, such as nuclear medicine scans and angiography of various types (CT, MRI, or standard angiography), for the early diagnosis of patients with severe hematochezia are utilized in many medical centers, only active bleeding can be detected by these techniques.
Would love to hear how diverticular bleeds are managed at your institution.
See how AGA members responded and join the discussion.
New update on perforation management
One of the most devastating complications in any endoscopic procedure is a perforation that may result in a life-threatening situation for the patient and abrupt termination of the intended procedure. The new AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review offers a practical approach to prevent GI perforations, as well as detect subtle signs of and endoscopically manage them.
Best practice advice
- The area of perforation should be kept clean to prevent any spillage of gastrointestinal contents into the perforation by aspirating liquids and, if necessary, changing the patient position to bring the perforation into a nondependent location while minimizing insufflation of carbon dioxide to avoid compartment syndrome.
- Use of carbon dioxide for insufflation is encouraged for all endoscopic procedures, especially any endoscopic procedure with increased risk of perforation. If available, carbon dioxide should be used for all endoscopic procedures.
- All endoscopists should be aware of the procedures that carry an increased risk for perforation such as any dilation, foreign body removal, any per oral endoscopic myotomy (Zenker’s, esophageal, pyloric), stricture incision, thermal coagulation for hemostasis or tumor ablation, percutaneous endoscopic gastrostomy, ampullectomy, endoscopic mucosal resectio, endoscopic submucosal dissection, endoluminal stenting with self-expanding metal stent, full-thickness endoscopic resection, endoscopic retrograde cholangiopancreatography in surgically altered anatomy, endoscopic ultrasound (EUS)–guided biliary and pancreatic access, EUS-guided cystogastrostomy, and endoscopic gastroenterostomy using a lumen apposing metal stent.
- Urgent surgical consultation should be highly considered in all cases with perforation even when endoscopic repair is technically successful.
One of the most devastating complications in any endoscopic procedure is a perforation that may result in a life-threatening situation for the patient and abrupt termination of the intended procedure. The new AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review offers a practical approach to prevent GI perforations, as well as detect subtle signs of and endoscopically manage them.
Best practice advice
- The area of perforation should be kept clean to prevent any spillage of gastrointestinal contents into the perforation by aspirating liquids and, if necessary, changing the patient position to bring the perforation into a nondependent location while minimizing insufflation of carbon dioxide to avoid compartment syndrome.
- Use of carbon dioxide for insufflation is encouraged for all endoscopic procedures, especially any endoscopic procedure with increased risk of perforation. If available, carbon dioxide should be used for all endoscopic procedures.
- All endoscopists should be aware of the procedures that carry an increased risk for perforation such as any dilation, foreign body removal, any per oral endoscopic myotomy (Zenker’s, esophageal, pyloric), stricture incision, thermal coagulation for hemostasis or tumor ablation, percutaneous endoscopic gastrostomy, ampullectomy, endoscopic mucosal resectio, endoscopic submucosal dissection, endoluminal stenting with self-expanding metal stent, full-thickness endoscopic resection, endoscopic retrograde cholangiopancreatography in surgically altered anatomy, endoscopic ultrasound (EUS)–guided biliary and pancreatic access, EUS-guided cystogastrostomy, and endoscopic gastroenterostomy using a lumen apposing metal stent.
- Urgent surgical consultation should be highly considered in all cases with perforation even when endoscopic repair is technically successful.
One of the most devastating complications in any endoscopic procedure is a perforation that may result in a life-threatening situation for the patient and abrupt termination of the intended procedure. The new AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review offers a practical approach to prevent GI perforations, as well as detect subtle signs of and endoscopically manage them.
Best practice advice
- The area of perforation should be kept clean to prevent any spillage of gastrointestinal contents into the perforation by aspirating liquids and, if necessary, changing the patient position to bring the perforation into a nondependent location while minimizing insufflation of carbon dioxide to avoid compartment syndrome.
- Use of carbon dioxide for insufflation is encouraged for all endoscopic procedures, especially any endoscopic procedure with increased risk of perforation. If available, carbon dioxide should be used for all endoscopic procedures.
- All endoscopists should be aware of the procedures that carry an increased risk for perforation such as any dilation, foreign body removal, any per oral endoscopic myotomy (Zenker’s, esophageal, pyloric), stricture incision, thermal coagulation for hemostasis or tumor ablation, percutaneous endoscopic gastrostomy, ampullectomy, endoscopic mucosal resectio, endoscopic submucosal dissection, endoluminal stenting with self-expanding metal stent, full-thickness endoscopic resection, endoscopic retrograde cholangiopancreatography in surgically altered anatomy, endoscopic ultrasound (EUS)–guided biliary and pancreatic access, EUS-guided cystogastrostomy, and endoscopic gastroenterostomy using a lumen apposing metal stent.
- Urgent surgical consultation should be highly considered in all cases with perforation even when endoscopic repair is technically successful.















