User login
Antifungal shows promise in hematologic conditions

WASHINGTON, DC—A new antifungal agent is as effective as an existing drug against invasive mold infection in patients with hematologic disorders, results of a phase 3 trial suggest.
Overall response and all-cause mortality rates were comparable with the newer drug, isavuconazole (ISA), and the existing drug, voriconazole (VRC).
The overall rates of treatment-emergent adverse events were comparable as well, but ISA was associated with a significantly lower incidence of several events.
Kieren Marr, MD, of Johns Hopkins University in Baltimore, Maryland, and her colleagues presented these results in a subset of patients from the SECURE trial at the 54th Interscience Conference on Antimicrobial Agents and Chemotherapy (poster M-1757).
Patient characteristics and safety outcomes
Of the 433 patients with a hematologic disorder enrolled in the trial, 217 had proven or probable invasive mold infection. The researchers divided patients into 2 groups according to disease: those with acute myeloid leukemia (AML) and those with acute lymphoblastic leukemia (ALL) or other conditions.
In all, 102 patients had AML, and 115 had ALL (n=28) or other conditions, including non-Hodgkin lymphoma (n=19), chronic lymphocytic leukemia (n=15), refractory anemia with excess blasts (n=9), myelodysplastic syndrome (n=8), chronic myeloid leukemia (n=6), and “other” underlying conditions (n=30).
Patients were randomized to receive VRC (n=105) or ISA (N=112). Thirty patients in the ISA arm and 26 in the VRC arm had undergone allogeneic transplant prior to therapy.
The primary outcome was all-cause mortality at day 42. Overall response and safety were secondary endpoints.
The overall rates of treatment-emergent adverse events were similar between ISA and VRC arms. Ninety-seven percent of patients in the ISA arm and 98% of patients in the VRC arm reported at least 1 treatment-emergent adverse event.
However, patients in the ISA arm had significantly fewer (P<0.05) events for the cardiac disorders, eye, psychiatric disorders, renal and urinary, and vascular system organ classes.
Response and mortality
All-cause mortality rates were comparable between the ISA and VRC arms—22% and 24%, respectively—as were overall response rates—39% and 34%, respectively—and complete response rates—13% and 10%, respectively.
All-cause mortality rates among patients with AML were 18% in the ISA arm and 15% in the VRC arm. Overall response rates were 36% and 48%, respectively.
For patients with ALL or other hematologic conditions, all-cause mortality rates were 26% in the ISA arm and 32% in the VRC arm. Overall response rates were 42% and 21%, respectively.
In transplant patients, the all-cause mortality rate was 27% for both the ISA and VRC arms. The overall response rate was 27% for both arms as well.
“These results show the potential of isavuconazole as a potent antifungal in the fight against invasive mold disease,” Dr Marr said.
ISA is an investigational antifungal under development by Astellas and Basilea Pharmaceutica International Ltd. The SECURE trial was funded by Astellas.
The US Food and Drug Administration recently accepted a new drug application seeking approval for ISA for the treatment of invasive aspergillosis and invasive mucormycosis. ![]()

WASHINGTON, DC—A new antifungal agent is as effective as an existing drug against invasive mold infection in patients with hematologic disorders, results of a phase 3 trial suggest.
Overall response and all-cause mortality rates were comparable with the newer drug, isavuconazole (ISA), and the existing drug, voriconazole (VRC).
The overall rates of treatment-emergent adverse events were comparable as well, but ISA was associated with a significantly lower incidence of several events.
Kieren Marr, MD, of Johns Hopkins University in Baltimore, Maryland, and her colleagues presented these results in a subset of patients from the SECURE trial at the 54th Interscience Conference on Antimicrobial Agents and Chemotherapy (poster M-1757).
Patient characteristics and safety outcomes
Of the 433 patients with a hematologic disorder enrolled in the trial, 217 had proven or probable invasive mold infection. The researchers divided patients into 2 groups according to disease: those with acute myeloid leukemia (AML) and those with acute lymphoblastic leukemia (ALL) or other conditions.
In all, 102 patients had AML, and 115 had ALL (n=28) or other conditions, including non-Hodgkin lymphoma (n=19), chronic lymphocytic leukemia (n=15), refractory anemia with excess blasts (n=9), myelodysplastic syndrome (n=8), chronic myeloid leukemia (n=6), and “other” underlying conditions (n=30).
Patients were randomized to receive VRC (n=105) or ISA (N=112). Thirty patients in the ISA arm and 26 in the VRC arm had undergone allogeneic transplant prior to therapy.
The primary outcome was all-cause mortality at day 42. Overall response and safety were secondary endpoints.
The overall rates of treatment-emergent adverse events were similar between ISA and VRC arms. Ninety-seven percent of patients in the ISA arm and 98% of patients in the VRC arm reported at least 1 treatment-emergent adverse event.
However, patients in the ISA arm had significantly fewer (P<0.05) events for the cardiac disorders, eye, psychiatric disorders, renal and urinary, and vascular system organ classes.
Response and mortality
All-cause mortality rates were comparable between the ISA and VRC arms—22% and 24%, respectively—as were overall response rates—39% and 34%, respectively—and complete response rates—13% and 10%, respectively.
All-cause mortality rates among patients with AML were 18% in the ISA arm and 15% in the VRC arm. Overall response rates were 36% and 48%, respectively.
For patients with ALL or other hematologic conditions, all-cause mortality rates were 26% in the ISA arm and 32% in the VRC arm. Overall response rates were 42% and 21%, respectively.
In transplant patients, the all-cause mortality rate was 27% for both the ISA and VRC arms. The overall response rate was 27% for both arms as well.
“These results show the potential of isavuconazole as a potent antifungal in the fight against invasive mold disease,” Dr Marr said.
ISA is an investigational antifungal under development by Astellas and Basilea Pharmaceutica International Ltd. The SECURE trial was funded by Astellas.
The US Food and Drug Administration recently accepted a new drug application seeking approval for ISA for the treatment of invasive aspergillosis and invasive mucormycosis. ![]()

WASHINGTON, DC—A new antifungal agent is as effective as an existing drug against invasive mold infection in patients with hematologic disorders, results of a phase 3 trial suggest.
Overall response and all-cause mortality rates were comparable with the newer drug, isavuconazole (ISA), and the existing drug, voriconazole (VRC).
The overall rates of treatment-emergent adverse events were comparable as well, but ISA was associated with a significantly lower incidence of several events.
Kieren Marr, MD, of Johns Hopkins University in Baltimore, Maryland, and her colleagues presented these results in a subset of patients from the SECURE trial at the 54th Interscience Conference on Antimicrobial Agents and Chemotherapy (poster M-1757).
Patient characteristics and safety outcomes
Of the 433 patients with a hematologic disorder enrolled in the trial, 217 had proven or probable invasive mold infection. The researchers divided patients into 2 groups according to disease: those with acute myeloid leukemia (AML) and those with acute lymphoblastic leukemia (ALL) or other conditions.
In all, 102 patients had AML, and 115 had ALL (n=28) or other conditions, including non-Hodgkin lymphoma (n=19), chronic lymphocytic leukemia (n=15), refractory anemia with excess blasts (n=9), myelodysplastic syndrome (n=8), chronic myeloid leukemia (n=6), and “other” underlying conditions (n=30).
Patients were randomized to receive VRC (n=105) or ISA (N=112). Thirty patients in the ISA arm and 26 in the VRC arm had undergone allogeneic transplant prior to therapy.
The primary outcome was all-cause mortality at day 42. Overall response and safety were secondary endpoints.
The overall rates of treatment-emergent adverse events were similar between ISA and VRC arms. Ninety-seven percent of patients in the ISA arm and 98% of patients in the VRC arm reported at least 1 treatment-emergent adverse event.
However, patients in the ISA arm had significantly fewer (P<0.05) events for the cardiac disorders, eye, psychiatric disorders, renal and urinary, and vascular system organ classes.
Response and mortality
All-cause mortality rates were comparable between the ISA and VRC arms—22% and 24%, respectively—as were overall response rates—39% and 34%, respectively—and complete response rates—13% and 10%, respectively.
All-cause mortality rates among patients with AML were 18% in the ISA arm and 15% in the VRC arm. Overall response rates were 36% and 48%, respectively.
For patients with ALL or other hematologic conditions, all-cause mortality rates were 26% in the ISA arm and 32% in the VRC arm. Overall response rates were 42% and 21%, respectively.
In transplant patients, the all-cause mortality rate was 27% for both the ISA and VRC arms. The overall response rate was 27% for both arms as well.
“These results show the potential of isavuconazole as a potent antifungal in the fight against invasive mold disease,” Dr Marr said.
ISA is an investigational antifungal under development by Astellas and Basilea Pharmaceutica International Ltd. The SECURE trial was funded by Astellas.
The US Food and Drug Administration recently accepted a new drug application seeking approval for ISA for the treatment of invasive aspergillosis and invasive mucormycosis. ![]()
Team identifies risk factors for vitiligo, AA in cGVHD

Credit: PLOS ONE
Results of a retrospective study have revealed factors that appear to increase the risk of vitiligo and alopecia areata (AA) in patients who develop chronic graft-vs-host disease (cGVHD) after a stem cell transplant.
Multivariable analysis suggested that a female donor to male recipient sex mismatch and positive test results for anticardiolipin immunoglobulin G (ACA-IgG) were both significantly associated with vitiligo and/or AA.
This research was published in JAMA Dermatology.
Edward W. Cowen, MD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues conducted the study in 282 adult and pediatric patients with cGVHD.
Fifteen of the patients (5.3%) had vitiligo and/or AA. One patient had only AA, 1 had vitiligo and AA, and the rest had vitiligo alone. The median age of these patients at enrollment was 38 years (range, 9-69 years), and most were male (n=10).
Most patients had received a transplant to treat chronic myelogenous leukemia (n=5) or acute leukemia/myelodysplastic syndrome (n=5). Most patients (n=13) had an HLA-identical donor and received a peripheral blood stem cell transplant (n=9).
Eleven patients had concomitant skin cGVHD at the time of evaluation, and it was most often sclerotic-type cGVHD (n=9).
For the 5 vitiligo patients in whom the onset of skin depigmentation was documented, pigment changes occurred at a median of 41 months (range, 24-84) after transplant.
Depigmentation was classic periorbital, perioral, acrofacial involvement in 6 patients, generalized in 6 patients, and torso-predominant in 2 patients. Trichrome vitiligo was present in 3 patients, and poliosis occurred in 5 patients. In both AA patients, hair loss was localized to the scalp.
The researchers evaluated demographic, clinical, and laboratory data from these patients, and used univariate and multivariable logistic regression analyses to identify risk factors for vitiligo and AA.
Univariate analysis suggested the following factors were significantly associated with vitiligo and/or AA: female donor to male recipient sex mismatch (P=0.003), positive test results for ACA-IgG (P=0.03) or antiparietal antibody (P=0.049), elevated CD19 (P=0.045), and normal or elevated IgG (P=0.02).
However, only positive ACA-IgG results and female donor to male recipient mismatch retained significance in multivariable analysis (P=0.01 and P=0.003, respectively).
The researchers said additional studies are needed to clarify whether these risk factors can lead to a better understanding of the pathomechanisms of cGVHD. ![]()

Credit: PLOS ONE
Results of a retrospective study have revealed factors that appear to increase the risk of vitiligo and alopecia areata (AA) in patients who develop chronic graft-vs-host disease (cGVHD) after a stem cell transplant.
Multivariable analysis suggested that a female donor to male recipient sex mismatch and positive test results for anticardiolipin immunoglobulin G (ACA-IgG) were both significantly associated with vitiligo and/or AA.
This research was published in JAMA Dermatology.
Edward W. Cowen, MD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues conducted the study in 282 adult and pediatric patients with cGVHD.
Fifteen of the patients (5.3%) had vitiligo and/or AA. One patient had only AA, 1 had vitiligo and AA, and the rest had vitiligo alone. The median age of these patients at enrollment was 38 years (range, 9-69 years), and most were male (n=10).
Most patients had received a transplant to treat chronic myelogenous leukemia (n=5) or acute leukemia/myelodysplastic syndrome (n=5). Most patients (n=13) had an HLA-identical donor and received a peripheral blood stem cell transplant (n=9).
Eleven patients had concomitant skin cGVHD at the time of evaluation, and it was most often sclerotic-type cGVHD (n=9).
For the 5 vitiligo patients in whom the onset of skin depigmentation was documented, pigment changes occurred at a median of 41 months (range, 24-84) after transplant.
Depigmentation was classic periorbital, perioral, acrofacial involvement in 6 patients, generalized in 6 patients, and torso-predominant in 2 patients. Trichrome vitiligo was present in 3 patients, and poliosis occurred in 5 patients. In both AA patients, hair loss was localized to the scalp.
The researchers evaluated demographic, clinical, and laboratory data from these patients, and used univariate and multivariable logistic regression analyses to identify risk factors for vitiligo and AA.
Univariate analysis suggested the following factors were significantly associated with vitiligo and/or AA: female donor to male recipient sex mismatch (P=0.003), positive test results for ACA-IgG (P=0.03) or antiparietal antibody (P=0.049), elevated CD19 (P=0.045), and normal or elevated IgG (P=0.02).
However, only positive ACA-IgG results and female donor to male recipient mismatch retained significance in multivariable analysis (P=0.01 and P=0.003, respectively).
The researchers said additional studies are needed to clarify whether these risk factors can lead to a better understanding of the pathomechanisms of cGVHD. ![]()

Credit: PLOS ONE
Results of a retrospective study have revealed factors that appear to increase the risk of vitiligo and alopecia areata (AA) in patients who develop chronic graft-vs-host disease (cGVHD) after a stem cell transplant.
Multivariable analysis suggested that a female donor to male recipient sex mismatch and positive test results for anticardiolipin immunoglobulin G (ACA-IgG) were both significantly associated with vitiligo and/or AA.
This research was published in JAMA Dermatology.
Edward W. Cowen, MD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues conducted the study in 282 adult and pediatric patients with cGVHD.
Fifteen of the patients (5.3%) had vitiligo and/or AA. One patient had only AA, 1 had vitiligo and AA, and the rest had vitiligo alone. The median age of these patients at enrollment was 38 years (range, 9-69 years), and most were male (n=10).
Most patients had received a transplant to treat chronic myelogenous leukemia (n=5) or acute leukemia/myelodysplastic syndrome (n=5). Most patients (n=13) had an HLA-identical donor and received a peripheral blood stem cell transplant (n=9).
Eleven patients had concomitant skin cGVHD at the time of evaluation, and it was most often sclerotic-type cGVHD (n=9).
For the 5 vitiligo patients in whom the onset of skin depigmentation was documented, pigment changes occurred at a median of 41 months (range, 24-84) after transplant.
Depigmentation was classic periorbital, perioral, acrofacial involvement in 6 patients, generalized in 6 patients, and torso-predominant in 2 patients. Trichrome vitiligo was present in 3 patients, and poliosis occurred in 5 patients. In both AA patients, hair loss was localized to the scalp.
The researchers evaluated demographic, clinical, and laboratory data from these patients, and used univariate and multivariable logistic regression analyses to identify risk factors for vitiligo and AA.
Univariate analysis suggested the following factors were significantly associated with vitiligo and/or AA: female donor to male recipient sex mismatch (P=0.003), positive test results for ACA-IgG (P=0.03) or antiparietal antibody (P=0.049), elevated CD19 (P=0.045), and normal or elevated IgG (P=0.02).
However, only positive ACA-IgG results and female donor to male recipient mismatch retained significance in multivariable analysis (P=0.01 and P=0.003, respectively).
The researchers said additional studies are needed to clarify whether these risk factors can lead to a better understanding of the pathomechanisms of cGVHD. ![]()
Overcoming an obstacle to RBC development

Researchers have discovered a natural barrier to hematopoiesis and a way to circumvent it, according to a paper published in Blood.
The group found that components of the exosome complex—exosc8 and exosc9—suppress red blood cell (RBC) maturation.
“From a fundamental perspective, this is very important because this mechanism counteracts the development of precursor cells into red blood cells, thereby establishing a balance between developed cells and the progenitor population,” said study author Emery Bresnick, PhD, of the UW School of Medicine and Public Health in Madison, Wisconsin.
“In the context of translation, if you want to maximize the output of end-stage red blood cells, which we’re not able to do at this time, our study provides a rational approach involving lowering the levels of these subunits.”
Specifically, the researchers found that GATA-1 and Foxo3 can repress the exosome components, thereby allowing for RBC maturation.
The barrier explained
Dr Bresnick and his colleagues noted that the primary obstacle in converting hematopoietic stem cells into RBCs involves late-stage maturation.
“The problem isn’t simply getting erythroid precursors produced by the bucket, but understanding how these cells systematically lose their nuclei and organelles to become a red blood cell, the final product,” Dr Bresnick said.
“This is the bottleneck, even in the stem cell world of embryonic and induced pluripotent stem cells. We know little about how the cell orchestrates the intricate processes that constitute late-stage maturation.”
At the end of RBC development, the erythroid precursor must eject its own genetic material via enucleation. Although it’s clear why enucleation is important (making the cell more flexible and allowing it to carry more oxygen), exactly how the cell does it has been unclear.
Besides ejecting the nucleus, the cell must be cleared of other organelles, such as the endoplasmic reticulum and mitochondria. This process (autophagy) is linked to a pair of transcription factors—GATA1 and Foxo3—that control gene expression important in RBC development.
Because they knew GATA1 and Foxo3 promote autophagy, Dr Bresnick and his colleagues wondered if the proteins these transcription factors repress play an important role in cell maturation.
This led them to identify exosc8 and exosc9, two units of the exosome that ultimately established the development barrier.
The researchers plan to continue studying the exosome because many RNAs in the cell are not degraded by the exosome. Determining exactly how the exosome decides what RNA to dispose of may provide an even better understanding of the newly discovered barrier.
“One goal we have is to establish the specific RNA targets the exosome is regulating that are responsible for the blockade,” Dr Bresnick said. “In doing so, we might even uncover targets that are easier to manipulate than the exosome itself.” ![]()

Researchers have discovered a natural barrier to hematopoiesis and a way to circumvent it, according to a paper published in Blood.
The group found that components of the exosome complex—exosc8 and exosc9—suppress red blood cell (RBC) maturation.
“From a fundamental perspective, this is very important because this mechanism counteracts the development of precursor cells into red blood cells, thereby establishing a balance between developed cells and the progenitor population,” said study author Emery Bresnick, PhD, of the UW School of Medicine and Public Health in Madison, Wisconsin.
“In the context of translation, if you want to maximize the output of end-stage red blood cells, which we’re not able to do at this time, our study provides a rational approach involving lowering the levels of these subunits.”
Specifically, the researchers found that GATA-1 and Foxo3 can repress the exosome components, thereby allowing for RBC maturation.
The barrier explained
Dr Bresnick and his colleagues noted that the primary obstacle in converting hematopoietic stem cells into RBCs involves late-stage maturation.
“The problem isn’t simply getting erythroid precursors produced by the bucket, but understanding how these cells systematically lose their nuclei and organelles to become a red blood cell, the final product,” Dr Bresnick said.
“This is the bottleneck, even in the stem cell world of embryonic and induced pluripotent stem cells. We know little about how the cell orchestrates the intricate processes that constitute late-stage maturation.”
At the end of RBC development, the erythroid precursor must eject its own genetic material via enucleation. Although it’s clear why enucleation is important (making the cell more flexible and allowing it to carry more oxygen), exactly how the cell does it has been unclear.
Besides ejecting the nucleus, the cell must be cleared of other organelles, such as the endoplasmic reticulum and mitochondria. This process (autophagy) is linked to a pair of transcription factors—GATA1 and Foxo3—that control gene expression important in RBC development.
Because they knew GATA1 and Foxo3 promote autophagy, Dr Bresnick and his colleagues wondered if the proteins these transcription factors repress play an important role in cell maturation.
This led them to identify exosc8 and exosc9, two units of the exosome that ultimately established the development barrier.
The researchers plan to continue studying the exosome because many RNAs in the cell are not degraded by the exosome. Determining exactly how the exosome decides what RNA to dispose of may provide an even better understanding of the newly discovered barrier.
“One goal we have is to establish the specific RNA targets the exosome is regulating that are responsible for the blockade,” Dr Bresnick said. “In doing so, we might even uncover targets that are easier to manipulate than the exosome itself.” ![]()

Researchers have discovered a natural barrier to hematopoiesis and a way to circumvent it, according to a paper published in Blood.
The group found that components of the exosome complex—exosc8 and exosc9—suppress red blood cell (RBC) maturation.
“From a fundamental perspective, this is very important because this mechanism counteracts the development of precursor cells into red blood cells, thereby establishing a balance between developed cells and the progenitor population,” said study author Emery Bresnick, PhD, of the UW School of Medicine and Public Health in Madison, Wisconsin.
“In the context of translation, if you want to maximize the output of end-stage red blood cells, which we’re not able to do at this time, our study provides a rational approach involving lowering the levels of these subunits.”
Specifically, the researchers found that GATA-1 and Foxo3 can repress the exosome components, thereby allowing for RBC maturation.
The barrier explained
Dr Bresnick and his colleagues noted that the primary obstacle in converting hematopoietic stem cells into RBCs involves late-stage maturation.
“The problem isn’t simply getting erythroid precursors produced by the bucket, but understanding how these cells systematically lose their nuclei and organelles to become a red blood cell, the final product,” Dr Bresnick said.
“This is the bottleneck, even in the stem cell world of embryonic and induced pluripotent stem cells. We know little about how the cell orchestrates the intricate processes that constitute late-stage maturation.”
At the end of RBC development, the erythroid precursor must eject its own genetic material via enucleation. Although it’s clear why enucleation is important (making the cell more flexible and allowing it to carry more oxygen), exactly how the cell does it has been unclear.
Besides ejecting the nucleus, the cell must be cleared of other organelles, such as the endoplasmic reticulum and mitochondria. This process (autophagy) is linked to a pair of transcription factors—GATA1 and Foxo3—that control gene expression important in RBC development.
Because they knew GATA1 and Foxo3 promote autophagy, Dr Bresnick and his colleagues wondered if the proteins these transcription factors repress play an important role in cell maturation.
This led them to identify exosc8 and exosc9, two units of the exosome that ultimately established the development barrier.
The researchers plan to continue studying the exosome because many RNAs in the cell are not degraded by the exosome. Determining exactly how the exosome decides what RNA to dispose of may provide an even better understanding of the newly discovered barrier.
“One goal we have is to establish the specific RNA targets the exosome is regulating that are responsible for the blockade,” Dr Bresnick said. “In doing so, we might even uncover targets that are easier to manipulate than the exosome itself.” ![]()
Fusion proteins enable expansion of HSPCs

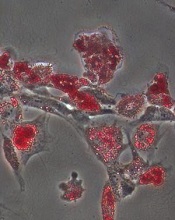
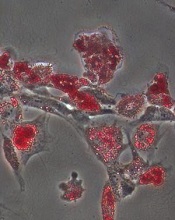
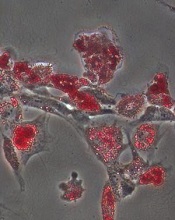
Credit: Chad McNeeley
A new technique has allowed researchers to expand hematopoietic stem and progenitor cells (HSPCs) from multiple sources.
The team developed fusion proteins and introduced them to HSPCs ex vivo.
This approach expanded cell populations whether HSPCs were derived from cord blood, bone marrow, or peripheral blood.
The potential clinical applications for this work range from immunodeficiency disorders to hematologic and other malignancies, according to the researchers.
Yosef Refaeli, PhD, of Taiga Biotechnologies, Inc. in Aurora, Colorado, and his colleagues described this work in PLOS ONE.
The team first cultured human or murine HSPCs with a pair of fusion proteins—the protein transduction domain of the HIV-1 transactivation protein (Tat) and either the Open Reading Frame for human MYC or a truncated form of human Bcl-2 that was deleted for the unstructured loop domain.
With this technique, the researchers were able to elicit an 87-fold expansion of HSPCs from mouse bone marrow, a 16.6-fold expansion of HSPCs from human cord blood, a 13.6-fold expansion of HSPCs from human peripheral blood cells mobilized by G-CSF, and a 10-fold expansion of HSPCs from human bone marrow.
The team then tested the biological function of the expanded cells, and they found the cells gave rise to BFU-E, CFU-M, CFU-G, and CFU-GM colonies in vitro.
When transplanted into irradiated mice, the expanded cells gave rise to mature hematopoietic populations and a self-renewing cell population that was able to support hematopoiesis upon serial transplantation.
The researchers said these results suggest their technique may be an attractive approach to expand human HSPCs ex vivo for clinical use.
The team’s goal now is to move the technology from the lab into clinical trials. Taiga Biotechnologies is in the process of setting up clinical trials testing this approach. ![]()

Credit: Chad McNeeley
A new technique has allowed researchers to expand hematopoietic stem and progenitor cells (HSPCs) from multiple sources.
The team developed fusion proteins and introduced them to HSPCs ex vivo.
This approach expanded cell populations whether HSPCs were derived from cord blood, bone marrow, or peripheral blood.
The potential clinical applications for this work range from immunodeficiency disorders to hematologic and other malignancies, according to the researchers.
Yosef Refaeli, PhD, of Taiga Biotechnologies, Inc. in Aurora, Colorado, and his colleagues described this work in PLOS ONE.
The team first cultured human or murine HSPCs with a pair of fusion proteins—the protein transduction domain of the HIV-1 transactivation protein (Tat) and either the Open Reading Frame for human MYC or a truncated form of human Bcl-2 that was deleted for the unstructured loop domain.
With this technique, the researchers were able to elicit an 87-fold expansion of HSPCs from mouse bone marrow, a 16.6-fold expansion of HSPCs from human cord blood, a 13.6-fold expansion of HSPCs from human peripheral blood cells mobilized by G-CSF, and a 10-fold expansion of HSPCs from human bone marrow.
The team then tested the biological function of the expanded cells, and they found the cells gave rise to BFU-E, CFU-M, CFU-G, and CFU-GM colonies in vitro.
When transplanted into irradiated mice, the expanded cells gave rise to mature hematopoietic populations and a self-renewing cell population that was able to support hematopoiesis upon serial transplantation.
The researchers said these results suggest their technique may be an attractive approach to expand human HSPCs ex vivo for clinical use.
The team’s goal now is to move the technology from the lab into clinical trials. Taiga Biotechnologies is in the process of setting up clinical trials testing this approach. ![]()

Credit: Chad McNeeley
A new technique has allowed researchers to expand hematopoietic stem and progenitor cells (HSPCs) from multiple sources.
The team developed fusion proteins and introduced them to HSPCs ex vivo.
This approach expanded cell populations whether HSPCs were derived from cord blood, bone marrow, or peripheral blood.
The potential clinical applications for this work range from immunodeficiency disorders to hematologic and other malignancies, according to the researchers.
Yosef Refaeli, PhD, of Taiga Biotechnologies, Inc. in Aurora, Colorado, and his colleagues described this work in PLOS ONE.
The team first cultured human or murine HSPCs with a pair of fusion proteins—the protein transduction domain of the HIV-1 transactivation protein (Tat) and either the Open Reading Frame for human MYC or a truncated form of human Bcl-2 that was deleted for the unstructured loop domain.
With this technique, the researchers were able to elicit an 87-fold expansion of HSPCs from mouse bone marrow, a 16.6-fold expansion of HSPCs from human cord blood, a 13.6-fold expansion of HSPCs from human peripheral blood cells mobilized by G-CSF, and a 10-fold expansion of HSPCs from human bone marrow.
The team then tested the biological function of the expanded cells, and they found the cells gave rise to BFU-E, CFU-M, CFU-G, and CFU-GM colonies in vitro.
When transplanted into irradiated mice, the expanded cells gave rise to mature hematopoietic populations and a self-renewing cell population that was able to support hematopoiesis upon serial transplantation.
The researchers said these results suggest their technique may be an attractive approach to expand human HSPCs ex vivo for clinical use.
The team’s goal now is to move the technology from the lab into clinical trials. Taiga Biotechnologies is in the process of setting up clinical trials testing this approach. ![]()
RIKEN’s initial STAP cell experiments failed

Investigators at the Japanese research institute RIKEN have failed to create STAP (stimulus-triggered acquisition of pluripotency) cells in the experiments they’ve conducted thus far.
However, the group plans to continue its attempts to replicate the STAP cell phenomenon—inducing pluripotency in somatic cells by exposing them to stress—until next March.
So far, the group has failed to create STAP cells by exposing cells from newborn C57BL/6 mice to a low-pH environment.
Going forward, the researchers plan to conduct their experiments in another mouse strain. They also intend to alter the methods of stressing the cells.
RIKEN investigator Haruko Obokata, PhD, and her colleagues initially reported the STAP cell phenomenon in an article and a letter published in Nature last January.
Not long after the papers were published, members of the scientific community began to question the validity of the research. They voiced concerns about published images, possible plagiarism, and an inability to replicate the experiments described.
So RIKEN launched an investigation, ultimately concluding that Dr Obokata was guilty of misconduct, and some of her colleagues—including the recently deceased Yoshiki Sasai, MD, PhD—were guilty of negligence.
RIKEN also called for the papers to be retracted, and, in July, they were.
Throughout these proceedings, Dr Obokata insisted the STAP cell phenomenon is real. To investigate this claim, RIKEN organized a group of researchers to recreate Dr Obokata’s experiments.
The group has performed 22 experiments using different types of stress and cells from different tissues in C57BL/6 mice, but they have not reproduced the STAP cell phenomenon described in the Nature papers. (A report on these attempts is available in Japanese.)
Still, the investigators are continuing with their experiments and hope to have definitive results by March. ![]()

Investigators at the Japanese research institute RIKEN have failed to create STAP (stimulus-triggered acquisition of pluripotency) cells in the experiments they’ve conducted thus far.
However, the group plans to continue its attempts to replicate the STAP cell phenomenon—inducing pluripotency in somatic cells by exposing them to stress—until next March.
So far, the group has failed to create STAP cells by exposing cells from newborn C57BL/6 mice to a low-pH environment.
Going forward, the researchers plan to conduct their experiments in another mouse strain. They also intend to alter the methods of stressing the cells.
RIKEN investigator Haruko Obokata, PhD, and her colleagues initially reported the STAP cell phenomenon in an article and a letter published in Nature last January.
Not long after the papers were published, members of the scientific community began to question the validity of the research. They voiced concerns about published images, possible plagiarism, and an inability to replicate the experiments described.
So RIKEN launched an investigation, ultimately concluding that Dr Obokata was guilty of misconduct, and some of her colleagues—including the recently deceased Yoshiki Sasai, MD, PhD—were guilty of negligence.
RIKEN also called for the papers to be retracted, and, in July, they were.
Throughout these proceedings, Dr Obokata insisted the STAP cell phenomenon is real. To investigate this claim, RIKEN organized a group of researchers to recreate Dr Obokata’s experiments.
The group has performed 22 experiments using different types of stress and cells from different tissues in C57BL/6 mice, but they have not reproduced the STAP cell phenomenon described in the Nature papers. (A report on these attempts is available in Japanese.)
Still, the investigators are continuing with their experiments and hope to have definitive results by March. ![]()

Investigators at the Japanese research institute RIKEN have failed to create STAP (stimulus-triggered acquisition of pluripotency) cells in the experiments they’ve conducted thus far.
However, the group plans to continue its attempts to replicate the STAP cell phenomenon—inducing pluripotency in somatic cells by exposing them to stress—until next March.
So far, the group has failed to create STAP cells by exposing cells from newborn C57BL/6 mice to a low-pH environment.
Going forward, the researchers plan to conduct their experiments in another mouse strain. They also intend to alter the methods of stressing the cells.
RIKEN investigator Haruko Obokata, PhD, and her colleagues initially reported the STAP cell phenomenon in an article and a letter published in Nature last January.
Not long after the papers were published, members of the scientific community began to question the validity of the research. They voiced concerns about published images, possible plagiarism, and an inability to replicate the experiments described.
So RIKEN launched an investigation, ultimately concluding that Dr Obokata was guilty of misconduct, and some of her colleagues—including the recently deceased Yoshiki Sasai, MD, PhD—were guilty of negligence.
RIKEN also called for the papers to be retracted, and, in July, they were.
Throughout these proceedings, Dr Obokata insisted the STAP cell phenomenon is real. To investigate this claim, RIKEN organized a group of researchers to recreate Dr Obokata’s experiments.
The group has performed 22 experiments using different types of stress and cells from different tissues in C57BL/6 mice, but they have not reproduced the STAP cell phenomenon described in the Nature papers. (A report on these attempts is available in Japanese.)
Still, the investigators are continuing with their experiments and hope to have definitive results by March. ![]()
Combo offers better detection of invasive aspergillosis

Results of a retrospective study may have revealed the most accurate way to diagnose invasive aspergillosis (IA).
The fungal infection can be life-threatening, particularly for immunosuppressed patients, but it remains difficult to diagnose.
So researchers compared 3 tests used to diagnose IA and found the combination of nucleic acid sequence-based amplification (NASBA) and real-time quantitative PCR (qPCR) had a 100% positive predictive value.
The team reported this discovery in The Journal of Molecular Diagnostics.
IA is caused by the fungus Aspergillus fumigatus, which is considered by many pathologists to be the world’s most harmful mold.
“Traditional diagnostic methods, such as culture and histopathology of infected tissues, often fail to detect Aspergillus,” said study investigator Yun Xia, PhD, of the First Affiliated Hospital of Chongqing Medical University in China.
With this in mind, he and his colleagues evaluated the diagnostic performance of 2 nucleic acid amplification assays—qPCR and NASBA—and 1 antigen-detection method—galactomannan enzyme-linked immunosorbent assay (GM-ELISA)—using blood samples from 80 patients at high risk of IA.
The researchers evaluated the tests alone and in combination. Of the 80 patients, 42.5% had proven or probable IA.
Tests showed that NASBA predicted IA with the highest sensitivity—76.47%, compared to 67.65% for qPCR and 52.94% for GM-ELISA. But qPCR offered the highest specificity—89.13%, compared to 80.43% for both NASBA and GM-ELISA.
NASBA had the highest negative predictive value—82.22%, compared to 78.85% for qPCR and 69.81% for GM-ELISA. And qPCR had the highest positive predictive value—82.14%, compared to 74.29% for NASBA and 66.67% for GM-ELISA.
NASBA and qPCR each had a high Youden index as well—0.5690 and 0.5678, respectively—compared to GM-ELISA—0.3337.
And combining the tests improved their accuracy. The combination of NASBA and qPCR led to 100% specificity and a 100% positive predictive value.
Dr Xia and his colleagues also noted that NASBA offers the advantages of rapid amplification (90 minutes) and simple operation with low instrument cost, compared with qPCR and GM-ELISA.
Finally, the team stressed that although GM-ELISA is widely and routinely used for aspergillosis diagnosis, this study indicates that it is inferior to both NASBA and qPCR. ![]()

Results of a retrospective study may have revealed the most accurate way to diagnose invasive aspergillosis (IA).
The fungal infection can be life-threatening, particularly for immunosuppressed patients, but it remains difficult to diagnose.
So researchers compared 3 tests used to diagnose IA and found the combination of nucleic acid sequence-based amplification (NASBA) and real-time quantitative PCR (qPCR) had a 100% positive predictive value.
The team reported this discovery in The Journal of Molecular Diagnostics.
IA is caused by the fungus Aspergillus fumigatus, which is considered by many pathologists to be the world’s most harmful mold.
“Traditional diagnostic methods, such as culture and histopathology of infected tissues, often fail to detect Aspergillus,” said study investigator Yun Xia, PhD, of the First Affiliated Hospital of Chongqing Medical University in China.
With this in mind, he and his colleagues evaluated the diagnostic performance of 2 nucleic acid amplification assays—qPCR and NASBA—and 1 antigen-detection method—galactomannan enzyme-linked immunosorbent assay (GM-ELISA)—using blood samples from 80 patients at high risk of IA.
The researchers evaluated the tests alone and in combination. Of the 80 patients, 42.5% had proven or probable IA.
Tests showed that NASBA predicted IA with the highest sensitivity—76.47%, compared to 67.65% for qPCR and 52.94% for GM-ELISA. But qPCR offered the highest specificity—89.13%, compared to 80.43% for both NASBA and GM-ELISA.
NASBA had the highest negative predictive value—82.22%, compared to 78.85% for qPCR and 69.81% for GM-ELISA. And qPCR had the highest positive predictive value—82.14%, compared to 74.29% for NASBA and 66.67% for GM-ELISA.
NASBA and qPCR each had a high Youden index as well—0.5690 and 0.5678, respectively—compared to GM-ELISA—0.3337.
And combining the tests improved their accuracy. The combination of NASBA and qPCR led to 100% specificity and a 100% positive predictive value.
Dr Xia and his colleagues also noted that NASBA offers the advantages of rapid amplification (90 minutes) and simple operation with low instrument cost, compared with qPCR and GM-ELISA.
Finally, the team stressed that although GM-ELISA is widely and routinely used for aspergillosis diagnosis, this study indicates that it is inferior to both NASBA and qPCR. ![]()

Results of a retrospective study may have revealed the most accurate way to diagnose invasive aspergillosis (IA).
The fungal infection can be life-threatening, particularly for immunosuppressed patients, but it remains difficult to diagnose.
So researchers compared 3 tests used to diagnose IA and found the combination of nucleic acid sequence-based amplification (NASBA) and real-time quantitative PCR (qPCR) had a 100% positive predictive value.
The team reported this discovery in The Journal of Molecular Diagnostics.
IA is caused by the fungus Aspergillus fumigatus, which is considered by many pathologists to be the world’s most harmful mold.
“Traditional diagnostic methods, such as culture and histopathology of infected tissues, often fail to detect Aspergillus,” said study investigator Yun Xia, PhD, of the First Affiliated Hospital of Chongqing Medical University in China.
With this in mind, he and his colleagues evaluated the diagnostic performance of 2 nucleic acid amplification assays—qPCR and NASBA—and 1 antigen-detection method—galactomannan enzyme-linked immunosorbent assay (GM-ELISA)—using blood samples from 80 patients at high risk of IA.
The researchers evaluated the tests alone and in combination. Of the 80 patients, 42.5% had proven or probable IA.
Tests showed that NASBA predicted IA with the highest sensitivity—76.47%, compared to 67.65% for qPCR and 52.94% for GM-ELISA. But qPCR offered the highest specificity—89.13%, compared to 80.43% for both NASBA and GM-ELISA.
NASBA had the highest negative predictive value—82.22%, compared to 78.85% for qPCR and 69.81% for GM-ELISA. And qPCR had the highest positive predictive value—82.14%, compared to 74.29% for NASBA and 66.67% for GM-ELISA.
NASBA and qPCR each had a high Youden index as well—0.5690 and 0.5678, respectively—compared to GM-ELISA—0.3337.
And combining the tests improved their accuracy. The combination of NASBA and qPCR led to 100% specificity and a 100% positive predictive value.
Dr Xia and his colleagues also noted that NASBA offers the advantages of rapid amplification (90 minutes) and simple operation with low instrument cost, compared with qPCR and GM-ELISA.
Finally, the team stressed that although GM-ELISA is widely and routinely used for aspergillosis diagnosis, this study indicates that it is inferior to both NASBA and qPCR. ![]()
Protein appears essential for NK cell survival

Credit: Walter and Eliza Hall
Institute of Medical Research
New research suggests the Mcl-1 protein is crucial for the survival of natural killer (NK) cells and, therefore, innate immune responses.
Researchers deleted Mcl-1 from NK cells in mice and observed a loss of the cells from all tissues.
This made the mice more receptive to allogeneic hematopoietic stem cell transplants and resistant to toxic shock following a sepsis challenge, but it also made the mice susceptible to melanoma metastases.
The researchers believe their findings, published in Nature Communications, will help to determine how NK cells can be manipulated to treat a range of disorders.
They said Mcl-1 could be a target for boosting or depleting NK cell populations when necessary.
The researchers first discovered that Mcl-1 is highly expressed in NK cells. And Mcl-1 is regulated by IL-15 in a dose-dependent manner via STAT5 phosphorylation and subsequent binding to the 3′-UTR of Mcl-1.
“We showed Mcl-1 levels inside the cell increase in response to [IL-15],” said study author Nick Huntington, PhD, of the Walter and Eliza Hall Institute of Medical Research in Victoria, Australia.
“We previously knew IL-15 boosted production and survival of natural killer cells, and we have shown that IL-15 does this by initiating a cascade of signals that tell the natural killer cell to produce Mcl-1 to keep it alive.”
To further explore this phenomenon, the researchers deleted Mcl-1 from NK cells in mice and observed depletion of the cells in all tissues. The team said this was the result of a failure to antagonize pro-apoptotic proteins in the outer mitochondrial membrane.
Additional experiments showed that the mice needed the NK cells to fight off invading melanoma cells that had spread past the original cancer site.
“Without natural killer cells, the body was unable to destroy melanoma metastases that had spread throughout the body, and the cancers overwhelmed the lungs,” Dr Huntington said.
However, the loss of NK cells also made mice more receptive to allogeneic stem cell transplants and resistant to toxic shock after polymicrobial sepsis challenge.
“Natural killer cells led the response that caused rejection of donor stem cells in bone marrow transplantations,” Dr Huntington said. “They also produced inflammatory signals that can result in toxic shock syndrome, a potentially fatal illness caused by bacterial toxins that causes a whole-body inflammatory reaction.”
The researchers said these results clearly show a non-redundant pathway linking IL-15 to Mcl-1 in the maintenance of NK cells and innate immune responses.
Dr Huntington said the discovery provides a solid lead to look for ways of boosting or depleting NK cells when necessary.
“Now that we know the critical importance of Mcl-1 in the survival of natural killer cells,” he said, “we are investigating how we might manipulate this protein, or other proteins in the pathway, to treat disease.” ![]()

Credit: Walter and Eliza Hall
Institute of Medical Research
New research suggests the Mcl-1 protein is crucial for the survival of natural killer (NK) cells and, therefore, innate immune responses.
Researchers deleted Mcl-1 from NK cells in mice and observed a loss of the cells from all tissues.
This made the mice more receptive to allogeneic hematopoietic stem cell transplants and resistant to toxic shock following a sepsis challenge, but it also made the mice susceptible to melanoma metastases.
The researchers believe their findings, published in Nature Communications, will help to determine how NK cells can be manipulated to treat a range of disorders.
They said Mcl-1 could be a target for boosting or depleting NK cell populations when necessary.
The researchers first discovered that Mcl-1 is highly expressed in NK cells. And Mcl-1 is regulated by IL-15 in a dose-dependent manner via STAT5 phosphorylation and subsequent binding to the 3′-UTR of Mcl-1.
“We showed Mcl-1 levels inside the cell increase in response to [IL-15],” said study author Nick Huntington, PhD, of the Walter and Eliza Hall Institute of Medical Research in Victoria, Australia.
“We previously knew IL-15 boosted production and survival of natural killer cells, and we have shown that IL-15 does this by initiating a cascade of signals that tell the natural killer cell to produce Mcl-1 to keep it alive.”
To further explore this phenomenon, the researchers deleted Mcl-1 from NK cells in mice and observed depletion of the cells in all tissues. The team said this was the result of a failure to antagonize pro-apoptotic proteins in the outer mitochondrial membrane.
Additional experiments showed that the mice needed the NK cells to fight off invading melanoma cells that had spread past the original cancer site.
“Without natural killer cells, the body was unable to destroy melanoma metastases that had spread throughout the body, and the cancers overwhelmed the lungs,” Dr Huntington said.
However, the loss of NK cells also made mice more receptive to allogeneic stem cell transplants and resistant to toxic shock after polymicrobial sepsis challenge.
“Natural killer cells led the response that caused rejection of donor stem cells in bone marrow transplantations,” Dr Huntington said. “They also produced inflammatory signals that can result in toxic shock syndrome, a potentially fatal illness caused by bacterial toxins that causes a whole-body inflammatory reaction.”
The researchers said these results clearly show a non-redundant pathway linking IL-15 to Mcl-1 in the maintenance of NK cells and innate immune responses.
Dr Huntington said the discovery provides a solid lead to look for ways of boosting or depleting NK cells when necessary.
“Now that we know the critical importance of Mcl-1 in the survival of natural killer cells,” he said, “we are investigating how we might manipulate this protein, or other proteins in the pathway, to treat disease.” ![]()

Credit: Walter and Eliza Hall
Institute of Medical Research
New research suggests the Mcl-1 protein is crucial for the survival of natural killer (NK) cells and, therefore, innate immune responses.
Researchers deleted Mcl-1 from NK cells in mice and observed a loss of the cells from all tissues.
This made the mice more receptive to allogeneic hematopoietic stem cell transplants and resistant to toxic shock following a sepsis challenge, but it also made the mice susceptible to melanoma metastases.
The researchers believe their findings, published in Nature Communications, will help to determine how NK cells can be manipulated to treat a range of disorders.
They said Mcl-1 could be a target for boosting or depleting NK cell populations when necessary.
The researchers first discovered that Mcl-1 is highly expressed in NK cells. And Mcl-1 is regulated by IL-15 in a dose-dependent manner via STAT5 phosphorylation and subsequent binding to the 3′-UTR of Mcl-1.
“We showed Mcl-1 levels inside the cell increase in response to [IL-15],” said study author Nick Huntington, PhD, of the Walter and Eliza Hall Institute of Medical Research in Victoria, Australia.
“We previously knew IL-15 boosted production and survival of natural killer cells, and we have shown that IL-15 does this by initiating a cascade of signals that tell the natural killer cell to produce Mcl-1 to keep it alive.”
To further explore this phenomenon, the researchers deleted Mcl-1 from NK cells in mice and observed depletion of the cells in all tissues. The team said this was the result of a failure to antagonize pro-apoptotic proteins in the outer mitochondrial membrane.
Additional experiments showed that the mice needed the NK cells to fight off invading melanoma cells that had spread past the original cancer site.
“Without natural killer cells, the body was unable to destroy melanoma metastases that had spread throughout the body, and the cancers overwhelmed the lungs,” Dr Huntington said.
However, the loss of NK cells also made mice more receptive to allogeneic stem cell transplants and resistant to toxic shock after polymicrobial sepsis challenge.
“Natural killer cells led the response that caused rejection of donor stem cells in bone marrow transplantations,” Dr Huntington said. “They also produced inflammatory signals that can result in toxic shock syndrome, a potentially fatal illness caused by bacterial toxins that causes a whole-body inflammatory reaction.”
The researchers said these results clearly show a non-redundant pathway linking IL-15 to Mcl-1 in the maintenance of NK cells and innate immune responses.
Dr Huntington said the discovery provides a solid lead to look for ways of boosting or depleting NK cells when necessary.
“Now that we know the critical importance of Mcl-1 in the survival of natural killer cells,” he said, “we are investigating how we might manipulate this protein, or other proteins in the pathway, to treat disease.”
More new insight into HSC generation

Credit: John Perry
Researchers say they have uncovered early clues that better explain how hematopoietic stem cells (HSCs) are generated.
Their research, conducted in zebrafish, provides new insight regarding the role of JAM proteins and the Notch signaling pathway, which was already known to be critical for HSC generation.
The new findings may help clear the way to producing HSCs from human pluripotent precursors, according to the researchers.
David Traver, PhD, of the University of California, San Diego School of Medicine, and his colleagues recounted these findings in a letter to Nature. A similar study, which revealed the role of endotome cells in HSC generation, was also recently published as a letter to Nature.
“Notch signaling between emitting and receiving cells is key to establishing HSC fate during development,” Dr Traver said. “What has not been known is where, when, and how Notch signal transduction is mediated.”
Through experiments in zebrafish models, Dr Traver and his colleagues found the Notch signal is transduced into HSC precursor cells from signal-emitting cells in the somite much earlier in the process than previously anticipated.
Specifically, the team found that JAM proteins, best known for helping maintain tight junctions between endothelial cells to prevent vascular leakage, were key mediators of Notch signaling.
When the researchers caused JAM proteins to lose function, Notch signaling and HSCs were also lost. When they enforced Notch signaling, the team rescued HSC development.
“To date, it has not been possible to generate HSCs de novo from human pluripotent precursors, like induced pluripotent stem cells,” Dr Traver said. “This has been due, in part, to a lack of understanding of the complete set of factors that the embryo uses to make HSCs in vivo. It has also likely been due to not knowing in what order each required factor is needed.”
“Our studies demonstrate that Notch signaling is required much earlier than previously thought. In fact, it may be one of the earliest determinants of HSC fate. This finding strongly suggests that in vitro approaches to instruct HSC fate from induced pluripotent stem cells must focus on the Notch pathway at early time-points in the process.”
“Our findings have also shown that JAM proteins serve as a sort of co-receptor for Notch signaling, in that they are required to maintain close contact between signal-emitting and signal-receiving cells to permit strong activation of Notch in the precursors of HSCs.”
Dr Traver and his colleagues believe the findings may have far-reaching implications for the eventual development of HSC-based therapies for diseases such as leukemia and congenital blood disorders.

Credit: John Perry
Researchers say they have uncovered early clues that better explain how hematopoietic stem cells (HSCs) are generated.
Their research, conducted in zebrafish, provides new insight regarding the role of JAM proteins and the Notch signaling pathway, which was already known to be critical for HSC generation.
The new findings may help clear the way to producing HSCs from human pluripotent precursors, according to the researchers.
David Traver, PhD, of the University of California, San Diego School of Medicine, and his colleagues recounted these findings in a letter to Nature. A similar study, which revealed the role of endotome cells in HSC generation, was also recently published as a letter to Nature.
“Notch signaling between emitting and receiving cells is key to establishing HSC fate during development,” Dr Traver said. “What has not been known is where, when, and how Notch signal transduction is mediated.”
Through experiments in zebrafish models, Dr Traver and his colleagues found the Notch signal is transduced into HSC precursor cells from signal-emitting cells in the somite much earlier in the process than previously anticipated.
Specifically, the team found that JAM proteins, best known for helping maintain tight junctions between endothelial cells to prevent vascular leakage, were key mediators of Notch signaling.
When the researchers caused JAM proteins to lose function, Notch signaling and HSCs were also lost. When they enforced Notch signaling, the team rescued HSC development.
“To date, it has not been possible to generate HSCs de novo from human pluripotent precursors, like induced pluripotent stem cells,” Dr Traver said. “This has been due, in part, to a lack of understanding of the complete set of factors that the embryo uses to make HSCs in vivo. It has also likely been due to not knowing in what order each required factor is needed.”
“Our studies demonstrate that Notch signaling is required much earlier than previously thought. In fact, it may be one of the earliest determinants of HSC fate. This finding strongly suggests that in vitro approaches to instruct HSC fate from induced pluripotent stem cells must focus on the Notch pathway at early time-points in the process.”
“Our findings have also shown that JAM proteins serve as a sort of co-receptor for Notch signaling, in that they are required to maintain close contact between signal-emitting and signal-receiving cells to permit strong activation of Notch in the precursors of HSCs.”
Dr Traver and his colleagues believe the findings may have far-reaching implications for the eventual development of HSC-based therapies for diseases such as leukemia and congenital blood disorders.

Credit: John Perry
Researchers say they have uncovered early clues that better explain how hematopoietic stem cells (HSCs) are generated.
Their research, conducted in zebrafish, provides new insight regarding the role of JAM proteins and the Notch signaling pathway, which was already known to be critical for HSC generation.
The new findings may help clear the way to producing HSCs from human pluripotent precursors, according to the researchers.
David Traver, PhD, of the University of California, San Diego School of Medicine, and his colleagues recounted these findings in a letter to Nature. A similar study, which revealed the role of endotome cells in HSC generation, was also recently published as a letter to Nature.
“Notch signaling between emitting and receiving cells is key to establishing HSC fate during development,” Dr Traver said. “What has not been known is where, when, and how Notch signal transduction is mediated.”
Through experiments in zebrafish models, Dr Traver and his colleagues found the Notch signal is transduced into HSC precursor cells from signal-emitting cells in the somite much earlier in the process than previously anticipated.
Specifically, the team found that JAM proteins, best known for helping maintain tight junctions between endothelial cells to prevent vascular leakage, were key mediators of Notch signaling.
When the researchers caused JAM proteins to lose function, Notch signaling and HSCs were also lost. When they enforced Notch signaling, the team rescued HSC development.
“To date, it has not been possible to generate HSCs de novo from human pluripotent precursors, like induced pluripotent stem cells,” Dr Traver said. “This has been due, in part, to a lack of understanding of the complete set of factors that the embryo uses to make HSCs in vivo. It has also likely been due to not knowing in what order each required factor is needed.”
“Our studies demonstrate that Notch signaling is required much earlier than previously thought. In fact, it may be one of the earliest determinants of HSC fate. This finding strongly suggests that in vitro approaches to instruct HSC fate from induced pluripotent stem cells must focus on the Notch pathway at early time-points in the process.”
“Our findings have also shown that JAM proteins serve as a sort of co-receptor for Notch signaling, in that they are required to maintain close contact between signal-emitting and signal-receiving cells to permit strong activation of Notch in the precursors of HSCs.”
Dr Traver and his colleagues believe the findings may have far-reaching implications for the eventual development of HSC-based therapies for diseases such as leukemia and congenital blood disorders.
Zebrafish research solves mystery of HSC generation

A cure for a range of blood and immune disorders is in sight, according to researchers who say they’ve solved a mystery of hematopoietic stem cell (HSC) generation.
By studying zebrafish embryos, the investigators found that migratory cells from a region known as the endotome are essential for HSC formation.
The team also discovered some of the signals required for HSC generation and identified genes necessary for endotome formation.
The researchers believe these findings, published in Nature, bring us one step closer to creating viable HSCs in the lab.
“HSCs are one of the best therapeutic tools at our disposal because they can make any blood cell in the body,” said study author Peter Currie, PhD, of the Australian Regenerative Medicine Institute at Monash University in Victoria, Australia.
“Potentially, we could use these cells in many more ways than current transplantation strategies to treat serious blood disorders and diseases, but only if we can figure out how they are generated in the first place.”
In an attempt to do just that, Dr Currie and his colleagues studied developing zebrafish. They used high-resolution microscopy to film how HSCs form inside the embryo.
The investigators noted that, in vertebrate embryos, HSCs are initially generated within the dorsal aorta. And previous research showed that signaling relayed from adjacent somites coordinates HSC induction.
Dr Currie and his colleagues found that somite specification of HSCs occurs thanks to an endothelial precursor cell population. These cells arise in a sub-compartment of the zebrafish somite the researchers dubbed “the endotome.”
Endothelial cells from the endotome are specified thanks to activity of the homeobox gene meox1. Specified endotome cells then migrate to and colonize the dorsal aorta, where they induce HSC formation via chemokine signaling that’s activated during endotome formation.
“Endotome cells act like a comfy sofa for pre-HSCs to snuggle into, helping them progress to become fully fledged stem cells,” Dr Currie said. “Not only did we identify some of the cells and signals required for HSC formation, we also pinpointed the genes required for endotome formation in the first place.”
“The really exciting thing about these results is that if we can find the signals present in the endotome cells responsible for embryonic HSC formation, then we can use them in vitro to make different blood cells on demand for all sorts of blood-related disorders.”
For the next phase of this research, Dr Currie and his colleagues are attempting to identify more of the molecular cues that trigger HSC production.

A cure for a range of blood and immune disorders is in sight, according to researchers who say they’ve solved a mystery of hematopoietic stem cell (HSC) generation.
By studying zebrafish embryos, the investigators found that migratory cells from a region known as the endotome are essential for HSC formation.
The team also discovered some of the signals required for HSC generation and identified genes necessary for endotome formation.
The researchers believe these findings, published in Nature, bring us one step closer to creating viable HSCs in the lab.
“HSCs are one of the best therapeutic tools at our disposal because they can make any blood cell in the body,” said study author Peter Currie, PhD, of the Australian Regenerative Medicine Institute at Monash University in Victoria, Australia.
“Potentially, we could use these cells in many more ways than current transplantation strategies to treat serious blood disorders and diseases, but only if we can figure out how they are generated in the first place.”
In an attempt to do just that, Dr Currie and his colleagues studied developing zebrafish. They used high-resolution microscopy to film how HSCs form inside the embryo.
The investigators noted that, in vertebrate embryos, HSCs are initially generated within the dorsal aorta. And previous research showed that signaling relayed from adjacent somites coordinates HSC induction.
Dr Currie and his colleagues found that somite specification of HSCs occurs thanks to an endothelial precursor cell population. These cells arise in a sub-compartment of the zebrafish somite the researchers dubbed “the endotome.”
Endothelial cells from the endotome are specified thanks to activity of the homeobox gene meox1. Specified endotome cells then migrate to and colonize the dorsal aorta, where they induce HSC formation via chemokine signaling that’s activated during endotome formation.
“Endotome cells act like a comfy sofa for pre-HSCs to snuggle into, helping them progress to become fully fledged stem cells,” Dr Currie said. “Not only did we identify some of the cells and signals required for HSC formation, we also pinpointed the genes required for endotome formation in the first place.”
“The really exciting thing about these results is that if we can find the signals present in the endotome cells responsible for embryonic HSC formation, then we can use them in vitro to make different blood cells on demand for all sorts of blood-related disorders.”
For the next phase of this research, Dr Currie and his colleagues are attempting to identify more of the molecular cues that trigger HSC production.

A cure for a range of blood and immune disorders is in sight, according to researchers who say they’ve solved a mystery of hematopoietic stem cell (HSC) generation.
By studying zebrafish embryos, the investigators found that migratory cells from a region known as the endotome are essential for HSC formation.
The team also discovered some of the signals required for HSC generation and identified genes necessary for endotome formation.
The researchers believe these findings, published in Nature, bring us one step closer to creating viable HSCs in the lab.
“HSCs are one of the best therapeutic tools at our disposal because they can make any blood cell in the body,” said study author Peter Currie, PhD, of the Australian Regenerative Medicine Institute at Monash University in Victoria, Australia.
“Potentially, we could use these cells in many more ways than current transplantation strategies to treat serious blood disorders and diseases, but only if we can figure out how they are generated in the first place.”
In an attempt to do just that, Dr Currie and his colleagues studied developing zebrafish. They used high-resolution microscopy to film how HSCs form inside the embryo.
The investigators noted that, in vertebrate embryos, HSCs are initially generated within the dorsal aorta. And previous research showed that signaling relayed from adjacent somites coordinates HSC induction.
Dr Currie and his colleagues found that somite specification of HSCs occurs thanks to an endothelial precursor cell population. These cells arise in a sub-compartment of the zebrafish somite the researchers dubbed “the endotome.”
Endothelial cells from the endotome are specified thanks to activity of the homeobox gene meox1. Specified endotome cells then migrate to and colonize the dorsal aorta, where they induce HSC formation via chemokine signaling that’s activated during endotome formation.
“Endotome cells act like a comfy sofa for pre-HSCs to snuggle into, helping them progress to become fully fledged stem cells,” Dr Currie said. “Not only did we identify some of the cells and signals required for HSC formation, we also pinpointed the genes required for endotome formation in the first place.”
“The really exciting thing about these results is that if we can find the signals present in the endotome cells responsible for embryonic HSC formation, then we can use them in vitro to make different blood cells on demand for all sorts of blood-related disorders.”
For the next phase of this research, Dr Currie and his colleagues are attempting to identify more of the molecular cues that trigger HSC production.
New insight into stem cell differentiation
Adam Engler, UC San Diego
Jacobs School of Engineering
The stiffness of the extracellular matrix may play a larger role in stem cell differentiation than we thought, according to a new study.
Scientists have recently suggested that protein tethering and matrix porosity, as well as matrix stiffness and ligand type, regulate stem cell differentiation.
However, new research published in Nature Materials indicates that matrix stiffness regulates stem cell differentiation independently of tethering and porosity.
Adam Engler, PhD, of the University of California, San Diego, and his colleagues discovered that human adipose stromal cells and mesenchymal stromal cells underwent osteogenic differentiation if placed in a stiff hydrogel. But the cells underwent adipogenesis if placed in a soft hydrogel.
The protein binding the stem cell to the hydrogel was not a factor in the differentiation process. Results suggested the protein layer was merely an adhesive.
The researchers found that stem cell differentiation is a response to the mechanical deformation of the hydrogel from the force exerted by the cell. With a series of experiments, the team showed that this happens whether the protein tethering the cell to the matrix is tight, loose, or nonexistent.
Across multiple samples using a stiff matrix, varying the degree of tethering made no significant difference in the rate of osteogenic or adipogenic differentiation.
Likewise, the size of the pores in the matrix had no effect on stem cell differentiation, as long as the stiffness of the hydrogel remained the same.
However, Dr Engler pointed out that matrix stiffness is only “one cue out of dozens that are important in stem cell differentiation.”
“That doesn’t mean the other cues are irrelevant,” he noted. “They may still push the cells into a specific cell type. We have just ruled out porosity and tethering, and further emphasized stiffness in this process.”
Adam Engler, UC San Diego
Jacobs School of Engineering
The stiffness of the extracellular matrix may play a larger role in stem cell differentiation than we thought, according to a new study.
Scientists have recently suggested that protein tethering and matrix porosity, as well as matrix stiffness and ligand type, regulate stem cell differentiation.
However, new research published in Nature Materials indicates that matrix stiffness regulates stem cell differentiation independently of tethering and porosity.
Adam Engler, PhD, of the University of California, San Diego, and his colleagues discovered that human adipose stromal cells and mesenchymal stromal cells underwent osteogenic differentiation if placed in a stiff hydrogel. But the cells underwent adipogenesis if placed in a soft hydrogel.
The protein binding the stem cell to the hydrogel was not a factor in the differentiation process. Results suggested the protein layer was merely an adhesive.
The researchers found that stem cell differentiation is a response to the mechanical deformation of the hydrogel from the force exerted by the cell. With a series of experiments, the team showed that this happens whether the protein tethering the cell to the matrix is tight, loose, or nonexistent.
Across multiple samples using a stiff matrix, varying the degree of tethering made no significant difference in the rate of osteogenic or adipogenic differentiation.
Likewise, the size of the pores in the matrix had no effect on stem cell differentiation, as long as the stiffness of the hydrogel remained the same.
However, Dr Engler pointed out that matrix stiffness is only “one cue out of dozens that are important in stem cell differentiation.”
“That doesn’t mean the other cues are irrelevant,” he noted. “They may still push the cells into a specific cell type. We have just ruled out porosity and tethering, and further emphasized stiffness in this process.”
Adam Engler, UC San Diego
Jacobs School of Engineering
The stiffness of the extracellular matrix may play a larger role in stem cell differentiation than we thought, according to a new study.
Scientists have recently suggested that protein tethering and matrix porosity, as well as matrix stiffness and ligand type, regulate stem cell differentiation.
However, new research published in Nature Materials indicates that matrix stiffness regulates stem cell differentiation independently of tethering and porosity.
Adam Engler, PhD, of the University of California, San Diego, and his colleagues discovered that human adipose stromal cells and mesenchymal stromal cells underwent osteogenic differentiation if placed in a stiff hydrogel. But the cells underwent adipogenesis if placed in a soft hydrogel.
The protein binding the stem cell to the hydrogel was not a factor in the differentiation process. Results suggested the protein layer was merely an adhesive.
The researchers found that stem cell differentiation is a response to the mechanical deformation of the hydrogel from the force exerted by the cell. With a series of experiments, the team showed that this happens whether the protein tethering the cell to the matrix is tight, loose, or nonexistent.
Across multiple samples using a stiff matrix, varying the degree of tethering made no significant difference in the rate of osteogenic or adipogenic differentiation.
Likewise, the size of the pores in the matrix had no effect on stem cell differentiation, as long as the stiffness of the hydrogel remained the same.
However, Dr Engler pointed out that matrix stiffness is only “one cue out of dozens that are important in stem cell differentiation.”
“That doesn’t mean the other cues are irrelevant,” he noted. “They may still push the cells into a specific cell type. We have just ruled out porosity and tethering, and further emphasized stiffness in this process.”