User login
Adolescent Obesity and Its Risks: How to Screen and When to Refer
From the Department of Pediatrics, University of Wisconsin, Madison, WI.
Abstract
- Objective: To provide information that will assist clinicians in assessing and addressing risk for obesity-related comorbidities in adolescents.
- Methods: Review of the literature.
- Results: Childhood obesity is a major public health concern. Prevention of obesity or early detection of its health consequences are important responsibilities or opportunities for primary care clinicians. While body mass index (BMI) screening is valuable, insulin resistance and other obesity-related comorbidities can develop even when BMI falls below the 95th percentile threshold for obesity. Detailed history and physical examination can help identify comorbidities and guide diagnostic evaluation. Referral to multidisciplinary clinics specializing in childhood obesity is warranted when obesity is particularly severe, comorbidities are present at baseline, or no improvement is noted after 6 months of intense lifestyle intervention.
- Conclusion: For optimal health outcomes, management of adolescent obesity and associated comorbidities is should be adapted based on an individual’s overall risk rather than BMI alone.
Case Study
Initial Presentation
A 14-year-old Hispanic male presents for a well child check.
History and Physical Examination
The patient and his mother have no complaints or concerns. A comprehensive review of systems is positive for fatigue and snoring but is otherwise unremarkable. Past medical history is unremarkable except for mild intermittent asthma. Family history is positive for type 2 diabetes in paternal grandmother and a maternal uncle and cardiovascular disease and hypertension in multiple extended family members. Both maternal and paternal grandparents are from Mexico.
Vital signs are within normal limits. Height is 160 cm (30th percentile for age), weight is 58.4 kg (75th percentile for age), and body mass index (BMI) is 22.8 kg/m2 (85th percentile for age). Blood pressure is 127/81 mm Hg (95th percentile for age and gender). Physical exam is pertinent for acanthosis nigricans on neck and axilla and nonviolaceous striae on abdomen. Waist circumference is 88 cm (90th percentile for age and ethnicity). Otherwise, physical exam is within normal limits.
• Does this child’s physical examination findings pose a cause for concern?
Yes. A key concept is that while obesity is widespread, the adverse health complications of adiposity and overnutrition affect some children much earlier and more profoundly than others. Some children exhibit adiposity-associated comorbidities even prior to meeting obesity criteria defined by BMI. Careful history and examination can help identify those most at risk for developing adiposity-associated comorbidities, prompting earlier intervention and, when appropriate, subspecialty referral.
Obesity is caused by a complex interplay of genetic, environmental, and metabolic programming, especially early in life, and lifestyle habits [1,2]. The vast majority of obesity is due to excess nutrition leading to energy imbalance, while less than 1% is due to endocrine or syndromic causes [3]. Obesity is defined as excessive body fat and is often estimated indirectly by using a surrogate marker, BMI. Diagnostically, a BMI > 95th percentile for age on sex-specific CDC growth charts is defined as obese, while a BMI from the 85th to 94th percentile is defined as overweight [4]. Using these criteria, the prevalence of childhood obesity more than tripled in the past 3 decades [5], leading to its classification as an epidemic and public health crisis [2]. Today, an estimated 12.5 million American children are obese [5]. For adolescents specifically, the prevalence of obesity is 18.4%, with more than one-third overweight [6].
Childhood obesity is associated with both short- and long-term morbidities including insulin resistance and type 2 diabetes, hypertension, dyslipidemia, asthma, obstructive sleep apnea, psychosocial problems, and decreased quality of life [7,8]. Obese children, particularly older children and adolescents, are more likely become obese adults [2,7]. Obesity in adulthood is associated with both significant morbidity and premature death [9]. Individual characteristics such as lifestyle habits, fitness level, and genetic predisposition influence the likelihood of development of both obesity and associated comorbidities [10].
The burden of obesity and its associated comorbidities are not equally distributed among racial/ethnic and socioeconomic groups. Hispanic and non-Hispanic black children are much more likely to be obese and overweight than non-Hispanic white children [6]. Low socioeconomic status is associated with increased rates of obesity in certain subgroups, including adolescents [2]. In addition, certain ethnic/racial minorities are more likely to develop obesity-associated comorbidities, such as insulin resistance, type 2 diabetes, and non-alcoholic fatty liver disease (NAFLD). With regard to insulin resistance and development of type 2 diabetes, the risk is greatest in Native Americans, but there is also increased risk in Hispanic/Latinos, non-Hispanic blacks, and Asian Americans as compared with non-Hispanic whites [11–13]. Collectively, these findings highlight the need for individualized assessment and the importance of obesity prevention and early intervention to improve long-term health outcomes. Primary care providers play a pivotal role in this process of preventing, identifying and treating childhood obesity and associated comorbidities [14]. In the case history, the child’s ethnicity, family history, and borderline overweight BMI indicate a high risk for future obesity-related morbidity and a critical opportunity for prevention intervention.
• What are the initial steps a practitioner can take to address overweight and obesity?
To encourage the development of healthy lifestyles and prevention of obesity, dietary and exercise counseling should be routinely provided as part of anticipatory guidance to all children and families regardless of weight status. It is critical to recognize individuals at high risk for becoming obese starting early in life. Risk factors for obesity in healthy weight children include rapid crossing of BMI percentiles, obese parent(s), maternal history of gestational diabetes during pregnancy, ethnicity, sedentary lifestyle, and excessive caloric intake [2]. Identification of these high-risk individuals can prompt more intensive counseling and early intervention with the goal of preventing the development of obesity and its complications. The use of automated BMI calculation and electronic medical records can facilitate identification of overweight and obesity status when already present and improve counseling rates [15].
Obesity due to excess nutrition is typically associated with linear growth acceleration that occurs subsequent to and to a lesser degree than the percentile shift in weight gain. A declining height velocity associated with obesity, therefore, is concerning and should prompt investigation for endocrine disease such as hypothyroidism, glucocorticoid excess, and growth hormone deficiency. Additional factors that warrant further investigation and/or referral include growth trajectory significantly below genetic potential, developmental delay, and dysmorphic features. A complete physical examination should be performed to evaluate for signs consistent with these conditions (eg, violaceous striae in glucocorticoid excess, microcephaly, and small hands/feet in Prader-Willi syndrome), and signs of obesity-associated comorbidities (eg, acanthosis nigricans). Accurate height, weight, BMI calculation, and blood pressure assessment using an appropriately sized cuff are essential.
While BMI screening is valuable, as noted above it is important to appreciate that insulin resistance (and other obesity-related comorbidities) can develop even when BMI is below the 95th percentile. Detailed history and physical examination can help identify these comorbidities of excess adiposity and guide diagnostic evaluation. Independent risk factors for insulin resistance and the development of type 2 diabetes include family history of diabetes, minority race/ethnicity, elevated waist circumference, and poor fitness level [18–20].
Further History
The patient reports skipping breakfast on most days, eats lunch at school, and snacks on chips and soda after school. Dinner is variable but usually contains carbohydrates and a protein and rarely includes vegetables. Family eats “take-out” about 3 times per week. Patient reports spending 3 hours a day watching television and playing on computer. He had gym last semester but currently reports very limited to no physical activity on most days.
• What are effective ways to raise the issue of obesity during an office visit?
Despite the strong connection of obesity with adverse health outcomes, discussion of obesity in routine office settings can be difficult and is often limited by many factors such as time, training, availability of support services, perceived lack of patient motivation, and low outcome expectations [21,22]. Perhaps most challenging is tactfully handling the stigma associated with obesity, which can make discussion awkward and difficult for patients, parents, and providers. To do this, efforts to choose words that convey a nonjudgmental message while maintaining focus on obesity as a health concern are helpful. For example, terms such as “fat” and “obese” are often perceived as stigmatizing and blaming while using the term “unhealthy weight” is less pejorative and can be motivating [23]. It can also be important to acknowledge and emphasize that some individuals are more susceptible to weight gain and its consequences than others and as a result can tolerate fewer calories without unwanted weight gain and health problems. These approaches shift the focus of the discussion toward the goal of restoring and preserving health rather than changing physical appearance without placing blame on the individual and/or family. Motivational interviewing techniques which can be performed effectively even in short office visits can help to actively engage families, reveal familial perception of obesity and assess readiness to change [2]. Their use may also improve the efficacy of other interventions [24].
Case Continued
The patient and his mother were asked if they had any concerns today, including concerns about future health. Mother expressed worry about the potential for diabetes given their family history. The clinician used this as an opportunity to discuss pertinent factors associated with insulin resistance and type 2 diabetes, including modifiable factors such as diet, fitness level, and weight.
• Should this non-obese adolescent be assessed for obesity comorbidities?
Yes. While there are multiple guidelines available for pediatric screening, all highlight the importance of obtaining individualized risk assessment to guide the extent of diagnostic workup. An Expert Committee comprised of representatives from 15 professional organizations appointed 3 writing groups to review the literature and recommend approaches to prevention, assessment, and treatment. Because effective strategies remain poorly defined, the writing groups used both available evidence and expert opinion to develop the recommendations [2]. In addition to routine blood pressure monitoring and universal lipid screening, the Expert Committee recommends obtaining additional laboratory assessment for obese children (BMI ≥ 95th percentile) including a fasting glucose and ALT/AST levels every 2 years starting at age 10 years. For overweight children (BMI > 85th percentile), the Expert Committee recommends obtaining these studies if additional risk factors are present [2]. The American Diabetes Association (ADA) recommends obtaining diabetes screening in all children classified as overweight (defined as either a BMI > 85th percentile for age and sex, weight for height > 85th percentile, or weight > 120% of ideal for height) once every 3 years beginning at age 10 or at pubertal onset (whichever is earliest) when 2 additional risk factors for diabetes are also present, including: (1) history of type 2 diabetes in a first- or second-degree relative, (2) race/ethnicity with increased risk for diabetes development (eg, Native American, African American, Latino, Asian American), (3) signs of insulin resistance or conditions associated with insulin resistance (eg, small for gestational age, polycystic ovary syndrome, hypertension) and (4) maternal history of gestational diabetes during pregnancy [25]. The ADA recommendations for diabetes screening test include either fasting plasma glucose, HgA1C, or oral glucose tolerance test [25].
With a BMI at the 85th percentile, on initial assessment our patient might be perceived as being at moderate or even low risk for obesity and its associated comorbidities. However, a more careful review has elicited several additional risk factors suggesting more appropriate classification in the high-risk category. First, family history of type 2 diabetes on both sides of his family suggests a degree of genetic predisposition. Second, Hispanic ethnicity is known to be independently associated with insulin resistance, type 2 diabetes, and NAFLD [26]. Moreover, physical exam findings of an elevated waist circumference (90th percentile for age and ethnicity [27]) and acanthosis nigricans are also supportive of insulin resistance. As a result, despite having a BMI at the 85th percentile, this adolescent is at high risk and further evaluation is warranted based on both Expert Committee and ADA guidelines. Detailed discussion of certain risk factors is outlined below.
Pattern of Adipose Tissue Distribution: Utility of BMI and Waist Circumference
BMI is a clinical tool that serves as a surrogate marker of adiposity, but since it does not directly measure body fat it provides a statistical, rather than inherent, description of risk. While it is a relatively specific marker (~95%) with moderately high sensitivity and positive predictive value (~70–80%) at BMI levels > 95th percentile, sensitivity and positive predictive value decrease substantially at lower BMI percentiles (PPV 18% in a sample of overweight children) [28]. Current CDC BMI percentile charts consider age and gender differences but do not take into account sexual maturation level or race/ethnicity, both of which are independently correlated with BMI [29]. That is, children with similar BMIs of the same age and sex may exhibit varying degrees of adiposity and risk attributable to their pubertal stage and/or ethnicity [30]. For example, many studies have demonstrated that at the same BMI percentile, Asian Americans tend to have more adiposity compared with non-Hispanic whites [31], whereas African Americans tend to have more fat-free mass compared with non-Hispanic whites [32]. As a result of these differences, some advocate for adjusting cut-offs for BMI based on ethnicity and/or utilizing alternative measures of adiposity such as waist circumference or waist to hip ratio. However, in order for these latter methods to be useful, standardized methods of measurement and normative reference values must be developed. In summary, though BMI can be a useful screening tool, it is an indirect measure of adiposity and cannot discern adipose distribution. Therefore, it is important to remember that when used alone, BMI may overlook children with high inherent risk for disease.
Abdominal adiposity is associated with increased metabolic risk, including insulin resistance, type 2 diabetes, hypertension, cardiovascular disease, and mortality [33]. Waist circumference, a marker of abdominal/truncal obesity, has been considered as a potential marker in place of or in combination with BMI to identify children with increased metabolic risk. In adults, it is well established that an elevated waist circumference is associated with increased health risk, even among those within a normal-weight BMI category [34], and it is recommended that waist circumference in addition to BMI be used to assess health risk [35]. Many studies have documented similar associations between increased waist circumference and metabolic risk factors in childhood and adolescence [36–38]. Specifically, waist circumference is an independent predictor of both insulin sensitivity and increased visceral adiposity tissue (VAT) in children and adolescents [39]. Waist circumference can provide valuable information beyond BMI alone and may be beneficial in the clinical setting in identifying adolescents at risk for obesity-associated comorbidities.
The use of waist circumference in routine clinical settings is complicated and limited by many factors. First, there is no universal method for waist circumference measurement. For example, the WHO recommends measurement at the midpoint between the superior iliac crest and inferior most rib, while the NIH and NHANES recommend measurement immediately above the iliac crest [40]. Since nationally representative data published by Fernandez et al [27] uses the latter method for waist circumference measurement, we recommend this method to allow for comparison of waist circumference percentile with available data for age, sex, and ethnicity. Second, while absolute waist circumference values are used as cut-offs in adulthood, in childhood use of waist circumference percentiles would be more appropriate to account for expected increases during childhood and changes related to pubertal stage. Unfortunately, a lack of standardized waist circumference percentile charts makes meaningful interpretation of waist circumference difficult. Moreover, even if standardized waist circumference percentile charts were developed, there are currently no accepted standards defining an abnormally elevated waist circumference percentile.
Many studies have identified increased metabolic risk factors associated with a waist circumference at or above the 90th percentile for age [41–43]. Based on these studies, the International Diabetes Federation uses waist circumference > 90th percentile as part of the criteria for metabolic syndrome in adolescents. While this ensures a high degree of specificity, use of waist circumference at the 75th percentile would allow for increased sensitivity. For example, Lee et al found that for insulin resistance use of waist circumference at the 75th percentile compared with the 90th percentile increased sensitivity from 61.3% to 86.1% while decreasing specificity from 91.4% to 71.5% [44]. Thus, for individuals at low risk based on history and clinical findings, a waist circumference threshold at the 90th percentile might be reasonable, while for individuals with additional risk factors for insulin resistance use of a lower waist circumference threshold (such as the 75th percentile) may be beneficial. Finally, since risk for insulin resistance and type 2 diabetes varies by race/ethnicity, which may correspond with visceral fat deposition, utilizing various threshold cut-offs based on race/ethnicity has been proposed by some. However, current data do not support this practice [44]. In summary, though there are many challenges to using waist circumference measurements in routine settings, if performed correctly determination of elevated waist circumference measurement can provide some additional information on an individual’s overall risk for complications of obesity.
Acanthosis Nigricans as an Indicator of Insulin Resistance
Insulin resistance, independent of adiposity, is associated with increased risk for type 2 diabetes, cardiovascular disease, ovarian hyperandrogenism, and certain forms of cancer [45]. Identification of insulin resistance in the clinical setting can lead to appropriate intervention (both lifestyle and, when warranted, pharmacologic) to reduce insulin resistance and improve health outcomes. Several risk factors for insulin resistance have been discussed above. Acanthosis nigricans, which is characterized by thick, velvety hyperpigmentation of the skin in intertriginous areas such as the neck and axilla, is an additional finding that is associated with insulin resistance. Its pathogenesis is felt to be related to activation of the IGF-1 receptor by high levels of circulating insulin [46]. Acanthosis nigricans is independently associated with fasting insulin levels and impaired glucose tolerance [47,48]. In addition to increased insulin resistance, one study found that 1 in 4 youths with acanthosis nigricans demonstrated abnormalities in glucose homeostasis and identified 2 individuals with diabetes who would not have been diagnosed based on fasting glucose levels alone [48]. The presence of acanthosis nigricans should alert the clinician to the likelihood of insulin resistance and prompt further investigation. Of note, the prevalence of acanthosis nigricans is increased among African American and Hispanic patients [49,50].
• What laboratory evaluation is warranted and practical in the office setting?
Laboratory evaluation is warranted when obesity or risk factors for comorbidities of obesity are present. At minimum, this should include lipid screening, liver enzymes (ALT and AST), and fasting glucose as outlined above. This approach, however, fails to identify all individuals with obesity-associated comorbidities. ALT is only moderately sensitive in detecting NAFLD [51], and fasting glucose levels only become abnormal when compensation for the degree of insulin resistance is inadequate to maintain normal fasting glucose homeostasis. As a result, while abnormal results on screening are suggestive of disease, normal results do not necessarily confer its absence. Thus, for high-risk subjects, additional testing and/or referral should be considered.
The hyperinsulinemic euglycemic clamp is the “gold standard” for measuring insulin sensitivity, but it is labor intensive and impractical in routine clinical settings. Alter-native approaches using surrogate markers have commonly been utilized, including fasting insulin and glucose levels and 2-hour oral glucose tolerance test (OGTT). The utility of these approaches in the clinical setting has been limited by several factors, including lack of a universal insulin assay. However, despite these limitations, obtaining fasting insulin in addition to fasting glucose or performing 2-hour OGTT can be useful in providing crude estimates of insulin resistance in certain high-risk subpopulations [52,53]. Recently, the ADA added HgA1C measurement as diagnostic criteria for pre-diabetes (5.7%–6.4%) and diabetes (> 6.5%) [54]. Benefits of HgA1C measurement include reliable measurements in nonfasting conditions and reflection of glucose over time. Studies in pediatric patients have shown the usefulness of HgA1C as a measure of future glucose intolerance or diabetes [55]. When fasting insulin or HgA1C are elevated and/or OGTT is abnormal, this suggests the presence of insulin resistance and need for intervention.
Proposed guideline criteria for the diagnosis of “metabolic syndrome” in adolescents include the following: (1) glucose intolerance, (2) elevated waist circumference or BMI, (3) hypertriglyceridemia, (4) low HDL, and 5) hypertension. There is no universal definition for metabolic syndrome in childhood and adolescence, and cut-off values in each category vary by study group [41–43,56]. When insulin resistance is present, it should alert the clinician to the increased likelihood for metabolic syndrome and NAFLD, and additional screening should be performed accordingly. NAFLD is present in about 25% of all overweight children and is strongly associated with insulin resistance and the metabolic syndrome [57]. Hispanic patients have an increased prevalence of NAFLD compared with patients of other ethnicities [58,59]. Elevated liver transaminases (AST and ALT) are commonly used to screen for NAFLD. However, since these markers are indicative of hepatocellular damage, they may remain within normal limits and correlate poorly with early steatosis [51]. Alternative approaches have been proposed in high-risk populations to detect early steatosis and improve long-term prognosis [60].
Case Continued
The patient underwent laboratory assessment that included fasting glucose and insulin, fasting lipid panel, and ALT. Results were suggestive of insulin resistance and metabolic syndrome and included the following: fasting glucose 108 mg/dL, fasting insulin 65 uIU/mL (reference range 3–25), HgA1C 5.9% (reference range 4.2–5.8), total cholesterol 178 mg/dL, HDL cholesterol 35 mg/dL, LDL cholesterol 110 mg/dL, triglycerides 157 mg/dL, and ALT 40 u/L. Blood pressure, as noted above, is at the 95th percentile for age and height.
• What is the recommended approach to intervention? When is referral warranted?
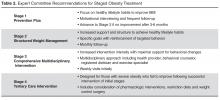
Staged Obesity Treatment
The initial stage, termed “Prevention Plus,” is similar to obesity prevention strategies and is focused on institution of healthy dietary and activity lifestyle habits tailored to the individual and family. Frequent follow-up and monitoring can be helpful and should be offered to families. Failure to demonstrate progress after 3 to 6 months warrants advancement to Stage 2, “Structured Weight Management,” which includes a planned diet with structured meals and snacks, reduction of screen time to 1 hour or less, 60 minutes of supervised physical activity, use of logs to document diet and activity levels, monthly follow-ups and positive reinforcement for achieving goals. Consultation with a dietician and health psychologist/counseling can be helpful at this level.
If no progress is noted after 3 to 6 months, progression to Stage 3, “Comprehensive Multidisciplinary Intervention,” is recommended. This stage emphasizes the importance of a multidisciplinary team including behavioral counselor, registered dietician and exercise specialist in addition to a medical provider. Current evidence suggests modest improvement of obesity and related comorbidities in adolescents participating in multidisciplinary weight management programs [62,63]. While these interventions can be implemented in community settings, coordination in this setting can be difficult and implementation more commonly involves weight management programs in tertiary care centers. Access to such programs can be limited by geographic accessibility, insurance coverage and physician awareness of available programs/resources [64]. Utilization of technology such as telemedicine visits is one way to overcome limited access [65]. Finally, Stage 4 “Tertiary Care Intervention”, involving discussion of pharmacologic or intensive/surgical weight loss options, can be considered for those who fail to show progression after successful intervention of previous stages.
Specialty Referral
Referral to multidisciplinary clinics specializing in childhood obesity is warranted when obesity is particularly severe, comorbidities are present at baseline, or no improvement is noted after 6 months of intense lifestyle intervention. Insulin resistance evidenced by impaired glucose tolerance (abnormal fasting or 2-hour glucose levels), HgA1C in the pre-diabetes range or higher (> 5.7%), or persistently elevated fasting insulin levels after 3 to 6 months of intensive lifestyle modification should prompt referral for consideration of metformin initiation. Metformin can reduce insulin resistance in children and may reduce progression from impaired glucose tolerance to diabetes [66]. For dyslipidemia related to metabolic syndrome, lifestyle interventions are most likely to be efficacious. Referral to preventative cardiology for consideration of pharmacologic intervention should be considered when severe hypertriglyceridemia is present (> 400 mg/dL) or LDL remains elevated after implementation of healthy lifestyle interventions. Elevations in ALT are highly specific for NAFLD and should prompt referral to gastroenterology. In addition, given the poor sensitivity of ALT for detection of early hepatic steatosis, referral might be considered when ALT is in the high normal ranges, especially in those with increased risk such as Hispanic patients [67]. Finally, when signs of obstructive sleep apnea are present, a sleep study should be performed. In summary, while specialty referral can aid targeted treatment of obesity-related morbidities, the central role of the primary care clinician in anticipating and preventing or minimizing their occurrence remains paramount.
Case Conclusion
The patient was referred to a multidisciplinary obesity clinic where he and his family met with dietician, exercise physiologist, health psychologist, and endocrinologist. Healthy lifestyle modifications with specific goals were instituted, including elimination of all calorie-containing beverages (except daily recommended intake of fat-free milk) and initiation of physical activity for 30 minutes a day 5 days per week. He was started on metformin due to glucose intolerance and increased risk for diabetes. Follow-up occurred at monthly intervals for the first 3 months. Additional goals and lifestyle interventions were implemented at each follow-up. At 6 months’ follow-up, the patient’s height was 164 cm, weight was stable at 58.4 kg and BMI was 21.7 (79th percentile). Blood pressure was slightly improved at 123/80 mm Hg. Repeat labs showed mild but consistent improvement in all areas. Specifically, fasting glucose 100 mg/dL, fasting insulin 40 uIU/mL, HgA1C 5.6%, total cholesterol 162 mg/dL, HDL cholesterol 40 mg/dL, LDL cholesterol 105 mg/dL, triglycerides 140 mg/dL, and ALT 38 u/L. The patient continues to be monitored closely with goal to improve metabolic health and long-term health outcomes.
Summary
Childhood obesity is a major public health concern. The health impact of obesity on children is broad and profound. Since treatment of obesity is often unsuccessful, prevention of obesity or early detection of its health consequences are crucial responsibilities and opportunities for primary care clinicians. While clinical guidelines can be instructive, application of clinical guidelines must be tailored to individual adolescent patients according to accompanying risk factors. This review aims to help clinicians stratify risk based on susceptibility to development of insulin resistance and other morbidities associated with adolescent obesity. While the enormity of the obesity epidemic can appear overwhelming to primary care providers, they remain in the best position to initiate early intervention strategies. Coordinating care between primary care providers and specialty clinics will continue to be an important partnership for the care of those experiencing health-threatening effects of adolescent obesity.
Corresponding author: Aaron L Carrel, MD, University of Wisconsin, 600 Highland Ave, H4-436, Madison, WI 53792.
Financial disclosures: Drs. Seibert and Carrel have received fellowship grants from Genentech.
1. CDC. Obesity task force report. 2010. Available at www.letsmove.gov/sites/letsmove.gov/files/TaskForce_on_Childhood_Obesity_May2010_FullReport.pdf. Accessed 4 Sept 2013.
2. Barlow SE, AAP Expert Committee. AAP Expert Committee Recommendations regarding prevention, assessment and treatment of child obesity. Pediatrics 2007;120:s164–92.
3. Dietz WH, Robinson TN. Overweight children and adolescents. N Engl J Med 2005;352:2100–9.
4. Centers for Disease Control and Prevention (CDC) 2012; Overweight and obesity. Available at www.cdc.gov/obesity/childhood/basics.html. Accessed 3 Sept 2013.
5. Centers for Disease Control and Prevention (CDC). Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2009–2010. Available at www.cdc.gov/nchs/data/hestat/obesity_child_09_10/obesity_child_09_10.pdf.
6. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–90.
7. August GP, Caprio S, Fennoy I, et al; Endocrine Society. Prevention and treatment of pediatric obesity: an endocrine society clinical practice guideline based on expert opinion. J Clin Endocrinol Metab 2008;93:4576–99.
8. Holmes ME, Eisenmann JC, Ekkekakis P, Gentile D. Physical activity, stress, and metabolic risk score in 8- to 18-year-old boys. J Phys Act Health 2008;5:294–307.
9. Peeters A, Barendregt JJ, Willekens F, et al. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 2003;138:24–32.
10. Sharifi M, Marshall G, Marshall R, et al. Accelerating progress in reducing childhood obesity disparities: exploring best practices of positive outliers. J Health Care Poor Underserved 2013;24(2 Suppl):193–9.
11. Cossrow N, Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. J Clin Endocrinol Metab 2004;89:2590–4.
12. Rosenbaum M, Fennoy I, Accacha S, et al. Racial/ethnic differences in clinical and biochemical type 2 diabetes mellitus risk factors in children. Obesity (Silver Spring) 2013;21:2081–90.
13. NIDDK. National diabetes statistics, 2011. Available at http://diabetes.niddk.nih.gov/dm/pubs/statistics/. Accessed 18 Sept 2013.
14. Janz KF, Butner KL, Pate RR. The role of pediatricians in increasing physical activity in youth. JAMA Pediatr 2013:1–2.
15. Coleman KJ, Hsii AC, Koebnick C, et al. Implementation of clinical practice guidelines for pediatric weight management. J Pediatrics 2012;160:918–22.
16. Ratcliff MB, Jenkins TM, Reiter-Purtill J, et al. Risk-taking behaviors of adolescents with extreme obesity: normative or not? Pediatrics 2011;127:827–34.
17. Goldenring J, Rosen D. Getting into adolescent heads: An essential update. Contemp Pediatr 2004;21:64.
18. Eisenmann JC, Welk GJ, Ihmels M, Dollman J. Fatness, fitness, and cardiovascular disease risk factors in children and adolescents. Med Sci Sports Exerc 2007;39:1251–6.
19. Weiss R, Shaw M, Savoye M, Caprio S. Obesity dynamics and cardiovascular risk factor stability in obese adolescents. Ped Diabetes 2009;10:360–7.
20. Rizzo NS, Ruiz JR, Ortega FB, Sjostrom M. Relationship of physical activity, fitness, and fatness with clustered metabolic risk in children and adolescents: The European Youth Heart Study. J Pediatr 2007;150:388–94.
21. Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics 2002;110(1 Pt 2):210–4.
22. Alexander SC, Ostbye T, Pollak KI, et al. Physicians’ beliefs about discussing obesity: results from focus groups. Am J Health Promot 2007;21:498–500.
23. Puhl RM, Peterson JL, Luedicke J. Weight-based victimization: bullying experiences of weight loss treatment-seeking youth. Pediatrics 2013;131:e1–9.
24. Christie D, Channon S. The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: a clinical review. Diabetes Obes Metab 2013. Aug 8 [Epub ahead of print].
25. Standards of medical care in diabetes--2010. Diabetes Care 2010;33 Suppl 1:S11–61.
26. Hasson RE, Adam TC, Davis JN, et al. Ethnic differences in insulin action in obese African-American and Latino adolescents. J Clin Endocrinol Metab 2010;95:4048–51.
27. Fernández JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatrics 2004;145:439–44.
28. Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics 2009;124 Suppl 1:S23–34.
29. Daniels SR, Khoury PR, Morrison JA. The utility of body mass index as a measure of body fatness in children and adolescents: differences by race and gender. Pediatrics 1997;99:804–7.
30. Curtis VA, Carrel AL, Eickhoff JC, Allen DB. Gender and race influence metabolic benefits of fitness in children: a cross-sectional study. Int J Pediatr Endocrinol 2012;2012:4.
31. Nightingale CM, Rudnicka AR, Owen CG, et al. Influence of adiposity on insulin resistance and glycemia markers among U.K. Children of South Asian, black African-Caribbean, and white European origin: child heart and health study in England. Diabetes Care 2013;36:1712–9.
32. Gutin B, Yin Z, Humphries MC, Hoffman WH, et al. Relations of fatness and fitness to fasting insulin in black and white adolescents. J Pediatr 2004;145:737–43.
33. Cook S. The metabolic syndrome: Antecedent of adult cardiovascular disease in pediatrics. J Pediatr 2004;145:427–30.
34. Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med 2002;162:2074–9.
35. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. September 1998. NIH Pub No. 98-4083. Available at www.ncbi.nlm.nih.gov/books/NBK2003/pdf/TOC.pdf. Accessed 29 Sept 2013.
36. Janssen I, Katzmarzyk PT, Srinivasan SR, et al. Combined influence of body mass index and waist circumference on coronary artery disease risk factors among children and adolescents. Pediatrics 2005;115:1623–30.
37. Freedman DS, Serdula MK, Srinivasan SR, Berenson GS. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr 1999;69:308–17.
38. Savva SC, Tornaritis M, Savva ME, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Rel Metab Disorders 2000;24:1453–8.
39. Lee S, Bacha F, Gungor N, Arslanian SA. Waist circumference is an independent predictor of insulin resistance in black and white youths. J Pediatrics 2006;148:188–94.
40. Wang J, Thornton JC, Bari S, et al. Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutrition 2003;77:379–84.
41. Cook S, Weitzman M, Auinger P, et al. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Ped Adol Med 2003;157:821–7.
42. Ford ES, Ajani UA, Mokdad AH. The metabolic syndrome and concentrations of C-reactive protein among U.S. youth. Diabetes Care 2005;28:878–81.
43. Cruz ML, Weigensberg MJ, Huang TT, et al. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. J Clin Endocrin Metab 2004;89:108–13.
44. Lee JM, Davis MM, Woolford SJ, Gurney JG. Waist circumference percentile thresholds for identifying adolescents with insulin resistance in clinical practice. Pediatric Diabetes 2009;10:336–42.
45. Li S, Chen W, Srinivasan SR, et al. Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am J Epidemiol 2012;1:S142–9.
46. Torley D, Bellus GA, Munro CS. Genes, growth factors and acanthosis nigricans. Br J Dermatol 2002;147:1096–101.
47. Mukhtar Q, Cleverley G, Voorhees RE, McGrath JW. Prevalence of acanthosis nigricans and its association with hyperinsulinemia in New Mexico adolescents. J. Adolesc Health 2001;28:372–6.
48. Brickman WJ, Huang J, Silverman BL, Metzger BE. Acanthosis nigricans identifies youth at high risk for metabolic abnormalities. J Pediatrics 2010;156:87–92.
49. Stuart CA, Pate CJ, Peters EJ. Prevalence of acanthosis nigricans in an unselected population. Am J Med 1989;87:269–72.
50. Brickman WJ, Binns HJ, Jovanovic BD, et al. Acanthosis nigricans: a common finding in overweight youth. Pediatr Dermatol 2007;24:601–6.
51. Yang HR, Kim HR, Kim MJ, et al. Noninvasive parameters and hepatic fibrosis scores in children with nonalcoholic fatty liver disease. World J Gastroenterol 2012;18:1525–30.
52. Chiarelli F, Marcovecchio ML. Insulin resistance and obesity in childhood. Eur J Endocrinol 2008;159 Suppl 1:S67–74.
53. Adam TC, Hasson RE, Lane CJ, Goran MI. Fasting indicators of insulin sensitivity: effects of ethnicity and pubertal status. Diabetes Care 2011;34:994–9.
54. Diagnosis and classification of diabetes mellitus. Diabetes Care 2013;36 Suppl 1:S67–74.
55. Nowicka P, Santoro N, Liu H, et al. Utility of hemoglobin A(1c) for diagnosing prediabetes and diabetes in obese children and adolescents. Diabetes Care 2011;34:1306–11.
56. Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 2004;350:2362–74.
57. Martins C, Pizarro A, Aires L, et al. Fitness and metabolic syndrome in obese fatty liver children. Ann Hum Biol 2013;40:99–101.
58. Taveras EM, Gillman MW, Kleinman KP, et al. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA Pediatr 2013;167:731–8.
59. Wolfgram PM, Connor EL, Rehm JL, et al. Ethnic differences in the effects of hepatic fat deposition on insulin resistance in non-obese middle school girls. Obesity (Silver Spring) 2014;22:243–8.
60. Sowa JP, Heider D, Bechmann LP, et al. Novel algorithm for non-invasive assessment of fibrosis in NAFLD. PLoS One 2013;8:e62439.
61. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120 Suppl 4:S164–192.
62. Woolford SJ, Sallinen BJ, Clark SJ, Freed GL. Results from a clinical multidisciplinary weight management program. Clin Pediatrics 2011;50:187–91.
63. Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA 2007;297:2697–704.
64. Woolford SJ, Clark SJ, Gebremariam A, et al. Physicians’ perspectives on referring obese adolescents to pediatric multidisciplinary weight management programs. Clin Pediatrics 2010;49:871–5.
65. Lipana LS, Bindal D, Nettiksimmons J, Shaikh U. Telemedicine and face-to-face care for pediatric obesity. Telemed J Ehealth 2013;19:806–8.
66. Park MH, Kinra S, Ward KJ, et al. Metformin for obesity in children and adolescents: a systematic review. Diabetes Care 2009;32:1743–5.
67. Urrutia-Rojas X, McConathy W, Willis B, et al. Abnormal glucose metabolism in Hispanic parents of children with acanthosis nigricans. ISRN Endocrinol 2011(Epub 2011 Dec 25.).
From the Department of Pediatrics, University of Wisconsin, Madison, WI.
Abstract
- Objective: To provide information that will assist clinicians in assessing and addressing risk for obesity-related comorbidities in adolescents.
- Methods: Review of the literature.
- Results: Childhood obesity is a major public health concern. Prevention of obesity or early detection of its health consequences are important responsibilities or opportunities for primary care clinicians. While body mass index (BMI) screening is valuable, insulin resistance and other obesity-related comorbidities can develop even when BMI falls below the 95th percentile threshold for obesity. Detailed history and physical examination can help identify comorbidities and guide diagnostic evaluation. Referral to multidisciplinary clinics specializing in childhood obesity is warranted when obesity is particularly severe, comorbidities are present at baseline, or no improvement is noted after 6 months of intense lifestyle intervention.
- Conclusion: For optimal health outcomes, management of adolescent obesity and associated comorbidities is should be adapted based on an individual’s overall risk rather than BMI alone.
Case Study
Initial Presentation
A 14-year-old Hispanic male presents for a well child check.
History and Physical Examination
The patient and his mother have no complaints or concerns. A comprehensive review of systems is positive for fatigue and snoring but is otherwise unremarkable. Past medical history is unremarkable except for mild intermittent asthma. Family history is positive for type 2 diabetes in paternal grandmother and a maternal uncle and cardiovascular disease and hypertension in multiple extended family members. Both maternal and paternal grandparents are from Mexico.
Vital signs are within normal limits. Height is 160 cm (30th percentile for age), weight is 58.4 kg (75th percentile for age), and body mass index (BMI) is 22.8 kg/m2 (85th percentile for age). Blood pressure is 127/81 mm Hg (95th percentile for age and gender). Physical exam is pertinent for acanthosis nigricans on neck and axilla and nonviolaceous striae on abdomen. Waist circumference is 88 cm (90th percentile for age and ethnicity). Otherwise, physical exam is within normal limits.
• Does this child’s physical examination findings pose a cause for concern?
Yes. A key concept is that while obesity is widespread, the adverse health complications of adiposity and overnutrition affect some children much earlier and more profoundly than others. Some children exhibit adiposity-associated comorbidities even prior to meeting obesity criteria defined by BMI. Careful history and examination can help identify those most at risk for developing adiposity-associated comorbidities, prompting earlier intervention and, when appropriate, subspecialty referral.
Obesity is caused by a complex interplay of genetic, environmental, and metabolic programming, especially early in life, and lifestyle habits [1,2]. The vast majority of obesity is due to excess nutrition leading to energy imbalance, while less than 1% is due to endocrine or syndromic causes [3]. Obesity is defined as excessive body fat and is often estimated indirectly by using a surrogate marker, BMI. Diagnostically, a BMI > 95th percentile for age on sex-specific CDC growth charts is defined as obese, while a BMI from the 85th to 94th percentile is defined as overweight [4]. Using these criteria, the prevalence of childhood obesity more than tripled in the past 3 decades [5], leading to its classification as an epidemic and public health crisis [2]. Today, an estimated 12.5 million American children are obese [5]. For adolescents specifically, the prevalence of obesity is 18.4%, with more than one-third overweight [6].
Childhood obesity is associated with both short- and long-term morbidities including insulin resistance and type 2 diabetes, hypertension, dyslipidemia, asthma, obstructive sleep apnea, psychosocial problems, and decreased quality of life [7,8]. Obese children, particularly older children and adolescents, are more likely become obese adults [2,7]. Obesity in adulthood is associated with both significant morbidity and premature death [9]. Individual characteristics such as lifestyle habits, fitness level, and genetic predisposition influence the likelihood of development of both obesity and associated comorbidities [10].
The burden of obesity and its associated comorbidities are not equally distributed among racial/ethnic and socioeconomic groups. Hispanic and non-Hispanic black children are much more likely to be obese and overweight than non-Hispanic white children [6]. Low socioeconomic status is associated with increased rates of obesity in certain subgroups, including adolescents [2]. In addition, certain ethnic/racial minorities are more likely to develop obesity-associated comorbidities, such as insulin resistance, type 2 diabetes, and non-alcoholic fatty liver disease (NAFLD). With regard to insulin resistance and development of type 2 diabetes, the risk is greatest in Native Americans, but there is also increased risk in Hispanic/Latinos, non-Hispanic blacks, and Asian Americans as compared with non-Hispanic whites [11–13]. Collectively, these findings highlight the need for individualized assessment and the importance of obesity prevention and early intervention to improve long-term health outcomes. Primary care providers play a pivotal role in this process of preventing, identifying and treating childhood obesity and associated comorbidities [14]. In the case history, the child’s ethnicity, family history, and borderline overweight BMI indicate a high risk for future obesity-related morbidity and a critical opportunity for prevention intervention.
• What are the initial steps a practitioner can take to address overweight and obesity?
To encourage the development of healthy lifestyles and prevention of obesity, dietary and exercise counseling should be routinely provided as part of anticipatory guidance to all children and families regardless of weight status. It is critical to recognize individuals at high risk for becoming obese starting early in life. Risk factors for obesity in healthy weight children include rapid crossing of BMI percentiles, obese parent(s), maternal history of gestational diabetes during pregnancy, ethnicity, sedentary lifestyle, and excessive caloric intake [2]. Identification of these high-risk individuals can prompt more intensive counseling and early intervention with the goal of preventing the development of obesity and its complications. The use of automated BMI calculation and electronic medical records can facilitate identification of overweight and obesity status when already present and improve counseling rates [15].
Obesity due to excess nutrition is typically associated with linear growth acceleration that occurs subsequent to and to a lesser degree than the percentile shift in weight gain. A declining height velocity associated with obesity, therefore, is concerning and should prompt investigation for endocrine disease such as hypothyroidism, glucocorticoid excess, and growth hormone deficiency. Additional factors that warrant further investigation and/or referral include growth trajectory significantly below genetic potential, developmental delay, and dysmorphic features. A complete physical examination should be performed to evaluate for signs consistent with these conditions (eg, violaceous striae in glucocorticoid excess, microcephaly, and small hands/feet in Prader-Willi syndrome), and signs of obesity-associated comorbidities (eg, acanthosis nigricans). Accurate height, weight, BMI calculation, and blood pressure assessment using an appropriately sized cuff are essential.
While BMI screening is valuable, as noted above it is important to appreciate that insulin resistance (and other obesity-related comorbidities) can develop even when BMI is below the 95th percentile. Detailed history and physical examination can help identify these comorbidities of excess adiposity and guide diagnostic evaluation. Independent risk factors for insulin resistance and the development of type 2 diabetes include family history of diabetes, minority race/ethnicity, elevated waist circumference, and poor fitness level [18–20].
Further History
The patient reports skipping breakfast on most days, eats lunch at school, and snacks on chips and soda after school. Dinner is variable but usually contains carbohydrates and a protein and rarely includes vegetables. Family eats “take-out” about 3 times per week. Patient reports spending 3 hours a day watching television and playing on computer. He had gym last semester but currently reports very limited to no physical activity on most days.
• What are effective ways to raise the issue of obesity during an office visit?
Despite the strong connection of obesity with adverse health outcomes, discussion of obesity in routine office settings can be difficult and is often limited by many factors such as time, training, availability of support services, perceived lack of patient motivation, and low outcome expectations [21,22]. Perhaps most challenging is tactfully handling the stigma associated with obesity, which can make discussion awkward and difficult for patients, parents, and providers. To do this, efforts to choose words that convey a nonjudgmental message while maintaining focus on obesity as a health concern are helpful. For example, terms such as “fat” and “obese” are often perceived as stigmatizing and blaming while using the term “unhealthy weight” is less pejorative and can be motivating [23]. It can also be important to acknowledge and emphasize that some individuals are more susceptible to weight gain and its consequences than others and as a result can tolerate fewer calories without unwanted weight gain and health problems. These approaches shift the focus of the discussion toward the goal of restoring and preserving health rather than changing physical appearance without placing blame on the individual and/or family. Motivational interviewing techniques which can be performed effectively even in short office visits can help to actively engage families, reveal familial perception of obesity and assess readiness to change [2]. Their use may also improve the efficacy of other interventions [24].
Case Continued
The patient and his mother were asked if they had any concerns today, including concerns about future health. Mother expressed worry about the potential for diabetes given their family history. The clinician used this as an opportunity to discuss pertinent factors associated with insulin resistance and type 2 diabetes, including modifiable factors such as diet, fitness level, and weight.
• Should this non-obese adolescent be assessed for obesity comorbidities?
Yes. While there are multiple guidelines available for pediatric screening, all highlight the importance of obtaining individualized risk assessment to guide the extent of diagnostic workup. An Expert Committee comprised of representatives from 15 professional organizations appointed 3 writing groups to review the literature and recommend approaches to prevention, assessment, and treatment. Because effective strategies remain poorly defined, the writing groups used both available evidence and expert opinion to develop the recommendations [2]. In addition to routine blood pressure monitoring and universal lipid screening, the Expert Committee recommends obtaining additional laboratory assessment for obese children (BMI ≥ 95th percentile) including a fasting glucose and ALT/AST levels every 2 years starting at age 10 years. For overweight children (BMI > 85th percentile), the Expert Committee recommends obtaining these studies if additional risk factors are present [2]. The American Diabetes Association (ADA) recommends obtaining diabetes screening in all children classified as overweight (defined as either a BMI > 85th percentile for age and sex, weight for height > 85th percentile, or weight > 120% of ideal for height) once every 3 years beginning at age 10 or at pubertal onset (whichever is earliest) when 2 additional risk factors for diabetes are also present, including: (1) history of type 2 diabetes in a first- or second-degree relative, (2) race/ethnicity with increased risk for diabetes development (eg, Native American, African American, Latino, Asian American), (3) signs of insulin resistance or conditions associated with insulin resistance (eg, small for gestational age, polycystic ovary syndrome, hypertension) and (4) maternal history of gestational diabetes during pregnancy [25]. The ADA recommendations for diabetes screening test include either fasting plasma glucose, HgA1C, or oral glucose tolerance test [25].
With a BMI at the 85th percentile, on initial assessment our patient might be perceived as being at moderate or even low risk for obesity and its associated comorbidities. However, a more careful review has elicited several additional risk factors suggesting more appropriate classification in the high-risk category. First, family history of type 2 diabetes on both sides of his family suggests a degree of genetic predisposition. Second, Hispanic ethnicity is known to be independently associated with insulin resistance, type 2 diabetes, and NAFLD [26]. Moreover, physical exam findings of an elevated waist circumference (90th percentile for age and ethnicity [27]) and acanthosis nigricans are also supportive of insulin resistance. As a result, despite having a BMI at the 85th percentile, this adolescent is at high risk and further evaluation is warranted based on both Expert Committee and ADA guidelines. Detailed discussion of certain risk factors is outlined below.
Pattern of Adipose Tissue Distribution: Utility of BMI and Waist Circumference
BMI is a clinical tool that serves as a surrogate marker of adiposity, but since it does not directly measure body fat it provides a statistical, rather than inherent, description of risk. While it is a relatively specific marker (~95%) with moderately high sensitivity and positive predictive value (~70–80%) at BMI levels > 95th percentile, sensitivity and positive predictive value decrease substantially at lower BMI percentiles (PPV 18% in a sample of overweight children) [28]. Current CDC BMI percentile charts consider age and gender differences but do not take into account sexual maturation level or race/ethnicity, both of which are independently correlated with BMI [29]. That is, children with similar BMIs of the same age and sex may exhibit varying degrees of adiposity and risk attributable to their pubertal stage and/or ethnicity [30]. For example, many studies have demonstrated that at the same BMI percentile, Asian Americans tend to have more adiposity compared with non-Hispanic whites [31], whereas African Americans tend to have more fat-free mass compared with non-Hispanic whites [32]. As a result of these differences, some advocate for adjusting cut-offs for BMI based on ethnicity and/or utilizing alternative measures of adiposity such as waist circumference or waist to hip ratio. However, in order for these latter methods to be useful, standardized methods of measurement and normative reference values must be developed. In summary, though BMI can be a useful screening tool, it is an indirect measure of adiposity and cannot discern adipose distribution. Therefore, it is important to remember that when used alone, BMI may overlook children with high inherent risk for disease.
Abdominal adiposity is associated with increased metabolic risk, including insulin resistance, type 2 diabetes, hypertension, cardiovascular disease, and mortality [33]. Waist circumference, a marker of abdominal/truncal obesity, has been considered as a potential marker in place of or in combination with BMI to identify children with increased metabolic risk. In adults, it is well established that an elevated waist circumference is associated with increased health risk, even among those within a normal-weight BMI category [34], and it is recommended that waist circumference in addition to BMI be used to assess health risk [35]. Many studies have documented similar associations between increased waist circumference and metabolic risk factors in childhood and adolescence [36–38]. Specifically, waist circumference is an independent predictor of both insulin sensitivity and increased visceral adiposity tissue (VAT) in children and adolescents [39]. Waist circumference can provide valuable information beyond BMI alone and may be beneficial in the clinical setting in identifying adolescents at risk for obesity-associated comorbidities.
The use of waist circumference in routine clinical settings is complicated and limited by many factors. First, there is no universal method for waist circumference measurement. For example, the WHO recommends measurement at the midpoint between the superior iliac crest and inferior most rib, while the NIH and NHANES recommend measurement immediately above the iliac crest [40]. Since nationally representative data published by Fernandez et al [27] uses the latter method for waist circumference measurement, we recommend this method to allow for comparison of waist circumference percentile with available data for age, sex, and ethnicity. Second, while absolute waist circumference values are used as cut-offs in adulthood, in childhood use of waist circumference percentiles would be more appropriate to account for expected increases during childhood and changes related to pubertal stage. Unfortunately, a lack of standardized waist circumference percentile charts makes meaningful interpretation of waist circumference difficult. Moreover, even if standardized waist circumference percentile charts were developed, there are currently no accepted standards defining an abnormally elevated waist circumference percentile.
Many studies have identified increased metabolic risk factors associated with a waist circumference at or above the 90th percentile for age [41–43]. Based on these studies, the International Diabetes Federation uses waist circumference > 90th percentile as part of the criteria for metabolic syndrome in adolescents. While this ensures a high degree of specificity, use of waist circumference at the 75th percentile would allow for increased sensitivity. For example, Lee et al found that for insulin resistance use of waist circumference at the 75th percentile compared with the 90th percentile increased sensitivity from 61.3% to 86.1% while decreasing specificity from 91.4% to 71.5% [44]. Thus, for individuals at low risk based on history and clinical findings, a waist circumference threshold at the 90th percentile might be reasonable, while for individuals with additional risk factors for insulin resistance use of a lower waist circumference threshold (such as the 75th percentile) may be beneficial. Finally, since risk for insulin resistance and type 2 diabetes varies by race/ethnicity, which may correspond with visceral fat deposition, utilizing various threshold cut-offs based on race/ethnicity has been proposed by some. However, current data do not support this practice [44]. In summary, though there are many challenges to using waist circumference measurements in routine settings, if performed correctly determination of elevated waist circumference measurement can provide some additional information on an individual’s overall risk for complications of obesity.
Acanthosis Nigricans as an Indicator of Insulin Resistance
Insulin resistance, independent of adiposity, is associated with increased risk for type 2 diabetes, cardiovascular disease, ovarian hyperandrogenism, and certain forms of cancer [45]. Identification of insulin resistance in the clinical setting can lead to appropriate intervention (both lifestyle and, when warranted, pharmacologic) to reduce insulin resistance and improve health outcomes. Several risk factors for insulin resistance have been discussed above. Acanthosis nigricans, which is characterized by thick, velvety hyperpigmentation of the skin in intertriginous areas such as the neck and axilla, is an additional finding that is associated with insulin resistance. Its pathogenesis is felt to be related to activation of the IGF-1 receptor by high levels of circulating insulin [46]. Acanthosis nigricans is independently associated with fasting insulin levels and impaired glucose tolerance [47,48]. In addition to increased insulin resistance, one study found that 1 in 4 youths with acanthosis nigricans demonstrated abnormalities in glucose homeostasis and identified 2 individuals with diabetes who would not have been diagnosed based on fasting glucose levels alone [48]. The presence of acanthosis nigricans should alert the clinician to the likelihood of insulin resistance and prompt further investigation. Of note, the prevalence of acanthosis nigricans is increased among African American and Hispanic patients [49,50].
• What laboratory evaluation is warranted and practical in the office setting?
Laboratory evaluation is warranted when obesity or risk factors for comorbidities of obesity are present. At minimum, this should include lipid screening, liver enzymes (ALT and AST), and fasting glucose as outlined above. This approach, however, fails to identify all individuals with obesity-associated comorbidities. ALT is only moderately sensitive in detecting NAFLD [51], and fasting glucose levels only become abnormal when compensation for the degree of insulin resistance is inadequate to maintain normal fasting glucose homeostasis. As a result, while abnormal results on screening are suggestive of disease, normal results do not necessarily confer its absence. Thus, for high-risk subjects, additional testing and/or referral should be considered.
The hyperinsulinemic euglycemic clamp is the “gold standard” for measuring insulin sensitivity, but it is labor intensive and impractical in routine clinical settings. Alter-native approaches using surrogate markers have commonly been utilized, including fasting insulin and glucose levels and 2-hour oral glucose tolerance test (OGTT). The utility of these approaches in the clinical setting has been limited by several factors, including lack of a universal insulin assay. However, despite these limitations, obtaining fasting insulin in addition to fasting glucose or performing 2-hour OGTT can be useful in providing crude estimates of insulin resistance in certain high-risk subpopulations [52,53]. Recently, the ADA added HgA1C measurement as diagnostic criteria for pre-diabetes (5.7%–6.4%) and diabetes (> 6.5%) [54]. Benefits of HgA1C measurement include reliable measurements in nonfasting conditions and reflection of glucose over time. Studies in pediatric patients have shown the usefulness of HgA1C as a measure of future glucose intolerance or diabetes [55]. When fasting insulin or HgA1C are elevated and/or OGTT is abnormal, this suggests the presence of insulin resistance and need for intervention.
Proposed guideline criteria for the diagnosis of “metabolic syndrome” in adolescents include the following: (1) glucose intolerance, (2) elevated waist circumference or BMI, (3) hypertriglyceridemia, (4) low HDL, and 5) hypertension. There is no universal definition for metabolic syndrome in childhood and adolescence, and cut-off values in each category vary by study group [41–43,56]. When insulin resistance is present, it should alert the clinician to the increased likelihood for metabolic syndrome and NAFLD, and additional screening should be performed accordingly. NAFLD is present in about 25% of all overweight children and is strongly associated with insulin resistance and the metabolic syndrome [57]. Hispanic patients have an increased prevalence of NAFLD compared with patients of other ethnicities [58,59]. Elevated liver transaminases (AST and ALT) are commonly used to screen for NAFLD. However, since these markers are indicative of hepatocellular damage, they may remain within normal limits and correlate poorly with early steatosis [51]. Alternative approaches have been proposed in high-risk populations to detect early steatosis and improve long-term prognosis [60].
Case Continued
The patient underwent laboratory assessment that included fasting glucose and insulin, fasting lipid panel, and ALT. Results were suggestive of insulin resistance and metabolic syndrome and included the following: fasting glucose 108 mg/dL, fasting insulin 65 uIU/mL (reference range 3–25), HgA1C 5.9% (reference range 4.2–5.8), total cholesterol 178 mg/dL, HDL cholesterol 35 mg/dL, LDL cholesterol 110 mg/dL, triglycerides 157 mg/dL, and ALT 40 u/L. Blood pressure, as noted above, is at the 95th percentile for age and height.
• What is the recommended approach to intervention? When is referral warranted?
Staged Obesity Treatment
The initial stage, termed “Prevention Plus,” is similar to obesity prevention strategies and is focused on institution of healthy dietary and activity lifestyle habits tailored to the individual and family. Frequent follow-up and monitoring can be helpful and should be offered to families. Failure to demonstrate progress after 3 to 6 months warrants advancement to Stage 2, “Structured Weight Management,” which includes a planned diet with structured meals and snacks, reduction of screen time to 1 hour or less, 60 minutes of supervised physical activity, use of logs to document diet and activity levels, monthly follow-ups and positive reinforcement for achieving goals. Consultation with a dietician and health psychologist/counseling can be helpful at this level.
If no progress is noted after 3 to 6 months, progression to Stage 3, “Comprehensive Multidisciplinary Intervention,” is recommended. This stage emphasizes the importance of a multidisciplinary team including behavioral counselor, registered dietician and exercise specialist in addition to a medical provider. Current evidence suggests modest improvement of obesity and related comorbidities in adolescents participating in multidisciplinary weight management programs [62,63]. While these interventions can be implemented in community settings, coordination in this setting can be difficult and implementation more commonly involves weight management programs in tertiary care centers. Access to such programs can be limited by geographic accessibility, insurance coverage and physician awareness of available programs/resources [64]. Utilization of technology such as telemedicine visits is one way to overcome limited access [65]. Finally, Stage 4 “Tertiary Care Intervention”, involving discussion of pharmacologic or intensive/surgical weight loss options, can be considered for those who fail to show progression after successful intervention of previous stages.
Specialty Referral
Referral to multidisciplinary clinics specializing in childhood obesity is warranted when obesity is particularly severe, comorbidities are present at baseline, or no improvement is noted after 6 months of intense lifestyle intervention. Insulin resistance evidenced by impaired glucose tolerance (abnormal fasting or 2-hour glucose levels), HgA1C in the pre-diabetes range or higher (> 5.7%), or persistently elevated fasting insulin levels after 3 to 6 months of intensive lifestyle modification should prompt referral for consideration of metformin initiation. Metformin can reduce insulin resistance in children and may reduce progression from impaired glucose tolerance to diabetes [66]. For dyslipidemia related to metabolic syndrome, lifestyle interventions are most likely to be efficacious. Referral to preventative cardiology for consideration of pharmacologic intervention should be considered when severe hypertriglyceridemia is present (> 400 mg/dL) or LDL remains elevated after implementation of healthy lifestyle interventions. Elevations in ALT are highly specific for NAFLD and should prompt referral to gastroenterology. In addition, given the poor sensitivity of ALT for detection of early hepatic steatosis, referral might be considered when ALT is in the high normal ranges, especially in those with increased risk such as Hispanic patients [67]. Finally, when signs of obstructive sleep apnea are present, a sleep study should be performed. In summary, while specialty referral can aid targeted treatment of obesity-related morbidities, the central role of the primary care clinician in anticipating and preventing or minimizing their occurrence remains paramount.
Case Conclusion
The patient was referred to a multidisciplinary obesity clinic where he and his family met with dietician, exercise physiologist, health psychologist, and endocrinologist. Healthy lifestyle modifications with specific goals were instituted, including elimination of all calorie-containing beverages (except daily recommended intake of fat-free milk) and initiation of physical activity for 30 minutes a day 5 days per week. He was started on metformin due to glucose intolerance and increased risk for diabetes. Follow-up occurred at monthly intervals for the first 3 months. Additional goals and lifestyle interventions were implemented at each follow-up. At 6 months’ follow-up, the patient’s height was 164 cm, weight was stable at 58.4 kg and BMI was 21.7 (79th percentile). Blood pressure was slightly improved at 123/80 mm Hg. Repeat labs showed mild but consistent improvement in all areas. Specifically, fasting glucose 100 mg/dL, fasting insulin 40 uIU/mL, HgA1C 5.6%, total cholesterol 162 mg/dL, HDL cholesterol 40 mg/dL, LDL cholesterol 105 mg/dL, triglycerides 140 mg/dL, and ALT 38 u/L. The patient continues to be monitored closely with goal to improve metabolic health and long-term health outcomes.
Summary
Childhood obesity is a major public health concern. The health impact of obesity on children is broad and profound. Since treatment of obesity is often unsuccessful, prevention of obesity or early detection of its health consequences are crucial responsibilities and opportunities for primary care clinicians. While clinical guidelines can be instructive, application of clinical guidelines must be tailored to individual adolescent patients according to accompanying risk factors. This review aims to help clinicians stratify risk based on susceptibility to development of insulin resistance and other morbidities associated with adolescent obesity. While the enormity of the obesity epidemic can appear overwhelming to primary care providers, they remain in the best position to initiate early intervention strategies. Coordinating care between primary care providers and specialty clinics will continue to be an important partnership for the care of those experiencing health-threatening effects of adolescent obesity.
Corresponding author: Aaron L Carrel, MD, University of Wisconsin, 600 Highland Ave, H4-436, Madison, WI 53792.
Financial disclosures: Drs. Seibert and Carrel have received fellowship grants from Genentech.
From the Department of Pediatrics, University of Wisconsin, Madison, WI.
Abstract
- Objective: To provide information that will assist clinicians in assessing and addressing risk for obesity-related comorbidities in adolescents.
- Methods: Review of the literature.
- Results: Childhood obesity is a major public health concern. Prevention of obesity or early detection of its health consequences are important responsibilities or opportunities for primary care clinicians. While body mass index (BMI) screening is valuable, insulin resistance and other obesity-related comorbidities can develop even when BMI falls below the 95th percentile threshold for obesity. Detailed history and physical examination can help identify comorbidities and guide diagnostic evaluation. Referral to multidisciplinary clinics specializing in childhood obesity is warranted when obesity is particularly severe, comorbidities are present at baseline, or no improvement is noted after 6 months of intense lifestyle intervention.
- Conclusion: For optimal health outcomes, management of adolescent obesity and associated comorbidities is should be adapted based on an individual’s overall risk rather than BMI alone.
Case Study
Initial Presentation
A 14-year-old Hispanic male presents for a well child check.
History and Physical Examination
The patient and his mother have no complaints or concerns. A comprehensive review of systems is positive for fatigue and snoring but is otherwise unremarkable. Past medical history is unremarkable except for mild intermittent asthma. Family history is positive for type 2 diabetes in paternal grandmother and a maternal uncle and cardiovascular disease and hypertension in multiple extended family members. Both maternal and paternal grandparents are from Mexico.
Vital signs are within normal limits. Height is 160 cm (30th percentile for age), weight is 58.4 kg (75th percentile for age), and body mass index (BMI) is 22.8 kg/m2 (85th percentile for age). Blood pressure is 127/81 mm Hg (95th percentile for age and gender). Physical exam is pertinent for acanthosis nigricans on neck and axilla and nonviolaceous striae on abdomen. Waist circumference is 88 cm (90th percentile for age and ethnicity). Otherwise, physical exam is within normal limits.
• Does this child’s physical examination findings pose a cause for concern?
Yes. A key concept is that while obesity is widespread, the adverse health complications of adiposity and overnutrition affect some children much earlier and more profoundly than others. Some children exhibit adiposity-associated comorbidities even prior to meeting obesity criteria defined by BMI. Careful history and examination can help identify those most at risk for developing adiposity-associated comorbidities, prompting earlier intervention and, when appropriate, subspecialty referral.
Obesity is caused by a complex interplay of genetic, environmental, and metabolic programming, especially early in life, and lifestyle habits [1,2]. The vast majority of obesity is due to excess nutrition leading to energy imbalance, while less than 1% is due to endocrine or syndromic causes [3]. Obesity is defined as excessive body fat and is often estimated indirectly by using a surrogate marker, BMI. Diagnostically, a BMI > 95th percentile for age on sex-specific CDC growth charts is defined as obese, while a BMI from the 85th to 94th percentile is defined as overweight [4]. Using these criteria, the prevalence of childhood obesity more than tripled in the past 3 decades [5], leading to its classification as an epidemic and public health crisis [2]. Today, an estimated 12.5 million American children are obese [5]. For adolescents specifically, the prevalence of obesity is 18.4%, with more than one-third overweight [6].
Childhood obesity is associated with both short- and long-term morbidities including insulin resistance and type 2 diabetes, hypertension, dyslipidemia, asthma, obstructive sleep apnea, psychosocial problems, and decreased quality of life [7,8]. Obese children, particularly older children and adolescents, are more likely become obese adults [2,7]. Obesity in adulthood is associated with both significant morbidity and premature death [9]. Individual characteristics such as lifestyle habits, fitness level, and genetic predisposition influence the likelihood of development of both obesity and associated comorbidities [10].
The burden of obesity and its associated comorbidities are not equally distributed among racial/ethnic and socioeconomic groups. Hispanic and non-Hispanic black children are much more likely to be obese and overweight than non-Hispanic white children [6]. Low socioeconomic status is associated with increased rates of obesity in certain subgroups, including adolescents [2]. In addition, certain ethnic/racial minorities are more likely to develop obesity-associated comorbidities, such as insulin resistance, type 2 diabetes, and non-alcoholic fatty liver disease (NAFLD). With regard to insulin resistance and development of type 2 diabetes, the risk is greatest in Native Americans, but there is also increased risk in Hispanic/Latinos, non-Hispanic blacks, and Asian Americans as compared with non-Hispanic whites [11–13]. Collectively, these findings highlight the need for individualized assessment and the importance of obesity prevention and early intervention to improve long-term health outcomes. Primary care providers play a pivotal role in this process of preventing, identifying and treating childhood obesity and associated comorbidities [14]. In the case history, the child’s ethnicity, family history, and borderline overweight BMI indicate a high risk for future obesity-related morbidity and a critical opportunity for prevention intervention.
• What are the initial steps a practitioner can take to address overweight and obesity?
To encourage the development of healthy lifestyles and prevention of obesity, dietary and exercise counseling should be routinely provided as part of anticipatory guidance to all children and families regardless of weight status. It is critical to recognize individuals at high risk for becoming obese starting early in life. Risk factors for obesity in healthy weight children include rapid crossing of BMI percentiles, obese parent(s), maternal history of gestational diabetes during pregnancy, ethnicity, sedentary lifestyle, and excessive caloric intake [2]. Identification of these high-risk individuals can prompt more intensive counseling and early intervention with the goal of preventing the development of obesity and its complications. The use of automated BMI calculation and electronic medical records can facilitate identification of overweight and obesity status when already present and improve counseling rates [15].
Obesity due to excess nutrition is typically associated with linear growth acceleration that occurs subsequent to and to a lesser degree than the percentile shift in weight gain. A declining height velocity associated with obesity, therefore, is concerning and should prompt investigation for endocrine disease such as hypothyroidism, glucocorticoid excess, and growth hormone deficiency. Additional factors that warrant further investigation and/or referral include growth trajectory significantly below genetic potential, developmental delay, and dysmorphic features. A complete physical examination should be performed to evaluate for signs consistent with these conditions (eg, violaceous striae in glucocorticoid excess, microcephaly, and small hands/feet in Prader-Willi syndrome), and signs of obesity-associated comorbidities (eg, acanthosis nigricans). Accurate height, weight, BMI calculation, and blood pressure assessment using an appropriately sized cuff are essential.
While BMI screening is valuable, as noted above it is important to appreciate that insulin resistance (and other obesity-related comorbidities) can develop even when BMI is below the 95th percentile. Detailed history and physical examination can help identify these comorbidities of excess adiposity and guide diagnostic evaluation. Independent risk factors for insulin resistance and the development of type 2 diabetes include family history of diabetes, minority race/ethnicity, elevated waist circumference, and poor fitness level [18–20].
Further History
The patient reports skipping breakfast on most days, eats lunch at school, and snacks on chips and soda after school. Dinner is variable but usually contains carbohydrates and a protein and rarely includes vegetables. Family eats “take-out” about 3 times per week. Patient reports spending 3 hours a day watching television and playing on computer. He had gym last semester but currently reports very limited to no physical activity on most days.
• What are effective ways to raise the issue of obesity during an office visit?
Despite the strong connection of obesity with adverse health outcomes, discussion of obesity in routine office settings can be difficult and is often limited by many factors such as time, training, availability of support services, perceived lack of patient motivation, and low outcome expectations [21,22]. Perhaps most challenging is tactfully handling the stigma associated with obesity, which can make discussion awkward and difficult for patients, parents, and providers. To do this, efforts to choose words that convey a nonjudgmental message while maintaining focus on obesity as a health concern are helpful. For example, terms such as “fat” and “obese” are often perceived as stigmatizing and blaming while using the term “unhealthy weight” is less pejorative and can be motivating [23]. It can also be important to acknowledge and emphasize that some individuals are more susceptible to weight gain and its consequences than others and as a result can tolerate fewer calories without unwanted weight gain and health problems. These approaches shift the focus of the discussion toward the goal of restoring and preserving health rather than changing physical appearance without placing blame on the individual and/or family. Motivational interviewing techniques which can be performed effectively even in short office visits can help to actively engage families, reveal familial perception of obesity and assess readiness to change [2]. Their use may also improve the efficacy of other interventions [24].
Case Continued
The patient and his mother were asked if they had any concerns today, including concerns about future health. Mother expressed worry about the potential for diabetes given their family history. The clinician used this as an opportunity to discuss pertinent factors associated with insulin resistance and type 2 diabetes, including modifiable factors such as diet, fitness level, and weight.
• Should this non-obese adolescent be assessed for obesity comorbidities?
Yes. While there are multiple guidelines available for pediatric screening, all highlight the importance of obtaining individualized risk assessment to guide the extent of diagnostic workup. An Expert Committee comprised of representatives from 15 professional organizations appointed 3 writing groups to review the literature and recommend approaches to prevention, assessment, and treatment. Because effective strategies remain poorly defined, the writing groups used both available evidence and expert opinion to develop the recommendations [2]. In addition to routine blood pressure monitoring and universal lipid screening, the Expert Committee recommends obtaining additional laboratory assessment for obese children (BMI ≥ 95th percentile) including a fasting glucose and ALT/AST levels every 2 years starting at age 10 years. For overweight children (BMI > 85th percentile), the Expert Committee recommends obtaining these studies if additional risk factors are present [2]. The American Diabetes Association (ADA) recommends obtaining diabetes screening in all children classified as overweight (defined as either a BMI > 85th percentile for age and sex, weight for height > 85th percentile, or weight > 120% of ideal for height) once every 3 years beginning at age 10 or at pubertal onset (whichever is earliest) when 2 additional risk factors for diabetes are also present, including: (1) history of type 2 diabetes in a first- or second-degree relative, (2) race/ethnicity with increased risk for diabetes development (eg, Native American, African American, Latino, Asian American), (3) signs of insulin resistance or conditions associated with insulin resistance (eg, small for gestational age, polycystic ovary syndrome, hypertension) and (4) maternal history of gestational diabetes during pregnancy [25]. The ADA recommendations for diabetes screening test include either fasting plasma glucose, HgA1C, or oral glucose tolerance test [25].
With a BMI at the 85th percentile, on initial assessment our patient might be perceived as being at moderate or even low risk for obesity and its associated comorbidities. However, a more careful review has elicited several additional risk factors suggesting more appropriate classification in the high-risk category. First, family history of type 2 diabetes on both sides of his family suggests a degree of genetic predisposition. Second, Hispanic ethnicity is known to be independently associated with insulin resistance, type 2 diabetes, and NAFLD [26]. Moreover, physical exam findings of an elevated waist circumference (90th percentile for age and ethnicity [27]) and acanthosis nigricans are also supportive of insulin resistance. As a result, despite having a BMI at the 85th percentile, this adolescent is at high risk and further evaluation is warranted based on both Expert Committee and ADA guidelines. Detailed discussion of certain risk factors is outlined below.
Pattern of Adipose Tissue Distribution: Utility of BMI and Waist Circumference
BMI is a clinical tool that serves as a surrogate marker of adiposity, but since it does not directly measure body fat it provides a statistical, rather than inherent, description of risk. While it is a relatively specific marker (~95%) with moderately high sensitivity and positive predictive value (~70–80%) at BMI levels > 95th percentile, sensitivity and positive predictive value decrease substantially at lower BMI percentiles (PPV 18% in a sample of overweight children) [28]. Current CDC BMI percentile charts consider age and gender differences but do not take into account sexual maturation level or race/ethnicity, both of which are independently correlated with BMI [29]. That is, children with similar BMIs of the same age and sex may exhibit varying degrees of adiposity and risk attributable to their pubertal stage and/or ethnicity [30]. For example, many studies have demonstrated that at the same BMI percentile, Asian Americans tend to have more adiposity compared with non-Hispanic whites [31], whereas African Americans tend to have more fat-free mass compared with non-Hispanic whites [32]. As a result of these differences, some advocate for adjusting cut-offs for BMI based on ethnicity and/or utilizing alternative measures of adiposity such as waist circumference or waist to hip ratio. However, in order for these latter methods to be useful, standardized methods of measurement and normative reference values must be developed. In summary, though BMI can be a useful screening tool, it is an indirect measure of adiposity and cannot discern adipose distribution. Therefore, it is important to remember that when used alone, BMI may overlook children with high inherent risk for disease.
Abdominal adiposity is associated with increased metabolic risk, including insulin resistance, type 2 diabetes, hypertension, cardiovascular disease, and mortality [33]. Waist circumference, a marker of abdominal/truncal obesity, has been considered as a potential marker in place of or in combination with BMI to identify children with increased metabolic risk. In adults, it is well established that an elevated waist circumference is associated with increased health risk, even among those within a normal-weight BMI category [34], and it is recommended that waist circumference in addition to BMI be used to assess health risk [35]. Many studies have documented similar associations between increased waist circumference and metabolic risk factors in childhood and adolescence [36–38]. Specifically, waist circumference is an independent predictor of both insulin sensitivity and increased visceral adiposity tissue (VAT) in children and adolescents [39]. Waist circumference can provide valuable information beyond BMI alone and may be beneficial in the clinical setting in identifying adolescents at risk for obesity-associated comorbidities.
The use of waist circumference in routine clinical settings is complicated and limited by many factors. First, there is no universal method for waist circumference measurement. For example, the WHO recommends measurement at the midpoint between the superior iliac crest and inferior most rib, while the NIH and NHANES recommend measurement immediately above the iliac crest [40]. Since nationally representative data published by Fernandez et al [27] uses the latter method for waist circumference measurement, we recommend this method to allow for comparison of waist circumference percentile with available data for age, sex, and ethnicity. Second, while absolute waist circumference values are used as cut-offs in adulthood, in childhood use of waist circumference percentiles would be more appropriate to account for expected increases during childhood and changes related to pubertal stage. Unfortunately, a lack of standardized waist circumference percentile charts makes meaningful interpretation of waist circumference difficult. Moreover, even if standardized waist circumference percentile charts were developed, there are currently no accepted standards defining an abnormally elevated waist circumference percentile.
Many studies have identified increased metabolic risk factors associated with a waist circumference at or above the 90th percentile for age [41–43]. Based on these studies, the International Diabetes Federation uses waist circumference > 90th percentile as part of the criteria for metabolic syndrome in adolescents. While this ensures a high degree of specificity, use of waist circumference at the 75th percentile would allow for increased sensitivity. For example, Lee et al found that for insulin resistance use of waist circumference at the 75th percentile compared with the 90th percentile increased sensitivity from 61.3% to 86.1% while decreasing specificity from 91.4% to 71.5% [44]. Thus, for individuals at low risk based on history and clinical findings, a waist circumference threshold at the 90th percentile might be reasonable, while for individuals with additional risk factors for insulin resistance use of a lower waist circumference threshold (such as the 75th percentile) may be beneficial. Finally, since risk for insulin resistance and type 2 diabetes varies by race/ethnicity, which may correspond with visceral fat deposition, utilizing various threshold cut-offs based on race/ethnicity has been proposed by some. However, current data do not support this practice [44]. In summary, though there are many challenges to using waist circumference measurements in routine settings, if performed correctly determination of elevated waist circumference measurement can provide some additional information on an individual’s overall risk for complications of obesity.
Acanthosis Nigricans as an Indicator of Insulin Resistance
Insulin resistance, independent of adiposity, is associated with increased risk for type 2 diabetes, cardiovascular disease, ovarian hyperandrogenism, and certain forms of cancer [45]. Identification of insulin resistance in the clinical setting can lead to appropriate intervention (both lifestyle and, when warranted, pharmacologic) to reduce insulin resistance and improve health outcomes. Several risk factors for insulin resistance have been discussed above. Acanthosis nigricans, which is characterized by thick, velvety hyperpigmentation of the skin in intertriginous areas such as the neck and axilla, is an additional finding that is associated with insulin resistance. Its pathogenesis is felt to be related to activation of the IGF-1 receptor by high levels of circulating insulin [46]. Acanthosis nigricans is independently associated with fasting insulin levels and impaired glucose tolerance [47,48]. In addition to increased insulin resistance, one study found that 1 in 4 youths with acanthosis nigricans demonstrated abnormalities in glucose homeostasis and identified 2 individuals with diabetes who would not have been diagnosed based on fasting glucose levels alone [48]. The presence of acanthosis nigricans should alert the clinician to the likelihood of insulin resistance and prompt further investigation. Of note, the prevalence of acanthosis nigricans is increased among African American and Hispanic patients [49,50].
• What laboratory evaluation is warranted and practical in the office setting?
Laboratory evaluation is warranted when obesity or risk factors for comorbidities of obesity are present. At minimum, this should include lipid screening, liver enzymes (ALT and AST), and fasting glucose as outlined above. This approach, however, fails to identify all individuals with obesity-associated comorbidities. ALT is only moderately sensitive in detecting NAFLD [51], and fasting glucose levels only become abnormal when compensation for the degree of insulin resistance is inadequate to maintain normal fasting glucose homeostasis. As a result, while abnormal results on screening are suggestive of disease, normal results do not necessarily confer its absence. Thus, for high-risk subjects, additional testing and/or referral should be considered.
The hyperinsulinemic euglycemic clamp is the “gold standard” for measuring insulin sensitivity, but it is labor intensive and impractical in routine clinical settings. Alter-native approaches using surrogate markers have commonly been utilized, including fasting insulin and glucose levels and 2-hour oral glucose tolerance test (OGTT). The utility of these approaches in the clinical setting has been limited by several factors, including lack of a universal insulin assay. However, despite these limitations, obtaining fasting insulin in addition to fasting glucose or performing 2-hour OGTT can be useful in providing crude estimates of insulin resistance in certain high-risk subpopulations [52,53]. Recently, the ADA added HgA1C measurement as diagnostic criteria for pre-diabetes (5.7%–6.4%) and diabetes (> 6.5%) [54]. Benefits of HgA1C measurement include reliable measurements in nonfasting conditions and reflection of glucose over time. Studies in pediatric patients have shown the usefulness of HgA1C as a measure of future glucose intolerance or diabetes [55]. When fasting insulin or HgA1C are elevated and/or OGTT is abnormal, this suggests the presence of insulin resistance and need for intervention.
Proposed guideline criteria for the diagnosis of “metabolic syndrome” in adolescents include the following: (1) glucose intolerance, (2) elevated waist circumference or BMI, (3) hypertriglyceridemia, (4) low HDL, and 5) hypertension. There is no universal definition for metabolic syndrome in childhood and adolescence, and cut-off values in each category vary by study group [41–43,56]. When insulin resistance is present, it should alert the clinician to the increased likelihood for metabolic syndrome and NAFLD, and additional screening should be performed accordingly. NAFLD is present in about 25% of all overweight children and is strongly associated with insulin resistance and the metabolic syndrome [57]. Hispanic patients have an increased prevalence of NAFLD compared with patients of other ethnicities [58,59]. Elevated liver transaminases (AST and ALT) are commonly used to screen for NAFLD. However, since these markers are indicative of hepatocellular damage, they may remain within normal limits and correlate poorly with early steatosis [51]. Alternative approaches have been proposed in high-risk populations to detect early steatosis and improve long-term prognosis [60].
Case Continued
The patient underwent laboratory assessment that included fasting glucose and insulin, fasting lipid panel, and ALT. Results were suggestive of insulin resistance and metabolic syndrome and included the following: fasting glucose 108 mg/dL, fasting insulin 65 uIU/mL (reference range 3–25), HgA1C 5.9% (reference range 4.2–5.8), total cholesterol 178 mg/dL, HDL cholesterol 35 mg/dL, LDL cholesterol 110 mg/dL, triglycerides 157 mg/dL, and ALT 40 u/L. Blood pressure, as noted above, is at the 95th percentile for age and height.
• What is the recommended approach to intervention? When is referral warranted?
Staged Obesity Treatment
The initial stage, termed “Prevention Plus,” is similar to obesity prevention strategies and is focused on institution of healthy dietary and activity lifestyle habits tailored to the individual and family. Frequent follow-up and monitoring can be helpful and should be offered to families. Failure to demonstrate progress after 3 to 6 months warrants advancement to Stage 2, “Structured Weight Management,” which includes a planned diet with structured meals and snacks, reduction of screen time to 1 hour or less, 60 minutes of supervised physical activity, use of logs to document diet and activity levels, monthly follow-ups and positive reinforcement for achieving goals. Consultation with a dietician and health psychologist/counseling can be helpful at this level.
If no progress is noted after 3 to 6 months, progression to Stage 3, “Comprehensive Multidisciplinary Intervention,” is recommended. This stage emphasizes the importance of a multidisciplinary team including behavioral counselor, registered dietician and exercise specialist in addition to a medical provider. Current evidence suggests modest improvement of obesity and related comorbidities in adolescents participating in multidisciplinary weight management programs [62,63]. While these interventions can be implemented in community settings, coordination in this setting can be difficult and implementation more commonly involves weight management programs in tertiary care centers. Access to such programs can be limited by geographic accessibility, insurance coverage and physician awareness of available programs/resources [64]. Utilization of technology such as telemedicine visits is one way to overcome limited access [65]. Finally, Stage 4 “Tertiary Care Intervention”, involving discussion of pharmacologic or intensive/surgical weight loss options, can be considered for those who fail to show progression after successful intervention of previous stages.
Specialty Referral
Referral to multidisciplinary clinics specializing in childhood obesity is warranted when obesity is particularly severe, comorbidities are present at baseline, or no improvement is noted after 6 months of intense lifestyle intervention. Insulin resistance evidenced by impaired glucose tolerance (abnormal fasting or 2-hour glucose levels), HgA1C in the pre-diabetes range or higher (> 5.7%), or persistently elevated fasting insulin levels after 3 to 6 months of intensive lifestyle modification should prompt referral for consideration of metformin initiation. Metformin can reduce insulin resistance in children and may reduce progression from impaired glucose tolerance to diabetes [66]. For dyslipidemia related to metabolic syndrome, lifestyle interventions are most likely to be efficacious. Referral to preventative cardiology for consideration of pharmacologic intervention should be considered when severe hypertriglyceridemia is present (> 400 mg/dL) or LDL remains elevated after implementation of healthy lifestyle interventions. Elevations in ALT are highly specific for NAFLD and should prompt referral to gastroenterology. In addition, given the poor sensitivity of ALT for detection of early hepatic steatosis, referral might be considered when ALT is in the high normal ranges, especially in those with increased risk such as Hispanic patients [67]. Finally, when signs of obstructive sleep apnea are present, a sleep study should be performed. In summary, while specialty referral can aid targeted treatment of obesity-related morbidities, the central role of the primary care clinician in anticipating and preventing or minimizing their occurrence remains paramount.
Case Conclusion
The patient was referred to a multidisciplinary obesity clinic where he and his family met with dietician, exercise physiologist, health psychologist, and endocrinologist. Healthy lifestyle modifications with specific goals were instituted, including elimination of all calorie-containing beverages (except daily recommended intake of fat-free milk) and initiation of physical activity for 30 minutes a day 5 days per week. He was started on metformin due to glucose intolerance and increased risk for diabetes. Follow-up occurred at monthly intervals for the first 3 months. Additional goals and lifestyle interventions were implemented at each follow-up. At 6 months’ follow-up, the patient’s height was 164 cm, weight was stable at 58.4 kg and BMI was 21.7 (79th percentile). Blood pressure was slightly improved at 123/80 mm Hg. Repeat labs showed mild but consistent improvement in all areas. Specifically, fasting glucose 100 mg/dL, fasting insulin 40 uIU/mL, HgA1C 5.6%, total cholesterol 162 mg/dL, HDL cholesterol 40 mg/dL, LDL cholesterol 105 mg/dL, triglycerides 140 mg/dL, and ALT 38 u/L. The patient continues to be monitored closely with goal to improve metabolic health and long-term health outcomes.
Summary
Childhood obesity is a major public health concern. The health impact of obesity on children is broad and profound. Since treatment of obesity is often unsuccessful, prevention of obesity or early detection of its health consequences are crucial responsibilities and opportunities for primary care clinicians. While clinical guidelines can be instructive, application of clinical guidelines must be tailored to individual adolescent patients according to accompanying risk factors. This review aims to help clinicians stratify risk based on susceptibility to development of insulin resistance and other morbidities associated with adolescent obesity. While the enormity of the obesity epidemic can appear overwhelming to primary care providers, they remain in the best position to initiate early intervention strategies. Coordinating care between primary care providers and specialty clinics will continue to be an important partnership for the care of those experiencing health-threatening effects of adolescent obesity.
Corresponding author: Aaron L Carrel, MD, University of Wisconsin, 600 Highland Ave, H4-436, Madison, WI 53792.
Financial disclosures: Drs. Seibert and Carrel have received fellowship grants from Genentech.
1. CDC. Obesity task force report. 2010. Available at www.letsmove.gov/sites/letsmove.gov/files/TaskForce_on_Childhood_Obesity_May2010_FullReport.pdf. Accessed 4 Sept 2013.
2. Barlow SE, AAP Expert Committee. AAP Expert Committee Recommendations regarding prevention, assessment and treatment of child obesity. Pediatrics 2007;120:s164–92.
3. Dietz WH, Robinson TN. Overweight children and adolescents. N Engl J Med 2005;352:2100–9.
4. Centers for Disease Control and Prevention (CDC) 2012; Overweight and obesity. Available at www.cdc.gov/obesity/childhood/basics.html. Accessed 3 Sept 2013.
5. Centers for Disease Control and Prevention (CDC). Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2009–2010. Available at www.cdc.gov/nchs/data/hestat/obesity_child_09_10/obesity_child_09_10.pdf.
6. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–90.
7. August GP, Caprio S, Fennoy I, et al; Endocrine Society. Prevention and treatment of pediatric obesity: an endocrine society clinical practice guideline based on expert opinion. J Clin Endocrinol Metab 2008;93:4576–99.
8. Holmes ME, Eisenmann JC, Ekkekakis P, Gentile D. Physical activity, stress, and metabolic risk score in 8- to 18-year-old boys. J Phys Act Health 2008;5:294–307.
9. Peeters A, Barendregt JJ, Willekens F, et al. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 2003;138:24–32.
10. Sharifi M, Marshall G, Marshall R, et al. Accelerating progress in reducing childhood obesity disparities: exploring best practices of positive outliers. J Health Care Poor Underserved 2013;24(2 Suppl):193–9.
11. Cossrow N, Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. J Clin Endocrinol Metab 2004;89:2590–4.
12. Rosenbaum M, Fennoy I, Accacha S, et al. Racial/ethnic differences in clinical and biochemical type 2 diabetes mellitus risk factors in children. Obesity (Silver Spring) 2013;21:2081–90.
13. NIDDK. National diabetes statistics, 2011. Available at http://diabetes.niddk.nih.gov/dm/pubs/statistics/. Accessed 18 Sept 2013.
14. Janz KF, Butner KL, Pate RR. The role of pediatricians in increasing physical activity in youth. JAMA Pediatr 2013:1–2.
15. Coleman KJ, Hsii AC, Koebnick C, et al. Implementation of clinical practice guidelines for pediatric weight management. J Pediatrics 2012;160:918–22.
16. Ratcliff MB, Jenkins TM, Reiter-Purtill J, et al. Risk-taking behaviors of adolescents with extreme obesity: normative or not? Pediatrics 2011;127:827–34.
17. Goldenring J, Rosen D. Getting into adolescent heads: An essential update. Contemp Pediatr 2004;21:64.
18. Eisenmann JC, Welk GJ, Ihmels M, Dollman J. Fatness, fitness, and cardiovascular disease risk factors in children and adolescents. Med Sci Sports Exerc 2007;39:1251–6.
19. Weiss R, Shaw M, Savoye M, Caprio S. Obesity dynamics and cardiovascular risk factor stability in obese adolescents. Ped Diabetes 2009;10:360–7.
20. Rizzo NS, Ruiz JR, Ortega FB, Sjostrom M. Relationship of physical activity, fitness, and fatness with clustered metabolic risk in children and adolescents: The European Youth Heart Study. J Pediatr 2007;150:388–94.
21. Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics 2002;110(1 Pt 2):210–4.
22. Alexander SC, Ostbye T, Pollak KI, et al. Physicians’ beliefs about discussing obesity: results from focus groups. Am J Health Promot 2007;21:498–500.
23. Puhl RM, Peterson JL, Luedicke J. Weight-based victimization: bullying experiences of weight loss treatment-seeking youth. Pediatrics 2013;131:e1–9.
24. Christie D, Channon S. The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: a clinical review. Diabetes Obes Metab 2013. Aug 8 [Epub ahead of print].
25. Standards of medical care in diabetes--2010. Diabetes Care 2010;33 Suppl 1:S11–61.
26. Hasson RE, Adam TC, Davis JN, et al. Ethnic differences in insulin action in obese African-American and Latino adolescents. J Clin Endocrinol Metab 2010;95:4048–51.
27. Fernández JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatrics 2004;145:439–44.
28. Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics 2009;124 Suppl 1:S23–34.
29. Daniels SR, Khoury PR, Morrison JA. The utility of body mass index as a measure of body fatness in children and adolescents: differences by race and gender. Pediatrics 1997;99:804–7.
30. Curtis VA, Carrel AL, Eickhoff JC, Allen DB. Gender and race influence metabolic benefits of fitness in children: a cross-sectional study. Int J Pediatr Endocrinol 2012;2012:4.
31. Nightingale CM, Rudnicka AR, Owen CG, et al. Influence of adiposity on insulin resistance and glycemia markers among U.K. Children of South Asian, black African-Caribbean, and white European origin: child heart and health study in England. Diabetes Care 2013;36:1712–9.
32. Gutin B, Yin Z, Humphries MC, Hoffman WH, et al. Relations of fatness and fitness to fasting insulin in black and white adolescents. J Pediatr 2004;145:737–43.
33. Cook S. The metabolic syndrome: Antecedent of adult cardiovascular disease in pediatrics. J Pediatr 2004;145:427–30.
34. Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med 2002;162:2074–9.
35. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. September 1998. NIH Pub No. 98-4083. Available at www.ncbi.nlm.nih.gov/books/NBK2003/pdf/TOC.pdf. Accessed 29 Sept 2013.
36. Janssen I, Katzmarzyk PT, Srinivasan SR, et al. Combined influence of body mass index and waist circumference on coronary artery disease risk factors among children and adolescents. Pediatrics 2005;115:1623–30.
37. Freedman DS, Serdula MK, Srinivasan SR, Berenson GS. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr 1999;69:308–17.
38. Savva SC, Tornaritis M, Savva ME, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Rel Metab Disorders 2000;24:1453–8.
39. Lee S, Bacha F, Gungor N, Arslanian SA. Waist circumference is an independent predictor of insulin resistance in black and white youths. J Pediatrics 2006;148:188–94.
40. Wang J, Thornton JC, Bari S, et al. Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutrition 2003;77:379–84.
41. Cook S, Weitzman M, Auinger P, et al. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Ped Adol Med 2003;157:821–7.
42. Ford ES, Ajani UA, Mokdad AH. The metabolic syndrome and concentrations of C-reactive protein among U.S. youth. Diabetes Care 2005;28:878–81.
43. Cruz ML, Weigensberg MJ, Huang TT, et al. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. J Clin Endocrin Metab 2004;89:108–13.
44. Lee JM, Davis MM, Woolford SJ, Gurney JG. Waist circumference percentile thresholds for identifying adolescents with insulin resistance in clinical practice. Pediatric Diabetes 2009;10:336–42.
45. Li S, Chen W, Srinivasan SR, et al. Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am J Epidemiol 2012;1:S142–9.
46. Torley D, Bellus GA, Munro CS. Genes, growth factors and acanthosis nigricans. Br J Dermatol 2002;147:1096–101.
47. Mukhtar Q, Cleverley G, Voorhees RE, McGrath JW. Prevalence of acanthosis nigricans and its association with hyperinsulinemia in New Mexico adolescents. J. Adolesc Health 2001;28:372–6.
48. Brickman WJ, Huang J, Silverman BL, Metzger BE. Acanthosis nigricans identifies youth at high risk for metabolic abnormalities. J Pediatrics 2010;156:87–92.
49. Stuart CA, Pate CJ, Peters EJ. Prevalence of acanthosis nigricans in an unselected population. Am J Med 1989;87:269–72.
50. Brickman WJ, Binns HJ, Jovanovic BD, et al. Acanthosis nigricans: a common finding in overweight youth. Pediatr Dermatol 2007;24:601–6.
51. Yang HR, Kim HR, Kim MJ, et al. Noninvasive parameters and hepatic fibrosis scores in children with nonalcoholic fatty liver disease. World J Gastroenterol 2012;18:1525–30.
52. Chiarelli F, Marcovecchio ML. Insulin resistance and obesity in childhood. Eur J Endocrinol 2008;159 Suppl 1:S67–74.
53. Adam TC, Hasson RE, Lane CJ, Goran MI. Fasting indicators of insulin sensitivity: effects of ethnicity and pubertal status. Diabetes Care 2011;34:994–9.
54. Diagnosis and classification of diabetes mellitus. Diabetes Care 2013;36 Suppl 1:S67–74.
55. Nowicka P, Santoro N, Liu H, et al. Utility of hemoglobin A(1c) for diagnosing prediabetes and diabetes in obese children and adolescents. Diabetes Care 2011;34:1306–11.
56. Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 2004;350:2362–74.
57. Martins C, Pizarro A, Aires L, et al. Fitness and metabolic syndrome in obese fatty liver children. Ann Hum Biol 2013;40:99–101.
58. Taveras EM, Gillman MW, Kleinman KP, et al. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA Pediatr 2013;167:731–8.
59. Wolfgram PM, Connor EL, Rehm JL, et al. Ethnic differences in the effects of hepatic fat deposition on insulin resistance in non-obese middle school girls. Obesity (Silver Spring) 2014;22:243–8.
60. Sowa JP, Heider D, Bechmann LP, et al. Novel algorithm for non-invasive assessment of fibrosis in NAFLD. PLoS One 2013;8:e62439.
61. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120 Suppl 4:S164–192.
62. Woolford SJ, Sallinen BJ, Clark SJ, Freed GL. Results from a clinical multidisciplinary weight management program. Clin Pediatrics 2011;50:187–91.
63. Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA 2007;297:2697–704.
64. Woolford SJ, Clark SJ, Gebremariam A, et al. Physicians’ perspectives on referring obese adolescents to pediatric multidisciplinary weight management programs. Clin Pediatrics 2010;49:871–5.
65. Lipana LS, Bindal D, Nettiksimmons J, Shaikh U. Telemedicine and face-to-face care for pediatric obesity. Telemed J Ehealth 2013;19:806–8.
66. Park MH, Kinra S, Ward KJ, et al. Metformin for obesity in children and adolescents: a systematic review. Diabetes Care 2009;32:1743–5.
67. Urrutia-Rojas X, McConathy W, Willis B, et al. Abnormal glucose metabolism in Hispanic parents of children with acanthosis nigricans. ISRN Endocrinol 2011(Epub 2011 Dec 25.).
1. CDC. Obesity task force report. 2010. Available at www.letsmove.gov/sites/letsmove.gov/files/TaskForce_on_Childhood_Obesity_May2010_FullReport.pdf. Accessed 4 Sept 2013.
2. Barlow SE, AAP Expert Committee. AAP Expert Committee Recommendations regarding prevention, assessment and treatment of child obesity. Pediatrics 2007;120:s164–92.
3. Dietz WH, Robinson TN. Overweight children and adolescents. N Engl J Med 2005;352:2100–9.
4. Centers for Disease Control and Prevention (CDC) 2012; Overweight and obesity. Available at www.cdc.gov/obesity/childhood/basics.html. Accessed 3 Sept 2013.
5. Centers for Disease Control and Prevention (CDC). Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2009–2010. Available at www.cdc.gov/nchs/data/hestat/obesity_child_09_10/obesity_child_09_10.pdf.
6. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–90.
7. August GP, Caprio S, Fennoy I, et al; Endocrine Society. Prevention and treatment of pediatric obesity: an endocrine society clinical practice guideline based on expert opinion. J Clin Endocrinol Metab 2008;93:4576–99.
8. Holmes ME, Eisenmann JC, Ekkekakis P, Gentile D. Physical activity, stress, and metabolic risk score in 8- to 18-year-old boys. J Phys Act Health 2008;5:294–307.
9. Peeters A, Barendregt JJ, Willekens F, et al. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 2003;138:24–32.
10. Sharifi M, Marshall G, Marshall R, et al. Accelerating progress in reducing childhood obesity disparities: exploring best practices of positive outliers. J Health Care Poor Underserved 2013;24(2 Suppl):193–9.
11. Cossrow N, Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. J Clin Endocrinol Metab 2004;89:2590–4.
12. Rosenbaum M, Fennoy I, Accacha S, et al. Racial/ethnic differences in clinical and biochemical type 2 diabetes mellitus risk factors in children. Obesity (Silver Spring) 2013;21:2081–90.
13. NIDDK. National diabetes statistics, 2011. Available at http://diabetes.niddk.nih.gov/dm/pubs/statistics/. Accessed 18 Sept 2013.
14. Janz KF, Butner KL, Pate RR. The role of pediatricians in increasing physical activity in youth. JAMA Pediatr 2013:1–2.
15. Coleman KJ, Hsii AC, Koebnick C, et al. Implementation of clinical practice guidelines for pediatric weight management. J Pediatrics 2012;160:918–22.
16. Ratcliff MB, Jenkins TM, Reiter-Purtill J, et al. Risk-taking behaviors of adolescents with extreme obesity: normative or not? Pediatrics 2011;127:827–34.
17. Goldenring J, Rosen D. Getting into adolescent heads: An essential update. Contemp Pediatr 2004;21:64.
18. Eisenmann JC, Welk GJ, Ihmels M, Dollman J. Fatness, fitness, and cardiovascular disease risk factors in children and adolescents. Med Sci Sports Exerc 2007;39:1251–6.
19. Weiss R, Shaw M, Savoye M, Caprio S. Obesity dynamics and cardiovascular risk factor stability in obese adolescents. Ped Diabetes 2009;10:360–7.
20. Rizzo NS, Ruiz JR, Ortega FB, Sjostrom M. Relationship of physical activity, fitness, and fatness with clustered metabolic risk in children and adolescents: The European Youth Heart Study. J Pediatr 2007;150:388–94.
21. Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics 2002;110(1 Pt 2):210–4.
22. Alexander SC, Ostbye T, Pollak KI, et al. Physicians’ beliefs about discussing obesity: results from focus groups. Am J Health Promot 2007;21:498–500.
23. Puhl RM, Peterson JL, Luedicke J. Weight-based victimization: bullying experiences of weight loss treatment-seeking youth. Pediatrics 2013;131:e1–9.
24. Christie D, Channon S. The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: a clinical review. Diabetes Obes Metab 2013. Aug 8 [Epub ahead of print].
25. Standards of medical care in diabetes--2010. Diabetes Care 2010;33 Suppl 1:S11–61.
26. Hasson RE, Adam TC, Davis JN, et al. Ethnic differences in insulin action in obese African-American and Latino adolescents. J Clin Endocrinol Metab 2010;95:4048–51.
27. Fernández JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatrics 2004;145:439–44.
28. Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics 2009;124 Suppl 1:S23–34.
29. Daniels SR, Khoury PR, Morrison JA. The utility of body mass index as a measure of body fatness in children and adolescents: differences by race and gender. Pediatrics 1997;99:804–7.
30. Curtis VA, Carrel AL, Eickhoff JC, Allen DB. Gender and race influence metabolic benefits of fitness in children: a cross-sectional study. Int J Pediatr Endocrinol 2012;2012:4.
31. Nightingale CM, Rudnicka AR, Owen CG, et al. Influence of adiposity on insulin resistance and glycemia markers among U.K. Children of South Asian, black African-Caribbean, and white European origin: child heart and health study in England. Diabetes Care 2013;36:1712–9.
32. Gutin B, Yin Z, Humphries MC, Hoffman WH, et al. Relations of fatness and fitness to fasting insulin in black and white adolescents. J Pediatr 2004;145:737–43.
33. Cook S. The metabolic syndrome: Antecedent of adult cardiovascular disease in pediatrics. J Pediatr 2004;145:427–30.
34. Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med 2002;162:2074–9.
35. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. September 1998. NIH Pub No. 98-4083. Available at www.ncbi.nlm.nih.gov/books/NBK2003/pdf/TOC.pdf. Accessed 29 Sept 2013.
36. Janssen I, Katzmarzyk PT, Srinivasan SR, et al. Combined influence of body mass index and waist circumference on coronary artery disease risk factors among children and adolescents. Pediatrics 2005;115:1623–30.
37. Freedman DS, Serdula MK, Srinivasan SR, Berenson GS. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr 1999;69:308–17.
38. Savva SC, Tornaritis M, Savva ME, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Rel Metab Disorders 2000;24:1453–8.
39. Lee S, Bacha F, Gungor N, Arslanian SA. Waist circumference is an independent predictor of insulin resistance in black and white youths. J Pediatrics 2006;148:188–94.
40. Wang J, Thornton JC, Bari S, et al. Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutrition 2003;77:379–84.
41. Cook S, Weitzman M, Auinger P, et al. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Ped Adol Med 2003;157:821–7.
42. Ford ES, Ajani UA, Mokdad AH. The metabolic syndrome and concentrations of C-reactive protein among U.S. youth. Diabetes Care 2005;28:878–81.
43. Cruz ML, Weigensberg MJ, Huang TT, et al. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. J Clin Endocrin Metab 2004;89:108–13.
44. Lee JM, Davis MM, Woolford SJ, Gurney JG. Waist circumference percentile thresholds for identifying adolescents with insulin resistance in clinical practice. Pediatric Diabetes 2009;10:336–42.
45. Li S, Chen W, Srinivasan SR, et al. Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am J Epidemiol 2012;1:S142–9.
46. Torley D, Bellus GA, Munro CS. Genes, growth factors and acanthosis nigricans. Br J Dermatol 2002;147:1096–101.
47. Mukhtar Q, Cleverley G, Voorhees RE, McGrath JW. Prevalence of acanthosis nigricans and its association with hyperinsulinemia in New Mexico adolescents. J. Adolesc Health 2001;28:372–6.
48. Brickman WJ, Huang J, Silverman BL, Metzger BE. Acanthosis nigricans identifies youth at high risk for metabolic abnormalities. J Pediatrics 2010;156:87–92.
49. Stuart CA, Pate CJ, Peters EJ. Prevalence of acanthosis nigricans in an unselected population. Am J Med 1989;87:269–72.
50. Brickman WJ, Binns HJ, Jovanovic BD, et al. Acanthosis nigricans: a common finding in overweight youth. Pediatr Dermatol 2007;24:601–6.
51. Yang HR, Kim HR, Kim MJ, et al. Noninvasive parameters and hepatic fibrosis scores in children with nonalcoholic fatty liver disease. World J Gastroenterol 2012;18:1525–30.
52. Chiarelli F, Marcovecchio ML. Insulin resistance and obesity in childhood. Eur J Endocrinol 2008;159 Suppl 1:S67–74.
53. Adam TC, Hasson RE, Lane CJ, Goran MI. Fasting indicators of insulin sensitivity: effects of ethnicity and pubertal status. Diabetes Care 2011;34:994–9.
54. Diagnosis and classification of diabetes mellitus. Diabetes Care 2013;36 Suppl 1:S67–74.
55. Nowicka P, Santoro N, Liu H, et al. Utility of hemoglobin A(1c) for diagnosing prediabetes and diabetes in obese children and adolescents. Diabetes Care 2011;34:1306–11.
56. Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 2004;350:2362–74.
57. Martins C, Pizarro A, Aires L, et al. Fitness and metabolic syndrome in obese fatty liver children. Ann Hum Biol 2013;40:99–101.
58. Taveras EM, Gillman MW, Kleinman KP, et al. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA Pediatr 2013;167:731–8.
59. Wolfgram PM, Connor EL, Rehm JL, et al. Ethnic differences in the effects of hepatic fat deposition on insulin resistance in non-obese middle school girls. Obesity (Silver Spring) 2014;22:243–8.
60. Sowa JP, Heider D, Bechmann LP, et al. Novel algorithm for non-invasive assessment of fibrosis in NAFLD. PLoS One 2013;8:e62439.
61. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120 Suppl 4:S164–192.
62. Woolford SJ, Sallinen BJ, Clark SJ, Freed GL. Results from a clinical multidisciplinary weight management program. Clin Pediatrics 2011;50:187–91.
63. Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA 2007;297:2697–704.
64. Woolford SJ, Clark SJ, Gebremariam A, et al. Physicians’ perspectives on referring obese adolescents to pediatric multidisciplinary weight management programs. Clin Pediatrics 2010;49:871–5.
65. Lipana LS, Bindal D, Nettiksimmons J, Shaikh U. Telemedicine and face-to-face care for pediatric obesity. Telemed J Ehealth 2013;19:806–8.
66. Park MH, Kinra S, Ward KJ, et al. Metformin for obesity in children and adolescents: a systematic review. Diabetes Care 2009;32:1743–5.
67. Urrutia-Rojas X, McConathy W, Willis B, et al. Abnormal glucose metabolism in Hispanic parents of children with acanthosis nigricans. ISRN Endocrinol 2011(Epub 2011 Dec 25.).