User login
Who Consults Us and Why? An Evaluation of Medicine Consult/Comanagement Services at Academic Medical Centers
The role of internists in consultation has considerably expanded over the past half century. Consulting general internists increasingly work across disciplines to coordinate complex care.1,2 Some internists assume a “comanagement” role with surgical specialties. This role requires sharing responsibility and accountability and involvement in admission/discharge processes.3-6 Internal medicine (IM) residents are required to serve as consultants.7 Yet, aside from observations collected 30 to 40 years ago, limited information is available for guiding educators in developing consultative curricula.2,8-10 We sought to assess current consultative practices across a sample of IM training programs. Specifically, we examined which services consult IM and their reasons for consultation (RFCs).
METHODS
We collected data on consultation requests at 11 US academic medical centers (AMCs). We applied a selective sampling approach that leveraged existing relationships and interest in consultative medicine to identify institutions across a variety of geographic locations. We collected data regarding the consult service structure at each site, including data on the presence or absence of comanagement services and consult requests received.
Data Collection Tool
Investigators at the University of Texas Health San Antonio (UTHSA) drafted the data collection tool. Iterative feedback on the data collection tool was obtained from the research consortium (final tool, Supplemental Figure). Data collected included service requesting consultation, RFC, time request was made (day/night), who first saw the patient (eg, resident, attending), whether requesting and consulting providers verbally communicated, and whether patients were transferred to medicine. Respondents also estimated how often RFCs were encountered during their general medicine services.
To streamline data collection, we used click boxes and drop-down lists that included diagnoses and symptoms. The use of these predetermined RFCs was based on prior studies and discussion with the research consortium on common RFCs in clinical practice. A write-in field was also included. Respondents could select multiple RFCs in the case of multiple questions. Respondents also provided data regarding clinical issues that were incidentally identified during their initial patient assessments. Incidentally identified issues are hereafter called “additional RFCs” for differentiation from stated RFCs. Prior to data collection, the tool was piloted at UTHSA.
Data Collection, Categorization, and Analysis
Participants submitted data using Survey Monkey (Palo Alto, California). Emails with the survey link were sent daily. Specific participants for each data collection period were chosen by each site. Days with no data entry were confirmed by the study coordinator. Each institution collected data for four 2-week periods from July 2014 to July 2015 for a total of 8 weeks. We did not track follow-up encounters. Repeat consultations for different reasons were considered new consults.
All survey responses and free-text RFC entries were independently reviewed and categorized by 2 authors (E.W. and M.S.). New categories were created if needed. If reviewers disagreed, a third reviewer (C.M.) reviewed the RFC. The research consortium reviewed the final list of categories and entries.
We calculated descriptive statistics using SAS version 9.3 (SAS Institute, Inc., Cary, North Carolina). Each analysis used complete responses for each survey component. We separately analyzed services with and without comanagement components. The study was approved by UTHSA’s Institutional Review Board.
RESULTS
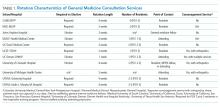
A total of 11 AMCs that represent 9 academic affiliations participated in this study (Table 1). Of the 11 AMCs, 7 were public nonprofit, 3 were private nonprofit, and 1 was a Veterans Health Administration facility. Out of the 11 AMCs, 9 sites included residents on the consult service, and the rotation was required at 6 of the sites. Most sites with residents had a formal curriculum that ranged from curated articles to online modules. Out of the 11 services, 4 were consult and comanagement services. All 4 co-managed orthopedic patients, and 1 also included other patients.
Data for 1,264 patient encounters with 2,778 RFCs were collected. A total of 1,218 of the surveys (96.4%) were fully completed, and only 5 surveys were missing data for multiple questions. A total of 7 sites adhered to the planned protocol. Among the sites, 1 site had 1 incomplete collection period, 1 site missed 1 collection period, and 1 site missed 2 collection periods.
Most consultations (87.1%) were requested during the day. Many patients (55.9%) were initially seen by residents, and 32.4% of the patients were initially seen by an attending. Respondents reported communicating verbally with the requesting team in 93.9% of instances. Among the patients, 7.8% were transferred to medicine following initial consultation. This percentage was higher (10.2%) in services without comanagement.
The average number of new consults per day per site was 2.24. The range for individual sites was 1.36-3.48. The maximum number of new consults in 1 day was 10. All sites had at least 1 day without new consults. The mean number of RFCs per encounter was 2.20 (median 2, range 1-13). In 226 of 360 encounters in which comanagement was an RFC, the respondent enumerated the other specific RFCs addressed. In these encounters, the mean number of RFCs (in addition to comanagement) was 3.02.
Most requests (82.2%) originated from surgical services. Among all surgical services, orthopedic surgery requested the highest number of consultations (67.5% for services with a comanagement component; 28.5% for services without) and 81.2% of the 360 comanagement encounters. Refer to Supplemental Table 1 for detailed information on the services that requested consultation.
The most common RFC was comanagement (13.0% across the entire study; 23.3% for services with a comanagement component; Table 2). For services without comanagement, preoperative evaluation was the most common RFC (16.4%). Other frequent RFCs across the entire study included blood pressure management (8.9%), glycemic management (7.2%), and renal failure (3.9%). Additional (unstated) RFCs were addressed in 944 patients (34.0%), and blood pressure management was the most common additional RFC.
Respondents indicated that 54.9% of RFCs were clinical topics that are “often” or “always” encountered in IM inpatient services. In 11.8% of encounters, the RFC was “rarely” or “never” encountered; the most common RFCs in such encounters were comanagement (53.4%), preoperative evaluation (17.4%), and transfer to medicine (5.4%).
DISCUSSION
Our study provides insights into the consultative landscape of AMCs and identified who consults IMs and their RFCs. Thus, our study has implications for resident consultative education. The consult services included in our study presented varied structures, including those that require medicine consultation as a resident rotation and those with comanagement agreements. Consistent with the results of prior studies, surgical services requested the majority of consults, with orthopedic surgery generating the highest number of requests. Consultation requests from neurosurgery were higher than previously reported.2,8,9
Our study reveals that comanagement and preoperative evaluation are the most common RFCs and are the least commonly encountered RFCs in IM inpatient services. The broad nature of these RFCs speaks to an increasing need for comprehensive consultative care. Consultants addressed a wide range of clinical issues, including rare entities that defy easy categorization (eg, Moyamoya disease). This broad landscape presents challenges in focusing curricular content areas outside of comanagement and preoperative evaluation but does provide evidence “to expect the unexpected” in IM consultation, as has been previously noted.8
In over a third of encounters, consultants addressed an issue that was not stated in the initial RFC. Consultants also addressed more than 2 RFCs per encounter. These observations suggest that medicine consult services may be essentially comanaging some patients even when a comanagement care model is not formally in place. These findings provide rationale for the continued expansion of comanagement services.11
Our study provides further evidence that, in modern consultative practice, “determining your customer” is more important than “determining the question.”12-14 We work in an era in which comanagement services are increasingly prevalent but are not ubiquitous and in which IM consultants routinely address multiple issues. Prior studies indicated that most surgeons do not believe that consults should be limited to specific questions and instead prefer comanagement.13 Understanding the expectations of the requesting physician is therefore important and highlights the importance of verbal communication at the time of initial consultation. Ongoing interprofessional communication is a vital skill that residents should acquire.
Our study has several limitations. Although our sites represented a varied sample, we focused on AMCs. Therefore, our study may not reflect consultative experiences in nonacademic hospitals or sites without dedicated consult services. Trade-offs exist in our data collection approach, which provided predetermined RFCs. We selected our methodology to facilitate data entry and to aid RFC categorization. Nevertheless, it may have lessened the clinical nuance of submitted data. The provision of predetermined RFCs may have influenced issue selection by the respondents. However, in 473 encounters (37.4%), the survey respondents provided free-text entries for the stated RFC, and 944 additional RFCs were written in as responses. These results demonstrated that respondents did not limit themselves to the predetermined list. We did not perform chart reviews to validate data. Finally, our data were a cross-section of initial consultations. We lack information on subsequent diagnoses or additional clinical issues that developed later.
In conclusion, we found varied consultative experiences across AMCs. However, preoperative evaluation and perioperative comanagement – particularly of orthopedic and neurosurgical patients – were common and should be included in curricula. Faculty should recognize the unique nature of IM consultation to prepare residents. Specifically, faculty should prepare residents to expect to identify and address unstated medical issues and to provide comprehensive assessments regardless of whether the consultative structure has a comanagement component. Given the unique nature of consultative IM work and the possibility of discordant expectations between consulting and requesting physicians, perhaps the most valuable skill to impart to residents is effective and regular communication.
Medicine Consult/Comanagement Consortium Members
The Medicine Consult/Comanagement Consortium consists of: Mary Anderson Wallace, MD, Brian Wolfe, MD (University of Colorado), Meridale Baggett, MD, Douglas Wright, MD, PhD (Harvard University), Joyeeta G. Dastidar MD, Maureen Kelly, MD (Columbia University), Leonard S. Feldman, MD (Johns Hopkins University), Cecily J. Gallup, MD, MPH (University of California, San Francisco), Paul J. Grant, MD (University of Michigan), Craig R. Keenan, MD (University of California, Davis), Fletcher Penney, MD (Medical University of South Carolina).
Acknowledgments
The authors thank the clinicians at each site who were involved in data collection for this study, including Barbara Statland, MD. The authors also thank Timothy Niessen, MD for data and physician coordination and Musarrat Nahid, MSc. for statistical analysis.
Disclosures
Paul J. Grant receives royalties from the medical textbook Perioperative Medicine: Medical Consultation and Comanagement, Wiley Publishing 2012. Craig R. Keenan receives medicolegal consultation fees from Weiss-Salinas Law Group and American Psychiatric Association Publishers for book royalties. All other authors declare that they do not have any conflicts of interest.
Funding Information
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration. Investigator salary support is provided through the South Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or our institutions.
1. Hollenberg CH, Langley GR. The Canadian general internist: education and future role. CMAJ. 1978;118(4):397-400. PubMed
2. Charlson ME, Cohen RP, Sears CL. General medicine consultation: lessons from a clinical service. Am J Med. 1983;75(1):121-128. https://doi.org/10.1016/0002-9343(83)91175-0. PubMed
3. Society of Hospital Medicine. The evolution of co-management in hospital medicine. http://www.hospitalmedicine.org/Web/Practice_Management/CoManagement.aspx. Accessed March 8, 2018.
4. Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010. 10.1001/archinternmed.2010.432. PubMed
5. Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368. 10.1001/archinternmed.2009.553. PubMed
6. Thompson RE, Pfeifer K, Grant PJ, et al. Hospital medicine and perioperative care: a framework for high-quality, high-value collaborative care. J Hosp Med. 2017;12(4):277-282. 10.12788/jhm.2717. PubMed
7. Accreditation Council for Graduate Medical Education. Common Program Requirements. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/140_internal_medicine_2017-07-01.pdf. Accessed March 8, 2018.
8. Moore RA, Kammerer WS, McGlynn TJ, Trautlein JJ, Burnside JW. Consultations in internal medicine: a training program resource. J Med Educ. 1977;52(4):323-327. PubMed
9. Robie PW. The service and educational contributions of a general medicine consultation service. J Gen Intern Med. 1986;1(4):225-227. https://doi.org/10.1007/BF02596187. PubMed
10. Devor M, Renvall M, Ramsdell J. Practice patterns and the adequacy of residency training in consultation medicine. J Gen Intern Med. 1993;8(10):554-560. 10.1007/BF02599639. PubMed
11. Siegal EM. Just because you can, doesn’t mean that you should: a call for the rational application of hospitalist comanagement. J Hosp Med. 2008;3(5):398-402. 10.1002/jhm.361. PubMed
12. Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143(9):1753-1755. 10.1001/archinte.1983.00350090131022. PubMed
13. Salerno SM. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007;167:271-275. 10.1001/archinte.167.3.271. PubMed
14. Merli GJ, Weitz HH. Medical management of the surgical patient E-Book. Elsevier Health Sciences; 2008. PubMed
The role of internists in consultation has considerably expanded over the past half century. Consulting general internists increasingly work across disciplines to coordinate complex care.1,2 Some internists assume a “comanagement” role with surgical specialties. This role requires sharing responsibility and accountability and involvement in admission/discharge processes.3-6 Internal medicine (IM) residents are required to serve as consultants.7 Yet, aside from observations collected 30 to 40 years ago, limited information is available for guiding educators in developing consultative curricula.2,8-10 We sought to assess current consultative practices across a sample of IM training programs. Specifically, we examined which services consult IM and their reasons for consultation (RFCs).
METHODS
We collected data on consultation requests at 11 US academic medical centers (AMCs). We applied a selective sampling approach that leveraged existing relationships and interest in consultative medicine to identify institutions across a variety of geographic locations. We collected data regarding the consult service structure at each site, including data on the presence or absence of comanagement services and consult requests received.
Data Collection Tool
Investigators at the University of Texas Health San Antonio (UTHSA) drafted the data collection tool. Iterative feedback on the data collection tool was obtained from the research consortium (final tool, Supplemental Figure). Data collected included service requesting consultation, RFC, time request was made (day/night), who first saw the patient (eg, resident, attending), whether requesting and consulting providers verbally communicated, and whether patients were transferred to medicine. Respondents also estimated how often RFCs were encountered during their general medicine services.
To streamline data collection, we used click boxes and drop-down lists that included diagnoses and symptoms. The use of these predetermined RFCs was based on prior studies and discussion with the research consortium on common RFCs in clinical practice. A write-in field was also included. Respondents could select multiple RFCs in the case of multiple questions. Respondents also provided data regarding clinical issues that were incidentally identified during their initial patient assessments. Incidentally identified issues are hereafter called “additional RFCs” for differentiation from stated RFCs. Prior to data collection, the tool was piloted at UTHSA.
Data Collection, Categorization, and Analysis
Participants submitted data using Survey Monkey (Palo Alto, California). Emails with the survey link were sent daily. Specific participants for each data collection period were chosen by each site. Days with no data entry were confirmed by the study coordinator. Each institution collected data for four 2-week periods from July 2014 to July 2015 for a total of 8 weeks. We did not track follow-up encounters. Repeat consultations for different reasons were considered new consults.
All survey responses and free-text RFC entries were independently reviewed and categorized by 2 authors (E.W. and M.S.). New categories were created if needed. If reviewers disagreed, a third reviewer (C.M.) reviewed the RFC. The research consortium reviewed the final list of categories and entries.
We calculated descriptive statistics using SAS version 9.3 (SAS Institute, Inc., Cary, North Carolina). Each analysis used complete responses for each survey component. We separately analyzed services with and without comanagement components. The study was approved by UTHSA’s Institutional Review Board.
RESULTS
A total of 11 AMCs that represent 9 academic affiliations participated in this study (Table 1). Of the 11 AMCs, 7 were public nonprofit, 3 were private nonprofit, and 1 was a Veterans Health Administration facility. Out of the 11 AMCs, 9 sites included residents on the consult service, and the rotation was required at 6 of the sites. Most sites with residents had a formal curriculum that ranged from curated articles to online modules. Out of the 11 services, 4 were consult and comanagement services. All 4 co-managed orthopedic patients, and 1 also included other patients.
Data for 1,264 patient encounters with 2,778 RFCs were collected. A total of 1,218 of the surveys (96.4%) were fully completed, and only 5 surveys were missing data for multiple questions. A total of 7 sites adhered to the planned protocol. Among the sites, 1 site had 1 incomplete collection period, 1 site missed 1 collection period, and 1 site missed 2 collection periods.
Most consultations (87.1%) were requested during the day. Many patients (55.9%) were initially seen by residents, and 32.4% of the patients were initially seen by an attending. Respondents reported communicating verbally with the requesting team in 93.9% of instances. Among the patients, 7.8% were transferred to medicine following initial consultation. This percentage was higher (10.2%) in services without comanagement.
The average number of new consults per day per site was 2.24. The range for individual sites was 1.36-3.48. The maximum number of new consults in 1 day was 10. All sites had at least 1 day without new consults. The mean number of RFCs per encounter was 2.20 (median 2, range 1-13). In 226 of 360 encounters in which comanagement was an RFC, the respondent enumerated the other specific RFCs addressed. In these encounters, the mean number of RFCs (in addition to comanagement) was 3.02.
Most requests (82.2%) originated from surgical services. Among all surgical services, orthopedic surgery requested the highest number of consultations (67.5% for services with a comanagement component; 28.5% for services without) and 81.2% of the 360 comanagement encounters. Refer to Supplemental Table 1 for detailed information on the services that requested consultation.
The most common RFC was comanagement (13.0% across the entire study; 23.3% for services with a comanagement component; Table 2). For services without comanagement, preoperative evaluation was the most common RFC (16.4%). Other frequent RFCs across the entire study included blood pressure management (8.9%), glycemic management (7.2%), and renal failure (3.9%). Additional (unstated) RFCs were addressed in 944 patients (34.0%), and blood pressure management was the most common additional RFC.
Respondents indicated that 54.9% of RFCs were clinical topics that are “often” or “always” encountered in IM inpatient services. In 11.8% of encounters, the RFC was “rarely” or “never” encountered; the most common RFCs in such encounters were comanagement (53.4%), preoperative evaluation (17.4%), and transfer to medicine (5.4%).
DISCUSSION
Our study provides insights into the consultative landscape of AMCs and identified who consults IMs and their RFCs. Thus, our study has implications for resident consultative education. The consult services included in our study presented varied structures, including those that require medicine consultation as a resident rotation and those with comanagement agreements. Consistent with the results of prior studies, surgical services requested the majority of consults, with orthopedic surgery generating the highest number of requests. Consultation requests from neurosurgery were higher than previously reported.2,8,9
Our study reveals that comanagement and preoperative evaluation are the most common RFCs and are the least commonly encountered RFCs in IM inpatient services. The broad nature of these RFCs speaks to an increasing need for comprehensive consultative care. Consultants addressed a wide range of clinical issues, including rare entities that defy easy categorization (eg, Moyamoya disease). This broad landscape presents challenges in focusing curricular content areas outside of comanagement and preoperative evaluation but does provide evidence “to expect the unexpected” in IM consultation, as has been previously noted.8
In over a third of encounters, consultants addressed an issue that was not stated in the initial RFC. Consultants also addressed more than 2 RFCs per encounter. These observations suggest that medicine consult services may be essentially comanaging some patients even when a comanagement care model is not formally in place. These findings provide rationale for the continued expansion of comanagement services.11
Our study provides further evidence that, in modern consultative practice, “determining your customer” is more important than “determining the question.”12-14 We work in an era in which comanagement services are increasingly prevalent but are not ubiquitous and in which IM consultants routinely address multiple issues. Prior studies indicated that most surgeons do not believe that consults should be limited to specific questions and instead prefer comanagement.13 Understanding the expectations of the requesting physician is therefore important and highlights the importance of verbal communication at the time of initial consultation. Ongoing interprofessional communication is a vital skill that residents should acquire.
Our study has several limitations. Although our sites represented a varied sample, we focused on AMCs. Therefore, our study may not reflect consultative experiences in nonacademic hospitals or sites without dedicated consult services. Trade-offs exist in our data collection approach, which provided predetermined RFCs. We selected our methodology to facilitate data entry and to aid RFC categorization. Nevertheless, it may have lessened the clinical nuance of submitted data. The provision of predetermined RFCs may have influenced issue selection by the respondents. However, in 473 encounters (37.4%), the survey respondents provided free-text entries for the stated RFC, and 944 additional RFCs were written in as responses. These results demonstrated that respondents did not limit themselves to the predetermined list. We did not perform chart reviews to validate data. Finally, our data were a cross-section of initial consultations. We lack information on subsequent diagnoses or additional clinical issues that developed later.
In conclusion, we found varied consultative experiences across AMCs. However, preoperative evaluation and perioperative comanagement – particularly of orthopedic and neurosurgical patients – were common and should be included in curricula. Faculty should recognize the unique nature of IM consultation to prepare residents. Specifically, faculty should prepare residents to expect to identify and address unstated medical issues and to provide comprehensive assessments regardless of whether the consultative structure has a comanagement component. Given the unique nature of consultative IM work and the possibility of discordant expectations between consulting and requesting physicians, perhaps the most valuable skill to impart to residents is effective and regular communication.
Medicine Consult/Comanagement Consortium Members
The Medicine Consult/Comanagement Consortium consists of: Mary Anderson Wallace, MD, Brian Wolfe, MD (University of Colorado), Meridale Baggett, MD, Douglas Wright, MD, PhD (Harvard University), Joyeeta G. Dastidar MD, Maureen Kelly, MD (Columbia University), Leonard S. Feldman, MD (Johns Hopkins University), Cecily J. Gallup, MD, MPH (University of California, San Francisco), Paul J. Grant, MD (University of Michigan), Craig R. Keenan, MD (University of California, Davis), Fletcher Penney, MD (Medical University of South Carolina).
Acknowledgments
The authors thank the clinicians at each site who were involved in data collection for this study, including Barbara Statland, MD. The authors also thank Timothy Niessen, MD for data and physician coordination and Musarrat Nahid, MSc. for statistical analysis.
Disclosures
Paul J. Grant receives royalties from the medical textbook Perioperative Medicine: Medical Consultation and Comanagement, Wiley Publishing 2012. Craig R. Keenan receives medicolegal consultation fees from Weiss-Salinas Law Group and American Psychiatric Association Publishers for book royalties. All other authors declare that they do not have any conflicts of interest.
Funding Information
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration. Investigator salary support is provided through the South Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or our institutions.
The role of internists in consultation has considerably expanded over the past half century. Consulting general internists increasingly work across disciplines to coordinate complex care.1,2 Some internists assume a “comanagement” role with surgical specialties. This role requires sharing responsibility and accountability and involvement in admission/discharge processes.3-6 Internal medicine (IM) residents are required to serve as consultants.7 Yet, aside from observations collected 30 to 40 years ago, limited information is available for guiding educators in developing consultative curricula.2,8-10 We sought to assess current consultative practices across a sample of IM training programs. Specifically, we examined which services consult IM and their reasons for consultation (RFCs).
METHODS
We collected data on consultation requests at 11 US academic medical centers (AMCs). We applied a selective sampling approach that leveraged existing relationships and interest in consultative medicine to identify institutions across a variety of geographic locations. We collected data regarding the consult service structure at each site, including data on the presence or absence of comanagement services and consult requests received.
Data Collection Tool
Investigators at the University of Texas Health San Antonio (UTHSA) drafted the data collection tool. Iterative feedback on the data collection tool was obtained from the research consortium (final tool, Supplemental Figure). Data collected included service requesting consultation, RFC, time request was made (day/night), who first saw the patient (eg, resident, attending), whether requesting and consulting providers verbally communicated, and whether patients were transferred to medicine. Respondents also estimated how often RFCs were encountered during their general medicine services.
To streamline data collection, we used click boxes and drop-down lists that included diagnoses and symptoms. The use of these predetermined RFCs was based on prior studies and discussion with the research consortium on common RFCs in clinical practice. A write-in field was also included. Respondents could select multiple RFCs in the case of multiple questions. Respondents also provided data regarding clinical issues that were incidentally identified during their initial patient assessments. Incidentally identified issues are hereafter called “additional RFCs” for differentiation from stated RFCs. Prior to data collection, the tool was piloted at UTHSA.
Data Collection, Categorization, and Analysis
Participants submitted data using Survey Monkey (Palo Alto, California). Emails with the survey link were sent daily. Specific participants for each data collection period were chosen by each site. Days with no data entry were confirmed by the study coordinator. Each institution collected data for four 2-week periods from July 2014 to July 2015 for a total of 8 weeks. We did not track follow-up encounters. Repeat consultations for different reasons were considered new consults.
All survey responses and free-text RFC entries were independently reviewed and categorized by 2 authors (E.W. and M.S.). New categories were created if needed. If reviewers disagreed, a third reviewer (C.M.) reviewed the RFC. The research consortium reviewed the final list of categories and entries.
We calculated descriptive statistics using SAS version 9.3 (SAS Institute, Inc., Cary, North Carolina). Each analysis used complete responses for each survey component. We separately analyzed services with and without comanagement components. The study was approved by UTHSA’s Institutional Review Board.
RESULTS
A total of 11 AMCs that represent 9 academic affiliations participated in this study (Table 1). Of the 11 AMCs, 7 were public nonprofit, 3 were private nonprofit, and 1 was a Veterans Health Administration facility. Out of the 11 AMCs, 9 sites included residents on the consult service, and the rotation was required at 6 of the sites. Most sites with residents had a formal curriculum that ranged from curated articles to online modules. Out of the 11 services, 4 were consult and comanagement services. All 4 co-managed orthopedic patients, and 1 also included other patients.
Data for 1,264 patient encounters with 2,778 RFCs were collected. A total of 1,218 of the surveys (96.4%) were fully completed, and only 5 surveys were missing data for multiple questions. A total of 7 sites adhered to the planned protocol. Among the sites, 1 site had 1 incomplete collection period, 1 site missed 1 collection period, and 1 site missed 2 collection periods.
Most consultations (87.1%) were requested during the day. Many patients (55.9%) were initially seen by residents, and 32.4% of the patients were initially seen by an attending. Respondents reported communicating verbally with the requesting team in 93.9% of instances. Among the patients, 7.8% were transferred to medicine following initial consultation. This percentage was higher (10.2%) in services without comanagement.
The average number of new consults per day per site was 2.24. The range for individual sites was 1.36-3.48. The maximum number of new consults in 1 day was 10. All sites had at least 1 day without new consults. The mean number of RFCs per encounter was 2.20 (median 2, range 1-13). In 226 of 360 encounters in which comanagement was an RFC, the respondent enumerated the other specific RFCs addressed. In these encounters, the mean number of RFCs (in addition to comanagement) was 3.02.
Most requests (82.2%) originated from surgical services. Among all surgical services, orthopedic surgery requested the highest number of consultations (67.5% for services with a comanagement component; 28.5% for services without) and 81.2% of the 360 comanagement encounters. Refer to Supplemental Table 1 for detailed information on the services that requested consultation.
The most common RFC was comanagement (13.0% across the entire study; 23.3% for services with a comanagement component; Table 2). For services without comanagement, preoperative evaluation was the most common RFC (16.4%). Other frequent RFCs across the entire study included blood pressure management (8.9%), glycemic management (7.2%), and renal failure (3.9%). Additional (unstated) RFCs were addressed in 944 patients (34.0%), and blood pressure management was the most common additional RFC.
Respondents indicated that 54.9% of RFCs were clinical topics that are “often” or “always” encountered in IM inpatient services. In 11.8% of encounters, the RFC was “rarely” or “never” encountered; the most common RFCs in such encounters were comanagement (53.4%), preoperative evaluation (17.4%), and transfer to medicine (5.4%).
DISCUSSION
Our study provides insights into the consultative landscape of AMCs and identified who consults IMs and their RFCs. Thus, our study has implications for resident consultative education. The consult services included in our study presented varied structures, including those that require medicine consultation as a resident rotation and those with comanagement agreements. Consistent with the results of prior studies, surgical services requested the majority of consults, with orthopedic surgery generating the highest number of requests. Consultation requests from neurosurgery were higher than previously reported.2,8,9
Our study reveals that comanagement and preoperative evaluation are the most common RFCs and are the least commonly encountered RFCs in IM inpatient services. The broad nature of these RFCs speaks to an increasing need for comprehensive consultative care. Consultants addressed a wide range of clinical issues, including rare entities that defy easy categorization (eg, Moyamoya disease). This broad landscape presents challenges in focusing curricular content areas outside of comanagement and preoperative evaluation but does provide evidence “to expect the unexpected” in IM consultation, as has been previously noted.8
In over a third of encounters, consultants addressed an issue that was not stated in the initial RFC. Consultants also addressed more than 2 RFCs per encounter. These observations suggest that medicine consult services may be essentially comanaging some patients even when a comanagement care model is not formally in place. These findings provide rationale for the continued expansion of comanagement services.11
Our study provides further evidence that, in modern consultative practice, “determining your customer” is more important than “determining the question.”12-14 We work in an era in which comanagement services are increasingly prevalent but are not ubiquitous and in which IM consultants routinely address multiple issues. Prior studies indicated that most surgeons do not believe that consults should be limited to specific questions and instead prefer comanagement.13 Understanding the expectations of the requesting physician is therefore important and highlights the importance of verbal communication at the time of initial consultation. Ongoing interprofessional communication is a vital skill that residents should acquire.
Our study has several limitations. Although our sites represented a varied sample, we focused on AMCs. Therefore, our study may not reflect consultative experiences in nonacademic hospitals or sites without dedicated consult services. Trade-offs exist in our data collection approach, which provided predetermined RFCs. We selected our methodology to facilitate data entry and to aid RFC categorization. Nevertheless, it may have lessened the clinical nuance of submitted data. The provision of predetermined RFCs may have influenced issue selection by the respondents. However, in 473 encounters (37.4%), the survey respondents provided free-text entries for the stated RFC, and 944 additional RFCs were written in as responses. These results demonstrated that respondents did not limit themselves to the predetermined list. We did not perform chart reviews to validate data. Finally, our data were a cross-section of initial consultations. We lack information on subsequent diagnoses or additional clinical issues that developed later.
In conclusion, we found varied consultative experiences across AMCs. However, preoperative evaluation and perioperative comanagement – particularly of orthopedic and neurosurgical patients – were common and should be included in curricula. Faculty should recognize the unique nature of IM consultation to prepare residents. Specifically, faculty should prepare residents to expect to identify and address unstated medical issues and to provide comprehensive assessments regardless of whether the consultative structure has a comanagement component. Given the unique nature of consultative IM work and the possibility of discordant expectations between consulting and requesting physicians, perhaps the most valuable skill to impart to residents is effective and regular communication.
Medicine Consult/Comanagement Consortium Members
The Medicine Consult/Comanagement Consortium consists of: Mary Anderson Wallace, MD, Brian Wolfe, MD (University of Colorado), Meridale Baggett, MD, Douglas Wright, MD, PhD (Harvard University), Joyeeta G. Dastidar MD, Maureen Kelly, MD (Columbia University), Leonard S. Feldman, MD (Johns Hopkins University), Cecily J. Gallup, MD, MPH (University of California, San Francisco), Paul J. Grant, MD (University of Michigan), Craig R. Keenan, MD (University of California, Davis), Fletcher Penney, MD (Medical University of South Carolina).
Acknowledgments
The authors thank the clinicians at each site who were involved in data collection for this study, including Barbara Statland, MD. The authors also thank Timothy Niessen, MD for data and physician coordination and Musarrat Nahid, MSc. for statistical analysis.
Disclosures
Paul J. Grant receives royalties from the medical textbook Perioperative Medicine: Medical Consultation and Comanagement, Wiley Publishing 2012. Craig R. Keenan receives medicolegal consultation fees from Weiss-Salinas Law Group and American Psychiatric Association Publishers for book royalties. All other authors declare that they do not have any conflicts of interest.
Funding Information
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration. Investigator salary support is provided through the South Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or our institutions.
1. Hollenberg CH, Langley GR. The Canadian general internist: education and future role. CMAJ. 1978;118(4):397-400. PubMed
2. Charlson ME, Cohen RP, Sears CL. General medicine consultation: lessons from a clinical service. Am J Med. 1983;75(1):121-128. https://doi.org/10.1016/0002-9343(83)91175-0. PubMed
3. Society of Hospital Medicine. The evolution of co-management in hospital medicine. http://www.hospitalmedicine.org/Web/Practice_Management/CoManagement.aspx. Accessed March 8, 2018.
4. Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010. 10.1001/archinternmed.2010.432. PubMed
5. Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368. 10.1001/archinternmed.2009.553. PubMed
6. Thompson RE, Pfeifer K, Grant PJ, et al. Hospital medicine and perioperative care: a framework for high-quality, high-value collaborative care. J Hosp Med. 2017;12(4):277-282. 10.12788/jhm.2717. PubMed
7. Accreditation Council for Graduate Medical Education. Common Program Requirements. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/140_internal_medicine_2017-07-01.pdf. Accessed March 8, 2018.
8. Moore RA, Kammerer WS, McGlynn TJ, Trautlein JJ, Burnside JW. Consultations in internal medicine: a training program resource. J Med Educ. 1977;52(4):323-327. PubMed
9. Robie PW. The service and educational contributions of a general medicine consultation service. J Gen Intern Med. 1986;1(4):225-227. https://doi.org/10.1007/BF02596187. PubMed
10. Devor M, Renvall M, Ramsdell J. Practice patterns and the adequacy of residency training in consultation medicine. J Gen Intern Med. 1993;8(10):554-560. 10.1007/BF02599639. PubMed
11. Siegal EM. Just because you can, doesn’t mean that you should: a call for the rational application of hospitalist comanagement. J Hosp Med. 2008;3(5):398-402. 10.1002/jhm.361. PubMed
12. Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143(9):1753-1755. 10.1001/archinte.1983.00350090131022. PubMed
13. Salerno SM. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007;167:271-275. 10.1001/archinte.167.3.271. PubMed
14. Merli GJ, Weitz HH. Medical management of the surgical patient E-Book. Elsevier Health Sciences; 2008. PubMed
1. Hollenberg CH, Langley GR. The Canadian general internist: education and future role. CMAJ. 1978;118(4):397-400. PubMed
2. Charlson ME, Cohen RP, Sears CL. General medicine consultation: lessons from a clinical service. Am J Med. 1983;75(1):121-128. https://doi.org/10.1016/0002-9343(83)91175-0. PubMed
3. Society of Hospital Medicine. The evolution of co-management in hospital medicine. http://www.hospitalmedicine.org/Web/Practice_Management/CoManagement.aspx. Accessed March 8, 2018.
4. Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010. 10.1001/archinternmed.2010.432. PubMed
5. Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368. 10.1001/archinternmed.2009.553. PubMed
6. Thompson RE, Pfeifer K, Grant PJ, et al. Hospital medicine and perioperative care: a framework for high-quality, high-value collaborative care. J Hosp Med. 2017;12(4):277-282. 10.12788/jhm.2717. PubMed
7. Accreditation Council for Graduate Medical Education. Common Program Requirements. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/140_internal_medicine_2017-07-01.pdf. Accessed March 8, 2018.
8. Moore RA, Kammerer WS, McGlynn TJ, Trautlein JJ, Burnside JW. Consultations in internal medicine: a training program resource. J Med Educ. 1977;52(4):323-327. PubMed
9. Robie PW. The service and educational contributions of a general medicine consultation service. J Gen Intern Med. 1986;1(4):225-227. https://doi.org/10.1007/BF02596187. PubMed
10. Devor M, Renvall M, Ramsdell J. Practice patterns and the adequacy of residency training in consultation medicine. J Gen Intern Med. 1993;8(10):554-560. 10.1007/BF02599639. PubMed
11. Siegal EM. Just because you can, doesn’t mean that you should: a call for the rational application of hospitalist comanagement. J Hosp Med. 2008;3(5):398-402. 10.1002/jhm.361. PubMed
12. Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143(9):1753-1755. 10.1001/archinte.1983.00350090131022. PubMed
13. Salerno SM. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007;167:271-275. 10.1001/archinte.167.3.271. PubMed
14. Merli GJ, Weitz HH. Medical management of the surgical patient E-Book. Elsevier Health Sciences; 2008. PubMed
© 2018 Society of Hospital Medicine
The Frontier of Transition Medicine: A Unique Inpatient Model for Transitions of Care
The transition of care from pediatric to adult providers has drawn increased national attention to the survival of patients with chronic childhood conditions into adulthood.ttps://www.ncbi.nlm.nih.gov/books/NBK11432/ While survival outcomes have improved due to advances in care, many of these patients experience gaps in medical care when they move from pediatric to adult healthcare systems, resulting in age-inappropriate and fragmented care in adulthood.4 Many youth with chronic childhood conditions are not prepared to move into adult healthcare, and this lack of transition preparation is associated with poorer health outcomes, including elevated glycosylated hemoglobin and loss of transplanted organs.5-7 National transition efforts have largely focused on the outpatient setting and there remains a paucity of literature on inpatient transitions of care.8,9 Although transition-age patients represent a small percentage of patients at children’s hospitals, they accumulate more hospital days and have higher resource utilization compared to their pediatric cohorts.10 In this issue, Coller et al.11 characterize the current state of pediatric to adult inpatient transitions of care among general pediatric services at US children’s hospitals. Over 50% of children’s hospitals did not have a specific adult-oriented hospital identified to receive transitioning patients. Fewer than half of hospitals (38%) had an explicit inpatient transition policy. Notably only 2% of hospitals could track patient outcomes through transitions; however, 41% had systems in place to address insurance issues. Institutions with combined internal medicine-pediatric (Med-Peds) providers more frequently had inpatient transition initiatives (P = .04). It is clear from Coller et al.11 that the adoption of transition initiatives has been delayed since its introduction at the US Surgeon’s conference in 1989, and much work is needed to bridge this gap.12
Coller et al.11 spearhead establishing standardized transition programs using the multidisciplinary Six Core Elements framework and highlight effective techniques from existing inpatient transition processes.13 While we encourage providers to utilize existing partnerships in the outpatient community to bridge the gap for this at-risk population, shifting to adult care continues to be disorganized in the face of some key barriers including challenges in addressing psychosocial needs, gaps in insurance, and poor care coordination between pediatric and adult healthcare systems.4
We propose several inpatient activities to improve transitions. First, we suggest the development of an inpatient transition or Med-Peds consult service across all hospitals. The Med-Peds consult service would implement the Six Core Elements, including transition readiness, transition planning, and providing insurance and referral resources. A Med-Peds consult service has been well received at our institution as it identifies clear leaders with expertise in transition. Coller et al.11 report only 11% of children’s hospitals surveyed had transition policies that referenced inpatient transitions of care. For those institutions without Med-Peds providers, we recommend establishing a hospital-wide transition policy, and identifying hospitalists trained in transitions, with multidisciplinary approaches to staff their transition consult service.
Tracking and monitoring youth in the inpatient transition process occurred in only 2% of hospitals surveyed. We urge for automatic consults to the transition service for adult aged patients admitted to children’s hospitals. With current electronic health records (EHRs), admission order sets with built-in transition consults for adolescents and young adults would improve the identification and tracking of youths. Assuming care of a pediatric patient with multiple comorbidities can be overwhelming for providers.14 The transition consult service could alleviate some of this anxiety with clear and concise documentation using standardized, readily available transition templates. These templates would summarize the patient’s past medical history and outline current medical problems, necessary subspecialty referrals, insurance status, limitations in activities of daily living, ancillary services (including physical therapy, occupational therapy, speech therapy, transportation services), and current level of readiness and independence.
In summary, the transition of care from pediatric to adult providers is a particularly vulnerable time for young adults with chronic medical conditions, and efforts focused on inpatient transitions of medical care have overall been limited. Crucial barriers include addressing psychosocial needs, gaps in insurance, and poor communication between pediatric and adult providers.4 Coller et al.11 have identified several gaps in inpatient transitions of care as well as multiple areas of focus to improve the patient experience. Based on the findings of this study, we urge children’s hospitals caring for adult patients to identify transition leaders, partner with an adult hospital to foster effective transitions, and to protocolize inpatient and outpatient models of transition. Perhaps the most concerning finding of this study was the widespread inability to track transition outcomes. Our group’s experience has led us to believe that coupling an inpatient transition consult team with EHR-based interventions to identify patients and follow outcomes has the most potential to improve inpatient transitions of care from pediatric to adult providers.
Disclosure
The authors have no conflicts of interests or financial disclosures.
1. Elborn JS, Shale DJ, Britton JR. Cystic fibrosis: current survival and population estimates to the year 2000. Thorax. 1991;46(12):881-885.
2. Reid GJ, Webb GD, Barzel M, McCrindle BW, Irvine MJ, Siu SC. Estimates of life expectancy by adolescents and young adults with congenital heart disease. J Am Coll Cardiol. 2006;48(2):349-355. doi:10.1016/j.jacc.2006.03.041.
3. Ferris ME, Gipson DS, Kimmel PL, Eggers PW. Trends in treatment and outcomes of survival of adolescents initiating end-stage renal disease care in the United States of America. Pediatr Nephrol. 2006;21(7):1020-1026. doi:10.1007/s00467-006-0059-9.
4. Sharma N, O’Hare K, Antonelli RC, Sawicki GS. Transition care: future directions in education, health policy, and outcomes research. Acad Pediatr. 2014;14(2):120-127. doi:10.1016/j.acap.2013.11.007.
5. Harden PN, Walsh G, Bandler N, et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ. 2012;344:e3718. doi:10.1136/bmj.e3718.
6. Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol. 2000;14(6):469-472.
7. Lotstein DS, Seid M, Klingensmith G, et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131(4):e1062-1070. doi:10.1542/peds.2012-1450.
8. Scal P. Transition for youth with chronic conditions: primary care physicians’ approaches. Pediatrics. 2002;110(6 Pt 2):1315-1321.
9. Kelly AM, Kratz B, Bielski M, Rinehart PM. Implementing transitions for youth with complex chronic conditions using the medical home model. Pediatrics. 2002;110(6 Pt 2):1322-1327.
10. Goodman DM, Hall M, Levin A, et al. Adults with chronic health conditions originating in childhood: inpatient experience in children’s hospitals. Pediatrics. 2011;128(1):5-13. doi:10.1542/peds.2010-2037.
11. Coller RJ, Ahrens S, Ehlenbach M, et al. Transitioning from General Pediatric to Adult-Oriented Inpatient Care: National Survey of US Children’s Hospitals. J Hosp Med. 2018;13(1):13-20.
12. Olson D. Health Care Transitions for Young People. In Field MJ, Jette AM, Institute of Medicine (US) Committee on Disability in America, editors. The Future of Disability in America. Washington, DC: National Academy Press; 2007. https://www.ncbi.nlm.nih.gov/books/NBK11432/.
13. GotTransition.org. http://www.gottransition.org/. Accessed September 15, 2017.
14. Okumura MJ, Kerr EA, Cabana MD, Davis MM, Demonner S, Heisler M. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics. 2010;125(4):e748-754. doi:10.1542/peds.2008-3451.
The transition of care from pediatric to adult providers has drawn increased national attention to the survival of patients with chronic childhood conditions into adulthood.ttps://www.ncbi.nlm.nih.gov/books/NBK11432/ While survival outcomes have improved due to advances in care, many of these patients experience gaps in medical care when they move from pediatric to adult healthcare systems, resulting in age-inappropriate and fragmented care in adulthood.4 Many youth with chronic childhood conditions are not prepared to move into adult healthcare, and this lack of transition preparation is associated with poorer health outcomes, including elevated glycosylated hemoglobin and loss of transplanted organs.5-7 National transition efforts have largely focused on the outpatient setting and there remains a paucity of literature on inpatient transitions of care.8,9 Although transition-age patients represent a small percentage of patients at children’s hospitals, they accumulate more hospital days and have higher resource utilization compared to their pediatric cohorts.10 In this issue, Coller et al.11 characterize the current state of pediatric to adult inpatient transitions of care among general pediatric services at US children’s hospitals. Over 50% of children’s hospitals did not have a specific adult-oriented hospital identified to receive transitioning patients. Fewer than half of hospitals (38%) had an explicit inpatient transition policy. Notably only 2% of hospitals could track patient outcomes through transitions; however, 41% had systems in place to address insurance issues. Institutions with combined internal medicine-pediatric (Med-Peds) providers more frequently had inpatient transition initiatives (P = .04). It is clear from Coller et al.11 that the adoption of transition initiatives has been delayed since its introduction at the US Surgeon’s conference in 1989, and much work is needed to bridge this gap.12
Coller et al.11 spearhead establishing standardized transition programs using the multidisciplinary Six Core Elements framework and highlight effective techniques from existing inpatient transition processes.13 While we encourage providers to utilize existing partnerships in the outpatient community to bridge the gap for this at-risk population, shifting to adult care continues to be disorganized in the face of some key barriers including challenges in addressing psychosocial needs, gaps in insurance, and poor care coordination between pediatric and adult healthcare systems.4
We propose several inpatient activities to improve transitions. First, we suggest the development of an inpatient transition or Med-Peds consult service across all hospitals. The Med-Peds consult service would implement the Six Core Elements, including transition readiness, transition planning, and providing insurance and referral resources. A Med-Peds consult service has been well received at our institution as it identifies clear leaders with expertise in transition. Coller et al.11 report only 11% of children’s hospitals surveyed had transition policies that referenced inpatient transitions of care. For those institutions without Med-Peds providers, we recommend establishing a hospital-wide transition policy, and identifying hospitalists trained in transitions, with multidisciplinary approaches to staff their transition consult service.
Tracking and monitoring youth in the inpatient transition process occurred in only 2% of hospitals surveyed. We urge for automatic consults to the transition service for adult aged patients admitted to children’s hospitals. With current electronic health records (EHRs), admission order sets with built-in transition consults for adolescents and young adults would improve the identification and tracking of youths. Assuming care of a pediatric patient with multiple comorbidities can be overwhelming for providers.14 The transition consult service could alleviate some of this anxiety with clear and concise documentation using standardized, readily available transition templates. These templates would summarize the patient’s past medical history and outline current medical problems, necessary subspecialty referrals, insurance status, limitations in activities of daily living, ancillary services (including physical therapy, occupational therapy, speech therapy, transportation services), and current level of readiness and independence.
In summary, the transition of care from pediatric to adult providers is a particularly vulnerable time for young adults with chronic medical conditions, and efforts focused on inpatient transitions of medical care have overall been limited. Crucial barriers include addressing psychosocial needs, gaps in insurance, and poor communication between pediatric and adult providers.4 Coller et al.11 have identified several gaps in inpatient transitions of care as well as multiple areas of focus to improve the patient experience. Based on the findings of this study, we urge children’s hospitals caring for adult patients to identify transition leaders, partner with an adult hospital to foster effective transitions, and to protocolize inpatient and outpatient models of transition. Perhaps the most concerning finding of this study was the widespread inability to track transition outcomes. Our group’s experience has led us to believe that coupling an inpatient transition consult team with EHR-based interventions to identify patients and follow outcomes has the most potential to improve inpatient transitions of care from pediatric to adult providers.
Disclosure
The authors have no conflicts of interests or financial disclosures.
The transition of care from pediatric to adult providers has drawn increased national attention to the survival of patients with chronic childhood conditions into adulthood.ttps://www.ncbi.nlm.nih.gov/books/NBK11432/ While survival outcomes have improved due to advances in care, many of these patients experience gaps in medical care when they move from pediatric to adult healthcare systems, resulting in age-inappropriate and fragmented care in adulthood.4 Many youth with chronic childhood conditions are not prepared to move into adult healthcare, and this lack of transition preparation is associated with poorer health outcomes, including elevated glycosylated hemoglobin and loss of transplanted organs.5-7 National transition efforts have largely focused on the outpatient setting and there remains a paucity of literature on inpatient transitions of care.8,9 Although transition-age patients represent a small percentage of patients at children’s hospitals, they accumulate more hospital days and have higher resource utilization compared to their pediatric cohorts.10 In this issue, Coller et al.11 characterize the current state of pediatric to adult inpatient transitions of care among general pediatric services at US children’s hospitals. Over 50% of children’s hospitals did not have a specific adult-oriented hospital identified to receive transitioning patients. Fewer than half of hospitals (38%) had an explicit inpatient transition policy. Notably only 2% of hospitals could track patient outcomes through transitions; however, 41% had systems in place to address insurance issues. Institutions with combined internal medicine-pediatric (Med-Peds) providers more frequently had inpatient transition initiatives (P = .04). It is clear from Coller et al.11 that the adoption of transition initiatives has been delayed since its introduction at the US Surgeon’s conference in 1989, and much work is needed to bridge this gap.12
Coller et al.11 spearhead establishing standardized transition programs using the multidisciplinary Six Core Elements framework and highlight effective techniques from existing inpatient transition processes.13 While we encourage providers to utilize existing partnerships in the outpatient community to bridge the gap for this at-risk population, shifting to adult care continues to be disorganized in the face of some key barriers including challenges in addressing psychosocial needs, gaps in insurance, and poor care coordination between pediatric and adult healthcare systems.4
We propose several inpatient activities to improve transitions. First, we suggest the development of an inpatient transition or Med-Peds consult service across all hospitals. The Med-Peds consult service would implement the Six Core Elements, including transition readiness, transition planning, and providing insurance and referral resources. A Med-Peds consult service has been well received at our institution as it identifies clear leaders with expertise in transition. Coller et al.11 report only 11% of children’s hospitals surveyed had transition policies that referenced inpatient transitions of care. For those institutions without Med-Peds providers, we recommend establishing a hospital-wide transition policy, and identifying hospitalists trained in transitions, with multidisciplinary approaches to staff their transition consult service.
Tracking and monitoring youth in the inpatient transition process occurred in only 2% of hospitals surveyed. We urge for automatic consults to the transition service for adult aged patients admitted to children’s hospitals. With current electronic health records (EHRs), admission order sets with built-in transition consults for adolescents and young adults would improve the identification and tracking of youths. Assuming care of a pediatric patient with multiple comorbidities can be overwhelming for providers.14 The transition consult service could alleviate some of this anxiety with clear and concise documentation using standardized, readily available transition templates. These templates would summarize the patient’s past medical history and outline current medical problems, necessary subspecialty referrals, insurance status, limitations in activities of daily living, ancillary services (including physical therapy, occupational therapy, speech therapy, transportation services), and current level of readiness and independence.
In summary, the transition of care from pediatric to adult providers is a particularly vulnerable time for young adults with chronic medical conditions, and efforts focused on inpatient transitions of medical care have overall been limited. Crucial barriers include addressing psychosocial needs, gaps in insurance, and poor communication between pediatric and adult providers.4 Coller et al.11 have identified several gaps in inpatient transitions of care as well as multiple areas of focus to improve the patient experience. Based on the findings of this study, we urge children’s hospitals caring for adult patients to identify transition leaders, partner with an adult hospital to foster effective transitions, and to protocolize inpatient and outpatient models of transition. Perhaps the most concerning finding of this study was the widespread inability to track transition outcomes. Our group’s experience has led us to believe that coupling an inpatient transition consult team with EHR-based interventions to identify patients and follow outcomes has the most potential to improve inpatient transitions of care from pediatric to adult providers.
Disclosure
The authors have no conflicts of interests or financial disclosures.
1. Elborn JS, Shale DJ, Britton JR. Cystic fibrosis: current survival and population estimates to the year 2000. Thorax. 1991;46(12):881-885.
2. Reid GJ, Webb GD, Barzel M, McCrindle BW, Irvine MJ, Siu SC. Estimates of life expectancy by adolescents and young adults with congenital heart disease. J Am Coll Cardiol. 2006;48(2):349-355. doi:10.1016/j.jacc.2006.03.041.
3. Ferris ME, Gipson DS, Kimmel PL, Eggers PW. Trends in treatment and outcomes of survival of adolescents initiating end-stage renal disease care in the United States of America. Pediatr Nephrol. 2006;21(7):1020-1026. doi:10.1007/s00467-006-0059-9.
4. Sharma N, O’Hare K, Antonelli RC, Sawicki GS. Transition care: future directions in education, health policy, and outcomes research. Acad Pediatr. 2014;14(2):120-127. doi:10.1016/j.acap.2013.11.007.
5. Harden PN, Walsh G, Bandler N, et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ. 2012;344:e3718. doi:10.1136/bmj.e3718.
6. Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol. 2000;14(6):469-472.
7. Lotstein DS, Seid M, Klingensmith G, et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131(4):e1062-1070. doi:10.1542/peds.2012-1450.
8. Scal P. Transition for youth with chronic conditions: primary care physicians’ approaches. Pediatrics. 2002;110(6 Pt 2):1315-1321.
9. Kelly AM, Kratz B, Bielski M, Rinehart PM. Implementing transitions for youth with complex chronic conditions using the medical home model. Pediatrics. 2002;110(6 Pt 2):1322-1327.
10. Goodman DM, Hall M, Levin A, et al. Adults with chronic health conditions originating in childhood: inpatient experience in children’s hospitals. Pediatrics. 2011;128(1):5-13. doi:10.1542/peds.2010-2037.
11. Coller RJ, Ahrens S, Ehlenbach M, et al. Transitioning from General Pediatric to Adult-Oriented Inpatient Care: National Survey of US Children’s Hospitals. J Hosp Med. 2018;13(1):13-20.
12. Olson D. Health Care Transitions for Young People. In Field MJ, Jette AM, Institute of Medicine (US) Committee on Disability in America, editors. The Future of Disability in America. Washington, DC: National Academy Press; 2007. https://www.ncbi.nlm.nih.gov/books/NBK11432/.
13. GotTransition.org. http://www.gottransition.org/. Accessed September 15, 2017.
14. Okumura MJ, Kerr EA, Cabana MD, Davis MM, Demonner S, Heisler M. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics. 2010;125(4):e748-754. doi:10.1542/peds.2008-3451.
1. Elborn JS, Shale DJ, Britton JR. Cystic fibrosis: current survival and population estimates to the year 2000. Thorax. 1991;46(12):881-885.
2. Reid GJ, Webb GD, Barzel M, McCrindle BW, Irvine MJ, Siu SC. Estimates of life expectancy by adolescents and young adults with congenital heart disease. J Am Coll Cardiol. 2006;48(2):349-355. doi:10.1016/j.jacc.2006.03.041.
3. Ferris ME, Gipson DS, Kimmel PL, Eggers PW. Trends in treatment and outcomes of survival of adolescents initiating end-stage renal disease care in the United States of America. Pediatr Nephrol. 2006;21(7):1020-1026. doi:10.1007/s00467-006-0059-9.
4. Sharma N, O’Hare K, Antonelli RC, Sawicki GS. Transition care: future directions in education, health policy, and outcomes research. Acad Pediatr. 2014;14(2):120-127. doi:10.1016/j.acap.2013.11.007.
5. Harden PN, Walsh G, Bandler N, et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ. 2012;344:e3718. doi:10.1136/bmj.e3718.
6. Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol. 2000;14(6):469-472.
7. Lotstein DS, Seid M, Klingensmith G, et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131(4):e1062-1070. doi:10.1542/peds.2012-1450.
8. Scal P. Transition for youth with chronic conditions: primary care physicians’ approaches. Pediatrics. 2002;110(6 Pt 2):1315-1321.
9. Kelly AM, Kratz B, Bielski M, Rinehart PM. Implementing transitions for youth with complex chronic conditions using the medical home model. Pediatrics. 2002;110(6 Pt 2):1322-1327.
10. Goodman DM, Hall M, Levin A, et al. Adults with chronic health conditions originating in childhood: inpatient experience in children’s hospitals. Pediatrics. 2011;128(1):5-13. doi:10.1542/peds.2010-2037.
11. Coller RJ, Ahrens S, Ehlenbach M, et al. Transitioning from General Pediatric to Adult-Oriented Inpatient Care: National Survey of US Children’s Hospitals. J Hosp Med. 2018;13(1):13-20.
12. Olson D. Health Care Transitions for Young People. In Field MJ, Jette AM, Institute of Medicine (US) Committee on Disability in America, editors. The Future of Disability in America. Washington, DC: National Academy Press; 2007. https://www.ncbi.nlm.nih.gov/books/NBK11432/.
13. GotTransition.org. http://www.gottransition.org/. Accessed September 15, 2017.
14. Okumura MJ, Kerr EA, Cabana MD, Davis MM, Demonner S, Heisler M. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics. 2010;125(4):e748-754. doi:10.1542/peds.2008-3451.
© 2018 Society of Hospital Medicine
Eye of the Storm
Editors’ note: When a disaster strikes—whether manmade or natural—we are wrenched from our normal existence into another realm entirely. The petty concerns of daily life fade from sight in the wake of destruction and death.
For the practitioner of medicine, this is a time of great challenge to demonstrate the highest ideals of medicine. The people of the Gulf Coast must now face a dawn where the life they knew is gone and must be built anew. In this issue we’re proud to include the memoirs of two New Orleans physicians who worked through this catastrophe.
For more information on how you can help with the recovery effort, visit www.hospitalmedicine.org.
Despite the best preparations and planning, many aspects of managing a physician practice change rapidly, and many new problems arise immediately following a disaster. Below, we present our experiences as a large hospitalist program in a tertiary-care referral center during the days before and the seven days after Hurricane Katrina, a category IV storm, devastated New Orleans.
PREPARATION
Ochsner Clinic Foundation (OCF) is an integrated medical institution with more than 700 physicians and 24 clinics throughout Southeast Louisiana, including Northshore and Baton Rouge. For nearly 60 years, Ochsner has cared for residents in the greater New Orleans communities at the Ochsner Main Campus, which includes a multispecialty clinic, a 500-bed hospital, and residency training programs. The Main Campus is located by the Mississippi River at the parish line between Orleans Parish and Jefferson Parish—areas protected from flooding under the levee system.
The Hospitalist Program at the Ochsner Main Campus has 18 physicians and four nurse practitioners. Approximately 60% of our patients are managed by Internal Medicine Residency teaching services and the rest by staff physicians. Prior to the landing of Hurricane Katrina, we cared for 60% of the hospitalized patients. Our past hurricane experience led us to develop a two-team system for disasters. Team A has four hospitalists who are required to stay on campus;
Team B is available within a week later to relieve Team A.
We tracked Hurricane Katrina following its exit from the Florida area. The decision analysis for our essential medical team was based on the category of the hurricane, staff location, and projected path. On Saturday, August 27, we were informed that Hurricane Katrina was reaching category V status and expected to hit New Orleans early Monday morning. This unexpected arrival required us to mobilize the hurricane emergency preparedness team rapidly. Hence both teams A and B were requested to remain on premise—preferably without family and pets. On the facility side, we had four generators on site and started to request other generators from around the country on the news of changing course of the hurricane.
SUNDAY, AUGUST 28:
The Day before Katrina Landed
New Orleans Mayor Ray Nagin ordered a mandatory evacuation of the city for the first time in history. At Ochsner, all essential personnel were expected to report to their stations by 7 p.m. The arrival of the hurricane gave little time to our staff to arrange alternative living arrangements for their significant others and pets. Consequently many non-medical dependents and pets arrived at the facility even though we didn’t have adequate supplies to be self-sufficient for more than a few days. Many expected our organization to have ample resources to accommodate all needs—food, shelter, and support. A hurricane disaster phone line was created to update the status of OCF following the hurricane.
MONDAY, AUGUST 29:
Katrina Lands in New Orleans
OCF lost power in the early morning of August 29. Our facility sustained water and roof damage on the top floors of the hospital and unexpected ceiling glass breaks in the walkways. The howling of the intense wind created an ominous feeling among all of those sheltered in the facility. Fortunately, only minor flooding occurred around the institution.
In contrast, major flooding was reported throughout metropolitan New Orleans—especially in New Orleans East and surrounding low-lying parishes. Major wind damage was seen in buildings in the central business district, and 100% of the power was out in that area.
Downtown New Orleans and the French Quarter were dry thanks to the pumping system. Disturbingly, though, breaches in the levee system protecting New Orleans were reported in the 17th Street Canal.
By Monday afternoon, our entire facility was running on emergency generators, which provided energy only for essential equipment and left the institution with no air-conditioning, minimal lighting, and no plumbing. Physicians used flashlights to see patients, and the rooms became unbearably hot and humid; the heat index outside was 105 degrees Fahrenheit.
All regular communications went off service, including telephone lines, cell phones, and outside pagers. Fortunately OCF had invested in Spectralink phones in the past few years; this internal, antenna-based phone system continued to function. We were even able to dial long-distance intermittently. Our information system also went down, but we kept generator power for intermittent use of the Internet and Intranet to allow our employees to access information and contact with the outside world. At night—from the towers of our hospital—it was strange to see our former city of lights in total darkness.
TUESDAY, AUGUST 30:
Hurricane Aftermath Day 1
Reports of catastrophic flooding and heroic rooftop rescues in New Orleans East and other parishes were announced on the radio and via the Internet. Unfortunately the levee breach at the 17th Street Canal became uncontrolled, and water began flowing from Lake Pontchartrain into New Orleans, ultimately flooding 80% of the city of New Orleans. The Superdome and the Convention Center began to fill with thousands of refugees.
The lack of electricity, inadequate food and water supplies, overcrowding, lack of adequate sanitary conditions, and—later—security concerns exponentially created a humanitarian crisis. We were devastated by the plight of our fellow New Orleans residents, whose only crime was, largely, being too poor to evacuate. Approximately 300,000 people never evacuated, and this posed an interminable challenge for city, state, and federal governments. Unfortunately the acts of a few heartless gangs tarnished the beautiful and friendly image of the Big Easy.
At Ochsner we began to conserve our resources because of the commitment to care for more than 500 people onsite. Our dietary department provided approximately 1,600 meals daily, working in hot and sweaty conditions. In the hospital the heat began to take a physical toll on everyone. We also suffered the psychological toll of not knowing what had happened to our families, friends, and belongings. We lost the ability to run most laboratory studies. We concentrated our efforts in preserving human lives with only basic means.
With no working elevators, navigating 11 floors of the hospital was a challenge for all. Our survival tactics included not just adequate fluid hydration, but electrolyte replacement. Unexpectedly, we discovered that OCF had invested in a deep-well water system separate
from the county water supply in the hospital. Thus the hospital continued to have water for at least the first three floors. The cool well water provided much-needed refreshing showers and maintained adequate sanitary conditions.
One of our hospitalists evacuated from OCF (along with several of our team’s family members) to Houston. On their way, they passed downed power-lines, a daiquiri shop in flames, and cars carrying boats on their roofs into New Orleans to help rescue stranded people.
WEDNESDAY, AUGUST 31:
Hurricane Aftermath Day 2
Conditions in downtown New Orleans became increasing dire with rising floodwater, hunger, thirst, and reports of looting and unrest. Rumors started to spread about the status and safety of OCF. One stated that OCF had looted a nearby Wal-Mart for food and supplies even though, in fact, senior executives of Wal-Mart personally inventoried the items and generously donated them to our institution.
There were also rumors about looters approaching from downtown. Family members outside the city were urging our employees to leave because of the danger of continued flooding and civil unrest. OCF administrators (under the leadership of the CEO Patrick Quinlan, MD, President and COO Warner Thomas, MD, and Medical Director Richard Guthrie, MD) actively addressed these issues to stop the rumors with scheduled and mandatory open forums. During the next few days, OCF was in a lock-down mode with the National Guard and our own security department providing security.
Not knowing the capability of our facility in this time of extreme uncertainly, we proceeded to discharge and move patients to other centers, such as Memorial Hermann Hospital in Houston and Summit Hospital in Baton Rouge via both helicopter and ambulance.
Simultaneously we focused on patients who were stable and ready for discharge to increase our organization capacity to create a plan for providing resource for both the east and west banks of the Mississippi River.
THURSDAY, SEPTEMBER 1:
Hurricane Aftermath Day 3
With the city of New Orleans under marshal law, OCF continued in lock-down mode. During the aftermath, a high priority was to contact all the evacuated employees. An employee outreach program was implemented in which each department accounted for the whereabouts of all personnel. As for our hospitalist program, we started to meet twice daily immediately after the hurricane to address concerns of emergency department volumes, maintain open communications, provide mutual psychological support, and foster a spirit of teamwork. During these meetings we believed that our department had cemented a bond that could not be created in normal circumstances. Our efforts through the storm and the unimaginable adversity were nothing short of extraordinary.
Our medical colleagues in Charity Hospital in downtown New Orleans faced unprecedented challenges caring for patients with minimal supplies. We heard reports of doctors giving each other IV hydration and medical personnel bagging ventilator patients in shifts. With no communication except the Internet, they resorted to e-mailing CNN for help.
FRIDAY, SEPTEMBER 2:
Hurricane Aftermath Day 4
President Bush arrived to visit New Orleans and other devastated areas in the Gulf region. With the National Guard moving in to provide security and relief efforts, Mayor Nagin declared the day a turning point for the city. After the hurricane, it was uncertain how many patients would require medical care in the community. From the Hurricane Ivan experience in Pensacola, Fla., we were advised that 10 days after the disaster, one could anticipate a doubling of the highest emergency department volume for several weeks.
We were uncertain that the evacuation of the whole city could provide such volume. To offer quality clinical care and remain in sound mind under such conditions, we hospitalists unanimously agreed to care for our patients 24/7 in weekly rotation. Our hospital census during this period was at 60% of usual and the admission was running at 40% of normal. We decreased the residents from three members per team to two in order to provide a five-day rotation of three teams. We utilized the staging center of Ochsner Baton Rouge to organize our employees and provide transportation to and from New Orleans. Employees were discouraged from driving in
their own vehicles due to gasoline shortage and safety concerns.
SATURDAY, SEPTEMBER 3:
Hurricane Aftermath Day 5
Conditions in New Orleans improved rapidly with better security. Evacuees were steadily transported out of the Superdome and Convention Center. Hurricane Katrina disasters posed new challenges in providing care. We saw patients with
- Severe dehydration;
- Exhaustion caused by the lack of use or incorrect use of their medications for days resulting in exacerbation of chronic conditions such as COPD;
- Water-borne illnesses from prolonged immersion in toxic water;
- Reactive airway diseases from environmental allergens;
- Cellulitis from cuts and bruises in evacuees, as well as people attempting home repairs;
- Carbon monoxide poisoning from generators used incorrectly inside homes; and
- Withdrawals from illicit drug uses.
SUNDAY, SEPTEMBER 4:
Hurricane Aftermath Day 6
During the Sunday ad-hoc church service at Ochsner, doctors, nurses, employees, patients, and families came together in spiritual healing. We sang praises of hope and optimism for our community. We were grateful for our status in this unbelievable disaster and offered prayers and hope for those who had lost so much. We had never been so proud of the efforts of every individual in our institution for maintaining this facility for patient care in such dire situations and promised to be optimistic about our future.
Fortunately, with the help of the Jefferson Parish emergency utility crews, power was restored to our institution. We became fully functional to take on the challenges of the community.
MONDAY, SEPTEMBER 5:
Hurricane Aftermath Day 7
The 17th Street Canal breach was controlled and the water pump back in operation. Residents of Jefferson Parish were allowed to return to take their personal items from their houses but were still under voluntary evacuation, while Orleans Parish was still closed. To plan the demand for medical care in the wake of gradual recovery, OCF began to maintain all of our employees through strategic deployments in various satellite clinics and hospitals according to the needs of the population in New Orleans and other areas.
LESSONS LEARNED
We have learned so much from this disaster. The key to overcome such adverse conditions entails strong psychosocial support from colleagues and family. Strong leadership is crucial to maintain a sense of serenity and an optimistic outlook in times of uncertainty. We experienced a sense of camaraderie after seeing all medical personnel participating in activities beyond of the boundary of usual roles.
The expansion of the essential personnel team list to include social workers and discharge planners is crucial to focus on the unique and nonconventional logistical challenges post-disaster. Intense focus on group dynamics was essential to avoid physical and emotional burnout. Frequent and predictably scheduled face-to-face communication was also important in disseminating accurate, unadulterated information because our decision-making changed hour-to-hour immediately after Hurricane Katrina, day-to-day in the few days afterward, and week-to-week just one week post-disaster.
Obviously the financial implications are immense for our city and our institution. We are developing financial plans, a relief fund, and other resources to assist our employees who have been severely affected by the hurricane. TH
Dr. Deitelzweig and Dr. Lee work at the Ochsner Clinic Foundation, Department of Hospital-Based Internal Medicine, New Orleans. You can contact Dr. Deitelzweig by phone at (504) 842-5766; his e-mail is [email protected]
Editors’ note: When a disaster strikes—whether manmade or natural—we are wrenched from our normal existence into another realm entirely. The petty concerns of daily life fade from sight in the wake of destruction and death.
For the practitioner of medicine, this is a time of great challenge to demonstrate the highest ideals of medicine. The people of the Gulf Coast must now face a dawn where the life they knew is gone and must be built anew. In this issue we’re proud to include the memoirs of two New Orleans physicians who worked through this catastrophe.
For more information on how you can help with the recovery effort, visit www.hospitalmedicine.org.
Despite the best preparations and planning, many aspects of managing a physician practice change rapidly, and many new problems arise immediately following a disaster. Below, we present our experiences as a large hospitalist program in a tertiary-care referral center during the days before and the seven days after Hurricane Katrina, a category IV storm, devastated New Orleans.
PREPARATION
Ochsner Clinic Foundation (OCF) is an integrated medical institution with more than 700 physicians and 24 clinics throughout Southeast Louisiana, including Northshore and Baton Rouge. For nearly 60 years, Ochsner has cared for residents in the greater New Orleans communities at the Ochsner Main Campus, which includes a multispecialty clinic, a 500-bed hospital, and residency training programs. The Main Campus is located by the Mississippi River at the parish line between Orleans Parish and Jefferson Parish—areas protected from flooding under the levee system.
The Hospitalist Program at the Ochsner Main Campus has 18 physicians and four nurse practitioners. Approximately 60% of our patients are managed by Internal Medicine Residency teaching services and the rest by staff physicians. Prior to the landing of Hurricane Katrina, we cared for 60% of the hospitalized patients. Our past hurricane experience led us to develop a two-team system for disasters. Team A has four hospitalists who are required to stay on campus;
Team B is available within a week later to relieve Team A.
We tracked Hurricane Katrina following its exit from the Florida area. The decision analysis for our essential medical team was based on the category of the hurricane, staff location, and projected path. On Saturday, August 27, we were informed that Hurricane Katrina was reaching category V status and expected to hit New Orleans early Monday morning. This unexpected arrival required us to mobilize the hurricane emergency preparedness team rapidly. Hence both teams A and B were requested to remain on premise—preferably without family and pets. On the facility side, we had four generators on site and started to request other generators from around the country on the news of changing course of the hurricane.
SUNDAY, AUGUST 28:
The Day before Katrina Landed
New Orleans Mayor Ray Nagin ordered a mandatory evacuation of the city for the first time in history. At Ochsner, all essential personnel were expected to report to their stations by 7 p.m. The arrival of the hurricane gave little time to our staff to arrange alternative living arrangements for their significant others and pets. Consequently many non-medical dependents and pets arrived at the facility even though we didn’t have adequate supplies to be self-sufficient for more than a few days. Many expected our organization to have ample resources to accommodate all needs—food, shelter, and support. A hurricane disaster phone line was created to update the status of OCF following the hurricane.
MONDAY, AUGUST 29:
Katrina Lands in New Orleans
OCF lost power in the early morning of August 29. Our facility sustained water and roof damage on the top floors of the hospital and unexpected ceiling glass breaks in the walkways. The howling of the intense wind created an ominous feeling among all of those sheltered in the facility. Fortunately, only minor flooding occurred around the institution.
In contrast, major flooding was reported throughout metropolitan New Orleans—especially in New Orleans East and surrounding low-lying parishes. Major wind damage was seen in buildings in the central business district, and 100% of the power was out in that area.
Downtown New Orleans and the French Quarter were dry thanks to the pumping system. Disturbingly, though, breaches in the levee system protecting New Orleans were reported in the 17th Street Canal.
By Monday afternoon, our entire facility was running on emergency generators, which provided energy only for essential equipment and left the institution with no air-conditioning, minimal lighting, and no plumbing. Physicians used flashlights to see patients, and the rooms became unbearably hot and humid; the heat index outside was 105 degrees Fahrenheit.
All regular communications went off service, including telephone lines, cell phones, and outside pagers. Fortunately OCF had invested in Spectralink phones in the past few years; this internal, antenna-based phone system continued to function. We were even able to dial long-distance intermittently. Our information system also went down, but we kept generator power for intermittent use of the Internet and Intranet to allow our employees to access information and contact with the outside world. At night—from the towers of our hospital—it was strange to see our former city of lights in total darkness.
TUESDAY, AUGUST 30:
Hurricane Aftermath Day 1
Reports of catastrophic flooding and heroic rooftop rescues in New Orleans East and other parishes were announced on the radio and via the Internet. Unfortunately the levee breach at the 17th Street Canal became uncontrolled, and water began flowing from Lake Pontchartrain into New Orleans, ultimately flooding 80% of the city of New Orleans. The Superdome and the Convention Center began to fill with thousands of refugees.
The lack of electricity, inadequate food and water supplies, overcrowding, lack of adequate sanitary conditions, and—later—security concerns exponentially created a humanitarian crisis. We were devastated by the plight of our fellow New Orleans residents, whose only crime was, largely, being too poor to evacuate. Approximately 300,000 people never evacuated, and this posed an interminable challenge for city, state, and federal governments. Unfortunately the acts of a few heartless gangs tarnished the beautiful and friendly image of the Big Easy.
At Ochsner we began to conserve our resources because of the commitment to care for more than 500 people onsite. Our dietary department provided approximately 1,600 meals daily, working in hot and sweaty conditions. In the hospital the heat began to take a physical toll on everyone. We also suffered the psychological toll of not knowing what had happened to our families, friends, and belongings. We lost the ability to run most laboratory studies. We concentrated our efforts in preserving human lives with only basic means.
With no working elevators, navigating 11 floors of the hospital was a challenge for all. Our survival tactics included not just adequate fluid hydration, but electrolyte replacement. Unexpectedly, we discovered that OCF had invested in a deep-well water system separate
from the county water supply in the hospital. Thus the hospital continued to have water for at least the first three floors. The cool well water provided much-needed refreshing showers and maintained adequate sanitary conditions.
One of our hospitalists evacuated from OCF (along with several of our team’s family members) to Houston. On their way, they passed downed power-lines, a daiquiri shop in flames, and cars carrying boats on their roofs into New Orleans to help rescue stranded people.
WEDNESDAY, AUGUST 31:
Hurricane Aftermath Day 2
Conditions in downtown New Orleans became increasing dire with rising floodwater, hunger, thirst, and reports of looting and unrest. Rumors started to spread about the status and safety of OCF. One stated that OCF had looted a nearby Wal-Mart for food and supplies even though, in fact, senior executives of Wal-Mart personally inventoried the items and generously donated them to our institution.
There were also rumors about looters approaching from downtown. Family members outside the city were urging our employees to leave because of the danger of continued flooding and civil unrest. OCF administrators (under the leadership of the CEO Patrick Quinlan, MD, President and COO Warner Thomas, MD, and Medical Director Richard Guthrie, MD) actively addressed these issues to stop the rumors with scheduled and mandatory open forums. During the next few days, OCF was in a lock-down mode with the National Guard and our own security department providing security.
Not knowing the capability of our facility in this time of extreme uncertainly, we proceeded to discharge and move patients to other centers, such as Memorial Hermann Hospital in Houston and Summit Hospital in Baton Rouge via both helicopter and ambulance.
Simultaneously we focused on patients who were stable and ready for discharge to increase our organization capacity to create a plan for providing resource for both the east and west banks of the Mississippi River.
THURSDAY, SEPTEMBER 1:
Hurricane Aftermath Day 3
With the city of New Orleans under marshal law, OCF continued in lock-down mode. During the aftermath, a high priority was to contact all the evacuated employees. An employee outreach program was implemented in which each department accounted for the whereabouts of all personnel. As for our hospitalist program, we started to meet twice daily immediately after the hurricane to address concerns of emergency department volumes, maintain open communications, provide mutual psychological support, and foster a spirit of teamwork. During these meetings we believed that our department had cemented a bond that could not be created in normal circumstances. Our efforts through the storm and the unimaginable adversity were nothing short of extraordinary.
Our medical colleagues in Charity Hospital in downtown New Orleans faced unprecedented challenges caring for patients with minimal supplies. We heard reports of doctors giving each other IV hydration and medical personnel bagging ventilator patients in shifts. With no communication except the Internet, they resorted to e-mailing CNN for help.
FRIDAY, SEPTEMBER 2:
Hurricane Aftermath Day 4
President Bush arrived to visit New Orleans and other devastated areas in the Gulf region. With the National Guard moving in to provide security and relief efforts, Mayor Nagin declared the day a turning point for the city. After the hurricane, it was uncertain how many patients would require medical care in the community. From the Hurricane Ivan experience in Pensacola, Fla., we were advised that 10 days after the disaster, one could anticipate a doubling of the highest emergency department volume for several weeks.
We were uncertain that the evacuation of the whole city could provide such volume. To offer quality clinical care and remain in sound mind under such conditions, we hospitalists unanimously agreed to care for our patients 24/7 in weekly rotation. Our hospital census during this period was at 60% of usual and the admission was running at 40% of normal. We decreased the residents from three members per team to two in order to provide a five-day rotation of three teams. We utilized the staging center of Ochsner Baton Rouge to organize our employees and provide transportation to and from New Orleans. Employees were discouraged from driving in
their own vehicles due to gasoline shortage and safety concerns.
SATURDAY, SEPTEMBER 3:
Hurricane Aftermath Day 5
Conditions in New Orleans improved rapidly with better security. Evacuees were steadily transported out of the Superdome and Convention Center. Hurricane Katrina disasters posed new challenges in providing care. We saw patients with
- Severe dehydration;
- Exhaustion caused by the lack of use or incorrect use of their medications for days resulting in exacerbation of chronic conditions such as COPD;
- Water-borne illnesses from prolonged immersion in toxic water;
- Reactive airway diseases from environmental allergens;
- Cellulitis from cuts and bruises in evacuees, as well as people attempting home repairs;
- Carbon monoxide poisoning from generators used incorrectly inside homes; and
- Withdrawals from illicit drug uses.
SUNDAY, SEPTEMBER 4:
Hurricane Aftermath Day 6
During the Sunday ad-hoc church service at Ochsner, doctors, nurses, employees, patients, and families came together in spiritual healing. We sang praises of hope and optimism for our community. We were grateful for our status in this unbelievable disaster and offered prayers and hope for those who had lost so much. We had never been so proud of the efforts of every individual in our institution for maintaining this facility for patient care in such dire situations and promised to be optimistic about our future.
Fortunately, with the help of the Jefferson Parish emergency utility crews, power was restored to our institution. We became fully functional to take on the challenges of the community.
MONDAY, SEPTEMBER 5:
Hurricane Aftermath Day 7
The 17th Street Canal breach was controlled and the water pump back in operation. Residents of Jefferson Parish were allowed to return to take their personal items from their houses but were still under voluntary evacuation, while Orleans Parish was still closed. To plan the demand for medical care in the wake of gradual recovery, OCF began to maintain all of our employees through strategic deployments in various satellite clinics and hospitals according to the needs of the population in New Orleans and other areas.
LESSONS LEARNED
We have learned so much from this disaster. The key to overcome such adverse conditions entails strong psychosocial support from colleagues and family. Strong leadership is crucial to maintain a sense of serenity and an optimistic outlook in times of uncertainty. We experienced a sense of camaraderie after seeing all medical personnel participating in activities beyond of the boundary of usual roles.
The expansion of the essential personnel team list to include social workers and discharge planners is crucial to focus on the unique and nonconventional logistical challenges post-disaster. Intense focus on group dynamics was essential to avoid physical and emotional burnout. Frequent and predictably scheduled face-to-face communication was also important in disseminating accurate, unadulterated information because our decision-making changed hour-to-hour immediately after Hurricane Katrina, day-to-day in the few days afterward, and week-to-week just one week post-disaster.
Obviously the financial implications are immense for our city and our institution. We are developing financial plans, a relief fund, and other resources to assist our employees who have been severely affected by the hurricane. TH
Dr. Deitelzweig and Dr. Lee work at the Ochsner Clinic Foundation, Department of Hospital-Based Internal Medicine, New Orleans. You can contact Dr. Deitelzweig by phone at (504) 842-5766; his e-mail is [email protected]
Editors’ note: When a disaster strikes—whether manmade or natural—we are wrenched from our normal existence into another realm entirely. The petty concerns of daily life fade from sight in the wake of destruction and death.
For the practitioner of medicine, this is a time of great challenge to demonstrate the highest ideals of medicine. The people of the Gulf Coast must now face a dawn where the life they knew is gone and must be built anew. In this issue we’re proud to include the memoirs of two New Orleans physicians who worked through this catastrophe.
For more information on how you can help with the recovery effort, visit www.hospitalmedicine.org.
Despite the best preparations and planning, many aspects of managing a physician practice change rapidly, and many new problems arise immediately following a disaster. Below, we present our experiences as a large hospitalist program in a tertiary-care referral center during the days before and the seven days after Hurricane Katrina, a category IV storm, devastated New Orleans.
PREPARATION
Ochsner Clinic Foundation (OCF) is an integrated medical institution with more than 700 physicians and 24 clinics throughout Southeast Louisiana, including Northshore and Baton Rouge. For nearly 60 years, Ochsner has cared for residents in the greater New Orleans communities at the Ochsner Main Campus, which includes a multispecialty clinic, a 500-bed hospital, and residency training programs. The Main Campus is located by the Mississippi River at the parish line between Orleans Parish and Jefferson Parish—areas protected from flooding under the levee system.
The Hospitalist Program at the Ochsner Main Campus has 18 physicians and four nurse practitioners. Approximately 60% of our patients are managed by Internal Medicine Residency teaching services and the rest by staff physicians. Prior to the landing of Hurricane Katrina, we cared for 60% of the hospitalized patients. Our past hurricane experience led us to develop a two-team system for disasters. Team A has four hospitalists who are required to stay on campus;
Team B is available within a week later to relieve Team A.
We tracked Hurricane Katrina following its exit from the Florida area. The decision analysis for our essential medical team was based on the category of the hurricane, staff location, and projected path. On Saturday, August 27, we were informed that Hurricane Katrina was reaching category V status and expected to hit New Orleans early Monday morning. This unexpected arrival required us to mobilize the hurricane emergency preparedness team rapidly. Hence both teams A and B were requested to remain on premise—preferably without family and pets. On the facility side, we had four generators on site and started to request other generators from around the country on the news of changing course of the hurricane.
SUNDAY, AUGUST 28:
The Day before Katrina Landed
New Orleans Mayor Ray Nagin ordered a mandatory evacuation of the city for the first time in history. At Ochsner, all essential personnel were expected to report to their stations by 7 p.m. The arrival of the hurricane gave little time to our staff to arrange alternative living arrangements for their significant others and pets. Consequently many non-medical dependents and pets arrived at the facility even though we didn’t have adequate supplies to be self-sufficient for more than a few days. Many expected our organization to have ample resources to accommodate all needs—food, shelter, and support. A hurricane disaster phone line was created to update the status of OCF following the hurricane.
MONDAY, AUGUST 29:
Katrina Lands in New Orleans
OCF lost power in the early morning of August 29. Our facility sustained water and roof damage on the top floors of the hospital and unexpected ceiling glass breaks in the walkways. The howling of the intense wind created an ominous feeling among all of those sheltered in the facility. Fortunately, only minor flooding occurred around the institution.
In contrast, major flooding was reported throughout metropolitan New Orleans—especially in New Orleans East and surrounding low-lying parishes. Major wind damage was seen in buildings in the central business district, and 100% of the power was out in that area.
Downtown New Orleans and the French Quarter were dry thanks to the pumping system. Disturbingly, though, breaches in the levee system protecting New Orleans were reported in the 17th Street Canal.
By Monday afternoon, our entire facility was running on emergency generators, which provided energy only for essential equipment and left the institution with no air-conditioning, minimal lighting, and no plumbing. Physicians used flashlights to see patients, and the rooms became unbearably hot and humid; the heat index outside was 105 degrees Fahrenheit.
All regular communications went off service, including telephone lines, cell phones, and outside pagers. Fortunately OCF had invested in Spectralink phones in the past few years; this internal, antenna-based phone system continued to function. We were even able to dial long-distance intermittently. Our information system also went down, but we kept generator power for intermittent use of the Internet and Intranet to allow our employees to access information and contact with the outside world. At night—from the towers of our hospital—it was strange to see our former city of lights in total darkness.
TUESDAY, AUGUST 30:
Hurricane Aftermath Day 1
Reports of catastrophic flooding and heroic rooftop rescues in New Orleans East and other parishes were announced on the radio and via the Internet. Unfortunately the levee breach at the 17th Street Canal became uncontrolled, and water began flowing from Lake Pontchartrain into New Orleans, ultimately flooding 80% of the city of New Orleans. The Superdome and the Convention Center began to fill with thousands of refugees.
The lack of electricity, inadequate food and water supplies, overcrowding, lack of adequate sanitary conditions, and—later—security concerns exponentially created a humanitarian crisis. We were devastated by the plight of our fellow New Orleans residents, whose only crime was, largely, being too poor to evacuate. Approximately 300,000 people never evacuated, and this posed an interminable challenge for city, state, and federal governments. Unfortunately the acts of a few heartless gangs tarnished the beautiful and friendly image of the Big Easy.
At Ochsner we began to conserve our resources because of the commitment to care for more than 500 people onsite. Our dietary department provided approximately 1,600 meals daily, working in hot and sweaty conditions. In the hospital the heat began to take a physical toll on everyone. We also suffered the psychological toll of not knowing what had happened to our families, friends, and belongings. We lost the ability to run most laboratory studies. We concentrated our efforts in preserving human lives with only basic means.
With no working elevators, navigating 11 floors of the hospital was a challenge for all. Our survival tactics included not just adequate fluid hydration, but electrolyte replacement. Unexpectedly, we discovered that OCF had invested in a deep-well water system separate
from the county water supply in the hospital. Thus the hospital continued to have water for at least the first three floors. The cool well water provided much-needed refreshing showers and maintained adequate sanitary conditions.
One of our hospitalists evacuated from OCF (along with several of our team’s family members) to Houston. On their way, they passed downed power-lines, a daiquiri shop in flames, and cars carrying boats on their roofs into New Orleans to help rescue stranded people.
WEDNESDAY, AUGUST 31:
Hurricane Aftermath Day 2
Conditions in downtown New Orleans became increasing dire with rising floodwater, hunger, thirst, and reports of looting and unrest. Rumors started to spread about the status and safety of OCF. One stated that OCF had looted a nearby Wal-Mart for food and supplies even though, in fact, senior executives of Wal-Mart personally inventoried the items and generously donated them to our institution.
There were also rumors about looters approaching from downtown. Family members outside the city were urging our employees to leave because of the danger of continued flooding and civil unrest. OCF administrators (under the leadership of the CEO Patrick Quinlan, MD, President and COO Warner Thomas, MD, and Medical Director Richard Guthrie, MD) actively addressed these issues to stop the rumors with scheduled and mandatory open forums. During the next few days, OCF was in a lock-down mode with the National Guard and our own security department providing security.
Not knowing the capability of our facility in this time of extreme uncertainly, we proceeded to discharge and move patients to other centers, such as Memorial Hermann Hospital in Houston and Summit Hospital in Baton Rouge via both helicopter and ambulance.
Simultaneously we focused on patients who were stable and ready for discharge to increase our organization capacity to create a plan for providing resource for both the east and west banks of the Mississippi River.
THURSDAY, SEPTEMBER 1:
Hurricane Aftermath Day 3
With the city of New Orleans under marshal law, OCF continued in lock-down mode. During the aftermath, a high priority was to contact all the evacuated employees. An employee outreach program was implemented in which each department accounted for the whereabouts of all personnel. As for our hospitalist program, we started to meet twice daily immediately after the hurricane to address concerns of emergency department volumes, maintain open communications, provide mutual psychological support, and foster a spirit of teamwork. During these meetings we believed that our department had cemented a bond that could not be created in normal circumstances. Our efforts through the storm and the unimaginable adversity were nothing short of extraordinary.
Our medical colleagues in Charity Hospital in downtown New Orleans faced unprecedented challenges caring for patients with minimal supplies. We heard reports of doctors giving each other IV hydration and medical personnel bagging ventilator patients in shifts. With no communication except the Internet, they resorted to e-mailing CNN for help.
FRIDAY, SEPTEMBER 2:
Hurricane Aftermath Day 4
President Bush arrived to visit New Orleans and other devastated areas in the Gulf region. With the National Guard moving in to provide security and relief efforts, Mayor Nagin declared the day a turning point for the city. After the hurricane, it was uncertain how many patients would require medical care in the community. From the Hurricane Ivan experience in Pensacola, Fla., we were advised that 10 days after the disaster, one could anticipate a doubling of the highest emergency department volume for several weeks.
We were uncertain that the evacuation of the whole city could provide such volume. To offer quality clinical care and remain in sound mind under such conditions, we hospitalists unanimously agreed to care for our patients 24/7 in weekly rotation. Our hospital census during this period was at 60% of usual and the admission was running at 40% of normal. We decreased the residents from three members per team to two in order to provide a five-day rotation of three teams. We utilized the staging center of Ochsner Baton Rouge to organize our employees and provide transportation to and from New Orleans. Employees were discouraged from driving in
their own vehicles due to gasoline shortage and safety concerns.
SATURDAY, SEPTEMBER 3:
Hurricane Aftermath Day 5
Conditions in New Orleans improved rapidly with better security. Evacuees were steadily transported out of the Superdome and Convention Center. Hurricane Katrina disasters posed new challenges in providing care. We saw patients with
- Severe dehydration;
- Exhaustion caused by the lack of use or incorrect use of their medications for days resulting in exacerbation of chronic conditions such as COPD;
- Water-borne illnesses from prolonged immersion in toxic water;
- Reactive airway diseases from environmental allergens;
- Cellulitis from cuts and bruises in evacuees, as well as people attempting home repairs;
- Carbon monoxide poisoning from generators used incorrectly inside homes; and
- Withdrawals from illicit drug uses.
SUNDAY, SEPTEMBER 4:
Hurricane Aftermath Day 6
During the Sunday ad-hoc church service at Ochsner, doctors, nurses, employees, patients, and families came together in spiritual healing. We sang praises of hope and optimism for our community. We were grateful for our status in this unbelievable disaster and offered prayers and hope for those who had lost so much. We had never been so proud of the efforts of every individual in our institution for maintaining this facility for patient care in such dire situations and promised to be optimistic about our future.
Fortunately, with the help of the Jefferson Parish emergency utility crews, power was restored to our institution. We became fully functional to take on the challenges of the community.
MONDAY, SEPTEMBER 5:
Hurricane Aftermath Day 7
The 17th Street Canal breach was controlled and the water pump back in operation. Residents of Jefferson Parish were allowed to return to take their personal items from their houses but were still under voluntary evacuation, while Orleans Parish was still closed. To plan the demand for medical care in the wake of gradual recovery, OCF began to maintain all of our employees through strategic deployments in various satellite clinics and hospitals according to the needs of the population in New Orleans and other areas.
LESSONS LEARNED
We have learned so much from this disaster. The key to overcome such adverse conditions entails strong psychosocial support from colleagues and family. Strong leadership is crucial to maintain a sense of serenity and an optimistic outlook in times of uncertainty. We experienced a sense of camaraderie after seeing all medical personnel participating in activities beyond of the boundary of usual roles.
The expansion of the essential personnel team list to include social workers and discharge planners is crucial to focus on the unique and nonconventional logistical challenges post-disaster. Intense focus on group dynamics was essential to avoid physical and emotional burnout. Frequent and predictably scheduled face-to-face communication was also important in disseminating accurate, unadulterated information because our decision-making changed hour-to-hour immediately after Hurricane Katrina, day-to-day in the few days afterward, and week-to-week just one week post-disaster.
Obviously the financial implications are immense for our city and our institution. We are developing financial plans, a relief fund, and other resources to assist our employees who have been severely affected by the hurricane. TH
Dr. Deitelzweig and Dr. Lee work at the Ochsner Clinic Foundation, Department of Hospital-Based Internal Medicine, New Orleans. You can contact Dr. Deitelzweig by phone at (504) 842-5766; his e-mail is [email protected]